Lyme Disease in Canada - A Federal Framework
Download the entire report
(PDF format, 1.39 MB, 36 pages)
Organization: Public Health Agency of Canada
Type: Report
Date published: 2017-05-30
Table of contents
- Message from the Chief Public Health Officer
- An act respecting a Federal Framework on Lyme Disease
- Introduction
- A shared federal responsibility
- Foundation
- Conclusion
- Appendix 1: Lyme Disease in Canada: A Federal Action Plan
- Appendix 2: Conference to Develop a Federal Framework on Lyme Disease
- References
Message from the Chief Public Health Officer
Lyme disease is an emerging infectious disease in many parts of Canada, and the Government of Canada recognizes the impact that it has on Canadians and their families. Efforts to prevent and control Lyme disease are being made by a variety of stakeholders, but more can and should be done.
As the interim Chief Public Health Officer, I am concerned about the challenges associated with Lyme disease in Canada. I am grateful to health care providers, patients and their families who took the time to share their experiences. I heard both from patients who have been diagnosed with Lyme disease, as well as others who have experienced various chronic symptoms consistent with Lyme disease or similar ailments.
Overwhelmingly, we have heard that patients and the health professionals that care for them wish to see a call to action. As such, this framework includes an Action Plan (Appendix 1), which includes the establishment of a Lyme disease research network.
This is an emerging disease and we don't have all of the answers. As we move forward collectively, it is critical that we come together with an evidence-based approach, and address knowledge gaps through further research.
The Federal Framework on Lyme Disease in Canada is intended to help guide a way forward in areas where the federal government has a role. The Public Health Agency of Canada will work with public health, healthcare, patient groups, and other interested parties as we move forward together on the three pillars of surveillance, education and awareness, and guidelines and best practices. Strong emphasis will focus on the prevention of Lyme disease, so that the risk posed by Lyme disease to Canadians is minimized.
I invite all those who have a role to play to join in our collective action on Lyme disease. We will accomplish much by working together in a collaborative manner to identify and implement the solutions.
Dr. Theresa Tam, BMBS (UK), FRCPC
Interim Chief Public Health Officer
Public Health Agency of Canada
An act respecting a Federal Framework on Lyme Disease
The Federal Framework on Lyme Disease ActFootnote 1, which received Royal Assent on December 16, 2014, requires the federal government to develop a Federal Framework on Lyme Disease that would include the following three pillars:
- Surveillance: The establishment of a national medical surveillance program to use data collected by the Public Health Agency of Canada to properly track incidence rates and the associated economic costs of Lyme disease.
- Education and Awareness: The creation and distribution of standardized educational materials related to Lyme disease, for use by any public health care provider within Canada, designed to increase national awareness about the disease and enhance its prevention, identification, treatment and management.
- Guidelines and Best Practices: The establishment of guidelines regarding the prevention, identification, treatment and management of Lyme disease, and the sharing of best practices throughout Canada.
To inform the development of this framework, the Public Health Agency of Canada, on behalf of the Minister of Health, held a conference in May 2016. Over 500 people participated in person and via an online interface. Lyme disease patients, their families and others shared their experiences with Lyme disease. In addition, Lyme disease experts provided information on current knowledge and research related to Lyme disease treatment, prevention, diagnosis and management. Appendix 2 includes the full Conference Summary Report.
Introduction
Lyme disease is an infectious disease caused by the bacterium Borrelia burgdorferi (B. burgdorferi). This bacterium is transmitted to people through the bite of select types of infected ticks, namely, blacklegged ticks and western blacklegged ticks. Many species of ticks in Canada do not transmit B. burgdorferi. Ticks may also transmit multiple other pathogens, including bacteria and viruses, with the potential to cause a range of human illnessFootnote 2.
Canadian public health authorities at all levels of government are coordinated in the effort to monitor the spread of the ticks that can transmit Lyme disease, as well as the cases of Lyme disease among Canadians exposed to these ticks. This information enables the identification of Lyme disease risk areas.
Currently known risk areas are identified in Figure 1. Due to a variety of factors, including climate change, the risk in some regions is expanding. In many parts of Canada, Lyme disease is an emerging infectious disease. In addition, the movement of migratory birds and other animals contributes to an increased possibility of humans acquiring Lyme disease outside of known risk areas.
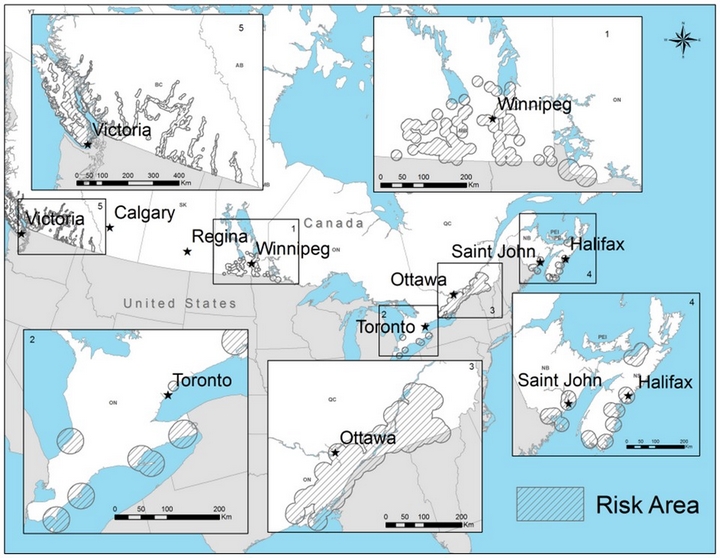
Figure 1 text description
This figure displays a background map showing 'risk areas'. Risk areas (hatched areas) are locations where the risk from tick bites and Lyme disease is known to occur, and where risk of tick bites and Lyme disease is possible.
The risk areas are indicated in insets on the map as follows:
Inset 1 - Southern Manitoba and Western Ontario
Risk areas can be found stretching from the Ontario border west to Turtle Mountain Provincial Park, and from the US border extending to the south shores of Lake Manitoba, Lake Winnipeg and into southern parts of the Interlake.
Inset 2 - Southern Ontario
There are five risk areas around Pointe-Pelee National Park, Rondeau Provincial Park, Turkey Point Provincial Park, Long Point peninsula including Long Point Provincial Park and the National Wildlife area, and Wainfleet bog near Welland on the Niagara peninsula.
Inset 3 - Southeastern Ontario and Southern Quebec
Risk areas are locations around Kingston in the Saint Lawrence valley that extend north east towards Ottawa, locations covering much of Montérégie, and parts of Estrie and Centre du Québec in the south of Québec.
Inset 4 - Maritime Provinces
In New Brunswick, risk areas are shown in Grand Bay/Westfield, Saint John, Rothesay, Quispamsis, St Stephen, Saint Andrews, St George and Grand Manan Island.
In Nova Scotia, risk areas are identified in areas of Halifax Regional Municipality and areas of the counties of Lunenburg, Shelburne, Yarmouth, Pictou and Queens.
Inset 5 - Southern British Columbia
Risk areas include much of Vancouver Island and the coast of British Columbia facing Vancouver Island, as well as river valleys across southern British Columbia.
The number of confirmed human cases in Canada has been growing steadily since Lyme disease became nationally notifiable in 2009 (see Figure 2). The number of cases is likely underreported, though the extent of this underreporting is not currently known.
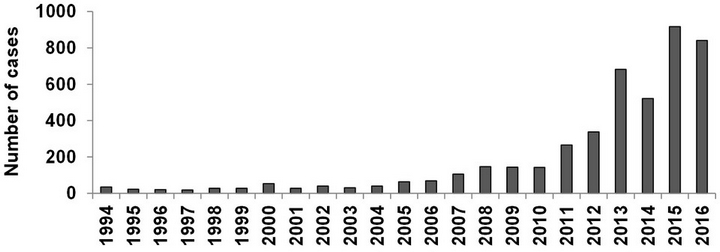
Figure 2 text description
| Year | Number of cases |
|---|---|
| 1994 | 35 |
| 1995 | 23 |
| 1996 | 21 |
| 1997 | 19 |
| 1998 | 28 |
| 1999 | 28 |
| 2000 | 53 |
| 2001 | 28 |
| 2002 | 40 |
| 2003 | 31 |
| 2004 | 40 |
| 2005 | 64 |
| 2006 | 69 |
| 2007 | 106 |
| 2008 | 147 |
| 2009 | 144 |
| 2010 | 143 |
| 2011 | 266 |
| 2012 | 338 |
| 2013 | 682 |
| 2014 | 522 |
| 2015 | 917 |
| 2016 | 841 |
The risk of exposure to Lyme disease occurs mainly in or near areas where tick populations that transmit the disease are established. Ticks that carry Lyme disease are active through much of the year. However, bites leading to human infection are much more common during the spring and summer months.
Adult ticks are about the size of a sesame seed, and nymphal (immature) ticks are about the size of a poppy seed. This means that people may not even know that they have a tick attached to them. The risk of exposure to ticks is highest in people engaging in occupational or leisure activities, such as camping and hiking, near or in forested or semi-forested areas where the ticks are found. Exposure to ticks can occur in other circumstances, such as gardening, golfing or dog walking, if these activities occur in locations where ticks are found.
A shared federal responsibility
The Government of Canada plays a national leadership role in preventing and controlling the spread of disease by helping to reduce the risk to Canadians posed by infectious diseases. It fulfills this role by tracking and monitoring infectious disease threats, undertaking research, promoting healthy behaviours, brokering knowledge transfer, and facilitating research and innovation.
Several federal government departments and agencies are involved in addressing Lyme disease in Canada:
The Public Health Agency of Canada (PHAC), as the Government of Canada's lead for public health, has focused efforts on tracking the incidence of Lyme disease nationally, increasing Lyme disease awareness among Canadians and front-line health professionals, monitoring the distribution and expansion of the Lyme disease risk areas in Canada to enhance prevention and control efforts, and supporting national consistency and standards in diagnosis across the country.
The Canadian Institutes of Health Research (CIHR) is the Government of Canada's health research funding agency, with a mandate to support the creation of new knowledge and its translation to various health areas including Lyme disease. For Lyme disease in particular, CIHR has supported work on the mode of action of B. burgdorferi, looking specifically at its molecular biology, virulence factors and pathogenicity.
Within Health Canada (HC), the First Nations and Inuit Health Branch supports the delivery of public health and primary health care services, including those related to Lyme disease, to on-reserve First Nations communities. The Health Products and Food Branch is responsible for: authorizing drugs for human and veterinary use, including antimicrobial agents and other drugs which may be used in the treatment of Lyme disease; authorizing vaccines for disease prevention; licensing diagnostic test kits used to support a clinical diagnosis of Lyme disease in humans; and the pre-market and post-market evaluation of veterinary drugs used for the treatment and control of tick infestations in animals. The Pest Management Regulatory Agency (PMRA) is responsible for pre-market evaluation and post-market monitoring of all pest control products, including those that are used to repel and control ticks.
The Department of National Defense (DND) / Canadian Armed Forces (CAF) is responsible for the delivery of health care services to CAF personnel in Canada and around the world. The DND/CAF, often in consultation with federal, provincial/territorial and local health partners, develops evidence-based policies, programs and interventions to prevent and manage Lyme disease among its military members, and to, as appropriate, support education and prevention programs for its civilian personnel.
Parks Canada (PC) raises awareness of Lyme disease risks in National Parks, National Historic Sites and National Marine Conservation Areas through the distribution of Lyme disease prevention/awareness materials.
In Canada, prevention and control of Lyme disease require collaboration among all levels of government and non-governmental organizations. As guided by the provisions of the Canada Health Act, provinces and territories are primarily responsible for the delivery of both direct health care services and public health activities. Provincial and territorial public health authorities, and Indigenous public health authorities, undertake prevention and control activities specific to their own jurisdictions. This work is conducted, in some jurisdictions, in collaboration with universities and other professional and non-governmental organisations.
Foundation
All stakeholders, including patients and their advocates, health care providers, and public health authorities, recognize the importance of evidence-based approaches to both public health and the practice of medicine. Similarly, many agree that additional research is needed to fill in evidence gaps that exist for Lyme disease prevention and control, diagnosis and treatment.
Moving forward with this Framework, the Public Health Agency of Canada will continue to use an evidence-based approach to prevent and control the spread of Lyme disease. Actions under the Framework will align with the federal role as they relate to the three pillars of: 1) surveillance; 2) education and awareness; and 3) guidelines and best practices. Implementation will require the involvement and collaboration of Lyme disease patients and their families, patient groups, health care providers, public health authorities, expert researchers, and federal, provincial and territorial governments.
To begin to address the evidence gaps, the Government of Canada will allocate new funding to address research gaps for Lyme disease, and will continue to collaborate with domestic and international partners to exchange best practices in the prevention, diagnosis and treatment of Lyme disease.
Surveillance
Surveillance is essential to understanding the risk posed to Canadians and is the foundation of the public health approach. Surveillance for Lyme disease includes monitoring both the distribution and spread of ticks that carry the pathogen Borrelia burgdorferi, and tracking human cases of the disease across the country.
Lyme disease in humans has been a nationally notifiable disease since 2009. Nationally notifiable diseases are infectious diseases that have been identified by the federal government and all provinces and territories as priorities for monitoring and control efforts. Data on these cases inform analyses of national and provincial trends in Lyme disease. The Public Health Agency of Canada's Lyme Disease Enhanced Surveillance (LDES) system aims to better identify where Lyme disease cases are occurring in Canada, what populations are most at risk, and disseminate information on the types of Lyme disease that are being reported in different jurisdictions.
Federal and provincial public health authorities will continue to build on surveillance activities through integration and dissemination of innovative methods and best practices for human surveillance. In addition, collection of human surveillance data in Canada for people who do not meet the case definition for probable or confirmed Lyme disease, but who experience various symptoms consistent with Lyme disease or similar ailments, will be initiated.
The increase in the distribution and number of individuals affected by Lyme disease in Canada is having a financial impact on the health care system. An analysis of the costs associated with Lyme disease will be undertaken, including both direct and indirect costs, where possible.
Moving forward, a national tick-borne surveillance system will be developed that includes Lyme disease and other possible co-infections. To reflect region-specific information where possible, the production of risk maps will be informed by: tick surveillance in national, provincial and regional parks, historic sites and ecological reserves, and on-reserve First Nations communities; integration of surveillance information available from veterinarians and their associations; and the use of electronic tools. This will inform prevention efforts through the provision of timely updates of the changing distribution of ticks capable of transmitting the disease.
Education and awareness
Efforts need to be strengthened to enhance Lyme disease educational efforts so that they are more effective and available to Canadians and front-line health professionals, in support of provincial and territorial governments and other efforts.
The Government of Canada's website (Canada.ca) provides information about the causes, symptoms, risks, treatment, and prevention tips for Lyme disease. This information is reviewed and updated on a regular basis to reflect the most current validated evidence. During the highest risk tick season, from April to October, public health authorities are engaged in delivering awareness activities to help educate the general public and front-line health professionals about Lyme disease.
Strengthening stakeholder engagement and partnerships will be critical to successful education and awareness campaigns. The development of early detection/early diagnosis educational materials, with a focus on high risk groups, will be supported to assist front-line health professionals and public health authorities in the prevention and timely diagnosis of Lyme disease using an evidence based and patient-centered approach.
Existing efforts will be strengthened, as there are a number of areas requiring attention by all Lyme disease stakeholders. Assessing the current knowledge base of front-line health professionals, and developing effective and targeted educational approaches would be beneficial to help improve the recognition of Lyme disease symptoms. Given that prevention is key in the public health approach for infectious diseases, a national tick and Lyme disease education and awareness campaign will be developed, in collaboration with partners, to complement existing outreach efforts aimed at reducing the risk of contracting Lyme disease and inform early intervention, diagnosis and treatment.
Guidelines and best practices
Guidelines and best practices that are evidence-based and effectively targeted to reach specific groups will be critical to address Lyme disease. To be of greatest use to front-line health professionals, it will be encouraged that guidelines focus on recommendations that are clear and actionableFootnote 4.
Focus on prevention
Currently, the best way to protect against Lyme disease is to prevent tick bites, or if bitten, to minimize the likelihood of infection by removing the tick in a timely, effective manner. Prevention and awareness programs are implemented by local public health authorities and other health care/veterinary providers to raise awareness of the risks of Lyme disease and measures to protect against tick bites. The Government of Canada will work with international public health partners to share best practices and these will be shared with all stakeholders.
Focus on diagnostics
The diagnosis of early Lyme disease infection by a physician or nurse practitioner is primarily a clinical one, based on symptoms and supported by a history of possible tick exposure, including travel history. Diagnosis is limited by the fact that not all patients will present with symptoms in the early stages. Current laboratory tests, which look for antibodies, perform better for untreated, later-stage Lyme disease, after the patient has developed an immune response.
The Canadian Public Health Laboratory Network, which provides national leadership through a proactive network of public health laboratories, monitors developments in laboratory diagnostics closely and publishes laboratory diagnostic guidelines that are consistent with those in the United States and Europe. New methods are evaluated, and any that prove to outperform current methods will be incorporated into updated guidelines for laboratories and front-line health professionals. Front-line health professionals and provincial laboratories will continue to be supported in the laboratory diagnosis of Lyme disease.
It is recognized that specific and more sensitive tests for Lyme disease are neededFootnote 5. Additional research would provide information about the impact of different strains of B. burgdorferi on diagnosis and disease in Canadians. Concerns about false negative tests results have led some patients to seek private testing. The development and availability of improved laboratory testing options may reduce the current practice where some patients seek laboratory testing in private, for-profit laboratories that may not be using standardized testing.
Focus on treatment
Current treatment guidelines for Lyme disease are developed by medical and scientific professional organizations, and are based on the best available evidence known worldwide. In Canada, the Association of Medical Microbiology and Infectious Diseases Canada (AMMI Canada) has endorsed and promoted the use of the Lyme disease treatment guidelines developed by the Infectious Diseases Society of America (IDSA), which represents physicians, scientists and other health care professionals who specialize in infectious disease. As such, the IDSA guidelines are used by the broader medical community.
There are a small number of front-line health professionals who follow guidelines developed by the International Lyme and Associated Disease Society (ILADS), a multidisciplinary medical society dedicated to the diagnosis and treatment of Lyme and its associated diseases. The treatment recommendations in the ILADS guideline are different from those in the IDSA, particularly with regards to antibiotic use. There remain evidence gaps which can be informed through further research on treatment options. Emerging evidence will be closely monitored and shared with patients, front-line health professionals, and other relevant stakeholders.
Some people experience symptoms that continue more than six months following treatment, described by some physicians as post-treatment Lyme disease syndrome or post Lyme disease syndrome. Other patients experience various chronic symptoms consistent with Lyme disease or similar ailments, sometimes referred to as chronic Lyme disease, which is not recognized by the majority of the medical community in Canada. Further research in this area is required into the causes of these persistent symptoms and chronic illness, and the methods of treatment. All partners, including provincial and territorial health care regulatory authorities, will be consulted on innovative, evidence-based approaches to address the needs of patients.
Focus on research
In recognition that additional research is needed to fill in evidence gaps, the Government of Canada will look to establish a Lyme disease research network that builds upon existing research and research networks, and will engage with clinical experts, researchers, and patient groups.
Conclusion
The Government of Canada has a national leadership role to play in the prevention and control of Lyme disease in Canada.
This Framework outlines key areas where progress is needed, and prioritizes areas of focus for action using a public health approach. An Action Plan is included in Appendix 1, and includes the establishment of a research network on Lyme disease.
While these actions will reflect those that can be undertaken by the Government of Canada, all interested parties are invited to identify actions that their respective organizations can take to contribute to progress for patients and the front-line health professionals that care for them.
This Framework will be reviewed within five years of its publication on the Canada.ca website.
Appendix 1
Lyme Disease in Canada: A Federal Action Plan
Lyme disease is a tick-borne infectious disease that is endemic or emerging in many parts of Canada.
The Federal Framework on Lyme Disease is intended to guide a way forward in areas where the Government of Canada has a role. The Government of Canada will work with public health, healthcare, patient groups, and other interested parties, and will place a strong emphasis on the prevention of Lyme disease so that the risk posed by Lyme disease to Canadians is minimized. Furthermore, the establishment of a Lyme disease research network will begin to address evidence gaps.
Public health actions under the Framework will align with the three pillars of: 1) surveillance; 2) education and awareness; and 3) guidelines and best practices. This work will be undertaken over the next five years, ending March 31, 2022.
1. Surveillance
- Integrate and disseminate innovative methods and best practices for human surveillance among an expanded group of partners
- Collect human surveillance data in Canada for people who do not meet the case definition for probable or confirmed Lyme disease
- Perform an analysis of the costs associated with Lyme disease
- Develop a national tick-borne surveillance system that includes Lyme disease and other possible co-infections
2. Education and awareness
- Support partners to develop early detection/early diagnosis education materials, with a focus on high risk groups, to assist front-line health professionals and public health authorities in the prevention and diagnosis of Lyme disease
- Develop a national tick and Lyme disease education and awareness campaign, in collaboration with partners, that addresses:
- Tick bite prevention and early intervention
- Recognition of Lyme disease symptoms, so that patients can seek help and front-line professionals can perform early diagnosis and treatment
3. Guidelines and best practices
- Establish a Lyme disease research network
- Work with international public health partners to share best practices and disseminate domestically
- Continue to support front-line health professionals and provincial laboratories in the laboratory diagnosis of Lyme disease
- Consult with provincial and territorial health care regulatory authorities on innovative, evidence-based approaches to address the needs of patients
Appendix 2 - Conference to Develop a Federal Framework on Lyme Disease, May 15-17, 2016
You can view the full version of the Conference Summary Report here.
References
- Footnote 1
-
http://laws-lois.justice.gc.ca/eng/acts/F-7.35/FullText.html
- Footnote 2
-
Biggs, H.M, et. al. Diagnosis and Management of Tickborne Rickettsial Diseases: Rocky Mountain Spotted Fever and Other Spotted Fever Group Rickettsioses, Ehrlichioses, and Anaplasmosis, US Centers for Disease Control and Prevention Morbidity and Mortality Weekly Report (MMWR) 2016: 65(2)1-44.
- Footnote 3
-
https://www.canada.ca/en/public-health/services/diseases/lyme-disease.html
- Footnote 4
-
Klasco, R. S., Glinert, L. Language for Actionable Recommendations (viewpoint) Journal of the American Medical Association (JAMA). 2017; 317(6), 583-4.
- Footnote 5
-
Statement for the House Foreign Affairs Committee Africa, Global Health and Human Rights Subcommittee's Hearing on Global Challenges in Diagnosing and Managing Lyme Disease - Closing Knowledge Gaps Submitted by the Infectious Diseases Society of America. 2012, July 17.
Page details
- Date modified: