Canadian Pain Task Force Report: October 2020
(PDF Version, 2.08MB, 75 pages)
Working together to better understand, prevent and, manage chronic pain: What We Heard
Table of contents
- Message from the authors
- Overview
- Executive summary
- Introduction and approach
- Reflecting on inequity, disadvantage, and trauma
- Consultation results
- Reflecting on the impact of the COVID-19 pandemic
- Conclusion and next steps
- Appendix A: Questionnaire demographic results
- Appendix B: Participant experiences
- References
Message from the authors
It is with a sense of urgency that we share this second report on elements of an improved approach to better understand, prevent, and manage chronic pain in Canada. The report reflects the evidence, ideas, stories, and practices that we heard through an extensive national consultation. Our engagement process unfolded in the context of two public health crises, the COVID-19 pandemic and record high numbers of opioid overdose deaths. Both of these crises - and the measures put in place to respond to them - have had tremendous impacts on people who live with pain in Canada. Efforts to address the pandemic and the overdose crisis must take people who live with pain into account.
It has been our privilege to hear from people across Canada through a series of engagement activities to identify best practices and elements of an improved approach to pain care, education, research, and data in Canada.
This report represents the voices of nearly two-thousand people who shared their thoughts and ideas through an extensive series of in-person, written, and online consultations. A heartfelt thank you to everyone who took time to contribute their stories, experience, expertise, and ideas during our consultation process. We are grateful to so many for their continued contribution to the movement for action on chronic pain in Canada - people living with chronic pain, Indigenous Peoples and organizations, Veterans, researchers, health care professionals, non-governmental organizations, and others.
To the people living with chronic pain who so bravely shared their personal experiences and reflections with us, your powerful testaments will facilitate change as we continue to work together to improve the understanding, prevention, and management of chronic pain in Canada.
The Federal-Provincial-Territorial Working Group on Chronic Pain, the Federal Government Interdepartmental Working Group on Pain, and a range of professional and stakeholder organizations across Canada helped with our engagement activities. We are thankful for this and for their continued commitment and collaboration in helping to move this important work forward.
Our deepest appreciation to our External Advisory Panel members for their vital contributions and the wide-ranging expertise they provided to inform this report. Lastly, a very special thank you to the Canadian Pain Task Force Secretariat who support us in our work and who worked tirelessly on the production of this report.
The engagement process not only brought forward best, promising, and emerging practices; it contributed to the mobilization of a network of people who live with, and care about, pain in Canada. We know the next phase of our mandate - continuing to move ideas into action - will be dependent on the sustained engagement of many people and organizations. We look forward to taking what we learned throughout this consultation process and advancing our work - together - to help better understand, prevent, and manage chronic pain for all people living in Canada.
With sincere gratitude,
The Canadian Pain Task Force
Fiona Campbell, Co-Chair
Maria Hudspith, Co-Chair
Manon Choinière
Hani El-Gabalawy
Jacques Laliberté
Michael Sangster
Jaris Swidrovich
Linda Wilhelm
Overview
An estimated 7.63 million, or one in four Canadians aged 15 or older, live with chronic pain - a condition that although often invisible, is now understood as a disease in its own right. It is often interwoven with other chronic conditions and can affect people across their lifetime. Chronic pain has significant impacts on physical and mental health, family and community life, society, and the economy, with the total direct and indirect cost of $38.3 to $40.4 billion in 2019.
Optimal treatment of chronic pain includes physical, psychological, and pharmacological therapies. Recent dramatic increases in opioid-related overdose deaths in North America have heightened awareness around the risks associated with both short- and long-term opioid use for chronic pain. However, efforts undertaken to respond to the overdose crisis have led to challenging unintended consequences for people living with chronic pain. There is now recognition of the importance of addressing pain prevention and management more broadly, not only in the context of action on substance use but also as a parallel public health priority.
Following publication of Chronic Pain in Canada: Laying a Foundation for Action in June 2019, the Canadian Pain Task Force undertook an extensive series of in-person and online consultations with people who either live with and/or care about chronic pain across Canada. The objectives of these consultations were to identify best practices and suggestions for the development of effective strategies to better understand, prevent, and manage chronic pain.
This report reflects the ideas raised during our engagement activities through five interconnected themes:
- Access to timely and patient-centred pain care - We heard from participants that access is impeded by shortages of health care professionals, long wait lists, and financial barriers, particularly for people on low incomes or those without private insurance. Some of the most successful practices for addressing these challenges are patient-oriented models, which provide flexibility to meet an individual's needs and goals, including stepped care and hub-and-spoke service delivery models, rapid access clinics, mobile and evening clinics, virtual care and telemedicine solutions, and self-management resources.
- Awareness, education, and specialized training for pain - People living with pain, health clinicians, and communities need to be empowered, knowledgeable, and supported to manage chronic pain. This starts with an understanding of chronic pain as a legitimate disease, improving public awareness and reducing stigma, and improving the quality and quantity of education for health professionals.
- Pain research and related infrastructure - We heard there is a need to improve our understanding of chronic pain by strengthening and funding pain research. This includes expanding pain research in Canada by establishing an integrated and common understanding of pain and minimum data collection standards, building more collaborative pain research programs, and supporting basic discovery and innovation. It also includes more patient-oriented research on the unique approaches to addressing pain for different populations, including Indigenous Peoples and people living with pain and other co-morbidities.
- Monitoring population health and health system quality - Participants told us we can address current limitations in monitoring pain outcomes and health system quality by developing standards for data collection, expanding surveys and administrative data, and better coordinating actions across jurisdictions.
- Indigenous Peoples - We learned about the negative experiences facing many Indigenous Peoples living with chronic pain when navigating a health system often containing bias and racism and privileging conventional approaches to health and wellness. Future approaches must recognize traditional Indigenous knowledge, medicine, and healing and apply trauma and violence-informed approaches.
Reflecting on inequity, disadvantage, and trauma
As with many chronic illnesses, chronic pain is not distributed equally among Canadians. Biological, psychological, social, cultural, and other factors influence the occurrence and severity of pain, and barriers to care are higher in populations affected by social inequities and discrimination. Trauma and violence-informed care is an essential best practice identified during our consultations, because it promotes compassion and takes into account the patient's experiences, preferences, and possible history of trauma to create an environment of trustworthiness and safety.
Reflecting on the impact of the COVID-19 pandemic
For many people with pre-existing pain conditions, the COVID-19 pandemic has led to stress, mental illness, disability, increased use of medications and substances, and disruptions to continuity of care. Access to services to treat pain and maintain function have been greatly reduced and increased cases of pain are likely to be seen over time. System responses to the pandemic including rapid mobilization of virtual care, centralized and multidisciplinary assessment and intake, stepped care platforms, and enhanced self-management tools and resources will help to improve capacity and pain care. There is an opportunity to leverage the current environment to conduct epidemiological work on post viral complications of COVID-19 and related pain, and to reinforce the importance of taking action on pain, especially during times of increased risk. Such considerations align with the best practices discussed through our consultations and we are hopeful for future action, which will support people living with pain and the health system as a whole.
Executive summary
An estimated 7.63 million, or one in four Canadians aged 15 or older, live with chronic painFootnote 1, a condition now understood as a disease in its own right. Pain experienced by patients is often diminished and misunderstood by health professionals, in part due to its invisibility. It is also often interwoven with other chronic conditions and can affect people across their lifetime. Chronic pain has significant impacts on physical and mental health, family and community life, society and the economy. The total direct and indirect cost of chronic pain totaled $38.3 to $40.4 billion in 2019.
Chronic pain should be understood within a biopsychosocial framework, and its treatment should include physical, psychological, and pharmacological therapies. When prescribed and used as directed by a health professional, opioids can play an important role in pain management for many. However, recent dramatic increases in opioid-related overdose deaths in North America have heightened awareness around the risks associated with both short- and long-term opioid use. A toxic illegal supply of opioids is currently the main factor for drug-related overdose deaths. However, over the last two decades increased availability and use of prescription opioids for both acute and chronic pain has also contributed to this complex public health crisis. The relationship between pain, opioids, and opioid-related harms in Canada is complex and actions taken to mitigate opioid-related harms have had negative unintended consequences for some people who live with pain. Finding solutions to address unmanaged pain, and the trauma and complexity that often accompany it, can be a key means for reducing first exposure to or reliance on opioids and preventing harms associated with substance use more generally.
With this context in mind, the Canadian Pain Task Force was established in March 2019 to help the Government of Canada better understand and address the needs of Canadians who live with chronic pain. The Task Force's first publication - Chronic Pain in Canada: Laying a Foundation for Action released in June 2019, highlighted gaps in access to timely and appropriate multi-modal care, chronic pain surveillance and health system quality monitoring, education, training and awareness for individuals and health care professionals, and research and related infrastructure. Since the publication of that report the Canadian Pain Task Force undertook an extensive series of in-person and online consultations with stakeholders across Canada to listen to people who live with and care about chronic pain. The objectives of these consultations were to identify best practices, and to gather suggestions for the development of effective strategies to better understand, prevent, and manage pain. This report aims to reflect the ideas and perspectives raised during our engagement activities and explores some new themes related to societal inequity and the COVID-19 pandemic.
Reflecting on inequity, disadvantage, and trauma
As with most chronic illnesses, chronic pain is not distributed equally among Canadians. Biological, psychological, social, cultural, and other factors not only influence how we experience pain, but also impact who of us will develop chronic pain in the first place. Occurrence of disease, severity of illness, and barriers to care are higher in populations affected by social inequities and discrimination including people who use drugs, those living in poverty, Indigenous Peoples, certain ethnic communities, and women. These groups are also more often affected by multiple forms of trauma.
Trauma and violence-informed care typically applies key principles, whereby practitioners take into account the patient's experience, preferences, and possible history of trauma including adverse childhood events. Through this approach, practitioners create an environment of trustworthiness and safety, including:
- Understanding trauma and violence and their impacts on peoples' lives and behaviours and how they experience pain;
- Creating emotionally, physically, and culturally safe environments;
- Creating options for choice, collaboration, and connection; and,
- Providing strengths-based and capacity-building approaches to support patient coping and resilience.
Trauma and violence-informed care does not seek to treat trauma, but rather to recognize that it may not only be present but also has an impact on health and well-being, and requires care to be adapted to support patients.
Access to timely and patient-centred pain care
Participants identified many factors contributing to not only the inadequate availability of pain care in communities and primary care across Canada, but also the challenges many face in accessing speciality pain services where they do exist. These include a shortage of family physicians, as well as primary care professionals' lack of knowledge about pain and the full range of treatments or services that could benefit people living with pain. Long wait lists for specialized chronic pain programs further delay the assessment of people living with chronic pain and the start of effective treatments early in the journey. Combined with a health system structure favouring acute over chronic care, it is often easier for patients to be prescribed pharmacological treatments, including opioids, even if these interventions are not the most evidence based treatment for their individual situation.
There is widespread agreement that many people living with pain and their families, particularly those on low incomes or those without private insurance, face considerable financial barriers to accessing pain management, including significant out-of-pocket expenses and lost income when attending specialized treatment and therapies. To address these challenges, innovative approaches to improve access to pain care are being taken, many of which could be adapted and implemented in other jurisdictions across Canada. Some of the most successful are patient-centred models, which provide maximum flexibility to an individual's needs and goals. Stepped care and hub-and-spoke service delivery models provide high volume, low-intensity resources in communities, progressing up to more specialized services taking into account individual needs, preferences, goals, and readiness for treatment. Rapid access clinics speed up the delivery of non-surgical options for treatment (e.g., manual therapy, use of medical devices), while mobile and evening clinics allow patients to access pain care closer to where they live and outside of usual business hours. Virtual care clinics and telemedicine consultations increase the capacity of chronic pain programs to see more patients, including those living in remote and rural communities, and reduce scheduling barriers.
Specialist interprofessional pain teams provide patient-centred, holistic care and increase knowledge sharing among health professionals and with patients, while community-based care networks also bring clinicians together to offer comprehensive care and connect expertise. Other clinics provide a bridge between acute and chronic pain care, helping to improve transitions between home, community-based, and institution-based care. Central to the success of these types of initiatives are clear referral pathways for patients and health care professionals to navigate both in-person and virtual services, to increase awareness of available resources, and to help patients access them.
More self-management tools and resources in multiple languages should be provided to patients without charge. Remuneration models for physicians and other professionals should be changed to recognize chronic pain as a distinct disease, which requires additional time to be spent with each patient. Care should be provided by the most appropriate professional, and additional funding should be made available for health care system improvements and for patients incurring uninsured and out-of-pocket expenses related to their care.
Participants told us Pan-Canadian leadership and coordination across jurisdictions would provide a unified, national approach to pain. They want people living with pain to be involved in the development of measures to improve the availability of pain resources in Canada, and to help ensure care is culturally informed and accessible. They want expanded early, government-insured, multimodal pain care and improved communication among health professionals to increase coordination in the delivery of care.
Awareness, education, and specialized training for pain
There was consensus throughout our consultations that people living with chronic pain, health care professionals, and the wider community need to be more empowered, knowledgeable, and supported to manage chronic pain. We heard that people want not only health professionals, insurers, and employers to better understand pain, but also importantly the public to become more aware of pain as a legitimate disease to help reduce the stigma many people living with pain experience.
The lack of public awareness of chronic pain in Canada often leaves people living with pain feeling stigmatized and despondent, particularly those taking opioids to manage their pain and those unable to work due to pain. Many participants favour including education about wellness and preventive strategies for pain in primary and high school curricula. National public awareness campaigns by the federal government, similar to those that have been conducted for other public health issues, are seen as an effective way to educate and raise awareness of pain as a chronic condition and disease in its own right.
Participants called for better quality and quantity of pain education for health care professionals, through pre-licensure training and continuing professional development opportunities. Primary care networks were cited as a way to improve consistency in care, knowledge dissemination, and networking, while cross-disciplinary training programs foster collaboration and knowledge translation across disciplines and professions.
People living with chronic pain want more to be done to increase self-education about pain management and more opportunities to share their experiences with and help others also living with pain. Many people do not know where to look for supports and are often left to navigate complex public and private health care services on their own.
Pain research and related infrastructure
There is a solid foundation in Canada for national action on chronic pain research upon which to build; however, several participants noted funding for pain research in Canada is disproportionately smaller than for other chronic diseases, such as cancer and heart disease, despite the fact that chronic pain is more prevalent and presents potentially higher societal and economic costs. While there are emerging networks and initiatives focused on pain research, better coordination is needed. Too few studies examine people with multiple conditions and complex needs, and the duration of funding is often too short to allow research over the extended period often involved in pain management. More research is needed to better understand pain mechanisms, allow for the development of novel treatments, test the effectiveness of treatments, and ultimately tailor treatments to the individual taking into consideration their unique biological, psychological, and social circumstances.
Engaging people living with pain in all aspects of the research process helps define questions to be answered and enriches the value of the research team. Although pain research is often separate from clinical care, our consultations showed the benefits of having researchers as active partners in the delivery of care, improving knowledge about successful interventions and the spread of knowledge across jurisdictions. Demonstration projects, dedicated investment in knowledge translation, and knowledge mobilization initiatives, are needed to enhance real-world impact. Investment is required with dedicated funding and coordination across agencies and organizations to build capacity for pain research on a national scale.
Proposals for improving and expanding pain research in Canada include establishing an integrated and common understanding of pain and minimum data collection standards, building interdisciplinary pain research and collaboration, and supporting basic discovery and innovation. More research should be done to obtain a better understanding of the unique approaches to addressing pain in different populations, including Indigenous Peoples and people living with pain and other co-morbidities. More investment is also required to facilitate translation of research into clinical practice. Participants called for dedicated federal and provincial funding to create a national pain research agenda, and a dedicated pain research champion to support information sharing and collaboration across disciplines and jurisdictions.
Monitoring population health and health system quality
Limitations to comprehensive pain-related data make it challenging to know the full impact of chronic pain in Canada or what is required to meet the demand for care and treatment. The data that does exist is scattered across public, private, and academic systems. Participants agreed that an insufficient understanding of the physical, psychological, and economic cost, both direct and indirect, makes it difficult to raise awareness about the need to allocate sufficient resources to address chronic pain.
Participants stressed that international disease classification system standards are adapting to recognize chronic pain as a disease, and while implementation may take several years this holds much promise for improving how we think about, document, investigate, and monitor pain. Researchers are also leveraging existing data sources to develop algorithms for estimating the prevalence of chronic pain. Similarly, there are pockets of surveillance in individual clinics and regions, which have invested in improved data collection. Electronic Medical Records (EMRs) are widely seen as a way to unify medical records and help unlock data already in the system. There are still shortcomings in using EMRs, however, including variations in the EMRs in use within and between provinces and territories, the absence of chronic pain specific disease classifications in current billing codes, and the inability of some private clinics to access EMRs. Prescription monitoring programs allow for greater surveillance of opioid and other pain medication prescribing and have the potential to bring pharmacists into the monitoring and surveillance process. They also present opportunities for improved practitioner and patient education and assessment of patient outcomes over time. Currently, such programs often focus solely on monitoring prescribing practices for irregularities and in some cases have resulted in increased stigma and challenges for people living with chronic pain.
Our consultations found widespread agreement on the need for more comprehensive information about the prevalence of pain in Canada, who is affected, and which interventions work best for different types of pain and populations. This type of data would help direct strategic investments in the health system. National standards should be further developed for data collection and actions co-ordinated across jurisdictions to ensure comprehensive and consistent pain indicators are reported at the national level. More data is required to monitor how patients are accessing services and the effects of those services so health professionals can identify and scale up practices that lead to successful outcomes. Dedicated funds should be provided at the federal and provincial levels to increase data and surveillance capacity.
Indigenous Peoples
We heard about the negative experiences of many Indigenous Peoples when navigating a health system that is often fraught with bias and racial discrimination. Systems commonly privilege conventional approaches to health and wellness, and do not recognize traditional Indigenous knowledge, medicine, and healing. The resulting stigmatization becomes another barrier to seeking health care. Comprehensive care for Indigenous Peoples includes access to family, community traditions, ceremonies, and rituals, all of which are central to healing. Yet many Indigenous Peoples, especially those who live rurally or remotely, must endure high costs, long travel, emotional stress, and removal from their community and/or family support system when required to travel to receive services. This cultural isolation, compounded by language barriers to accessing culturally safe services, creates additional challenges and further complicates care.
Participants told us an improved approach to pain must include interventions that successfully address concurrent challenges related to chronic pain: trauma and violence, mental health conditions, and substance use. These interventions should be identified, planned, and co-ordinated with Indigenous Peoples and communities as active partners. We heard that research into the prevalence, impact, and outcomes of chronic pain in Indigenous Peoples should be culturally safe, including data collection methods that are culturally appropriate, community-led, and respectful of traditional healing. Support centres and programs, which reflect the identity and healing traditions of First Nations, Inuit, and Métis peoples are needed. Indigenous cultural safety training for health professionals should be expanded and integrated into pre-licensure and continuous learning, and culture change in the health system.
Resources that provide information, services, and referral pathways should include traditional healing approaches and activities in each community. First Nations, Inuit, and Métis communities need resources to support sharing, translating, and applying knowledge. Participants told us about the need to improve coverage and access to traditional Indigenous medicines and a more fulsome range of pain management options under the Non-Insured Health Benefits Program.
Reflecting on the impact of the COVID-19 pandemic
For many people with pre-existing pain conditions, the COVID-19 pandemic has led to stress, mental health conditions, disability, increased use of medications and substances, and disruptions to continuity of care. People living with pain also report negative socio-economic effects, such as financial stressors and emotional duress (e.g., lost wages, jobs, uncertainty of care), which can further exacerbate pain. Access to chiropractic care, massage therapy, physical therapy, rehabilitation programs, psychological services, and other services to manage pain and maintain function have been greatly reduced and elective surgeries and procedures to treat long-held pain and related conditions are being postponed. Increased cases of pain could be seen over time as newly triggered pain goes unmanaged and is worsened by common risk factors of the COVID-19 pandemic, or if chronic pain develops as a result of COVID-19 infection.
System responses to the pandemic, including rapid mobilization of virtual care, centralized and multidisciplinary assessment and intake, stepped care platforms, and enhanced self-management tools and resources could help to improve health system capacity and hold great promise for improving pain care. There is also an opportunity to leverage the unique environment post pandemic to conduct epidemiological work on post viral complications and related pain, and to reinforce the importance of taking action on pain, especially during times of increased risk. Such considerations align with the best practices discussed through our consultations and we are hopeful for future action, which will support people living with pain and the health system as a whole.
Introduction and approach
The Canadian Pain Task Force was established in March 2019 to help the Government of Canada better understand and address the needs of Canadians who live with chronic pain. Through to December 2021, the Task Force is mandated to provide advice and information to guide government decision-makers towards an improved approach to the prevention and management of chronic pain in this country. The eight Task Force members include people personally impacted by chronic pain, Indigenous Peoples, researchers, educators, and health professionals with experience and expertise in preventing and managing chronic pain across major professions (i.e., medicine, pharmacy, psychology, and physiotherapy). The Task Force is also supported by an External Advisory Panel, which provides up-to-date scientific evidence, information, and advice to the Task Force. Members represent a broad range of knowledge, experience, expertise, and perspectives on the issue of chronic pain.
Addressing pain and opioid overdose deaths - a role for the Canadian Pain Task Force
When prescribed and used as directed by a health professional, opioids can play an important role in pain management for many. New studies have demonstrated limited long term-effectiveness, and recent dramatic increases in opioid-related overdose deaths in North America have heightened awareness about the risks associated with both short- and long-term opioid use. However, there are people who require opioids to manage pain and maintain quality of life.
A toxic illegal supply of opioids is currently the main factor in drug overdose deaths. However, over the last two decades increased availability and use of prescription opioids for both acute and chronic pain has also contributed to this complex public health crisis. While the relationship between pain, opioids, and opioid-related harms in Canada requires further clarification, available evidence warranted action.
Efforts undertaken to respond to the overdose crisis have led to challenging unintended consequences for people living with chronic pain. Some people in Canada have been unable to access opioid medications, and others who previously relied on opioids to manage their pain have been unable to continue their medications, or have had significant adjustments to lower their prescriptions, sometimes against their will. Increased stigma, anxiety, and fear surrounding opioid use for pain management has compounded these challenges and created additional barriers for people living with pain. As a result, this has caused some people to obtain illicit drugs to self-manage their pain, putting them at serious risk for potential overdose. Finding solutions to address unmanaged pain and the trauma and complexity that often accompany it, is a key means for reducing first exposure to or longer-term reliance on opioids, preventing harms associated with substance use, and improving a system-oriented response to these challenges.
While the overdose crisis was the impetus for the creation of the Task Force, there is now recognition of the importance of addressing pain prevention and management more broadly, not only in the context of action on substance use but also as a parallel public health priority.
Phase I
Phase I of the Task Force mandate involved assessing how chronic pain is currently addressed in Canada. In June 2019, the Task Force submitted their first report to Health Canada on the state of chronic pain - Chronic Pain in Canada: Laying a Foundation for Action. The report highlighted gaps in access to timely and appropriate multi-modal care, chronic pain surveillance and health system quality monitoring, education, training and awareness for individuals and health care professionals, and research and related infrastructure.
Phase II
Phase II of the Task Force mandate involved conducting national consultations and reviewing available evidence to identify best and leading practices, potential areas for improvement, and elements of an improved approach to the prevention and management of chronic pain in Canada. As part of this engagement process, the Task Force undertook an extensive series of consultations with Canadians between July 2019 and August 2020, which included:
- A series of regional workshops and targeted stakeholder discussions held across the country between September 2019 and August 2020, with more than 400 participants. These workshops examined various issues related to pain in Canada, including Indigenous perspectives, research-focused dialogue, and the intersection of pain, mental health, and substance use. Summaries of those workshops and discussions were prepared by Health Canada and were used to develop an analytical framework for an online consultation and for integration into this report.
- A national online consultation was conducted from February to June 2020 on the Health Canada online engagement platform Let's Talk Health and Parlons Santé. The platform provided both the public and pain stakeholders the opportunity to provide feedback through a questionnaire and a tool designed to share personal experiences with chronic pain. We received a total of 1,408 questionnaire responses (1,115 in English, 293 in French) and 103 submissions (89 in English, 14 in French) noting personal experiences from people living with pain, their families, health care professionals, and other stakeholders in the health system.
- 13 longer form submissions were also received from interested stakeholder organizations.
Hill+Knowlton Strategies (H+K) was retained by Health Canada to analyze and report on data collected through all engagement activities. Consultative inputs were analyzed both quantitatively and qualitatively and coded according to a coding structure subdivided by themes. The codes were developed based on a review and analysis of the workshop summary reports, as well as a subset of questionnaire responses, to identify key ideas and themes. This approach ensured the coding categories were empirical (i.e., based on similar consultative data), as opposed to preconceived (i.e., based on hypothetical range of anticipated responses). Throughout the process, samples of data were reviewed by two or more analysts to ensure a consistent approach. H+K created a first draft of the report, which was subsequently refined and expanded based on engagement with the Task Force and its External Advisory Panel, including a two-day virtual workshop in September 2020. The Task Force also consulted federal, provincial, and territorial government representatives and key stakeholders, reviewed reports and scientific literature, and conducted a series of rapid reviews and economic analyses.
The report herein summarizes the findings from this consultation process on approaches to better understanding, preventing, and managing chronic pain in Canada. The activities undertaken to inform this report mark the completion of Phase II of the Task Force's mandate. Phase III will commence in Fall 2020 and calls for the Task Force to continue to increase awareness of chronic pain and to build relationships and networks for change across the country. This work includes collaborating with key stakeholders, such as the chronic pain community, federal, provincial and territorial governments, health professionals, researchers, and Indigenous Peoples, to disseminate information related to best practices for the prevention and management of chronic pain, including for populations disproportionally affected by chronic pain. The final Task Force report is expected in December 2021 and will focus on strategies for improving approaches to chronic pain in Canada.
A note on our approach to best practices
Throughout our engagement activities and this summary report, we define and approach best practices as follows:
"Best, promising, and emerging practices are defined generally to include programs, interventions, strategies, and policies that have been evaluated or have the potential to be successful, and which are likely to be adapted and used in different settings and jurisdictions."
In the report we include several examples of such best practices, which were identified by consultation participants. We hope this will help to illustrate the principles and ideas that we heard from stakeholders, but we are not listing a comprehensive scan of all activities across Canada. The practices listed through this report are representative of examples raised by participants in our process and only point to some of the work going on across the country. Similarly, as the respondents did not represent a nationally representative sample (demographic information from our online consultation can be found in appendix A), the consultation feedback cannot be interpreted as reflecting the views of all participants or the full spectrum of opinions regarding chronic pain in Canada.
Reflecting on inequity, disadvantage, and trauma
As with most chronic illnesses, chronic pain is not distributed equally among Canadians. A broad range of biological, psychological, social, cultural, and other factors influence how we experience pain, and also influence who of us will develop chronic pain. Often the occurrence of disease, as well as the severity of illness, is higher in populations affected by social inequities and discrimination including those living in poverty, Indigenous Peoples, certain ethnic communities, and women. It is important to reflect on such inequity in relation to pain and the importance of taking a trauma and violence-informed approach to situate this report in a broader societal context.
Race/ethnicity
Research has demonstrated that people who experience marginalization, including those from black, Indigenous, and people of colour (BIPOC) communities, are more vulnerable to chronic conditions, including those that result in pain (Craig et al., 2020; Turk et al., 2002; Williams et al., 2017). For example, African Americans experience a greater prevalence of many chronic pain conditions (e.g., migraine headache, jaw pain, postoperative pain, myofascial pain, angina pectoris, joint pain, non-specific daily pain, arthritis) than their white counterparts (Campbell et al., 2012; Green et al., 2003; Klonoff, 2009).
Considering this, it is of even greater concern that there are disparities in pain treatment for BIPOC in comparison to white people. A large body of literature demonstrates BIPOC individuals receive fewer pain medication prescriptions or at lower doses, are less likely to be screened for pain, and are given less priority when presenting with acute injuries (e.g., broken bones) and more ambiguous pain conditions (e.g., back pain) (Allan et al., 2015; Burgess et al., 2013; Craig et al., 2020; Hewes et al., 2018; Lord et al., 2019; Mossey et al., 2011; Owens et al., 2020; Todd, Deaton, D'Admo & Goe, 2000). These disparities are driven by multiple factors, including unconscious biases held by practitioners, as racially stereotyped beliefs are related to lower health professional ratings of the patient's pain intensity and less accurate treatment recommendations (Hoffman et al., 2016; Mossey et al., 2011).
Indigenous Peoples in Canada and the US experience higher incidence of pain/pain-related disability than the non-Indigenous population, both in children and adults, and chronic pain related symptoms are among the primary reasons for seeking health care (Craig et al., 2020; Jimenez et al., 2011; Latimer et al., 2018; Meana et al., 2004). Based on evidence collected from both patients and clinicians, Indigenous populations experience systemic discrimination, which can influence pain management. Indigenous Peoples seeking pain treatment often have their pain dismissed because of clinician assumptions around credibility, drug seeking behavior, and other discriminatory beliefs (Allan et al., 2015; Browne et al., 2016; McConkey, 2017; Wylie et al., 2019). As a result, Indigenous Peoples may not seek treatment out of fear of having their experience minimized or of suffering further marginalization or harm through the experience of seeking care itself (Craig et al., 2020; Denison et al., 2014; Latimer, Rudderham, et al., 2018).
Sex and gender
Epidemiological, clinical, and empirical studies have consistently revealed that women are at greater risk than men of chronic pain diagnosis across their lifespan (Quintner, 2020; Reitsma et al., 2011; Schopflocher et al., 2011; Stanford et al., 2008). Many biopsychosocial differences between men and women have been identified, which may contribute to this gender bias, including pain intensity/sensitivity, reaction to pain medication, impact of certain pain management strategies, pain beliefs, certain health care resources, sex hormones, endogenous opioid function, genetic factors, pain coping, and gender roles (Bartley et al., 2013; Mogil et al., 2020; Racine et al., 2014). Another possible contributor is that women are more likely than men to be victims of gender-based violence, including domestic abuse, and to suffer injury due to such violence. For example, the odds of experiencing a chronic condition, including chronic pain conditions (e.g., irritable bowel syndrome, frequent headaches, activity limitations, poor physical or mental health), were significantly higher for rape victims compared with non-victims in the US (Office of the Federal Ombudsman for Victims of Crime, 2020).
Conditions that are more prevalent in women and where pain is the primary or only symptom, often do not easily fit into the biomedical model of health care (e.g., fibromyalgia, myalgic encephalomyelitis/chronic fatigue syndrome) (Grace et al., 2001; Katz et al., 2008; Samulowitz et al., 2018). Such diagnoses are often treated with skepticism and women appear to be treated as if the illness does not actually exist (Barker, 2011; Katz et al., 2008; Samulowitz et al., 2018). Some empirical research has suggested women are less likely to receive diagnoses or pain related interventions than men when presenting with similar clinical symptoms (Chapman et al., 2013; Chen et al., 2008). However, it appears the influence of patient gender on treatment decisions sometimes favours women and other times favors men (Bartley et al., 2013; Leresche et al., 2011). Also, the gender of the physician and patient have potential to interact and influence pain treatment.
"Many marginalized groups, in particular people of colour, Indigenous people and women, have their pain outright dismissed by the public and medical professionals. People of colour and Indigenous people are often regarded as 'drug seekers' and women are regarded as being 'dramatic'. These barriers not only prevent people from getting proper care but also prevent them from seeking help in the first place, due to negative experiences and shame."
Questionnaire Respondent
Sexual orientation and gender diversity
Based on recent research findings, gender based pain disparities also apply to gender diverse individuals and the LGBTQ2S community, who experience greater prevalence of disability and marginalization than heterosexual individuals (Craig et al., 2020; Fredriksen-Goldsen et al., 2017; National LGBT Health Education Centre, 2018). Preliminary evidence suggests transgender individuals who are older or diagnosed with a disability are more likely to have chronic pain than cisgender counterparts (Craig et al., 2020; Dragon et al., 2017). Transgender women may display a similar disproportionate burden of chronic pain to cisgender women, as a recent study found that trans- and cisgender women report similarly greater chronic pain rates and similar responses to painful stimuli compared to cisgender men (Strath et al., 2020).
Incarcerated populations
There is limited research examining chronic pain in the incarcerated population; however, it appears that chronic disease is higher than in the general population (Office of the Correctional Investigator, 2019). Chronic pain was examined in a report on the aging population in Canadian prisons and was found to be one of the more prevalent chronic diseases reported (Office of the Correctional Investigator, 2019). The prison population is disproportionately affected by a number of factors that may increase the prevalence of chronic pain and further challenge clinicians, including experiences of trauma and marginalization and a high prevalence of mental illness, substance use disorders, and traumatic brain injury (CSC, 2019). While the prevalence of chronic pain in incarcerated populations is not clear, barriers to pain-management in prisons have been identified. An investigation conducted by the Correctional Investigator of Canada found newly admitted inmates could be denied medication for 30 days or longer when waiting to be seen by physicians, far longer than the common clinical guidance of 72 hours (White, 2015). Limitations on prescription medications often leave inmates reliant on over-the-counter medications, such as acetaminophen or ibuprofen, or turn inmates towards illicit drugs for self-management (White, 2015; Office of the Correctional Investigator, 2019). In addition, the incarcerated environment limits multidisciplinary intervention options, further impacting treatment of chronic pain and proper attention to the role of trauma (CSC, 2019). In its review of the aging population in prison, the Office of the Correctional Investigator of Canada (2019) provide several suggestions for promoting wellness, which may be also generalizable to the broader prison population, including:
"Review barriers to prescribing narcotics for pain management and continue its pilot project on pain management where a multi-disciplinary team utilizes a range of strategies to address the needs of those with chronic pain."
"Review offender medications with an aim to 'de-prescribing' medications deemed unnecessary or inappropriate and/or introduce new medications that may improve outcomes."
Correctional Service Canada has worked to develop guidance for chronic non-cancer pain management, articulating recommendations and strategies to assist practitioners involved in assessing and managing pain in inmates and emphasizing patient-centred interdisciplinary approaches, which incorporate pharmacological, physical, psychosocial, and culturally-appropriate interventions (CSC, 2019).
Veterans
While past studies have estimated that approximately one in five Canadians report living with chronic pain (Schopflocher et al., 2011; Reitsma et al., 2011; Steingrímsdóttir et al., 2017), this is doubled (41%) for Veterans. The results were even more concerning for female Veterans who experience chronic pain at a rate of 50%. The problem is further complicated by the fact that 63% of Veterans with chronic pain have also been diagnosed with a mental health condition (Veterans Affairs Canada Research Directorate, 2018). Post-traumatic stress disorder (PTSD) and chronic pain are frequently concurrent conditions noted in Veteran populations. Veterans with co-existing pain and PTSD experience higher pain, disability, depression, sleep disturbance, and health care utilization as well as lower function and pain self-efficacy compared to Veterans without PTSD (Benedict et. al., 2020).
With these challenges in mind, the Chronic Pain Centre of Excellence for Canadian Veterans (CPCoE) was established to conduct research and help improve the well-being of Veterans, and their families, suffering from chronic pain. At the core of all CPCoE activities is the principle of Veteran engagement. As such, consultation and engagement with Veterans, including an Advisory Council for Veterans, began prior to establishing the CPCoE and continues as a lasting priority. According to recent CPCoE consultations conducted in parallel to the work of the Task Force, Veterans experience substantial isolation, in particular after leaving the Service, which makes accessing treatments in the civilian world challenging. When a Canadian joins the Canadian Armed Forces, the military becomes responsible for their health care. Once they complete their military service, these Canadians return as Veterans to the care of their respective provincial and territorial health systems. This transition can often create delays, and Veterans who were previously seeing specialized medical professionals in the military will no longer have access to these practitioners, sometimes waiting years before receiving care for pre-existing conditions.
In the spring of 2020, a series of qualitative one on one interviews were conducted by the CPCoE with Veterans to better understand their experiences in order to help prioritize research. These interviews, which will inform a much larger quantitative survey, brought forward four key priorities.
- Prevention of chronic pain, including improved management of acute pain / injuries and post-surgical care;
- Coordination of chronic pain care, including access to services, military to civilian transition, and finding a primary care provider;
- Knowledge and competencies in pain management, including a lack of military knowledge in civilian health care and the need for more holistic care and patient involvement; and,
- Options for chronic pain management, including assistance sorting through the wide range of treatment options and consideration of contributing factors.
On behalf of CPCoE, Healthcare Human Factors (HHF) conducted a series of context labs in spring 2020 with Veterans living with chronic pain to learn and understand their experiences. Common themes included the loss of identity and invisibility of disability that accompanies chronic pain, the lack of support through long cycles of waiting for access to care, the challenges of managing chronic pain as a complex balancing act and often difficult to articulate, and pain often creating a barrier between Veterans and their loved ones. While the mandate of the CPCoE focuses on Veterans, its research-based learnings, and their planned focus on exploring gender specific factors, may ultimately help both Veterans and civilians alike by improving the understanding and care of chronic pain for all Canadians.
Mental health and substance use disorders
People living with chronic pain are at an increased risk of a number of concurrent conditions, including mental health issues such as depression and anxiety, decreased cognitive function, reduced health (e.g., fatigue, disability), and impairments in social functioning. In addition, a substantial portion of individuals who report using drugs or who are taking opioid agonist treatment for opioid use disorder (e.g., methadone; buprenorphine) also report experiencing chronic pain (Alford et al., 2016; Dunn et al., 2015; Heimer et al., 2015; Peles et al., 2005; Voon et al., 2015).
Unfortunately, people who use drugs often face discrimination when trying to access the health care system, and people with chronic pain and a history of substance use are less likely to receive adequate pain management (Baldacchino et al., 2010; Breitbart et al., 1997; Dassieu et al., 2019). Stigma associated with chronic pain, lack of accessible pain treatment and management options, and reluctance from health care professionals to deliver specific interventions, such as opioids, can further complicate treatment efforts, potentially resulting in untreated chronic pain, worsening mental health, and increased risk of problematic substance use.
A rapid review was conducted for the Task Force through the Drug Safety and Effectiveness Network (DSEN) to identify best practices for managing chronic pain in the context of concurrent mental health and/or substance use disorders. The review looked at clinical practice guidelines (CPGs) and literature meant to synthesize various studies. The review found there were a limited number of high quality guidelines with specific and consistent recommendations for managing chronic pain within the context of a concurrent mental health or substance use disorder, and there were more available recommendations related to concurrent mental health disorders than concurrent substance use disorders. Even so, such guidance was generally high level (e.g., "provide medical management") and did not provide specific interventions (e.g., provide a trial of selective serotonin reuptake inhibitors).
CPGs that made recommendations for substance use disorders focused disproportionately on patients with opioid use disorder, compared to other types of substance use disorders, and included recommendations for pharmacotherapy - specifically opioid agonist treatment (e.g., buprenorphine/naloxone) - and simultaneous treatment of pain and mental health conditions. Alternatively, available guidance for the treatment of pain with concurrent mental health issues recommended ongoing psychological care or nursing support. For both types of concurrent conditions, recommendations often involved approaches to care delivery, such as tailoring services based on needs, implementing adherence monitoring measures, and using weaker potency opioids and immediate release formulations for the treatment of pain. The review also found that rather than providing evidence of effective strategies to work through with patients, much of the available best practice guidance focused on avoiding interventions that are contraindicated among individuals with chronic pain and concurrent mental health and/or substance use disorders (e.g., avoiding certain drugs for those with a history of psychosis, abstinence-based detoxification generally). Given the lack of best practice guidance for the treatment of people with pain and concurrent mental health and substance use disorders, future research priorities should ensure that studies do not exclude this complex population.
Trauma and violence
Chronic pain, mental health conditions, substance use disorders, and other chronic conditions are often interconnected and share multidirectional relationships, as well as common risk factors. Evidence suggests that adverse childhood experiences (ACE), past traumatic events, and Post Traumatic Stress Disorder (PTSD) are linked to the development and experience (e.g., intensity and severity) of chronic pain (Kascakova et al., 2020; Nicol et al., 2016). Studies have shown 80% of children and youth with chronic pain have had at least one ACE. In the presence of multiple ACEs, more complex trauma and susceptibility to the negative impacts of trauma may develop (Nelson, Simon, & Logan, 2018). Furthermore, individuals who experience, witness, or hear of trauma or past life-threatening events may develop PTSD (Greenberg, 2020; Veterans Affairs Canada, 2019). PTSD is associated with cognitive (thoughts, beliefs), emotional, and biological reactions, including nervous system dysregulation and endocrine system changes (e.g., increased cortisol levels and inflammation) (Greenberg, 2020; Purkey, Patel, & Philips, 2018) - which research links to chronic pain. People with PTSD may dissociate, or have physical reactions to stressors and triggers - things that remind them of their past traumatic event (Greenberg, 2020; Driscoll, Adams, & Satchell, 2020).
Many people living with chronic pain have experienced trauma in the context of medical care. They may have had invasive investigations and procedures or negative interactions with health professionals. Such experiences can be damaging on their own, but when compounded with previous trauma can lead to more drastic challenges such as changes in sense of self, view of the world, and nervous system dysregulation, which may all contribute to increased pain and difficulties coping.
Using trauma and violence-informed approaches in chronic pain management
Trauma and adverse events may negatively impact one's experiences with the health care system (e.g., feeling lack of control or privacy, uncomfortable with intrusive procedures, feeling overwhelmed), which could result in individuals avoiding care, seeming disinterested, or failing to follow the advice of health professionals (Driscoll, Adams, & Satchell, 2020). It has also been suggested that individuals with chronic pain who have experienced trauma or adverse events may be seen by clinicians as difficult patients (Driscoll, Adams, & Satchell, 2020). Therefore, adopting a sensitive approach using trauma and violence-informed care may lead to improved patient experiences and outcomes. It can be helpful to screen for past traumatic experiences or adverse childhood events during clinical care in a similar manner as other impairments or risk factors (Driscoll, Adams, & Satchell, 2020).
Trauma-informed care typically applies four key principles (See figure 1), whereby health professionals take into account the patient's experience, preferences, and possible history of trauma, violence, or adverse childhood events, to create an environment of trustworthiness and safety. Care and behaviours are adjusted so that approaches are sensitive to patient needs (Canadian Public Health Association, 2019; Government of Nova Scotia, Nova Scotia Health Authority, & IWK Health Centre, 2015; Public Health Agency of Canada, 2018). Trauma and violence-informed care does not seek to treat trauma, but rather recognize it may be present, and adapt care to support patients where possible responses to trauma or events may cause resurgence of symptoms (Canadian Public Health Association, 2019; Government of Nova Scotia, Nova Scotia Health Authority, & IWK Health Centre, 2015; Public Health Agency of Canada, 2018). Practicing trauma and violence-informed care also integrates acknowledgement and sensitivity to cultural, historical, and gender-related issues and experiences with trauma and violence (Purkey, Patel, & Philips, 2018).
Figure 1 - Four principles of trauma and violence-informed care
Understand trauma and violence and their impacts on peoples' lives and behaviours
Create emotionally, physically, and culturally safe environments
Create options for choice, collaboration, and connection
Provide strengths-based and capacity-building approach to support patient coping and resilience
(Canadian Public Health Association, 2019; Government of Nova Scotia, Nova Scotia Health Authority, & IWK Health Centre, 2015; Public Health Agency of Canada, 2018)
Consultation results
Access to timely and patient-centred pain care
The first phase of our work reviewed the state of chronic pain treatment and management in Canada, noting many Canadians do not have access to a range of adequate pain management services. Where services do exist, the lack of a clear pathway to care means patients often must identify on their own whom they should see and in what order. They must also navigate across multiple systems for reimbursement of services, including the public system, private insurance, and personal expenses. All of this combines to leave many people living with pain, particularly those with low income or no private insurance, with inadequate treatment.
Our review noted the limited body of evidence on the effectiveness of specific interventions and therapies for addressing various types of chronic pain, and the quality of available evidence. That said, we identified clear benefits of programs integrating pharmacological, psychological, physical/rehabilitative/manual, procedural, and self-management treatments, through wellness-oriented, community-based care or specialized, inter-professional care.
In Phase II consultations, we explored these gaps and challenges in greater detail, and identified existing best practices that could be scaled up and shared across jurisdictions to improve the diagnosis, assessment, and management of chronic pain in Canada. We also asked participants for their views on the most appropriate strategies for further progress, including how to meet the needs of populations disproportionately affected by chronic pain.
Gaps and challenges
Shortages in primary care practitioners interrupt continuity and reduce quality of pain care
For most Canadians, the first point of contact within the health system for the assessment of pain is a family physician or other primary care practitioner, many of whom often lack the knowledge, skill, and judgment to treat chronic pain. For many people, primary care may be the only health service available in their community. For others, shortages in primary care force people to find other ways to begin their pain management journey. Consultation participants noted many people wait years before being placed with a family physician, and those without one have few to no options for referral to pain specialists. If a person has been able to access a pain specialist or other prescribed pain therapy, the absence of a primary care physician reduces options for transitioning back to community care and ensuring optimization of care and best patient outcomes. Individuals without a primary care physician disproportionately use walk-in clinics to access care. For people with chronic pain, this can involve being seen by multiple clinicians over an extended period, requiring patients to repeatedly explain their diagnosis and its impact to different health professionals. These individuals endure significant obstacles to obtaining care, and lack support in implementing and monitoring a long-term treatment program.
Lack of recognition of the impacts of the pain experience
A major topic of discussion throughout our consultations was the difference in perception of the impacts of pain between health professionals and people living with pain. The first step to pain care is an acknowledgement that a person's pain experience is real. Without this acknowledgement, we heard that people living with pain may spend months or years without a diagnosis, delaying the beginning of care. Pain experienced by patients is often diminished and misunderstood by health professionals, in part due to its invisibility. This in turn can create disagreements and conflict in the care relationship and hinder quality of care. We also heard it can be difficult to access adequate pain care or establish a care plan because patient concerns and experiences are at times dismissed in the primary care setting. People's experiences with pain are not always acknowledged and validated in care settings due to unconscious bias and stigmatizing beliefs around pain, a lack of understanding of pain by clinicians, and gaps in pain-related training.
"I am able to work, but my prescription medication makes me foggy and that, in combination with my pain, makes it difficult to concentrate. I have to take an average of two days off sick per month. I am extremely fortunate to have an understanding employer, but my previous employer was not as good. I have to constantly tell myself that I'm not lazy, I'm legitimately sick."
Personal Experience Submission
Differing expectations between patients and clinicians
We heard during our engagement activities that differing expectations arise between patients and clinicians on the outcomes of pain care, the potential for improvement, the duration of treatment, and the role of the clinician and patient. Misaligned expectations between clinicians and patients can be detrimental to patient outcomes and the optimization of a patient's care plan. Differing expectations can stem from poor communication between clinicians and patients, including a lack of understanding by both parties about the condition and its severity, and the pain care options available. These expectations may also stem from many patients' inability to access therapies included in their treatment plan due to unavailability or inaccessibility - especially multimodal therapies. As a result, patients may not be able to follow the recommended course of treatment.
"I would consider myself lucky, but like many of you, I saw many different physician specialists, 8 physiotherapists, a massage therapist, 2 chiropractors, 2 osteopaths, yoga teachers, counsellors, and pedorthists. In this health care journey, I share the frustration that many of you likely have of health care providers who think they can 'cure' or believe the pain to be not as bad as we make it out to be. One of the challenges of my journey was to maintain hope that my pain could improve despite the many failures I had to endure."
Personal Experience Submission
The health care system does not adopt the biopsychosocial model integral to managing chronic disease
The structure of Canada's health system favours acute care based on medical models over complex long-term care, based on a biopsychosocial approach. The biopsychosocial model of pain treatment requires an interprofessional approach, which addresses the interconnected biological, psychological, and socio-environmental factors that may influence the pain experience. Although the importance of applying such models and delivering interprofessional care is often recognized in broader policy discussions, there are still tremendous gaps in advancing biopsychosocial approaches at the clinical level and in the broader policies that govern various health systems. To illustrate these points, many participants noted the current fee structure within primary care often incentivizes the treatment of individual symptoms rather than developing comprehensive, multidisciplinary treatment plans. This is particularly concerning for the aging population of Canada, who often present with multiple chronic conditions and require numerous services and coordinated care to manage this range of needs. Citing broader challenges related to the crisis of drug-related overdose deaths, participants also noted the lack of access to non-pharmacological pain care options as a major challenge. They highlighted that opioid therapy may sometimes be prescribed even though other first line therapies with less potential for dependence could have been explored, simply because those alternatives were not respected, recognized, or accessible.
Long wait times, limited access to specialists, and geographic disparities can delay intervention
Long wait times to see pain specialists can delay the diagnosis of chronic pain and initiation of treatments. Such delays can lead to increased disability, functional impairment, and the despair and mental health challenges that often accompany chronic pain. Consultation participants highlighted that although primary care physicians often lead chronic pain management, most do not have the knowledge, skill, or judgment to deliver effective pain interventions or to develop multimodal pain management plans. As a result, patients are often treated with pharmacological options even if these may not be the most evidence based treatment suited. Citing broader challenges, participants also noted a reluctance among health professionals to deliver specific therapies, including opioids because of the fear and stigma that surrounds them. They also noted clinicians may prescribe pharmacological options off-label (i.e., for an indication other than what the medication was approved to treat), which affects the coverage of certain medications in different jurisdictions and under different insurance policies.
Rural and remote communities in Canada, including Indigenous reserves, experience unique and additional barriers to access. In addition to a shortage of specialists across jurisdictions, these communities may not have access to pain care services. In instances where alternatives to traditional referral models and in-person appointments are available to people living with pain through virtual options, accessing care can still remain a barrier. Participants recognized virtual solutions can be difficult for people in rural or remote communities with limited or no Internet service, and people who cannot afford computers, smartphones or broadband Internet.
Overall, participants also said heavy caseloads for many primary care providers and specialists result in limited capacity to follow-up throughout their patients' pain management trajectory, and few had the time or resources to take part in knowledge-sharing initiatives, mentoring opportunities, or chances to advocate for improvements to pain care. Siloed communications between primary care providers and specialists can also impede assessment and treatment of chronic pain, and pose a barrier to coordinated care. This includes inconsistent nomenclature and prescribing patterns, as well as the absence of standardized objectives and practices, which can lead to a lack of collaboration and agreed upon best guidelines for care.
Financial barriers make effective treatment options and therapies difficult to obtain
Throughout all consultation activities, people highlighted financial inaccessibility as a significant barrier to pain services, particularly for people who are living in poverty and with low incomes, and those without private health plans and in jurisdictions with gaps in public health insurance. Online consultation respondents and regional workshop participants agreed addressing these financial barriers is the measure that would best help to improve access to pain care. Many therapies integral to the effective management of pain - including physical and manual therapy and psychological services - are not covered by public health insurance, and coverage under private plans is limited. Often these treatments are viewed as supplemental to pharmacological treatments, a view that is reinforced by the lack of coverage under public health insurance, despite numerous guidelines noting physical, psychological, and other non-pharmacological interventions as first-line treatments for pain. Other treatments essential in addressing certain cases, such as pain related dentistry or optometry, are also typically not included in public health insurance plans. In addition to the challenges posed by inadequate public coverage of services, people living with pain who could obtain private insurance through their workplace might not be able to do so because their pain limits their ability to maintain full-time employment. Participants also discussed other out-of-pocket costs associated with pain management, such as travel expenses to access care and lost income when attending medical and other treatment appointments, as well as the costs of multimodal treatments and social supports.
"What happens when I lose insurance coverage because I'm too old to be covered under my parents' plan? I could get a job with insurance coverage, but I won't be able to hold a job with more than half a month of 'sick' days. It's an endless loop."
Questionnaire Respondent
Best and promising practices
Throughout our engagement activities, we identified a number of innovative and successful approaches to improve access to pain care across Canada, approaches that could serve as sustainable models for the future. The practices identified most often and consistently across different engagement activities included:
- Patient-centred care models, including stepped care frameworks, which adapt services based on the needs of people living with pain;
- Community-based care, strategic networks and communities of practice, which are building capacity in primary care settings;
- Innovative models focused on rapid access to pain care and early intervention;
- Interprofessional teams incorporating different clinical approaches and specialties;
- Clinics supporting transitions across different levels and sites of care; and,
- Common, centralized, and clear referral pathways integrating services and improving navigation of care.
Individual practices outlined in this discussion are not comprehensive but rather representative examples and illustrative of the principles heard during consultations.
Innovative patient-centred care models are optimal when matching type and intensity of care to individual needs and goals
Consultation participants saw great value in approaches to care and models that put the patient at the centre of assessment and clinical decision-making. One approach receiving widespread support is the stepped care model for health care delivery. In the stepped care approach, the first part of a patient's care trajectory would be to implement the most relevant and effective, yet least resource intensive, interventions. Patients would then receive additional and potentially more intensive care based on their unique needs and response to earlier interventions. An example of successful application of this approach is the Ottawa Hospital Pain Clinic, which has considerably reduced its wait list after implementing such a model (See figure 2). Some practices employing the stepped care model use triage algorithms and criteria for pain specialist referrals to help ensure patients who most urgently need an appointment are seen first. Online algorithms also alert health care professionals when they should contact patients for a follow-up based on their self-reported symptoms. The use of algorithms and stepped or triaged models have allowed health professionals including nurses, physiotherapists, and psychologists, more latitude in patient management, with physicians making adjustments to care plans only as needed. Participants consistently noted significant improvements in pain outcomes under such models.

Figure 2 - The Ottawa Hospital Pain Clinic eight-tiered interprofessional chronic pain management stepped care framework (Bell et. al., 2020): Text description
This figure shows a model of tiered pain care options labelled as interventions. Interventions are listed in ascending order, based on the required level of resources and time commitment for each type. The interventions stack in the following order:
- education modules
- peer-led self-management programs
- interactive workshops by health care professionals
- online therapist-assisted self-directed therapy
- online or in-person group therapy
- interprofessional chronic pain program
- one on one treatment
- case management
A one on one session helps to develop a personal plan outlining what therapies will be provided and external resources from other clinics are leveraged and incorporated as needed.
Another successful approach cited by many participants is the hub-and-spoke model, which connects primary care providers with specialists and other services to receive guidance on cases involving complex pain conditions. In such models, the greatest level of expertise and capacity to provide a range of services is located in specialty "hubs" often housed at pain clinics or tertiary-care settings, which have greater infrastructure and access to resources. These hubs are also connected to smaller community facilities representing the "spokes", which further deliver care to people across a region. As expertise grows across community facilities, they can start to serve as hubs for surrounding communities. Such platforms typically use online technology to link health professionals who might otherwise have been unable to connect.
"It's been very helpful having health practitioners that understand how I'm feeling both physically and emotionally. It also helps to speak with other people who have gone through something similar. Speaking with a therapist has also been very helpful."
Questionnaire Respondent
Community-based care networks are building options and capacity in primary care and connecting expertise
Across all consultation activities, participants saw considerable value in community-based care networks, which bring together local physicians and other health professionals to offer comprehensive care for the communities they serve. These programs, projects, and services help to build capacity in primary care by facilitating exchanges of information and best practices with specialists in pain using e-platforms, virtual visits, and telephone consultation services. Examples of successful networks mentioned by participants included:
- Alberta's Collaboration for Change, which draws from specialty clinics across the province to helps build pain capacity across the more than 40 Primary Care Networks in the province.
- Saskatchewan's e-health service that clinicians can use to provide in-home virtual visits to troubleshoot problems in pain management, and a provincial telephone consultation service (Leveraging Immediate Non-urgent Knowledge) providing primary care providers and their patients rapid access to specialists to discuss less-serious patient conditions.
- Nova Scotia's Pain Collaborative Care Network, which is a partnership among family physicians and chronic pain and substance use specialists aimed at enhancing communication between specialists and family physicians to ensure optimal care is provided for patients awaiting assessment in the pain management unit.
- Ontario's Project ECHO - Extension for Community Healthcare Outcomes and BASE eConsult, which support primary care providers' ability to meet the needs of patients in community-based settings by connecting them to pain specialists and other services to receive guidance on complex pain cases.
Models focused on rapid access and early intervention are reducing wait times and improving care
Participants noted the success of virtual clinics and telemedicine consultations, many of which have reduced the wait time for people in need of pain specialist care. Such models can allow specialists to see more patients, and help reduce the transportation and scheduling barriers, which can impede people living with pain from seeking care. Rapid access clinics, such as those available for hip and knee osteoarthritis and low back pain, were identified as successful examples, in part because they provide patients with a range of education, alternative and non-surgical treatment options, and self-management plans early in a person's care trajectory while pain is easier to manage (e.g., Ontario's ISAEC (Inter-professional Spine Assessment and Education Clinics) program).
Community-based, publicly funded clinics dedicated to pain care services are seen as a way to decrease the burden on patients who otherwise would have to take time off work to travel to appointments with specialists. An example of programming noted by participants is evening and mobile clinics, which allow physicians and nurses to reach patients during evenings and outside of urban centres. Some of the mobile outpatient street health services also offer support for primary care and substance use disorders in collaboration with pain specialists. Participants also cited programming that brings together professional coaches and patients and is adapted to the schedule and needs of the patient, eliminating the need for travel, taking time off work or school, and interrupting normal routines (e.g., the Strongest Families Institute at IWK Health Centre in Halifax, Nova Scotia). Other models highlighted by participants brought together university faculty, students, and professional mentors from a range of disciplines and professions to provide free health services to community members (e.g., Winnipeg Interprofessional Student-Run Health Clinic).
Patient outcomes are improved when multiple professions and caretakers are involved
Consultation participants saw many benefits of interprofessional teams working to prevent, assess, and manage chronic pain. Such teams draw upon a range of health professionals who could assist with different aspects of pain care, including its pharmacological, physical, and psychological components. They provide patient-centred holistic care and increase knowledge sharing among clinicians and people living with pain. Participants also noted the role that various practitioners can play in educating patients on how to self-manage and take an active role in their care and the care of their families in the home. Caretakers and professions outside health can also play a role in supporting people living with pain with social and employment services, education, cultural and spiritual needs, and through family- and community-based support networks. This can help to address the complex needs of individuals more holistically.
"Teams with health care workers of different areas of expertise are better able to respond to the unique needs of individual patients and provide complementary and coordinated therapies for the best outcome."
Questionnaire Respondent
Various models for interprofessional pain care teams exist, all centred on a multimodal approach to care, which incorporates the biopsychosocial model of pain. Such teams are better able to meet the needs of patients due to shared patient medical records and ease of communication between different practitioners. Clinics often have multiple specialties, case managers, and alternative reimbursement models, reflecting the complex care needs of people living with pain. It is less clear which types of teams and professions work best together for various types of pain, contexts, and patient populations. More work is needed to link and monitor such teams across Canada and to better understand what types of models work best for whom, when, and under what circumstances.
Clinics are building pain services that improve transitions between home, community-based, and institution-based care
Gaps in pain care can occur when patients move from care in institution-based settings, such as hospitals and other facilities, back to home and community-based settings. Transitional pain clinics can act as a bridge between acute in-hospital pain care and care in the home by providing interprofessional care and individualized pain care plans for patients both prior to and after surgery, particularly for major surgeries that may lead to significant pain. They also help patients with pre-existing chronic pain, including in particular those who already require opioids for pain management. Such services can also be provided through telemedicine follow-ups and appointments, reducing barriers posed by travel and scheduling for patients. They may help to reduce the incidence of post-surgical chronic pain, improve patient functional outcomes and quality of recovery post-surgery, and decrease patient reliance on opioid medications via multi-modal analgesia and multidisciplinary pain management strategies. Some services use screening tools to identify patients at a higher risk of developing chronic pain following surgery and provide a range of multidisciplinary services to reduce the risk (e.g., the Transitional Pain Service at Toronto General Hospital, and similar service models in Alberta, British Columbia, and Quebec). Participants also noted the importance of extended pain management care to children, teens, and their families who are recently discharged from the hospital or following painful procedures, such as surgery, citing the example of the Transitional Pain Service at SickKids in Toronto, which aids in the transition from post-surgery to community-based care.
Centralized and clear referral pathways increase awareness and access to resources
Participants spoke about the value of creating clear assessment and referral pathways for use by people living with chronic pain and their partners in care. Centralization and single-source coordination of referrals localizes all information in a single place. Such pathways are easier to navigate because they offer a single window for assessment, which may involve multiple professionals, increase patient and clinician awareness of the resources available, and assist patients in accessing those resources. The Toronto Academic Pain Medicine Institute (TAPMI) was cited as an example where all referrals for adults with pain are first sent to TAPMI, which then coordinates these referrals and triages to appropriate professionals across Ontario. Participants identified the value in delivering centralized referral programs both in-person and online to maximize their usefulness and availability.
"Becoming a Pain Management Coach and Senior Peer Support has given me a lot of hope and courage that my experience matters and that I have valuable knowledge and experience in managing my own pain and my mental health."
Questionnaire Respondent
Elements of an improved approach to pain care access
Enable the health system to provide patient-centred care, which addresses the multi-dimensional nature of pain
There was wide agreement that understanding the unique needs of people living with pain is central to improving access to pain services. By taking into consideration the unique personal histories of patients - their diverse backgrounds and origins, medical needs, exposures to adverse situations and trauma, and their individual coping mechanisms and varying degrees of resilience - health professionals can better support people living with pain using a biopsychosocial approach.
Participants resoundingly called for the inclusion of people living with chronic pain in the development of policies, processes, and standards, to assist in disseminating best practices across Canada. This can be accomplished by including people living with pain in research and study design, in initiatives to bolster primary care capacity, and by fostering connections and facilitating networking between patients to encourage peer support, collaboration, and planning of next steps in individuals' care trajectories. We also heard calls for more innovative and inclusive measures to ensure that care is culturally informed and accessible, including making available Indigenous traditional medicine in the health system and coverage for care and associated expenses, and improving access to community-based programming, which accounts for the unique needs of different cultural and socio-economic groups.
People living with pain told us they recognize their role in managing their pain, but noted they do not always know where to go for tools and resources to support their care trajectory. Overall, participants supported additional actions to increase awareness among patients and clinicians alike of available self-management resources, and to improve access to those resources, including dedicated support workers to help patients navigate the health system.
Participants noted how important it is to hear from and be supported by others who have experienced or are currently experiencing similar challenges. Community and peer-led support groups for people with chronic pain were seen as a way to help increase awareness and access. Pain BC and l'Association québécoise de la douleur chronique (AQDC) were highlighted as examples of provincial organizations offering support groups, patient networking opportunities, and resources for people with lived or living experience with pain. It was stressed by many participants that self-management resources should be provided at no cost and be available in multiple languages.
Improve coordination and implementation of innovative models supporting multidisciplinary and tiered care delivery
We heard that better coordination, connection, and sharing of information across the various places where people are receiving pain care would improve access and outcomes. The collection, evaluation, and sharing of data on best practices would help to enable the creation of standardized clinical practice guidelines and care services. Participants also called for expanded and early multimodal pain care, which includes a variety of professions and expertise in community clinics and primary care teams. This should be organized using a stepped- or tiered-care model, with clear referral pathways, particularly for cases involving multiple or complex needs, and include navigators (such as a person or an algorithm) and centralized intake and triage hubs. More work should be done to link and monitor such teams across Canada to better understand what types of models work best for whom, when, and under what circumstances.
Several participants noted the need to reinforce the capacity of primary care providers to prevent and manage pain, as they are the first line of care for most, and in the long term, most people are referred back to their primary care provider for the remainder of their treatment after assessment and care by a pain specialist. Primary care providers should receive enhanced training and education to identify pain before it becomes chronic and to be able to refer patients to interventions such as physical or manual therapy and counselling while they wait to see pain specialists. Additionally, questionnaires and algorithms could be used to develop new protocols, which help to identify risk factors for pain within primary care settings. Appropriate pain management and care should be provided as early as possible, with action on acute and transitioning pain before it becomes chronic and before the development of other possible co-morbidities associated with pain, such as depression and potential problematic substance use.
Remove financial barriers to care through improved and innovative funding structures
Future efforts to improve access to pain services should focus on simultaneously building human resource capacity to prevent, diagnose, and treat chronic pain, while also building system capacity to manage complex cases involving concurrent pain, mental health disorders, and substance use disorders. Several participants called for enhanced funding for currently non-insured services for people living with pain, such as physical therapy, massage therapy, dental care, and counselling. In some cases, pain care services may be partly or fully insured for Canadians in certain jurisdictions and under certain conditions as part of public plans, however improved standards for publicly insured services are necessary to reduce disparities.
There were many recommendations during our consultations to change the current remuneration models for clinicians in Canada to recognize chronic pain as a distinct disease and to remove the disincentive to see patients with complex needs who often require longer appointments. Participants noted that complex care fee codes exist for many other chronic diseases and this could serve as a basis from which to build. Change could include pain specific billing codes and implementing remuneration models for clinicians that account for interprofessional care.
"Money is a huge barrier. Almost all treatments for pain that are not just doctor-prescribed drugs are expensive and not affordable to most. Spending $100 to get a massage for an hour is not affordable."
Questionnaire Respondent
Provide Pan-Canadian coordination and leadership through a national pain strategy or other supporting mechanisms
Recognizing that chronic pain crosses many service settings and professions and impacts our economy and society beyond just the health system, participants stressed the need to acknowledge pain as a legitimate chronic condition and public health priority and called for strengthened leadership from both the top-down (e.g., government and health authority acknowledgement and dedicated investment) and bottom-up (e.g., health professional champions, and mobilization and leadership by people with lived experience). They acknowledged the efforts of several provinces to develop provincial pain strategies and are looking for national leadership to provide a unified, national approach to pain and to address geographical inconsistencies in care. They also called for greater reporting and accountability mechanisms such as a national report card to assess jurisdictional actions and an accreditation mechanism building on standards set by Health Standards Organization - Accreditation Canada and other similar bodies.
Participants noted the Task Force has helped to create connections between provinces and territories but they would like to see a formal mechanism to lead this coordination in a more substantive and sustainable way. Pain-specific funding is seen as critical to enable implementation of any strategy put forward.
"A provincial strategy should ensure that, whether you're an infant, a person with fibromyalgia having surgery or a 50-year-old with end-stage cancer, health care professionals speak the same language around pain and have the necessary tools and support to treat it properly."
Questionnaire Respondent
Rapid review: Preventing transition of acute to chronic pain
Acute pain typically results from an identifiable cause (e.g., injury, surgery) and occurs for a short duration. It serves as a protective factor and typically responds well to analgesics, anti-inflammatories, and other modalities. When acute pain persists beyond 3 months, it has transitioned to chronic pain. A rapid review of summary literature and clinical practice guidelines was conducted through the Drug Safety and Effectiveness Network (DSEN) to determine the best practices for reducing the risk of acute pain transitioning to chronic pain after injury or surgery and what factors increase or reduce the risk of transition to chronic pain.
Potentially generalizable recommendations and interventions to reduce the risk of transition from acute to chronic pain encompass a variety of treatment options. Physical/active interventions (e.g., exercise, manual therapy) and multimodal care (e.g., manual therapy, exercises, and education) were recommended for acute neck pain for whiplash patients. Provision of educational material, psychological support, active perioperative psychological intervention (e.g., cognitive behavior therapy or relaxation therapy) were recommended for concussion patients and adults more generally. Pharmacological treatment recommendations included multimodal analgesia including options such as intravenous ketamine, intravenous lidocaine, and local/regional anaesthesia dependent on the condition / procedure. It was recommended that patients already taking opioids and undergoing surgery, be referred to a perioperative pain specialist to tailor an opioid and pain management plan for both the in-hospital stay, and for transitioning home. Recommendations also include broader methods around how care is delivered, such as screening for risk factors of transition from acute to chronic pain, monitoring specific symptoms in certain conditions (e.g., in cases of concussion), and referring to interdisciplinary teams or specialized services for certain conditions if there is slow recovery or additional symptoms (e.g., depression) develop. The available evidence suggests multidisciplinary approaches should be taken to reduce the risk of transition to chronic pain, but additional approaches that can be generalized across different conditions are limited. Therefore, a patient-centred model of care with individualized treatment tailored to the patient's condition (e.g., type of surgery or trauma) is necessary, and research will need to identify effective treatment strategies within specific patient conditions and for specific patient risk factors.
Understanding the risk factors for acute-to-chronic pain transition is the first step in prevention. In several included reviews, pain catastrophizing and parental catastrophizing in adolescent populations were found to be associated with poor/non-recovery or chronic pain development, especially following surgery (Burns et al., 2015; Khatib et al., 2015; Samoborec et al., 2018; Theunissen et al., 2012). Several other psychological factors were also identified, including poor recovery expectation, post-traumatic stress disorder, symptoms of depression or anxiety, expectancy and causal beliefs, acute stress response, pain-related emotions, pain coping efficacy, mood, and mental health status (Khatib et al., 2015; Pinheiro et al., 2016; Rabbits et al., 2017; Samoborec et al., 2018). Many reviews found evidence of strong associations between severity and duration of previous pain experiences, acute pain post-injury, or pain perioperatively and development of chronic pain or poor recovery from injury (Rabbits et al., 2017; Samoborec et al., 2018; Verwoerd et al., 2019; Wang et al., 2016). Adequate control of acute pain through pharmacological, physical, psychological, or multimodal interventions is imperative to reduce the risk of transition to chronic pain.
The impacts of psychological risk factors and acute pain are potentially modifiable through interventions. For example, acceptance and commitment therapy or mindfulness-based interventions may be considered to improve outcomes through reduced pain catastrophizing (Trompetter et al., 2015; Dorado et al., 2018). However, many biological and social risk factors are less amenable to intervention, including female sex, age (younger or older, depending on the condition), BMI, employment- and disability-related factors, sickness absence or health-seeking behaviour, and low education level (Ding et al., 2018; Samoborec et al., 2018; Verwoerd et al., 2019; Wang et al., 2016). Awareness of the biological and social contributors influencing pain transition may facilitate identification of patients that may benefit from more frequent follow-up and early intervention.
Incorporating a biopsychosocial approach to pain management, which accounts for the complex interaction of risk factors that may influence the transition to chronic pain, could aid in reducing the risk of chronic pain. However, there are considerable gaps in available evidence and the evidence that is available often approaches pain prevention in different, not always comparable ways. Future research should focus on determining which interventions work best for whom, under what conditions, and for what type of pain or clinical condition to establish a more tailored patient-centred approach.
Awareness, education, and specialized training for pain
In our first report, we highlighted the need for pre-licensure education, continuing professional development, and better integration of sufficient, pain-specific learning into curricula to provide health professionals with the knowledge and skills they need to prevent, assess, and treat pain. We noted the use of common learning resources and outcomes across disciplines would reduce disparities and improve quality assurance of training programs. We called for additional collaborative learning experiences in recognition that effective pain management is often complex and requires a range of treatment modalities and approaches beyond the expertise of any one profession.
We also emphasized the importance of increasing public awareness to help Canadians better prevent and manage pain, and to shift attitudes contributing to the stigma and discrimination experienced by those living with chronic pain. We recommended activities be coordinated, trauma and violence-informed, and sensitive to different social and cultural needs. In addition, they should target multiple populations and settings as well as leverage lessons from existing efforts. Our consultations confirm and reinforce these findings, with a general consensus that people living with pain, health care professionals, and the wider community need to be more empowered, knowledgeable, and supported to understand, prevent, and manage pain.
Gaps and challenges
Canadians lack understanding and awareness of pain, its impacts, and options for prevention and management
Our consultations confirmed the level of public awareness and understanding of pain in Canada is insufficient to meet the needs of people living with pain and their families and to address the stigma they often face. Many individuals who live with pain experience stigma - especially those with pain conditions that do not produce external symptoms others can see (pain itself is invisible), those who cannot work because of their pain, and those requiring opioids to manage their pain. Such discrimination is in part due to a general lack of awareness and understanding of chronic pain as a legitimate disease, as opposed to acute, which is a symptom. This can lead to feelings of despair and worthlessness, reduced sociability, and act as a deterrent to seeking treatment. Many people who do seek treatment told us they do not feel supported by their physicians and instead often feel dismissed, unheard, and discouraged. The lack of public awareness of pain in Canada also undermines efforts to reduce some of the underlying causes of chronic pain, such as certain lifestyle behaviours.
"I feel like nobody believes the pain that I am suffering every day. I do not feel my doctor and specialists really care. They bounce me back and forth between appointments between them. I am very frustrated with the doctors not spending time with me to listen to my concerns and pain. I feel like they do not believe me and do not want to spend time with me."
Questionnaire Respondent
There is limited education on the full spectrum of pain and patient-centred approaches
Participants told us health care professionals need to be better educated on pain mechanisms, manifestations, and treatment, including the non-medical aspects of pain management. Chronic pain needs to be understood within a biopsychosocial framework as a complex chronic disease.
Pain education that does exist often focuses on building the technical skills required to diagnosis and treat pain related conditions. While it is important to ensure that clinicians have such skills, participants emphasized the importance of supplementing this training with education around models of patient-oriented care. For example, participants noted the value in building knowledge of supportive care practices, which includes violence and trauma-informed care, anti-racist approaches, and culturally appropriate practices. We also heard the way pain education in Canada is presented, often does not focus on the value and unique contributions of clinicians in helping people work through complex challenges nor does it entice students to enter the field, which can add to the lack of pain-focused professionals.
There is limited information and understanding of what supports are available for pain
Participants felt many health professionals, and in particular primary care providers, are often unaware of the full spectrum of available treatment options, resources, and tools for self-management. This has led to many professionals feeling underprepared to assess chronic pain, to educate patients adequately, or to utilize recommended treatment modalities other than medication. Even when professionals recognize their limitations, participants noted it can be difficult to stay up to date with current information and the resources available across an often fragmented set of care systems. Health care professionals more generally also noted the difficulty in being able to find time in their schedules to undertake additional training on pain.
"I believe that the biggest barrier and challenge is the stigma that is related to those living with chronic pain. Many people in the community do not have adequate knowledge of what chronic pain is and how it affects those who live with it. Another challenge to managing pain, not only in our community but all communities, is that there is a misconception of opioids and people living with chronic pain. The majority of people living with chronic pain are not drug [users] looking for opioids."
Questionnaire Respondent
Inefficient knowledge mobilization and duplication of educational initiatives
Institutions across the country have embedded more pain science into curricula, established clinical supports, tools, and continuing education programs to fill gaps in the current education, awareness, and understanding of pain and pain management. However, participants noted a great deal of duplication and inadequate knowledge mobilization to encourage uptake and spread of pain science and awareness of pain mechanisms and options for management. More coordination is required to avoid duplication, extend reach, and realize impact.
Best and promising practices
Stakeholders provided many examples of initiatives across the country they believe are helping to address challenges related to pain awareness, education, and training. The main characteristics of these practices include:
- Public awareness and public education initiatives;
- Provincial and national networks to connect speciality and primary care;
- Institutionally based leadership and infrastructure;
- Development of joint and interfaculty training initiatives and competency development;
- Activities to increase care clinician awareness and understanding of the patient experience;
- Clinical decision-making tools and resources;
- Resources and tools specific to the use of opioids;
- Online and in-person self-management programs; and,
- Peer-support networks, organizations, and tools.
Individual practices provided in this discussion are not comprehensive but rather representative examples and illustrative of the principles heard during consultations.
Pain awareness and public education initiatives are helping to improve knowledge and reduce stigma
Information campaigns can educate the public and raise awareness and understanding of the value and role of acute pain and how this differs from the experience of pain as a chronic condition or disease. Participants felt large scale, national knowledge mobilization campaigns have the potential to reach large groups, particularly through social media platforms. They also assist in shifting research into practice, increasing awareness and decreasing stigma through myth-busting and evidence-based education. Furthermore, effective knowledge mobilization activities can amplify and spread information to the public, which is easy to locate, understand, and share. These strategies can also be leveraged to explain the important social, economic, and societal impacts and costs pain places on individuals, families, and providers in ways that make sense to general audiences. As such, participants stressed that any public awareness campaign must ensure all materials and information produced is respectful of and tailored to different social and cultural populations, contexts, and situations.
National Pain Awareness Week, an existing yearly initiative was identified as a opportunity to better leverage and amplify pain networks and organizations, which have a large advocacy presence on social media and foundations in pain education (e.g., Solutions for Kids in Pain, the Canadian Pain Society, Pain BC, and Association québécoise de la douleur chronique). Such networks and organizations can help to share information on the experience of living with chronic pain as well as tools and resources designed to translate clinical knowledge into more easily digestible formats for the public (e.g., patient and clinician tools developed by the Canadian Agency for Drugs and Technologies in Health).
Provincial and national networks are helping to connect speciality and primary care
Participants stressed the importance of primary care networks and actions to unify specialized knowledge across health authorities and primary care settings. Such connections help ensure standardization, knowledge dissemination, networking, and collaboration and ultimately build capacity for care. Participants identified examples of projects employing such approaches by using e-platforms to connect primary care clinicians and patients to specialized health care clinicians, services, and resources, and to provide guidance from dedicated care coordinators to patients who require assistance in navigating available services (e.g., Technology-Enabled Collaborative Care for Youth). Consultation participants also acknowledged the importance of e-platforms and tools to build communities of practice and forums for enabling knowledge transfer across jurisdictions, sharing of practices, and facilitating connections between specialists and primary care providers (e.g., Atlantic Mentorship Network for Pain and Addiction, Ontario's and British Columbia's Project ECHO - Extension for Community Healthcare Outcomes and Mentoring Program for Mental Health, Addiction, and Chronic Pain). Participants suggested identifying champions who can help move away from ownership of care to understanding care as a team effort with needed support across professions and care sites.
Institutionally based leadership is building capacity, sharing practices, and creating quality improvements through broader organizational change
Broader organizational change and strengthening embedded practices can create more extensive quality improvements within organizations and institutions. For example, recognizing that accreditation programs help to standardize pain care, participants noted pain was a major priority at the institutional level at pediatric hospitals, such as Alberta Children's Hospital or SickKids in Toronto, when they decided to seek the international ChildKind designation. ChildKind certifies an institution's commitment to comfort and address children's pain, establishes communities of practice, and provides resources and tools on best and promising practices. Not only has this initiative resulted in extensive education of health professionals working at pediatric hospitals, it has also assisted provinces in rolling out services based on learnings from the certification process and expanding access to the resource repository. Participants called for more detailed institutional accreditation initiatives led through Health Standards Organization - Accreditation Canada, or adjustment of the ChildKind designation, tailored to adults, which could be used across the country.
Joint and interfaculty training initiatives and competency development enable interprofessional care
Participants cited a range of programs working to support training programs across disciplines and professions in academic institutions across Canada. Whether through undergraduate, graduate, or continuing medical education, such programs are focusing on teaching evidence-based clinical practice with an interprofessional perspective by including professors and students from across medicine, nursing, occupational therapy, pharmacology, physical therapy, psychology, and related disciplines in the same training environment. Such work is building a knowledge translation-oriented community across faculties and breaking down traditional siloed education (e.g., University of Toronto's Interfaculty Pain Curriculum, University of Saskatchewan Centre for Integrative Medicine, University of Calgary and Calgary Chronic Pain Centre, University of Regina, McGill University, and Université de Sherbrooke).
Consultation participants stressed the importance of having a unified pain curricula and common competency framework for undergraduate and post-graduate medical students, coordinated across universities and education institutions. A promising example noted was the Association of Faculties of Medicine of Canada (AFMC) which, in partnership with Canada's 17 medical schools, is creating a national, bilingual, comprehensive, and competency-based curriculum for undergraduate medical students in pain management and substance use. The evidence-based training aims to fill gaps in undergraduate educational programs across Canada, including the diagnosis, treatment, and management of pain. The AFMC will also develop a repository of questions and oral practical structured clinical examinations, which could be included in the national licensing examinations of physicians in Canada. Similar initiatives for other professions were also cited as examples, including projects designed to build capacity for future nurses, pharmacists, and social workers (e.g., Empowering The Next Generation of Health Care and Social Service Professionals with Knowledge, Skills, Tools and Supports to Address Substance Use Issues in Canada). Participants also noted the interprofessional competences for pain education, Pain Curriculum Outline, and competencies for individual professionals created by the International Association for the Study of Pain (IASP) as important frameworks that could be leveraged in Canada.
Initiatives working to increase clinician awareness and understanding of the patient experience
For people living with chronic pain, having their experience acknowledged and validated can positively affect interaction with health care professionals and ultimately a patient's care trajectory and outcomes. This form of support builds a stronger patient-clinician relationship and can restore or build trust in the health care system. Participants cited programs where health science students and professionals complement their clinical training with activities designed to bring people living with chronic pain into the learning environment to share their experiences. Participants also felt students should be instructed on how to take on the role of a "helper" (rather than "fixer") in the care of patients.
"I wish I had a pain clinic that could consist of a team of medical professionals including counsellors and physio that would work as a collective on a single patient to try to integrate all the different issues I am facing to create a treatment plan. As it stands, I have so many different specialists telling me all different diagnoses and therefore no clear treatment plan that helps in a holistic way.
…I dream of having a professional who is my pain specialist who helps me navigate through things and builds a treatment plan with me, as constantly advocating for myself when I am already in pain is exhausting."
Questionnaire Respondent
Clinical decision-making tools and resources are improving capacity and confidence
There are a wide range of initiatives across Canada aimed at helping to make pain-related care decisions. Some operate in specific locations while others are regional or national in scope. They include reference documents, guidelines, training modules, and mentoring opportunities. Standardized clinical tools, policies, and processes grounded in evidence, as well as actions to promote system-level educational standards, were all identified as successful practices by participants in our consultations. These actions help to standardize care, create a common understanding and awareness of pain, and benchmark pain education across institutions. Overall, such work helps to create a unified approach to pain prevention, assessment, diagnosis, and management. For example, pain focused Health Quality Standards developed by Health Quality Ontario, were noted as clinical tools that outline a standard level of assessment and care for professionals.
Participants also noted several other tools working to standardize pain care by:
- Providing continuing education opportunities focused on building foundations in chronic pain management, including online courses, workshops, and virtual learning platforms (e.g., Pain BC's Pain Foundations Online Course).
- Improving knowledge and capacity to treat the unique needs of specific populations, such as children (e.g., SickKids Online Paediatric Pain Curriculum);
- Building capacity in primary care settings so clinicians are aware of available resources and tools related to pharmacological, physical, and psychological pain treatment options (e.g., Centre for Effective Practice, Primary Health Care Opioid Response, Canadian Chiropractic Guideline Initiative, RxFiles Academic Detailing);
- Adapting institutional processes and approaches (e.g., triage, patient chart reviews) to recognize the unique needs of pain patients; and,
- Improving knowledge around the utility of diagnostic tests and treatments, to reduce unnecessary procedures and improve patient outcomes (e.g., Choosing Wisely Canada).
Provincially, there has been work to better support health systems in addressing pain. In Quebec, for example, materials developed by the Ministère de la Santé et des Services Sociaux (MSSS) help physicians address long waiting lists by prioritizing which patients to see first. Online pain care guidelines help clinicians make evidence-based decisions about patient care. Many pharmacists in Quebec are now trained in recognizing and addressing pain, allowing them to support the care of people living with pain and easily accessible e-learning modules and online training support the continuing education of other health care professionals on pain prevention and management. In Alberta, health professional organizations such as the Pain Society of Alberta and the Alberta College of Family Physicians, provide prescribing guidelines, opioid management resources, and general practice tools, and mentoring is facilitated by the Alberta Collaborative Mentorship Network for Chronic Pain and Addiction.
Clinical practices for the management of pain - reflecting on the state of reviews and guidelines
Multidisciplinary pain care is considered the optimal method for the treatment of chronic pain (Pain Clinic Guidelines Task Force, IASP). Many reviews to date have examined multiple and diverse care options, which span across pharmacological, psychological, exercise/rehabilitative, medical device/procedural, practitioner administered/manual, and self-management interventions. The availability and quality of evidence around the effectiveness of any individual therapy for addressing chronic pain is limited and most studies are limited to specific types of pain and rarely compare individual interventions to one another and/or to inventions in combination. There are many international reviews of clinical treatments for individual pain conditions. In the US, the Pain Management Best Practices Inter-Agency Task Force has produced an extensive review of pain management interventions and the Agency of Healthcare Research and Quality has several publications on pain management and opioid medications. In the UK, the National Institute for Health and Care Excellence (NICE), is creating a guidance for chronic pain, which has involved extensive reviews of various interventions. In Canada, the Canadian Agency for Drugs and Technologies in Health (CADTH), has an extensive set of evidence on pain management, which included rapid responses, scans, and reviews of most clinical treatment options. This large body of review literature provided by educational institutions, health authorities, professional bodies, and non-government organizations is lengthy and difficult to traverse. Subsequently, it is challenging to access empirically informed guidelines for both supported and unsupported clinical practices. The majority of this work does not identify a universally efficacious treatment for all pain conditions or patient-related factors. As a result, care will vary based on the individual, and options must be discussed and weighed carefully through shared decision-making by people living with pain and their health professionals.
Resources specific to opioid prescribing are improving education and training
Participants identified many examples of projects working to create and disseminate education and training on the use of opioids for pain management, as well as clinical guidance tools for pain and co-occurring conditions (e.g., substance use disorder). Broadly, there have been innovative approaches to training for physicians, nurse practitioners, and pharmacists involved in chronic pain management and opioid prescribing. Many involve online platforms and self-learning modules, which have contributed to capacity-building in this area and encouraged the uptake of clinical guidelines (e.g., McMaster University's Opioids Clinical Primer and Safer Opioid Prescribing, the Saskatchewan Health Authority Opioid Stewardship Program, and the Northern Ontario School of Medicine Overcoming Barriers to Safe Opioid Prescribing online learning module).
"Self-Management BC is an amazing course provided through the University of Victoria and supported by the Minister of Health. In Ontario, my doctor sent me to a rehab program that was very helpful to learn ways to deal with my pain. When I moved to BC, I learned about this free program. Six weeks, 2.5 hours once a week, free book and you learn how to manage your pain on your own, how to work with doctors, how to advocate for yourself, some thing you could do to decrease your pain, how to communicate with others, etc. Family members can attend as well to better understand someone in their life. This program has made a tremendous difference for me in being able to self-manage my pain. And a doctor's referral is not necessary to be in the program. In addition, volunteer facilitators have been invited to webinars which help us and those we would like to help"
Questionnaire Respondent
Online and in-person self-management programs are empowering people to take ownership of their pain management
People living with chronic pain stressed the importance of self-education about pain management, and want more opportunities to share their experiences and to help others also living with pain. Online self-management programs that can be delivered directly to patients in their homes were seen by many participants as successful initiatives helping to fill the gap in access to self-management and building capacity among health care professionals to support people living with chronic pain. Such resources can be delivered while people are waiting for specialized care and in the current context of the global COVID-19 pandemic, they are ever more important. Participants identified several examples of self-management programs, which employ:
- Virtual hubs to connect people with guidance and support using service directories, educational and supportive resources, and online programming (e.g., Bridge the gApp);
- Online self-management programs supporting chronic disease management in general as well as offering pain education and self-management strategies (e.g., Ontario's Online Chronic Disease Self- Management Program, Living Well, and TAPMI's Pain U Online platforms, Nova Scotia's Chronic Pain Self-Management Program, and British Columbia's MyCarePath).
- In-person group workshops providing attendees with coping and self-management skills and strategies for chronic pain and other chronic conditions; often co-led by trained leaders who have been personally impacted by chronic conditions (e.g., Alberta's Better Choices, Better Health - Chronic Pain workshops, and Newfoundland and Labrador's Improving Health: My Way program).
Peer-support networks, organizations, and tools are essential
People living with chronic pain are often looking for guidance and mentoring from people who have lived through similar experiences. Peer-support programs and networks connect individuals with others impacted by similar conditions to share experiences, provide support and acknowledgement, develop life skills, identify self-management resources, and share consistent goal-setting messaging with a strong support system. Peer support and mentorship programs also help patients and their families navigate their journey through the health care system. Consultation participants noted the importance of peer-led online and in-person support groups and telephone lines. Such initiatives help to connect individuals to supports to share mutual experiences and understanding, assist with system navigation, and pain management self-care (e.g., the Association québécoise de la douleur chronique peer support groups and provincial peer support line, Pain BC Pain Support and Wellness Groups, Coaching for Health, Making Sense of Pain/Making Sense of Pain for Indigenous Peoples and Pain Support Line, or Help_AB online, telephone, and in-person supports).
Participants noted peer support and mentoring among clinicians are also important activities. They cited examples that offer peer and social support in a trauma and violence-informed manner and coordinate mentor-mentee matching across jurisdictions (e.g., the SickKids peer-to-peer support program, the Canadian Physiotherapy Association Pain Science Mentorship Program).
Elements of an improved approach to pain awareness, education, and specialized training
Build awareness through investments in public education
Participants noted a large-scale, unified public awareness and education campaign would help immensely to build a basic understanding of pain, reduce stigma (particularly around the use of prescribed opioid medications and other pharmaceuticals to manage pain), and promote education around the mechanisms of pain as well as available resources for pain management. A national pain awareness campaign should also disseminate information on the intersection of pain, mental health conditions, and substance use, given the high prevalence of co-morbidity amongst these conditions. The highly successful Bell Let's Talk campaign was described as a promising example upon which to model a pain awareness campaign. This can be done by leveraging communities, networks, and stakeholders not necessarily primarily focused on pain but with a vested interest and established social media and public awareness presence (e.g., insurers, major employers, other industry stakeholders). The role of the federal government in increasing awareness of pain and pain management was also noted by several participants who pointed to previous federal campaigns that have had a positive impact on changing attitudes toward other public health issues (e.g., use of seat belts, concussion prevention, smoking cessation). Support of a pain-focused campaign by federal and/or provincial and territorial governments might assist in extending the reach of such a campaign.
To reach the widest possible audience and to have maximum effects, it was suggested a campaign should span industries, systems, and health care professions, as well as sub-populations, and leverage support from pre-existing organizations that have a large advocacy presence on social media and foundations in pain education (e.g., Solutions for Kids in Pain, the Canadian Pain Society, Pain BC, and Association québécoise de la douleur chronique). Several participants believed that explaining the neuroscience of pain to the public could be done through a large-scale, national awareness campaign, and offers huge potential for significantly increasing understanding and awareness. Such work could also help publicize resources and tools for people personally impacted by pain. The public should also receive information on basic strategies for preventing acute pain from becoming chronic. One way to do this would be to include basic pain concepts, neuroscience, and prevention and self-management strategies in health curricula in primary and secondary schools and in workplace safety training.
Many consultation participants voiced support for a heightened focus on wellness, fitness, nutrition, and mental health in the context of pain. Presenting children and youth with basic pain concepts and introducing pain into the curricula of K-12 education would create foundational knowledge and awareness, which could assist in not only shifting societal acceptance and understanding of pain more broadly, but also play a role in pain prevention. Participants also recommended educating children and teens at school about the benefits of an active lifestyle and educating the public about basic preventative strategies for pain, as this could mitigate the need for pharmacological interventions.
Public education and awareness should be culturally safe, trauma and violence-informed, translated to multiple languages, and comply with accessibility standards (e.g., go beyond written form and include videos, infographics, and other media). Participants also cautioned that the health system and clinicians must have the capacity, resources, and infrastructure to ensure access to the tools, supports, and services disseminated and highlighted within the campaign for those who choose to seek care and support.
"I appreciated the non-medicinal techniques I learned at my local pain program at the hospital. We learned about breathing exercises, meditation, body scans, laughter, gratitude, and had an option of pool therapy and a specific physical therapy program to get core muscles back to working."
Questionnaire Respondent
Create balanced public messaging around the benefits and harms of opioids
There should be balanced public messaging about the benefits and potential harms of opioids, as some participants noted that actions to promote appropriate opioid prescribing in Canada have had unintended consequences on people with chronic pain, such as increased stigma and additional barriers to receiving care (including prescription opioid medications). Balanced public messaging would support patient-centred opioid prescribing through mutual patient-clinician decision-making, which is based on the unique needs of each person. Incorporating the experiences and collaboration of individuals with pain into the development of public messaging could be a strategy by which to obtain the desired tone of balanced messaging.
Invest in accessible self-management to empower people living with pain and reduce service gaps
Participants emphasized that much more needs to be done to improve self-management resources throughout Canada and to make them more accessible. This includes ensuring materials and resources are available in a range of languages. More should be done to educate people on acute and chronic pain definitions, the range of biopsychosocial and cultural factors that contribute to pain, and available resources and supports. Easily accessible and clear information on available supports and resources, as well as navigation of pathways to care, would improve experiences of people in pain and those who care for them.
Several participants recommended the creation of a smartphone app (or apps) to help people living with pain to locate services. As well, participants suggested a "map" of available information and an inventory of resources, along with toolkits and pain-tracking apps, that could facilitate better patient-clinician communication. It was noted one goal of enhanced availability of and access to self-management tools and resources should be to shift the focus - for patients and clinicians - from reducing or eliminating pain to improving each patient's functioning and quality of life.
Participants also emphasized that is it not enough to simply provide a list of resources. Self-management resources, apps, and other tools must also be accompanied with practical supports to help manage the many dimensions of pain. Such supports as peer groups, coaching, and guidance focused on skill development are all active and practical things often cited as needs by people living with pain.
"Often pain treatments are available, however, it takes a great deal of individual effort and knowledge and determination to 'ferret' out treatment options and drive one's own health care. There are many people who do not have the ability or capability to drive their own processes and treatments. Greater easily accessible information resources at and with health care professionals, clinics, libraries, community centres and online is necessary to support this."
Questionnaire Respondent
Build capacity among all health professionals through better pre- and post-licensure education on pain
It was widely agreed all health professions that are part of the pain landscape (e.g., family medicine, surgery, pharmacy, psychology, physiotherapy, occupational therapy, chiropractic, social work, dentistry) should be educated on pain as a disease and how to apply knowledge about pain in clinical practice. Such training should be integrated into all aspects of health education rather than just as an area of specialization and should be embedded within both pre-licensure and continuing professional education. Furthermore, pain education or training should extend to all who have the potential to be the first point of contact or entry way to different health care settings (e.g., first people to interact with patients such as triage nurses, receptionists, medical office professionals, physician assistant, or homecare aids), as their interactions with patients may positively or negatively influence their pain experience and trust in the health care team.
Participants commented on how joint training initiatives foster knowledge of pain and encourage interprofessional collaboration approaches to prevention and management. Exposing students and professionals to different types of pain care options is paramount for improving pain education and training. Educating about the different roles each professions can play can facilitate multidisciplinary approaches to pain care, ensure students understand the full spectrum of pain care, and demonstrate opportunities within the pain care field. It was also suggested there should be more emphasis on pain knowledge in the testing, licensing, and regulation of health care professionals, including national standards that include a holistic approach to pain and violence and trauma-informed principles.
All participants said there must be an increased understanding amongst clinicians, as well as people living with pain and those who care for them, about the range of pharmacological, physical, psychological, and self-management treatment options, as well as their effectiveness and risks, so that patients and their carers can choose how to manage their pain with a sense of autonomy. To establish quality, base-level pain understanding, assessment, and management, education and training must be comparable and standardized across institutions and jurisdictions to reduce misunderstanding and stigma, and create a common language and understanding across disciplines and professions. Participants suggested the creation of standardized clinical practice guidelines for all pain clinics receiving funding through Ministries of Health. Such guidelines should also include approaches to data collection and analysis and evaluation to enable the identification and spread of best practices. This is particularly important for pain specialist services, as credentialing and certification is not standardized. Additionally, institutional leadership and focus on culture change have the ability to improve care and patient outcomes overtime.
Educate clinicians on the importance of social, cultural, and spiritual factors and different ways of knowing
Participants noted the importance of respecting and understanding culturally-based knowledge systems and different ways of knowing. Respecting the role of social, cultural, and spiritual factors in shaping the pain experience and helping to manage it would enable more culturally appropriate care for individuals of various cultures, backgrounds, and experiences (e.g., new Canadians, refugees, and immigrants who may have different understandings and approaches to pain). For example, in some Indigenous languages, there is no word for pain. This can limit one's ability to express their experience, add to the complexity of interpreting symptoms and conditions by care professionals, and must be taken into account. Participants also emphasized the importance of Indigenous knowledge systems and practices, other traditional knowledge systems and practices (e.g., traditional Chinese medicine; ayurvedic medicine), and approaches that incorporate spirituality, ceremony, mindfulness and breathing exercises, coaching, and other approaches outside the traditional biomedical model.
We heard calls for holistic approaches to pain care training, which would allow clinicians to increase their awareness and understanding of the patient experience in addition to enhancing their technical skills in pain. This could include training on rapport building, collaborative practice, cultural safety, Indigenous and other ways of knowing, supporting patient needs, and motivational interviewing (a form of counselling that supports individuals to use their own desire and drive to create behavioural change).Footnote 2 This form of support builds a stronger patient-clinician relationship and can restore trust in health professionals. Furthermore, pain education must be grounded in violence and trauma-informed care, taking into account past adverse events, trauma, and systemic roots of marginalization, such as colonialism, racism, and prejudice. Clinicians must be able to recognize and understand how these factors affects an individual's whole being and how creating safe environments is critical to managing pain.
Enable peer support and mentorship to reduce isolation and improve outcomes for patients and clinicians
Participants emphasized the need for more peer-support programs and networks to connect individuals together, share experiences, provide support and self-management resources, and share consistent goal-setting approaches. Peer support and mentorship programs are also critical for helping patients and their families navigate their journey through the health care system
Participants agreed health professionals need additional mentorship programs, academic detailing, communities of practice, and online platforms and groups to share information and to learn from and support each other. Participants also believed including mentoring opportunities and real-life applications in pain training would help pain education initiatives result in real-world impact. Initiatives are needed to support clinicians in knowledge transfer and cross-discipline learning, and to encourage skill development through education and mentorship. Using models that connect people together, learn from successes, and share best practices has the potential to meet this need.
"…all regulatory health organizations and advocacy groups ought to propagate a standardized position statement on pain, its prevention and management, to both the public and health care providers."
Questionnaire Respondent
Pain research and related infrastructure
Our first report identified the need for more research to understand key aspects of pain and to translate basic discoveries and mechanistic insights into safe and effective pain prevention and management strategies. We noted Canada's pain research activities are a key part of a global pain research ecosystem and, given the breadth and scope of the pain research agenda, it is important to identify research priorities where Canadians can continue to excel and leverage the strengths of their existing programs.
Between 2007-08 to 2018-19, the Canadian Institutes of Health Research (CIHR) invested $177.3M in a total of 834 pain-related research grants and awards, across the four themes of CIHR-funded research. The themes and their funding amounts were: Biomedical ($63.4M, 127 grants, 108 awards), Clinical ($44.5M, 141 grants, 187 awards), Health Systems and Services ($21.4M, 45 grants, 46 awards), and Population and Public Health ($10M, 36 grants, 49 awards). An additional 95 projects ($38M) were considered multi-themed. The majority of funds were awarded through CIHR's Project Grant competition ($114M) with $42M through targeted strategic priority competitions.
While we noted that significant research investment is concentrated in basic sciences or clinical trials, there is a need to examine the effectiveness of pain prevention and treatment interventions offered by primary and allied health professionals in Canada. There are also gaps in research into how best to match and tailor treatments to individual patients. More recently, Canada has become a leader in patient engagement in research, which places people living with pain and their experiences at the centre of research, policy, and program design and implementation.
Building on these observations, we asked participants in this phase of our consultations to offer their perspectives on the state of pain research and related infrastructure in Canada and how we can strengthen and advance Canadian pain research activities.
Gaps and challenges
Given the relative economic and societal costs of pain, research in this field is largely underfunded compared to other fields
Participants cited inadequate funding devoted to pain-related research, human resource support, and incentives for researchers as major challenges. Many noted there is no dedicated funding mechanism for pain-specific research programs, and funding is typically distributed in pockets and across programs and disciplines (e.g., cancer, neurosciences, arthritis). They noted the limited funding that is available for pain, and highlighted that it is disproportionately smaller than for other chronic diseases and illnesses as a whole, such as cancer and heart disease, even though pain is equally, if not more, prevalent. Pain research funding typically covers programs and/or projects in the short term (e.g., 12 months), whereas granting agencies need to consider longer-term projects (e.g., 3-5 years) to establish reputable and reliable infrastructure and enable true innovation and discovery.
It was noted pain grants are currently distributed across various funding agency committees or panels, and there is often insufficient expertise and availability of individuals to serve on all of them. As a result, many submitted grants are reviewed by those who are not in the pain field. Participants also noted funding opportunities for knowledge mobilization are rare and this funding is often embedded in grants, being overshadowed by other aspects. Ultimately, participants stressed the need to understand the research submission process, composition of peer-review committees, the success rates of pain-related submissions across program areas, and to which institutions they were submitted.
There is a need for better national capacity, collaboration, and coordination in pain research
While some provinces have or are building specific research networks (e.g., British Columbia, Quebec, Alberta), respondents expressed a need for improved national capacity in the form of a unified national presence across organizations or a dedicated pain champion. Such a champion would need the capacity to support information dissemination and collaboration across disciplines and jurisdictions in Canada. While the CIHR-funded Strategy for Patient-Oriented Research Chronic Pain Network (CPN) exists at a national level ($2.5M/year for 6 years, 2016-2022 with a requirement for an additional $2.5M/year to be matched by partner sources), participants felt its future is unclear and that the closed network of researchers is not resourced enough to coordinate emerging networks and individual researchers across the country. There is also a need to evaluate federally funded research networks, such as the CPN, and provincial initiatives, such as the Quebec Pain Research Network, to better understand gaps and successes, and to ascertain how alternative or additional research funding programs could fill gaps in the future. Similar evaluations should be initiated across funding agencies and networks for pain research, to better coordinate the distribution of funds across priority areas, and to ensure sufficient funds are dedicated to investigator-led innovation.
Participants also noted the potential drawbacks for innovation when restricting pain research funding to a single funding institution. These limitations can pose barriers to the multi-disciplinary nature of pain research, and place restrictions and added challenges to investigator-initiated research. Alternatively, the drawback of diffusing pain research across a number of institutions is that by living everywhere and it therefore lives nowhere. Funding institutions must balance the advantages and disadvantages of either funding model, and participants encouraged better coordination of funding to facilitate collaborative and innovative pain research across disciplines. Finally, while there are many gaps in data availability in pain, the need for improved biopsychosocial data collection was highlighted, with suggestions to facilitate collaborations across governments (national and provincial funding agencies), researchers, and people living with pain to ensure the applicability of data in practice.
There is a lack of a common and integrated approach for measuring pain
A current methodology for objectively measuring, as well as capturing, the dynamic nature of pain (e.g., chronic duration, varying intensity) is limited in the field. Participants indicated there is no objective and agreed upon measurement for pain, which may explain the disconnect between the pain experience of the patient and the pain severity perceived by health professionals. Others cited the lack of standardized chronic pain indicators, interdisciplinary definitions or knowledge frameworks, or developmental approaches (e.g., pain across the lifespan) as a gap to understanding pain as a disease or condition of its own, rather than a symptom of another problem. Current evaluation tools available to clinicians to assess pain are limited to a fixed time-point and a 0-10 intensity scale, whereas the pain experience spans beyond these types of frameworks and such measures fail to recognize level of function and other important aspects that matter to individuals living with pain. They can also negatively impact the patient-clinician relationship and communication, and contribute to stigma and lack of understanding.
There is little real-world research exploring the multidimensional and complex nature of pain
Participants noted the need to improve knowledge about the multidimensional and complex nature of pain amongst the public, clinicians, and policy makers. Where chronic pain may have a clear relationship with complex issues spanning the biological, psychological, social, and clinical sciences, too few studies examine the multidimensional nature of pain, as well as the needs of patients presenting with multiple conditions and more complex needs. While pain lives in many disciplines, researchers are often required to abide by strict exclusion criteria, which eliminate the ability to study multiple conditions in order to create a "clean" sample. One example cited was the exclusion from pain studies of people who use drugs, making it difficult to study the intersect of the two issues.
Participants also noted barriers to conducting complex and multidimensional research across sites throughout Canada due to a lack of infrastructure to facilitate research of this nature, barriers to developing wide-reaching research designs, such as multi-site trials, and limited collaboration across research centres. An example of such a barrier includes distinct research ethics board (REB) processes established by many universities, which may apply or interpret varying criteria and standards in different ways. This can create barriers to multi-site studies by forcing such researchers to apply to multiple boards, each of which uses different standards, for the same study. While the REB process extends beyond the scope of pain research, participants noted the current process prevents researchers from conducting clinical trials in a quick and efficient manner and across trial sites.
Research and clinical care can be disconnected
While participants highlighted recent advancement in the pain agenda across Canada, they also pointed out barriers to effective knowledge translation (e.g., translation of research, translational infrastructure). We heard a disconnect and separation between research and clinical quality improvement. It is difficult to find resources to fund translation of successful research into clinical practice and often this requires different skill sets and experience, which spans "beyond the lab". Some participants spoke to a lack of expertise bridging basic science research and clinical trial design and operation. Researchers noted limitations for innovative and early stage discovery, advocating for more time for discovery activities - that is, independent researchers' time for "open discovery" rarely exists.
There are gaps in predicting how patients will respond to different care plans and in understanding population-based differences
There is not enough understanding of the factors that can predict who will do well on certain treatments and therapies and who will not. Nor is there enough research into the effectiveness of therapies, which span beyond pharmacological interventions. More research is needed to understand the potential effectiveness of each treatment and what combination of treatments could be applied to different people.
Our consultations also identified a gap in researching the unique needs of different populations (e.g., Indigenous Peoples, ethnic and cultural communities, seniors, infants and children, people with pain and other co-morbidities) in order to build knowledge around the most appropriate therapies and interventions needed for different types of pain, and identifying effective models and pathways to care. Participants suggested pain researchers should aim to better integrate and understand the broader social contexts of pain and related inequities.
Best and promising practices
Stakeholders provided many examples of initiatives across the country they believe are helping to address challenges related to research and research infrastructure, including:
- Patient-oriented research approaches;
- Initiatives dedicated to knowledge mobilization;
- Common methods for the measurement and assessment of pain;
- Networks and collaboration;
- Infrastructure that supports complex trials; and,
- Large-scale trans-agency initiatives dedicated to understanding, managing, and treating pain.
"Involve persons who suffer chronic pain and ask what would be beneficial - what they find best and worst about their care and caregivers. Build best practices and train around the best of what the people who are satisfied with care say."
Questionnaire Respondent
Patient-oriented research builds capacity among patients and more meaningful knowledge creation
Several workshop participants highlighted successful initiatives across Canada, which engage people living with pain in all aspects of the research process, from conceptualization to knowledge translation. Such engagement enriches the value of the research team and helps to define questions that need to be answered, producing benefits for patients, clinicians, and researchers. Co-designing research with patients also ensures feasibility, adaptability, and applicability of research.
Participants noted a number of examples where patients, along with researchers, policy makers, academic health centres, and other stakeholders, are involved in identifying research priorities. This accelerates the translation of research findings into patient care and health policy. In addition, participants spoke to the importance of training patients and citizens in various research methods to facilitate the co-design process, build community capacity, and to ensure that data is integrated and usefully applied to community challenges. The CIHR Strategy for Patient-Oriented Research (SPOR) program, Centre of Excellence for Partnership with Patients and the Public (CEPPP), and Patient and Community Engagement Research (PaCER) initiative are all examples that implement these approaches to patient-oriented research, capacity-building, and training.
Translating research into practice requires dedicated mobilization initiatives and investments
The importance of translating research findings into improved clinical care and better patient outcomes was a recurring theme throughout our consultations. As world leaders in pain science, Canadian researchers are well positioned to further develop a more coordinated research dissemination strategy with relevant stakeholders. Participants told us that having researchers as active partners in the delivery of care has helped to improve knowledge about which interventions work, for whom, when, and under what circumstances. Community groups, clinicians, governments and administrators, and researchers are collaborating, with many research disciplines coming together to form networks and support knowledge creation and mobilization.
Some of the practices cited by participants integrate researchers into pain clinics to allow for pragmatic real-world studies and better integration of research to practice. In such models, researchers are integrated into pain clinics to assist in tracking patient outcomes from the start of the program, through the care process, and following up at key points post-program. Having researchers embedded in the clinic site allows for quick and responsive research based on real-world questions and needs. Integration can also allow for tailored research that is specific to particular communities or population groups thus allowing for a better understanding of the care need of different populations and how to better tailor and target care to these needs and experiences. Examples cited by participants included clinics that are integrated with academic institutions such as the Michael G. DeGroote Pain Clinic at McMaster University, the Stollery Children's Hospital connected to the University of Alberta, and the Centre for Pediatric Pain Research at IWK Health Centre and affiliated with Dalhousie University. Participants also noted the Aboriginal Children's Hurt and Healing Initiative, which works with Indigenous communities, health centres, and clinicians to bridge the gap in the understanding of Indigenous children's pain, and with universities and clinicians to improve their knowledge so they can provide more appropriate, culturally safe care.
Finally, programs such as Solutions for Kids in Pain (SKIP), a newly formed knowledge mobilization network based at Dalhousie University and co‐led by Children's Healthcare Canada, bridges the gap between current treatment practices and available evidence‐based solutions for children's pain in Canadian health institutions.
Researchers are building common methods for the measurement and assessment of pain
Participants spoke to several initiatives working to create minimum data collection standards and outcomes for both adult and pediatric populations. Such work allows for greater comparability and coordination of different research studies. Common elements across this work explore indicators across a range of domains, which look at both pain and function. They include exploring pain intensity, physical functioning, emotional functioning, general ratings of improvement and satisfaction with treatment, adverse events, and patient disposition. Participants mentioned the Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials (IMMPACT), the work of the Chronic Pain Network (CPN) to implement the Canadian pediatric and adult pain patient registries in different pain clinics across Canada, and the work of the Chronic Pain Centre of Excellence for Canadian Veterans, all of which aim to build core outcome measures. They also mentioned the US National Institutes of Health Task Force on Research Standards for Chronic Low-Back Pain, which successfully developed a multidimensional uniform minimal dataset and standard set of data collection questions to increase consistency amongst researchers. Participants noted that while such work holds great promise, it is not being applied consistently across clinical settings and research studies and more work is needed in this field.
Networks are working to improve coordination of research activities and initiatives across jurisdictions
Throughout the consultation process, we heard how provincial research networks (e.g., Quebec Pain Research Network, Alberta Pain Research Network, British Columbia Pain Research Network) can facilitate partnerships and improve the applicability and impact of research in their respective regions. These initiatives aim to represent a wide-range of provincial research stakeholders, sectors, and systems by integrating an interdisciplinary community of scientists, clinicians, scholars, and community partners to develop strategic priorities and partnerships. Common network priorities and areas of focus aim to understand the cellular and molecular basis of pain, improve the assessment and treatment of pain, improve prevention efforts, and ensure efficient and effective knowledge translation across multiple sectors.
We also heard that national level networks, initiatives, and programs can create linkages and research opportunities, facilitate collaboration and knowledge dissemination, and unite pain research across the country. Furthermore, national organizations can bring together stakeholders and build capacity for pain research, education, training, and knowledge sharing and development (e.g., Canadian Pain Society, Pain in Child Health initiative). Participants spoke to certain aspects of the CPN, which they felt illustrated the potential of national networks, including how the CPN has brought together individuals with various forms of expertise (e.g., clinical trial design, basic sciences, translation, knowledge mobilization) to collaborate more effectively, linked clinical sites to enable common approaches to research, and developed foundational aspects of research and related infrastructure (e.g., common measures and outcomes, patient registries, common prioritization processes). Participants also expressed excitement around the newly announced Chronic Pain Centre of Excellence for Canadian Veterans. The initiative has involved the creation of a national organization, which partners with Veterans and their families to build research and knowledge around evidence-based strategies for care. The Centre is focusing on setting a clear research agenda, designing pain management therapies, and helping Veterans access care in the community, all of which is facilitated through a national network of interprofessional pain management centres.
Participants felt an important next step for networks in Canada would be to look further at their accomplishments to gain a deeper insight into what they have achieved. In addition, gaps should be assessed to note what is missing and what does not work so that we can identify what can be improved. Participants also felt further coordination activities were necessary to expand and better link provincial and national networks to enable a unified approach in Canada.
Initiatives are working to better coordinate research and enable multi-site and more complex studies
Participants noted a few examples of initiatives working to enable more complex study design. One such example is the facilitated research ethics board (REB) process resulting from a multi-institute (CIHR-Institute of Human Development, Child and Youth Health and CIHR-Institute of Genetics) streamlined, national pediatric REB process. It was noted this recently funded REB process, entitled Promoting Child Health Research through a Collaborative Approach to a Streamlined Ethics Review or Pediatric REB Initiative, has potential to be duplicated and scaled up in other areas of research and for different populations impacted by pain. Additionally, Clinical Trials Ontario (CTO) is supporting the movement for a single provincial ethics review for multi-site research in Ontario. The CTO streamlined approach provides an efficient way to conduct research ethics reviews and make research studies more efficient and cost-effective. This process allows a multi-site research study to undergo a single ethics review rather than separately applying to their local research ethics boards. Participants felt such models could be scaled nationally to allow for multi-site studies across jurisdictions in Canada.
Large-scale initiatives spanning different research agencies and organizations are building a variety of approaches to tackle complex problems
Participants noted the potential of large-scale initiatives, which involve dedicated funding by multiple agencies and organizations and coordination of that funding, to build capacity for research on a national scale. The example discussed the most by participants is the Helping to End Addiction Long-Term initiative established by the US National Institutes of Health (or NIH HEAL Initiative). The initiative is funding hundreds of projects across the US, each focused on various aspects of understanding, managing, and treating pain as well as improving treatment for problematic opioid use or opioid use disorder. It is the combination of these different types of research, dedicated funding, and national scale coordination, which has accelerated and incentivized research into pain.
Elements of an improved approach to pain research
Establish national capacity to advance pain research through funding and coordination
A central aspect identified by participants for improving approaches to pain in Canada is the need for appropriate and dedicated funding for pain research, and investments in a national pain research agenda. Historically, pain has been integrated into many places and crosses the mandates of many funding bodies - this can be positive and create a range of opportunities for different individual researchers and teams. However, without national capacity for research and better coordinated infrastructure, funding remains both inadequate and difficult to access for many. Some researchers suggested the formation of a peer review panel at CIHR to review interdisciplinary grant submissions focused on pain research. However, it was also noted, if pain research had a dedicated panel, pain researchers may have fewer funding opportunities for which they are eligible to apply. It is important to strike a balance between supporting investigator-led opportunities and strategic funding specific to pain. They encouraged further exploration of current funding mechanisms, peer review committees, and submission processes, and the creation of a map of pain research in Canada to better assess how pain research compares to other research in competitions and grants. Data on the success rates of pain-related grant submissions across CIHR Institutes and other funding agencies should be collected and disseminated to better understand the gaps, successes, and potential biases in pain-related research funding. Participants also noted the importance of connecting funding agencies with people living with pain and decision-makers at the federal and provincial levels and in various industries to better understand research priorities.
Participants suggested a mixed funding model or multi-pronged approach that ensures pain research continues to compete with other priorities in open competitions, but is also supported in strategic priority areas with adequate targeted funding and coordination. Several participants noted the need for more long-term grants, which recognize the longer-term nature of basic discovery, clinical translation, and providing care and sophisticated community-based interventions to patients with chronic pain. Participants also identified the need for innovative funding opportunities that support the development of larger foundational research projects across institutions and networks as well as streamlined funding processes for joint research initiatives. Research infrastructure must also be developed to provide the tools and resources to better integrate research within existing networks and initiatives. Participants also highlighted the significance of supporting trainees and dedicating fellowships in pain, with incentives to further develop the research workforce interested in pain.
Respondents suggested a way to address this range of needs would be more leadership to better manage pain-related funding within existing agencies, and to dedicate specific funding mechanisms for cross-cutting and interdisciplinary research, duplicating what has been done with the US HEAL Initiative. Participants felt there could be better engagement and coordination across all federal funding agencies in Canada - CIHR and the Social Sciences and Humanities Research Council (SSHRC) and the Natural Sciences and Engineering Research Council (NSERC) - to support pain. Improved coordination and opportunity-building across these agencies may result in better representation of broad perspectives ranging from biomedical to socio-cultural in studying pain solutions. Recently, the Canada Research Coordinating Committee, which is a committee that improves coordination across all funding bodies as well as the Canada Foundation for Innovation, announced the New Frontiers in Research Fund (NFRF). The initiative funds international, interdisciplinary, fast-breaking, and high-risk research. Programs such as these facilitate discovery by encouraging Canadian researchers to work with partners across disciplines and research interests. They can also better integrate efforts to understand the biopsychosocial model of pain and the broader social determinants/contexts of pain and related inequities. Future pain research must take a strong developmental approach to thoroughly understand the biopsychosocial variables that influence pain and to better understand the various risk factors for chronic pain and how they may manifest across the lifespan.
Participants noted the creation of the Canadian Pain Task Force demonstrated the importance of a national presence and improved coordination and collaboration across jurisdictions and existing initiatives, to achieve better alignment of research priorities for a national pain agenda. Participants felt a national pain research network, mechanism, or organization could align or streamline the process of creating a unified approach across the provinces and territories, encourage collaboration with industry and relevant stakeholders and communication among existing networks, and help to enable new networks in jurisdictions that currently have gaps. They also advocated for funding for research within the federal government, which spans beyond the health portfolio through broader engagement with other ministries.
Support basic discovery and innovation
Researchers advocated for longer term programs and grants, which provide more time for basic discovery and activities and support innovative and collaborative basic science. Participants also discussed public-private partnerships as a possible strategy to improve pain research, noting this is currently occurring in other countries to develop incubator and accelerator programs. Researchers highlighted the potential role private industry can play in advancing pain-related research, catalyzing basic discovery, and improving access to innovative treatment options. However, they also recognized the double-edged sword of involving industry with a vested interested and bias toward certain interventions and treatment options for pain.
Build capacity and infrastructure to evaluate innovative care solutions and facilitate translation into real-world practice
Participants called for integrating research capacity into clinics and the delivery of care to enable better knowledge creation and exploration of real-world care. This can be incorporated by linking researchers with clinicians and investing in clinical scientist positions and knowledge mobilization infrastructure to support the translation of research into practice. More research is also needed to examine the effectiveness of pain prevention and treatment interventions offered by primary and allied health professionals in Canada and what combination of treatments could be applied to different types of chronic pain and patient circumstances. Such research needs to incorporate the broader socio-cultural context of pain and related inequities to enable improved personalized pain management and tailoring treatment to an individual's context. Participants also spoke to the importance of funding real-world research designed to evaluate the effectiveness of system solutions (e.g., virtual care solutions, low-intensity programming and care, day-to-day clinical practice and care models). They stressed the need to invest in programming and interventions in a manner that supports implementation science and refining and scaling of innovations based on their success in addressing individual and system related outcomes.
Participants also discussed the need to invest in dedicated knowledge translation and mobilization activities, designed and driven by those with appropriate expertise, to expand the reach and digestibility of pain research and to fuel future research and clinical care. The concept of reverse translation, taking what end-users (e.g., people living with pain) tell researchers about their experience with pain and related interventions back into lab to generate ideas that are grounded in clinical practice, was explored briefly throughout discussions. Many participants noted this concept has produced more effective practice and improved patient outcomes.
Participants also discussed ideas for enabling translation of basic science research into clinical practice. Examples provided include the effective use of community partners, third-party investors, and other support networks. The principle of reduced administrative burden and improving research dissemination were suggested more broadly, with innovative strategies to improve research-related infrastructure being discussed. For example, the University of Calgary imbeds translation support into its institution to facilitate and encourage translation of basic science discoveries into clinical trials. It was suggested a similar model could be successful for pain-related research.
Establish an integrated and common understanding of pain and minimum data collection standards
Enhanced research and data capacity in the area of pain would facilitate the spread of best practices across the country. Participants highlighted the importance of the broad collection of common data to counter the variability of pain data across geographic centres and jurisdictions. One participant quoted Sharma's principle "what gets measured, gets improved" as a principle for data collection in the field of pain.
Participants noted a multidisciplinary and common understanding of pain would enable future research and improve the comparability of various research projects. They spoke of the need for minimum data collection standards and outcomes for both adult and pediatric populations, building on the foundations established by projects such as the IMMPACT core measures, the CPN Canadian pediatric and adult pain patient registries, and other research standards. Successful development and application of a multidimensional, uniform minimal dataset and standard set of data collection questions, is needed to increase consistency amongst researchers. Work to enable uniform data collection, which is aligned with international actors, should be scaled up and applied more consistently across Canada. The development of a national working group may facilitate the integration of minimum data collection standards and should be considered. With the adoption of minimum data collection standards, progress for understanding, managing, and preventing chronic pain can be achieved. Pain, similar to other information such as sex and gender, should also be integrated into existing surveys, cohort studies, and population health data.
Monitoring population health and health system quality
Any initiatives to improve pain care and pain management in Canada must be based on a solid understanding of the existing situation and measurement of the effectiveness of proposed actions. In our first report, we noted the need for more comprehensive, standardized data on prevalence, course, impact, and outcomes of chronic pain in Canada. There is also a need to monitor the impact of interventions intended to improve health system performance and health outcomes. Public health surveillance is the ongoing, systematic collection and analysis of health data for evaluation of programs and practice, and the application of these data in prevention and management efforts at clinical and policy levels. Surveillance is essential to continued system improvement. Such data helps to create health profiles at federal, provincial, territorial, and/or regional levels, enable identification of populations at risk, monitor changes over time, and enable evidence-informed policy, programming, and investments.
To enable quality improvement and reduce the great variability currently present across jurisdictions, Canada needs appropriate frameworks for common approaches to public health surveillance and health system performance monitoring. This includes the development of common indicators, minimum datasets, standardized data collection, and reporting methods. Participants across each of our consultation activities were asked their views about the current state of such work and they provided suggestions for ways to further strengthen the system.
Gaps and challenges
More survey work is needed to report on relevant pain indicators
We heard efforts to measure the prevalence of pain in Canada are scattered across the country and fragmentation of data and systems and a lack of standardized pain indicators pose challenges to assessing the extent of unmanaged pain within and across jurisdictions. Currently there are national surveys with modules that have some pain related information, such as the Canadian Community Health Survey (CCHS) and the First Nations Regional Health Survey. However, these modules need to be further expanded to capture a more comprehensive definition of chronic pain, the impact of pain on the lives of people in Canada and data on specific pain conditions.
Participants discussed a range of data gaps, which make it challenging to identify how many people at the national level have chronic pain, how these numbers might change over time, factors associated with pain, and the resulting impacts, longitudinally. There are limitations to collecting some kinds of data in rural and remote communities due to limited electronic infrastructure. In addition, while record linkages between administrative health data (e.g., Canadian Census Health Environment Cohort) may fill some data gaps for certain populations and conditions, many populations disproportionately affected by pain (e.g., people who are homeless, Indigenous Peoples living on reserve or in remote areas) are often not in scope for some national health survey data. Obtaining more comprehensive information on pain in national surveys is critical to providing resources to people living with pain, understanding what interventions work best for different types of pain and populations, and directing strategic investments by governments, insurers, and other health system actors.
Lack of clear diagnostic and coding standards for pain in administrative data systems
While some national survey data on pain prevalence and expenditures exist, Canada lacks a robust surveillance system and infrastructure at the federal and provincial/territorial levels for monitoring chronic pain. One of the greatest barriers is the absence of an appropriate chronic pain definition and precise diagnostic codes within administrative data, which can be used for its identification. Several participants noted that monitoring pain in the community is often difficult because of challenges in registering pain-related events due to the lack of pain-specific health professional diagnostic codes or the low use of codes that do exist due to lack of implementation and/or training. Such limitations can often cause health care professionals to underdiagnose or misdiagnose chronic pain.
If coding practices for chronic pain are inaccurate or not standardized, this creates limitations and a lack of reliability of chronic pain estimates when collecting and coding data. Chronic pain can accompany other medical conditions, so it is often not diagnosed and treated as a singular condition, but instead as one that manifests based on other causes or co-morbidities. As a result, chronic pain is coded in many different forms with no singular coding standard. Currently, extraction based on primary diagnosis underestimates the prevalence of pain and therefore resources needed to treat it. There have been recent changes to international standards related to the diagnosis of disease, which acknowledge pain as a distinct condition. Implementation, uptake, and training to the 11th revision of the International Statistical Classification of Diseases (ICD-11) will help to respond to these challenges, however, the adoption of such standards by individual countries, or by all provinces and territories in Canada, is complicated and will take years to be implemented consistently. In order to accelerate the adoption of these standards across Canada, there is a need for continued investment and resourcing for pain-related monitoring across jurisdictions.
It is challenging to develop provincially and nationally relevant indicators without adequate capture of people presenting to the health care system. Without a coordinated effort to implement the most up-to-date classification system, surveillance and monitoring efforts, chronic pain will continue to lag behind other chronic disease surveillance systems in Canada. Lack of comprehensive data and surveillance infrastructure inhibits federal and provincial monitoring of the health care and societal costs associated with chronic pain, as well as the policies and programs needed to sufficiently resource these challenges. Due to the current state of surveillance infrastructure, governments, researchers, and health care professionals do not have enough information about chronic pain (e.g., mechanisms, manifestations, management), the unique challenges and needs for people living with pain, and the capacity of respective health care systems to respond to these needs.
Lack of acknowledgement and coordination of pain in quality of care monitoring
Participants highlighted the importance of improved federal leadership to drive changes in surveillance capacity and quality monitoring. Chronic pain has not received enough attention despite international recognition of chronic pain as a disease in its own right as well as its social, economic, and societal impacts and costs. Prioritization of chronic pain as a health issue and leadership from relevant federal and industry stakeholder's writ large (e.g., workplaces, insurers) could enable improvements to surveillance and quality of care. Designation of chronic pain as a priority by Health Canada and the Public Health Agency of Canada could create opportunities to include associated measures on the CCHS, the Canadian Health Measures Survey (CHMS), Canadian Census Health and Environment Cohorts (CanCHEC), or other national survey collection mechanisms through Statistics Canada as well as more dedicated efforts to coding pain in administrative data managed by the Canadian Institute for Health Information (CIHI).
Given the fragmented nature of available data for surveillance and monitoring efforts, stakeholders emphasized a need for better coordination across jurisdictions. Action to develop provincial measures for chronic pain should be coordinated and scaled up such that comprehensive and consistent indicators of pain are reported at a national level, similar to any other common chronic conditions. There is an insufficient understanding of the economic cost of chronic pain, both direct and indirect, which makes it difficult to raise awareness about the need to allocate adequate resources and funding to address it. Several participants told us the absence of adequate data and surveillance systems means pain must compete with more visible diseases, which are perceived as more immediate priorities. Overall, improved data and monitoring efforts to provide more reliable prevalence estimates will facilitate a better understanding of the human and economic burden of chronic pain on the health system and society.
Best and promising practices
Consultation participants provided many examples of initiatives across the country they believe are helping to address challenges related to monitoring population health and health system quality, including:
- Disease classification standards;
- Development of pain-related outcomes and frameworks;
- Electronic records and common coding practices;
- Monitoring the outcomes of prescriptions; and,
- Use of algorithms and innovative approaches to surveillance.
Disease classification standards are adapting to recognize pain as a disease in and of itself
Many participants expressed optimism about recent changes by the World Health Organization to acknowledge chronic pain as a specific disease classification in the ICD-11, noting it will facilitate the collection of more data about chronic pain in Canada. They noted these central, common diagnostic codes would be important for physicians and all allied health professionals. However, the implementation of the international standard for chronic pain diagnostic codes will take several years and resources to be fully realized. In the meantime, participants emphasized the need for improving and implementing currently available coding resources by establishing minimum datasets, standardizing chronic pain indicators, and educating clinicians on the use of these tools.
Efforts are underway to develop pain-related outcomes and frameworks for surveillance
Participants noted there are pockets of surveillance in individual clinics and regions that have invested in better data collection but it is not always clear how best to compare different clinical environments and contexts (e.g., primary care networks vary in scope, size, and services provided). Nevertheless, research networks in Canada are developing registries of people living with pain and standards to collect key information (minimum data-sets) from all patients who seek care at the clinics involved in these networks (e.g., demographic data, pain diagnosis and associated pain related disability, treatments and outcomes).
Several examples of standards and electronic platforms intended to improve communication among practitioners and allow for potential surveillance efforts were identified by consultation participants, including:
- Provincial efforts to educate clinicians on coding resources, establish chronic pain outcomes and measures, and integrate health surveillance capacity into provincial health strategies (e.g., Alberta Pain Strategy working group on outcomes and measures, Health Quality Ontario quality standards and measurement guide); and,
- Development of chronic pain registries gathering information and details on outcomes related to chronic pain from clinics across Canada based on established minimum datasets. For example, the Canadian Chronic Pain Network and the Canadian Network of Pediatric Pain Centers are currently developing a chronic pain registry for adults and one for pediatric patients followed in 23 tertiary clinics across Canada (11 pediatric and 12 adult). The Chronic Pain Centre of Excellence for Canadian Veterans is also incorporating this minimum dataset in the Veteran Registry they are in the process of developing within their affiliated network of clinics to track care and outcomes to improve pain management for Veterans.
Electronic records and common coding practices and measures are enabling better surveillance
The use and coordination of Electronic Medical Records (EMRs) were widely seen as a way to unify medical records and facilitate clinician access to patient health records and communication overall. However, it was noted EMR initiatives are fragmented and vary from province to province and across institutions, and clinicians in private clinics do not utilize the same EMRs as public clinics.
Examples of initiatives identified by participants included:
- Province-wide systems working to enable comprehensive medication profiles for everyone who gets a prescription filled in a community (e.g., Nova Scotia Drug Information System, Newfoundland Pharmacy Network);
- Provincially based online portals containing diagnostic imaging and data, laboratory results, health information, digital health records, medication profiles, and information regarding patient access to health services (e.g., eDOCSNL, Connecting Ontario Clinical Viewer); and,
- Systems that allow for the transference of patient information between EMR systems and members of a patient's care team who may be based in different care settings to foster health-system integration, continuity of care, and evaluation, and real-world research (e.g., Community Information Integration, Central Patient Attachment Registry).
Prescription monitoring programs hold potential for exploring treatment options and patient outcomes
Prescription monitoring programs (PMPs) are seen as a way to allow for greater monitoring of opioid and other pain medication prescribing. They also bring community pharmacists into the health care team as part of the monitoring and surveillance process, leveraging their skillsets, knowledge, and abilities. Participants observed that efforts across multiple jurisdictions to monitor prescriptions present an opportunity for better communication of pain education and treatments, as well as monitoring patient therapeutic outcomes (e.g., pain intensity, side effects, level of function) over time. While not all PMPs may be applied in such a manner, participants nevertheless discussed the potential of using such programs to monitor at a larger scale for better understanding of the effectiveness of various interventions for specific populations as well as risk and protective factors.
Researchers are leveraging existing data sources to develop algorithms for estimating prevalence of chronic pain
Participants noted examples of research being conducted in Canada to develop reliable and valid algorithms for estimating the prevalence of chronic pain. While algorithms often rely on national surveys, such as the CCHS, others have created and established algorithms to identify cases of chronic pain using health administrative databases and common diagnostic criteria, validating them against known cases of chronic pain patients. Some of this work is explored later in this section in our discussion of the cost of pain in Canada.
Participants shared a non-exhaustive list of potential data sources and tool, which could be leveraged for low-cost methods to obtain reliable prevalence and economic cost estimates for chronic pain:
- Algorithms used for other chronic conditions that have been validated across Canadian jurisdictions (e.g., The Health Data Research Network Canada);
- National pain patient registries across Canada (e.g., CPN Clinical Research Network Sites);
- Population-based surveys with cycles containing pain and disability specific information (e.g., Statistics Canada's Canadian Community Health Survey);
- National networks connecting research stakeholders to provide evidence based information (e.g., SPOR Evidence Alliance);
- Health records and administrative data (e.g., CIHI's Discharge Abstract Database, National Prescription Drug Utilization Information System Database, National Ambulatory Care Reporting System, and the Hospital Morbidity Database);
- Large-scale, longitudinal cohort studies (e.g., Canadian Longtudinal Study on Aging);
- Databases recording prescriptions (e.g., Canada Health Infoway's PrescribeIT service and platform); and,
- Existing primary care systems (e.g., Canadian Primary Care Sentinel Surveillance Network).
Elements of an improved approach to monitoring pain and health system quality
Reach consensus on relevant and comprehensive provincial and national pain indicators
There was general agreement that Canada needs comprehensive frameworks for common approaches to public health surveillance and health system performance monitoring to reduce the variability of chronic pain care across Canada. Such frameworks would include common indicators, minimum datasets, national standards for data collection and reporting methods, and better guidance on the most important indicators for chronic pain. Governments should also consider supporting the accelerated adoption of recently developed ICD-11 codes and formally acknowledging pain as a disease in its own right to enable a more unified administrative classification of chronic pain for monitoring purposes. Action to develop provincial measures for chronic pain should be coordinated across jurisdictions and scaled up so comprehensive and consistent indicators of pain are reported at the national level, similar to any other chronic condition. A national report card could be implemented to assess actions in different jurisdictions.
Enable better knowledge around the clinical experience and patient outcomes
At the practical level, more clinical research is needed to examine patient outcomes and monitor how patients are accessing services and the effects of those services. This could include number of visits to health care professionals and the time spent in each of those visits, changes to pain levels, and self-reported quality of life assessments before and after treatment. Such information could help to identify the current issues with chronic pain coding practices, and to understand who and where chronic pain patients are, how their treatment is progressing, and which clinicians they are connected to. It would also allow health care professionals to identify and scale up practices that lead to successful outcomes and to share those findings with other practitioners.
Existing systems and databases should be leveraged to enhance surveillance and data collection, including more comprehensive pain-related standardized administrative data collection and investments in ongoing national surveys, either through the creation of pain-specific surveys or through provision of resources to better integrate pain into ongoing population-based surveys such as the CCHS. Participants stressed the importance of ensuring that pain related modules in the CCHS (e.g., Health Utilities Index) include more comprehensive indicators of chronic pain on a regular and ongoing basis. In addition, the importance of including or linking similar modules to assess Indigenous communities, immigrants, or temporary residents within the scope of regularly performed surveys, such as the CanCHEC, should be considered. There is a need for quality data and a more robust system in the long term to provide national prevalence estimates and to monitor the impact of interventions intended to improve health systems.
Participants also noted the potential of common clinical tools and processes, such as centralized intake and assessment forms, for better capturing outcomes and monitoring patients over time. Improvements in chronic pain indicators and algorithms can facilitate the delineation of chronic pain patients at the system level and improve quality of care. They noted the importance of collecting relevant socioeconomic determinants of health and other known risk factors and predictors (e.g., demographics, race, lifestyle and behaviors, trauma) associated with chronic pain and data to enhance the understanding of conditions that co-occur with pain (e.g., mental illness, substance use). Efforts across multiple jurisdictions to monitor prescriptions present an opportunity for better communication of pain education and treatments, as well as monitoring patient outcomes over time.
Build federal leadership and coordination of pain surveillance systems
Data from surveillance informs policy, program development, and resourcing appropriate health care interventions by improving government understanding of the efficiency of investments, the calculation of the economic costs of pain, and continued monitoring of chronic pain. Participants noted improved data and surveillance efforts would provide more reliable prevalence estimates and facilitate a better understanding of the economic cost of chronic pain on the health system and society. They highlighted the importance of improved federal leadership to drive changes in surveillance capacity and improved quality monitoring and capacity across the board for chronic pain. Improvements in these areas would facilitate better knowledge transfer and communication of data in formats that are easily understood and interpreted by Canadians. Dedicated funds should be provided at both the federal and provincial levels to increase surveillance capacity. However, participants noted the importance of also allocating resources to ensure the establishment of a coordination mechanism, which could engage researchers and data stewards, and allow for sharing of expertise and improved monitoring of pain.
A new study on the cost of chronic pain in Canada
The economic burden associated with pain is significant. In addition to the health care resources utilized in the treatment of pain, the associated disability and impact on quality of life result in further economic costs in terms of lost productivity. Together the economic burden attributable to chronic pain has been estimated to be as high as $60 billion CAD per year (Wilson et al., 2015). In this section, the results from a recent Canadian study by the Policy, Research, Economics, and Analytics Unit at Health Canada (Milliken et al., forthcoming) are presented. The objective of the study was to estimate the economic costs associated with chronic pain in Canada, including health care (direct) costs and the value of lost production (indirect costs), from a societal perspective.
Few studies have assessed the cost of chronic pain - Table A presents a summary of the estimates from a number of studies. Annual health care costs ranged from $1,340 to $4,790 per individual living in pain, and the per capita production losses ranged from $1,790 to $21,150. Two Canadian studies, which have examined unique patient populations, estimated the per person annual costs to be in the range of $10,880 to $21,490 (CAD 2019) (Lalonde et al., 2014; Guerriere et al., 2010). In addition to not being representative of the general Canadian population with chronic pain, these two studies included overall costs incurred by individuals with chronic pain, which may include costs associated with co-morbid conditions, rather than incremental costs due to pain. They also accounted for many health care and time costs incurred privately by patients and their families.
| Study | Population coverage | Annual health care costs, per person with pain (CAD 2019) | Annual lost production costs, per working age person with pain (CAD 2019) |
|---|---|---|---|
| Deloitte Access Economics (2019) | Australia | 2,060Table A note * (3,480) | 21,150 |
| Gaskin and Richard (2012) | U.S. | 4,790 | 6,590-7,430 |
| Hogan et al. (2016) | Ontario | 1,850 | NA |
| Azevedo et al. (2016) | Portugal | 1,340 | 1,790 |
| Lalonde et al. (2014) | A group of 483 patients with chronic pain recruited from pharmacies in Quebec | 10,880 | 8,040 |
| Guerriere et al. (2010) | A group of 370 patients in multidisciplinary pain treatment facilities in Canada | 21,490 | NA |
Table A notes
|
|||
The direct health care costs in the present study, comprising hospital and physician care and prescribed medications, are estimated using an attribution method similar to the approach used in the Australian study (Deloitte Access Economics, 2019). In the absence of systematic coding of chronic pain in the International Classification of Diseases (ICD-10) according to which health system expenditures have so far been collected, the present approach relies on the assumption that chronic pain is attributable to various causes (e.g., musculoskeletal diseases, neurological disorders, injuries).Footnote 3 Thus, the total health care system cost of chronic pain represents a portion of the total costs attributable to these causes (also described as "origins of pain"). This study provides a range of cost estimates based on three Canadian studies exploring the prevalence and distribution of various types of chronic pain conditions (Table B). Expenditure data was obtained from previous estimates (Public Health Agency of Canada, 2017; Canadian Institute for Health Information, 2020), while prevalence data was obtained from the 2019 Canadian Community Health Survey for the household population aged 12 or more years (Statistics Canada, 2020).Footnote 4
| Pain origins (respective ICD-10 chapter) | Percentage of chronic pain due to its origins from the following studies | ||
|---|---|---|---|
| Queen's University (2012) - Mann et al. (2016)Table B note * | Schopflocher et al. (2011) | Quebec Pain Registry (2008-2014)Table B note * | |
| Injury | 4.8 | 15.0 | 3.0 |
| Diseases of the musculoskeletal system and connective tissue | 50.6 | 60.1 | 65.6 |
| Neoplasms | 2.0 | 0.0 | 0.7 |
| Diseases of the digestive system | 0.0 | 0.6 | 0.7 |
| Diseases of the nervous system | 16.9 | 8.8 | 19.1 |
| Diseases of the circulatory system | 0.0 | 0.6 | 0.3 |
| Certain infectious and parasitic diseases | 2.3 | 0.0 | 1.4 |
| Diseases of genitourinary system | 0.0 | 0.6 | 0.7 |
| Endocrine, nutritional and metabolic diseases | 6.4 | 0.00 | 0.5 |
| Other | 17.1 | 14.2 | 7.8 |
| Total | 100.0 | 100.0 | 100.0 |
Table B notes
|
|||
In estimating the economic production loss due to pain, both reduced employment and absenteeism were considered. A regression analysis was employed to examine the effect of having chronic pain on employment status and absenteeism, using 2019 and 2010 CCHS data, respectively. Confounding variables, including age, sex, education, various health conditions, and unhealthy behaviours were accounted for in the analysis. Average annual and daily earnings for the year 2019 were used to estimate costs of unemployment and absenteeism, respectively.
The total economic cost associated with chronic pain totaled $38.3 to $40.4 billion in 2019
In 2019, an estimated 7.63 million (95% CI: 6.72-8.54), or one in four Canadians aged 15 or older, were living with chronic pain.Footnote 5 This is an estimated increase of 16.8% from 6.35 million in 2015.Footnote 6 Of all Canadians living with chronic pain in 2019, over 28% (95% CI: 24.0% - 32.9%) were individuals aged 65 years or older. Approximately 55% (95% CI: 48.9% - 60.8%) of Canadians age 15 or older and living with chronic pain, are women. Chronic pain prevented most activities of daily living for 13.8% (95% CI: 9.9%-18.9%) of Canadians aged 15 or older who live with pain; it also prevented some activities for 21.8% (95% CI: 16.6%-28.0%) and few activities for 33.2% (95% CI: 26.9%-40.1%) in those with pain.Footnote 7
It was estimated that in 2019, annual health care cost due to chronic pain was between $15.09 and $17.23 billion or $1,980 to $2,260 per person living with chronic pain (See table C). If the cost of pain is limited to only individuals with activity restrictions due to chronic pain, then the estimated cost ranges from $10.38 billion to $11.85 billion (or 68.8% of total direct costs of chronic pain).Footnote 8 The health system costs of chronic pain included inpatient and outpatient hospital care expenditures borne by the government, which represent the bulk (61% to 70%) of total health system costs. Services of physicians (employed outside of hospitals) represented 14% to 25% of total health system costs, while public and private prescription drug costs (purchases from retail pharmacies) represented 14% to 19% of total health system costs.
In 2019, indirect costs represented in large part a reduced participation in the Canadian workforce of individuals living with chronic pain. Chronic pain that prevents daily activities was associated with a 13% reduction in employment.Footnote 9 These annual losses were valued at $22.5 billion in 2019. In addition, annual production losses due to absenteeism are estimated at $650 million in 2019 (Table C).
| Cost component | Cost ($ billion, CAD 2019) based on a distribution of pain origins from the following studies: | |||||
|---|---|---|---|---|---|---|
| Queen's University (2012) - Mann et al. (2016)Footnote * | Schopflocher et al. (2011) | Quebec Pain Registry (2008-2014)Footnote * | ||||
| $ billion (95% CIFootnote **) |
% | $ billion (95% CI) |
% | $ billion (95% CI) |
% | |
| Hospital inpatient and outpatient care | 10.8 (9.5 - 12.1) |
64.6 | 10.5 (9.2 - 11.7) |
60.8 | 10.5 (9.3 - 11.8) |
69.8 |
| Physician care | 2.8 (2.5 - 3.1) |
16.7 | 4.3 (3.8 - 4.8) |
24.9 | 2.1 (1.8-2.3) |
13.7 |
| Prescribed drugs | 3.1 (2.7 - 3.5) |
18.6 | 2.5 (2.2 - 2.8) |
14.3 | 2.5 (2.2 - 2.8) |
16.5 |
| Total direct cost | 16.7 (14.7 - 18.7) |
100 | 17.2 (15.2 - 19.3) |
100 | 15.1 (13.3 - 16.9) |
100 |
| Productivity losses due to unemployment | 22.5 |
|||||
| Absenteeism | 0.65 |
|||||
| Total indirect cost | 23.15 |
|||||
Table C notes
|
||||||
The direct cost estimates (Table C) are comparable to other studies despite differences in analytical methods and data sources.Footnote 10 In 2019, direct costs of chronic pain in Canada were between $15.09 and $17.23 billion, which represented about 10% to 11.4% of total combined health expenditures on prescribed drugs, physician services, and hospital care.
Similar to other analyses of the cost of chronic pain, this study found production losses were higher than health care expenditures (Azevedo et al., 2016; Breivik et al., 2013; Deloitte Access Economics, 2019; and Gaskin & Richard, 2012). Any comparisons must be made with caution given differences in methodologies, cost components, and population groups.
This study presents the first, comprehensive, national estimates of the cost of chronic pain in Canada. Nevertheless, it was not possible to capture all potential direct and indirect cost components, including those associated with services provided in community and those not covered by provincial and territorial health insurance plans, services of other health professionals (e.g., chiropractors, physiotherapists, psychologists, occupational therapists, massage therapists), formal and informal caregiving, and costs of reduced hours of work and presenteeism.Footnote 11 Due to data limitations it was not possible to include the cost of chronic pain in children and youth. Further research in this area is important given the health and economic implications over life course in terms of reduced educational attainment and employment in this population group. In addition, further analysis examining the cost of chronic pain in most affected groups of the population could provide additional insights into strategies to prevent and better manage chronic pain.
Additional details on this study, including assumptions, data sources, detailed methodology, results, and conclusions, are available in a separate technical report (Milliken et al., forthcoming). Next steps of research include estimating the projected future costs associated with pan, as well as examining the potential health and economic impacts of interventions aimed at reducing chronic pain.
Indigenous Peoples
First Nations, Inuit, and Métis populations are disproportionately affected by chronic pain, conceptualize pain differently from other groups, and often articulate the experience of physical pain as being secondary to emotional pain. Indigenous Peoples face many of the same challenges described thus far in the report and also must endure several unique issues, which affect their ability to obtain timely pain care. This can include access to culturally safe and trauma and violence-informed care, historical and ongoing colonialism, and present day racism within the health care system and broader society.
Indigenous Peoples provided input to the Canadian Pain Task Force engagement process through the online questionnaire, written submissions, regional workshops, and a Talking Circle and follow-up workshop specific to improving the understanding, prevention, diagnosis, and management of pain in First Nations and Métis people living in Manitoba and Saskatchewan. The Task Force worked with Elders and Knowledge Keepers as well as representatives from the Native Women's Association of Canada, the Assembly of First Nations, Thunderbird Partnership Foundation, and Indigenous Services Canada to plan the Talking Circle and workshop and to ensure input was gathered in a compassionate, socially- and culturally-informed, and inclusive manner.
Gaps and challenges
Stigma and racism are barriers to seeking and receiving health care, and result in fear when accessing services
Many Indigenous People with lived experience expressed feeling fearful when navigating the health care system, including worry and reluctance to disclose their pain because they would be stereotyped or labelled by health professionals as "drug seekers" or seen as malingering. They told us this fear is present every time they visit a health institution due to a history of intergenerational violence, racism, and trauma, which has an impact on how they seek out and receive care for their pain. Health professionals also expressed concerns related to the stigmatization of Indigenous practitioners who attempt to integrate traditional medicines into their practice. Individuals spoke to internal stigmatization experienced within their own community or family (e.g., negative perceptions around the use of CBD oil and cannabis products for pain relief). Indigenous women shared experiences of misogyny they and others have faced when receiving care for women's health and associated pain conditions.
Predominance of conventional approaches to health and wellness
The dominance of conventional approaches to health and wellness in the current health system and the general unwillingness among clinicians and administrators to recognize traditional Indigenous knowledge, medicine, and healing as effective, valued, and important to pain care creates a systemic barrier to seeking care. Participants shared experiences of long wait times, systemic racism in the Emergency Department, and fragmented care received from health professionals. They sensed a lack of communication between clinicians, which delayed treatment and led to repetition of previously trialed unsuccessful interventions. They spoke to a "damaged relationship" between First Nations and Métis people and their health professionals due to negative experiences such as being denied medications. Others noted suicidal ideation linked to substance use disorder and a lack of belief in one's pain by others. Ongoing loss of Indigenous language and a lack of information in Indigenous languages is also a barrier to care. Furthermore, in some Indigenous languages, there is no word for "pain", making expression and understanding difficult.
"Being from a First Nations background, as well as a health care background, I am not blind to the systemic racism that exists within the health care system towards Indigenous People in Canada. …We have doctors overprescribing, and doctors under-prescribing; there is the notion that all Indigenous People suffer with addiction issues, mental health, etc. These things all affect the pain experience of the individual, and further, their health outcomes."
Questionnaire Respondent
Benefits and risks to pharmacological pain management options can complicate care
Participants highlighted many benefits of pharmacological pain management options, such as effectiveness in managing their pain and ease of attainment (e.g., opioids are often cheaper and easier to access than physical or psychological services and, they noted that if required, opioids can be obtained illicitly from the street). However, they also said pharmacological options are often too costly to afford out-of-pocket, produce side effects, cause allergic reactions, cease to be effective over time, and cause some to feel "incapacitated" following use. Pharmacies in Northern/rural/remote locations do not stock the same medications as those in Southern or urban centres, often resulting in drug shortages and access challenges. Participants expressed a fear of developing substance use disorder and accusations of having a substance use disorder when seeking pharmacological pain management options. Many participants noted the Non-Insured Health Benefits (NIHB) Program provides coverage for opioids as a pain management solution but lacks coverage for important non-pharmacological forms of care. In their experiences, they stated that many physicians prescribe opioids to Indigenous patients due to a lack of non-opioid and non-pharmacological options for pain management under the NIHB.
There is poor data and inadequate monitoring of the prevalence, impact, and outcomes of pain in Indigenous Peoples
There is insufficient data on the prevalence, impact, and outcomes of chronic pain in Indigenous Peoples. Studies to obtain current population health statistics often face several challenges in recruitment and involvement of Indigenous, rural, and remote communities. Participants said current data collection methods can often discourage participation because of culturally inappropriate language and questions, and quantitative methods, which do not account for or capture the narrative experience of pain.
Additional knowledge, engagement, and a deeper understanding of cultural and non-biomedical components is needed in order to capture meaningful data. Tracking of pain-related billing codes only captures information from Indigenous Peoples who seek and receive care in clinical settings for physical pain.
Health benefits and geography are challenging for many individuals to navigate
Participants felt navigating the NIHB Program for First Nations and Inuit clients was difficult and confusing, with several participants noting the lack of funding under the program for traditional Indigenous medicines and non-opioid analgesics to pain management. However, in addition to opioid medications, the NIHB Program does provide coverage to all classes of non-opioid medications (although specific products sought by individuals may not covered). Thus, this point of contradiction demonstrates a disconnect between the patient receiving care, professionals delivering care and sharing knowledge of the program, and the program itself, which signals a need for better understanding of the program by both patients and clinicians. This idea was reflected through consultations, as participants also called for an improved understanding among health practitioners and individuals about the services and coverage included and how to navigate the program.
Like other people living in Northern, rural, and remote parts of Canada, many Indigenous Peoples face inequities in access to health services for the diagnosis, prevention, treatment, and management of pain. Limited access to physicians, and even more so to specialists, often means clinical care is provided through nursing stations. As well, although the NIHB Program provides coverage for the costs of medical transportation (e.g., travel, meals, accommodation), participants noted many Indigenous Peoples endure high costs, long travel, emotional stress, and removal from their community and/or family support system when required to travel south to receive pain care services. This cultural isolation, compounded by language barriers, creates additional challenges, further complicating care. A joint review of the NIHB Program, alongside representative First Nations, Inuit, and Métis organizations and people living with pain, could identify specific areas of coverage that require revision or inclusion, thus expanding the scope of coverage to meet specific needs of Indigenous Peoples (e.g., access to traditional healers and Elders).
Indigenous Peoples often live with a range of complex overlapping health challenges, including mental illness, trauma, violence, substance use, and pain
Participants noted Indigenous Peoples experience disproportionate rates of mental illness, substance use, and chronic pain and often have histories of trauma and abuse (mental, physical, sexual, and spiritual), which can lead to emotional pain, and in turn contributes to the overall pain experience. Participants also expressed concern about emotional pain resulting from Indigenous children and youth being removed from their homes and the history of the residential school system. Some participants also referred to their experience within the foster care system, speaking to the sense of "not belonging in either world" (i.e., Indigenous and non-Indigenous), feeling pain within the system, and turning to substances and a community of those who use substances as a way to feel belonging and solidarity.
Pain care options are often inaccessible due to a lack of financial resources and poverty
Participants shared examples of how poverty and low incomes are significant barriers to pain care. For example, they spoke to the inability to afford Kinesiology tape, so they purchased and used hockey tape instead. It was also mentioned that healthy, nutritious food is important to health and wellness, but is expensive in Indigenous communities and rural/remote areas. They noted "junk food" is more affordable and easier to attain. Some mentioned receiving and appreciating nutritional consultations, but were unable to act on the recommendations due to the unaffordable costs of wholesome foods in rural, remote, and northern communities.
"I work at a health building on a reserve. …Part of the challenge here is that non-public health care is expensive. RMT sessions are $100 for one hour. The medical services premium plan in my province pays $23 per treatment regardless of length of treatment, so I have a system where I do some treatments for people with chronic pain at that rate because they can't afford anything more. But I can't afford to provide that for everyone who could use it."
Questionnaire Respondent
Individuals spoke to their desire for access to and funding for multidisciplinary and non-pharmacological care including Traditional Healing, Acupuncture, Massage Therapy, Chiropractic care, Reiki, CBD Oil, Kinesiology, and Reflexology. Many participants spoke to the inability of many Indigenous Peoples to afford physical, psychological, and alternative forms of care, as well as being unable to afford some pharmacological pain management options.
Best and promising practices
Stakeholders provided many examples of initiatives across the country they believe are helping to address challenges described above, including:
- Building cultural safety education and training;
- Enabling family and community to provide support; and,
- Blending conventional and traditional medicine.
Individual practices provided in this discussion are not comprehensive but rather representative of examples and principles heard during consultations.
Cultural safety education and training are building competencies and changing the culture of care
Participants noted many provinces offer training to health professionals specific to Indigenous culture and that such programs are improving the accessibility and appropriateness of care for Indigenous Peoples (e.g., Manitoba Indigenous Cultural Safety Training). Universities are also incorporating Indigenous studies and social accountability into undergraduate and graduate training programs, and participants noted the value of such early education for spreading increased cultural understanding and awareness (e.g., training at the University of Saskatchewan). There are also more Indigenous faculty and instructors, and an increase in the number of Elders in the classrooms and on campuses. Similarly, more programs are needed to support and increase the number of Indigenous students enrolled in health professional programs and to ensure Indigenous ways of knowing are preserved and carried through students' education and training (e.g., the University of Manitoba, Ongomiizwin Education program). Participants felt such practices should be expanded and mandatory curriculum implemented throughout each jurisdiction to ensure continuous learning and culture change.
The Aboriginal Children's Hurt & Healing Initiative (ACHH Initiative) is working with communities and clinicians to bridge the gap in our understanding of Indigenous children's pain. Tools are designed for culturally appropriate communication and treatment, and the ACHH APP - Pain Communication tool allows children and youth to articulate their pain through stories and descriptions, while remaining stoic in their pain expression.
Family and community play an important role in care by providing support and resources
Family and community are powerful support systems and central to healing - they look after each other and provide care, comfort, and support to Indigenous Peoples with chronic pain. Therefore, accessing care within communities, where people feel supported and have access to family and traditional medicines, is a key best practice. Participants noted several programs working to create care neighbourhoods or networks in communities to ensure that care is better coordinated and accessible. A few examples of such programs noted by participants included Northern Medical Services by the University of Saskatchewan Department of Family Medicine, which allows patients access to care options within their community whenever possible. In Manitoba, participants noted Home Clinics and My Health Teams, which is a program designed to provide patients with a home base for care, and a team or network of practitioners who work together to plan and deliver primary care services both virtually and in-person in communities. In addition, Norway House Cree Nation Centre of Excellence, one of the largest health infrastructure projects ever announced by Indigenous Services Canada, will be community run and involve a comprehensive state-of-the-art medical facility focused on a range of health, social, and wellness (social, physical, mental, and spiritual) needs. Participants noted it is seen as an exemplary model for building supports, resources, and capacity in communities.
Beyond pain specific services, participants spoke to some successes in the area of mental health, which have built the capacity of communities to provide care. People accessing the NIHB Program are supported to access traditional healing services for mental health challenges through community-based projects delivered by First Nations and Inuit partners. Such a community-driven approach respects unique cultural contexts and is in accordance with the advice given by the Assembly of First Nation's Elders Council. These resources are provided via contributions, so community organizations have the flexibility to determine appropriate providers of care, to compensate providers in a manner that is culturally appropriate in their region, and to define the types of activities that Traditional Healers may undertake. Increasing such contributions and partnerships to enable the delivery of services by local community partners could be a model for improving pain care for Indigenous Peoples.
Blending conventional medicine and traditional Indigenous medicine is improving approaches to pain
A common theme among participants involved Indigenous traditional medicine as well as conventional medicine. Participants noted Indigenous Peoples have managed pain with traditional medicine for a long time, prior to the implementation of conventional approaches to care. Participants discussed that many Indigenous traditional practices are not written down, but passed down from generation to generation through oral tradition. For example, there are many ceremonies with the aim of helping people heal from mental, sexual, or emotional abuse. Even with this valuable history, some participants acknowledge the limitations of such traditions, such as when an Elder or Knowledge Keeper dies, their knowledge can die with them.
Participants noted several promising practices working to incorporate culturally safe and traditional healing practices within conventional medicine and health systems, which could serve as good models to build upon and scale up:
- Traditional Healing spaces and rooms, which are incorporated into health care centers, hospitals, and other institutions to provide spaces for Indigenous patients and their families to access or deliver traditional healing practices and ceremonies (e.g., Giigewigamig, Traditional Wellness Clinic, All Nations Healing Room);
- Multidisciplinary clinics that incorporate and/or provide access to Indigenous healing ceremonies and medicines, patient advocates and navigators, and translators (e.g., Pan Am Clinic) and others that provide patient-centred care to disadvantaged populations (e.g., Mount Carmel Clinic); and,
- Integrating culturally respectful approaches and principles into the organization and delivery of all services and the culture of care, such as Health Services Resources provided by the Saskatoon Health Authority.
Elements of an improved approach to pain care for Indigenous Peoples
Improve access to equitable and culturally safe pain care and integrate Indigenous traditional medicine into the health system
It was noted by some, that in addition to health professionals, not all Indigenous Peoples know about traditional medicine. Participants suggested blending Indigenous traditional medicine alongside conventional medicine and increasing the use of traditional Indigenous medicine in clinical practice. This would look different at each health site, given Indigenous Peoples are not a homogenized group. Doing so would require support for local First Nations, Inuit, and Métis communities to translate knowledge and facilitate its implementation. As well, local Elders and Knowledge Keepers would be essential to the development and implementation.
Grounding education in de-colonial, anti-oppression approaches, which are trauma and violence-informed and respectful of diverse social and cultural needs would allow for health care professionals to value diversity, improve their understanding and responses to cultural differences, and lead to increased patient satisfaction and improved health outcomes. Participants called for health care professionals to receive cultural awareness training aimed at system-wide awareness and acceptance of holistic approaches and improving interactions with Indigenous Peoples seeking care. They want these programs expanded, with mandatory curriculum implemented throughout each jurisdiction to ensure continuous learning and culture change at both the pre- and post-licensure stages for health professionals and to go beyond classroom training so learning can be applied in practical situations.
"We need to be open-minded in treating pain - it is what the individual experiencing it says it is. Each pain assessment and story is individualized, a personal journey. In order to properly treat, we need to understand the client's experience, to further prevent the issues surrounding their pain, and hopefully find a helpful management plan for them to function to the best of their ability."
Questionnaire Respondent
Comprehensive care among Indigenous Peoples includes access to family, community and nation traditions, ceremonies, and rituals, all of which are central to healing (e.g., On-the-land healing, Elder support, and traditional medicines). Implementing support centres and programs, which reflect the identity and healing traditions of First Nations, Inuit, and Métis peoples would help to ensure Indigenous knowledge and traditional healing approaches are central to chronic pain care and are provided compassionately and in a culturally safe manner. Hospitals could include ceremony rooms, along with discharge navigators and advocacy services to develop transition plans to other community programs and services. Participants felt increased communication between health professionals, and hiring people from within the community who know the language and inhabitants, would improve interactions within the health system. Participants also called for the integration of Indigenous healing and medicines within the NIHB Program and retention of clinicians who do not rotate or "cycle" quickly, which would enhance continuity of care, improve patient-clinician relationships, and overall improve quality of care for Indigenous Peoples in Canada.
Provide information about services as well as clear referral pathways and process to navigate health benefits
Participants stressed resources providing information, services, and referral pathways related to chronic pain should include information on traditional healing approaches and activities available in different communities. They suggested the creation of a jurisdictional repository of information to increase awareness of the services offered within regions and to facilitate clear referral pathways to both conventional and non-conventional care. Participants identified resources could be listed in a way that identifies safety and acceptance, suggesting to follow similar models established by OUTSaskatoon's Q List - a referral list of businesses, organizations, professionals, and health professionals that commit to being knowledgeable, comfortable, and supportive of lesbian, gay, bisexual, transgender, Two Spirit, intersex, and queer people. Individuals also called for accessible and affordable tools and resources (e.g., hydrotherapy, educational workshops, assistive devices), which could be accessed in-community. Health professionals and individuals should also have a better understanding about the services and coverage included within the NIHB Program. An initiative currently within the NIHB Program, which could be scaled up to address this need, are NIHB Navigators. These Navigators are a part of the Assembly of First Nations and provide services to help clients improve, understand, and navigate the NIHB Program.
Develop concurrent approaches to mental health, substance use, trauma, and pain
Participants emphasized an improved approach to pain must include interventions that successfully integrate and address concurrent challenges related to chronic pain, trauma and violence, mental health conditions, and substance use. Such interventions should be identified, planned, and coordinated with Indigenous communities as active partners. Community programs that provide free walk-in services and alternatives to pharmacological treatments, such as the Student Wellness Initiative Toward Community Health (SWITCH) and the Winnipeg Interprofessional Student-Run Health Clinic (WISH Clinic), were described as successful models for improving access and delivery.
Improve research and surveillance activities along with related infrastructure
Participants identified the need for better and standardized data, which broadly encompasses various social determinants of health, mechanisms of chronic pain, and options for pain management beyond pharmaceutical interventions. Additional knowledge, engagement, and a deeper understanding of cultural and non-biomedical components are needed to capture more meaningful data. Participants noted due to the diversity in which pain manifests and is experienced, comprehensive functional limitations, emotional symptoms, physical sensations, and behavioral changes should be assessed and documented.
Elders and Indigenous communities must be actively involved in defining research priorities, questions, and protocols, and be compensated appropriately. Collected information should be shared back with communities in a manner that can aid or benefit the community. Examples include community data dashboards, which can ensure communities receive community-specific data in a timely manner and help to build trust and facilitate knowledge translation.
Participants spoke to a need for research that includes women and a focus on women's pain. Research involving Indigenous Peoples often lacks sex and gender-based analyses, which recognize the impact of colonialism on Indigenous understandings of gender and gendered relationships. Participants emphasized research studies focused on culturally appropriate pain assessment, integration of traditional approaches to pain care, outreach programs, and harm reduction service delivery models are important elements to establish improved approaches to pain.
Participants noted the importance of funding and innovation for facilitating novel and working tools to collect data, while ensuring privacy and data security are considered. Comprehensive billing codes and quality indicators, which capture the full spectrum of services, which might be required to address the pain experience of Indigenous Peoples, including spiritual, emotional, and physical need, would help to improve understanding of what interventions work best for different situations and people. Participants also noted future surveillance and indicators must be culturally appropriate and meaningful for communities. Groups such as the Health Information Research Governance Committee, a program established by the First Nations Health and Social Secretariat of Manitoba designed to build respectful research relationships, are needed to ensure future research and evaluation reflects Indigenous priorities and values. Funding to support Indigenous-specific conferences (e.g., Annual Indigenous Health Research Symposium) and other research mentoring and training programs for First Nations, Inuit, and Métis researchers would support cross-sectoral work impacting Indigenous health.
Provide services to address geographical and financial barriers to accessing health care for those living in Northern, rural, and remote locations in Canada
Participants stressed improved approaches to pain must include the development of solutions tailored to the individual and be reflective of their physical, emotional, and financial burden. These solutions should aim to minimize the need for individuals to seek care far from home and, when necessary to do so, should alleviate challenges of travelling. Participants called for investments in in-home care services and continued investments in health infrastructure to support care options in local communities. For example, resources for housing to facilitate relocation of health professionals to northern, and rural and remote locations might enable more permanent health professionals or longer-term locums for speciality care. Other examples include mobilization of services, such as the mobile mammography clinic provided by Cancer Care Manitoba and Saskatchewan Cancer Agency. Telemedicine, video/teleconferencing, and online platforms could also be valuable tools for improving access. However, challenges related to connectivity and access to information and technology equipment in rural and remote locations must be considered and addressed prior to a widespread implementation. Overall health system change should focus on the social determinants of health, such as education, housing, and affordable nutritious foods, which will support overall health and wellness.
Reflecting on the impact of the COVID-19 pandemic
As can be seen from our work on the current state of chronic pain in Canada, as well as the consultations completed over the last several months, chronic pain represents a long-standing and prevalent public health issue, with significant costs for the Canadian health care system. The health system is often ill-equipped to effectively manage pain, support biopsychosocial approaches, and provide timely and equitable access to care. People who live with pain often lack information and management strategies, encounter stigma and other barriers, and report difficulty navigating pathways to care. At the same time, health professionals are inadequately trained to assess, diagnose, and treat pain and lack knowledge and resources to support effective multi-modal approaches to pain care. These challenges have been further exacerbated by the COVID-19 pandemic and its related public health restrictions. The Task Force could not complete this report without summarizing some of the challenges for people living with pain during this difficult and unprecedented time.
"The isolation is nothing new for me. I am an expert. However, when I hear all the discussion about the difficulties of isolating, I am reminded of the invisibility I have endured for most of the last 25 years."
Questionnaire Respondent
The widespread impacts of the COVID-19 pandemic are challenging our health and social systems, and touching communities and individuals around the globe. The effects of the pandemic have not been equally distributed, and certain groups are experiencing increased vulnerability. Older adults, immunosuppressed individuals, and those with underlying medical conditions are all at greater risk of becoming infected by COVID-19 and experiencing more severe symptoms and potential longer-term effects.Footnote 12 People living with chronic pain are among those at increased risk and they have been significantly impacted by the pandemic in the care they receive, their financial situation, and their overall stress and mental health (Hovey, Linkiewich, & Brachaniec, 2020).
Many people living with chronic pain have underlying health conditions, which could put them at increased risk for COVID-19. This increased risk may be due to either the condition itself or the treatments people are using. For example, chronic opioid therapy and steroid injections for pain are immune-suppressing, as are some medications for conditions like arthritis. Populations with higher prevalence of pain are more likely to experience higher incidence of COVID-19 complications, infections, greater disruption in their care, and significant consequences of altered care, including a worsening of pain and increased disability (Eccleston et al., 2020).
Many people with pain rely on physical therapy (e.g., manual therapy, massage therapy), rehabilitation programs (e.g., local pool, recreation centre, movement classes) and psychological supports (from therapists to peer support groups) to manage pain and maintain function. Most of these services have been cancelled or shifted to virtual models, which may not be accessible to all patients. There has also been a range of cancelled elective surgeries and procedures to treat long-held pain and related conditions. These challenges will only worsen as systems are strained to integrate cancelled/postponed surgeries and procedures back into already full schedules. The lack of access to these types of services has meant that for many people with pre-existing pain conditions, the COVID-19 pandemic has led to complex hardships including:
- Increased stress and mental health conditions - In a Canadian survey 43% of individuals living with chronic pain across Canada reported moderate to severe psychological distress (Pagé et al.,2020). In a survey of pain clinics across Canada, 71% reported that patients' pain levels may have increased due to increased stress related to the pandemic (Lynch, Williamson, & Banfield 2020).
- Increased disability - Evidence has shown that more than two thirds of patients are reporting increased pain levels during the COVID-19 pandemic (Pagé et al.,2020, Lynch, Williamson, & Banfield, 2020).
- Increased use of medications - Restrictions and limited access to care during the COVID-19 pandemic has led to an increase in use of pharmaceutical interventions to manage pain, with 53% of Canadian adult multidisciplinary pain clinics reporting an increase in medication use by patients, including 47% increase in prescribed opioid and cannabinoid use (Lynch, Williamson, & Banfield, 2020).
- Increased disruptions to continuity of care - 65% of Canadian pain clinics report providing limited pain care procedures and 35% report performing no procedures at all (Lynch, Williamson, & Banfield, 2020). This causes significant concerns because patients seeing changes to pharmacological pain treatments and non-pharmacological pain treatments are more likely to see pain worsen (Pagé et al., 2020).
"I am unable to have appointments with physicians as the COVID-19 is keeping me inside and the telephone consultations all require tests and follow-up - none of which can happen."
Questionnaire Respondent
People living with pain also report experiencing negative socio-economic effects, such as financial stressors and emotional duress (e.g., lost wages, job security, uncertainty of care), which can further exacerbate pain (Hovey, Linkiewich, & Brachaniec, 2020).
There are potential long-term effects of the COVID-19 pandemic, which could drastically impact people living with chronic pain, as well as Canada's health system. We could see increased cases of chronic pain over time, as newly triggered pain goes unmanaged and is worsened by many risk factors common during the COVID-19 pandemic (e.g., increased stress, fear, inactivity, substance use, mental health conditions) and reluctance to seek medical care for fear of contracting COVID-19. There is also the possible deteriorated health of people living with pain and other chronic conditions as access to care is impeded. Lastly, there is increasing evidence chronic pain could follow viral infections such as COVID-19 (Liu et al, 2020; Eccleston et al., 2020; Clauw et al., 2020).
"As the mom of a child who has a serious chronic condition, these COVID times have wrecked havoc on our family. My child has had 4 acute bouts of her condition and the latest was one week ago. We had no way of reaching her specialist since his clinic was closed and her condition was worsening by the day."
Questionnaire Respondent
There are tangible system responses to the COVID-19 pandemic, which could help to improve health system capacity and pain care post-pandemic and beyond. Many of these best practices have also been identified by pain stakeholders across the country and described throughout our report. Such things as rapid mobilization of virtual care, centralized and multidisciplinary assessment and intake, stepped care platforms, and enhanced self-management tools and resources will all play a role in helping to improve access to care and patient outcomes over time. Based on what we have heard through our consultations, some potential actions, which could improve care for people living with pain and the health system as whole would be to:
- Identify pain as a priority - many pain related policies, initiatives, and services have been stalled and there is a need to reinforce the importance of taking action, especially during times of increased risk.
- Support epidemiological work on pain prevalence and post viral pain - there is an opportunity to leverage the unique environment post pandemic to conduct epidemiological work on post viral complications and related pain. The impacts of the COVID-19 pandemic and related lack of access should be explored for impacts on increased health complications and disability.
- Enable virtual stepped care models for primary and specialist pain care - when implementing virtual care models for primary care and mental heath, consider equipping and aligning these systems to also deliver on virtual pain care needs and create psychological care and supports tailored to people living with pain.
- Increase access to self-management tools and resources - provide necessary information and supports to empower people to self-manage where possible, create new routines, and improve stress management.
- Implement centralized and interdisciplinary assessment, intake, and care - combining single-entry models and team-based interdisciplinary care that includes specialists in pain management, has the potential to address surgical backlog across the country in addition to improving pain care, allocation of scarce resources, and ultimately patient outcomes.
Conclusion and next steps
Our continued work reinforces that chronic pain is a significant public health issue impacting individuals, families, the health system, and society. People living with chronic pain have limited access to the services they require and often face stigma and undue suffering as a result of their condition. These challenges intersect with other health challenges related to the social determinants of health (e.g., poverty, housing, employment instability, race and ethnicity, ACE's, trauma, oppression) and other chronic conditions, such as mental illness and substance use disorder. The COVID-19 pandemic has only exacerbated these challenges further. Canadians living with pain must not be forgotten as the health system works to re-adjust and recover from this global challenge.
There are a range of made-in-Canada approaches and successes, which can serve as the foundation for much needed change. Our Phase I work highlighted many of these initiatives working in the areas of access, education, research, and surveillance. Our Phase II consultation work has highlighted further opportunities to leverage and improve existing practices in Canada. Ultimately, leadership and resources are needed to amplify, spread, and accelerate current activities, coordinate responses, address current gaps and inequities, and reduce the variability across jurisdictions. International best practice indicates this sort of national leadership and investment will yield significant returns in both human and economic terms.
The Canadian Pain Task Force would like to thank all who participated in this extensive consultation process on best practices, gaps, and elements of an improved approach to chronic pain in Canada. Priority areas for change have been further reinforced but much work remains. Building on our first two reports, the Task Force will continue to conduct additional consultations with stakeholders across Canada and work to disseminate best practices to enable change. The next and final phase of our work will involve collaborating with key stakeholders, including the chronic pain community, federal, provincial and territorial governments, health professionals, researchers, and Indigenous Peoples, and others to disseminate information related to best practices for the prevention and management of chronic pain, including for populations disproportionally affected by chronic pain (e.g., women, older Canadians, Indigenous populations, children, Veterans). The final Task Force report is expected in December 2021 and will focus on strategies for improving approaches to pain in Canada. We will continue to increase awareness of chronic pain and to build relationships and networks for change across the country. We believe that together, by igniting a commitment to change, we can improve the health and well-being of Canadians.
Appendix A: Questionnaire demographic results
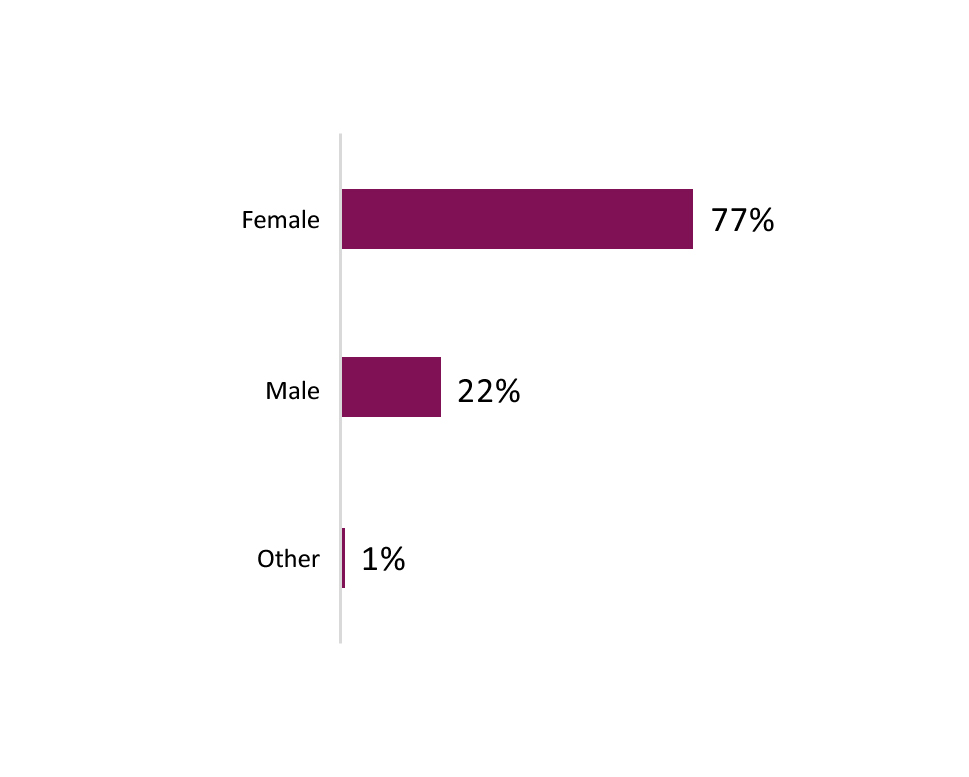
Q1: What is your gender?: Text description
This graph shows the percentage of consultation participants who identify as female, male, or other gender.
- Female: 77%
- Male 22%
- Other 1%
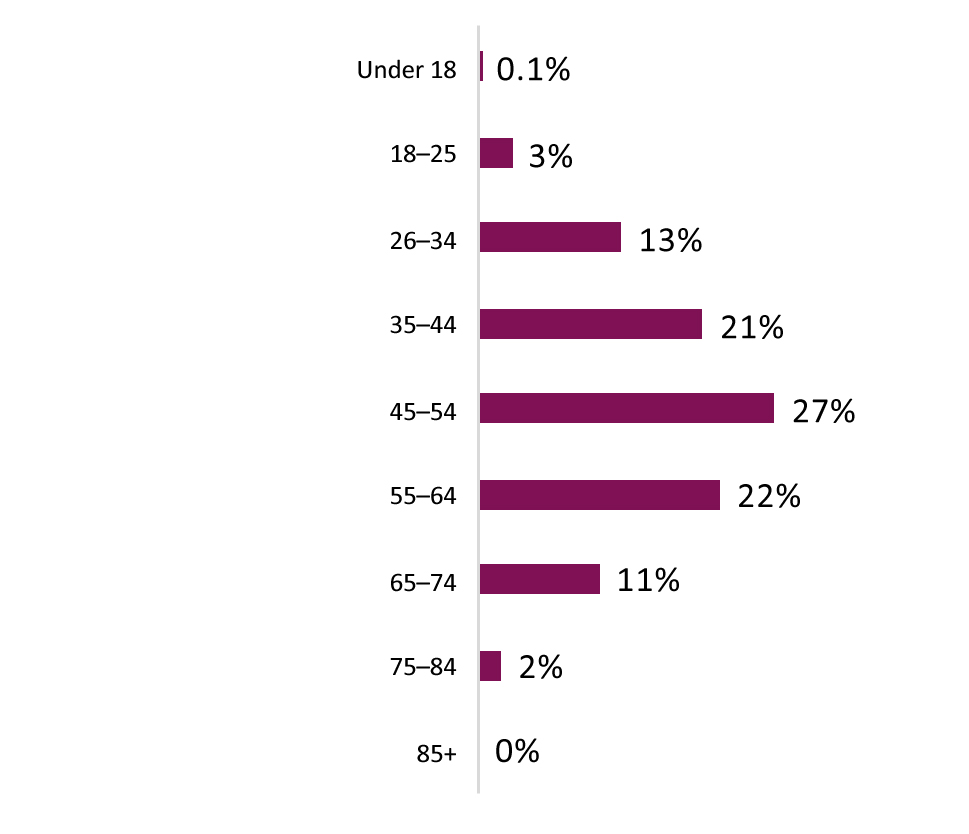
Q2: What is your age?: Text description
This graph shows the percentage of consultation participants across age groups.
- Under 18: 0.1%
- 18-25: 3%
- 26-34: 13%
- 35-44: 21%
- 45-54: 27%
- 55-64: 22%
- 65-74: 11%
- 75-84: 2%
- 85+: 0%
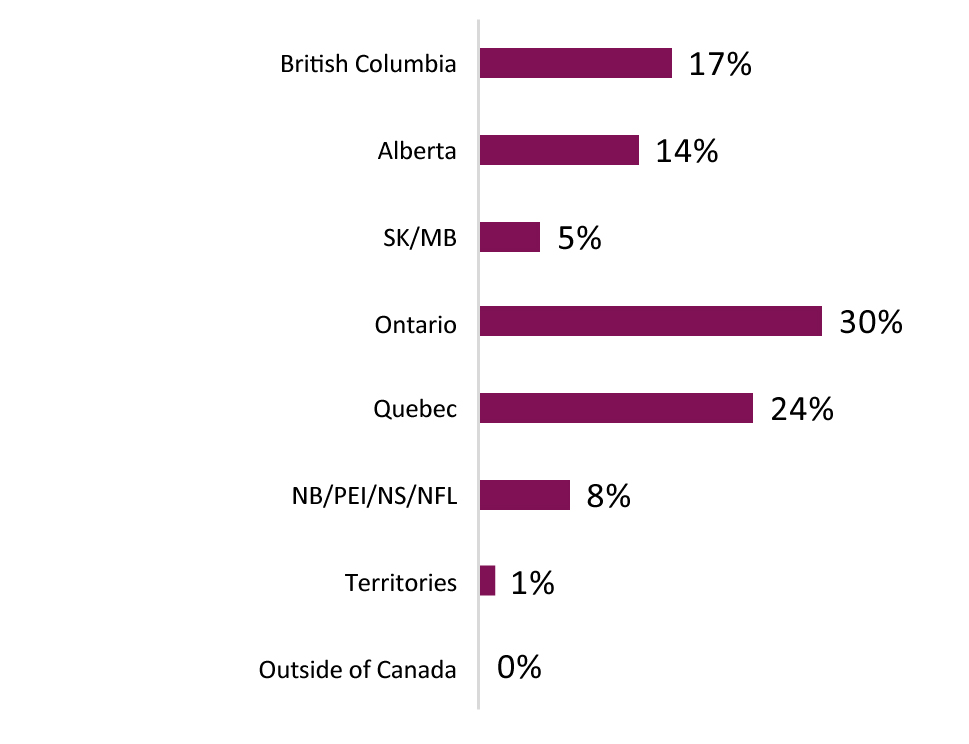
Q3: In which province/territory do you live?: Text description
This graph shows the percentage of consultation participants that reside in each province or territory.
- British Columbia: 17%
- Alberta: 14%
- Saskatchewan and Manitoba: 5%
- Ontario: 30%
- Quebec: 24%
- New Brunswick, Prince Edward Island, Nova Scotia, and Newfoundland and Labrador: 8%
- Territories: 1%
- Outside of Canada: 0%

Q4: Please choose the region that best describes the area where you live?: Text description
This graph shows the percentage of consultation participants that reside in rural and small, medium, and large population centres.
- Rural area (e.g., population less than 1,000): 6%
- Small population centre (e.g., 1,000 to 29,999): 21%
- Medium population centre (30,000 to 99,999): 18%
- Large urban population centre (e.g., 100,000 or greater): 54%
- Other: 1%
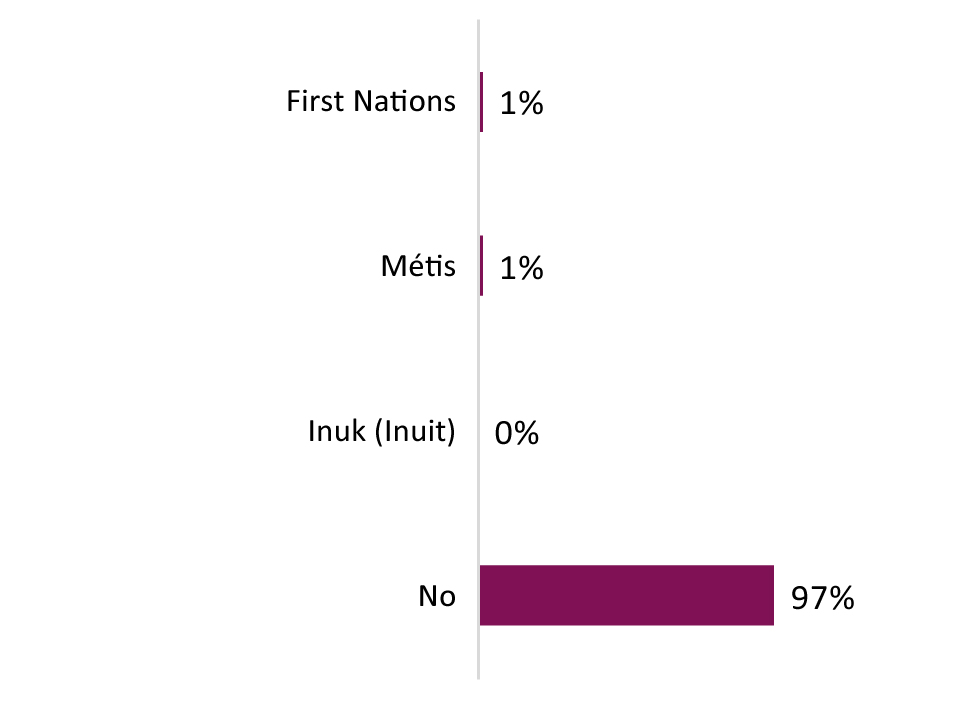
Q5: Are you First Nations, Métis, or Inuk (Inuit)? [Select all that apply]: Text description
This graph shows the percentage of consultation participants who self-identify as First Nations, Métis, or Inuk (Inuit).
- First Nations: 1%
- Metis: 1%
- Inuk (Inuit): 0%
- No: 97%
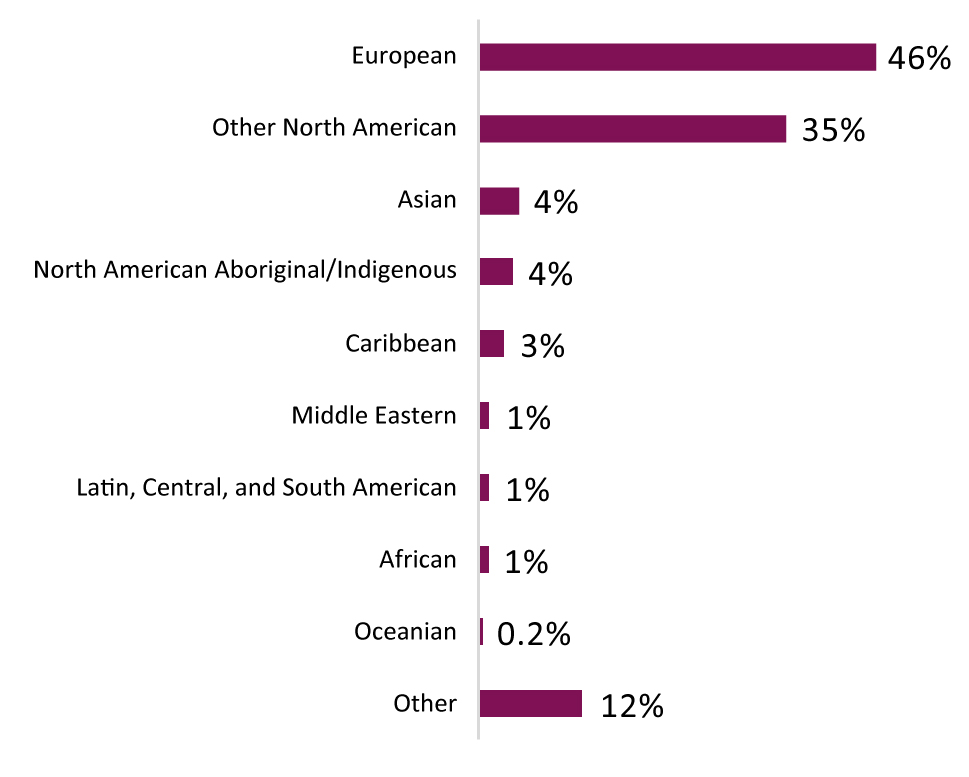
Q6: With which ethnic or cultural group or groups do you identify? [Select all that apply]: Text description
This graph shows the percentage of consultation participants who self-identify with various ethnic or cultural groups.
- European: 46%
- Other North American: 35%
- Asian: 4%
- North American Aboriginal/Indigenous: 4%
- Caribbean: 3%
- Middle Eastern: 1%
- Latin, Central and South America: 1%
- African: 1%
- Oceanian: 0.2%
- Other: 12%
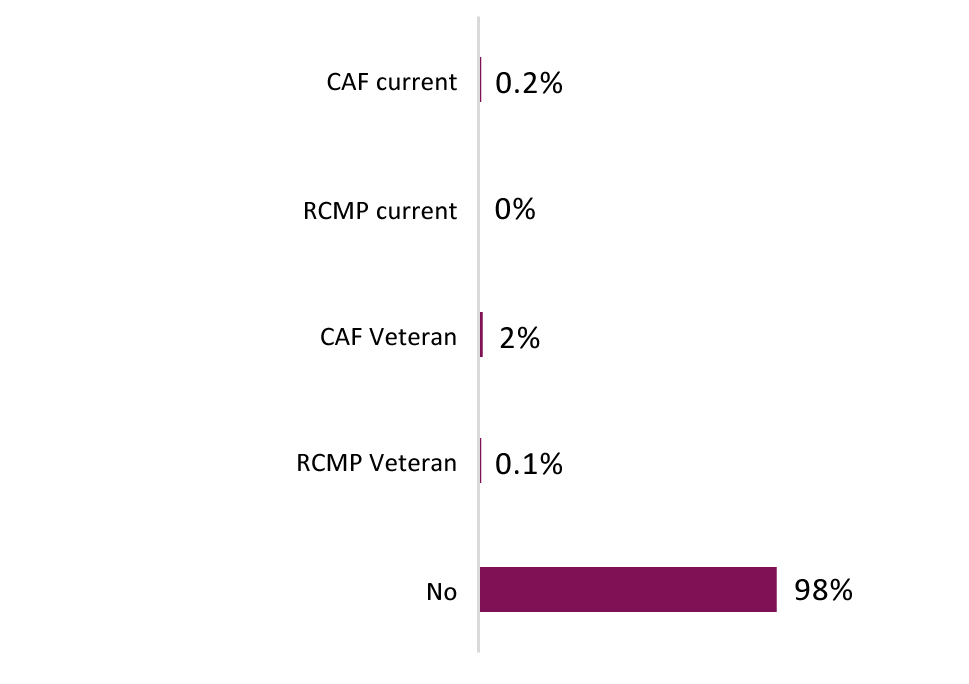
Q7: Are you a current or former member of the Canadian Armed Forces (CAF) or Royal Canadian Mounted Police (RCMP)?: Text description
This graph shows the percentage of consultation participants that are current or former members of the Canadian Armed Forces or Royal Canadian Mounted Police.
- CAF current: 0.2%
- RCMP current: 0%
- CAF Veteran: 2%
- RCMP Veteran: 0.1%
- No: 98%
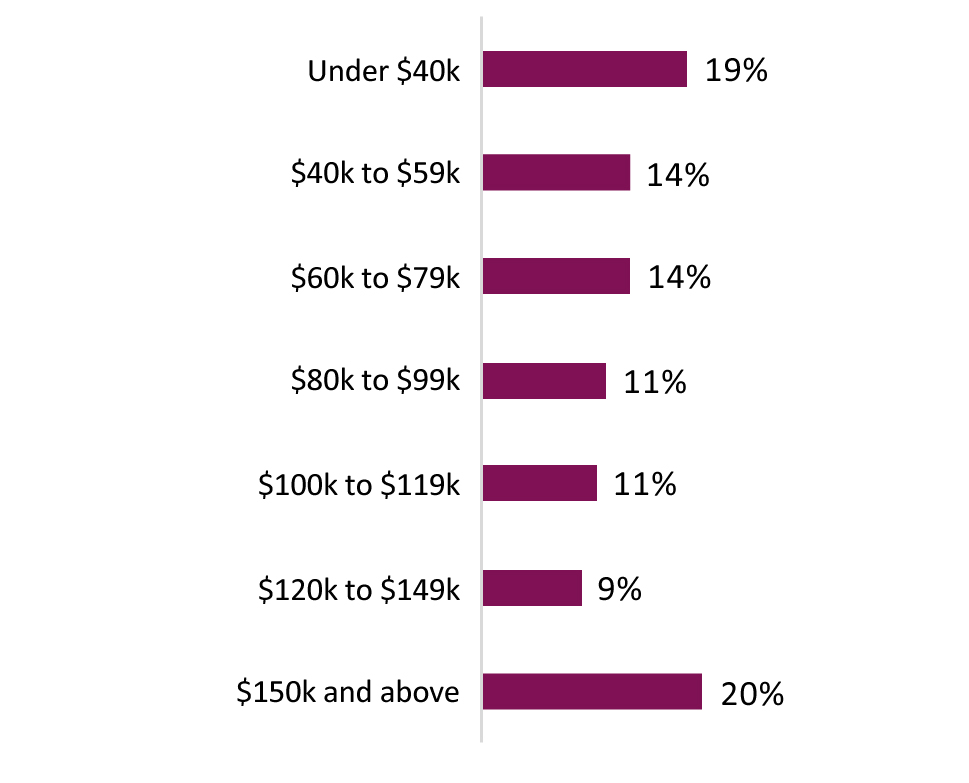
Q8: Which of the following categories best describes the total annual income of all persons in your household, before taxes?: Text description
This graph shows the percentage of total annual income categories self-reported by participants.
- Under $40k: 19%
- $40k to $59k: 14%
- $60k to $79k: 14%
- $80k to $99k: 11%
- $100 to $119k: 11%
- $120k to $149k: 9%
- $150k and above: 20%
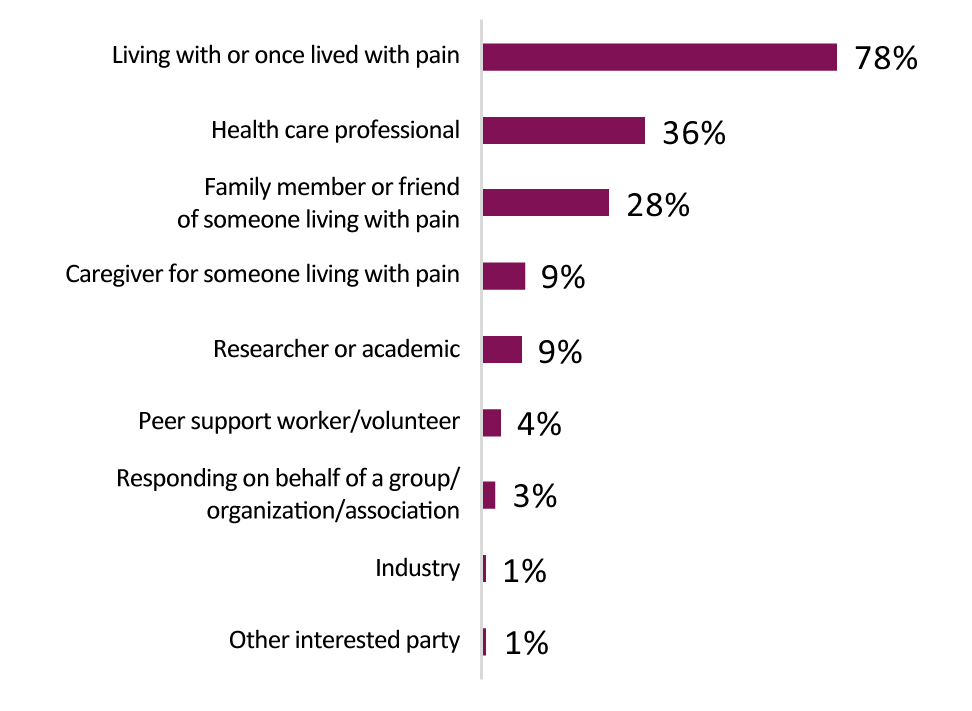
Q9: Please choose the group(s) that best describes you, or your experience(s) with pain. [Select all that apply]: Text description
This graph shows the percentage of participants identifying with different types of stakeholder categories.
- Living with or once lived with pain: 78%
- Health care professional: 36%
- Family member or friend of someone living with pain: 28%
- Caregiver for someone living with pain: 9%
- Researcher or academic: 9%
- Peer support worker/volunteer: 4%
- Responding on behalf of a group/organization/association: 3%
- Industry: 1%
- Other interested party: 1%
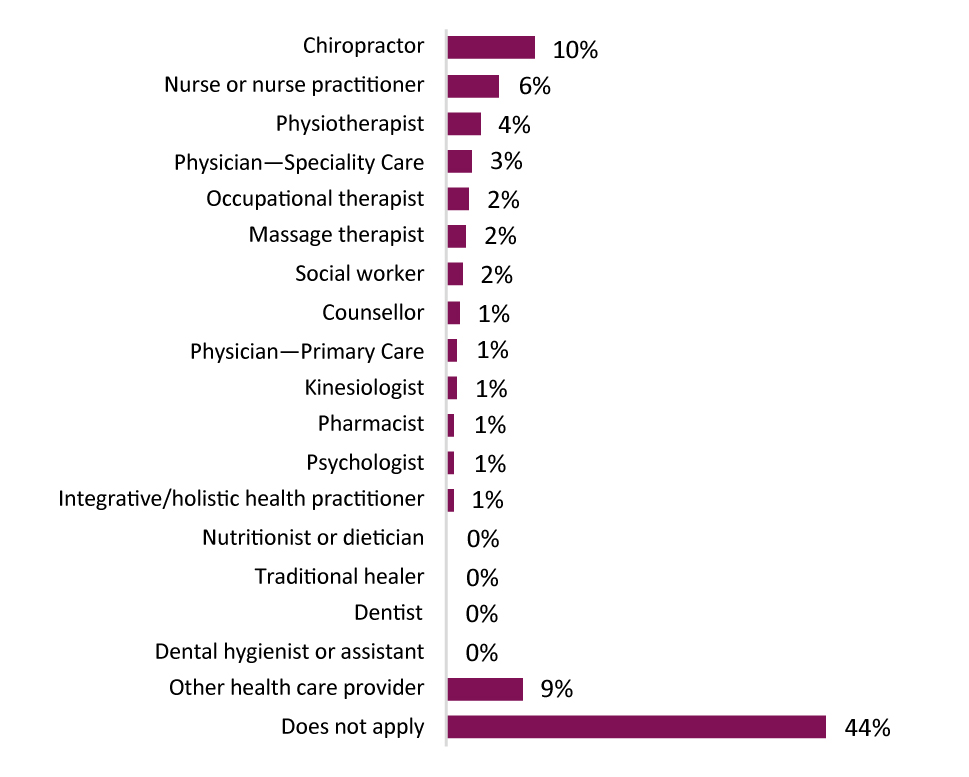
Q10: If you are a health care provider, please select the occupation(s) that best describes you. [Select all that apply]: Text description
This graph shows the percentage of participants self-identifying with various health care professional occupations.
- Chiropractor: 10%
- Nurse or nurse practitioner: 6%
- Physiotherapist: 4%
- Physician - specialty care: 3%
- Occupational therapist: 2%
- Massage therapist: 2%
- Social worker: 2%
- Counsellor: 1%
- Physician - primary care: 1%
- Kinesiologist: 1%
- Pharmacist: 1%
- Psychologist: 1%
- Integrative/holistic health practitioner: 1%
- Nutritionist or dietician: 0%
- Traditional healer: 0%
- Dentist: 0%
- Dental hygienist or assistant: 0%
- Other health care provider: 9%
- Does not apply: 44%
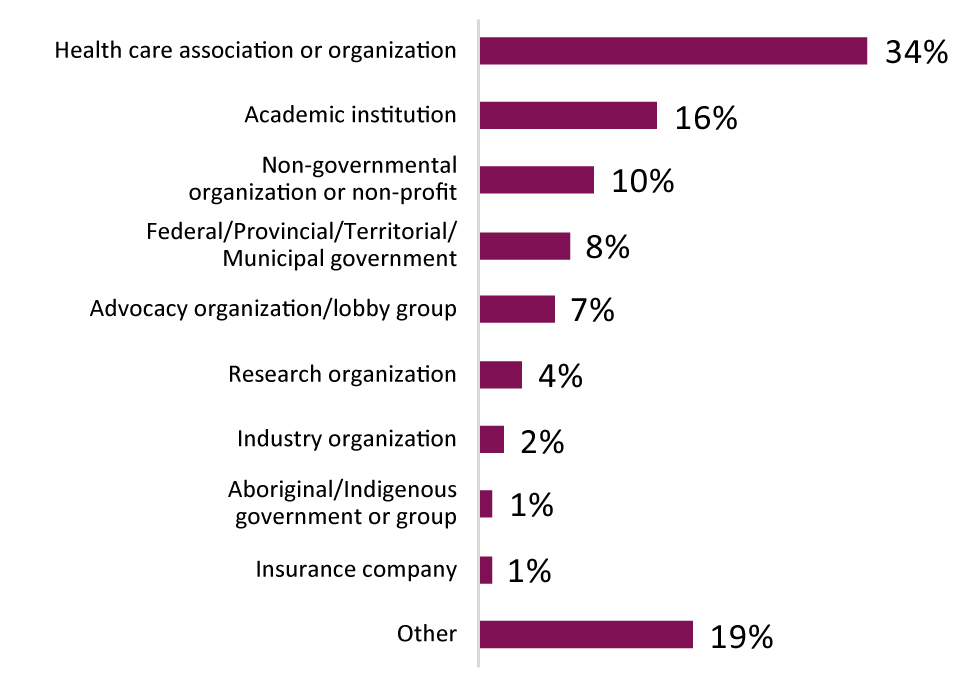
Q11: Please choose the group(s)/organization type(s) to which you belong. [Select all that apply]: Text description
This graph shows the percentage of consultation participants belonging to different organizations and/or groups.
- Health care association or organization: 34%
- Academic institution: 16%
- Non-governmental organization or non-profit: 10%
- Federal/Provincial/Territorial/Municipal government: 8%
- Advocacy organization/lobby group: 7%
- Research organization: 4%
- Industry organization: 2%
- Aboriginal/Indigenous government or group: 1%
- Insurance company: 1%
- Other: 19%
Appendix B: Participant experiences
There are millions of people living with chronic pain across Canada. When engaging Canadians to better understand, prevent, and manage pain, the Canadian Pain Task Force asked people to outline:
- How pain has affected their life;
- The pain they have experienced, or are experiencing;
- Challenges they have faced; and,
- What has helped them the most.
After examining submissions, a number of key findings emerged. Those findings are outlined below, with supporting passages from individual contributions.
Self-advocacy and education are important tools for those living with pain
For many people living with pain, self-advocacy is often the only mechanism to receive the care and treatment that works for them. Several submissions mention instances where advocacy only occurs after years of mistrials and, often unsuccessful, experimentation with treatment options. Unfortunately, there are still many people living with pain who are unable to advocate for themselves.
"If you believe that pain only effects older people, you are vastly mistaken. I do believe that my chronic pain has made me resilient and great at advocating for myself. A great analogy I once heard and resonate with in explaining pain was that: pain is like a smoke alarm constantly going off, sometimes the alarm is really loud and all you can focus on, other times it is quieter and you are able to tune it out."
"As you can now surmise, I keep many balls in the air attending to my pain, all day, everyday, and it is what I must continue to do to maintain my current level of pain management. I have now gone through enough "pain emergencies" to understand that I cannot slack off...that if my supports were to be taken away, if I could no longer afford them, I would slide back into living in that zombie-like pain haze that is no life at all."
"I've lost all faith in our medical system. The neurologists were dismissive. When the neurologist ran out of drugs from the blue Pharmaceuticals book, he told me he could do nothing more. I went to a pain management clinic. Yep, more drugs. My family doctor sent a letter and said he'd taken on too many patients and was dropping me. I need an advocate."
Barriers to access for prescription opioid medications
Prescription opioid medications are sometimes a necessary treatment option for people living with pain and can provide stable pain relief. However, in light of increased awareness of the overdose crisis, there is often a stigma associated with prescription opioid medications and a sentiment among health care professionals and members of the public that people taking opioid medications are exhibiting drug seeking behaviour.
"I am a chronic pain sufferer … and had never indulged in anything stronger than anti-inflammatory medications. I was made to suffer major acute pain, and no one understood. If the Emergency room physician took the time to look at my past medical history, he would have discovered I don't take anything for pain, I try to manage it conservatively - I was prejudged. It has been five years since my last day of work and I have yet to see a pain specialist!"
"Two doctors refused to take me on because I was on opioids. I found a Nurse Practitioner to take me on but she was concerned about my using a Fentanyl Patch so she wanted me to use only MS Contin. I am struggling at times now because at times the MS Contin makes my feet and legs swell and does not always work for the pain. The Fentanyl Patch took care of a lot of the pain without that side effect. I am an adult. I am a former nurse and of sound mind. I understand the benefits and risks of opioid treatment and as such I should be able to get the medication that worked well for me. The Health Care Consent Act allows for autonomy and I am being denied the privilege of deciding my treatment."
"Many people living with chronic pain need some amount and duration of opioid painkiller to have any quality of life. Some may need it for life. The removal of this therapy from individuals against their will is shameful. Doctors should not be allowed to refuse patients because they are using opioids prescribed to them by other doctors."
"There is a very large stigma on pain regarding painkillers pain management you could say even if you mention that you have pain the doctors these days will automatically look at you differently almost as though you're seeking narcotics or are … just looking to get a prescription and get the hell out of the office."
Loss of dignity and autonomy
Many people living with pain detailed the physical, psychological, and emotional toll their pain has taken on them. Pain affects every part of their life, from their ability to hold down employment to their ability to maintain relationships and a social network. Pain is all encompassing and can define a person's existence.
"The pain has effected all aspects of my life over the 4 years I that have dealt with it in. This means it has affected me mentally, physically, emotionally, socially and financially. On the mental side of things, it has become next to impossible to focus as the pain consumes most of your focus at all times and makes thinking clearly extremely difficult. Physically it has taken away the ability to have the dignity of holding a job, altered my life in terms of my capability to do things as there is a price to pay for any activity you do."
"My emotional state has suffered greatly as I was always very independent and started working at 10 years old. To learn to rely on someone else for financial and physical support had been humiliating and heart breaking. I no longer feel like a contributing member if society."
"I wish for something that is more integrative and for a medical team trained in pain science and narrative medicine approaches that are able to figure out the underlying issues as a collective."
"I went from incredibly active, relevant and respected to home bound, ignored and judged a drug addict. It's been 8 years since this started. My self esteem is close to nonexistent."
"The emotional impact of pain is different for each person. For me, it was devastating when the pain was really bad. It took away my quality of life, my drive, and some of my passions as well. Till this day I live in fear of experiencing the same type of pain. I never want to experience that type of pain ever again so; I'm hesitant from doing certain things till this day."
Resiliency and adaption
Even in the face of chronic pain, people find ways to continue their daily lives and are contributing members of society. People living with pain find different ways of coping and managing their condition. For some, this includes social or spiritual approaches, others have found a combination of approaches, which have helped. With their firsthand experience of chronic pain, some people living with pain have become advocates and peer supports in the hopes of helping others.
"There's no one-size-fits-all one-pill-and-done treatment out there. The biggest challenge is to keep going. To work or school or both and deal with the household and everyday tasks and everything. What helps is sheer stubbornness but that's not always a positive character trait."
"Slow baby steps within this new way of being and supported by learning the power of formal meditation on the mind/body connection and how that all relates to chronic pain, set me on the path to gradual pain maintenance."
"I have good friends. I drink alcohol. Oh, not all the time. Days go by without a drop. A psychologist explained the difference between our sympathetic and parasympathetic nervous system and how alcohol relaxes the body. I only watch happy tv shows, no blood or guns or anything else that would depress me. OK, I do watch the news. Laughter is the best medicine."
"What kept me going was my family, my employer, friends, and God. My supervisor stood by me through the good and bad days. Giving me the room i needed to get to where i am today. That is priceless."
Coverage and out-of-pocket costs
For many people living with pain across Canada, coverage of treatments and medicines remains a concern. According to some, provincially funded health care plans could do a much better job at covering practitioner administered/manual therapy style interventions, such as physical or manual therapy. Even among those with private or employer provided insurance coverage, there is frustration at the lack of coverage for interventions such as medicinal cannabis or alternative therapies.
"I also believe I could return to gainful employment if I could afford my medical marijuana & get Real Rehabilitation aimed at improving my physical function & pain outcomes."
"I have chronic migraine. 28 days a month, at my worst. Un-medicated, 15 days at best. With $800/month medication, 3 days at best and 5 days at worst. What happens when I lose insurance coverage because I'm too old to be covered under my parent's plan? I could get a job with insurance coverage, but I won't be able to hold a job with more than half a month of "sick" days. It's an endless loop."
"Over the years, I have had to do battle on many fronts with my long-term disability insurance and extended health benefits provider to make them honour my coverage."
"All Canadians should have fair access to chiropractic services. Government health plans should fully cover patients for chiropractic care. Chiropractic care is proven scientifically to be safe, natural form of health care."
"Options like massage therapy, hydrotherapy, electro therapy, acupuncture - are not covered and I don't have the insurance or money like most."
"Traditional medication, opioids, and physiotherapy do not work for me, but that is all that is really covered for my plan. THC and CBD would cost a lot less then prescriptions!"
Understanding and empathy among health care professionals
Many people living with pain describe barriers to access for care based on stigma, or lack of understanding, by health care professionals. Several submissions highlight challenges with finding a health care professional willing to take them on as a patient, or who are reluctant to prescribe prescription opioid medications. According to some people living with chronic pain, the level of education and awareness among health care professionals about treatment options and chronic pain is lacking.
"All of my conditions have caused me debilitating pain throughout my life and it has been challenging to be taken seriously by my peers and even by doctors…"
"I'm afraid to even talk to the doctor about what I'm going through it seems like doctors are prejudiced against pain when doctors should be thinking about helping to treat people and the pain that they are having and try and communicate with patients about the potential harm with taking controlled substances or narcotics as a matter of fact the harm when taking any type of medication."
"As a health care professional, I know firsthand the stigma associated with chronic pain. Labels and assumptions abound. I have pasted on a smile and said I was okay even when I had used heat treatments to the point of developing blisters on my back. The 2 times that I worked up the courage to ask what I could do to help manage I was greeted to an open door, a suggestion to take acetaminophen and ibuprofen and end of conversation."
"My doctor dropped me as she did not want to deal with my symptoms and I was forced to drive 50 km away to find a doctor who would treat me because everyone pre-screened me by phone and would not accept me as a patient."
"I hope that the health industry can take education and support of pain to the next level because many suffer and are not fortunate to have the support I had."
Public awareness and understanding
There is a demonstrable lack of awareness and understanding in the public domain around chronic pain. For some people living with chronic pain, this has impacted their lives, relationships, and ability to function in society.
"One loses friends and even loved ones because of diminished capacity and the stigma of being "sick" in our societal norm of "being positive". Frequently, comments the individual with chronic pain makes about daily difficulties are met with either disbelief or minimization."
"Even though women with disabilities are becoming pregnant at increasing rates, they continue to experience a great deal of stigma related to sexuality and motherhood."
"I was ashamed and afraid of showing my nose outside my home, for being the topic of conversation, comments like "sure, she has a bad back…what a great way to get out of work…why is she parking in the disability spot, she got nothing wrong with her…etc."
Effects of the COVID-19 pandemic
The COVID-19 pandemic has impacted the lives of all Canadians. For people living with chronic pain, it has greater potential to impact the care they receive, their financial situation, and their overall mental health.
"I am unable to have appointments with physicians as the COVID-19 is keeping me inside and the telephone consultations all require tests and follow-up - none of which can happen."
"As the mom of a child who has a serious chronic condition, these COVID times have wrecked havoc on our family. My child has had 4 acute bouts of her condition and the latest was one week ago. We had no way of reaching her specialist since his clinic was closed and her condition was worsening by the day."
"My life has changed. COVID-19 has been stressing me out and only makes the pain worse."
"The isolation is nothing new for me. I am an expert. However, when I hear all the discussion about the difficulties of isolating, I am reminded of the invisibility I have endured for most of the last 25 years."
References
Alford, D. P., German, J. S., Samet, J. H., Cheng, D. M., Lloyd-Travaglini, C. A., & Saitz, R. (2016). Primary Care Patients with Drug Use Report Chronic Pain and Self-Medicate with Alcohol and Other Drugs. Journal of General Internal Medicine, 31(5), 486-491.
Allan, B., & Smylie, J. (2015). First Peoples, Second Class Treatment: The Role of Racism in the Health and Well-being of Indigenous Peoples in Canada, Discussion Paper. Wellesley Institute.
Azevedo, L. F., Costa-Pereira, A., Mendonça, L., Dias, C. C., & Castro-Lopes, J. M. (2016). The economic impact of chronic pain: A nationwide population-based cost-of-illness study in Portugal. The European Journal of Health Economics, 17(1), 87-98.
Baldacchino, A., Gilchrist, G., Fleming, R., & Bannister, J. (2010). Guilty until proven innocent: a qualitative study of the management of chronic non-cancer pain among patients with a history of substance abuse. Addictive behaviors, 35(3), 270-272.
Bartley, E. J., & Fillingim, R. B. (2013). Sex differences in pain: a brief review of clinical and experimental findings. British journal of anaesthesia, 111(1), 52-58.
Bell L., Cornish P., Gauthier R., Kargus C, Rash J., Robbins R., Ward S. & Poulin P. (2020) Implementation of the Ottawa Hospital Pain Clinic stepped care program: A preliminary report, Canadian Journal of Pain, 4:1, 168-178, DOI: https://doi.org/10.1080/24740527.2020.1768059
Benedict, T. M., Keenan, P. G., Nitz, A. J., & Moeller-Bertram, T. (2020). Post-traumatic stress disorder symptoms contribute to worse pain and health outcomes in veterans with PTSD compared to those without: a systematic review with meta-analysis. Military medicine.
Breitbart, W., Rosenfeld, B., Passik, S., Kaim, M., Funesti-Esch, J., & Stein, K. (1997). A comparison of pain report and adequacy of analgesic therapy in ambulatory AIDS patients with and without a history of substance abuse. Pain, 72(1-2), 235-243.
Breivik, H., Eisenberg, E., & O'Brien, T. (2013). The individual and societal burden of chronic pain in Europe: The case for strategic prioritisation and action to improve knowledge and availability of appropriate care. BMC Public Health, 13(1), 1229.
Browne, A. J., Varcoe, C., Lavoie, J., Smye, V., Wong, S. T., Krause, M.,... & Fridkin, A. (2016). Enhancing health care equity with Indigenous populations: evidence-based strategies from an ethnographic study. BMC Health Services Research, 16(1), 544.
Burgess, D. J., Gravely, A. A., Nelson, D. B., Van Ryn, M., Bair, M. J., Kerns, R. D.,... & Partin, M. R. (2013). A national study of racial differences in pain screening rates in the VA health care system. The Clinical journal of pain, 29(2), 118-123.
Burns LC, Ritvo SE, Ferguson MK, Clarke H, Seltzer Ze, Katz J. Pain catastrophizing as a risk factor for chronic pain after total knee arthroplasty: a systematic review. Journal of pain research. 2015; 8:21.
Campbell, C. M., & Edwards, R. R. (2012). Ethnic differences in pain and pain management. Pain management, 2(3), 219-230.
Canadian Institute for Health Information. (2020). Total number of unique patient count and total estimate hospital cost per specific ICD-10-CA chapters of interest, by patient type, submitted to Discharge Abstract Database and/or National Ambulatory Care Reporting System during the study period of fiscal year 2018-2019. Report. Information request for aggregated data by Health Canada, June 2020.
Canadian Public Health Association (2019). Integrating Trauma and Violence Informed Care Into Organizational Practice. https://www.publichealthontario.ca/-/media/event-presentations/grand-rounds-april-9-2019.pdf?la=en
Chapman, E. N., Kaatz, A., & Carnes, M. (2013). Physicians and implicit bias: how doctors may unwittingly perpetuate health care disparities. Journal of general internal medicine, 28(11), 1504-1510.
Chen, E. H., Shofer, F. S., Dean, A. J., Hollander, J. E., Baxt, W. G., Robey, J. L.,... & Mills, A. M. (2008). Gender disparity in analgesic treatment of emergency department patients with acute abdominal pain. Academic Emergency Medicine, 15(5), 414-418.
Clauw DJ, Häuser W, Cohen SP, Fitzcharles MA. Considering the potential for an increase in chronic pain after the COVID-19 pandemic [published online ahead of print, 2020 Jun 26]. Pain. 2020; 10.1097/j.pain.0000000000001950.
Correctional Service Canada (2019). Guidance for Chronic Non-Cancer Pain Management.
Craig, K. D., Holmes, C., Hudspith, M., Moor, G., Moosa-Mitha, M., Varcoe, C., & Wallace, B. (2020). Pain in persons who are marginalized by social conditions. Pain, 161(2), 261.
Dassieu, L., Kaboré, J. L., Choinière, M., Arruda, N., & Roy, É. (2019). Chronic pain management among people who use drugs: A health policy challenge in the context of the opioid crisis. International Journal of Drug Policy, 71, 150-156.
Deloitte Access Economics. (2019). The cost of pain in Australia: Painaustralia. Canberra: Deloitte.
Denison, J., Varcoe, C., & Browne, A. J. (2014). Aboriginal women's experiences of accessing health care when state apprehension of children is being threatened. Journal of advanced nursing, 70(5), 1105-1116.
Ding Y-Y, Yao P, Wu L, et al. Body mass index and persistent pain after breast cancer surgery: findings from the women's healthy eating and living study and a meta-analysis. Oncotarget. 2017;8(26):43332.
Dorado, K., Schreiber, K. L., Koulouris, A., Edwards, R. R., Napadow, V., & Lazaridou, A. (2018). Interactive effects of pain catastrophizing and mindfulness on pain intensity in women with fibromyalgia. Health psychology open, 5(2), 2055102918807406.
Dragon, C. N., Guerino, P., Ewald, E., & Laffan, A. M. (2017). Transgender Medicare beneficiaries and chronic conditions: exploring fee-for-service claims data. LGBT health, 4(6), 404-411.
Driscoll, M., Adams, L., & Satchell, J. (June 19, 2020). Optimizing Care Using a Trauma-Informed Approach. Practical Pain Management, 20(3), pp. 29-31 https://www.practicalpainmanagement.com/treatments/psychological/optimizing-care-using-trauma-informed-approach
Dworkin, R. H., Turk, D. C., Farrar, J. T., Haythornthwaite, J. A., Jensen, M. P., Katz, N. P.,... Witter, J. (2005). Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain, 113(1) Retrieved from https://journals.lww.com/pain/Fulltext/2005/01000/Core_outcome_measures_for_chronic_pain_clinical.5.aspx
Dunn, K. E., Finan, P. H., Tompkins, D. A., Fingerhood, M., & Strain, E. C. (2015). Characterizing pain and associated coping strategies in methadone and buprenorphine-maintained patients. Drug and alcohol dependence, 157, 143-149.
Eccleston C, Blyth FM, Dear BF, et al. Managing patients with chronic pain during the COVID-19 outbreak: considerations for the rapid introduction of remotely supported (eHealth) pain management services. Pain. 2020;161(5):889-893. doi:10.1097/j.pain.0000000000001885
Fredriksen-Goldsen, K. I., Kim, H. J., Shui, C., & Bryan, A. E. (2017). Chronic health conditions and key health indicators among lesbian, gay, and bisexual older US adults, 2013-2014. American journal of public health, 107(8), 1332-1338.
Gaskin, D. J., & Richard, P. (2012). The economic costs of pain in the united states. The Journal of Pain, 13(8), 715-724.
Gladstone, E. J., Smolina, K., Weymann, D., Rutherford, K., & Morgan, S. G. (2015). Geographic variations in prescription opioid dispensations and deaths among women and men in British Columbia, Canada. Medical Care, 53(11), 954-959.
Government of Nova Scotia, Nova Scotia Health Authority, & IWK Health Centre. (2015). Trauma-informed approaches to care. https://novascotia.ca/dhw/addictions/documents/TIP_Discussion_Guide_1.pdf
Grace, V. (2001). Critical encounters with the medical paradigm: Encouraging dialogue. Feminism & Psychology, 11(3), 421-428.
Green, C. R., Anderson, K. O., Baker, T. A., Campbell, L. C., Decker, S., Fillingim, R. B.,... & Todd, K. H. (2003). The unequal burden of pain: confronting racial and ethnic disparities in pain. Pain medicine, 4(3), 277-294.
Greenberg, M. (July 27, 2020). Trauma, PTSD, and Chronic Low-Grade Inflammation. https://www.psychologytoday.com/us/blog/the-mindful-self-express/202007/trauma-ptsd-and-chronic-low-grade-inflammation
Guerriere, D. N., Choinière, M., Dion, D., Peng, P., Stafford-Coyte, E., Zagorski, B.,... Clark, A. J. (2010). The Canadian STOP-PAIN project-Part 2: What is the cost of pain for patients on waitlists of multidisciplinary pain treatment facilities? Canadian Journal of Anesthesia/Journal Canadien d'Anesthésie, 57(6), 549-558.
Heimer, R., Zhan, W., & Grau, L. E. (2015). Prevalence and experience of chronic pain in suburban drug injectors. Drug and alcohol dependence, 151, 92-100.
Hewes, H. A., Dai, M., Mann, N. C., Baca, T., & Taillac, P. (2018). Prehospital pain management: disparity by age and race. Prehospital Emergency Care, 22(2), 189-197.
Hoffman, K. M., Trawalter, S., Axt, J. R., & Oliver, M. N. (2016). Racial bias in pain assessment and treatment recommendations, and false beliefs about biological differences between blacks and whites. Proceedings of the National Academy of Sciences, 113(16), 4296-4301.
Hogan, M., Taddio, A., Katz, J., Shah, V., & Krahn, M. (2016). Incremental health care costs for chronic pain in Ontario, Canada: A population-based matched cohort study of adolescents and adults using administrative data. Pain, 157(8), 1626-1633.
Hovey, Richard B. Dr.; Linkiewich, Delane Ms.; and Brachaniec, Mary Ms. (2020) "Chronic pain, vulnerability and human spirit while living under the umbrella of COVID-19," Patient Experience Journal: Vol. 7: Iss. 2, Article 8.
Jimenez, N., Garroutte, E., Kundu, A., Morales, L., & Buchwald, D. (2011). A review of the experience, epidemiology, and management of pain among American Indian, Alaska Native, and Aboriginal Canadian peoples. The Journal of Pain, 12(5), 511-522.
Kascakova, N., Furstova, J., Hasto, J., Madarasova Geckova, A., & Tavel, P. The Unholy Trinity: Childhood Trauma, Adulthood Anxiety, and Long-Term Pain. Int. J. Environ. Res. Public Health 2020, 17, 414.https://www.mdpi.com/1660-4601/17/2/414#cite
Katz, J. D., Seaman, R., & Diamond, S. (2008). Exposing gender bias in medical taxonomy: Toward embracing a gender difference without disenfranchising women. Women's Health Issues, 18(3), 151-154.
Khatib Y, Madan A, Naylor JM, Harris IA. Do psychological factors predict poor outcome in patients undergoing TKA? A systematic review. Clinical Orthopaedics and Related Research®. 2015;473(8):2630-2638.
Klonoff, E. A. (2009). Disparities in the provision of medical care: an outcome in search of an explanation. Journal of behavioral medicine, 32(1), 48.
Lalonde, L., Choiniere, M., Martin, E., Berbiche, D., Perreault, S., & Lussier, D. (2014). Costs of moderate to severe chronic pain in primary care patients - a study of the ACCORD program. Journal of Pain Research, 7, 389-403. doi:10.2147/JPR.S55388
Langley, P., Müller-Schwefe, G., Nicolaou, A., Liedgens, H., Pergolizzi, J., & Varrassi, G. (2010). The impact of pain on labor force participation, absenteeism and presenteeism in the European Union. Journal of Medical Economics, 13(4), 662-672.
Latimer, M., Rudderham, S., Lethbridge, L., MacLeod, E., Harman, K., Sylliboy, J. R.,... & Finley, G. A. (2018). Occurrence of and referral to specialists for pain-related diagnoses in First Nations and non-First Nations children and youth. CMAJ, 190(49), E1434-E1440.
LeResche, L. (2011). Defining gender disparities in pain management. Clinical Orthopaedics and Related Research®, 469(7), 1871-1877.
Liu J, Zhang G, Zhang F, Song C. The Lessons and Experiences That Can Be Learned From China in Fighting Coronavirus Disease 2019. Front Public Health. 2020; 8:227. Published 2020 May 27. doi:10.3389/fpubh.2020.00227
Lord, B., & Khalsa, S. (2019). Influence of patient race on administration of analgesia by student paramedics. BMC emergency medicine, 19(1), 32.
Lynch, M., Williamson, O., & Banfield, J. (2020) COVID-19 Impact and Response by Canadian Pain Clinics: A National Survey of Adult Pain Clinics, Canadian Journal of Pain, DOI: https://doi.org/10.1080/24740527.2020.1783218
Mann, E. G., Johnson, A., & VanDenKerkhof, E. G. (2016). Frequency and characteristics of healthcare visits associated with chronic pain: results from a population-based Canadian study. Canadian Journal of Anesthesia/Journal canadien d'anesthésie, 63(4), 411-441.
McConkey, S. (2017). Indigenous access barriers to health care services in London, Ontario. University of Western Ontario Medical Journal, 86(2), 6-9.
Meana, M., Cho, R., & DesMeules, M. (2004). Chronic pain: the extra burden on Canadian women. BMC women's health, 4(1), 1-11.
Milliken, O.V., et al. (forthcoming). Cost of chronic pain in Canada. Technical report. Health Canada
Mogil, J. S. (2020). Qualitative sex differences in pain processing: emerging evidence of a biased literature. Nature Reviews Neuroscience, 1-13.
Mossey, J. M. (2011). Defining racial and ethnic disparities in pain management. Clinical Orthopaedics and Related Research®, 469(7), 1859-1870.
National LGBT Health Education Centre. Addressing opioid use disorder among LGBTQ populations. Boston: Fenway Institute, 2018.
Nelson, S., Simon, L., & Logan, D. (2018) The Incidence of Adverse Childhood Experiences (ACEs) and Their Association With Pain-related and Psychosocial Impairment in Youth With Chronic Pain. The Clinical Journal of Pain, 34(5), pp. 402-408. https://www.ingentaconnect.com/content/wk/cjpn/2018/00000034/00000005/art00002
Nicol, A. L. et al. (2016). The Association Between a History of Lifetime Traumatic Events and Pain Severity, Physical Function, and Affective Distress in Patients with Chronic Pain. The Journal of Pain, 17(12), pp 1334-1348. https://www.jpain.org/action/showPdf?pii=S1526-5900%2816%2930222-X
Office of the Correctional Investigator (2019). Aging and Dying in Prison: An Investigation into the Experiences of Older Individuals in Federal Custody. https://www.oci-bec.gc.ca/cnt/rpt/oth-aut/oth-aut20190228-eng.aspx
Office of the Federal Ombudsman for the Victims of Crime (2020) Crime Victims' Experience with Chronic Pain in Canada. A formal submission to the Canadian Pain Task Force.
Owens, A., Holroyd, B. R., & McLane, P. (2020). Patient race, ethnicity, and care in the emergency department: A scoping review. Canadian Journal of Emergency Medicine, 22(2), 245-253.
Pagé MG, Lacasse A, Dassieu L, Hudspith M, Moor G, Sutton K, Thompson J, Dorais M, Janelle-Montcalm A, Sourial N, Choinière M. Pain status and psychological distress among individuals who live with chronic pain during the COVID-19 pandemic: The Chronic pain & COVID-19 Pan-Canadian Study. Paper under review for publication in Lancet, 2020.
Pain Clinic Guidelines Task Force, IASP. Pain Treatment Services. Available from URL; https://www.iasp-pain.org/Education/Content.aspx?ItemNumber=1381 (accessed August 31, 2020).
Patrick White (2015). New inmates denied medicine due to drug-plan flaw: prison ombudsman. The Globe and Mail.
Peles, E., Schreiber, S., Gordon, J., & Adelson, M. (2005). Significantly higher methadone dose for methadone maintenance treatment (MMT) patients with chronic pain. Pain, 113(3), 340-346.
Pinheiro MB, Ferreira ML, Refshauge K, et al. Symptoms of depression as a prognostic factor for low back pain: a systematic review. The Spine Journal. 2016;16(1):105-116.
Public Health Agency of Canada (2018). Trauma and violence-informed approaches to policy and practice. https://www.canada.ca/en/public-health/services/publications/health-risks-safety/trauma-violence-informed-approaches-policy-practice.html#s5
Public Health Agency of Canada. (2017). The economic burden of illness in Canada, 2010. Ottawa, Canada: The Government of Canada.
Purkey, E., Patel, R., & Phillipa, S. (2018). Trauma-informed care. Better care for everyone. Canadian Family Physician, 64(3), pp. 170-172.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5851387/
Quintner, J. (2020). Why are women with fibromyalgia so stigmatized? Pain Medicine (Malden, Mass.).
Rabbitts JA, Fisher E, Rosenbloom BN, Palermo TM. Prevalence and predictors of chronic postsurgical pain in children: a systematic review and meta-analysis. The journal of pain. 2017;18(6):605-614.
Racine, M., Dion, D., Dupuis, G., Guerriere, D. N., Zagorski, B., Choinière, M.,... & Gordon, A. (2014). The Canadian STOP-PAIN project: the burden of chronic pain—does sex really matter? The Clinical journal of pain, 30(5), 443-452.
Reitsma, M. L., Tranmer, J. E., Buchanan, D. M., & Vandenkerkhof, E. G. (2011). The prevalence of chronic pain and pain-related interference in the Canadian population from 1994 to 2008. Chronic Dis Inj Can, 31(4), 157-164.
Reitsma, M.I., J.E. Tranmer, D.M. Buchanan & E.G. VanDenKerhof. (2012). The epidemiology of chronic pain in Canadian men and women between 1994 and 2007: Results from the longitudinal component of the National Population Health Survey. Pain research and management 17(3): 166-172.
Rush et al. (2008). Prevalence of co-occurring substance use and other mental disorders in the Canadian population. Canadian Journal of Psychiatry, 53: 800-9.
Samoborec S, Ruseckaite R, Ayton D, Evans S. Biopsychosocial factors associated with non-recovery after a minor transport-related injury: a systematic review. PloS one. 2018;13(6):e0198352.
Samulowitz, A., Gremyr, I., Eriksson, E., & Hensing, G. (2018). "Brave men" and "emotional women": A theory-guided literature review on gender bias in health care and gendered norms towards patients with chronic pain. Pain Research and Management, 2018.
Schopflocher, D., Taenzer, P., & Jovey, R. (2011). The prevalence of chronic pain in Canada. Pain research and management, 16.
Stanford, E. A., Chambers, C. T., Biesanz, J. C., & Chen, E. (2008). The frequency, trajectories and predictors of adolescent recurrent pain: a population-based approach. Pain, 138(1), 11-21.
Statistics Canada. 2020. Canadian Community Health Survey. Annual component (shared file). Statistics Canada (producer). Accessed at Health Canada, September 2020.
Steingrímsdóttir, Ó. A., Landmark, T., Macfarlane, G. J., & Nielsen, C. S. (2017). Defining chronic pain in epidemiological studies: a systematic review and meta-analysis. Pain, 158(11), 2092-2107.
Strath, L. J., Sorge, R. E., Owens, M. A., Gonzalez, C. E., Okunbor, J. I., White, D. M.,... & Goodin, B. R. (2020). Sex and Gender are Not the Same: Why Identity Is Important for People Living with HIV and Chronic Pain. Journal of Pain Research, 13, 829.
Theunissen M, Peters ML, Bruce J, Gramke H-F, Marcus MA. Preoperative anxiety and catastrophizing: a systematic review and meta-analysis of the association with chronic postsurgical pain. The Clinical journal of pain. 2012;28(9):819-841.
Todd, K. H., Deaton, C., D'Adamo, A. P., & Goe, L. (2000). Ethnicity and analgesic practice. Annals of emergency medicine, 35(1), 11-16.
Totsch, S. K., & Sorge, R. E. (2017). Immune system involvement in specific pain conditions. Molecular Pain. https://doi.org/10.1177/1744806917724559
Trompetter, H. R., Bohlmeijer, E. T., Fox, J. P., & Schreurs, K. M. (2015). Psychological flexibility and catastrophizing as associated change mechanisms during online Acceptance & Commitment Therapy for chronic pain. Behaviour research and therapy, 74, 50-59.
Turk, D. C., & Okifuji, A. (2002). Psychological factors in chronic pain: Evolution and revolution. Journal of consulting and clinical psychology, 70(3), 678.
Verwoerd M, Wittink H, Maissan F, de Raaij E, Smeets RJ. Prognostic factors for persistent pain after a first episode of nonspecific idiopathic, non-traumatic neck pain: A systematic review. Musculoskeletal Science and Practice. 2019; 42:13-37.
Veterans Affairs Canada (2019). Learn about PTSD. https://www.veterans.gc.ca/eng/health-support/mental-health-and-wellness/understanding-mental-health/learn-ptsd#b1
Veterans Affairs Canada Research Directorate (2018). Chronic Pain in veterans. https://www.veterans.gc.ca/pdf/about-vac/research/research-directorate/info-briefs/chronic-pain.pdf
Voon, P., Callon, C., Nguyen, P., Dobrer, S., Montaner, J. S., Wood, E., & Kerr, T. (2015). Denial of prescription analgesia among people who inject drugs in a Canadian setting. Drug and Alcohol Review, 34(2), 221-228.
Voon, P., Callon, C., Nguyen, P., Dobrer, S., Montaner, J., Wood, E., & Kerr, T. (2014). Self-management of pain among people who inject drugs in Vancouver. Pain management, 4(1), 27-35.
Wang, L., Guyatt, G. H., Kennedy, S. A., Romerosa, B., Kwon, H. Y., Kaushal, A.,... & Parascandalo, S. R. (2016). Predictors of persistent pain after breast cancer surgery: a systematic review and meta-analysis of observational studies. CMAJ, 188(14), E352-E361.
Williams, A. C. D. C., & Amris, K. (2017). Treatment of persistent pain from torture: review and commentary. Medicine, conflict and survival, 33(1), 60-81.
Wilson, M. G., Lavis, J. N., & Ellen, M. E. (2015). Supporting chronic pain management across provincial and territorial health systems in Canada: Findings from two stakeholder dialogues. Pain Research & Management, 20(5), 269-279.
Wylie, L., & McConkey, S. (2019). Insiders' insight: discrimination against indigenous peoples through the eyes of health care professionals. Journal of racial and ethnic health disparities, 6(1), 37-45.
Footnotes
- Footnote 1
-
This estimate is based on the total noninstitutionalized population living in Canadian provinces from the 2019 Canadian Community Health Survey.
- Footnote 2
- Footnote 3
-
Even primary pain, as per a new International Classification of Diseases (ICD-11), is assigned an origin: e.g., in this study, fibromyalgia and chronic migraine are classified under diseases of musculoskeletal and nervous system, respectively, using the current ICD-10 classification.
- Footnote 4
-
The Statistics Canada's 2019 Canadian Community Health Survey contains a question: "Are you usually free of pain or discomfort?" This definition has proved to be a valid measure of chronic pain in the general population (Reitsma et al., 2011).
- Footnote 5
-
This estimate is based on the total noninstitutionalized population living in Canadian provinces from the 2019 CCHS (Statistics Canada, 2020).
- Footnote 6
-
This 2019 estimate is compared to an estimate from the 2015 CCHS.
- Footnote 7
-
Pain prevented no activities for 31.2% (95% CI: 25.2%-37.9%).
- Footnote 8
-
Note, whether costs differ by the level of activity limitation could not be discerned. The estimate is based on the estimate of the number of Canadians age 15 or older, whose pain prevents at least some activities of daily living.
- Footnote 9
-
This estimate is statistically significant at a 1% level.
- Footnote 10
-
The per-person direct cost estimates are similar to those for Ontario ($1,850, CAD 2019) and Australia ($2,040, CAD 2019), although the Ontario study (Hogan et al., 2016) uses a different method, which prevents a direct comparison. Note that while Deloitte (2019) includes both allocated (by pain origin) and unallocated health expenditures in its cost estimate, for comparison purposes, the Deloitte's estimate for allocated health expenditures is used here.
- Footnote 11
-
Presenteeism, here, refers to losses in productivity as employees are present at work, but are not fully functioning due to pain.
- Footnote 12
-
People who are at high risk for severe illness from COVID-19
Page details
- Date modified: