Communicating the Health Risks of Extreme Heat Events
Toolkit for Public Health and Emergency Management Officials
ISBN: 978-1-100-17344-3
Cat. No.: H128-1/10-623E
HC Pub.: 100596
Acknowledgements
Health Canada gratefully acknowledges the contributions of the following people in reviewing chapters:
To receive more information about climate change and health activities at Health Canada, please contact:
Chris Brown (City of Windsor), Quentin Chiotti (Pollution Probe), Lorraine Davidson (Canadian Centre for Occupational Health and Safety), Nancy Dubois (University of Toronto), Stephan Hamel (New Brunswick Public Health), Sandi Hirst (University of Calgary), Toni Morris-Oswald (Manitoba Health and Healthy Living), Fred Ruf (Outsourcing Services Inc.), Scott Sheridan (Kent State University), Trevor Smith Diggins (Risk Communications Specialist), Sue Sullivan (Canadian Public Health Association), Rae-Anne van de Lande (City of Hamilton).
Table of Contents

- Foreword
- 1. Extreme Heat and Health Risks
- 2. Communicating Health Risks from Extreme Heat
- 2.1. Identifying and Analyzing Target Audiences
- 2.2. Setting Goals and Objectives
- 2.3. Choosing the Means of Communication
- 2.4. Tailoring Risk Communication Products and Removing Barriers to Action
- 2.5. When to Communicate Risks to Health from Extreme Heat
- 2.6. Special Considerations for Rural Communities
- 2.7. Developing Heat-Health Messages
- 2.8. Scientifically Sound Heat-Health Messages for the Public
- 3. Evaluating Heat-Health Communication Campaigns
- Appendices
- References
Foreword

Extreme heat is a current health risk. As our climate continues to change, extreme heat events/heat waves are expected to increase in frequency, length and severity, resulting in increased health risks for many Canadians. Older adults, those who are chronically ill and socially disadvantaged people, among others, are more vulnerable to health effects related to extreme heat. These effects can include serious illness and even death. In some parts of Canada, the annual number of extremely hot days is expected to more than double over the next 30 years.
Public health and emergency management officials play a key role in implementing communication strategies to provide practical and useful information to health service providers, caregivers and the public to help manage health risks from extreme heat events. These strategies and their associated messages must be effective, consistent and targeted to the appropriate audiences. Communicating the Health Risks of Extreme Heat Events: Toolkit for Public Health and Emergency Management Officials was developed by Health Canada to help achieve this goal.
The Toolkit is based on best communication practices for addressing health risks from extreme heat events. The practices are drawn from experiences in Canadian communities and internationally. They were developed with input from public health officials and health communication experts, as well as a review of the existing literature.
Using the Toolkit
This Toolkit is intended for use by public health and emergency management officials who are developing or updating heat-health communication strategies. It is designed to guide the development of targeted heat-health communication campaigns and necessary outreach products for specific audiences. Currently, many Canadians do not follow the prevention advice provided by public health fact sheets and the media when extreme heat events occur.1,2 Systematic application of best communication practices in the design and evaluation of heat-health communication campaigns is required to communicate heat-health messages consistently and effectively.
To this end the Toolkit provides:
- an overview of extreme heat events and the potential health risks to all Canadians, especially those most vulnerable to heat-health impacts
- guidance on communicating heat-health risks and strategies, including scientifically sound health messages to support the development of effective communication campaigns
- guidance to help develop community-specific and tailored heat-health communication campaigns
- template materials for public health and emergency management officials, such as fact sheets, a media release and checklists
Individual Canadians have an important responsibility to prepare for extreme heat events and modify their behaviour when weather poses a health risk. Information about the dangers of extreme heat and adaptation options delivered in a timely manner will support the widespread adoption of protective actions by people in communities across Canada.
1. Extreme Heat and Health Risks
1.1 Extreme Heat Events
There is no standard definition of an extreme heat event, commonly known as a "heat wave." Footnote a
Most jurisdictions define extreme heat events based on the potential for hot weather conditions to result in an unacceptable level of health effects, including increased mortality. Environment Canada (Ontario Region) defines a heat wave as "a period with more than three consecutive days of maximum temperatures at or above 32°C [90°F]."Footnote 3
However, temperature is only one component of heat, which also depends on humidity, wind speed and radiant load. The weather conditions that could result in health risks depend on the sensitivity, acclimatization and adaptability of the population to extreme heat - that is, heat vulnerability.
In Canada, extreme heat events are not well documented and attributed deaths are often estimated using sources such as media reports. According to the Canadian Disaster Database, five extreme heat events were reported in Canada between 1900 and 2005 (1912, 1936, 1953, 1963, 1988) causing just over 1,200 deaths.Footnote 4 Other research indicates that in Toronto alone, an average of 120 deaths from extreme heat occurred annually between 1954 and 2000.Footnote 5 Most recently, in 2005 Toronto experienced 41 extremely hot days (exceeding 30°C/86°F).Footnote 6 Internationally, there have been a number of devastating extreme heat events, such as:
Chicago (1995) - resulting in over 700 deaths.Footnote 8 Footnote 7
Europe (2003) - resulting in over 70,000 deaths.Footnote 9
In 2007, the Intergovernmental Panel on Climate Change (IPCC) concluded that "hot extremes"
and "heat waves"
are very likely (>90% probability of occurrence) to increase as our climate continues to change.Footnote 10 This predicted temperature increase is particularly pronounced for night temperatures, resulting in reduced night-time relief from the heat.Footnote 11 In addition, Environment Canada (Figure 1) forecasts that many cities in Canada can expect a substantial increase in the number of days with temperatures exceeding 30°C/86°F, levels that are dangerous to human health.Footnote 12 Footnote 13 These changing weather conditions are a growing concern for individuals and communities in Canada.
The number of hot days for each city is based on the observed temperature data between 1961 and 1990, and projected for 2021-2040, 2041-2060 and 2081-2100.
Figure 1: Current and projected number of days exceeding 30°C/86°F for Canadian cities
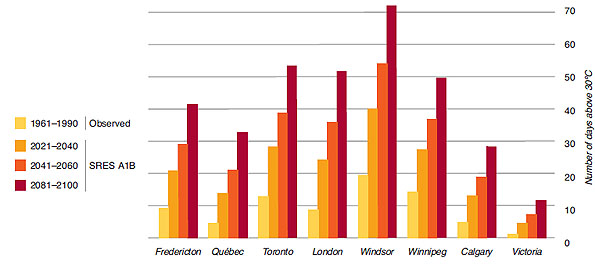
Text description
Bar chart showing the number of hot days for eight Canadian cities (Fredericton, Québec, Toronto, London, Windsor, Winnipeg, Calgary, Victoria). The number is based on the observed temperature data between 1961 and 1990, and projected for 2021-2040, 2041-2060 and 2081-2100 using the Intergovernmental Panel on Climate Change middle-of-the-road emissions scenario (A1B).
1961-1990: Fredericton = 9, Québec = 4, Toronto = 12, London = 9, Windsor = 19, Winnipeg = 14, Calgary = 5, Victoria = 1
2021-2040: Fredericton = 21, Québec = 13, Toronto = 28, London = 23, Windsor = 40, Winnipeg = 27, Calgary = 12, Victoria = 4
2041-2060: Fredericton = 29, Québec = 21, Toronto = 39, London = 35, Windsor = 53, Winnipeg = 37, Calgary = 19, Victoria = 7
2081-2100: Fredericton = 41, Québec = 32, Toronto = 53, London = 51, Windsor = 72, Winnipeg = 50, Calgary = 29, Victoria = 11
Source: Developed by Kharin Slava, Canadian Centre for Climate Modeling and Analysis, Canadian Global Climate Change Model version 3.1, personal communication, 2009. The temperature projections were analyzed with the Special Report on Emissions Scenarios (SRES) using the IPCC middle-of-the-road emissions scenario (A1B).Footnote 120
1.2 Community and Individual Factors Affecting Heat Vulnerability

During extreme heat events, many people succumb to underlying health conditions (e.g. respiratory, cardiovascular),Footnote 14 while some may experience heat stroke (Table 1) that could result in death. These health outcomes are preventable and are primarily caused by over-exposure to extreme heat and/or over-exertion for a person's age and/or physical condition.Footnote 15 To prevent negative health impacts from extreme heat events, public health and emergency management officials can assess community and individual factors contributing to vulnerability and develop intervention programs supported by appropriate communication strategies.
| Heat stroke | The most serious type of heat illness is a result of body heat overload. Signs of heat stroke may include a core body temperature of more than 40°C/104°F, complete or partial loss of consciousness and/or reduced mental ability.Footnote 15 Sweating is not a good indicator, as there are two types of heat stroke:
|
|---|---|
| Heat exhaustion | Caused by excessive loss of water and salt. Symptoms may include heavy sweating, weakness, dizziness, nausea, headache, diarrhea and muscle cramps. |
| Heat fainting (parade syncope) | Caused by the loss of body fluids through sweating and by lowered blood pressure due to pooling of blood in the legs. Symptoms include temporary dizziness and fainting resulting from an insufficient flow of blood to the brain while a person is standing. |
| Heat cramps | Caused by a salt imbalance resulting from a failure to replace salt lost through excessive sweating. Symptoms are sharp muscle pains. |
| Heat rash (miliaria rubra) | A result of inflammation of clogged sweat glands and accompanied by tiny red spots on the skin, which may give a prickling sensation. |
| Heat edema | Heat-induced swelling frequently noticeable in the ankles, feet and hands, and most often seen in people who are not regularly exposed to heat. |
Source: Canadian Centre for Occupational Health and Safety, 2005.Footnote 39
Community factors that can increase the likelihood of heat exposure or affect the risk associated with it may includeFootnote 16 Footnote 17 :
- Local climate - higher frequency, length and severity of extreme heat events, humidity levels, night-time temperatures, seasonal weather variability.
- Community design - cities are often warmer than their non-urban surroundings (phenomenon referred to as the urban heat island effect) which is increased by black roofs or concrete surfaces that hold heat and release it at nig
- ht, and limited tree-shaded areas that have a cooling effect and could be as much as 5°C/9°F cooler than the surrounding area.Footnote 18
- Availability and accessibility of services to cope with extreme heat - public transportation, health services, community outreach services, easy-to-access cooling options with air-conditioning.Footnote 19
Individual factors that can increase the likelihood of heat exposure or the risk associated with it may include:
- Health status - chronic illness, need for medications that increase heat-health risks, dependence on caregiver.
- Availability of an air conditioner and its use during extreme heat events.
- Social isolation - limited access to heat-health information and services.
- Income level - utility bill arrears, concerns with costs associated with running an air conditioner and accessing other cooling options.
- Behaviours during extreme heat events - strenuous physical activity, inadequate hydration, inappropriate clothing.
- Type and location of place of work/residence - individuals in occupations with high temperature exposure or those living on higher residential floors without an air conditioner.20

Heat sensitivity is increased for those who are not regularly exposed to hot environments.Footnote 21,Footnote 22 Extreme heat events early in the summer generally result in higher mortality and morbidity than those later in the season.Footnote 21 This "acclimatization"
is due to physiological adaptation in both cardiovascular and sweating systems.Footnote 23 Furthermore, the body's ability to acclimatize may be limited for some, such as those with heart disease,Footnote 24,Footnote 25 older adultsFootnote 25 and young children, who are also considered to be heat-vulnerable.Footnote 25
1.3 Heat-Vulnerable Groups
Analyses of extreme heat events help to identify heat-vulnerable groups for which hot weather Table 2.
Health risks from extreme heat may be compounded for those with more than one risk factor. For example, people with a psychiatric illness, taking an antipsychotic drug that affects heat sensitivity, and who live alone may be at greater risk than those with only one of these three risk factors.
Current and future heat vulnerabilities have been studied in Quebec. Climate modelling and a social vulnerability index consisting of age, poverty, social isolation and education indices were used in prediction models (Box 1). This type of forecasting is limited by uncertainty about future socio-demographic conditions. However, by studying populations at risk, health officials can learn about the unique needs in their communities, identify the most heat-vulnerable individuals, and provide targeted advice and services to those in greatest need.
| Heat-Vulnerable Groups | Examples of Challenges |
|---|---|
| Older adultsFootnote 26 |
|
| Infants and young childrenFootnote 29 |
|
| People with chronic illness or who are physically impairedFootnote 32 |
|
Socially disadvantaged individuals and communities:
|
|
| Newcomers to Canada and transient populations such as tourists |
|
| Occupational groups |
|
| The physically activeFootnote 39,Footnote 40 |
|
Limite est égal à un virgule cinq multiplié par mille divisé par dix égaux cent cinquante ppm.
Box 1: Method used to assess heat vulnerability in Quebec
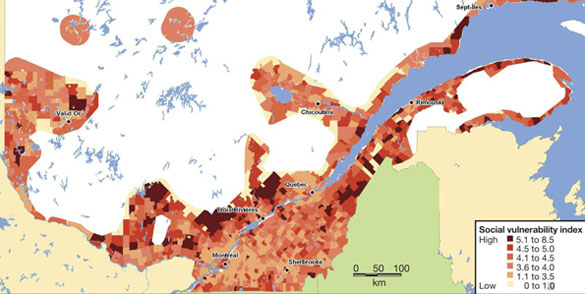
Box 1: Method used to assess heat vulnerability in Quebec - Text equivalent
A map of southern Quebec overlaid with social vulnerability index scores assigned by regions and ranging from high (5.1 to 8.5) to low (0 to 1.0). Areas of high vulnerability based upon age of the population, and poverty, social isolation and education levels are found largely north of the St. Lawrence River above Montreal and east of the river across from Quebec City. Montreal has medium vulnerability and Quebec City has lower vulnerability.
Climate models can be used to demonstrate current and projected biophysical vulnerability. Vescovi (2007) evaluated the heat vulnerability of individuals by examining geo-spatial characteristics of climate hazards and social vulnerability, as follows:
- Age index - people older than 65.
- Poverty index - low-income earners.
- Social isolation index - single-person households.
- Education index - people older than 20 years of age with less than 13 years of education.
1.4 Reducing Heat Illnesses and Deaths
As our climate continues to change, weather conditions that already pose risks to health may increase in the future.
The amount of lead time in forecasts of extreme heat events is now allowing public health officials and the public to prepare for dangerous conditions. Heat-related illnesses can be reduced with measures that help people to maintain a normal body temperature (approximately 37°C/99°F). To reduce the likelihood of morbidity and mortality, public health and emergency management officials, together with individual Canadians, need to take measures that include both short- and long-term strategies.
Short-term strategies provide targeted groups with timely, consistent and accurate information to help people make informed decisions and change their behaviour to minimize health risks, such as drinking more water and going to cooling shelters during extreme heat. Many communities in Canada and around the world have developed heat alert and response systems that encourage people to take actions to protect their health.Footnote 41 The four typical components of heat alert and response systems include:
- Alert Protocol - Designed to identify extremely hot weather conditions that could result in increased morbidity and mortality in a region. The protocol is used to alert officials and stakeholders (e.g. managers of long-term care facilities) who can then take actions to inform the target audience and/or physically adapt the facility.
- Community Response Plan - Developed for a network of stakeholders with a goal of reducing barriers to action and meeting the needs of the community and especially those who are most heat-vulnerable during an extreme heat event.
- Communication Plan - Raises awareness about heat-health impacts and provides advice on how to reduce health risks by educating the audience about protective actions and services and resources that are available (described in detail in Section 2).
- Evaluation Plan - Provides continual improvement to a heat alert and response system to meet the needs of the community.
Long-term strategies are designed to reduce the exposure of the general public to extreme heat and help them adapt more effectively. Such strategies include:

Green roof in Ottawa
Source: Craig A.L. Riedl
- minimizing the urban heat island effect by modifying infrastructures to decrease heat absorption, retention and release over time (e.g. planting trees to decrease heat absorption and increase shade, designing streets and buildings to allow maximum air flow)Footnote 42
- designing the community to include easy access to heat-relief places and drinking water
- encouraging public participation in planning exercises and using their skills, knowledge and experiencesFootnote 43 Footnote 44
- adapting the awareness campaign and alert system to reach people at risk and encourage them to change their perceptions and behaviour
Public health and emergency management officials play an important role in communicating short-term and long-term strategies to help individuals, organizations and communities take the most appropriate adaptive actions and make informed decisions to reduce health risks.
2. Communicating Health Risks from Extreme Heat
To overcome barriers to behavioural change, communication activities must acknowledge that"there is no 'general public' ... there are many publics, each with differing views and perceptions of health and environment risks."Footnote 45
Past experiences with health promotion campaigns to prepare for public health emergencies and natural disasters provide useful guidance for developing effective heat-health communication campaigns. Campaigns are most effective when public health and emergency management officialsFootnote 46 :
- identify and analyze the audiences and their needs
- take a collaborative approach with stakeholders and government organizations
- set clear goals and objectives that fit budgets and are logically linked to the campaign
- choose effective communication channels and vehicles
- develop risk communication products and materials tailored to specific audiences
- build on existing health communication campaigns (e.g. emergency preparedness, public health)
- offer programs and services to minimize barriers to action
- follow critical timelines for effective heat-health
- take into consideration needs of specific communities (e.g. rural versus urban)
- use pre-tested, consistent and scientifically sound heat-health messages
2.1 Identifying and Analyzing Target Audiences
Know your target audience - Identify who you are trying to reach with your heat-health communication campaign and consider their physical conditions, level of knowledge and needs, demographic characteristics, recent experiences, beliefs and values.
The characteristics of a community and population groups (Table 2) that increase heat vulnerability should be assessed at the beginning of your campaign so you can choose appropriate communication strategies and tools. This process, often called formative evaluation, allows you to identify individuals and groups who should be targeted to receive risk communication materials and interventions, and ensure that the needs of your stakeholders are met. This process also focuses efforts and resources to prepare for extreme heat events and helps to tailor the development of "how-to"
information.
Successful heat-health communication campaigns should be targeted to guide heat-vulnerable individuals at four distinct levels of audience organizationFootnote 47 :
- heat-vulnerable individuals
- social networks
- organizations
- communities and/or societies
Targeting communication campaigns requires that heat-vulnerable individuals be separated into groups according to their characteristics. These characteristics could relate to demographics, specific behaviours, attitudes, perceptions of heat-health risks, personal values, lifestyles and opinions.Footnote 48 These characteristics are key determinants of how people receive and process information from education and outreach campaigns. Empower interested individuals to play a key role in your campaign by including them in the process. This will encourage active participation and increase the chance that communication activities will have an impact.Footnote 49
You can reach target groups directly and/or indirectly by involving their social networks (e.g. family members, friends, co-workers, opinion leaders, and gatekeepers to information goods and services) to spread heat-health messages and increase awareness of health risks.Footnote 47 Involving members of social networks also helps them learn about the need to pay close attention to heat-vulnerable people during extreme heat events.
Your heat-health communication campaigns should also target supporting organizations, to raise awareness about heat-health issues, guide the establishment of heat-health action plans (e.g. emergency plans for extreme heat events), and provide direction on preventative measures to minimize health impacts. This will help to ensure that heat-health messages are adopted and distributed (Box 2) and that the information flows to target audiences.
Relevant organizations include:
- schools
- worksites
- long-term care facilities
- retirement homes
- landlord associations
- community outreach groups
- primary health care settings
When community organizations are engaged, they can often bring additional resources to the table along with knowledge of the target audiences and their needs. They may also be encouraged to take the lead on heat-health issues and act as role models for other organizations in the community.Footnote 47
At the societal level, effective heat-health campaigns aim for long-term impacts to help communities and people cope with extreme heat events. A longer-term impact can be achieved by modifying social norms and implementing supportive policies and regulations to protect those most vulnerable and bring about needed environmental changes, such as reducing the urban heat island effect.
Box 2: Canadian Red Cross - Expect the Unexpected program

Source: Canadian Red Cross
The Canadian Red Cross developed its Expect the Unexpected program in 1997, following the major floods in Saguenay, Quebec, in 1996. Intended for educators and parents, the program is designed to help youth and their families deal with the impact of natural disasters and adopt disaster preparedness behaviours. The Canadian Red Cross is grateful to the American Red Cross for permitting the adaptation of its Masters of Disasters™ program in order to create the Expect the Unexpected program.
The only disaster-based educational program of its kind in Canada, Expect the Unexpected is designed to help children, youth, educators and parents learn about the importance of disaster preparedness. It features in-class and at-home activities on topics such as climate change, weather events, knowing the risks in your community, safety rules, making a plan, getting a kit and dealing with emotions related to emergencies.Footnote 41 Footnote 50
2.2 Setting Goals and Objectives
After identifying your target audiences for a campaign, the next step is to develop realistic objectives that fit budgets and that focus on health-related outcomes of both ultimate goals and intermediate objectives.
The ultimate goal of your communication campaign is to reduce heat-related morbidity and mortality. To achieve this, intermediate objectives need to be set toFootnote 1 Footnote 47 :
- raise awareness and increase knowledge about the effect of extreme heat on health
- change health-related behaviours and develop skills for behavioural change to improve self-care during extreme heat events
- provide timely warnings about extreme heat events
- improve social network interactions by engaging family members, friends, co-workers, neighbours
- build credibility and engage stakeholders in heat-health communication campaigns
2.3 Choosing the Means of Communication
Choose the right messenger - In advance of an extreme heat event, you should identify and train credible and empathetic messengers who can move the message forward (e.g. health care providers and caregivers).Footnote 51
There is no single approach to developing an effective communication campaign. The most appropriate strategy will depend on:
- communication goals and objectives
- available resources
- audience reach - which relates toFootnote 48 :
- audience size
- ability for messages to be passed on to others
- relevance to the heat-vulnerable audience
- specific needs of target audiences
- involvement of community partners
Successful heat-health communication campaigns often include three means of communication to reach the target audience, all of which should be community-based:
- media
- mass/broadcast
- targeted (also known as narrowcast)
- interpersonal networks
- community and group events

Source: The Weather Network
Mass/broadcast media include television, radio, Internet, newspapers and magazines that reach very large audiences.Footnote 47 To reach specific audiences, campaign planners tailor messages and deliver them through selected vehicles and messengers at times when these audiences are likely to be accessing or using certain sections of particular media.
Recent surveys of Canadians show that most people receive their extreme weather information from mass/broadcast media, through television (56%), radio (35%) and the Internet (27%).Footnote 52 Partnering and engaging local media is important to establish credibility and ensure dissemination of consistent messages. Messages from mass/broadcast media can often blend into other channels of communication by stimulating discussion, especially if the campaign messages are presented as "news"
rather than "advertising."
Box 3: Heat-health communication framework used by Montréal's public health authority
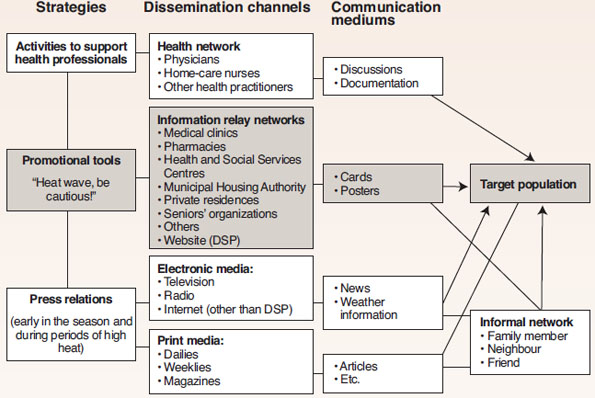
Box 3: Heat-health communication framework used by Montréal's public health authority - Text Equivalent
Strategies include: activities to support health professionals, dissemination of promotional tools "Heat wave, be cautious!" and press relations (early in the season and during periods of high heat).
A process diagram showing strategies, dissemination channels and communication media used by Montréal's public health authority to communicate heat-health risks.
Dissemination channels include: health network (physicians, home-care nurses, other health parishioners), information relay networks (medical clinics, pharmacies, Health and Social Services Centres, Municipal Housing Authority, private residences, seniors' organizations, others, website (DSP)), electronic media (television, radio, internet (other than DSP)), print media (dailies, weeklies, magazines).
The communication media are also provided to informal networks (family members, neighbours, friends) that have contact with the targeted population.
The communication framework developed by the Direction de santé publique de l'Agence de la santé et des services sociaux de Montréal is a good example of how interpersonal networks (activities to support health professionals), targeted media (promotional tools) and mass/broadcast media (press relations) are used to communicate heat-health messages to the target audience.
The three communication strategies used include:
- Activities to support health professionals - During the heat season, information is sent electronically to health professionals, in particular to physicians and professionals in health and social services centres. This information encourages them to pay particular attention to patients at risk and provide appropriate prevention advice about coping with extreme heat.
- Promotional tools - Promotional material is sent out in early May. Posters and information cards are mailed to a broad and varied distribution network responsible for communicating with the target population. Information cards can also be downloaded from the Direction de santé publique website.
- Press relations - Early in the heat season, a press release is sent to health and social services centres for publication in local weeklies. It contains information on health risks related to extreme heat events, identifies heat-vulnerable populations and suggests protective measures to guard against the effects of heat. During periods of high heat and humidity warnings, media releases are distributed and interviews in electronic and print media are conducted with community officials to remind the population of this information.
Communication strategies should also be supplemented with targeted media such as fact sheets, pamphlets, posters, fridge magnets, and personal alerts through short message service (SMS), facsimile and e-mail. Some of these could be mailed directly to people's homes or inserted into the newspapers your audience is likely to read. This method gives people an information resource they can use as they become more interested in the campaign.Footnote 44
Interpersonal networks are crucial and often most powerful. They allow for greater participation in the issue, especially when feedback is required. Interpersonal networks spread public messages by community leaders, health care providers, educators, friends and relatives who will often endorse the messages and enhance their impact.Footnote 47
Distributing heat-health messages during community and group events is also important. The attention of the targeted audience is already captured, as community events are often well promoted and reported on by the media. For example, messages could be integrated into activities planned by faith-based groups, scientific conferences, and industry, community and outdoor events (e.g. festivals).
Multiple, diverse channels and vehicles should be coordinated to distribute heat-health messages and to reinforce them. For example, mailed fact sheets or fridge magnets should be supplemented with an awareness campaign before the mail-out to increase the likelihood of an audience keeping this material. Shortly after, it is beneficial to follow up with additional heat-health messages using multiple means to spike interest and entice the audience to read the mailed material.Footnote 44 Apply the rule: three messages, three times, using three different ways.Footnote 48
If the community borders another jurisdiction, the target audience may also receive their health information during extreme heat events from other authorities. It is important to coordinate these heat-health messages and alerts as much as possible to build and maintain credibility, and to make the best use of available resources.
Box 4: Tailored extreme heat and health fact sheets

The U.S. Environmental Protection Agency (EPA) has developed fact sheets on risks to health from extreme heat that are tailored to the needs of specific target audiences. The "It's Too Darn Hot"
fact sheet is offered in 17 languages and comes in two versions - the high-literacy version and a simpler version for those with a lower reading ability. EPA also offers a large-font series of fact sheets for people with a visual impairment.Footnote 53
Source: www.epa.gov/aging/resources/factsheets/index.htm.
2.4 Tailoring Risk Communication Products and Removing Barriers to Action
Communication products should be tailored to each target audience (Box 4). To enhance understanding and retention of the message, heat-health written material and graphics must be appropriate for the reading level, age range, and ethnic or cultural background of the audience. Focus the message on the abilities of the audience and address their unique challenges and perspectives. The information provided should emphasize practical steps to protect health within available community resources.
Socio-economic factors may prevent people from changing their behaviours in the face of serious risks to health. These challenges include insufficient financial resources for air conditioning, lack of clean water or adequate shelter, inadequate skills and knowledge, limited physical ability, and certain views and beliefs (local preferences, accepted behavioural patterns). Risk communication efforts have more chance of influencing behaviour when they are complemented by programs that remove barriers to action and provide opportunities for citizens to adopt coping strategies. For example, providing free bus tickets during extreme heat events will encourage people to go places where they can cool down. Interventions to overcome barriers to action should take into account the existing capacity of communities and partners. They should also address the need of target audiences and be based on service utilization, availability and accessibility of services, and stakeholders' perceptions of audience need (Box 5).
2.5 When to Communicate Risks to Health from Extreme Heat
Effective communication planning must begin well in advance of an extreme heat event to positively influence behavioural change and to help the audience deal with extremely hot weather. Extreme heat and health communication campaigns generally occur over three phases:
- before the heat season
- during the heat season
- during an extreme heat event
Choose the right moment - Your message will have the greatest impact if it is in the right place at the right time. Choose the means of distribution that are most appropriate for your audiences. Look for ways to tie messages to events that will catch the audiences' attention and spark their interest.
Before the Heat Season
To reach targeted individuals in time, awareness campaigns should begin in the spring before extremely hot weather begins and continue during the summer months. Educate audiences about available resources in communities, such as cooling facilities, utility rebates, subsidies and transportation assistance.
Before summer, raising public and stakeholder awareness is more challenging than communication during the heat season. This is because both the media and the public are less likely to get interested and involved in heat-health issues. Communication activities should focus on raising the audiences' curiosity about heat-health issues. This will encourage information sharing and a desire to look for more details from multiple sources. Make sure these sources are available in advance (e.g. websites, fact sheets). This will empower audiences and give people an opportunity to plan their own protective measures.Footnote 44
It is beneficial to build on and possibly incorporate (where appropriate) heat-health awareness activities into existing community and group events and health promotion campaigns (e.g. West Nile virus) held in the spring. Properly timed and audience-appropriate messages will ensure the best use of resources, contribute to wider audience reach and increase the likelihood of messages being understood and retained.
Box 5: Interventions and communication strategies used in Canadian programs to encourage adaptation to extreme heat
Many steps to encourage adaptation to extreme heat address more than one barrier to action.
Socio-economic challenges

- Open cooling facilities and extend their hours:
- free swimming
- spray pads
- cooling rooms in apartment buildings and retirement
homes - cooling shelters (e.g. libraries, government buildings,
shopping malls).
- Promote the use of available cooling options (e.g. waterfront,
tree-shaded areas, public libraries). - Provide subsidy programs and social services to eligible
residents (e.g. for purchasing a fan or air conditioner, public transportation to cooling facilities). - Assist with utility arrears, disconnections and security deposits to restore services where necessary so that vulnerable populations have access to power and water for the duration of an extreme heat event.
- Install water fountains and distribute water in locations where heat-vulnerable populations are likely to gather.
Newcomers to Canada and cultural barriers
- Use culturally appropriate risk communication strategies by translating heat-health materials into multiple languages.
- Adapt culturally appropriate themes with photographs, imagery, symbols and graphic elements as determined through public involvement methods (e.g. focus groups).
- Use cultural leaders and ethnic media outlets to help disseminate culturally appropriate heat-health messages.
- Include both degrees Fahrenheit and Celsius in the messages if the audience might find this information useful (e.g. older adults, newcomers to Canada, transient populations).
Inadequate skills and knowledge
- Actively distribute targeted media (e.g. fridge magnets, tailored fact sheets) and use media, interpersonal channels, community and group events to disseminate heat-health messages.
- Provide maps with locations of cooling facilities.
- Provide support and services that help audiences maintain independence.
Limited mobility
- Provide transportation assistance to and from cooling facilities.
- Involve family members, neighbours and friends to provide support during extreme heat.
Source: Examples are based on actions being taken by the cities of Toronto, Hamilton and Montréal.Footnote 63 Footnote 123
During the Heat Season and During an Extreme Heat Event
Heat stroke has a fast onset and low survival rate.Footnote 32
The timing of communication activities is critical. Early summer extreme heat events result in higher mortality and morbidity than do those occurring later in the season.Footnote 21 Extra communication efforts are needed early in the season to warn and help protect heat-vulnerable individuals.
During an extreme heat event, providing effective and rapid communication materials emphasizing only three to seven bits of familiar information that audiences can/should remember is very important. This will increase the likelihood of retention of key messages. By repeating these messages often, through different channels and vehicles, you will increase the reach and number of times they hear your message, demonstrate credibility, and provide needed support to those most at risk.Footnote 54
Heat-related mortality also continues to occur shortly after extreme heat events,Footnote 55 so it is a good idea to build the recovery phase into your communication campaign. Provide ongoing reminders to the public even after such events have passed (e.g. "we are still recovering from an extreme heat event, continue to drink cool water before you feel thirsty"
).
Be prepared - use the "window of opportunity"
after the extreme heat event to communicate with your audience. This will increase the likelihood of messages being heard and picked up by the audience, and encourage behavioural change.Footnote 44
2.6 Special Considerations for Rural Communities
Although residents of rural and small town communities are less likely to be affected by the urban heat island effect (i.e. there is more night-time relief from the heat) or crime if they keep their windows open, they are likely to be at high risk for several reasons:

- Small towns and rural communities are home to many heat-vulnerable individuals, including older adults whose numbers are growing rapidly in rural regions.Footnote 56
- There are occupational hazards resulting from exposure to environmental heat (e.g. farming and outdoor work).Footnote 57
- There is a greater likelihood of people being isolated compared with those living in urban settings.Footnote 58
- Without convenient public transportation, people without vehicles may not be able to go to a cooler place.Footnote 58
- Communities may also be resort/tourist towns and attract transient populations during the summer months, which need to be considered when developing communication campaigns.Footnote 59
Small towns and rural communities often face unique challenges in developing and implementing extreme heat and health communication campaigns.
These can include:
- limited financial resourcesFootnote 60
- lower levels of formal educationFootnote 60
- access to health services that may require travel outside the communityFootnote 58
- fewer public health and emergency management staff to set up communication campaignsFootnote 58
- a smaller number of community support organizations and facilities (e.g. shelters, retirement homes, emergency assistance)Footnote 58
- fewer services that allow vulnerable people to maintain their independence in the community (e.g. public transportation and housing options)Footnote 58
- limited channels for communicating with the audience during extreme heat events (weekly newspapers, few local radio stations)
These communities also have important strengths that can be drawn upon when developing communication plans. These may include:
- strong community and social networksFootnote 61 Footnote 62
- highly credible and trusted communicators (e.g. community leaders in places of worship)
- gathering places familiar to most residents
- capacity to go door-to-door to disseminate information (in some communities)Footnote 62
- rapid decision-making capacity
- high numbers of volunteers to help get the messages outFootnote 61 Footnote 62
Authorities in rural communities may need to find innovative approaches to use their strengths and address challenges. For example, because of fewer ways to communicate with the public, heat awareness campaigns may need to focus on empowering people to take independent action by monitoring important weather information and the health of those around them. To facilitate communication with audiences in summer, officials may inform the public about the severity of extreme heat events by displaying a "heat meter"
sign by the side of the road, an entrance to a park or recreational facility. The sign could display community-specific heat warnings such as an advisory, warning or alert. The heat monitor design used by the City of Hamilton is one example that could be adapted to develop a local heat meter sign in rural areas (Box 6).
Box 6: Heat meter used by the City of Hamilton
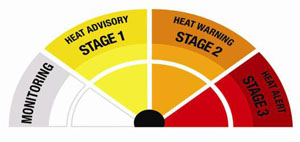
Source: City of Hamilton
Box 6: Heat meter used by the City of Hamilton
A half circle gauge used by the City of Hamilton to communicate heat-health risk. The gauge has a monitoring stage shown in gray and three alerting stages: stage 1 (heat advisory) = yellow; stage 2 (heat warning) = orange; stage 3 (heat alert) = red.
To distribute heat-health information in rural areas, you could use:
- postings on bulletin boards in public placesFootnote b (e.g. post office, grocery store)Footnote 64
- community and group events (e.g. festivals)
- local newspapers, bulletins and radio
- tourist and recreational facilities
- schools
- interpersonal channels (e.g. word of mouth, telephone, community centres, places of worship)
2.7 Developing Heat-Health Messages
When communicating with intended audiences, take advantage of techniques designed to capture attention, along with strategies that will influence behavioural outcomes.Footnote 65 It is important to ensure that heat-health messages are accessible, credible, personally relevant, take into consideration existing knowledge and focus on achievable outcomes (Box 7). See Appendix B for the Toronto Health Communication Unit's Message Review Tool to develop messages that address an audience's level of understanding and relevance.
Successful public education campaigns, such as "Quit smoking,"
"Fasten your seat belt"
and "Don't litter,"
have had three strategies in commonFootnote 44 :
- They introduced uncertainty in the target audiences - Introduce uncertainty by discussing the chance of an extreme heat event and the possibility of impact on the audience. Guide them to additional resources where they can find weather information or heat-health information (e.g. websites, doctors' offices, fact sheets).
- They provided simple solutions to protect health - Describe an extreme heat event using
"the local angle"
and the possible impacts that the target audience care about (e.g. health for parents with young children and older adults, performance for those who are physically active) and offer simple solutions (e.g. drink water). - They reinforced messages through stakeholder communication activities - Present a united voice with your stakeholders. Give the right amount of detail about actions that audiences can take before, during and after an extreme heat event to minimize health impacts.
It is important to keep messages consistent throughout all stages of the campaign and between distribution vehicles (e.g. fact sheets, media releases, websites). Consistent messages from all public officials, community leaders, health care providers, educators and other sources help develop and maintain credibility and trust with the audiences. To do this, look for potential inconsistencies with other health-promotion campaigns (e.g. ultraviolet radiation, air quality, infectious diseases, physical activity, green city and energy-use reduction campaigns). It is very important to ensure that heat-health messages are complementary before you distribute them.
- Identify and test key messages and required actions - Use simple, focused, scientifically sound (see Section 2.8) and audience-relevant heat-health messages emphasizing health and safety. Prioritize the messages and communicate actions that your audience should take when they receive the information.
- Communicate clearly - Grab the attention of the audiences with plain language (Appendix A), personal pronouns (e.g. you) and action verbs, and use them throughout the message.
- Motivate your audience -
"It's good for you"
is not a reward that motivates people. Understand the needs of audiences and what will motivate them to consider changing their behaviour (e.g. improved performance for those who are physically active). - Use vivid and appropriate images - A good comparison (e.g. image) can be a very powerful method to communicate a message. People will remember it, relate to it and repeat it. Make sure the comparison is relevant and appropriate for the audience.
- Build trust by providing evidence and acknowledge any lack of certainty - Target audiences may need examples of how your heat-health campaign saved a life or made a lasting difference. At the same time, acknowledge that extreme heat does not impact everyone the same way and that some may be more vulnerable than others.
- Avoid - Technical jargon, unnecessary words, condescending/judgmental phrases, promises or guarantees, and humour which can be misinterpreted and requires testing with the audience.

Address contradictory messages by integrating heat-health messages into other health-promotion campaigns (Box 8) or developing a databank of health messages for the public when extreme heat events happen at the same time as other public health emergencies or events. This would help to maintain consistency, minimize confusion among the public and give appropriate health protection guidance to your audiences.

Solution:
Incorporate messages about the need to take protective measures against vector-borne diseases into heat-health communication materials (see Appendix D for a fact sheet example).
2.8 Scientifically Sound Heat-Health Messages for the Public
The following heat-health messages were developed through a review of the scientific literature about risks to health from extreme heat, best practices in health risk communication and the most effective actions to protect Canadians. The messages were reviewed by health communication experts and public health officials in communities developing heat alert and response systems. Explanations for each message and considerations to help minimize contradictory and confusing statements are provided.
The messages are not presented in order of importance. Some may be more appropriate depending on the target audience, timing and vehicle chosen for communication. Testing of these messages with your audience is important to ensure relevance and applicability. Fact sheets aimed at older adults, those who are physically active and parents with young children, which use many of these messages, are included in Appendix D.
Message 1:

Heat illnesses are preventable.
Explanation:
This message empowers the reader. It reduces barriers to action.
Message 2:
While extreme heat can put everyone at risk from heat illnesses, health risks are greatest for:
- older adults;
- infants and young children;
- people with chronic illnesses, such as breathing difficulties, heart conditions, or psychiatric illnesses;
- people who work in the heat;
- people who exercise in the heat;
- homeless people; and
- low-income earners.

Explanation:
Heat-vulnerable individuals - The list should accurately represent populations at higher risk in your community (determined through an assessment of individual- and community-level vulnerabilities).
Older adults - Older adults may be faced with compounding factors that could put them at increased risk during extreme heat events. These factors may include chronic illnesses,Footnote 68,Footnote 69 impaired thermoregulatory system,Footnote 70 medications that interfere with the body's cooling mechanisms,Footnote 36,Footnote 71-73 social isolation,Footnote 32 lower literacyFootnote 26 and poverty.Footnote 26 The term "older adults"
is seen as appropriate for this target group because it eliminates association with a specific age (e.g. "senior"
usually denotes a person 65 years of age or older). The term "elderly"
may be inappropriate or confusing when addressing communities that include Aboriginal people. "Elder"
is a title given to some Aboriginal people in recognition of their wisdom and is often reserved as a title of honour.Footnote 74
Infants and young children - Given the unique physiological characteristics of children's bodies and their high dependency on caregivers, they are likely to be at risk during extreme heat events.Footnote 75 Footnote 76
People with chronic illnesses - Individuals with breathing difficultiesFootnote 77 , heart problemsFootnote 78 and psychiatric illnessesFootnote 79-81 are at a higher risk of heat-related health effects.
People who work in the heat - Some work environments expose people to higher heat-health risks. Examples include foundries, steel mills, smelters and glass factories. As well, people who work outdoors (e.g. construction, road repair, open-pit mining and farming), in laundries, restaurant kitchens, bakeries and canneriesFootnote 39 are at higher risk.Footnote 82
People who exercise in the heat - Physically active individuals who exercise in the heat (e.g. professional athletes, marathon runners, recreational athletes, people who walk or bike outdoors) could face greater environmental heat exposure and physical strain. In addition, some of these people may expect their usual performance despite the dangerous weather conditions.
Homeless people and low-income earners - These populations have limited financial resources to take protective actions and often experience greater social isolation. They therefore experience greater environmental exposures to heat and may also be faced with less access to clean water, cool places, and health and social services.
Message 3:
If you are taking medication or have a health condition, ask your doctor or pharmacist if it increases your health risk in the heat and follow their recommendations.

Explanation:
Some drugs interfere with the body's ability to maintain normal body temperature. Sensitivity can vary widely, so people should be encouraged to seek advice from their doctors and pharmacists.
Message 4:
Heat illnesses include heat stroke, heat exhaustion, heat fainting, heat edema (swelling of hands, feet and ankles), heat rash and heat cramps (muscle cramps).
Watch for symptoms of heat illness, which include:
- dizziness or fainting;
- nausea or vomiting;
- headache;
- rapid breathing and heartbeat;
- extreme thirst; and
- decreased urination with unusually dark yellow urine.
If you experience any of these symptoms during extreme heat, immediately move to a cool place and drink liquids. Water is best.

Explanation:
Urgency of the situation - Immediate actions need to be taken when signs of heat illness are seen. If not treated immediately, they may result in a life-threatening condition such as heat stroke.Footnote 13 This urgency should be highlighted in the message.
First aid advice - When symptoms of heat exhaustion are seen, the most effective treatment is to move the person to a cool place.Footnote 82 Footnote 83 Footnote 84 The message should focus on a cool place rather than an air-conditioned place (e.g. shopping mall, public building). This will °C/9°F cooler than the surrounding area.Footnote 18
Heat stroke is a medical emergency! Call 911 or your local emergency number immediately if you are caring for someone, such as a neighbour, who has a high body temperature and is either unconscious, confused or has stopped sweating.
While waiting for help - cool the person right away by:
- moving them to a cool place, if you can;
- applying cold water to large areas of the skin or clothing; and
- fanning the person as much as possible.

Explanation:
Medical emergency - Heat stroke is a medical emergency and requires immediate medical attention, as the mortality rate can be high.Footnote 32 Emphasize the immediate need to call 911 or a local emergency number, which should be included in the message.
Sweating - Sweating is not a good indicator of heat stroke for the general public because there are two types of heat stroke - classic (accompanied by little or no sweating, usually occurring in children, those who are chronically ill and older adults) and exertional (accompanied by an increase in body temperature because of strenuous exercise or occupational exposure along with environmental heat, and where sweating is usually present).Footnote 39
High body temperature - Core body temperature over 40°C/104°F is indicative of heat stroke. However, to get an accurate reading you need to use a rectal thermometer, which may not be available or convenient. Therefore, "high body temperature"
was chosen to describe this sign of heat stroke since immediate action is required.
Cooling advice - Full body submersion in cool water is the fastest method to treat exercise-induced heat stroke (effective among young people, military personnel and athletes with exertional-related heat stroke). However, it is mainly applicable in a clinical setting.Footnote 85 Footnote 86 Footnote 87 In other settings, cool the person by applying cold water to large areas of the skin or clothing and fan them as much as possible, keeping in mind that cooling larger areas will improve efficiency.Footnote 88 Footnote 89 Footnote 90
Message 6:
Frequently visit neighbours, friends and older family members, especially those who are chronically ill, to make sure that they are cool and hydrated.

Explanation:
Importance of visiting - Visitors can help identify signs of heat illness that could be missed over the telephone. Checking with a telephone call is sufficient only for people who have excellent self-care ability.
Frequency of visits - It is essential to use careful judgment of a person's ability for self-care and past experiences in hot environments when determining how often to visit the person under your care.
Message 7:
Drink plenty of cool liquids, especially water, before you feel thirsty to decrease your risk of dehydration. Thirst is not a good indicator of dehydration.

Explanation:
Drink "before you feel thirsty"
- Many people, especially older adults, may be in a state of chronic dehydration because of a reduced ability to feel thirst, the body's reduced ability to react to dehydration and concern over frequent urination.Footnote 26 Footnote 27 By the time a person feels thirst, they have already lost about 2% of their body water and dehydration has occurred.Footnote 91 One method of reminding people to drink water is by advising them to leave a colourful glass by the sink and to drink from it after every hand washing.Footnote 92
Volume of water - Individuals should take personal responsibility for keeping hydrated.Footnote 93 People gain water from food and liquid intake, and lose water through urination, sweating and normal metabolic processes. Everyone has different water needs, depending on their activity level, diet, exposure to heat, perspiration rate and sodium concentration in sweat.Footnote 94 Canada's Food Guide recommends drinking "more water in hot weather or when you are very active."Footnote 95
- People who eat very little, such as older adults, may not be getting sufficient amounts of water and may need to drink more.Footnote 83 However, it is important not to over-hydrate as it may lead to a medical emergency (hyponatremia) caused by low plasma salt levels.Footnote 96
- Research has also shown that people who do not take part in intense activity do not need to take supplements, such as salt tablets, to maintain proper plasma salt levels.Footnote 97
Water versus juice or sports drinks - Water is the best hydrating liquid. Sports drinks and juices are popular but are also expensive. Considering the large quantities of juice or sports drinks that need to be consumed to stay properly hydrated in the heat, consumption of these liquids could be dangerous for diabetics. On the other hand, as our society has developed a taste for juices and sodas, flavouring water with natural fruit juice may make it more appealing.Footnote 83
Caffeinated beverages - Caffeine is a diuretic that increases urination. Regular caffeine users are adjusted to the effect of caffeine, minimizing its diuretic properties.Footnote 98 Therefore, people may continue to drink caffeinated beverages during extreme heat, but should not increase consumption during this time.
Cool liquids - Research suggests that people will not drink enough water unless it has been cooled (21-24°C/70-65°F).Footnote 25
Fruits and vegetables - Fruits and vegetables have high water content and are a great snack to increase daily water consumption.
Message 8:
Reschedule or plan outdoor activities during cooler parts of the day.

Explanation:
Defining "cooler parts of the day"
- Every region has its own micro-climate. Depending on the location of a person's residence, their body could get a heat load from direct sunlight during the day or from pavement and buildings even after the sun sets.Footnote 99 It is important to let people decide which time is cooler and more comfortable for outdoor activities.
Give options - For those who may want to participate in outdoor activities, offer safer options such as:
- rescheduling outdoor activities to a cooler part of the day or another day;
- exercising in an air-conditioned place rather than heading outdoors;
- choosing a cooler outdoor location such as a tree-shaded area away from high traffic to avoid high levels of air pollution; or
- if one of these options is not possible, the activity duration and intensity should be reduced.Footnote 100
West Nile virus - Mosquitoes can transmit West Nile virus and are most active during cooler parts of the day. To minimize the possibility of infection, include the following West Nile virus safety tip from Health CanadaFootnote 101 :
- If you are in an area where mosquitoes are active, protect yourself with insect repellent and follow the manufacturer's directions.
Encourage the audience to move around - Moving around may actually reduce the possibility of fainting in the heat. People who sit or stand for an extended period of time may be at greater risk during extreme heat events.Footnote 83
Acclimatization - Exposure to outdoor temperatures in the summer helps to prepare a healthy person's body for the heat through acclimatization and may reduce the probability of heat illnesses. Acclimatization takes time and will depend on individual characteristics. Guidelines for healthy people who exercise or work in the heat indicate that it requires 10 to 14 days of exposure to hot temperatures for the body to adapt.Footnote 102 Consequently, even for healthy people strenuous activities in the heat could be dangerous, especially early in the heat season.
Message 9:
Wear loose-fitting, light-coloured clothing made of breathable fabric.

Explanation:
Clothing - Clothing thickness and the amount of skin covered will affect the efficiency of heat transfer and the evaporation of sweat from the skin.Footnote 103 Insulation, permeability and breathability are characteristics important to consider when determining the most appropriate clothes to wear during extreme heat.Footnote 104
Message 10:
Never leave people or pets in your care inside a parked vehicle or in direct sunlight.

Explanation:
"People or pets in your care"
versus "anyone"
- It is not feasible to list all people (e.g. infants, those who are chronically ill) who should not be left in the vehicle during extreme heat. The designation "people or pets in your care"
implies those with caregiver needs. Indicating "anyone"
may appear to be too generic and could result in mistrust and disregard of the message.
Temperature inside a vehicle could get very dangerous - When the outside air temperature is 23°C/73°F, the temperatures inside a vehicle can be extremely dangerous - more than 50°C/122°F.Footnote 105
Message 11:
Take a break from the heat by spending a few hours in a cool place. It could be a tree-shaded area, swimming facility or an air-conditioned spot such as a public building, shopping mall, grocery store, place of worship or public library.

Explanation:
Time needed for sufficient cooling - This depends on individual characteristics. Every person needs to judge their own comfort level and when they feel refreshed after cooling.
Unique community cooling options - Develop this message based on the existing air-conditioned resources and programs that are most appropriate for your target audience and their demographics (e.g. cooling centre, public library, cooling room in an apartment building, place of worship, shopping mall, grocery store). Keep in mind that some people may not have access to air-conditioned places. Therefore, it is a good idea to highlight other cooling options (e.g. waterfront locations, tree-shaded areas, swimming facility or spray pads - some of these may be excellent choices for children).
Air-conditioned spot - Use of air conditioners during extreme heat events diminishes heat-health risks.Footnote 32 However, air conditioners can use a lot of energy, give off greenhouse gases and may decrease acclimatization to heat. Therefore, public health information should highlight alternatives and educate about the most efficient use of air conditioners. Messages that suggest using air conditioners should include user guidelines such as:
- If you have an air conditioner, make sure it works properly before the hot weather starts.
- If you have an air conditioner with a thermostat, keep it set to the highest setting that is comfortable (somewhere between 22°C/72°F and 26°C/79°F), which will reduce your energy costs and provide you with needed relief.Footnote 106
- If you are using a window air conditioner, cool only one room where you can go for heat relief.
Message 12:
Take cool showers or baths until you feel refreshed.

Explanation:
"Cool"
versus "cold"
- Some people who are at a higher risk from extreme heat may have other health conditions such as cardiovascular disorders. Exposure to a rapid shift in temperature could have health consequences.Footnote 107 Recommending a "cool"
rather than "cold"
shower or bath minimizes this risk.
Bathroom safety - Older adultsFootnote 108 and childrenFootnote 109 may be at increased risk of injuries while in the bath tub. Messages to these groups could add additional suggestions to protect them from injuries, such as including Health Canada's fall prevention guidelines:
- For older adults - Make sure to use non-slip surfaces in the tub and shower, and wipe up moisture or spills immediately to avoid slipping.Footnote 110
- For children - Always supervise your child in the bath.Footnote 111
Misting - Misting with cool water is helpful during extreme heat. Mist cools the body by conductive cooling and contributes to evaporative cooling, especially when windy.
Cooling hands and forearms - Cooling a person's hands and forearms can improve athletic and occupational performance and comfort while reducing heat strainFootnote 13 Footnote 36 Footnote 73 Footnote 84 Footnote 85 Footnote 112 .
Message 13:
Prepare meals that don't need to be cooked in your oven.

Explanation:
Ovens produce a lot of heat. Cooking with an oven will increase the indoor temperature, which is difficult to lower during extreme heat events, especially without an air conditioner.
Message 14:
Block sun out by closing awnings, curtains or blinds during the day.

Explanation:
"Greenhouse effect"
- Allowing the sun to beam through the windows will increase your indoor temperature due to the "greenhouse effect"
and will result in trapping hot air in the home. Installing and closing awnings or shutters is very effective at keeping the heat outside, since the sun's rays will be blocked before they reach the window.
Plan for the future - Planting a broadleaf tree on the side of the house where the sun hits during the hottest part of the day will provide shade during the summer months and shelter the house from radiant heat.
Message 15:
Avoid sun exposure. Shade yourself by wearing a wide-brimmed, breathable hat or using an umbrella.

Explanation:
Heat is made up of four main physical and environmental factors that contribute to the body's heat load: humidity, radiant load, temperature and wind speed.Footnote 39 Direct sun exposure will increase the radiant load and total heat exposure. This is why shaded areas are cooler and wearing a wide-brimmed, breathable hat or using an umbrella in the sun is recommended.
Hats - Basic scientific principles, as well as designs that have evolved in hot climates, indicate that hats worn to protect against the sun's ultraviolet (UV) rays and sunburn should be:
- Wide-brimmed - Peaked baseball caps offer good protection to the nose, but not other areas of the face, ears and back of the neck. Hats with a wide brim (at least 7.5 cm/3 ins.) are necessary to provide adequate protection.Footnote 113
- Breathable - Breathable fabrics are practical for evaporative cooling and decreasing heat accumulation in the hat.Footnote 114
Umbrella - Using an umbrella to avoid sun (radiant load) exposure is ideal as it does not interfere with evaporative cooling and provides a lot of shade.
Sunburn - UV exposure could result in sunburn. Sunburned skin loses its sweating efficiency, which impairs the ability of the body to regulate its temperature.Footnote 115
Sun safety - If sun exposure is unavoidable, recommend the use of a sunscreen lotion that is SPF 15 or higher and that users follow the manufacturer's directions for safe use.Footnote 116 Remind your audience that sunscreen and insect repellents can be safely used together, and that they should apply the sunscreen first, then the insect repellent.
3. Evaluating Heat-Health Communication Campaigns
Formal evaluation of heat-health communication campaigns can help to improve communication strategies and messages, and will ensure that they are costeffective and appropriate for your audience.
There are three main types of evaluation:
- formative (described in Section 2)
- process
- outcome

To evaluate programs, campaign leaders may use informal feedback from stakeholders and target audiences, as well as their own observations from past experiences. However, this type of evaluation is often based on incomplete data and may be biased. Formal evaluation is more credible and is better for accurately capturing the strengths and weaknesses of heat-health communication campaigns.Footnote 117
Formal and informal evaluations shouldFootnote 117 :
- aim to strengthen and improve the campaign
- use multiple approaches when feasible
- address real community issues identified in the early stages of the evaluation
- use a participatory process as much as possible
The evaluation plan should be simple and costeffective. It should also include those involved in developing and participating in the campaign (e.g. audiences, stakeholders, government and nongovernment organizations).Footnote 118 Engaging these groups and receiving constant feedback will ensure identification of common goals among stakeholders, realistic expectations of the campaign outcomes, and appropriate measurable indicators for use in evaluation.Footnote 119
Develop an evaluation plan along with the communication campaign to best capture opportunities for data gathering during the implementation phase. Base the plan on the ultimate goals and intermediate objectives of the campaign.
Evaluations could be completed using qualitative (focus groups, interviews, questionnaires, diaries) and quantitative (surveys, analysis of records, service utilization, morbidity/mortality data) methods (Appendix F).
Campaign evaluations will help you toFootnote 117 Footnote 118 :
- assess the effectiveness/impacts of campaign activities by identifying successes and shortfalls
- evaluate the use of time and resources (cost- benefit analysis)
- assess whether the needs of your partner organizations and target audiences were met
- assess progress in achieving intermediate goals and ultimate objectives
- apply lessons learned to improve future heat-health communication activities
- justify financial support
3.1 Process Evaluation
Process evaluation is used to examine a program during its implementation.
A process evaluation examines services related to implementation of the campaign and allows the campaign leader to assessFootnote 117 Footnote 118 :
- the effectiveness of the campaign regarding use of channels and vehicles to get your heat-health messages to audiences
- whether the audience has equal opportunity to participate in the program
- target audience reach, especially for specific services offered to reduce barriers to action (e.g. number and demographic make-up of visitors to cooling facilities)
- the clarity of messages identifying actions needed to protect health
- the appropriate use of resources to realize objectives
- Type of work performed
- Staff time spent on program at various stages
- Expenditures/costs
- Promotion/publicity earned
- Participation rate of your stakeholders (could be measured over time)
- Number and type(s) of inquiries received
- Number and type(s) of resources distributed
- Number and type(s) of groups formed
- Number and type(s) of training sessions held
- Number of contacts made
- Level of client/stakeholder satisfaction
Source: Health Communication Unit, 2007.117
As part of a process evaluation, it is important to monitor and evaluate news and trends to identify emerging needs of the audience and stakeholders, allow for timely response to new scientific developments, address criticisms and build partnerships.Footnote 119 Monitoring includes:
- collecting and reviewing published documents (e.g. peer-reviewed literature, newsletters, reports)
- analyzing media coverage for consistency and support
- performing Internet searches of reliable sites (e.g. Health Canada) to get the latest information about heat-health risks and effective adaptation strategies
- tracking Internet traffic on heat-health web pages
- meeting with key players (e.g. target audience, stakeholders, health care professionals)
- interviewing stakeholders and the public following awareness-raising activities
3.2 Outcome Evaluation
Outcome evaluation is appropriate for well-developed heat-health communication campaigns that have been implemented over a number of years and have made progress toward campaign objectives.
Outcome evaluation, also known as summative evaluation, should focus onFootnote 117 :
- Intermediate objectives - immediate changes in people's behaviour and views of heat-health issues.
- Ultimate goals - reductions in heat-related morbidity and mortality.
Intermediate objectives
- Changes in policies (e.g. urban heat island, building standards)
- Changes in awareness, knowledge or beliefs
- Benefits to participants or barriers to actions
- Changes in service utilization
- Level of self-care before and during extreme heat events
- Changes in social network interactions such as engagement with family members, friends, co-workers, neighbours
Ultimate goals
- Changes in morbidity and mortality rates
- Changes in health-protective behaviours
- Changes in social norms that protect health
Source: Health Communication Unit, 2007.Footnote 117
3.3 Evaluation Results
Document the results of the formal evaluation to guide future efforts to strengthen heat-health communication activities. Share them with team members and stakeholders, through presentations, discussions, meetings and e-mail updates.Footnote 119 The evaluation reports should be published and available for disseminationFootnote c .Footnote
Evaluation activities are most beneficial when they are ongoing, as behaviour changes take place over time. Long-term efforts to measure impacts are needed to ensure sustained behavioural adaptations during extreme heat events. Even if behavioural changes are observed shortly after a program is launched, it does not mean that they will be sustained over time.Footnote 119
Appendices
Appendix A: Plain-Language Checklist
The plain-language checklist can be used to develop or modify heat-health messages.
- Avoid acronyms and complex/technical language or provide definitions where necessary.
- Use familiar words and a conversational, personal tone.
- Proceed logically, in order of importance, and provide links between paragraphs.
- Use action verbs and active construction (versus passive).
- Favour short words and short sentences.
- Use short paragraphs when possible.
- Use concrete examples to illustrate ideas or concepts.
- Present ideas with illustrations or diagrams if this makes them easier to understand.
- Highlight main ideas and important information with sub-headings, point-form lists and boldface type.
Source: Adapted from Health Canada, 1999 and U.S. Centers for Disease Control and Prevention, 2002.Footnote 54 Footnote 124
Appendix B: Heat-Health Communication Message Review Tool
This message review tool can be used with stakeholders and target audiences to evaluate the appropriateness of heat-health messages.
| Excellent | Very Good | Fair | Fail | |
|---|---|---|---|---|
| The message will get and maintain the attention of the audience. | ||||
| The strongest points are given at the beginning of the message. | ||||
| The message is clear (i.e. it is easy for the audience to point out the actions to take; the incentives or reasons for taking those actions; the evidence for the incentives and any background information or definitions). | ||||
| The action you are asking the audience to take is reasonably easy. | ||||
| The message uses incentives effectively (more than one type of incentive is used; the audience cares about the incentives presented; the audience thinks the incentives are serious and action is likely to be taken). | ||||
| Good evidence for threats and benefits is provided. | ||||
| The messenger is seen as a credible source of information. | ||||
| Messages are believable. | ||||
| The message uses an appropriate tone for the audience. | ||||
| The message uses an appeal that is appropriate for the audience (i.e. rational or emotional). | ||||
| The message will not harm or be offensive to people who see or hear it. | ||||
| Target audience identity is displayed throughout the message. | ||||
| The message is consistent with other health promotional materials (e.g. ultraviolet radiation, air quality, infectious diseases, green city, energy-use reduction campaigns). |
Final Recommendation
- Use
- Adapt
- Reject
- Comments:
Source: Adapted from the Health Communication Unit, 2002.Footnote 125
Appendix C: Heat-Health Messages
Message 1:
Heat illnesses are preventable.
Message 2:
While extreme heat can put everyone at risk from heat illnesses, health risks are greatest for:
- older adults;
- infants and young children;
- people with chronic illnesses, such as breathing difficulties, heart conditions, or psychiatric illnesses;
- people who work in the heat;
- people who exercise in the heat;
- homeless people; and
- low-income earners.
Message 3:
If you are taking medication or have a health condition, ask your doctor or pharmacist if it increases your health risk in the heat and follow their recommendations.
Message 4:
Heat illnesses include heat stroke, heat exhaustion, heat fainting, heat edema (swelling of hands, feet and ankles), heat rash and heat cramps (muscle cramps).
Watch for symptoms of heat illness, which include:
- dizziness or fainting;
- nausea or vomiting;
- headache;
- rapid breathing and heartbeat;
- extreme thirst; and
- decreased urination with unusually dark yellow urine.
If you experience any of these symptoms during extreme heat, immediately move to a cool place and drink liquids. Water is best.
Message 5:
Heat stroke is a medical emergency! Call 911 or your local emergency number immediately if you are caring for someone, such as a neighbour, who has a high body temperature and is either unconscious, confused or has stopped sweating.
While waiting for help - cool the person right away by:
- moving them to a cool place, if you can;
- applying cold water to large areas of the skin or clothing; and
- fanning the person as much as possible.
Message 6:
Frequently visit neighbours, friends and older family members, especially those who are chronically ill, to make sure that they are cool and hydrated.
Message 7:
Drink plenty of cool liquids, especially water, before you feel thirsty to decrease your risk of dehydration. Thirst is not a good indicator of dehydration.
Message 8:
Reschedule or plan outdoor activities during cooler parts of the day.
Message 9:
Wear loose-fitting, light-coloured clothing made of breathable fabric.
Message 10:
Never leave people or pets in your care inside a parked vehicle or in direct sunlight.
Message 11:
Take a break from the heat by spending a few hours in a cool place. It could be a tree-shaded area, swimming facility or an air-conditioned spot such as a public building, shopping mall, grocery store, place of worship or public library.
Message 12:
Take cool showers or baths until you feel refreshed.
Message 13:
Prepare meals that don't need to be cooked in your oven.
Message 14:
Block sun out by closing awnings, curtains or blinds during the day.
Message 15:
Avoid sun exposure. Shade yourself by wearing a wide-brimmed, breathable hat or using an umbrella.
Appendix D: Heat-Health Fact Sheet-Older Adults
Protect yourself from the dangers of very HOT weather
It's way too HOT!
Know your risks

Hot temperatures can be dangerous, especially if you have:
- breathing difficulties;
- heart problems
- hypertension;
- kidney problems;
- a mental illness such as depression or dementia;
- Parkinson's disease; or
- if you take medication for any of these conditions.
If you are taking medication or have a health condition, ask your doctor or pharmacist if it increases your health risk in the heat and follow their recommendations.
Heat illnesses include heat stroke, heat exhaustion, heat fainting, heat edema (swelling of hands, feet and ankles), heat rash and heat cramps (muscle cramps). Heat illnesses can affect you quickly and are mainly caused by over-exposure to heat or over-exertion in the heat.
Five steps to protect your health in very HOT weather
Step 1 Prepare for the heat
Tune in regularly to local weather forecasts and alerts so you know when to take extra care.
Arrange for regular visits by family members, neighbours or friends during very hot days in case you need assistance. Visitors can help identify signs of heat illness that could be missed over the phone.
If you have an air conditioner, make sure it works properly before the hot weather starts. Otherwise, find an air-conditioned spot close by where you can cool off for a few hours during very hot days. This will help you cope with the heat better.
Step 2 Pay close attention to how you - and those around you - feel
Watch for symptoms of heat illness, which include:
- dizziness or fainting;
- nausea or vomiting;
- headache;
- rapid breathing and heartbeat;
- extreme thirst (dry mouth or sticky saliva); and
- decreased urination with unusually dark yellow urine.
If you experience any of these symptoms during hot weather, immediately move to a cool place and drink liquids. Water is best.
Heat stroke is a medical emergency! Call 911 or your local emergency number immediately if you are caring for someone, such as a running partner, who has a high body temperature and is either unconscious or confused.
While waiting for help - cool the person right away by:
- moving them to a cool place, if you can;
- applying cold water to large areas of the skin or clothing; and
- fanning the person as much as possible.
Step 3 Stay hydrated
Drink plenty of cool liquids, especially water, before you feel thirsty to decrease your risk of dehydration. Thirst is not a good indicator of dehydration.
- Remind yourself to drink water by leaving a glass by the sink.
- Flavouring water with natural fruit juice may make it more appealing.
- Eat more fruits and vegetables as they have a high water content.
- If you eat less, you may need to drink more water.
Step 4 Stay cool
Dress for the weather - Wear loose-fitting, light-coloured clothing made from breathable fabric.
Keep your home cool.
- If you have an air conditioner with a thermostat, keep it set to the highest setting that is comfortable (somewhere between 22°C/72°F and 26°C/79°F), which will reduce your energy costs and provide you with needed relief. If you are using a window air conditioner, cool only one room where you can go for heat relief.
- Prepare meals that don't need to be cooked in your oven.
- Block the sun by closing awnings, curtains or blinds during the day.
- If safe, open your windows at night to let cooler air into your home.
If your home is extremely hot:
- Take a break from the heat by spending a few hours in a cool place. It could be a tree-shaded area, swimming facility or an air-conditioned spot such as a shopping mall, grocery store, place of worship or public library.
- Take cool showers or baths until you feel refreshed. Make sure to use non-slip surfaces in the tub and shower, and wipe up moisture immediately to avoid slipping.
- Use a fan to help you stay cool and aim the air flow in your direction.
Step 5 Avoid exposure to very hot temperatures when outdoors
Never leave people or pets in your care inside a parked vehicle or in direct sunlight.
- When outside air temperature is 23°C/73°F, the temperature inside a vehicle can be extremely dangerous - more than 50°C/122°F.
Reschedule or plan outdoor activities during cooler parts of the day.
- Before heading out, check the Air Quality Health Index (AQHI) in your area, if available - air pollution tends to be at higher levels during very hot days.
- If you are in an area where mosquitoes are active, protect yourself with insect repellent and follow the manufacturer's directions.
Avoid sun exposure. Shade yourself by wearing a wide-brimmed, breathable hat or using an umbrella.
- Tree-shaded areas could be as much as 5°C/9°F cooler than the surrounding area.
- Use a sunscreen that is SPF 15 or higher and follow the manufacturer's directions. Remember, sunscreen will protect against the sun's ultraviolet (UV) rays but not from the heat.
- Sunscreen and insect repellents can be safely used together. Apply the sunscreen first, then the insect repellent.
Additional Resources
Public Health Agency of Canada's "You CAN prevent falls!"
www.phac-aspc.gc.ca/seniors-aines/publications/public/injury-blessure/preventeviter/ index-eng.php
Health Canada's "It's Your Health - Insect Repellents"
www.hc-sc.gc.ca/hl-vs/iyh-vsv/life-vie/insect-eng.php
Health Canada's "Sun Safety"
www.hc-sc.gc.ca/hl-vs/pubs/sun-sol/safety-prudence-eng.php
Environment Canada's "Air Quality Health Index"
www.airhealth.ca
Appendix D: Heat-Health Fact Sheet-Physically Active
Protect yourself from the dangers of EXTREME HEAT
You're ACTIVE in the HEAT! You're at RISK!
Know your risks

Being physically active provides many health benefits, but during extreme heat it can put you at risk even if you are healthy. Your risk increases if you have:
- breathing difficulties;
- heart problems;
- a mental illness such as depression;
- hypertension; or
- kidney problems.
If you are taking medication or have a health condition, ask your doctor or pharmacist if it increases your health risk in the heat and follow their recommendation.
Heat illnesses can lead to long-term health problems and even death. These illnesses include heat stroke, heat exhaustion, heat fainting, heat edema (swelling of hands, feet and ankles), heat rash and heat cramps (muscle cramps), and are mainly caused by over-exposure to extreme heat or over-exertion for a person's age and physical condition.
How your body regulates its temperature
Your body produces heat, especially during physical activity. Hot air and exposure to direct sun rays or hot surfaces also heat your body. This heat is lost by contact with cool air and by sweat production, which cools your body as the sweat evaporates. Weather conditions play a big role in how your body regulates its temperature. For example, if it's windy, sweat evaporates faster, which helps to cool you. However, high humidity slows down this process, contributing to increased body temperature.
Four steps to increase your comfort and protect your health during extreme heat:
Step 1 Get ready for extreme heat
Your body is not used to (not acclimatized to) extreme heat at the beginning of the summer. You are also not acclimatized if you don't exercise regularly during hot weather.
- Know what the outdoor temperature is before you start so you can modify your physical activity as needed.
- Ask your sports organization or trainer if they have a plan for extreme heat.
- Ask your coach, trainer or a teammate to pay special attention to you during extreme heat if you are particularly at risk. If you suffer from asthma, make sure you carry your inhaler with you, and that those around you are aware of your condition.
Step 2 Stay alert and pay close attention to how you - and those around you - feel
Protect your health - watch for symptoms of heat illness, which include:
- dizziness or fainting;
- nausea or vomiting;
- headache;
- unusually rapid breathing and heartbeat; and
- extreme thirst.
If you experience any of these symptoms during extreme heat, immediately move to a cool place and drink liquids. Water is best.
Heat stroke is a medical emergency! Call 911 or your local emergency number immediately if you are caring for someone, such as a running partner, who has a high body temperature and is either unconscious or confused.
While waiting for help - cool the person right away by:
- moving them to a cool place, if you can;
- applying cold water to large areas of the skin or clothing; and
- fanning the person as much as possible.
Never leave people or pets in your care inside a parked vehicle or in direct sunlight.
- When the outside air temperature is 23°C/73°F, temperatures inside a vehicle can be extremely dangerous - more than 50°C/122°F.
Step 3 Stay cool and hydrated
Drink plenty of cool liquids, especially water, before you feel thirsty. Thirst is not a good indicator of dehydration. By the time you feel thirsty, you are already dehydrated.
- Drink plenty of water before, during and after being physically active.
- Wear loose-fitting, light-coloured clothing made of breathable fabric.
- Increase your comfort by splashing yourself with cold water.
Step 4 Modify your activities
Reschedule or find alternatives - If you can, reschedule strenuous outdoor activity to a cooler part of the day or another day. There are ways in which you can still be physically active while avoiding the heat, such as:
- exercising in an air-conditioned place; or
- choosing a cooler outdoor location such as a tree-shaded area away from high traffic to avoid higher levels of air pollution. These spots can be as much as 5°C/9°F cooler than the surrounding area.
- Before heading out, check the Air Quality Health Index (AQHI) in your area, if available - air pollution tends to be higher during extreme heat. When active, you are more sensitive to air pollution because you breathe deeply and allow more air to enter your lungs.
- If you are in an area where mosquitoes are active, protect yourself with insect repellent and follow the manufacturer's directions.
Be realistic - Try not to expect the usual performance from yourself during extreme heat.
Take extra water breaks - Move into the shade, drink water and remove gear, such as a helmet or equipment, to let your body cool off.
Avoid sun exposure - Exposure to direct sun will heat your body and can result in sunburn. Sunburned skin loses its sweating efficiency, which impairs your body's ability to regulate its temperature.
- Shade yourself by wearing a wide-brimmed, breathable hat or using an umbrella.
- If you can't avoid the sun, use a sunscreen that is SPF 15 or higher and follow the manufacturer's directions. Remember, sunscreen will protect you from the sun's ultraviolet (UV) rays but not from the heat.
- Sunscreen and insect repellents can be safely used together. Apply the sunscreen first, then the insect repellent.
Recover - Allow your body to recover after heat exposure. Spend a few hours in a cooler tree-shaded area or somewhere that's air conditioned, such as your home, a shopping mall, grocery store, public building or public library.
Additional Resources
Health Canada's "It's Your Health - Insect Repellents"
www.hc-sc.gc.ca/hl-vs/iyh-vsv/life-vie/insect-eng.php
Health Canada's "Sun Safety"
www.hc-sc.gc.ca/hl-vs/pubs/sun-sol/safety-prudence-eng.php
Public Health Agency of Canada's "Canada's Physical Activity Guide to Healthy Active Living"
www.phac-aspc.gc.ca/hp-ps/hl-mvs/pag-gap/pdf/handbook-eng.pdf
Environment Canada's "Air Quality Health Index"
www.airhealth.ca
Appendix D: Heat-Health Fact Sheet-Young Children
Protect your child from the dangers of EXTREME HEAT
Keep children COOL!
Children are at risk

Extreme heat can be dangerous for all children, especially for infants and young children.
Heat illnesses include heat stroke, heat exhaustion, heat fainting, heat edema (swelling of the hands, feet and ankles), heat rash (prickly heat) and heat cramps (muscle cramps). They are mainly caused by over-exposure to heat or over-exertion in the heat, and if not prevented, can lead to long-term health problems
Five steps to protect your child's health during extreme heat
Step 1 Prepare for extreme heat
Stay informed about local weather forecasts and alerts so you know when to take extra care.
If you have an air conditioner, make sure it works properly before the hot weather starts. Otherwise, find an air-conditioned spot near you that you can use to cool off for a few hours during extreme heat.
Learn about ways to keep your home cool during the summer. For example, if you live in a house, plant trees on the side where the sun hits the house during the hottest part of the day.
Step 2 Watch your child's health closely
Stay alert for symptoms of heat illness. They include:
- changes in behaviour (sleepiness or temper tantrums);
- dizziness or fainting;
- nausea or vomiting;
- headache;
- rapid breathing and heartbeat;
- extreme thirst; and
- decreased urination with unusually dark yellow urine.
If you see any of these signs during extreme heat immediately move the child to a cool place and give liquids. Water is best. If you are breastfeeding your child, breast milk will provide adequate hydration, but remember to keep yourself hydrated so you can produce a sufficient amount of milk.
Heat stroke is a medical emergency! Call 911 or your local emergency number immediately if you are caring for a child who has a high body temperature and is unconscious, confused, or has stopped sweating.
While waiting for help - cool the child right away by:
- moving them to a cool place;
- applying cold water to large areas of the skin or clothing; and
- fanning the child as much as possible.
Children most at risk include those with breathing difficulties (asthma), heart conditions, kidney problems, mental and physical disabilities, developmental disorders, diarrhea, and those who take certain medications. Ask your doctor or pharmacist if the medication increases risk to their health in the heat and follow their recommendations.
Step 3 Keep your child hydrated
DEHYDRATION is dangerous. Give plenty of cool liquids to drink, especially water, before your child feels thirsty.
- Make it fun - leave a colourful glass by the sink and remind your child to drink after every hand washing.
- Make it tasty - flavouring water with natural fruit juice may make it more appealing.
- Make it healthy - provide extra fruits and vegetables as they have a high water content.
- Make it a routine - encourage your child to drink water before and after physical activity.
Step 4 Keep your child cool
Dress your child in loose-fitting, light-coloured clothing made from a breathable fabric.
Keep your home cool.
- If you have an air conditioner with a thermostat, keep it set to the highest setting that is comfortable (somewhere between 22°C/72°F and 26°C/79°F), which will reduce your energy costs and provide needed relief. If you are using a window air conditioner, cool only one room where you can go for heat relief.
- Prepare meals that don't need to be cooked in your oven.
- Block the sun by closing awnings, curtains or blinds during the day.
- If safe, open your windows at night to let cooler air into your home.
If your home is extremely hot:
- Take a break from the heat and spend a few hours with your child in a cool place. It could be a tree-shaded area, swimming facility, spray pad or an air-conditioned spot such as a shopping mall, grocery store or public library.
- Bathe your child in a cool bath until your child feels refreshed.
- Always supervise your child in the bath.
- If using a fan, keep it at a safe distance from the child and aim the air flow in their direction.
Step 5 Avoid exposing your child to extreme heat when outdoors
Never leave children inside a parked vehicle or in direct sunlight.
- When outside air temperature is 23°C/73°F, the temperature inside a vehicle can be extremely dangerous - more than 50°C/122°F.
Reschedule or plan outdoor activities during cooler parts of the day.
- Before heading out, check the Air Quality Health Index (AQHI) in your area, if available - children are more sensitive to air pollution, which tends to be at higher levels during extreme heat.
- If you are in an area where mosquitoes are active, protect uncovered skin with insect repellent and follow the manufacturer's directions.
Avoid sun exposure - Keep your child in the shade or protected from the sun by wearing a wide-brimmed, breathable hat or shade them with an umbrella.
- Tree-shaded areas could be as much as 5°C/9°F cooler than the surrounding area.
- If sun exposure can't be avoided, use sunscreen that is SPF 15 or higher and follow the manufacturer's directions. Remember, sunscreen will protect against the sun's ultraviolet (UV) rays but not from the heat.
- Don't apply sunscreen to a child less than 6 months old.
- Sunscreen and insect repellents can be used safely together. Apply the sunscreen first, then the insect repellent.
Additional Resources
Health Canada's "Babies, children and sun safety"
www.hc-sc.gc.ca/hl-vs/pubs/sun-sol/babies_child-bebes_enfant-eng.php
Health Canada's "Is your child safe?"
www.hc-sc.gc.ca/cps-spc/pubs/cons/child-enfant/index-eng.php
Health Canada's "It's Your Health - Insect Repellents"
www.hc-sc.gc.ca/hl-vs/iyh-vsv/life-vie/insect-eng.php
Environment Canada's "Air Quality Health Index"
www.airhealth.ca
Appendix E: Heat Advisory Media Release Template
[Citizens of public] Urged to Take Precautions for Upcoming Extreme Heat Event
[DATE] For Immediate Release
[PLACE] - The Chief Medical Officer of Health, [NAME], is advising [PLACE] to take steps to prevent heat-related illness during the upcoming extreme heat event, also known as a "heat wave."
With temperatures expected to rise in the next [days], Environment Canada has issued a humidex advisory (humidex values in excess of 40).
While extreme heat can put everyone at risk from heat illnesses, health risks are greatest for older adults, infants and young children, people with chronic illnesses such as breathing difficulties, heart conditions or psychiatric illnesses, people who work or who exercise in the heat, homeless people and low-income earners. Those who take medication or have a health condition should ask their doctor or pharmacist if it increases their health risk in the heat and follow their recommendations.
Heat illnesses are preventable, but they can lead to long-term health problems and even death. If any symptoms of heat illness are present (such as dizziness or fainting, nausea or vomiting, headache, rapid breathing and heartbeat, or extreme thirst), immediately move to a cool place and drink liquids. Water is best. The most dangerous heat illness is heat stroke, with symptoms that include complete or partial loss of consciousness or confusion and high body temperature. If caring for someone with these symptoms, call [LOCAL EMERGENCY NUMBER] immediately. While waiting for help, cool the person right away by moving them to a cool place, applying cold water to large areas of the skin or clothing and fanning the person as much as possible.
Public health officials urge everyone to stay alert and take precautions. Remember to frequently visit neighbours, friends and older family members, especially those who are chronically ill, to make sure that they are cool and hydrated.
[PLACE] Public Health recommends taking the following actions to stay cool:
- Drink plenty of cool liquids, especially water, before feeling thirsty.
- Wear loose-fitting, light-coloured clothing made of breathable fabric.
- Take cool showers or baths until you feel refreshed.
- Take a break from the heat by spending a few hours in a cool place.
- Block sun out by closing awnings, curtains or blinds during the day.
- Avoid sun exposure. Shade yourself by wearing a wide-brimmed, breathable hat or using an umbrella.
- Reschedule or plan outdoor activities during cooler parts of the day.
- Never leave people or pets in your care inside a parked vehicle or in direct sunlight.
Additional tips on how to stay safe and what to do during an extreme heat-related emergency are available on the following websites: [Insert web links]
MEDIA CONTACT: [NAME, PHONE NUMBER]
Appendix F: Public Involvement Strategies
| Method Description | Excellent | Limitations |
|---|---|---|
Focus groups
|
|
|
In-depth interviews
|
|
|
Open-ended survey questions
|
|
|
Diaries
|
|
|
Surveys
|
|
|
Process tracking forms/records
|
|
|
Large data sets
|
|
|
Source: Adapted from the Health Communication Unit, 2007.Footnote 117