Systematic review of the barriers for HIV testing in Canada; 2009–2019

 Download this article as a PDF
Download this article as a PDFPublished by: The Public Health Agency of Canada
Issue: Volume 47-2: HIV Testing in Canada in the Past Decade 2009–2019
Date published: February 2021
ISSN: 1481-8531
Submit a manuscript
About CCDR
Browse
Volume 47-2, February 2021: HIV Testing in Canada in the Past Decade 2009–2019
Systematic review
Understanding barriers and facilitators to HIV testing in Canada from 2009–2019: A systematic mixed studies review
Claudie Laprise1, Clara Bolster-Foucault1
Affiliation
1 Public Health Agency of Canada, Health Security and Infrastructure Branch, Public Health Capacity and Knowledge Management Unit, Québec Regional Office; Montréal, QC
Correspondence
Suggested citation
Laprise C, Bolster-Foucault C. Understanding barriers and facilitators to HIV testing in Canada from 2009–2019: A systematic mixed studies review. Can Commun Dis Rep 2021;47(2):105–25. https://doi.org/10.14745/ccdr.v47i02a03
Keywords: HIV, barriers, facilitators, testing, screening, Canada, systematic review, mixed studies, key populations
Abstract
Background: HIV testing is a core pillar of Canada's approach to sexually transmitted and blood-borne infection (STBBI) prevention and treatment and is critical to achieving the first Joint United Nations Programme on HIV/AIDS (UNAIDS) 90-90-90 target. Despite progress toward this goal, many Canadians remain unaware of their status and testing varies across populations and jurisdictions. An understanding of drivers of HIV testing is essential to improve access to HIV testing and reach the undiagnosed.
Objective: To examine current barriers and facilitators of HIV testing across key populations and jurisdictions in Canada.
Methods: A systematic mixed studies review of peer-reviewed and grey literature was conducted identifying quantitative and qualitative studies of barriers and facilitators to HIV testing in Canada published from 2009 to 2019. Studies were screened for inclusion and identified barriers and facilitators were extracted. The quality of included studies was assessed and results were summarized.
Results: Forty-three relevant studies were identified. Common barriers emerge across key populations and jurisdictions, including difficulties accessing testing services, fear and stigma surrounding HIV, low risk perception, insufficient patient confidentiality and lack of resources for testing. Innovative practices that could facilitate HIV testing were identified, such as new testing settings (dental care, pharmacies, mobile units, emergency departments), new modalities (oral testing, peer counselling) and personalized sex/gender and age-based interventions and approaches. Key populations also face unique sociocultural, structural and legislative barriers to HIV testing. Many studies identified the need to offer a broad range of testing options and integrate testing within routine healthcare practices.
Conclusion: Efforts to improve access to HIV testing should consider barriers and facilitators at the level of the individual, healthcare provider and policy and should focus on the accessibility, inclusivity, convenience and confidentiality of testing services. In addition, testing services must be adapted to the unique needs and contexts of key populations.
Introduction
The World Health Organization estimated that approximately 37.9 million people were living with HIV/AIDS worldwide in 2018, including about 1.7 million who were newly infected that yearFootnote 1. In Canada, more than 63,000 people were living with HIV in 2016, and nearly 23,000 new cases were diagnosed between 2008 and 2017Footnote 2.
HIV testing and diagnosis is a critical first step in the HIV care cascade (HIV diagnosis, linkage to care, antiretroviral therapy initiation and achievement of viral suppression). For people living with HIV who know their status, receiving appropriate treatment reduces the long-term impact of the disease and prevents further transmissionFootnote 3.
In 2014, the Joint United Nations Programme on HIV/AIDS (UNAIDS) Programme Coordinating Board established the 90-90-90 targets with the goal of ending the AIDS epidemic by 2020. The aim of these targets are for 90% of all people living with HIV to know their HIV status, 90% of all people diagnosed with HIV to receive appropriate antiretroviral therapy (ART) and 90% of all people receiving ART to achieve viral suppressionFootnote 4Footnote 5. Canada has yet to achieve the first of these targets, and an estimated 14% of Canadians living with HIV in 2016 were unaware of their statusFootnote 2.
Although HIV testing coverage in Canada continues to expand, testing rates vary considerably across CanadaFootnote 6. Regional testing rates may be influenced by jurisdictional policies and programs determining accessibility of testing and the types of testing available (e.g. point-of-care testing)Footnote 7. Certain populations are also known to be disproportionately affected by HIV, including gay, bisexual and other men who have sex with men (gbMSM), transgender individuals, people who inject drugs (PWID) and sex workersFootnote 8Footnote 9Footnote 10Footnote 11Footnote 12. Owing to the intersection of stigma, discrimination and social determinants of health, these populations are often marginalized and underserved, leading to greater likelihood of HIV acquisition and transmission, and limited access to and uptake of testingFootnote 13Footnote 14. The differential distribution of these populations across Canada may contribute to regional variation in HIV testingFootnote 2.
A comprehensive overview of the barriers and facilitators of HIV testing that exist across key populations and jurisdictional boundaries in the current Canadian context is currently lacking. This knowledge is essential to orient public health policies and action toward the undiagnosed and mitigate the health impact of HIV in Canada. Two reviews describe the barriers and facilitators to HIV testing in the Canadian contextFootnote 7Footnote 15 and identified many barriers and facilitators to testing at the level of the individual (e.g. low risk perception, fear), healthcare provider (e.g. time constraints, insufficient resources) and institution/policy (e.g. cost/accessibility of testing)Footnote 7Footnote 15Footnote 16Footnote 17. However, these reviews were not systematic, do not cover the last decade and did not examine trends in HIV testing in key populations and in specific jurisdictions. Moreover, few studies conducted in Canada were identified in these reviews.
The objective of this systematic mixed studies review is to examine the barriers and facilitators to HIV testing that have been reported across populations and jurisdictions in Canada throughout the last decade and to conduct a narrative synthesis of identified works.
Methods
Search strategy
A systematic mixed studies review was conductedFootnote 18 of barriers and facilitators to HIV testing in Canada in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelinesFootnote 19 (appendix available upon request). Based on a pre-specified protocol and in collaboration with information specialists, the reviewers developed an electronic search strategy to identify original quantitative, qualitative and mixed-methods studies reporting on barriers and facilitators to HIV testing in Canada and published between January 1, 2009 and December 9, 2019 (appendix available upon request). Medline, Embase, PsycInfo, ProQuest Public Health, ProQuest Sociology Collection and Scopus were searched for peer-reviewed publications, and Google and Google Scholar for grey literature, government and non-governmental organization reports, and dissertations. Government webpages from each province/territory were also searched, and partners of regional offices of the Public Health Agency of Canada were consulted to retrieve other relevant works. In addition, the reference lists of included studies were manually searched for relevant publications.
Eligibility criteria
Studies were eligible for inclusion if they were original quantitative and/or qualitative studies reporting on barriers and/or facilitators to HIV testing in one or more Canadian province or territory; published between January 2009 and November 2019; and written in French or English. There were no restrictions in terms of the study sample size, type of study population or the study context/setting. Studies were excluded if they reported barriers and facilitators to testing for multiple sexually transmitted and blood-borne infections (STBBI) without reporting results for HIV separately, or if study data were collected prior to 2009.
Study selection and data collection
Two reviewers independently screened the titles and abstracts of all identified studies. Potentially relevant records were then retrieved for independent full-text review by both reviewers. Disagreements between reviewers at screening and full-text review stages were resolved by consensus.
The two reviewers independently extracted data from included studies using a piloted data extraction form that was created based on a sample of two quantitative and four qualitative studies selected for their high-quality reporting. For all included publications, the study province/territory, study aim(s), study design, population, sample size, data collection method, years of data collection, inclusion/exclusion criteria and basic demographic data of study participants including the age, sex or gender, sexual orientation and race/ethnicity were extracted. For quantitative studies, the analytical method, study exposure(s), outcome(s), covariates and main effect measures of identified barriers and facilitators to HIV testing were extracted. For qualitative studies, the analytical method and identified themes pertaining to barriers and facilitators to HIV testing were extracted.
Quality appraisal
Two investigators independently assessed the quality of included works using the Mixed Methods Appraisal Tool (MMAT)Footnote 20Footnote 21. The MMAT has been validated to critically appraise the methodological quality of studies with diverse designs. The tool includes five questions requiring "yes," "no" or "can't tell" answers. The questions are adapted to each type of study design and assess the appropriateness of the study design for the research question, the likelihood of bias and the appropriateness of measurements and analyses.
Based on the responses to these questions, a five-point quality score was created, assigning one point for each "Yes" response. Studies with four or more "Yes" answers were considered strong in quality, studies with three "Yes" answers were considered moderate in quality and studies with two or fewer "Yes" answers were considered weak in quality. Disagreements in the score assigned by both reviewers were resolved by consensus. No studies were excluded based on their quality, as the objective of this review was to synthesize all available evidence on barriers and facilitators to HIV testing in Canada. (Appendix available upon request).
Data analysis
Barriers were defined as any obstacle or reason given by study participants for declining or being unable to access HIV testing. Conversely, facilitators were defined as any reason that study participants gave for accepting or being able to access an HIV test. Sociodemographic characteristics and behaviours (e.g. age, sex/gender, sexual behaviours) that were associated with decreased or increased HIV testing uptake were considered barriers and facilitators, respectively. To avoid repetition, sociodemographic characteristics that operate both as barriers and facilitators to HIV testing are presented in terms of characteristics associated with increased testing.
Identified barriers and facilitators to HIV testing were analyzed using a convergent qualitative synthesis design in which quantitative data are transformed into qualitative findingsFootnote 18Footnote 22. The results were then integrated using inductive thematic synthesis in which themes are derived from the data without a predefined coding frame. The synthesis was guided by a conceptual framework developed by Deblonde et al. (2010)Footnote 17 that categorizes determinants of HIV testing according to the level at which they occur: the individual-level; the healthcare provider-level; and the institutional or policy level. To meet research objectives, an overall synthesis of results was conducted followed by a synthesis by key population and by jurisdiction.
Results
Study selection and characteristics
The initial search yielded 1,694 peer-reviewed studies and 49 grey literature records. After the removal of duplicates and publications not meeting eligibility criteria based on their title/abstract, 156 manuscripts were retained for full-text review. Of these, 33 peer-reviewed studiesFootnote 23Footnote 24Footnote 25Footnote 26Footnote 27Footnote 28Footnote 29Footnote 30Footnote 31Footnote 32Footnote 33Footnote 34Footnote 35Footnote 36Footnote 37Footnote 38Footnote 39Footnote 40Footnote 41Footnote 42Footnote 43Footnote 44Footnote 45Footnote 46Footnote 47Footnote 48Footnote 49Footnote 50Footnote 51Footnote 52Footnote 53Footnote 54Footnote 55 and 10 grey literature recordsFootnote 6Footnote 56Footnote 57Footnote 58Footnote 59Footnote 60Footnote 61Footnote 62Footnote 63Footnote 64 were retained (Figure 1).
Figure 1: PRISMA flow diagram
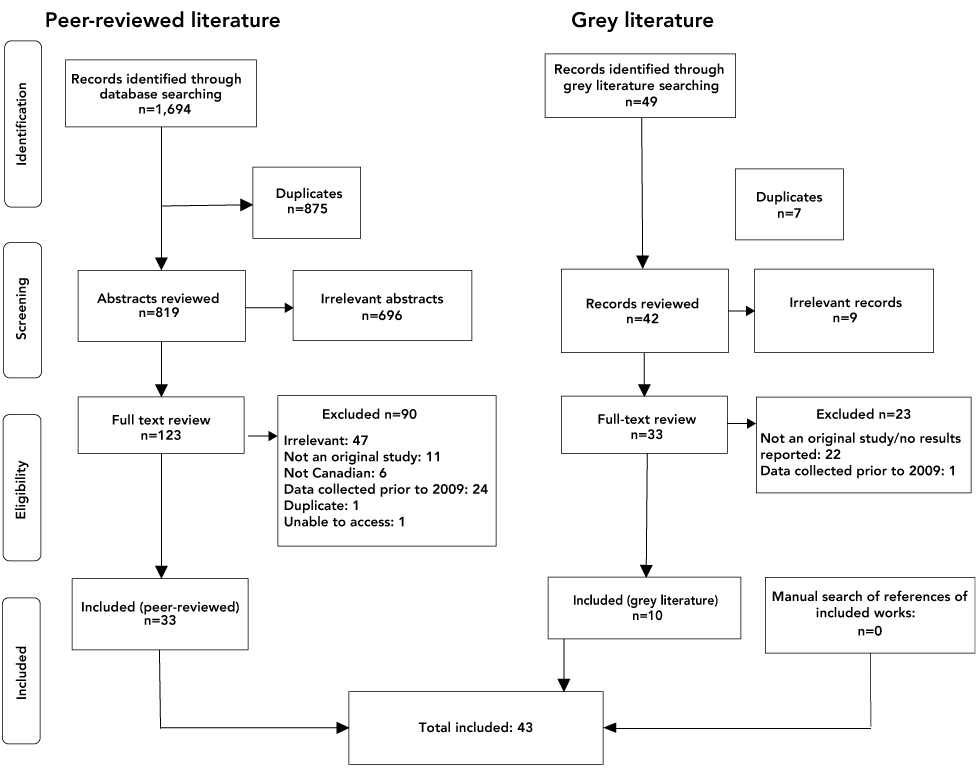
Text description: Figure 1
The figure shows the PRISMA flow diagram of manuscript identification, selection and inclusion of peer-reviewed and grey literature, in Canada from 2010 to 2019. The number of records identified through database searching for peer-reviewed literature was 1,694. After removal of duplicates, irrelevant records, and manuscripts not meeting our inclusion criteria, 33 manuscript were retained. The number of records identified through database searching for grey literature was 49. After removal of duplicates, irrelevant records, and records not meeting our inclusion criteria, 10 manuscript were retained. In total, 43 records were included in the systematic mixed studies review.
Table 1 shows the characteristics of included studies. Included studies were conducted in British Columbia (n=12)Footnote 23Footnote 24Footnote 26Footnote 27Footnote 30Footnote 32Footnote 34Footnote 37Footnote 38Footnote 43Footnote 50Footnote 52; Manitoba (n=1)Footnote 39; Ontario (n=10)Footnote 35Footnote 36Footnote 40Footnote 44Footnote 45Footnote 46Footnote 47Footnote 51Footnote 60Footnote 64; Québec (n=5)Footnote 29Footnote 41Footnote 49Footnote 58Footnote 61; Nova Scotia (n=4)Footnote 31Footnote 42Footnote 56Footnote 59; and Newfoundland and Labrador (n=1)Footnote 25. Seven studies included multiple provinces/territories (Atlantic provincesFootnote 28Footnote 62, all of CanadaFootnote 6Footnote 33Footnote 48Footnote 54Footnote 57) and two did not specify a province/territoryFootnote 53Footnote 55. Of the 43 publications, 42 were cross-sectional studies and one was a cohort study. Of these, 20 were quantitative, 13 were qualitative and 10 were mixed methods studies.
| Citation and location | Years of data collection | Study population | Sample size |
Age (years) | Male (%) | Study type | Research question | Quality score (/5) |
|---|---|---|---|---|---|---|---|---|
| Peer-reviewed literature | ||||||||
| Anderson et al., 2016Footnote 23 Vancouver, British Columbia |
2011–2014 | Migrant sex workers, managers and business owners of indoor sex work venues | 46 | Median: 42 (IQR: 24–54) |
2 | Qualitative: Semi-structured interviews with thematic analysis | Assess the impact of criminalization of sex work on HIV/STI prevention | 5 |
| Armstrong et al., 2019Footnote 24 Vancouver, British Columbia |
2012–2014 | gbMSM | 535 | Median: 30 (IQR: 24–39) |
100 | Quantitative: Questionnaire (self-administered) | Determine the reasons for HIV testing and never having tested, and explore correlates of testing | 4 |
| Boyd et al., 2019Footnote 25 Newfoundland and Labrador |
2006–2016 | Patients diagnosed with HIV | Quantitative: 58 Qualitative: 10 |
Categorical: 20–29 (20.7%), 30–39 (19.0%), 40–49 (41.4%), 50+ (19.0%) |
91.4 | Mixed methods: Semi-structured interviews with thematic analysis, and retrospective chart review | Determine the timeliness of HIV testing, missed opportunities for testing, and barriers to HIV testing | 4 |
| Brondani et al., 2016Footnote 26 Vancouver, British Columbia |
2010–2015 | General population | 519 | Categorical: 19–24 (15 %), 25–44 (74%), 45+ (11%) |
71.3 | Quantitative: Questionnaire (self-administered) | Identify patients' response to, and attitudes toward opt-out HIV rapid screening in a dental setting | 3 |
| Deering et al., 2015Footnote 27 Vancouver, British Columbia |
2010–2012 | Women sex workers | 435 | Median 35 (IQR: 38–42) |
0 | Quantitative: Questionnaire (interviewer-administered) | Assess prevalence and correlates of accessing HIV testing | 5 |
| Dube et al., 2017Footnote 28 Atlantic provinces |
NR | Stakeholders including policy makers, healthcare providers and youth | 68 | NR | NR | Qualitative: Semi-structured interviews and focus-group discussions with thematic analysis | Explore the scope and accessibility of existing youth-oriented HIV and HCV prevention | 5 |
| Engler et al., 2016Footnote 29 Montréal, Québec |
2012–2013 | Heterosexual clients of an MSM-oriented clinic | 202 | NR | 72.8 | Quantitative: Questionnaire (self-administered) | Understand the HIV prevention and sexual health service needs of heterosexual women clients of an MSM-oriented clinic | 3 |
| Feng et al., 2018Footnote 30 Vancouver, British Columbia |
2015–2016 | General population | 114 | NR | 31.2 | Mixed methods: Focus groups and individual interviews, and questionnaire (self-administered) | Determine the feasibility and acceptability of point-of-care HIV screening in dental hygiene settings | 4 |
| Gahagan et al., 2011Footnote 31 Nova Scotia |
2009–2010 | General population | Quantitative: 15,518 Qualitative: 50 |
NR | 38 | Mixed methods: Semi-structured interviews with thematic analysis, and regional HIV laboratory surveillance data | Explore the individual and structural barriers and facilitators to HIV counselling and testing | 4 |
| Gilbert et al., 2013Footnote 1Footnote 32 Vancouver, British Columbia |
2006–2012 | MSM | NR | NR | 100 | Quantitative: HIV testing laboratory surveillance data | Examine the impact of NAAT HIV testing and social marketing campaign on diagnosis of acute HIV infection among MSM | 2 |
| Gilbert et al., 2013Footnote 2Footnote 33 All provinces |
2011–2012 | MSM | 8,388 | Median: 43 (IQR: 18–84) |
100 | Quantitative: Questionnaire (self-administered) | Assess the perceived advantages and disadvantages of internet-based testing among MSM | 5 |
| Holtzman et al., 2016Footnote 34 Vancouver, British Columbia |
2010–2011 | MSM living outside major urban centres | 153 | Mean: 39.7 (SD: 15.4) |
100 | Quantitative: Questionnaire (self-administered) | Investigate behaviours and predictors of HIV testing among MSM living outside major urban centres | 5 |
| Iqbal et al., 2014Footnote 35 Ontario |
2011 | Women in labour | 92 | Mean: 32 (SD: 4.4) |
0 | Quantitative: Questionnaire (self-administered) | Assess attitudes and opinions surrounding point-of-care HIV testing | 2 |
| Kesler et al., 2018Footnote 36 Toronto, Ontario |
2010–2012 | MSM | 150 | Median: 44.5 (IQR: 37–50) |
100 | Quantitative: Questionnaire (self-administered) | Quantify the potential impact of nondisclosure prosecutions on HIV testing and transmission among MSM | 4 |
| Knight et al., 2016Footnote 1Footnote 37 Vancouver, British Columbia |
2013 | Young men | 50 | Mean: 21.7 (SD: NR) |
100 | Qualitative: Semi-structured interviews with critical discourse analysis | Explore the values that influence decisions and motivations to voluntarily access HIV testing | 4 |
| Knight et al., 2016Footnote 2Footnote 38 Vancouver, British Columbia |
2013 | Young men | 50 | NR Presumed to be the same as Knight et al., 2016Footnote 37 |
100 | Qualitative: Semi-structured interviews with grounded theory analysis | Determine how HIV-related stigma is experienced differentially across subgroups of young men within voluntary and routine testing practices | 5 |
| Lau et al., 2017Footnote 39 Winnipeg, Manitoba |
2016 | Patients admitted to inpatient care | 144 | Median: 58 (IQR: 42–68) |
48 | Quantitative: Questionnaire (interviewer-administered) | Evaluate the attitudes toward routine point-of-care HIV testing in patients admitted to inpatient care | 3 |
| Lazarus et al., 2016Footnote 40 Ottawa, Ontario |
2013 | PWID | 550 | Median: 43 (IQR 34–50), No: 39 (IQR: 30–48) |
78.2 | Quantitative: Questionnaire (interviewer-administered) | Determine the factors associated with the uptake of community-based HIV point-of-care testing | 4 |
| Lessard et al., 2015Footnote 41 Montréal, Québec |
2013–2014 | Immigrant MSM | 40 | Mean: 33 (SD: 10) |
100 | Mixed methods: Phone interview with thematic analysis | Analyze factors contributing to immigrant MSM's use of a community-based rapid HIV testing | 3 |
| Lewis et al., 2013Footnote 42 Halifax, Nova Scotia |
2011 | General population | 258 | 78.1% 20–40 | 53.5 | Quantitative: Questionnaire (self-administered) | Gauge community demand for rapid point-of-care HIV testing | 4 |
| Markwick et al., 2014Footnote 43 Vancouver, British Columbia |
2011–2012 | PWID | 600 | 50.8% >48 | 67.5 | Quantitative: Questionnaire (interviewer-administered) | Characterize PWID's willingness to receive peer-delivered voluntary counselling and HIV testing | 4 |
| O'Byrne & Bryan, 2013Footnote 44 Ottawa, Ontario |
NR | Individuals who identify as gay, bisexual, transsexual, two-spirited, queer or questioning | 721 | Mean: 37.8 (SD: 12.1) |
97.2 | Quantitative: Questionnaire (self-administered) | Examine sexual practices and STI/HIV testing and diagnosis histories | 5 |
| O'Byrne et al., 2013Footnote 1Footnote 45 Ottawa, Ontario |
NR | MSM | 441 | Mean: 38.0 (SD: 13.1) |
100 | Quantitative: Questionnaire (self-administered) | Investigate impact of nondisclosure prosecutions and HIV prevention | 5 |
| O'Byrne & Watts, 2014Footnote 46 Ottawa, Ontario |
NR | Gay male youth | 8 | Mean: 23.3 (SD: NR) |
100 | Qualitative: Semi-structured interviews with thematic analysis | Explore perceptions of stigma in health care in gay male youth | 5 |
| O'Byrne et al., 2013Footnote 2Footnote 47 Ottawa, Ontario |
NR | MSM | 27 | Categorical: 19–30 (48%), 31–40 (30%), 41–50 (13%), 51–60 (9%) |
100 | Mixed methods: Semi-structured interviews with thematic analysis | Examine HIV testing and attitudes of MSM following regional media releases about a local nondisclosure prosecution | 4 |
| Pai et al., 2018Footnote 48 All provinces |
2015 | Stakeholders involved in HIV self-testing initiatives across Canada | 183 | NR | NR | Mixed methods: Questionnaire (self-administered), open-ended questions and comments | Identify the concerns, opportunities and challenges to implementing HIV self-testing in Canada | 4 |
| Pai et al., 2014Footnote 49 Montréal, Québec |
2011–2012 | Students from a university health clinic | 145 | Median: 22 (IQR: NR) |
39.8 | Mixed methods: Questionnaire (self-administered), open-ended questions | Investigated the feasibility of offering an unsupervised self-testing strategy to Canadian students | 5 |
| Rich et al., 2017Footnote 50 Vancouver, British Columbia |
2012–2014 | Gay, bisexual and queer transgender men | 11 | Median: 26 (IQR: 25–28) |
100 | Qualitative: Semi-structured interviews with thematic analysis | Explore sexual HIV risk for transgender men in an environment of publicly funded universal access to healthcare including HIV testing and treatment | 5 |
| Scheim & Travers, 2017Footnote 51 Ontario |
2013 | Transgender MSM | 40 | Categorical: 18–24 (25%), 25–34 (48%), 35v44 (23%), 45+ (5%) |
100 | Qualitative: Semi-structured interviews with thematic analysis | Identify trans MSM's perspectives on barriers and facilitators to HIV and STI testing | 5 |
| Stenstrom et al., 2016Footnote 52 Vancouver, British Columbia |
2009–2011 | Tertiary care emergency patients | 1,402 | Mean: 43.3 (SD: 11.6) |
58.4 | Quantitative: Questionnaire (self-administered) | Estimate the acceptability of point-of-care HIV testing in an emergency department | 4 |
| Stephenson et al., 2014Footnote 53 Not specified |
2011–2012 | Male Facebook users indicating an interest in men | 344 | Categorical: 18–24 (42%), 25–34 (26%), 35–44 (13%), 45+ (19%) |
100 | Quantitative: Questionnaire (self-administered) | Examine the associations between individual characteristics and willingness of MSM couples to use couples' voluntary HIV counselling and testing | 5 |
| Worthington et al., 2015Footnote 54 All provinces/territories |
2011 | General population | 2,139 | Categorical: 16–29 (23.3%), 30–59 (50.8%), 60+ (25.9%) |
48.2 | Quantitative: Questionnaire (self-administered and interviewer-administered) | Describe voluntary HIV testing in the general population and examine individual knowledge, behaviours and sociodemographic factors associated with testing | 5 |
| Worthington et al., 2016Footnote 55 Not specified |
NR | Nurses | 40 | NR | NR | Mixed methods: Semi-structured interviews with thematic analysis | Assess the impact of an HIV care mentorship intervention on knowledge, attitudes and practices with nurses and PLWHIV | 4 |
| Grey literature | ||||||||
| Barbour, 2017Footnote 56 Halifax, Nova Scotia |
NR | Indigenous communities | 6 | NR | 50 | Qualitative: Semi-structured interviews with thematic analysis | Obtain community knowledge and understanding of the perceived barriers/facilitators associated with the access/acceptability of HIV testing within Indigenous populations | 5 |
| CATIE (Community AIDS Treatment Information Exchange), 2016Footnote 57 All provinces/territories |
2016 | Stakeholders working in HIV programming | 65 | NR | NR | Qualitative: Deliberative group dialogue | Produce key priority directions in HIV testing and linkage programming to improve the ability to reach the undiagnosed and link them to care | 2 |
| Centre Sida amitié, 2019Footnote 58 Laurentides, Québec |
NR | PLWHIV, PWID, expert partners | 196 | NR | NR | Qualitative: Questionnaire (self-administered and interviewer-administered) | Generate recommendations for communities to attain the 90-90-90 targets | 2 |
| Gahagan et al., 2012Footnote 59 Halifax, Nova Scotia |
2011 | Clients of the Halifax Sexual Health Centre | 258 | NR | NR | Mixed methods: Questionnaire (self-administered), open-ended questions | Assess performance of Anonymous HIV Testing Program, gauge clients' interest in rapid point-of-care HIV testing and willingness to pay a fee to have this testing option | 3 |
| Konkor, 2019Footnote 60 London/Ottawa /Toronto/Windsor, Ontario |
2018–2019 | Heterosexual men of ACB communities | 156 | Categorical: 16–19 (14%), 20–29 (32%), 30–39 (26%), 40–49 (16%), 50+ (12%) |
100 | Quantitative: Questionnaire (self-administered) | Identify the factors that influence uptake of HIV testing services among heterosexual ACB men | 4 |
| Messier-Peet et al., 2018Footnote 61 Montréal, Québec |
2017–2018 | gbMSM | 551 | NR | 100 | Quantitative: Questionnaire (self-administered) | Investigate factors associated with not being tested for HIV among gbMSM at high-risk for HIV | 4 |
| Our Youth, Our Response, 2014Footnote 62 Atlantic provinces |
2011–2013 | Stakeholders from government, community and research sectors, health service providers and clients of community organizations | 69 | Categorical: 16–25 (16%), 26–35 (20%), 36–45 (19%), 46–55 (20%), 56+ (19%) |
45.4 | Mixed methods: Interviews and focus groups with thematic analysis | Develop evidence-based recommendations for stakeholders in government, community and research sectors on prevention, policy and programming approaches needed to help mitigate the impact of HIV/HVC | 4 |
| PHAC, 2018Footnote 63 All provinces/territories |
2010–2012 | PWID | 2,687 | Mean: 39.4 (SD: NR) |
68.2 | Quantitative: Questionnaire (interviewer-administered) | To inform HIV prevention and control efforts, public health policy development, and program evaluation | 4 |
| Vannice, 2016Footnote 64 Ottawa, Ontario |
NR | Women in ACB communities | 10 | Range: 18–60 | 0 | Qualitative: Semi-structured interviews with thematic analysis | Examine the experiences, perceptions and knowledge regarding HIV testing among ACB women | 3 |
| Wertheimer, 2011Footnote 6 All provinces/territories |
2009–2010 | Service providers | Quantitative: 75 Qualitative: 15 |
NR | NR | Mixed methods: Questionnaire (self-administered online), individual interviews | Identify the barriers that affect women's access to HIV testing | 2 |
Quality appraisal
Most of the included publications were of strong quality (n=32; 74%), while some were moderate (n=6; 14%) or weak quality (n=5; 12%). (Appendix available upon request). The weakest element in the qualitative studies was a lack of the detail necessary for an evaluation of whether the data substantiated the interpretation of results. The weakest element in the quantitative studies was the risk of non-response bias, which is expected as many of these studies were conducted in hard-to-reach populations. The weakest element in the mixed methods studies was a lack of consideration of divergence between qualitative and quantitative results.
Synthesis of results
The following narrative synthesis of results summarizes identified barriers and facilitators overall and by key population and jurisdiction. Sociodemographic characteristics and behaviours associated with HIV testing are presented separately because they represent individual-level drivers of testing uptake rather than external barriers/facilitators.
Overview of barriers and facilitators to HIV testing
At the level of the individual, several barriers to HIV testing emerged across multiple contexts: fear of receiving a positive resultFootnote 6Footnote 25Footnote 39Footnote 56Footnote 58Footnote 64; stigma surrounding HIV and behaviours or identities perceived to be associated with HIVFootnote 23Footnote 31Footnote 38Footnote 41Footnote 56Footnote 58Footnote 60Footnote 64; the perception of being at low risk for exposure to HIVFootnote 6Footnote 24Footnote 26Footnote 50Footnote 51Footnote 61Footnote 62; insufficient knowledge of HIV and testing optionsFootnote 56Footnote 61Footnote 64 ; difficulty accessing testing services, for example, limited clinic opening hours, difficulty getting an appointmentFootnote 23Footnote 28Footnote 41Footnote 58Footnote 60Footnote 64; and insufficient confidentiality in testing servicesFootnote 28Footnote 41Footnote 42Footnote 56Footnote 58Footnote 64. Certain sociodemographic characteristics were identified as being associated with increased testing, including engaging in behaviours associated with HIV (e.g. increased number of sexual partners, injection drug use)Footnote 24Footnote 27Footnote 40Footnote 54Footnote 60Footnote 61Footnote 63 and having been previously tested for STBBIFootnote 24Footnote 25Footnote 38.
At the level of the healthcare provider, common barriers were identified as HIV-related stigma from healthcare providersFootnote 46Footnote 57; perception that a patient is at low risk of HIV exposureFootnote 6Footnote 64; and reluctance/refusal to offer testing for individuals who were not perceived to be at riskFootnote 38Footnote 58. Many studies reported healthcare providers suggesting an HIV testFootnote 25Footnote 26Footnote 58 and that non-stigmatizing healthcare practicesFootnote 23Footnote 50Footnote 51 facilitated testing.
At the institutional or policy level, the criminalization of certain behaviours (e.g. sex work, drug use, HIV nondisclosure)Footnote 23Footnote 57 and the lack of resources and adequate healthcare infrastructure in rural and remote regionsFootnote 28Footnote 56Footnote 58Footnote 62 represent structural barriers to testing. Conversely, policies and institutional practices that increase the accessibility, convenience and confidentiality of testing (e.g. broad range of testing options, reducing wait times, low-cost testing)Footnote 6Footnote 23Footnote 25Footnote 26Footnote 27Footnote 29Footnote 41Footnote 49Footnote 50Footnote 51Footnote 58Footnote 62 and integrate testing with routine healthcare servicesFootnote 25Footnote 31Footnote 38Footnote 51Footnote 58Footnote 63Footnote 64, educational/promotional campaignsFootnote 6Footnote 28Footnote 32Footnote 62Footnote 64 and intersectoral collaborationFootnote 6Footnote 28Footnote 62 were reported as facilitators to testing.
Results by key population
A large number of studies focused on gbMSM (n=15)Footnote 24Footnote 32Footnote 33Footnote 34Footnote 36Footnote 37Footnote 38Footnote 44Footnote 45Footnote 46Footnote 47Footnote 50Footnote 51Footnote 53Footnote 61, reflecting the historical epidemiology of HIV in Canada. Other key populations include sex workers (n=2)Footnote 23Footnote 27, PWID (n=3)Footnote 43Footnote 58Footnote 63 , immigrant populations (n=3)Footnote 23Footnote 41Footnote 60, Indigenous communities (n=1)Footnote 56, and African, Caribbean and Black communities (n=2)Footnote 60Footnote 64. Results are summarized by key population to highlight the unique needs and context of each population in Table 2.
| Population type | Provinces reporting on population | Barriers | Facilitators |
|---|---|---|---|
| gbMSM (including two-spirited, queer, trans or questioning) | All provinces |
|
|
| Sex workers (including managers and business owners of sex work venues) | British Columbia |
|
|
| PWID | All provinces |
|
|
| Immigrant populations | British Columbia, Ontario, Québec |
|
|
| Indigenous communities | Nova Scotia |
|
|
| African, Caribbean and Black communities | Ontario |
|
|
Several barriers to HIV testing were common across key populations. These included the fear of a positive diagnosisFootnote 23Footnote 41Footnote 51Footnote 56Footnote 64; experiences of HIV-related stigmaFootnote 41Footnote 56, the perception of being at low risk for exposure to HIVFootnote 24Footnote 50Footnote 51Footnote 56Footnote 63; limited accessibility of testing servicesFootnote 23Footnote 27Footnote 41Footnote 56Footnote 60Footnote 64; and insufficient knowledge about HIVFootnote 56Footnote 64. Other common barriers represent particularly significant obstacles to testing for marginalized populations, including stigma relating to behaviours or identities perceived to be associated with HIV (e.g. sexual behaviours, sexual orientation, sex work, injection drug use)Footnote 23Footnote 24Footnote 31Footnote 41Footnote 46Footnote 50Footnote 51Footnote 56Footnote 60Footnote 64 and insufficient confidentiality in testing services, including the lack of anonymous testing and concerns about privacy in small or remote communitiesFootnote 23Footnote 41Footnote 44Footnote 47Footnote 56Footnote 64.
Other barriers were unique to key populations. Legislation that criminalizes HIV nondisclosure and sex work are barriers to testing among gbMSMFootnote 36Footnote 45Footnote 47 and sex workersFootnote 23, respectively. In addition, insufficient knowledge about the health-related concerns and needs of certain populations (e.g. gbMSM/transgender identities, sex workers) by healthcare providers is an obstacle to testing in these populationsFootnote 23Footnote 51Footnote 56Footnote 60. Many populations also face distinct issues of accessibility, such as limited availability of multilingual health services and lack of health insurance among immigrant populationsFootnote 23Footnote 41Footnote 60, and geographic barriers to health care in rural and remote Indigenous communitiesFootnote 56.
Despite the diverse contexts of these populations, several common facilitators emerged. Offering HIV testing in a broad range of modalities (e.g. anonymous testing, unsupervised self-testing) and settings (e.g. mobile clinics, point-of-care testing)Footnote 23Footnote 27Footnote 33Footnote 56 as well as the integration of members of key populations with lived experience (e.g. peer-delivered post-test counselling, community-based outreach initiatives)Footnote 43Footnote 56Footnote 64 were frequently identified as means to improve the accessibility and acceptability of HIV testing services to key populations.
Finally, some facilitators were uniquely relevant for certain key populations. Healthcare practices that are inclusive and non-stigmatizing were identified as important facilitators by queer and transgender communitiesFootnote 50Footnote 51. The availability of translators or multilingual health services facilitated testing for immigrant populationsFootnote 23. Among the African, Caribbean and Black community, enabling social connections with people living with HIV and educational initiatives focused on navigating cultural silences around HIV facilitated testingFootnote 64.
Results by jurisdiction
Identified sociodemographic characteristics associated with HIV testing, and barriers and facilitators to HIV testing are summarized by jurisdiction in Table 3.
| Province/territory | Individual level | Healthcare provider level | Policy level |
|---|---|---|---|
| British Columbia | |||
| Sociodemographic characteristics and behaviours associated with increased HIV testing |
|
|
|
| Barriers |
|
|
|
| Facilitators |
|
|
|
| Manitoba | |||
| Barriers |
|
|
|
| Ontario | |||
| Sociodemographic characteristics and behaviours associated with increased HIV testing |
|
|
|
| Barriers |
|
|
|
| Facilitators |
|
|
|
| Québec | |||
| Sociodemographic characteristics and behaviours associated with increased HIV testing |
|
|
|
| Barriers |
|
|
|
| Facilitators |
|
|
|
| Nova Scotia | |||
| Sociodemographic characteristics and behaviours associated with increased HIV testing |
|
|
|
| Barriers |
|
|
|
| Facilitators |
|
|
|
| Newfoundland and Labrador | |||
| Sociodemographic characteristics and behaviours associated with increased HIV testing |
|
|
|
| Barriers |
|
|
|
| Facilitators |
|
|
|
| Atlantic provinces | |||
| Barriers |
|
|
|
| Facilitators |
|
|
|
| Canada-wide or unspecified provinces/territories | |||
| Sociodemographic characteristics and behaviours associated with increased HIV testing |
|
|
|
| Barriers |
|
|
|
| Facilitators |
|
|
|
Although jurisdictions share many common barriers and facilitators to HIV testing, several trends emerged in particular jurisdictions. Studies conducted in British Colombia highlight the criminalization and stigmatization of sex work and issues related to immigrant status as major barriers to HIV testingFootnote 23Footnote 24Footnote 27. Studies conducted in Ontario feature cultural barriers and issues of stigma and fear of behaviours associated with HIV more prominently than other jurisdictionsFootnote 38Footnote 60Footnote 64. Studies conducted in the Atlantic provinces uniquely highlight youth-adapted services as a key facilitatorFootnote 28Footnote 62. Differences in the barriers and facilitators to HIV testing across jurisdictions were driven primarily by differential presence of key populations across jurisdictions and reflect regional public health priorities.
Discussion
In this systematic mixed studies review, it included results from 43 studies conducted in Canada to document and understand recent and emerging barriers and facilitators to HIV testing in the last decade. The principal motivation was to orient future research and public health action toward reaching the first global HIV target in Canada, taking into consideration key populations and jurisdictional contexts. Another motivation was to identify specific areas for intervention to improve access to HIV testing in a broad range of contexts, including providing accessible, low-cost and convenient testing, ensuring confidentiality, reducing HIV-related stigma, improving education about HIV (e.g. modes of transmission, testing, treatments), normalizing offering HIV testing and integrating testing into routine healthcare practices.
Common barriers emerge across key populations and jurisdictions, including low risk perception, fear and stigma surrounding HIV, lack of knowledge of HIV and testing, insufficient patient confidentiality, limited access to cultural and linguistically appropriate services and lack of resources for testingFootnote 7Footnote 15. This review identified several emerging innovative practices, including integrating HIV point-of-care testing in a variety of new settings including Internet-based HIV testingFootnote 33, sex work venuesFootnote 27, dental careFootnote 26Footnote 30 , emergency roomsFootnote 52, pharmaciesFootnote 59 and in mobile testing unitsFootnote 26Footnote 27. Several innovative testing modalities were also identified: couples voluntary HIV counselling and testingFootnote 53, oral swab and oral-self testingFootnote 26Footnote 49 and peer-delivered post-test counsellingFootnote 43. Gender-based approachesFootnote 28, queer and transgender-competent healthcare providers and adapted interventions and approachesFootnote 50, age-adapted education and promotion material, testing sites (e.g. school-based clinics for youth) and youth engagement in the development and implementation of HIV prevention initiatives were also clearly identified as important facilitatorsFootnote 62.
The evidence summarized above highlights the importance of adapting public health policy and programming to the unique contexts of each jurisdiction, including the distribution of key populations and burden of disease. Potential strategies for improving access to HIV testing among key populations include increasing the accessibility of HIV testing by expanding available testing options and promoting health outreach initiatives for hard-to-reach populations. In addition, ensuring inclusive and non-stigmatizing healthcare services and integrating the knowledge of members of these communities are essential to improve the acceptability of HIV testing to key populations. Policy makers and healthcare providers should also consider the intersectionality of identities and experiences in order to better understand the specific drivers of HIV testing in each populationFootnote 65. These results underscore the importance of adopting a person-centred approach to HIV testing and the need to reach people where they are.
Many of the barriers and facilitators identified in this review operate at the institutional/policy level, potentially indicating an increased focus on up-stream determinants of HIV testing in the last decade. This recent trend underscores the importance of public health action at the systemic level and suggests that HIV testing initiatives could be enhanced by leveraging the expertise of a range of stakeholders including community partners, primary health care, harm reduction services and public health authorities. Expanding intersectoral partnership and collaboration may offer important opportunities to bridge testing gaps and ensure equitable access to HIV testing.
The Pan-Canadian Framework recognizes the importance of testing in achieving global STBBI targets and outlines specific opportunities for action that align with the facilitators identified in this reviewFootnote 66. As outlined in the Government of Canada STBBI action planFootnote 67, improving access to STBBI testing is a core component of a coordinated approach to reducing the impact of STBBI in Canada, with a particular focus on populations that are disproportionately affected by STBBI. This review contributes to existing knowledge of the drivers of HIV testing in Canada and highlights several important gaps and opportunities that can be used to inform public health action toward this goal.
Strengths and limitations
A major strength of this work is the systematic mixed studies review design, which synthesizes quantitative and qualitative data in order to answer complex research questions such as the identification of determinants of HIV testingFootnote 18. The inclusion of multiple forms of evidence creates a rich synthesis of extant barriers and facilitators by combining diverse perspectives (i.e. population-level data and individual experiences) and produces results that are directly relevant to decision-makersFootnote 22. In addition, the broad scope allows for the identification of emerging and lesser known barriers and facilitators, as well as population and jurisdiction-specific trends in HIV testing in Canada, informing targeted public health actionFootnote 68.
Nevertheless, this review has limitations. It is possible that some relevant works were not identified by our search strategy and so certain barriers/facilitators may be absent from this synthesis. In addition, the intrinsic nature of the data made it impossible to assess the causal nature of any of the identified barriers or facilitators.
This review may also be limited by publication bias, as published literature reflects historical and regional contexts and priorities, potentially resulting in gaps in the literature to do with non-priority populations and settings. As such, although this review presents results across populations and jurisdictions, some key populations (e.g. PWID, sex workers, immigrants, Indigenous communities and African, Caribbean and Black communities) and some provinces (e.g. Alberta, Manitoba, Saskatchewan) and the territories are underrepresented, potentially limiting the generalizability of results. In addition, emerging key populations may be missing.
Finally, the scope of this review was limited to barriers and facilitators of HIV testing and may omit other important shared barriers and facilitators to testing for other STBBI.
Conclusion
HIV testing acts as the gateway for HIV treatment and prevention and is a core pillar of Canada’s efforts to reduce the health impact of HIV and other STBBI. This work provides a comprehensive and detailed understanding of the barriers and facilitators to HIV testing in Canada and highlights several important factors that can be leveraged to increase HIV testing. The results provide key evidence to influence practice, policy and future research toward achieving global HIV targets.
Authors’ statement
CL and CBF contributed equally to this work: conceptualization, development of search strategy, screening of identified works for inclusion, quality appraisal, data extraction, analysis and interpretation of data and manuscript preparation.
Competing interests
The authors have no conflicts of interest to declare.
Acknowledgements
We would like to thank L Pogany, J Insogna and G Tremblay from the Public Health Agency of Canada’s Centre for Communicable Disease and Infection Control, in Ottawa, as well as A Blair, L Turcotte and D Parisien from the Public Health Agency of Canada’s Québec Regional Office, in Montréal for their contribution to the conceptualization and design of this review. Finally, we would like to thank K Merucci and L Glandon from the Health Canada Library, in Ottawa, for their assistance in the development of the search strategy.
Funding
This work was supported by the Public Health Agency of Canada.
References
- Footnote 1
-
World Health Organization. Global HIV, hepatitis and STIs programme. HIV data and statistics. Geneva (CH): WHO; 2020 (accessed 2020-11-19). https://www.who.int/hiv/data/en/
- Footnote 2
-
Public Health Agency of Canada. Summary: Estimates of HIV incidence, prevalence and Canada's progress on meeting the 90-90-90 HIV targets, 2016. Ottawa (ON): PHAC; 2018. https://www.canada.ca/en/public-health/services/publications/diseases-conditions/summary-estimates-hiv-incidence-prevalence-canadas-progress-90-90-90.html
- Footnote 3
-
Samji H, Cescon A, Hogg RS, Modur SP, Althoff KN, Buchacz K, Burchell AN, Cohen M, Gebo KA, Gill MJ, Justice A, Kirk G, Klein MB, Korthuis PT, Martin J, Napravnik S, Rourke SB, Sterling TR, Silverberg MJ, Deeks S, Jacobson LP, Bosch RJ, Kitahata MM, Goedert JJ, Moore R, Gange SJ; North American AIDS Cohort Collaboration on Research and Design (NA-ACCORD) of IeDEA. Closing the gap: increases in life expectancy among treated HIV-positive individuals in the United States and Canada. PLoS One 2013;8(12):e81355. https://doi.org/10.1371/journal.pone.0081355
- Footnote 4
-
UNAIDS. Knowledge is power-Know your status, know your viral load. Geneva (CH): UNAIDS; 2018. https://www.unaids.org/en/resources/documents/2018/knowledge-is-power-report
- Footnote 5
-
UNAIDS. 90-90-90: An ambitious treatment target to help end the AIDS epidemic. Geneva (CH): UNAIDS; 2014. https://www.unaids.org/sites/default/files/media_asset/90-90-90_en.pdf
- Footnote 6
-
Wertheimer S. Women and HIV testing in Canada: barriers and recommendations as identified by service providers: a summary of key research findings. Ottawa (ON): Canadian AIDS Society; 2011. https://www.cdnaids.ca/wp-content/uploads/Women-and-HIV-Testing-in-Canada-A-Summary-of-Key-Research-Findings.pdf
- Footnote 7
-
Traversy GP, Austin T, Ha S, Timmerman K, Gale-Rowe M. An overview of recent evidence on barriers and facilitators to HIV testing. Can Commun Dis Rep 2015;41(12):302-21. https://doi.org/10.14745/ccdr.v41i12a02
- Footnote 8
-
MacCarthy S, Poteat T, Xia Z, Roque NL, Hyun Jin Kim A, Baral S, Reisner SL. Current research gaps: a global systematic review of HIV and sexually transmissible infections among transgender populations. Sex Health 2017;14(5):456-68. https://doi.org/10.1071/SH17096
- Footnote 9
-
Degenhardt L, Charlson F, Stanaway J, Larney S, Alexander LT, Hickman M, Cowie B, Hall WD, Strang J, Whiteford H, Vos T. Estimating the burden of disease attributable to injecting drug use as a risk factor for HIV, hepatitis C, and hepatitis B: findings from the Global Burden of Disease Study 2013. Lancet Infect Dis 2016;16(12):1385-98. https://doi.org/10.1016/S1473-3099(16)30325-5
- Footnote 10
-
Baral S, Beyrer C, Muessig K, Poteat T, Wirtz AL, Decker MR, Sherman SG, Kerrigan D. Burden of HIV among female sex workers in low-income and middle-income countries: a systematic review and meta-analysis. Lancet Infect Dis 2012;12(7):538-49. https://doi.org/10.1016/S1473-3099(12)70066-X
- Footnote 11
-
Iles L, Consolacion T, Wong J, Grennan T, Gilbert M, Prescott C, Moore D. HIV diagnoses and testing patterns among young gay, bisexual and other men who have sex with men: an analysis of HIV surveillance data in British Columbia, 2008-2015. Can J Public Health 2019;110(5):668-74. https://doi.org/10.17269/s41997-019-00225-0
- Footnote 12
-
Dolan K, Wirtz AL, Moazen B, Ndeffo-Mbah M, Galvani A, Kinner SA, Courtney R, McKee M, Amon JJ, Maher L, Hellard M, Beyrer C, Altice FL. Global burden of HIV, viral hepatitis, and tuberculosis in prisoners and detainees. Lancet 2016;388(10049):1089–102. https://doi.org/10.1016/S0140-6736(16)30466-4
- Footnote 13
-
Fitzgerald-Husek A, Van Wert MJ, Ewing WF, Grosso AL, Holland CE, Katterl R, Rosman L, Agarwal A, Baral SD. Measuring stigma affecting sex workers (SW) and men who have sex with men (MSM): A systematic review. PLoS One 2017;12(11):e0188393. https://doi.org/10.1371/journal.pone.0188393
- Footnote 14
-
DeBeck K, Cheng T, Montaner JS, Beyrer C, Elliott R, Sherman S, Wood E, Baral S. HIV and the criminalisation of drug use among people who inject drugs: a systematic review. Lancet HIV 2017;4(8):e357–74. https://doi.org/10.1016/S2352-3018(17)30073-5
- Footnote 15
-
Kaai S, Bullock S, Burchell AN, Major C. Factors that affect HIV testing and counseling services among heterosexuals in Canada and the United Kingdom: an integrated review. Patient Educ Couns 2012;88(1):4–15. https://doi.org/10.1016/j.pec.2011.11.011
- Footnote 16
-
Bolsewicz K, Vallely A, Debattista J, Whittaker A, Fitzgerald L. Factors impacting HIV testing: a review--perspectives from Australia, Canada, and the UK. AIDS Care 2015;27(5):570–80. https://doi.org/10.1080/09540121.2014.986050
- Footnote 17
-
Deblonde J, De Koker P, Hamers FF, Fontaine J, Luchters S, Temmerman M. Barriers to HIV testing in Europe: a systematic review. Eur J Public Health 2010;20(4):422–32. https://doi.org/10.1093/eurpub/ckp231
- Footnote 18
-
Pluye P, Hong QN. Combining the power of stories and the power of numbers: mixed methods research and mixed studies reviews. Annu Rev Public Health 2014;35:29–45. https://doi.org/10.1146/annurev-publhealth-032013-182440
- Footnote 19
-
Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009;339:b2535. https://doi.org/10.1136/bmj.b2535
- Footnote 20
-
Hong QN, Gonzalez-Reyes A, Pluye P. Improving the usefulness of a tool for appraising the quality of qualitative, quantitative and mixed methods studies, the Mixed Methods Appraisal Tool (MMAT). J Eval Clin Pract 2018;24(3):459–67. https://doi.org/10.1111/jep.12884
- Footnote 21
-
Pace R, Pluye P, Bartlett G, Macaulay AC, Salsberg J, Jagosh J, Seller R. Testing the reliability and efficiency of the pilot Mixed Methods Appraisal Tool (MMAT) for systematic mixed studies review. Int J Nurs Stud 2012;49(1):47–53. https://doi.org/10.1016/j.ijnurstu.2011.07.002
- Footnote 22
-
Hong QN, Pluye P, Bujold M, Wassef M. Convergent and sequential synthesis designs: implications for conducting and reporting systematic reviews of qualitative and quantitative evidence. Syst Rev 2017;6(1):61. https://doi.org/10.1186/s13643-017-0454-2
- Footnote 23
-
Anderson S, Shannon K, Li J, Lee Y, Chettiar J, Goldenberg S, Krüsi A. Condoms and sexual health education as evidence: impact of criminalization of in-call venues and managers on migrant sex workers access to HIV/STI prevention in a Canadian setting. BMC Int Health Hum Rights 2016;16(1):30. https://doi.org/10.1186/s12914-016-0104-0
- Footnote 24
-
Armstrong HL, Wang L, Zhu J, Lachowsky NJ, Card KG, Wong J, Jollimore J, Edward J, Roth EA, Hogg RS, Moore DM. HIV testing among a representative community sample of gay, bisexual, and other men who have sex with men in Vancouver, Canada. AIDS Behav 2019;23(2):347–58. https://doi.org/10.1007/s10461-018-2259-2
- Footnote 25
-
Boyd SE, Allison J, Penney CC, Burt K, Allison D, Daley PK. Timeliness of diagnosis of HIV in Newfoundland and Labrador, Canada: a mixed-methods study. JAMMI 2019;4(1):15–23. https://doi.org/10.3138/jammi.2018-0029
- Footnote 26
-
Brondani M, Chang S, Donnelly L. Assessing patients’ attitudes to opt-out HIV rapid screening in community dental clinics: a cross-sectional Canadian experience. BMC Res Notes 2016;9:264. https://doi.org/10.1186/s13104-016-2067-6
- Footnote 27
-
Deering KN, Montaner JS, Chettiar J, Jia J, Ogilvie G, Buchner C, Feng C, Strathdee SA, Shannon K. Successes and gaps in uptake of regular, voluntary HIV testing for hidden street- and off-street sex workers in Vancouver, Canada. AIDS Care 2015;27(4):499–506. https://doi.org/10.1080/09540121.2014.978730
- Footnote 28
-
Dube A, Harris G, Gahagan J, Doucet S. Bridging the silos in HIV and Hepatitis C prevention: a cross-provincial qualitative study. Int J Public Health 2017;62(7):739–46. https://doi.org/10.1007/s00038-016-0914-9
- Footnote 29
-
Engler K, Rollet K, Lessard D, Thomas R, Lebouché B. Explaining the presence of “heterosexual” female clients of a rapid HIV testing site located in the gay village of Montreal, Quebec. J Prim Care Community Health 2016;7(2):122–9. https://doi.org/10.1177/2150131915626563
- Footnote 30
-
Feng I, Brondani M, Chong KL, Donnelly L. Evaluating point-of-care HIV screening in dental hygiene education settings: patient, faculty, and student perspectives. J Dent Educ 2018;82(8):819–27. https://doi.org/10.21815/JDE.018.076
- Footnote 31
-
Gahagan JC, Fuller JL, Proctor-Simms EM, Hatchette TF, Baxter LN. Barriers to gender-equitable HIV testing: going beyond routine screening for pregnant women in Nova Scotia, Canada. Int J Equity Health 2011;10(1):18. https://doi.org/10.1186/1475-9276-10-18
- Footnote 32
-
Gilbert M, Cook D, Steinberg M, Kwag M, Robert W, Doupe G, Krajden M, Rekart M. Targeting screening and social marketing to increase detection of acute HIV infection in men who have sex with men in Vancouver, British Columbia. AIDS 2013;27(16):2649–54. https://doi.org/10.1097/QAD.0000000000000001
- Footnote 33
-
Gilbert M, Hottes TS, Kerr T, Taylor D, Fairley CK, Lester R, Wong T, Trussler T, Marchand R, Shoveller J, Ogilvie G. Factors associated with intention to use internet-based testing for sexually transmitted infections among men who have sex with men. J Med Internet Res 2013;15(11):e254. https://doi.org/10.2196/jmir.2888
- Footnote 34
-
Holtzman S, Landis L, Walsh Z, Puterman E, Roberts D, Saya-Moore K. Predictors of HIV testing among men who have sex with men: a focus on men living outside major urban centres in Canada. AIDS Care 2016;28(6):705–11. https://doi.org/10.1080/09540121.2016.1164288
- Footnote 35
-
Iqbal S, De Souza LR, Yudin MH. Acceptability, predictors and attitudes of Canadian women in labour toward point-of-care HIV testing at a single labour and delivery unit. Can J Infect Dis Med Microbiol 2014;25(4):201–6. https://doi.org/10.1155/2014/160370
- Footnote 36
-
Kesler MA, Kaul R, Loutfy M, Myers T, Brunetta J, Remis RS, Gesink D. Prosecution of non-disclosure of HIV status: potential impact on HIV testing and transmission among HIV-negative men who have sex with men. PLoS One 2018;13(2):e0193269. https://doi.org/10.1371/journal.pone.0193269
- Footnote 37
-
Knight R, Small W, Shoveller J. How do ‘public’ values influence individual health behaviour? An empirical-normative analysis of young men’s discourse regarding HIV testing practices. Public Health Ethics 2016;9(3):264–75. https://doi.org/10.1093/phe/phv031
- Footnote 38
-
Knight R, Small W, Shoveller JA. HIV stigma and the experiences of young men with voluntary and routine HIV testing. Sociol Health Illn 2016;38(1):153–67. https://doi.org/10.1111/1467-9566.12345
- Footnote 39
-
Lau L, Wudel B, Lee E, Darraj M, Richert Q, Trajtman A, Bresler K, Bullard J, Kasper K, Becker M, Keynan Y. Evaluation of the utility of point-of-care HIV testing on a Canadian internal medicine inpatient unit. Can J Infect Dis Med Microbiol 2017;2017:8495307. https://doi.org/10.1155/2017/8495307
- Footnote 40
-
Lazarus L, Patel S, Shaw A, Leblanc S, Lalonde C, Hladio M, Mandryk K, Horvath C, Petrcich W, Kendall C, Tyndall MW; Proud Community Advisory Committee. Uptake of community-based peer administered HIV point-of-care testing: findings from the PROUD study. PLoS One 2016;11(12):e0166942. https://doi.org/10.1371/journal.pone.0166942
- Footnote 41
-
Lessard D, Lebouché B, Engler K, Thomas R, Machouf N. Explaining the appeal for immigrant men who have sex with men of a community-based rapid HIV-testing site in Montreal (Actuel sur Rue). AIDS Care 2015;27(9):1098–103. https://doi.org/10.1080/09540121.2015.1028880
- Footnote 42
-
Lewis NM, Gahagan JC, Stein C. Preferences for rapid point-of-care HIV testing in Nova Scotia, Canada. Sex Health 2013;10(2):124–32. https://doi.org/10.1071/SH12100
- Footnote 43
-
Markwick N, Ti L, Callon C, Feng C, Wood E, Kerr T. Willingness to engage in peer-delivered HIV voluntary counselling and testing among people who inject drugs in a Canadian setting. J Epidemiol Community Health 2014;68(7):675–8. https://doi.org/10.1136/jech-2013-203707
- Footnote 44
-
O’Byrne P, Bryan A. Anonymous HIV testing and public health in Ontario, Canada: understanding HIV surveillance. Surveill Soc 2013;11(1):35–54. https://doi.org/10.24908/ss.v11i1/2.4326
- Footnote 45
-
O’Byrne P, Bryan A, Woodyatt C. Nondisclosure prosecutions and HIV prevention: results from an Ottawa-based gay men’s sex survey. J Assoc Nurses AIDS Care 2013;24(1):81–7. https://doi.org/10.1016/j.jana.2012.01.009
- Footnote 46
-
O’Byrne P, Watts J. Include, differentiate and manage: gay male youth, stigma and healthcare utilization. Nurs Inq 2014 Mar;21(1):20–9. https://doi.org/10.1111/nin.12014
- Footnote 47
-
O’Byrne P, Willmore J, Bryan A, Friedman DS, Hendriks A, Horvath C, Massenat D, Bouchard C, Remis RS, Etches V. Nondisclosure prosecutions and population health outcomes: examining HIV testing, HIV diagnoses, and the attitudes of men who have sex with men following nondisclosure prosecution media releases in Ottawa, Canada. BMC Public Health 2013;13(1):94. https://doi.org/10.1186/1471-2458-13-94
- Footnote 48
-
Pai NP, Smallwood M, Gulati D, Lapczak N, Musten A, Gaydos C, Johnston C, Steben M, Wong T, Engel N, Kim J. What do key stakeholders think about HIV self-testing in Canada? Results from a cross-sectional survey. AIDS Behav 2018;22(2):606–15. https://doi.org/10.1007/s10461-017-1764-z
- Footnote 49
-
Pant Pai N, Bhargava M, Joseph L, Sharma J, Pillay S, Balram B, Tellier PP. Will an unsupervised self-testing strategy be feasible to operationalize in Canada? Results from a pilot study in students of a large canadian university. Aids Res Treat 2014;2014(747619):1–8. https://doi.org/10.1155/2014/747619
- Footnote 50
-
Rich A, Scott K, Johnston C, Blackwell E, Lachowsky N, Cui Z, Sereda P, Moore D, Hogg R, Roth E. Sexual HIV risk among gay, bisexual and queer transgender men: findings from interviews in Vancouver, Canada. Cult Health Sex 2017;19(11):1197–209. https://doi.org/10.1080/13691058.2017.1299882
- Footnote 51
-
Scheim AI, Travers R. Barriers and facilitators to HIV and sexually transmitted infections testing for gay, bisexual, and other transgender men who have sex with men. AIDS Care 2017;29(8):990–5. https://doi.org/10.1080/09540121.2016.1271937
- Footnote 52
-
Stenstrom R, Ling D, Grafstein E, Barrios R, Sherlock C, Gustafson R, Osati F, Poureslami I, Anis A. Prevalence of HIV infection and acceptability of point-of-care testing in a Canadian inner-city emergency department. Can J Public Health 2016 Oct;107(3):e291–5. https://doi.org/10.17269/CJPH.107.5318
- Footnote 53
-
Stephenson R, Chard A, Finneran C, Sullivan P. Willingness to use couples voluntary counseling and testing services among men who have sex with men in seven countries. AIDS Care 2014;26(2):191–8. https://doi.org/10.1080/09540121.2013.808731
- Footnote 54
-
Worthington CA, Calzavara LM, White SJ, Allman D, Tyndall MW. Individual and jurisdictional factors associated with voluntary HIV testing in Canada: results of a national survey, 2011. Can J Public Health 2014;106(2):e4–9. https://doi.org/10.17269/CJPH.106.4625
- Footnote 55
-
Worthington CA, O’Brien KK, Mill J, Caine V, Solomon P, Chaw-Kant J. A mixed-methods outcome evaluation of a mentorship intervention for Canadian nurses in HIV care. J Assoc Nurses AIDS Care 2016;27(5):677–97. https://doi.org/10.1016/j.jana.2016.02.011
- Footnote 56
-
Barbour TL. HIV testing in Nova Scotia: an Indigenous perspective on access and acceptability. Halifax, (NS): Dalhousie University; 2017. https://dalspace.library.dal.ca/bitstream/handle/10222/73293/Barbour-Tammy-MA-August-29-2017.pdf?sequence=3&isAllowed=y
- Footnote 57
-
CATIE. National deliberative dialogue on reaching the HIV undiagnosed: scaling up effective programming approaches to HIV testing and linkage to prevention and care. Thursday, October 13 and Friday, October 14, 2016. Meeting report. Toronto (ON): Canada's source for HIV and hepatitis C information; 2016. https://www.catie.ca/ga-pdf.php?file=sites/default/files/Reaching-the-hiv-undiagnosed-EN.pdf
- Footnote 58
-
Centre SIDA Amitié. Rapport d58e recommandations de lutte contre le VIH et le sida pour atteindre les cibles mondiales à l'échelle régionale. Saint-Jérôme (QC) : Centre SIDA Amitié; 2019. https://centresidaamitie.app.box.com/s/2bq649o1iueolzfpzzqqydz7oc9t4l9n
- Footnote 59
-
Gahagan J, Stein C, Campbell A. Report on anonymous HIV Testing program and perceptions of acceptability of rapid point-of-care testing at Halifax Sexual Health Centre, Halifax, Nova Scotia. Halifax (NS): Halifax Sexual Health Center; 2012. https://novascotia.ca/aids/documents/Report-Anonymous-HIV-Testing-Program-HSHC-2012.pdf
- Footnote 60
-
Konkor I. HIV vulnerabilities among heterosexual African, Caribbean and other Black men in London, Ontario. London (ON): University of Western Ontario; 2019. https://ir.lib.uwo.ca/etd/6243/
- Footnote 61
-
Messier-Peet M, Apelian H, Moodie E, Cox J, Hart T, Grace D, Moore D, Lachowsky N, Jollimore J, Rodrigues R, Sparling D, Noor S, Olarewaju G, Armstrong H, Lambert G. Investigating factors associated with sub-optimal HIV testing among high-risk gay, bisexual, and other men who have sex with men: results from Engage Montreal 2017-2018. Canadian Association of HIV Researchers Conference; 2019 May 10-12; Saskatoon, SK. https://www.engage-men.ca/our-work/posters/
- Footnote 62
-
Gender and Health Promotion Studies Unit. Our Youth, Our Response: Building capacity for effective HIV/HCV policy and programming responses across the Atlantic Region. Final report. Halifax (NS): Dalhousie University; 2014. https://www.dal.ca/diff/gahps/research-projects/oyor.html
- Footnote 63
-
Public Health Agency of Canada. I-Track: Enhanced surveillance of HIV, hepatitis C, and associated risk behaviours among people who inject drugs in Canada - Phase 3 (2010-2012) Report. Ottawa (ON): Government of Canada; 2018. https://www.canada.ca/en/public-health/services/publications/diseases-conditions/itrack-enhanced-surveillance-hiv-hepatitis-associated-risk-behaviours-people-who-inject-drugs-canada-phase-3.html
- Footnote 64
-
Vannice S. Barriers, access, resources, and knowledge (B.A.R.K.): an analysis of HIV testing vis Women’s Voices in Ottawa: Ottawa (ON): University of Ottawa; 2016. https://ruor.uottawa.ca/bitstream/10393/35602/5/Vannice_Sarah_2016_thesis.pdf
- Footnote 65
-
Heard E, Fitzgerald L, Wigginton B, Mutch A. Applying intersectionality theory in health promotion research and practice. Health Promot Int 2020;35(4):866–76. https://doi.org/10.1093/heapro/daz080
- Footnote 66
-
Public Health Agency of Canada. Reducing the health impact of sexually transmitted and blood-borne infections in Canada by 2030: A pan-Canadian STBBI framework for action. Ottawa (ON): Government of Canada; 2018. https://www.canada.ca/en/public-health/services/infectious-diseases/sexual-health-sexually-transmitted-infections/reports-publications/sexually-transmitted-blood-borne-infections-action-framework.html
- Footnote 67
-
Public Health Agency of Canada. Accelerating our response: Government of Canada five-year action plan on sexually transmitted and blood-borne infections. Ottawa (ON): Government of Canada; 2019. https://www.canada.ca/en/public-health/services/reports-publications/accelerating-our-response-five-year-action-plan-sexually-transmitted-blood-borne-infections.html
- Footnote 68
-
Cerigo H, Quesnel-Vallée A. Systematic mixed studies reviews: leveraging the literature to answer complex questions through the integration of quantitative and qualitative evidence. Int J Public Health 2020;65(5):699–703. https://doi.org/10.1007/s00038-020-01386-3
Page details
- Date modified:
