Rabies vaccines: Canadian Immunization Guide
For health professionals
Updated: January 2015
On this page
- Key Information
- Epidemiology
- Preparations Authorized for Use in Canada
- Efficacy, Effectiveness and Immunogenicity
- Recommendations for Use
- Vaccine Administration
- Serologic Testing
- Storage Requirements
- Simultaneous Administration with Other Vaccines
- Vaccine and Immunoglobulin Safety and Adverse Events
- Other Considerations
- Selected References
Key information (refer to text for details)
- What
-
- Rabies is a rare viral central nervous system infection most often transmitted to humans through the bite of an infected mammal.
- Transmission of rabies from salivary contamination of scratches, broken skin or the mucous membranes without a bite is rare.
- Pre-exposure immunization for high risk persons produces rabies neutralizing antibodies.
- Post-exposure prophylaxis is highly effective in preventing rabies.
- Adverse reactions for rabies vaccines include injection site reactions, such as pain, erythema, swelling and itching.
- Who
-
- Pre-exposure immunization is given to people at high risk of close contact with rabid animals or the rabies virus (e.g., people with occupational exposure to animals; laboratory workers handling the rabies virus; certain travellers; hunters and trappers in areas with confirmed rabies; and spelunkers).
- Evaluation of an individual's need for post-exposure prophylaxis includes risk assessment related to the exposure to the potentially rabid animal.
- How
-
- Pre-exposure immunization: three 1.0 mL intramuscular (IM) or 0.1 mL intradermal (ID) doses of rabies vaccine given on days 0, 7 and any time between days 21 to 28. Rabies vaccine must never be given into the gluteal muscle due to the risk of a decreased immune response.
- Post-exposure management requires consideration of: the exposure to the potentially rabid animal; management of the potentially rabid animal; and management of the exposed person.
- If indicated, initiate post-exposure prophylaxis as soon as possible but administer regardless of the time interval since exposure. Post-exposure prophylaxis of immunocompetent persons who have not been previously immunized with rabies vaccine consists of: local wound treatment; rabies immunoglobulin (20 IU/kg body weight) given on day 0 with as much as possible infiltrated into and around the wound; and four 1.0 mL IM doses of rabies vaccine given on days 0, 3, 7 and 14. In those who have not previously been immunized, and either are immunocompromised or are taking antimalarial drugs, a fifth dose of vaccine should be given on day 28.
- Post-exposure prophylaxis of persons previously appropriately immunized with rabies vaccine consists of: local wound treatment and two 1.0 mL IM doses of rabies vaccine given on days 0 and 3. Rabies immunoglobulin should not be given to persons who have previously received appropriate rabies vaccinations.
- Vaccination schedules for post-exposure prophylaxis should be adhered to as closely as possible; it is essential that all doses be received. Post-vaccination serology is recommended: after pre-exposure immunization using the ID route; following immunization of immunocompromised individuals or people taking chloroquine; or if there has been a significant deviation from the recommended vaccination schedule.
- Why
-
- Human rabies occurs very rarely in Canada, but if not prevented, is almost always fatal once symptoms develop. Recent cases have been due to bat exposures.
- Pre-exposure immunization and post-exposure prophylaxis result in antibodies that prevent the virus from entering the peripheral nervous system.
Epidemiology
Disease description
Infectious agent
Rabies virus is a ribonucleic acid (RNA) virus of the Rhabdoviridae family. There are different antigenic variants of rabies virus distinguished by laboratory testing. Specific variants tend to occur in specific species of mammals, although these variants can be found in other mammalian species as well. The virus is easily killed by sunlight, soap and drying.
Reservoir
Rabies is a disease of mammals, both domestic and wild. Dogs are the main carriers of the disease in Asia and Africa. In Canada and the US, foxes, skunks, raccoons and bats may be reservoirs capable of transmitting infection to dogs, cats, livestock and people.
Transmission
Rabies is spread to humans when virus in the saliva of an infected animal enters through a bite, scratch, broken skin, the mucous membranes or the respiratory tract. The virus then gains access to the central nervous system through peripheral nerves. Bites from an infected animal are the main route of exposure. Transmission also occurs through transplantation of organs from undiagnosed infected persons. The usual incubation period is proportional to the distance from the portal of entry to the brain, and may vary from several days to years (most commonly 3 to 8 weeks).
Risk factors
People who work in close contact with animals, such as veterinarians and veterinary staff, animal control and wildlife workers, and laboratory workers who handle the rabies virus are at higher risk for exposure to rabies. Individuals who engage in activities such as hunting and trapping or cave exploration (spelunkers) that place them in close contact with potentially rabid animals, such as bats, foxes, skunks and raccoons, in areas where rabies is found, may also be considered at higher risk of rabies exposure.
Children are considered at higher risk for exposure to rabies because they may be more likely to approach animals and are less likely to report bites or scratches. Additionally, children may be more likely to be bitten on the face which carries a higher risk of infection and bites to children can be severe.
Risk to travellers varies depending on itinerary, purpose and duration of the trip, as well as activities and access to medical care.
Spectrum of clinical illness
Rabies is an almost always fatal viral infection of the central nervous system. Early symptoms of rabies may include headache, malaise, fever and fatigue. There may be discomfort or pain at the exposure site (i.e., the site where the person was bitten). Symptoms progress quickly as the central nervous system is attacked, and the illness generally presents in one of two ways. The more common, agitated (furious) form presents with the classic symptoms of hydrophobia and aerophobia (severe laryngeal or diaphragmatic spasms and a sensation of choking when attempting to drink or when air is blown in the face) with a rapidly progressing encephalitis and death. The paralytic form of the disease manifests in progressive flaccid paralysis, has a more protracted course, and is more difficult to diagnose. A more detailed description of the clinical signs of rabies in animals is available at: Fact Sheet: Rabies.
Disease distribution
Incidence/prevalence of human rabies
Global
Rabies occurs worldwide, although most human deaths occur in Asia and Africa. In recent years, bat-related rabies has become the most important public health concern for rabies in the Americas and the Caribbean. A map of the areas where rabies transmission occurs is available from the World Health Organization (WHO) website: Rabies countries or areas at risk.
National
Human rabies occurs very rarely in Canada. Between 1924 and 2009, 24 people in six provinces died of rabies (Figure 1): Quebec (12), Ontario (6), Saskatchewan (2), Alberta (2), British Columbia (1) and Nova Scotia (1). The three most recent human cases in Canada were bat-related; the cases occurred in Quebec in 2000, British Columbia in 2003 and Alberta in 2007.
Rabies incidence rates are similar in Canada and the US and are reported in cases per billion person-years because of the extremely low number of cases. Between 1990 and September 2007, 36 bat-related human rabies cases were identified in Canada (3 cases) and the US (33 cases), resulting in an incidence rate of 6.7 cases per billion person-years. Of these 36 bat-related human cases, the types of exposures reported were as follows:
- Direct contact with a bat: 52.8%
- With recognized bite: 27.8%
- Without recognized bite: 25%
- History of household exposure to a bat: 16.7%
- No history of exposure to a bat: 30.5%
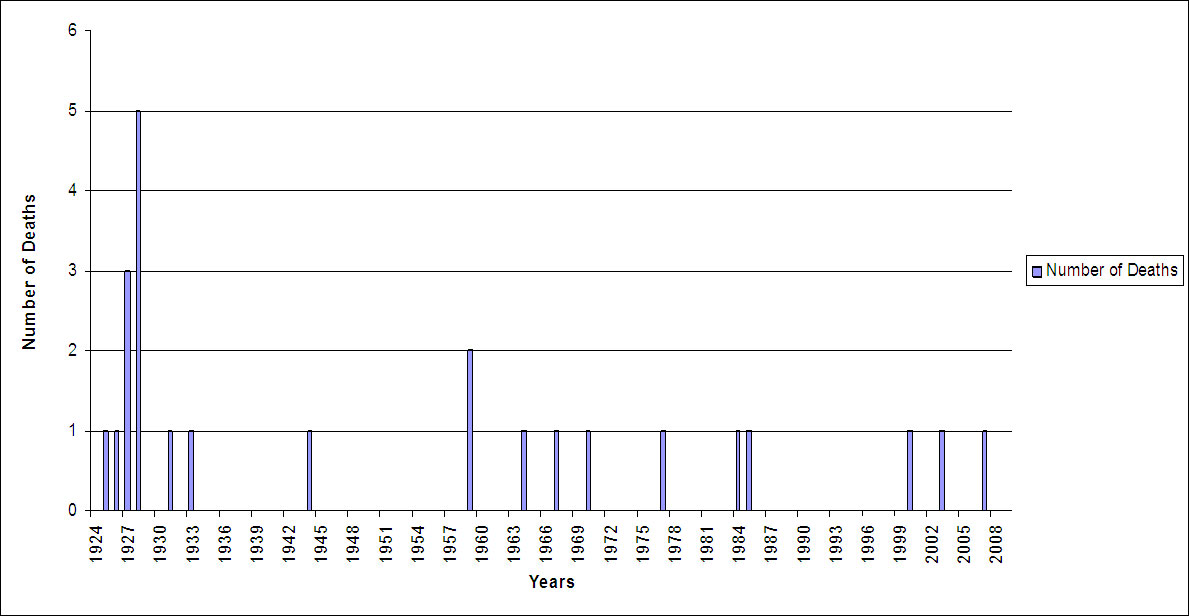
Figure 1: Rabies - Number of Deaths in Canada, 1924-2009: Text description
This is a histogram that identifies that there was one death from rabies in 1925, 1926 1931, 1933, 1944, 1964, 1967, 1970, 1977, 1984, 1985, 2000, 2003, 2007.
There were two deaths in 1959, three deaths in 1927 and five deaths in 1928. The rest of the years there were no reported deaths from rabies. The last reported death was in 2007.
Incidence/prevalence of animal rabies
Rabies testing of animals is carried out mainly when there has been a possible exposure involving a human or other animal, or for special studies. Therefore, the incidence and prevalence data for animal rabies are influenced by the likelihood that an animal will have these types of encounters in the different jurisdictions, and that the animal will be captured and submitted for testing. The number of rabid animals detected in Canada has decreased considerably from 670 in 2000 to 145 in 2009. Part of this decline is related to wildlife rabies control measures, such as oral rabies vaccinations delivered through baiting programs and trap-vaccinate-release programs.
There are regional differences in the prevalence of animal rabies and the specific species infected in each region vary over time. Therefore, it is important for health care providers to consult local public health departments regarding local epidemiology and for public health officials to remain current, based on information from the Canadian Food Inspection Agency (CFIA) website: Positive Rabies in Canada
Between 2006 and 2010, a total of 1005 cases of confirmed animal rabies were reported in Canada. Four provinces accounted for the majority of these cases: Ontario (35%), Manitoba (22%), Quebec (16%) and Saskatchewan (13%). North West Territories had 66 cases (6.5%), British Columbia 54 cases (5%), and Alberta 11 (11%). Nova Scotia reported 3 cases, New Brunswick 2 cases and Prince Edward Island 1 case. The Yukon, and Newfoundland and Labrador, had no reported cases of animal rabies.
Over the same time period, skunks accounted for 37% of reported cases, followed by bats (33%), raccoons (9%) and foxes (6%). Dogs accounted for 4% and cats accounted for 2% of animal rabies cases. The species most commonly identified as having rabies by region, based on total numbers of positive test results, were as follows: foxes in the Northwest Territories and Nunavut Territory (70%), skunks in Manitoba (75%) and Saskatchewan (70%), and bats in British Columbia (99%), Alberta (81%), Quebec (70% since 2008 when raccoon rabies was last detected) and Ontario (56%); In Ontario, the second most affected species was skunks (27%).
Raccoon rabies arrived in Canada from the US in 1999 and was found mainly in Ontario, New Brunswick, and Quebec. A small number of rabid raccoons were also found in Manitoba and Saskatchewan. An active eradication program was put in place and, based on reports to September 2011, no rabid raccoons have been detected in Canada since 2008.
Rabies occurs in larger rodents such as ground hogs (woodchucks) and beavers in some areas of the US. Rabies in these animals is rare in Canada with only three rabid ground hogs (woodchucks) detected from 1998 to mid-2011, two in Manitoba in 1999 and one in Ontario in 2000.
Rabid bats have been found in most regions across Canada. The prevalence of rabies in wild bats is generally unknown, although older studies suggest a prevalence of between less than 1% and 4.1%. In 2006, the CFIA tested 2,150 bats, 3.3% of which were positive.
Bat strains of rabies virus have occasionally been identified in other animals such as foxes, cows, horses, squirrels, skunks, dogs and cats. Almost any mammal that has been exposed to an infected bat may become infected. No human cases of rabies associated with bat strains have been known to be transmitted from exposure to other animals.
Preparations authorized for use in Canada
Rabies vaccines (Rab)
- IMOVAX®Rabies (inactivated, human diploid cell rabies vaccine). Sanofi Pasteur Ltd. (HDCV)
- RABAVERT® (inactivated, purified chick embryo cell rabies vaccine), Bavarian Nordic A/S (PCECV)
Rabies immunoglobulins (RabIg)
- HyperRAB® (300 IU/mL, rabies immunoglobulin [human]), Grifols Therapeutics LLC.*
- KamRABTM (150 IU/mL, rabies immunoglobulin [human]), Kamada Ltd.*
- * NACI has not yet deliberated on the use of KamRAB™ or HyperRAB®. NACI will review these immunizing agents and update the chapter in due course. For information regarding the use of these immunizing agents in the interim, please refer to the product monograph available through Health Canada's Drug Product Database.
RabIg is a solution of anti-rabies Ig for IM administration, prepared from the pooled human plasma of screened donors immunized with rabies vaccine. RabIg is available on an emergency basis through local public health officials.
For complete prescribing information, consult the product leaflet or information contained within the product monograph available through the Health Canada's Drug Product Database. Refer to Contents of Immunizing Agents Authorized for Use in Canada in Part 1 for a list of vaccines and passive immunizing agents authorized for use in Canada and their contents.
Efficacy, effectiveness and immunogenicity
Efficacy and effectiveness
HDCV or PCECV administered at the same time as RabIg (using a separate needle, syringe and injection site) and local treatment are highly effective in preventing rabies in exposed individuals. Failures of post-exposure management have occurred, although almost always after deviation from the recommended post-exposure prophylaxis protocol. No post-exposure prophylaxis failures have occurred in Canada or the US.
Immunogenicity
Pre-exposure immunogenicity
The immunogenicity of PCECV and HDCV for pre-exposure vaccination has been demonstrated in clinical trials. When PCECV was administered according to the recommended immunization schedule, 100% of subjects attained an adequate antibody titre by Day 28 or earlier. Persistence of adequate antibody titres for up to 2 years after immunization with PCECV has been demonstrated. After a three-dose primary series of HDCV, all vaccinees reached an adequate antibody titre. A 10-year follow-up study of subjects who received three doses of HDCV, followed by a booster dose at 1 year, has shown the maintenance of protective antibody up to 5 years in 96.2%. A seroconversion rate of 95.1% was demonstrated in travellers who received three ID injections of HDCV or PCECV, with a booster after 12 months.
Post-exposure immunogenicity
Clinical studies in patients exposed to rabies virus have demonstrated that PCECV, when used in a five- or six-dose post-exposure schedule, provided protective antibody titres in 98% of patients within 14 days and in 100% of patients by Day 30. In a study of subjects who received HDCV in a five-dose post-exposure schedule as well as RabIg on day 0, all vaccinees reached a protective antibody titre by day 14 and remained at that level through day 90. One year later, protective antibody concentrations were maintained in 98.3% of subjects.
Recommendations for use
Pre-exposure immunization
Pre-exposure rabies immunization with either HDCV or PCECV should be offered to people at high risk of close contact with rabid animals or the rabies virus, for example:
- Laboratory workers who handle the rabies virus.
- Veterinarians, veterinary staff, animal control and wildlife workers. Refer to Workers.
- Certain travellers. Refer to Travellers.
- Hunter and trappers in areas with confirmed rabies.
- Spelunkers (cavers).
Post-exposure management
Risk assessment related to the exposure to the potentially rabid animal
Rabies prophylaxis must be considered in every incident in which human exposure to potentially rabid animals has occurred, unless rabies is known to be absent from the local animal population. In evaluating each case, local public health officials should be consulted. When considering the need for post-exposure management, the following should be reviewed:
- The species of animal, including the prevalence of rabies in that species and the prevalence of rabies in other species in the area.
- The type of exposure - bite, non-bite (e.g. salivary contact with open skin or mucous membrane, transplant of infected organs), or direct contact with a bat. Unless one of these three potential modes of exposure has occurred, transmission of rabies is highly unlikely.
- The circumstances of the exposure - provoked, unprovoked.
- The vaccination status and behaviour of a domestic animal.
- The age of the exposed person.
- The location and severity of the bite (e.g., the size and number of bites).
In addition, the availability of the animal for observation or testing influences the management of the animal and the exposed person. Table 1 summarizes factors to be considered when assessing the risk related to the exposure to a potentially rabid animal.
Species of animal
The animals in Canada most often proven rabid are wild terrestrial carnivores (e.g. skunks, foxes and raccoons), bats, cattle and stray dogs and cats. As the distribution of animal rabies and the species involved vary considerably across Canada, it is important to consult local public health officials in cases of possible exposure. In North America, domestic dog and cat exposures may be managed differently than in other areas of the world, where the prevalence of rabies in these animals is higher, and where programmes to control the populations of stray dogs are not in place.
If the incident involves a dog or cat, determining if it is a stray or domestic animal assists with the risk assessment. Generally, rabies is less likely in domestic animals, particularly domestic dogs, compared to stray animals, due to the following factors: domestic animals are more likely to be vaccinated; and domestic animals may spend less time outdoors where exposure to a potentially rabid animal could occur. In addition, an encounter with a potentially rabid animal is more likely to be recognized in a domestic animal.
Human exposures to livestock are usually confined to salivary contamination, with the exception of horses and swine, from which bites have been reported. The risk of infection after exposure to rabid cattle is low. Squirrels, hamsters, guinea-pigs, gerbils, chipmunks, rats, mice or other small rodents, as well as lagomorphs (such as rabbits and hares), are rarely found to be infected with rabies because it is believed that they are likely to be killed by the larger animal that could have potentially transmitted rabies to them. These small animals can, theoretically, become infected by bat strains of rabies; however, no cases of transmission of bat strains of rabies from these animals to humans have been documented. Because these small animals are not known to have caused human rabies in North America, post-exposure prophylaxis should be considered only if the animal's behaviour is highly unusual. For example, a bite from a squirrel while feeding it would not be considered unusual behaviour and so does not warrant post-exposure prophylaxis, based on this information alone. Rabies in larger rodents such as groundhogs (woodchucks) and beavers is rare in Canada; exposure to these animals requires an assessment of the circumstances of the exposure to determine the need for post-exposure prophylaxis.
The manifestations of rabies and the incubation periods vary in different species. The length of time virus may be excreted in saliva before the development of symptoms (asymptomatic carriage) has not been determined for the purpose of defining rabies exposure except in dogs, cats and ferrets. In dogs, cats and ferrets, rabies virus excretion does not generally precede symptom development beyond 10 days.
Type of exposure
Rabies is transmitted only when the virus is introduced into a bite wound, open cuts in skin, or onto mucous membranes such as the mouth or eyes. Transmission of rabies occurs most commonly through bites. Corneal transplants are the most common non-bite exposures leading to human rabies. In 2004, the US Centers for Disease Control and Prevention confirmed the first reported case of rabies following solid organ transplantation. Between 1956 and 1977, four cases of human rabies may have been acquired through aerosolized virus across mucous membranes. Two of these cases of rabies have been attributed to probable aerosol exposures in laboratories, and two cases have been attributed to possible airborne exposures in caves containing millions of bats; however, alternative infection routes cannot be discounted in several of these cases. Similar airborne incidents have not occurred in approximately 25 years, possibly because of elevated awareness of such risks resulting in increased use of appropriate preventive measures.
The contamination of open wounds, abrasions, scratches or mucous membranes with saliva or neural tissues are also considered forms of non-bite exposures. Only eight instances of human rabies from cutaneous or mucous membrane exposures were found in a review published in 2002 and these were not well documented, raising the possibility of other routes of exposure. The reports of scratches consist of a facial scratch from a bat in 1985 and a scratch from a rabid calf in the 1940s.
Types of exposures can be considered in three broad categories: bite exposures, non-bite exposures and bat exposures as follows:
- Bite exposure: A bite is defined as any penetration of the skin by teeth. Bites inflicted by most animals are readily apparent with the exception of bats. Bites inflicted by bats may not be felt and may leave no visible bite marks (refer to Bat Exposure).
-
Non-bite exposure: Non-bite exposures, other than organ or tissue transplants, have almost never been proven to cause rabies, and post-exposure prophylaxis is not indicated unless the non-bite exposure involves saliva or neural tissue being introduced into fresh, open cuts or scratches in skin or onto mucous membranes. These exposures require a risk assessment that consider the likelihood of saliva contamination (e.g., did the animal lick the wound?), the prevalence of rabies in the area, the species involved (domestic or stray dog or cat, wild terrestrial animal, or bat) and the circumstances of the exposure (e.g., provoked or unprovoked; the behaviour of a domestic animal). Petting a rabid animal or handling its blood, urine or feces is not considered to be an exposure; however, such contact should be avoided. Being sprayed by a skunk is also not considered an exposure. These incidents do not warrant post-exposure prophylaxis.
Post-exposure prophylaxis or testing of a bat is generally recommended after direct contact with the bat (refer to Bat Exposure) because it is very difficult to ensure that a bite did not take place.
Post-exposure prophylaxis is recommended in rare instances, such as inhalation of aerosolized virus by spelunkers exploring caves inhabited by infected bats or by laboratory technicians homogenizing tissues infected with rabies virus without appropriate precautions; however, the efficacy of prophylaxis after such exposures is unknown.
Exposures occurring in the course of caring for humans with rabies could, theoretically, transmit the infection. No case of rabies acquired in this way has been documented, but post-exposure prophylaxis should be considered for individuals exposed to saliva or neural tissue from a person with rabies.
-
Bat exposure: Post-exposure rabies prophylaxis following bat contact is recommended when both of the following conditions apply:
- There has been direct contact with a bat, AND
- A bite, scratch, or saliva exposure into a wound or mucous membrane cannot be ruled out.
Direct contact with a bat is defined as a bat touching or landing on a person. When there is no direct contact with a bat, the risk of rabies is extremely rare and rabies post-exposure prophylaxis is not recommended. In an adult, a bat landing on clothing would be considered reason for intervention only if a bite, scratch or saliva exposure into a wound or mucous membrane cannot be ruled out. In a child, a bat landing on clothing could be considered a reason for intervention, as a history to rule out a bite, scratch or mucous membrane exposure may not be reliable. When a bat is found in the room with a child or an adult who is unable to give a reliable history, assessment of direct contact may be difficult. Factors indicating that direct contact may have occurred include the individual waking up crying or upset while the bat was in the room or observation of an obvious bite or scratch mark.
From 1998 to 2009, NACI recommended that people who may not be aware of or able to report a bat bite (e.g., sleeping person, young child, cognitively impaired) be offered intervention if a bat was found in the room with them. This recommendation was revised (as described above) in 2009 based on the rarity of human rabies related to bats (one case in Canada reported approximately every 5 years). Analysis conducted in Canada estimated that a case of human rabies related to bedroom exposure to a bat (i.e., finding a bat in the room of a sleeping person with no recognized physical contact with the bat) is expected to occur in Canada once every 84 years. In addition, it has been determined that, to prevent one case of rabies from bedroom exposure to a bat, using a conservative estimate, 314,000 people would need to be treated.
Circumstance of the exposure
An unprovoked attack is more likely to indicate that the animal is rabid, although, rabid animals may become uncharacteristically quiet. Bites inflicted on a person attempting to feed or handle an apparently healthy animal should generally be regarded as provoked. Untrained individuals should never handle wild or stray animals or any domestic animal that is behaving unusually and children should be taught this precaution.
Vaccination status and behaviour of the animal
Domestic pets with up-to-date rabies vaccination are unlikely to become infected with rabies. A veterinarian should be consulted to determine if the animal is up-to-date with its vaccinations. Any domestic dog, cat or ferret (regardless of vaccination history) that has bitten a human should be reported to public health officials for appropriate follow-up.
A history of abnormal or aggressive behaviour in a domestic animal, potential for exposure of a domestic animal to other animals that could transmit rabies to the domestic animal, and a previous encounter of a domestic animal with a wild animal should be considered as factors that increase the likelihood that a domestic animal exposure carries a risk of rabies transmission. Generally, behaviour in wild animals cannot be accurately evaluated and should not be considered part of the risk assessment; however, some behaviours in bats may be considered abnormal and indicative of rabies, such as a bat attacking a person or hanging on tenaciously to a person.
The age of the exposed person
The history obtained from a child who has been potentially exposed to an animal can be difficult to interpret and potentially unreliable. This factor should be considered when determining the appropriate post-exposure management.
The location and severity of the bite
When the rabies virus is inoculated into a wound, it must be taken up at a nerve synapse to travel to the brain, where it causes fatal encephalitis. The virus may enter a nerve rapidly or it may remain at the site of the bite for an extended period before gaining access to the nervous system. Post-exposure prophylaxis is ineffective after the rabies virus invades the nervous system.
More severe bites may be more likely to suggest the animal is rabid and these bites may also provide more opportunity for transmission of the virus, because of the increased extent of exposure to saliva.
A higher density of nerve endings in the region of the bite increases the risk of developing rabies encephalitis. Bites on the hands and face, because of the density of nerve endings, are considered higher-risk exposures.
Table 1 provides an outline of factors to consider in the risk assessment related to exposure to potentially rabid animals.
Table 1: Risk assessment related to the exposure to the potentially rabid animal
This table and accompanying text are guides for management and do not replace clinical judgment.
Factors to Consider
Animal
- How prevalent is rabies in the species of animal involved in the exposure?
- In North America, rabies occurs mainly in bats, foxes, skunks, raccoons and stray dogs and cats.
- Is the animal a domestic pet, wild animal or stray animal?
- Domestic dogs and cats are less likely to be rabid than stray dogs or cats. Clinical signs of rabies in wild animals cannot be interpreted reliably.
- Is the wild animal available for testing?
- In the event of exposure to a fox, skunk, raccoon or bat in areas where rabies is known to occur in these animals, post-exposure prophylaxis should begin immediately unless the animal is available for rabies testing and rabies is not considered likely. Post-exposure prophylaxis should not be delayed beyond 48 hours while waiting for test results in wild animals.
- Is the dog, cat or ferret available for observation?
- If the dog, cat or ferret is healthy after a 10-day observation period, the animal would not have been shedding rabies virus in their saliva and would not have been infectious at the time of the exposure.
- If the dog, cat or ferret is available, is it clinically healthy?
- If the dog, cat or ferret has or develops signs of rabies, post-exposure prophylaxis should be initiated as soon as possible.
- Was the animal behaving unusually?
- Abnormal behaviour in a domestic pet may indicate that the animal is rabid. Generally, it is not possible to assess animal behaviour in wild animals.
- If the animal is a domestic pet, what is the vaccination status of the animal?
- Domestic pets with up-to-date rabies vaccination are unlikely to be infected with rabies.
- If the animal is a domestic pet, has it been exposed to wild or outdoor animals?
- Rabies may be transmitted to domestic pets during exposure to rabid wild or outdoor animals. Indoor animals have little opportunity to be exposed to rabid animals.
Geographic
- In what geographic area did the exposure occur?Table 1 - Footnote *
- How prevalent is rabies in the involved species in the geographic area?
- How prevalent is rabies in other animal species in the geographic area?
Exposure
- What was the type of exposure: bite, non-bite (e.g.salivary contact on open skin or mucous membrane), or bat?
- Transmission rarely occurs from non-bite exposures. Petting a rabid animal or handling its blood, urine or feces are not considered exposures.
- Can a bite or saliva exposure into a scratch, wound or mucous membrane be ruled out?
- Rabies transmission occurs most commonly through a bite. Aerosol transmission is rare as is transmission when scratches, wounds, or mucous membrane are contaminated from saliva or infected neural tissue.
- What were the circumstances of the exposure (e.g., provoked or unprovoked attack)?
- An unprovoked attack is more likely to indicate that the animal is rabid.
Person
- What is the age of the exposed person? Is the exposed person able to provide a reliable history?
- The history obtained from a child may be difficult to interpret and, potentially, unreliable. Assessment of the exposure may also be difficult in a cognitively impaired adult.
- What is the location and severity of the wounds?
- Bites on the face, neck or hand are considered higher-risk exposures due to the density of nerve endings in these areas. More severe bites may suggest the animal is rabid and also provide more opportunity for transmission.
Management of the potentially rabid animal
Any animal that has bitten a human or is suspected of being rabid should be reported to local public health officials.
Rabies testing of animals is done at the CFIA Rabies Laboratories at Ontario Laboratory Fallowfield (OLF - Rabies unit), and the CFIA Lethbridge Laboratory (LET-Rabies unit) using a fluorescent antibody test of brain tissue, which is the gold standard recommended by the WHO. The test has a reported sensitivity of 98% to 100%. Further information and testing advice may be obtained from the CFIA web site.
Dogs, cats and ferrets
Exposures to dogs, cats and ferrets that could potentially result in rabies transmission (as described in Type of exposure) should be reported to local public health officials. Dogs, cats and ferrets that are apparently healthy should be confined and observed for 10 days after a bite, regardless of the animal's rabies vaccination status. If these animals - are alive and healthy at the end of the 10-day period, they would not have transmitted rabies in their saliva at the time of the bite. If illness suggestive of rabies exists at the time of the bite or develops during the observation period, the animal should be humanely euthanized in a way that does as little damage to the brain as possible, and the head submitted for laboratory examination and rabies testing. Rabies virus is readily demonstrable in brains of animals with neurologic symptoms. The CFIA veterinarian should be contacted to assist with determining the need for testing, organizing the testing and following-up potential exposures to other domestic animals.
The confinement and observation of an apparently healthy dog, cat or ferret can take place at the owner's home, an animal shelter, or a veterinarian's office, depending on circumstances, including the reliability of the owner, the capacity to keep the animal away from people and other animals, the ability to prevent the animal's escape, and the suspicion of rabies in the animal. The person responsible for observation of the animal should be advised to notify public health officials if the animal becomes ill or escapes during the observation period. The animal should be observed by a public health official or veterinarian at the end of the 10-day observation period to ensure that it is alive and healthy. Unvaccinated animals that remain healthy should be vaccinated at the end of the observation period.
Stray or unwanted dogs, cats or ferrets involved in an exposure that could potentially transmit rabies should be confined and observed as outlined above. If this is not possible, the animal should be humanely euthanized in a way that does as little damage to the brain as possible, and the head submitted for laboratory examination and rabies testing in consultation with the local CFIA veterinarian.
If the dog, cat or ferret has escaped, attempts should be made to find the animal and owner. If the dog, cat or ferret cannot be located, a decision should be made in consultation with public health officials regarding the need for post-exposure prophylaxis. Refer to Management of the person after exposure to a potentially rabid animal for additional information.
Wild terrestrial carnivores and exotic pets (other than ferrets)
The period of rabies virus shedding in a wild terrestrial carnivore (such as a skunk, fox or raccoon) or in an exotic pet (other than a ferret) is unknown. Therefore, when these animals are involved in an exposure that could potentially transmit rabies, a trained wildlife or animal control worker should be contacted to capture the animal. The worker should use extreme caution to ensure that there is no further exposure to the animal. The animal should be immediately humanely euthanized in a way that does as little damage to the brain as possible, and the head submitted for laboratory examination and rabies testing in consultation with the local CFIA veterinarian.
Bats
If there has been no direct contact with the bat, the bat should not be captured for testing and should be safely released. To remove a bat from a building, the area with the bat should be closed off from the rest of the building and people and pets kept out of the area. The doors or windows in the area with the bat should be opened to the exterior to let the bat escape.
If there has been direct contact with a bat (as defined in Bat exposure), a trained wildlife or animal control worker should be contacted to attempt to capture the bat. The worker should use extreme caution to ensure that there is no further exposure to the bat. She or he should wear thick leather gloves, should avoid touching the bat, and should place the intact bat in a closed secure container. Once the bat has been captured, local public health officials should be contacted. The public health agency will contact the CFIA regarding rabies testing of the bat. Bats should be submitted intact for rabies testing, i.e. they should not be decapitated.
Management of the person after exposure to a potentially rabid animal
Table 2 outlines recommendations for the management of people after possible exposure to rabies. These recommendations are intended as a guide and may need to be modified in accordance with the specific circumstances of the exposure.
The objective of post-exposure management is to neutralize the rabies virus at the site of infection before the virus can enter the central nervous system. Immediate and thorough cleaning and flushing of the wound with soap and water is imperative and is probably the most effective procedure in the prevention of rabies. Care should be taken to clean the wound to its full depth. Flushing for approximately 15 minutes is suggested. Some guidelines also suggest the application of a viricidal agent, such as iodine-containing or alcohol solutions. Suturing the wound should be avoided if possible, and tetanus prophylaxis and antibiotics should be given as appropriate.
If exposure to rabies is considered highly likely, post-exposure prophylaxis should be started as soon as possible after the exposure. If the initiation of post-exposure prophylaxis is delayed until test results from the involved animal are available, a maximum waiting period of 48 hours is recommended. In consultation with public health officials, post-exposure prophylaxis may be discontinued if the animal tests negative for rabies.
If indicated, based on the risk assessment, post-exposure prophylaxis should be offered to exposed individuals regardless of the time interval after exposure.
Exposures to dogs, cats and ferrets
If the suspect animal is a dog, cat or ferret that is healthy and available for observation, post-exposure prophylaxis may be withheld, pending the animal's status after a 10-day observation period. However, if the animal has or develops signs suggestive of rabies, post-exposure prophylaxis of exposed persons should be initiated immediately. The animal should be humanely euthanized in a way that does as little damage to the brain as possible, and the head submitted for immediate laboratory examination and rabies testing. In consultation with public health officials, post-exposure prophylaxis may be discontinued if the animal tests negative for rabies.
If the dog, cat or ferret has escaped and cannot be located, a decision should be made in consultation with public health officials regarding the need for post-exposure prophylaxis. The decision should consider several factors, including the rate of occurrence of rabies in the area, if it was a domestic or stray animal, the type of exposure, the circumstances of the exposure, including whether it was a provoked or unprovoked exposure, and the severity and location of the wound.
Exposures to wild animals and exotic pets (other than ferrets)
Post-exposure prophylaxis should begin immediately following exposure to a wild terrestrial carnivore (such as a fox, skunk or raccoon) in enzootic areas, unless the animal is available for rabies testing and rabies is not considered likely. The decision to start post-exposure prophylaxis while awaiting the laboratory test results should consider several factors, including when the test results will be available, the species of animal, the rate of occurrence of rabies in that species and in other species in the area, the type of exposure, the circumstances of the exposure including whether it was a provoked or unprovoked exposure, and the severity and locations of the wounds. Initiation of post-exposure prophylaxis should not be delayed beyond 48 hours while waiting for laboratory tests, if the exposure is from a terrestrial animal in an enzootic area. If post-exposure prophylaxis is started before the test results are available, in consultation with public health officials, the rabies vaccine may be discontinued if the animal tests negative for rabies.
Exposure to small rodents (such as squirrels, chipmunks, rats, mice, hamsters, guinea pigs, gerbils) and lagomorphs (such as rabbits and hares) has rarely been known to transmit rabies; therefore, post-exposure prophylaxis is rarely indicated after exposure to these animals. Post-exposure prophylaxis should only be considered if the animal was behaving very unusually.
Larger rodents such as ground hogs (woodchucks) and beavers can potentially carry rabies, although it is rare in Canada. The management of exposures to these animals requires a risk assessment, which includes the frequency of rabies in these animals in the geographic area, the frequency of rabies in other animals, the type of exposure, and the circumstances of the bite including whether it was provoked or unprovoked.
Exposures to bats
When there is a known bat bite, scratch or saliva exposure into a wound or mucous membrane, rabies post-exposure prophylaxis should be initiated immediately because of the higher prevalence of rabies in bats. It is particularly important to do so when the exposure involves the face, neck or hands, or when the behaviour of the bat is clearly abnormal, such as a bat that attacks a person or hangs on tenaciously. If the bat is available for testing, post-exposure prophylaxis may be discontinued after consultation with public health officials if the bat tests negative for rabies.
If a person is touched by a bat (such as a bat in flight) and the bat is available for rabies testing, the health care provider may decide to delay post-exposure prophylaxis. Post-exposure prophylaxis should not be delayed more than 48 hours. If a bat tests positive for rabies, the need for post-exposure prophylaxis should depend on whether direct contact with the bat occurred and not the rabies status of the bat. If a person is touched by a bat, but the bat is not available for testing it should be considered a direct contact and post-exposure prophylaxis should be given.
| Animal species | Condition of animal at time of exposure | Management of exposed persons not previously immunized against rabies | Management of exposed persons previously immunized against rabies |
|---|---|---|---|
| Dog, cat or ferret | Healthy and available for a 10-day observation period |
|
|
| Unknown or escaped |
|
|
|
| Rabid or suspected to be rabidTable 2 - Footnote * |
|
|
|
| Skunk, bat, fox, coyote, raccoon and other carnivores. | Regard as rabidTable 2 - Footnote * unless geographic area is known to be rabies-free |
|
|
| Livestock, rodents or lagomorphs (hares and rabbits) | Consider individually. Consult appropriate public health and CFIA officials. Bites of squirrels, chipmunks, rats, mice, hamsters, gerbils, guinea pigs, other small rodents, rabbits and hares would only warrant post-exposure rabies prophylaxis if the behaviour of the biting animal was highly unusual. Bites from larger rodents (e.g., ground hogs (woodchucks), beavers) require a risk assessment. |
||
Pregnancy and breastfeeding
Pregnancy and breastfeeding are not contraindications to post-exposure rabies prophylaxis, but it is prudent to delay pre-exposure immunization of pregnant women unless there is a substantial risk of exposure. Refer to Immunization in Pregnancy and Breastfeeding in Part 3 for additional general information.
Immunocompromised persons
Corticosteroids, other immunosuppressive agents, and immunosuppressive illnesses (e.g., congenital immunodeficiency, human immunodeficiency virus [HIV] infection, leukemia, lymphoma, generalized malignancy) may interfere with the antibody response to rabies vaccine. Because of suboptimal response, in general, immunocompromised persons should be counselled to avoid situations of rabies exposure. If possible, pre-exposure immunization should be delayed in immunocompromised individuals until the immunocompromised state has resolved. In situations in which immunosuppression is planned (such as before organ transplant) and pre-exposure rabies vaccine is necessary, the vaccine series should be given only by the intramuscular route and should be completed at least 14 days prior to starting immunosuppression if possible. For hematopoietic stem cell transplant recipients, pre-exposure rabies vaccination can be started 6 to12 months after transplant. Depending on the risk of exposure, it may be appropriate to consider temporarily discontinuing immunosuppressive medications, in consultation with the attending physician, or to vaccinate once the person is no longer considered immunocompromised. If pre-exposure vaccination of an immunocompromised person is considered necessary because animal exposure cannot be avoided and the immunocompromising condition cannot be corrected, the vaccination should be given only by the intramuscular route and serology should be checked 7 to 14 days post-vaccination to ensure that an acceptable antibody response has developed.
When post-exposure prophylaxis is administered to an immunocompromised person, a full five-dose series (days 0, 3, 7, 14 and 28 days) should be used along with one dose of RabIg on day 0; serology should be checked 7 to 14 days after completion of the series to ensure that an acceptable antibody response has developed. If no acceptable antibody response is detected, the patient should be managed in consultation with their physician and appropriate public health officials to receive a second rabies vaccine series. RabIg should not be repeated at the initiation of this second course. Immunosuppressive agents should not be administered during post-exposure prophylaxis unless essential for the treatment of other conditions.
Refer to Immunization of Immunocompromised Persons in Part 3 for additional information.
Travellers
Risk to travellers varies depending on itinerary, purpose and duration of the trip, as well as activities and access to medical care. Travellers to rabies endemic areas where there is poor access to adequate and safe post-exposure management, as well as frequent and long-term travellers to high risk areas, should seriously consider receiving pre-travel rabies immunization. Children, especially those who are too young to understand the need both to avoid animals and to report a traumatic contact, are considered at greater risk of rabid animal exposure and should receive pre-exposure immunization when travelling to endemic areas. The WHO website includes a map of global areas where rabies transmission occurs: Rabies, countries or areas at risk.
Public health officials should be consulted regarding travellers who have had an exposure to a potentially rabid animal in a developing country, even if the traveller received a complete course of post-exposure prophylaxis in that country. The prevalence of rabies in developing countries is generally higher than in Canada, and there may be concerns about the potency of available vaccines in these countries. Options for consideration in the management of travellers exposed in developing countries include initiating or repeating all or part of the post-exposure management obtaining post-vaccination serology or both. The Committee to Advise on Tropical Medicine and Travel (CATMAT) provides additional information on assessing a traveller's need for pre-travel vaccination or post-travel post-exposure prophylaxis, and identifies the rabies vaccines that meet the WHO's safety, potency and efficacy requirements.
Refer to Immunization of Travellers in Part 3 for additional general information.
Workers
Pre-exposure rabies immunization should be offered to workers at high risk of occupational exposure to potentially rabid animals or to the rabies virus. High risk individuals may include veterinarians, veterinary staff, animal control and wildlife workers, and laboratory workers exposed to the rabies virus. Refer to Immunization of Workers in Part 3 for additional general information.
Vaccine administration
Dose, route of administration, and schedule
Dose
The IM dose is 1.0 mL; the ID dose is 0.1ml. Each 1.0 mL dose of HDCV or PCECV contains at least 2.5 international units (IU) of rabies antigen, which is the WHO recommended standard.
Pre-exposure immunization: route and schedule
Three doses of HDCV or PCECV are required and should be given on days 0, 7 and any time between days 21 to 28. The vaccine can be given as a 1.0 mL IM dose or a 0.1 mL ID dose. Rabies vaccine should never be administered in the gluteal muscle due to variable immune response.
While IM administration of pre-exposure rabies vaccine is the gold standard, the WHO considers the ID regimen an acceptable alternative, as it uses less vaccine to produce a comparable degree of protection against rabies. The ID route should not be used in persons who are immunocompromised due to illness or medication, or are taking chloroquine, as the immune response to the vaccine may not be protective under these circumstances. In these individuals, vaccine should be administered by the IM route only. This precaution is not known to apply to other antimalarial drugs. If a decision is made to give pre-exposure prophylaxis by the ID route to a person requiring chloroquine, chloroquine use must be delayed for at least one month after vaccination or given only if the person has been found to have an adequate titre post-vaccination. If the intradermal route is used, rabies vaccine should be administered only by fully trained staff in settings in which there is a well-established cold chain. The use of the proper syringe and needle is essential to ensure that the correct route and dose are used. Improper technique may result in a suboptimal dose of vaccine being administered or inadvertent subcutaneous injection of the vaccine. Vaccine wastage should be minimized by immunizing enough individuals at the same time to use all of the contents of a vial of vaccine, whenever possible.
When rabies vaccine is administered ID, post-immunization antibody titres should be determined at least 2 weeks after completion of the vaccine series to ensure that an acceptable level of protection has been achieved. If using the ID route for a booster dose, serology should be checked at least 2 weeks after the booster dose.
Post-exposure prophylaxis of previously unimmunized individuals
Post-exposure prophylaxis of previously unimmunized individuals should consist of both RabIg and rabies vaccine. The RabIg provides immediate passive protection until the exposed person mounts an immune response to the rabies vaccine.
Rabies vaccine and RabIg may be given at the same time but at different injection sites, using separate needles and syringes. Rabies vaccine and RabIg should never be mixed in the same syringe.
Rabies Immunoglobulin (RabIg)
The recommended dose of RabIg is 20 IU/kg body weight for all age groups, including children, given on the first day of initiation of therapy (day 0). Because of possible interference of RabIg with the immune response to the rabies vaccine, the dose of RabIg should not be exceeded. If possible, the full dose of RabIg should be thoroughly infiltrated into the wound and surrounding area. Any remaining volume of RabIg should be injected intramuscularly, using a separate needle, at a site distant from the site of vaccine administration. When more than one wound exists, each wound should be locally infiltrated with a portion of the RabIg using a separate needle. In such instances, the RabIg can be diluted in a diluent permitted by the specific product labeling to provide RabIg in sufficient volume for thorough infiltration of all wounds. If the site of the wound is unknown, the entire dose should be administered intramuscularly at a separate site from the administration of rabies vaccine. Rabies vaccine and RabIg should never be mixed in the same syringe. If RabIg is not administered as recommended at the initiation of the rabies vaccine series, it should be administered up to and including day 7 after vaccine is initiated but should not be administered after that time.
Rabies vaccine
For post-exposure prophylaxis of immunocompetent persons previously unimmunized with rabies vaccine, four 1.0 mL doses of HDCV or PCECV should be administered IM. This is in addition to the RabIg as discussed above. The first dose (day 0) of the four-dose course of rabies vaccine should be administered as soon as possible after exposure based on the considerations discussed in the Management of the person after exposure to a potentially rabid animal section. Additional doses should be administered on days 3, 7 and 14 after the first vaccination.
Previously unimmunized immunocompromised persons, including those taking corticosteroids or other immunosuppressive agents, and those who have immunosuppressive illnesses, and those taking chloroquine and other antimalarials, should receive a five-dose vaccination regimen on days 0, 3, 7, 14 and 28 with one dose of RabIg on day 0.
Vaccine should be administered IM into the deltoid muscle in older children and adults or into the vastus lateralis muscle (anterolateral thigh) in infants, but never in the gluteal region as this may result in decreased response to the vaccine. The rabies vaccine and RabIg should be given at different anatomical sites on day 0, using a separate needle and syringe. For subsequent vaccine doses, the limb where the RabIg was administered can be used.
The vaccination schedule for post-exposure prophylaxis should be adhered to as closely as possible and it is essential that all recommended doses of vaccine be administered. Although there is little or no evidence, in keeping with routine immunization practice, it is recommended that, if a dose of vaccine is given at less than the recommended interval, that dose should be ignored and the dose given at the appropriate interval from the previous dose. If a dose of vaccine is delayed, it should be given as soon as possible and the schedule resumed, respecting the appropriate intervals from the latest dose. If the vaccination schedule has been altered and there is doubt about a sufficient immune response, post-vaccination serology should be obtained 7 to 14 days after completing the vaccination series.
Post-exposure prophylaxis of previously immunized individuals
RabIg is not indicated and should not be given to someone who has been previously appropriately immunized as indicated below. In previously appropriately immunized individuals who require post-exposure prophylaxis, two doses of HDCV or PCECV, one administered immediately and the other 3 days later, are recommended. Appropriate previous rabies immunization consists of:
- Documentation of a complete course of pre-exposure or post-exposure prophylaxis with HDCV or PCECV, OR
- Documentation of complete immunization with other types of rabies vaccine, or with HDCV or PCECV according to unapproved schedules, with the demonstration of an acceptable concentration of neutralizing rabies antibody in serum after completion of the series. Refer to Serologic Testing for information regarding criteria for serologic testing.
A complete course of either HDCV or PCECV, as well as RabIg, is recommended for those who may have received rabies vaccines in the past but do not fulfill the criteria listed above for appropriate vaccination. A serum sample may be collected before the initiation of post-exposure prophylaxis to test for rabies antibody, and if an acceptable antibody concentration (0.5 IU/mL or greater) is demonstrated, the vaccine course may be discontinued, provided that at least two doses of vaccine have been given. If in doubt, consultation with an infectious diseases or public health physician is recommended.
Booster doses and re-immunization
Some individuals with ongoing high risk of exposure to rabies, such as veterinarians and veterinary staff, animal control or wildlife workers, those with ongoing bat exposures or those working with live rabies virus, may require pre-exposure booster doses if their antibody titres fall below 0.5 IU/mL (refer to Serologic Testing for information regarding when serologic testing is recommended). People with ongoing high risk of exposure and inadequate titres should be given a booster dose of either rabies vaccine. Both HDCV and PCECV have been shown to be effective in boosting immunity in previously immunized individuals, if given either as a pre-exposure booster or for post-exposure management. A rapid anamnestic response is obtained, regardless of whether the primary vaccine was HDCV or PCECV. Refer to Post-exposure prophylaxis of previously immunized individuals for information on the post-exposure management of these individuals.
Refer to Vaccine Administration Practices in Part 1 for additional information.
Serologic and cerebrospinal fluid testing
The Public Health Agency of Canada's National Microbiology Laboratory (NML) is the Canadian rabies reference laboratory. NML conducts testing on serum and cerebrospinal fluid samples from all provinces and territories in Canada with the exception of Ontario, where serological testing is performed by the Public Health Ontario Laboratory (PHOL).
Following vaccination, neutralizing antibodies begin to develop within seven days and persist for at least two years. For testing vaccine response, NML uses a modified Fluorescent Antibody Virus Neutralization (FAVN) assay, while PHOL uses a modification of the Rapid Fluorescent-Focus Inhibition Test (RFFIT). Both institutions consider the antibody titre of at least 0.5 IU/mL as an acceptable correlate of protection. Protective antibodies are present immediately after passive vaccination with RabIg and have a half-life of approximately 21 days.
Healthy people
Because of the excellent immune response to rabies vaccine, healthy people immunized with an appropriate regimen do not require routine antibody determinations after either pre-exposure or post-exposure rabies vaccination, unless one of the following applies:
- Pre-exposure vaccination was given by the ID route. In this circumstance, antibody concentration should be checked at least 2 weeks after completion of the vaccine series. If using the ID route for a booster dose, serology should be checked at least 2 weeks after the booster dose.
- The person is at ongoing high risk of exposure to rabies. Refer to People with ongoing high risk of exposure.
- There has been substantial deviation from the recommended post-exposure schedule. In this circumstance, antibody concentration should be checked 7 to 14 days after completing the series.
- The person has been immunized with a vaccine other than HDCV or PCECV. In this circumstance, antibody concentration should be checked at least 7 to 14 days after completing the series.
People with ongoing high risk of exposure
People with ongoing high risk of exposure to the rabies virus or potentially rabid animals require periodic serological testing to ensure the persistence of circulating antibodies. If antibody levels fall below an acceptable concentration (less than 0.5 IU/mL), a booster dose of HDCV or PCECV is recommended. Serologic testing should occur at the following frequencies:
- Continuous risk (e.g. people who work with the rabies virus in a research or vaccine production laboratory) -serology should be checked every 6 months.
- Frequent risk (rabies diagnostic laboratory workers; spelunkers; those who frequently handle bats; veterinarians, veterinary staff, animal control and wildlife workers in areas where rabies is enzootic) - serology should be checked every 2 years.
Others who have less frequent risk of exposure to potentially rabid animals or whose risk is likely to be from a recognized source (such as veterinarians, veterinary staff, and animal control officers who work with terrestrial animals in areas where rabies is uncommon; veterinary students; and travellers to enzootic areas) do not require periodic serologic testing.
Immunocompromised people
If it is possible to avoid exposure to rabies, pre-exposure immunization should be deferred in immunocompromised people until they are no longer immunocompromised. If pre-exposure immunization must be given to immunocompromised individuals, antibody response should be determined after completion of the series. Determination of antibody response is also advisable if post-exposure vaccination is given to those whose immune response may be reduced by illness or medication. In these groups, antibody titres should be determined 7 to 14 days after completing the pre-exposure or post-exposure immunization series to ensure that an acceptable antibody concentration has been achieved. If an acceptable concentration is not obtained, revaccination with a second rabies vaccine series is recommended, followed by further serologic testing. Some immunocompromised people may never mount an appropriate immune response. Refer to Immunocompromised persons.
Intradermal administration
If vaccine is given by the ID route, post-immunization antibody titres should be determined at least 2 weeks after completion of the vaccine series, and after booster doses, to ensure that an acceptable level of protection has been achieved.
Storage requirements
HDCV (IMOVAX® Rabies) should be stored at +2°C to +8°C, and should not be used if it has been frozen.
PCECV (RABAVERT®) should be stored at +2°C to +8°C and protected from light.
Once reconstituted, these vaccines should be administered promptly.
Refer to Storage and Handling of Immunizing Agents in Part 1 for additional information.
Simultaneous administration with other vaccines
Data are not available regarding the concurrent administration of rabies vaccines with other vaccines. Based on expert opinion, live vaccines given by nasal or oral route and essential inactivated vaccines, may be administered at the same time as rabies vaccines. Vaccines should be provided at different injection sites using separate needles and syringes.
If rabies immunoglobulin is administered, this may interfere with the response to live vaccines. Refer to Blood Products, Human Immunoglobulin and Timing of Immunizations, and Timing of Vaccine Administration chapters in Part 1.
Vaccine and immunoglobulin safety and adverse events
Refer to Adverse Events Following Immunization in Part 2 for additional general information.
Common and local adverse events
HDCV
Local injection site reactions such as pain, erythema, swelling, pruritus and induration at the injection site were reported in 60% to close to 90% of recipients. Mild systemic reactions such as headache, nausea, abdominal pain, muscle aches and dizziness were reported in about 6% to 55% of recipients.
PCECV
Local injection site reactions were reported in 11% to 57% of recipients, consisting of pain, tenderness, swelling, erythema and induration at the injection site lasting for 2 to 3 days. Systemic reactions are generally less common (i.e., 1% to 10% of recipients) and may consist of malaise, myalgia, arthralgia, headache and fever. Lymphadenopathy, nausea and rash have been reported occasionally.
RabIg
Local injection site pain, erythema and induration are commonly reported following administration of RabIg, as are systemic reactions such as headache and low-grade fever. The majority of reported events were mild.
Less common and serious or severe adverse events
Serious adverse events are rare following immunization and, in most cases, data are insufficient to determine a causal association.
HDCV
Anaphylactic reactions have occurred in up to 1 in 10,000 vaccine recipients. Systemic allergic reactions characterized by generalized urticaria and accompanied in some cases by arthralgia, angioedema, fever, nausea and vomiting have been reported. These reactions are uncommon in people receiving primary immunization but have occurred in up to 7% of those receiving a booster dose, with onset 1 to 21 days after immunisation. Such reactions have been shown to follow the development of IgE antibodies to beta propiolactone-altered human serum albumin in the vaccine. Neurologic complications are rare, but three cases of neurologic illness resembling Guillain-Barré syndrome, which resolved without sequelae within 12 weeks, were reported in the early 1980s, but a causal relationship has not been established.
PCECV
Anaphylaxis following immunization with PCECV has been rarely reported. Temporally associated neurologic events have also been very rarely reported but causal association with vaccination has not been established.
RabIg
Local pain, erythema and induration are common. Headache and low-grade fever may follow administration of RabIg. The majority of reported events were mild.
Guidance on reporting Adverse Events Following Immunization (AEFI)
Vaccine providers are asked to report, through local public health officials, any serious or unexpected adverse event felt to be temporally related to vaccination. An unexpected AEFI is an event that is not listed in available product information but may be due to the immunization, or a change in the frequency of a known AEFI. Refer to Reporting Adverse Events Following Immunization (AEFI) in Canada for additional information about AEFI reporting.
Contraindications and precautions
There are no contraindications to the use of rabies vaccine or RabIg after significant exposure to a proven rabid animal; however, care should be taken if post-exposure prophylaxis is to be administered to persons who are hypersensitive to the products or to any ingredient in the formulation or component of the container. Expert opinion should be sought in the management of these individuals.
If indicated, RabIg should be given with caution to persons with a history of prior systemic allergic reactions following the administration of human Ig preparations.
Persons with a proven history of hypersensitivity to the vaccine or any component of the vaccine or its container should not be given the vaccine for pre-exposure immunization if possible. For specific advice, consult an allergy specialist. Refer to Table 1 and Table 2 in Contents of Immunizing Agents Authorized for use in Canada in Part 1 for lists of all vaccines and passive immunizing agents authorized for use in Canada and their contents. For rabies vaccines and rabies immunoglobulin, potential allergens include:
- IMOVAX®Rabies: neomycin, phenol red
- RABAVERT®: amphotericin B, chicken protein, egg protein, chlortetracycline, neomycin, polygeline (gelatin)
Persons with egg allergies are not necessarily at increased risk of a hypersensitivity reaction to PCECV. However, for pre-exposure vaccination, an alternative vaccine, HDCV, should be used in vaccinees with a history of hypersensitivity reactions to egg or egg products. If an alternative vaccine is not available, post-exposure prophylaxis using PCECV should be administered to a person with a hypersensitivity to egg with strict medical monitoring. Facilities for emergency treatment of anaphylactic reactions should be available. Refer to Contraindications and Precautions in Part 2 for additional information.
Persons with specific IgA deficiency have increased potential for developing antibodies to IgA after receipt of blood products, including rabies immunoglobulin, and may be at risk for anaphylactic reactions to subsequent administration of blood products containing IgA, such as RabIg.
Infiltration of wounds with RabIg in some anatomical sites (finger tips) must be carried out with care to avoid increased pressure in the tissue compartment.
A history of a serious allergic or neuroparalytic reaction occurring during the administration of rabies vaccine poses a significant dilemma in the post-exposure situation. The risk of rabies must be carefully considered before a decision is made to discontinue immunization. The use of corticosteroids to attenuate the allergic response may inhibit the immune response to the vaccine. The existing titre of rabies antibodies should be determined and expert opinion in the management of these individuals should be sought promptly.
Pregnancy is not a contraindication to post-exposure prophylaxis with rabies vaccine and RabIg, but it would be prudent to delay pre-exposure immunization of pregnant women, unless there is a substantial risk of exposure.
Pre-exposure immunization with rabies vaccine should be postponed in persons with moderate or severe acute illness. Persons with minor acute illness (with or without fever) may be vaccinated. Post-exposure vaccination should never be postponed.
Refer to Contraindications and Precautions in Part 2 for additional information.
Drug interactions
Radiation therapy, chloroquine, corticosteroids, and other immunosuppressive agents may diminish the efficacy of rabies vaccine. There is no evidence that interference occurs with antimalarial drugs other than chloroquine.
Other considerations
Interchangeability of vaccines
Wherever possible, an immunization series should be completed with the same product. However, if it is not feasible to do so, PCECV and HDCV are considered interchangeable. People who require a booster dose of rabies vaccine can be given PCECV or HDCV, regardless of the vaccine used for the initial vaccination series. Refer to Principles of Vaccine Interchangeability in Part 1 for additional general information.
Selected references
- Centers for Disease Control and Prevention. Compendium of animal rabies prevention and control, 2005. MMWR Recomm Rep 2005;54(RR-3):1-8.
- Centers for Disease Control and Prevention. Health Information for International Travel 2010. The Yellow Book. Accessed October 2010 at: http://wwwnc.cdc.gov/travel/content/yellowbook/home-2010.aspx
- Centers for Disease Control and Prevention. Human rabies prevention - United States, 2008: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2008;57(RR03):1-26,28.
- Centers for Disease Control and Prevention. Use of a reduced (4-Dose) vaccine schedule for postexposure prophylaxis to prevent human rabies - recommendations of the Advisory Committee on Immunization Practices. MMWR Recomm Rep 2010;59(RR-2):1-9.
- Davis AD, Rudd RJ, Bowen RA. Effects of aerosolized rabies virus exposure on bats and mice. J Infect Dis. 2007 Apr 15;195(8):1144-50.
- Gibbons RV. Cryptogenic Rabies, Bats and the Question of Aerosol Transmission. Ann Emerg Med, 2002;39(5):528-36.
- National Advisory Committee on Immunization. Update on rabies vaccines. Can Commun Dis Rep;2005;31(ACS-5):1-7.
- National Advisory Committee on Immunization. Statement on recommendations regarding the management of bat exposures to prevent human rabies. Can Commun Dis Rep;2009;35(ACS-7):1-28.
- National Association of State Public Health Veterinarians. Compendium of animal rabies control, 1998. MMWR Recomm Rep 1998;47(RR-9):1-9.
- Novartis Vaccines and Diagnostics. Product Monograph - RabAvert®. February 2010.
- Parker R, McKay D, Hawes C, et al. Human rabies, British Columbia - January, 2003. Can Commun Dis Rep 2003;29(16):137-38.
- Public Health Agency of Canada. Population and Public Health Branch. Disease Information Rabies. Travel Medicine Program. Accessed October 2010 at: http://www.phac-aspc.gc.ca/tmp-pmv/info/rage_e.html.
- Rupprecht CE, Briggs D, Brown CM, et al. Evidence for a 4-dose vaccine schedule for human rabies post-exposure prophylaxis in previously non-vaccinated individuals. Vaccine 2009;27:7141-48.
- Ruppercht CE, Gibbons RV. Prophylaxis against rabies. N Engl J Med 2004;351:2626-35.
- Sanofi Pasteur Ltd. Product Monograph - IMOGAM®Rabies Pasteurized, October 2005.
- Sanofi Pasteur Ltd. Product Monograph - IMOVAX®Rabies, March 2006.
- Grifols Therapeutics, LLC. Product Monograph - HYPERRAB®, March 2019.
- Turgeon N, Tucci M, Deshaies D, et al. A case report: human rabies in Montreal, Quebec, October 2000. Can Commun Dis Rep 2000;26(24):209-10.
- Varughese P. Human rabies in Canada - 1924-2000. Can Commun Dis Rep 2000;26(24):210-11.
- World Health Organization. Rabies vaccines: WHO position paper. Geneva: World Health Organization, 2010;32:309-20.
- World Health Organization. WHO recommendations on rabies post-exposure treatment and the correct technique of intradermal immunization against rabies. Geneva: World Health Organization, 1997. WHO/EMC/Zoo.96.6.
Page details
- Date modified: