Syphilis in Canada: Technical report on epidemiological trends, determinants and interventions

Download the alternative format
(PDF format, 5.9 MB, 181 pages)
Organization: Public Health Agency of Canada
Published: 2020-11-18
Table of Contents
- Foreword
- Table of figures
- Table of tables
- Abbreviations
- Executive summary
- 1. Syphilis: Natural history, diagnosis and treatment
- 2. Burden of syphilis and co-infections
- 3. Epidemiological trends of syphilis in Canada, 2009-2018
- 4. Determinants and risk factors of syphilis in Canada
- 5. Congenital syphilis: Trends, determinants and response
- 5.1 Congenital syphilis trends in Canada over the past 25 years
- 5.2 Epidemiological situation across Provinces and Territories
- 5.3 Factors associated with Canadian trends
- 5.4 Comparison of recent trends in Canada to those of other countries
- 5.5 Addressing Congenital Syphilis in Canada: Potential solutions
- 6. Interventions and policy for syphilis prevention and control
- 7. Conclusion
- References
- Appendix A: Clinical algorithm for syphilis staging and treatment
- Appendix B: Case definitions of syphilis used in Canada
- Appendix C: Data and methods
- Appendix D: Rates of infectious syphilis per 100,000 population by sex in countries of the Organization for Economic Co-operation and Development, 2008-2017
- Appendix E: Proportion of cases by syphilis stage overall and by sex in Canada, 1991-2017
- Appendix F: Rates of reported cases of infectious syphilis per 100,000 population by age group and sex in Canada, 2009-2018
- Appendix G: Rates of reported cases of infectious syphilis by province/territory and by sex in Canada, 2009-2018
- Appendix H: Number of cases and rates of congenital syphilis, rates of infectious syphilis among women aged 15 – 39 and rates of infectious syphilis among females, 1993-2018
Foreword
The Centre for Communicable Diseases and Infection Control at the Public Health Agency of Canada (PHAC) is pleased to present the report: Syphilis in Canada, Technical Report on Epidemiological Trends, Determinants and Interventions. The purpose of this report is to provide information to the public health sector, to clinicians and to policy makers about trends in syphilis cases and infection rates in Canada. This report was developed in response to the current rise of syphilis rates in Canada. It presents evidence on the current trends in rates of syphilis infection in Canada, associated risk factors, and some interventions that were implemented in response to the increase in cases of syphilis in Canada.
Syphilis is a notifiable disease in Canada. The report Syphilis in Canada, Technical Report on Epidemiological Trends, Determinants and Interventions is primarily based on surveillance data submitted to the Canadian Notifiable Disease Surveillance System (CNDSS) by provincial and territorial health authorities and also presents data published in provincial and territorial surveillance reports as well as information from the scientific literature and from the grey literature including media releases and international reports.
We welcome all comments and suggestions for improving future publications. We invite you to contact the staff of the Centre for Communicable Diseases and Infection Control, Public Health Agency of Canada, at phac.sti-hep-its.aspc@canada.ca.
Table of figures
- Figure 1. Summary of the natural history of untreated syphilis and its associated clinical manifestations
- Figure 2. Percentage change in rates of reported cases of STBBI in Canada, relative to the reference year of 2008, 2008-2017
- Figure 3. Factors contributing to the HIV-syphilis syndemic
- Figure 4. Total, infectious stages and non-infectious stages rates of reported cases of syphilis in Canada, 1979-2017
- Figure 5. Comparison of rates of reported cases of infectious syphilis in OECD countries, 2008-2017
- Figure 6. Proportion of reported cases of syphilis by stage of infection in Canada, 1991-2017
- Figure 7. Proportion of reported cases of syphilis by stage of infection among males in Canada, 1991-2017
- Figure 8. Proportion of reported cases of syphilis by stage of infection among females in Canada, 1991-2017
- Figure 9. Rates of reported cases of infectious syphilis by sex in Canada, 1991-2018
- Figure 10. Comparison of reported male-to-female rate ratios of infectious syphilis in OECD countries, 2008-2017
- Figure 11. Rates of reported cases of infectious syphilis by sex in OECD countries, 2017
- Figure 12. Rates of reported cases of infectious syphilis by age group in Canada, 1991-2018
- Figure 13. Rates of reported cases of infectious syphilis by age group among males in Canada, 2009-2018
- Figure 14. Rates of reported cases of infectious syphilis by age group among females in Canada, 2009-2018
- Figure 15. Proportion of reported cases of infectious syphilis by age group and sex in Canada, 2018
- Figure 16. Rates of reported cases of infectious syphilis by province and territory in Canada, 2017
- Figure 17. Reported rates of infectious syphilis by province and territory in Canada, 2018 (preliminary data)
- Figure 18. Change in rates of reported cases of infectious syphilis from 2014 to 2018 by province and territory in Canada
- Figure 19. Percentage change in rate of reported cases of infectious syphilis between 2014 and 2018 in males by province and territory in Canada
- Figure 20. Percentage change of rate of reported cases of infectious syphilis between 2014 and 2018 in females by province and territory in Canada
- Figure 21. Proportion of reported cases of females and percentage change by province and territory from 2014 to 2018 in Canada
- Figure 22. Rates of reported cases of infectious syphilis cases in British Columbia, Canada, 1979-2018
- Figure 23. Rates of reported cases of infectious syphilis by sex in British Columbia, Canada, 2009-2018
- Figure 24. Rates of reported cases of infectious syphilis in Alberta, Saskatchewan and Manitoba, Canada, 1979-2018
- Figure 25. Rates of reported cases of infectious syphilis by sex in Alberta, Saskatchewan and Manitoba, Canada, 2009-2018
- Figure 26. Rates of reported cases of infectious syphilis in Ontario and Quebec, Canada, 1979-2018
- Figure 27. Rates of reported cases of infectious syphilis by sex in Ontario and Quebec, Canada, 2009-2018
- Figure 28. Rates of reported cases of infectious syphilis in New Brunswick, Newfoundland and Labrador, Nova Scotia and Prince Edward Island, Canada, 1979-2018
- Figure 29. Overall rates of reported cases of infectious syphilis by sex in New Brunswick, Newfoundland and Labrador, Nova Scotia, and Prince Edward Island, Canada, 2009-2018
- Figure 30. Rates of reported cases of infectious syphilis in Yukon, Northwest Territories and Nunavut, Canada, 1979-2018
- Figure 31. Rates of reported cases of infectious syphilis by sex in Yukon, Northwest Territories and Nunavut, Canada, 2009-2018
- Figure 32. Conceptual framework of syphilis infection in Canada
- Figure 33. Number and rates of reported cases of congenital syphilis and rates of reported cases of infectious syphilis among females of reproductive age (15 to 39 years of age), Canada, 1993-2018
- Figure 34. Most commonly reported risk factors associated with maternal syphilis and related congenital syphilis in the Canadian literature
Table of tables
- Table 1. Provincial and territorial comparison with the national case definition for congenital syphilis
- Table 2. Provincial comparison with the national case definition of neurosyphilis and primary, secondary, early latent, late latent and tertiary syphilis
- Table 3. Comparison of syphilis reporting practices across provinces and territories over time in Canada
Abbreviations
- AB
- Alberta
- aOR
- Adjusted odds ratio
- aIRR
- Adjusted incidence rate ratio
- ART
- Antiretroviral therapy
- BC
- British Columbia
- BCCDC
- British Columbia Centre for Disease Control
- CDC
- Centers for Disease Control and Prevention
- CGSTI
- Canadian Guidelines for Sexually Transmitted Infections
- CI
- Confidence interval
- CIA
- Chemiluminescence immunoassays
- CNDSS
- Canadian Notifiable Disease Surveillance System
- CSF
- Cerebrospinal fluid
- CPHA
- Canadian Public Health Association
- DBS
- Dried blood spot [testing]
- DFA-TP
- Direct fluorescent antibody test for T. pallidum
- DNA
- Deoxyribonucleic acid
- ECDC
- European Centre for Disease Prevention and Control
- EIA
- Enzyme immunoassay (Treponemal screening test)
- EMIS
- The European Men-Who-Have-Sex-With-Men Internet Survey
- EU
- European Union
- FTA-ABS
- Fluorescent treponemal antibody absorbed test (treponemal screening test)
- gbMSM
- Gay, bisexual and other men who have sex with men
- GHB
- Gamma-hydroxybutyrate
- HAV
- Hepatitis A virus
- HBV
- Hepatitis B virus
- HCV
- Hepatitis C virus
- HIV
- Human immunodeficiency virus
- HPV
- Human papilloma virus
- IHC
- Immunohistochemistry
- IM
- Intramuscular
- LA
- Long acting
- LIA
- Line immunoassay
- MB
- Manitoba
- MBIA
- Microbead immunoassay
- MLST
- Multilocus sequence typing
- NAT
- Nucleic acid test
- NAAT
- Nucleic acid amplification testing
- NB
- New Brunswick
- NCCID
- National Collaborating Centre for Infectious Diseases
- NL
- Newfoundland and Labrador
- NS
- Nova Scotia
- NT
- Northwest Territories
- NU
- Nunavut
- OECD
- Organization for Economic Co-operation and Development
- ON
- Ontario
- OR
- Odds ratio
- PCR
- Polymerase chain reaction
- PE
- Prince Edward Island
- PEP
- Post-exposure prophylaxis
- PHAC
- Public Health Agency of Canada
- POC
- Point-of-care [testing]
- Pap
- Papanicolaou [test]
- PT
- Provinces/Territories
- PrEP
- Pre-exposure prophylaxis
- QC
- Quebec
- RNA
- Ribonucleic acid
- RPR
- Rapid plasma reagin test (non-treponemal screening test)
- rRNA
- Ribosomal ribonucleic acid
- RSSS
- Reverse sequence screening for syphilis
- SIECCAN
- Sex Information and Education Council of Canada
- SMS
- Short message service [text messaging]
- SOICC
- Syphilis Outbreak Investigation Coordination Committee
- ST
- Sequence type
- STBBI
- Sexually transmitted blood-borne infections
- STI
- Sexually transmitted infection
- SK
- Saskatchewan
- TP-PA
- T. pallidum particle agglutination test (treponemal screening test)
- UK
- United Kingdom
- US
- United States [of America]
- VDRL
- Venereal disease research laboratory test (non-treponemal screening test)
- YT
- Yukon
- WHO
- World Health Organization
Executive summary
This report provides information on syphilis to public health professionals, clinicians and decision-makers.
The report is organized around six thematic areas:
- Syphilis: natural history, testing and treatment
- Burden of syphilis and co-infections
- Epidemiological trends of syphilis in Canada, 2009-2018
- Determinants and risk factors of syphilis in Canada
- Congenital syphilis: trends, determinants and response
- Interventions and policy for syphilis prevention and control
The first two thematic areas are addressed by summarizing existing guidance from the Canadian Guidelines for Sexually Transmitted Infections (CGSTI) and clinical and laboratory literature. In order to describe syphilis trends in Canada, the third section uses surveillance data from the Canadian Notifiable Disease Surveillance System (CNDSS) from 1971 to 2017, along with preliminary 2018 data provided directly to PHAC by the provinces and territories. Wherever possible, Canadian trends are compared to international trends. The report also describes recent syphilis outbreaks across Canada, as well as the factors that have been associated with syphilis infection in studies conducted in Canada (Section 4). Lastly, interventions and policies proposed to support the control of syphilis in Canada are discussed in Section 5 and Section 6.
1. Syphilis: natural history, testing and treatment
Syphilis is an infection caused by the bacteria Treponema pallidum. Syphilis is primarily transmitted sexually, although blood-borne transmission is possible. If left untreated, the infection can progress through four stages: primary, secondary, latent and tertiary. Individuals can transmit the infection during the early stages of infection (primary, secondary and early latent syphilis). Chancres and unspecific symptoms, such as fever, malaise or headaches, are among the most common symptoms in the early stages. Tertiary syphilis can cause severe neurological, cardiologic and musculoskeletal manifestations. The infection can also be transmitted from a mother to her fetus/child during pregnancy or at delivery, causing congenital syphilis. Congenital syphilis can lead to stillbirth, birth defects or infant death.
Guidelines for screening vary across the provinces and territories. The CGSTI recommends screening for any individual presenting with signs and symptoms or with risk factors, such as having engaged in condomless sex. Syphilis is usually diagnosed using serological tests on blood samples. Microscopic examination or Polymerase Chain Reaction (PCR) can also be used to detect T. pallidum or its deoxyribonucleic acid (DNA). Syphilis is usually treated with penicillin. Resistance of T. pallidum to penicillin has not been reported.
2. Burden of syphilis and co-infections
National rates of chlamydia, gonorrhea and syphilis have been increasing, with syphilis having the highest relative rate increase of all three over 2009 to 2018. Some populations, such as gay, bisexual and other men who have sex with men (gbMSM), have been more affected in the past few decades. However, over the past five years, infection rates have substantially increased in other populations including females of reproductive age. As a result, the highest number of congenital syphilis cases observed in the last 25 years in Canada (17 cases) were reported in 2018. Though syphilis is not associated with high levels of mortality in Canada, it is associated with reduced functioning, a lowered quality of life as well as psychosocial repercussions. Specific populations are affected by overlapping epidemics, such as syphilis and Human Immunodeficiency Virus (HIV) infection, which exacerbate the burden of these infections for affected individuals and communities. Syphilis interacts with HIV to amplify the impacts of both infections, as one may lead to the acquisition of the other and intensify its progression.
3. Epidemiological trends of syphilis in Canada, 2009-2018
Following a sustained decline in the 1990s, syphilis rates began to increase in Canada once again in the early 2000s. In the past few years, rates in Canada have reached their highest point in decades. Similar trends can be found in other high-income countries, such as Australia, the European Union (EU), New Zealand, the United States (US), and the United Kingdom (UK).
In the 1990s, rates among males and females were similar, but beginning in the 2000s, rates among males began to increase rapidly. In 2012, syphilis rates among males were 18 times higher than among females. However, in 2018, preliminary data indicate a reduction in the male-to-female ratio of new syphilis infections from 8:1 in 2017 to 4:1in 2018. In 2017, the highest rates were observed in the 25 to 29 year old age group and the 30 to 39 year old age groups. Female cases tend to be younger than male cases, as the proportion of male cases increases with age.
Between 2014 and 2018, most provinces and territories reported increases in their infectious syphilis rates. Outbreaks of syphilis have recently been reported in nine provinces and territories. The provinces and territories with the highest increases in rates over this time were Alberta (831%), Northwest Territories (550%), Manitoba (538%), and Saskatchewan (393%). Currently, the jurisdiction with the highest infectious syphilis rate is Nunavut with 261.1 cases per 100,000 population in 2018.
4. Determinants and risk factors of syphilis in Canada
Various social determinants of health and health behaviours shape the risk of acquiring syphilis. These include a broad range of underlying factors, such as age, sex and gender, socioeconomic factors, culture, norms, and health policies and programs, which influence individual-level risk factors, such as sexual activity, substance use, experiences of violence and discrimination and access to health care and services. There is a synergistic interaction at play between the concurrent epidemics of syphilis, other sexually transmitted and blood-borne infections (STBBI) and substance use, given their common risk factors and aggravating social forces.
5. Congenital syphilis: trends, determinants and response
As rates of syphilis increase among women of reproductive age, the number of early congenital syphilis (i.e., within two years of birth) cases is also rising in Canada. From 1993 (when congenital syphilis became notifiable) to 2017, between one and ten cases of congenital syphilis cases were reported each year in Canada. In 2018, 17 cases were reported, and over 50 cases are expected for 2019. The situation is particularly worrisome in the Prairies, which have reported the bulk of congenital syphilis cases in 2018 and 2019. Moreover, several provinces and territories have recently reported their first congenital syphilis case in years.
While there have been few studies examining the risk factors for congenital syphilis, findings from those that exist have reported inadequate prenatal care as one of the main reasons for the occurrence of congenital syphilis. Pregnant women with syphilis who are not screened and treated in a timely manner are at high risk of transmitting the infection to their baby.
6. Interventions and policy for syphilis prevention and control
The Pan-Canadian STBBI Framework for Action identifies four pillars of action for addressing STBBI, including syphilis: prevention, testing, initiation of care and treatment, and ongoing care and support. The following section reviews the published literature on interventions and policy for syphilis prevention and control originating from Canada and abroad. Strategies to address syphilis are described according to the four pillars for action, starting with improving primary syphilis prevention to addressing underlying social determinants of health. This section also summarizes educational and clinical strategies to increase screening accessibility and uptake as well as approaches to ensure effective case management, and adapt surveillance practices to current epidemiologic case profiles. Areas for future research concerning the syphilis cascade of care, genomic analysis, and program evaluation are noted.
A note on language around sex and gender identity
Throughout the report, considerations of sex and gender are limited by data sources available. Syphilis trends and risk factors are presented according to sex (male, female), as these data are collected in most of the surveillance systems operating within Canada as well as most observational studies. Given that the multi-level determinants of syphilis infection can vary according to gender identity and experiences, discussion of influences of gender identity on how individuals perceive themselves or others, how they act, and how inequities are distributed across society have been included wherever possible throughout this report.
1. Syphilis: natural history, diagnosis and treatment
1.1 The origins of syphilis and means of transmission
Syphilis is a complex systemic illness caused by a bacterial infection. Specifically, it is caused by the spirochete bacterium Treponema pallidum, subspecies pallidum.
The origins of syphilis are unclear. Several hypotheses have been suggested, from a possible emergence in South-Western Asia around 3000 BC, to navigators from the Columbus fleet having brought back the disease from the New World - where it had existed in the pre-Columbian period - to the Old World in 1493Footnote 1.
Syphilis is transmitted primarily via genital, anal, or oral sexual contactFootnote 2. Other routes of transmission, such as through kissing with exchange of saliva, blood transfusion and sharing of needles, are possible, but rareFootnote 3. Congenital syphilis occurs mainly via vertical transmission during pregnancy, although transmission from mother to child can also happen due to contact with an active lesion at the time of deliveryFootnote 1. Transplacental transmission can occur as early as nine weeks of gestation and the remainder of the pregnancyFootnote 4. Syphilis in pregnancy can cause miscarriage, stillbirth or neonatal death. In 2012, syphilis resulted in 350,000 adverse pregnancy outcomes globally, including 143,000 early fetal deaths and stillbirths and 62,000 neonatal deathsFootnote 5.
In Canada, syphilis has been a notifiable disease since 1924, and congenital syphilis has been notifiable since 1993Footnote 6. However, reporting has been heterogeneous across provinces and territories (PTs) over time. Furthermore, for congenital syphilis cases, only cases diagnosed in infants less than two years of age are currently reportable nationally.
1.2 Infectious syphilis staging and clinical manifestations
If left untreated, syphilis infection can progress through four stages: primary, secondary, latent (early and late) and tertiary (stage progression described in Figure 1 ). However, reinfections are possible following treatment.
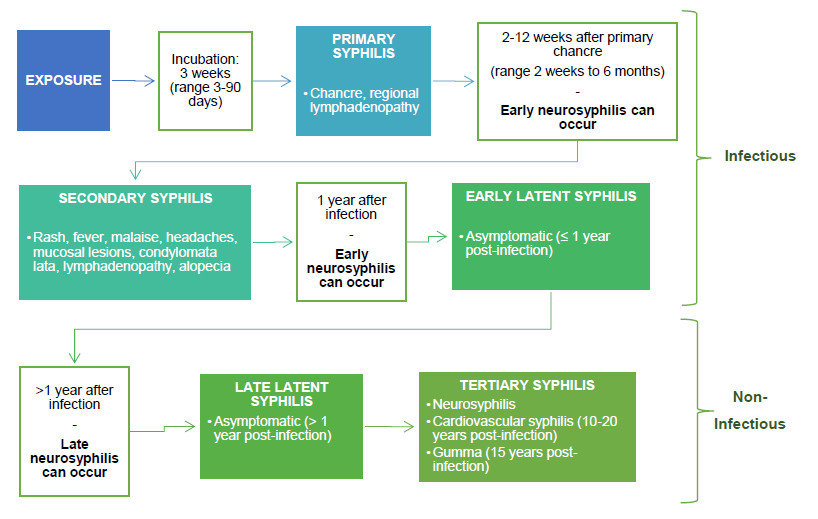
Figure 1 - Text description
Infectious stages:
Exposure → Incubation: 3 weeks (range 3-90 days) → Primary syphilis: chancre, regional lymphadenopathy → Secondary incubation: 2-12 weeks after primary chancre (range 2 weeks to 6 months) - Early neurosyphilis can occur → Secondary syphilis: rash, fever, malaise, headaches, mucosal lesions, condyomata lata, lymphadenopathy, alopecia → 1 year after infection - Early neurosyphilis can occur → Early Latent syphilis: asymptomatic (≤1 year post-infection) → Pathway linked to non-infectious syphilis
Non-infectious stages:
>1 year incubation - Late neurosyphilis can occur → Late latent syphilis: asymptomatic (>1 year-post infection) → Tertiary syphilis: neurosyphilis, cardiovascular syphilis (10-20 years post-infection), gumma (15 years post-infection)
1.2.1 Primary syphilis
Primary stage syphilis usually occurs after an incubation period of three weeks, on average. However, the incubation period can last between 3 and 90 days. At this stage, a lesion (chancre) may occur as well as regional lymphadenopathy. The chancre may not be readily apparent, as it may be internal (e.g., intra-anal, oral or on the internal genital tract in females), and therefore can frequently go unnoticed. This stage of syphilis is considered infectious with an estimated risk of transmission of approximately 60% per sexual partnerFootnote 2.
1.2.2 Secondary syphilis
After a secondary incubation period of two to 12 weeks (which can last up to six months), infectious syphilis may progress to the secondary stage. Symptoms at this stage can include rashes, fever, malaise, headaches, mucosal lesions, condylomata lata (wart-like lesions), lymphadenopathy, and patchy or diffuse alopecia, signs and symptoms of meningitis, uveitis/retinitis (e.g. blurred vision, eye redness, flashes or floaters) or otic symptoms (e.g., hearing loss, tinnitus). This secondary stage is also considered infectious, with an estimated risk of approximately 60% per sexual partnerFootnote 2.
1.2.3 Latent syphilis (early, late)
Without treatment, secondary syphilis can progress to the latent stage, during which no symptoms are present. Latent syphilis infections that occur within the first year following infection are considered “early” latent syphilisFootnote 3. This stage is considered infectious because one in four cases can relapse to secondary stage manifestationsFootnote 7. An asymptomatic infection that persists over a year after the infection acquisition is considered “late” latent syphilis.
1.2.4 Neurosyphilis
At any stage of infection, Treponema pallidum can invade the central nervous system causing neurosyphilis. Neurosyphilis may be asymptomatic or may present with symptoms. Early neurosyphilis occurs within the first year of infection, and approximately 5% of cases experience symptoms, such as meningitis, cranial neuritis, ocular involvement and meningovascular diseaseFootnote 8. Neurosyphilis is considered late if its onset is more than one year after infection. At this stage, 2-5% experience general paresis and 2-9% experience tabes dorsalis (loss of coordination of movement)Footnote 8. Other signs and symptoms of neurosyphilis include ataxia, vertigo, dementia, headaches, personality changes, Argyll Robertson pupil, otic symptoms (e.g. tinnitus, hearing loss) and ocular symptoms (e.g. blurred vision, bright flashes, floating spots).
1.2.5 Tertiary syphilis
Though rare, latent infections can progress to tertiary syphilis. Tertiary infections are not infectious. At this stage, the infection can affect several organs, including the brain, nerves, eyes, heart, blood vessels, liver, bones, and joints. Tertiary syphilis can manifest as neurosyphilis (described above). It can also manifest as to cardiovascular syphilis, which occurs ten to 30 years following initial exposure and can lead to development of aortic aneurysms or regurgitation, or coronary artery ostial stenosis. Although most cases will develop within 15 years, syphilis can manifest between one and 46 years following initial exposure, and can lead to gummatous lesions (gumma) on any organ, with clinical manifestations varying based on the site involvedFootnote 3.
1.2.6 Congenital syphilis
The risk of vertical transmission varies depending on the stage of maternal syphilis, with the risk being over 50% if the pregnant woman has untreated primary or secondary syphilisFootnote 9Footnote 10. Congenital syphilis can lead to stillbirth. Early congenital syphilis occurs within the first two years of life. Manifestations can include fulminant disseminated infection, rhinitis (snuffles), mucocutaneous lesions, hepatosplenomegaly, anemia, osteochondritis and neurosyphilis. Symptom onset after two years is defined as late congenital syphilis. Symptoms include interstitial keratitis, lymphadenopathy, hepatosplenomegaly, anemia, bone involvement, dental abnormalities such as Hutchinson’s teeth, and neurosyphilis.
1.2.7 Syphilis staging
Syphilis staging can be challenging, as infection stage cannot be determined by laboratory testing alone. Patient history and clinical presentation of disease are essential to determine syphilis stage and allow proper treatment. For primary and secondary stages, positive serology and clinical manifestation are needed to stage cases, as these stages can only be distinguished by signs and symptoms. In the case of asymptomatic patients with positive serology, patient history is necessary to determine staging; those who previously tested negative in the last 12 months are most likely to be in the early latent stage of syphilis, while those without negative serology in the previous 12 months may be in the late latent stage. Neurosyphilis can manifest in early (infectious neurosyphilis) or late stages (non-infectious neurosyphilis) of syphilis infection. Similar to what was discussed above, patient history is pivotal, as only previous serology testing and the history of physical symptoms can distinguish infectious from non-infectious neurosyphilis cases. This distinction is important, as early stages and late stages will require different courses of treatment. Appendix A presents an algorithm of syphilis staging according to the CGSTI.
1.3 Syphilis screening
1.3.1 Target population for screening
The Public Health Agency of Canada (PHAC) guidelines recommend that any individual presenting signs or symptoms compatible with syphilis and individuals presenting with risk factors for syphilis should be screenedFootnote 3. These risk factors include:
- Having sexual contact with someone who has received a syphilis diagnosis
- Being a man who has sex with men
- Being engaged in transactional sex
- Having experienced homelessness or street involvement
- Having used injection drugs
- Reporting multiple sexual partners
- Personal history of syphilis, HIV infection or other sexually transmitted infections (STIs)
- Being born to a mother diagnosed with infectious syphilis in pregnancy
- Having lived in a country or region with a high prevalence of syphilis
- Having a sexual partner with any of the above risk factors
Guidelines for screening vary across provinces and territories. Local, provincial and territorial recommendations should be followed.
1.3.2 Screening in pregnancy
Given the rising rates of syphilis and congenital syphilis in Canada, universal screening of all pregnant women continues to be important and is the standard of care in all jurisdictions. Universal screening of pregnant women is recommended during the first trimester or at first prenatal visitFootnote 11. Repeat screening at 28-32 weeks (third trimester) and at delivery is recommended in areas with outbreaks and for women at high risk of acquiring syphilis. More frequent screening should be considered for women at high risk. It is also recommended that pregnant women with no history of prenatal care or testing be tested at delivery. Lastly, any person delivering a stillborn infant after 20 weeks gestation should be screened for syphilis.
1.3.3 Screening in immigrants to Canada
Currently, syphilis testing is mandatory for all individuals aged 15 years and older who undergo an immigration medical examFootnote 12. This medical exam is mandatory for all foreign nationals applying for permanent residency and for temporary resident applicants who intend to work in an occupation in which the protection of public health is essential (workers in the health sector field, for example)Footnote 13. Cases that are positive must document appropriate treatment according to Canadian protocol by providing a completed Syphilis Treatment Form with the immigration medical exam contentFootnote 14.
1.4 Laboratory Diagnosis of Syphilis
Pathogenic treponemal bacteria include Treponema pallidum subspecies pallidum (subsequently referred to as T. pallidum) that causes venereal syphilis, T. pallidum subspecies endemicum that causes bejel or endemic syphilis, T. pallidum subspecies pertenue that causes yaws, and T. carateum that causes pinta. Since the commonly used serological tests for the diagnosis of syphilis cannot differentiate between infection caused by T. pallidum and infections due to other pathogenic non-venereal treponemal agents, the differential diagnosis of skin lesions suspected of syphilis or other treponemal infection should therefore, include a careful clinical examination and consideration of the patient’s background history including any travel to endemic areas for non-venereal treponematosis.
Syphilis can be diagnosed using serological tests (treponemal or non-treponemal), microscopic examination or nucleic acid amplification tests (NAAT). Point-of-care testing is increasingly of interest for underserved populations, but is not yet licensed by Health Canada for use in Canada.
1.4.1 Serological diagnosis
Initial screening for syphilis can be conducted using a non-treponemal test or a treponemal test, both of which are applied on a serum sample. Once reactive, the treponemal test will most often remain so throughout the person’s life, even in the presence of treatmentFootnote 2. However, 15-25% will serorevert (non-reactive test result) if the individual is successfully treated while their infection is at the primary stageFootnote 2.
Non-treponemal antibody test
Non-treponemal tests approved by Health Canada include the Rapid Plasma Reagin (RPR) and the Venereal Disease Research Laboratory (VDRL) tests. These tests detect non-specific antibodies to a complex mixture of cardiolipin, lecithin, and cholesterol. Both tests are flocculation tests (clumping of antigen mixture by positive test sample) and therefore, are subjective tests that require experience on the part of the test operator. Positive non-treponemal tests are indicative of active infection at the primary, secondary, or latent stages of infection; and when done quantitatively, they can be used to follow successful treatment of infection by observing a drop in the antibody titreFootnote 3.
RPR is slightly more sensitive (86%) than VDRL (78%) for the detection of primary syphilis but both tests are 100% sensitive in secondary syphilisFootnote 15. RPR can only be used on serum samples, while VDRL can be used to detect antibodies in serum and cerebrospinal fluid (CSF) and is the only approved non-treponemal serological test to be used on CSF for the diagnosis of neurosyphilisFootnote 16. Interpretation of non-treponemal test results may be complicated by the prozone phenomenon, which occurs with very high titre samples that give negative results unless the test samples are diluted. Biological false positives, which may occur due to factors unrelated to treponemal infections, such as older age, some viral, bacterial, and parasitic infections, and some autoimmune diseases and pregnancy, may also interfere with the interpretation of non-treponemal test results.
Treponemal antibody test
Unlike non-treponemal tests, these tests use treponemal antigens to detect anti-treponemal antibodies. Since a positive treponemal antibody test result may remain positive for a very long time, treponemal antibody tests cannot be used to differentiate active infections from previous infections that have been treated in the past, nor can they be used to monitor and confirm success of treatment. There are many Health Canada approved serological tests that detect treponemal antibodies and these include amongst others, the fluorescent treponemal antibody absorption (FTA-ABS) test, Treponema pallidum particle agglutination (TP-PA) assay, various traditional enzyme immunoassays (EIAs), newer EIAs such as the chemiluminescence immunoassay (CIA) or the microbead immunoassay (MBIA), and the line immunoassay (LIA).
When the sensitivity and specificity of some of these treponemal antibody tests were compared, FTA-ABS has the lowest sensitivity in detecting both primary (78.2%) and secondary syphilis (92.8%) compared to other immunoassays (TP-PA, Trep-Sure, Inno-LIA, CIA and MBIA) that were found to be 100% sensitive in detecting secondary syphilis, while their sensitivities for primary syphilis were between 94.5% to 86.4%. The overall specificity was lowest for Trep-Sure (82.6%) and highest for TP-PA (100%), with FTA-ABS achieving a specificity of 98.0%Footnote 17. False positive treponemal tests have been reported in patients with gingivitis and periodontitis due to cross-reactive antigens present on oral spirochete organismsFootnote 18.
Algorithm of syphilis serology
Two types of serologic screening algorithms are currently used in Canada: traditional and reverse algorithmsFootnote 19. Traditionally, the serological detection of syphilis infection starts by screening with a non-treponemal antibody test. When positive, it is confirmed using a treponemal antibody test. For high risk individuals, both non-treponemal and treponemal antibody tests are done at the same time to detect possible latent infection when the non-treponemal antibody test may be negativeFootnote 20.
The reverse sequence syphilis screening (RSSS) algorithm approach uses a treponemal test to screen and a quantitative non-treponemal test to confirm the positives. With increasing sample volumes for syphilis screening and the availability of automatic high-throughput platforms (such as CIA and MBIA) for performing treponemal antibody tests, many laboratories have opted for the reverse approach screening of syphilis, using high throughput treponemal antibody tests and confirming any positive findings with a non-treponemal antibody test. Presently, most provinces and territories favour the reverse algorithmFootnote 3. In general, since the interpretation of serology results can be complex, and different algorithms may be employed across provinces and territories, consultation with public health laboratories regarding testing protocols is recommended.
When screening is done with the more sensitive treponemal test, discordant positive treponemal test results that cannot be confirmed by a non-treponemal test becomes a diagnostic and clinical issueFootnote 21. For example, in a study involving over three million test samples in a major Canadian city, it was found that 2.2% of the samples screened positive for syphilis when CIA was used vs. only 0.6% positive when screening was done by RPRFootnote 22. However, of the 2.2% that screened positive by CIA, 1.4% were RPR negative and only 0.6% of the samples having screened positive by CIA but negative by RPR were cases of early primary syphilis. These cases showed seroconversion to RPR positive, in a follow-up test sample. Therefore, under the RSSS algorithm, those who screened positive by EIA but who were RPR-negative may represent either early primary syphilis, treated past syphilis infection, latent syphilis of unknown duration, or false positive reaction. Consistent with this, in another study that examined the impact of the RSSS algorithm, an increase in the diagnosis of late latent syphilis was notedFootnote 23.
1.4.2 Other methods of detection
Microscopic examination
The method of choice to detect T. pallidum may depend on the type of specimen taken for examination. Tissue specimens taken for histological examination can be used to examine the presence of T. pallidum using either silver staining or an immunohistochemistry (IHC) reaction. The former test relies on a morphological recognition of spirochetes in tissue samples made visible by the silver nitrate deposit or impregnation around the bacteriaFootnote 24. The IHC method has enhanced sensitivity and specificity from the use of antibodies, such as monoclonal antibodies to T. pallidum and an enzyme reaction such as peroxidase reacting with an insoluble substrate to allow the antigen-antibody reaction to be visible under light microscopyFootnote 25. However, both methods are prone to potential false positives due to staining artifacts and the presence of cross-reacting bacteriaFootnote 26.
Direct observation of T. pallidum in fresh specimens, such as serous fluids from genital, skin or mucous membrane lesions of primary and secondary syphilis cases, can be carried out by dark-field microscopy. This method requires a trained microscopist to recognize the live motile spirochetes. As a result, the test has to be performed at, or near, the location of specimen collection. It is not suitable for oral and anal lesion specimens due to the presence of other spirochete organisms whose morphology is indistinguishable from T pallidum. The use of microscopic examination is now limited in Canada, with only one provincial public health laboratory still using microscopy as a mean for laboratory diagnosis of primary syphilis, due to the difficulties in maintaining the technical expertise and methodological limitations of the technique.
Another method for detection of T. pallidum is the direct fluorescent antibody test for T. pallidum (DFA-TP). This method is now almost obsolete due to lack of a reliable source of direct fluorescent anti-T. pallidum antibody.
Nucleic acid amplification test
Detection of T. pallidum nucleic acid by polymerase chain reaction (PCR) is a sensitive test capable of detecting ten to 100 copies of the target geneFootnote 27. PCR testing to detect DNA or ribonucleic acid (RNA) targets have been describedFootnote 28Footnote 29. However, there is currently no Health Canada-licensed PCR test commercially available for use in Canada. As a result, many laboratories have developed their own in-house test or adopted methods described in academic journals. In the last two decades, the use of PCR for the diagnosis of syphilis has provided some information about its optimal use. PCR is most useful for the diagnosis of primary syphilis before seroconversion occursFootnote 30Footnote 31. This method performs best in specimens taken from moist lesions in both primary and secondary syphilis. Its performance in blood specimens is only about 50%, except in neonates with congenital syphilisFootnote 32. Positive PCR results have been reported with urine and semen specimens as well as in the oral cavity of secondary syphilis cases involving men who have sex with men, even without oral lesionsFootnote 33-35. Another use of PCR is in testing the involvement of T. pallidum in unusual pathology, such as lung abscess, tonsillitis or a non-healing oral ulcer that extends to the lower lipFootnote 36-38.
1.4.3 Typing of T. Pallidum
Although various methods have been in use in the past, it appears likely that the recently proposed multi-locus sequencing typing (MLST) will become the widely adopted method of choice for the typing of T. pallidumFootnote 39. Since MLST has been used widely in the tracking of other bacterial pathogens like meningococci, pneumococci, methicillin-resistant Staphylococcus aureus and many others, clinicians and public health officials are familiar with the method and the terminology used.
As of September 2018, 40 Sequence Types (STs) of T. pallidum have been documented, and they have been reported from Europe, North America, South America, and Asia. These STs can be grouped into two clonal complexes: the SSl4-like clonal complex and the Nichols-like clonal complex. Although not part of the MLST scheme, PCR amplification and sequencing of the 23S ribosomal RNA (rRNA) gene that encodes for macrolide resistance or susceptibility can identify resistant strains as well as the type of resistance. Mutations at positions 2058 or 2059, corresponding to the 23S rRNA gene of Escherichia coli (accession number V00331), results in an A to G substitution, which has been shown to cause macrolide resistanceFootnote 40Footnote 41. The A2058G mutation causes azithromycin resistance, but not resistance to spiramycin, while the A2059G causes resistance to both antibiotics.
1.4.4 Point-of-care test for syphilis
Diagnostic testing conducted at or near the site of patient care, called point-of-care (POC) testing, can provide results to a clinician without time spent waiting for sample transport and laboratory processingFootnote 42. While the World Health Organization (WHO) studies POC tests for syphilis and other STIs as a means for control in developing countries and in resource-limited settings, their use and need in high-income countries like Canada are less definedFootnote 43Footnote 44. Nevertheless, there is much interest in the role of POC tests for STIs (including syphilis) in STI clinics, remote regions, and underserved populations, particularly during outbreak situations. Currently there are no licensed POC test kits for the diagnosis of syphilis in Canada, although access to these tests might be possible through the Special Access Programme for Medical DevicesFootnote 45. Field evaluations are currently underway to examine the diagnostic utilities of such POC tests across different settings, venues and populations who may benefit from such methods.
1.5 Syphilis Treatment
Syphilis is usually treated with penicillin, a treatment method that was established in 1943Footnote 46. A single dose (2.4 million units delivered through intra-muscular (IM) injection) of benzathine penicillin G-Long acting (LA) can render T. pallidum non-infectious within 24 hours for early syphilis infectionFootnote 47. Infection of longer duration requires repeated dosing. There are limited data supporting the efficacy of alternate antibiotics, such as doxycycline or ceftriaxone, for patients with penicillin allergies. These treatments may take longer to render a person non-infectious, so close patient follow-up is required. A more complete summary of treatment guidelines is available.Footnote 3
Syphilis is usually treated with penicillin. Resistance of T. pallidum to penicillin has not been reported.
Resistance of T. pallidum to penicillin (the drug of choice) has not been reported, however resistance to macrolide antibiotics — including azithromycin — has been reported in many parts of the world including CanadaFootnote 48. Unless the T. pallidum strain has been tested and found to be sensitive, azithromycin is not recommended for the treatment of syphilis.
1.5.1 Treatment for people living with HIV
Though the literature on syphilis treatment for people living with HIV is limited, existing studies suggest that this population should receive the same penicillin treatment as people who are HIV-negative (single dose benzathine penicillin G-LA for treatment of early syphilis infection). It should be noted, however, that some experts suggest a higher dosage (three weekly doses of 7.2 million units IM) for people living with HIVFootnote 3.
1.5.2 Treatment during pregnancy
For early syphilis cases in pregnant women, a single penicillin dose is reported to be effectiveFootnote 49. However, given the difficulty in staging cases among pregnant women and the association between pregnancy and both lower plasma penicillin levels and modified pharmacokinetics of penicillin, some experts recommend infectious cases be treated with two doses of benzathine penicillin G-LA 2.4 million units one week apart, particularly in the third trimesterFootnote 50. In general, treatment during pregnancy should be managed in collaboration with an obstetrician or maternal fetal medicine specialist.
1.5.3 Treatment of newborns (congenital syphilis)
No newborn should be discharged from hospital without confirmation that either the mother or newborn infant has undergone syphilis serology testing during pregnancy or at the time of labour and delivery and that the results will be followed up according to local protocolFootnote 11. Treatment is recommended for all neonates and children who are symptomatic. Furthermore, all infants for whom adequate follow-up cannot be ensured including those for whom the non-treponemal test yielded a titre that was at least four-fold higher than that of the birthing parent, and those for whom the treatment of the birthing parent was inadequate, unknown, did not contain penicillin, or occurred in the last month of pregnancy, should also be treatedFootnote 10. Preferred penicillin treatments vary based on the age of the child (<1 month versus ≥ 1 month of age) and presence of symptomsFootnote 10.
- Syphilis is a notifiable disease caused by a bacterium, Treponema pallidum, and is transmitted primarily through genital, anal or oral sexual contact.
- Congenital syphilis occurs via vertical transmission mainly during pregnancy and can cause miscarriage, stillbirth or infant death shortly after birth.
- If left untreated, a primary syphilis infection can progress through secondary, latent and tertiary disease stages. Out of the four stages of syphilis, three are infectious: primary, secondary and early latent syphilis.
- PHAC’s guidelines recommend that, any individual presenting signs or symptoms compatible with syphilis and any individual presenting with risk factors for syphilis be tested.
- Universal screening is recommended for pregnant women in the first trimester or at least once during pregnancy. Moreover, consideration should be given to repeat screening at 28-32 weeks of gestation and at delivery, particularly in areas experiencing outbreaks or for women at risk of syphilis acquisition.
- Syphilis is diagnosed most often using serologic tests and can be easily treated with penicillin.
2. Burden of syphilis and co-infections
2.1 Epidemiology of syphilis in Canada
Following chlamydia and gonorrhea, syphilis is the third most commonly reported notifiable STI in CanadaFootnote 51. Canada, in 1998, announced a national goal of maintaining a syphilis rate below 0.5 per 100,000 population by the year 2000. However, since the early 2000s, rates of syphilis infection have been steadily increasingFootnote 52. In recent years, many jurisdictions are experiencing a major surge in their number of syphilis cases (Section 3). Between 2008 and 2017, the rate of infectious syphilis increased nationally by 167%, the highest relative increase of all three STIsFootnote 51. In 2017, the most recent year for which pan-Canadian syphilis data have been published, the rate of infectious syphilis in Canada was 11.2 cases per 100,000 populationFootnote 51. That year, the rate was 2.4 cases per 100,000 females, and 20.0 cases per 100,000 malesFootnote 51. Though the rate is lower among females, provincial reports suggest that up to 86% of female syphilis cases are among women of childbearing age (15 to 39 years), leading to a higher risk of congenital syphilis incidenceFootnote 53. Provincial and territorial reports suggest that since 2017, rates of infectious and congenital syphilis have increased significantly, with a national rate of 17.0 in 2018, according to preliminary 2018 data (Section 5).
The risk of syphilis is not distributed evenly across the Canadian population. Certain populations, such as gbMSM, are known to experience high rates. Moreover, large increases in rates have been observed recently in other populations, especially women of reproductive ageFootnote 54. As a result of this recent trend, Canada reported its highest number of congenital syphilis cases in past 25 years in Canada in 2018 (17 cases). Section 4 of this report describes in detail social inequalities with regard to syphilis risk, highlighting the importance of considering health equity in syphilis prevention and control.
2.2 Burden of the disease on those affected
Among people diagnosed with syphilis in Canada, data on the distribution of staging is currently lacking. Most published studies do not distinguish between stages of infection in their reporting, and consistent staging data are not currently available across all provinces and territoriesFootnote 55. Studies that do detail staging indicate a broad distribution of cases across stages at diagnosis. Among 1,473 syphilis cases diagnosed between 1995 and 2005 in British Columbia, 50% were at primary or secondary stages, and 50% were early latentFootnote 56. In another study of a randomly selected set of 350 syphilis cases among gbMSM in British Columbia in 2013, 20% of cases were diagnosed at a primary stage, 25% were secondary, and 55% were early latentFootnote 57. In a Winnipeg-based study of 151 infectious syphilis cases in 2014 and 2015, 41% were primary, 35% were secondary, and 21% were early latentFootnote 58. Additionally, in an Alberta-based review of retrospective cases from 1975 to 2016, 8,874 cases of syphilis were reported, of which 51% of cases were infectious (i.e. primary, secondary or early latent), while 49% were classified as non-infectious (i.e. late latent or tertiary)Footnote 59. Of the 254 cases of neurosyphilis and tertiary syphilis identified in this review, 251 cases were neurosyphilis (52% early neurosyphilis and 46% late neurosyphilis) and three were cardiovascular syphilis.
In the same Winnipeg-based study referenced above, when comparing the distribution of stages among males and females, the authors found that although the proportions diagnosed at a primary stage were similar for both sexes (approximately 41%), female cases were diagnosed later (18% secondary and 35% early latent) than males (37% secondary and 19% early-latent)Footnote 58. Studies suggest that the higher rates of later-stage syphilis diagnosis among females may be due to the fact that primary lesions may be less visible for females than males, thus making it more difficult for females to know to seek assessment and diagnosisFootnote 2. Other reported reasons for this difference include the fact that females may be less likely than males to be screened for syphilis when another STI is suspected, and they may be more likely to seek over-the-counter treatments, which may mask STI presence and delay diagnosisFootnote 60. Furthermore, while many health clinic programs and community-based organizations have conducted considerable outreach activities among gbMSM communities to promote access to sexual health resources and services, there have been fewer efforts geared towards women. Additionally, it has been reported in existing literature that cases of congenital syphilis usually occur because of absence or delays in access to prenatal care for pregnant women (Section 5). These disparities in the targeting of sexual health outreach may also contribute to delays in syphilis diagnosis among women. Overall, the large proportion of cases diagnosed at an early-latent phase may indicate gaps in syphilis screening and knowledge in the country. Inequalities in stage distribution represent an important health equity issue.
If left untreated, syphilis can progress from primary to subsequent stages, each associated with distinct clinical burdens for those affectedFootnote 2. Available studies suggest that between 15% and 40% of untreated cases will experience complications associated with late stage syphilis, such as late neurosyphilis or tertiary syphilisFootnote 2. Late stage syphilis requires a more intensive treatment, with possible side effects and greater risk of treatment failureFootnote 2. Treatment failure is characterized by increasing or stable non-treponemal test titers at the recommended follow-up test one month after treatment.
Syphilis during pregnancy can lead to adverse outcomes for the fetus, including miscarriage, stillbirth and infant death. Although syphilis is not associated with high levels of mortality in Canada, it is associated with a reduction in functioning and poorer quality of life. A study conducted in Ontario reported that untreated syphilis was associated with the equivalent of 18 years of life lost due to reduced functioning, 94% of which was attributable to neurosyphilisFootnote 61. However, given that there may be considerable under-diagnosis and under-reporting of syphilis, the authors note that it is possible that these estimates underestimate the true number of years of life lostFootnote 61. Furthermore, beyond the physical health burden associated with syphilis infection, some studies also identify psychosocial repercussions of syphilis-related stigmaFootnote 62Footnote 63.
2.3 Risk of sexual transmission
It is understood that the transmission rate of infectious syphilis (primary, secondary, and early latent stages) per sexual partner is approximately 64% for primary and secondary syphilis64. There are few studies exploring the per-act transmission risk of syphilisFootnote 64. An American study that focused on transmission among gbMSM found that the probability of transmission is of 0.5% to 1.4% per sexual act during the primary and secondary syphilis stages, with lower probability in the early latent stage64. Lastly, though few studies have explored possible sex differences in transmission probability, experts hypothesize that as with HIV and gonorrhea, transmission probabilities may be higher from men-to-women than from women-to-menFootnote 65.
In general, the probability of transmission is dependent on the susceptibility of the sexual partner that is exposed64. Population-level risk of transmission is lower when pro-active screening occurs, cases are treated, cases’ contacts are traced and treated, and preventive strategies, such as condoms, are employedFootnote 64. These factors, as well as other strategies to reduce transmission risk, are described in Section 6 of this report.
2.4 Adverse pregnancy outcomes
As mentioned previously, the majority of female syphilis cases are among individuals of childbearing age (15 to 49 years, as defined by the WHO, although the PHAC STBBI surveillance team uses 15-39 years, in accordance with CNDSS age groups categories)Footnote 51Footnote 53.
Studies on mother-to-child syphilis transmission risk are rare. In a systematic review, transmission rates ranging from 2.3% to 40.9% have been reported, with a pooled mother-to-child transmission rate of 15.5%Footnote 66.
Among pregnant women, the risk of transmission is dependent on the stage of the syphilis infection as well as the timing of infection, diagnosis, and treatment during the pregnancy. However, evidence indicates that vertical transmission can occur at any time during pregnancyFootnote 64Footnote 67. The risk of vertical transmission is highest when syphilis is acquired near termFootnote 67. Research suggests that the risk of vertical transmission is 70% to 100% during primary and secondary stages, and 40% in the early latent phaseFootnote 3. If untreated, approximately 77% of maternal syphilis cases will result in adverse outcomes, which could include pre-term birth, stillbirth, neonatal mortality or clinical manifestations of congenital syphilisFootnote 64Footnote 68. Risks of adverse outcomes are higher compared to uninfected pregnancies, even after treatmentFootnote 69. As adverse pregnancy outcomes cause physical and psychological burdens both for the parent and the child, maternal syphilis and congenital syphilis are of significant public health concern.
2.5 Co-infections and syndemics
In recent years, the incidence of STIs has been increasing both in Canada and internationally (Figure 2 and Figure 5).
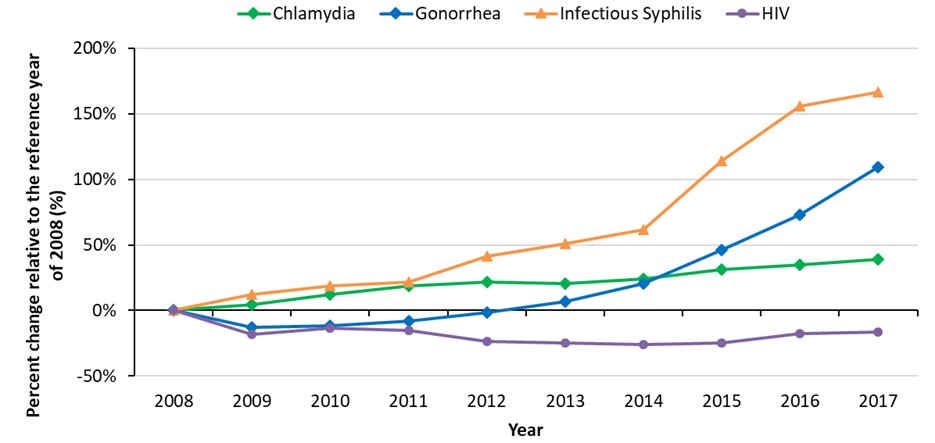
Figure 2 - Text description
This graph displays the percent change in chlamydia, gonorrhea, infectious syphilis, and human immunodeficiency virus (HIV) rates relative to the reference year of 2008, between 2008 and 2017 in Canada. The horizontal axis shows the calendar years from 2008 to 2017. The vertical axis shows the percent change of rates of chlamydia, gonorrhea, infectious syphilis, and HIV.
| Year | Percent change relative to the reference year of 2008 (%) | |||
|---|---|---|---|---|
| Chlamydia | Gonorrhea | Infectious Syphilis | HIV | |
| 2008 | 0 | 0 | 0 | 0 |
| 2009 | 4% | -13% | 12% | -18% |
| 2010 | 12% | -12% | 19% | -13% |
| 2011 | 19% | -8% | 22% | -15% |
| 2012 | 22% | -1% | 41% | -24% |
| 2013 | 21% | 7% | 51% | -25% |
| 2014 | 24% | 21% | 62% | -26% |
| 2015 | 31% | 46% | 114% | -25% |
| 2016 | 35% | 73% | 156% | -17% |
| 2017 | 39% | 109% | 167% | -16% |
Source: Public Health Agency of Canada (2019). Canadian Notifiable Disease Surveillance System.
There is a trend with regard to co-infection of syphilis with HIV. The current epidemics of syphilis and other STIs have been described as a syndemic, given their concurrence (co-infections are common), interactions between these infections, associated health consequences, and shared underlying determinants (Figure 3)Footnote 62Footnote 70Footnote 71. National surveillance data do not track co-infections, but existing Canadian studies have reported the prevalence of syphilis among HIV-positive individuals to be around 8% to 11%Footnote 72Footnote 73.
Syphilis increases the risk of acquisition and transmission of HIV in several waysFootnote 74. First, syphilitic chancres provide an entry portal for the HIV virusFootnote 75. Secondly, the bacterium causing the syphilis infection, T. pallidum, has been observed to increase the expression of the CCR5 chemokine receptor—one of the principal receptors for macrophage-tropic viruses, such as HIV. This leads to a higher likelihood of HIV transmissionFootnote 75.
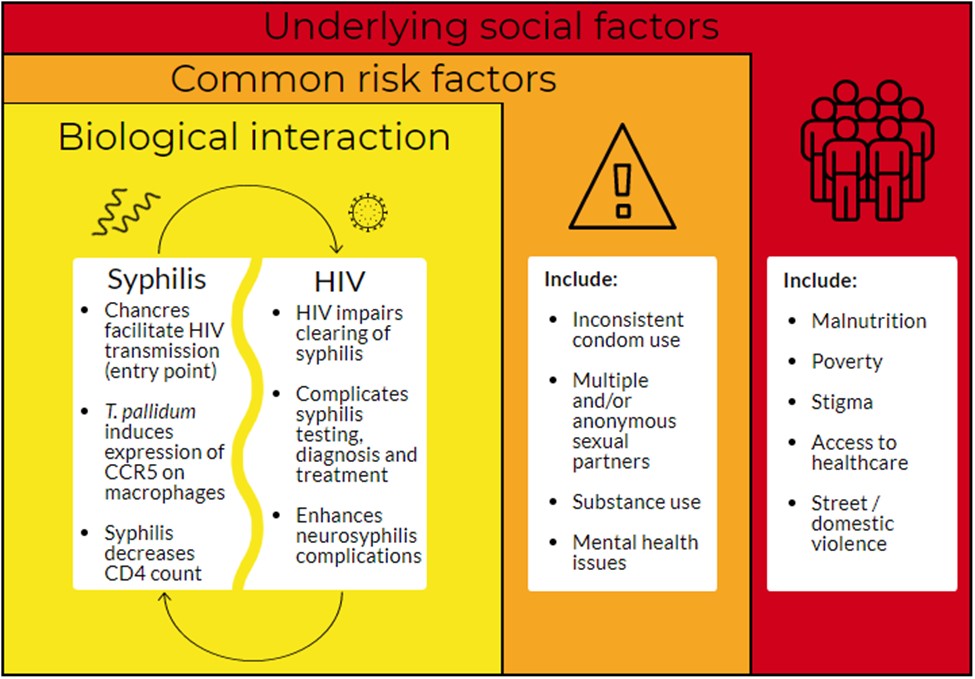
Figure 3 - Text description
Factors contributing to the HIV-syphilis syndemic:
- Biological interaction (syphilis influences HIV in the following ways: chancres facilitate HIV transmission (entry point), T. pallidum induces expression of CCR5 on macrophages, and syphilis decreases CD4 counts; HIV influences syphilis in the following ways: HIV impairs clearing of syphilis, complicates syphilis testing, diagnosis and treatment, and enhances neurosyphilis complications)
- There are common risk factors such as inconsistent condom use, multiple and/or anonymous sexual partners, substance use and mental health issues
- There are also underlying social factors which include malnutrition, poverty, stigma, access to healthcare and street/domestic violence
Adapted from Jiang et al. (2017), Yu et al. (2018), Singer and Clair (2003), Singer et al. (2006), Lang et al. (2018), Remis et al. (2016), Solomon et al. (2016) and Karp G et al. (2009)
Adapted from Jiang et al. (2017)Footnote 70, Yu et al. (2018)Footnote 62, Singer and Clair (2003)Footnote 71, Singer et al. (2006)Footnote 76, Lang et al. (2018)Footnote 72, Remis et al. (2016)Footnote 73, Solomon et al. (2016)Footnote 74 and Karp G et al. (2009)Footnote 75.
In turn, people living with HIV are eight times more likely to be infected with syphilis compared to the general populationFootnote 75. Several factors can explain the association between HIV and syphilis infection. First, the immune suppression associated with HIV is believed to impair clearance of syphilisFootnote 75. Further, HIV alters the natural evolution of syphilis, leading to more rapid progression through the disease stages —namely, to neurosyphilis and more aggressive and atypical signs of infection— and syphilis treatment complications have also been observedFootnote 2Footnote 75Footnote 77. Studies also indicate that it can be difficult to diagnose neurosyphilis in people living with HIV, insofar as CSF invasion-related symptoms can occur without syphilis infectionFootnote 2. Lastly, due to the shared risk factors for both HIV and syphilis infections (including biological susceptibility and sexual behaviours), people living with HIV are more likely to have repeated syphilis infections following successful syphilis treatmentFootnote 64Footnote 78.
Inconsistent condom use and sex with multiple or anonymous partners are major risk factors for both syphilis and HIVFootnote 76Footnote 79. Condom use is an effective prevention method to reduce the spread of STIs, but inconsistent or improper use decreases its effectivenessFootnote 80. A study conducted by Remis et al.Footnote 73 (n=442) showed that condomless anal and oral sex with casual partners was correlated with syphilis infection among gbMSM living with HIV in Toronto. Another study (n=194) identified syphilis co-infection in populations living with HIV and underlined a number of additional risk factors for syphilis co-infection, such as being a man who has sex with men, as well as alcohol and recreational substance useFootnote 72.
Overarching adverse social conditions, such as malnutrition, poverty, stigma, discrimination and exposure to violence, can put individuals at risk for syndemics, exacerbating the likelihood of acquiring co-occurring infectionsFootnote 71Footnote 76. These inequalities all have an impact on health and can lead to adverse health outcomes in key populations and can limit access to healthcare and appropriate treatmentFootnote 62Footnote 80.
Key messages
- National rates of syphilis infection have had a higher relative increase between 2013 and 2018, compared to chlamydia and gonorrhea rates.
- Gay, bisexual and other men who have sex with men are the most affected population in past decades but high relative increases in rates have been observed in women of reproductive age in recent years.
- The female syphilis rate increase in recent years has translated to an increase in the number of congenital syphilis cases.
- Untreated syphilis is associated with a high burden of congenital cases and with reduced functioning for other cases.
- Trends of syphilis and other STIs have been described as a syndemic.
3. Epidemiological trends of syphilis in Canada, 2009-2018
3.1 Historical and recent national rates of syphilis in Canada
In Canada, syphilis has been nationally notifiable since 1924. In this section, Canadian syphilis CNDSS data covering the period of 1979 to 2017 are presented, along with preliminary data for 2018, provided directly by PTs. Current case definitions and details concerning data sources and analysis are described in Appendix B and Appendix C.
3.1.1 Historical syphilis trends in Canada
Canadian rates of syphilis were high until the 1940s, when they started to decrease significantly, a trend that continued until the 1980s. Rates remained low for most of the 1990s (Figure 4). This trend was also observed in other countries, such as the UKFootnote 81. Following this period of decline, Canadian rates began to climb again in the early 2000s (Figure 4). A similar increase in incidence rates was observed in the UK and the US over this time (Figure 5)Footnote 81Footnote 82.
Several hypotheses have been proposed to explain the growing incidence of syphilis in Canada over the past decades. In the 1990s and 2000s, a number of significant events occurred, including the introduction of antiretroviral therapy (ART) for HIV treatment in the late 1990s. This was followed by the arrival of the Internet and online apps for meeting potential sexual partners, as well as an increase in the use of certain drugs, such as crystal methamphetamine for chemsex in the 2000sFootnote 83. The term “chemsex” (or Party and Play, “PnP”) refers to the planned use of certain substances, including but not limited to methamphetamines, to extend the duration (hours to days) and intensity of sexual encounters (number of partners, types of practices)Footnote 84. While it is hypothesized that these ecological factors have shaped current STI incidence patterns in North America, no Canadian studies have confirmed the correlation between these population-level shifts and changes in syphilis incidenceFootnote 83.
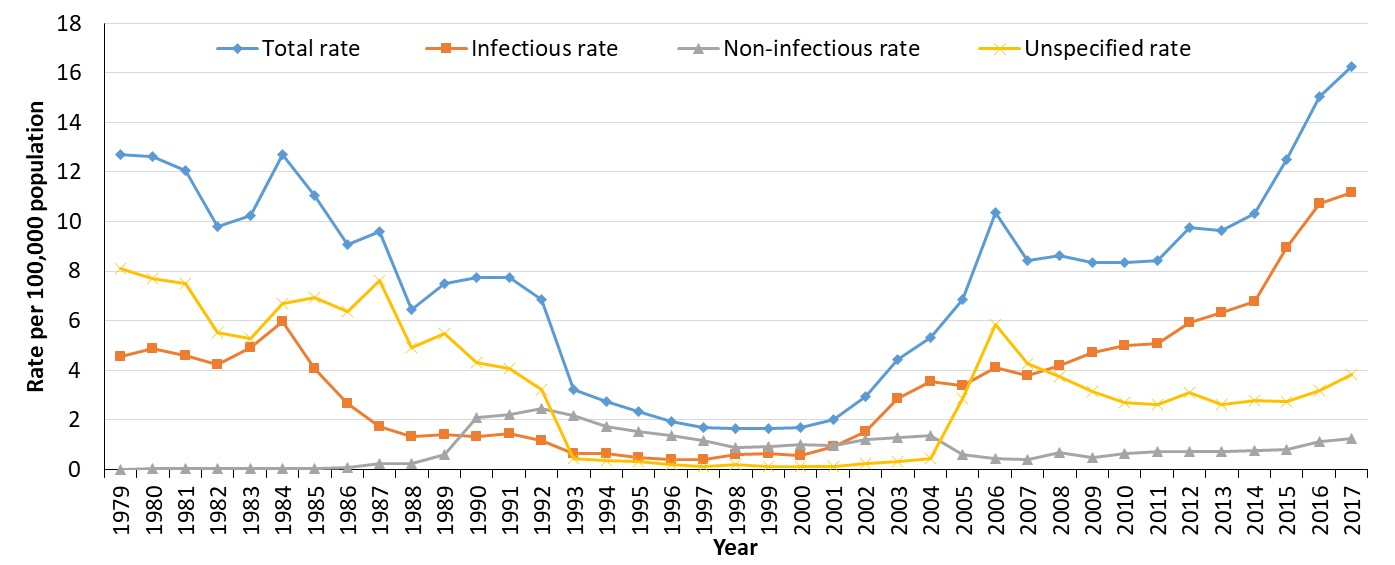
Figure 4 - Text description
This graph displays the rate per 100,000 population for syphilis, between 1979 and 2017 in Canada. The horizontal axis shows the calendar years from 1979 to 2017. The vertical axis shows the rate per 100,000 population for syphilis overall, infectious syphilis, non-infectious syphilis and unspecified syphilis.
| Year | Rate per 100,000 population | |||
|---|---|---|---|---|
| Total Rate | Infectious Rate | Non-Infectious Rate | Unspecified Rate | |
| 1979 | 12.7 | 4.6 | 0.0 | 8.1 |
| 1980 | 12.6 | 4.9 | 0.0 | 7.7 |
| 1981 | 12.1 | 4.6 | 0.0 | 7.5 |
| 1982 | 9.8 | 4.2 | 0.0 | 5.5 |
| 1983 | 10.2 | 4.9 | 0.0 | 5.3 |
| 1984 | 12.7 | 6.0 | 0.0 | 6.7 |
| 1985 | 11.1 | 4.1 | 0.1 | 6.9 |
| 1986 | 9.1 | 2.6 | 0.1 | 6.4 |
| 1987 | 9.6 | 1.7 | 0.2 | 7.6 |
| 1988 | 6.4 | 1.3 | 0.2 | 4.9 |
| 1989 | 7.5 | 1.4 | 0.6 | 5.5 |
| 1990 | 7.7 | 1.3 | 2.1 | 4.3 |
| 1991 | 7.8 | 1.5 | 2.2 | 4.1 |
| 1992 | 6.8 | 1.2 | 2.5 | 3.2 |
| 1993 | 3.2 | 0.6 | 2.2 | 0.4 |
| 1994 | 2.7 | 0.6 | 1.7 | 0.3 |
| 1995 | 2.3 | 0.5 | 1.5 | 0.3 |
| 1996 | 1.9 | 0.4 | 1.4 | 0.2 |
| 1997 | 1.7 | 0.4 | 1.2 | 0.1 |
| 1998 | 1.7 | 0.6 | 0.9 | 0.2 |
| 1999 | 1.6 | 0.6 | 0.9 | 0.1 |
| 2000 | 1.7 | 0.6 | 1.0 | 0.1 |
| 2001 | 2.0 | 0.9 | 1.0 | 0.1 |
| 2002 | 3.0 | 1.5 | 1.2 | 0.2 |
| 2003 | 4.4 | 2.9 | 1.3 | 0.3 |
| 2004 | 5.3 | 3.6 | 1.4 | 0.4 |
| 2005 | 6.8 | 3.4 | 0.6 | 2.9 |
| 2006 | 10.4 | 4.1 | 0.4 | 5.9 |
| 2007 | 8.4 | 3.8 | 0.4 | 4.3 |
| 2008 | 8.6 | 4.2 | 0.7 | 3.8 |
| 2009 | 8.3 | 4.7 | 0.5 | 3.1 |
| 2010 | 8.4 | 5.0 | 0.7 | 2.7 |
| 2011 | 8.4 | 5.1 | 0.7 | 2.6 |
| 2012 | 9.7 | 5.9 | 0.7 | 3.1 |
| 2013 | 9.6 | 6.3 | 0.7 | 2.6 |
| 2014 | 10.3 | 6.8 | 0.8 | 2.8 |
| 2015 | 12.5 | 9.0 | 0.8 | 2.7 |
| 2016 | 15.0 | 10.7 | 1.1 | 3.2 |
| 2017 | 16.3 | 11.2 | 1.3 | 3.8 |
Source: Public Health Agency of Canada (2019). Canadian Notifiable Disease Surveillance System.
Infectious syphilis rates have continued to increase in Canada (Figure 5) in the last decade. Similar increases have been observed in other Organisation for Economic Co-operation and Development (OECD) countries (Figure 5). Canadian rates tend to be similar to those of England and slightly higher than those reported in the US. Detailed rates of infectious syphilis for Canada and other selected OECD countries for the last decade are presented in Appendix D.
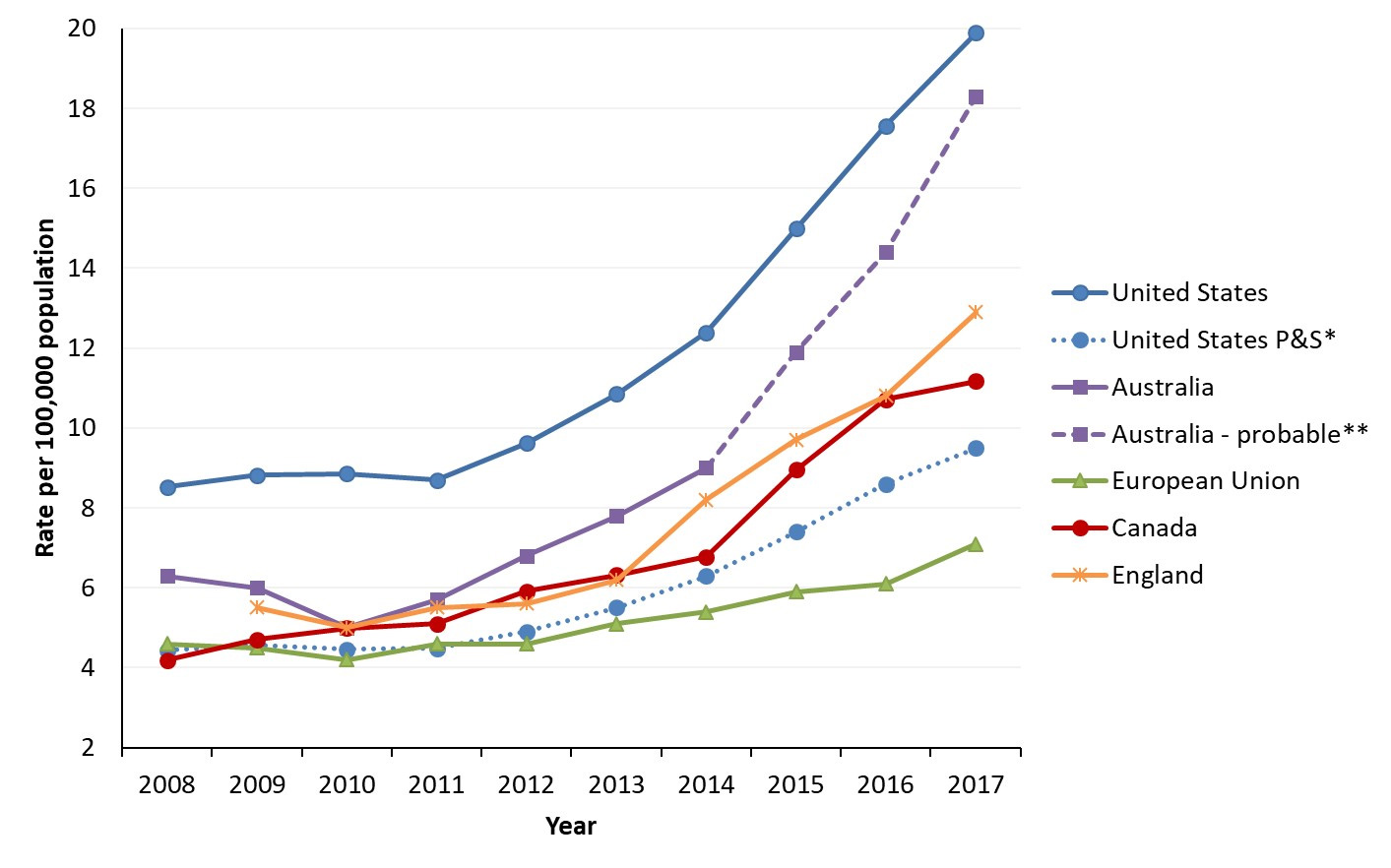
Figure 5 - Text description
This graph displays the infectious syphilis rate per 100,000 population for OECD countries and Canada, between 2008 and 2017. The horizontal axis shows the calendar years from 2008 to 2017. The vertical axis shows the rate per 100,000 population for the United States (US), Australia, European Union (EU), Canada, and England.
| Year | Rate per 100,000 population | ||||||
|---|---|---|---|---|---|---|---|
| United States | United States P&SFootnote * | Australia | Australia-probableFootnote ** | European Union | Canada | England | |
| 2008 | 4.4 | 8.5 | 6.3 | 4.6 | 4.2 | ||
| 2009 | 4.6 | 8.8 | 6.0 | 4.5 | 4.7 | 5.5 | |
| 2010 | 4.5 | 8.9 | 5.0 | 4.2 | 5.0 | 5.0 | |
| 2011 | 4.5 | 8.7 | 5.7 | 4.6 | 5.1 | 5.5 | |
| 2012 | 4.9 | 9.6 | 6.8 | 4.6 | 5.9 | 5.6 | |
| 2013 | 5.5 | 10.9 | 7.8 | 5.1 | 6.3 | 6.2 | |
| 2014 | 6.3 | 12.4 | 9.0 | 9.0 | 5.4 | 6.8 | 8.2 |
| 2015 | 7.4 | 15.0 | 11.9 | 5.9 | 9.0 | 9.7 | |
| 2016 | 8.6 | 17.6 | 14.4 | 6.1 | 10.7 | 10.8 | |
| 2017 | 9.5 | 19.9 | 18.3 | 7.1 | 11.2 | 12.9 | |
Note: Canada’s definition of infectious syphilis includes confirmed cases of primary, secondary and early latent syphilis. Please note that some of the countries presented have slightly different definitions.
|
|||||||
Note: Canada’s definition of infectious syphilis includes confirmed cases of primary, secondary and early latent syphilis. Please note that some of the countries presented have slightly different definitions.
* The US includes confirmed primary and secondary stages only in its definition of infectious cases (US- P&S- blue dotted line). Confirmed early latent cases were added to primary and secondary cases to produce US rate estimates for the definition of infectious syphilis used in Canada (solid blue line).
** The dotted line for Australia represents the years for which the case definition included probable cases of infectious syphilis (in addition to confirmed cases of primary, secondary and early latent syphilis). In 2015, approximately 9% were reported as such.
The EU includes all cases of syphilis regardless of stage, although of the countries that provided staging information, 95% of cases were reported as either primary, secondary or early latent.
- Footnote a
-
Sources:
- Australia: Kirby Institute. HIV, viral hepatitis and sexually transmissible infections in Australia: annual surveillance report 2018. 2018. Australia’s notifiable disease status, 2015: Annual report of the National Notifiable Diseases Surveillance System, NNDSS Annual Report working group
- European Union: European Centre for Disease Prevention and Control (ECDC). Syphilis - Annual epidemiological report for 2017. 2019 12 July 2019.
- United States: Centers for Disease Control and Prevention (CDC). Table 27. Primary and Secondary Syphilis — Reported Cases and Rates of Reported Cases by State/Area and Region in Alphabetical Order, United States and Outlying Areas, 2013–2017. 2018; Accessed September 10, 2019.
- Canada: Government of Canada. Canadian Notifiable Disease Surveillance System. 2018; 2019.
- England: Public Health England, Official Statistics, Sexually transmitted infections (STIs): annual data tables. Table 1 (b): Rates of new STI diagnoses in England by gender, 2008 – 2017, Rates per 100 000, Syphilis: primary, secondary, early latent, total.
Over the past 25 years, the distribution of syphilis cases across the four stages of infection has evolved. Historically, the vast majority of cases were diagnosed in the late latent phase (Figure 6). For example, in the 1990s, only 20% of cases for which a status was specified were diagnosed in the infectious stages. However, over time, cases have tended to be diagnosed earlier. Since 2006, primary, secondary and early latent cases now comprise at least 75% of the reported cases in Canada (Figure 6)Footnote 85-88. This increase in the proportion of cases diagnosed during an infectious stage may be related to the introduction of PCR testing used in the diagnosis of syphilis, especially at early stages and for individuals without antibody response. Increased screening in key populations may also play a role. Few provinces, including British Columbia and Ontario, stopped reporting non-infectious cases in the late 1990s, which has affected the proportion of non-infectious cases reported nationally. However, the observed pattern of an increased proportion of cases that are infectious over time holds even after excluding British Columbia and Ontario from the analysis. Reporting patterns by PT are presented in Appendix B.
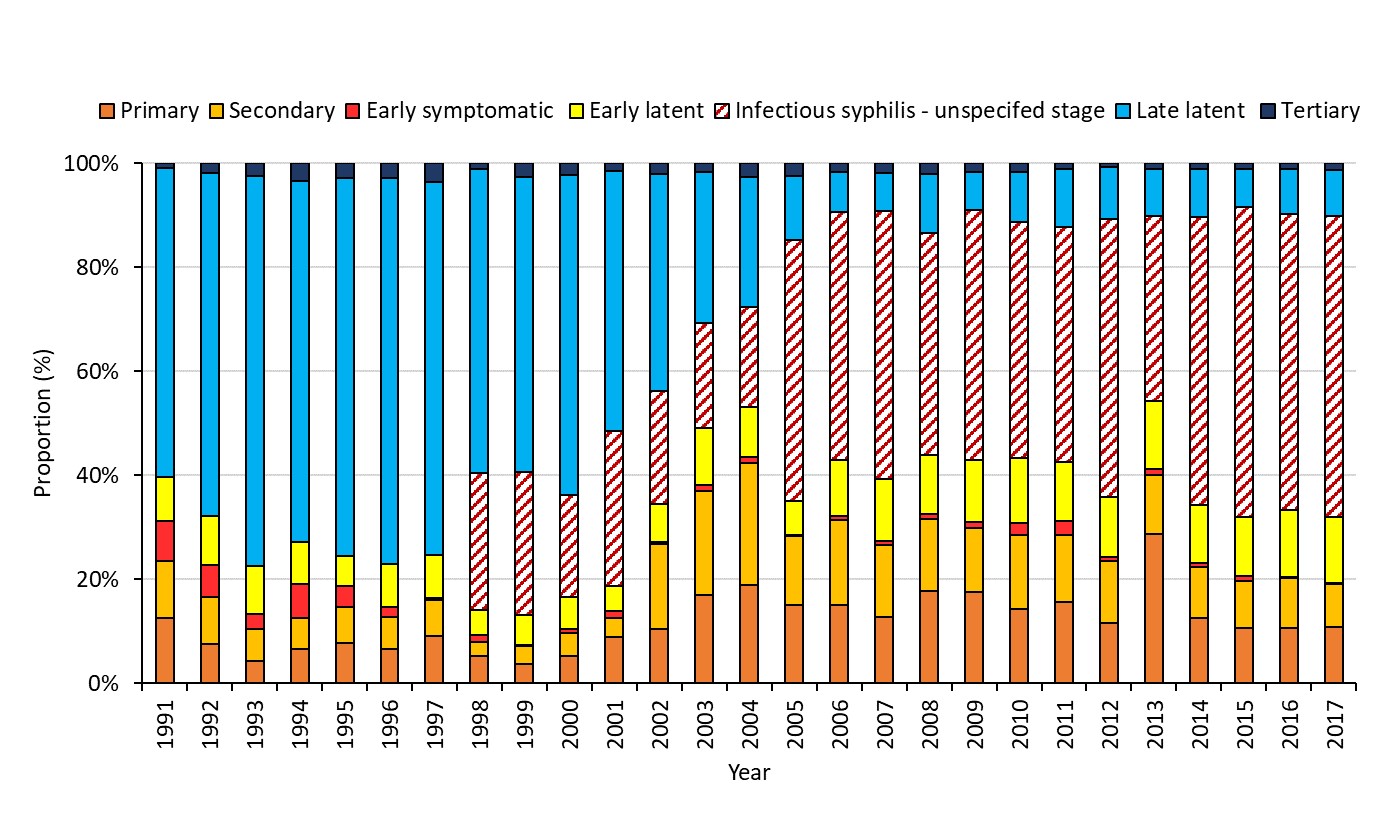
Figure 6 - Text description
This graph displays the proportion of reported syphilis cases by stage of infection, between 1991 and 2017 in Canada. The horizontal axis shows the calendar years from 1991 to 2017. The vertical axis shows the proportion of total reported syphilis cases of primary, secondary, early symptomatic, early latent, unspecified infectious syphilis, late latent, and tertiary syphilis.
| Year | Proportion of Reported Syphilis Cases (%) | ||||||
|---|---|---|---|---|---|---|---|
| Primary | Secondary | Early symptomatic | Early latent | Infectious syphilis- unspecified stage | Late latent | Tertiary | |
| 1991 | 12.6% | 10.9% | 7.8% | 8.4% | 0.0% | 59.5% | 0.9% |
| 1992 | 7.6% | 9.1% | 6.1% | 9.4% | 0.0% | 66.0% | 1.9% |
| 1993 | 4.4% | 6.1% | 2.9% | 9.1% | 0.0% | 75.0% | 2.5% |
| 1994 | 6.7% | 5.9% | 6.5% | 8.1% | 0.0% | 69.5% | 3.3% |
| 1995 | 7.7% | 7.0% | 4.1% | 5.6% | 0.0% | 72.6% | 2.9% |
| 1996 | 6.5% | 6.2% | 1.9% | 8.3% | 0.0% | 74.2% | 2.9% |
| 1997 | 9.2% | 6.8% | 0.4% | 8.3% | 0.0% | 71.6% | 3.6% |
| 1998 | 5.2% | 2.7% | 1.4% | 4.8% | 26.3% | 58.5% | 1.1% |
| 1999 | 3.7% | 3.4% | 0.2% | 5.8% | 27.6% | 56.7% | 2.6% |
| 2000 | 5.3% | 4.3% | 0.8% | 6.2% | 19.5% | 61.6% | 2.3% |
| 2001 | 9.0% | 3.6% | 1.4% | 4.7% | 29.8% | 50.0% | 1.5% |
| 2002 | 10.5% | 16.3% | 0.4% | 7.4% | 21.7% | 41.8% | 2.0% |
| 2003 | 17.0% | 19.9% | 1.3% | 10.9% | 20.1% | 29.2% | 1.6% |
| 2004 | 18.9% | 23.5% | 1.2% | 9.5% | 19.4% | 25.0% | 2.5% |
| 2005 | 15.0% | 13.4% | 0.2% | 6.5% | 50.2% | 12.3% | 2.4% |
| 2006 | 15.1% | 16.4% | 0.7% | 10.9% | 47.5% | 7.8% | 1.6% |
| 2007 | 12.8% | 13.8% | 0.7% | 12.1% | 51.4% | 7.4% | 1.8% |
| 2008 | 17.8% | 13.9% | 0.9% | 11.4% | 42.5% | 11.4% | 2.0% |
| 2009 | 17.6% | 12.3% | 1.1% | 11.9% | 48.1% | 7.3% | 1.7% |
| 2010 | 14.2% | 14.3% | 2.3% | 12.6% | 45.3% | 9.7% | 1.6% |
| 2011 | 15.6% | 12.8% | 2.8% | 11.4% | 45.0% | 11.2% | 1.2% |
| 2012 | 11.7% | 11.9% | 0.7% | 11.6% | 53.5% | 10.0% | 0.7% |
| 2013 | 28.7% | 11.3% | 1.1% | 13.2% | 35.5% | 9.1% | 1.1% |
| 2014 | 12.6% | 9.8% | 0.8% | 11.2% | 55.4% | 9.1% | 1.1% |
| 2015 | 10.6% | 9.2% | 0.8% | 11.5% | 59.6% | 7.1% | 1.2% |
| 2016 | 10.7% | 9.5% | 0.2% | 12.9% | 57.0% | 8.6% | 1.1% |
| 2017 | 10.7% | 8.3% | 0.3% | 12.7% | 57.8% | 9.0% | 1.2% |
Note: Early symptomatic includes both primary and secondary cases.
Source: Public Health Agency of Canada (2019). Canadian Notifiable Disease Surveillance System.
Slight variations in staging, according to sex, have been observed in Canada. Between 1991 and 2017, the proportion of infectious syphilis cases was higher amongst males (Figure 7) than females (Figure 8) (case proportions by syphilis stage overall and sex are presented in Appendix E). Potential reasons for the difference in proportion of infectious syphilis by sex are presented in Section 2.2.
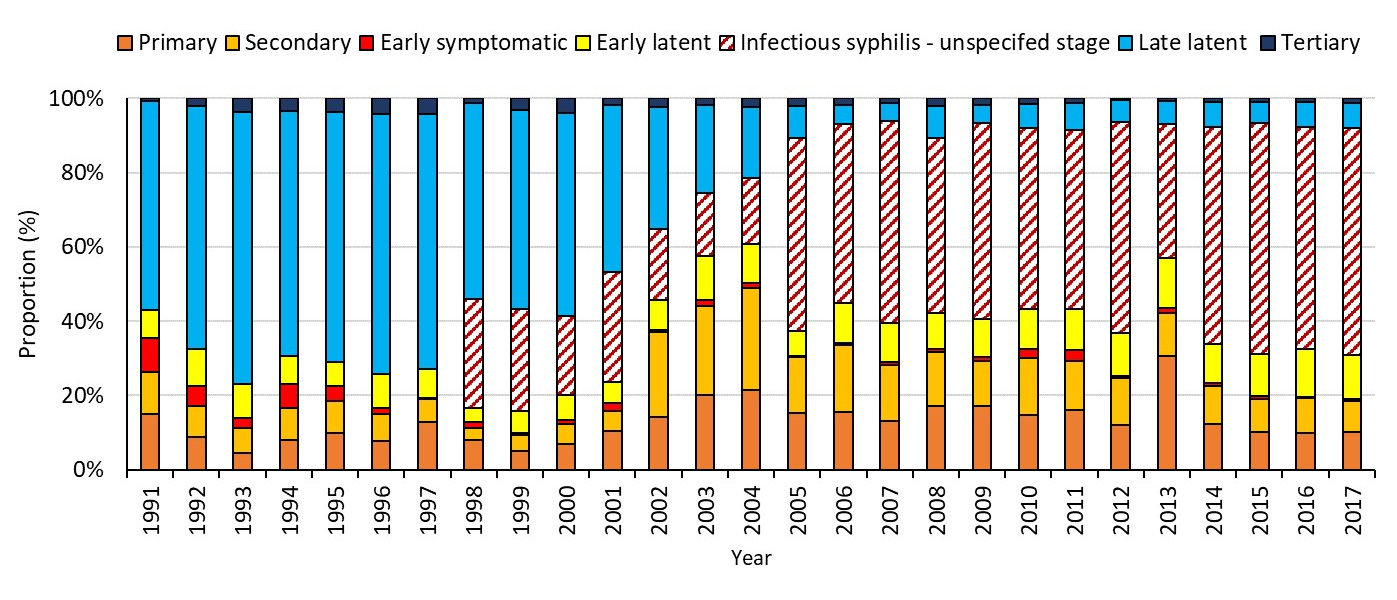
Figure 7 - Text description
This graph displays the proportion of reported syphilis cases by stage of infection, between 1991 and 2017 in Canada for males. The horizontal axis shows the calendar years from 1991 to 2017. The vertical axis shows the proportion of total reported syphilis cases of primary, secondary, early symptomatic, early latent, unspecified infectious syphilis, late latent, and tertiary syphilis.
| Year | Proportion of Reported Syphilis Cases | ||||||
|---|---|---|---|---|---|---|---|
| Primary | Secondary | Early symptomatic | Early latent | Infectious syphilis- unspecified stage | Late latent | Tertiary | |
| 1991 | 15.0% | 11.2% | 9.3% | 7.4% | 0.0% | 56.2% | 0.9% |
| 1992 | 8.9% | 8.2% | 5.4% | 9.9% | 0.0% | 65.4% | 2.2% |
| 1993 | 4.4% | 6.8% | 2.6% | 9.4% | 0.0% | 73.1% | 3.7% |
| 1994 | 8.1% | 8.4% | 6.6% | 7.6% | 0.0% | 65.9% | 3.4% |
| 1995 | 10.0% | 8.4% | 4.0% | 6.5% | 0.0% | 67.3% | 3.7% |
| 1996 | 7.8% | 7.1% | 1.8% | 9.2% | 0.0% | 69.9% | 4.3% |
| 1997 | 12.8% | 6.2% | 0.4% | 7.8% | 0.0% | 68.7% | 4.1% |
| 1998 | 7.9% | 3.3% | 1.7% | 3.7% | 29.5% | 52.7% | 1.2% |
| 1999 | 5.1% | 4.3% | 0.4% | 5.9% | 27.5% | 53.7% | 3.1% |
| 2000 | 6.8% | 5.4% | 1.1% | 6.8% | 21.2% | 54.7% | 4.0% |
| 2001 | 10.4% | 5.5% | 2.0% | 5.8% | 29.7% | 45.0% | 1.7% |
| 2002 | 14.1% | 23.1% | 0.3% | 8.2% | 19.0% | 32.8% | 2.4% |
| 2003 | 20.1% | 24.0% | 1.5% | 11.9% | 17.0% | 23.7% | 1.8% |
| 2004 | 21.5% | 27.5% | 1.3% | 10.6% | 17.6% | 19.1% | 2.4% |
| 2005 | 15.4% | 14.9% | 0.3% | 6.7% | 52.0% | 8.7% | 2.0% |
| 2006 | 15.6% | 17.8% | 0.6% | 10.9% | 48.1% | 5.1% | 1.8% |
| 2007 | 13.0% | 15.1% | 0.8% | 10.4% | 54.6% | 4.7% | 1.3% |
| 2008 | 17.2% | 14.6% | 0.7% | 9.8% | 47.1% | 8.6% | 2.0% |
| 2009 | 17.0% | 12.2% | 1.0% | 10.2% | 52.9% | 4.9% | 1.7% |
| 2010 | 14.7% | 15.3% | 2.4% | 10.8% | 48.8% | 6.3% | 1.7% |
| 2011 | 16.0% | 13.4% | 2.7% | 11.1% | 48.2% | 7.3% | 1.2% |
| 2012 | 12.1% | 12.6% | 0.7% | 11.5% | 56.7% | 5.9% | 0.5% |
| 2013 | 30.6% | 11.7% | 1.2% | 13.4% | 36.3% | 6.1% | 0.8% |
| 2014 | 12.3% | 10.2% | 0.8% | 10.6% | 58.4% | 6.6% | 1.1% |
| 2015 | 10.1% | 9.1% | 0.7% | 11.3% | 62.2% | 5.4% | 1.1% |
| 2016 | 9.8% | 9.5% | 0.3% | 13.0% | 59.8% | 6.5% | 1.1% |
| 2017 | 10.2% | 8.5% | 0.4% | 12.0% | 61.0% | 6.8% | 1.2% |
Note: Early symptomatic includes both primary and secondary cases.
Source: Public Health Agency of Canada (2019). Canadian Notifiable Disease Surveillance System.
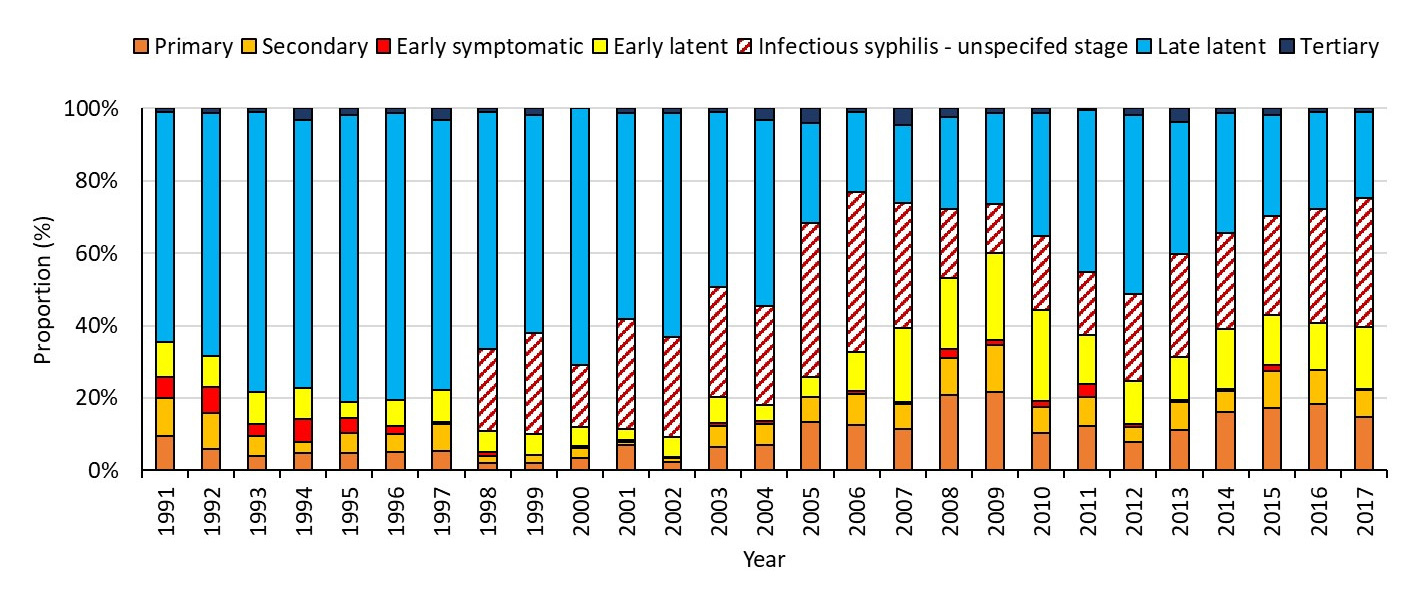
Figure 8 - Text description
This graph displays the proportion of reported syphilis cases by stage of infection, between 1991 and 2017 in Canada for females. The horizontal axis shows the calendar years from 1991 to 2017. The vertical axis shows the proportion of total reported syphilis cases of primary, secondary, early symptomatic, early latent, unspecified infectious syphilis, late latent, and tertiary syphilis.
| Year | Proportion of Reported Syphilis Cases | ||||||
|---|---|---|---|---|---|---|---|
| Primary | Secondary | Early symptomatic | Early latent | Infectious syphilis- unspecified stage | Late latent | Tertiary | |
| 1991 | 9.6% | 10.5% | 5.8% | 9.6% | 0.0% | 63.7% | 0.9% |
| 1992 | 5.8% | 10.0% | 7.2% | 8.4% | 0.0% | 67.1% | 1.4% |
| 1993 | 4.1% | 5.4% | 3.2% | 8.9% | 0.0% | 77.3% | 1.1% |
| 1994 | 4.8% | 2.9% | 6.5% | 8.7% | 0.0% | 73.9% | 3.2% |
| 1995 | 4.9% | 5.3% | 4.2% | 4.5% | 0.0% | 79.2% | 1.9% |
| 1996 | 5.0% | 5.0% | 2.1% | 7.1% | 0.0% | 79.4% | 1.3% |
| 1997 | 5.3% | 7.6% | 0.4% | 8.9% | 0.0% | 74.7% | 3.1% |
| 1998 | 2.0% | 2.0% | 1.0% | 6.0% | 22.5% | 65.5% | 1.0% |
| 1999 | 1.9% | 2.4% | 0.0% | 5.8% | 27.9% | 60.1% | 1.9% |
| 2000 | 3.3% | 2.9% | 0.5% | 5.3% | 17.2% | 70.8% | 0.0% |
| 2001 | 7.0% | 0.8% | 0.4% | 3.3% | 30.2% | 57.0% | 1.2% |
| 2002 | 2.3% | 1.1% | 0.4% | 5.4% | 27.6% | 62.1% | 1.1% |
| 2003 | 6.5% | 5.8% | 0.7% | 7.2% | 30.5% | 48.3% | 1.0% |
| 2004 | 7.0% | 5.9% | 0.7% | 4.5% | 27.3% | 51.4% | 3.1% |
| 2005 | 13.4% | 6.9% | 0.0% | 5.7% | 42.5% | 27.5% | 4.0% |
| 2006 | 12.4% | 8.6% | 0.9% | 10.7% | 44.2% | 22.3% | 0.9% |
| 2007 | 11.5% | 6.9% | 0.5% | 20.6% | 34.4% | 21.6% | 4.6% |
| 2008 | 20.9% | 10.3% | 2.3% | 19.8% | 19.0% | 25.5% | 2.3% |
| 2009 | 21.6% | 13.1% | 1.4% | 23.9% | 13.6% | 24.9% | 1.4% |
| 2010 | 10.2% | 7.2% | 1.7% | 25.1% | 20.4% | 34.0% | 1.3% |
| 2011 | 12.1% | 8.3% | 3.4% | 13.6% | 17.5% | 44.7% | 0.5% |
| 2012 | 7.8% | 4.1% | 0.9% | 11.9% | 24.2% | 49.3% | 1.8% |
| 2013 | 11.2% | 7.9% | 0.4% | 12.0% | 28.5% | 36.4% | 3.7% |
| 2014 | 16.0% | 6.0% | 0.4% | 16.8% | 26.4% | 33.2% | 1.2% |
| 2015 | 17.4% | 10.2% | 1.5% | 14.0% | 27.2% | 27.9% | 1.9% |
| 2016 | 18.3% | 9.5% | 0.0% | 12.8% | 31.6% | 26.9% | 0.9% |
| 2017 | 14.8% | 7.4% | 0.2% | 17.1% | 35.8% | 23.7% | 1.0% |
Note: Early symptomatic includes both primary and secondary cases.
Source: Public Health Agency of Canada (2019). Canadian Notifiable Disease Surveillance System.
3.1.2 Infectious syphilis trends in Canada by sex
Figure 9 presents historical infectious syphilis trends by sex since 1991, the year when CNDSS began collecting information on sex at diagnosis. Between 1991 and the early 2000s, infectious syphilis rates were similar among males and females, with males experiencing slightly higher rates. The male-to-female rate ratio in the 1990s ranged from 1:1 to 2:1 (Figure 9). However, starting in 2002, rates among males began to increase more rapidly compared to female rates. By 2012, rates of syphilis were 18 times higher in males compared to females (male-to-female rate ratio of 18:1). This rapid increase was driven mainly by gbMSM cases, as outlined in Section 4 of this report. According to preliminary data, in 2018, there was a major increase in both male and female rates (Figure 9). In that year, the number of female cases nearly tripled from what was observed in 2017, with outbreaks reported in heterosexual populations in several jurisdictions. This increase in the number of female cases resulted in a decrease in the male-to-female rate ratio from 8:1 in 2017 to 4:1 in 2018.
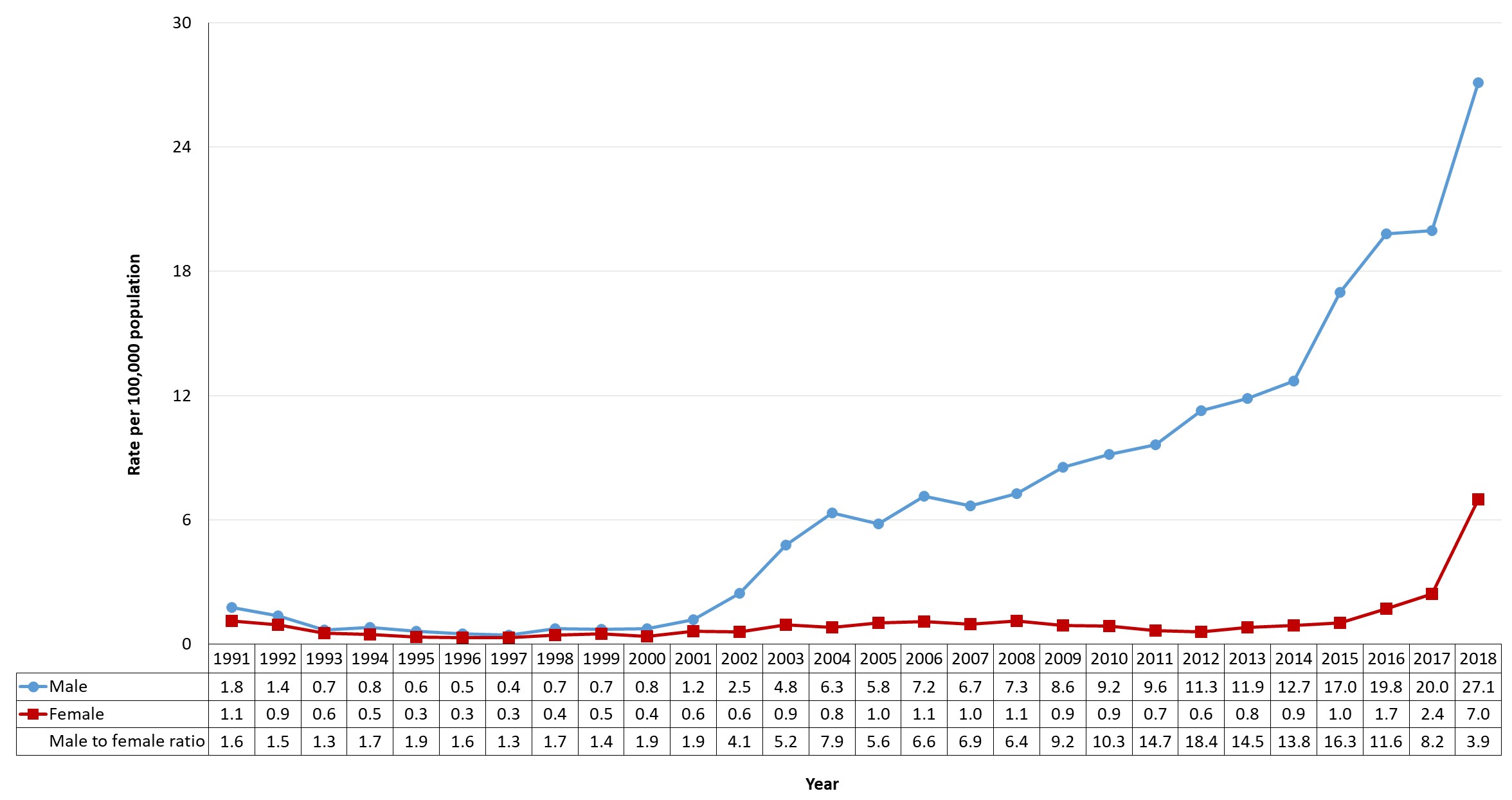
Figure 9 - Text description
This graph displays the rate of reported infectious syphilis cases by sex, between 1991 and 2018 in Canada. The horizontal axis shows the calendar years from 1991 to 2018. The vertical axis shows the rate of infectious syphilis per 100,000 population for males and females. The male to female ratio is presented on the horizontal axis.
| Year | Rate per 100,000 population | ||
|---|---|---|---|
| Male | Female | Male to Female Ratio | |
| 1991 | 1.8 | 1.1 | 1.6 |
| 1992 | 1.4 | 0.9 | 1.5 |
| 1993 | 0.7 | 0.6 | 1.3 |
| 1994 | 0.8 | 0.5 | 1.7 |
| 1995 | 0.6 | 0.3 | 1.9 |
| 1996 | 0.5 | 0.3 | 1.6 |
| 1997 | 0.4 | 0.3 | 1.3 |
| 1998 | 0.7 | 0.4 | 1.7 |
| 1999 | 0.7 | 0.5 | 1.4 |
| 2000 | 0.8 | 0.4 | 1.9 |
| 2001 | 1.2 | 0.6 | 1.9 |
| 2002 | 2.5 | 0.6 | 4.1 |
| 2003 | 4.8 | 0.9 | 5.2 |
| 2004 | 6.3 | 0.8 | 7.9 |
| 2005 | 5.8 | 1.0 | 5.6 |
| 2006 | 7.2 | 1.1 | 6.6 |
| 2007 | 6.7 | 1.0 | 6.9 |
| 2008 | 7.3 | 1.1 | 6.4 |
| 2009 | 8.6 | 0.9 | 9.2 |
| 2010 | 9.2 | 0.9 | 10.3 |
| 2011 | 9.6 | 0.7 | 14.7 |
| 2012 | 11.3 | 0.6 | 18.4 |
| 2013 | 11.9 | 0.8 | 14.5 |
| 2014 | 12.7 | 0.9 | 13.8 |
| 2015 | 17.0 | 1.0 | 16.3 |
| 2016 | 19.8 | 1.7 | 11.6 |
| 2017 | 20.0 | 2.4 | 8.2 |
| 2018 | 27.1 | 7.0 | 3.9 |
Note: Age and Sex data for infectious syphilis began to be reported by PTs in 1991.
Source: Public Health Agency of Canada (2019). Canadian Notifiable Disease Surveillance System. Preliminary 2018 data received directly from provinces and territories.
Between 2008 and 2017, the male-to-female rate ratio was generally higher in Canada than in other OECD countries (Figure 10). The subsequent decrease in male-to-female rate ratio observed in Canada has also been reported in other OECD countries (Figure 10)Footnote 6Footnote 85-87.
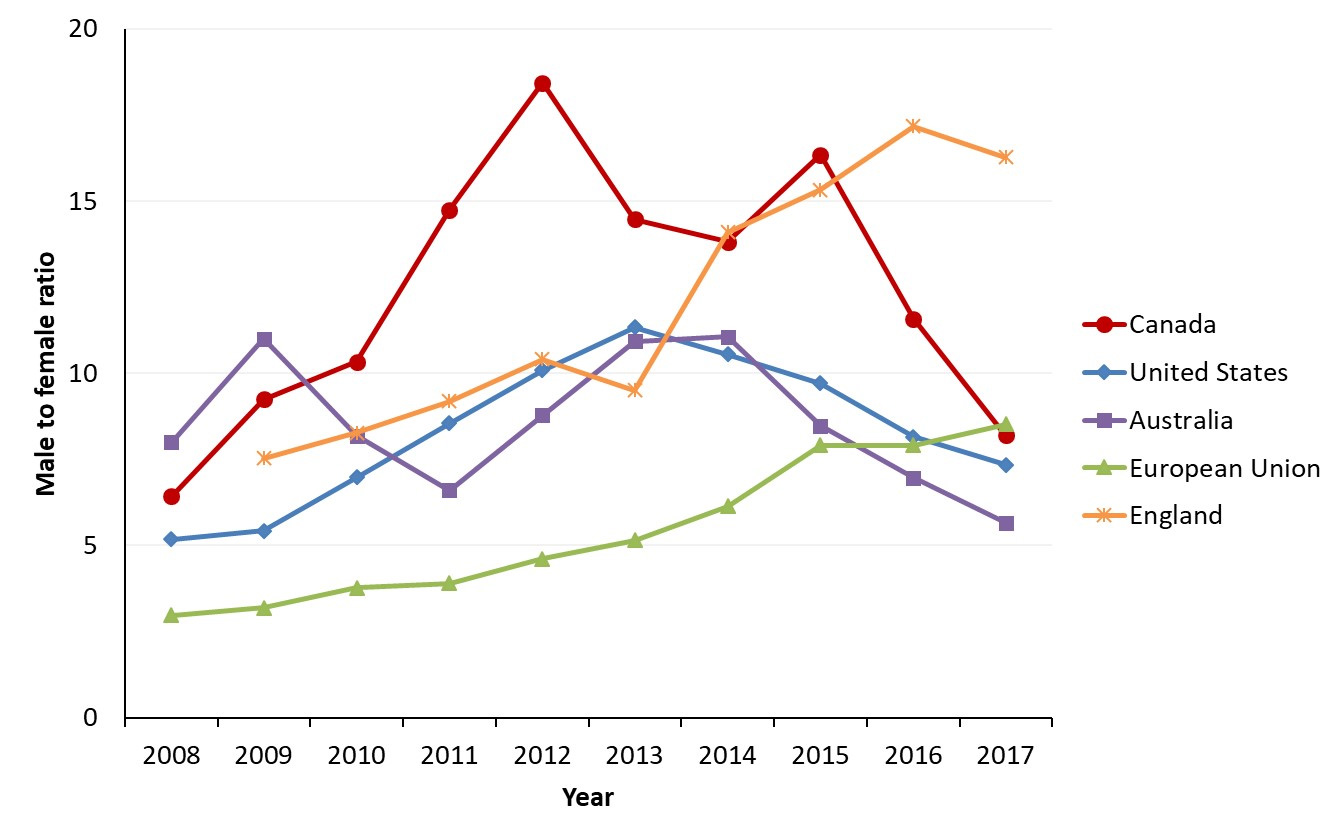
Figure 10 - Text description
This graph displays the reported male to female rate ratios of infectious syphilis of OECD countries and Canada, between 2008 and 2017. The horizontal axis shows the calendar years from 2008 to 2017. The vertical axis shows male to female rate ratios of the US, Australia, the EU, Canada, and England.
| Year | Male to Female Rate Ratios | ||||
|---|---|---|---|---|---|
| Canada | United States | Australia | European Union | England | |
| 2008 | 6.4 | 5.2 | 8.0 | 3.0 | |
| 2009 | 9.2 | 5.4 | 11.0 | 3.2 | 7.5 |
| 2010 | 10.3 | 7.0 | 8.2 | 3.8 | 8.3 |
| 2011 | 14.7 | 8.5 | 6.6 | 3.9 | 9.2 |
| 2012 | 18.4 | 10.1 | 8.8 | 4.6 | 10.4 |
| 2013 | 14.5 | 11.3 | 10.9 | 5.1 | 9.5 |
| 2014 | 13.8 | 10.5 | 11.1 | 6.1 | 14.1 |
| 2015 | 16.3 | 9.7 | 8.5 | 7.9 | 15.3 |
| 2016 | 11.6 | 8.2 | 7.0 | 7.9 | 17.2 |
| 2017 | 8.2 | 7.3 | 5.7 | 8.5 | 16.3 |
Note: Canada’s definition of infectious syphilis includes confirmed cases of primary, secondary and early latent syphilis. Please note that some of the countries presented have slightly different definitions. The US includes confirmed primary and secondary stages only in its definition of infectious syphilis. In addition to confirmed primary, secondary and early latent cases, Australia include probable cases of infectious cases (approximately 9% were reported as such).
The EU includes all cases of syphilis regardless of stage, although of the countries that provided staging information, 95% of cases were reported as either primary, secondary or early latent.
- Footnote b
-
Sources:
- Australia: Kirby Institute. HIV, viral hepatitis and sexually transmissible infections in Australia: annual surveillance report 2018. 2018.
- European Union: European Centre for Disease Prevention and Control (ECDC). Syphilis - Annual epidemiological report for 2017. 2019 12 July 2019.
- United States: Centers for Disease Control and Prevention (CDC). Table 27. Primary and Secondary Syphilis — Reported Cases and Rates of Reported Cases by State/Area and Region in Alphabetical Order, United States and Outlying Areas, 2013–2017. 2018; Accessed September 10, 2019.
- Canada: Government of Canada. Canadian Notifiable Disease Surveillance System. 2018
- England: Public Health England, Official Statistics, Sexually transmitted infections (STIs): annual data tables. Table 1 (b): Rates of new STI diagnoses in England by gender, 2008 – 2017, Rates per 100 000, Syphilis: primary, secondary & early latent – total.
In 2017, Canada’s ratio (8.2) was similar to those observed in the US (7.3) and the EU (8.5), and slightly higher than that of Australia (5.7) (Figure 10). Of countries with available data, England reported the highest male-to-female rate ratio in 2017 (15.7)Footnote 6Footnote 85-87.
Figure 11 presents a comparison of rates of infectious syphilis by sex in selected OECD settings. Rates for both males and females tended to vary among countries. Canada reported higher rates among males compared to the US and the EU, although this should be interpreted with caution, as slightly different case definitions for infectious syphilis are used by each country. In contrast, female rates were higher in Canada than in all countries except Australia (Figure 11)Footnote 6Footnote 85-87.
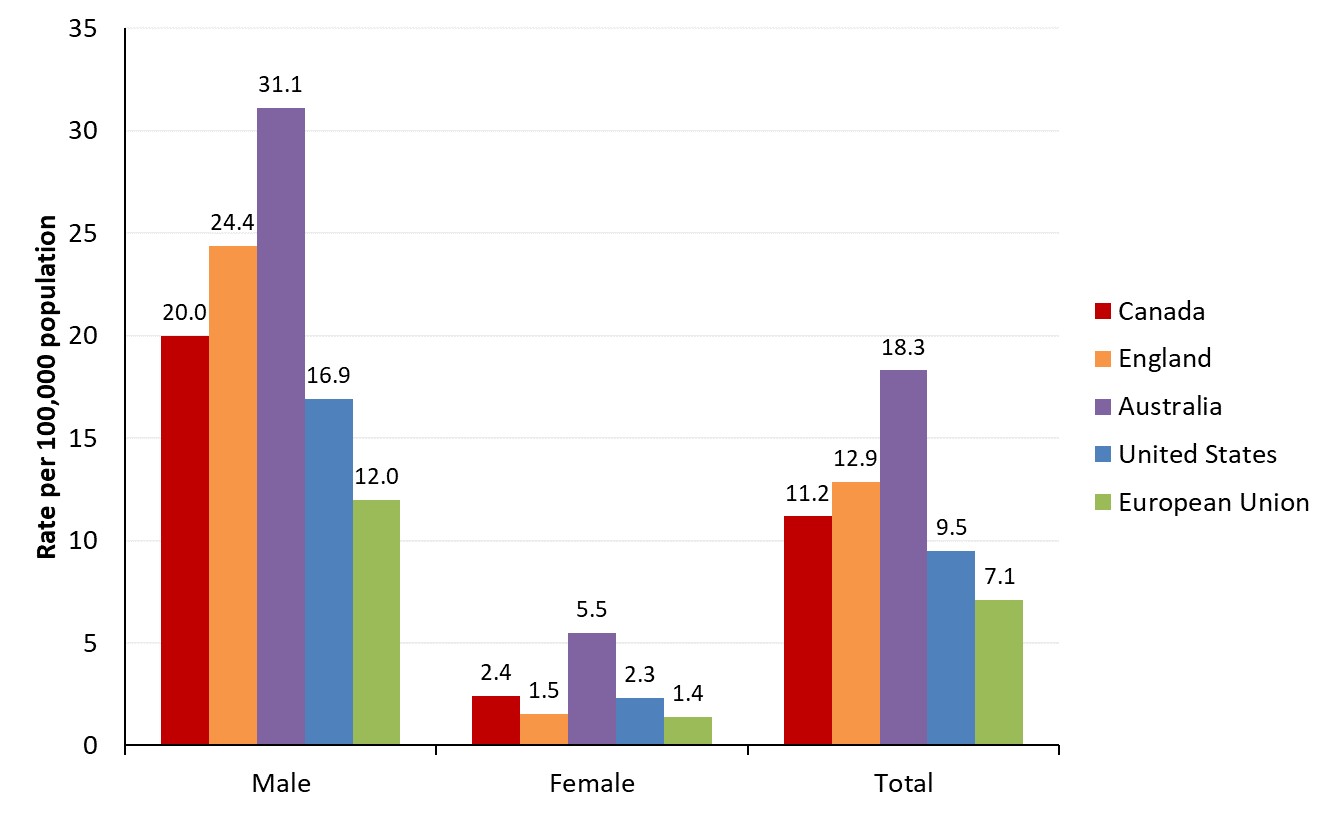
Figure 11 - Text description
This graph displays the reported rates per 100,000 population of infectious syphilis by sex of OECD countries in 2017. The horizontal axis shows the different OECD countries, which include: Canada, England, Australia, US, and the EU. The vertical axis shows the rate per 100,000 population for male, female and the total population per country.
| Country/Region | Rate per 100,000 population | ||
|---|---|---|---|
| Male | Female | Total | |
| Canada | 20.0 | 2.4 | 11.2 |
| England | 24.4 | 1.5 | 12.9 |
| Australia | 31.1 | 5.5 | 18.3 |
| United States | 16.9 | 2.3 | 9.5 |
| European Union | 12.0 | 1.4 | 7.1 |
Note: Canada’s definition of infectious syphilis includes confirmed cases of primary, secondary and early latent syphilis. Please note that some of the countries presented have slightly different definitions. The US includes confirmed primary and secondary stages only in its definition of infectious syphilis. In addition to confirmed primary, secondary and early latent cases, Australia include probable cases of infectious cases (approximately 9% were reported as such).
The EU includes all cases of syphilis regardless of stage, although of the countries that provided staging information, 95% of cases were reported as either primary, secondary or early latent.
- Footnote c
-
Sources:
- Australia: Kirby Institute. HIV, viral hepatitis and sexually transmissible infections in Australia: annual surveillance report 2018. 2018.
- European Union: European Centre for Disease Prevention and Control (ECDC). Syphilis - Annual epidemiological report for 2017. 2019 12 July 2019.
- United States: Centers for Disease Control and Prevention (CDC). Table 27. Primary and Secondary Syphilis — Reported Cases and Rates of Reported Cases by State/Area and Region in Alphabetical Order, United States and Outlying Areas, 2013–2017. 2018; Accessed September 10, 2019.
- Canada: Government of Canada. Canadian Notifiable Disease Surveillance System. 2018
- England: Public Health England, Official Statistics, Sexually transmitted infections (STIs): annual data tables. Table 1 (b): Rates of new STI diagnoses in England by gender, 2008 – 2017, Rates per 100 000, Syphilis: primary, secondary & early latent – total.
3.1.3 Infectious syphilis trends in Canada by age group
Infectious syphilis rates tend to vary by age. Since the 1990s, all age groups, with the exception of those under 15 years of age, have experienced increases in infectious syphilis rates (Figure 12). The largest increase has been observed in the 25 to 29 year age group, closely followed by the 30 to 39 year age group. Rates were also high in the 20 to 24 and 40 to 59 year age groups. The situation was similar in other OECD countries, with the highest rates reported among the 25 to 29 age group in Australia, England and the US (Appendix D).
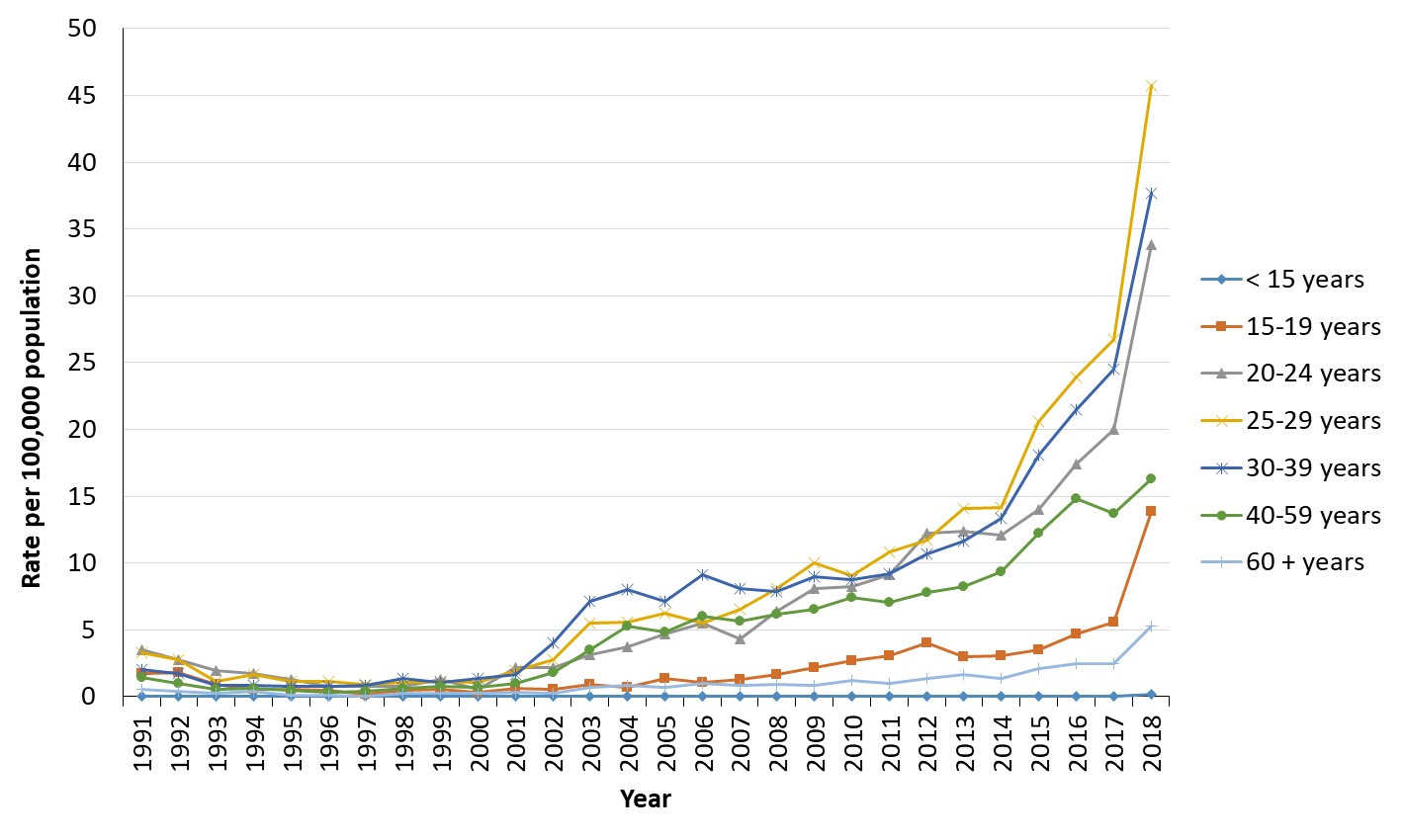
Figure 12 - Text description
This graph displays the reported rates per 100,000 population of infectious syphilis by age group in Canada, between 1991 and 2018. The horizontal axis shows the calendar years from 1991 to 2018. The vertical axis shows the rate per 100,000 population for age groups less than 15 years of age, 15 to 19 years of age, 20 to 24 years of age, 25 to 29 years of age, 30 to 39 years of age, 40 to 59 years of age, and those aged 60 and older.
| Year | Rate per 100,000 population | ||||||
|---|---|---|---|---|---|---|---|
| < 15 years | 15-19 years | 20-24 years | 25-29 years | 30-39 years | 40-59 years | 60 + years | |
| 1991 | 0.0 | 1.7 | 3.5 | 3.3 | 2.0 | 1.4 | 0.6 |
| 1992 | 0.0 | 1.8 | 2.8 | 2.8 | 1.7 | 1.0 | 0.4 |
| 1993 | 0.0 | 0.9 | 2.0 | 1.1 | 0.9 | 0.6 | 0.3 |
| 1994 | 0.0 | 0.6 | 1.7 | 1.6 | 0.9 | 0.6 | 0.4 |
| 1995 | 0.0 | 0.6 | 1.3 | 1.1 | 0.8 | 0.5 | 0.1 |
| 1996 | 0.0 | 0.5 | 0.8 | 1.1 | 0.8 | 0.3 | 0.1 |
| 1997 | 0.0 | 0.1 | 0.8 | 0.9 | 0.9 | 0.4 | 0.0 |
| 1998 | 0.0 | 0.4 | 0.7 | 1.1 | 1.3 | 0.6 | 0.3 |
| 1999 | 0.0 | 0.5 | 1.3 | 1.1 | 1.1 | 0.8 | 0.3 |
| 2000 | 0.0 | 0.3 | 0.5 | 1.1 | 1.3 | 0.7 | 0.3 |
| 2001 | 0.0 | 0.6 | 2.2 | 1.9 | 1.7 | 1.0 | 0.3 |
| 2002 | 0.0 | 0.6 | 2.1 | 2.7 | 4.0 | 1.8 | 0.2 |
| 2003 | 0.0 | 0.9 | 3.2 | 5.5 | 7.1 | 3.5 | 0.7 |
| 2004 | 0.0 | 0.7 | 3.8 | 5.6 | 8.0 | 5.3 | 0.8 |
| 2005 | 0.0 | 1.4 | 4.7 | 6.3 | 7.1 | 4.8 | 0.7 |
| 2006 | 0.0 | 1.1 | 5.5 | 5.5 | 9.1 | 6.0 | 1.0 |
| 2007 | 0.1 | 1.3 | 4.3 | 6.6 | 8.1 | 5.6 | 0.8 |
| 2008 | 0.0 | 1.6 | 6.4 | 8.1 | 7.9 | 6.2 | 0.9 |
| 2009 | 0.0 | 2.2 | 8.1 | 10.0 | 9.0 | 6.5 | 0.8 |
| 2010 | 0.0 | 2.7 | 8.2 | 9.0 | 8.7 | 7.4 | 1.2 |
| 2011 | 0.0 | 3.1 | 9.1 | 10.9 | 9.2 | 7.0 | 1.0 |
| 2012 | 0.0 | 4.0 | 12.2 | 11.7 | 10.7 | 7.8 | 1.4 |
| 2013 | 0.0 | 3.0 | 12.4 | 14.1 | 11.6 | 8.2 | 1.6 |
| 2014 | 0.0 | 3.1 | 12.1 | 14.1 | 13.3 | 9.3 | 1.4 |
| 2015 | 0.0 | 3.5 | 14.0 | 20.6 | 18.0 | 12.3 | 2.1 |
| 2016 | 0.0 | 4.7 | 17.4 | 23.9 | 21.5 | 14.9 | 2.5 |
| 2017 | 0.1 | 5.6 | 20.0 | 26.7 | 24.5 | 13.7 | 2.5 |
| 2018 | 0.2 | 13.9 | 33.8 | 45.7 | 37.7 | 16.3 | 5.3 |
Note: Age and sex data for infectious syphilis reporting by PTs began in 1991.
Source: Public Health Agency of Canada (2019). Canadian Notifiable Disease Surveillance System. Preliminary 2018 data received directly from provinces and territories.
The number of cases of syphilis has been low in those younger than 15 years of age. Since 1991, only 125 cases of syphilis were reported among those aged 15 years and younger. These cases were distributed almost equally among males and females. Only 14.4% (18 cases) of these 125 cases were infectious; 45 cases (36%) were congenital cases; four cases were non-infectious (3%); and 58 (46%) were of unspecified status. The large proportion of unspecified cases highlights the difficulty of obtaining staging information on syphilis cases that may be a result of congenital acquisition, sexual abuse or early sexual activity.
There was a large increase in rates for all age groups in 2018, compared to previous years (Figure 12). When examining infectious rates among males between 2009 and 2018, the largest increases were observed among those in the 60+, the 25 to 29, and the 30 to 39 year age groups, with increases of 551%, 284% and 270%, respectively (Figure 13). In comparison, the largest increases in infectious rates among females were observed in the 15 to 19, the 30 to 39 and the 25 to 29 year age groups, with an increase of 1768%, 793% and 740%, respectively (Figure 14). In 2018, infectious syphilis rates for males were highest among the 25 to 29 and 30 to 39 year age group (65.1 and 60.6 per 100,000 respectively) while among females the rates were highest among the 20 to 24 and 25 to 29 year age groups (with rates of 26.4 and 24.7 per 100,000, respectively). Detailed rates of infectious syphilis by age group and sex from 2009 to 2018 are presented in Appendix F.
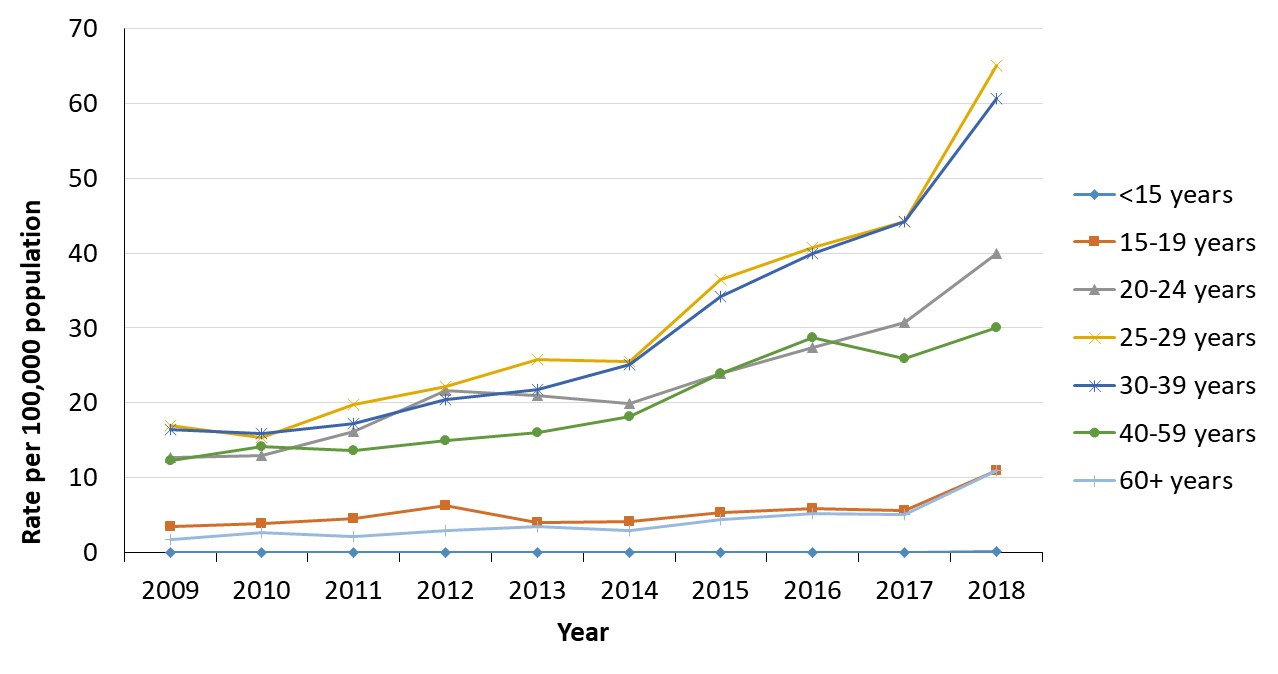
Figure 13 - Text description
This graph displays the reported rates per 100,000 population of infectious syphilis by age group in males in Canada, between the years 2009 and 2018. The horizontal axis shows the calendar years from 2009 to 2018. The vertical axis shows the rate per 100,000 population for males in age groups less than 15 years of age, 15 to 19 years of age, 20 to 24 years of age, 25 to 29 years of age, 30 to 39 years of age, 40 to 59 years of age, and those aged 60 and older.
| Year | Rate per 100,000 population | ||||||
|---|---|---|---|---|---|---|---|
| < 15 years | 15-19 years | 20-24 years | 25-29 years | 30-39 years | 40-59 years | 60 + years | |
| 2009 | 0.0 | 3.4 | 12.7 | 17.0 | 16.4 | 12.3 | 1.7 |
| 2010 | 0.0 | 3.9 | 12.9 | 15.4 | 15.9 | 14.2 | 2.6 |
| 2011 | 0.0 | 4.5 | 16.1 | 19.8 | 17.3 | 13.6 | 2.1 |
| 2012 | 0.0 | 6.3 | 21.6 | 22.2 | 20.5 | 15.0 | 2.9 |
| 2013 | 0.0 | 4.0 | 20.9 | 25.7 | 21.8 | 16.0 | 3.4 |
| 2014 | 0.0 | 4.1 | 19.9 | 25.5 | 25.0 | 18.1 | 2.9 |
| 2015 | 0.0 | 5.3 | 23.9 | 36.5 | 34.2 | 24.0 | 4.4 |
| 2016 | 0.0 | 5.9 | 27.4 | 40.8 | 39.9 | 28.7 | 5.2 |
| 2017 | 0.0 | 5.6 | 30.7 | 44.2 | 44.2 | 26.0 | 5.1 |
| 2018 | 0.1 | 11.0 | 40.0 | 65.1 | 60.0 | 30.0 | 10.9 |
Source: Public Health Agency of Canada (2019). Canadian Notifiable Disease Surveillance System Preliminary 2018 data received directly from provinces and territories.
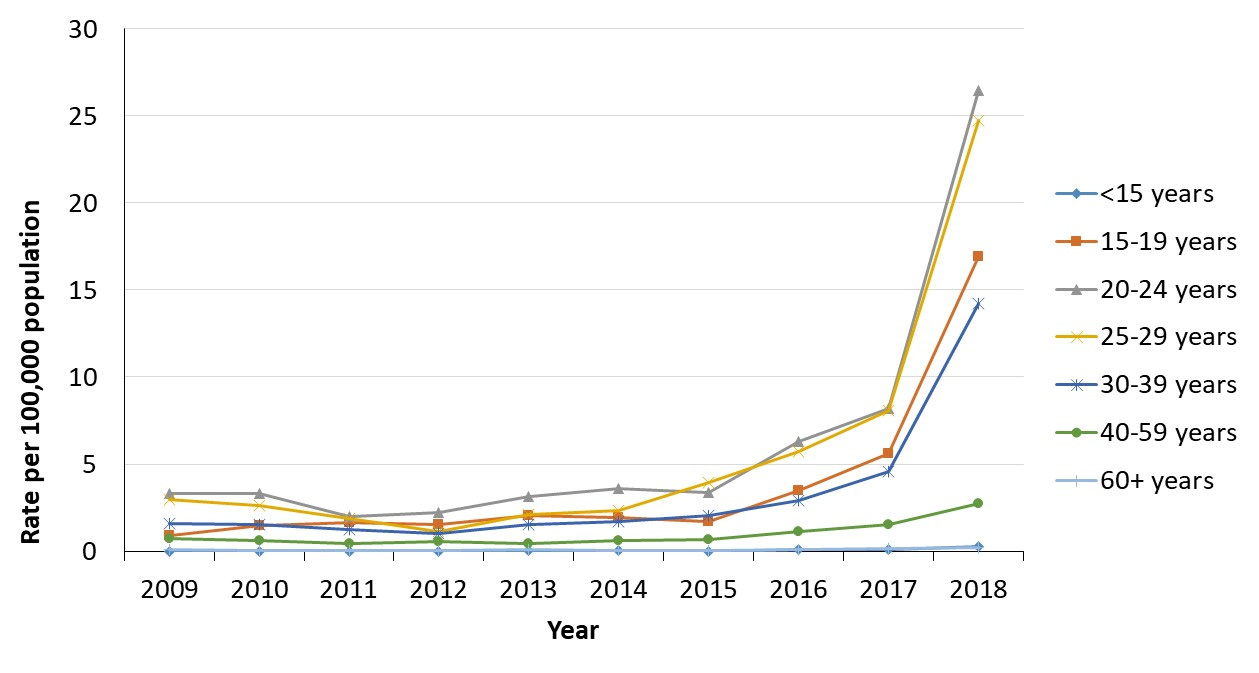
Figure 14 - Text description
This graph displays the reported rates per 100,000 population of infectious syphilis by age group in females in Canada, between the years 2009 and 2018. The horizontal axis shows the calendar years from 2009 to 2018. The vertical axis shows the rate per 100,000 population for females in age groups less than 15 years of age, 15 to 19 years of age, 20 to 24 years of age, 25 to 29 years of age, 30 to 39 years of age, 40 to 59 years of age, and those aged 60 and older.
| Year | Rate per 100,000 population | ||||||
|---|---|---|---|---|---|---|---|
| < 15 years | 15-19 years | 20-24 years | 25-29 years | 30-39 years | 40-59 years | 60 + years | |
| 2009 | 0.0 | 0.9 | 3.3 | 2.9 | 1.6 | 0.7 | 0.1 |
| 2010 | 0.0 | 1.5 | 3.3 | 2.6 | 1.5 | 0.6 | 0.1 |
| 2011 | 0.0 | 1.7 | 2.0 | 1.9 | 1.2 | 0.4 | 0.0 |
| 2012 | 0.0 | 1.5 | 2.2 | 1.1 | 1.0 | 0.5 | 0.0 |
| 2013 | 0.0 | 2.0 | 3.1 | 2.1 | 1.5 | 0.4 | 0.1 |
| 2014 | 0.0 | 2.0 | 3.6 | 2.4 | 1.7 | 0.6 | 0.0 |
| 2015 | 0.0 | 1.7 | 3.4 | 3.9 | 2.0 | 0.6 | 0.0 |
| 2016 | 0.1 | 3.5 | 6.3 | 5.7 | 2.9 | 1.1 | 0.1 |
| 2017 | 0.1 | 5.6 | 8.2 | 8.1 | 4.5 | 1.5 | 0.1 |
| 2018 | 0.3 | 16.9 | 26.4 | 24.7 | 14.2 | 2.7 | 0.2 |
Source: Public Health Agency of Canada (2019). Canadian Notifiable Disease Surveillance System. Preliminary 2018 data received directly from provinces and territories.
On average, male infectious syphilis cases tend to be older than female cases. In 2018, the proportion of infectious syphilis cases observed among females tended to decrease as age increased (Figure 15). Over half of the infectious syphilis cases (59%) in the 15-19 year age group were female, whereas only 2% of cases among those 60 years and above were female (Figure 15).
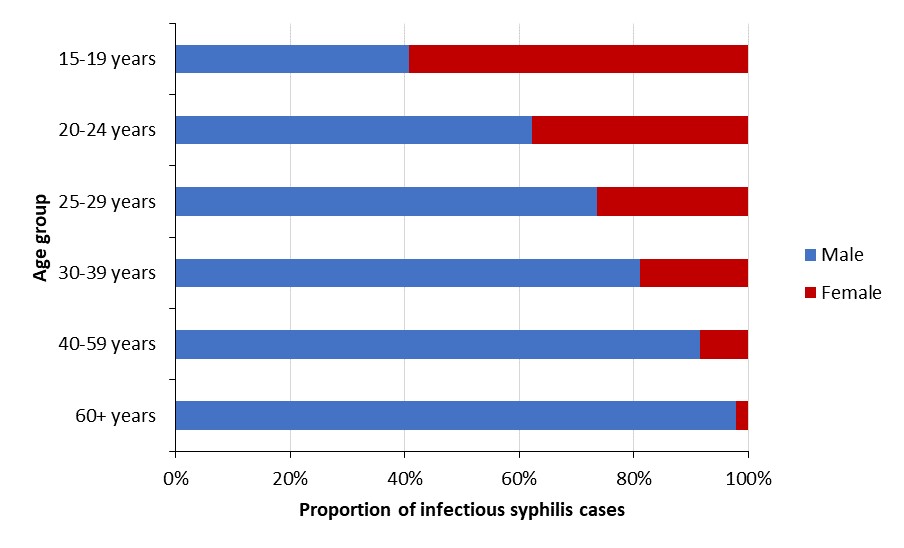
Figure 15 - Text description
This graph displays the proportion of reported infectious syphilis cases by age group and sex in Canada in 2018. The horizontal axis shows the age groups: 15 to 19 years of age, 20 to 24 years of age, 25 to 29 years of age, 30 to 39 years of age, 40 to 59 years of age, and those aged 60 and older. The vertical axis shows the proportion of infectious syphilis cases for males and females.
| Age Group | Proportion of infectious syphilis cases | |
|---|---|---|
| Male | Female | |
| 15-19 years | 40.7% | 59.3% |
| 20-24 years | 62.3% | 37.7% |
| 25-29 years | 73.6% | 26.4% |
| 30-39 years | 81.1% | 18.9% |
| 40-59 years | 91.6% | 8.5% |
| 60+ years | 97.8% | 2.2% |
Source: Preliminary 2018 data received directly from provinces and territories.
Key messages
- From the 1940s onwards, rates of infectious syphilis remained high in Canada. Then, after decades of high syphilis rates in Canada, rates of infectious syphilis began to decrease in the 1980s, and they remained low for most of the 1990s before beginning to climb again in the early 2000s.
- Similar increases were observed in other countries from the OECD.
- Syphilis mostly affects men, especially gbMSM. However, there has been a sharp increase in the number of female cases observed in recent years.
- Since the 1990s, all age groups with the exception of those under 15 years of age have experienced increases in infectious syphilis rates. The largest increases have been observed in the 25 to 29 year age group, closely followed by the 30 to 39 year age group.
- On average, male infectious syphilis cases tend to be older than their female counterparts.
3.2 Current epidemiological situation across provinces and territories
In Section 3.1, an overview of national syphilis data is presented. However, syphilis trends vary across the provinces and territories. In this section, rates of infectious syphilis reported to the CNDSS by provinces and territories from 2008 to 2017 are reported (detailed rates are presented in Appendix G). In addition, this section also features preliminary 2018 data sent to PHAC directly by the PTs and more recent numbers reported in provincial and territorial surveillance reports and media releases.
3.2.1 Overview of provincial and territorial rates
Figure 16 shows the most recent rates for PTs in CNDSS (2017), while Figure 17 presents preliminary data reported by the PTs in 2018. From 2017 to 2018, all provinces and territories reported increases in rates, with the exception of Newfoundland and Labrador and Prince Edward Island.
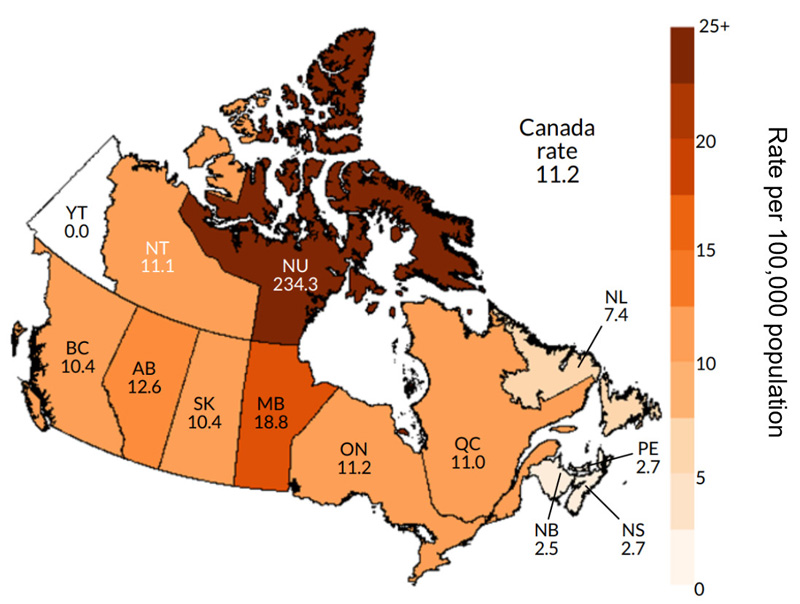
Figure 16 - Text description
This map displays the rates of reported infectious syphilis per 100,000 population by province and territory as well as the overall rate in Canada in 2017.
| Province/Territory | Rate per 100,000 population |
|---|---|
| BC | 10.4 |
| AB | 12.6 |
| SK | 10.4 |
| MB | 18.8 |
| ON | 11.2 |
| QC | 11.0 |
| NB | 2.5 |
| NS | 2.7 |
| PE | 2.7 |
| NL | 7.4 |
| NU | 234.3 |
| NT | 11.1 |
| YT | 0.0 |
| Canada | 11.2 |
Source: Public Health Agency of Canada (2019). Canadian Notifiable Disease Surveillance System.
In 2017 and 2018, the highest rates of infectious syphilis were observed in Nunavut, followed by Manitoba and Alberta. The younger age structure of Nunavut might explain the higher infectious syphilis rates, as rates are usually higher in young adults. In order to test this hypothesis, a standardization by age was performed to assess the effect of the population age distribution on infectious syphilis rates. However, even after age-standardizing rates using the 2011 Canadian population as the reference population (for those 15 years of age and above), Nunavut’s standardized rates remained the highest in the country (249.3 per 100,000 in 2017) (Appendix F). For other PTs, crude rates and age-standardized rates were largely similar.
According to preliminary 2018 data, rates of infectious syphilis in the PTs ranged from 2.6 per 100,000 population in Prince Edward Island to 260.6 per 100,000 per population in Nunavut (Figure 17). Northwest Territories rate more than doubled from 11.1 per 100,000 in 2017 to 24.7 per 100,000 in 2018. While there were no cases of infectious syphilis reported in 2017 in Yukon, its reported rate of infectious syphilis was 4.9 per 100,000 in 2018. Other provinces that have shown an increase in rates were British Columbia, Saskatchewan, Ontario and Nova Scotia. The other Atlantic provinces and Quebec remained relatively stable from 2017 to 2018.
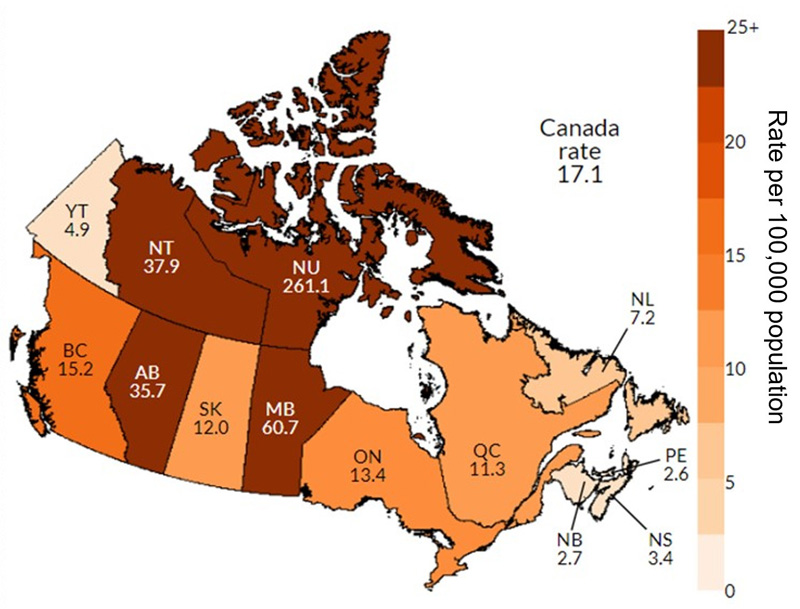
Figure 17 - Text description
This map displays the preliminary data rates of reported infectious syphilis per 100,000 population by province and territory as well as the overall rate in Canada in 2018.
| Province/Territory | Rate per 100,000 population |
|---|---|
| BC | 15.2 |
| AB | 35.7 |
| SK | 12.0 |
| MB | 60.7 |
| ON | 13.4 |
| QC | 11.3 |
| NB | 2.7 |
| NS | 3.4 |
| PE | 2.6 |
| NL | 7.2 |
| NU | 261.1 |
| NT | 37.9 |
| YT | 4.9 |
| Canada | 17.1 |
Source: Preliminary 2018 data received directly from provinces and territories.
However, most PTs experienced increases in crude rates of infectious syphilis between 2014 and 2018 (Figure 18). The overall percentage change from 2014 to 2018 in Canada was a 153% increase in rates. PTs with the highest increases in rates were Alberta (835%), Northwest Territories (735%), Manitoba (560%), and Saskatchewan (378%). In 2018 and 2019, eight PTs (British Columbia, Alberta, Saskatchewan, Manitoba, Ontario, Quebec, Northwest Territories and Nunavut) were experiencing jurisdiction-wide or regional syphilis outbreaks due to high increases in rates in the general population, new or increased number of congenital syphilis cases and shifts in populations affected. Nova Scotia declared a syphilis outbreak in January 2020Footnote 89.
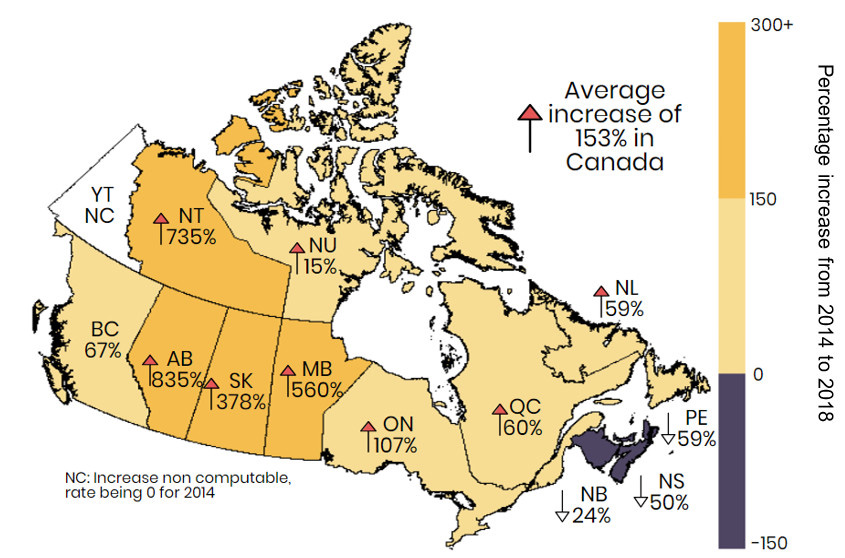
Figure 18 - Text description
This map displays the percent changes of infectious syphilis rates per 100, 000 population by province and territory, as well as the overall average increase in Canada between 2014 and 2018.
| Province/Territory | Percent change from 2014 to 2018 (%) |
|---|---|
| BC | 67% |
| AB | 835% |
| SK | 378% |
| MB | 560% |
| ON | 107% |
| QC | 60% |
| NB | -24% |
| NS | -50% |
| PE | -59% |
| NL | 59% |
| NU | 15% |
| NT | 735% |
| YT | NC |
| Canada | 153% |
| NC: Increase non computable, rate being 0 for 2014 | |
Source: Public Health Agency of Canada (2019). Canadian Notifiable Disease Surveillance System. Preliminary 2018 data received directly from provinces and territories.
Provincial and territorial infectious syphilis rates for 2014 to 2018, including the associated percentage change are presented in Appendix G.
Overall, relative increases in rates from 2014 to 2018 were generally lower in males (Figure 19) than in females, except for Nunavut (Figure 20). In provinces experiencing a decrease in rates of infectious syphilis, this decrease was less pronounced in females than in males.
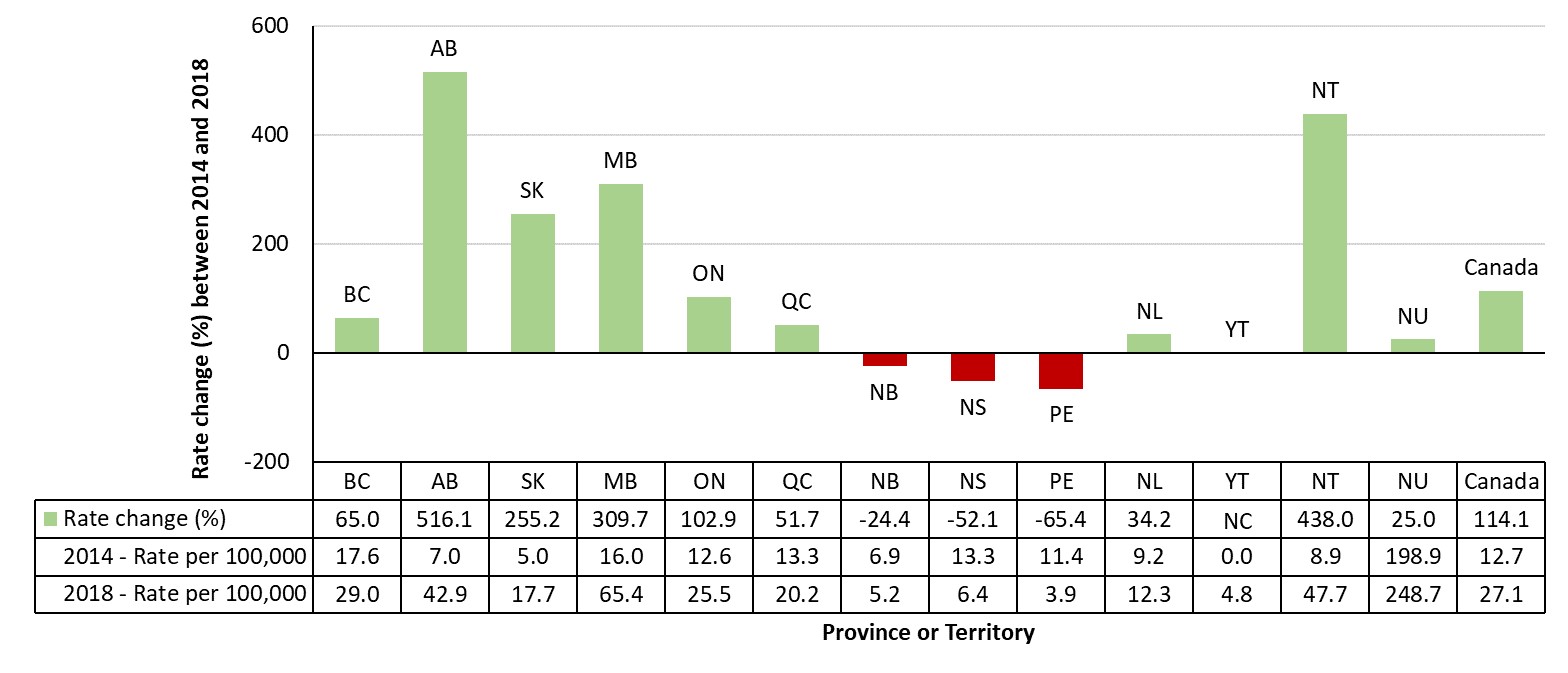
Figure 19 - Text description
This graph displays the percent change in infectious syphilis rates for males by provinces and territories, between 2014 and 2018 in Canada. The horizontal axis shows all provinces and territories of Canada while the vertical axis displays the percent rate change of infectious syphilis between the years 2014 and 2018 for males. The data table presents rates per 100,000 population for each province and territory for 2014 and 2018, as well as the relative percent rate change from 2014 to 2018.
| Rate change | Rate change (%) between 2014 and 2018 | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BC | AB | SK | MB | ON | QC | NB | NS | PE | NL | YT | NT | NU | Canada | |
| Rate change (%) | 65.0 | 516.1 | 255.2 | 309.7 | 102.9 | 51.7 | -24.4 | -52.1 | -65.4 | 34.2 | NC | 438.0 | 25.0 | 114.1 |
| 2014-rate per 100,000 | 17.6 | 7.0 | 5.0 | 16.0 | 12.6 | 13.3 | 6.9 | 13.3 | 11.4 | 9.2 | 0.0 | 8.9 | 198.9 | 12.7 |
| 2018- rate per 100,000 | 29.0 | 42.9 | 17.7 | 65.4 | 25.5 | 20.2 | 5.2 | 6.4 | 3.9 | 12.3 | 4.8 | 47.7 | 248.7 | 27.1 |
Source: Public Health Agency of Canada (2019). Canadian Notifiable Disease Surveillance System. Preliminary 2018 data received directly from provinces and territories.
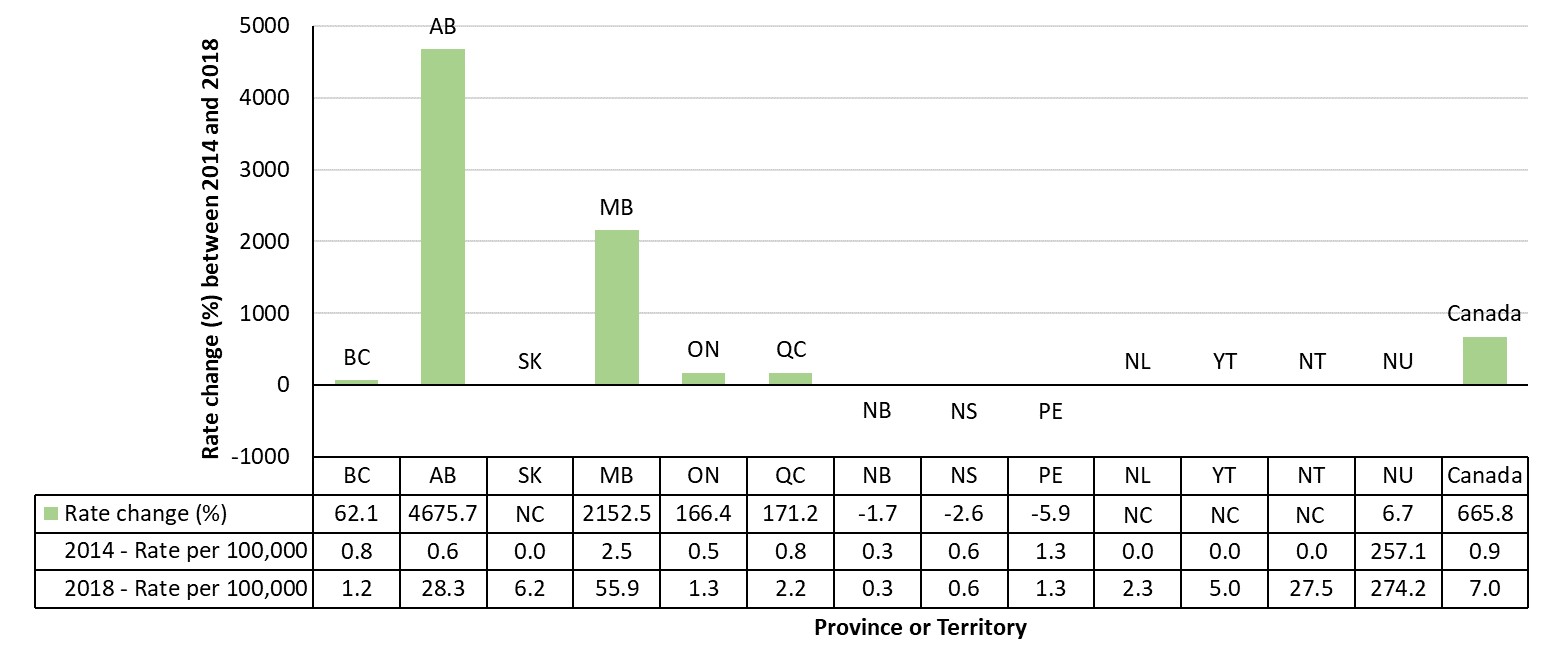
Figure 20 - Text description
This graph displays the percent change in infectious syphilis rates for females by provinces and territories, between 2014 and 2018 in Canada. The horizontal axis shows all provinces and territories of Canada while the vertical axis displays the percent rate change of infectious syphilis between the years 2014 and 2018 for females. The data table presents the rates per 100,000 population for each province and territory for 2014 and 2018, as well as the relative percent rate change from 2014 to 2018.
| Rate change | Rate change (%) between 2014 and 2018 | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BC | AB | SK | MB | ON | QC | NB | NS | PE | NL | YT | NT | NU | Canada | |
| Rate change (%) | 62.1 | 4,675.7 | NC | 2,152.5 | 166.4 | 171.2 | -1.7 | -2.6 | -5.9 | NC | NC | NC | 6.7 | 665.8 |
| 2014-rate per 100,000 | 0.8 | 0.6 | 0.0 | 2.5 | 0.5 | 0.8 | 0.3 | 0.6 | 1.3 | 0.0 | 0.0 | 0.0 | 257.1 | 0.9 |
| 2018- rate per 100,000 | 1.2 | 28.3 | 6.2 | 55.9 | 1.3 | 2.2 | 0.3 | 0.6 | 1.3 | 2.3 | 5.0 | 27.5 | 274.2 | 7.0 |
Source: Public Health Agency of Canada (2019). Canadian Notifiable Disease Surveillance System. Preliminary 2018 data received directly from provinces and territories.
From 2014 to 2018, almost every PT reported increases in the proportion of females, with an overall increase of 204% in Canada (Figure 21). The highest increase in the proportion of females was seen in Alberta and Manitoba, with a 416% and 240% increases, respectively. Both jurisdictions have recently reported heterosexual population outbreaks.
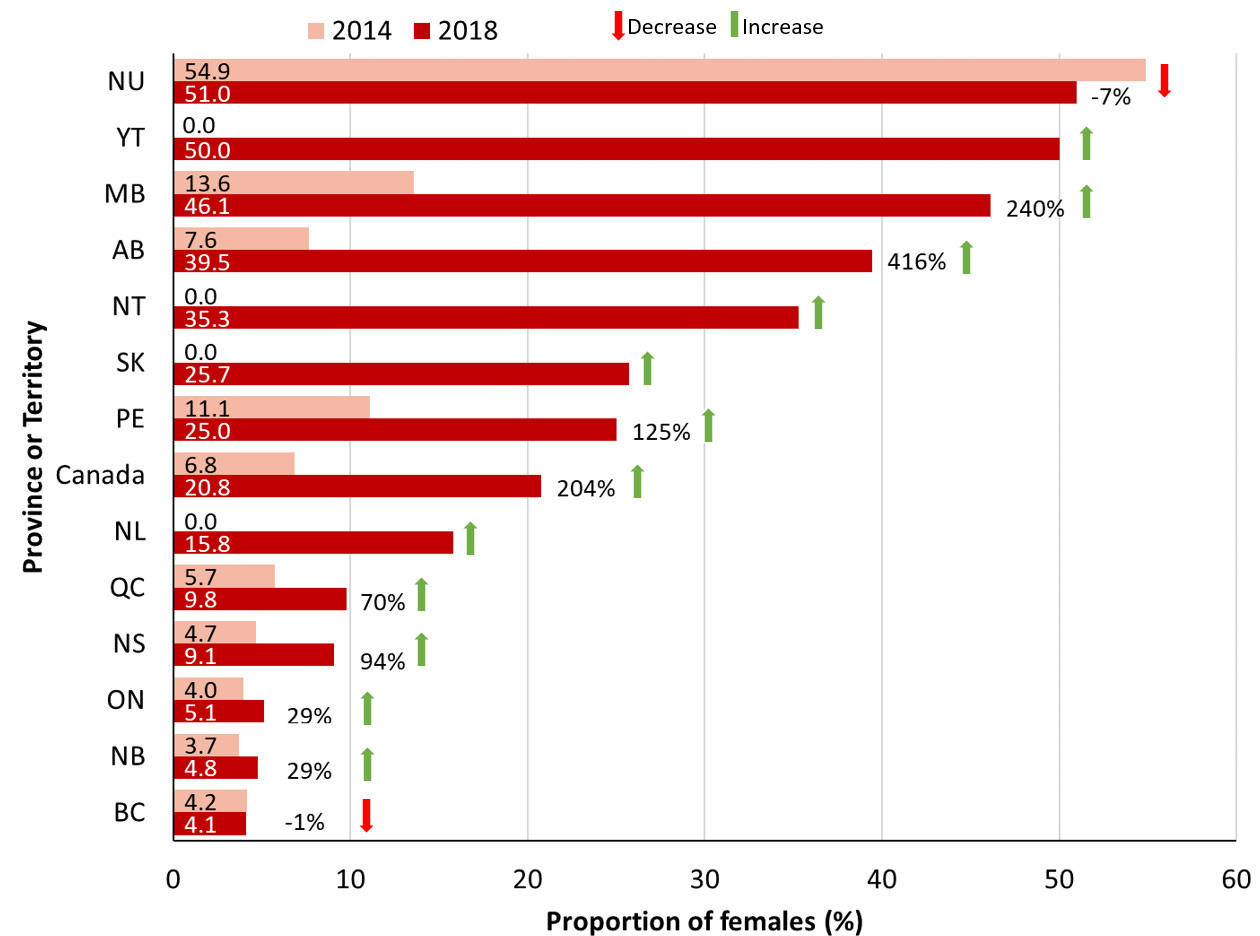
Figure 21 - Text description
This graph displays the proportion of female cases in 2014 and 2018 and percent changes of that proportion by province and territory in Canada, between 2014 and 2018. The vertical axis shows provinces and territories in Canada, as well as Canada as a whole. The horizontal axis displays the proportion of female cases for the years 2014 and 2018 as well as the percent change in proportions for those years.
| Province or Territory | 2014 | 2018 | % Change |
|---|---|---|---|
| NU | 54.9 | 51.0 | -7% |
| YT | 0.0 | 50.0 | N/A |
| MB | 13.6 | 46.1 | 240% |
| AB | 7.6 | 39.5 | 416% |
| NT | 0.0 | 35.3 | N/A |
| SK | 0.0 | 25.7 | N/A |
| PE | 11.1 | 25.0 | 125% |
| Canada | 6.8 | 20.8 | 204% |
| NL | 0.0 | 15.8 | N/A |
| QC | 5.7 | 9.8 | 70% |
| NS | 4.7 | 9.1 | 94% |
| ON | 4.0 | 5.1 | 29% |
| NB | 3.7 | 4.8 | 29% |
| BC | 4.2 | 4.1 | -1% |
Note: Non applicable, the number of female cases in YT, NT, SK and NL being 0 in 2014
Source: Public Health Agency of Canada (2019). Canadian Notifiable Disease Surveillance System. Preliminary 2018 data received directly from provinces and territories.
Key messages
- Between 2014 and 2018, most provinces and territories experienced increases in their infectious syphilis rates.
- In 2017 and 2018, the highest rates of infectious syphilis were observed in Nunavut, followed by Manitoba and Alberta.
- Other provinces that have reported increases in rates were British Columbia, Saskatchewan, Ontario and Nova Scotia. Quebec and the other Atlantic provinces remained relatively stable from 2017 to 2018.
- In 2018, large increases in the proportion of female cases were observed, especially in Alberta and Manitoba, with 415% and 239% increases, respectively. Both jurisdictions have recently reported outbreaks in the heterosexual population.
The next section presents the latest surveillance data and epidemiological information by PT.
3.2.2 Pacific Region: British Columbia
Figure 22 presents the overall rate of infectious syphilis per 100,000 population in British Columbia, between 1979 and 2018. Following a period of high rates up until the late 1980s, rates decreased and remained low in the early 1990s, and then began climbing again in the late 1990s.
Barring a dip between 2009 and 2010, rates have increased since the late 1990s. In 2015, British Columbia experienced its highest rate of infectious syphilis since 1971 (12.7 per 100,000, 608 cases). In 2017, 510 cases of infectious syphilis were reported to CNDSS, corresponding to a rate of 10.4 per 100,000 population. In 2018, 919 cases of infectious syphilis were reported by the British Columbia Centre for Disease Control (BCCDC), corresponding to a rate of 18.4 per 100,000 population and a 33% increase from 2017Footnote 90. These are the highest rates of infectious syphilis reported in the region for the last 30 years.
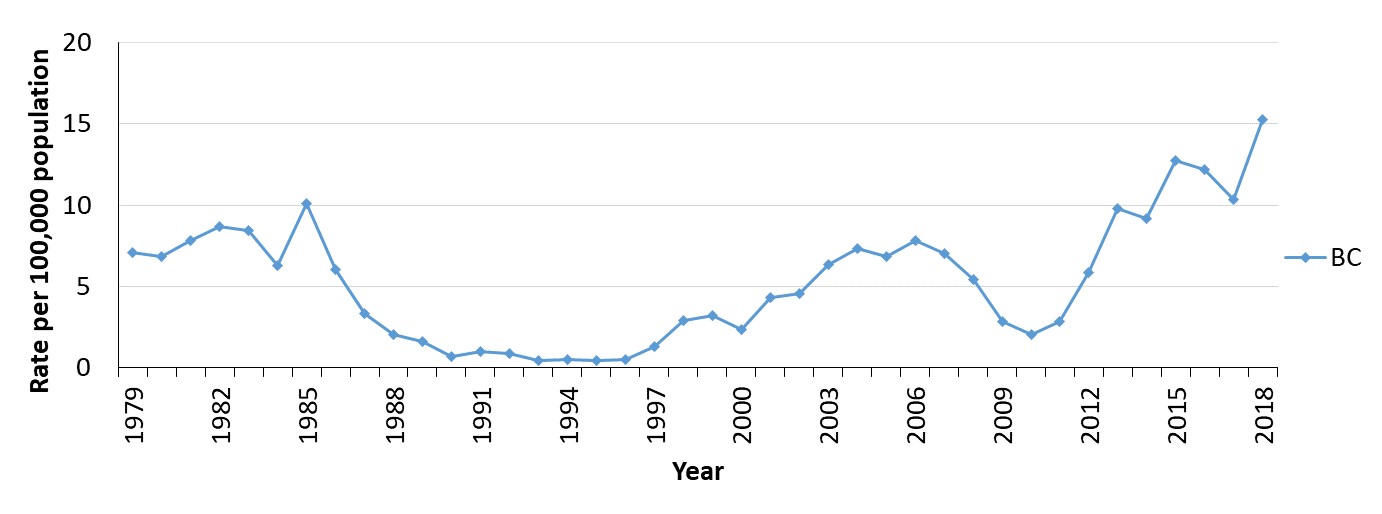
Figure 22 - Text description
This graph displays the rate of reported infectious syphilis cases per 100,000 population in British Columbia, between 1979 and 2018. The horizontal axis shows the calendar years from 1979 to 2018. The vertical axis shows the rate of infectious syphilis per 100,000 population per each calendar year.
| Year | Rate per 100,000 population |
|---|---|
| 1979 | 7.1 |
| 1980 | 6.8 |
| 1981 | 7.8 |
| 1982 | 8.7 |
| 1983 | 8.5 |
| 1984 | 6.3 |
| 1985 | 10.1 |
| 1986 | 6.1 |
| 1987 | 3.3 |
| 1988 | 2.1 |
| 1989 | 1.6 |
| 1990 | 0.7 |
| 1991 | 1.0 |
| 1992 | 0.9 |
| 1993 | 0.4 |
| 1994 | 0.5 |
| 1995 | 0.5 |
| 1996 | 0.5 |
| 1997 | 1.3 |
| 1998 | 2.9 |
| 1999 | 3.2 |
| 2000 | 2.4 |
| 2001 | 4.3 |
| 2002 | 4.5 |
| 2003 | 6.4 |
| 2004 | 7.3 |
| 2005 | 6.9 |
| 2006 | 7.8 |
| 2007 | 7.0 |
| 2008 | 5.4 |
| 2009 | 2.9 |
| 2010 | 2.1 |
| 2011 | 2.8 |
| 2012 | 5.8 |
| 2013 | 9.8 |
| 2014 | 9.2 |
| 2015 | 12.7 |
| 2016 | 12.2 |
| 2017 | 10.4 |
| 2018 | 15.2 |
Source: Public Health Agency of Canada (2019). Canadian Notifiable Disease Surveillance System. Preliminary 2018 data received directly from provinces and territories.
From 2009 to 2018, rates of reported infectious syphilis cases in British Columbia were substantially higher among males than females (Figure 23). Rates among males increased by 437% between 2009 and 2018 (from 5.4 to 29.0 per 100,000 population), while rates among females increased by 300% (from 0.3 to 1.2 per 100,000 population). In 2018, the rate of infectious syphilis was 24.2 times higher in males compared to females. This male-to-female ratio was much higher than the observed 2018 Canadian average of 3.9:1 (Figure 9). While there were only 16 cases of infectious syphilis reported among females in British Columbia in 2017, there were 54 cases reported among females in 2018, accounting for 6% of the province’s total number of infectious syphilis casesFootnote 91.
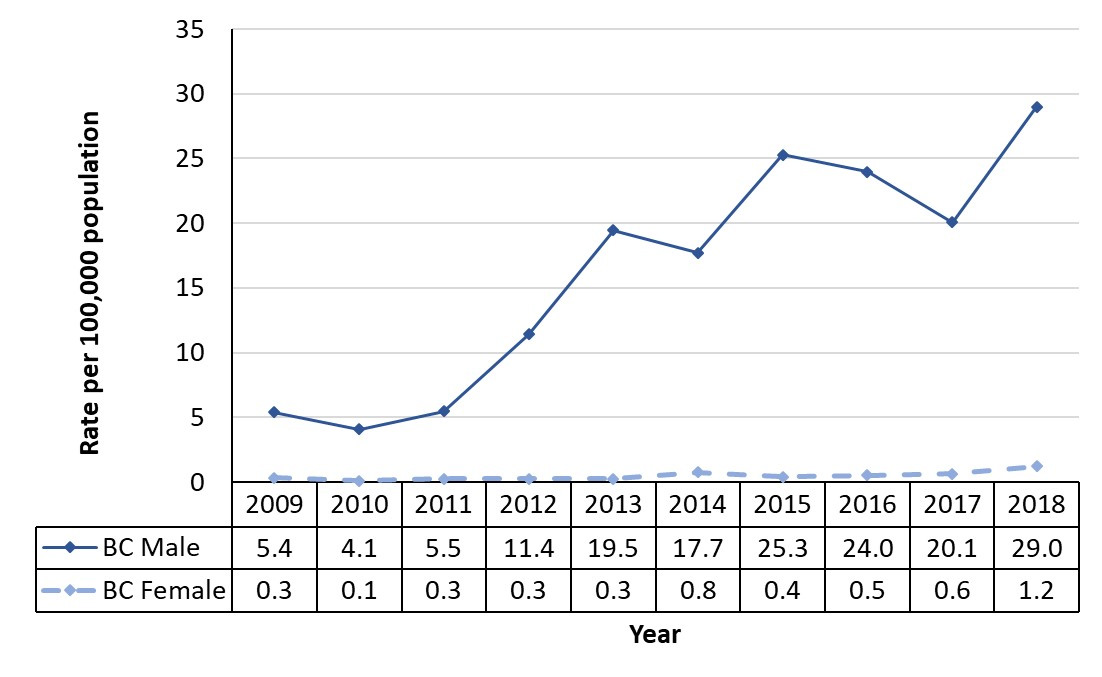
Figure 23 - Text description
This graph displays the rate of reported infectious syphilis cases per 100,000 population in British Columbia by sex, between 2009 and 2018. The horizontal axis shows the calendar years from 2009 to 2018. The vertical axis shows the rate of infectious syphilis per 100,000 population per each calendar year for males and females.
| Year | Rate per 100,000 population | |
|---|---|---|
| BC Male | BC Female | |
| 2009 | 5.4 | 0.3 |
| 2010 | 4.1 | 0.1 |
| 2011 | 5.5 | 0.3 |
| 2012 | 11.4 | 0.3 |
| 2013 | 19.5 | 0.3 |
| 2014 | 17.7 | 0.8 |
| 2015 | 25.3 | 0.4 |
| 2016 | 24.0 | 0.5 |
| 2017 | 20.1 | 0.6 |
| 2018 | 29.0 | 1.2 |
Source: Public Health Agency of Canada (2019). Canadian Notifiable Disease Surveillance System. Preliminary 2018 data received directly from provinces and territories.
Detailed sociodemographic data of the most recent cases in British Columbia are available through the BCCDC’s 2016 detailed STI report, 2017 summary report and 2018 data available in the BCCDC dashboardFootnote 91-93. Insofar as the BCCDC reports both confirmed and probable cases, the province’s reported case numbers and rates tend to be much higher (approximately 40% of reported cases are probable cases) than the confirmed case numbers provided to the CNDSS.
Provincial data suggest that from 2016 to 2018, the incidence of infectious syphilis was highest among the 25 to 29 year age group, followed closely by the 30 to 39 year age groupFootnote 91-93. Among females, rates tended to be higher in those of reproductive age (the highest rates were found in the 20 to 24 year age group). Concurrent with data available through the CNDSS, the majority of reported cases in the province were among males (725 of 759 cases diagnosed in 2016 (95%) and 849 of 919 cases diagnosed in 2018 (92%)). In 2016, almost half of the male cases self-identified as Caucasian (47%), while the remaining cases self-identified as Asian (7%), Hispanic (5%), Indigenous (2%), South Asian (3%), Black (1%) or Arab/West Asian or other/mixed ethnicity (1%)Footnote 92. Ethnicity was unknown for 34% of the male cases. In 2016, most of the 33 female cases self-identified as either Caucasian (15%), Asian (15%), South Asian (6%) or Indigenous (6%). Ethnicity data were not available for 58% of female cases.
In 2016, the majority of cases occurred among gbMSM (655 of 725 male cases (90%); 86% of all cases). Of the 635 gbMSM cases with known HIV status, 43% were living with HIV at the time of their syphilis diagnosis, a decrease since 2015 (52%). The majority of female cases identified as heterosexual. Overall, the proportion of heterosexual cases (male or female) without other risk factors increased slightly between 2015 (86 cases, 11% of all cases) and 2016 (95 cases, 13% of all cases)Footnote 92.
From 2007 to 2018, most of the infectious syphilis cases and the highest overall rates of infectious syphilis in British Colombia were identified in the urban region of Vancouver (Vancouver Coastal Health Authority; 70.9 per 100,000). Rates were also high in South Vancouver Island (home to the urban centre of Victoria and Central Vancouver Island; 18.4 and 14.4 per 100,000, respectively), and Richmond (12.9 per 100,000)Footnote 91.
3.2.3 Prairies Region: Alberta, Manitoba and Saskatchewan
Figure 24 presents the overall rate of infectious syphilis per 100,000 population in Alberta, Saskatchewan and Manitoba, between 1979 and 2018. Rates were high in the early to mid-1980s in Alberta and Manitoba, before decreasing significantly. For more than a decade, from 1987 to 2002, rates for all three provinces remained low before increasing in the early 2000s and peaking after 2012, with the highest rates observed in Manitoba in 2018. According to 2017 CNDSS data, there were 251 cases reported in Manitoba, corresponding to a rate of 18.8 per 100,000 and 535 cases of infectious syphilis reported in Alberta, corresponding to a rate of 12.6 per 100,000. In comparison, Saskatchewan reported 120 cases, corresponding to a rate of 10.4 per 100,000. Preliminary 2018 data indicate an increase in rates for all three provinces (60.7 per 100,000 for Manitoba, 35.7 per 100,000 for Alberta and 12.0 per 100,000 for Saskatchewan (Appendix F).
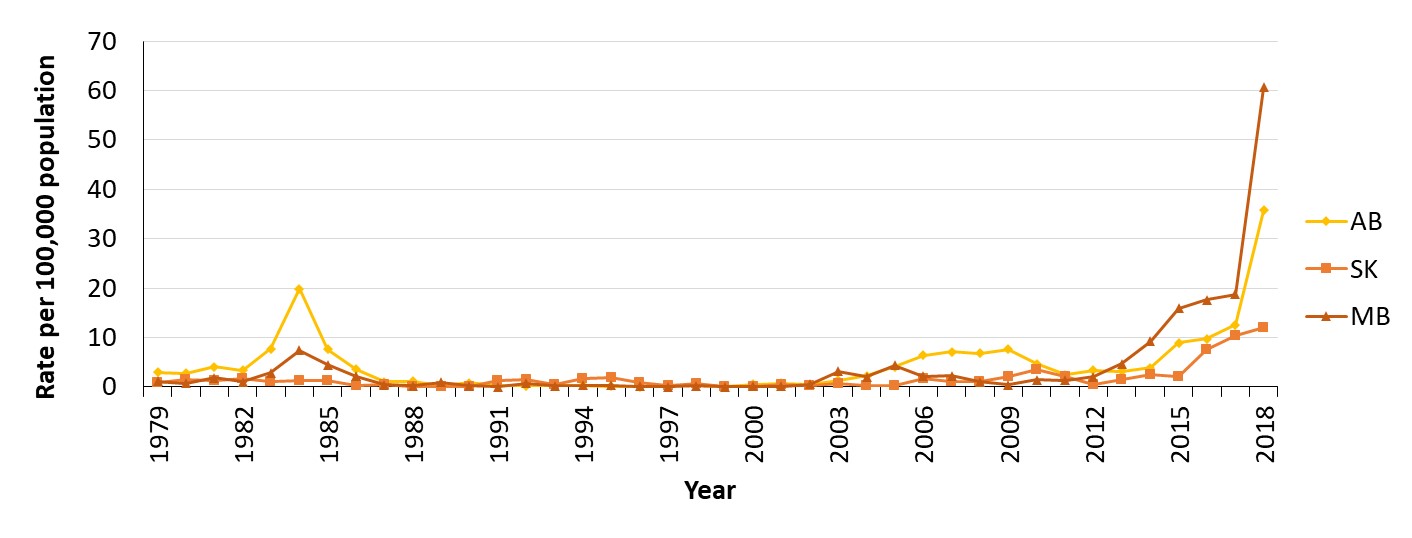
Figure 24 - Text description
This graph displays the rate of reported infectious syphilis cases per 100,000 population in Alberta, Saskatchewan, and Manitoba, between 1979 and 2018. The horizontal axis shows the calendar years from 1979 to 2018. The vertical axis shows the rate of infectious syphilis per 100,000 population per each calendar year for Alberta, Saskatchewan, and Manitoba respectively.
| Year | Rate per 100,000 population | ||
|---|---|---|---|
| Alberta | Saskatchewan | Manitoba | |
| 1979 | 3.0 | 0.9 | 1.2 |
| 1980 | 2.7 | 1.4 | 0.8 |
| 1981 | 4.1 | 1.2 | 1.8 |
| 1982 | 3.3 | 1.6 | 1.1 |
| 1983 | 7.7 | 1.0 | 2.8 |
| 1984 | 19.8 | 1.3 | 7.4 |
| 1985 | 7.6 | 1.3 | 4.5 |
| 1986 | 3.6 | 0.3 | 2.2 |
| 1987 | 1.1 | 0.4 | 0.5 |
| 1988 | 1.1 | 0.1 | 0.2 |
| 1989 | 0.2 | 0.0 | 0.9 |
| 1990 | 0.8 | 0.0 | 0.2 |
| 1991 | 0.2 | 1.2 | 0.0 |
| 1992 | 0.2 | 1.5 | 0.7 |
| 1993 | 0.2 | 0.5 | 0.3 |
| 1994 | 0.3 | 1.8 | 0.4 |
| 1995 | 0.1 | 1.9 | 0.4 |
| 1996 | 0.0 | 0.9 | 0.1 |
| 1997 | 0.3 | 0.2 | 0.0 |
| 1998 | 0.2 | 0.6 | 0.3 |
| 1999 | 0.1 | 0.1 | 0.0 |
| 2000 | 0.5 | 0.1 | 0.1 |
| 2001 | 0.8 | 0.5 | 0.1 |
| 2002 | 0.4 | 0.2 | 0.5 |
| 2003 | 1.3 | 0.6 | 3.2 |
| 2004 | 2.3 | 0.2 | 2.0 |
| 2005 | 4.1 | 0.2 | 4.3 |
| 2006 | 6.4 | 1.7 | 2.2 |
| 2007 | 7.1 | 1.0 | 2.3 |
| 2008 | 6.8 | 1.2 | 1.1 |
| 2009 | 7.6 | 2.0 | 0.4 |
| 2010 | 4.6 | 3.4 | 1.4 |
| 2011 | 2.5 | 2.2 | 1.3 |
| 2012 | 3.3 | 0.6 | 2.0 |
| 2013 | 3.1 | 1.5 | 4.7 |
| 2014 | 3.8 | 2.5 | 9.2 |
| 2015 | 8.9 | 2.1 | 15.9 |
| 2016 | 9.7 | 7.5 | 17.7 |
| 2017 | 12.6 | 10.4 | 18.8 |
| 2018 | 35.7 | 12.0 | 60.7 |
Source: Public Health Agency of Canada (2019). Canadian Notifiable Disease Surveillance System. Preliminary 2018 data received directly from provinces and territories.
Between 2009 and 2012, male and female rates were generally low in all three provinces, with male rates generally higher than female rates (Figure 25). Starting in 2013, rates among males began to increase at a more rapid pace than female rates, which led to an increase in the male-to-female rate ratio in all three provinces. Nonetheless, female rates have also been on the rise in all three provinces. In 2018, female rates were especially high in Manitoba (55.9 per 100,000 females), much higher than the Canadian national female rate of 7.0 per 100,000 that year.
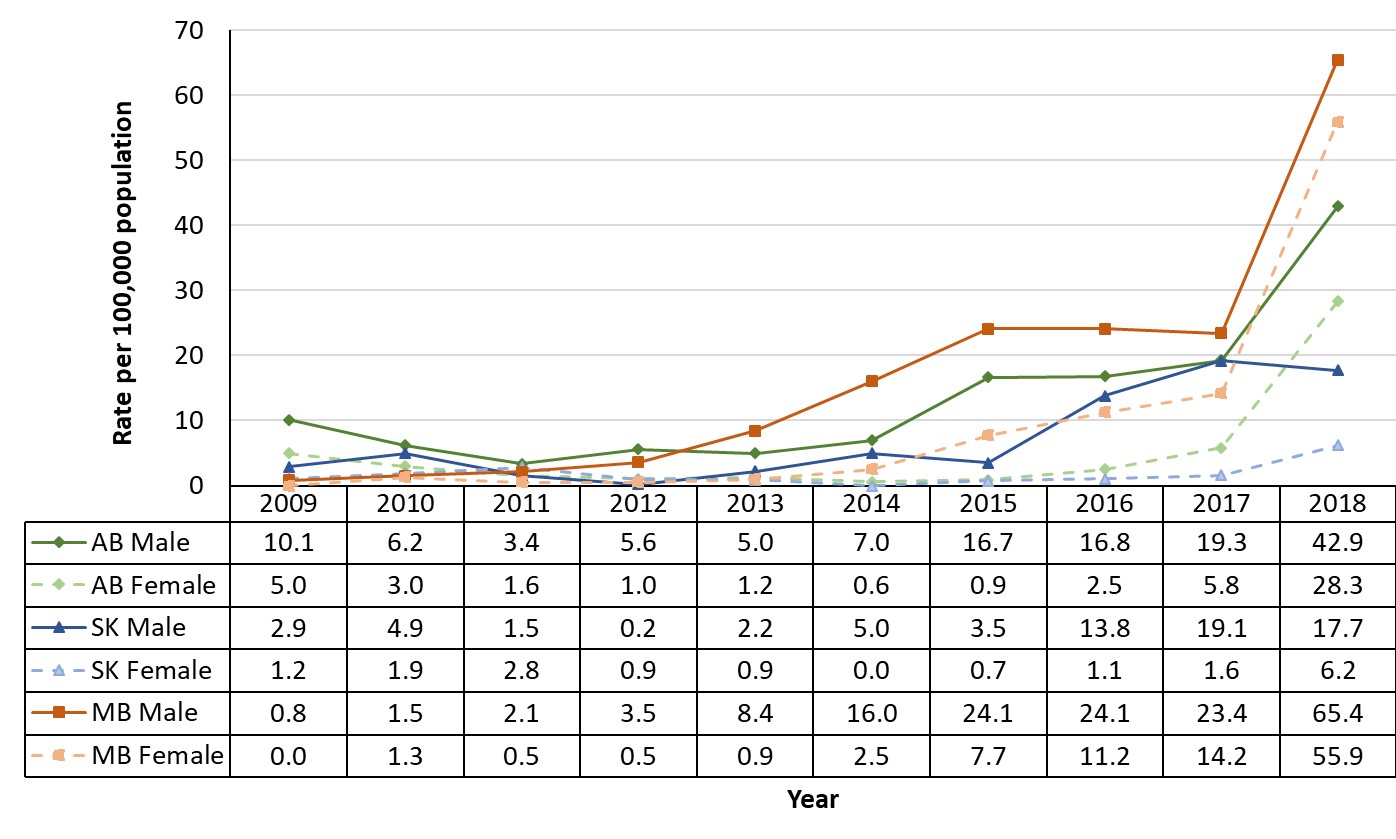
Figure 25 - Text description
This graph displays the rate of reported infectious syphilis cases per 100,000 population in Alberta, Saskatchewan, and Manitoba by sex, between 2009 and 2018. The horizontal axis shows the calendar years from 2009 to 2018. The vertical axis shows the rate of infectious syphilis per 100,000 population per each calendar year for males and females for Alberta, Saskatchewan, and Manitoba respectively.
| Year | Rate per 100,000 population | |||||
|---|---|---|---|---|---|---|
| AB Male | AB Female | SK Male | SK Female | MB Male | MB Female | |
| 2009 | 10.1 | 5.0 | 2.9 | 1.2 | 0.8 | 0.0 |
| 2010 | 6.2 | 3.0 | 4.9 | 1.9 | 1.5 | 1.3 |
| 2011 | 3.4 | 1.6 | 1.5 | 2.8 | 2.1 | 0.5 |
| 2012 | 5.6 | 1.0 | 0.2 | 0.9 | 3.5 | 0.5 |
| 2013 | 5.0 | 1.2 | 2.2 | 0.9 | 8.4 | 0.9 |
| 2014 | 7.0 | 0.6 | 5.0 | 0.0 | 16.0 | 2.5 |
| 2015 | 16.7 | 0.9 | 3.5 | 0.7 | 24.1 | 7.7 |
| 2016 | 16.8 | 2.5 | 13.8 | 1.1 | 24.1 | 11.2 |
| 2017 | 19.3 | 5.8 | 19.1 | 1.6 | 23.4 | 14.2 |
| 2018 | 42.9 | 28.3 | 17.7 | 6.2 | 65.4 | 55.9 |
Source: Public Health Agency of Canada (2019). Canadian Notifiable Disease Surveillance System. Preliminary 2018 data received directly from provinces and territories.
Alberta
Recent case numbers and rates are available through the province’s 2018 STI and HIV reportFootnote 94. In 2018, there were 1,536 cases of infectious syphilis in Alberta, corresponding to a rate of 35.7 cases per 100,000 populationFootnote 94. This represents a 187.1% increase in case numbers from 2017 (n=535)Footnote 94. Similar to 2017 data (Figure 25), males were the most affected population in 2018, representing 60% of all reported cases, of which 31% were in the 20 to 29 year age group. The highest incidence was observed among the 25 to 29 year age group. Information on sexual orientation and ethnicity was not available in the 2018 report. However, in 2016, 73% of male cases reported same sex partnersFootnote 95. According to preliminary data for 2019, 1,958 cases of infectious syphilis were reported in AlbertaFootnote 96. As a result of this sharp rise in the number of cases, the province declared a provincial outbreak on July 16th 2019.
In 2018, the highest incidence of infectious syphilis was observed in the urban zone of Edmonton (977 cases; 65% of all provincial cases; 70 cases per 100,000). The second highest rate was observed in the northern region of the province (North health zone; 43.5 cases per 100,000), which also observed the greatest infectious syphilis rate increase of all of the province’s five zones since 2017 (321.5%). The other three regions (Central, Calgary and South zones) reported rates of infectious syphilis ranging from 10.1 to 18.5 per 100,000Footnote 94. Cases reported in 2019 were also primarily located in Edmonton zone and North zone.
Saskatchewan
Available provincial surveillance products reported 120 cases of infectious syphilis in the province in 2017 (corresponding rate of 10.4 per 100,000 population), which is similar to the Canadian average rate that yearFootnote 97. In 2019, Saskatchewan Ministry of Health reported 381 cases of syphilis compared to just 140 in 2018, an increase of 172%Footnote 98Footnote 99.
From 2017 to 2018, gbMSM were the group most affected by syphilisFootnote 97. However, the proportion of female cases is increasing in Saskatchewan. In 2017, 92% of reported cases were among males. According to preliminary data, this proportion dropped to 70% in 2018 and to 57% in 2019Footnote 97Footnote 99. In 2018, 95% of female cases were of reproductive age (15 to 45 years of age)Footnote 97. From 2012 to 2016, the most important risk factors for syphilis incidence in the Saskatoon Health Region (the region that saw the largest proportion of cases in 2017) included condomless sex with a same-sex partner, having a new partner within the previous three months, having met partner(s) on the Internet, and having an unknown or anonymous partnerFootnote 100.
Most of the 2017 cases in the province (77%) were diagnosed in the urban regions of former Regina and Saskatoon regional health authoritiesFootnote 97. In 2019, the Saskatchewan Health Authority declared a syphilis outbreak in the regions of Battleford and Lloydminster, in the west central region of the province, following a surge of 42 cases in the first six months of the yearFootnote 101. A syphilis outbreak was also declared in First Nations on-reserve communities, with 80% of cases occurring among the 15 to 29 year age groupFootnote 102. In 2018, the average reported rate in First Nations communities in the province was 25.7 per 100,000, almost three times higher than the provincial averageFootnote 103. According to media outlets, rates reached 83 per 100,000 in the affected First Nations communities during the outbreak in 2019Footnote 104. Crystal methamphetamine use seems to be a driver in the current 2019 outbreakFootnote 99.
Manitoba
While the last comprehensive surveillance report from the province describes data up to 2014, other summary reports and news publications for more recent years have been producedFootnote 105. In 2015, a syphilis outbreak was declared across the provinceFootnote 106. As in previous years, rates in 2015 were highest among men, and gbMSM were the most affected populationFootnote 53. Nonetheless, rates among females have been steadily increasing. In 2017, the female rate was 14.2 per 100,000, and the male rate was 23.4 per 100,000 (Figure 25). Approximately 48% of all cases diagnosed in 2018 were female, up from 22% in 2015. This was one of the highest proportion of female cases of all PTs, giving rise to a female rate of 55.9 per 100,000, according to preliminary data (Figure 25)Footnote 6Footnote 53. The highest rate of reported cases was among the 20 to 24 (45.7 per 100,000) and 25 to 29 year age groups (65.3 per 100,000).
In 2018, approximately 15% of the cases were people living with HIV, and 50 to 60% of patients identified themselves as IndigenousFootnote 107Footnote 108. Preliminary data suggest that heterosexual transmission is prominent in the province in 2019Footnote 109. Risk factors within the urban region of Winnipeg include use of crystal methamphetamineFootnote 110.
In 2012, a syphilis outbreak was declared in the urban region of Winnipeg (Winnipeg Health Regional Authority) which continued into 2019Footnote 105. In 2018, the infectious syphilis rate reached 87 per 100,000 in Winnipeg, nearly five times greater than it was in 2017 (18 per 100,000)Footnote 110. As of 2019, a large proportion of cases have also been identified in the more rural northern region of the province (Northern Health Region), which is home to 26 First Nation communitiesFootnote 109Footnote 111.
3.2.4 Central Region: Ontario and Quebec
In the 1980s, high rates were observed in both Ontario and Quebec. Significant decreases in rates occurred in the 1990s (Figure 26). Rates began to gradually increase in the 2000s and have peaked in recent years. In 2018, rates for both provinces were similar to or lower than the Canadian average for that year (25.5 per 100,000 for Ontario and 20.2 per 100,000 for Quebec, while the Canadian average was 27.1 per 100,000) (Appendix G).
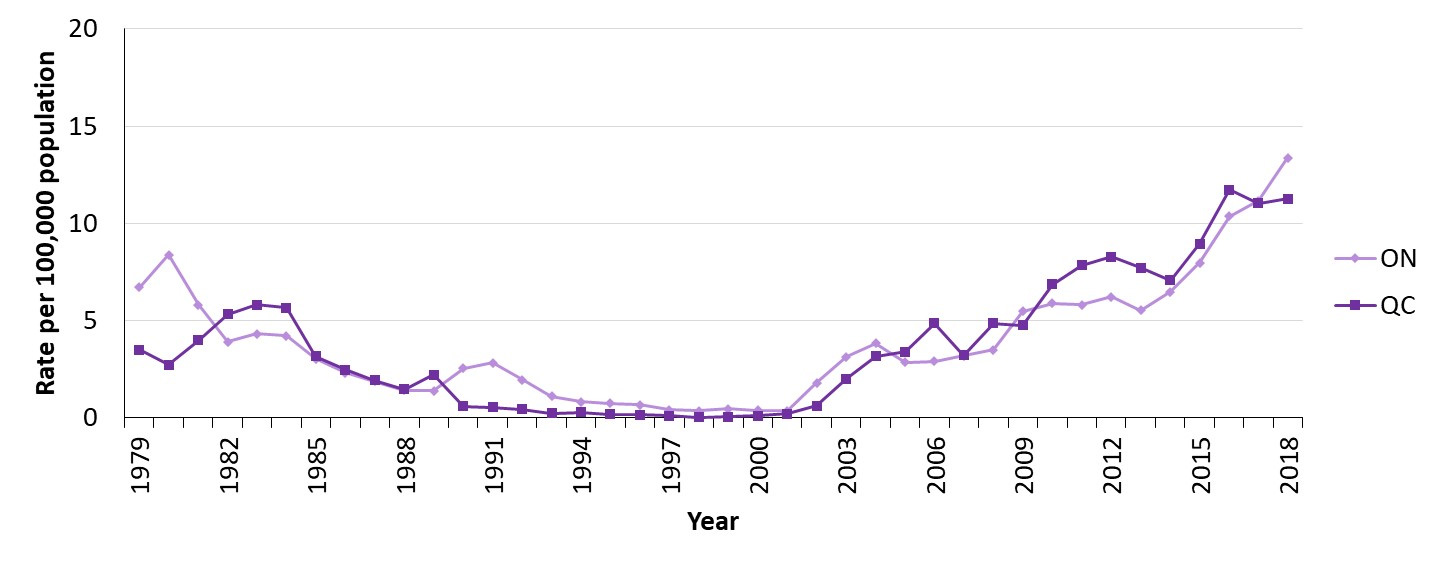
Figure 26 - Text description
This graph displays the rate of reported infectious syphilis cases per 100,000 population in Ontario and Quebec, between 1979 and 2018. The horizontal axis shows the calendar years from 1979 to 2018. The vertical axis shows the rate of infectious syphilis per 100,000 population per each calendar year for Ontario and Quebec respectively.
| Year | Rate per 100,000 population | |
|---|---|---|
| Ontario | Quebec | |
| 1979 | 6.7 | 3.5 |
| 1980 | 8.4 | 2.7 |
| 1981 | 5.8 | 4.0 |
| 1982 | 3.9 | 5.3 |
| 1983 | 4.3 | 5.8 |
| 1984 | 4.2 | 5.7 |
| 1985 | 3.0 | 3.2 |
| 1986 | 2.3 | 2.5 |
| 1987 | 1.9 | 1.9 |
| 1988 | 1.4 | 1.5 |
| 1989 | 1.4 | 2.2 |
| 1990 | 2.5 | 0.6 |
| 1991 | 2.8 | 0.5 |
| 1992 | 2.0 | 0.5 |
| 1993 | 1.1 | 0.2 |
| 1994 | 0.8 | 0.3 |
| 1995 | 0.8 | 0.2 |
| 1996 | 0.7 | 0.2 |
| 1997 | 0.4 | 0.1 |
| 1998 | 0.4 | 0.0 |
| 1999 | 0.5 | 0.1 |
| 2000 | 0.4 | 0.1 |
| 2001 | 0.4 | 0.2 |
| 2002 | 1.8 | 0.6 |
| 2003 | 3.1 | 2.0 |
| 2004 | 3.8 | 3.2 |
| 2005 | 2.8 | 3.4 |
| 2006 | 2.9 | 4.9 |
| 2007 | 3.2 | 3.2 |
| 2008 | 3.5 | 4.9 |
| 2009 | 5.5 | 4.8 |
| 2010 | 5.9 | 6.9 |
| 2011 | 5.8 | 7.8 |
| 2012 | 6.2 | 8.3 |
| 2013 | 5.5 | 7.7 |
| 2014 | 6.5 | 7.1 |
| 2015 | 8.0 | 9.0 |
| 2016 | 10.4 | 11.7 |
| 2017 | 11.2 | 11.0 |
| 2018 | 13.4 | 11.3 |
Source: Public Health Agency of Canada (2019). Canadian Notifiable Disease Surveillance System. Preliminary 2018 data received directly from provinces and territories.
In both provinces, the reported rates among males are substantially higher than the corresponding rates for females (Figure 27). Rates among males gradually increased between 2009 and 2018, while female rates have slightly increased since 2014 in both provinces. In 2018, the rate of infectious syphilis in Ontario was 19.6 times greater in males than females, while for Quebec, it was 9.2 times greater in males than in females.
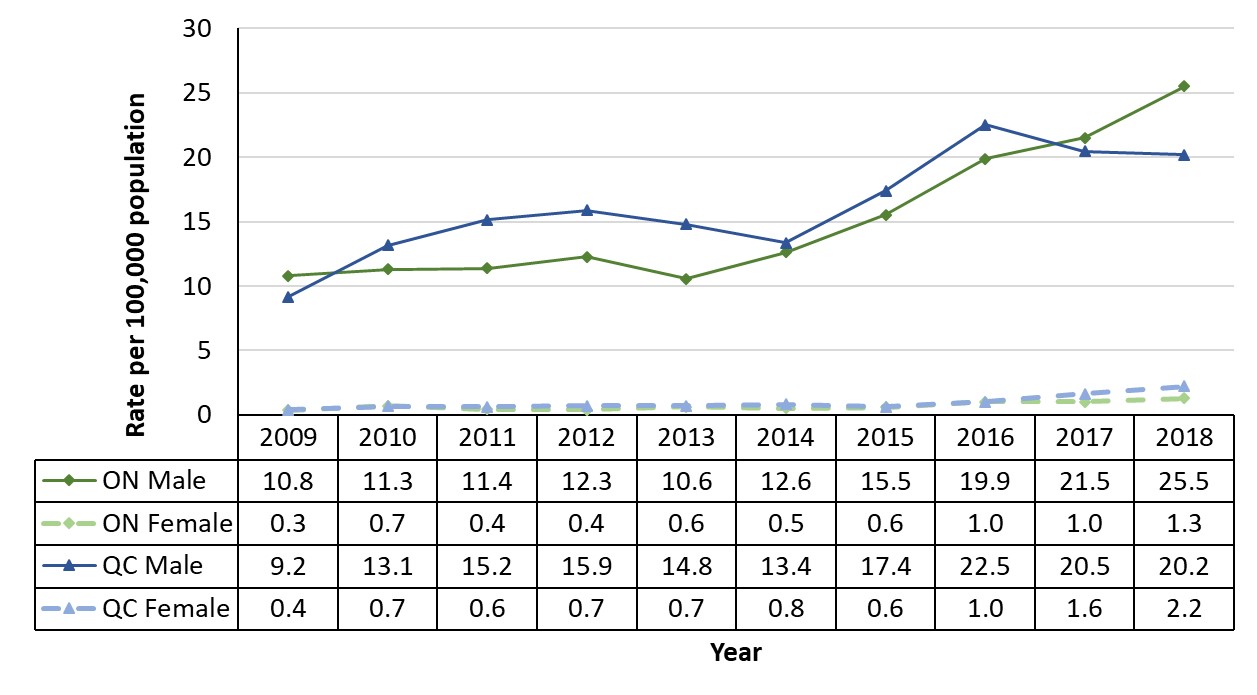
Figure 27 - Text description
This graph displays the rate of reported infectious syphilis cases per 100,000 population in Ontario and Quebec by sex, between 2009 and 2018. The horizontal axis shows the calendar years from 2009 to 2018. The vertical axis shows the rate of infectious syphilis per 100,000 population per each calendar year for males and females for Ontario and Quebec respectively.
| Year | Rate per 100,000 population | |||
|---|---|---|---|---|
| ON Male | ON Female | QC Male | QC Female | |
| 2009 | 10.8 | 0.3 | 9.2 | 0.4 |
| 2010 | 11.3 | 0.7 | 13.1 | 0.7 |
| 2011 | 11.4 | 0.4 | 15.2 | 0.6 |
| 2012 | 12.3 | 0.4 | 15.9 | 0.7 |
| 2013 | 10.6 | 0.6 | 14.8 | 0.7 |
| 2014 | 12.6 | 0.5 | 13.4 | 0.8 |
| 2015 | 15.5 | 0.6 | 17.4 | 0.6 |
| 2016 | 19.9 | 1.0 | 22.5 | 1.0 |
| 2017 | 21.5 | 1.0 | 20.5 | 1.6 |
| 2018 | 25.5 | 1.3 | 20.2 | 2.2 |
Source: Public Health Agency of Canada (2019). Canadian Notifiable Disease Surveillance System. Preliminary 2018 data received directly from provinces and territories.
Ontario
According to CNDSS data, there were 1,571 cases of infectious syphilis in Ontario in 2017, corresponding to a rate of 11.2 per 100,000. Overall, 95% of cases reported by the province were male, and the highest rates were observed in the 25 to 39 year age groups (approximately 26 per 100,000).
In 2018, 1,800 cases of infectious syphilis were reported, corresponding to a rate of 12.5 per 100,000, a slight increase from the 2017 rate, and a large increase since 2015 (1,068 cases; 7.7 per 100,000)Footnote 112Footnote 113. After releasing a first notice in October 2018, the Ontario Northwestern Health Unit declared a syphilis outbreak in 2019, following the detection of 48 cases from August 1st, 2018 to July 30th, 2019Footnote 114Footnote 115. During this period, the rate of reported cases was 58.6 per 100,000. Of the 48 cases, 50% occurred among males (24 cases), primarily in the 25 to 29, 35 to 39 and 65 to 69 year age groups. The other 50% occurred among females (24 cases), most of which affected the 20 to 24 year age group. Risk factor information at the time of reporting was available for more than two-thirds of the cases (33 of the 48). The most common risk factors included condomless sex (85% of cases), heterosexual sex (67%), injection drug use (61%) and being under-housed/homeless (46%)Footnote 114. Concurrent condomless sex and injection drug use were reported by a majority (72%) of the cases. More than 30% of the cases had undergone testing as a result of contact tracingFootnote 114. Case investigations suggest that this outbreak is linked to the Winnipeg Regional Health Authority outbreak referenced aboveFootnote 116Footnote 117.
The Middlesex-London Health Unit also reported a syphilis outbreak in 2019Footnote 118. Since 2014, the number of cases reported to the Health Unit has more than tripled to 113Footnote 118. Previous data reported by this Health Unit suggested the rise in cases was occurring mainly among gbMSMFootnote 118. However, more recent data show increases among heterosexuals and in those engaged in the sale or purchase of sexFootnote 118.
The City of Peterborough also declared an outbreak in January 2020, following a surge in the number of cases in 2019 compared to 2018 (15 vs 9 cases)Footnote 119. In Ottawa, the number of cases increased from 30 to 159 between 2013 and 2018Footnote 120.
Quebec
In 2017, the province of Quebec reported 915 cases to CNDSS, corresponding to a rate of 11.0 per 100,000 population, similar to the Canadian average. In 2018, 938 infectious syphilis cases were identified (11.1 cases per 100,000 population), and 1,141 cases are projected for 2019 (based on the number of cases reported during the first 222 days of the year), corresponding to a rate of 13.3 per 100,000 populationFootnote 121. In 2017 and 2018, the majority of cases (92% and 89%, respectively) were found in malesFootnote 121Footnote 122. The age group reporting the highest rates shifted from those in the 30 to 34 year age group (25.5 per 100,000 in 2017), to those in the 20 to 29 year age group (26.3 per 100,000 population in 2018)Footnote 121Footnote 122. GbMSM continue to be the most affected populationFootnote 122. However, the province also noted an increase of cases among women, most of which (89%) occurred in women of reproductive age (15 to 49 years of age).
The Montreal region continues to be one of the most affected regions of the province, contributing to 53% of all Quebec cases in 2018, a rate of 24.4 per 100,000 populationFootnote 121. However, rates were highest (116.5 per 100,000) in Nunavik, a northern Inuit region, where a syphilis outbreak has been ongoing since 2016Footnote 121. In 2017, the majority of cases reported in Nunavik were in the 15 to 34 year age group, of which 59% (19/32 cases) were femaleFootnote 122.
3.2.5 Atlantic Region: New Brunswick, Newfoundland and Labrador, Nova Scotia and Prince Edward Island
The overall rates of infectious syphilis per 100,000 population for the provinces of New Brunswick, Newfoundland and Labrador, Nova Scotia and Prince Edward Island from 1979 to 2018 are presented in Figure 28. Throughout the 1980s and 1990s, the rates of infectious syphilis for all four provinces varied slightly, but were generally low, especially between 1995 and 2002. In the mid-to-late 2000s, the rates began increasing. Despite these increases, rates in the region continue to be lower than the Canadian average each year.
According to the New Brunswick Communicable Disease 2017 Annual Surveillance Report, there were 20 cases of infectious syphilis in the province in 2017, corresponding to a rate of 2.6 per 100,000 populationFootnote 123. CNDSS data for the province of Nova Scotia reported 26 cases, corresponding to a rate of 2.7 per 100,000. Four cases were reported in Prince Edward Island, for a rate of 2.7 per 100,000. Newfoundland and Labrador had both the highest number of cases (39 cases) and the highest rate (7.4 per 100,000).
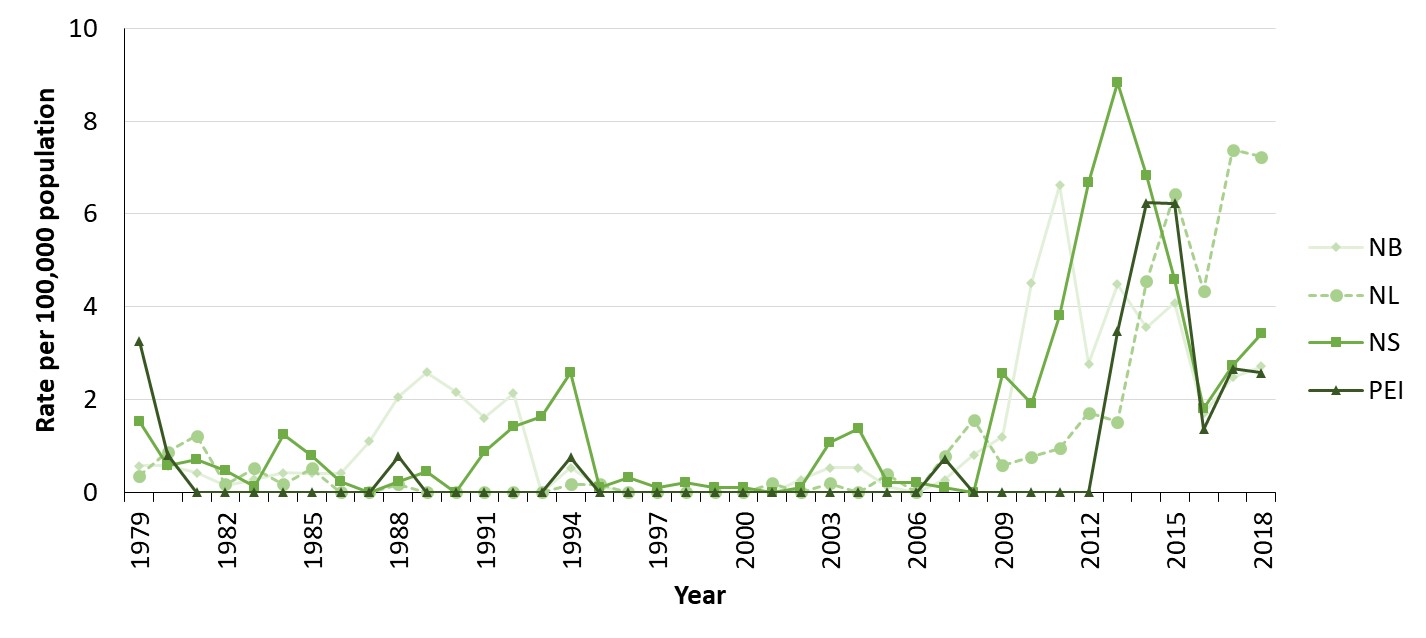
Figure 28 - Text description
This graph displays the rate of reported infectious syphilis cases per 100,000 population in Nova Scotia, New Brunswick, Prince Edward Island, and Newfoundland and Labrador, between 1979 and 2018. The horizontal axis shows the calendar years from 1979 to 2018. The vertical axis shows the rate of infectious syphilis per 100,000 population per each calendar year for New Brunswick, Nova Scotia, Prince Edward Island, and Newfoundland and Labrador respectively.
| Year | Rate per 100,000 population | |||
|---|---|---|---|---|
| New Brunswick | Newfoundland and Labrador | Nova Scotia | Prince Edward Island | |
| 1979 | 0.6 | 0.4 | 1.5 | 3.3 |
| 1980 | 0.6 | 0.9 | 0.6 | 0.8 |
| 1981 | 0.4 | 1.2 | 0.7 | 0.0 |
| 1982 | 0.1 | 0.2 | 0.5 | 0.0 |
| 1983 | 0.3 | 0.5 | 0.1 | 0.0 |
| 1984 | 0.4 | 0.2 | 1.3 | 0.0 |
| 1985 | 0.4 | 0.5 | 0.8 | 0.0 |
| 1986 | 0.4 | 0.0 | 0.2 | 0.0 |
| 1987 | 1.1 | 0.0 | 0.0 | 0.0 |
| 1988 | 2.1 | 0.2 | 0.2 | 0.8 |
| 1989 | 2.6 | 0.0 | 0.4 | 0.0 |
| 1990 | 2.2 | 0.0 | 0.0 | 0.0 |
| 1991 | 1.6 | 0.0 | 0.9 | 0.0 |
| 1992 | 2.1 | 0.0 | 1.4 | 0.0 |
| 1993 | 0.0 | 0.0 | 1.6 | 0.0 |
| 1994 | 0.5 | 0.2 | 2.6 | 0.7 |
| 1995 | 0.1 | 0.2 | 0.1 | 0.0 |
| 1996 | 0.0 | 0.0 | 0.3 | 0.0 |
| 1997 | 0.0 | 0.0 | 0.1 | 0.0 |
| 1998 | 0.0 | 0.0 | 0.2 | 0.0 |
| 1999 | 0.0 | 0.0 | 0.1 | 0.0 |
| 2000 | 0.0 | 0.0 | 0.1 | 0.0 |
| 2001 | 0.0 | 0.2 | 0.0 | 0.0 |
| 2002 | 0.3 | 0.0 | 0.1 | 0.0 |
| 2003 | 0.5 | 0.2 | 1.1 | 0.0 |
| 2004 | 0.5 | 0.0 | 1.4 | 0.0 |
| 2005 | 0.1 | 0.4 | 0.2 | 0.0 |
| 2006 | 0.0 | 0.0 | 0.2 | 0.0 |
| 2007 | 0.3 | 0.8 | 0.1 | 0.7 |
| 2008 | 0.8 | 1.6 | 0.0 | 0.0 |
| 2009 | 1.2 | 0.6 | 2.6 | 0.0 |
| 2010 | 4.5 | 0.8 | 1.9 | 0.0 |
| 2011 | 6.6 | 1.0 | 3.8 | 0.0 |
| 2012 | 2.8 | 1.7 | 6.7 | 0.0 |
| 2013 | 4.5 | 1.5 | 8.8 | 3.5 |
| 2014 | 3.6 | 4.5 | 6.8 | 6.2 |
| 2015 | 4.1 | 6.4 | 4.6 | 6.2 |
| 2016 | 1.7 | 4.3 | 1.8 | 1.4 |
| 2017 | 2.5 | 7.4 | 2.7 | 2.7 |
| 2018 | 2.7 | 7.2 | 3.4 | 2.6 |
Source: Public Health Agency of Canada (2019). Canadian Notifiable Disease Surveillance System. Preliminary 2018 data received directly from provinces and territories.
Figure 29 presents the male and female rates of infectious syphilis per 100,000 population in New Brunswick, Newfoundland and Labrador, Nova Scotia and Prince Edward Island from 2009 to 2018. Male rates have generally been higher than female rates in all four provinces. The largest male-to-female rate ratio in the region was observed in New Brunswick in 2018, where the infectious syphilis rate was 17.3 times greater among males than females. Female rates have generally been low for all provinces through time.
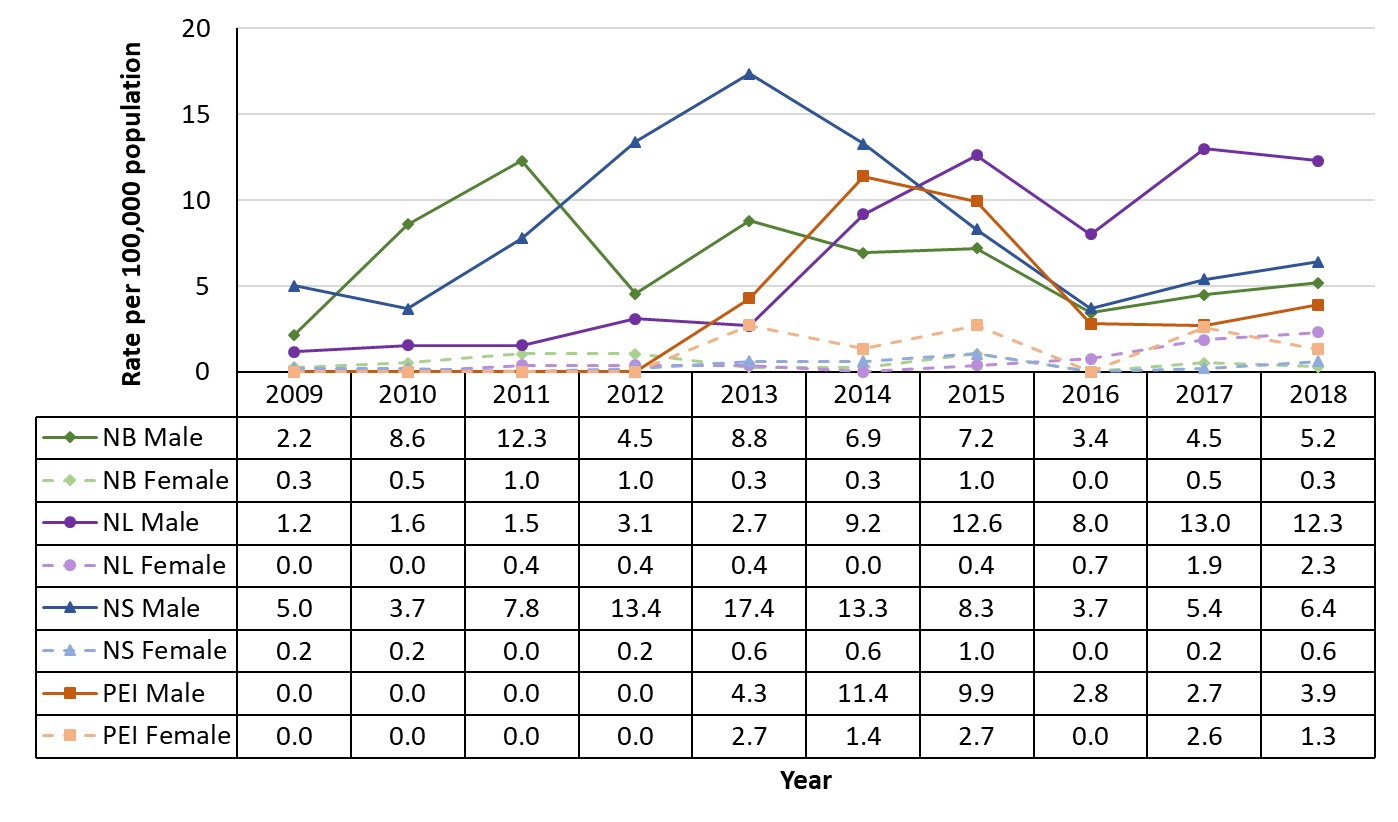
Figure 29 - Text description
This graph displays the rate of reported infectious syphilis cases per 100,000 population in New Brunswick, Nova Scotia, Prince Edward Island, and Newfoundland and Labrador by sex, between 2009 and 2018. The horizontal axis shows the calendar years from 2009 to 2018. The vertical axis shows the rate of infectious syphilis per 100,000 population per each calendar year for males and females for New Brunswick, Nova Scotia, Prince Edward Island, and Newfoundland and Labrador respectively.
| Year | Rate per 100,000 population | |||||||
|---|---|---|---|---|---|---|---|---|
| NB Male | NB Female | NL Male | NL Female | NS Male | NS Female | PEI Male | PEI Female | |
| 2009 | 2.2 | 0.3 | 1.2 | 0.0 | 5.0 | 0.2 | 0.0 | 0.0 |
| 2010 | 8.6 | 0.5 | 1.6 | 0.0 | 3.7 | 0.2 | 0.0 | 0.0 |
| 2011 | 12.3 | 1.0 | 1.5 | 0.4 | 7.8 | 0.0 | 0.0 | 0.0 |
| 2012 | 4.5 | 1.0 | 3.1 | 0.4 | 13.4 | 0.2 | 0.0 | 0.0 |
| 2013 | 8.8 | 0.3 | 2.7 | 0.4 | 17.4 | 0.6 | 4.3 | 2.7 |
| 2014 | 6.9 | 0.3 | 9.2 | 0.0 | 13.3 | 0.6 | 11.4 | 1.4 |
| 2015 | 7.2 | 1.0 | 12.6 | 0.4 | 8.3 | 1.0 | 9.9 | 2.7 |
| 2016 | 3.4 | 0.0 | 8.0 | 0.7 | 3.7 | 0.0 | 2.8 | 0.0 |
| 2017 | 4.5 | 0.5 | 13.0 | 1.9 | 5.4 | 0.2 | 2.7 | 2.6 |
| 2018 | 5.2 | 0.3 | 12.3 | 2.3 | 6.4 | 0.6 | 3.9 | 1.3 |
Source: Public Health Agency of Canada (2019). Canadian Notifiable Disease Surveillance System. Preliminary 2018 data received directly from provinces and territories.
New Brunswick
From November 2009 to December 2012, New Brunswick experienced a syphilis outbreak, which resulted in 121 cases of infectious syphilis. The outbreak began in the Moncton region at the end of 2009 and affected all regions of the province. The cities of Moncton, Fredericton and Saint John were the most affected cities. Most cases occurred among males (92%), of which three quarters self-identified as gbMSM (75%). Rates were highest among the 15 to 24 year age group (12.4 per 100,000)Footnote 124.
In 2017 as in previous years, most cases occurred among males (18/20 cases, 4.8 per 100,000), and the highest incidence rates were observed among the 30 to 39 year age group (13.3 per 100,000). All of the male cases self-identified as gbMSMFootnote 123. Moreover, the province’s most recent published report on STBBI risk factors (2016) reported other risk factors for infectious syphilis. For the 14 cases reported in 2016, these included condomless sex (69%), past-year substance use (50%), having casual or anonymous sexual contacts (46%), having two or three sexual partners (36%), and having had five or more sexual partners in the last 12 months (27%). Furthermore, three of the cases (21%) had concurrent STI infections (co-infections)Footnote 125.
In 2017, cases were reported in different regions of the provinceFootnote 123. The largest proportion of cases (40%) was identified in the southeastern region surrounding the urban area of Moncton (Region 1).
Newfoundland and Labrador
The province declared a provincial outbreak of infectious syphilis in October 2014. The majority of cases occurred in the urban region of St. John’s and among gbMSMFootnote 126.
At the same time, an outbreak of infectious syphilis was declared in the Eastern Health region of Newfoundland and Labrador. From January 2014 to December 2016, there were 82 cases of outbreak-related syphilis, of which 77 were infectious syphilis cases. At the peak of the outbreak, the rate of infectious syphilis reached 11.3 cases per 100,000. By comparison, the Eastern Health rate of infection was 1.9 per 100,000 in pre-outbreak 2013. During this time, 92% of all syphilis cases occurred among malesFootnote 127. HIV co-infection was reported in 21% of the 82 outbreak-related cases.
According to preliminary data, in Newfoundland and Labrador in 2018, the rate of infectious syphilis cases (7.2 per 100,000) represented a 59% increase from the rate reported in 2014 (4.5 per 100,000)Footnote 6.
Nova Scotia
In 2017, there were 26 reported cases of infectious syphilis in Nova Scotia, corresponding to a rate of 2.7 per 100,000—well below the Canadian average. According to the province’s 2017 Notifiable Disease Surveillance Report, most cases occurred among males (96%) (25/26 cases; 5.3 per 100,000) and overall, the highest rates were reported among the 25 to 39 year age group (13.5 per 100,000 males; 1.1 per 100,000 females)Footnote 128. The majority of these cases were from to the Central Zone of Nova Scotia (which encompasses the urban area of Halifax). Prior to 2019, the last syphilis outbreak reported in the province was declared in September 2008 in Nova Scotia’s Central Zone and occurred mainly among men in Halifax. This outbreak peaked in 2013, where there were 84 cases of infectious syphilis reported in the provinceFootnote 128Footnote 129.
In 2018, Nova Scotia reported 50 cases of syphilis, two thirds of which were infectiousFootnote 89. Preliminary 2019 data has indicated a 70% increase in the number of syphilis cases from 2018: 82 infectious and non-infectious cases have been reported to-date in 2019. Preliminary analysis of the 2019 syphilis cases has indicated a greater proportion of female syphilis cases reported in 2019 (20%), relative to previous years (approximately 10% female in 2018, approximately 5% female in 2017)Footnote 89Footnote 130.
Prince Edward Island
Overall, the rate of infectious syphilis has remained stable and low in Prince Edward Island over the last 10 years131. In 2017, four infectious syphilis cases were reported in Prince Edward Island, corresponding to a rate of 2.7 per 100,000—well below the Canadian averageFootnote 131. In 2017, infectious syphilis cases were evenly distributed among males and females (50% respectively)Footnote 6. Prior to 2014, most individuals diagnosed with syphilis had acquired it in other provinces or countries; however, local transmission is now more commonFootnote 132. In 2018, the rate of infectious syphilis in Prince Edward Island was 2.6 per 100,000 according to preliminary data.
3.2.6 Northern Region: Yukon, Northwest Territories and Nunavut
Figure 30 presents the rate of reported infectious syphilis cases per 100,000 population in the Yukon and the Northwest Territories from 1979 to 2018, and in Nunavut, from the time of its creation in 1999 to 2018. Despite some spikes in cases in the 2000s, rates in both the Northwest Territories and Yukon have remained low and stable. Conversely, after low rates for multiple years, Nunavut has seen increases in cases since 2011.
According to CNDSS data, there were no cases of infectious syphilis reported in Yukon in 2017. In comparison, five cases were reported in Northwest Territories, corresponding to a rate of 11.1 per 100,000 population, and 88 cases were reported in Nunavut, a rate of 234.3 per 100,000. From 2017 to 2018, substantial increases in rates have been reported in all three territories (Figure 17 and Figure 18).
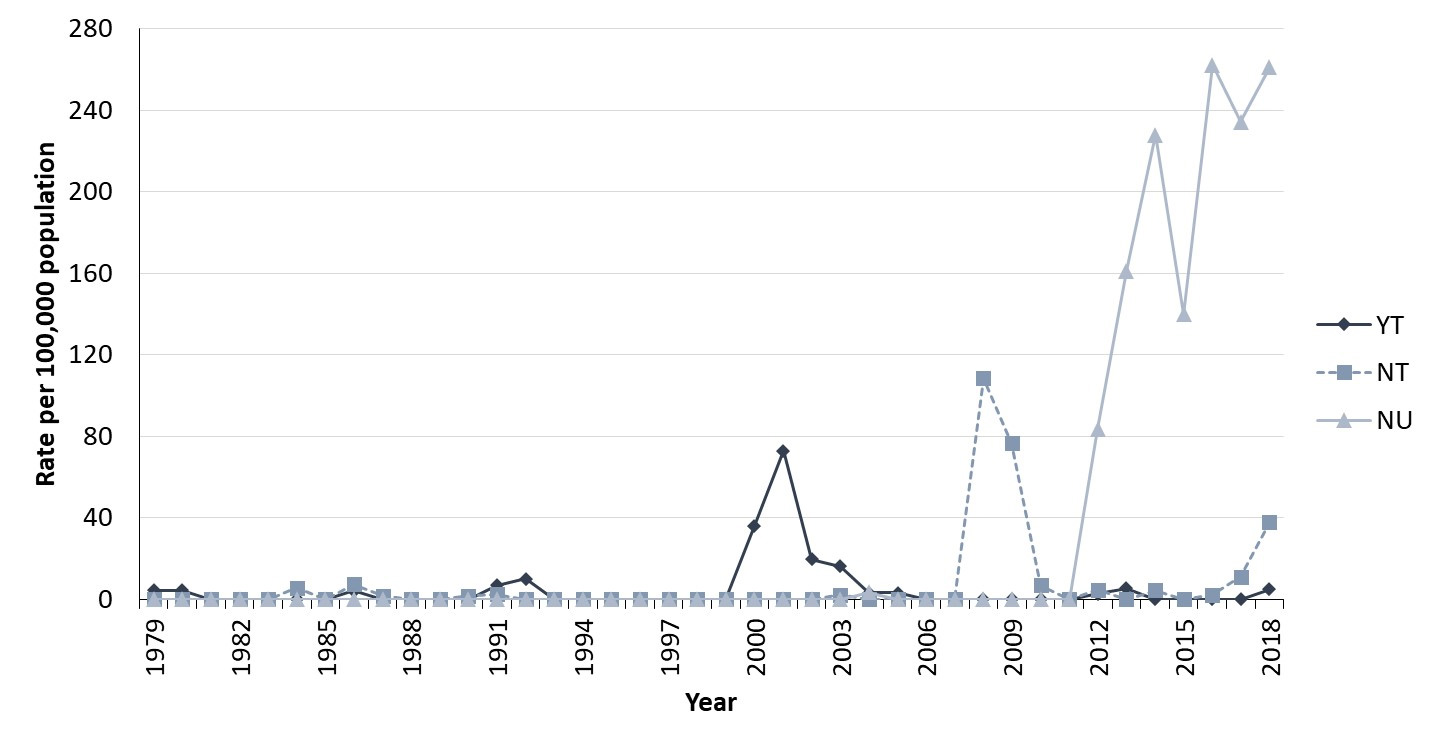
Figure 30 - Text description
This graph displays the rate of reported infectious syphilis cases per 100,000 population in Yukon, Northwest Territories and Nunavut, between 1979 and 2018. The horizontal axis shows the calendar years from 1979 to 2018. The vertical axis shows the rate of infectious syphilis per 100,000 population per each calendar year for Yukon, Northwest Territories, and Nunavut respectively.
| Year | Rate per 100,000 population | ||
|---|---|---|---|
| Yukon | Northwest Territories | Nunavut | |
| 1979 | 4.4 | 0.0 | |
| 1980 | 4.3 | 0.0 | |
| 1981 | 0.0 | 0.0 | |
| 1982 | 0.0 | 0.0 | |
| 1983 | 0.0 | 0.0 | |
| 1984 | 0.0 | 5.7 | |
| 1985 | 0.0 | 0.0 | |
| 1986 | 4.1 | 7.3 | |
| 1987 | 0.0 | 1.8 | |
| 1988 | 0.0 | 0.0 | |
| 1989 | 0.0 | 0.0 | |
| 1990 | 0.0 | 1.7 | |
| 1991 | 6.9 | 2.6 | |
| 1992 | 10.0 | 0.0 | |
| 1993 | 0.0 | 0.0 | |
| 1994 | 0.0 | 0.0 | |
| 1995 | 0.0 | 0.0 | |
| 1996 | 0.0 | 0.0 | |
| 1997 | 0.0 | 0.0 | |
| 1998 | 0.0 | 0.0 | |
| 1999 | 0.0 | 0.0 | 0.0 |
| 2000 | 36.1 | 0.0 | 0.0 |
| 2001 | 72.9 | 0.0 | 0.0 |
| 2002 | 19.8 | 0.0 | 0.0 |
| 2003 | 16.2 | 2.3 | 0.0 |
| 2004 | 3.2 | 0.0 | 3.3 |
| 2005 | 3.1 | 0.0 | 0.0 |
| 2006 | 0.0 | 0.0 | 0.0 |
| 2007 | 0.0 | 0.0 | 0.0 |
| 2008 | 0.0 | 108.4 | 0.0 |
| 2009 | 0.0 | 76.5 | 0.0 |
| 2010 | 0.0 | 6.9 | 0.0 |
| 2011 | 0.0 | 0.0 | 0.0 |
| 2012 | 2.8 | 4.6 | 83.6 |
| 2013 | 5.5 | 0.0 | 161.3 |
| 2014 | 0.0 | 0.0 | 228.0 |
| 2015 | 0.0 | 2.3 | 139.8 |
| 2016 | 0.0 | 0.0 | 262.3 |
| 2017 | 0.0 | 11.1 | 234.3 |
| 2018 | 4.9 | 37.9 | 261.1 |
Source: Public Health Agency of Canada (2019). Canadian Notifiable Disease Surveillance System. Preliminary 2018 data received directly from provinces and territories.
Between 2009 and 2018, Yukon reported very few cases of infectious syphilis in both males and females (Figure 31). In the Northwest Territories, both male and female rates were high in 2008 and 2009, before decreasing in subsequent years. Between 2016 and 2018, rates in males began to increase again. In Nunavut, following the territory’s outbreak in 2012, a considerable increase in both male and female rates of syphilis was observed, with female rates exceeding male rates since 2014 (Figure 31).
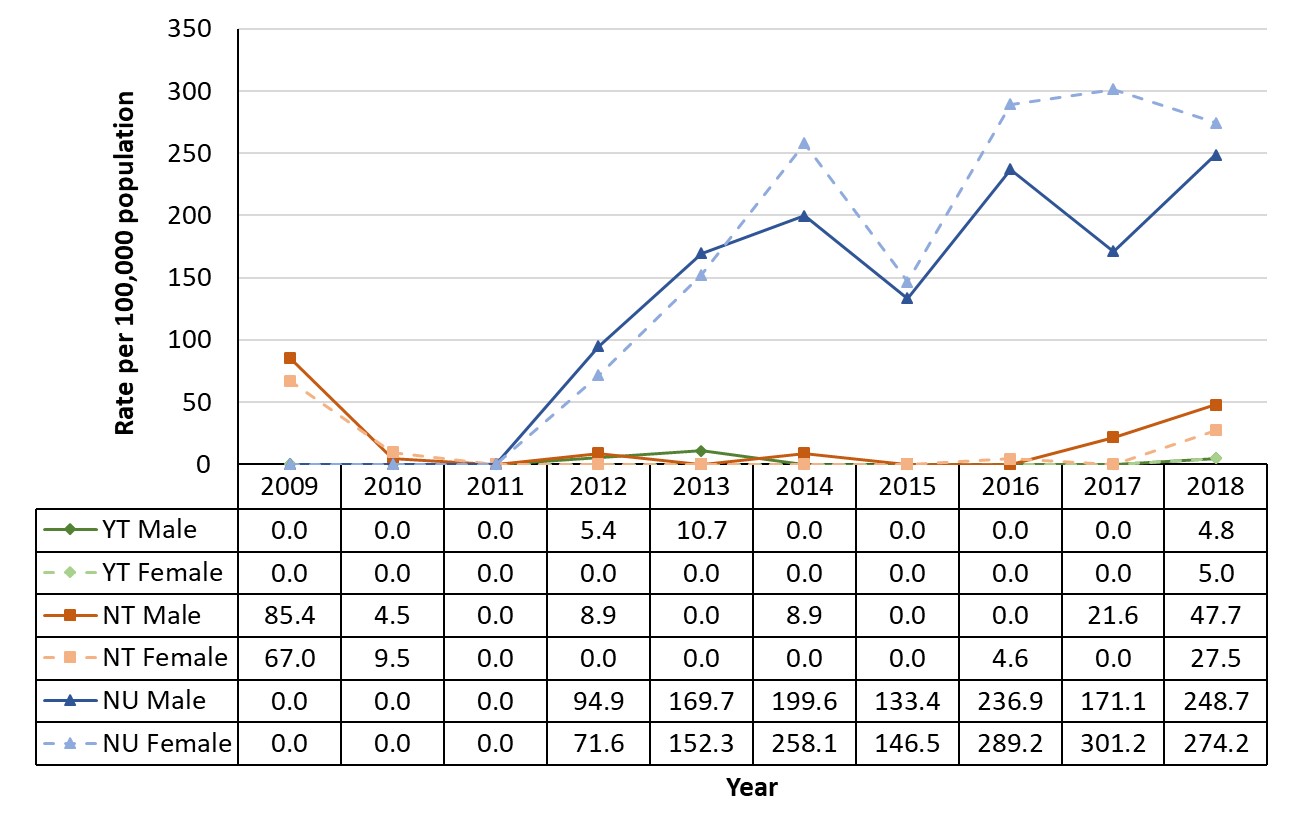
Figure 31 - Text description
This graph displays the rate of reported infectious syphilis cases per 100,000 population in Yukon, Northwest Territories, and Nunavut by sex, between 2009 and 2018. The horizontal axis shows the calendar years from 2009 to 2018. The vertical axis shows the rate of infectious syphilis per 100,000 population per each calendar year for males and females for Yukon, Northwest Territories, and Nunavut respectively.
| Year | Rate per 100,000 population | |||||
|---|---|---|---|---|---|---|
| YT Male | YT Female | NT Male | NT Female | NU Male | NU Female | |
| 2009 | 0.0 | 0.0 | 85.4 | 67.0 | 0.0 | 0.0 |
| 2010 | 0.0 | 0.0 | 4.5 | 9.5 | 0.0 | 0.0 |
| 2011 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| 2012 | 5.4 | 0.0 | 8.9 | 0.0 | 94.9 | 71.6 |
| 2013 | 10.7 | 0.0 | 0.0 | 0.0 | 169.7 | 152.3 |
| 2014 | 0.0 | 0.0 | 0.0 | 0.0 | 199.6 | 258.1 |
| 2015 | 0.0 | 0.0 | 4.4 | 0.0 | 133.4 | 146.5 |
| 2016 | 0.0 | 0.0 | 0.0 | 0.0 | 236.9 | 289.2 |
| 2017 | 0.0 | 0.0 | 21.6 | 0.0 | 171.1 | 301.2 |
| 2018 | 4.8 | 5.0 | 47.7 | 27.5 | 248.7 | 274.2 |
Source: Public Health Agency of Canada (2019). Canadian Notifiable Disease Surveillance System. Preliminary 2018 data received directly from provinces and territories.
Yukon
In Yukon, rates increased in 2000, decreased in 2004, and have remained low and stable since then. Less than five cases were reported from 2010 to 2014, and zero cases of infectious syphilis were reported in 2017 (Figure 31). There have not been any recent outbreaks in the territoryFootnote 133. However, a few cases have been reported in 2018.
Northwest Territories
In 2008, the Northwest Territories’ syphilis rates spiked due to an outbreak, which mainly affected the smaller communities in the Territory and a transient population in the urban centre of YellowknifeFootnote 134. The outbreak was resolved by 2010Footnote 134. Since then, the number of reported cases has been low, until a recent resurgence of cases in late 2017, which carried over into 2018Footnote 135Footnote 136. In 2017, five cases were reported, corresponding to a rate of 11.1 per 100,000 population. It should be noted that due to these small numbers, an increase by a few cases is likely to have a large impact on computed rates. An outbreak of syphilis was declared in the Northwest Territories on August 22nd 2019, following a surge of 28 cases of syphilis, including one case of congenital syphilis, the first since 2009. Approximately 70% of these cases were reported in YellowknifeFootnote 135Footnote 137.
Nunavut
The first infectious syphilis case reported in Nunavut since the territory’s creation in 1999 occurred in 2004 (one case). Rates were low until 2012Footnote 6. In 2012, Nunavut’s syphilis rates increased significantly following an outbreak that year, and have remained high since then. In the 2012 outbreak, a slightly higher proportion of cases occurred among females (55% of cases) compared to males (45%)Footnote 138. In the 15 to 19 year age group, most cases were reported among femalesFootnote 139. Risk factors observed during the 2012 outbreak included not using a condom (96% of cases), reported alcohol or substance use (74% of cases; frequency or intensity of consumption was not specified); and having had another STI in the previous year (71% of cases)Footnote 139.
The 2012 outbreak began in the Qikiqtaaluk region (northern-most Baffin region) and was later reported in other regions, affecting five communities. Between 2007 and 2014, 98% of all syphilis cases reported in the territory were from the Qikiqtaaluk region.
Nunavut’s outbreak is ongoing. In 2015, there were 51 infectious syphilis cases reported (139.8 per 100,000), 97 in 2016 (262.3 per 100,000) and 88 in 2017 (234.3 per 100,000). Since 2014, a larger number of cases were reported among females than malesFootnote 54. In 2017, 63% of cases reported by the territory to CNDSS were female, while preliminary 2018 data showed the proportion of female cases to be 51%. In 2017, the highest rate was observed among those aged 15 to 19 years (788.4 per 100,000), followed by those 20 to 24 year of age (680.5 per 100,000) and 25 to 29 years of age (447.8 per 100,000).
4. Determinants and risk factors of syphilis in Canada
4.1 Proposed conceptual framework of the determinants of infectious syphilis
It has been well established that many factors can affect or influence health. Determinants of health include personal, social, economic and environmental factors, such as gender, culture, race, education, employment, physical environments, healthy behaviors and access to health servicesFootnote 140Footnote 141. Several researchers have proposed conceptual frameworks of the determinants of either health behaviours that may place individuals or populations at higher risk of sexually transmissible infections or of the determinants of infectious disease outcomesFootnote 142-145. Figure 32 below is an adaptation of existing frameworks. It summarizes categories of underlying and proximate determinants of syphilis transmission dynamics, infection and disease outcomes.
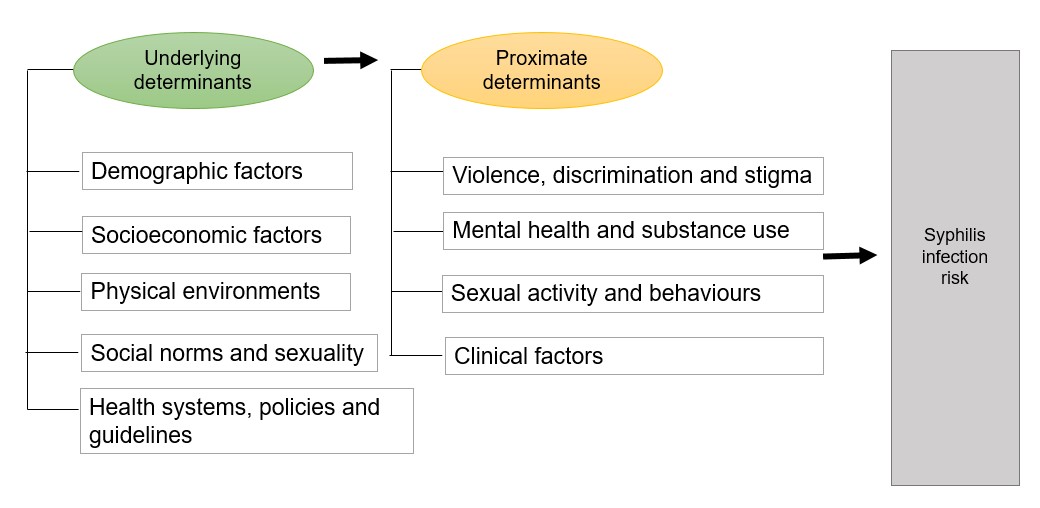
Figure 32 - Text description
Underlying determinants, such as: demographic factors, socioeconomic factors, physical environments, social norms and sexuality, and health systems, policies and guidelines can influence proximate determinants, such as: violence, discrimination and stigma, mental health and substance use, sexual activity and behaviours, and clinical factors, which inadvertedly influence the risk for contracting syphilis infection.
Adapted from frameworks proposed by Boerma and Weir (2005)Footnote 144, Aral (2002)Footnote 143, Galea et al. (2003)Footnote 142, Government of Canada (2019)Footnote 141, Public Health Agency of Canada (2016)Footnote 146, and the British Columbia Centre for Disease Control (2016)Footnote 145 and based on existing published Canadian literature.
Within this framework, factors considered to be “underlying” are those that tend to operate beyond the individual level. They shape the contexts in which individuals live and behaveFootnote 144. These underlying determinants influence individuals’ exposure to or adoption of more proximate determinants of syphilis infection and transmission. Thus, proximate determinants tend to be experienced at an individual level, with ties to either behaviour or biologyFootnote 144. This section summarizes the underlying and proximate determinants of syphilis infection documented in the Canadian literature mainly, as well as in the international literature. Gaps in knowledge and research are highlighted.
4.2 Underlying determinants of syphilis in Canada
4.2.1 Demographic factors
Sex and gender identity
Federal surveillance and studies conducted across Canada on infectious syphilis trends from 2003 to 2017 note significantly higher rates among males compared to females, with males representing the vast majority of cases (over 90%)Footnote 55Footnote 58Footnote 147-149. In Canada, similar to the US, most male syphilis cases are among gbMSMFootnote 150.
As indicated in Section 3, in the 1990s and 2000s, infectious syphilis rates increased at a greater pace for males than for femalesFootnote 55Footnote 149. However, in recent years, rates of infectious syphilis have risen considerably in females, thereby reducing the male-to-female rate ratio. This is especially true for the provinces of Alberta, Saskatchewan and Manitoba, as well as for certain northern communities in other parts of CanadaFootnote 53Footnote 94Footnote 97Footnote 151. As epidemics shift into heterosexual populations, rates appear to be increasing in both heterosexual females and males in certain jurisdictionsFootnote 151.
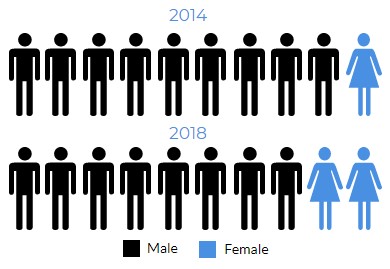
Infographic 1 - Text description
In 2014, females represented 1 infectious syphilis case in every 10 cases. In 2018, females represented 2 infectious syphilis case in every 10 cases.
Source: Public Health Agency of Canada (2019). Canadian Notifiable Disease Surveillance System
Biological sex is a particularly relevant determinant of syphilis staging, as primary lesions may be less visible for females than males, thus making it more difficult for females to know to seek early testing and diagnosisFootnote 2Footnote 58. However, though sex differences in syphilis risk have been observed in Canada, literature suggests that these are likely mostly attributable to gender-based differences in risk behaviours rather than biological risk.
Gender roles, ideologies and norms are key social determinants of STI vulnerabilityFootnote 152-154. For instance, for women, especially in young adulthood, internalization of ‘femininity ideologies’, associated with passivity, compliance, and altruism, can be associated with difficulties in communicating needs or boundaries in sexual relationshipsFootnote 155. This can interfere with sexual agency and protective sexual practices and compromise healthFootnote 155.
Among heterosexual women, research has documented that STI risk can be determined by their partner’s behaviours (number of other partners their partner has, etc.) rather than their own behavioursFootnote 156. In a study conducted in the province of Quebec between 2010 and 2011 (n=51), 51% of female cases reported a recent sexual contact with a partner who was at higher risk of syphilis, either because of their history of substance use, being gbMSM, engagement in sex work, having multiple partners, or having sexual relations outside of CanadaFootnote 122. Sexual violence can also put women at significantly higher risk of STIsFootnote 157.
Additionally, women’s experiences of STI screening and care can also differ from men’s experiences. Specifically, research conducted in the US in 1999, has documented instances where physicians are less likely to recommend syphilis screening for women when an STI is suspected compared to menFootnote 158. More recent Canadian research on STI screening inequities is currently not available.
For men, societal pressures to perform according to masculine norms and ideals can be a considerable source of stressFootnote 159. For example, masculine gender norms can include peer pressure to have multiple sexual partnersFootnote 160. In younger members of the gbMSM population, condomless sexual intercourse has been reported as a normative component in certain settings, as it is associated with a desire for greater intimacy and spontaneityFootnote 161. Condomless sex is, however, a frequent occurrence among heterosexual partners as well. A pan-Canadian survey of adults aged 16 years and older (n=2,452), the majority of which self-identified as heterosexual, noted that 63% of respondents reported inconsistent condom useFootnote 162. Among the 15% of respondents who reported never using condoms, the four most frequent reasons given were trust in their partner (25%), a dislike for condom use (17%), a lack of perceived pregnancy risk when not using condoms (11%), and finding that condoms were not easy to obtain or were too costly (9%)Footnote 162.
All told, factors pertaining to sexuality, gender, partnership status, and related power dynamics can influence risk-taking behavioursFootnote 76. Though not commonly documented in Canadian literature, these factors likely contribute to observed sex differences in syphilis-related outcomes.
Age
Recent Canadian research and surveillance data suggest that younger age is associated with a higher risk of syphilis incidence. Overall, CNDSS data suggest that syphilis incidence has been increasing for most age groups. According to preliminary data provided by the provinces and territories, in 2018, the largest proportion of male cases was observed in the 25 to 39 year age group (48%), while the largest proportion of cases in women—over half (61%)—was observed in the 15 to 29 year age group. These proportions vary slightly across provinces and territories, and across sub-populationsFootnote 58Footnote 122Footnote 163.
It should also be noted that among cases aged 15 years and younger, syphilis infection could occur due to vertical transmission from mother to child. However, syphilis acquired post-natally can also indicate sexual abuse, which has implications for reporting requirements and follow-up recommendationsFootnote 164. In addition, early onset of sexual behaviors (before the age of 15) has been associated with a higher risk of STI. However, high levels of support (from family, school and community) are associated with delayed first intercourseFootnote 165. Section 3.1.3 summarizes infectious syphilis trends in Canada by age groupFootnote 166.
Ethnicity and cultural background
Published Canadian studies suggest that certain ethnocultural groups may be more vulnerable to syphilis than others. Much of the research exploring the association between ethnocultural identity and syphilis infection has been focused specifically on male populations. In such instances, most cases were reported among Caucasian menFootnote 57Footnote 148Footnote 167Footnote 168.
Several studies observed no differences in syphilis incidence risk across racial or ethnic groups. This was the case in two large studies of gbMSM in CanadaFootnote 163Footnote 169. Others indicate that although racial and ethnic minorities represent smaller proportions of cases overall, syphilis incidence has at times been observed to be proportionally higher among these populations than in Caucasians. However, findings vary by geographic location, sex, and subgroup populations. For instance, Quebec reports disproportionately higher rates of infectious syphilis in its northern region of Nunavik, in which 83% of the population are Inuit, compared to other regionsFootnote 122Footnote 170. In another study looking at infectious syphilis among 362 females in the Winnipeg Health Region from 2003 to 2015, 67% of reported cases self-identified as Indigenous, a number of cases disproportionate to the size of the Indigenous population in the city (12% of the population)Footnote 58Footnote 170. These findings echo those from previous outbreaks in the late 1980s and early 2000s in Alberta, in which at least half of female cases identified as First Nations, Métis or InuitFootnote 171Footnote 172. Inuit were also overrepresented in an outbreak in Manitoba in the late 1980sFootnote 173.
Canadian literature has documented that Indigenous Peoples often face syndemic conditions pertaining stigma and discrimination, violence, mistrust of health care systems, and higher rates of concurrent health issues and problematic substance use, all of which are tied to legacies of colonization and structural disenfranchisementFootnote 174. Additionally, lack of information and awareness on sexual health, taboos related to sex, and intergenerational unresolved trauma that is linked with violence, alcohol and substance use, place Indigenous communities at higher risk for experiencing STBBI. These factors indicate a need to consider a syndemic-informed approach designed and led by Indigenous Peoples, to mitigate syphilis risk in First Nations, Inuit and Métis communitiesFootnote 174Footnote 175.
Immigration
Syphilis infections can be acquired abroad through exposure in regions of high incidence. A Canadian study published in 1998 (n=890) determined that approximately 20% of total syphilis cases diagnosed between 1990 and 1994 were identified during immigration screening. Syphilis screening is a component of Canada’s immigration medical assessmentFootnote 176. From 2000 and 2004, a period where Canada received just over two million immigration applications, the average rate of syphilis (infectious and non-infectious) was 110 cases per 100,000 applicants to CanadaFootnote 12. Some of the latter cases were identified (and treated) prior to arrival. Among refugees, whose screening was only upon arrival in Canada, the average rate was 286 cases per 100,000 applicantsFootnote 12. However, recent studies of syphilis rates among immigrants are limited. One study found that in a sample of 442 gbMSM living with HIV in Toronto between 2010 and 2012, those born in Canada or the US had lower odds of syphilis infection (adjusted odds ratio (aOR)=0.41, 95% confidence interval (CI): 0.20, 0.84) than those born in other countriesFootnote 73. Due to the limited number of published studies or reports on the topic, it remains unclear as to what proportion of cases recently diagnosed in Canada may be attributable to infections acquired abroad, or to a heightened risk of infection experienced by immigrants once they arrived in the country.
4.2.2 Socioeconomic factors
Socioeconomic status is considered to be one of the most important social determinants of sexual health-related outcomesFootnote 177. Income, employment status, housing stability, and education shape access to resources needed for health-promoting behaviours, such as healthy sexual practices, as well as access to and use of health care servicesFootnote 177.
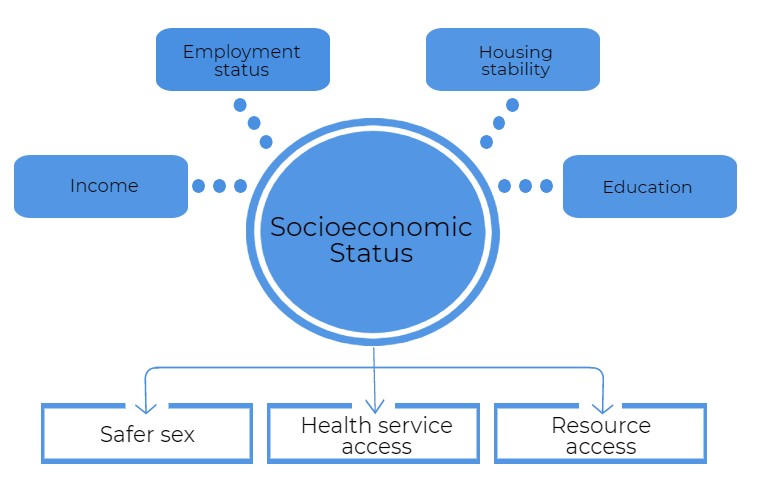
Infographic 2 - Text description
Factors which influence socioeconomic status include: income, employment status, housing stability, and education. Socioeconomic status in turn, influences STI risk factors such as: safer sex, health service access, and resource access.
Currently missing from the Canadian literature is an understanding of the potential differences in socioeconomic determinants of syphilis incidence across genders. Additional research in this area will be valuable, as these factors may influence the effectiveness of surveillance and prevention activities.
Income
An ecological study conducted in British Columbia between 2005 and 2016 observed a correlation between the proportion of low-income households in an area and increased rates of infectious syphilis among men in that areaFootnote 178. These results aligned with findings from a large ecological study conducted in the US (n=4,472)Footnote 179. However, few studies in Canada have explored the association at an individual level, and results from those have reported mixed results. For example, one pan-Canadian study conducted among 7,872 gbMSM, and another which focused specifically on 2,280 gbMSM living with HIV in Ontario, found no association between income and syphilis diagnosisFootnote 163Footnote 167. In contrast, a Toronto-based study of 442 HIV-negative gbMSM found that individuals with a household income less than $20,000 were more likely to report a syphilis infection than those earning higher incomes (aOR=6.41, 95% CI: 1.84-22.40)Footnote 73.
Education
Mixed results have been reported for the association between educational attainment and syphilis incidence in Canada. The pan-Canadian gbMSM study mentioned above did not find an association between level of education and having a recent syphilis diagnosis (n=7,872)Footnote 163. On the other hand, a study of gbMSM living with HIV in Ontario, found a positive association between individuals with university education level and having a first diagnosis of syphilis compared to those who had completed high school education or lessFootnote 167.
Housing stability
Several jurisdictions across Canada have noted that housing instability and homelessness may be contributing to current syphilis outbreaksFootnote 114Footnote 180. A study comparing reported syphilis cases among heterosexuals in Winnipeg, Manitoba, in 2017-2018, to those diagnosed in 2011-2012, noted that the prevalence of cases reporting no fixed address was higher in more recent years than in the past (15% in 2017-2018 vs. 2% in 2011-2012)Footnote 151. These results aligned with findings from the US, wherein social vulnerability, due to homelessness or precarious housing, has been associated with higher risk of maternal syphilisFootnote 181.
4.2.3 Physical environments
Section 3 of the report covers the case and rate distribution of infectious syphilis per province and territory in Canada. As was noted, considerable variability in rates have been observed across Canada, with the territories and Prairie Provinces most affected. The lowest rates were observed in the Atlantic Provinces. Beyond provincial and territorial distribution of syphilis infection, reports have also explored geographic heterogeneity in case distribution within jurisdictions. Though the highest levels of incidence have largely been observed in urban settings across the country, some rural areas have seen high rates as well. For example, in their reporting of infectious syphilis cases across regions in British Columbia, in 2018, the BCCDC described how rates varied from 2 cases per 100,000 population in the more rural interior and northern regions of the province to 70.9 per 100,000 in VancouverFootnote 91. In Alberta, rates vary from 10.1 per 100,000 population in the southern health region of the province, up to 70 per 100,000 in the region of EdmontonFootnote 182. Rates were also high in the rural, northern part of Alberta (43.5 per 100,000 population)Footnote 182. In 2017 in Quebec, although cases were observed in all regions of the province, the highest rates were observed in the northern region of Nunavik (236.3 per 100,000)Footnote 122.

Detailed analyses of the association between rural or urban residence and syphilis risk are currently lacking in Canada. One cross-sectional pan-Canadian study of gbMSM (n=7,872) noted no association between area of residence (urban vs. suburban and rural) and odds of recent syphilis diagnosis after adjustment for other sociodemographic factorsFootnote 163. No recent studies have explored potential differences in risk associated with area of residence in women. Recent studies are also lacking on the role of mobility within or across provinces. In the early 2000s, a study of 102 reported syphilis cases in Ottawa noted that movement between major cities in Quebec and Ontario were common among the gbMSM population, which likely contributed to parallel rises of cases in both provincesFootnote 183. Early evidence suggests that interprovincial mobility may also be contributing to transmission dynamics in northern Manitoba and Ontario in 2018 and 2019Footnote 184. Lastly, to a smaller extent, population mobility between provinces, as well as between cities and more rural areas, and between Indigenous communities and off-reserve communities, also present an additional challenge for syphilis outbreak control in CanadaFootnote 116Footnote 185
Incarceration
In Canada, there is a paucity of studies assessing the association between an individual’s experience of incarceration, or their partner’s experience of incarceration, and syphilis risk. In a study conducted in the US found that among congenital syphilis cases, mothers with personal experiences of incarceration or having a partner who experienced incarceration may have places them at higher risk of syphilisFootnote 181. Some jurisdictions across Canada have noted a potential correlation between the incarceration of index patients or their partners and increased syphilis riskFootnote 185. A study comparing heterosexual syphilis cases identified in Winnipeg, Manitoba, in 2017-2018, to those diagnosed in 2011-2012, found that the prevalence of cases reporting a history of incarceration was higher in more recent years than in the past (36% in 2017-2018 vs. 14% in 2011-2012)Footnote 151.
4.2.4 Social norms and sexuality
With the advent of hormonal contraception in the 1960s during the sexual revolution, changes in sexual behaviors and shifts in population-level sexual culture and norms worldwide are believed to have influenced STI riskFootnote 186. Although findings on the association between oral hormonal contraception use and reported number of partners and condom use are mixed, studies have noted that women who have a regular partner are more likely to use hormonal contraception without barrier methods because of the low risk of unintended pregnancy, as well as low STI risk perceptionFootnote 187.
Among the most important secular changes observed globally since the 2000s has been the growing uptake of internet-based dating apps and websitesFootnote 83. In the 2017 European Men-Who-Have-Sex-With-Men Internet Survey (EMIS), which surveyed 6,059 Canadian gbMSM respondents, 54% reported using a mobile phone app for partner finding, and 74% reported having met their current non-steady partner onlineFootnote 188. However, it should be noted that the latter findings are likely over-estimations due to the survey’s reliance on websites and apps for respondent sampling. For reference, a 2013 phone survey in Canada, 50% of 1,830 gbMSM interviewed noted that they had used internet sites to meet partners in the previous six monthsFootnote 189. Nonetheless, the frequency of use for dating apps and websites has been noted to vary according to the population’s age, gender, and ethnicityFootnote 190.
The rise in the use of dating apps and websites marks a shift in social norms and sexuality in Canadian society. Among gbMSM communities in particular, these changes highlight a shift in norms between age cohorts. For example, a qualitative study of 31 gbMSM in Toronto noted that compared to peers who lived through the 1980s and 1990s, a time during which there was a higher perceived risk associated with anal sex, younger cohorts had different views. These younger cohorts described current social expectations of condomless sex and greater concerns for having “good sex”, rather than reducing STI riskFootnote 191. The use of dating apps and platforms among gbMSM has been associated with greater numbers of reported sexual partners and higher odds of inconsistent condom useFootnote 192Footnote 193.
Among women, evidence suggests that dating app or website use is correlated with a higher number of sexual partnersFootnote 194. In a study of 362 reported syphilis cases in the Winnipeg Health Region, a statistically significant higher proportion of female cases (n=52) indicated having met partners on websites or online in 2014-2015 (18%) compared to 2003-2005 (0%)Footnote 58.
Although these platforms are associated with certain behaviours that may place individuals at higher risk for syphilis, they also represent sites for potential social marketing for STBBI prevention, and have indeed been leveraged for such purposes by public health actors in Canada and abroadFootnote 189.
Lastly, many studies report that certain social or cultural understandings of syphilis may also be contributing to its emergence in several settings in Canada. For example, two qualitative studies with small samples have documented how, for many gbMSM, syphilis can be viewed as something that is more treatable and manageable than HIV, making it of lesser concern in sexual health decision-makingFootnote 62Footnote 191.
4.2.5 Health systems, policy and guidelines
In addition to shifts in culture and norms, elements of health policy and systems are also believed to influence STBBI risk at a population level.
Screening guidelines
The implementation of, or changes to, screening guidelines for STBBI can influence screening uptake. For example, in 2012, cervical cancer screening guidelines changed recommendations to a lower frequency of Papanicolaou (Pap) testing in Canada– shifting from screening every year to every three years after becoming sexually active or after reaching the age of 21 yearsFootnote 195.Since then, it has been documented that screening for chlamydia and gonorrhea has decreasedFootnote 196-198. Screening rates declined the most among females 15 to 19 years of age, following the change in guidelines, since it results in fewer opportunities for health professionals to screen for STIsFootnote 198. A study carried out at a Toronto, Ontario hospital, which looked at 200 women aged 19 to 25, found that they had lower odds of being tested for syphilis after the release of the updated guidelines compared to beforeFootnote 196. Despite a limited number of studies exploring the effects of such guideline changes, researchers have recommended that clinicians be vigilant to identify higher risk individuals and recommend STBBI testing when patients present themselves to clinical settingsFootnote 198Footnote 199.
Other factors influence STI screening uptake. For example, HIV screening barriers can occur at the patient level (e.g., low risk perception, fear, difficulty accessing services), the healthcare provider level (e.g., lack of time, staff, knowledge) and at the institutional/policy level (e.g., cost of testing delivery and access, impact on other medical services). In addition to screening guidelines, interventions to increase the availability of STI tests and to introduce testing into new settings (e.g., making HIV testing available as a routine service at the healthcare provider and institutional level), as well as improve awareness and knowledge about STIs, should be promotedFootnote 200-202.
Sexual education
In Canada, sexual education is within provincial jurisdiction, and is believed to be a key determinant in population-level knowledge of STBBI risk factors and risk reduction methodsFootnote 203Footnote 204. Indeed, in a 2002-2003 survey of 3,536 Canadian high school students, 51% of boys and 41% of girls indicated that school was their main source of information about human sexuality and sexual healthFootnote 205. In another survey of 2,310 teenagers and their mothers in 2005, school was also noted as one of the most valuable providers of sexual health-related informationFootnote 206. However, studies also note limits to the effectiveness of current sexual health curriculums in informing teenagers about STI risk factors and transmission methods in Canada, and propose that these educational gaps may be contributing to high STI prevalence among younger adults in the countryFootnote 206. Recent studies of the effects of sexual education reform in Canada on STI risk, and particularly on syphilis risk, are not available and remain an area of interest for future policy planning. The Sex Information and Education Council of Canada (SIECCAN) leads a series of project activities to increase the capacity of the education sector to provide effective sexual health education, including the revision and dissemination of the Canadian Guidelines for Sexual Health EducationFootnote 204.
4.3 Proximate determinants of syphilis in Canada
4.3.1 Violence, discrimination and stigma
Though the body of existing research is limited, it does suggest that an individual’s experience of violence and discrimination may affect their risk of acquiring a syphilis infection. In a national study of 7,872 gbMSM in Canada, intimate partner violence, defined as being threatened, emotionally abused, or physically assaulted by a partner, boyfriend, or sexual partner, was reported by 13% of respondentsFootnote 163. Those who experienced intimate partner violence had more than two times the odds of reporting a recent syphilis diagnosis, after adjustment for individual-level sociodemographic characteristics and HIV status (aOR=2.3, 95% CI: 1.7-3.1) compared to those who did not. This finding is consistent with research conducted outside of Canada in women experiencing intimate partner violence who have been shown to experience higher STI riskFootnote 207Footnote 208. Experiences of intimate partner violence can be a barrier to individuals’ self-efficacy in negotiating condom use, thereby placing individuals at higher risk of STI infection.
In the same pan-Canadian gbMSM study referenced above, participants were also asked if they had experienced homophobic discrimination in the health care system within the last 12 months. Of the 7,872 survey respondents, 3% reported having experienced health care discrimination. These individuals had four times higher odds of reporting a recent syphilis diagnosis (aOR=4.1, 95% CI: 2.4-7.0)Footnote 163. Discrimination in health care settings can shape individuals’ likelihood of undergoing regular STI screening. Conversely, researchers have noted the potential importance of emergency room departments as sites of screening and other programs pertaining to STIs and intimate partner violence, given their importance for individuals with limited health care access or who use health care services infrequentlyFootnote 208. Improving the cultural competency of health professionals to minimize discrimination and bias for sexual minorities and other groups has also been identified as an area for potential intervention to address STI risk and transmissionFootnote 163Footnote 174.
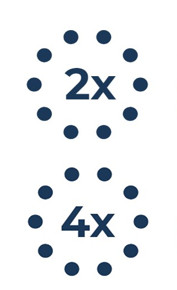
Those who experienced intimate partner violence had over two times the odds of reporting a recent syphilis diagnosis (Ferlatte, 2018).
Those who experienced health care discrimination had over four times the odds of reporting a recent syphilis diagnosis (Ferlatte, 2018).
As recognized by the Truth and Reconciliation Commission Report, experiences of discrimination and stigma are common among Indigenous Peoples accessing health care services in Canada. These are a direct result of historical colonial policies, including the Residential School systemFootnote 174Footnote 209. These elements represent important structural barriers to health-promotion services including STI testingFootnote 210. Harm reduction practices that do not stigmatize substance use, and that integrate components of mental, spiritual, and emotional health, have been identified as promising strategies to address the latter barriersFootnote 210.
4.3.2 Mental health and substance use
Mental health
Similarly to experiences of violence and discrimination, mental health issues, such as anxiety and depression, have been associated with lower self-esteem and self-efficacy in negotiating condom useFootnote 159. In Canada overall, there remains a paucity of studies exploring the association between mental health issues and increased syphilis risk. What has been documented, however, is the high prevalence of affective symptomatology among populations who are typically at higher risk of syphilis. For example, in a 2014-2015 study of 7,872 gbMSM in Canada, participants were ask if they had mental health issues in the last 12 monthsFootnote 163. Among them, 19% reported having suicidal thoughts or ideations and 30% reported depressive or anxiety symptoms.
In addition, a few studies have focused on the association between substance use and syphilis risk, as mental health issues have been, at time, correlated with substance use-related issues. Substances, such as alcohol or other drugs, are sometimes used to self-medicate against affective symptomatology, and their consumption can sometimes lead to dependence and substance use issuesFootnote 211.
Alcohol
Regarding syphilis risk specifically, a study of 194 people living with HIV attending a sexual health clinic in Alberta between 2006 and 2016, found that individuals with a history of problematic alcohol use (>14 drinks per week or binge drinking) were more likely to have tested positive for a syphilis infection compared to those who did not report such behaviorFootnote 72. The latter findings are consistent with those from a Winnipeg Health Region study in 2014-2015 that found that 21% of 362 cases of infectious syphilis reported alcohol use (without specification of frequency or quantity)Footnote 58. In that study, females with infectious syphilis were more likely to report alcohol use than their male counterparts (53% vs. 18%, p value<0.001)Footnote 58. Problematic alcohol use continues to be an issue across several populations. A Canadian study of 7,872 gbMSM in 2014-2015, noted that at least 7% of participants reported binge drinking in the past yearFootnote 163.
Injection and non-injection drug use
In a study of 442 gbMSM who were HIV-negative in Toronto, injection drug use was more common in individuals with syphilis infections than those without (21% vs. 2%)Footnote 73. Additionally, in the US, among primary and secondary syphilis cases, the proportion of women that reported using injection drugs increased from 4.0% to 10.5% between 2013 and 2017, while it increased from 2.8% to 6.3% in men who have sex with womenFootnote 212. Injection drug use was stable among gbMSM for the same time period. Existing studies suggest that non-injection drug use may be a more common risk factor than injection drug use. For example, among 164 infectious syphilis cases identified in Winnipeg in 2014-2015, 2% of cases reported injection drug use and 18% reported non-injection drug useFootnote 58. Though the latter study did not provide information on the type of drug or frequency of use, it noted that the prevalence of non-injection drug use has been increasing over time among female infectious syphilis cases (4% reported use in 2003-2005, 13% in 2006-2013, and 29% in 2014-2015)Footnote 58. In the US, Kidd et al. also observed that although there were increases in heroin use from 0.8 to 1.7% between 2013 and 2017, the prevalence of methamphetamine use was the highest, among drugs included in the study (7.9% in 2013 to 9.6% in 2017)Footnote 212. This increase in methamphetamine use was observed in women and in men who have sex with women (from 6.2% to 16.6% and from 5.0% to 13.3%, respectively) and not in gbMSM, suggesting that a substantial proportion of heterosexual syphilis transmission occurs in persons who use these drugs.
In a study of 7,872 gbMSM in Canada in 2014-2015, 16% reported substance use (cocaine, crystal methamphetamine, ecstasy, gamma-hydroxybutyrate (GHB), ketamine, or crack cocaine), and substance use was independently associated with having a recent syphilis diagnosis after adjustment for demographic and socioeconomic characteristics (aOR=2.4, 95% CI: 1.8-3.2)Footnote 163. Such substances may be used recreationally for their ability to reduce inhibitions and increase pleasureFootnote 213. In the context of sexual relations, especially among gbMSM, the term “chemsex” (or Party and Play, “PnP”) refers to the planned use of certain substances to extend the duration (hours to days) and intensity of sexual encounters (number of partners, types of practices)Footnote 84. More recently, increases in crystal methamphetamine (crystal meth) and Viagra® consumption, have been noted as potential contributing risk factors to STBBI outbreaks, especially among gbMSMFootnote 193. In the 2017 EMIS study (n=6,059), 6% of Canadian gbMSM respondents reported engaging in chemsex in the four weeks preceding the surveyFootnote 188. In a Montreal-based sample of the cross-sectional Engage survey of 2017-2018, nearly one-in-ten respondents (9% of 1,179 gbMSM respondents) had consumed a psychoactive drug (GHB, methamphetamine, ketamine, cocaine, or ecstasy) with at least one of his last five sexual partners, in a recreational chemsex contextFootnote 214. Cocaine use was more prevalent (25% had sniffed or inhaled cocaine in the previous six months and 12% had consumed cocaine in the context of chemsex).
While chemsex has predominantly been described as a phenomenon in the gbMSM community, more widespread recreational substance use has been observed across other population sub-groups. Overall in Canada, self-reported lifetime methamphetamine use appears to be increasing for those aged 25 years and over (e.g. from 2.5% in 2015 to 4% in 2017)Footnote 215. Overall, substance use has been associated with higher likelihoods of having condomless sex and of being at higher risk of experiencing STIsFootnote 216.
Historically, consumption of substances, such as crack cocaine, was noted as a determinant of past syphilis outbreaks during the 1990s in both Canada and the USFootnote 217Footnote 218. Crack cocaine use often intersects with experiences of transactional sex, namely as a source of income to support continued substance useFootnote 218. Researchers studying past syphilis outbreaks in British Columbia noted how dense sexual networks of concurrent partnerships were tied to crack cocaine use, transactional sex and limited condom use, and led to an increase of syphilis transmission and risk in both gbMSM and heterosexual populations in the late 1990sFootnote 218. In the latter contexts, partner notification was impeded by index cases’ unwillingness or inability—due to ongoing substance use or due to the anonymity of transactional sex clients—to name their sexual partnersFootnote 218.
Early data from 2018 and 2019 suggest that substance use may be a contributing factor to syphilis risk in certain areas of CanadaFootnote 219Footnote 220. A study comparing heterosexual syphilis cases identified in Winnipeg, Manitoba, in 2017-2018 to those diagnosed in 2011-2012, noted crystal methamphetamine use was more prevalent in the more recent cases (30% in 2017-2018 versus 3% in 2011-2012)Footnote 151. The intersection between mental health, illicit substance use, and syphilis risk merits attention in future Canadian research and surveillance activities.
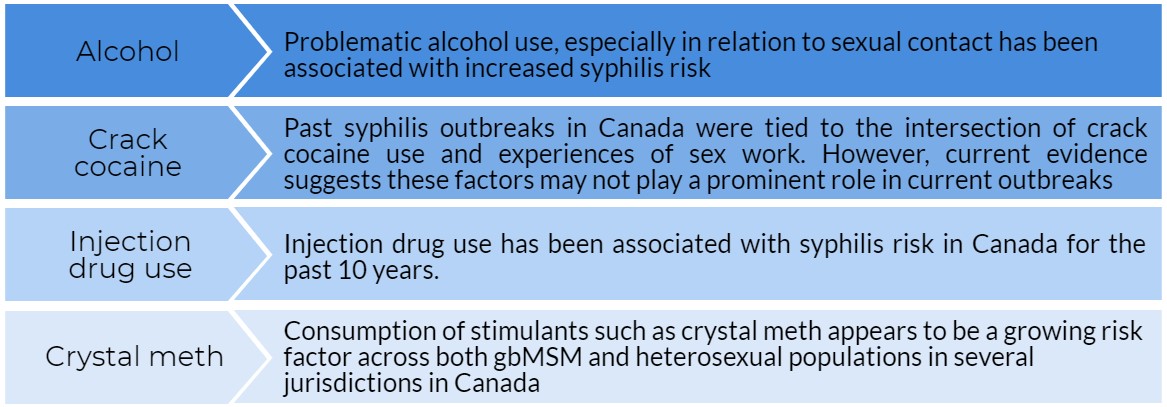
Infographic 5 - Text description
Several substances have been linked with increasing syphilis risk, these substances include: alcohol, crack cocaine, injection drug use, and crystal meth. Problematic alcohol use, especially in relation to sexual contact has been associated with increased syphilis risk. Past syphilis outbreaks in Canada were tied to the intersection of crack cocaine use and experiences of sex work. However, current evidence suggests these factors may not play a prominent role in current outbreaks. Injection drug use has been associated with syphilis risk in Canada for the past decade. Consumption of stimulants such as crystal meth appears to be a growing risk factor across both gbMSM and heterosexual populations in several jurisdictions in Canada.
4.3.3 Sexual activity and behaviors
Condom use and number of partners
Risk of syphilis transmission tends to be higher among those who have a greater number of partners and those who do not use physical barriers, such as condoms, consistently, given that both risk factors increase likelihood of syphilis exposure and infection. Indeed, syphilis outbreak investigations in Canada have consistently noted the association between condomless sex, multiple sex partners and syphilis infection across provincesFootnote 58Footnote 73Footnote 148Footnote 163Footnote 221. Though these risk factors are relevant for both male and female cases, gbMSM appear to be at particularly high risk of syphilis, due in part to a high prevalence of multiple sexual partners and the risk associated with condomless sexFootnote 73Footnote 163Footnote 221Footnote 222. Though multiple reasons can explain inconsistent condom use, including low perceived STI risk, the 2017 EMIS survey noted that 22% of Canadian gbMSM respondents did not consistently use condoms due to issues of availability and accessFootnote 188. Population-level gaps in access to condoms remain a public health issue in Canada.
Sex in public venues
Certain studies note that the venues in which sexual activities are engaged in can also be correlated with higher syphilis risk, mainly due to their associations with inconsistent use of condoms or a higher number of sexual partnersFootnote 188. For example, Canadian studies note an association between attendance at sex venues or cruising locations, such as bathhouses and saunas and syphilis risk, especially among gbMSMFootnote 58. Following a spatial network investigation of a syphilis outbreak in Toronto between 2006 and 2010, researchers identified certain bathhouses as sites contributing to syphilis transmission in the network of gbMSM in the city, even if only 6% of surveyed cases had indicated having met sexual partners at the bathhouses in questionFootnote 221. Attending bathhouses was also reported by 6 of 17 cases surveyed in a social network investigation of a 2009-2010 Ottawa syphilis outbreakFootnote 148. Though public venues such as saunas, sex clubs, or bars are not as commonly used for sex by gbMSM as private dwellings, group sex or sex with multiple partners tend to be more common in public sites, as is consumption of substances, such as nitrite inhalants (poppers) or erectile dysfunction medicationsFootnote 58Footnote 188. For these reasons and for accessibility reasons, venues such as bathhouses and saunas remain of particular importance for targeted STBBI prevention efforts. The 2017 EMIS survey indicated that 46% of Canadian gbMSM respondents reported that they obtained condoms in targeted locations, including bars or saunas in the previous yearFootnote 188. They also represent potential sites for targeted STI screeningFootnote 223.
Transactional sex
Lastly, while the sale or purchase of sex was associated with syphilis risk in past outbreaks in Canada, it does not appear to be a driving factor behind syphilis emergence in more recent yearsFootnote 218. In the few studies that explore history of transactional sex among syphilis cases since 2008, it was noted that the majority of male and female cases were not engaging in the sale or purchase of sexFootnote 58. However, though few recent publications explore the potential association between transactional sex and syphilis infection, risk remains, especially if other concurrent factors such as substance use are present. For example, the Middlesex-London Health Unit recently declared a syphilis outbreak and reported that increases in the number of cases are also being seen among people who have sex with the opposite sex and people engaging in transactional sexFootnote 118. From another perspective, human trafficking for sexual exploitation in Canada, in which women and girls are most often victims, is a context where sexual abuse and violence is commonFootnote 224Footnote 225. Both of these determinants are well known to increase the risk of STI and HIVFootnote 71Footnote 76Footnote 224Footnote 225.
4.3.4 Clinical factors
HIV co-infection
Historically, syphilis incidence has been correlated with incidence of other STBBI, especially HIV since the 1980sFootnote 222. The concurrence of STBBI infections, such as HIV, is an important determinant of syphilis incidence for reasons noted previously in Section 2. That is, HIV infection can impair syphilis clearance, lead to more rapid progression through the disease stages, and result in complicated treatmentFootnote 2Footnote 75Footnote 148Footnote 221.
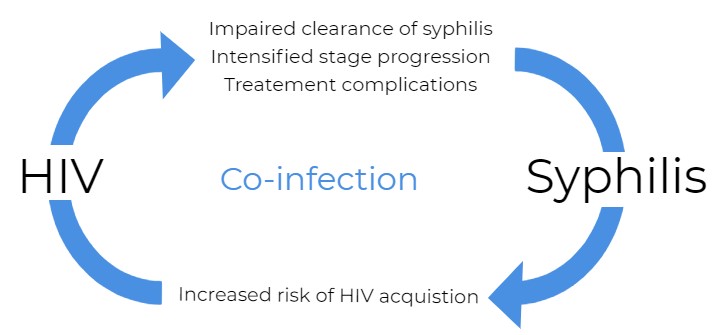
Infographic 6 - Text description
HIV influences syphilis by impairing clearance, intensifying stage progression, and causing treatment complications. In turn, syphilis also influences HIV by increasing its risk of acquisition.
Across Canadian provinces and territories, studies have documented syphilis and HIV co-infectionsFootnote 78Footnote 226. A study investigating a syphilis outbreak in Ottawa (n=72) looked at the characteristics of infectious syphilis cases and noted that 26% had a coinfection with HIVFootnote 148. In a cross-sectional study of syphilis cases among Toronto males between 2006 and 2010, 47% of cases occurred in people living with HIVFootnote 221. Among 119 ocular syphilis cases identified in Montreal, Quebec between 2000 and 2015, approximately 48% were living with HIVFootnote 221. In recent years, HIV and syphilis co-infection have tended to be more prevalent among gbMSM populations in Canada, compared to other populationsFootnote 57Footnote 73Footnote 163Footnote 167Footnote 169. Recent Canadian studies suggest that younger (less than 30 years of age) gbMSM who report higher numbers of partners, condomless anal intercourse, and injection drug use or problematic alcohol use, are at particularly high risk of HIV and syphilis co-infectionFootnote 72Footnote 73Footnote 167. In a British Colombia study, all individuals who reported more than three infectious syphilis diagnoses between 2005 and 2014 (n=30) identified as gbMSM, and a majority (96%) were living with HIVFootnote 78. HIV infection and its associated risk factors appears to represent a risk factor for both syphilis infection and re-infection in Canada.
It should be noted that the association between HIV and syphilis infection does not hold true for every population. A 2009-2010 cross-sectional study that looked specifically at STI co-infections among 126 HIV-positive and 291 HIV-negative African-Caribbean women recruited in downtown Toronto, found that syphilis prevalence did not significantly differ by HIV status (0.8% vs. 0.3%)Footnote 73. Similarly, in a Winnipeg-based study, all of the female infectious syphilis cases in 2014-2015 (n=17) were HIV-negative individualsFootnote 58. The few small studies that focus on female syphilis cases suggest that female cases may be at higher risk of co-infection with other STIs, such as chlamydia compared to male syphilis casesFootnote 58. However, associations between HIV, syphilis, and both gonorrhea and chlamydia infections have been reported in both males and females in CanadaFootnote 72.
Lastly, there were no notable associations found in Canadian studies that have assessed the impacts of HIV antiretroviral therapy or viral load suppression on syphilis risk among people living with HIVFootnote 72Footnote 167.
HIV pre-exposure prophylaxis (PrEP)
Concerns have been raised suggesting that the use of pre-exposure prophylaxis (PrEP) could lead individuals to engage in condomless sexual practices due to their perception of a decreased risk of HIV acquisition. However, very few Canadians studies have looked at the relationship between the use of HIV PrEP and the risk of syphilis. Furthermore, measuring such associations is challenged by various sources of bias. For example, insofar as PrEP therapy requires regular STI screening, those on PrEP are more likely than their peers to be screened for other STIs. One Montreal-based study conducted on 195 gbMSM observed a significant association between the prescription of PrEP and the number of all STI cases (chlamydia, gonorrhea, and syphilis) reported among gbMSM in the subsequent year, compared to the year prior to prescriptionFootnote 228. However, after adjustment for frequency of screening visits during the 12 months before and after PrEP prescription, the association between PrEP use and STI infection was not significant (adjusted incidence rate ratio (aIRR)=1.4 , 95% CI: 0.98-1.96). Similarly, this relationship did not hold when looking at the risk of syphilis acquisition, specifically (aIRR=1.5, 95% CI: 0.6-3.4)Footnote 228.
Similarly, a longitudinal Australian study following 2,981 gbMSM who received daily PrEP was found that STI incidence increased from before- to after- commencing PrEP with the increase greatest for chlamydia infection (adjusted incidence rate ratio=1.12, 95% CI: 1.02-1.23). However, after adjusting for testing frequency between periods, no significant change in syphilis incidence was observed in the group of participantsFootnote 229. Although these studies have not been able to show an association, it should be noted that other studies have shown that PrEP use was associated with condomless sex and increases in STIsFootnote 230Footnote 231. In communities in which PrEP was widely used, condom use decreased even in gbMSM not using PrEPFootnote 231Footnote 232. Similarly, a higher incidence of STIs and faster time to first symptomatic STI was observed in a US longitudinal study among gbMSM on PrEP (n=365) compared to gbMSM not using PrEP (n=730)Footnote 233. The adjusted IRR for early syphilis was 2.9 (95% CI: 1.5-5.6), comparing PrEP users to nonusers. Time to first symptomatic STI was of 120 days (95% CI: 77-171) among PrEP users compared to 185 days (95% CI: 163-256) among non-users.
Other STBBI co-infection
Beyond HIV, associations between syphilis and chlamydia and gonorrhea risk have also been explored in Canada. A British Columbia study of 133,264 individuals who were diagnosed with either chlamydia or gonorrhea between 2006 and 2017, found that individuals who subsequently received a syphilis diagnosis were more likely to be men, to live with HIV or have a history of lymphogranuloma venereumFootnote 234. Among a sample of female infectious syphilis cases in Winnipeg between 2003 and 2015, 24% had concomitant chlamydia infection, while few presented with HIV (7%) or gonorrhea (4%)Footnote 58. Recent studies suggest that syphilis, chlamydia and gonorrhea co-infections may be on the rise in certain populations in Canada. For example, a study comparing heterosexual syphilis cases identified in Winnipeg, Manitoba, in 2017-2018, to those diagnosed in 2011-2012, noted that chlamydia was more prevalent in recent cases (23% co-infection in 2017-2018 vs. 10% in 2011-2012), as was gonorrhea (21% vs. 3%)Footnote 151.
Lastly, a study conducted between 2005 to 2018 among 4,139 gbMSM in Montreal found no association between HCV infection and higher likelihood of current or lifetime syphilis infectionFootnote 235. However, this form of co-infection remains understudied.
Key messages
- Experience of violence and discrimination increase the likelihood of recent syphilis diagnosis.
- Mental health issues such as anxiety and depression have been associated with lower self-esteem and self-efficacy in negotiating safer sex practices.
- Crystal methamphetamine consumption has been noted as a potential contributing factor to increased syphilis rates, especially among gbMSM.
- Inconsistent condom use and multiple sex partners have been consistently associated with syphilis outbreaks in Canada.
5. Congenital syphilis: trends, determinants and response
5.1 Congenital syphilis trends in Canada over the past 25 years
According to CNDSS data, from 1993 to 2004, the number of confirmed congenital syphilis cases reported was low, ranging from one to four cases per year, corresponding to a rate of 0.3 to 1.2 cases per 100,000 live births (Figure 33, Appendix G). Since 2004, the number of cases reported yearly has fluctuated, with the highest number of cases reported in 2009 (ten cases). The number of congenital syphilis cases dipped between 2013 and 2014, but has been on the rise ever since. There were seven confirmed congenital syphilis cases in 2017 (1.9 cases per 100,000 live births). In 2018, the number of cases more than doubled to reach 17 confirmed cases (4.6 per 100,000 live births). It is expected that the number of cases in 2019 will exceed 50 cases. Further details on recent congenital syphilis trends are described in Section 5.2 below.
The WHO defines women of reproductive age as 15 to 49 years of age. However, as CNDSS uses different age groupings, the computation of rates for this age group is not possible. Instead, the CNDSS age grouping of 15 to 39 years of age is used to capture females of reproductive age, although this will underestimate the true number of females of reproductive age. Over time, the rate of congenital syphilis has loosely followed the rate of infectious syphilis among females of reproductive age, which while relatively low in the 1990s, has increased steadily until peaking in 2018 with 19.0 cases per 100,000 females, more than triple the 2017 rate of 6.2 cases per 100,000 females (Figure 33, Appendinx G). The overall female rate in 2018 reached 7.0 cases per 100, 000 females, compared to only 2.4 cases per 100,000 females in 2017. These data highlight the increased population-level risk for vertical transmission of syphilis infections.
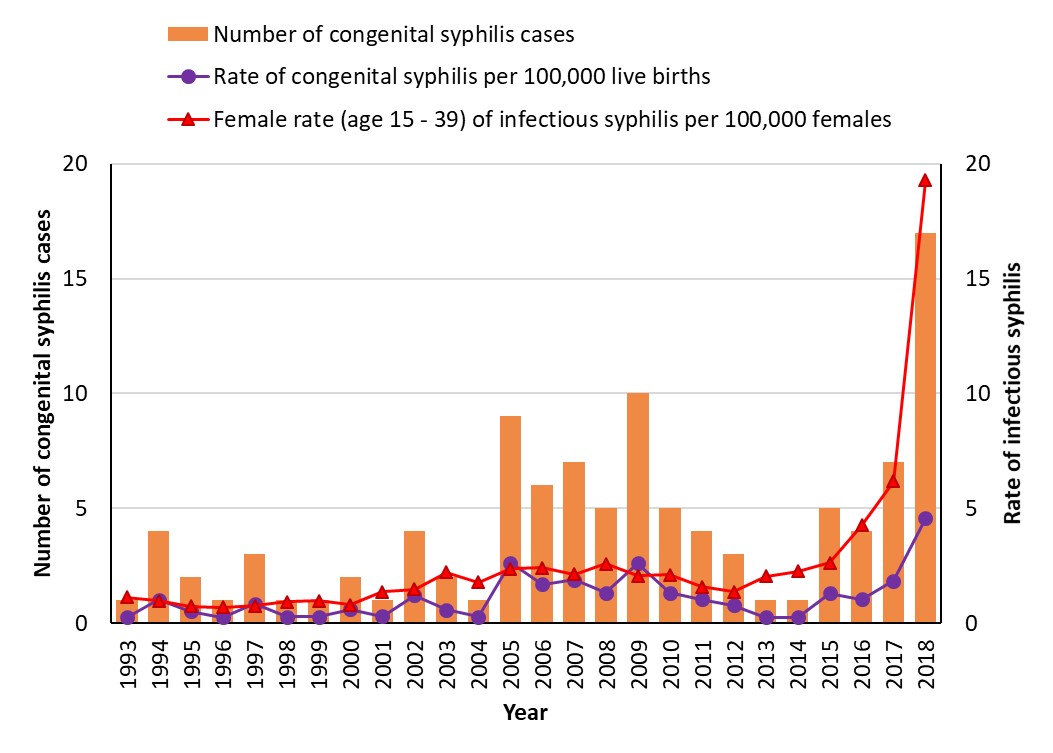
Figure 33 - Text description
This graph displays the number and rates of congenital syphilis among females of reproductive age in Canada, from 1993 to 2018. The horizontal axis shows the calendar years from 1993 to 2018. The vertical axis shows the number of congenital syphilis cases, the rates of congenital syphilis per 100,000 live births, and the female rate of infectious syphilis per 100,000 females per each calendar year.
| Year | Number of Congenital Syphilis Cases | Rate of Congenital Syphilis per 100 000 Live Births | Female rate (age 15 to 39) of Infectious syphilis per 100 000 females |
|---|---|---|---|
| 1993 | 1 | 0.3 | 1.1 |
| 1994 | 4 | 1.0 | 1.0 |
| 1995 | 2 | 0.5 | 0.7 |
| 1996 | 1 | 0.3 | 0.7 |
| 1997 | 3 | 0.9 | 0.8 |
| 1998 | 1 | 0.3 | 0.9 |
| 1999 | 1 | 0.3 | 1.0 |
| 2000 | 2 | 0.6 | 0.8 |
| 2001 | 1 | 0.3 | 1.4 |
| 2002 | 4 | 1.2 | 1.5 |
| 2003 | 2 | 0.6 | 2.2 |
| 2004 | 1 | 0.3 | 1.8 |
| 2005 | 9 | 2.6 | 2.4 |
| 2006 | 6 | 1.7 | 2.4 |
| 2007 | 7 | 1.9 | 2.1 |
| 2008 | 5 | 1.3 | 2.6 |
| 2009 | 10 | 2.6 | 2.1 |
| 2010 | 5 | 1.3 | 2.1 |
| 2011 | 4 | 1.1 | 1.6 |
| 2012 | 3 | 0.8 | 1.4 |
| 2013 | 1 | 0.3 | 2.1 |
| 2014 | 1 | 0.3 | 2.3 |
| 2015 | 5 | 1.3 | 2.6 |
| 2016 | 4 | 1.0 | 4.3 |
| 2017 | 7 | 1.9 | 6.2 |
| 2018 | 17 | 4.6 | 19.3 |
Source: Public Health Agency of Canada (2019). Canadian Notifiable Disease Surveillance System. Preliminary 2018 data received directly from provinces and territories.
5.2 Epidemiological situation across Provinces and Territories
Over time, congenital syphilis incidence in Canada has varied across provinces and territories. Between 2016 and 2019, seven provinces and one territory published reports that included information relating to congenital syphilis cases. Of these, two provinces—Manitoba and Quebec—described maternal risk factor information. No congenital syphilis information was publicly available for Saskatchewan, Nova Scotia, Prince Edward Island, Yukon and Nunavut. Note that national surveillance data only present confirmed cases. Several probable cases have been reported in various jurisdictions (Alberta, Saskatchewan, Manitoba and Quebec all have probable case definitions for early congenital syphilis). PHAC will begin work on the revision of the national syphilis case definitions in 2020.
5.2.1 Pacific Region: British Columbia
From 2008 to 2017, five cases of congenital syphilis were reported to CNDSS by British Columbia. The BCCDC’s 2016 STI report indicated that the number of prenatal syphilis tests performed each year was steadily increasing and that 51,377 prenatal syphilis tests were conducted in 2016, resulting in the identification of eight maternal syphilis cases that did not lead to congenital casesFootnote 92. In 2019, two cases of congenital syphilis were reported in British Columbia, making these cases the first reported since 2013Footnote 236.
5.2.2 Prairie Region: Alberta, Saskatchewan and Manitoba
In Alberta, between 2015 and 2016, one confirmed congenital syphilis case was reported to CNDSS. In 2017, four confirmed cases of early congenital syphilis and three probable cases of congenital syphilis were reported by the provinceFootnote 94. By 2018, the number of confirmed and probable cases in Alberta doubled (eight confirmed cases—one of whom was stillborn—and six probable cases). According to preliminary data, in 2019, 40 cases, including confirmed, probable and stillborn cases of congenital syphilis were reported in the province—more than 30 of which were identified in the Edmonton regionFootnote 237. Some of the risk factors associated with these cases included homelessness, insecure housing and substance useFootnote 238. Most women had not received prenatal care or did not receive it early enough to prevent vertical transmission of the infection.
From 2008 to 2017, Saskatchewan reported one case of congenital syphilis to CNDSS. According to 2019 Saskatchewan news releases, recent cases of syphilis were reported in pregnant women; however, cases received medical treatment, which prevented the vertical transmission of the infection, and no congenital cases of syphilis were reported in the first five months of 2019Footnote 239.
In 2015, the Manitoba government reported one case of congenital syphilis, the first case in the province in over 30 yearsFootnote 53Footnote 240. In 2017, another case was identifiedFootnote 241. On February 25th, 2019, the government of Manitoba informed health care providers that at least ten infants had been treated for congenital syphilis in the previous six months, and that substance use and lack of prenatal care were risk factors associated with identified casesFootnote 109. So far, in 2019, the number of congenital syphilis cases reported by Manitoba is among the highest of all the Canadian provinces and territories.
5.2.3 Central Region: Ontario and Quebec
From 2008 to 2017, Ontario reported ten confirmed cases of congenital syphilis to CNDSS. One case was reported in 2018, followed by two additional cases identified between January and August 2019Footnote 112Footnote 242Footnote 243. Although the Ontario Northwestern Health Unit, which borders Manitoba, experienced an outbreak of infectious syphilis in 2019, no cases of congenital syphilis were reported in this region between January and March 2019Footnote 184Footnote 244.
From 2008 to 2017, five confirmed cases of congenital syphilis were reported to CNDSS from Quebec. Most recent available provincial reporting suggests that three cases of congenital syphilis were reported in 2016, followed by one case in 2017, one in 2018 and two in 2019Footnote 121Footnote 122. Lack of prenatal care or delayed prenatal care and treatment was a factor identified in most cases diagnosed between 2016 and 2018.
5.2.4 Atlantic Region: New Brunswick, Nova Scotia, Prince Edward Island and Newfoundland and Labrador
Overall, Nova Scotia, Prince Edward Island and Newfoundland and Labrador did not report any cases of congenital syphilis to CNDSS from 2008 to 2017. In the same time period, New Brunswick reported two cases of congenital syphilis to CNDSS, one of which occurred in 2017Footnote 123. In 2018, one case of congenital syphilis was identified by the Eastern Health authority of Newfoundland and LabradorFootnote 245.
5.2.5 Northern Region: Yukon, Northwest Territories and Nunavut
From 2008 to 2017, neither Yukon nor Nunavut reported any congenital syphilis cases, while the Northwest Territories reported two cases to CNDSS during that period. In 2019, the Northwest Territories Health and Social Services reported another case of congenital syphilis—the same year for which the territory declared a pan-territorial syphilis outbreakFootnote 135Footnote 137.
5.3 Factors associated with Canadian trends
Very few publications in Canada have reported on the determinants and risk factors associated with maternal or congenital syphilis, or on the characteristics of women seeking or not seeking prenatal care. Current publications from British Columbia, Alberta, Manitoba, Ontario and Quebec, offer some indications of the potential determinants of congenital syphilis in Canada. However, evidence remains limited and might not be representative of the whole country. In consequence, the following section, which summarizes what has been published in peer-reviewed and grey literature between 2009 and 2019, should be interpreted with caution. Figure 34 summarizes documented risk factors for maternal and congenital syphilis in Canada.
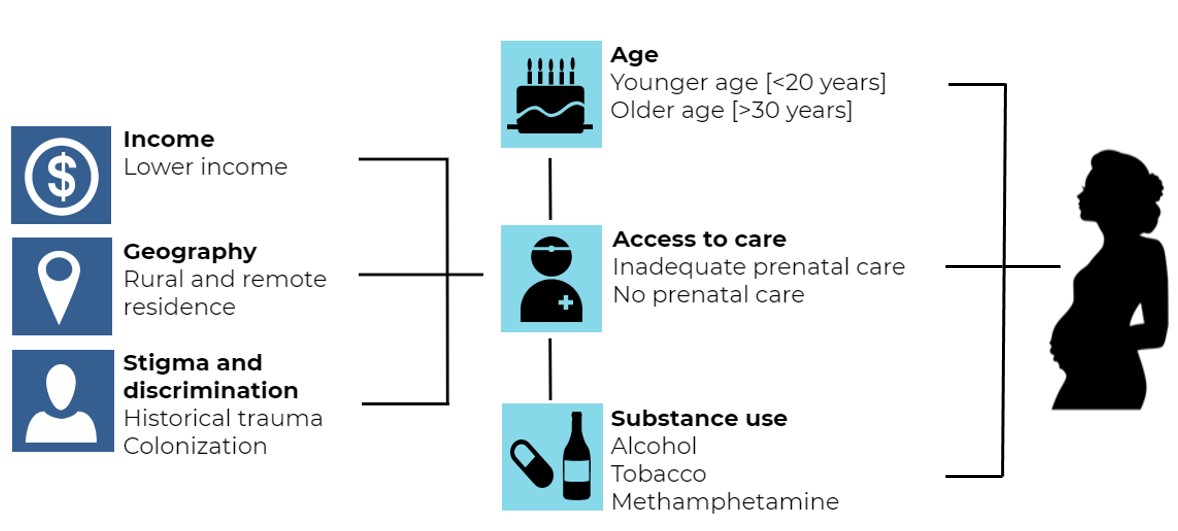
Figure 34 - Text description
Income (lower income), geography (rural and remote residence), stigma and discrimination (historical trauma, colonization) all affect access to care (inadequate prenatal care, no prenatal care). In addition to access to care, age (younger age (<20 years), older age (>30 years)) and substance use (alcohol, tobacco, methamphetamine) are the most commonly reported risk factors of maternal syphilis associated congenital syphilis in Canadian literature.
Note: Existing studies and reports published from 2009 to 2019 in British Columbia, Alberta, Manitoba, Ontario and Quebec.
5.3.1 Access to care
PHAC’s CGSTI recommends universal screening in pregnancy. The initial syphilis screen should be performed in the first trimester or at the first prenatal visit. In areas experiencing a resurgence of syphilis or for women at ongoing risk of syphilis, consideration should be given to repeating the screening in the third trimester (28 to 32 weeks) and again at deliveryFootnote 11. Lastly, any person delivering a stillborn infant after 20 weeks gestation should be screened for syphilis. It is important to note that provincial and territorial screening guidelines may vary across jurisdictions, and take precedence over the CGSTI recommendations.
Access to appropriate prenatal care, including syphilis screening and timely and effective treatment, have been identified as key resources to prevent maternal and congenital syphilisFootnote 246. Indeed, lack of access to care is among the most commonly reported risk factors for congenital syphilis incidence. The occurrence of congenital cases might indicate missed opportunities for prevention.
A British Columbia study on prenatal syphilis screening uptake and case detection in a cohort of women aged 16 to 45 years of age (n=233,203), found that between 2007 and 2011, uptake of prenatal screening for syphilis was high in the province (over 90% of pregnant individuals were tested at least once, which was consistent with provincial guidelines) and improved annuallyFootnote 236Footnote 247. In 2011, 96% (n=44,614) of the women who received any prenatal tests were tested for syphilis, a statistically significant increase from 2007 (91% tested, n=42,154, p value<0.001)Footnote 247. Of interest is the fact that 41% (n=19) of maternal syphilis cases detected between 2010 and 2016 in the province (n=46) were diagnosed in the second or third trimester or at deliveryFootnote 248, highlighting the potential importance of repeat screening during pregnancy or at delivery.
In 2009, Alberta implemented syphilis screening guidelines which recommended universal, repeated screening throughout pregnancy (at first trimester, mid-gestation and delivery). In a study of all pregnancies resulting in a live or stillborn infant between 2010 and 2011 in Alberta (n=99,609), 1.5% of pregnant individuals received no syphilis screening at all, and 98.5% had received at least one prenatal syphilis test. Of these, 1.5% had received screening only at the time of deliveryFootnote 246. Only 20.7% (n=20,624) of all pregnant individuals had received prenatal syphilis screening tests at all three recommended time pointsFootnote 246. Compared to women who had received screening for syphilis at all three recommended time points, women who were underscreened were more likely to not have received any prenatal care, or to have received prenatal care through a midwife only or through a combination of midwifery and physician-based care (compared to physician-based care alone). The authors suggest that the observed association between midwifery-based prenatal care and lower likelihood of repeat syphilis screening may be due to midwives’ or their patients’ lower perceived risk of syphilis infection, or due to the clientele’s potential reluctance to undergo screening, as one of many health care proceduresFootnote 246.
In Quebec, for one of the three cases confirmed in 2016, the mother had not received prenatal care. For another, the mother tested negative for syphilis at the beginning of her pregnancy and was not tested a second time, as she did not present syphilis-related symptoms nor did she report any new partners. For the latter case, both mother and child tested positive for syphilis one month post-delivery. For the third, the mother tested positive for syphilis at the start of her pregnancy, but only underwent treatment two weeks prior to deliveryFootnote 122. For the 2017 case, the mother did not receive any prenatal care. In 2018, the mother of the case received no prenatal care prior to the 31st week of pregnancy, and only underwent syphilis screening during the 35th week of pregnancy. For the 2019 cases, one mother had not received prenatal care, and diagnosis occurred at delivery, while the other mother had received a negative syphilis result early in pregnancy, but had not presented to subsequent prenatal visitsFootnote 121.
There do exist inequities in access to prenatal care by ethnicity. In Alberta, in 2010 and 2011, First Nations women were more likely to have not received the three recommended prenatal syphilis screening tests compared to women who did not report being First Nations (aOR=1.78, 95% CI: 1.62-1.96, n=99,609)Footnote 246. Of the 17 confirmed and three probable congenital syphilis cases born in the Edmonton Health Zone of Alberta between 2002 and 2010, 65% (n=13) were born to mothers who identified as First Nations, Métis or InuitFootnote 249. Syphilis outbreaks in Winnipeg, an especially hard-hit city, have seen a disproportionate number of cases in Indigenous womenFootnote 210. Colonization has contributed to the health inequities Indigenous peoples face today through systemic discrimination across the social, criminal justice, health care and employment environmentFootnote 250. As mentioned in Section 4.2, due to legacies of colonization and structural disenfranchisement, Indigenous peoples in Canada often face stigma, discrimination, violence, mistrust of health care systems, and concurrent health issues, such as HIV and problematic subtance use, which place them at higher risk for experiencing STBBIFootnote 174. The unequal power dynamics created by colonization and reinforced by ongoing colonialism are important drivers of stigma. The discriminatory interpersonal behaviour of health professionals, along with Eurocentric health professionnal training have led to the reduced seeking, or avoidance, of healthcare services and poorer quality of services received by Indigenous peoplesFootnote 251. The gendered impacts of colonization along with patriarchal systems and inequitable education opportunities have led to the marginalisation of Indigenous women and their increased risk for sexually transmitted infectionsFootnote 210. In consequence, factors associated with higher risk of syphilis infection, such as methamphetamine use and survival sex, have been observed among Indigenous womenFootnote 210.
Studies also indicate that delays in maternal syphilis treatment following diagnosis may contribute to congenital syphilis risk. An Alberta study of the management of positive prenatal syphilis serologies in a Calgary STI clinic from 2009 to 2010 (n=48 charts reviewed) noted that while the average time needed to contact and inform patients of their diagnosis was fairly short (one or two days), the average time to receive the first dose of treatment was longer (nine to 20 days on average), highlighting the need to improve the follow-up and support of affected patientsFootnote 252. Another study in Alberta, in the Edmonton Health Zone, noted that of the 17 confirmed and three probable congenital syphilis cases born between 2002 and 2010, 30% of cases (n=6) were born to mothers who received syphlis treatment before delivery, but in whom the treatment was deemed to be inadequate—and 70% (n=14) received postnatal treatment onlyFootnote 249.
5.3.2 Age
Three existing studies from Alberta and British Columbia suggest that both youngest and oldest reproductive age groups included in their studies may be at highest risk for maternal syphilis, and thereby vertical transmission. A study conducted in British Columbia (n=233,203), the highest maternal diagnosis rates were observed in the youngest (16 to 20 years of age and oldest (41 to 45 years of age) age groups; however, these differences were not statistically significantFootnote 247. Similarly, Alberta has seen a statistically significant increase in the proportion of positive syphilis specimens collected through prenatal screening among women aged 30 years and older between 2002 and 2016 (n=821,910)Footnote 253. In Alberta, youngest (<20 years of age) and oldest (≥40 years of age) pregnant women in 2010 to 2011 were significantly less likely to have received syphilis screening at all three of the time periods recommended by the province (at first and third trimester and at delivery) (n=99,609)Footnote 246.
5.3.3 Income
Though few studies have explored the relationship between lower income and likelihood of prenatal syphilis screening uptake and thereby congenital syphilis risk, evidence from Alberta suggests that lower income may be associated with lower likelihood of receiving repeated prenatal screening(at first and third trimester and at delivery) when universal repeated screening is recommended (n=99,609)Footnote 246. This is consistent with findings from a study conducted in Ontario (n=264,737), which found that lower income, particularly living in lower-income areas, has been associated with lower likelihood of prenatal screening uptake for publicly insured screening testsFootnote 254.
5.3.4 Geography
Information on the risk of maternal and congenital syphilis among individuals living in urban vs. rural areas is limited. Evidence from Alberta suggests that that living in rural areas may be associated with lower likelihood of receiving repeated prenatal screening when universal repeated screening is recommended. The odds of not having received all three tests was approximately four times higher among rural and remote areas compared to those living in metropolitan areas (n=99,609, aOR=3.61, 95% CI: 3.10-4.20)Footnote 246. This is consistent with findings from Ontario (n=264,737) indicating that living in more rural or remote areas has been associated with lower likelihood of prenatal screening uptake for publicly insured screening testsFootnote 254.
5.3.5 Ethnicity
Ethnic disparities were also observed in British Columbia. In a study of maternal syphilis cases in British Columbia between 2010 and 2016, almost half of all cases (46%) did not identify as Caucasian. Of all maternal syphilis cases identified in the latter period (n=45), 20% identified as Asian, 13% identified as Indigenous, 11% identified as South Asian, and 2% identified as Black; compared to 24% who identified as CaucasianFootnote 248. Data were missing for 30% of all cases. This overrepresentation of women of ethnic minorities among maternal syphilis cases is distinct from what has traditionally been observed for male cases in Canada. In fact, among the latter, a majority of infectious syphilis cases (40% to 70%) have been reported to occur among males who identify as CaucasianFootnote 92Footnote 167. However, ethnicity data are rarely collected for STBBI by most jurisdictions. As described in the access to care section above, due to legacies of colonization and structural disenfranchisement, Indigenous people have limited access to quality care. This might explain why Indigenous women seem to be disproportionately affected by maternal syphilis or congenital syphilis in their infantsFootnote 210Footnote 251.
5.3.6 Immigration status
The evidence related to immigration status and congenital syphilis risk is sparse. Evidence from British Columbia between 2010 and 2016 suggests that up to one third (29%, n=13) of maternal syphilis cases were either born outside of Canada or had a partner in a developing countryFootnote 92. This is aligned with preliminary data from Quebec, which suggests that sexual contact with a partner who may be having sexual partnerships abroad may be a contributing risk factor to female syphilis risk in the provinceFootnote 122.
5.3.7 Sexual partnerships
For pregnant individuals, partnership status appears to be an important correlate of screening follow-through. A study in Alberta from 2010 to 2011 reported that women who were not married were more likely to be under-screened for syphilis, as defined by the province’s recommendation of universal screening in the first and third trimester and at delivery (aOR=1.09, 95% CI: 1.04-1.13, n=99,609)Footnote 246.
Though a higher reported number of sexual partners and casual sex are known risk factors for syphilis risk in general, very few studies describe the potential role of these factors in determining maternal or congenital syphilis risk. Among maternal syphilis cases identified in British Columbia between 2010 and 2016 (n=45), 13% (n=6) reported having two or more partners in the previous year, and two thirds (n=4) reported engaging in casual sex with more than four partners in the previous yearFootnote 248. Thus, though these behaviours may be associated with higher risk, they are not highly prevalent among reported cases.
Lastly, concerning sexual practices and partnerships, it is important to consider the extent to which pregnant individuals’ risk may be attributable to their partners’ behaviours and exposures. For example, in Quebec, it was estimated that between 2010 and 2011 (n=51), the most common risk factor reported by female syphilis cases (51% of cases) was having had sexual contact with a partner who was at risk. Partner’s risk level was determined based on whether they were a man who had sex with other men, reported use of substances, were engaging in sex work, had multiple other partners or had sexual relations abroadFootnote 122.
5.3.8 Sex work
Few available studies reported on sex work as a potential risk factor for maternal or congenital syphilis. In British Columbia between 2010 and 2016, only 2% (n=1) of maternal syphilis cases reported transactional sexFootnote 248. No information was provided regarding the type of transactional sex activities or the frequency of transactional sex. Though engagement in sex work was a known risk factor during past outbreaks in Canada, existing evidence does not suggest that it plays as important a role in the current epidemiologic contextFootnote 218.
5.3.9 Substance use
Preliminary reports from Manitoba suggest that substance use may be a contributing factor to the province’s observed congenital syphilis cases in 2019Footnote 109Footnote 255. In fact, of the 16 confirmed and the 12 probable cases of congenital syphilis reported in Manitoba from January 2015 to July 2019, substance use, including crystal methamphetamine, was identified in 50% of mothersFootnote 256. Since questions on substance use are not always asked, it is probable that substance use among pregnant women with syphilis may be underestimated. In Alberta, homelessness, insecure housing and a history of substance use were associated with most of the 40 cases of congenital syphilis reported in the province in 2019Footnote 238. Substance use may be a relevant determinant of congenital syphilis in part due to its correlation with lower prenatal testing uptake. In Alberta, women who reported smoking or alcohol consumption during pregnancy were more likely to report no prenatal syphilis testing or late testingFootnote 246. The hesitancy to present for prenatal care might be even higher for people who use substances. People who use drugs often face stigma in health care settings due to a lack of training in harm reduction among health care professionals. This stigma has led to decreased health care use and poorer quality of health and social services for people who use drugsFootnote 251.
The prevalence of substance use as a risk factor appears to vary according to jurisdictions, however. For example, in British Columbia, only 9% (n=4) of maternal syphilis cases identified between 2010 and 2016, reported substance useFootnote 248.
5.4 How do recent trends in Canada compare to those in other countries?
5.4.1 Australia
In Australia, the rate of congenital syphilis has fluctuated in the past decade. Unlike Canada, Australia’s case definition for congenital syphilis includes all cases of congenitally acquired syphilis among infants and children, as well as syphilitic stillbirths. Overall, 44 cases of congenital syphilis were reported between 2008 and 2017, of which the majority (60%, n=26) were born to mothers who identified as Indigenous (i.e. Aboriginal and Torres Strait Islander population). In 2017, specifically, 71% of cases (5/7 cases) were born to mothers who identified as Indigenous, corresponding to a rate of 26.9 cases per 100,000 live births in that population. Among non-Indigenous mothers, three congenital cases were confirmed, corresponding to a rate of one case per 100,000 live births. From 2008 to 2017, the congenital syphilis rates among the Australian non-Indigenous population were slightly lower than the average Canadian rate of congenital syphilis (1.9 cases per 100,000 live births in 2017)Footnote 85. Both countries are similar in their observation of inequities in maternal and congenital syphilis risk according to Indigenous ancestryFootnote 85Footnote 246Footnote 257. Aboriginal and Torres Strait Islander people are disproportionately impacted by STIs compared to non-Indigenous populations, due to a lack of access to testing and treatment and to being more frequently exposed to environments and situations where there is an increased risk of exposure to STIsFootnote 85.
In 2017, the infectious syphilis rate for females of all ages reached 5.5 cases per 100,000 females in Australia. Recent (2015-2017) female infectious syphilis rates are therefore slightly higher in Australia than in Canada, where a rate of 2.4 cases per 100,000 females was observed in 2017. However, Australian rates include both probable and confirmed infectious syphilis cases, which is not the case in Canada, where only confirmed cases are reportedFootnote 85.
5.4.2 European Union
Overall, congenital syphilis rates among the EU and European Economic Area countries have decreased since 2005, and are mostly comparable to rates in CanadaFootnote 258. In 2017, 36 cases of congenital syphilis were reported in the EU and European Economic Area, from a total of 23 member states, corresponding to a crude rate of 1.1 cases per 100,000 live births. It should be noted that these values might be an underestimation as information was missing from eight countries. It should also be noted that case definitions vary across European countries. Although the majority of countries reported syphilis data according to EU case definitions during the last data collection, five countries used national case definitions and five others did not state which definitions were used. Similarly to Canadian case definitions, EU congenital syphilis case definitions do not include stillbirths, abortions or fetal deaths and only include cases under two years of ageFootnote 258. In 2017, confirmed cases were reported in Bulgaria (n=14), Romania (n=6), Portugal (n=4), Germany (n=3), Hungary (n=3), Spain (n=2), Czech Republic (n=1), Ireland (n=1), Lithuania (n=1) and Poland (n=1). These case numbers corresponded to rates of congenital syphilis that ranged from 0.3 cases per 100,000 live births (Poland) to 21.5 cases per 100,000 live births (Bulgaria)Footnote 258.
Overall, infectious syphilis rates among females of all ages have also been decreasing in the EU and European Economic Area since 2005Footnote 258. In 2015, the female rate was 1.3 cases per 100,000 females, before increasing slightly to 1.4 cases per 100,000 females in 2017Footnote 259. As such, the 2017 EU and European Economic Area female infectious syphilis rates were lower than the Canadian average for that year (2.4 cases per 100,000 females).
In Europe, risk factors associated with maternal syphilis included: (1) high-risk sexual behaviour and/or drug use, (2) history of incarceration, (3) low income and younger age, (4) east-European ethnicity and (5) factors related to the healthcare system capacity to identify and treat syphilis infection during pregnancyFootnote 258.
5.4.3 United Kingdom
In the UK, the number of cases of congenital syphilis has been increasing since 2011. Between 2010 and 2017, 21 cases of congenital syphilis were reported in England, including six cases in 2016-2017. Of these cases, 57% (12/21 cases) had not received prenatal syphilis screening. Of those who did receive screening (43% of all cases, 9/21 cases), 77% (7/9 cases) had received a negative test result during their first trimester, suggesting that these mothers acquired the infection later in their pregnancy.
Between 2010 and 2015, the number of cases reported corresponded to a yearly incidence rate that varied between 0.1 to 1.5 cases per 100,000 live births, slightly lower than the Canadian averageFootnote 260. In 2017, the rate of infectious syphilis among all females in England was 1.5 per 100,000 females – lower than the Canadian average that year (2.4 per 100,000 females)Footnote 261. Comparisons between Canadian and UK rates should be interpreted with caution, as there were no publicly available syphilis case definitions from the UK at the time this report was written.
5.4.4 United States
The CDC case definition for congenital syphilis used for reporting purposes includes cases of congenitally acquired syphilis among infants and children, as well as syphilitic stillbirths. Additionally, infants born to a mother who was untreated or inadequately treated for syphilis are counted as probable cases of syphilis, regardless of their signs or symptoms. In the US, the rates of reported congenital syphilis have been increasing since 2012Footnote 262. After noting a rate of 16.2 cases per 100,000 live births in 2016, a 44% rate increase was observed between 2016 and 2017. In 2017, 918 cases of congenital syphilis were confirmed, corresponding to a rate of 23.3 per 100,000 live births (compared to the Canadian rate of 1.9 per 100,000 live births). Of the cases diagnosed in 2017, there were 64 syphilitic stillbirths and 13 infant deathsFootnote 262. In 2018, the number of reported congenital syphilis cases reached 1,306 (33.1 per 100,000 live births), a 40% increase from 2017Footnote 263. In 2018, 78 of the cases were syphilitic stillbirths and 16 resulted in infant deaths. Like in Canada, congenital syphilis trends in the US have largely been correlated with the increasing trend of primary and secondary syphilis among females, which reached a rate of 3.0 cases per 100,000 females in the US in 2018.
Rates of congenital syphilis varied considerably according to ethnicity. In 2018, the highest rates of congenital syphilis were observed among cases whose mothers identified as Black (86.6 cases per 100,000 live births), followed by those identifying as Indigenous (79.2 cases per 100,000 live births—double the 2017 rate of 35.5 cases per 100,000 live births in this group), Hispanic (44.7 cases per 100,000 live births), White (13.5 cases per 100,000 live births), and Asian/Pacific Islander (9.2 cases per 100,000 live births—also double the 2017 rate of 4.3 cases per 100,000 live births among this group)Footnote 262.
In 2018 as in previous years, the geographical distribution of rates varied across the country. Rates were highest in the West (48.5 cases per 100,000 live births), followed by the South (44.7 cases per 100,000 live births), the Midwest (12.4 cases per 100,000 live births) and the Northeast (8.5 cases per 100,000 live births)Footnote 263.
Previous CDC reports have indicated that late or limited prenatal care is associated with congenital syphilis incidenceFootnote 262. Similar to Canadian guidelines, the CDC recommends universal screening of pregnant women at the first trimester and at delivery if the woman had not been screened before or if she delivered a stillborn childFootnote 264. Screening in the third trimester (between 28 and 32 weeks) and at delivery are also recommended for women at high risk of syphilis acquisition or those living in regions that experience a significant increase in the number of casesFootnote 264. Even among those receiving prenatal care, syphilis is often detected or treated too late during the pregnancy to prevent vertical transmission. Non-adherence to prenatal syphilis screening recommendations by health care professionals, as well as infection acquisition post-initial screening test can contribute to vertical transmission of infectionFootnote 262. In the US, every state’s Medicaid program is mandated to cover prenatal care for lower-income females (i.e., those reporting incomes below 133% of the federal poverty level)Footnote 265. However, it was estimated that up to 25% of reproductive-age women were uninsured, at least at some point in the year, and that neither private health insurance nor Medicaid covered 10% of pregnant individuals, during the early 2010 decade.Footnote 266. Though the Affordable Care Act led to a reduction in the estimated proportion of uninsured women of all ages, in 2017, approximately 11% of all women in the US remained uninsuredFootnote 267. The proportion of uninsured women of all ages was highest among non-citizens (32% uninsured), Hispanic (22% uninsured) and Black (12% uninsured) women, as well as women whose income was 200% lower than the federal poverty line in 2017 (i.e. reporting an individual yearly income of $24,100) (20% uninsured)Footnote 267. According to the CDC, the fact of being uninsured or underinsured for women, as well as substance use, increase the risk of receiving inadequate or no prenatal careFootnote 268.
5.5 What can be done to address congenital syphilis in Canada
Although research on effective interventions to reduce congenital syphilis incidence is limited, certain countries have implemented various interventions in order to control the growing number of cases.
5.5.1 Using adequate screening guidelines
Canadian guidelines recommend universal testing for syphilis in the first trimester of pregnancy, and further screening at third trimester (between 28 and 32 weeks) and at d for individuals at high riskFootnote 3. The guidelines also note that consideration should be given to re-screening all pregnant individuals, regardless of risk profile, in areas experiencing heterosexual outbreaks of syphilis or where congenital syphilis cases have been reported in pregnant individuals with no personal risk factors for syphilisFootnote 3.
Given epidemiologic shifts observed in syphilis cases in Canada, especially towards heterosexual populations, as well as the emergence of congenital syphilis cases, several jurisdictions in Canada have recommended repeat screening in the third trimester and/or at delivery for all pregnant individuals, in addition to universal screening during the first trimester. For example, in 2019 British Columbia developed interim guidelines that added a recommendation of universal screening at deliveryFootnote 269. In 2019, Manitoba issued a recommendation for universal third trimester screening (completing additional screening at delivery for higher risk individuals)Footnote 109. In Ontario, in 2019, the Northwestern Health Unit recommended universal screening for all pregnant individuals in the region both during the third trimester and at deliveryFootnote 184. This is aligned with recommendations in northern Quebec, Nunavut, and Alberta. After experiencing high rates of syphilis, the northern Nunavik region of Quebec has recommended universal screening at the first visit for pregnancy, at 28 weeks and at 36 weeks of pregnancy (or at the time of delivery if not performed at 36 weeks) since 2017Footnote 270. Universal screening during the first and third trimester and at delivery has been recommended since 2013 in Nunavut and as an interim measure during an outbreak between 2009 and 2011 in AlbertaFootnote 246Footnote 271Footnote 272. Since then, Alberta recommended screening in the first trimester and at delivery with additional testing suggested for individuals with ongoing risks.
In the US, universal repeat testing during pregnancy is recommended for women who live in high-prevalence areasFootnote 273. Historically, CDC guidance has suggested that universal screening at delivery be considered in areas where infectious syphilis incidence among women of reproductive age is of four to five cases per 100,000 populationFootnote 274. It remains up to individual states to define high-prevalence thresholds after which universal screening in the third trimester be consideredFootnote 274. As of 2018, 12 states required universal screening during the third trimester, and three required universal screening at delivery for all pregnant individualsFootnote 275. Among states that recommended third trimester screening for all pregnant individuals, incidence rates for females of reproductive age ranged from 0.7 (Connecticut) to 7.8 (Louisiana) per 100,000 population in 2017Footnote 276.
Seven countries in Europe currently recommend universal screening in the first and third trimester of pregnancy (Czech Republic, Estonia, Latvia, Lithuania, Romania, Slovakia and Spain)Footnote 277.
5.5.2 Evaluating screening guidelines
Overall, few evaluations on the acceptability and feasibility of universal guideline changes, as well as their effectiveness in increasing screening uptake during pregnancy have been performed. One Canadian study based in Alberta explored the effects of recommending universal screening in the first and third trimester and at deliveryFootnote 246. Out of the of 99,609 pregnancies that occurred in Alberta in 2010-2011, 99% had at least one prenatal screening for syphilis, but just 21% had all three recommended tests (first trimester, mid-gestation and at delivery)Footnote 246. A smaller proportion of pregnant individuals (2%, n=1,494) were screened only at delivery of childbirth, and the same proportion received no screening. The women that were more at risk of not having the three recommended screenings were those registered as First Nations or Inuit (aOR=1.78, 95% CI: 1.62-1.96), those living in a remote rural area (aOR=3.61, 95% CI: 3.10-4.20), and those receiving prenatal care only from a midwife (aOR=13.70, 95% CI: 9.20-20.39). Thus, despite an increase in recommended screening frequency, which was documented in other subsequent studies, social and structural barriers appeared to persist in the province, limiting the effectiveness of interventions related to changes in guidelines aloneFootnote 253. Ensuring compliance with recommended screening guidelines and increasing health provider awareness are therefore essential to reducing congenital syphilis cases in Canada. Evaluating screening guidelines frequently is necessary to ensure that they align with the epidemiological situation.
5.5.3 Increasing access to care
As mentioned in Section 5.3, lack of access to care has been identified as a major obstacle for women at risk of transmitting syphilis vertically and has contributed to the increase of congenital syphilis cases in Canada. Testing facilitates entry to care and provides opportunities for health promotion, disease prevention and linkage to treatmentFootnote 278. Considering congenital syphilis is preventable, vigilant follow-up of patients undergoing treatment is essential to reduce the growing number of cases.
Certain researchers and public health experts have expressed the need to consider innovative strategies to promote prenatal syphilis testing. Potential strategies proposed have included testing pregnant individuals if they present to emergency rooms throughout their pregnancy, or encouraging syphilis screening for individuals who present to clinical settings for other concerns, such as symptoms of pelvic inflammatory diseaseFootnote 279.
Additionally, ensuring access to care to populations such as Indigenous women with a suboptimal access to quality care is paramount. To achieve this, working on upstream factors that put women at higher risk for syphilis, and in consequence at higher risk of vertical transmission, are necessary to prevent congenital syphilis. This requires direct actions to address structural barriers. For cases born to Indigenous mothers, peer-education, provision of harm reduction services, and prevention interventions led and developed by Indigenous organisations, are therefore crucial to address the growing number of congenital cases in these communitiesFootnote 280. The stigma, racism and discrimination that Indigenous women have historically and currently face, contributes to their mistrust of health care providers, and in consequence, their reduced access to health care. In April 2019, PHAC, Health Canada and the British Columbia First Nation Health Authority signed the Declaration of Commitment to Advance Cultural Safety and Humility in Health and Wellness Services and OrganizationsFootnote 251. The aim of this declaration is to identify opportunities to reduce the systemic barriers and harms that Indigenous peoples experience, raise awareness about existing systemic discrimination, and address inequities in outcomes for Indigenous peoplesFootnote 251. These actions are essential in addressing the structural barriers Indigenous women face when accessing health care. As mentioned in the Government of Canada’s five-year action plan on STBBI, STBBI testing facilitates entry to care and provides opportunities for health promotion and preventionFootnote 278. Reaching individuals by providing supportive and stigma-free testing environments facilitates dialogue on sexual health, mental health and substance useFootnote 278. It will in turn allow improved health outcomes through sustained engagement with culturally safe health and social servicesFootnote 278. Supporting women by eliminating stigma associated with sex and substance use, engaging them in their own care, and building trust is essential to increasing access to health care, and in consequence, reducing the number of congenital syphilis casesFootnote 210Footnote 280.
5.5.4 Identifying and addressing missed opportunities for diagnosis and treatment
In the case that congenital syphilis occurs, identifying the upstream factors that led to the vertical transmission of the disease is important to prevent new cases. Review boards have been implemented in the US to identify missed opportunities to prevent congenital syphilis cases. In a Canadian context, review boards would connect provincial and local health authorities along with representatives of key specialized programs such as harm reduction units to contribute to identifying and addressing opportunities to prevent congenital syphilis. In fact, according to a review board of all congenital syphilis cases reported from January 2016 to July 2017 in Louisiana (n=79), 59% (n=47) of congenital cases were deemed preventable or somewhat preventable if patients had received adequate prenatal careFootnote 281. Among these cases, lack of adherence to screening recommendations, lack of follow-up treatment, and delayed treatment, were listed as associated factors. In fact, CDC’s Call to Action regarding syphilis outbreaks identifies the immediate treatment of women infected with syphilis and the confirmation of syphilis testing at delivery as key actions for the control of congenital syphilisFootnote 282. Review of congenital syphilis cases by the means of review boards and the identification of missed opportunities of care and prevention have also been ongoing in New Zealand and are included in their National Syphilis Action PlanFootnote 283. By reviewing cases, it would be possible to identify gaps in access to care and improve the quality of care.
Key messages
- From 1993 to 2017, the number of confirmed congenital syphilis cases reported was relatively low, ranging from one to ten cases per year.
- In 2018, the number of cases reached 17 confirmed cases (rate of 4.56 per 100,000 live births), and it is expected that the number of cases in 2019 will exceed 50 cases.
- Over time, the rate of congenital syphilis has loosely followed the rate of infectious syphilis among females of reproductive age, which was relatively low in the 1990s and increased steadily afterwards.
- Other countries have experienced similar increases in the number of congenital cases.
- Access to appropriate prenatal care, including syphilis screening and timely and effective treatment, have been identified as key interventions to prevent congenital syphilis.
- Ensuring compliance with screening guidelines, identifying gaps in access to care, and tackling upstream factors that lead to congenital syphilis, is essential to reduce the growing number of cases.
6. Interventions and policy for syphilis prevention and control
Key messages
- Condoms are effective at reducing the risk of syphilis transmission.
- School-based sexual education initiatives can be effective in promoting sexual risk reduction strategies, including condom use.
- Programs or interventions that address the underlying social determinants of syphilis infection (such as addressing structural barriers to basic needs, managing co-infections, using culturally adapted approaches, and considering traumatic life experiences as determinants of health) may help curb outbreaks in Canada.
- Although educational social media campaigns around testing have been shown to be feasible, the evaluation of their effectiveness still appears limited.
- Syphilis testing in emergency departments may be a way to detect syphilis in vulnerable populations who do not have access to or avoid routine primary care.
- Online screening services have also been found to promote screening among harder-to-reach populations.
- Partner notification led by a health care professional may be a more effective strategy to ensure those contacted pursue appropriate screening and treatment than compared to partner notification led by the individual. However, patient-initiated notification may be a useful community-based tool to ensure outbreak surge capacity.
Given the shifts in the epidemiology of infectious and congenital syphilis cases across Canada in recent years, and the known social determinants of syphilis incidence, pressing questions remain concerning the best strategies to employ in order to prevent and respond to syphilis outbreaks in the country, as well as addressing the social inequities in syphilis incidence.
The Pan-Canadian STBBI Framework for Action identifies four pillars of action to address STBBI, including syphilis: prevention, testing, initiation of care and treatment, and ongoing care and support. In this section, we review published literature in Canada and abroad, and describe strategies to address syphilis in accordance with these pillars for action, starting with improving primary syphilis prevention, promoting access and uptake of timely syphilis testing, and ensuring effective case management and surveillance.
6.1 Primary prevention
6.1.1 Healthy sexuality practices
Condoms are effective at reducing the risk of syphilis transmissionFootnote 64. For example, in a study conducted by Ferlatte et al., in a pan-Canadian sample of 7,872 gbMSM observed that the odds of receiving a syphilis diagnosis were almost two times higher among those who did not use condoms during anal intercourse, compared to those who did, after adjustment for sociodemographic factors (aOR=1.9, 95% CI: 1.3-2.6)Footnote 163. Similar observations were made in other study settings, where syphilis diagnosis was associated with infrequent condom useFootnote 148Footnote 221. Female condoms can also prevent syphilis transmission64. Studies conducted outside of Canada have also assessed the use of targeted condom distribution programs. Though organized condom distribution programs appear feasible, only a few studies have assessed the effectiveness of such programs in increasing condom use and reducing the risk of syphilis transmissionFootnote 284.
This section provides an overview of approaches to promoting the use of condoms for the prevention of syphilis, including education-based initiatives and educational resources for service providers.
Education-based initiatives
Though only a few studies in Canada have studied the effectiveness of interventions that promote safer sex practices in reducing syphilis incidence, studies conducted outside of Canada suggest that certain education-based initiatives to promote risk reduction strategies may be effectiveFootnote 285. A literature review was conducted, which analyzed 62 non-Canadian studies of pedagogical group-based risk reduction interventions (which lasted an average of 15 hours and were delivered in school or community settings and delivered by a trained adult)Footnote 286. These interventions were associated with reduced odds of condomless sexual activity (Odds ratio [OR]=0.70, 95% CI: 0.60-0.82) and higher odds of condom use (OR=1.49, 95% CI: 1.20-1.74) in adolescentsFootnote 286.They were also associated with reduced odds of STI diagnosis (OR=0.65, 95% CI: 0.47-0.90). Unfortunately, odds estimation pertaining specifically to syphilis risk reduction was not available. For youth, educational programs that address both pregnancy and STBBI prevention as well as distribute condoms appears to be effective in decreasing self-reported condomless sexFootnote 285Footnote 287.
The Sex Information and Education Council of Canada has recently released guidelines to help develop sexual health education programs targeting different sexual health issuesFootnote 204. The guidelines use established theoretical models to create the foundation of education programsFootnote 204. In an intervention aimed to increase condom use, the Information-Motivation-Behavioural Skills Model was used to target three key areas to help encourage behavioural change: information, motivation, and behavioural skillsFootnote 204. The information component included aspects such as increasing knowledge of STIs, the effectiveness of condom use in preventing STIs and pregnancy, as well as where contraception can be accessed and how to use it. The information also addressed how to discuss contraception use with their partner, amongst other subjectsFootnote 204. The motivation aspect involved discussion of specific individual benefits to using condoms, vulnerability to STIs, personal responsibility, sexual scripts and gender norms, attitudes and norms of contraception use or non-useFootnote 204. Finally, the behavioural skills portion helped participants practice and apply practice knowledge of how to access condoms and other barriers, how to negotiate condom use with partner, how to use condoms, how to engage in other forms of sex if condoms are unavailable, as well as scripting unilateral use of a condom amongst other thingsFootnote 204. These education programs help to increase the understanding of effective condom use as well as increase self-efficacy with regards to condom useFootnote 204.
International organizations, such as the US CDC and the US National Institute for Health Care Excellence have also provided recommendations to support condom use promotion. Both institutions recommend providing condom distribution schemes or programs at structural levels to help change the environment and promote condom useFootnote 204Footnote 288. These interventions can include a variety of different projects, such as the distribution of free condoms, the use of social media campaigns, as well as policy changeFootnote 288.
Beyond condom use, researchers have also explored the importance of promoting healthy sexual relationships as a way to improve the uptake of safe sex practices. Given that gender socialization influences factors, such as age of first sexual contact, number of partners, as well as relative comfort levels in discussing and negotiating safer sex practices, including condom use, women can be at higher risk of experiencing domestic violence and face resistance in negotiating safer sex practices60. Empowerment-based pedagogical interventions as well as interventions to improve financial independence between partners have been identified as upstream strategies to promote safer sex practices and prevent bacterial STI incidence in CanadaFootnote 60. An example includes Quebec’s northern region of Nunavik Good Touch/Bad Touch Program, which teaches body-safety and addresses the topic of abuseFootnote 289. However, the need remains for rigorous studies on such interventions for reducing syphilis risk.
Lastly, researchers have also commented on the potential effectiveness of media-based educational initiatives in promoting safer sex practices for syphilis prevention. Following an analysis of the interventions implemented during Vancouver’s syphilis outbreak in the late 1990s—which included a media-based campaign through mainstream media outlets, as well as street-level communications—researchers suggested that educational messages alone might prove insufficient to modify the behaviors that place certain individuals at higher risk of syphilis infectionFootnote 218. Social marketing campaigns may also have a more limited effect on long-term condom useFootnote 290. Researchers have noted that products and services designed to support the behavioural changes promoted by these campaigns may be relevant. These include extended clinic hours, free or low-cost testing options, including convenient testing sites, expedited testing processes, or subsidized transportation initiativesFootnote 291.
Resources for health care providers
Health professionals play a key role in educating sexually active patients on the risks of various sexual behavioursFootnote 3. For this reason, PHAC’s CGSTI offer several resources for health professionals, including motivational interviewing scripts about condom use and guiding questions for STI risk assessments to be used when providing counselling on safer sexFootnote 292. Given time constraints, concerns about patient privacy, and difficulties in asking patients questions pertaining to sex and sexual health, studies have explored the use of computer-generated consultation aids for primary care practitioners, and various institutions have proposed resources to guide discussions with adolescents or adultsFootnote 293Footnote 294.
Fuzzel et al. interviewed 40 heterosexual teens and teens belonging to sexual minority groups (lesbian, gay, bisexual, pansexual, etc.), endeavouring to better understand their experiences of communicating with Canadian physicians about sexualityFootnote 295. Both groups of teens noted that sexuality was not sufficiently discussed. Participants made a number of suggestions to address this gap in services, such as providing a welcoming environment for sexual minorities and using various tools to help teens educate themselves about sexuality (social media, websites, etc.). Participants also noted that educational resources regarding sexual minorities might help clinicians to gain a better understanding of the issues and challenges faced by this population.
In response to observed structural barriers to health care and institutional stigma faced by sexual minorities, the Canadian Public Health Association (CPHA) has developed training and awareness workshops on stigma in sexual health services for health professionals. Evaluation of these materials by way of pilot workshops with health professionals in 14 Canadian cities was conducted throughout 2015 and 2016. The workshops focused on various forms of stigma and sought to make people more comfortable discussing issues around sexuality and STBBIFootnote 296. The CPHA has developed a guide for service providers on methods to discuss sexual health, substance use, and STBBI, which is available free-of-charge online in both French and EnglishFootnote 297. PHAC has also developed resources to promote inclusive healthcare practice in the prevention of STBBI among ethno-cultural minorities, which are also available onlineFootnote 298.
In the Chief Public Health Officer’s latest Report on the State of Public Health in Canada (2019) entitled “Addressing Stigma – Towards a more inclusive Health System”, an Action Framework for Building an Inclusive Health System was developedFootnote 251. The Action Framework provides direction on developing multi-level and comprehensive approaches that respect differences across stigma experiences, while offering potential lasting effects across these various experiences. For example, it includes approaches related to “cultural safety,” which move away from a focus on differences in culture to a view of the health system environment as a site for change. Institutional-level cultural safety interventions include building partnerships with communities, creating safe and welcoming physical spaces reflective of the populations they serve (e.g., signage in Indigenous languages, sacred spaces in hospitals), institutional commitments to cultural safety, and hiring and supporting Indigenous healthcare providers. Healthcare organizations can also change internal policies to support cultural safety, such as creating flexibility in appointment scheduling to increase responsiveness, while building trusting relationshipsFootnote 251.
6.1.2 Pre-exposure prophylaxis
Syphilis can be treated using penicillin, the treatment of choice, or alternative antibiotics, such as doxycycline (for those who are allergic to penicillin)Footnote 299. PrEP can be administered to individuals deemed to be at high risk of contracting infections and consists of daily intake of antimicrobials in order to reduce the risk of contracting disease. Currently, no Canadian studies have assessed the effectiveness of antibacterial PrEP on the acquisition of syphilis. At the time this report was drafted, exploratory research to assess the acceptability, feasibility, effectiveness, and potential antimicrobial resistance related to this strategy, was ongoing in British ColumbiaFootnote 300. Previously, a 2018 study of 424 gbMSM in Toronto and Vancouver, documented that 44% of participants indicated willingness to use syphilis PrEP (60% were willing to use syphilis post-exposure prophylaxis if it was available)Footnote 301. Those most likely to indicate willingness to use syphilis PrEP were those who had previously or were currently using HIV PrEP, and those who reported being “very concerned” with STI acquisitionFootnote 301. Additionally, a pilot study- the Dual Daily HIV and Syphilis PrEP (DuDHS) Study in Canada- is currently underway and is examining concurrent daily HIV PrEP (Truvada ®) and doxycycline PrEP in gbMSM without HIV. Fifty participants will take part in the study and will be randomized to immediate doxycycline PrEP vs. delayed initiation after six months; all participants will receive one year of HIV PrEP. The acceptability, adherence, and tolerability of daily HIV PrEP and doxycycline PrEP, as well as STI incidence and sexual behaviours of participants, will be examinedFootnote 302.
A randomized, controlled pilot trial in the US studied the association between pre-exposure doxycycline use and syphilis incidence among a sample of high-risk gbMSM who live with HIV and who had had syphilis at least two times since receiving their HIV diagnosis. The authors found that doxycycline PrEP was associated with overall lower odds of infection of any STI (gonorrhea, chlamydia, and/or syphilis) after 48 weeks of follow-up (OR=0.27, 95% CI: 0.09-0.83). However, the association was not significant when considering syphilis acquisition alone (OR=0.24, 95% CI: 0.04-1.33, p value:0.10) possibly due to the small sample size (n=30)Footnote 303. A qualitative US study conducted among 19 adult gbMSM who were diagnosed with early syphilis at least twice within the previous five years observed that PrEP was considered an acceptable intervention. However, respondents raised some concerns regarding potential side effects, development of antibiotic resistance (a topic which is explored in greater detail in section 6.3.8 below), and difficulties in following daily treatment protocolsFootnote 304.
It remains to be seen whether pre-exposure prophylaxis for syphilis prevention represents a feasible and effective strategy for outbreak prevention in Canada. Looking at the example of HIV PrEP in Canada, public health officials may face some challenges in promoting syphilis PrEP uptake. According to the 2017 EMIS report, approximately 8% of the 6,059 survey respondents from Canada reported currently being on HIV PrEP, despite 25% reporting condomless intercourse with non-steady partners of unknown HIV status in the past year, among other risk factorsFootnote 188. The authors noted that general understanding of HIV PrEP was lacking, and recommended community-based education initiatives be used to promote knowledge to high risk groupsFootnote 188. The same strategy may be needed for syphilis PrEP, if it is to be promoted in Canada.
6.1.3 Addressing social determinants of health
Beyond clinical risk factors, several Canadian studies have documented underlying social determinants of syphilis infection (see Section 4). However, few Canadian studies have assessed how potential modifications of social or economic exposures may help reduce syphilis incidence.
Structural barriers
One Canadian narrative review summarized elements of conceptual frameworks related to potential action pathways to reduce health inequities, using an Indigenous health lensFootnote 174. Elements of successful interventions summarized in the review included the importance of addressing structural barriers such as access to food, water, and housing, managing STBBI co-infections, protecting patients’ confidentiality, using culturally adapted approaches, and considering traumatic life experiences as both the determinants of health and of health services useFootnote 174. These elements are echoed in other Indigenous-led efforts, such as the Inuit Women of Canada’s 2018 Ikajurniq Inuit Cascade of Care Framework for STBBIFootnote 305. These frameworks and summaries express how strategies to address STI-related syndemics can be implemented at the patient care-, clinic-, and community-levels.
Health service-related actions
At a patient-care level, promising practices include asking patients about social challenges they are facing or ensuring that patient are referred to local resources, benefits programs, and support servicesFootnote 174. At the clinic level, use of patient navigators (individuals who guide patients through the healthcare system) or peer educators have been identified as a way to increase the uptake of health care servicesFootnote 174Footnote 305. Studies have also explored the use of an integrated sexual health care approach for service deliveryFootnote 306. Models in the UK, for example, have explored provision of services pertaining to contraception and reproductive health, infection care, sexual well-being, education, and partner notification, within a single clinic settingFootnote 306. These types of integrated approaches to general practice tend to be appreciated by patients seeking sexual health care servicesFootnote 307.
Furthermore, insofar as adverse childhood experiences and experiences of interpersonal or sexual violence can influence the likelihood of seeking medical care, many scholars have promoted the importance of trauma-informed careFootnote 308. The final report from the National Inquiry into Missing and Murdered Indigenous Women and Girls has also outlined the importance of developing a continuum of care grounded in a trauma-informed approach, which takes into account an understanding of trauma in all aspects of service deliveryFootnote 309. Several resources have been developed in Canada to support healthcare providers in creating safe environments (summarized namely by the Canadian Centre on Substance Abuse), including checklists to support organizational changeFootnote 310Footnote 311.
Community-level actions
At the community level, cooperation with community groups and local leaders can help ensure that STI-related stigma is reduced, and that health inequalities are addressed or mitigatedFootnote 174Footnote 305Footnote 312. An example of such practices observed outside of Canada was noted in a UK-based study of the modernization of a health clinic aimed to promote sexual health services for gbMSM. The clinic collaborated with charitable organizations and drug and alcohol support services to publicize their new clinical servicesFootnote 313. In Canada, examples of partnerships include those between First Nations communities, provincial health ministries and federal departments, such as Indigenous Services Canada, Health Canada, and PHAC. What remains to be seen is how specific examples of such approaches may successfully reduce syphilis incidence or help curb outbreaks in Canada.
6.1.4 Vaccination
Currently, no syphilis vaccine exists. Researchers have noted that an effective syphilis vaccine would provide a valuable contribution to syphilis prevention efforts, given that challenges exist in relation to the clinical diagnosis of the disease, and to effective treatment of infections (due to barriers in health care access, follow-up, and potential limitations in penicillin supplies)Footnote 314. Early Canadian evidence suggests that a vaccine may likely be acceptable to populations at high risk of infection. For example, a recent study of 293 sexual health clinic patients in British Columbia noted that 87% respondents would be interested in receiving an STI vaccineFootnote 315.
Experts have noted that vaccination programs targeted towards key populations, such as gbMSM, may be particularly effective in reducing syphilis incidenceFootnote 316. Challenges in vaccine development include the need to ensure vaccine safety and effectiveness for pregnant individuals as well as individuals on HIV PrEP, or those who live with HIVFootnote 316. In 2019, the US National Institutes of Health awarded funds to researchers at the University of Connecticut to formulate and test candidate antigens for the eventual development of a syphilis vaccineFootnote 317.
Vaccination of higher risk individuals remains an important STBBI prevention strategy for other sexually transmitted infections, such as hepatitis A (HAV) and B viruses (HAV and HBV respectively), and human papilloma virus (HPV), which can co-occur in sexually active individualsFootnote 318.

Infographic 7 - Text description
Areas for Prevention:
- Using condoms during vaginal, anal, and oral sex
- Tackling stigma related to gender and sexuality in health care settings
- Having culturally adapted and trauma-informed health care practices
- Ensuring access to key resources such as housing and other social determinants of health.
Areas for Future Research:
- No syphilis vaccine is currently available
- Effectiveness of syphilis PrEP has yet to be determined in Canada
- Feasibility and effectiveness of integrated approach to prevent syphilis has yet to be evaluated
6.2 Screening – Methods to increase access and uptake
As described in Section 1, regular screening for syphilis is recommended for individuals at higher risk of infection and for pregnant women. It is also mandatory for all individuals 15 years and over who undergo a medical exam for immigrationFootnote 14. Infection risk should be determined by consulting local guidelines and referring to the latest surveillance reports that describe risk factors.
Screening is an important strategy to detect infections earlier and identify individuals who require treatmentFootnote 319. However, screening is accompanied by certain risks and costs, which must be weighed when considering changes to screening guidelines or policies. Possible harms of syphilis screening include the possibility of inaccurate results, unnecessary stress for the patient, and potential consequences related to unnecessary antimicrobial treatmentFootnote 320. However, existing estimates suggest that the reverse screening algorithm that is currently favored in most Canadian jurisdictions has a sensitivity, specificity, and validity of over 99%Footnote 321.
Published literature has explored interventions to either promote screening uptake among certain key populations, increase the frequency of testing, or reduce the time between testing and notification. Key findings are summarized below.
6.2.1 Educational social media campaigns
Education-based initiatives and social marketing campaigns have been identified as potential areas of intervention to increase population-wide knowledge and uptake of syphilis testing. However, Canadian literature studying the effectiveness of education-based initiatives at improving testing uptake is limited. Available studies suggest that educational initiatives may have little impact on increasing public knowledge or promoting uptake of testing for syphilis, especially over the longer term.
One Winnipeg-based study evaluated the effectiveness of an advertisement-based intervention on social media and dating sites (the Gay ad Network, Facebook, Grindr and Squirt) to promote syphilis screening among gbMSMFootnote 322. They compared the number of syphilis tests ordered before and after the campaign’s implementation and studied the number of “clicks” elicited by the advertisements. The month-long intervention generated 2,166 clicks (0.3% of the over 808,200 ad appearances) and led to no statistically significant change in the number of tests ordered in the city. Unfortunately, no data on the effects of the intervention among gbMSM, specifically, were available. Though this type of intervention appeared acceptable and feasible, its effectiveness appeared limited. In another example, a 2017 syphilis awareness campaign implemented in Vancouver (“Syphistory”), included the use of posters in gbMSM community spaces (physical spaces and online) as well as a websiteFootnote 323. Of a sample of patients at STI clinics in Vancouver who were tested on their knowledge of syphilis before (n=137) and after (n=266) the campaign, no statistically significant difference in mean knowledge scores was observed pre- or post-campaignFootnote 323.
These studies’ null findings are similar to those from studies conducted outside of Canada. For example, an Australia-based study targeting 761 gbMSM found that their campaigns were not associated with a reduction of the time elapsed between infection and treatmentFootnote 324. Another study of a media campaign based in Florida, involving posters, cards, ads, and TV/radio public service announcements targeting gbMSM, found no significant change in knowledge of 851 participants about syphilis, clinic visits, or syphilis testing or treatment during the 6-month study periodFootnote 325. It has been noted that the integration of an evaluation phase in the planning of social marketing campaigns is critical, insofar as it may allow public health jurisdictions to adjust and adapt messaging and dissemination strategiesFootnote 290.
6.2.2 Integration of syphilis into other routine STI screening
Syphilis testing during routine STI screening
Syphilis screening can be achieved opportunistically when individuals present themselves to health centres for regular STI testing or other health issuesFootnote 326. Though many Canadian PTs have embraced an integrated STBBI screening approach—once such example is Saskatchewan’s “Test One, Test All” strategy, which promotes comprehensive STBBI testing, and is also currently employed by Manitoba—few studies have assessed the effectiveness of integrated screening strategies in CanadaFootnote 106Footnote 327.
Outside of Canada, interventions have been explored to adapt screening guidelines to increase screening uptake and reduce rates of STIs. For example, in Australia, in 2002, screening guidelines for gbMSM were updated (these were later revised in subsequent years) to recommend that all men who have had any type of sex with another man in the previous year be tested for multiple STIs (including syphilis) every year. A study of gbMSM attending a sexual health clinic in Sydney reported that 61% of patients were screened for the complete list of STIs, following the guideline implementation, compared to 46% before implementation (p<0.05) (n=559)Footnote 328. In the 2014 version of Australia’s guidelines, all gbMSM who had had any condomless sex, had more than ten sexual partners in the previous six months, participated in group sex, used recreational drugs during sex, or who were living with HIV, were recommended to be screened for all designated STIs (including syphilis) up to four times per yearFootnote 329.
Syphilis testing during routine HIV clinical monitoring (among people living with HIV)
In Canada, early evaluations have explored the effects of integrating routine syphilis screening in HIV testing or monitoring programs. A study of 3,893 HIV-positive men in Ontario found that the inclusion of syphilis serological testing with HIV load testing led to a small, but statistically non-significant, increase in detection of new cases of infectious syphilis (2.5 cases per 100 person-years of follow-up in treated vs.1.5 cases in controls receiving provider-initiated syphilis testing)Footnote 326. Outside of Canada, an Australian study compared testing-related outcomes 18 months before and after a sexual health centre in Melbourne implemented a policy to include syphilis screening with every routine blood sample collected from gbMSM patients who were HIV-positiveFootnote 330. The authors observed an increase in the median number of syphilis tests and in the proportion of asymptomatic syphilis infections diagnosedFootnote 330. A US study (n=245) identified a higher syphilis detection rate (16%) after syphilis testing was included in routine clinic-based HIV monitoring compared to the pre-intervention rate (7% detection rate)Footnote 331. An Australian study also noted that increasing testing coverage in gbMSM living with HIV via opt-out syphilis testing during routine HIV monitoring was associated with a reduction in the proportion of syphilis cases detected at a secondary stageFootnote 319.
Frequency of syphilis testing among higher risk groups
Few studies have explored the frequency at which syphilis screening should occur for populations at higher risk of infection. A US study assessed various screening frequencies (quarterly, semi-annually, and symptom-based) and their association with early syphilis detection in a sample of gbMSM and transgender women using HIV PrEP (n=557)Footnote 259Footnote 332. The results indicated that 20% of detected syphilis cases would have been missed without quarterly testing. Furthermore, a mathematical modeling study conducted in Winnipeg noted that focused screening every three months for gbMSM who had a high number of partners (i.e., using existing evidence, authors estimated that approximately 20% of all gbMSM had approximately ten or more partners in the preceding six months) could potentially avert 59% of incident cases and reduce syphilis prevalence by 95%Footnote 333. Enhanced quarterly screening of gbMSM with a prior diagnosis of syphilis could reduce incident cases by 52% and prevalence by 89%Footnote 333. Manitoba’s Winnipeg Regional Health Authority currently encourages ongoing STBBI testing every three months for gbMSMFootnote 327. In the context of Winnipeg, gbMSM represented 80% of infectious syphilis cases diagnosed between 2011 and 2015 (171 of 213 cases), and the estimated size of the gbMSM population in the city was approximately 7,100 (3% of the city’s estimated 237,760 men in 2011)Footnote 333. However, the proportion of syphilis cases who are female has consistently increased in Manitoba since then (Section 3.2). It is possible that these high frequency, targeted testing strategies may be less relevant in contexts with different demographic profiles or in which most syphilis cases are heterosexual.
Although quarterly testing may be ideal in some epidemiologic circumstances, it may be difficult to achieve. Since 2005-2006, Australia has recommended opt-out quarterly syphilis testing in men living with HIV as part of routine HIV monitoring. The change in screening guideline was associated with an increase in syphilis testing. However, only 41% of individuals succeeded in undergoing quarterly testingFootnote 334.
6.2.3 Outreach screening activities
Venue-based targeted outreach screening interventions have been identified as a potential strategy to increase syphilis screening uptake among more vulnerable populations. These interventions can occur in spaces that are frequented for sex, such as saunas and commercial sex venues, events linked to sexual activity, such as adult lifestyle conferences, or clinical spaces, such as emergency departments.
Community spaces (bars, hotels, drop-in centres)
To date, the effectiveness of place-based screening interventions to promote screening uptake and case finding has rarely been studied in Canada. One descriptive study of Vancouver’s syphilis outbreak in the late 1990s noted that in the 30 months between July 1997 and December 1999, outreach workers provided syphilis testing in bars, hotels, and community spaces frequented by sex workers. However, despite these concerted place-based screening efforts, few new cases were identified. The number of tests conducted and cases diagnosed was not provided. The researchers posited that low diagnosis might have been due to low overall prevalence of the disease, even in the outbreak context, and that those most vulnerable may not have frequented the selected locationsFootnote 218.
Saunas and commercial sex venues
Studies have also documented interventions in sex-based venues. In the UK, following an increase in syphilis incidence in Walsall, England, a survey on risk-taking behaviour and syphilis screening was administered at a local sauna frequented by gbMSM. The survey identified four of the 51 cases (8%) diagnosed between 2003 and 2004, and 73% of the study’s 142 respondents indicated that they would use screening services if they were provided in a community setting, such as the saunaFootnote 335. In Brisbane, Australia, a survey (n=1,653) was administered at two outreach clinics that were located at private male saunas and a mainstream health clinicFootnote 336. The sauna-based clinics drew a higher proportion of gbMSM to testing, and identified five of the 16 (31%) syphilis diagnoses during the study period, despite a lower number of visits compared to the mainstream clinicFootnote 336. These findings led the authors to conclude that targeted health clinics in male saunas may be an effective strategy for promoting syphilis screening and case identification.
Events
While many STI testing kiosks and events have been implemented in Canada, especially around HIV Testing Day (June 27th), or Pride events across the country, few Canadian studies have assessed the effectiveness of event-based screening initiatives in increasing screening uptakeFootnote 337Footnote 338. Outside of Canada, one UK-based study assessed the merits of STI screening outreach in a National Health Service health bus at two adult sexuality and lifestyle events and exhibitions (London’s Erotica 2013 and Sexpo 2015 events)Footnote 339. A total of three syphilis cases were identified among the 381 individuals screened at the events (of over 20,000 attendees). Though the proportion of attendees who accessed the screening services was low, the authors observed that many of those screened had never been screened in their lifetime (31% had never had an HIV test before).Thus, the event may have helped screen populations that have limited access to careFootnote 339. Another example was an evaluation of a syphilis and STI testing tent set up at the annual Sydney Gay and Lesbian Mardi Gras Fair Day in Australia. The tent’s services were restricted to gbMSM who had had sex with another man in the past year. Very few of the fair’s total participants were estimated to have frequented the tent (approximately 0.23% to 0.26%), and the cost of running the service was relatively highFootnote 340. Moreover, in contrast to the previous study’s findings, only 18% of these participants had never been tested for STIs in their lifetimeFootnote 340. This initiative identified only one infectious syphilis case.
Emergency departments
Emergency departments have been identified as a potential relevant site for targeted syphilis screening for two main reasons. First, for populations who do not have access to, or are less likely to use routine primary care services, emergency departments can represent a more accessible clinical settingFootnote 341. Second, identifying cases within hospital settings can facilitate treatment follow-upFootnote 342. Outside of Canada, a US-based study assessed the feasibility and effectiveness of using syphilis POC testing in emergency departments on men aged 18 to 34 during a syphilis outbreak that was occurring among gbMSM living with HIV in DetroitFootnote 342. Among 871 patients tested, six (0.7%) active syphilis diagnoses were identifiedFootnote 342. The authors concluded that the implementation of emergency-department syphilis screening was feasible to detect new syphilis cases. Currently in Canada, Saskatchewan and some areas of Alberta are exploring ways to promote screening in emergency departments.
Correctional facilities
Few Canadian studies have explored opportunities for syphilis screening outreach in provincial or federal correctional facilities in Canada. A study of STBBI testing between 2012 and 2015 in three provincial correctional facilities in Alberta found that syphilis prevalence was 3.2% overall (n=5,135)Footnote 343. Prevalence was significantly higher in adult facilities (remand and mixed long-term and remand; 3% to 4.1% prevalence) compared to youth facilities (0.4% prevalence), and higher in female compared to male facilities (5.4% versus 2.4% prevalence, respectively)Footnote 343. The authors propose that an “opt-out” screening strategy—through which patients would be routinely screened for syphilis and all other STBBI unless a patient refuses—be considered for correctional facilitiesFootnote 343. The province of Alberta followed that recommendation and implemented an STBBI opt-out testing in provincial correctional facilities in 2019.
Door-to-door visits
Although this approach may not be feasible in all areas or jurisdictions, a pilot of systematic door-to-door visits was implemented in Quebec’s northern Nunavik region to promote STBBI screening for all without singling out specific settings or householdsFootnote 185. Community residents expressed appreciation for the home visits, given their hesitancy in visiting local health clinic because of privacy and stigma concernsFootnote 185. Although most new STI cases identified were of chlamydia and gonorrhea, at least five syphilis cases were identifiedFootnote 185.
6.2.4 Communications (SMS) reminder systems
One of the strategies explored to promote syphilis screening uptake among higher-risk groups was the use of texting-based (i.e. Short Message Service (SMS)-based) reminder messagingFootnote 326. To date, Canadian studies have yet to explore this area of intervention. Evidence from other countries suggest that although this strategy is feasible, evidence on its acceptability is mixed. For example, one US-based study examined the acceptability of quarterly SMS STI testing reminders (using 2SMS software), offered to (n=4,087) gbMSM who had been diagnosed with syphilis, gonorrhea or chlamydia Footnote 344Footnote 345. The SMS content was: “It’s time for your follow-up testing at Harborview” (Harborview was the largest hospital in the county). Of those offered the SMS reminders, only 13% accepted (80% refused, 7% received some other form of SMS reminder). Among those who refused, 37% used no other form of reminder (i.e. no reminder from medical providers, no testing during routine physicals, no smartphone app or calendar reminders, etc.)Footnote 344Footnote 345. A qualitative US study of 19 adult gbMSM diagnosed with early syphilis at least twice within the previous five years, noted that though most respondents viewed automated text or email-based reminders favourably, they also expressed two areas of concern. First, participants feared that the message content could be viewed by someone else (a partner, parent) who may look at their phone. Second, participant expressed concerns about redundancy, given that they already had mechanisms in place to remind themselves to be tested regularlyFootnote 304.
Studies on the effectiveness of these interventions for increasing the likelihood of repeated screening obtained mixed results. One US study found no statistically significant difference in STI screening re-attendance between intervention and control groups (all of which were high-risk patients) following the implementation of a SMS reminder system (intervention group n=274, control group n=266)Footnote 346. In contrast, an Australia study of SMS reminders used to promote STI retesting among gbMSM found that those receiving the text messages had four times higher odds of re-testing compared to the study’s comparison groupFootnote 347. It remains to be seen how this type of intervention would affect re-screening in Canada.
Automated reminder systems have also been designed to target health care professionals during healthcare consultations. For example, researchers in Australia studied the use of a computer alert system that reminded health professionals of the recommended frequency of syphilis screening for higher-risk gbMSM, and found that it was associated with an increase in syphilis screening uptake in the latter population (n=6,789 consultations before intervention; n=8,036 consultations after intervention)Footnote 348. Studies of such interventions in Canada have yet to be conducted.
6.2.5 Express testing and triage systems
As a way to promote the accessibility, feasibility and acceptability of syphilis and STI screening, researchers and health settings have explored ways to streamline STI screening among certain groups. Various strategies fall under the rubric of “express” testing. These interventions, typically implemented in primary care settings, are designed to shorten wait-times for testing for a pre-defined sub-group of patients. Strategies include the offering of a walk-in screening system for high-risk groups, or the possibility for low-risk groups to skip physical examinations and pass directly to specimen collectionFootnote 313Footnote 349. These have been implemented in Alberta and in Quebec’s northern Nunavik regionFootnote 185Footnote 349.
A study based in Edmonton assessed the impact of express testing for 4,789 low-risk patients on total visit time and the number of STIs diagnosedFootnote 349. Individuals who were asymptomatic, had not had contact with a person with an STI, had not had receptive anal intercourse since their last testing visit, had no history of sexual assault in the last two weeks, and had no involvement in transactional sex in the previous six months were considered low-risk. These patients were given the option to forgo a complete physical examination and pass directly to specimen sampling for STBBI testingFootnote 349. This clinical policy change was implemented as a strategy to curb wait times and reduce the number of patients who were being turned away from the clinic. The authors observed that visit times with a registered nurse were reduced by a median of 13 minutes per low-risk female visit and 9 minutes per low-risk male visitFootnote 349. Though the absolute number of visits associated with a syphilis diagnosis was higher post-intervention (67 post- vs. 22 pre-intervention), the proportion of visits resulting in diagnosis of syphilis was smaller post-intervention (0.1% post- vs. 0.2% pre-intervention) (p value=0.03)Footnote 349. The authors also noted that a higher proportion of high-risk patients was diagnosed with STIs following the policy change. Though this increase in the number of visits post-intervention may be due to increasing secular trends in STI rates over the study period, the authors posit that the increase may also be attributable to higher overall testing capacity made possible by time saved through express testingFootnote 349.
6.2.6 Online screening services
Among the strategies to link individuals to testing are web-based interventions through which patients answer sexual history questions online and can then receive a test requisition form to use at a local laboratory. In 2014, the BCCDC launched its GetCheckedOnline website, which surveys users on their sexual history, generates a test requisition, and links them to designated specimen collection centres in VancouverFootnote 271. The website also links to an online appointment booking system to make an appointment for sample collectionFootnote 350. Results are communicated online via the GetCheckedOnline account. Between September 2014 and December 2015, 868 users created accounts on the platform. Of these, 43% were gbMSM, and 13% were tested for STIs for the first time. A total of 37% submitted specimens and 3% received a positive STI diagnosisFootnote 271. Researchers evaluating the intervention concluded that GetCheckedOnline is an acceptable and feasible intervention, with the capacity to promote screening among populations that traditionally may have been under-screenedFootnote 271. Based on these results, GetCheckedOnline was expanded to selected communities in Vancouver Island and Interior BC in March 2016Footnote 351. A later study of the platform, comparing 1,093 clients using the website to the 18,404 STI clinic clients in the province between 2014 and 2017, found that GetCheckedOnline clients were more likely to be women or men who have sex with women (compared to gbMSM), have a history of STI diagnosis, and to have a partner living with HIVFootnote 352. GetCheckedOnline clients also demonstrated a higher rate of repeat testing, suggesting the interface may facilitate repeated testing if the latter is neededFootnote 352.
Results from British Columbia are aligned with findings of studies conducted outside of Canada, including a study conducted in the UK (n=2,072), which also reported higher rates of completion rates of STI testing in groups receiving online screening servicesFootnote 353.
Despite the latter strengths, a qualitative evaluation with 39 respondents prior to BC’s GetCheckedOnline implementation reported certain concerns with internet-based testing that could prevent participation in online screening services. These include reluctance to share personal data online, mistrust of data protection mechanisms, and concern over inadequate pre- or post-test counselingFootnote 354. Mitigation strategies to address these concerns include strategies to ensure data privacy and security, and provide sufficient resources and referrals for counseling and support servicesFootnote 354.
6.2.7 Incentive-based screening
One of the strategies proposed to promote screening uptake is to use financial incentives (e.g., cash payments, conditional cash transfers, vouchers). Though there is evidence that STI health clinics in Canada have used incentives, such as the use of gift cards or lunches —namely, in Saskatchewan and Alberta—to promote STI screening and treatment, the effectiveness of these incentive-based strategies has not been widely studiedFootnote 327. In Edmonton, Alberta, an intervention was implemented, which offered a $10 gift card for STI testing, including syphilis testing, and another gift card of the same amount for returning to obtain results and treatment. This intervention was targeted at individuals who resided in subsidized housing locations, were street-involved, or who frequented community-based organizationsFootnote 355. Among the 342 individuals who participated, 34 individuals tested positive for syphilis (11% seropositivity rate). Most participants (60%) reported substance use, 19% reported injection drug use, and 6% reported involvement in transactional sexFootnote 355. The authors conclude that incentivized testing may be an effective approach for improving STI testing among populations who may be less likely to access regularly primary health careFootnote 355.
Outside of Canada, a qualitative US study of 19 gbMSM adults diagnosed with early syphilis at least twice within the previous five years, asked participants if they would take advantage of getting paid for syphilis testing, and if so, what amount they would want to receiveFootnote 304. Most participants were favorable to financial incentives, and monetary amounts preferred ranged from $0 to $100, with at least one of the 19 participants expressing an interest in receiving compensation for transportation to the clinic and hours missed at workFootnote 304. These findings should be interpreted with caution, however, given the small sample size and distinct health service context of the study.
6.2.8 Point-of-care testing
POC testing refers to medical diagnostic testing used outside of a clinical setting. POC testing for syphilis has been proposed as a strategy to increase the accessibility of screening in populations that may be more hesitant or unable to access traditional screening.
Rapid point-of-care testing
Rapid POC testing allows for a rapid sample collection, testing, and results, which can all be communicated in a single session by a health professional, with the possibility of follow-up sessions as needed (for confirmatory results communication and post-test counseling).
There are two main types of POC syphilis tests: (1) Immunochromatographic strip tests, which react to whole blood or serum when antibodies are present, and (2) particle agglutination tests, wherein treponemal antigen-coated gelatin particles clump together when in contact with whole blood or serum, in which antibodies against Treponema are presentFootnote 356. These tests cannot differentiate between a new or previous infection, and require additional confirmation using quantitative non-treponemal testingFootnote 356. Due to these limitations, researchers have indicated that rapid POC tests would be of most benefit in areas with low but rising rates of infectious syphilis or low rates of screening and testingFootnote 356Footnote 357.
Although there exist over a dozen rapid POC syphilis tests to detect treponemal antibodies, to date, no rapid POC syphilis tests have been approved for use in CanadaFootnote 342. While POC tests for syphilis are not routinely used in Canada, they have been used in research studies. For example, an Edmonton-based study assessed the acceptability and field performance of rapid POC tests for syphilis (SD Bioline 3.0 test) in key populations (gbMSM, people engaged in the sale or purchase of sex, persons who inject drugs, Indigenous people, etc.) in clinical and community settings (n=1,183)Footnote 358. Acceptability of the test was high, as 82% of individuals approached agreed to be screened. Testing performed at places frequented by gbMSM (e.g., saunas, etc.) had the highest acceptance rate (91% tested), followed by drug rehabilitation facilities (89%), detention centres (80%), healthcare facilities (74%), and community organizations (70%). High acceptance may have been attributable to the sample, insofar as tests were being offered to a group of people who had largely been screened previously. Nonetheless, findings are aligned with qualitative evidence outside of Canada that indicated the high level of acceptability of POC testingFootnote 304Footnote 359. A study funded by the Canadian Institutes of Health Research will commence shortly in the Arctic communities of Nunavut and Nunavik to evaluate the acceptability, performance and utility of a point-of-care test for syphilisFootnote 360.
Another international multi-site study with a study arm based in Montreal, Quebec, assessed the feasibility and impact of a multiplex rapid POC syphilis test, which could also test for HIV, Hepatitis C virus (HCV) and HBV (Miriad Rapid TP/HBV/HIV/HCV Antibody Test) in a sample of at-risk individuals (n=375 in Mumbai, n=119 in Montreal)Footnote 357. They found that 92% of individuals agreed to testing, and that 97% of respondents preferred the multiplex test to conventional testing, and 99% would recommend it to othersFootnote 357.
Though evidence shows that POC testing appears highly acceptable, regulatory approvals, clinical guidelines, and accompanying screening and quality assessment policies are necessary to ensure how and where POC testing can have a meaningful impact on halting transmission of infectionsFootnote 361.
Dried blood spot testing
Although not a form of rapid POC testing, dried blood spot (DBS) testing for syphilis has been proposed as a complementary alternative to standard syphilis testingFootnote 362. DBS samples do not require refrigeration, are very stable, and can be collected by non-medical professionals, making them particularly useful for populations who may be hesitant to seek screening services due to systemic barriers and stigma, or communities in remote areasFootnote 362Footnote 363. DBS samples can also be transported via novel technological methods, such as drones, to microbiology laboratory sitesFootnote 364.
Interventions using DBS testing are currently implemented in Canada, namely in Alberta, Saskatchewan, Ontario and Prince Edward IslandFootnote 363Footnote 365. Preliminary evidence from a DBS testing implementation in a First Nations community in Ontario indicated that DBS testing is highly feasible and acceptableFootnote 363. However, some concerns remain in relation to the communication of results back to participants, and time required to adequately perform the testsFootnote 363. These preliminary Canadian results are aligned with those from other countries, which indicate high feasibility and acceptability in higher risk groups, such as gbMSM and people living with HIV and HBVFootnote 366.
6.3 Case management
6.3.1 Partner elicitation and identification
Identifying partners depends on an individual’s willingness and ability to disclose information on sexual partners. Life course histories of discrimination or anticipated stigma can lead individuals to fear disclosing contacts. Indeed, a study by Lukac et al. conducted in 2017 (n=491) found that gbMSM living with HIV were less likely than gbMSM who were HIV-negative to disclose their sexual partners to the public health nurse (70% vs. 80%)Footnote 367. Other documented barriers of partner elicitation in Canada include mental health or substance use issues, which prevent cases from being able to complete interviews, as well as partners being anonymous and unidentifiableFootnote 218.
Social network elicitation questions
Various strategies have been detailed in the literature to encourage partner elicitation. In Canada, some public health units have adapted how they inquire about sexual contacts, namely by asking broader question such as “Who do you hang out with?” rather than asking individuals to name their sexual partnersFootnote 368. It remains to be assessed whether using alternative questions during partner elicitation interviews represent more effective strategies for partner identification than traditional approaches.
Use of communicable disease investigators
A literature review conducted by the BCCDC noted that several existing studies have observed that the use of Communicable Disease Intervention Specialists (non-medical staff specialized in communicable disease follow-up activities) placed in outbreak sites and health departments, has been associated with greater success in eliciting contacts compared to conventional public health or health care providersFootnote 369. Communicable Disease Intervention Specialists have been utilized predominantly outside of Canada, especially in the USFootnote 370. Their strength is a specialization in finding and providing supportive services for patients diagnosed with STIs and their contactsFootnote 369Footnote 370.
Targeted elicitation interviews
BCCDC’s literature review also noted that existing literature supports targeting elicitation interviews and partner notification to higher risk groups when faced with limited resourcesFootnote 369. These groups include partners who are more vulnerable to negative health outcomes, including STI transmission, those who themselves may have more partners and are more likely to contribute to onward community transmission, and those who may be more hesitant or less likely to access STI testing and care servicesFootnote 369. The need for assessment of the effectiveness of targeted partner elicitation and notification practices in Canada remains.
6.3.2 Partner notification
The notifying of partners is a secondary prevention measure to identify sexual partners of confirmed syphilis cases so they can be offered testing and treatment, and thus reduce the risk of infection in the original patient or othersFootnote 292. PHAC’s STI guidelines recommend that all sexual or perinatal contacts of primary syphilis cases be notified within a 3-month trace-back period (i.e., the time prior to symptom onset or date of specimen collection if asymptomatic). Additionally, the trace-back period is six months for secondary syphilis, one year for early latent syphilis. All long-term partners and children of individuals diagnosed with late latent and tertiary syphilis should also be notifiedFootnote 292. Various approaches designed for successful notification of partners are presented below.
Patient or health professional-led notification
Partner notification may be completed directly by the patient receiving the syphilis diagnosis or can be carried out by a health professional. Though more costly and resource-intensive, existing Canadian literature suggests that notification led by health professionals may be a more effective strategy to ensure a patient contacts pursue appropriate screening and treatmentFootnote 371Footnote 372. For example, in a Canadian study of partner notification outcomes among gbMSM in British Columbia from 2010 to 2013 (n=350), researchers observed that a greater proportion of partners was tested for syphilis when notified by a health professional (54%) than when notified by the patient (21%)Footnote 57. These findings align with those observed outside of CanadaFootnote 373. Furthermore, in certain circumstances when protection of anonymity is paramount, such as when an index patient may have experienced sexual assault or may be concerned about the potential emotional or physical consequences of referring a partner, professional-led notification remains an important methodFootnote 371Footnote 372.
However, patient-initiated partner notification remains a useful approach. Many patients prefer having the option to communicate directly with their sexual partners about potential exposure to an STIFootnote 372. Furthermore, the growing number of syphilis cases across several jurisdictions in Canada continues to place pressure on front-line workers, especially public health nurses, to keep up with partner notification. Ensuring appropriate availability of human and financial resources to appropriately identify and contact partners is already a challenge for several jurisdictionsFootnote 369. A recent study from British Columbia documented that of the 648 infectious syphilis cases confirmed among gbMSM in the province between 2006 and 2016, 42% of first-diagnosed and 62% re-diagnosed cases chose patient-initiated partner notification (rather than provider-initiated)Footnote 374. Among those with a first diagnosis of syphilis (73% of gbMSM cases), patient-initiated partner notification led to a 19 percentage-point higher proportion of partners’ notified (89%), compared to provider-initiated cases (70% partners notified)Footnote 374. Patient-initiated partner notification is a valuable strategy, especially during outbreaks.
Cluster notification
Enhanced syphilis contact tracing and notification using a cluster-based approach may be useful, and it has been carried out previously in Canada (e.g., to investigate an HIV outbreak in Saskatchewan, or in response to a syphilis outbreak in British Columbia)Footnote 375Footnote 376. In this approach, index patients are asked to identify others in their social networks or community whom they believe may benefit from counseling and testing (e.g. “Who do you think should be tested for syphilis?”Footnote 375-377. Though this approach may result in a smaller proportion of positive cases compared to one based solely on contacting sexual contacts, it remains a potentially useful approach in areas with high infectious syphilis rates, and can additionally provide useful information for social network analysisFootnote 378.
Internet-based notification
In Canada and abroad, given the increased use of dating apps and websites, strategies have been explored to find and notify contacts of cases via web-based channels. Though these approaches may be perceived as more impersonal, they are especially relevant when partners meet and communicate online, and when contact information traditionally used to trace contacts is more challenging to obtainFootnote 371.
A recent Canadian literature review summarizes two broad types of approaches for internet-based partner notification (those applied through social networking sites and those contacting cases via email), as well as potential challenges that may occur when applying such strategiesFootnote 379. The review found that most partner notification strategies applied via social networking sites required public health entities to have a profile on the site in question, and communicate with the profiles provided by index casesFootnote 379. Outside of Canada, published studies suggest partner notification via social networking sites is largely feasible and acceptable, including with certain key populations, such as gbMSMFootnote 380-387. It has also been associated with an increase in the number of partners notified and screenedFootnote 380Footnote 384. Given the paucity of Canadian evidence, whether such interventions would be effective in Canadian contexts remains to be assessed. The provinces of Alberta, Saskatchewan, and Newfoundland and Labrador are currently exploring innovative approaches to partner notification via social media and dating apps.
Another internet-based notification strategy has been the use of websites to facilitate anonymous email contact notification. In Canada, these include British Columbia’s CheckHimOut site, which allows for anonymous contact notification through email or text message and provides information about local sexual health clinics for testingFootnote 388. Another similar website is InSpot.org,which allows individuals to notify partners in Ottawa, Toronto, or in British Columbia that they may have been exposed to an STI. Outside of Canada, sites include Australia’s Let Them Know and the Netherlands’ Suggest a Test platformsFootnote 389Footnote 390. Studies evaluating these types of programs are limited. Those that exist suggest that website-based contact notification is largely acceptable, especially for those in more casual relationshipsFootnote 391. However, despite advertising campaigns to promote the use of sites, uptake tends to be lowFootnote 392Footnote 393. Website-based approaches face an additional challenge if potential users do not have the email addresses of their contactsFootnote 379.
6.3.3 Treatment
Early, successful treatment of syphilis remains an important strategy for outbreak management and secondary prevention. Treatment reduces the duration of infectivity and transmission efficiencyFootnote 144. Current Canadian STI guidelines recommend that non-pregnant adults with infectious syphilis be treated with a 2.4 million units of benzathine penicillin G, as a single dose administered intra-muscularlyFootnote 3. Suggested treatments vary slightly for non-infectious syphilis, for pregnant individuals and infants with congenital syphilisFootnote 3. Currently, the CGSTI recommend that all sexual and perinatal contacts be located, tested and treated if serology is reactiveFootnote 3. The guidelines also note that if follow-up cannot be assured, it may be appropriate to administer a post-exposure prophylaxis for infectious syphilisFootnote 3. In general, clinicians are advised to consult with their provincial and territorial guidelines to guide their prescription practices.
Decreasing delays in treatment
Few Canadian studies have assessed potential strategies to reduce delays between syphilis diagnosis and treatment. Among the strategies used outside of Canada are SMS-based test result communication strategiesFootnote 394. A US-based study (n=4,081) used a text-messaging strategy to convey STI test results and found that over half of the study participants (57%) who received the intervention were treated within one to four days, compared to 41% in the control groupFootnote 394. Researchers noted that in the study context, up to 50% of patients were offered presumptive treatment the day of testing, and these cases were therefore excluded from the analyses. In contrast, a UK-based study of an online screening and SMS messaging intervention (n=2,072) found no statistically significant difference in time to treatment between treated and control groupsFootnote 353. However, the latter study did not provide treatment delays by STI type. Results from these two studies are difficult to compare given differences in the operationalization of their outcomes measures. The first study presents differences in the proportions of cases treated one to four days after receiving results (versus eight or more days or never)Footnote 394, while the second study presents differences in mean time to treatmentFootnote 353. Given the heterogeneity in study measures and limited available evidence, it remains unclear whether such communication-based interventions could contribute to reducing treatment delays in Canada. Therefore, further research is required.
Post-exposure prophylaxis
Currently, no Canadian studies have assessed the effectiveness of antibacterial post-exposure prophylaxis (PEP) on the acquisition of syphilis. However, use of the latter may represent a potential strategy to reduce syphilis incidence in higher-risk populationsFootnote 395. A randomized controlled trial conducted in France assessed the effectiveness of PEP with doxycycline at reducing risk of a first episode of syphilis among 232 HIV-negative men who have condomless sex with men and who were currently using PrEP for HIV preventionFootnote 396. The study observed a statistically significantly lower risk of syphilis acquisition among those receiving PEP compared to those who were not (Hazard ratio=0.27, 95% CI: 0.07-0.98)Footnote 396.
A recent study (2018) of 424 gbMSM in Toronto and Vancouver documented that 60% of participants indicated willingness to use syphilis PEP if it was available. It remains to be seen whether syphilis PEP represents a feasible and effective strategy for outbreak control and prevention in CanadaFootnote 301. Looking to the example of HIV PEP, challenges may occur if such a treatment strategy is promoted in Canada, including issues of general awareness of syphilis PEP and barriers to access. For example, according to the 2017 European Men-Who-Have-Sex-With-Men Internet Survey, 26% of the Canadian sample of 6,059 gbMSM remained unaware of HIV PEP, and almost half (47%) were not confident they could access PEPFootnote 188. The findings suggest that visible and accessible services as well as community education initiatives are among the strategies that could increase PEP awareness and use. A similar strategy may be needed for syphilis PEP if ever it is to be promotedFootnote 188.
Antimicrobial resistance
Existing studies have begun to document the emergence of antimicrobial-resistant syphilis infections, and to predict whether resistance will become a global issueFootnote 397. For example, macrolide- (alternative antibiotics to penicillin) resistant T. pallidum strains have been observed in Canada, China, Europe, and the USFootnote 48Footnote 398Footnote 399.These have been associated with a specific mutation in the pathogen (mutations in the T. pallidum 23S rRNA genes)Footnote 398. Specific mutations and T. pallidum strains known to have antimicrobial resistance can be identified by genomic analysis. Experts recommend that all syphilis patients who receive macrolides be closely followed, clinically and serologically, to identify instances of resistanceFootnote 398. In addition to treatment failures of HIV co-infections or other clinical issues, the risk of increased antimicrobial resistance is among one of the reasons why some scientists continue to advocate for the need to develop a syphilis vaccineFootnote 314.
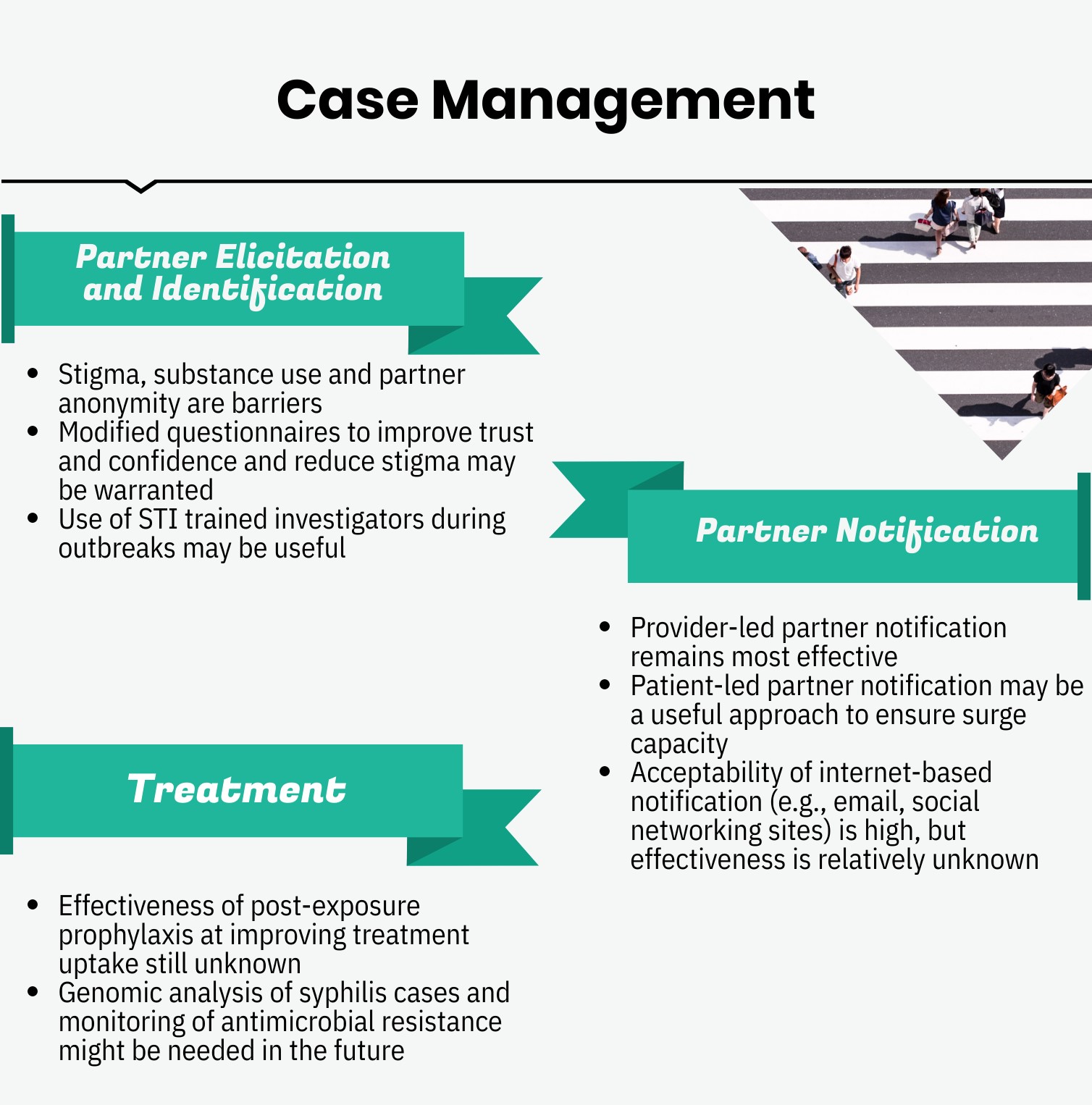
Infographic 8 - Text description
Partner Elicitation and Identification:
- Stigma, substance use and partner anonymity are barriers
- Modified questionnaires to improve trust and confidence and reduce stigma may be warranted
- Use of STI trained investigators during outbreaks may be useful.
Partner notification:
- Provider-led partner notification remains most effective
- Patient-led partner notification may be a useful approach to ensure surge capacity
- Acceptability of internet-based notification (e.g., email, social networking sites) is high, but effectiveness is relatively unknown.
Treatment:
- Effectiveness of post-exposure prophylaxis at improving treatment uptake still unknown
- Genomic analysis of syphilis cases and monitoring of antimicrobial resistance might be needed in the future
6.4 Surveillance
Syphilis is a notifiable disease in Canada, and therefore passive surveillance of reported cases is conducted via CNDSS. In addition to this standard passive syphilis surveillance, other surveillance strategies have been employed in Canada to track syphilis trends and inform outbreak management.
6.4.1 Enhanced surveillance
Enhanced federal surveillance activities
At the federal level, in collaboration with PT partners, community organizations and academic researchers, PHAC has designed and launched the Tracks enhanced surveillance systemFootnote 400-403. The Tracks involves periodic, cross-sectional surveys at sentinel sites across Canada of key populations (gbMSM, people who inject drugs, people born in countries where HIV is endemic, youth who are living on the streets, and Indigenous peoples)Footnote 401-405. Given its non-random sampling methods, Tracks surveillance findings may not be generalized to the entire Canadian population. Enhanced survey-based surveillance offers important opportunities to identify risk factors and determinants of syphilis incidence and related outcomes. In July 2019, PHAC established a Syphilis Outbreak Investigation Coordination Committee (SOICC) to support the coordination of the Canadian response in dealing with the rise in the number of syphilis cases and jurisdictionally declared outbreaks. All of the provinces and territories have collected and shared with PHAC preliminary 2018 and 2019 enhanced syphilis surveillance data on gbMSM status, pregnancy status and substance use, in addition to age and sex. PHAC published an infographic, using the preliminary reported data, focusing on infectious syphilis cases in Canada from 2009 to 2018Footnote 54. SOICC members continue to discuss the collection of enhanced syphilis surveillance data on an ongoing basis.
Enhanced provincial and territorial surveillance activities
In Canada, enhanced provincial syphilis surveillance activities have been implemented in some provinces and territories, each varying in scope and timeframe of application, based on local contexts. For example, in New Brunswick, following a resurgence of syphilis cases, a standardized enhanced surveillance investigation form was implemented in 2011-2012 to collect information on cases, their sexual contacts and risk factors, as a response to the outbreak. In 2016, the province implemented routine enhanced surveillance. This form is used by the province’s public health staff when following up on each new infectious syphilis case. The data collected provided information necessary for social network analysis of cases and their contacts. Manitoba has also developed enhanced surveillance protocols, which were implemented in 2004 in partnership with the province’s Stop Syphilis campaignFootnote 406.The province’s strategy included aggressive case-finding initiatives, and the delegation of syphilis testing and treatment provision to Public Health NursesFootnote 406.
Following increases in infectious syphilis incidence in the province, enhanced syphilis surveillance was also initiated in Quebec. The province collected, pooled, and analysed additional information on infectious cases that occurred between 2004 and 2005Footnote 407. The same was done for female infectious syphilis cases that occurred between 2009 and 2012Footnote 408.
In Toronto, in 2010, an online monitoring tool was tested for 27 men with infectious syphilisFootnote 409. Respondents were asked to complete a self-administered survey on the number of sexual partners they had and on the venues they frequented when seeking to meet sexual partners.
Lastly, British Columbia’s sentinel surveillance system uses administrative medical databases from specific STI clinics to assess social and demographic determinants of syphilis incidence in the provinceFootnote 169. The latest reported data from British Columbia were published in 2015 (data from 2000-2013)Footnote 169. In 2016, BCCDC established additional data collection procedures to assess determinants of viral load at and around the time of syphilis diagnosis, and HIV co-infectionFootnote 145.
6.4.2 Social network analysis
Once data are obtained on cases, their sexual contacts, and locations frequented, an analysis of sexual networks can help public health professionals prevent and screen for syphilis. Social network analysis helps to shed light on how syphilis is transmitted, the role of meeting and gathering places, as well as the role that individuals who have acquired the infection and their sexual contacts, may play in outbreaks.
In the late 1990s, social network analysis helped to identify a link between female transactional sex, crack cocaine use, and increased syphilis transmission, in British ColumbiaFootnote 218. More recently, social network analysis has been conducted in several settings in Canada. For example, a social network study of 52 STI clinic patients in Alberta identified a network of 94 gbMSMFootnote 410. Within this network, there were 18 individuals with infectious syphilis linked to 76 sexual contacts through 21 meeting placesFootnote 410. Just over three-quarters of participants (77%) said they had met a sexual partner in a social venue, and sexual partners were often met onlineFootnote 410. The authors suggested that web venues could therefore be targeted for future primary or secondary syphilis prevention efforts. In Toronto, following the implementation of an online monitoring tool for patients diagnosed with infectious syphilis, a social network analysis (n=27) was conductedFootnote 409. The study identified six meeting places linked to the cases (three websites, two saunas and one bar)Footnote 409. Most participants found their sexual partners online (88%) and in bathhouses (60%). This information allowed public health officials to glean where future public health messaging and case finding efforts should be focused. In New Brunswick, a social network analysis (n=56) identified that gbMSM aged 18 to 55 were at highest risk of syphilis infection in the province, and often met partners through websites, bars, and saunasFootnote 411. These findings led the province to target media content through identified websites and meeting placesFootnote 411. In Ontario, at the request of the Ontario Ministry of Health, PHAC’s Canadian Field Epidemiology Program helped conduct an enhanced social network analysis of syphilis cases diagnosed between 2009 and 2010Footnote 148. Information on cases, contacts and social venues was plotted, connecting many of the single individuals and dyads and allowing for identification of potential venues for targeted sexual-health messaging.
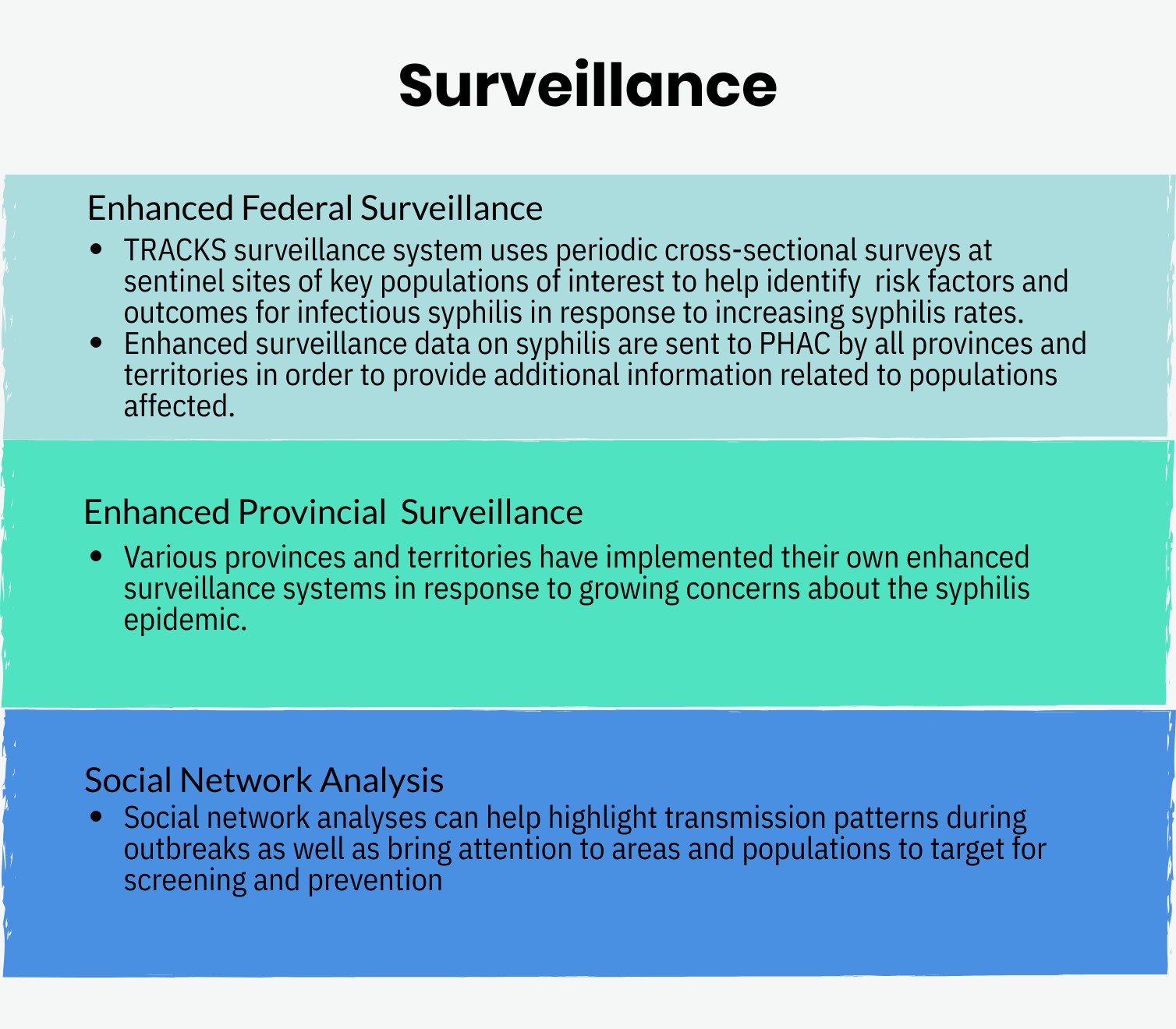
Infographic 9 - Text description
- Enhanced Federal Surveillance: TRACKS surveillance system uses periodic cross-sectional surveys at sentinel sites of key populations of interest to help identify risk factors and outcomes for infectious syphilis in response to increasing syphilis rates. Enhanced surveillance data on syphilis are sent to PHAC by all provinces and territories in order to provide additional information related to populations affected.
- Enhanced Provincial Surveillance: Various provinces and territories have implemented their own enhanced surveillance systems in response to growing concerns about the syphilis epidemic.
- Social Network Analysis: Social network analyses can help highlight transmission patterns during outbreaks as well as bring attention to areas and populations to target for screening and prevention.
6.5 Gaps in research and data
Throughout this section, a number of gaps in Canadian syphilis research have been identified and potential areas for future research are discussed. First, some have highlighted that knowledge is missing on the “cascade of care” for syphilis in Canada, including testing coverage, access to treatment, and cureFootnote 3Footnote 363. Although attempts have been made to estimate outcomes of the cascade of care for HIV and HCV in Canada—from screening uptake, to treatment initiation and follow-up—little has been done on the subject of syphilis. Second, researchers have also identified that very little genomic analysis of T. pallidum has been conducted, which limits our epidemiologic understanding on the epigenetic drivers of syphilis outbreaks, and of the risk of potential antimicrobial resistanceFootnote 48Footnote 397. Third, an area of future syphilis research is in the domain of mathematical modeling, which can allow public health units to test hypotheses and can provide evidence to inform targeted screening strategies, among other interventionsFootnote 412. Similarly, network analysis of current outbreaks may help guide areas of interventionFootnote 218.
Effective research requires data. Provinces such as British Columbia have developed a data governance model that allows for data linkage, which provides opportunities for research and analysis into the determinants of syphilis outbreaks in the province. Linked vital statistics, STBBI case data, laboratory data, enhanced surveillance data on cases and their contacts, and other sources of clinical data (e.g., prescriptions) provide resources for policy planning in the provinceFootnote 327.
Overall, one of the most important gaps in the syphilis and STBBI literature resides in the lack of evaluation of implemented programs, interventions and policies. Rigorous evaluation design, using data on both pre- and post-intervention periods, among intervention and control groups, is needed, in order to expand our scientific understanding on the effectiveness of interventions for syphilis prevention and controlFootnote 291. Other evaluation methods can also be used, as required.
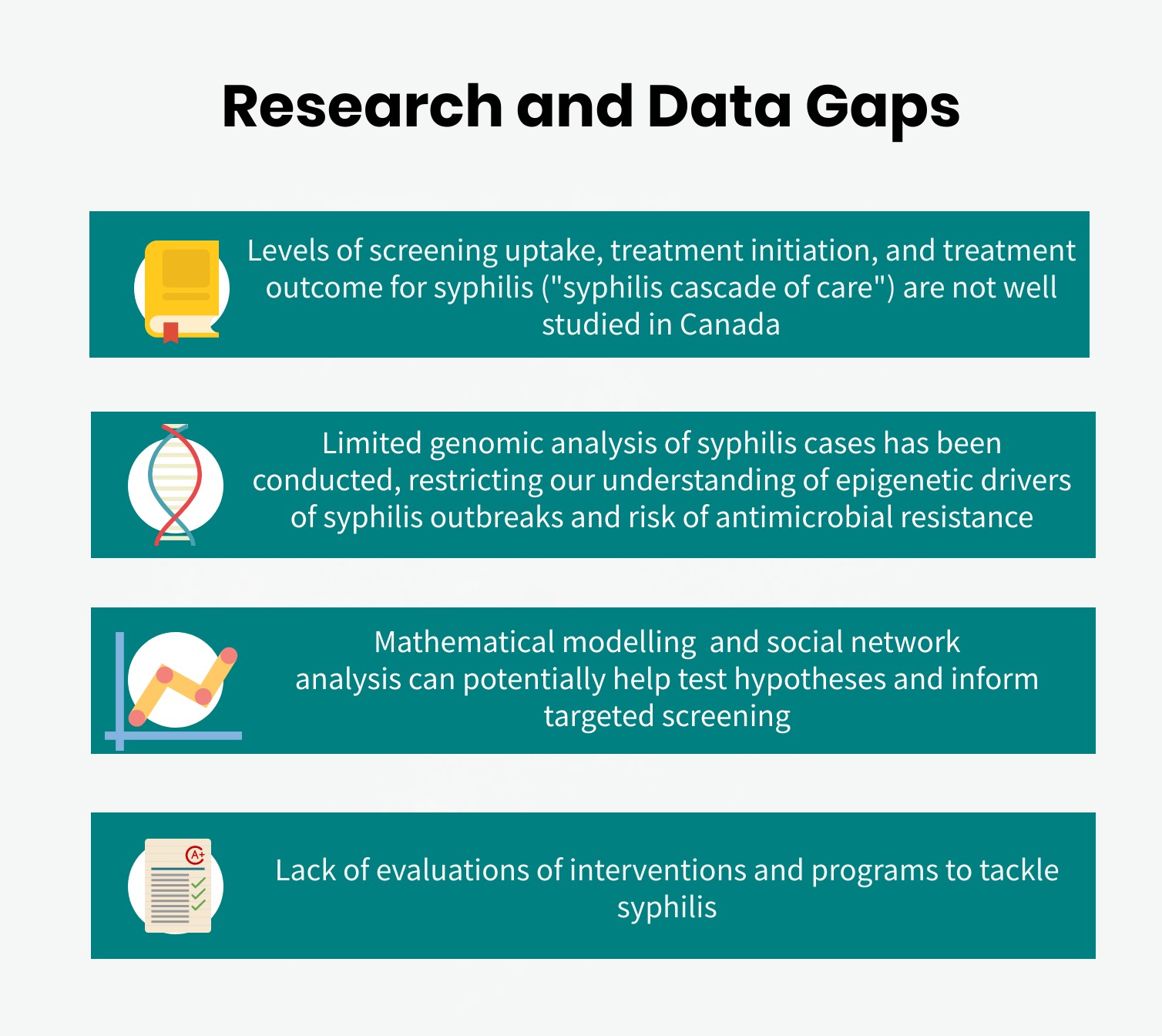
Infographic 10 - Text description
- Levels of screening uptake, treatment initiation, and treatment outcome for syphilis (“syphilis cascade of care”) are not well studied in Canada
- Limited genomic analysis of syphilis cases has been conducted, restricting our understanding of epigenetic drivers of syphilis outbreaks and risk of antimicrobial resistance
- Mathematical modelling and social network analysis can potentially help test hypotheses and inform targeted screening
- Lack of evaluations of interventions and programs to tackle syphilis
6.6 Strategic policy and planning
6.6.1 Canada’s response
In June 2018, federal, provincial and territorial Ministers of Health jointly released a Pan-Canadian STBBI Framework for Action. The Framework provides a common vision, strategic goals, and guiding principles to support cohesive action to address STBBI, including syphilis. The Framework envisions a Canada where STBBI are rare and people living with these infections receive the care and support they need. The Framework outlines how Canada will contribute to reaching the global targets set by WHO for the year 2030 for HIV, viral hepatitis, and STIs (specifically syphilis, gonorrhea and HPV). Canada has endorsed these global targets. WHO’s global targets for syphilis for the year 2030 are as follows:
- 90% reduction of T. pallidum incidence globally;
- Fifty or fewer cases of congenital syphilis per 100,000 live births in 80% of countries.
In response to the Pan-Canadian STBBI Framework for Action, the Government of Canada launched its five-year action plan for these infections in July 2019 titled “Accelerating our response: Government of Canada five-year action plan on sexually transmitted and blood-borne infections”Footnote 278. The Action Plan aims to help address health inequalities and build more supportive environments for Canadians affected by STBBI, such as the syphilis outbreaks currently experienced in the country. In order to reduce the public health impact of STBBI, like syphilis, and support Canada’s contributions to meeting the global STBBI targets outlined above, the Action Plan aims to accelerate Canada’s efforts to prevent, diagnose and treat STBBI, and address barriers to care through the identification of seven priority areas:
- Moving toward truth and reconciliation with First Nations, Inuit and Métis Peoples;
- Addressing stigma and discrimination;
- Promoting community innovation—putting a priority on prevention;
- Reaching the undiagnosed—increasing access to STBBI testing;
- Providing prevention, treatment and care to populations that receive health services or coverage of health care benefits from the federal government;
- Leveraging existing knowledge and targeting future research; and
- Measuring impact—monitoring and reporting on trends and results.
In addition, as described in Section 6.4, SOICC was established in July 2019 in Canada in response to the increase in syphilis rates across the country. This committee includes representatives from all PTs, in particular those reporting current outbreaks, as well as representatives from various federal agencies (including PHAC, Indigenous Services Canada, Immigration, Refugees and Citizenship Canada, Department of National Defense). The committee, coordinated by PHAC, aims to share data on current syphilis outbreaks as well as best practices and lessons learned.
6.6.2 Planning in other OECD countries
Outside of Canada, several countries have developed national strategies for syphilis elimination.
In Australia, the Fourth National STI Strategy aims to reduce the transmission, morbidity and mortality associated with all STIs in the countryFootnote 257. Given outbreaks in Aboriginal and Torres Strait Islander communities, the National Strategy aims to eliminate the negative impact of stigma, discrimination and human rights issues on people’s health, as well as minimize the personal and social impacts of STIs. It also aims to reduce the prevalence of chlamydia, gonorrhea and infectious syphilis and eliminate congenital syphilis by 2022. Their priority areas include prevention education, testing and treatment, equitable access to care with a focus on innovative and emerging models of service delivery, such as peer-based testing and peer support, community-based testing and online testing. It also includes increasing the health workforce, addressing stigma, improving data quality and implementing enhanced surveillance.
In England, substantial increases of infectious syphilis diagnoses between 2008 and 2018 demonstrated a need to strengthen public health measures to reduce transmissionFootnote 261. England’s response for syphilis control and prevention emphasizes four prevention pillars: increasing testing frequency of high-risk gbMSM and re-testing cases after treatment, increasing the quality of partner notification, maintaining high antenatal screening coverage and vigilance for syphilis throughout antenatal care and sustaining targeted health promotion.
Following concerns raised about the increase of syphilis in the EU, the ECDC published a technical report, which included a range of response optionsFootnote 259. The proposed interventions were enhanced screening of key populations during routine testing or clinical monitoring, expanding testing outreach in venues, appropriate and effective partner notification, prevention education directed at the general population, and education of healthcare providers. In order to sustain low rates of congenital syphilis in the EU, prevention measures include universal early prenatal screening, retesting women at risk of acquiring syphilis during pregnancy, testing all women at delivery if they had not been tested before, collecting surveillance data in order to identify gaps in prevention, and the harmonization of congenital case definitions across the EU.
Ireland responded to STI and HIV outbreaks among gbMSM by identifying effective prevention interventions from the best available evidence and the resources required to implement them in an Irish settingFootnote 284. According to their evidence review, the interventions with the strongest evidence base include interventions aiming to increase condom use, peer-led group interventions, peer outreach within the gbMSM community, and in the case of HIV, universal coverage of antiretroviral treatment and treatment as prevention.
New Zealand identified priority actions under four key action areas, with the aim of covering the full spectrum of syphilis prevention and careFootnote 283. The first priority action is prevention and health promotion through promoting a healthy sexuality culture, which includes improving knowledge and awareness of syphilis, and promoting condom use and regular STI testing. The second priority, testing and management, is needed to ensure availability and access to syphilis testing, by increasing health professional awareness and understanding of syphilis, improving contact tracing, and ensuring the availability of sexual health specialists. The third priority is the prevention of congenital syphilis through antenatal testing and appropriate treatment of syphilis during pregnancy. Lastly, high quality surveillance and monitoring aims to improve the understanding of risk factors, and planning and evaluation of prevention and control activities.
Finally, faced with a growing syphilis epidemic in the 1990s, the US published The National Plan to Eliminate Syphilis from the USFootnote 413. The US’ plan supported activities in several areas, including sustained STBBI prevention programs, a commitment to multi-sectoral partnerships, a comprehensive health communication plan, a systematic approach to quality assurance and evaluation of screening, treatment, and surveillance systems, as well as, training, planning and priority-setting for researchFootnote 413. The CDC has recently published a call to action detailing what can be done in specific populations to reduce syphilis transmissionFootnote 282. These specific populations include pregnant women, gbMSM, health-care providers, decision-makers, biomedical scientists and more. This call to action highlights the need to create new tools to detect and treat syphilis, to increase testing, to control the further spread of syphilis, and to improve electronic medical records in order to improve patient outcomes.
7. Conclusion
This report on syphilis provides a comprehensive overview of the latest infectious and congenital syphilis epidemiological trends in Canada, associated risk factors, and interventions that can be implemented in an effort to reduce the burden of disease in affected populations, The report highlights the complexity of the disease, in terms of its natural history, screening and diagnosis, as well as epidemiology and prevention.
Syphilis is a complex, multi-stage sexually and vertically transmitted infection. Some symptoms are unspecific and, as a result, it is easy for syphilis to go undetected. Testing is also challenging; the wide variety of tests that are currently in use for diagnosing and staging syphilis can make the interpretation of testing results complex, and may require the insights of an experienced clinician. If syphilis goes undetected and is left untreated, the infection can cause serious health consequences in babies, youth and adults.
The epidemiology of syphilis has changed markedly over the past few decades in Canada, a trend that has been paralleled in numerous high-income countries. Following years of low and stable rates of syphilis in the 1990s, rates began to increase in the 2000s, mainly among gbMSM. Since then, in the past three years, rates have increased significantly in other populations, such as women and heterosexual men, although gbMSM remain the most affected population. Risk factors of infectious syphilis vary across these populations, making it difficult to apply a one-size-fits-all intervention. Determinants of health, such as socioeconomic factors, physical environment, sexual behaviours, experiences of discrimination and stigma, as well as health policy and programs, are examples of broader social determinants, which shape an individual’s risk of syphilis acquisition.
Syphilis is a preventable and treatable disease. Condom use, as well as education-based initiatives and educational resources on healthy sexuality for both patients and service providers, can be effective primary prevention measures. Interventions designed to make accessing testing more comfortable, convenient and responsive to the needs of particular populations, such as gbMSM, can help ensure quicker access to care and improved linkage to treatment. It is recommended that pregnant women undergo screening at first trimester, at 28-32 weeks (3rd trimester) and at delivery, particularly in areas at high risk of transmission. Among harder-to-reach populations, several initiatives, such as syphilis testing in emergency departments, as well as online screening services, have been found to promote higher rates of screening. Another proposed strategy for improving linkage to care is POC testing, which is designed to increase the accessibility of screening in populations that may be more hesitant or who may experience barriers to accessing traditional screening. Addressing structural barriers and adopting culturally adapted approaches is of paramount importance to all syphilis prevention and control efforts. Moreover, collaboration between clinicians, public health professionals, community-based organizations and researchers is key to successfully prevent and control syphilis in Canada.
References
- Footnote 1
-
Tampa M, Sarbu I, Matei C, Benea V, Georgescu SR. Brief history of syphilis. J Med Life. 2014;7(1):4-10.
- Footnote 2
-
Singh AE, Romanowski B. Syphilis: Review with Emphasis on Clinical, Epidemiologic, and Some Biologic Features. Clin Microbiol Rev. 1999;12(2):187-209.
- Footnote 3
-
Public Health Agency of Canada. Section 5-10: Canadian Guidelines on Sexually Transmitted Infections- Management and treatment of specific infections - Syphilis. 2018;2019.
- Footnote 4
-
Harter C, Benirschke K. Fetal syphilis in the first trimester. Am J Obstet Gynecol. 1976;124(7):705-711.
- Footnote 5
-
Wijesooriya NS, Rochat RW, Kamb ML, et al. Global burden of maternal and congenital syphilis in 2008 and 2012: a health systems modelling study. Lancet Glob Health. 2016;4(8):e525-33.
- Footnote 6
-
Public Health Agency of Canada. List of nationally notifiable diseases. https://diseases.canada.ca/notifiable/diseases-list. Updated 20182019.
- Footnote 7
-
Gjestland T. The Oslo study of untreated syphilis; an epidemiologic investigation of the natural course of the syphilitic infection based upon a re-study of the Boeck-Bruusgaard material. Acta Derm Venereol Suppl (Stockh). 1955;35(Suppl 34):3-368.
- Footnote 8
-
Fast D, Small W, Wood E, Kerr T. The perspectives of injection drug users regarding safer injecting education delivered through a supervised injecting facility. Harm Reduct J. 2008;5:32.
- Footnote 9
-
Tsimis ME, Sheffield JS. Update on syphilis and pregnancy. Birth Defects Res. 2017;109(5):347-352.
- Footnote 10
-
Canadian Paediatric Society. Congenital syphilis: No longer just of historical interest. https://www.cps.ca/en/documents/position/congenital-syphilis. Updated 20182019.
- Footnote 11
-
Public Health Agency of Canada. Section 6-4: Canadian Guidelines on Sexually Transmitted Infections - Specific populations - Pregnancy. 2017. https://www.canada.ca/en/public-health/services/infectious-diseases/sexual-health-sexually-transmitted-infections/canadian-guidelines/sexually-transmitted-infections/canadian-guidelines-sexually-transmitted-infections-41.html.
- Footnote 12
-
MacPherson DW, Gushulak BD. Syphilis in immigrants and the Canadian immigration medical examination. J Immigr Minor Health. 2008;10(1):1-6.
- Footnote 13
-
Government of Canada. Who must submit to an immigration medical examination. https://www.canada.ca/en/immigration-refugees-citizenship/corporate/publications-manuals/operational-bulletins-manuals/standard-requirements/medical-requirements/exam/who-must-submit-immigration-medical-examination.html. Updated 20192019.
- Footnote 14
-
Immigration, Refugees and Citizenship Canada. Syphilis Screening and Management. 2015. https://www.canada.ca/content/dam/ircc/migration/ircc/english/department/partner/pp/pdf/imei_syphilis.pdf.
- Footnote 15
-
Ratnam S. The laboratory diagnosis of syphilis. Can J Infect Dis Med Microbiol. 2005;16(1):45-51.
- Footnote 16
-
Larsen S, Pope V, Johnson R, Kennedy E. A manual of tests for syphilis, American Public Health Association. 9th ed. American Public Health Association; 1998:361.
- Footnote 17
-
Park IU, Fakile YF, Chow JM, et al. Performance of Treponemal Tests for the Diagnosis of Syphilis. Clin Infect Dis. 2019;68(6):913-918.
- Footnote 18
-
Riviere GR, Wagoner MA, Baker-Zander SA, et al. Identification of spirochetes related to Treponema pallidum in necrotizing ulcerative gingivitis and chronic periodontitis. N Engl J Med. 1991;325(8):539-543.
- Footnote 19
-
Tsang RS, Radons SM, Morshed M. Laboratory diagnosis of syphilis: A survey to examine the range of tests used in Canada. Can J Infect Dis Med Microbiol. 2011;22(3):83-87.
- Footnote 20
-
Singh AE, Wong T, De P. Characteristics of primary and late latent syphilis cases which were initially non-reactive with the rapid plasma reagin as the screening test. Int J STD AIDS. 2008;19(7):464-468.
- Footnote 21
-
Park IU, Chow JM, Bolan G, Stanley M, Shieh J, Schapiro JM. Screening for syphilis with the treponemal immunoassay: analysis of discordant serology results and implications for clinical management. J Infect Dis. 2011;204(9):1297-1304.
- Footnote 22
-
Mishra S, Boily MC, Ng V, et al. The laboratory impact of changing syphilis screening from the rapid-plasma reagin to a treponemal enzyme immunoassay: a case-study from the Greater Toronto Area. Sex Transm Dis. 2011;38(3):190-196.
- Footnote 23
-
Gratrix J, Plitt S, Lee BE, et al. Impact of reverse sequence syphilis screening on new diagnoses of late latent syphilis in Edmonton, Canada. Sex Transm Dis. 2012;39(7):528-530.
- Footnote 24
-
Walter EK, Smith JL, Israel CW, Gager WE. A new modification of the Krajian silver stain for Treponema pallidum. Br J Vener Dis. 1969;45(1):6-9.
- Footnote 25
-
Hoang MP, High WA, Molberg KH. Secondary syphilis: a histologic and immunohistochemical evaluation. J Cutan Pathol. 2004;31(9):595-599.
- Footnote 26
-
Fernandez-Flores A. Immunostaining for Treponema pallidum: caution in its evaluation. Am J Dermatopathol. 2010;32(5):523-525.
- Footnote 27
-
Chen CY, Ballard RC. The molecular diagnosis of sexually transmitted genital ulcer disease. Methods Mol Biol. 2012;903:103-112.
- Footnote 28
-
Centurion-Lara A, Castro C, Shaffer JM, Van Voorhis WC, Marra CM, Lukehart SA. Detection of Treponema pallidum by a sensitive reverse transcriptase PCR. J Clin Microbiol. 1997;35(6):1348-1352.
- Footnote 29
-
Golden M, O'Donnell M, Lukehart S, et al. Treponema pallidum Nucleic Acid Amplification Testing To Augment Syphilis Screening among Men Who Have Sex with Men. J Clin Microbiol. 2019;57(8):19. Print 2019 Aug.
- Footnote 30
-
Heymans R, van der Helm JJ, de Vries HJ, Fennema HS, Coutinho RA, Bruisten SM. Clinical value of Treponema pallidum real-time PCR for diagnosis of syphilis. J Clin Microbiol. 2010;48(2):497-502.
- Footnote 31
-
Gayet-Ageron A, Sednaoui P, Lautenschlager S, et al. Use of Treponema pallidum PCR in testing of ulcers for diagnosis of primary syphilis. Emerg Infect Dis. 2015;21(1):127-129.
- Footnote 32
-
Gayet-Ageron A, Lautenschlager S, Ninet B, Perneger TV, Combescure C. Sensitivity, specificity and likelihood ratios of PCR in the diagnosis of syphilis: a systematic review and meta-analysis. Sex Transm Infect. 2013;89(3):251-256.
- Footnote 33
-
Dubourg G, Edouard S, Prudent E, Fournier PE, Raoult D. Incidental Syphilis Diagnosed by Real-Time PCR Screening of Urine Samples. J Clin Microbiol. 2015;53(11):3707-3708.
- Footnote 34
-
Godornes C, Ciccarese G, Drago F, Giacani L. Treponema pallidum subsp. pallidum DNA and RNA in Semen of a Syphilis Patient Without Genital or Anal Lesions. Sex Transm Dis. 2019;46(6):e62-e64.
- Footnote 35
-
Yang CJ, Chang SY, Wu BR, et al. Unexpectedly high prevalence of Treponema pallidum infection in the oral cavity of human immunodeficiency virus-infected patients with early syphilis who had engaged in unprotected sex practices. Clin Microbiol Infect. 2015;21(8):787.e1-787.e7.
- Footnote 36
-
Futami S, Takimoto T, Nakagami F, et al. A lung abscess caused by secondary syphilis - the utility of polymerase chain reaction techniques in transbronchial biopsy: a case report. BMC Infect Dis. 2019;19(1):598.
- Footnote 37
-
Smith JR, Tsang RS, Kadkhoda K. Tonsillar Syphilis: an Unusual Site of Infection Detected by Treponema pallidum PCR. J Clin Microbiol. 2015;53(9):3089-3091.
- Footnote 38
-
Anid G, Isaac M, Penner CR, Van Caeseele P, Tsang RS, Kadkhoda K. A non-healing syphilid: Another face of the great imitator. IDCases. 2017;8:14-16.
- Footnote 39
-
Grillova L, Jolley K, Šmajs D, Picardeau M. A public database for the new MLST scheme for Treponema pallidum subsp. pallidum: surveillance and epidemiology of the causative agent of syphilis. PeerJ. 2019;6:e6182.
- Footnote 40
-
Lukehart SA, Godornes C, Molini BJ, et al. Macrolide resistance in Treponema pallidum in the United States and Ireland. N Engl J Med. 2004;351(2):154-158.
- Footnote 41
-
Matejkova P, Flasarova M, Zakoucka H, et al. Macrolide treatment failure in a case of secondary syphilis: a novel A2059G mutation in the 23S rRNA gene of Treponema pallidum subsp. pallidum. J Med Microbiol. 2009;58(Pt 6):832-836.
- Footnote 42
-
Drain PK, Hyle EP, Noubary F, et al. Diagnostic point-of-care tests in resource-limited settings. Lancet Infect Dis. 2014;14(3):239-249.
- Footnote 43
-
World Health Organization. Point-Of-Care Diagnostic Tests (POCTs) for Sexually Transmitted Infections (STIs). https://www.who.int/reproductivehealth/topics/rtis/pocts/en/. Updated 20192019.
- Footnote 44
-
Marks M, Mabey DC. The introduction of syphilis point of care tests in resource limited settings. Expert Rev Mol Diagn. 2017;17(4):321-325.
- Footnote 45
-
Government of Canada. Medical Devices - Special Access Programme. https://www.canada.ca/en/health-canada/services/drugs-health-products/special-access/medical-devices.html. Updated 20202020.
- Footnote 46
-
Mahoney JF, Arnold RC, Harris A. Penicillin Treatment of Early Syphilis-A Preliminary Report. Am J Public Health Nations Health. 1943;33(12):1387-1391.
- Footnote 47
-
Peter G, Dudley MN. Clinical pharmacology of benzathine penicillin G. Pediatr Infect Dis. 1985;4(5):586-591.
- Footnote 48
-
Shuel M., Hayden K., Kadkhoda K., Tsang R.S.W. Molecular typing and macrolide resistance of syphilis cases in Manitoba, Canada, from 2012 to 2016. Sex Transm Dis. 2018;45(4):233-236.
- Footnote 49
-
Clement ME, Okeke NL, Hicks CB. Treatment of syphilis: a systematic review. JAMA. 2014;312(18):1905-1917.
- Footnote 50
-
Donders GG, Desmyter J, Hooft P, Dewet GH. Apparent failure of one injection of benzathine penicillin G for syphilis during pregnancy in human immunodeficiency virus-seronegative African women. Sex Transm Dis. 1997;24(2):94-101.
- Footnote 51
-
Public Health Agency of Canada. Report on Sexually Transmitted Infections in Canada, 2017. 2019. https://www.canada.ca/en/public-health/services/publications/diseases-conditions/report-sexually-transmitted-infections-canada-2017.html.
- Footnote 52
-
Health Canada. Proceedings of National STD Consensus Meeting and National Goals for the Prevention and Control of Sexually Transmitted Diseases in Canada. CCDR. 1997;23(S6). http://publications.gc.ca/collections/collection_2016/aspc-phac/HP3-1-23-S6-eng.pdf.
- Footnote 53
-
Manitoba Health, Seniors and Active Living. Update of Infectious Syphilis in Manitoba - Dec 2015. 2015. https://www.gov.mb.ca/health/publichealth/factsheets/syph_update.pdf.
- Footnote 54
-
Public Health Agency of Canada. Infectious syphilis in Canada, 2018. https://www.canada.ca/en/public-health/services/reports-publications/canada-communicable-disease-report-ccdr/monthly-issue/2019-45/issue-11-november-7-2019/article-5-infectious-syphilis-canada-2009-2018.html. Updated 2019. Accessed November 8, 2019.
- Footnote 55
-
Choudhri Y, Miller J, Sandhu J, Leon A, Aho J. Infectious and congenital syphilis in Canada, 2010-2015. Can Commun Dis Rep. 2018;44(2):43-48.
- Footnote 56
-
Ogilvie GS, Taylor DL, Moniruzzaman A, et al. A population-based study of infectious syphilis rediagnosis in British Columbia, 1995-2005. Clin Infect Dis. 2009;48(11):1554-1558.
- Footnote 57
-
Deonarine A., Ogilvie G., Montgomery C., et al. Trends in Syphilis Partner Notification among Gay, Bisexual, and Other Men who Have Sex with Men in British Columbia, 2010 to 2013. Sex Transm Dis. 2016;43(8):489-493.
- Footnote 58
-
Shaw S.Y., Ross C., Nowicki D.L., et al. Infectious syphilis in women: what's old is new again? Int J STD AIDS. 2017;28(1):77-87.
- Footnote 59
-
Landry T, Smyczek P, Cooper R, et al. Retrospective review of tertiary and neurosyphilis cases in Alberta, 1973-2017. BMJ Open. 2019;9(6):e025995.
- Footnote 60
-
Wong T, Singh A, Mann J, Hansen L, McMahon S. Gender Differences in Bacterial STIs in Canada. BMC Womens Health. 2004;4(Suppl 1):S26-6874-4-S1-S26.
- Footnote 61
-
Kwong JC, Crowcroft NS, Campitelli MA, et al. Ontario Burden of Infectious Diseases Study (ONBOIDS). 2010.
- Footnote 62
-
Yu D, Hatala AR, Reimer J, Lorway R. 'I'm more aware of my HIV risk than anything else': syndemics of syphilis and HIV among gay men in Winnipeg. Cult Health Sex. 2018;20(9):1036-1048.
- Footnote 63
-
Rzepa T, Zaba R, Silny W. Management of the stressful stigma attached to sexually transmitted disease (preliminary report). Ginekol Pol. 2011;82(9):675-679.
- Footnote 64
-
Stoltey JE, Cohen SE. Syphilis transmission: a review of the current evidence. Sex Health. 2015;12(2):103-109.
- Footnote 65
-
Garnett GP, Aral SO, Hoyle DV, Cates W,Jr, Anderson RM. The natural history of syphilis. Implications for the transmission dynamics and control of infection. Sex Transm Dis. 1997;24(4):185-200.
- Footnote 66
-
Gomez GB, Kamb ML, Newman LM, Mark J, Broutet N, Hawkes SJ. Untreated maternal syphilis and adverse outcomes of pregnancy: a systematic review and meta-analysis. Bull World Health Organ. 2013;91(3):217-226.
- Footnote 67
-
De Santis M, De Luca C, Mappa I, et al. Syphilis Infection during pregnancy: fetal risks and clinical management. Infect Dis Obstet Gynecol. 2012;2012:430585.
- Footnote 68
-
Qin J, Yang T, Xiao S, Tan H, Feng T, Fu H. Reported estimates of adverse pregnancy outcomes among women with and without syphilis: a systematic review and meta-analysis. PLoS One. 2014;9(7):e102203.
- Footnote 69
-
Lumbiganon P, Piaggio G, Villar J, et al. The epidemiology of syphilis in pregnancy. Int J STD AIDS. 2002;13(7):486-494.
- Footnote 70
-
Jiang H, Lukac C, Ogilvie G, Gilbert M, Grennan T, Wong J. O13.5 Core groups of individuals with chlamydia and/or gonorrhoea reinfections have increased odds of diagnosis with infectious syphilis: a population-based retrospective cohort study in British Columbia, Canada, 2006-2015. Sex Transm Infect. 2017;93(Suppl 2):A30-A31.
- Footnote 71
-
Singer M, Clair S. Syndemics and public health: reconceptualizing disease in bio-social context. Med Anthropol Q. 2003;17(4):423-441.
- Footnote 72
-
Lang R, Read R, Krentz HB, et al. Increasing incidence of syphilis among patients engaged in HIV care in Alberta, Canada: a retrospective clinic-based cohort study. BMC Infect Dis. 2018;18(1):125-4.
- Footnote 73
-
Remis RS, Liu J, Loutfy MR, et al. Prevalence of Sexually Transmitted Viral and Bacterial Infections in HIV-Positive and HIV-Negative Men Who Have Sex with Men in Toronto. PLoS One. 2016;11(7).
- Footnote 74
-
Solomon MM, Mayer KH, Glidden DV, et al. Syphilis predicts HIV incidence among men and transgender women who have sex with men in a preexposure prophylaxis trial. Clin Infect Dis. 2014;59(7):1020-1026.
- Footnote 75
-
Karp G, Schlaeffer F, Jotkowitz A, Riesenberg K. Syphilis and HIV co-infection. Eur J Intern Med. 2009;20(1):9-13.
- Footnote 76
-
Singer MC, Erickson PI, Badiane L, et al. Syndemics, sex and the city: understanding sexually transmitted diseases in social and cultural context. Soc Sci Med. 2006;63(8):2010-2021.
- Footnote 77
-
Zetola NM, Klausner JD. Syphilis and HIV infection: an update. Clin Infect Dis. 2007;44(9):1222-1228.
- Footnote 78
-
Konrad S, Mak DB, Grennan T, et al. Characteristics of Gay, Bisexual and Other Men Who Have Sex With Men With Multiple Diagnoses of Infectious Syphilis in British Columbia, Canada, 2005-2014. Sex Transm Dis. 2019;46(7):423-428.
- Footnote 79
-
Gross G, Tyring SK, eds. Sexually Transmitted Infections and Sexually Transmitted Diseases. Springer, Berlin, Heidelberg; 2011.
- Footnote 80
-
World Health Organization. Global Health Sector Strategy on Sexually Transmitted Infections 2016-2021. WHO. 2016. https://apps.who.int/iris/bitstream/handle/10665/246296/WHO-RHR-16.09-eng.pdf;jsessionid=712E73B29806C8179B33AF4587528BD2?sequence=1.
- Footnote 81
-
Simms I, Goh BT, French P, et al. A brief recent history of the epidemiology of congenital syphilis in the United Kingdom. Int J STD AIDS. 2018;29(11):1110-1119.
- Footnote 82
-
Centers for Disease Control and Prevention. Figure 40. Primary and Secondary Syphilis - Rates of Reported Cases by Sex and Male-to-Female Rate Ratios, United States, 1990-2017. https://www.cdc.gov/std/stats17/figures/40.htm. Updated 2018. Accessed September 10, 2019.
- Footnote 83
-
Nguyen TQ, Kohn RP, Ng RC, Philip SS, Cohen SE. Historical and Current Trends in the Epidemiology of Early Syphilis in San Francisco, 1955 to 2016. Sex Transm Dis. 2018;45(9S Suppl 1):S55-S62.
- Footnote 84
-
Hegazi A, Lee MJ, Whittaker W, et al. Chemsex and the city: sexualised substance use in gay bisexual and other men who have sex with men attending sexual health clinics. Int J STD AIDS. 2017;28(4):362-366.
- Footnote 85
-
Kirby Institute. HIV, viral hepatitis and sexually transmissible infections in Australia: annual surveillance report 2018. 2018. https://kirby.unsw.edu.au/sites/default/files/kirby/report/KI_Annual-Surveillance-Report-2018.pdf.
- Footnote 86
-
European Centre for Disease Prevention and Control. Syphilis - Annual epidemiological report for 2017. 2019. https://ecdc.europa.eu/en/publications-data/syphilis-annual-epidemiological-report-2017#no-link.
- Footnote 87
-
Centers for Disease Control and Prevention. Table 27. Primary and Secondary Syphilis - Reported Cases and Rates of Reported Cases by State/Area and Region in Alphabetical Order, United States and Outlying Areas, 2013-2017. https://www.cdc.gov/std/stats17/tables/27.htm. Updated 2018. Accessed September 10, 2019.
- Footnote 88
-
Government of Canada. Canadian Notifiable Disease Surveillance System. https://diseases.canada.ca/notifiable/charts-list. Updated 2018-2019.
- Footnote 89
-
Nova Scotia Health Authority. Public Health warns of syphilis outbreak in Nova Scotia. 2020. http://www.nshealth.ca/news/public-health-warns-syphilis-outbreak-nova-scotia.
- Footnote 90
-
British Columbia Centre for Disease Control. BC experiencing highest rates of infectious syphilis in the last 30 years. http://www.bccdc.ca/bc-experiencing-highest-rates-of-infectious-syphilis-in-the-last-30-years. Updated 20192019.
- Footnote 91
-
British Columbia Centre for Disease Control. Reportable Diseases Data Dashboard. http://www.bccdc.ca/health-professionals/data-reports/reportable-diseases-data-dashboard?Disease=Syphilis. Updated 20192019.
- Footnote 92
-
British Columbia Centre for Disease Control. STI in British Columbia: Annual Surveillance Report 2016. 2018. http://www.bccdc.ca/resource-gallery/Documents/Statistics%20and%20Research/Statistics%20and%20Reports/STI/STI_Annual_Report_2016.pdf.
- Footnote 93
-
British Columbia Centre for Disease Control. British Columbia Annual Summary of Reportable Diseases 2017. 2019:70. http://www.bccdc.ca/resource-gallery/Documents/Statistics%20and%20Research/Statistics%20and%20Reports/Epid/Annual%20Reports/Syphilis.pdf.
- Footnote 94
-
Alberta Health. Alberta Sexually Transmitted Infections and HIV 2018. 2019. https://open.alberta.ca/dataset/c6850032-20d3-4845-a465-568ed7e61b7c/resource/bc62d5d8-9b20-4e26-820e-65d43cabf3c5/download/alberta-sexually-transmitted-infections-and-hiv-2018.pdf.
- Footnote 95
-
Alberta Health. Alberta STI 2016 Summary Report. 2017. https://open.alberta.ca/dataset/3a5f31be-a941-4bdf-9f95-7f5741d72fcf/resource/0444424f-71d1-4370-9328-9cb54485ab87/download/sti-alberta-2016-summary.pdf.
- Footnote 96
-
Alberta Health. Personal Communication with the Public Health Agency of Canada.
- Footnote 97
-
Government of Saskatchewan. Sexually Transmitted and Blood Borne Infections in Saskatchewan in 2017. https://www.saskatchewan.ca/residents/health/accessing-health-care-services/sexually-transmitted-infections-services.
- Footnote 98
-
Baxter D. Sask. HIV diagnoses up 18%, syphilis up 172% in 2019. Global News. February 4, 2020 2020. Available from: https://globalnews.ca/news/6491890/sask-hiv-diagnoses-up-18-syphilis-up-172-in-2019/.
- Footnote 99
-
International Society for Infectious Diseases. PRO/EDR> Syphilis - Canada (08): (SK,ON) incr. incidence, indigenous, women, meth use. 2019.
- Footnote 100
-
Saskatoon Health Region. Sexually Transmitted Infection - Syphilis. http://www.communityview.ca/pdfs/2017_shr_series4_sti_syphilis.pdf.
- Footnote 101
-
The Canadian Press. Saskatchewan experiencing HIV, syphilis outbreaks, health authority says. The Star. June 14 2019 2019. Available from: https://www.thestar.com/news/canada/2019/06/14/saskatchewan-experiencing-hiv-syphilis-outbreaks-health-authority-says.html.
- Footnote 102
-
Canadian Broadcasting Company News. Sask. reserves see outbreak of syphilis with 'unprecedented' 295% spike in cases. CBC News. July 19 2019 2019. Available from: https://www.cbc.ca/news/canada/saskatchewan/syphilis-outbreak-sask-reserves-1.5218482.
- Footnote 103
-
First Nations and Inuit Health Branch-Saskatchewan and Northern Inter-Tribal Health Authority. Sexually Transmitted Infections (STI) Saskatchewan Fist Nations Communities. 2019. http://s3.documentcloud.org/documents/6207405/Sexually-transmitted-infections-in-Sask.pdf.
- Footnote 104
-
Radio-Canada. Épidémie de syphilis déclarée dans les réserves autochtones en Saskatchewan. CBC. 2019. https://ici.radio-canada.ca/nouvelle/1229130/augmentation-cas-syphilis-saskatchewan-reserves-autocthones-epidemie.
- Footnote 105
-
Manitoba Health, Seniors and Active Living. Sexually Transmitted Infections in Manitoba 2014. 2016. https://www.gov.mb.ca/health/publichealth/surveillance/docs/stim2014.pdf.
- Footnote 106
-
Manitoba Health, Seniors and Active Living. Sexually Transmitted and Bloodborne Infections (STBBI) in Manitoba. 2018. https://www.gov.mb.ca/health/publichealth/cdc/docs/stbbi_poster.pdf.
- Footnote 107
-
Winnipeg Regional Health Authority. Syphilis Letter. 2018. http://www.wrha.mb.ca/professionals/familyphysicians/files/Syphilisletter.pdf.
- Footnote 108
-
Dunham J. Winnipeg grappling with unprecedented spike in syphilis cases. CTV News. August 15 2018 2018. Available from: https://www.ctvnews.ca/health/winnipeg-grappling-with-unprecedented-spike-in-syphilis-cases-1.4053719.
- Footnote 109
-
Manitoba Health, Seniors and Active Living. RE: Congenital Syphilis in Manitoba. 2019. http://www.manitoba.ca/health/publichealth/cdc/docs/hcp/2019/022519.pdf.
- Footnote 110
-
Froese I. Winnipeg's syphilis outbreak getting worse, health authority says. CBC News. May 15 2019 2019. Available from: https://www.cbc.ca/news/canada/manitoba/winnipeg-syphilis-outbreak-rising-wrha-worsening-1.5137687.
- Footnote 111
-
Manitoba Healthcare Providers Network. Northern Health Region. http://www.mhpnetwork.ca/mb-ho-northern.html. Accessed September 12, 2019.
- Footnote 112
-
Public Health Ontario. Monthly Infectious Diseases Surveillance Report (February 2019). 2019. https://www.publichealthontario.ca/-/media/documents/surveillance-reports/infectious/surveillance-report-infectious-diseases-jan-dec-2018.pdf?la=en.
- Footnote 113
-
Public Health Ontario. Reportable Disease Trends in Ontario: Archive of 2015 Summaries. 2017. https://www.publichealthontario.ca/-/media/documents/rdto-summaries-2015.pdf?la=en.
- Footnote 114
-
Northwestern Health Unit. Syphilis Epidemiologic Summary. 2019. https://www.nwhu.on.ca/Audiences/Documents/Syphilis%20Epi%20Summary%20-%20July%2030%202019.pdf.
- Footnote 115
-
Northwestern Health Unit. Medical Alert: Syphilis. 2018. https://www.nwhu.on.ca/Audiences/Documents/Health%20Alert%20-%20Syphilis.pdf.
- Footnote 116
-
Canadian Broadcasting Company News. Syphilis outbreak reported in northwestern Ontario. CBC News. July 15 2019 2019. Available from: https://www.cbc.ca/news/canada/thunder-bay/northwestern-ontario-syphilis-outbreak-1.5210288.
- Footnote 117
-
Northwestern Health Unit. Increase in Syphilis cases in the Region. 2019. https://www.nwhu.on.ca/MediaPressCentre/Media%20Releases/media%20release%20-%20Syphilis%20-%20July%202019.pdf.
- Footnote 118
-
Middlesex-London Health Unit. Health Unit Declares Community-Wide Syphilis Outbreak. 2019. https://www.healthunit.com/news/community-wide-syphilis-outbreak.
- Footnote 119
-
Peterborough Public Health. Alert: Syphilis Outbreak Declared. 2020. https://www.peterboroughpublichealth.ca/wp-content/uploads/2020/01/2020-01-03_Syphilis-Outbreak-Declared.pdf.
- Footnote 120
-
Payne E. Ottawa syphilis cases take 400 percent jump in five years. Ottawa Citizen. August 29, 2019 2019. Available from: https://ottawacitizen.com/news/local-news/ottawa-syphilis-cases-take-400-per-cent-jump-in-five-years.
- Footnote 121
-
Institut national de santé publique du Québec. Portrait des infections transmissibles sexuellement et par le sang (ITSS) au Québec: Année 2018 et Projections 2019. INSPQ. 2019. https://www.inspq.qc.ca/sites/default/files/publications/2612_infections_transmissibles_sexuellement_sang.pdf.
- Footnote 122
-
Institut national de santé publique du Québec. Portrait des infections transmissibles sexuellement et par le sang (ITSS) au Québec: Année 2017 et Projections 2018. 2018. https://www.inspq.qc.ca/sites/default/files/publications/2471_infections_transmissibles_sexuellement_sang_2017.pdf.
- Footnote 123
-
Government of New Brunswick. New Brunswick Communicable Disease 2017 Annual Surveillance Report. 2018. https://www2.gnb.ca/content/dam/gnb/Departments/h-s/pdf/en/CDC/HealthProfessionals/Annual_Report_CDC_Branch_2017.pdf.
- Footnote 124
-
Government of New Brunswick. Syphilis Outbreak Investigation Report. 2014. https://www.voixfemmesnb-voiceswomennb.ca/content/dam/gnb/Departments/h-s/pdf/en/CDC/HealthProfessionals/SyphillisReport.pdf.
- Footnote 125
-
Government of New Brunswick. New Brunswick Report on Sexually Transmitted and Blood Borne Infections, 2016. https://www2.gnb.ca/content/dam/gnb/Departments/h-s/pdf/en/CDC/STBBI-Report-2016.pdf.
- Footnote 126
-
Government of Newfoundland and Labrador. Syphilis Clinical Management 2015. 2015. https://www.health.gov.nl.ca/health/publichealth/cdc/Syphilis_Clinical_Mgnt.pdf.
- Footnote 127
-
Eastern Health. Health Status Report Chapter 15: Sexual Health. 2017. http://www.easternhealth.ca/OurCommunity.aspx?d=1&id=2217&p=379.
- Footnote 128
-
Nova Scotia Department of Health and Wellness. Notifiable Diseases in Nova Scotia 2017 Surveillance Report. https://novascotia.ca/dhw/populationhealth/documents/Annual-Notifiable-Disease-Surveillance-Report-2017.pdf.
- Footnote 129
-
Nova Scotia Health and Wellness. Notifiable Diseases in Nova Scotia 2014 Surveillance Report. https://novascotia.ca/dhw/populationhealth/documents/Annual-Notifiable-Disease-Surveillance-Report-2014.pdf.
- Footnote 130
-
Nova Scotia Health Authority. Public Health Alert - SA-004115 Subject: Increase in Syphilis Cases in Nova Scotia. 2020. https://www.nshealth.ca/news/public-health-warns-syphilis-outbreak-nova-scotia.
- Footnote 131
-
Prince Edward Island Health and Wellness. Sexually Transmitted and Bloodborne Infection Rates in PEI. https://www.princeedwardisland.ca/en/information/health-and-wellness/sexually-transmitted-and-bloodborne-infection-rates-pei. Updated 2019. Accessed September 12, 2019.
- Footnote 132
-
Prince Edward Island Health and Wellness. Promote, Prevent, Protect - PEI Chief Public Health Officer's Report 2016 Health for all Islanders. https://www.princeedwardisland.ca/sites/default/files/publications/cphorpt16_linkd.pdf.
- Footnote 133
-
Yukon Health and Social Services. Yukon Health Status Report 2015: Focus on Substance Use. http://www.yukoncmoh.ca/files/health_status_report_2015.pdf.
- Footnote 134
-
Northwest Territories Health and Social Services. Northwest Territories Health Status Report. 2011. https://www.assembly.gov.nt.ca/sites/default/files/11-08-22td60-166.pdf.
- Footnote 135
-
Northwest Territories Health and Social Services. Syphilis. https://www.hss.gov.nt.ca/en/services/syphilis. Accessed September 12, 2019.
- Footnote 136
-
Northwest Territories Health and Social Services. STI Rates Increasing. https://www.hss.gov.nt.ca/en/newsroom/sti-rates-increasing. Updated 2019. Accessed September 12, 2019.
- Footnote 137
-
Strong W. N.W.T. health officials using dating apps to combat syphilis outbreak. CBC News. 22 August 2019 2019. Available from: https://www.cbc.ca/news/canada/north/syphilis-outbreak-nwt-1.5255813.
- Footnote 138
-
Government of Nunavut. Sexually Transmitted Infection Rates in Nunavut, 2008-2015. https://www.gov.nu.ca/sites/default/files/170714_sti_report_nu_2015_update.pdf.
- Footnote 139
-
Government of Nunavut. Syphilis Outbreak in Nunavut: 2013 Summary. https://gov.nu.ca/sites/default/files/files/Syphilis%20Outbreak%20Summary%202013(1).pdf.
- Footnote 140
-
Public Health Agency of Canada. Chief Public Health Officer of Canada: A Health Equity Approach and Areas of Focus. 2018. https://www.canada.ca/content/dam/phac-aspc/images/corporate/canadas-chief-public-health-officer/CPHO-Priorities-Placemat-Tags-EN.pdf.
- Footnote 141
-
Government of Canada. Social determinants of health and health inequalitites. https://www.canada.ca/en/public-health/services/health-promotion/population-health/what-determines-health.html. Updated 2019.
- Footnote 142
-
Galea S, Ahern J, Vlahov D. Contextual determinants of drug use risk behavior: a theoretic framework. J Urban Health. 2003;80(4 Suppl 3):iii50-8.
- Footnote 143
-
Aral SO. Determinants of STD epidemics: implications for phase appropriate intervention strategies. Sex Transm Infect. 2002;78 Suppl 1:i3-13.
- Footnote 144
-
Boerma JT, Weir SS. Integrating demographic and epidemiological approaches to research on HIV/AIDS: the proximate-determinants framework. J Infect Dis. 2005;191 Suppl 1:S61-7.
- Footnote 145
-
British Columbia Centre for Disease Control. BC Syphilis Action Plan. 2016. http://www.bccdc.ca/resource-gallery/Documents/Statistics%20and%20Research/Statistics%20and%20Reports/STI/Syphilis%20Action%20Plan.pdf. Accessed March 4, 2020.
- Footnote 146
-
Public Health Agency of Canada. Pan-Canadian sexually transmitted and blood-borne infections framework for action: infographic. 2016. https://www.canada.ca/en/services/health/publications/diseases-conditions/pan-canadian-sexually-transmitted-blood-borne-infections-framework-action-infographic.html.
- Footnote 147
-
Public Health Agency of Canada. Update on Sexually Transmitted Infections in Canada, 2016. 2019:18. https://www.canada.ca/fr/sante-canada/services/publications/maladies-et-affections/mise-a-jour-infections-transmissibles-sexuellement-canada-2016.html#5.2.
- Footnote 148
-
D'Angelo-Scott H., Cutler J., Friedman D., Hendriks A., Jolly A.M. Social network investigation of a syphilis outbreak in ottawa, Ontario. Can J Infect Dis Med Microbiol. 2015;26(5):268-272.
- Footnote 149
-
Totten S, MacLean R, Payne E. Infectious syphilis in Canada: 2003-2012. Can Commun Dis Rep. 2015;41(2):30-34.
- Footnote 150
-
de Voux A, Kidd S, Grey JA, et al. State-Specific Rates of Primary and Secondary Syphilis Among Men Who Have Sex with Men - United States, 2015. MMWR. 2017(66(13)):349-354.
- Footnote 151
-
Shaw S., Lapple A., Reimer J., et al. The evolution of an infectious syphilis epidemic in a Canadian urban setting. Sex Transm Infect. 2019;95:A330. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emexb&NEWS=N&AN=629059743.
- Footnote 152
-
Gupta GR. Gender, sexuality, and HIV/AIDS: the what, the why, and the how. Can HIV AIDS Policy Law Rev. 2000;5(4):86-93.
- Footnote 153
-
Gahagan J, Ricci C. HIV/AIDS Prevention for Women in Canada: A Meta-Ethnographic Synthesis. 2011. https://www.catie.ca/sites/default/files/HIV%20AIDS%20prevention%20for%20women%20in%20canada.pdf.
- Footnote 154
-
Gahagan J. Gender Matters in HIV Prevention. Prevention in Focus. 2012. https://www.catie.ca/en/pif/spring-2012/gender-matters-hiv-prevention.
- Footnote 155
-
Curtin N, Ward LM, Merriwether A, Caruthers A. Femininity Ideology and Sexual Health in Young Women: A focus on Sexual Knowledge, Embodiment, and Agency. Int J Sex Health. 2011;23(1):48-62.
- Footnote 156
-
Dworkin SL, Exner T, Melendez R, Hoffman S, Ehrhardt AA. Revisiting "Success": Posttrial analysis of a gender-specific HIV/STD prevention intervention. AIDS Behav. 2006;10(1):41-51.
- Footnote 157
-
Spiwak R, Afifi TO, Halli S, Garcia-Moreno C, Sareen J. The relationship between physical intimate partner violence and sexually transmitted infection among women in India and the United States. J Interpers Violence. 2013;28(13):2770-2791.
- Footnote 158
-
Garfinkel M, Blumstein H. Gender differences in testing for syphilis in emergency department patients diagnosed with sexually transmitted diseases. J Emerg Med. 1999;17(6):937-940.
- Footnote 159
-
Safren SA, Reisner SL, Herrick A, Mimiaga MJ, Stall R. Mental Health and HIV Risk in Men Who Have Sex with Men. J Acquir Immune Defic Syndr. 2010;55(Suppl 2):S74-7.
- Footnote 160
-
Kerrigan D, Andrinopoulos K, Chung SE, Glass B, Ellen J. Gender ideologies, socioeconomic opportunities, and HIV/STI-related vulnerability among female, African-American adolescents. J Urban Health. 2008;85(5):717-726.
- Footnote 161
-
Goedel WC, Safren SA, Mayer KH, Duncan DT. Community-level norms and condomless anal intercourse among gay, bisexual, and other men who have sex with men who use geosocial-networking smartphone applications in the Deep South. J HIV AIDS Soc Serv. 2017;16(4):382-389.
- Footnote 162
-
EKOS Research Associates Inc. Canadians' Awareness, Knowledge and Attitudes Related to Sexually Transmitted and Blood-Borne Infections: 2018 Findings Report. 2018. http://epe.lac-bac.gc.ca/100/200/301/pwgsc-tpsgc/por-ef/public_health_agency_canada/2018/056-17-e/report.pdf.
- Footnote 163
-
Ferlatte O, Salway T, Samji H, et al. An Application of Syndemic Theory to Identify Drivers of the Syphilis Epidemic Among Gay, Bisexual, and Other Men Who Have Sex With Men. Sex Transm Dis. 2018;45(3):163-168.
- Footnote 164
-
Centers for Disease Control and Prevention. 2015 Sexually Transmitted Diseases Treatment Guidelines, Sexual Assault and Abuse and STDs. https://www.cdc.gov/std/tg2015/sexual-assault.htm. Updated 2015-2019.
- Footnote 165
-
Public Health Agency of Canada. Canadian Guidelines on Sexually Transmitted Infections-Supplementary statement for the management and follow-up of sexual abuse in peripubertal and prepubertal children. 2014. https://www.canada.ca/en/public-health/services/infectious-diseases/sexual-health-sexually-transmitted-infections/canadian-guidelines/sexually-transmitted-infections/canadian-guidelines-sexually-transmitted-infections-15.html.
- Footnote 166
-
Public Health Agency of Canada. Healthy Behaviour in School-aged Children in Canada: Focus on Relationships. 2015. https://healthycanadians.gc.ca/publications/science-research-sciences-recherches/health-behaviour-children-canada-2015-comportements-sante-jeunes/index-eng.php#c14a3.
- Footnote 167
-
Burchell AN, Allen VG, Gardner SL, et al. High incidence of diagnosis with syphilis co-infection among men who have sex with men in an HIV cohort in Ontario, Canada. BMC Infect Dis. 2015;15:356-015-1098-2.
- Footnote 168
-
Lang R., Read R., Krentz H., Gill J. Incident syphilis infections in an HIV population: Presentation and care. Open Forum Infect Dis. 2017;4:S667.
- Footnote 169
-
Ling D.I., Janjua N.Z., Wong S., et al. Sexually transmitted infection trends among gay or bisexual men from a clinic-based sentinel surveillance system in British Columbia, Canada. Sex Transm Dis. 2015;42(3):153-159.
- Footnote 170
-
Statistics Canada. Census Profile, 2016 Census. https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/prof/details/page_Download-Telecharger.cfm?Lang=E&Tab=1&Geo1=HR&Code1=2417&Geo2=PR&Code2=24&SearchText=Region%20du%20Nunavik&SearchType=Begins&SearchPR=01&B1=All&TABID=1&type=0. Updated 20192019.
- Footnote 171
-
Gratix J, Honish L, Mashinter L, et al. Case series descriptive analysis of a primary syphilis outbreak in Edmonton, Alberta, July 2004-April 2006. Can Commun Dis Rep. 2007;33(6):61-67.
- Footnote 172
-
Romanowski B, Sutherland R, Love EJ, Mooney D. Epidemiology of an outbreak of infectious syphilis in Alberta. Int J STD AIDS. 1991;2(6):424-427.
- Footnote 173
-
Lee CB, Brunham RC, Sherman E, Harding GK. Epidemiology of an outbreak of infectious syphilis in Manitoba. Am J Epidemiol. 1987;125(2):277-283.
- Footnote 174
-
Andermann A. Outbreaks in the age of syndemics: New insights for improving Indigenous health. Can Commun Dis Rep. 2017;43(6):125-132.
- Footnote 175
-
Pauktuutit Inuit Women of Canada. tavva: National Inuit Sexual Health Strategy. 2017. https://www.pauktuutit.ca/wp-content/uploads/Tavva_SexualHealth_English.pdf.
- Footnote 176
-
Reynolds DL, Evangelista F, Ward BM, Notenboom RH, Young ER, D'Cunha CO. Syphilis in an urban community. Can J Public Health. 1998;89(4):248-252.
- Footnote 177
-
Hogben M, Leichliter JS. Social determinants and sexually transmitted disease disparities. Sex Transm Dis. 2008;35(12 Suppl):S13-8.
- Footnote 178
-
Salway T, Gesink D, Lukac C, et al. Spatial-Temporal Epidemiology of the Syphilis Epidemic in Relation to Neighborhood-Level Structural Factors in British Columbia, 2005-2016. Sex Transm Dis. 2019;46(9):571-578.
- Footnote 179
-
Smock L, Caten E, Hsu K, DeMaria A. Economic Disparities and Syphilis Incidence in Massachusetts, 2001-2013. Public Health Rep. 2017;132(3):309-315.
- Footnote 180
-
Johnson L. Worst since 1948: Edmonton the epicentre of syphilis outbreak declared in Alberta. Edmonton Journal. July 16 2019 2019. Available from: https://edmontonjournal.com/news/local-news/infectious-syphilis-outbreak-declared-in-alberta.
- Footnote 181
-
DiOrio D, Kroeger K, Ross A. Social Vulnerability in Congenital Syphilis Case Mothers: Qualitative Assessment of Cases in Indiana, 2014 to 2016. Sex Transm Dis. 2018;45(7):447-451.
- Footnote 182
-
Alberta Health. Interactive Health Data Application. http://www.ahw.gov.ab.ca/IHDA_Retrieval/selectSubCategoryParameters.do. Updated 20192019.
- Footnote 183
-
Leber A, MacPherson P, Lee BC. Epidemiology of infectious syphilis in Ottawa. Recurring themes revisited. Can J Public Health. 2008;99(5):401-405.
- Footnote 184
-
Northwestern Health Unit. Medical Alert - Syphilis Update. 2019. https://www.nwhu.on.ca/Audiences/Documents/Medical%20Alert%20-%20Syphilis%20Update%2003.12.19.pdf.
- Footnote 185
-
Morin V, Michaud S, Zoungrana H. Department of Public Health Update on Syphilis. Régie régionale de la Nunavik. 2019.
- Footnote 186
-
Dhont M. History of oral contraception. Eur J Contracept Reprod Health Care. 2010;15 Suppl 2:S12-8.
- Footnote 187
-
Raine T, Minnis AM, Padian NS. Determinants of contraceptive method among young women at risk for unintended pregnancy and sexually transmitted infections. Contraception. 2003;68(1):19-25.
- Footnote 188
-
European Centre for Disease Prevention and Control. EMIS-2017 - The European Men-Who-Have-Sex-With-Men Internet Survey. 2019. https://www.ecdc.europa.eu/en/publications-data/emis-2017-european-men-who-have-sex-men-internet-survey.
- Footnote 189
-
Brennan DJ, Lachowsky NJ, Georgievski G, et al. Online Outreach Services Among Men Who Use the Internet to Seek Sex With Other Men (MISM) in Ontario, Canada: An Online Survey. J Med Internet Res. 2015;17(12):e277.
- Footnote 190
-
Badal HJ, Stryker JE, DeLuca N, Purcell DW. Swipe Right: Dating Website and App Use Among Men Who Have Sex With Men. AIDS Behav. 2018;22(4):1265-1272.
- Footnote 191
-
Gesink D., Connell J., Kimura L. What do guys know about syphilis anyways? Sex Transm Infect. 2019;95:A317. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emexb&NEWS=N&AN=629060501.
- Footnote 192
-
Goedel WC, Duncan DT. Geosocial-Networking App Usage Patterns of Gay, Bisexual, and Other Men Who Have Sex With Men: Survey Among Users of Grindr, A Mobile Dating App. JMIR Public Health Surveill. 2015;1(1):e4.
- Footnote 193
-
Hirshfield S, Remien RH, Humberstone M, Walavalkar I, Chiasson MA. Substance use and high-risk sex among men who have sex with men: a national online study in the USA. AIDS Care. 2004;16(8):1036-1047.
- Footnote 194
-
Watchirs Smith L, Guy R, Degenhardt L, et al. Meeting Sexual Partners Through Internet Sites and Smartphone Apps in Australia: National Representative Study. J Med Internet Res. 2018;20(12):e10683.
- Footnote 195
-
Dickinson J, Tsakonas E, Conner Gorber S, et al. Recommendations on screening for cervical cancer. CMAJ. 2013;185(1):35-45.
- Footnote 196
-
Bogler T., Farber A., Stall N., et al. Missed connections: Unintended consequences of updated cervical cancer screening guidelines on screening rates for sexually transmitted infections. Can Fam Phys. 2015;61(10):e459-e466. http://www.cfp.ca/content/61/10/e459.full.pdf+html; http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emed16&NEWS=N&AN=606480168.
- Footnote 197
-
ICES. Guideline changes to frequency of Pap tests has led to less screening and diagnosis of chlamydia. https://www.ices.on.ca/Newsroom/News-Releases/2017/Guideline-changes-to-frequency-of-Pap-tests-has-led-to-less-screening-and-diagnosis-of-chlamydia. Updated 2017-2019.
- Footnote 198
-
Naimer MS, Kwong JC, Bhatia D, et al. The Effect of Changes in Cervical Cancer Screening Guidelines on Chlamydia Testing. Ann Fam Med. 2017;15(4):329-334.
- Footnote 199
-
Allen U.D., MacDonald N.E., Bridger N.A., et al. Sexually transmitted infections in adolescents: Maximizing opportunities for optimal care. Paediatr Child Health. 2014;19(8):429-433. http://www.cps.ca/pdfreactor/pdf.php?lang=en&paper=sexually-transmitted-infections; http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emed15&NEWS=N&AN=600240885.
- Footnote 200
-
Bolsewicz K, Vallely A, Debattista J, Whittaker A, Fitzgerald L. Factors impacting HIV testing: a review--perspectives from Australia, Canada, and the UK. AIDS Care. 2015;27(5):570-580.
- Footnote 201
-
Brookfield S, Dean J, Forrest C, Jones J, Fitzgerald L. Barriers to Accessing Sexual Health Services for Transgender and Male Sex Workers: A Systematic Qualitative Meta-summary. AIDS Behav. 2020;24(3):682-696.
- Footnote 202
-
Deblonde J, De Koker P, Hamers FF, Fontaine J, Luchters S, Temmerman M. Barriers to HIV testing in Europe: a systematic review. Eur J Public Health. 2010;20(4):422-432.
- Footnote 203
-
Kumar MM, Lim R, Langford C, Seabrook JA, Speechley KN, Lynch T. Sexual knowledge of Canadian adolescents after completion of high school sexual education requirements. Paediatr Child Health. 2013;18(2):74-80.
- Footnote 204
-
Sex Information and Education Council of Canada. 2019 Canadian Guidelines for Sexual Health Education. SIECCAN. 2019. http://sieccan.org/sexual-health-education/.
- Footnote 205
-
Council of Ministers of Education, Canada. Canadian Youth, Sexual Health and HIV/AIDS Study: Factors influencing knowledge, attitudes and behaviours. 2003. http://www.cmec.ca/Publications/Lists/Publications/Attachments/180/CYSHHAS_2002_EN.pdf.
- Footnote 206
-
Frappier JY, Kaufman M, Baltzer F, et al. Sex and sexual health: A survey of Canadian youth and mothers. Paediatr Child Health. 2008;13(1):25-30.
- Footnote 207
-
Díaz-Olavarrieta C, Wilson KS, García SG, et al. The co-occurrence of intimate partner violence and syphilis among pregnant women in Bolivia. J Womens Health (Larchmt). 2009;18(12):2077-2086.
- Footnote 208
-
Seth P, Raiford JL, Robinson LS, Wingood GM, Diclemente RJ. Intimate partner violence and other partner-related factors: correlates of sexually transmissible infections and risky sexual behaviours among young adult African American women. Sex Health. 2010;7(1):25-30.
- Footnote 209
-
Truth and Reconciliation Commission of Canada. Truth and Reconciliation Commission of Canada: Calls to Action. 2015. http://trc.ca/assets/pdf/Calls_to_Action_English2.pdf.
- Footnote 210
-
National Collaborating Centre for Infectious Diseases. Exploring the determinants of syphilis in Indigenous women in Winnipeg: Laverne Gervais. 2019. https://nccid.ca/webcast/how-public-health-can-best-support-indigenous-women-with-syphilis-laverne-gervais/?hilite=%27syphilis%27.
- Footnote 211
-
Robinson J, Sareen J, Cox BJ, Bolton JM. Role of self-medication in the development of comorbid anxiety and substance use disorders: a longitudinal investigation. Arch Gen Psychiatry. 2011;68(8):800-807.
- Footnote 212
-
Kidd SE, Grey JA, Torrone EA, Weinstock HS. Increased Methamphetamine, Injection Drug, and Heroin Use Among Women and Heterosexual Men with Primary and Secondary Syphilis - United States, 2013-2017. MMWR Morb Mortal Wkly Rep. 2019;68(6):144-148.
- Footnote 213
-
McCall H, Adams N, Mason D, Willis J. What is chemsex and why does it matter? BMJ. 2015;351:h5790.
- Footnote 214
-
Lambert G, Cox J, Messier-Peet M, Apelian H, Moodie EEM, Engage research team. Engage Montréal, Portrait of the sexual health of men who have sex with men in Greater Montréal, Cycle 2017-2018, Highlights. 2019. https://www.engage-men.ca/wp-content/uploads/2019/04/Engage_Highlights_ENG_Mars-2019.pdf.
- Footnote 215
-
Canadian Centre on Substance Use and Addiction. Canadian Drug Summary: Methamphetamine. 2018. https://www.ccsa.ca/sites/default/files/2019-04/CCSA-Canadian-Drug-Summary-Methamphetamine-2018-en.pdf.
- Footnote 216
-
Woods-Jaeger BA, Jaeger JA, Donenberg GR, Wilson HW. The Relationship between Substance Use and Sexual Health among African American Female Adolescents with a History of Seeking Mental Health Services. Womens Health Issues. 2013;23(6):e365-71.
- Footnote 217
-
Schumacher CM, Ellen J, Rompalo AM. Changes in demographics and risk behaviors of persons with early syphilis depending on epidemic phase. Sex Transm Dis. 2008;35(2):190-196.
- Footnote 218
-
Patrick DM, Rekart ML, Jolly A, et al. Heterosexual outbreak of infectious syphilis: epidemiological and ethnographic analysis and implications for control. Sex Transm Infect. 2002;78 Suppl 1:i164-9.
- Footnote 219
-
Singh AE, Romanowski B. The return of syphilis in Canada: A failed plan to eliminate this infection. JAMMI. 2019;4(4). https://jammi.utpjournals.press/doi/pdf/10.3138/jammi.2019-08-22.
- Footnote 220
-
Vescera Z. Sask. syphilis outbreak continues as doctors struggle to find patients. Saskatoon StarPhoenix. December 19 2019 2019. Available from: https://thestarphoenix.com/news/local-news/sask-syphilis-outbreak-continues-as-doctors-struggle-to-find-patients.
- Footnote 221
-
Gesink D., Wang S., Norwood T., Sullivan A., Al-Bargash D., Shahin R. Spatial epidemiology of the syphilis epidemic in Toronto, Canada. Sex Transm Dis. 2014;41(11):637-648. http://journals.lww.com/stdjournal; http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emed15&NEWS=N&AN=604585040.
- Footnote 222
-
Solomon MM, Mayer KH. Evolution of the syphilis epidemic among men who have sex with men. Sex Health. 2015;12(2):96-102.
- Footnote 223
-
Ko NY, Lee HC, Hung CC, et al. Effects of structural intervention on increasing condom availability and reducing risky sexual behaviours in gay bathhouse attendees. AIDS Care. 2009;21(12):1499-1507.
- Footnote 224
-
Government of Canada. National Action Plan to Combat Human Trafficking. 2012. https://www.publicsafety.gc.ca/cnt/rsrcs/pblctns/ntnl-ctn-pln-cmbt/index-en.aspx#toc-01.1.
- Footnote 225
-
World Health Organization, United Nations Population Fund, Joint United Nations Programme on HIV/AIDS, Global Network of Sex Work Projects, World Bank, United Nations Development Programme. Implementing Comprehensive HIV/STI Programmes with Sex Workers: Approaches from Collaborative Interventions. 2013:19. https://www.who.int/hiv/pub/sti/sex_worker_implementation/swit_chpt2.pdf.
- Footnote 226
-
Hamze H., Ryan V., Cumming E., et al. HIV seropositivity and early syphilis stage associated with ocular syphilis diagnosis: A case-control study in British Columbia, Canada, 2010-2018. Clin Infect Dis. 2019. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emexb&NEWS=N&AN=629103572.
- Footnote 227
-
Vadboncoeur J., Labbe A.-C., Fortin C., et al. Ocular syphilis: case series (2000-2015) from 2 tertiary care centres in Montreal, Canada. Can J Ophthalmol. 2019. http://www.sciencedirect.com/science/journal/00084182; http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emexb&NEWS=N&AN=2002483311.
- Footnote 228
-
Nguyen VK, Greenwald ZR, Trottier H, et al. Incidence of sexually transmitted infections before and after preexposure prophylaxis for HIV. AIDS. 2018;32(4):523-530.
- Footnote 229
-
Traeger MW, Cornelisse VJ, Asselin J, et al. Association of HIV Preexposure Prophylaxis With Incidence of Sexually Transmitted Infections Among Individuals at High Risk of HIV Infection. JAMA. 2019;321(14):1380-1390.
- Footnote 230
-
Traeger MW, Schroeder SE, Wright EJ, et al. Effects of Pre-exposure Prophylaxis for the Prevention of Human Immunodeficiency Virus Infection on Sexual Risk Behavior in Men Who Have Sex With Men: A Systematic Review and Meta-analysis. Clin Infect Dis. 2018;67(5):676-686.
- Footnote 231
-
Quaife M, MacGregor L, Ong JJ, et al. Risk compensation and STI incidence in PrEP programmes. Lancet HIV. 2020;7(4):e222-e223.
- Footnote 232
-
Holt M, Lea T, Mao L, et al. Community-level changes in condom use and uptake of HIV pre-exposure prophylaxis by gay and bisexual men in Melbourne and Sydney, Australia: results of repeated behavioural surveillance in 2013-17. Lancet HIV. 2018;5(8):e448-e456.
- Footnote 233
-
Montaño MA, Dombrowski JC, Dasgupta S, et al. Differences in sexually transmitted infection risk comparing preexposure prophylaxis users and propensity score matched historical controls in a clinic setting. AIDS. 2019;33(11):1773-1780.
- Footnote 234
-
Consolacion T., Mercado J., Mazo O., et al. Characteristics of chlamydia/gonorrhea infections associated with a subsequent syphilis diagnosis in British Columbia, Canada. Sex Transm Infect. 2019;95:A322. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emexb&NEWS=N&AN=629060881.
- Footnote 235
-
Delaunay C.L., Cox J., Klein M., Lambert G., Maheu-Giroux M. Trends in hepatitis C virus (HCV) seroprevalence and associated risk factors among men who have sex with men (MSM) in Montreal from 2005 to 2018: Results from three cross-sectional surveys. Canadian Liver J. 2019;2(2):29-30. https://canlivj.utpjournals.press/toc/canlivj/2/2; http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emexb&NEWS=N&AN=628673030.
- Footnote 236
-
British Columbia Centre for Disease Control. Interim guidline on syphilis screening in pregnancy. 2019. http://www.perinatalservicesbc.ca/Documents/Guidelines-Standards/Maternal/Guideline-syphilis-screening-in-pregnancy.pdf.
- Footnote 237
-
Alberta Health Services. Public Health Alert: Outbreak: Syphilis. 2019. https://www.albertahealthservices.ca/assets/info/hp/phys/if-hp-phys-moh-ez-syphilis-outbreak.pdf.
- Footnote 238
-
Nolt S. Personal Communication with the Public Health Agency of Canada. 2020.
- Footnote 239
-
Saskatoon StarPhoenix. Health authority declares HIV, syphilis outbreaks in west-central Saskatchewan. 2019. https://thestarphoenix.com/news/local-news/health-authority-declares-hiv-syphilis-outbreaks-in-west-central-saskatchewan/.
- Footnote 240
-
National Collaborating Centre for Infectious Diseases. Congenital syphilis webcast. 2019.
- Footnote 241
-
Pursaga J. Syphilis outbreak in Manitoba puts women and babies at risk. Winnipeg Sun. 25 February 2019 2019. Available from: https://winnipegsun.com/news/news-news/syphilis-outbreak-in-manitoba-puts-women-and-babies-at-risk.
- Footnote 242
-
Public Health Ontario. Monthy Infectious Diseases Surveillance Report: Diseases of Public Health Significance cases for January to August 2019. 2019. https://www.publichealthontario.ca/-/media/documents/surveillance-reports/infectious/surveillance-report-infectious-diseases-2019.pdf?la=en.
- Footnote 243
-
Public Health Ontario. Surveillance Report: Monthly Infectious Diseases Surveillance Report (February 2018). 2018. https://www.publichealthontario.ca/-/media/documents/surveillance-reports/infectious/surveillance-report-infectious-diseases-jan-dec-2017.pdf?la=en.
- Footnote 244
-
Northwestern Health Unit. About Us. https://www.nwhu.on.ca/AboutUs/Pages/AboutUs.aspx.
- Footnote 245
-
Eastern Health. Public Advisory: Eastern Health Reports Increase in Syphilis Cases. 2019. http://www.easternhealth.ca/newsReleaseArchive.aspx.
- Footnote 246
-
Plitt SS, Osman M, Sahni V, Lee BE, Charlton C, Simmonds K. Examination of a prenatal syphilis screening program, Alberta, Canada: 2010-2011. Can J Public Health. 2016;107(3):e285-e290.
- Footnote 247
-
Kuo M, Money DM, Alvarez M, et al. Test uptake and case detection of syphilis, HIV, and hepatitis C among women undergoing prenatal screening in British Columbia, 2007 to 2011. J Obstet Gynaecol Can. 2014;36(6):482-490.
- Footnote 248
-
Wong J, Arkell C, Durigon M, et al. Maternal syphilis in british columbia, Canada: 2010 to 2016. Sex Transm Infect. 2017;93.
- Footnote 249
-
Verghese VP, Hendson L, Singh A, Guenette T, Gratrix J, Robinson JL. Early Childhood Neurodevelopmental Outcomes in Infants Exposed to Infectious Syphilis In Utero. Pediatr Infect Dis J. 2018;37(6):576-579.
- Footnote 250
-
Public Health Agency of Canada. Key Health Inequalities in Canada: A National Portrait. 2018. https://www.canada.ca/content/dam/phac-aspc/documents/services/publications/science-research/key-health-inequalities-canada-national-portrait-executive-summary/key_health_inequalities_full_report-eng.pdf.
- Footnote 251
-
Public Health Agency of Canada. Addressing Stigma: Towards a More Inclusive Health System. PHAC. 2019. https://www.canada.ca/content/dam/phac-aspc/documents/corporate/publications/chief-public-health-officer-reports-state-public-health-canada/addressing-stigma-what-we-heard/stigma-eng.pdf.
- Footnote 252
-
Chu A, Read R, Scarrott R. An audit of management of prenatal syphilis serology in the STI Clinic, Calgary, AB, Canada. Sex Transm Infec. 2011;87.
- Footnote 253
-
Adeleye AO, Plitt SS, Douglas L, Charlton CL. Overview of a Provincial Prenatal Communicable Disease Screening Program: 2002-2016. J Obstet Gynaecol Can. 2019.
- Footnote 254
-
Hayeems RZ, Campitelli M, Ma X, Huang T, Walker M, Guttmann A. Rates of prenatal screening across health care regions in Ontario, Canada: a retrospective cohort study. CMAJ Open. 2015;3(2):E236-43.
- Footnote 255
-
Manitoba Health, Seniors and Active Living. RE: Congenital HIV and Congenital Syphilis in Manitoba!. 2019. https://www.gov.mb.ca/health/publichealth/cdc/docs/hcp/2019/060319.pdf.
- Footnote 256
-
Manitoba Health, Seniors and Active Living. Re: Updates to Syphilis Protocol. 2019. https://www.gov.mb.ca/health/publichealth/cdc/protocol/syphilis.pdf.
- Footnote 257
-
Australian Government Department of Health. Fourth National Sexually Transmissible Infections Strategy 2018-2022. 2018.
- Footnote 258
-
European Centre for Disease Prevention and Control. Annual Epidemiological Report for 2017: Congenital syphilis. 2019. https://ecdc.europa.eu/sites/portal/files/documents/AER_for_2017-congenital-syphilis.pdf.
- Footnote 259
-
European Centre for Disease Prevention and Control. Syphilis and congenital syphilis in Europe: A review of epidemiological trends (2007-2018) and options for response. 2019. https://ecdc.europa.eu/sites/portal/files/documents/Syphilis-and-congenital-syphilis-in-Europe.pdf.
- Footnote 260
-
Simms I, Tookey PA, Goh BT, et al. The incidence of congenital syphilis in the United Kingdom: February 2010 to January 2015. BJOG. 2017;124(1):72-77.
- Footnote 261
-
Public Health England. Addressing the increase in syphilis in England: PHE Action Plan. 2019. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/806076/Addressing_the_increase_in_syphilis_in_England_Action_Plan_June_2019.pdf.
- Footnote 262
-
Centers for Disease Control and Prevention. Syphilis. https://www.cdc.gov/std/stats17/Syphilis.htm. Updated 20182019.
- Footnote 263
-
Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2018. 2019. https://www.cdc.gov/std/stats18/toc.htm.
- Footnote 264
-
Centers for Disease Control and Prevention. Recommended Clinician Timeline for Screening Syphilis, HIV, HBV, HCV, Chlamydia, and Gonorrhea. https://www.cdc.gov/nchhstp/pregnancy/screening/clinician-timeline.html. Updated 20192019.
- Footnote 265
-
Medicaid and CHIP Payment and Access Commission. Access in Brief: Pregnant Women and Medicaid. 2018. https://www.macpac.gov/wp-content/uploads/2018/11/Pregnant-Women-and-Medicaid.pdf.
- Footnote 266
-
Kozhimannil KB, Abraham JM, Virnig BA. National trends in health insurance coverage of pregnant and reproductive-age women, 2000 to 2009. Womens Health Issues. 2012;22(2):e135-41.
- Footnote 267
-
Kaiser Family Foundation. Women's Health Insurance Coverage. https://www.kff.org/womens-health-policy/fact-sheet/womens-health-insurance-coverage-fact-sheet/. Updated 20182019.
- Footnote 268
-
Centers for Disease Control and Prevention. Syphilis Challenges. https://www.cdc.gov/nchhstp/pregnancy/challenges/syphilis.html. Updated 2019.
- Footnote 269
-
Fraser Health. Interim guidance on perinatal syphilis screening - June 2019. https://www.fraserhealth.ca/employees/medical-health-officer-updates/interim-guidance-on-perinatal-syphilis-screening--june-2019#.XZTMwlVKipq. Updated 20192019.
- Footnote 270
-
Nunavik Department of Public Health. Call for Vigilance: Syphilis. 2017;5(1). https://nrbhss.ca/sites/default/files/Info-Mado%20de%20la%20DSP%20Nunavik%20-%20vol.%205%2C%20no%201%20-%20Call%20for%20vigilance%20Syphillis.pdf.
- Footnote 271
-
Gilbert M, Salway T, Haag D, et al. Use of GetCheckedOnline, a Comprehensive Web-based Testing Service for Sexually Transmitted and Blood-Borne Infections. J Med Internet Res. 2017;19(3):e81.
- Footnote 272
-
Government of Nunavut. Nunavut Communicable Disease and Surveillance Manual. 2016. https://www.gov.nu.ca/sites/default/files/nu_communicable_diseases_manual_-_complete_2018-_april19.pdf.
- Footnote 273
-
U.S. Preventive Services Task Force. Draft Recommendation Statement: Syphilis Infection in Pregnant Women: Screening. https://www.uspreventiveservicestaskforce.org/Page/Document/draft-recommendation-statement/syphilis-infection-in-pregnancy-screening1. Updated 2018-2019.
- Footnote 274
-
Centers for Disease Control and Prevention. Personal Communication between Division of STD Prevention (Centers for Disease Control and Prevention) and PHAC. CDC. 2019.
- Footnote 275
-
Warren HP, Cramer R, Kidd S, Leichliter JS. State Requirements for Prenatal Syphilis Screening in the United States, 2016. Matern Child Health J. 2018;22(9):1227-1232.
- Footnote 276
-
Centers for Disease Control and Prevention. Table 28. Primary and Secondary Syphilis Among Women - Reported Cases and Rates of Reported Cases by State/Area and Region in Alphabetical Order, United States and Outlying Areas, 2013-2017. CDC. 2018. https://www.cdc.gov/std/stats17/tables/28.htm;.
- Footnote 277
-
European Centre for Disease Prevention and Control. Antenatal screening for HIV, hepatitis B, syphilis and rubella susceptibility in the EU/EEA. ECDC. 2016. https://www.ecdc.europa.eu/sites/default/files/media/en/publications/Publications/antenatal-screening-HIV-hepatitis-B-syphilis-rubella-EU.pdf.
- Footnote 278
-
Public Health Agency of Canada. Accelerating our Response: Government of Canada five-year action plan on sexually transmitted and blood-borne infections. 2019. https://www.canada.ca/en/public-health/services/reports-publications/accelerating-our-response-five-year-action-plan-sexually-transmitted-blood-borne-infections.html#a2-4.
- Footnote 279
-
Lee S., Poliquin V., Pymar H. CLINICAL ENCOUNTERS FOR PELVIC INFLAMMATORY DISEASE: MISSED OPPORTUNITIES TO SCREEN FOR SYPHILIS AND HIV? J Obstet Gynaecol Can. 2019;41(5):723. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emexb&NEWS=N&AN=2001738982.
- Footnote 280
-
National Collaborating Centre for Infectious Diseases. Exploring the determinants of syphilis in Indigenous women in Winnipeg: Marcia Anderson. 2019. https://nccid.ca/webcast/the-determinants-of-syphilis-transmission-in-indigenous-women-marcia-anderson/.
- Footnote 281
-
Rahman MM, Hoover A, Johnson C, Peterman TA. Preventing Congenital Syphilis-Opportunities Identified by Congenital Syphilis Case Review Boards. Sex Transm Dis. 2019;46(2):139-142.
- Footnote 282
-
Centers for Disease Control and Prevention. CDC Call to Action: Let's Work Together to Stem the Tide of Rising Syphilis in the United States. 2017. https://www.cdc.gov/std/syphilis/SyphilisCalltoActionApril2017.pdf.
- Footnote 283
-
Ministry of Health. National Syphilis Action Plan: An action plan to stop the syphilis epidemic in New Zealand. 2019. https://www.health.govt.nz/system/files/documents/publications/national_syphilis_action_plan_final.pdf.
- Footnote 284
-
Health Protection Surveillance Centre. Action Plan: Response to the National Increase in HIV and STIs in MSM. 2017. https://www.hpsc.ie/a-z/specificpopulations/menwhohavesexwithmenmsm/guidance/MSM%20outbreak%20response%20action%20plan_June_2017.pdf.
- Footnote 285
-
United Nations Educational, Scientific and Cultural Organization. International technical guidance on sexuality education: an evidence-informed approach. UNESCO. 2018. https://unesdoc.unesco.org/ark:/48223/pf0000260770.
- Footnote 286
-
Chin HB, Sipe TA, Elder R, et al. The effectiveness of group-based comprehensive risk-reduction and abstinence education interventions to prevent or reduce the risk of adolescent pregnancy, human immunodeficiency virus, and sexually transmitted infections: two systematic reviews for the Guide to Community Preventive Services. Am J Prev Med. 2012;42(3):272-294.
- Footnote 287
-
Sex Information and Education Council of Canada. Sexual Health Education in the Schools: Questions and Answers 3rd Edition. 2010. http://sieccan.org/wp-content/uploads/2018/05/SIECCAN_Q-A-Sexual-health-education-in-the-schools.pdf.
- Footnote 288
-
Centers for Disease Control and Prevention. Condom Distribution as a Structural-Level Intervention. CDC. 2015. https://www.cdc.gov/hiv/pdf/programresources/guidance/condoms/cdc-hiv-condom-distribution.pdf.
- Footnote 289
-
Nunavik Regional Board of Health and Social Services. Good Touch/Bad Touch Program. https://nrbhss.ca/en/departments/public-health/prevention-and-health-promotion/good-touch-bad-touch-program. Updated 20192019.
- Footnote 290
-
Mercure S, Savard N. Effectiveness of interventions for syphilis prevention and control in MSM: A summary of published research findings. NCCID. 2014. https://nccid.ca/publications/effectiveness-of-interventions-for-syphilis-prevention-and-control-in-msm/.
- Footnote 291
-
Friedman AL, Kachur RE, Noar SM, McFarlane M. Health Communication and Social Marketing Campaigns for Sexually Transmitted Disease Prevention and Control: What Is the Evidence of their Effectiveness? Sex Transm Dis. 2016;43(2 Suppl 1):S83-101.
- Footnote 292
-
Public Health Agency of Canada. Section 2: Canadian Guidelines on Sexually Transmitted Infections - Primary care and sexually transmitted infections. 2013. https://www.canada.ca/en/public-health/services/infectious-diseases/sexual-health-sexually-transmitted-infections/canadian-guidelines/sexually-transmitted-infections/canadian-guidelines-sexually-transmitted-infections-17.html#a9.
- Footnote 293
-
Macdowall W, Parker R, Nanchahal K, et al. 'Talking of Sex': developing and piloting a sexual health communication tool for use in primary care. Patient Educ Couns. 2010;81(3):332-337.
- Footnote 294
-
National Coalition for Sexual Health. Sexual Health and Your Patients: Pocket Cards. https://nationalcoalitionforsexualhealth.org/tools/for-healthcare-providers/sexual-health-your-patients-pocket-cards.
- Footnote 295
-
Fuzzell L, Fedesco HN, Alexander SC, Fortenberry JD, Shields CG. "I just think that doctors need to ask more questions": Sexual minority and majority adolescents' experiences talking about sexuality with healthcare providers. Patient Educ Couns. 2016;99(9):1467-1472.
- Footnote 296
-
MacLean R. Resources to address stigma related to sexuality, substance use and sexually transmitted and blood-borne infections. Can Commun Dis Rep. 2018;44(2):62-67.
- Footnote 297
-
Canadian Public Health Association. Discussing Sexual Health, Substance Use and STBBIs: A Guide for Service Providers. 2017. https://www.cpha.ca/sites/default/files/uploads/resources/stbbi/discussionguide_e.pdf.
- Footnote 298
-
Public Health Agency of Canada. Questions & Answers: Inclusive Practice in the Prevention and of Sexually Transmitted and Blood Borne Infections among Ethnocultural Minorities. PHAC. 2014. http://sieccan.org/wp-content/uploads/2018/05/phac_STIs-blood-borne-infections_ethnocultural-minorities.pdf.
- Footnote 299
-
Dai T, Qu R, Liu J, Zhou P, Wang Q. Efficacy of Doxycycline in the Treatment of Syphilis. Antimicrob Agents Chemother. 2016;61(1):10.1128/AAC.01092-16. Print 2017 Jan.
- Footnote 300
-
Grennan JT. Tenofovir/Emtricitabine With Doxycycline for Combination HIV and Syphilis Pre-exposure Prophylaxis in HIV-negative MSM (DuDHS). BCCID. 2019.
- Footnote 301
-
Fusca L., Hull M., Ross P., et al. High interest in syphilis pre-and post-exposure prophylaxis among gay, bisexual and other msm in vancouver and toronto. Sex Transm Infect. 2019;95:A200. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emexb&NEWS=N&AN=629060786.
- Footnote 302
-
Connell J. The DuDHS Trial: PrEP for syphilis and HIV. 2018. https://smartsexresource.com/health-providers/blog/201806/dudhs-trial-prep-syphilis-and-hiv.
- Footnote 303
-
Bolan RK, Beymer MR, Weiss RE, Flynn RP, Leibowitz AA, Klausner JD. Doxycycline Prophylaxis to Reduce Incident Syphilis among HIV-Infected Men who have Sex with Men who Continue to Engage in High Risk Sex: A Randomized, Controlled Pilot Study. Sex Transm Dis. 2015;42(2):98-103.
- Footnote 304
-
Stahlman S, Plant A, Javanbakht M, et al. Acceptable Interventions to Reduce Syphilis Transmission Among High-Risk Men Who Have Sex With Men in Los Angeles. Am J Public Health. 2015;105(3):e88-94.
- Footnote 305
-
Ashton S., Enuaraq S. Ikajurniq: an inuit cascade of care framework for sexually transmitted and blood borne infections. Sex Transm Infect. 2019;95:A261-A262. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emexb&NEWS=N&AN=629060907.
- Footnote 306
-
Dawson SG, Callander N, Roche C, Kingsland T, Desmond N. Integrated sexual healthcare: the development and review of one model of service delivery. Int J STD AIDS. 2000;11(7):428-434.
- Footnote 307
-
Gray D, Mercer CH, Graham A, French RS, Salisbury C. Under one roof? A population-based survey of patient use and preference for sexual health services. Primary Health Care Research & Development. 2009;10(3):223-235. Accessed 2019/10/02.
- Footnote 308
-
Center for Substance Abuse Treatment (US). Chapter 1. Trauma-Informed Care: A Sociocultural Perspective. In: Trauma-Informed Care in Behavioral Health Services. Rockville (MD); 2014. NBK207201 [bookaccession].
- Footnote 309
-
National Inquiry into Missing and Murdered Indigenous Women and Girls. Reclaiming Power and Place: The Final Report of the National Inquiry into Missing and Murdered Indigenous Women and Girls, Volume 1b. https://www.mmiwg-ffada.ca/wp-content/uploads/2019/06/Final_Report_Vol_1b.pdf.
- Footnote 310
-
Urquhart C, Jasiura F, TIP Project Team, TIP Advisory Committee. Trauma-Informed Practice Guide. BC Ministry of Health, Mental Health and Substance Use Branch. 2013. http://bccewh.bc.ca/wp-content/uploads/2012/05/2013_TIP-Guide.pdf.
- Footnote 311
-
Canadian Centre on Substance Use and Addiction. Trauma-informed Care (The Essentials of...Series). 2014. https://www.ccsa.ca/trauma-informed-care-essentials-series.
- Footnote 312
-
National Collaborating Centre for Infectious Diseases. Forward Thinking on Syphilis: An Information Exchange on Innovative Approaches to Syphilis, Focused on MSM. 2014. https://nccid.ca/publications/forward-thinking-on-syphilis/.
- Footnote 313
-
Haidari, G., Youssef, E., Tooke, B., Boyt, T., Smith, G., Bannister, A., Haughton, D., & Richardson, D. Modernising services: a new strategy to increase uptake of sexual health services in high-risk men who have sex with men. HIV Medicine. 2014;15:30. https://www.researchgate.net/publication/293364144_Modernising_services_a_new_strategy_to_increase_uptake_of_sexual_health_services_in_high-risk_men_who_have_sex_with_men.
- Footnote 314
-
Lithgow KV, Cameron CE. Vaccine development for syphilis. Expert Rev Vaccines. 2017;16(1):37-44.
- Footnote 315
-
Plotnikoff K., Ogilvie G., Smith L., et al. Interested? Why or why not? STI clinic client perceptions of bacterial STI vaccines in British Columbia, Canada. Sex Transm Infect. 2019;95:A73. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emexb&NEWS=N&AN=628984618.
- Footnote 316
-
Cameron CE, PhD. Syphilis Vaccine Development: Requirements, Challenges, and Opportunities. Sex Transm Dis. 2018;45:S17. https://search.proquest.com/docview/2125723572?accountid=27430.
- Footnote 317
-
Salazar JC. GLOBAL SEQUENCE AND SURFACE ANTIGENIC DIVERSITY OF TREPONEMA PALLIDUM OUTER MEMBRANE PROTEINS. National Institues of Health. https://projectreporter.nih.gov/project_info_description.cfm?aid=9729229&icde=47542247.
- Footnote 318
-
Workowski KA, Berman SM. Centers for Disease Control and Prevention Sexually Transmitted Disease Treatment Guidelines. Clin Infect Dis. 2011;53 Suppl 3:S59-63.
- Footnote 319
-
Chow EPF, Callander D, Fairley CK, et al. Increased Syphilis Testing of Men Who Have Sex With Men: Greater Detection of Asymptomatic Early Syphilis and Relative Reduction in Secondary Syphilis. Clin Infect Dis. 2017;65(3):389-395.
- Footnote 320
-
US Preventive Services Task Force, Curry SJ, Krist AH, et al. Screening for Syphilis Infection in Pregnant Women: US Preventive Services Task Force Reaffirmation Recommendation Statement. JAMA. 2018;320(9):911-917.
- Footnote 321
-
Morshed MG, Singh AE. Recent trends in the serologic diagnosis of syphilis. Clin Vaccine Immunol. 2015;22(2):137-147.
- Footnote 322
-
Ross C, Shaw S, Marshall S, et al. Impact of a social media campaign targeting men who have sex with men during an outbreak of syphilis in Winnipeg, Canada. Can Commun Dis Rep. 2016;42(2):45-49. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=prem1&NEWS=N&AN=29770003.
- Footnote 323
-
Ryan V., Cumming E., Haag D., et al. An evaluation of the provincial 'syphistory' campaign in British Columbia, Canada. Sex Transm Infect. 2019;95:A325-A326. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emexb&NEWS=N&AN=629061117.
- Footnote 324
-
Chow EP, Dutt K, Fehler G, et al. Duration of syphilis symptoms at presentations in men who have sex with men in Australia: are current public health campaigns effective? Epidemiol Infect. 2016;144(1):113-122.
- Footnote 325
-
Darrow WW, Biersteker S. Short-term impact evaluation of a social marketing campaign to prevent syphilis among men who have sex with men. Am J Public Health. 2008;98(2):337-343.
- Footnote 326
-
Burchell AN, Lisk R, Yeung A, et al. Community-Directed Bacterial Sexually Transmitted Infection Testing Interventions Among Men Who Have Sex With Men: Protocol for an E-Delphi Study in Toronto, Canada. JMIR Res Protoc. 2019;8(7):e13801. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=prem&NEWS=N&AN=31274111.
- Footnote 327
-
Neufeld J. Plains Speak on STBBIs, 2019: An emergent challenge for the prairies. NCCID. 2019. https://nccid.ca/wp-content/uploads/sites/2/2019/06/Final_Plains-Speak-on-STBBIs-2019-Meeting-Proceedings.pdf.
- Footnote 328
-
Ryder N, Bourne C, Rohrsheim R. Clinical audit: adherence to sexually transmitted infection screening guidelines for men who have sex with men. Int J STD AIDS. 2005;16(6):446-449.
- Footnote 329
-
STIs in Gay Men Action Group. Australian Sexually Transmitted Infection & HIV Testing Guidelines 2014. 2014. https://stipu.nsw.gov.au/wp-content/uploads/STIGMA_Testing_Guidelines_Final_v5-2.pdf.
- Footnote 330
-
Bissessor M, Fairley CK, Leslie D, Howley K, Chen MY. Frequent screening for syphilis as part of HIV monitoring increases the detection of early asymptomatic syphilis among HIV-positive homosexual men. J Acquir Immune Defic Syndr. 2010;55(2):211-216.
- Footnote 331
-
Cheeks MA, Fransua M, Stringer HG,Jr, Silva S, Relf M. A Quality Improvement Project to Increase Early Detection of Syphilis Infection or Re-infection in HIV-infected Men Who Have Sex With Men. J Assoc Nurses AIDS Care. 2016;27(2):143-152.
- Footnote 332
-
Cohen S, Vittinghoff E, Philip SS, et al. Quarterly STI Screening Optimizes STI Detection Among PrEP Users in the Demo Project. CROI. http://www.croiconference.org/sessions/quarterly-sti-screening-optimizes-sti-detection-among-prep-users-demo-project-0.
- Footnote 333
-
Tuite A.R., Shaw S., Reimer J.N., Ross C.P., Fisman D.N., Mishra S. Can enhanced screening of men with a history of prior syphilis infection stem the epidemic in men who have sex with men? A mathematical modelling study. Sex Transm Infect. 2018;94(2):105-110. http://sti.bmj.com/; http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emexb&NEWS=N&AN=621051867.
- Footnote 334
-
Callander D, Baker D, Chen M, Guy R. Including syphilis testing as part of standard HIV management checks and improved syphilis screening in primary care. Sex Transm Dis. 2013;40(4):338-340.
- Footnote 335
-
Arumainayagam J, Pallan MJ, Buckley E, et al. Syphilis outbreak in Walsall, UK: lessons for control and prevention. Int J STD AIDS. 2007;18(1):55-57.
- Footnote 336
-
Debattista J, Dwyer J, Anderson R, Rowling D, Patten J, Mortlock M. Screening for syphilis among men who have sex with men in various clinical settings. Sex Transm Infect. 2004;80(6):505-508.
- Footnote 337
-
AIDS Committee of Toronto (ACT). Give HIV the Finger During Pride! https://www.actoronto.org/events-news/calendar-of-events/event-details?eventID=249. Updated 2016-2019.
- Footnote 338
-
Nine Circles Community Health Centre. Nine Circles at Pride 2019. https://ninecircles.ca/news-events/nine-circles-at-pride-2019/. Updated 20192019.
- Footnote 339
-
Lampejo T, Turner R, Roberts C, et al. Novel outreach settings to enhance sexually transmitted infection/HIV awareness, diagnosis and treatment in hard-to-reach populations. Int J STD AIDS. 2018;29(3):266-272.
- Footnote 340
-
Read PJ, Knight V, Bourne C, et al. Community event-based outreach screening for syphilis and other sexually transmissible infections among gay men in Sydney, Australia. Sex Health. 2013;10(4):357-362.
- Footnote 341
-
Canadian Institute for Health Information. In Pursuit of Health Equity: Defining Stratifiers for Measuring Health Inequality A Focus on Age, Sex, Gender, Income, Education and Geographic Location. CIHI. 2018. https://www.cihi.ca/sites/default/files/document/defining-stratifiers-measuring-health-inequalities-2018-en-web.pdf.
- Footnote 342
-
Manteuffel J, Markowitz N, Ham DC, et al. 388 Implementation of an Emergency Department Syphilis and HIV Point-of-Care Screening Process During an Outbreak of Syphilis in Detroit, MI in Collaboration With the Infectious Disease Department and the Centers for Disease Control and Prevention. Ann Emerg Med. 2016;68(4):S148.
- Footnote 343
-
Gratrix J, Smyczek P, Bertholet L, et al. A cross-sectional evaluation of opt-in testing for sexually transmitted and blood-borne infections in three Canadian provincial correctional facilities: a missed opportunity for public health? Int J Prison Health. 2019;15(3):273-281. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=prem&NEWS=N&AN=31329036.
- Footnote 344
-
2SMS LLC. 2sms.com. http://www.2sms.com/. Updated 20192019.
- Footnote 345
-
Ronen K, Golden MR, Dombrowski JC, Kerani RP, Bell TR, Katz DA. Uptake and Impact of Short Message Service Reminders via STI Partner Services on HIV/STI Testing Frequency among Men Who Have Sex with Men. Sex Transm Dis. 2019.
- Footnote 346
-
Burton J, Brook G, McSorley J, Murphy S. The utility of short message service (SMS) texts to remind patients at higher risk of STIs and HIV to reattend for testing: a controlled before and after study. Sex Transm Infect. 2014;90(1):11-13.
- Footnote 347
-
Bourne C, Knight V, Guy R, Wand H, Lu H, McNulty A. Short message service reminder intervention doubles sexually transmitted infection/HIV re-testing rates among men who have sex with men. Sex Transm Infect. 2011;87(3):229-231.
- Footnote 348
-
Bissessor M, Fairley CK, Leslie D, Chen MY. Use of a computer alert increases detection of early, asymptomatic syphilis among higher-risk men who have sex with men. Clin Infect Dis. 2011;53(1):57-58.
- Footnote 349
-
Gratrix J, Bergman J, Brandley J, Parker P, Smyczek P, Singh AE. Impact of Introducing Triage Criteria for Express Testing at a Canadian Sexually Transmitted Infection Clinic. Sex Transm Dis. 2015;42(11):660-3. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med11&NEWS=N&AN=26457490.
- Footnote 350
-
Get Checked Online. Giving Samples. https://getcheckedonline.com/Pages/GivingSamples.aspx. Updated 2016-2019.
- Footnote 351
-
British Columbia Centre for Disease Control. GetCheckedOnline in British Columbia: Expansion Outcomes (March 2016-August 2017). BCCDC. http://www.bccdc.ca/resource-gallery/Documents/Educational%20Materials/STI/Expansion_Fact%20Sheet_PROV_v3.pdf.
- Footnote 352
-
Gilbert M, Salway T, Haag D, et al. A cohort study comparing rate of repeat testing for sexually transmitted and blood-borne infections between clients of an internet-based testing programme and of sexually transmitted infection clinics in Vancouver, Canada. Sex Transm Infect. 2019;95(7):540-546. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=prem&NEWS=N&AN=31467134.
- Footnote 353
-
Wilson E, Free C, Morris TP, et al. Internet-accessed sexually transmitted infection (e-STI) testing and results service: A randomised, single-blind, controlled trial. PLoS Med. 2017;14(12):e1002479.
- Footnote 354
-
Hottes T.S., Farrell J., Bondyra M., Haag D., Shoveller J., Gilbert M. Internet-based HIV and sexually transmitted infection testing in British Columbia, Canada: opinions and expectations of prospective clients. J Med Internet Res. 2012;14(2):e41. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emed13&NEWS=N&AN=365014756.
- Footnote 355
-
Niruban J., Meyer G., Parker P., Gratrix J., Smyczek P. Incentive testing and treatment for STBBI in hard to reach populations in Edmonton, Alberta, Canada. Sex Transm Infect. 2019;95:A171. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emexb&NEWS=N&AN=629060044.
- Footnote 356
-
Singh AE, Chernesky MA, Morshed M, Wong T. Canadian Public Health Laboratory Network laboratory guidelines for the use of point-of-care tests for the diagnosis of syphilis in Canada. Can j infect dis med microbiol. 2015;26 Suppl A:29A-32A. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=prem1&NEWS=N&AN=25798163.
- Footnote 357
-
Pai N.P., Dhurat R., Potter M., et al. Will a quadruple multiplexed point-of-care screening strategy for HIV-related co-infections be feasible and impact detection of new co-infections in at-risk populations? Results from cross-sectional studies. BMJ Open. 2014;4(12):e005040. http://bmjopen.bmj.com/content/4/12/e005040.full.pdf+html; http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emed15&NEWS=N&AN=601130197.
- Footnote 358
-
Bergman J, Gratrix J, Plitt S, et al. Feasibility and Field Performance of a Simultaneous Syphilis and HIV Point-of-Care Test Based Screening Strategy in at Risk Populations in Edmonton, Canada. AIDS Res Treat. 2013;2013:819593. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=prem1&NEWS=N&AN=24527210.
- Footnote 359
-
Gliddon HD, Peeling RW, Kamb ML, Toskin I, Wi TE, Taylor MM. A systematic review and meta-analysis of studies evaluating the performance and operational characteristics of dual point-of-care tests for HIV and syphilis. Sex Transm Infect. 2017;93(S4):S3-S15.
- Footnote 360
-
Yansouni CP, Goldfarb DM, Maheu-Giroux M, et al. Stopping Syphilis Transmission in Arctic communities through Rapid Diagnostic Testing (STAR study). CIHR. http://webapps.cihr-irsc.gc.ca/decisions/p/project_details.html?applId=388947&lang=en.
- Footnote 361
-
Pai NP, Steben M. Commentary on POCT for HIV/STBBI : an analysis of contextual factors impeding implementation in Canada. NCCID. 2018. https://nccid.ca/publications/poct-for-hiv-stbbi-an-analysis-of-contextual-factors-impeding-implementation-in-canada/.
- Footnote 362
-
Smit PW, van der Vlis T, Mabey D, et al. The development and validation of dried blood spots for external quality assurance of syphilis serology. BMC Infect Dis. 2013;13:102.
- Footnote 363
-
CATIE, National Collaborating Centre for Infectious Diseases, REACH 2.0. Webinar Series 2017-2018 Reaching the Undiagnosed: Innovative Approaches for HIV, HCV, and other Sexually Transmitted Infection (STIs) Testing. https://www.catie.ca/sites/default/files/reaching-dbs-02212018.pdf.
- Footnote 364
-
Kim J. Hepatitis C & HIV Testing from Dried Blood Spots: Simplifying Testing to Broaden Community Based Testing. 2019;2019.
- Footnote 365
-
Spencer B. Health PEI offers first blood spot testing clinic for HIV and hepatitis C. CBC News. February 19, 2019 2019. Available from: https://www.cbc.ca/news/canada/prince-edward-island/pei-dry-blood-spot-testing-1.5024372.
- Footnote 366
-
van Loo IHM, Dukers-Muijrers NHTM, Heuts R, van der Sande MAB, Hoebe CJPA. Screening for HIV, hepatitis B and syphilis on dried blood spots: A promising method to better reach hidden high-risk populations with self-collected sampling. PLoS One. 2017;12(10):e0186722.
- Footnote 367
-
Lukac C.D., Consolacion T., Brownrigg B., et al. Enhanced surveillance of infectious syphilis and the cascade-of-care among HIV-positive and HIV-negative men who have sex with men in British Columbia, Canada. Sex Transm Infect. 2017;93:A145. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emexb&NEWS=N&AN=624997938.
- Footnote 368
-
Indigenous Services Canada. Personal Communication with the Public Health Agency of Canada's Center for Communicable Diseases and Infection Control. 2020.
- Footnote 369
-
Campbell A. Public Health Partner Notification (PN): Review of Current Practices, Options, and Considerations, for Evaluating PN Approaches. 2018. http://www.bccdc.ca/resource-gallery/Documents/Guidelines%20and%20Forms/Guidelines%20and%20Manuals/STI/PH%20PN%20REPORT%202018.pdf.
- Footnote 370
-
MacDonald PD, Nelson AL, Hightow-Weidman L, Leone PA. Disease intervention specialists as a resource in a public health emergency. Biosecur Bioterror. 2007;5(3):239-248.
- Footnote 371
-
Taylor D. Outcomes Related to STI Partner Notification. NCCID. 2013. https://nccid.ca/wp-content/uploads/sites/2/2015/03/NCCID_PartnerNotify_Taylor_04.pdf.
- Footnote 372
-
National Collaborating Centre for Infectious Diseases. Partner Notification for Sexually-transmitted Infections: Policy Options. NCCID. 2014. https://nccid.ca/publications/partner-noti%ef%ac%81cation-for-sexually-transmitted-infections-policy-options/?hilite=%27syphilis%27.
- Footnote 373
-
Brewer DD. Case-finding effectiveness of partner notification and cluster investigation for sexually transmitted diseases/HIV. Sex Transm Dis. 2005;32(2):78-83.
- Footnote 374
-
Lukac C., Consolacion T., Ryan V., et al. Evaluation of the provincial infectious syphilis partner notification program in British Columbia, Canada. Sex Transm Infect. 2019;95:A318. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emexb&NEWS=N&AN=629060565.
- Footnote 375
-
Saskatoon Health Region. Investigation of an HIV Cluster Among Injection Drug Users (IDUs) in Saskatoon, Saskatchewan. 2006.
- Footnote 376
-
Ogilvie G, Knowles L, Wong E, et al. Incorporating a social networking approach to enhance contact tracing in a heterosexual outbreak of syphilis. Sex Transm Infect. 2005;81(2):124-127.
- Footnote 377
-
Centers for Disease Control and Prevention. Cluster Interview Template Instructions. 2013. https://www.cdc.gov/std/Program/forms/CIT/CITInstructions.pdf.
- Footnote 378
-
Centers for Disease Control and Prevention. Recommendations for Partner Services Programs for HIV Infection, Syphilis, Gonorrhea, and Chlamydial Infection. CDC. 2008. https://www.cdc.gov/mmwr/preview/mmwrhtml/rr5709a1.htm.
- Footnote 379
-
Public Health Ontario. Case and Contact Management for STIs: Internet-Based Contact Tracing. PHO. 2019. https://www.publichealthontario.ca/-/media/documents/eb-internet-contact-tracing.pdf?la=en.
- Footnote 380
-
Ehlman DC, Jackson M, Saenz G, et al. Evaluation of an innovative internet-based partner notification program for early syphilis case management, Washington, DC, January 2007-June 2008. Sex Transm Dis. 2010;37(8):478-485.
- Footnote 381
-
Pennise M, Inscho R, Herpin K, et al. Using smartphone apps in STD interviews to find sexual partners. Public Health Rep. 2015;130(3):245-252.
- Footnote 382
-
Hunter P, Oyervides O, Grande KM, et al. Facebook-augmented partner notification in a cluster of syphilis cases in Milwaukee. Public Health Rep. 2014;129 Suppl 1:43-49.
- Footnote 383
-
McFarlane M, Kachur R, Klausner JD, Roland E, Cohen M. Internet-based health promotion and disease control in the 8 cities: successes, barriers, and future plans. Sex Transm Dis. 2005;32(10 Suppl):S60-4.
- Footnote 384
-
Hightow-Weidman L, Beagle S, Pike E, et al. "No one's at home and they won't pick up the phone": using the Internet and text messaging to enhance partner services in North Carolina. Sex Transm Dis. 2014;41(2):143-148.
- Footnote 385
-
Udeagu CC, Bocour A, Shah S, Ramos Y, Gutierrez R, Shepard CW. Bringing HIV partner services into the age of social media and mobile connectivity. Sex Transm Dis. 2014;41(10):631-636.
- Footnote 386
-
Klausner JD, Wolf W, Fischer-Ponce L, Zolt I, Katz MH. Tracing a syphilis outbreak through cyberspace. JAMA. 2000;284(4):447-449.
- Footnote 387
-
Bolding G, Davis M, Sherr L, Hart G, Elford J. Use of gay Internet sites and views about online health promotion among men who have sex with men. AIDS Care. 2004;16(8):993-1001.
- Footnote 388
-
Health Initiative for Men. What's Your Number? Tell Your Partners. http://checkhimout.ca/testing/tell-your-partners/2019.
- Footnote 389
-
Guy RJ, Micallef JM, Mooney-Somers J, et al. Evaluation of Chlamydia Partner Notification Practices and Use of the "Let Them Know" Website by Family Planning Clinicians in Australia: Cross-Sectional Study. J Med Internet Res. 2016;18(6):e173.
- Footnote 390
-
Gotz HM, van Rooijen MS, Vriens P, et al. Initial evaluation of use of an online partner notification tool for STI, called 'suggest a test': a cross sectional pilot study. Sex Transm Infect. 2014;90(3):195-200.
- Footnote 391
-
Bilardi JE, Fairley CK, Hopkins CA, et al. Experiences and outcomes of partner notification among men and women recently diagnosed with Chlamydia and their views on innovative resources aimed at improving notification rates. Sex Transm Dis. 2010;37(4):253-258.
- Footnote 392
-
Hochberg CH, Berringer K, Schneider JA. Next-Generation Methods for HIV Partner Services: A Systematic Review. Sex Transm Dis. 2015;42(9):533-539.
- Footnote 393
-
Rietmeijer CA, Westergaard B, Mickiewicz TA, et al. Evaluation of an online partner notification program. Sex Transm Dis. 2011;38(5):359-364.
- Footnote 394
-
Bilello LA, Livingood WC, Lukens-Bull K, Smotherman C, Choe U. Texting Test Results Reduces the Time to Treatment for Sexually Transmitted Infections. J Public Health Manag Pract. 2019;25(2):165-170.
- Footnote 395
-
Grennan T, Gilbert M, Hull M. A new avenue to explore in STI prevention. BCMJ. 2017;59(9):480. https://www.bcmj.org/bccdc/new-avenue-explore-sti-prevention.
- Footnote 396
-
Molina JM, Charreau I, Chidiac C, et al. Post-exposure prophylaxis with doxycycline to prevent sexually transmitted infections in men who have sex with men: an open-label randomised substudy of the ANRS IPERGAY trial. Lancet Infect Dis. 2018;18(3):308-317.
- Footnote 397
-
Beale MA, Marks M, Sahi SK, et al. Genomic epidemiology of syphilis reveals independent emergence of macrolide resistance across multiple circulating lineages. Nat Commun. 2019;10(1):3255.
- Footnote 398
-
Stamm LV. Global challenge of antibiotic-resistant Treponema pallidum. Antimicrob Agents Chemother. 2010;54(2):583-589.
- Footnote 399
-
Martin IE, Tsang RS, Sutherland K, et al. Molecular characterization of syphilis in patients in Canada: azithromycin resistance and detection of Treponema pallidum DNA in whole-blood samples versus ulcerative swabs. J Clin Microbiol. 2009;47(6):1668-1673.
- Footnote 400
-
Agence de la santé et des services sociaux de Montréal. Surveillance de seconde génération du VIH auprès des communautés montréalaises originaires d'Afrique subsaharienne et des Caraïbes anglophones. 2014. https://www.inspq.qc.ca/sites/default/files/documents/itss/surveillance_2e_generation_vih_ssg-afcar.pdf.
- Footnote 401
-
Government of Canada. I-Track: Enhanced surveillance of HIV, hepatitis C, and associated risk behaviours among people who inject drugs in Canada - Phase 3 (2010-2012) Report. https://www.canada.ca/en/public-health/services/diseases/hiv-aids/surveillance-hiv-aids/itrack-enhanced-surveillance-hiv-hepatitis-associated-risk-behaviours-people-who-inject-drugs-canada-phase-3.html.
- Footnote 402
-
Public Health Agency of Canada. Summary of key findings from Y-Track Phase 6 (2009-2012). 2017. https://www.canada.ca/content/dam/phac-aspc/documents/services/publications/diseases-conditions/y-track-2002-2009/y-track-2009-2012-eng.pdf.
- Footnote 403
-
Public Health Agency of Canada. M-Track: Enhanced Surveillance of HIV, Sexually Transmitted and Blood-borne Infections, and Associated Risk Behaviours among Men Who Have Sex with Men in Canada. Phase 1 Report. 2011. http://publications.gc.ca/collections/collection_2012/aspc-phac/HP40-64-1-2011-eng.pdf.
- Footnote 404
-
Public Health Agency of Canada. Summary of Key Findings from the A-Track Pilot Survey (2011-2012). PHAC. 2014. http://publications.gc.ca/collections/collection_2014/aspc-phac/HP40-118-2014-eng.pdf.
- Footnote 405
-
Public Health Agency of Canada. HIV/AIDS Epi Update - Chapter 13: HIV/AIDS in Canada among people from countries where HIV is endemic. PHAC. 2012. https://www.catie.ca/sites/default/files/HIV-Aids_EpiUpdates_Chapter13_EN.pdf.
- Footnote 406
-
Winnipeg Regional Health Authority. Outbreak of Infectious Syphilis in the Winnipeg Health Region Final Report Summary- March 2004. WRHA. 2004. http://www.wrha.mb.ca/healthinfo/preventill/files/Syphilis_080604.pdf.
- Footnote 407
-
Institut national de santé publique du Québec. Analyse des cas déclarés d'infection génitale à chlamydia trachomatis, d'infection gonococcique et de syphilis au Québec par année civile 2001-2006. INSPQ. 2007. https://www.inspq.qc.ca/sites/default/files/publications/710-itss.pdf.
- Footnote 408
-
Institut national de santé publique du Québec. Vigie rehaussée de la syphilis. https://www.inspq.qc.ca/espace-itss/vigie-rehaussee-de-la-syphilis. Updated 2012-2019.
- Footnote 409
-
Kinniburgh B., Rank C., Jolly A.M., et al. Social network analysis of a syphilis outbreak in Toronto, Ontario. Am J Epidemiol. 2011;173:S106. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emed12&NEWS=N&AN=70699232.
- Footnote 410
-
Fur R., Henderson E.A., Read R.R., Godley J., Roy C., Bush K. The use of social network analysis to quantify the importance of sex partner meeting venues in an infectious syphilis outbreak in Alberta, Canada. Sex Transm Infect. 2011;87:A164-A165. http://sti.bmj.com/content/87/Suppl_1/A164.full.pdf+html?sid=733cb530-c23f-4fe9-be0c-0e567d109fb2; http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emed12&NEWS=N&AN=70728630.
- Footnote 411
-
Frosst G., Tremblay F.W., Allard D. Infectious syphilis in New Brunswick: Using data for action in a small Canadian province. Sex Transm Infect. 2011;87:A354. http://sti.bmj.com/content/87/Suppl_1/A354.2.full.pdf+html?sid=919978c1-bada-42ec-b29a-79a1d9b832a5; http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emed12&NEWS=N&AN=70729087.
- Footnote 412
-
National Collaborating Centre for Infectious Diseases. Behind the Curtain of Mathematical Modelling: Inside a collaborative modelling project on public health strategies for syphilis management. 2018.
- Footnote 413
-
Centers for Disease Control and Prevention. The National Plan to Eliminate Syphilis from the United States. 1999. https://www.cdc.gov/stopsyphilis/plan.pdf.
Appendix A: Clinical algorithm for syphilis staging and treatment
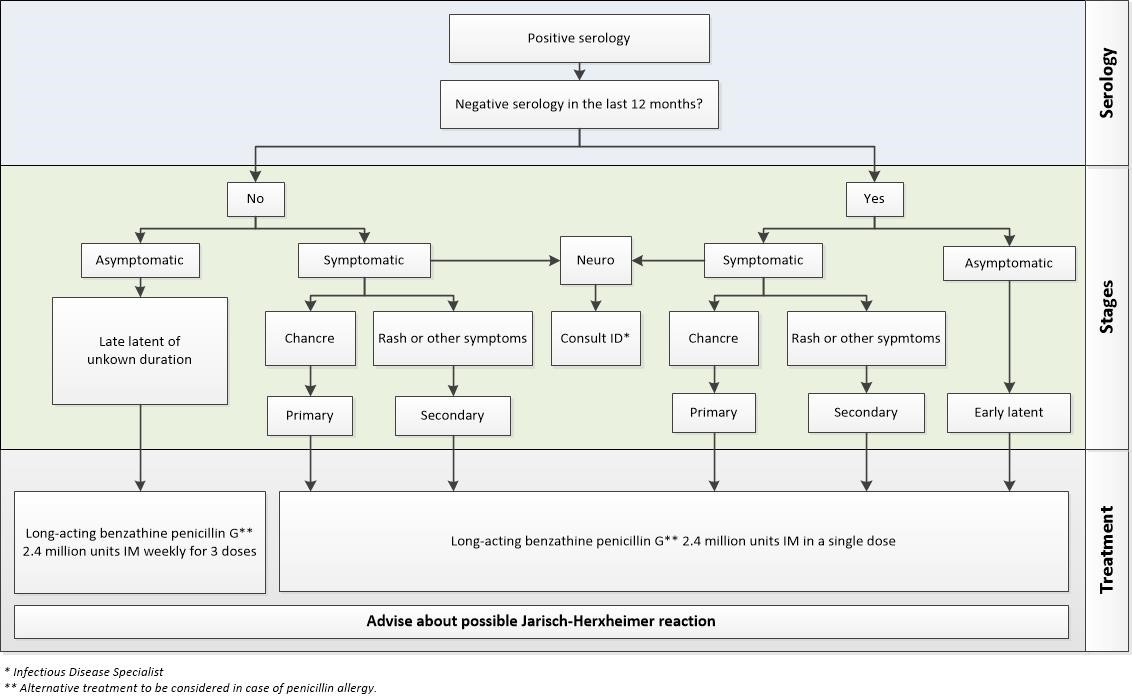
Clinical algorithm for syphilis staging and treatment - Text description
This decision tree displays the diagnostic pathway between syphilis serology, syphilis staging and the subsequent treatment.
The first row starts with Serology:
- Positive serology (No/Yes), move to serology in the past 12 months
- Negative serology in the last 12 months? Move to presence of symptoms
The second row involves determining the stage of syphilis based on symptom presentation:
- If Positive serology OR Negative serology in the last 12 months is NO
- Asymptomatic
- Late latent of unknown duration (move to treatment)
- Symptomatic
- Neuro
- consult IDFootnote *
- Rash or other symptoms
- Secondary (move to treatment)
- Chancre
- Primary (move to treatment)
- Neuro
- Asymptomatic
- If Positive serology OR Negative serology in the last 12 months is YES
- Asymptomatic
- Early latent (move to treatment)
- Symptomatic
- Neuro
- consult IDFootnote *
- Rash or other symptoms
- Secondary (move to treatment)
- Chancre
- Primary (move to treatment)
- Neuro
- Asymptomatic
The final row shows the treatment options based on the stage of syphilis:
- If the syphilis stage is determined to be Primary, Secondary or Early Latent
- Long-acting benzathine penicillin GFootnote ** 2.4 million units IM in a single dose
- If the syphilis stage is determined to be Late latent of unknown duration
- Long-acting benzathine penicillin GFootnote ** 2.4 million units IM weekly for 3 doses
- Advise about possible Jarisch-Herxheimer reaction
This staging diagram was kindly shared by Dr Troy Grennan, Clinical Lead, HIV/STI Program Medicine (Division of Infectious Diseases), University of British Columbia, BC Centre for Disease Control, British Columbia and by Dr. Todd F. Hatchette, Chief of Service, Division of Medical Microbiology, Department of Pathology and Laboratory Medicine, Capital District Health Authority, Nova Scotia
- Footnote *
-
Infectious Disease specialist
- Footnote **
-
Alternative treatment to be considered in case of penicillin allergy
Appendix B: Case definitions of syphilis used in Canada
B.I Federal case definitions
Source: Public Health Agency of Canada. Case Definitions for Communicable Diseases under National Surveillance. Canada Communicable Disease Report CCDR 2009, 35S2: 1 – 123.
Confirmed case—Early congenital syphilis (within two years of birth)
Laboratory confirmation of infection:
- Identification of T. pallidum by dark-field microscopy, fluorescent antibody or equivalent examination of material from nasal discharges, skin lesions, placenta, umbilical cord or autopsy material of a neonate (up to four weeks of age);
OR - reactive serology (non-treponemal and treponemal) from venous blood (not cord blood) in an infant/child with clinical, laboratory or radiographic evidence of congenital syphilis whose mother is without documented evidence of adequate treatment;
OR - detection of T. pallidum DNA in an appropriate clinical specimen.
Confirmed case—Primary syphilis
Laboratory confirmation of infection:
- Identification of T. pallidum by dark-field microscopy, fluorescent antibody, nucleic acid testing (NAT), or equivalent examination of material from a chancre or a regional lymph node;
OR - presence of one or more typical lesions (chancres) and reactive treponemal serology, regardless of non-treponemal test reactivity, in individuals with no previous history of syphilis;
OR - presence of one or more typical lesions (chancres) and a fourfold or greater increase in the titre over the last known non-treponemal test in individuals with a past history of syphilis treatment.
Confirmed case—Secondary syphilis
Laboratory evidence of infection:
- Identification of T. pallidum by dark-field microscopy, fluorescent antibody, NAT or equivalent examination of mucocutaneous lesions, condylomata lata and reactive serology (non-treponemal and treponemal);
OR - presence of typical signs or symptoms of secondary syphilis (e.g. mucocutaneous lesions, alopecia, loss of eyelashes and lateral third of eyebrows, iritis, generalized lymphadenopathy, fever, malaise or splenomegaly) AND either a reactive serology (non-treponemal and treponemal OR a fourfold or greater increase in titre over the previous known non-treponemal test.
Confirmed case—Early latent syphilis (< one year after infection)
Laboratory confirmation of infection:
- An asymptomatic patient with reactive serology (treponemal and/or non-treponemal) who, within the previous 12 months, had one of the following:
- non-reactive serology
- symptoms suggestive of primary or secondary syphilis
- exposure to a sexual partner with primary, secondary or early latent syphilis.
Confirmed case—Late latent syphilis (> one year after infection or of unknown duration)
Laboratory confirmation of infection:
- An asymptomatic patient with persistently reactive treponemal serology (regardless of non-treponemal serology reactivity) who does not meet the criteria for early latent disease and who has not been previously treated for syphilis.
Confirmed case—Neurosyphilis
Infectious (< one year after infection):
Laboratory confirmation of infection:
- Fits the criteria of primary, secondary OR early latent syphilis above AND one of the following:
- reactive CSF-VDRL in non-bloody CSF
- clinical evidence of neurosyphilis AND either elevated CSF leukocytes OR elevated CSF protein in the absence of other known causes.
Non-infectious (> one year after infection):
Laboratory confirmation of infection:
- Reactive treponemal serology (regardless of non-treponemal serology reactivity) AND one of the following:
- reactive CSF-VDRL in non-bloody CSF
- clinical evidence of neurosyphilis AND either elevated CSF leukocytes OR elevated CSF protein in the absence of other known causes.
Confirmed Case—Tertiary syphilis other than Neurosyphilis
Laboratory confirmation of infection:
- Reactive treponemal serology (regardless of non-treponemal test reactivity) together with characteristic late abnormalities of the cardiovascular system, bone, skin or other structures, in the absence of other known causes of these abnormalities (T. pallidum is rarely seen in these lesions although, when present, it is diagnostic);
- AND
- no clinical or laboratory evidence of neurosyphilis.
B.II Provincial and territorial case definitions for congenital syphilis
Differences between national and provincial/territorial congenital syphilis case definitions are described below. Currently, seven jurisdictions use the national case definition for early congenital syphilis or have similar definitions (Alberta, New Brunswick, Nova Scotia, Prince Edward Island, Newfoundland and Labrador, Northwest Territories and Nunavut). Five jurisdictions use a different case definition than the national early congenital syphilis case definition (British Columbia, Saskatchewan, Manitoba, Ontario and Quebec). British Columbia, Saskatchewan and Manitoba have the additional option of diagnosing according to non-treponemal test titre. However, these provinces do not use these tests in the same way. In British Columbia, a fourfold higher titre in the newborn than in the mother in combination with a confirmatory treponemal test and clinical evidence is sufficient to confirm a case. Whereas, Saskatchewan and Ontario do not take into consideration maternal status in their confirmed case definition. In Quebec, the case definition is similar to the national definition, but Quebec requires the addition of two serology tests with at least one treponemal test. At the time this report, case definitions for the Yukon were not available publicly or upon request.
Lastly, additional case definitions for early congenital syphilis are used in five provinces (British Columbia, Alberta, Saskatchewan, Manitoba and Quebec). These additional case definitions include a maternal syphilis definition, probable early congenital syphilis, clinically confirmed early congenital syphilis, syphilitic stillbirth, probable syphilitic stillbirth, and late congenital syphilis.
| Province/ Territory |
Comparison with national early congenital syphilis case definition | Additional case definitions |
|---|---|---|
| BCFootnote i | Differs | Maternal syphilis Late congenital syphilis |
| ABFootnote ii | √ | Probable early congenital syphilis Syphilitic stillbirth (confirmed, probable) |
| SKFootnote iii | Differs | Early congenital syphilis (laboratory confirmed, clinically confirmed, probable) Syphilitic stillbirth (confirmed, probable) |
| MBFootnote iv | Differs | Early congenital syphilis (laboratory confirmed, clinically confirmed, probable) Syphilitic stillbirth (confirmed, probable) |
| ONFootnote v | Differs | |
| QCFootnote vi | Differs | Probable early congenital syphilis |
| NB | √ | |
| NS | √ | |
| PE | √ | |
| NL | √ | |
| YT | NA | |
| NT | √ | |
| NU | √ | |
Note: A check mark (√) indicates a match with the national case definition. “NA” indicates that the information were not available publicly or upon request at the time this report was drafted.
|
||
B.III Other provincial and territorial syphilis case definitions
Differences between national and provincial/territorial syphilis case definitions are described below. Currently, four jurisdictions use the national case definitions for all stages of syphilis (Saskatchewan, New Brunswick, Prince Edward Island and Northwest Territories), two jurisdictions have case definitions that are similar to the national case definition for all stages of syphilis (Nova Scotia and Nunavut), and six jurisdictions have at least one case definition that differs from the national case definition (British Columbia, Alberta, Manitoba, Ontario, Quebec and Newfoundland and Labrador). At the time of this report, information on case definitions used in Yukon as well as case definitions for late latent, neurosyphilis and tertiary syphilis used in British Columbia, were not available either publicly or upon request. Saskatchewan has additional suspect case definitions for primary, secondary and early latent syphilis and British Columbia has additional case definitions for ocular syphilis and unspecified syphilis stage. Quebec is the only province who has a different case definition for every stage of syphilis, but this is mainly due to their definitions reflecting their testing algorithm, as they specify that two serological tests are required, with at least one being treponemal.
Secondary syphilis and neurosyphilis are the two stage case definitions with the most variability between the provinces and territories. Three provinces have differences in their confirmed secondary syphilis definitions. Contrary to the federal case definition, British Columbia and Quebec do not require serology testing in addition to direct testing (by microscopy or fluorescent antibody detection or NAT). In Alberta, detection of syphilis DNA by PCR (polymerase chain reaction) is sufficient on its own to confirm secondary syphilis. In the case of neurosyphilis, all provinces except Quebec and Newfoundland and Labrador distinguish between infectious neurosyphilis from non-infectious neurosyphilis. In provinces that do distinguish between these two forms of neurosyphilis, only Alberta and Manitoba have slight differences from the federal case definition.
Beyond the latter differences, minor differences can also be observed in relation to early latent syphilis and late latent syphilis definitions used across jurisdictions.
In the case of early latent syphilis, the national case definition requires treponemal or non-treponemal serology in asymptomatic patients. British Columbia and Quebec’s definitions differ slightly in that British Columbia requires both tests or a four-fold increase in titres, while Quebec requires two tests with at least one being a treponemal test. Further, in British Columbia’s case definition, in addition to criteria of (1) non-reactive serology or (2) the presence of symptoms or (3) reported history of being exposed to syphilis in the previous 12 months, an individual considered to be “at risk” or an individual presenting a titre higher than 1:16 can also fit the criteria of early latent syphilis. In Quebec, an individual meeting one of those first three criteria, or having had a previous episode of syphilis and having been treated, can fit the case definition for early latent syphilis.
Two provinces have differences in their definitions for late latent syphilis. The national case definition requires persistent treponemal serology, while Ontario and Quebec only require positive serology. Ontario requires treponemal or non-treponemal serology, while Quebec requires two tests with at least one being treponemal. For Ontario, the national definition’s requirement that the individual was not previously treated for syphilis is replaced by the requirement that the individual was not adequately treated for syphilis or has an increase in titre. For Quebec, the province specifies that the individual must not have been at risk for syphilis acquisition in the past 12 months.
| Province or Territory |
National case classification | ||||||
|---|---|---|---|---|---|---|---|
| Primary | Secondary | Early Latent | Late Latent | Neurosyphilis | Tertiary | ||
| Infectious | Non-infectious | ||||||
| BC | √ | DiffersFootnote i | DiffersFootnote i | NA | NA | NA | NA |
| AB | √ | DiffersFootnote ii | √ | √ | DiffersFootnote ii | √ | √ |
| SK | √ + suspectFootnote iii |
√ + suspectFootnote iii |
√ + suspectFootnote iii |
√ | √ | √ | √ |
| MB | √ | √ | √ | √ | DiffersFootnote iv | √ | √ |
| ON | √ | √ | √ | DiffersFootnote v | √ | √ | √ |
| QC | DiffersFootnote vi | DiffersFootnote vi | DiffersFootnote vi | DiffersFootnote vi | DiffersFootnote vi | DiffersFootnote vi | DiffersFootnote vi |
| NB | √ | √ | √ | √ | √ | √ | √ |
| NS | √ | √ | √ | √ | √ | √ | √ |
| PE | √ | √ | √ | √ | √ | √ | √ |
| NL | √ | √ | √ | √ | DiffersFootnote vii | DiffersFootnote vii | √ |
| YT | NA | NA | NA | NA | NA | NA | NA |
| NT | √ | √ | √ | √ | √ | √ | √ |
| NU | √ | √ | √ | √ | √ | √ | √ |
Note: A check mark (√) indicates a match with the national case definition. “NA” indicates that the information were not available publicly or upon request at the time this report was drafted. “Suspect” indicates the presence of a case definition for suspect cases. “Differs” indicates an instance in which the PT case definition differs from the national case definition.
|
|||||||
B.IV Provincial reporting to CNDSS from 2008 to 2017
| Provinces | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 |
|---|---|---|---|---|---|---|---|---|---|---|
| BCFootnote i | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| AB | √ | √ | √ | √ | √Footnote ii | √Footnote ii | √Footnote ii | √Footnote ii | √Footnote ii | √Footnote ii |
| SK | √ | √ | √ | √ | √Footnote iii | √ | √ | √ | √ | √ |
| MB | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| ONFootnote iv | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| QC | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| NBFootnote v | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| NS | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| PE | √Footnote vi | √Footnote vi | √Footnote vi | √Footnote vi | √Footnote vi | |||||
| NLFootnote vii | √ | √ | √ | √ | √ | √ | √ | √Footnote viii | √ | √ |
| YT | √Footnote ix | √Footnote x | ||||||||
| NT | √ | √ | √Footnote xi | √Footnote xii | √Footnote xi | √Footnote v | ||||
| NU | √ | √ | √ | √ | √ | √ | ||||
Note: A check mark (√) indicates that the PT reported syphilis data on that given year
|
||||||||||
| Provinces | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 |
|---|---|---|---|---|---|---|---|---|---|---|
| BC | ||||||||||
| AB | √ | √ | √ | √ | ||||||
| SK | √Footnote i | √Footnote ii | √Footnote ii | √Footnote ii | √ | √Footnote ii | √Footnote i | |||
| MB | √ | √Footnote iii | √Footnote iii | √Footnote iii | √Footnote iii | √ | √Footnote iii | |||
| ON | ||||||||||
| QC | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| NBFootnote iv | √ | √ | √ | √ | √ | √ | √ | √ | √ | |
| NS | √Footnote v | √Footnote v | √ | √ | √Footnote v | √Footnote v | √ | √ | √Footnote v | √ |
| PE | ||||||||||
| NL | √Footnote vi | Footnote vii | √ | √Footnote vii | √Footnote vii | √Footnote vii | √ | √ | √ | √ |
| YT | √Footnote viii | √Footnote viii | √Footnote viii | √ | √Footnote viii | √Footnote viii | √Footnote viii | √Footnote viii | ||
| NT | √ | √ | √Footnote ix | √Footnote ix | √Footnote ix | √Footnote ix | √Footnote ix | |||
| NU | √Footnote x | √Footnote x | √Footnote x | √Footnote x | √ | |||||
Note: A check mark (√) indicates that the PT reported syphilis data on that given year
|
||||||||||
Appendix C: Data and methods
C.I. Syphilis surveillance data
Data sources
Numerator data
Provincial and territorial health authorities provide non-nominal data on laboratory-confirmed cases to PHAC via CNDSS. Data from January 1, 1971 to December 31, 2017, were available from all provinces and territories as per their reporting history (Table 2) and were extracted from CNDSS in April and May 2019. Syphilis has been notifiable since 1924, while congenital syphilis became notifiable in 1993. Reported cases adhere to the national case definitions (see Appendix B – Case definitions). Variables submitted along with the diagnosis include stage of syphilis, sex, age at time of diagnosis, year of diagnosis and province/territory of diagnosis. CNDSS began to collect information on these variables at various times; stage of syphilis and province/territory has been reported since 1971, while age and sex has been reported since 1991. Preliminary syphilis surveillance data for 2018-2019, stratified by age and by sex were received directly from the provinces and territories. All data received were validated in collaboration with the corresponding province or territory.
Denominator data
Population estimates from Canada between 1979 and 2018 were extracted from Statistics Canada census (2018). The data includes the total Canadian population, as well as provincial population stratified by both age (0-100+) and sex (Male, Female, Both). As per the Statistics Canada data extraction, estimates are adjusted for under coverage and postcensal estimates are based on the 2016 census. Population estimates for the Northwest Territories and Nunavut were not separately provided prior to July 1991. To calculate rates of congenital syphilis, the number of live births, by place of residence of mother, was extracted from Statistics Canada data between 1993 and 2017 (Statistics Canada. Table 13-10-0414-01 Live births, by place of residence of mother DOI). The total for “Canada, place of residence of mother” was used, and the total for “Place of residence of mother outside Canada” was excluded. For data pertaining to live births within women of childbearing age only, data were extracted from Statistics Canada between 1993 and 2017 from the “Live births, by age of mother” table (Statistics Canada. Table 13-10-0416-01 Live births, by age of mother DOI).
| Province/Territory | Reporting history |
|---|---|
| British Columbia | Began to report on syphilis cases in 1939. Only reported on infectious cases from 1998 to 2016. |
| Alberta | Began to report on syphilis cases in 1931. Only reported on infectious cases since 2006. |
| Manitoba | Began to report on syphilis cases in 1938. |
| Saskatchewan | Began to report on syphilis cases in 1931. Only reported on infectious cases from 2005 to 2011 and in 2016. |
| Ontario | First reported in 1924 and then each year since 1927. Has only reported on infectious cases since 2005. |
| Quebec | Began to report on syphilis cases in 1944. |
| New Brunswick | Began to report on syphilis cases in 1931. |
| Nova Scotia | Began to report on syphilis cases in 1925. |
| Prince Edward Island | Began to report on syphilis cases in 1931. |
| Newfoundland and Labrador | Joined the confederation in 1949. Began to report on syphilis cases in 1949. |
| Nunavut | Established as a territory in 1999. Preliminary data reported as of 2015. |
| Northwest Territories | Began to report on syphilis cases in 1959. |
| Yukon | Began to report on syphilis cases in 1956. |
| Note: These details were obtained from: https://diseases.canada.ca/notifiable/charts?c=pd | |
Data analysis
Data analysis was performed using Microsoft Excel and RStudio version 3.6.0. All stages of syphilis are notifiable, but infectious stages (primary, secondary, and early latent) form the majority of content presented in this report. National annual rates of reported cases of infectious syphilis were computed using the number of cases from the CNDSS as numerators, and Statistics Canada July 2018 yearly population estimates as denominators. Age group, sex and province/territory-specific incidence rates were also calculated. For all years, incidence rates were given per 100,000 population. For congenital syphilis, rates were reported per 100,000 live births. Rates, percentages, and change in rates were calculated using unrounded numbers. No statistical procedures were used for comparative analyses.
Previous reports may present different rates for some years due to reporting delays, data being updated from provinces and territories, or improvements in data cleaning and validation.
Rates of infectious syphilis by age group and sex over time can be retrieved from the Notifiable Disease Online website.
Data source and analysis for OECD countries
Data for figures comparing rate values from OECD countries were obtained from the most recent reports from the following institutions: CDC (US), The Kirby Institute (Australia), ECDC (Europe) and Public Health England. Tables were generated using reported data for each country between the years of 2008 and 2017
International syphilis response environmental scan
International responses to syphilis were analyzed from the following organizations: Institute of Public Health in Ireland, Public Health England, CDC, Australian Government Department of Health, and the ECDC from August 12, 2019 to August 30, 2019. Searches were performed in their respective public health websites with the following key words: “syphilis” AND “intervention” OR “response” OR “evaluation” OR “campaign”. From the resulting selected resources, the following data items were extracted: location/setting, outcome to be modified, intervention, evaluation method, and results.
C.II Literature review
Research Strategy: A PHAC reference librarian used the Medline, Embase, ProQuest Public Health and Scopus databases to search for articles on the topic of syphilis in Canada published between January 2009 and December 2018. The search was completed on December 18, 2018. To ensure references were up to date for the purposes of this report, another search was conducted in September 2019.
Using the Boolean operator “OR”, the terms employed to capture articles pertaining to syphilis were: syphilis, neurosyphilis, Treponema pallidum, and Great Pox. Terms used to identify Canadian publications were: Canada, Canadian, Canadien, Ottawa, British Columbia, Colombie-Britannique, Vancouver, Alberta, Edmonton, Calgary, Saskatchewan, Regina, Saskatoon, Manitoba, Winnipeg, Ontario, Toronto, Quebec, Quebecois, Montreal, New Brunswick, Nouveau Brunswick, Fredericton, Nova Scotia, Nouvelle-Écosse, Halifax, Prince Edward Island, Île-du-Prince-Édouard, Charlottetown, Newfoundland, Terre-Neuve, Yukon, Whitehorse, Northwest Territories, Territoires du Nord-Ouest, Nunavut, Yellowknife, and Iqaluit. These two sets of terms were combined using the Boolean operator "AND". Additional publications were identified using a snowball-based approach, based on relevant publications’ reference lists.
Inclusion and exclusion criteria
Works were included in the literature review if they covered the topic of the epidemiology of syphilis in Canada, the risk factors associated with the rise of syphilis rates in Canada, or the public health efforts to reduce syphilis rates in Canada. Studies were included if they used data from 2009 to 2019. Scientific peer-reviewed articles, governmental reports, conference and article abstracts, and scientific posters were all included. No language restrictions were applied.
Works were excluded if they did not address the aforementioned topics of syphilis or if they were based outside of Canada. Furthermore, clinical case studies, research notes, and articles on sampling techniques, molecular characterization, and economic evaluations of public health interventions were excluded. When multiple publications by the same author explored a similar topic (e.g.,. repeat publications), only the most recent work was included. Finally, publications that were not available online or via the PHAC Health Library were excluded from the review.
Study selection and data extraction
To select relevant, non-duplicative works, one researcher reviewed the publication’s titles, and then subsequently reviewed the retained abstract summaries, followed by the retained full-text works. A second researcher independently reviewed a sample of the identified full-text works to validate the initial selection approach. Where divergence in opinions occurred between the two reviewers, consensus was reached between the first two reviewers and a third researcher.
From the final selection of works, two researchers extracted the following data items for narrative synthesis: title, author, year, setting, design, objectives, years of data collection, study population, sample size, syphilis stage, syphilis measure, co-infection measure, risk factors, type of analysis, primary results, challenges identified during the intervention, secondary results, and study limitations.
Additional searches were conducted in a targeted way in the international scientific evidence when Canadian studies were limited on specific themes.
C.III Outbreak data
National outbreak environmental scan
All resources included in the the outbreak environmental scan were published after January 1, 2005, were restricted to Canada, included the keywords “syphilis” and “outbreak,” and” were collected from February 2019 to September 2019. Publically available resources included media sources (Canadian Broadcasting Corporation News, Canadian Television Network, Maclean’s, Global News, The Western Star, etc.), provincial and municipal websites (Ontario Public Health, Government of Northwest Territories, Vancouver Coastal Health, etc.), alerts from the International Society for Infectious diseases (Pro-MED), peer-reviewed articles (PubMed, Google Scholar), and articles and podcasts from the National Collaborating Centre for Infectious Diseases (NCCID). Internal resources, including PowerPoint slide decks from the NCCID Knowledge Exchange Forum on Syphilis, were also incorporated if they matched the inclusion criteria. Overall, over 100 resources were found which met the stated criteria.
From the selected resources, the following data items were extracted: location, date of outbreak, number of cases, proportion of infectious cases, profile of cases, detailed description of the outbreak, outbreak evolution, female to male ratio, main risk factors, main interventions, and additional information of interest.
Outbreak time periods were estimated based on the following:
- The beginning of an outbreak time period was determined by sources which indicated that an outbreak was declared at a certain time or the earliest sources available which indicate that a syphilis outbreak is occurring in that region
- The end of an outbreak time period was determined by sources which indicated that a syphilis outbreak was declared over at a certain time or the latest available sources which indicate that a syphilis outbreak is occurring
In some cases, multiple syphilis outbreaks were found in one region in the post-2005 time period. This was determined if a source was found which indicated that multiple outbreaks had occurred post-2005, or if a source was found which referred to an older outbreak in the past tense.
The environmental scan was used to complement the scientific literature review, given lags in publication, and to allow for the presentation of a more up-to-date picture, by jurisdiction.
Appendix D: Rates of infectious syphilis per 100,000 population by sex in countries of the Organization for Economic Co-operation and Development, 2008-2017
| Year | Canada | United States | England | Australia | European Union | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | Ratio | Male | Female | Ratio | Male | Female | Ratio | Male | Female | Ratio | Male | Female | Ratio | |
| 2008 | 7.3 | 1.1 | 6.4 | 7.5 | 1.5 | 5.2 | NA | NA | 11.2 | 1.4 | 8.0 | - | - | 3.0 | |
| 2009 | 8.6 | 0.9 | 9.2 | 7.8 | 1.4 | 5.4 | 9.8 | 1.3 | 7.5 | 11 | 1 | 11.0 | - | - | 3.2 |
| 2010 | 9.2 | 0.9 | 10.3 | 7.9 | 1.1 | 7.0 | 9.1 | 1.1 | 8.3 | 9 | 1.1 | 8.2 | - | - | 3.8 |
| 2011 | 9.6 | 0.7 | 14.7 | 8.1 | 1.0 | 8.5 | 10.1 | 1.1 | 9.2 | 9.9 | 1.5 | 6.6 | - | - | 3.9 |
| 2012 | 11.3 | 0.6 | 18.4 | 9.2 | 0.9 | 10.1 | 10.4 | 1.0 | 10.4 | 12.3 | 1.4 | 8.8 | - | - | 4.6 |
| 2013 | 11.9 | 0.8 | 14.5 | 10.2 | 0.9 | 11.3 | 11.4 | 1.2 | 9.5 | 14.2 | 1.3 | 10.9 | - | - | 5.1 |
| 2014 | 12.7 | 0.9 | 13.8 | 11.6 | 1.1 | 10.5 | 15.5 | 1.1 | 14.1 | 16.6 | 1.5 | 11.1 | - | - | 6.1 |
| 2015 | 17.0 | 1.0 | 16.3 | 13.6 | 1.4 | 9.7 | 18.4 | 1.2 | 15.3 | 21.2 | 2.5 | 8.5 | - | - | 7.9 |
| 2016 | 19.8 | 1.7 | 11.6 | 15.5 | 1.9 | 8.2 | 20.6 | 1.2 | 17.2 | 25.1 | 3.6 | 7.0 | - | - | 7.9 |
| 2017 | 20.0 | 2.4 | 8.2 | 16.9 | 2.3 | 7.3 | 24.4 | 1.5 | 16.3 | 31.1 | 5.5 | 5.7 | 12.0 | 1.4 | 8.5 |
| Note: Data for England was available starting 2009 | |||||||||||||||
Data was retrieved online from the Surveillance Atlas of Infectious Diseases. To calculate the Male to Female ratio, reported syphilis cases from 2008 to 2017 were extracted. Rates before 2017 were not available, so the ratio was calculated by comparing the male to female total number of confirmed cases and the proportion of male to female cases (distribution by gender) for the EU.
United States data sources
Centers for Disease Control and Prevention, Sexually Transmitted Disease Surveillance 2017, Table 28. Primary and Secondary Syphilis among women – reported cases and rates of reported cases by State/Area and Region in Alphabetical order, US and Outlying Areas, 2013 – 2017
Centers for Disease Control and Prevention, Sexually Transmitted Disease Surveillance 2017, Table 29. Primary and Secondary Syphilis among men – reported cases and rates of reported cases by State/Area and Region in Alphabetical order, US and Outlying Areas, 2013 – 2017
CDC Wonder, Selected Sexually Transmitted Diseases by Age, Race/Ethnicity, and Gender, 1996-2014 Request, Primary and Secondary Syphilis, Male AND Female, All ages, All races/ethnicities, 2008 – 2013
Australia data source
HIV, viral hepatitis and sexually transmissible infections in Australia, Annual surveillance report 2018. Chapter 4, Section 4.3 – Syphilis. Data retrieved from Figure 4.3.1 Infectious syphilis notification rate per 100 000 population, 2008 – 2017, by sex.
England data source
Public Health England, Official Statistics Sexually Transmitted infections (STIs): annual data tables. Table 1 (b): Rates of new STI diagnoses in England by gender, 2008 – 2017 Rates per 100 000, Syphilis: primary, secondary & early latent – total
European Union data source
European Center for Disease Prevention and Control, Surveillance Atlas of Infectious Diseases. Criteria: Syphilis, confirmed cases, reported cases, Export: Reported cases, Distribution by gender, 2008 – 2017
European Center for Disease Prevention and Control, Syphilis – Annual Epidemiological Report for 2017, Gender, Figure 2. Syphilis, male-to-female ratio in 27 EU and European Economic Area countries, 2017
Appendix E: Proportion of cases by syphilis stage overall and by sex in Canada, 1991-2017
| Year | Primary | Secondary | Early symptomatic | Early latent | Infectious syphilis - unspecified stage | Late latent | Tertiary |
|---|---|---|---|---|---|---|---|
| 1991 | 15.0% | 11.2% | 9.3% | 7.4% | 0.0% | 56.2% | 0.9% |
| 1992 | 8.9% | 8.2% | 5.4% | 9.9% | 0.0% | 65.4% | 2.2% |
| 1993 | 4.4% | 6.8% | 2.6% | 9.4% | 0.0% | 73.1% | 3.7% |
| 1994 | 8.1% | 8.4% | 6.6% | 7.6% | 0.0% | 65.9% | 3.4% |
| 1995 | 10.0% | 8.4% | 4.0% | 6.5% | 0.0% | 67.3% | 3.7% |
| 1996 | 7.8% | 7.1% | 1.8% | 9.2% | 0.0% | 69.9% | 4.3% |
| 1997 | 12.8% | 6.2% | 0.4% | 7.8% | 0.0% | 68.7% | 4.1% |
| 1998 | 7.9% | 3.3% | 1.7% | 3.7% | 29.5% | 52.7% | 1.2% |
| 1999 | 5.1% | 4.3% | 0.4% | 5.9% | 27.5% | 53.7% | 3.1% |
| 2000 | 6.8% | 5.4% | 1.1% | 6.8% | 21.2% | 54.7% | 4.0% |
| 2001 | 10.4% | 5.5% | 2.0% | 5.8% | 29.7% | 45.0% | 1.7% |
| 2002 | 14.1% | 23.1% | 0.3% | 8.2% | 19.0% | 32.8% | 2.4% |
| 2003 | 20.1% | 24.0% | 1.5% | 11.9% | 17.0% | 23.7% | 1.8% |
| 2004 | 21.5% | 27.5% | 1.3% | 10.6% | 17.6% | 19.1% | 2.4% |
| 2005 | 15.4% | 14.9% | 0.3% | 6.7% | 52.0% | 8.7% | 2.0% |
| 2006 | 15.6% | 17.8% | 0.6% | 10.9% | 48.1% | 5.1% | 1.8% |
| 2007 | 13.0% | 15.1% | 0.8% | 10.4% | 54.6% | 4.7% | 1.3% |
| 2008 | 17.2% | 14.6% | 0.7% | 9.8% | 47.1% | 8.6% | 2.0% |
| 2009 | 17.0% | 12.2% | 1.0% | 10.2% | 52.9% | 4.9% | 1.7% |
| 2010 | 14.7% | 15.3% | 2.4% | 10.8% | 48.8% | 6.3% | 1.7% |
| 2011 | 16.0% | 13.4% | 2.7% | 11.1% | 48.2% | 7.3% | 1.2% |
| 2012 | 12.1% | 12.6% | 0.7% | 11.5% | 56.7% | 5.9% | 0.5% |
| 2013 | 30.6% | 11.7% | 1.2% | 13.4% | 36.3% | 6.1% | 0.8% |
| 2014 | 12.3% | 10.2% | 0.8% | 10.6% | 58.4% | 6.6% | 1.1% |
| 2015 | 10.1% | 9.1% | 0.7% | 11.3% | 62.2% | 5.4% | 1.1% |
| 2016 | 9.8% | 9.5% | 0.3% | 13.0% | 59.8% | 6.5% | 1.1% |
| 2017 | 10.2% | 8.5% | 0.4% | 12.0% | 61.0% | 6.8% | 1.2% |
| Year | Primary | Secondary | Early symptomatic | Early latent | Infectious syphilis - unspecified stage | Late latent | Tertiary |
|---|---|---|---|---|---|---|---|
| 1991 | 9.6% | 10.5% | 5.8% | 9.6% | 0.0% | 63.7% | 0.9% |
| 1992 | 5.8% | 10.0% | 7.2% | 8.4% | 0.0% | 67.1% | 1.4% |
| 1993 | 4.1% | 5.4% | 3.2% | 8.9% | 0.0% | 77.3% | 1.1% |
| 1994 | 4.8% | 2.9% | 6.5% | 8.7% | 0.0% | 73.9% | 3.2% |
| 1995 | 4.9% | 5.3% | 4.2% | 4.5% | 0.0% | 79.2% | 1.9% |
| 1996 | 5.0% | 5.0% | 2.1% | 7.1% | 0.0% | 79.4% | 1.3% |
| 1997 | 5.3% | 7.6% | 0.4% | 8.9% | 0.0% | 74.7% | 3.1% |
| 1998 | 2.0% | 2.0% | 1.0% | 6.0% | 22.5% | 65.5% | 1.0% |
| 1999 | 1.9% | 2.4% | 0.0% | 5.8% | 27.9% | 60.1% | 1.9% |
| 2000 | 3.3% | 2.9% | 0.5% | 5.3% | 17.2% | 70.8% | 0.0% |
| 2001 | 7.0% | 0.8% | 0.4% | 3.3% | 30.2% | 57.0% | 1.2% |
| 2002 | 2.3% | 1.1% | 0.4% | 5.4% | 27.6% | 62.1% | 1.1% |
| 2003 | 6.5% | 5.8% | 0.7% | 7.2% | 30.5% | 48.3% | 1.0% |
| 2004 | 7.0% | 5.9% | 0.7% | 4.5% | 27.3% | 51.4% | 3.1% |
| 2005 | 13.4% | 6.9% | 0.0% | 5.7% | 42.5% | 27.5% | 4.0% |
| 2006 | 12.4% | 8.6% | 0.9% | 10.7% | 44.2% | 22.3% | 0.9% |
| 2007 | 11.5% | 6.9% | 0.5% | 20.6% | 34.4% | 21.6% | 4.6% |
| 2008 | 20.9% | 10.3% | 2.3% | 19.8% | 19.0% | 25.5% | 2.3% |
| 2009 | 21.6% | 13.1% | 1.4% | 23.9% | 13.6% | 24.9% | 1.4% |
| 2010 | 10.2% | 7.2% | 1.7% | 25.1% | 20.4% | 34.0% | 1.3% |
| 2011 | 12.1% | 8.3% | 3.4% | 13.6% | 17.5% | 44.7% | 0.5% |
| 2012 | 7.8% | 4.1% | 0.9% | 11.9% | 24.2% | 49.3% | 1.8% |
| 2013 | 11.2% | 7.9% | 0.4% | 12.0% | 28.5% | 36.4% | 3.7% |
| 2014 | 16.0% | 6.0% | 0.4% | 16.8% | 26.4% | 33.2% | 1.2% |
| 2015 | 17.4% | 10.2% | 1.5% | 14.0% | 27.2% | 27.9% | 1.9% |
| 2016 | 18.3% | 9.5% | 0.0% | 12.8% | 31.6% | 26.9% | 0.9% |
| 2017 | 14.8% | 7.4% | 0.2% | 17.1% | 35.8% | 23.7% | 1.0% |
Source: Public Health Agency of Canada (2019). Canadian Notifiable Disease Surveillance System.
Appendix F: Rates of reported cases of infectious syphilis per 100,000 population by age group and sex in Canada, 2009-2018
| Year | Age group | ||||||
|---|---|---|---|---|---|---|---|
| <15 | 15 to 19 | 20 to 24 | 25 to 29 | 30 to 39 | 40 to 59 | 60+ | |
| 2009 | 0.0 | 3.4 | 12.7 | 17.0 | 16.4 | 12.3 | 1.7 |
| 2010 | 0.0 | 3.9 | 12.9 | 15.4 | 15.9 | 14.2 | 2.6 |
| 2011 | 0.0 | 4.5 | 16.1 | 19.8 | 17.3 | 13.6 | 2.1 |
| 2012 | 0.0 | 6.3 | 21.6 | 22.2 | 20.5 | 15.0 | 2.9 |
| 2013 | 0.0 | 4.0 | 20.9 | 25.7 | 21.8 | 16.0 | 3.4 |
| 2014 | 0.0 | 4.1 | 19.9 | 25.5 | 25.0 | 18.1 | 2.9 |
| 2015 | 0.0 | 5.3 | 23.9 | 36.5 | 34.2 | 24.0 | 4.4 |
| 2016 | 0.0 | 5.9 | 27.4 | 40.8 | 39.9 | 28.7 | 5.2 |
| 2017 | 0.0 | 5.6 | 30.7 | 44.2 | 44.2 | 26.0 | 5.1 |
| 2018 | 0.1 | 11.0 | 40.0 | 65.1 | 60.6 | 30.0 | 10.9 |
This table presents the rates of syphilis in males by age group from 2009 to 2018 in Canada. It is the data presented in Figure 13.
| Year | Age group | ||||||
|---|---|---|---|---|---|---|---|
| <15 | 15 to 19 | 20 to 24 | 25 to 29 | 30 to 39 | 40 to 59 | 60+ | |
| 2009 | 0.0 | 0.9 | 3.3 | 2.9 | 1.6 | 0.7 | 0.1 |
| 2010 | 0.0 | 1.5 | 3.3 | 2.6 | 1.5 | 0.6 | 0.1 |
| 2011 | 0.0 | 1.7 | 2.0 | 1.9 | 1.2 | 0.4 | 0.0 |
| 2012 | 0.0 | 1.5 | 2.2 | 1.1 | 1.0 | 0.5 | 0.0 |
| 2013 | 0.0 | 2.0 | 3.1 | 2.1 | 1.5 | 0.4 | 0.1 |
| 2014 | 0.0 | 2.0 | 3.6 | 2.4 | 1.7 | 0.6 | 0.0 |
| 2015 | 0.0 | 1.7 | 3.4 | 3.9 | 2.0 | 0.6 | 0.0 |
| 2016 | 0.1 | 3.5 | 6.3 | 5.7 | 2.9 | 1.1 | 0.1 |
| 2017 | 0.1 | 5.6 | 8.2 | 8.1 | 4.5 | 1.5 | 0.1 |
| 2018 | 0.3 | 16.9 | 26.4 | 24.7 | 14.2 | 2.7 | 0.2 |
This table presents the rates of syphilis in females by age group from 2009 to 2018 in Canada. It is the data presented in Figure 14.
Source: Public Health Agency of Canada (2019). Canadian Notifiable Disease Surveillance System. Preliminary 2018 data received directly from provinces and territories.
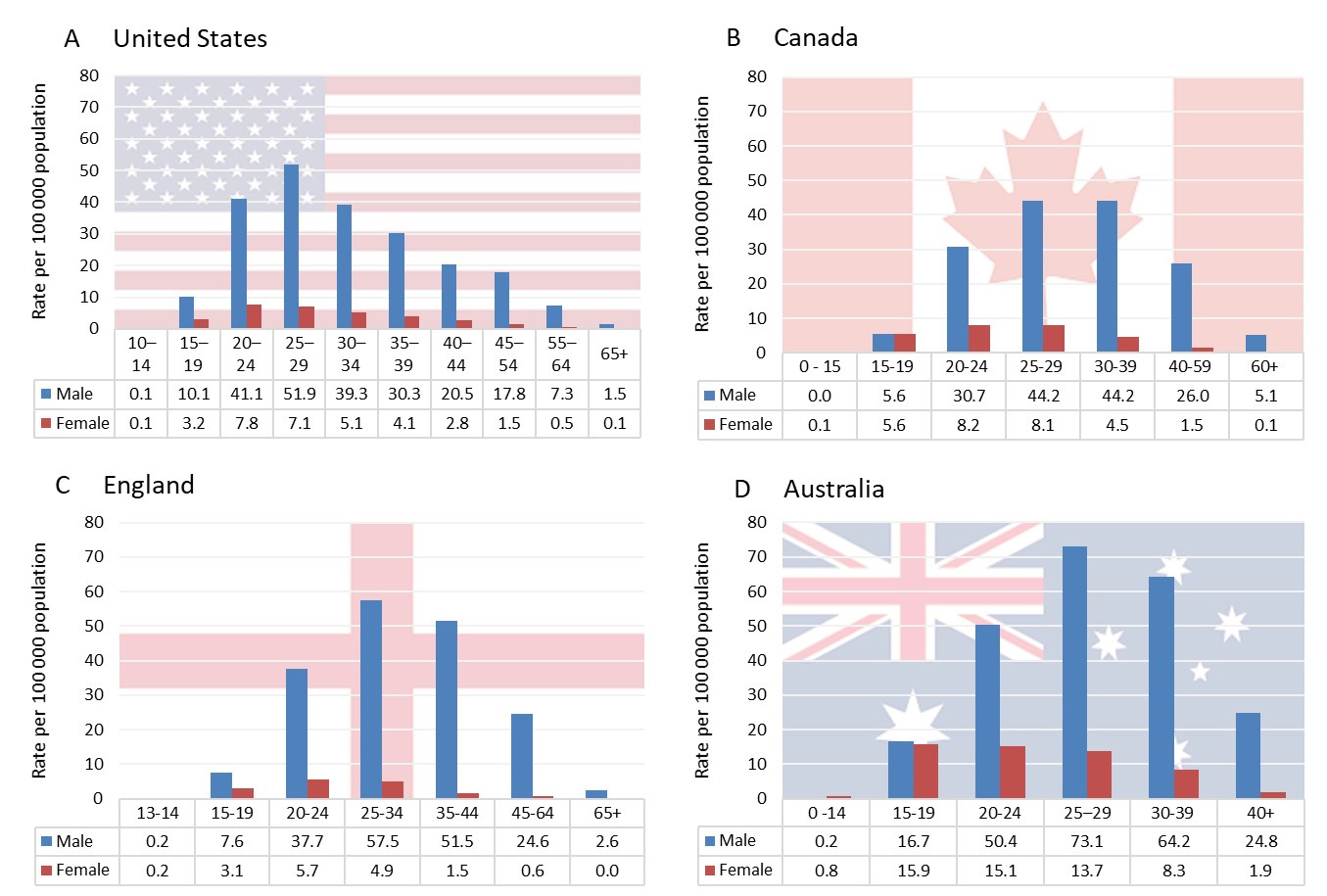
Figure - Text description
This graph compares the rate of infectious syphilis by age group and sex among four OECD countries; the United States, Canada, England and Australia in 2017. The horizontal axis shows the age groups reported by each country for Males and Females. The vertical axis shows the rate of infectious syphilis per 100,000 population reported in 2017.
| United States | Canada | England | Australia | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Age group | Rate per 100,000 population | Age group | Rate per 100,000 population | Age group | Rate per 100,000 population | Age group | Rate per 100,000 population | ||||
| Male | Female | Male | Female | Male | Female | Male | Female | ||||
| 10 – 14 | 0.1 | 0.1 | 0 – 15 | 0.0 | 0.1 | 13 – 14 | 0.2 | 0.2 | 0 – 14 | 0.2 | 0.8 |
| 15 – 19 | 10.1 | 3.2 | 15 – 19 | 5.6 | 5.6 | 15 – 19 | 7.6 | 3.1 | 15 – 19 | 16.7 | 15.9 |
| 20 – 24 | 41.1 | 7.8 | 20 – 24 | 30.7 | 8.2 | 20 – 24 | 37.7 | 5.7 | 20 – 24 | 50.4 | 15.1 |
| 25 – 29 | 51.9 | 7.1 | 25 – 29 | 44.2 | 8.1 | 25 – 34 | 57.5 | 4.9 | 25 – 29 | 73.1 | 13.7 |
| 30 – 34 | 39.3 | 5.1 | 30 – 39 | 44.2 | 4.5 | 35 – 44 | 51.5 | 1.5 | 30 – 39 | 64.2 | 8.3 |
| 35 – 39 | 30.3 | 4.1 | 40 – 59 | 26.0 | 1.5 | 45 – 64 | 24.6 | 0.6 | 40+ | 24.8 | 1.9 |
| 40 – 44 | 20.5 | 2.8 | 60+ | 5.1 | 0.1 | 65+ | 2.6 | 0.0 | |||
| 45 – 54 | 17.8 | 1.5 | |||||||||
| 55 – 64 | 7.3 | 0.5 | |||||||||
| 65+ | 1.5 | 0.1 | |||||||||
Note: Each country above has its own standard for reporting age group.
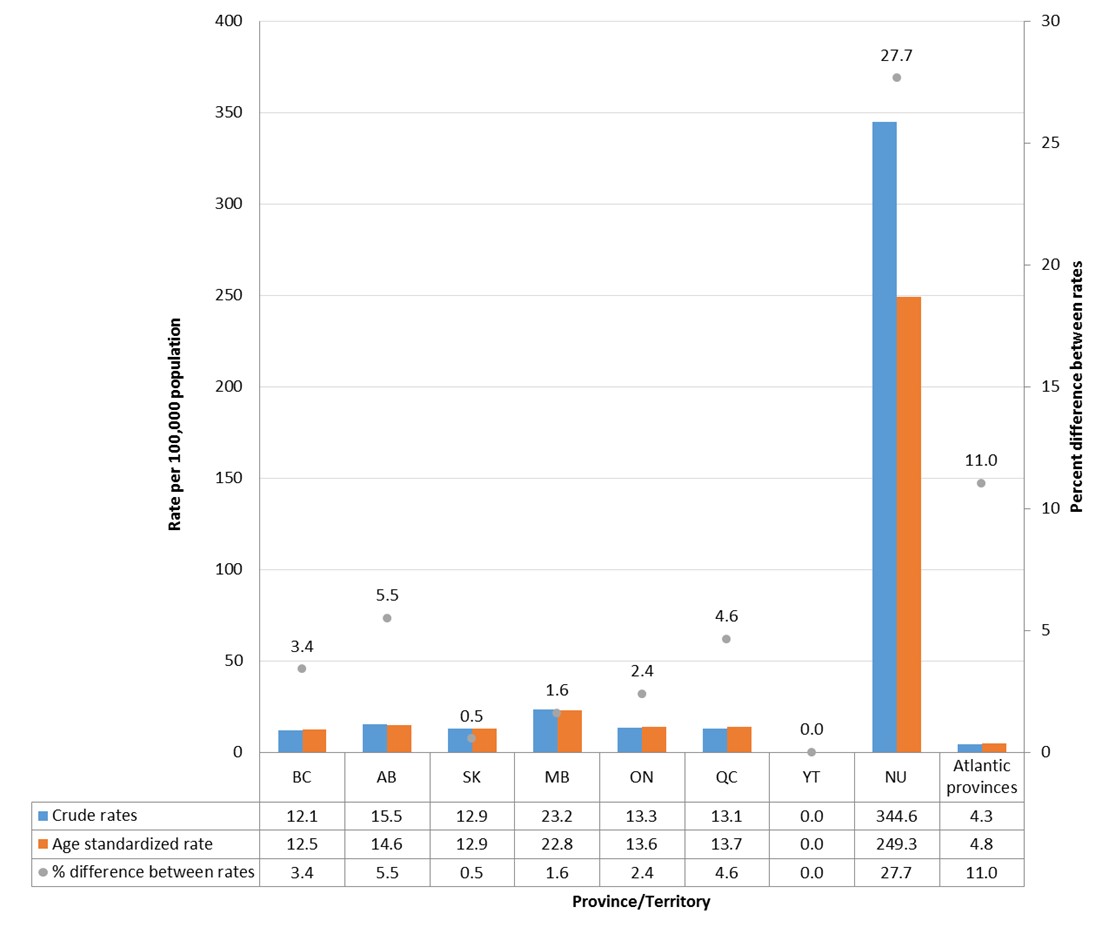
Figure - Text description
This graph displays the crude rates and age standardized rates per 100,000 population for infectious syphilis by province and territory, for those aged 15 and over in 2017. The horizontal axis shows each province and territory (the Atlantic provinces combined). The left vertical axis shows the rate per 100,000 population for infectious syphilis, while the right vertical axis shows the percent difference between the crude and age standardized rates.
| Province or Territory | Crude rates | Age standardized rates | Percent difference between rates |
|---|---|---|---|
| BC | 12.1 | 12.5 | 3.4 |
| AB | 15.5 | 14.6 | 5.5 |
| SK | 12.9 | 12.9 | 0.5 |
| MB | 23.2 | 22.8 | 1.6 |
| ON | 13.3 | 13.6 | 2.4 |
| QC | 13.1 | 13.7 | 4.6 |
| YT | 0.0 | 0.0 | 0.0 |
| NU | 344.6 | 249.3 | 27.7 |
| Atlantic provinces | 4.3 | 4.8 | 11.0 |
Note: Crude rates presented vary from the ones presented in Figure 17 because of the fact that the <15 year age group was excluded from the age-standardization procedure due to low counts of cases.
Source: Public Health Agency of Canada (2019). Canadian Notifiable Disease Surveillance System.
Appendix G: Rates of reported cases of infectious syphilis by province/territory and by sex in Canada, 2009-2018
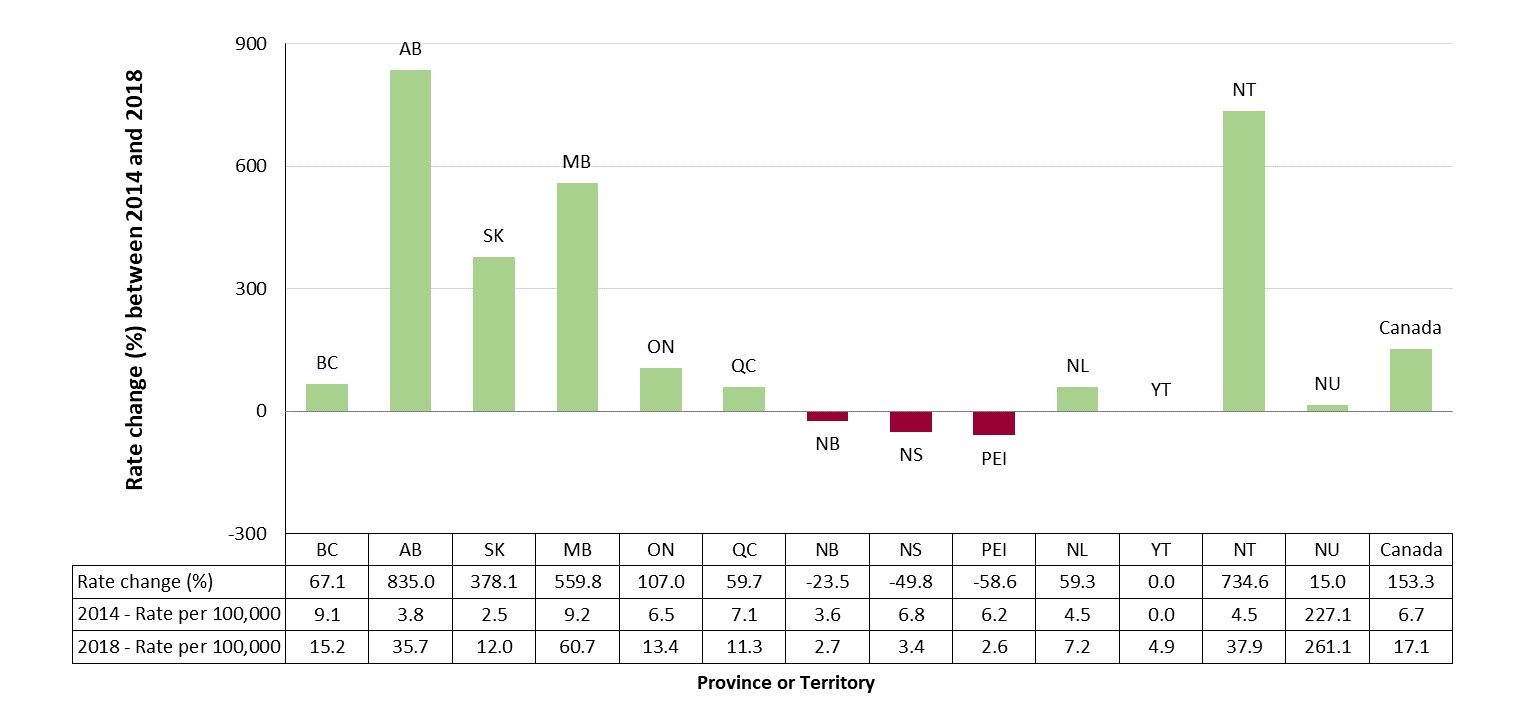
Figure - Text description
This graph displays the percent change in infectious syphilis rates by provinces and territories, between 2014 and 2018 in Canada. The horizontal axis shows the rate per 100,000 population for calendar years 2014 and 2018, as well as the percent rate change of infectious syphilis between the years 2014 and 2018. The vertical axis shows all of the provinces and territories in Canada as well as the total Canadian rate change and rates for 2014 and 2018.
| Rate change (%) between 2014 and 2018 | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BC | AB | SK | MB | ON | QC | NB | NS | PE | NL | YT | NT | NU | Canada | |
| Rate change (%) | 67.1 | 835.0 | 378.1 | 559.8 | 107.0 | 59.7 | -23.5 | 49.8 | 58.6 | 59.3 | 0.0 | 734.6 | 15.0 | 153.3 |
| 2014-rate per 100,000 | 9.1 | 3.8 | 2.5 | 9.2 | 6.5 | 7.1 | 3.6 | 6.8 | 6.2 | 4.5 | 0.0 | 4.5 | 227.1 | 6.7 |
| 2018-rate per 100,000 | 15.2 | 35.7 | 12.0 | 60.7 | 13.4 | 11.3 | 2.7 | 3.4 | 2.6 | 7.2 | 4.9 | 37.9 | 261.1 | 17.1 |
| Year | Province/Territory | Canada rate |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BC | AB | SK | MB | ON | QC | NB | NS | PE | NL | YT | NU | NT | ||
| 2009 | 2.9 | 7.6 | 2.0 | 0.4 | 5.5 | 4.8 | 1.2 | 2.6 | 0.0 | 0.6 | 0.0 | 0.0 | 76.5 | 4.7 |
| 2010 | 2.1 | 4.6 | 3.4 | 1.4 | 5.9 | 6.9 | 4.5 | 1.9 | 0.0 | 0.8 | 0.0 | 0.0 | 6.9 | 5.0 |
| 2011 | 2.8 | 2.5 | 2.2 | 1.3 | 5.8 | 7.8 | 6.6 | 3.8 | 0.0 | 1.0 | 0.0 | 0.0 | 0.0 | 5.1 |
| 2012 | 5.8 | 3.3 | 0.6 | 2.0 | 6.2 | 8.3 | 2.8 | 6.7 | 0.0 | 1.7 | 2.8 | 83.6 | 4.6 | 5.9 |
| 2013 | 9.8 | 3.1 | 1.5 | 4.7 | 5.5 | 7.7 | 4.5 | 8.8 | 3.5 | 1.5 | 5.5 | 161.3 | 0.0 | 6.3 |
| 2014 | 9.2 | 3.8 | 2.5 | 9.2 | 6.5 | 7.1 | 3.6 | 6.8 | 6.2 | 4.5 | 0.0 | 228.0 | 4.6 | 6.7 |
| 2015 | 12.7 | 8.9 | 2.1 | 15.9 | 8.0 | 9.0 | 4.1 | 4.6 | 6.2 | 6.4 | 0.0 | 139.8 | 0.0 | 8.9 |
| 2016 | 12.2 | 9.7 | 7.5 | 17.7 | 10.4 | 11.7 | 1.7 | 1.8 | 1.4 | 4.3 | 0.0 | 262.3 | 2.2 | 10.7 |
| 2017 | 10.4 | 12.6 | 10.4 | 18.8 | 11.2 | 11.0 | 2.5 | 2.7 | 2.7 | 7.4 | 0.0 | 234.3 | 11.1 | 11.1 |
| 2018 | 15.2 | 35.7 | 12.0 | 60.7 | 13.4 | 11.3 | 2.7 | 3.4 | 2.6 | 7.2 | 4.9 | 261.1 | 37.9 | 17.1 |
| Year | Province/Territory | Canada rate |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BC | AB | SK | MB | ON | QC | NB | NS | PE | NL | YT | NU | NT | ||
| 2009 | 5.4 | 10.1 | 2.9 | 0.8 | 10.8 | 9.2 | 2.2 | 5.0 | 0.0 | 1.2 | 0.0 | 0.0 | 85.4 | 8.6 |
| 2010 | 4.1 | 6.2 | 4.9 | 1.5 | 11.3 | 13.1 | 8.6 | 3.7 | 0.0 | 1.6 | 0.0 | 0.0 | 4.5 | 9.2 |
| 2011 | 5.5 | 3.4 | 1.5 | 2.1 | 11.4 | 15.2 | 12.3 | 7.8 | 0.0 | 1.5 | 0.0 | 0.0 | 0.0 | 9.6 |
| 2012 | 11.4 | 5.6 | 0.2 | 3.5 | 12.3 | 15.9 | 4.5 | 13.4 | 0.0 | 3.1 | 5.4 | 94.9 | 8.9 | 11.3 |
| 2013 | 19.5 | 5.0 | 2.2 | 8.4 | 10.6 | 14.8 | 8.8 | 17.4 | 4.3 | 2.7 | 10.7 | 169.7 | 0.0 | 11.9 |
| 2014 | 17.7 | 7.0 | 5.0 | 16.0 | 12.6 | 13.4 | 6.9 | 13.3 | 11.4 | 9.2 | 0.0 | 199.6 | 8.9 | 12.7 |
| 2015 | 25.3 | 16.7 | 3.5 | 24.1 | 15.5 | 17.4 | 7.2 | 8.3 | 9.9 | 12.6 | 0.0 | 133.4 | 0.0 | 17.0 |
| 2016 | 24.0 | 16.8 | 13.8 | 24.1 | 19.9 | 22.5 | 3.4 | 3.7 | 2.8 | 8.0 | 0.0 | 236.9 | 0.0 | 19.8 |
| 2017 | 20.1 | 19.3 | 19.1 | 23.4 | 21.5 | 20.5 | 4.5 | 5.4 | 2.7 | 13.0 | 0.0 | 171.1 | 21.6 | 20.0 |
| 2018 | 29.0 | 42.9 | 17.7 | 65.4 | 25.5 | 20.2 | 5.2 | 6.4 | 3.9 | 12.3 | 4.8 | 248.7 | 47.7 | 27.1 |
| Year | Province/Territory | Canada rate |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BC | AB | SK | MB | ON | QC | NB | NS | PE | NL | YT | NU | NT | ||
| 2009 | 0.3 | 5.0 | 1.2 | 0.0 | 0.3 | 0.4 | 0.3 | 0.2 | 0.0 | 0.0 | 0.0 | 0.0 | 67.0 | 0.9 |
| 2010 | 0.1 | 3.0 | 1.9 | 1.3 | 0.7 | 0.7 | 0.5 | 0.2 | 0.0 | 0.0 | 0.0 | 0.0 | 9.5 | 0.9 |
| 2011 | 0.3 | 1.6 | 2.8 | 0.5 | 0.4 | 0.6 | 1.0 | 0.0 | 0.0 | 0.4 | 0.0 | 0.0 | 0.0 | 0.7 |
| 2012 | 0.3 | 1.0 | 0.9 | 0.5 | 0.4 | 0.7 | 1.0 | 0.2 | 0.0 | 0.4 | 0.0 | 71.6 | 0.0 | 0.6 |
| 2013 | 0.3 | 1.2 | 0.9 | 0.9 | 0.6 | 0.7 | 0.3 | 0.6 | 2.7 | 0.4 | 0.0 | 152.3 | 0.0 | 0.8 |
| 2014 | 0.8 | 0.6 | 0.0 | 2.5 | 0.5 | 0.8 | 0.3 | 0.6 | 1.4 | 0.0 | 0.0 | 258.1 | 0.0 | 0.9 |
| 2015 | 0.4 | 0.9 | 0.7 | 7.7 | 0.6 | 0.6 | 1.0 | 1.0 | 2.7 | 0.4 | 0.0 | 146.5 | 0.0 | 1.0 |
| 2016 | 0.5 | 2.5 | 1.1 | 11.2 | 1.0 | 1.0 | 0.3 | 0.0 | 0.0 | 0.7 | 0.0 | 289.2 | 4.6 | 1.7 |
| 2017 | 0.6 | 5.8 | 1.6 | 14.2 | 1.0 | 1.6 | 0.5 | 0.2 | 2.6 | 1.9 | 0.0 | 301.2 | 0.0 | 2.4 |
| 2018 | 1.2 | 28.3 | 6.2 | 55.9 | 1.3 | 2.2 | 0.3 | 0.6 | 1.3 | 2.3 | 5.0 | 274.2 | 27.5 | 7.0 |
Source: Public Health Agency of Canada (2019). Canadian Notifiable Disease Surveillance System. Preliminary 2018 data received directly from provinces and territories.
Appendix H: Number of cases and rates of congenital syphilis, rates of infectious syphilis among women aged 15 – 39 and rates of infectious syphilis among females, 1993-2018
| Year | Number of congenital syphilis cases | Rate of congenital syphilis per 100,000 live births | Female rate (age 15 - 39) of infectious syphilis per 100,000 females | Total female rate of infectious syphilis per 100,000 females |
|---|---|---|---|---|
| 1993 | 1 | 0.3 | 1.1 | 0.6 |
| 1994 | 4 | 1.0 | 1.0 | 0.5 |
| 1995 | 2 | 0.5 | 0.7 | 0.3 |
| 1996 | 1 | 0.3 | 0.7 | 0.3 |
| 1997 | 3 | 0.9 | 0.8 | 0.3 |
| 1998 | 1 | 0.3 | 0.9 | 0.4 |
| 1999 | 1 | 0.3 | 1.0 | 0.5 |
| 2000 | 2 | 0.6 | 0.8 | 0.4 |
| 2001 | 1 | 0.3 | 1.4 | 0.6 |
| 2002 | 4 | 1.2 | 1.5 | 0.6 |
| 2003 | 2 | 0.6 | 2.2 | 0.9 |
| 2004 | 1 | 0.3 | 1.8 | 0.8 |
| 2005 | 9 | 2.6 | 2.4 | 1.0 |
| 2006 | 6 | 1.7 | 2.4 | 1.1 |
| 2007 | 7 | 1.9 | 2.1 | 1.0 |
| 2008 | 5 | 1.3 | 2.6 | 1.1 |
| 2009 | 10 | 2.6 | 2.1 | 0.9 |
| 2010 | 5 | 1.3 | 2.1 | 0.9 |
| 2011 | 4 | 1.1 | 1.6 | 0.7 |
| 2012 | 3 | 0.8 | 1.4 | 0.6 |
| 2013 | 1 | 0.3 | 2.1 | 0.8 |
| 2014 | 1 | 0.3 | 2.3 | 0.9 |
| 2015 | 5 | 1.3 | 2.6 | 1.0 |
| 2016 | 4 | 1.0 | 4.3 | 1.7 |
| 2017 | 7 | 1.9 | 6.2 | 2.4 |
| 2018 | 17 | 4.6 | 19.3 | 7.0 |
Source: Public Health Agency of Canada (2019). Canadian Notifiable Disease Surveillance System. Preliminary 2018 data received directly from provinces and territories.
Page details
- Date modified: