Guidelines for Canadian drinking water quality – Malathion: Health considerations, derivation of the health-based value
On this page
Health considerations
All pesticides, including malathion, are regulated by Health Canada's PMRA. PMRA conducts extensive evaluations and cyclical reviews of pesticides, including unpublished and proprietary information, as well as foreign reviews by other regulatory agencies such as the United States Environmental Protection Agency (U.S. EPA). As such, this health assessment is primarily based on PMRA evaluations (Health Canada, 2003, 2010, 2012) and supporting documentation. Any reviews and relevant literature available since the PMRA evaluations were completed were also considered.
Kinetics
Absorption
Following oral exposure, malathion is readily and rapidly absorbed from the gastrointestinal tract (mostly in the intestine) in mammals, including humans (based on excretion data), with peak plasma levels being reached 15 minutes post-dosing in rats (Reddy et al., 1989; Aston, 2000; Gillies and Dickson, 2000; Jellinek, Schwartz & Connolly Inc., 2000; ATSDR, 2003; EFSA, 2009; Health Canada, 2010; IARC, 2017; WHO, 2017a). Dermal absorption of malathion occurs readily and is expected to be slower than oral absorption and varied among species, with rabbits demonstrating a substantially greater capacity for dermal absorption of malathion (for example, 64.6% for rabbits, 15.5% for pigs in vitro, 6% for rats and 0.2% to 8.2% for humans) (ATSDR, 2003; Gervais et al., 2009; Health Canada, 2010; WHO, 2017a).
Distribution
Malathion is rapidly distributed in the body, with no evidence of bioaccumulation (Health Canada, 2010). In human volunteers, no malathion nor malaoxon was detected in plasma at 1 to 12 hours following the administration of a single oral dose (LOD = 100 to 102 and 99.8 to 100 ng/ml, respectively) (Aston, 2000; Gillies and Dickson, 2000; Jellinek, Schwartz & Connolly Inc., 2000). In rats gavaged with 14C-malathion, less than 1.5% of the administered dose was detected in the tissues at 72 hours, with the highest concentration observed in the liver, followed by skin, fat, bone and gastrointestinal tract (Reddy et al., 1989).
Metabolism
Following oral exposure in rats and humans, malathion is fully metabolized, with no parent compound present in urine (Reddy, 1989; ATSDR, 2003; Health Canada, 2010; WHO, 2017a). The major metabolic pathway for both malathion and malaoxon is hydrolysis by tissue, liver or plasma carboxylesterases, resulting in the production of MCA and DCA metabolites (˃ 80% in rats) (Health Canada, 2010). Unlike rats, humans have no detectable levels of carboxylesterases in serum, plasma or erythrocytes, but may have more active liver carboxylesterases (ATSDR, 2003; IARC, 2017; WHO, 2017a). Malaoxon, the active metabolite of malathion, may be formed to a lesser extent (4% to 6% in rats) via oxidative desulphuration of malathion (minor pathway) by microsomal enzymes (ATSDR, 2003; Health Canada, 2010). Once formed, malaoxon is either excreted in the urine, rapidly hydrolyzed to malathion MCA and DCA, or further metabolized by phosphatases and carboxylesterase enzymes. In rats, no dose-related or sex-related differences in malathion metabolism were observed (Health Canada, 2010).
Excretion
In mammals, including humans, excretion of ingested malathion is rapid and occurs primarily in urine and to a lesser amount in feces (Reddy et al., 1989; Aston, 2000; Gillies and Dickson, 2000; Jellinek, Schwartz & Connolly Inc., 2000; ATDSR, 2003; Health Canada, 2010; WHO, 2017a). In human volunteers administered a single dose of malathion, approximately 90% of the dose was excreted in urine within 12 hours, with the entire dose excreted after 24 to 48 hours (Aston, 2000; Gillies and Dickson, 2000; Jellinek, Schwartz & Connolly Inc., 2000; WHO, 2017a). Malathion MCA was the most prevalent metabolite, followed by O,O-dimethyl phosphorothiolate, malathion DCA, dimethyl phosphate and dimethyl dithiophosphate (U.S. EPA, 2016; WHO, 2017a). In the rat, 76% to 88% of excretion occurred in urine within 72 hours of dosing (mainly as malathion MCA and DCA), whereas 6% to 14% occurred in feces. The excretion profile was similar for single or repeat low dose or single high dose administration in rats, with no sex differences reported (Health Canada, 2010).
Health effects
The toxicology database for malathion is adequate, covering several endpoints and various types of exposures (see ATSDR, 2003; IARC, 2017; WHO, 2017a for more thorough reviews). Signs of acute toxicity due to malathion exposure are consistent with ChE inhibition (tremors, convulsions, salivation and dyspnea) and were observed in a variety of species and by all routes of exposure. Young animals showed greater sensitivity to the effects of malathion on erythrocyte ChE than adults. From repeated-dose studies with malathion, the increase in severity of chronic progressive nephropathy in rats is considered the most sensitive adverse effect. Malathion was not found to be genotoxic or teratogenic in animal studies. It is unlikely to possess carcinogenic potential or pose a carcinogenic risk for humans based on its current registered use (Health Canada, 2010, 2021a).
Effects in humans
No human effects were discussed in PMRA assessments or their supporting documents (U.S. EPA, 2009; Health Canada, 2010, 2012). Studies were available from the literature concerning both cancer and non-cancer endpoints.
Agricultural Health Study
The Agricultural Health Study (AHS) is a large, ongoing questionnaire-based prospective cohort study of licensed pesticide applicators and their spouses (over 89,000 participants) who live in Iowa and North Carolina that investigates cancer and non-cancer endpoints. It began in 1993 with the collection of baseline information on farming practices (including pesticide use), lifestyle and health. Follow-up interviews/questionnaires (including dietary information) and DNA collection were done periodically. Cancer registries were used to assess cancer incidence. Overall, strengths of the AHS include its large size; the inclusion of a large number of women; the collection of baseline, health and lifestyle information and genetic factors; the use of cancer registries and the many different pesticides and diseases assessed. Its limitations include the indirect assessment of exposure (questionnaires), the lack of exposure refinement measurements (no induction time or latency discussion) and selection bias when controlling for multiple confounders due to the exclusion of many subjects with missing data (Sathiakumar et al., 2011).
Cancer
Several investigators have published studies based on their analyses of the AHS cohort data. No associations were observed between exposure to malathion and the incidence of colorectal cancer (Lee et al., 2007), pancreatic cancer (Andreotti et al., 2009) and childhood cancer (Flower et al. 2004). Lerro et al. (2015) reported a significant increase in thyroid cancer incidence among AHS spouses, but also indicated they failed to control for exposure to elevated nitrate levels in food and drinking water, which has been proposed to play a role in thyroid cancer development in agricultural regions. Although Engel et al. (2005) reported no increased risk of breast cancer in spouses enrolled in the AHS who had used malathion themselves, an association was noted in wives whose husbands had used the pesticide. The inconsistencies in findings may be due to limitations such as self-reported exposure and the potential for exposure to multiple pesticides (WHO, 2017a). In case-control analyses by Mills and Yang (2005) and Mills et al. (2019), an elevated risk of breast cancer was observed in Hispanic agricultural workers who had used malathion. Findings in these studies were difficult to interpret, as the number of exposed cases were either not mentioned or were small. In Mills et al. (2019), the response fraction for controls was only 3% compared to 66% for cases, while in Mills and Yang (2005), the response rate was not reported. Although pesticide exposure estimates in both studies used an ecological exposure assessment method and were obtained through record linkages, thus avoiding recall bias, the use of pesticide use reports rather than individual pesticide exposure data may have resulted in exposure misclassification (IARC, 2017).
In examining AHS data from 1993 to 2007, Koutros et al. (2013) reported a significant increase in aggressive prostate cancer risk in the highest malathion exposure category, but found no association between total prostate cancer and malathion exposure. In a case-control study, Mills and Yang (2003) also found no evidence of an association between total prostate cancer and malathion exposure among Californian farm workers. However, the data may have been subject to misclassification as the classification of exposure was based on ecological rather than individual exposure (IARC, 2017; WHO, 2017b). In contrast, Band et al. (2011) reported a correlation between malathion usage and total prostate cancer in British Columbian farmers, with significant dose-response effects. However, pesticide exposures were assessed using a job-exposure matrix and were susceptible to misclassification; also, the data were not corrected for multiple pesticide exposure (Band et al., 2011; IARC, 2017; WHO, 2017b).
Based on the AHS cohort data, no increased risk of non-Hodgkin's lymphoma (NHL) was observed in male pesticide applicators using malathion, while a decreased association was observed in spouses of applicators using the pesticide (Alavanja et al., 2014; Lerro et al., 2015). Investigating agricultural cohorts from France and Norway and from AHS in the United States, Leon et al. (2019) also reported a lack of association between malathion use and risk of NHL, although there is a possibility of exposure misclassification due to the use of "crop-exposure matrices" to estimate exposures. In contrast, a cross-Canada, population-based, case-control study demonstrated a significant association between NHL and "ever use" of malathion in comparison to "never use" and for annual days of use amongst men in a diversity of occupations (McDuffie et al., 2001). A similar association was reported in pooled data from 3 United States Midwestern case-control studies. However, the association was attenuated or no longer significant upon removal of proxy respondents from the analyses and more robust adjustments for other pesticides (Waddell et al., 2001; De Roos, 2003; WHO, 2017b). Koutros et al. (2019) further evaluated the potential link between malathion exposure and NHL using pooled data from the cross-Canada study and the 3 United States Midwestern studies. A significantly increased risk of NHL was observed among "ever users" of malathion compared to "never users" after adjustment for use of other pesticides, as well as an association between malathion use and certain NHL subtypes. Analyses of the pooled data also demonstrated a significant exposure-response relationship with years of malathion use (Koutros et al., 2019). While the larger dataset considered by Koutros et al. (2019) allowed for a more powerful assessment, limitations attributable to the individual case-control studies (for example, recall bias, use of proxy respondents) create a potential for exposure misclassification.
Although positive associations have been observed between exposure to malathion and certain cancers, most notably NHL, no associations have been seen in other studies for the same cancer endpoint making the findings difficult to interpret. Study limitations (for example, small number of cases, failure to control for confounders, use of proxy respondents, recall bias and potential for exposure misclassification) and the limited number of populations studied may account for some of the inconsistencies between different study findings and preclude definitive conclusions on the relationship between exposure to malathion and cancer risk.
Non-cancer
In evaluating non-cancer endpoints in the AHS cohort data, investigators have reported respiratory effects, including wheeze, chronic bronchitis symptoms (occurring with and without chronic obstructive pulmonary disease) and adult onset of allergic asthma in females and non-allergic asthma in males related to malathion exposure (Hoppin et al., 2002, 2006, 2008, 2009; Rinsky et al., 2019). Kamel et al. (2007) did not find a strong association between Parkinson's disease and exposure to malathion in the AHS. In studies evaluating the associations between "ever usage" of malathion and incidence of diabetes, no association was observed among farmers or their wives (Montgomery et al., 2008; Starling et al., 2014). Goldner et al. (2010, 2013) observed no significant association between "ever use" of malathion and hypothyroidism in either male applicators or their female spouses in the AHS based on data collected up to 2010. However, follow-up studies by Shrestha et al. (2018, 2019) using AHS data up to 2016, reported an increased risk of incidence of hypothyroidism and a reduced risk of hyperthyroidism with malathion exposure.
In a controlled ingestion study, groups of five male volunteers were administered malathion-containing capsules (purity not specified) in doses of approximately 0.11 mg/kg body weight (bw) per day for 32 days, 0.23 mg/kg bw per day for 47 days or 0.34 mg/kg bw per day for 56 days (Moeller and Rider, 1962; ATSDR, 2003). No significant decrease of plasma or erythrocyte activity or changes in blood counts or urinalyses resulted from the administration of 0.11 mg/kg bw per day of malathion for 32 days or 0.23 mg/kg bw per day for 47 days. Volunteers receiving 0.34 mg/kg bw per day for 56 days of malathion were observed to have a maximum 25% decrease in plasma ChE and erythrocyte ChE in absence of clinical signs (Moeller and Rider, 1962; ATSDR, 2003). The Moeller and Rider (1962) study was considered to be of poor quality owing to the inadequate reporting detail and limited protocol, including the use of small group sizes, extended exposure durations (32 to 56 days), and the apparent treatment of volunteers with other chemical substances. However, the study confirmed that animal species were indeed appropriate surrogates for assessing toxicity in humans as erythrocyte ChE depression was identified. This inhibition of ChE activity is corroborated by poison control center findings that associate cholinergic symptoms in humans with malathion exposure (Health Canada, 2021a).
A randomized double-blind study in human volunteers administered a single dose of malathion ranging from 0.5 to 15.0 mg/kg bw (27 male and 7 females test subjects, 11 male and 3 female controls), reported the absence of any treatment-related adverse effects on erythrocytes and plasma AChE activities and no alterations in vital signs, electrocardiograms, hematology, clinical chemistry, urinalysis and physical parameters, up to 24 or 48 hours after dosing (Gillies and Dickson, 2000). Similarly, another volunteer study examining the same dose levels administered as a single dose reported no treatment-related adverse effects on AChE activity (Jellinek, Schwartz and Connolly Inc., 2000).
Kidney injury, including nephrotic syndrome and acute renal failure, has been reported following acute inhalation and dermal exposure to malathion (Albright et al., 1983; Yokota et al., 2017).
Effects in animals
Repeat exposure studies in rats, mice, rabbits and dogs showed malathion-induced primarily kidney and neurological effects although other effects have also been noted (Shellenberger and Billups, 1987; Daly, 1993a, 1993b, 1996; ATSDR, 2003; EFSA, 2009; U.S. EPA, 2009; Health Canada, 2010; Barnett Jr., 2012a, 2012b; WHO, 2017a).
Malathion has been shown to be slightly acutely toxic to experimental animals via the oral, dermal and inhalation routes. The acute toxicity of malathion depends on its purity level. Oral median lethal dose (LD50) values of 2,382 to 8,200 mg/kg bw in rats (96.0% to 99.1% purity level), 6,100 mg/kg bw in female mice (95% purity level) and > 4,000 mg/kg bw in dogs (98% purity level) were reported for malathion. Dermal LD50 values for malathion were > 2 000 mg/kg bw in rats (96% to 98% purity level) and 8,900 mg/kg bw in rabbits (95.6% purity level). An inhalation medial lethal concentration (LC50) value of > 5.2 mg/L in rats (96% to 98% purity level) was also reported for malathion (FAO/WHO, 1997; Decker et al., 2003; U.S. EPA, 2009; Health Canada, 2010).
Kidney effects
Nephrotoxicity has been observed in rats and beagle dogs following oral administration (all durations of exposure) of malathion.
In a 24-month chronic toxicity/carcinogenicity study, groups of Fischer 344 rats (90/sex/dose) were administered malathion (97.1% pure) in the diet at doses of 0, 100/50 (reduced day 113), 500, 6,000 or 12,000 ppm (equivalent to 0, 2.4, 26, 327 or 677 mg/kg bw per day in males and 0, 3.0, 32, 386 or 817 mg/kg bw per day in females). Interim sacrifices (10 to 15/dose/sex) were performed at 3, 6 and 12 months (Daly, 1996). At 12 months and at terminal sacrifice, kidney weights (absolute, relative to body brain weights) were statistically significantly increased in both male and female rats at ≥ 6,000 ppm (≥ 327/386 mg/kg bw per day in males/females). Macroscopic findings at the end of the study included increased incidence of irregular surfaces of the kidneys at 500, 6,000 and 12,000 ppm (26, 327 and 677 mg/kg bw per day) in males and at 12,000 ppm (817 mg/kg bw per day) in females (U.S. EPA, 1997). An increased severity of chronic progressive nephropathy was observed in both sexes, that is, in females administered ≥ 500 ppm (≥ 32 mg/kg bw per day) of malathion and males administered ≥ 6 000 ppm (327 mg/kg bw per day), with the males also demonstrating an earlier onset of the disease at interim sacrifice (Health Canada, 2010).
Similar effects have been observed in sub-chronic toxicity studies with higher doses of malathion in both beagle dogs and rats. In a 52-week oral study, beagle dogs (6/sex/dose) were administered 62.5 to 250 mg/kg bw per day of malathion (95% pure) in capsules. At doses of ≥ 62.5 mg/kg bw per day, decreases in creatinine and blood urea nitrogen levels were observed accompanied by increases in absolute and relative kidney weights (Shellenberger and Billups, 1987). In a 90-day dietary toxicity study, groups of F344 rats (10/sex/group) were administered 100 to 20,000 ppm (equivalent to 6.6 to 1,190 mg/kg bw per day in males and 7.9 to 1,597 mg/kg bw per day in females) of malathion (96.4% pure). Increased relative kidney weights were observed at ≥ 340/384 mg/kg bw per day in males/females, and increased absolute kidney weights were observed at 680 mg/kg bw per day in males and ≥ 1 597 mg/kg bw per day in females. As well, an increased severity of chronic nephropathy was observed in males at ≥ 340 mg/kg bw per day (Daly, 1993b). In 2 dietary toxicity studies (28- and 29/30-day) where rats were administered malathion (95.8% and 96.4% pure, respectively), increases in relative kidney weights were observed starting at 457.5 mg/kg bw per day (Daly, 1993a; Barnett Jr., 2012a).
Toxic effects on kidney tissues were also observed in single-dose toxicity studies (≥ 100 mg/kg bw) in rats (Alp et al., 2011; Akbel et al., 2018; Selmi et al., 2018).
Neurotoxicity
Dose-related inhibition of plasma ChE, erythrocyte ChE and brain ChE activity has been observed in experimental animals (rats, mice, rabbits and beagle dogs) administered malathion by all exposure routes and for various durations of exposure (ATSDR, 2003; U.S. EPA, 2009; Health Canada, 2010; WHO, 2017a). Malathion neurotoxicity is due mainly to its activated metabolite malaoxon (refer to the section on mode of action).
Depression of erythrocyte ChE is considered an appropriate surrogate measure of potential effects on the nervous system, while depression of plasma ChE is not considered to be a toxicologically adverse effect, but serves as a marker of exposure following exposure to malathion (Health Canada, 2010). For animals exposed to malathion, erythrocyte ChE is the most sensitive compartment for ChE inhibition and is a suitable surrogate for peripheral neurotoxic effects in acute and some short-term studies. However, in longer studies, depression of erythrocyte ChE is not considered a toxicologically adverse effect due to the limitations related to the low rate of re-synthesis of erythrocyte ChE over extended periods.
Brain ChE inhibition typically occurred at higher doses than erythrocyte ChE and plasma ChE inhibition in all species. Clinical signs commonly associated with organophosphate exposure, including salivation, tremors, prostration and hypoactivity, were observed in repeat-dose studies at doses of malathion starting from 150 mg/kg bw per day (Health Canada, 2010). Assessment of the relative sensitivity of ChE activity with oral dosing reveals no appreciable species differences between mice, rats and dogs. Similarly, studies conducted via all exposure routes do not suggest a sex difference in sensitivity to the effects of malathion on ChE inhibition (Health Canada, 2010).
However, the current neurotoxicity database suggests that pre-weanling rats are more susceptible than adult rats to the neurotoxic effects of malathion following exposure from the oral route. Finally, neuropathological changes were not observed in the majority of mammalian toxicity studies. However, several isolated incidences of neuropathological changes have been observed in 2 rat studies at very high doses (1,500 mg/kg bw per day) in only 1 sex (males) and are considered equivocal (Health Canada, 2010).
In the 24-month chronic toxicity/carcinogenicity study by Daly (1996) where Fischer 344 rats (90/sex/dose) were fed diets containing 50 to 12,000 ppm (equivalent to 2.4 to 677 mg/kg/bw per day for males and 3.0 to 817 mg/kg bw per day for females) of malathion (97.1% pure), decreases in plasma ChE activity were observed at ≥ 500 ppm (≥ 26/32 mg/kg bw per day in males/females) while erythrocyte ChE and brain ChE activities were decreased at ≥ 6,000 ppm (≥ 327/386 mg/kg bw per day in males/females). In an 18-month dietary carcinogenicity study where malathion (96.4% pure) was administered to B6C3F1 mice (65/sex/group), decreases in plasma ChE and erythrocyte ChE activities were observed at ≥ 143/167 mg/kg bw per day (lowest dose tested) in males/females and decreases in brain ChE were observed at 2,978/3 448 mg/kg bw per day (highest dose tested) in males/females (Health Canada, 2010).
In sub-chronic oral toxicity studies with malathion (95% to 96.4% pure), inhibition of erythrocyte ChE, plasma ChE and/or brain ChE was observed at dose levels as low as 7.9 mg/kg per day (rats), 62.5 mg/kg bw per day (dogs) and 250 mg/kg bw per day (dogs), respectively (Shellenberger and Billups, 1987; Daly, 1993a; 1993b; Barnett Jr., 2012a, 2012b). In a 21-day dermal toxicity study in rabbits (10/sex/group), inhibition of erythrocyte ChE occurred at ≥ 75 mg/kg bw per day of malathion (96% pure) (lowest dose tested) and inhibition of plasma ChE and brain ChE occurred at 500 mg/kg per day (highest dose tested) (Health Canada, 2010).
In an acute delayed neurotoxicity study (gavage) using 12 hens, there was no evidence of delayed type neuropathology caused by the administration of malathion (EFSA, 2009; Health Canada, 2010; WHO, 2017a).
In a developmental neurotoxicity study, dose levels of 0, 5, 50 or 150 mg/kg bw per day of malathion (96.0% pure) in corn oil were administered (gavage) to 24 dams from gestational day (GD) 6 to postnatal day (PND) 10 and from PND 11 to 21 to the pups. At the highest dose, clinical signs were observed in the dams (post-dosing salivation) and the pups (for example, tremors, hypoactivity, prostrate posture, partially closed eyelids). Also in the pups, increased incidence of flattened gait (PND 60, males) and decreased motor activity (PND 17/22, females) were observed at ≥ 50 mg/kg bw per day. In a comparative ChE rat study, adults and PND 11 pups (8/sex/group) were treated (gavage) with 0, 5, 50, 150 or 450 mg/kg bw of malathion (96.0%) for 1 day. Repeated exposure by gavage (11 days) was also assessed in this study using similar doses in adults and PND 11 to 21 pups (8/sex/group), in 19 adult females (9 females treated GD 6-20, 10 females treated GD 1-10) and in pups (2/sex/litter/group) sacrificed 4 hours after dosing of the dam at PND 4. The results of the study showed that, at similar dose levels, PND 11 and PND 21 pups are more sensitive than are adult animals to the ChE-inhibiting effects of malathion. Benchmark dose calculations (using a benchmark dose response of 20% for erythrocyte ChE) suggest that the young animals are approximately 6.4 times and 1.8 times more sensitive to the ChE inhibiting effects of malathion compared to adults following acute and repeat dose oral exposure, respectively (Health Canada, 2010).
Reproductive/developmental toxicity
Malathion did not induce reproductive toxicity in rats at the highest dose tested, while fetotoxic effects occurred only at maternally toxic doses in rats and rabbits (Health Canada, 2010).
In a 2-generation (2 litters/generation) dietary reproductive toxicity study, Sprague-Dawley rats (25/sex/group) were administered 550 to 7,500 ppm (equivalent to 43 to 612 mg/kg bw per day in males and 51 to 703 mg/kg bw per day in females) of malathion (94% pure). No effect on the reproductive parameters or reproductive tissues was observed. However, decreases in weight gain in the parental rats (F0) (during gestation and lactation [females]) and in the first generation - first litter (F1) (during pre-mating) were observed at the highest dose. Decreased weights were observed in some first- and second-generation pups (1 of 2 litters in each generation) at PND 21 at 394/451 mg/kg bw per day in males/females and in all second-generation pups (4 litters) at the highest dose tested (Health Canada, 2010). In 80-week and 103-week feeding studies, no treatment-related gross or microscopic alterations in the prostate or testis of male rats or histopathological alteration in the mammary gland, uterus or ovaries of female rats were observed following the administration of up to 622 mg/kg per day and 332 mg/kg per day of malathion (95% pure), respectively (NCI 1978, 1979). Similar results were noted in male mice administered in the diet up to 2,980 mg/kg per day of malathion (95% pure) for 80 weeks. However, in the females, an increased incidence of cystic endometrial hyperplasia was observed following administration of 1,490 mg/kg bw per day of malathion (95% pure) for 80 weeks (NCI, 1978).
Malathion was evaluated for developmental toxicity in rats and rabbits. Following administration (gavage) to pregnant rabbits (20/group) of 25 to 100 mg/kg bw per day of malathion (95% pure) on GD 6-18, a slightly increased incidence of dams with resorptions (embryo-fetal loss) was observed at ≥ 50 mg/kg per day in the presence of maternal toxicity (decreases in weight gain during dosing). When malathion (94% pure) was administered by gavage to pregnant Sprague-Dawley rats (24 to 25/group, 200 to 800 mg/kg per day, GD: 6-15), a slightly increased incidence of dams with resorption sites was also observed at the highest dose in the presence of maternal toxicity. Maternal toxicity included red lacrimal secretion, discharge of a pigmented secretion from the nose, urine staining of abdominal fur and decreases in weight gain and food consumption during dosing. Neither developmental study showed evidence of treatment-induced malformations (Health Canada, 2010).
Other effects
Reported treatment-related effects including increases in liver and thyroid/parathyroid weights have been observed at 62.5 mg/kg bw per day and greater in dogs, and liver effects were also observed in rats following repeated oral exposure, with non-cholinergic hematological effects being observed at higher dose levels (Shellenberger and Billups, 1987; Daly, 1996; Health Canada, 2010).
Non-neoplastic liver changes were observed in experimental animals but may represent adaptive responses. However, more serious histopathological damage may be observed in the liver with high single doses of malathion (ATSDR, 2003).
There is insufficient evidence to indicate that malathion affects the endocrine system. However, there is some indication that malathion may elicit an immune response in experimental animals by affecting both humoral and cellular immunity based on findings from published studies (Health Canada, 2010).
Genotoxicity and carcinogenicity
Based on an extensive review of available published and unpublished scientific evidence, including proprietary information, the PMRA did not consider malathion to be genotoxic or carcinogenic (Health Canada, 2010, 2012, 2015, 2021a).
Overall, the database for malathion did not indicate that malathion has genotoxic potential based on the weight of evidence. Although some in vitro and in vivo genotoxicity studies reported positive findings in the published literature, the relevance of these findings is unclear since the positive results were typically noted at levels that were cytotoxic. In addition, the identity and/or purity of the test substance was not always stated in the positive genotoxicity studies (Health Canada, 2010, 2021a; WHO, 2017a).
In in vitro studies, malathion was not mutagenic in bacteria (Ames tests using several bacterial strains, with and without metabolic activation) or in yeast (Saccharomyces cerevisiae gene mutation assay) and did not cause unscheduled DNA synthesis (UDS) in cultured rat hepatocytes (U.S. EPA, 1977; Traul, 1987; Pluth et al., 1996; U.S. EPA, 2009; Health Canada, 2010; IARC, 2017; WHO, 2017a). Some in vitro genotoxicity assays (Comet, DNA-protein-crosslinking, sister-chromatid exchange) reported positive results, although only at high malathion doses (that is, cytotoxic doses) or while using a test material of unspecified purity (Chen et al., 1981; Nishio and Uyeki, 1981; Health Canada, 2010; Ojha and Srivastava, 2014; Ojha and Gupta, 2015; IARC, 2017; WHO, 2017a).
In animals in vivo, malathion did not cause mutations in spermatogonia of mice (dominant lethal assay), or chromosomal aberrations in bone marrow of rats (Health Canada, 2010; IARC, 2017; WHO, 2017a). In contrast, other rodent studies detected chromosomal aberrations and DNA damage (as assessed by the Comet assay) following oral administration of malathion at either cytotoxic doses or while using a test material of unspecified identity and/or purity (Dulout et al., 1983; Giri et al., 2002; Health Canada, 2010; Ojha et al., 2013; IARC, 2017).
In human cells, malathion did not cause UDS in lung fibroblasts, but induced mutations in T lymphocytes in the HRPT assay and 8-OH-dG adduct formation in human peripheral blood mononuclear cells (U.S. EPA, 1977; Pluth et al., 1996; Ahmed et al., 2011). Mixed results were reported for sister chromatid exchange and DNA damage (assessed by the Comet assay), with positive findings observed only at near cytotoxic to cytotoxic doses, or with malathion of unspecified purity (Blasiak et al., 1999; Health Canada, 2010; Moore et al., 2010; Olakkaran et al., 2020). Chromosomal aberrations were observed in human peripheral leukocytes, but with test material of unspecified purity (Health Canada, 2010). An increase in micronucleated cells was found in cultured lymphocytes treated with high doses of malathion. However, in vivo studies with agricultural workers exposed specifically to malathion reported negative results for both micronuclei formation and glycophorin A mutations in peripheral lymphocytes of the cohorts examined (Titenko-Holland et al., 1997; Windham et al., 1998).
Overall, the database for malathion did not suggest that malathion has carcinogenic potential for humans based on the weight of evidence (Health Canada, 2010, 2015, 2021a).
In an 18-month study where B6C3F1 mice were fed malathion at 100 to 16,000 ppm, an increased incidence of benign liver tumours (adenomas) was observed in both sexes at 8,000 ppm (1,476 mg/kg bw per day for males, 1,707 mg/kg bw per day for females) and 16,000 ppm (2,978 mg/kg bw per day for males, 3,448 mg/kg bw per day for females) (Slauter, 1994). In another study where F344 rats were given 100 to 12,000 ppm of malathion in the diet for 24 months, an increased incidence of liver adenomas was also noted but only in females at 12,000 ppm (817 mg/kg bw per day) (Daly, 1996). However, the maximum tolerated dose was exceeded at the dose levels at which the liver tumours were observed in the chronic toxicity/carcinogenicity studies by Slauter (1994) and Daly (1996), as demonstrated by increased mortality and decreased body weight gain observed in these dose groups. Further, there was no evidence of progression from non-neoplastic (such as hyperplasia) to neoplastic lesions. All of the identified tumours noted following exposure to malathion were classified as benign and no progression from benign to malignant tumours was observed. No dose-response relationship in tumour incidence was observed at dose levels below those deemed to be excessively toxic. As well, evidence of a decrease in tumour latency was not observed following exposure to malathion. Although liver tumours were reported in mice, the liver is the site of metabolism of malathion and demonstrated signs of metabolic saturation. Furthermore, liver tumours are a common neoplasm in mice. The organophosphates are not, generally speaking, known to be carcinogenic (Health Canada, 2010, 2012, 2021a). In the 24-month rat study, Daly (1996) also reported solitary rare nasal and oral tumours at 6,000 and 12,000 ppm in rats. However, these tumours could not be distinguished as treatment-related or caused by random occurrence (Health Canada, 2010, 2021a). Further evaluations by peer reviewers and some regulatory agencies concluded that the nasal tumours resulted from irritation of the nasal epithelium from either volatilization or inhalation of very high concentrations of malathion from the feed (U.S. EPA, 2000a; Jensen and Whatling, 2010; FAO/WHO, 2016).
Overall, the PMRA did not consider malathion to be genotoxic based on an examination of the full weight of evidence available to the PMRA, including unpublished and proprietary information (Health Canada, 2010, 2021a). Using a risk-based approach, PMRA concluded malathion is unlikely to possess carcinogenic potential for humans (Health Canada, 2010, 2021a). The U.S. EPA has classified malathion as having "suggestive evidence of carcinogenicity but not sufficient to assess human carcinogenic potential", while the European Food Safety Agency did not propose a classification with regard to the carcinogenicity of malathion (FIFRA, 2000; EFSA, 2009; U.S. EPA, 2009). Although IARC classified malathion as "probably carcinogenic to humans" (Group 2A), IARC uses a hazard-based approach which does not take into consideration the levels of human exposure, in contrast to the risk-based approach used by Health Canada (IARC, 2017; Health Canada, 2021a). Pesticides are registered for use in Canada only if risks to human health are acceptable, meaning that the level of exposure to Canadians does not cause any harmful effects, including cancer (Health Canada, 2015; Health Canada, 2021a).
Mode of action
Malathion was found to increase oxidative stress markers and creates an imbalance in antioxidant status in different tissues. This causes tissue injuries, including lipid peroxidation, DNA damage, and/or changes in antioxidant enzyme (Akhgari et al., 2003; IARC, 2017; Akbel et al., 2018; Selmi et al., 2018). This mode of action could explain the nephrotoxicity observed in rats and dogs following malathion exposure that was reported in some studies presented in the section on effects in animals (Akbel et al., 2018; Selmi et al., 2018; Gyuraszova et al., 2019; Obert and Frazier, 2019).
In mammals, malathion undergoes metabolic activation to form malaoxon, a minor metabolite. Malathion and malaoxon both have the ability to inhibit plasma ChE, erythrocyte ChE and brain ChE activity via phosphorylation of the active site of the enzyme, although malaoxon is noted to have a higher potency compared to malathion for ChE inhibition (ATSDR, 2003; Krstic et al., 2008; Health Canada, 2010; Jensen and Whatling, 2010). The ChE enzyme is responsible for the hydrolysis of the neurotransmitter acetylcholine. Therefore, its inhibition causes acetylcholine to accumulate in the synapses, overstimulating the nicotinic and muscarinic receptors in the central and/or peripheral nervous system. This overstimulation leads to smooth muscle contractions (for example, abdominal cramps, glandular secretions, skeletal muscle twitching and paralysis) and possible effects on learning, memory and other behavioural parameters (ATSDR, 2003; Health Canada, 2010; Jokanovic, 2018; Naughton and Terry Jr., 2018).
Selected key study
In its proposed re-evaluation decision for the continuing registration of malathion (PRVD2010-18), Health Canada (2010) identified the kidney as the most sensitive target organ across the database. An increase in severity of chronic progressive nephropathy was observed in rats of both sexes, with the females being affected at a lower dose (32 mg/kg bw per day) than males in a chronic rat bioassay (Daly, 1996). At higher doses, chronic nephropathy has also been observed as early as 90 days in a subchronic rat study (Daly, 1993b). A comparison of the results from subchronic and chronic studies conducted with malathion demonstrates that duration of dosing has an impact on toxicity, with the chronic no-observed-adverse-effect level (NOAEL) for chronic nephropathy in the Daly study (1996) being 14-fold lower than that derived in a subchronic bioassay using the same strain of rats (Health Canada, 2010). Therefore, the chronic oral toxicity/carcinogenicity study in rats conducted by Daly (1996) was identified as the key study for the human health risk assessment of malathion in drinking water (Health Canada, 2010, 2019a, 2021a).
In the Daly (1996) study, groups of rats (90/sex/dose) were fed a diet of 0, 100/50 (reduced day 113), 500, 6,000 or 12,000 ppm (equivalent to 0, 2.4, 26, 327 or 677 mg/kg/bw per day for males and 0, 3.0, 32, 386 or 817 mg/kg bw per day for females) of malathion (97.1%) for 24 months (Health Canada, 2010). After 3 months, the lowest dose was reduced from 100 ppm to 50 ppm due to the observation of statistically significant erythrocyte ChE inhibition at 100 ppm in females (U.S. EPA, 1997; Health Canada, 2010; WHO, 2017a). Rats were checked twice a day for toxicity and mortality and examinations were performed each week. Interim sacrifices took place after 3, 6 and 12 months (U.S. EPA, 1997) Treatment-related clinical signs (that is, anogenital staining) were observed only in females at the highest dietary dose (U.S. EPA, 1997; Health Canada, 2010). Mortality was significantly increased in males at 6,000 and 12,000 ppm (327 and 677 mg/kg bw per day) (starting at month 20 and 14, respectively) and in females at 12,000 ppm (817 mg/kg bw per day) (closer to study completion), with deaths attributed in part to chronic nephropathy (U.S. EPA, 1997; Health Canada, 2010; WHO, 2017a). Although a high incidence of chronic nephropathy was reported across all groups (including controls), a treatment-related increase in severity of the effect was observed in females exposed to ≥ 500 ppm (≥ 32 mg/kg bw per day) and males exposed to ≥ 6,000 ppm (≥ 327 mg/kg bw per day), with males also demonstrating an earlier onset of the disease at interim sacrifice (U.S. EPA, 1997; Health Canada, 2010). Decreased body weights and increased food consumption was recorded for both sexes at ≥ 6,000 ppm (≥ 327/386 mg/kg bw per day in males/females), along with increased absolute and relative liver weights and kidney weights. Lesions of the nasal mucosa (degeneration and hyperplasia of the olfactory epithelium), nasopharynx irritation (inflammation and hyperplasia of the respiratory epithelium) were reported in both sexes at ≥ 6,000 ppm (≥ 327/386 mg/kg bw per day in males/females).
Solitary oral and nasal tumours were also observed in both sexes; however, they could not be distinguished as either treatment-related or of random occurrence (oral tumours in females at ≥ 6,000 ppm [≥ 386 mg/kg bw per day]; nasal tumours in females at ≥ 6 000 ppm and in males at 12,000 ppm [≥ 386 and 677 mg/kg bw per day, respectively]). An increase in the incidence of liver adenomas was noted in females at 12,000 ppm (817 mg/kg bw per day), but not in males (Health Canada, 2010).
In both sexes, erythrocyte ChE and brain ChE inhibition was noted at ≥ 6,000 ppm (≥ 327/386 mg/kg bw per day in males/females), while plasma ChE inhibition was noted at ≥ 500 ppm (≥ 26/32 mg/kg bw per day in males/females). Effects on erythrocyte and clinical chemistry parameters were observed in males and females exposed to the 2 highest doses.
An oral NOAEL of 3.0 mg/kg bw per day was identified based on a treatment-related increase in severity of chronic progressive nephropathy in female rats at the next dosage level of 32 mg/kg bw per day.
Although ChE inhibition was also a target of malathion toxicity, it was not the most sensitive endpoint of chronic toxicity. Across the database, dose-related inhibition of plasma, erythrocyte and brain ChE activity occurred by all routes and durations of exposure to malathion in repeat dose animal studies, including the key study. As explained in the section on effects in animals, depression of plasma ChE activity is not a toxicologically adverse effect but serves as a marker of exposure to malathion. Depression of erythrocyte ChE activity in acute and short-term toxicology studies can be viewed as a surrogate for adverse peripheral neurotoxic effects. However, in studies of longer duration, depression of erythrocyte ChE is not considered informative due to limitations related to the low rate of re-synthesis of erythrocyte ChE over extended periods of time. Only brain ChE inhibition is considered adverse following longer-term exposures and occurred at higher dose levels of malathion (typically ≥ 150 mg/kg bw per day, observed at 327/386 mg/kg bw per day in males/females in Daly (1996)) than those causing nephrotoxicity. As such, the NOAEL of 3.0 mg/kg bw per day based on a treatment-related increase in severity of chronic progressive nephropathy in female rats is considered protective of effects on ChE activity (Health Canada, 2021a).
While sensitivity of the young has been demonstrated, the most sensitive endpoint following repeat exposure (behavioural effects) to young animals occurs at doses exceeding the NOAEL for chronic nephropathy. Chronic nephropathy is a disease related to aging and has been observed following long-term exposure in adult rats (Health Canada, 2010).
Derivation of the health-based value
As noted above, the NOAEL of 3.0 mg/kg bw per day for increase in severity of chronic progressive nephropathy in female rats was selected as the basis for the current risk assessment. Using the NOAEL of 3.0 mg/kg bw per day, the acceptable daily intake (ADI) for malathion (Health Canada, 2010) is calculated as follows:
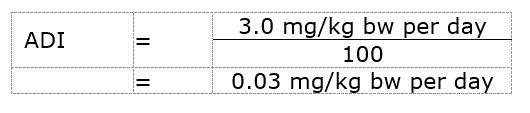
Figure - Text description
The ADI for malathion is 0.03 mg/kg bw per day. This is calculated by dividing the NOAEL of 3.0 mg/kg bw per day by the uncertainty factor of 100.
where:
- mg/kg bw per day is the NOAEL based on chronic progressive nephropathy in female rats (Health Canada, 2010) and
- 100 is the uncertainty factor, selected to account for interspecies variation (×10) and intraspecies variation (×10)
Based on the ADI of 0.03 mg/kg bw per day, a health-based value (HBV) for malathion in drinking water was derived as follows:

Figure - Text description
The HBV for malathion in drinking water is 0.29 mg/L. This is calculated by multiplying the ADI for malathion (0.03 mg/kg bw per day) by the average body weight for an adult (74 kg) by the allocation factor for water (0.20). The result is divided by the daily volume of water consumed by an adult (1.53 L/day).
where:
- 0.03 mg/kg bw per day is the ADI calculated using a NOAEL of 3.0 mg/kg bw per day (Health Canada, 2010)
- 74 kg is the adult body weight (Health Canada, 2021b)
- 1.53 L per day is the daily volume of tap water consumed by an adult (Health Canada, 2021b) and
- 0.20 is the default allocation factor since drinking water is not a major source of exposure to malathion and there is evidence of malathion in other exposure sources (for instance, low levels in food) (Krishnan and Carrier, 2013)
PMRA's use of a TAF in its risk assessment was considered a conservative approach required in the regulatory assessment to account for potential residues of malaoxon that may be present below the limit of detection. This document does not support using an additive approach (that is, use of a TAF) for malathion and malaoxon in drinking water based on their environmental fate and available water monitoring data. Malathion can inhibit ChE but at higher doses than those causing nephrotoxicity. Although malaoxon is a more potent ChE inhibitor than malathion, malaoxon is expected to be present at negligible levels in raw and treated water in Canada.
Malaoxon is not a major transformation product of malathion in the environment. Both malathion and malaoxon are non-persistent in the environment and unlikely to leach into groundwater. As demonstrated by the extensive U.S. water monitoring data presented in the section on exposure, malaoxon levels in groundwater and surface water were negligible. Although the conversion of malathion to malaoxon can also occur during oxidation or advanced oxidation processes during water treatment, given the low levels of exposure to malathion observed in Canadian drinking water sources (as presented in Table 3), any formation of malaoxon during water treatment is expected to be negligible.