A Dementia Strategy for Canada: Together We Achieve - 2023 Annual Report
Download in PDF format
(3,547 KB, 64 pages)
Organization: Public Health Agency of Canada
Date published: October 2023
Cat.: HP22-1E-PDF
ISSN: 2562-7805
Pub.: 230469
Contents
- Minister's message
- Introduction
- Tracking the state of dementia in Canada
- Supporting progress on the national dementia strategy
- Reaching Canadians and creating new tools: Project results
- Sharing Dance with People Living with Dementia – Canada's National Ballet School
- Stronger Together – The Dementia Society of Ottawa and Renfrew County
- Mind Over Matter – Women's Brain Health Initiative
- Opens Minds, Open Hearts – Conestoga College
- Dementia-Friendly Canada – Alzheimer Society of Canada
- Therapeutic Dementia Care Program – Cummings Jewish Centre for Seniors
- Empowering Dementia-Friendly Communities Hamilton, Haldimand Project – Hamilton Council on Aging
- National public education campaign
- New Public Health Agency of Canada investments
- Enhanced Dementia Surveillance Initiative: Strengthening Canada's data
- Investing in research on brain health in aging
- Gaining a better understanding of dementia in Canada
- Dementia-inclusiveness and dementia-related stigma
- Reaching Canadians and creating new tools: Project results
- Conclusion
- Appendices
- Endnotes
Minister's message
This year, the annual report on the national dementia strategy marks four years since the release of the strategy and the announcement of five-year funding to support its implementation. This report focuses primarily on investments through the Public Health Agency of Canada (PHAC) to support progress on the national strategy and highlights projects funded through the Dementia Strategic Fund, the Dementia Community Investment, and the Enhanced Dementia Surveillance Initiative. The federal government also continues to support the national dementia strategy in multiple ways through its investments and supports to provinces and territories in areas such as health care, home care and long-term care.
Funded projects are helping to improve the wellbeing of people living with dementia and support their families and caregivers; increase awareness of dementia risk factors, address dementia-related stigma, and promote dementia-inclusive communities; improve access to high-quality dementia guidance; and strengthen data on dementia. While some of the 76 projects funded by PHAC to date are just beginning, others have been completed or are well underway and we are starting to see their results.
In 2019-2020, almost 474,000 Canadians were living with diagnosed dementia. Most Canadians report some experience with dementia, with close to 8 in 10 knowing someone living or who has lived with dementia. There are signs that we are making progress on reducing dementia-related stigma in Canada. However, there is still work to do. For example, public opinion research conducted in early 2023 asked Canadians how their views towards dementia have changed in the past five years. Over a quarter of respondents (26%) indicated that they have a more positive view, while 10% indicated that they have a more negative view.
We are also seeing positive news on dementia risk reduction. The number of Canadians who are intentionally taking steps to reduce their risk of developing dementia has risen from 22% in 2020 to 34% in 2023. Research underscores the need to do more on increasing awareness about dementia risk factors. A national public education campaign on risk reduction was launched in early 2023 through PHAC. Messages ran on digital platforms and digital outdoor ads across Canada. Digital ads were displayed 83 million times and the Canada.ca/dementia website received more than 5,000 daily visits on average. The national campaign will continue over the next year to share messages on both risk reduction and stigma reduction with Canadians.
The Government of Canada is also supporting research to help us better understand, prevent, and effectively treat dementia. This year, the Canadian Institutes of Health Research launched its Brain Health and Cognitive Impairment in Aging Research Initiative. This initiative is supporting the latest areas of research to study the brain as it ages and to identify what can be done to reduce the risk of dementia and other forms of cognitive impairment, while also addressing the complex care needs of people living with dementia and caregivers.
To have the greatest impact, we are working in collaboration with community organizations, provincial and territorial partners and the Ministerial Advisory Board on Dementia to implement the strategy.
In closing, thank you to all those contributing to progress on the national dementia strategy across Canada. Whether it is in our health care system, within our communities or as a caregiver within the home, it is through our combined efforts that we move closer to the aspirations of our shared strategy.
Introduction
Canada's dementia strategy has three national objectives: prevent dementia, advance therapies and find a cure, and improve the quality of life of people living with dementia and caregivers. Projects undertaken through federal investments to support the strategy have reached millions of Canadians to date, creating innovative and tailored resources to promote risk and stigma reduction, and to support more inclusive communities for people living with dementia and caregivers. This year's report highlights a few of the Public Health Agency of Canada funded projects now completed and some of the newest projects launched.
Tracking the state of dementia reveals some positive trends in risk reduction and work related to advancing therapies through research and innovation. However, more work is needed to increase awareness of some key risk factors and encourage Canadians to take more action to reduce risk. As well, recent public opinion research on stigma suggests that while there have been some positive developments in perceptions and attitudes among Canadians related to dementia, there is still much to be done. Finally, the most recent data related to the quality of life of people living with dementia and caregivers, which now incorporates the early months of the COVID-19 pandemic, shows either trends in the wrong direction or no change. This annual report shares information that was current as of June 2023.Footnote 1
Dementia is a term used to describe symptoms affecting brain function. It may be characterized by a decline in cognitive (thinking) abilities such as: memory; planning; judgement; basic math skills; and awareness of person, place and time. Dementia can also affect language, mood and behaviour, and the ability to maintain activities of daily living. Dementia is not an inevitable part of aging.
Dementia is a chronic and progressive condition that may be caused by neurodegenerative diseases (affecting nerve cells in the brain), vascular diseases (affecting blood vessels like arteries and veins) or injuries. Types of dementia include vascular, Lewy body, frontotemporal, Alzheimer's disease and mixed (a combination of more than one type). In rare instances, dementia may be linked to infectious diseases, including Creutzfeldt-Jakob disease.
Tracking the state of dementia in Canada
Each year, the annual report to Parliament on Canada's national dementia strategy provides the most recent data available for a consistent set of data points aligned with the strategy's three national objectives, which are to prevent dementia, advance therapies and find a cure, and improve the quality of life of people living with dementia and caregivers. Over time, these data points provide insights on the progress being made towards the strategy's aspirations.
Objective: Prevent dementia
Overall, data points related to reducing the risk of dementia and moving Canada towards prevention are moving in the right direction. While the number of Canadians diagnosed with dementia has been growing as the population aged 65 and older increases, the rate of newly diagnosed cases of dementia has been decreasing since 2009-2010, when adjusted for the aging of the population (age-standardized).
In 2009-2010 there were 1,577 new cases per 100,000 Canadians aged 65+ years (age-standardized).
In 2019-2020 there were 1,409 new cases per 100,000 Canadians aged 65+ years (age-standardized).Footnote 2
The prevalence of some dementia risk factors among Canadians, including drinking, less education, hypertension, and smoking, is moving in the right direction. The prevalence of some other risk factors, such as cholesterol, sleep, social isolation, and stroke has stayed relatively the same. However, the prevalence of diabetes, obesity and physical inactivity has increased. See Appendix D for further details on the prevalence of risk factors across Canada.
Objective: Advance therapies and find a cure
Data points aligned with the national objective focused on research and innovation are also generally trending in a positive direction. Over the past three years, the total investment in dementia research by the Canadian Institutes of Health Research (CIHR), including investigator-initiated research (e.g., funded through the Project Grant Program), research in priority areas (e.g., the Canadian Consortium on Neurodegeneration in Aging), and training and career support programs (e.g., fellowships) has increased.
| Year | Spending ($) |
|---|---|
| 2021-2022 | approximately $54 million |
| 2020-2021 | approximately $49 million |
| 2019-2020 | approximately $42 million |
Further, in 2021-2022, CIHR supported 297 unique nominated principal investigators Footnote 3 through 346 grants and awards focused on dementia research, an increase of 35 investigators since 2019-2020.
| Year | Investigators (number) |
|---|---|
| 2021-2022 | 297 |
| 2020-2021 | 290 |
| 2019-2020 | 262 |
Finally, the number of funded dementia grants and awards has also grown. This data point reports on the total funded grants (including priority announcements and bridge grants) and awards in dementia research across all of CIHR's programs, including investigator-initiated research, research in priority areas, and training and career support programs.
| Year | Grants / awards (number) |
|---|---|
| 2021-2022 | 346 |
| 2020-2021 | 344 |
| 2019-2020 | 306 |
Objective: Improve the quality of life of people living with dementia and caregivers
Data on pain, depression and social interaction among people living with dementia receiving home care are used to track some aspects of quality of life over time. These data points are stable or worsening in terms of trends. The 2021-2022 statistics include reporting during the early stage of the COVID-19 pandemic. Based on data from four jurisdictions, the percentage of people living with dementia in home care settings, exhibiting withdrawal from activities of interest and/or reduced social interaction and showing a potential or actual problem with depression, increased in 2021-2022 compared with 2018-2019. However, the percentage of those experiencing daily pain stayed relatively stable.
| Data point | Percentage (%) in 2018-2019 | Percentage (%) in 2019-2020 | Percentage (%) in 2020-2021 | Percentage (%) in 2021-2022 | Trend between 2018-2019 and 2021-2022 Footnote 6 |
|---|---|---|---|---|---|
| Exhibiting withdrawal from activities of interest and/or reduced social interaction | 18.3 | 19.1 | 21.1 | 19.1 | Worse |
| Displaying a potential or actual problem with depression, based on a depression rating scale | 24.0 | 24.8 | 24.9 | 24.8 | Worse |
| Experiencing daily pain (severe and not severe) | 34.6 | 34.6 | 33.8 | 34.5 | No statistically significant change |
Since 2018-2019, the percentage of caregivers of people living with dementia experiencing distress remains higher than caregivers of those without dementia. The data point below compares distress experienced by caregivers Footnote 7 of people living with dementia who receive home care in contrast to caregivers who provided care to people without dementia who receive home care.Footnote 8
| Data point | Percentage (%) in 2018-2019 | Percentage (%) in 2019-2020 | Percentage (%) in 2020-2021 | Percentage (%) in 2021-2022 | Trend between 2018-2019 and 2021-2022 Footnote 10 |
|---|---|---|---|---|---|
| Caregivers providing home care to people living with dementia experienced distress | 37.6 | 37.1 | 36.6 | 38.1 | No statistically significant change |
| Caregivers who provided care for someone without dementia experienced distressFootnote 11 | 18.6 | 18.9 | 18.5 | 19.7 | Worse |
Supporting progress on the national dementia strategy
The Public Health Agency of Canada (PHAC) manages the Dementia Strategic Fund (DSF), the Dementia Community Investment (DCI), and the Enhanced Dementia Surveillance Initiative (EDSI). Competitive solicitation processes are used to fund projects that support key elements of the strategy's implementation and identify gaps, including awareness raising projects, dementia guidance projects, community-based projects, and enhanced dementia surveillance. Through these projects, funding recipients are creating innovative and accessible tools, often tailored to specific populations and communities, to support risk and stigma reduction and make Canada more dementia-inclusive. These projects are supporting the wellbeing of people living with dementia and caregivers and strengthening dementia data collection in Canada. Please refer to Appendix A to see the geographic coverage of projects, and Appendix B for the list of all PHAC-funded projects.
PHAC also provides funding to the Centre for Aging and Brain Health Innovation (CABHI), which aims to improve the quality of life for older adults by supporting promising innovations across the country that help meet the needs of older adults and people living with brain health issues, including dementia. More information about CABHI can be found in Appendix C. In addition, the Canadian Institutes of Health Research (CIHR), as the federal lead on dementia research in Canada, funds projects and initiatives, including the Brain Health and Cognitive Impairment in Aging (BHCIA) Research Initiative, that support all three of the strategy's national objectives. The BHCIA Research Initiative aims to promote brain health and support research to improve the care, services, and wellbeing for people living with dementia, caregivers and care providers and is discussed in further detail later in the report.
This past year saw the completion of 11 of the 14 initial projects focused on awareness raising funded under the DSF, along with 17 of the 22 initial projects focused on intervention research funded under the DCI. One of the 10 initial projects focused on enhancing dementia surveillance funded under the EDSI was also completed. In addition, 10 new projects were launched under the DSF to continue awareness raising efforts and 11 new projects were launched to improve access to high-quality dementia guidance. Three new community-based projects funded under the DCI began this past year to continue intervention research on dementia, and five new projects were funded under the EDSI to continue efforts to enhance dementia surveillance.
Reaching Canadians and creating new tools: Project results
Progress on the national dementia strategy was supported by a number of projects. Below are highlights of a few of those that have been completed.
Sharing Dance with People Living with Dementia – Canada's National Ballet School
Through the Sharing Dance with People Living with Dementia project, funded through the Dementia Strategic Fund (DSF), Canada's National Ballet School (NBS) increased awareness about the value of dance for people living with dementia and care providers; developed and delivered dance training across Canada that is accessible for people living with dementia; and, established a network of organizations and individuals committed to supporting implementation of dementia-inclusive dance practices, knowledge sharing and exchange. Working closely with partners, NBS engaged over 25,000 individuals directly during the project. Key awareness-raising products included a national Dancer Not Dementia campaign and the documentary film, Dancer Not Dementia.
Project reach included:
- 2,914,876 individuals reached through social and print media, podcasts, radio, project videos, and newsletters
- 25,804 individuals engaged directly in project activities
- 800+ dancers accessing Sharing Dance at Home classes
- 200+ dance classes designed to be accessible to people living with dementia, available online
- 40+ organizations and groups accessing classes
- 21 dance teachers trained to support dance opportunities for people living with dementia
Project results include:Footnote 12
- 96% of respondents reported an increased/new understanding of using dance to support people living with dementia.
- 93% of respondents articulated actions they plan to take to make their community dementia-inclusive.
- 85% of respondents reported that the event they attended either changed or reinforced their way of thinking about people living with dementia in a positive way, including:
- the ability of people living with dementia to experience a good quality of life; and,
- whether they feel comfortable interacting with someone living with dementia.
"It was very touching to see the joy in being able to express oneself through music, song and movement. The sheer happiness was palpable…"
"I will say that seeing the resident – who could not talk nor move without assistance – smiling and laughing as a caregiver helped her participate in dance was very moving; it taught me that even those who cannot move on their own, who need assistance to dance, can still benefit from the movement and art of dancing."
Stronger Together – The Dementia Society of Ottawa and Renfrew County
Through the DSF, The Dementia Society of Ottawa and Renfrew County provided dementia-inclusive training to individuals and businesses working in public transportation, retail, financial, health care, and leisure fields. The organization has used its Dementia613.ca website to identify businesses and organizations that have received the training within Ottawa and Renfrew County, making them easier to find for people living with dementia and caregivers. Additionally, new content on brain health, modifiable risks, and protective factors is now available on the Dementia Help website. Finally, the project team created a Playbook to help inspire others to create more dementia-inclusive communities, which is being shared with its regional network of dementia-care partners and other organizations nationally.
Text description
10 Tips to Communicate Well with a Person Living with Dementia from the Dementia Society Ottawa and Renfrew County
- Approach the person from the front. If they are seated go down to that level.
- Identify yourself. Tell them your name and offer to help.
- Maintain eye contact. It will help them focus on what you're saying.
- Address the person by name. Speak slowly and clearly.
- Present one idea at a time. It will help them understand.
- Repeat or rephrase the persons' responses. This can help clarify what they are trying to tell you.
- Ask "yes" or "no" questions. Allow time for a response.
- Use gestures. They can help back up your words.
- Listen actively. Acknowledge their emotional state.
- Let the person know if you are going to touch them. It will help them understand.
There is a website at the bottom of the image, which is DementiaHelp.ca
The image also has the following text at the bottom: Financial contribution from the Public Health Agency of Canada.
Project reach included:
- 2,018 individuals received training in the Ottawa and Renfrew regions, including:
- 566 students
- 286 bankers/financial service professionals
- 205 health care professionals
- 105 first responders
- 23 service organizations
- 21 businesses
Project results include:
- After training, 90% of 436 individuals reported strong or very strong confidence in communicating with individuals living with dementia. Before training, 36% reported neutral and 32% reported poor or very poor confidence.
- After training, 72% of 141 university students reported feeling somewhat or extremely competent in communicating with individuals living with dementia. Before training, 43% reported feeling somewhat incompetent or extremely incompetent and 28% reported felt neutral.
"My staff and I attended the dementia-inclusive training and found it to be informative and enjoyable. The use of the videos helped to illustrate some of the concepts and the section on the physical environment made us realize that we need to make a few small changes in the public washroom! I have taken this to our Corporate Office to see if we can offer this training to all Giant Tiger managers and staff."
Mind Over Matter – Women's Brain Health Initiative
Women's Brain Health Initiative (WBHI) focuses on brain health, dementia prevention, and stigma reduction, highlighting the unique risks for women. As part of its national Mind Over Matter® campaign supported by the DSF, WBHI released new free resources such as videos and podcasts, and a new digital application, BrainFit – Habit Tracker. This interactive mobile app encourages users to modify and track their behaviour to help reduce dementia risk. With input from a diverse group of participants that included caregivers and people with lived/living experience, WBHI's evidence-informed campaign was developed around The Six Pillars of Brain Health (stress reduction, exercise, sleep, social activity, mental stimulation, and nutrition).
The WBHI project reach included:
- 673,614 individuals
- 166,799 podcast listens
- 24,728 unique app downloads since December 2022 launch
- 6,700 video views
Project results include:
- 77% of those who listened to the podcasts or watched the videos demonstrated increased awareness of certain aspects of dementia and 41% demonstrated an improved attitude towards people living with dementia.
- Of those who used the BrainFit app, 31% of users improved their nutrition, 24% improved their exercise habits, 18% increased their mental stimulation, 14% improved their stress management, 11% improved their sleep and 4% increased their social activity.
"I had no idea that markers for Alzheimer's and dementia could start 20 to 25 years before symptoms are apparent… The awareness you are bringing about is so invaluable – I ended up sharing the article and podcast and recommended the app to several friends and family as I don't think any of them were aware of how much lifestyle can help prevent [dementia]."
Opens Minds, Open Hearts – Conestoga College
The DSF also funded Conestoga College's Open Minds, Open Hearts project. This project has fostered social cohesion and a sense of belonging through guided intergenerational group activities between post-secondary students and people living with dementia to raise awareness, reduce negative assumptions and decrease the stigma of dementia among younger adults. More than 3,800 interactions between people living with dementia and caregivers and students were facilitated. Docu-films, including interviews featuring students sharing their stories and experiences, were developed and disseminated among college communities and community organizations across Canada.
Project reach included:
- 20 docu-films produced during this project resulted in:
- 3,238 impressions
- 926 total views
- 448 unique viewers
- 28.6% average click through rate
- 3,844 interactions between post-secondary students and people living with dementia and caregivers including:
- 2,279 people living with dementia and caregiver interactions
- 1,565 student interactions
- 202 in-person sessions
- 200 virtual sessions
Project results from survey responses related to viewing the docu-films include:
- 93% strongly agreed/agreed that they feel comfortable interacting with someone living with dementia.
- 93% strongly agreed/agreed that people living with dementia can remain active in and contribute to their community.
- 80% strongly agreed/agreed that some people living with dementia can continue working for years after the onset of symptoms.
- 80% strongly agreed/agreed that people living with dementia can experience a good quality of life.
Project results from survey responses for participants of the intergenerational group activities include:
- 62% of students had positive responses on what steps they would take to make their community more dementia-inclusive (e.g., educating people through health-based student clubs, encouraging others to help and maintain healthy contact and care for people they might know who may be living with dementia).
- 58% of students expressed positive changes in their attitudes towards people living with dementia (e.g., having a better attitude towards people living with dementia, feeling less wary and more comfortable, thinking more about different approaches when interacting with people living with dementia).
"Doing the activities totally changed my perspective on their [people living with dementia] limitations. I realized that they deserve more than just having their basic needs met. They deserve to have good days and fun experiences just like the rest of us. They need to meet new people and feel valued, and it's important to show them that their mental health matters and that people care about them. Now, when I have a chance to connect with people with dementia, I'll find ways to challenge their creativity, and show them that they can have amazing days with fun activities and that there are people who care about their stories, favourite colour, hobbies, and their journey in general."
Dementia-Friendly Canada – Alzheimer Society of Canada
Supported by the Dementia Community Investment (DCI), the Alzheimer Society of Canada's Dementia-Friendly Canada project built on the work of Alzheimer Societies across the country to foster the creation of dementia-inclusive communities across Canada. This project aimed to train Canada's workforce to be dementia friendly, promote and educate the public about dementia, and ensure the growth of the Dementia-Friendly Canada initiative through the development of online courses, awareness campaigns, and other resources.
Project reach included:
- 18,548,655 individuals:
- 18,458,506 general population
- 97 caregivers
- 52 people living with dementia
- 44 knowledge products produced included:
- 18 videos/podcasts
- 13 webinars/presentations
- 1 social media campaign
Project results, from one year after the course pilot, include:
- Participants scored 95% or better on key questions assessing knowledge about course-related material.
- 52% were fairly confident and 24% were completely confident about interacting with people living with dementia.
- 40% reported learning information that resulted in changes in their daily work routine.
"It's a well-designed, thoughtful course that outlines the different areas service providers can focus on. It empowers people in all levels of an organization to have conversations and destigmatize what living with dementia or caring for someone living with dementia means. We all have a role we can play and the barriers that we can chip away can help so many others and hopefully develop thriving and connected communities."
Therapeutic Dementia Care Program – Cummings Jewish Centre for Seniors
The Cummings Jewish Centre for Seniors developed a Therapeutic Dementia Care Program in Côte Saint-Luc, Quebec with funding from the DCI. This day program offered a variety of programs such as art and music therapy, intergenerational programming, informational workshops, peer-to-peer navigation, and respite for caregivers. Therapeutic programming continued virtually through many Zoom class offerings when in-person programming was not possible. All the activities were designed to reduce social isolation and increase meaning and purpose for people living with dementia at various stages.
Project reach included:
- 739 individuals:
- 452 general population
- 156 caregivers
- 131 people living with dementia
Project results include:
- 100% of caregiver participants reported improved wellbeing of the people living with dementia they care for.
- 100% of participants living with dementia and 92% of caregiver participants reported improved wellbeing.
- 93% of participants living with dementia and caregiver participants reported an increase in knowledge and/or skills.
- 89% of participants living with dementia and caregiver participants reported improved protective factors.
- 88% of participants living with dementia and caregivers reported improved health behaviours.
"[My wife] has an AMAZING time with you. She cannot stop saying how much she enjoys herself. I am so very, very grateful that this program exists. It is literally helping me become more mentally stable and confident in my 24/7 caring for [my wife]!"
Empowering Dementia-Friendly Communities Hamilton, Haldimand Project – Hamilton Council on Aging

Text description
Next to the text is an image of a poster from the Faces of Dementia campaign. In this poster, a woman is holding a piece of art, with other pieces of art around her.
The text of the poster is:
I am more than a stereotype. I am an artist.
People living with dementia are more than their diagnosis. Help us build dementia-friendly communities.
There is a website listed in the poster: www.facesofdementia.ca
At the bottom of the image, there is text that reads: Financial contribution from the Public Health Agency of Canada and the Hamilton Council on Aging.
With funding from the DCI, the Hamilton Council on Aging has worked towards raising awareness and reducing stigma through the development of a dementia-inclusive communities training workshop and the Faces of Dementia awareness campaign. Communities were engaged in the development of action plans that reflected community priorities to improve the quality of life for people living with dementia in Hamilton and Haldimand County in Ontario. The activities were co-designed and co-led by people living with dementia.
Project reach included:
- 16,021,137 individuals:
- 16,020,813 general population
- 277 caregivers
- 47 people living with dementia
Project results include:
- 100% of people living with dementia indicated improved wellbeing.
- 85% of participants in the three project components (the campaign, lived experience leadership teams, and the education program) reported an increase in knowledge and/or skills.
- 83% of participants in the education program reported improved health behaviours.
- 83% of participants in the campaign and lived experience leadership teams reported experiencing improved protective factors.
"I realized that I did have some preconceived notions about dementia, and I am happy to have that corrected. While the subject is sad, there were so many moments of joy. Seeing and learning more about dementia and the people who have that diagnosis, and hearing their stories, goes such a long way in understanding..."
National public education campaign
A national public education campaign is a major element of the DSF. Through this campaign, a public relations tour with two well-known spokespersons and a digital influencer campaign, millions of Canadians received information about dementia over the last year.
A national digital advertising campaign on reducing stigma ran between September 19 to October 23, 2022. Digital ads were shown 31.7 million times and users clicked on the ads a total of 156,800 times. The Canada.ca/dementia website received a total of 140,586 visits during the campaign period.
The campaign focused on dementia risk reduction in early 2023 from January 23 to March 31. It included: new video ads on two dementia risk factors, (physical inactivity and high blood pressure); interactive quizzes; search engine marketing; digital banners; and outdoor ads. The ads were shown 83 million times and users clicked on the ads a total of 408,700 times. The Canada.ca/dementia website received a total of 362,578 visits during this period.

Figure 1 - Text description
There are three images related to the campaign on this page.
The first one shows an ad that has an image of a woman smiling, holding a mug, with others around her.
The text on top of this image reads: Social isolation can increase the risk of dementia by 60%.
The second one shows an ad that has an image of a grand-father and grand-daughter cooking together in a kitchen.
The text on top of this image reads: Another reason to choose homemade. Too much sodium in highly processed foods can lead to high blood pressure, increasing the risk of dementia by 60%.
Learn how to reduce the risk of dementia
Canada.ca/dementia
The third one shows an ad that has an image of a woman climbing up the stairs at a public transit terminal.
The text on top of this image reads: Physical inactivity can increase the risk of dementia by 40%. Try stepping off one stop early.
Learn how to reduce the risk of dementia
Canada.ca/dementia
Figure 2: Blood pressure and physical activity videos from PHAC's national advertising campaign
Dementia risk reduction – High blood pressure
Dementia risk reduction – Physical inactivity
Two national spokespersons, Jay Ingram and Martin Carli, supported the risk reduction campaign. Their public relations tour resulted in 39 interviews on television and radio, and generated digital media content for a combined reach of 13.7 million impressions across Canada and a positive sentiment of 99%. PHAC also partnered with six digital influencers who encouraged followers to take action to help reduce their risk of developing dementia. Influencer social media posts resulted in 182,869 impressions, 7,240 engagements including a 99% positive sentiment rate, and a 4.7% video completion rate, well above the benchmark rate of 1 to 2%. Work continues on the next elements of the campaign.
"Brain health matters at any age. Steps such as paying attention to and addressing hearing loss as we age, staying active, not smoking, socializing, and learning new things throughout life can all contribute to a healthier brain and help reduce the risk of developing dementia. Beyond individual efforts, we must ensure our communities are inclusive and provide everyone with access to the opportunities and supports they need to make healthier choices. It's never too late or too early to make brain health a priority."
New Public Health Agency of Canada investments
Public Health Agency of Canada (PHAC) investments continue to support the advancement of the dementia strategy's national objectives of preventing dementia and improving quality of life of people living with dementia and caregivers. These projects are helping to reach Canadians across the country, including those who may be at higher risk of developing dementia and/or face barriers to equitable care.
Preventing dementia
Some of the latest awareness raising projects funded under the Dementia Strategic Fund (DSF) and Dementia Community Investment (DCI) add to the efforts underway to improve Canadians' knowledge of the risk factors linked to developing dementia and actions to take to reduce the risk.
These projects include:
- Expanding the scope of the Luci program, to reach a more diverse population across Canada, including people facing health inequities. The Luci program aims to increase awareness of modifiable risk and protective factors for dementia and help individuals adopt healthy lifestyle habits (Lucilab Inc.).
- Evaluating the effectiveness of e-learning resources and promoting e-learning tools to help raise awareness and improve knowledge about dementia risk factors (McMaster University).
- Developing a website, videos, infographics, and a podcast (Defy Dementia) to address risk factors and stigma; co-designed with older adults, people living with dementia, and caregivers (The Baycrest Academy for Research and Education).
- Developing and administering an early intervention program to those at a high risk of or living with dementia and caregivers in rural and remote communities on Cape Breton Island through physical activity, music, art, and social program (Cape Breton University).
Improving the quality of life for people living with dementia and caregivers
New projects funded through the DSF and DCI are also building on efforts to improve the quality of life of Canadians living with dementia and caregivers by, for example, focusing on stigma reduction, improving person-centred communication and care, and supporting dementia-inclusive communities.
Some examples are highlighted below:
- Contributing to dementia guidance and information tailored for ethnic and cultural communities, such as practical guidelines for family doctors to use for all Canadians with an additional focus on the needs of Black Canadians and Chinese Canadians when disclosing a dementia diagnosis which will support improved dementia care (Alzheimer Society of Canada) and by providing South Asian communities with language-specific workshops, activity kits, and culturally appropriate awareness-raising campaigns on dementia and brain health delivered in multiple languages within the region of Peel in Toronto (Indus Community Services).
- Adapting the Multi-specialty Interprofessional (MINT) Memory Clinic Model to improve access to and use of person-centred dementia guidance in primary care for those who face barriers to equitable dementia care in three diverse settings: a South Asian community in British Columbia, Indigenous and/or northern communities in Alberta and Saskatchewan, and a francophone community in New Brunswick (Centre for Family Medicine Family Health Team).
- Improving access to dementia care for Indigenous communities by establishing Indigenous-led community-based memory clinics that focus on complete care and support for Indigenous persons living with dementia and caregivers in Northern Ontario (Maasmwesying North Shore Community Health Services).
- Improving guidance tailored for Indigenous communities by engaging communities in northern British Columbia, including Indigenous communities, to create culturally appropriate and culturally safe college and community materials (College of New Caledonia) and addressing gaps in current dementia guidance by defining best practices in Indigenous-centred dementia care and sharing outputs with the broader community of dementia care providers (The Governors of the University of Calgary).
- Updating and adapting existing guidance on community services and supports for people living with dementia and intellectual/developmental disabilities (Reena).
- Undertaking a national bilingual awareness campaign to promote the acceptance and understanding of people living with dementia in 2SLGBTQI+ communities and strengthen supports for chosen families as their primary carers (Egale Canada).
- Improving guidance for paid care providers by: developing a comprehensive education program for first responders focused on emotion-based approaches to support people living with dementia and equip them with the skills to de-escalate situations (Regional Municipality of Peel); and enabling easier access to evidence-informed online resources on the behavioural and psychological symptoms of dementia (Canadian Coalition of Seniors' Mental Health through the Canadian Academy of Geriatric Psychiatry).
- Reducing stigma and promoting inclusion within communities including: through a community-centred campaign and a community plan (City of Vernon); in-person events in British Columbia and virtual events nationally (Brella Community Services Society); and developing and sharing multimedia materials with intergenerational program facilitators and service providers (Families Canada).
- Developing IncludeMe™ Dementia Edition for Caregivers, an online educational experience designed to enhance understanding of dementia behaviours and support for caregivers of people living with dementia including encouraging self-care (Iris the Dragon).
- Expanding the Forward with Dementia initiative across Canada by adapting resources, developing website content, and designing and implementing campaign strategies to address stigma within diverse cultural and linguistic groups, specifically Chinese, South Asian, Italian and Hispanic communities (Schlegel-UW Research Institute for Aging Foundation).
- Implementing a community-based music-making intervention for people living with dementia and caregivers, including official language minority communities, immigrants and ethnic minorities, with expected impacts on wellness, including mental health and social connectedness (University of Ottawa).
- Co-adapting and implementing an eight-week, bi-weekly healthy lifestyle program to improve the physical, mental, and social wellbeing of people living with dementia for those living in rural locations, and Cantonese- and Mandarin-speaking individuals (University of Waterloo).
Some of the newest DSF projects support both prevention and quality of life:
- Expand a volunteer training method developed in Japan to enable dementia-inclusive Japanese communities across Canada, increase awareness of dementia risk factors and reduce dementia-related stigma (Japanese Medical Support Network in Canada).
- Develop a user-friendly online dementia guidance resource hub for individuals from Chinese communities across Canada to find reliable dementia guidance resources applicable to the Canadian context in languages that they can easily access and understand (e.g., English, Traditional Chinese, and Simplified Chinese) (Yee Hong Centre for Geriatric Care).
Enhanced Dementia Surveillance Initiative: Strengthening Canada's data
One of the five pillars of Canada's national dementia strategy is surveillance and data which inform efforts to reduce risk and improve the quality of life of people living with dementia and caregivers. The Enhanced Dementia Surveillance Initiative (EDSI) has supported 15 projects whose findings will be shared publicly as they become available. Some projects are helping to collect data on specific populations who may be more at risk of developing dementia, as well as data on dementia risk and protective factors. Other projects are providing insights to better the care and lives of those impacted by dementia. Some examples include:
Preventing dementia
Canadian Indigenous Cognitive Assessment Training & Implementation: Building the Foundation for Indigenous Dementia Surveillance (building on findings from previously funded project: National Indigenous Dementia Surveillance Initiative – A Feasibility Study)
Through a continued partnership with the Anishinabek Nation and Za-Geh-Do-Win Information Clearing House, a team of community partners and university researchers is developing and piloting a robust training platform to increase uptake of the Canadian Indigenous Cognitive Assessment (CICA). The CICA is a culturally informed cognitive assessment tool developed with Anishinaabe partners on Manitoulin Island, Ontario. The project team also aims to integrate the CICA into electronic medical record systems in four First Nation communities. To date, CICA training has been provided to 30 health care providers that serve First Nations health organizations in Northern Ontario. The research team continues to engage in relationship building and knowledge sharing opportunities with other communities to increase the uptake of CICA. The results of this work may improve the identification of individuals who present an increased risk of dementia and support the development of a risk profile in these communities. This evidence can inform programs and policies to delay or prevent the onset of the condition.
Homelessness Counts: Exploring dementia in people experiencing homelessness
Researchers from the Lawson Health Research Institute analyzed administrative health care data from Ontario to better understand the context of those experiencing homelessness and dementia. These researchers compared the proportion of people living with dementia over the age of 45 in 2019 between three groups: people experiencing homelessness, low-income housed residents, and general population housed residents.
Some highlights of the analysis include:
- Among those experiencing homelessness, the proportion of people living with dementia was significantly elevated across all age groups and sex (1.6 to 4.8 times higher), except for individuals aged 85 and over.
- Comparing dementia cases across the three housing groups, those experiencing homelessness were diagnosed with dementia at a younger age (homelessness median age: 71 vs low-income median age: 79 and general population median age: 80) and were more likely to be male.
- Those who were experiencing homelessness also had a higher prevalence of health conditions associated with dementia, including head trauma, epilepsy, mental illness, and substance-related disorders.
These findings add to the limited surveillance evidence in homeless populations, as they relate to dementia and clearly illustrate the importance of considering the broader factors linked to the condition, such as housing status and other social determinants of health, when developing prevention strategies.
Climate change surveillance for chronic health effects in populations: Enhanced activities focused on dementia
This project, led by researchers from the University of Alberta, aims to investigate the risk of dementia in relation to weather and air pollution exposures, and modification of those risks by social and environmental factors. The researchers are conducting analyses to examine relationships between weather, air pollution, and dementia-related hospitalizations and primary care visits. In addition, a scoping review exploring the relationship between dementia and climate change has been developed. This evidence will help inform climate change adaptation and health surveillance strategies and increase the knowledge surrounding dementia prevention.
Improving the quality of life for people living with dementia and caregivers
Dementia in long-term care and home care settings
The Canadian Institute for Health Information (CIHI) is analyzing data on people living with dementia and caregivers, looking at the progression of the condition and transitions from community to long-term care settings, as well as the experiences and outcomes of caregiving.
The main findings show:
- those who moved to long-term care were more likely to have moderate or more severe cognitive impairment relative to those who stayed in home care (31% vs 21%); and,
- those who moved to long-term care were more likely to be cared for by a family caregiver experiencing distress (41%), relative to those who stayed in homecare (32%).Footnote 13
Findings from this project can help capture the challenges and needs of people living with dementia across care settings and of those who are providing unpaid care.
National Dementia Caregiver Surveillance through First Link®: A Pilot Project by Alzheimer Society of Canada
This pilot project led by the Alzheimer Society of Canada in collaboration with the Alzheimer Society Federation aims to develop a profile of dementia caregivers using the First Link®program. First Link®connects people to dementia-focused health services, support and information. About 80% of the users are caregivers. Anonymized caregiver profile data was initially collected across five participating provinces funded by PHAC: New Brunswick, Quebec, Ontario, Saskatchewan and Alberta. Building on this, additional data collection has taken place in Newfoundland and Labrador, Prince Edward Island, Nova Scotia, Manitoba and Northwest Territories. The project is expected to improve understanding of caregiver needs and inform future efforts to provide support.
Enhanced use of health administrative data for surveillance of dementia in Canada
Researchers from the Ottawa Hospital Research Institute are supporting improved health care planning for dementia by estimating the costs of health care resources used by people living with dementia. This project will examine health care costs in four stages (pre-diagnosis, diagnosis, progression, end-of-life). Policymakers and administrators may use these costs to better estimate and allocate health and social services to ensure people living with dementia have enough supports to improve and maintain their quality of life.
Investing in research on brain health in aging
In March 2023, the CIHR Institute of Aging (CIHR-IA) launched its new Strategic Plan 2023-2028 – Reframing Aging and Empowering Older Adults. The Plan commits to supporting research that reframes aging, refocuses on the value of lived and living experiences, and repositions health care and supports to meet the needs of Canada's increasing older adult population.
As an early deliverable of the new Strategic Plan, CIHR-IA also launched the new Brain Health and Cognitive Impairment in Aging (BHCIA) Research Initiative, which will support research to study the brain as it ages and help identify what can be done to reduce the risks of dementia and other forms of cognitive impairment. The new Strategic Plan and the BHCIA Research Initiative represent important milestones in advancing the goals of the research and innovation pillar of Canada's national dementia strategy.
The Brain Health and Cognitive Impairment in Aging Research Initiative
Informed by extensive stakeholder consultations, the vision of the BHCIAResearch Initiative is to promote brain health in aging while addressing the complex care needs of people living with dementia, caregivers and care providers. The initiative will support research across the continuum from the healthy aging brain to cognitive impairment and care for those impacted by dementia.
The BHCIA Research Initiative will support research and knowledge mobilization activities that aim to:
- create knowledge about resilience in brain aging, identify, and reduce risks that can lead to cognitive impairment, mobilizing this knowledge to change approaches to brain health;
- improve care and services for people with cognitive impairment and dementia; and,
- develop, evaluate, and implement strategies to improve the health and wellbeing of caregivers and care providers.
The BHCIA Research Initiative represents a total investment of approximately $38.3 million over five years. This includes a federal investment of $20 million over five years to CIHR for dementia and brain health research, announced in Budget 2022, and leverages funding from external partners. Research supported through this initiative will consider aspects of equity, diversity, and inclusion, with dedicated funding for research related to the social determinants of health, Indigenous health research, and historically excluded populations.
The first two funding opportunities under this initiative were launched in March 2023 and will help to create knowledge on risk reduction by supporting up to 32 research projects starting in Fall 2023. Importantly, knowledge mobilization activities will ensure that the research findings generated through the BHCIA Research Initiative will be shared with a wide audience, including people with lived experience, health care professionals, and decision-makers. CIHR also looks forward to collaborating with partners to support capacity development and training opportunities for Canada's dementia research leaders of tomorrow through this initiative.
Pia Kontos of the KITE Research Institute – University Health Network and the University of Toronto and her team (Sherry Dupuis, Alisa Grigorovich, Julia Gray, and Christine Jonas-Simpson) are developing digital knowledge translation initiatives to reduce stigma and support social inclusion for people living with dementia with funding from CIHR. In 2022, the team received the CIHR Institute of Aging Betty Havens Prize for Knowledge Mobilization in Aging for two of these initiatives. Cracked: new light on dementia, is a research-based theatre production and film that has been seen by approximately 10,000 people. In 2023, the findings demonstrated how the filmed version prompted transformational change in the understanding of dementia and changes in practice. Dementia in New Light: A Digital Learning Experienceis an interactive educational tool that uses a wide breadth of multi-media resources, many of which draw upon the arts (e.g., theatre, film, music, poetry, animation). The tool is currently being evaluated, but is already being used in hospitals and universities to deepen learning and engagement.
An online Driving and Dementia roadmap is available for families with lived experience of dementia and for health care providers. This is a free online resource (toolkit), developed by the Canadian Consortium on Neurodegeneration in Aging (CCNA) researchers at Baycrest and Sunnybrook Health Sciences. Between October 19, 2022 and June 20, 2023, more than 26,200 visitors have accessed the toolkit website with over 96,000 page views. Recognizing when it becomes unsafe to drive is the most viewed page for families, and Assessing fitness to drive is the most viewed page for health care providers.
Gaining a better understanding of dementia in Canada
The Public Health Agency of Canada (PHAC) continues to conduct public opinion research to better understand dementia and provide an evidence-based foundation for current and future efforts. This section of the report highlights some of the recent findings related to the strategy's national objectives of preventing dementia and improving the quality of life of people living with dementia and caregivers. Recent public opinion research has included a focus on official language minority communities (OLMCs), a population identified as being likely to be at higher risk and to face barriers to equitable care. When Canadians were asked how their views towards dementia have changed in the past five years, more respondents (26%) indicated they have a more positive view than a more negative view (10%). Footnote 14 This same survey found a relatively high level of discomfort remains in sharing news of a diagnosis. In addition, while the number of Canadians who are intentionally taking steps to reduce their dementia risk has risen, more work is needed to increase awareness about dementia risk factors. All final public opinion reports are published online on the Library and Archives Canada site.Footnote 15
Risk reduction behaviors and beliefs
Recent public opinion research shows some positive developments related to reducing dementia risk in Canada while also highlighting areas for additional work. Footnote 16 Over time, it appears that more people in Canada recognize that dementia is not an inevitable part of aging and that there are things that can be done to reduce the risk of dementia. These views are important in encouraging Canadians to take steps to reduce risk.
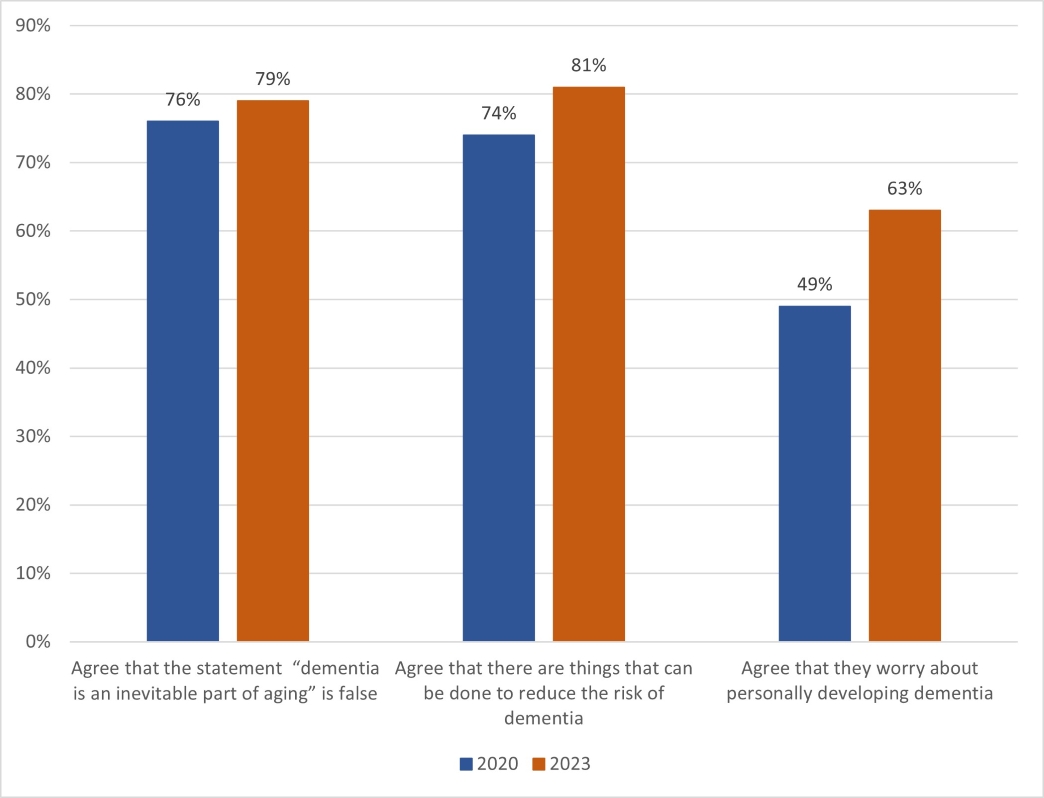
Figure 3 - Text description
- Agree that the statement "dementia is an inevitable part of aging" is false
- 2020: 76%
- 2023: 79%
- Agree that there are things that can be done to reduce the risk of dementia
- 2020: 74%
- 2023: 81%
- Agree that they worry about personally developing dementia
- 2020: 49%
- 2023: 63%
While more Canadians in 2023 (63%) worry about personally developing dementia compared to 2020, a slightly higher number (67%) believe they have a moderate to high ability to reduce their own personal dementia risk (see Figure 4). Footnote 17 Almost three-quarters (71%) of respondents to a 2022 survey on dementia prevention reported that they have engaged in activities over the past year that are linked to reducing dementia risk, without intentionally meaning to reduce that risk. Women were more likely than men to say they will continue these activities (76% compared to 69%). Further, it is encouraging that the number of those who intentionally took steps to reduce their risk of developing dementia increased since 2020 from 22% to 34% (see Table 6).
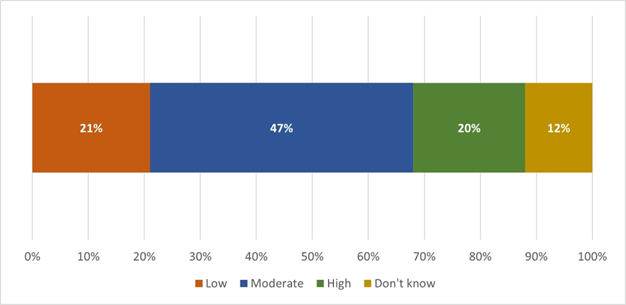
Figure 4 - Text description
- Low: 21%
- Moderate: 47%
- High: 20%
- Don't know: 12%
- 69% had been unintentionally taking steps that are linked to reducing the risk of dementia
- 89% of those unintentionally taking steps linked to reducing the risk of dementia planned to continue all or most of these steps
| Year | Percentage (%) |
|---|---|
| 2023 | 34% |
| 2020 | 22% |
Evidence suggests that risk factors in midlife account for 15% of preventable cases worldwide compared to 18% in later life and 7% in early life. While some risk factors are more important to act on at different stages of life, it is never too late or too early to reduce dementia risk. Even for those diagnosed with dementia, action on dementia risk factors may help to delay the progression of symptoms.Footnote 19,Footnote 20
Figure 5: At what age do you think it's important for people to start taking action to reduce their risk of dementia?

Figure 5 - Text description
- Under 35 years: 13%
- 35-54 years: 31%
- 55-74 years: 23%
- 75 years or older: 2%
- At any age: 25%
- Don't know: 6%
Many Canadians may not be aware of the variety of risk factors linked to dementia. For example, when asked about risk factors that come to mind, only about one in four or one in five correctly identified physical inactivity (25%), a lack of cognitive stimulation (24%), an unhealthy diet (21%), and loneliness and social isolation (18%) as dementia risk factors. Almost none identified less education, hearing loss or depression as risk factors (between 0% and 1%). Further, just under a third of respondents to this survey (28%) indicated that they either did not know the risk factors for dementia or did not respond to this question.
Genetics is the most often identified risk factor (34%). However, evidence suggests that genetic risk is not likely to be a significant factor in most cases of dementia. Further, some ethnic groups have been identified as being more likely to have a higher risk of developing dementia. In the survey, 31% agreed that there is an increased risk among ethnic and cultural groups, while 69% either disagreed or were unsure.Footnote 21,Footnote 22 These findings suggest further potential to integrate information about dementia risk reduction in public messaging on health behaviours.
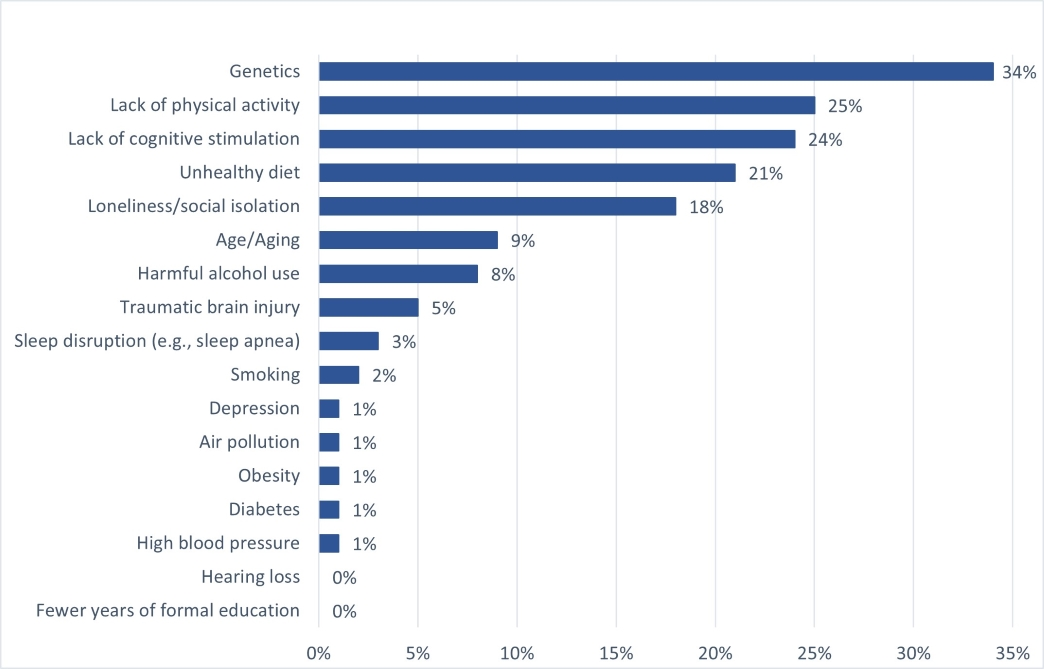
Figure 6 - Text description
- Genetics: 34%
- Lack of physical activity: 25%
- Lack of cognitive stimulation: 24%
- Unhealthy diet: 21%
- Loneliness/social isolation: 18%
- Age/Aging: 9%
- Harmful alcohol use: 8%
- Traumatic brain injury: 5%
- Sleep disruption (e.g., sleep apnea): 3%
- Smoking: 2%
- Depression: 1%
- Air pollution: 1%
- Obesity: 1%
- Diabetes: 1%
- High blood pressure: 1%
- Hearing loss: 0%
- Fewer years of formal education: 0%
What motivates Canadians to reduce their risk of developing dementia? Top reasons reported:
- Knowing someone with dementia (50%)
- Aware of credible evidence (28%)
- Experiencing changes in health status that increased their concern of developing dementia (28%)
Individuals living in official language minority communities (OLMCs) and dementia risk reduction
A recent study on dementia and individuals living in OLMCs (anglophone and francophone) found similar results compared with public opinion research done with the general population. Footnote 23 For example, OLMC respondents tended to identify genetics and aging as key risk factors for dementia. Very few correctly identified key modifiable risk or protective factors for dementia when describing their own personal risk, such as eating better, exercising more and cutting back on alcohol and smoking. Participants reported that the steps they generally take that happen to be linked to reducing the risk of dementia were based on a general desire to be healthier rather than specifically to reduce dementia risk.
Modifiable risk factors can be acted on to reduce risk. Other risk factors include age, sex and gender.
For some of the OLMC participants, having a close relative who had lived with dementia was a motivating factor for remaining intellectually engaged to reduce risk. While participants did not feel there was anything specifically preventing them from taking steps to reduce their risk, a lack of motivation and time were noted as potential barriers. The availability of activities that could help reduce dementia risk in the official language of choice was not considered a barrier to participation, though most participants would opt for activities in their preferred official language if they were available.
Few OLMC study participants had talked to a health professional or explored information about how to reduce dementia risk. Those seeking this type of information, regardless of whether they were anglophones in Quebec or francophones outside of Quebec, found it most often online and in English, with the default search language tending to be English. A few francophones living outside of Quebec mentioned they feel it is better to go straight to the English source as sometimes the quality of the French translation is poor.
Efforts have been underway to better inform, equip and support Francophone minorities living in British Columbia, Alberta, Saskatchewan and Yukon on reducing the risk of developing dementia. In February 2023, RésoSanté Colombie-Britannique launched a 28-day challenge "Un cerveau bien alimenté, activé et allumé en février" in support of healthy lifestyles that promote good physical and cognitive health, through funding from PHAC.
Dementia-inclusiveness and dementia-related stigma
Stigma can be a significant barrier to participation in the community and affect the quality of life of people living with dementia. Stigma is often the result of uninformed attitudes and beliefs and affects people living with dementia, their loved ones and caregivers. Stigma can happen in many ways such as the assumption that those living with dementia will inevitably experience a lower quality of life. It may also result in feelings of discomfort when interacting with someone living with dementia.
People living with dementia can experience stigma through having others talk to caregivers rather than directly to them or having others concentrate on the things they can no longer do rather than the things they can do. There are actions people can take to reduce stigma, such as making efforts to include people living with dementia in conversations and activities, treating them with dignity and respect, and encouraging them to share their experiences.
Almost one-quarter (24%) of Canadians work and 20% volunteer or did in the past, in a sector where they may need or have needed to interact with someone living with dementia, suggesting that understanding and enabling dementia-inclusive communities is broadly relevant for many Canadians. Footnote 24 Public opinion research in 2023 is helping to measure progress and deepen our understanding of dementia related stigma in Canada. Footnote 25
Research suggests both a growing awareness of dementia-related stigma in Canada and highlights the need to continue to make efforts to counter negative perceptions. Footnote 26 When asked about their own personal perceptions of people living with dementia, the majority agree that people living with dementia are sometimes able to continue to do a variety of things after diagnosis, such as continuing to be active in their communities (72%), to live in their own home (70%) and to do activities they enjoy (69%). Views on quality of life are more optimistic, as fewer Canadians in 2023 believe that people living with dementia generally face a lower quality of life than people without dementia compared to 2020. However, Canadians are less optimistic about the ability of people living with dementia to continue working for years after the onset of symptoms when compared to 2020 (see Figure 7). Fewer Canadians in 2023 feel at least moderately comfortable interacting with people living with dementia.
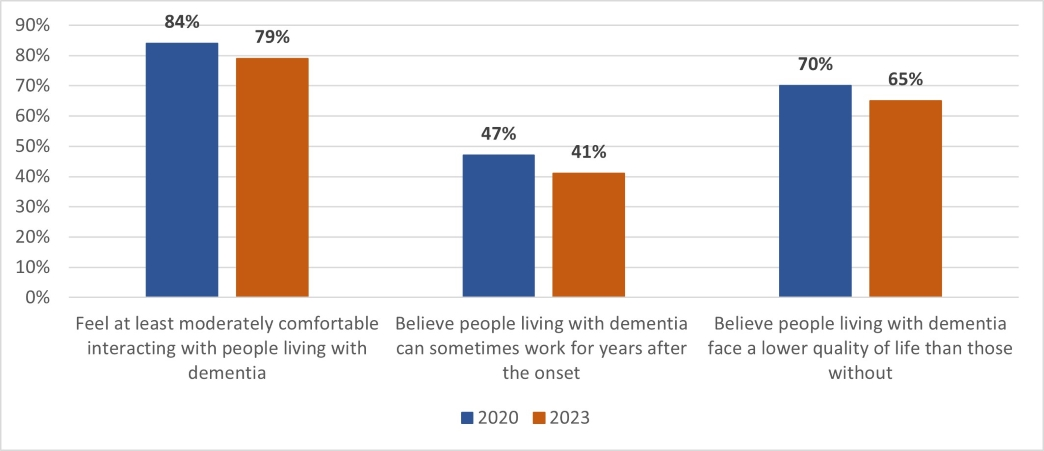
Figure 7 - Text description
- Feel at least moderately comfortable interacting with people living with dementia
- 2020: 84%
- 2023: 79%
- Believe people living with dementia can sometimes work for years after the onset
- 2020: 47%
- 2023: 41%
- Believe people living with dementia face a lower quality of life than those without
- 2020: 70%
- 2023: 65%
Canadians are also less comfortable talking with a health care provider about dementia symptoms in 2023 than in 2020 (see Figures 8 and 9). The level of comfort disclosing a dementia diagnosis to others has also decreased among Canadians since 2020. This suggests a need for more efforts to reduce dementia-related stigma, so that people have the confidence to discuss symptoms with health care providers or seek the information and supports, including social supports, needed to improve their quality of life.
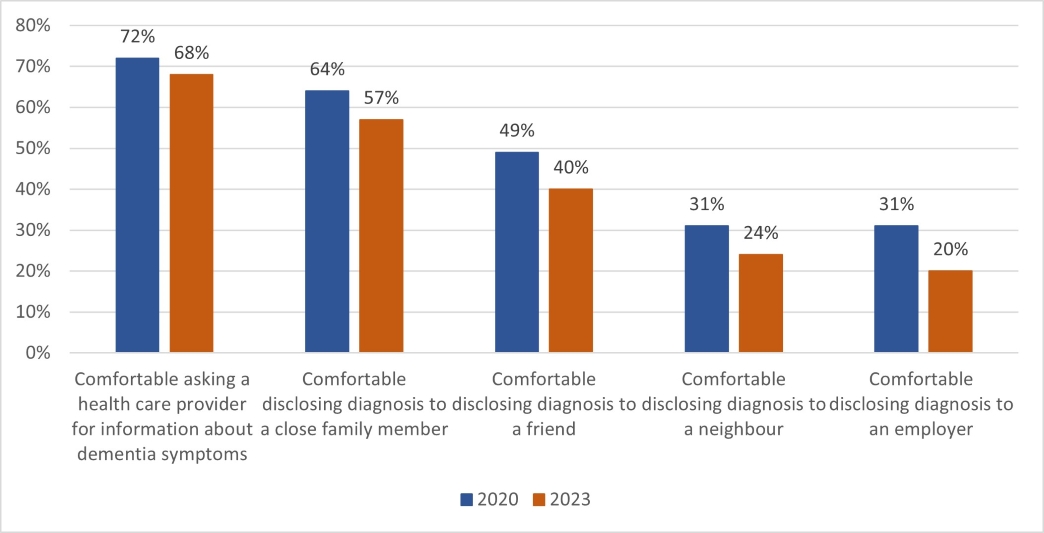
Figure 8 - Text description
- Comfortable asking a health care provider for information about dementia symptoms
- 2020: 72%
- 2023: 68%
- Comfortable disclosing diagnosis to a close family member
- 2020: 64%
- 2023: 57%
- Comfortable disclosing diagnosis to a friend
- 2020: 49%
- 2023: 40%
- Comfortable disclosing diagnosis to a neighbour
- 2020: 31%
- 2023: 24%
- Comfortable disclosing diagnosis to an employer
- 2020: 31%
- 2023: 20%

Figure 9 - Text description
- Concern of what lies ahead: 75%
- Others would treat them differently: 56%
- Lack of trust the health care system will provide proper care: 47%
- Alarming the people close to them: 46%
- Employer may find out / they may have to stop working: 31%
- Feeling that there is no point in knowing as nothing can be done to change progression: 21%
Recent research suggests that dementia is often portrayed negatively in the media and that this may influence perceptions. Footnote 27, Footnote 28 Canadians have mixed views on how accurately dementia is portrayed in popular culture (see Figure 10). Footnote 29 One third (33%) feel the portrayal of dementia is inaccurate, while 18% feel it is accurate. Of those who feel the portrayal is inaccurate, more feel that dementia is portrayed more negatively (60%) than positively (17%) compared to reality.
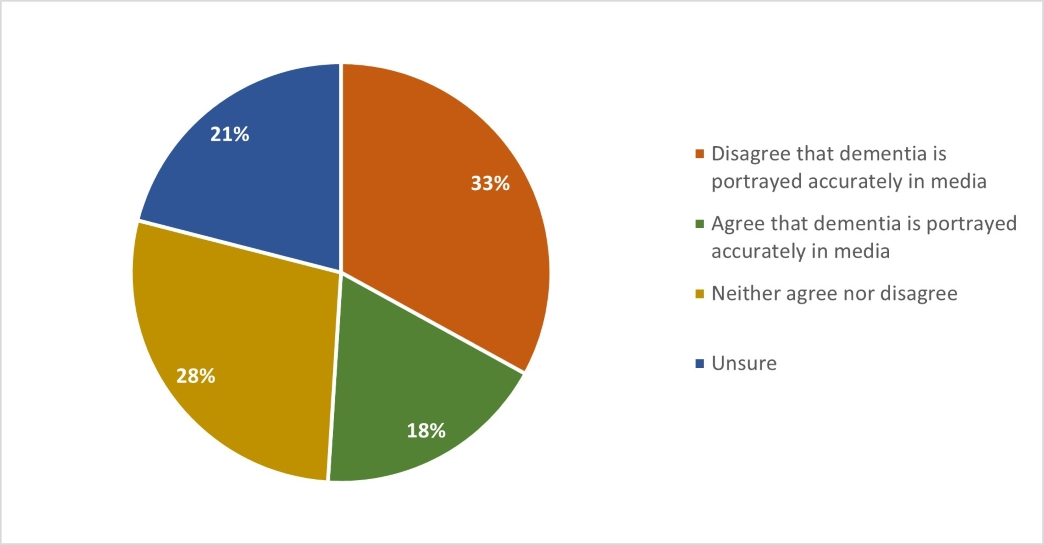
Figure 10 - Text description
- Disagree that dementia is portrayed accurately in media: 33%
- Agree that dementia is portrayed accurately in media: 18%
- Neither agree nor disagree: 28%
- Unsure: 21%
The COVID-19 pandemic may have had a role in amplifying dementia-related stigma on social media since 2020. A study analyzing Twitter between February 15 to September 7, 2020, found many tweets contained stigmatizing language about dementia, with people living with dementia often stereotyped as highly vulnerable people at the end stages of their lives. The study also noted that some tweets challenged stigma by providing accurate facts, highlighting issues faced by people with dementia during the COVID-19 pandemic, or directly confronting dementia-related myths and stereotypes. The findings suggest that dementia education and awareness campaigns need to incorporate a strategy to counter misinformation and disinformation shared through social media. Footnote 30
Canadians were also asked to share their perceptions with regards to how others feel about people living with dementia. Footnote 31 Respondents indicated they believe most Canadians see dementia as resulting in a loss of autonomy and ability, and potentially dangerous behaviour (see Figure 11). More Canadians appear to agree in 2023, that people have negative assumptions about the abilities of people living with dementia, than in 2020. Only around a quarter feel that people in their community are knowledgeable and respectful of people living with dementia (28%) or that people living with dementia can communicate their ideas and wishes to others (24%).
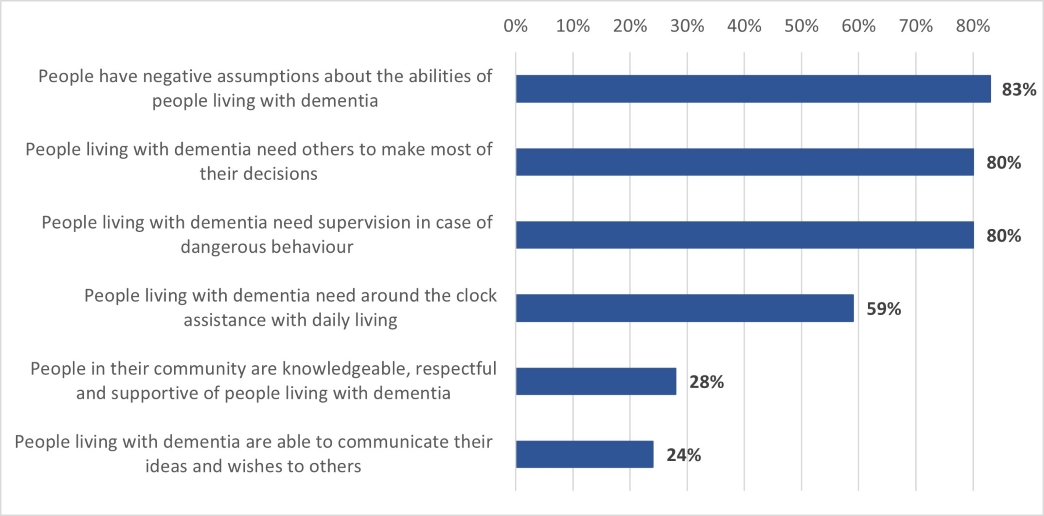
Figure 11 - Text description
- People have negative assumptions about the abilities of people living with dementia: 83%
- People living with dementia need others to make most of their decisions: 80%
- People living with dementia need supervision in case of dangerous behaviour: 80%
- People living with dementia need around the clock assistance with daily living: 59%
- People in their community are knowledgeable, respectful and supportive of people living with dementia: 28%
- People living with dementia are able to communicate their ideas and wishes to others: 24%
The survey also found that close to 75% of the respondents who are unpaid dementia caregivers reported experiencing some challenges related to stigma and how inclusive their community is:
- 51% have experienced people talking to the caregiver and not the person living with dementia
- 45% have had people focus on the things the person living with dementia can no longer do instead of the things they can do
- 20% have experienced difficulty accessing appropriate housing for the person living with dementia
- 17% have encountered accessibility issues that prevent them from going where they need or want to, such as accessible transportation and buildings
- 17% have had difficulty navigating a public space, such as a grocery store, bus or train
In a dementia-inclusive community, measures are in place that make it more possible for people living with dementia to protect and improve their health and wellbeing, live independently, safely navigate and access local activities, and maintain social networks.
Experiences of those living in Official Language Minority Communities (OLMCs) with dementia-inclusiveness
Public opinion research with individuals living in OLMCs Footnote 32 found a significant lack of awareness of dementia-inclusive communities, highlighting a need for more public education. Once a definition was provided, participants generally reported that their own communities were not dementia-inclusive. Very few were aware of programs or services available to people living with dementia within their communities.
Some participants believed that dementia is something communities are trying to avoid or forget about, rather than embrace, and doubted whether people in the community would want to volunteer to make the community more dementia-inclusive, citing that even close relatives struggled to support someone with dementia.
« La démence n'est pas quelque chose dont les gens aiment parler. C'est quelque chose qui fait peur. […] Il y a des gens que je connaissais au collège qui me connaissaient bien et ils ont appris ça de bouche à oreille, des choses se répandent quand on ne le veut pas et ils ne me regardent plus jamais de la même façon. » ["Dementia is not something people like to talk about. It can be scary. […] People I knew in college and who knew me well heard about it from word-of-mouth, news goes around even when we don't want it to, and they don't look at me the same now."]
Interviews with people living with dementia in OLMCs found that some had cut back on social activities after diagnosis because they did not want to take any unnecessary risks in public or they did not feel like being around other people. Some barriers to accessing activities specifically intended for people living with dementia in their communities included:
- limited interest in participating in activities available;
- lack of awareness of activities; and,
- concern about the impact of deteriorating language skills on the ability to participate.
Those who might be interested in programming tailored to people living with dementia, noted that activities would need to be in a judgement-free and open-minded environment that is close to home. The types of activities of interest to participants living with dementia included music lessons, physical activity (e.g., weightlifting, yoga, swimming), reading rooms, park visits, outdoor cafes, and group classes such as cooking and knitting. They also indicated interest in programs and spaces where the caregiver also has a place to go and something to do while the person living with dementia is participating in an activity.
Conclusion
The national dementia strategy is being supported by federal investments of almost $400M since 2015 in research and innovation, community-based projects, awareness, surveillance, and guidance. While PHAC is leading the implementation of the national dementia strategy, other federal partners, levels of government, and stakeholders from across the country are also undertaking many activities that directly support the objectives of Canada's national dementia strategy.
We thank all those who contributed information in this year's report, including those who participated in PHAC's public opinion research studies. While this report shares just a few of the results, all of the public opinion research conducted on behalf of PHAC can be accessed through Library and Archives Canada.
We also thank the many individuals and organizations across Canada working to support Canada's national dementia strategy and its vision of a Canada in which all people living with dementia and caregivers are valued and supported, quality of life is optimized, and dementia is prevented, well understood and effectively treated.
If you would like to receive communications about the national dementia strategy and funding opportunities or provide information about relevant dementia-related activities, please contact the PHAC Dementia Policy Secretariat.
Appendices
Appendix A: Map of projects distributed across the country
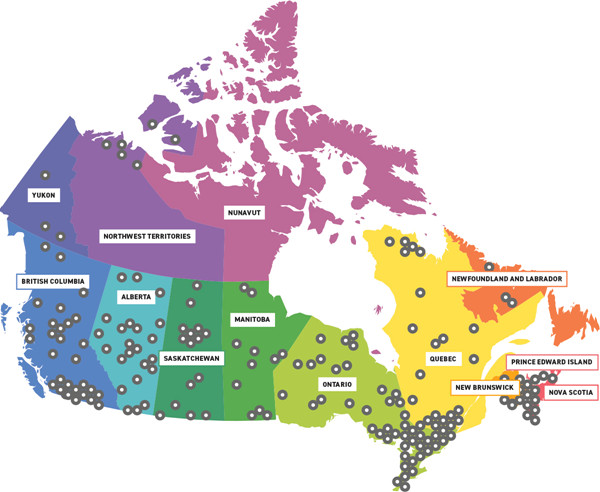
Figure A - Text description
Map of Canada with indicators on provinces/territories where PHAC has invested in a project (numbers seen in table 1 below).
| Total projects funded | National projects | Provincial projects | Number of project sites | |
|---|---|---|---|---|
| DSF | 36 | 17 | 19 | 70 |
| DCI | 25 | 4 | 21 | 81 |
| EDSI | 15 | 5 | 10 | 33 |
| Total | 76 | 26 | 50 | 184 |
| NL | PEI | NS | NB | QC | ON | MB | SK | AB | BC | YT | NWT | NU | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| DSF | 2 | 1 | 2 | 2 | 4 | 14 | 2 | 11 | 18 | 12 | 2 | 0 | 0 |
| DCI | 0 | 0 | 3 | 6 | 13 | 23 | 9 | 2 | 2 | 14 | 0 | 6 | 0 |
| EDSI | 1 | 1 | 2 | 2 | 6 | 8 | 2 | 2 | 3 | 5 | 1 | 0 | 0 |
| Total | 3 | 2 | 7 | 10 | 23 | 45 | 13 | 14 | 23 | 31 | 3 | 6 | 0 |
Appendix B: List of project titles
Note: Projects marked with an asterisk (*) indicate that they are national in scope
Dementia Strategic Fund (DSF) projects
Awareness Raising Initiatives
- Abécédaire d'un cerveau en santé – Sensibilisation à la démence dans l'Ouest et le Nord (La Société Réso Santé Colombie-Britannique)
- Acquainting Canadian Seniors with State of the Art Dementia Prevention Strategies: Up Close and Personal (Cyber-Seniors: Connecting Generations)
- Addressing Dementia Stigma (ADS) and Inclusiveness in Small Rural Communities (City of Vernon)
- Addressing Stigma and Supporting Living Well for Persons Living with Dementia and Care Partners: The Forward with Dementia Initiative (Schlegel-UW Research Institute for Aging Foundation)
- *Améliorer le programme Luci et le déployer à plus large échelle pour toucher une population diversifiée (Luci-3) (Lucilab Inc.)
- Apna Mind, Apna Body – Dementia Awareness in South Asians (Indus Community Services)
- Artful Moments: Shared Learning (Art Gallery of Hamilton)
- Awareness Builds Connections in Dementia-Friendly Communities (ABCD Initiative) (Alberta Rural Development Network)
- Culturally-Appropriate Dementia Awareness and Education Project for Diverse Immigrant Communities (S.U.C.C.E.S.S.)
- *Curating, designing, and disseminating co-designed knowledge products to raise awareness about dementia prevention (The Baycrest Academy for Research and Education in the Baycrest Centre for Geriatric Care)
- Dementia-Inclusive Streets and Community Access, Participation, and Engagement (DemSCAPE) (Simon Fraser University)
- *Dementia Prevention Internet-Based Intervention: Randomized Controlled Trial and Knowledge Translation (McMaster University)
- *Dementia Supporter (Volunteer) Training and Making Support Network Titled Team Orange in Each Japanese / Japanese Canadian Community (Japanese Medical Support Network in Canada)
- *Luci : une application mobile personnalisée, accompagnée par un entraîneur, servant à adopter et à conserver des habitudes de vie saine pour réduire le risque de la démence chez les personnes d'âge moyen et les jeunes aînés présentant des facteurs de risque modifiables (Lucilab Inc.)
- Mesures visant à prévenir ou combattre la stigmatisation des personnes âgées atteintes de démence dans leurs collectivités et promouvoir leur inclusion (Cégep de Drummondville)
- *Mind Over Matter®– A Comprehensive Brain Health Awareness Campaign (Women's Brain Health Initiative)
- Open Minds, Open Hearts (Conestoga College Institute of Technology and Advanced Learning)
- Partnering for Dementia Friendly Communities (Department of Health and Community Services, Newfoundland and Labrador)
- *Please Be Patient: I'm Still me (Brella Community Services Society)
- *Promoting Dementia Awareness in Intergenerational Programming in Canada (Families Canada)
- Reducing dementia-related stigma by using person-centred language to describe responsive behaviours in hospital admissions (Regional Geriatric Program of Toronto)
- Sharing Dance with People with Dementia (Canada's National Ballet School)
- *Stigma: An Exploration of Lived Experience, Understandings and Behaviours of Dementia within Indigenous Communities (Native Women's Association of Canada)
- *Strengthening Chosen Family – Dementia Awareness and Inclusivity in the 2SLGBTQI+ Community (Egale Canada)
- Stronger Together: Making Ottawa and Renfrew County Dementia Inclusive (Dementia Society of Ottawa and Renfrew County)
Dementia Guidelines and Best Practices Initiative
- *Best Practice Directions in Indigenous-Centred Dementia Care (The Governors of the University of Calgary)
- *Best Practice Resource Hub on the Identification, Assessment and Management of Behavioural and Psychological Symptoms of Dementia for Health Care Providers and People Living with Dementia (Canadian Coalition for Seniors' Mental Health through the Canadian Academy of Geriatric Psychiatry)
- *Bonifier et élargir l'accès à des conseils de qualité par la personnalisation du parcours et des contenus mutimédias dans le programme numérique Luci visant à prévenir la démence chez les personnes à risque (Luci-2) (Lucilab Inc.)
- *Canadian Best Practice Guidance for Quality Community Supports and Care for Adults with Intellectual Disabilities and Dementia and Their Caregivers (Reena)
- *Creation of National Dementia Guidelines and Best Practices for Person-Centred Communication and Care: A Culture-First Approach (Alzheimer Society of Canada)
- Cultural Adaptation of MINT Memory Clinics: Improving Equitable Access to High-Quality Dementia Guidance for Older Canadians (Centre for Family Medicine Family Health Team)
- Dementia Guidelines for Regional and Indigenous Populations in Northern British Columbia: Consultation, Calibration, and Creation of Community and College Curricula (College of New Caledonia)
- Emotion-Based Dementia Care Training for First Responders (Regional Municipality of Peel)
- *IncludeMeTM Dementia Edition for Caregivers: The engaging, interactive and transformative educational experience that prepares Canadians facing caregiver responsibilities for someone diagnosed with Dementia (Iris the Dragon)
- Maamwesying North Shore Community Health Services Indigenous-Led Collaborative Community-Based Memory Clinics (Maamwesying North Shore Community Health Services)
- *Online Dementia Guidance Resource Hub for Chinese Communities in Canada (Yee Hong Centre for Geriatric Care)
Dementia Community Investment (DCI) projects
Emerging Stream – Projects are based on some evidence (e.g., with theoretical underpinnings); funding is used to develop, implement and evaluate the intervention.
- Building Capacity for Meaningful Participation by People Living with Dementia (University of British Columbia)
- Ce qui nous lie ~ What connects us: A mixed methods ethnography to evaluate an intersectoral participatory approach for sustainable community-based initiatives to destigmatize dementia (CIUSSS du Centre-Ouest-de-L'île de Montréal)
- Community-based music intervention as a means to enhance health and wellbeing of people living with dementia and bring support to their family and caregivers (University of Ottawa)
- Cummings Centre Therapeutic Dementia Care Program (Cummings Jewish Centre for Seniors)
- Dementia Dialogue Podcast Network (Lakehead University)
- *Dementia-Friendly Canada (Alzheimer Society of Canada)
- Dementia Lifestyle Intervention for Getting Healthy Together (DELIGHT) (University of Waterloo)
- Des collectivités en soutien à la trajectoire de vie des personnes allochtones et autochtones atteintes de démence (Centre de recherche sur le vieillissement de Sherbrooke)
- Ethno-Cultural and Linguistically Based Support Services to People Living with Dementia (COSTI Immigrant Services)
- Empowering Dementia Friendly Communities – Hamilton and Haldimand (Hamilton Council on Aging)
- Intergenerational and Mobile In-Community Interventions to Support People Living with Dementia and those at risk (Cape Breton University)
- Inuvialuit Settlement Region Dementia Awareness and Intervention (Inuvialuit Regional Corporation)
- L'approche par le plaisir en milieu communautaire : créer des environnements accueillants pour les personnes avec des atteintes cognitives (Société Alzheimer de Granby et région)
- Living with Dementia in Rural First Nations Communities: A Health and Wellness Project (University of Manitoba)
- New Brunswick Dementia Friendly Initiative (The New Brunswick Association of Nursing Homes)
- *Supporting a Circle of Care: A Culturally Informed Support Group and Toolkit for Indigenous Caregivers of People Living with Dementia (Native Women's Association of Canada)
- Supporting Family Caregivers of Persons Living with Dementia: Effectiveness and Sustainability of My Tools 4 Care-In Care (University of Alberta)
- *The Integration, Optimization and Promotion of Inclusive Approaches for 2SLGBTQI+ People Living With Dementia and their Caregivers (Egale Canada)
Advanced Stream – Projects that have been previously assessed and found to have a strong evidence of effectiveness; funding is used to support scale up and expansion of reach to new populations/jurisdictions/sectors.
- Enhancing Minds in Motion®as a Virtual Program Delivery Model for People Living with Dementia and Their Care Partners (Alzheimer Society of Ontario)
- Evaluating co-designed tools for strong partnerships in the dementia care triad (Saint Elizabeth Health Care)
- Implementing Computer Interactive Reminiscing and Conversation Aid in Canada (CIRCA-CA) (University Health Network)
- Mobilizing and Equipping Community Based Organizations to Promote Awareness and Support for Person-Centered Care for People Living with Dementia and their Caregivers (Institute for Health System Transformation and Sustainability)
- Moving, Eating, and Living Well (University of Waterloo)
- Ten Online Modules Over Ten Weeks for Adult Learners (TOTAL) eLearning for Family/Friend Caregivers of Persons Living with Dementia (PLWD) (McGill University)
Knowledge Hub
- *The Canadian Dementia Learning and Resource Network (CDLRN) (Schlegel-UW Research Institute for the Aging)
Enhanced Dementia Surveillance Initiative (EDSI) projects
- A comprehensive and holistic approach to dementia surveillance in Canada (Schlegel-UW Research Institute for Aging)
- *A National Indigenous dementia surveillance initiative – A feasibility study (Part 1) (McMaster University)
- A National Indigenous dementia surveillance initiative – A feasibility study (Part 2) (McMaster University)
- *Ascertaining dementia and surveillance of risk factors in the Canadian Longitudinal Study on Aging (McMaster University)
- Canadian Chronic Disease Surveillance System case capture and dementia prevalence in long-term care settings (Participants: British Columbia, Ontario and Quebec)
- Climate change surveillance for chronic health effects in populations: Enhanced activities focused on dementia (University of Alberta) – Amendment
- *Dementia in long-term care and home care settings: An in-depth data exploration and analysis of the Canadian Institute for Health Information's data holdings (Canadian Institute for Health Information)
- Disease and mortality trajectory among Canadians with dementia (Participants: British Columbia, Ontario, Prince Edward Island and Quebec)
- Exploring linkage opportunities to enrich Canadian Chronic Disease Surveillance System data (Participants: British Columbia and Quebec)
- Health surveillance of community-dwelling, person-with-dementia and caregiver dyads (LIFE Research Institute, University of Ottawa)
- Homelessness Counts: Exploring dementia in people experiencing homelessness (Lawson Health Research Institute) – Amendment
- National Dementia Caregiver Surveillance through First Link®: A Pilot Project (Alzheimer Society of Canada)
- *Population Health Model (POHEM), a microsimulation model for dementia projections (Health Analysis Division, Statistics Canada)
- *The implementation of the 'Canadian Primary Care Sentinel Surveillance Network Data Presentation Tool' in primary care clinics to enhance the surveillance, prevention and management of chronic disease: Phase 3 (Queen's University) – Amendment
- Total and average costs of health care resources utilized by people living with dementia (Ottawa Hospital Research Institute)
Appendix C: Centre for Aging and Brain Health Innovation (CABHI)
From 2015-2021, the Public Health Agency of Canada (PHAC) provided $44 million to Baycrest Health Sciences to launch CABHI and support its work to accelerate innovation in aging and brain health. Budget 2022 provided an additional $30 million in federal funding for CABHI (2022-2025) to help accelerate innovations in brain health and aging.
CABHI has engaged partners and collaborators in most provinces and territories across Canada, including the establishment of partnerships with national organizations such as the Canadian Consortium of Neurodegeneration in Aging (CCNA), Brain Canada, AgeWell, the Seniors Quality LEAP Initiative, and the Alzheimer Society of Canada. CABHI has also formed partnerships with the international innovation consortia and innovators from around the world (e.g., IBM, Quanta, Fuji, Sompo Digital Labs, Berkeley SkyDeck, 500 Startups, and MaRS Innovation). Since its establishment in 2015, CABHI has supported more than 345 projects, including over 275 unique innovative solutions. Some of these innovative solutions include:
- Laser Walk: A device that can be affixed to mobility devices to guide safe walking for those affected by neurological conditions.
- IlluminAid: A motion-detection lighting system that attaches under beds and furniture and enables residents of Long-Term Care (LTC) to use the bathroom or walk out of their rooms more safely.
- MouvMat: An interactive game to promote exercise and socializing among residents in LTC.
Appendix D: Trends in risk factors across Canada
Dementia risk and protective factors among Canadians
The data points below outline the age-standardized Footnote 33 prevalence of known dementia risk and protective factors among Canadians over two time points including the most recently available data. Data is shown between a period of five years (when available) in order to assess a trend. No significant change indicates that the risk or protective factor has not changed in a statistically significant way from one time point to the other.
| Dementia risk or protective factor | Percentage (%) of Canadians with factor (Year 1) | Percentage (%) of Canadians with factor (Year 2) | Trend Footnote 34, Footnote 35 | Source Footnote 36,Footnote 37 |
|---|---|---|---|---|
| % of population (aged 12+) that reports heavy drinkingFootnote 38, Footnote 39 | 19.0 (2016) | 15.6 (2021) | Better | Canadian Community Health Survey (CCHS), 2016; 2021 |
| % of population (aged 20+) that reports having less than a high school educationFootnote 40 | 12.2 (2016) | 8.1 (2021) | Better | CCHS, 2016 (CCDI); Custom tabulations by BELD/CSAR, 2021 |
| % of population (aged 20+) with diagnosed hypertension (high blood pressure) | 24.0 (2014-2015) | 23.1 (2019-2020) | Better | Canadian Chronic Disease Surveillance System (CCDSS), 2014-2015; 2019-2020 |
| % of population (aged 12+) that reports being current smokers (daily or occasional) | 16.9 (2016) | 11.8 (2021) | Better | CCHS, 2016; 2021 |
| % of population (aged 18–79) with elevated blood cholesterol | 18.4 (2014-2015) | 14.0 (2018-2019) | No statistically significant change | Canadian Health Measures Survey (CHMS), 2014-2015; 2018-2019 |
| % of population (aged 18–79) that reports obtaining the recommended amount of daily sleepFootnote 41 | 61.8 (2009-2011) | 64.9 (2014-2015) | No statistically significant change | CHMS, 2009-2011; 2014-2015 |
| % of population (aged 12+) that reports a "very strong" or "somewhat strong" sense of belonging to their local community (social isolation is a dementia risk factor)Footnote 42 | 68.8 (2016) | 69.5 (2021) | No statistically significant change | CCHS, 2016; 2021 |
| % of population (aged 20+) with diagnosed stroke | 2.6 (2014-2015) | 2.6 (2019-2020) | No statistically significant change | CCDSS, 2014-2015; 2019-2020 |
| % of population (aged 20+) with diagnosed diabetes | 10.0 (2014-2015) | 10.4 (2019-2020) | Worse | CCDSS, 2014-15; 2019-20 |
| % of adults (aged 18+) that are living with obesity (self-reported, adjusted BMI) Footnote 43 | 26.5 (2016) | 29.2 (2021) | Worse | CCHS, 2016; 2021 |
| % of population (aged 18+) who report accumulating at least 150 minutes of moderate-to-vigorous physical activity each week, in bouts of 10 minutes or moreFootnote 44, Footnote 45 | 58.5 (2016) | 53.9 (2021) | Worse | CCHS, 2016; 2021 |
Dementia risk and protective factors across Canada
Table 2 shows the levels of dementia risk and protective factors in Canada, broken down by province and territory compared with the overall national average.
| Dementia risk factor | Source Footnote 48,Footnote 49 | National | AB | BC | MB | NB | NFL | NWT | NS | NU | ON | PEI | QC | SK | YK |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % of population (aged 20+) with diagnosed diabetes | CCDSS (2019-2020) |
10.4 | 10.0 | 10.2 | 12.1 | 11.5 | 11.8 | N/A | 10.5 | N/A | 11.4 | 9.9 | 8.6 | 10.7 | 9.5 |
| % of population (aged 12+) that reports heavy drinkingFootnote 50 | CCHS (2021) |
15.6 | 16.0 | 15.1 | 14.6 | 18.9 | 22.8 | N/A | 19.4 | N/A | 14.7 | 19.0 | 15.9 | 16.7 | N/A |
| % of population (aged 20+) that reports having less than a high school educationFootnote 51 | CCHS (2021) |
8.1 | 8.8 | 4.7 | 9.0 | 8.5 | 11.6 | N/A | 8.5 | N/A | 7.1 | 8.9 | 10.7 | 8.6 | N/A |
| % of population (aged 20+) with diagnosed hypertension (high blood pressure) | CCDSS (2019-2020) |
23.1 | 24.7 | 22.1 | 28.2 | 27.2 | 30.2 | N/A | 25.9 | N/A | 23.5 | 23.9 | 19.8 | 25.4 | 21.7 |
| % of population (aged 18+) that are living with obesity (self-reported, adjusted BMI)Footnote 52 | CCHS (2021) |
29.2 | 29.7 | 24.6 | 33.9 | 39.2 | 42.2 | N/A | 37.0 | N/A | 29.3 | 35.9 | 27.6 | 34.6 | N/A |
| % of population (aged 12+) that reports being current smokers (daily or occasional) | CCHS (2021) |
11.8 | 11.5 | 9.6 | 11.1 | 12.4 | 13.4 | N/A | 13.5 | N/A | 11.6 | 14.2 | 13.3 | 12.6 | N/A |
| % of population (aged 20+) with diagnosed stroke | CCDSS (2019-2020) |
2.6 | 2.4 | 2.6 | 2.9 | 2.2 | 2.1 | N/A | 1.9 | N/A | 2.7 | 3.0 | 2.4 | 2.8 | 2.1 |
| Dementia protective factor | Source Footnote 54,Footnote 55 | National | AB | BC | MB | NB | NFL | NWT | NS | NU | ON | PEI | QC | SK | YK |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % of population (aged 18+) that report accumulating at least 150 minutes of moderate-to-vigorous physical activity each week, in bouts of 10 minutes or more Footnote 56, Footnote 57 | CCHS (2021) |
53.9 | 58.0 | 62.4 | 52.8 | 50.6 | 50.3 | N/A | 55.4 | N/A | 51.5 | 51.3 | 51.7 | 52.2 | N/A |
| % of population (aged 12+) that reports a "very strong" or "somewhat strong" sense of belonging to their local community (social isolation is a dementia risk factor)Footnote 58 | CCHS (2021) |
69.5 | 68.3 | 70.9 | 70.5 | 76.7 | 80.5 | N/A | 75.8 | N/A | 69.4 | 78.1 | 66.0 | 76.1 | N/A |
Note: For Tables 2a and 2b, provincial and territorial differences observed with the CCDSS should be interpreted with caution. Even though differences are statistically significant, methodological differences may explain the patterns observed in addition to actual differences in the health status of the populations. For instance, differences in detection and treatment practices, as well as differences in data coding, remuneration models and shadow billing practices likely play a role in the patterns observed.
Endnotes
- Footnote 1
-
Please note that some of the websites this report links to may not have content in both English and French.
- Footnote 2
-
Public Health Agency of Canada. Canadian Chronic Disease Surveillance System (CCDSS), Data Tool 2000–2019, 2021 Edition. Government of Canada. 2023. Available from: https://health-infobase.canada.ca/ccdss/data-tool/Index
- Footnote 3
-
The nominated principal investigator is the grantee on a Canadian Institutes of Health Research funding application responsible for leading the intellectual direction of the proposed activities as well as coordinating the financial and administrative aspects of the grant/award.
- Footnote 4
-
This data point reports on the number of unique nominated principal investigators funded across all of the Canadian Institutes of Health Research's programs, including investigator-initiated research (e.g., funded through the Project Grant competition), research in priority areas (e.g., the Canadian Consortium on Neurodegeneration in Aging), and training and career support programs (e.g., fellowships).
- Footnote 5
-
Parts of these materials are based on data and information provided by the Canadian Institute for Health Information. However, the analyses, conclusions, opinions and statements expressed herein are those of the author and not necessarily those of the Canadian Institute for Health Information. This data was drawn from the Resident Assessment Instrument - Home Care©- Home Care Reporting System, fiscal year 2021-2022. It is representative of people living with dementia receiving home care in British Columbia (all regions except Northern Health), the Yukon, Alberta (except the Calgary Zone), and Newfoundland and Labrador.
- Footnote 6
-
Chi-square tests were applied. Significance level set at 0.05, indicating whether any changes in trends are statistically significant.
- Footnote 7
-
Caregivers who are distressed are defined as primary caregivers who express feelings of distress, anger or depression and/or any caregiver who is unable to continue in their caring activities.
- Footnote 8
-
These data points are from the Yukon, British Columbia, Alberta and Newfoundland and Labrador in 2020–2021.
- Footnote 9
-
Parts of these materials are based on data and information provided by the Canadian Institute for Health Information. However, the analyses, conclusions, opinions and statements expressed herein are those of the author and not necessarily those of the Canadian Institute for Health Information. This data was drawn from the Resident Assessment Instrument - Home Care©- Home Care Reporting System, fiscal year 2021-2022. It is representative of people living with dementia receiving home care in British Columbia (all regions except Northern Health), the Yukon, Alberta (except the Calgary Zone), and Newfoundland and Labrador.
- Footnote 10
-
Chi-square tests were applied. Significance level set at 0.05, indicating that any changes in trends are statistically significant.
- Footnote 11
-
Parts of these materials are based on data and information provided by the Canadian Institute for Health Information. However, the analyses, conclusions, opinions and statements expressed herein are those of the author and not necessarily those of the Canadian Institute for Health Information. This data was drawn from the Resident Assessment Instrument - Home Care©- Home Care Reporting System, fiscal year 2021-2022. It is representative of people living with dementia receiving home care in British Columbia (all regions except Northern Health), the Yukon, Alberta (except the Calgary Zone), and Newfoundland and Labrador.
- Footnote 12
-
The project evaluation was conducted in partnership with KITE Research Institute, Toronto Rehabilitation Institute – University Health Network and Kunin Lunenfeld Centre for Applied Research and Evaluation.
- Footnote 13
-
Emerging findings from Canadian Institute of Health Information used a cohort of persons living with dementia who had their first community encounter for dementia in 2017-2018, across three provinces where this data was available, to describe the care journey and potential predictors for transitions.
- Footnote 14
-
Preliminary data from Nanos Research's Stigma Related to Dementia in Canada for the Public Health Agency of Canada.
- Footnote 15
-
For further information (such as, methods, geographic coverage, and margin of error), please refer to the publications on the Library and Archives Canada site.
- Footnote 16
-
Preliminary data from Nanos Research's Stigma Related to Dementia in Canada for the Public Health Agency of Canada.
- Footnote 17
-
Ekos Research Associates Inc. for the Public Health Agency of Canada. Survey of Canadians Regarding Dementia Prevention: Final Report. Government of Canada. 2022. Available from: https://publications.gc.ca/site/eng/9.915265/publication.html
- Footnote 18
-
Preliminary data from Nanos Research's Stigma Related to Dementia in Canada for the Public Health Agency of Canada.
- Footnote 19
-
In 2020, the medical journal the Lancet reported that 12 potentially modifiable risk factors account for approximately 40% of dementia cases worldwide, each at different life stages. This report and other related research findings help to provide insight into how Canadians may be able to reduce their risk of developing dementia at all stages of life (https://doi.org/10.1016/S0140-6736(20)30367-6).
- Footnote 20
-
Swinnen N, Vandenbulcke M, de Bruin ED, Akkerman R, Stubbs B, Firth J, Vancampfort D. The efficacy of exergaming in people with major neurocognitive disorder residing in long-term care facilities: a pilot randomized controlled trial. Alzheimers Res Ther. 2021 Mar 30;13(1):70. Available from: https://doi.org/10.1186/s13195-021-00806-7
- Footnote 21
-
Ekos Research Associates Inc. for the Public Health Agency of Canada. Survey of Canadians Regarding Dementia Prevention: Final Report. Government of Canada. 2022. Available from: https://publications.gc.ca/site/eng/9.915265/publication.html
- Footnote 22
-
Livingston G, Huntley J, Sommerlad A, Ames D, Ballard C, Banerjee S, Brayne C, Burns A, Cohen-Mansfield J, Cooper C, Costafreda SG, Dias A, Fox N, Gitlin LN, Howard R, Kales HC, Kivimäki M, Larson EB, Ogunniyi A, Orgeta V, Ritchie K, Rockwood K, Sampson EL, Samus Q, Schneider LS, Selbæk G, Teri L, Mukadam N. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet. 2020 Aug 8;396(10248):413-446. Available from: https://doi.org/10.1016/S0140-6736(20)30367-6
- Footnote 23
-
The Public Health Agency of Canada conducted public opinion research in 2022 focused on dementia and Official Language Minority Communities to gain a deeper understanding of their knowledge, experiences, and attitudes related to dementia prevention and dementia-inclusiveness and to what extent these differ from the general population in Canada. This research was conducted through focus groups with members of the general public, as well as interviews with people living with dementia and caregivers, from either English speaking communities within Quebec, or French speaking communities outside of Quebec (https://epe.lac-bac.gc.ca/100/200/301/pwgsc-tpsgc/por-ef/public_health_agency_canada/2022/128-21-e/POR128-21-FINAL-EN.pdf).
- Footnote 24
-
Preliminary data from Nanos Research's Stigma Related to Dementia in Canada for the Public Health Agency of Canada.
- Footnote 25
-
The 2023 public opinion research on stigma survey is comprised of 4,689 Canadians, 18 years of age and older, including 1,516 self-identified caregivers (defined as someone who provides or has provided unpaid care and support to someone living with dementia in the last five years). Caution should be used when comparing the 2023 results against the results of the 2020 baseline survey, which included a smaller sample of 938 caregivers and did not distinguish between paid and unpaid caregivers.
- Footnote 26
-
Preliminary data from Nanos Research's Stigma Related to Dementia in Canada for the Public Health Agency of Canada.
- Footnote 27
-
Sm-Rahman A, Lo CH, Jahan Y. Dementia in Media Coverage: A Comparative Analysis of Two Online Newspapers across Time. Int J Environ Res Public Health. 2021 Oct 8;18(19):10539. Available from: https://doi.org/10.3390/ijerph181910539
- Footnote 28
-
Low LF, Purwaningrum F. Negative stereotypes, fear and social distance: a systematic review of depictions of dementia in popular culture in the context of stigma. BMC Geriatr. 2020 Nov 17;20(1):477. Available from: https://doi.org/10.1186/s12877-020-01754-x
- Footnote 29
-
Preliminary data from Nanos Research's Stigma Related to Dementia in Canada for the Public Health Agency of Canada.
- Footnote 30
-
Bacsu JD, Fraser S, Chasteen AL, Cammer A, Grewal KS, Bechard LE, Bethell J, Green S, McGilton KS, Morgan D, O'Rourke HM, Poole L, Spiteri RJ, O'Connell ME. Using Twitter to Examine Stigma Against People With Dementia During COVID-19: Infodemiology Study. JMIR Aging. 2022 Mar 31;5(1):e35677. Available from: https://doi.org/10.2196/35677
- Footnote 31
-
Preliminary data from Nanos Research's Stigma Related to Dementia in Canada for the Public Health Agency of Canada.
- Footnote 32
-
Quorus Consulting Group Inc. for the Public Health Agency of Canada. Official Language Minority Communities and Dementia: Final Report. Government of Canada. 2022. Available from: https://epe.lac-bac.gc.ca/100/200/301/pwgsc-tpsgc/por-ef/public_health_agency_canada/2022/128-21-e/POR128-21-FINAL-EN.pdf
- Footnote 33
-
Age-standardized rates account for the differences in the age structure of the populations being compared. In the calculation of the age-standardized rate, either one population is mathematically adjusted to have the same age structure as the other; or both populations are mathematically adjusted to have the same age structure as a third population, called the standard population. In this way, the two groups are given the same age distribution structure so that a more representative picture of the characteristic in question is provided (https://www.statcan.gc.ca/en/dai/btd/asr).
- Footnote 34
-
For Canadian Community Health Survey data: Significant differences for these indicators are based on 95% confidence intervals (i.e., "better" or "worse" if confidence intervals between two points do not overlap AND "no significant change" is confidence intervals overlap between two data points. Please note that data interpretation of significant differences based on confidence intervals is a conservative approach. The current table includes an estimate using the most recent data available (e.g., Canadian Community Health Survey 2021 for alcohol heavy drinking, education, smoking, and community belonging).
- Footnote 35
-
For Canadian Chronic Disease Surveillance System data: Trend analyses were calculated using the Joinpoint software, which tests the statistical significance of the trend over different time periods (P ≤.05). A statistically increasing trend was labelled as 'worse' and on the contrary, a statistically decreasing trend was labelled as 'better'. If the trend was not statistically significant (P >.05), it was reported as 'no significant change'.
- Footnote 36
-
Statistics Canada. Table 13-10-0096-01 Health characteristics, annual estimates. Government of Canada. 2023. Available from: https://doi.org/10.25318/1310009601-eng
- Footnote 37
-
Public Health Agency of Canada. Canadian Chronic Disease Surveillance System (CCDSS), Data Tool 2000–2019, 2021 Edition. Government of Canada. 2023. Available from: https://health-infobase.canada.ca/ccdss/data-tool/Index
- Footnote 38
-
Heavy alcohol drinking is defined as binge drinking (i.e., five or more drinks for males and four or more drinks for females, on a single occasion) at least once a month in the past year.
- Footnote 39
-
Both numbers are exact from Statistics Canada (crude estimates).
- Footnote 40
-
All rates are age-standardized to the 2011 Canadian population. All data from the Canadian Community Health Survey and Canadian Health Measures Survey are representative of Canada, excluding the territories. There are other exclusions in the Canadian Community Health Survey that limit its generalizability: "persons living on reserves and other Aboriginal settlements in the provinces; full-time members of the Canadian Forces; the institutionalized population, children aged 12-17 that are living in foster care, and persons living in the Quebec health regions of Région du Nunavik and Région des Terres-Cries-de-la-Baie-James."
- Footnote 41
-
All rates are age-standardized to the Canadian population. All data from the Canadian Community Health Survey and Canadian Health Measures Survey are representative of Canada, excluding the territories.
- Footnote 42
-
Sense of belonging to a local community illustrates the social attachment of individuals with communities. Social isolation tends to be detrimental to health, while social engagement and attachments are associated with positive health outcomes (both physical and mental).
- Footnote 43
-
Obesity among adults is defined as a body mass index ≥ 30.0 kg/m2. This indicator is based on self-reported weight and height. Body mass index calculations are adjusted to respondent bias to more closely approximate measured values. Pregnant women excluded.
- Footnote 44
-
This physical activity measure uses self-reported data from the Canadian Community Health Survey. Self-reported estimates of physical activity, which report perceived time, are often significantly higher than device-based measures, which measure actual movement. Self-report and device-measured data provide complementary information about different aspects of physical activity but should not be used interchangeably.
- Footnote 45
-
Numbers come from Statistics Canada - crude rates: Although in surveillance we continue recommending using measured data from Canadian Health Measures Survey (also note that the physical activity recommendations within the Canadian 24-H Movement Guidelines changed in 2020 to "without bouts"), we recognize that self-reported data (currently only available "with bouts") as presented in this indicator is still useful to examine trends in particular pre and during COVID.
- Footnote 46
-
Provincial and territorial data for blood cholesterol and daily sleep are not available.
- Footnote 47
-
Territorial estimates based on the 2021 Canadian Community Health Survey are unavailable. Data are only representative in the territories after two years of data collection. The latest estimates for territories come from the 2019-2020 Canadian Community Health Survey (https://doi.org/10.25318/1310011301-eng). The next territorial estimates will come from the 2021-2022 Canadian Community Health Survey.
- Footnote 48
-
Statistics Canada. Table 13-10-0096-01 Health characteristics, annual estimates. Government of Canada. 2023. Available from: https://doi.org/10.25318/1310009601-eng
- Footnote 49
-
Public Health Agency of Canada. Canadian Chronic Disease Surveillance System (CCDSS), Data Tool 2000–2019, 2021 Edition. Government of Canada. 2023. Available from: https://health-infobase.canada.ca/ccdss/data-tool/Index
- Footnote 50
-
Heavy alcohol drinking is defined as binge drinking (i.e., five or more drinks for males and four or more drinks for females, on a single occasion) at least once a month in the past year.
- Footnote 51
-
All rates are age-standardized to the 2011 Canadian population.
- Footnote 52
-
Obesity among adults is defined as a body mass index ≥ 30.0 kg/m2. This indicator is based on self-reported weight and height. Body mass index calculations are adjusted to respondent bias to more closely approximate measured values. Pregnant women excluded.
- Footnote 53
-
Territorial estimates based on the 2021 Canadian Community Health Survey are unavailable. Data are only representative in the territories after two years of data collection. The latest estimates for territories come from the 2019-2020 Canadian Community Health Survey (https://doi.org/10.25318/1310011301-eng). The next territorial estimates will come from the 2021-2022 Canadian Community Health Survey.
- Footnote 54
-
Statistics Canada. Table 13-10-0096-01 Health characteristics, annual estimates. Government of Canada. 2023. Available from: https://doi.org/10.25318/1310009601-eng
- Footnote 55
-
Public Health Agency of Canada. Canadian Chronic Disease Surveillance System (CCDSS), Data Tool 2000–2019, 2021 Edition. Government of Canada. 2023. Available from: https://health-infobase.canada.ca/ccdss/data-tool/Index
- Footnote 56
-
This physical activity measure uses self-reported data from the Canadian Community Health Survey. Self-reported estimates of physical activity, which report perceived time, are often significantly higher than device-based measures, which measure actual movement. Self-report and device-measured data provide complementary information about different aspects of physical activity but should not be used interchangeably.
- Footnote 57
-
Numbers come from Statistics Canada - crude rates: Although in surveillance we continue recommending using measured data from Canadian Health Measures Survey (also note that the physical activity recommendations within the Canadian 24-H Movement Guidelines changed in 2020 to "without bouts"), we recognize that self-reported data (currently only available "with bouts") as presented in this indicator is still useful to examine trends in particular pre and during COVID.
- Footnote 58
-
Sense of belonging to a local community illustrates the social attachment of individuals with communities. Social isolation tends to be detrimental to health, while social engagement and attachments are associated with positive health outcomes (both physical and mental).
Page details
- Date modified:
