Summary of the Report of the CF Expert Panel on Suicide Prevention
Suicide is an important public health problem in industrialized nations. It is the second leading cause of death in the demographic group that makes up the bulk of military organizations, namely young and middle-aged men. Hence, it is an important contributor to premature mortality in the armed forces. Suicide rates tend to be somewhat lower in service members relative to the general population: In the Canadian Forces, the suicide rate for Regular Force males 1 is approximately 20% lower than those of the general population of the same age. Those who have (or who develop) the serious mental disorders that present the greatest risk for suicide 2 are excluded from the military, so this lower suicide rate is not surprising. Nevertheless, suicide remains an important public health threat in the military. For this reason alone, military organizations need to take an active interest in suicide prevention.
Public interest in military suicides has been particularly acute over the past year or two, coincident with a rise in the suicide rates seen in the US Army and Marine Corps. Other militaries coping with the extraordinary demands of the conflicts in SW Asia are concerned that they, too, will see such increases in time. In the CF, however, the suicide rate has remained steady since the beginning of the mission in Afghanistan, and previous deployment does not appear to be associated with a significantly increased risk of suicide. Nevertheless, the public, Members of Parliament, and military leaders often ask what the CF is doing in terms of suicide prevention.
Public interest notwithstanding, suicide in the military does have special significance. Mental health problems are important precursors to suicide, and certain types of military work (notably exposure to operational stressors such as combat) can trigger mental health problems. More importantly, military organizations have control over a broader range of potential targets for suicide prevention than does a civilian employer. For example, the military generally delivers its own mental health care, with such care being a central tool in suicide prevention.
It is against this backdrop that the CF Surgeon General convened the CF Expert Panel on Suicide Prevention in September 2009. Over two days, CF and external experts reviewed and evaluated the CF’s suicide prevention activities.
Targets for Suicide Prevention in the CF: The Panel began by reviewing a familiar model of targets for suicide prevention in civilians. This model included the following elements:
- Education and awareness programs;
- Screening and assessment;
- Pharmacotherapy;
- Psychotherapy;
- Follow-up care for suicide attempters and high-risk patients;
- Restriction of access to lethal means; and
- Media engagement (to encourage responsible reporting of suicides).
The Panel then extended this model by adding additional prevention targets in military organizations, including:
- Organizational interventions intended to mitigate work stress/strain (leadership training, policy, programs, etc.);
- Selection, resilience training, and primary risk factor modification;
- Interventions to overcome barriers to mental health care; and
- Systematic efforts to improve the quality of mental health care.
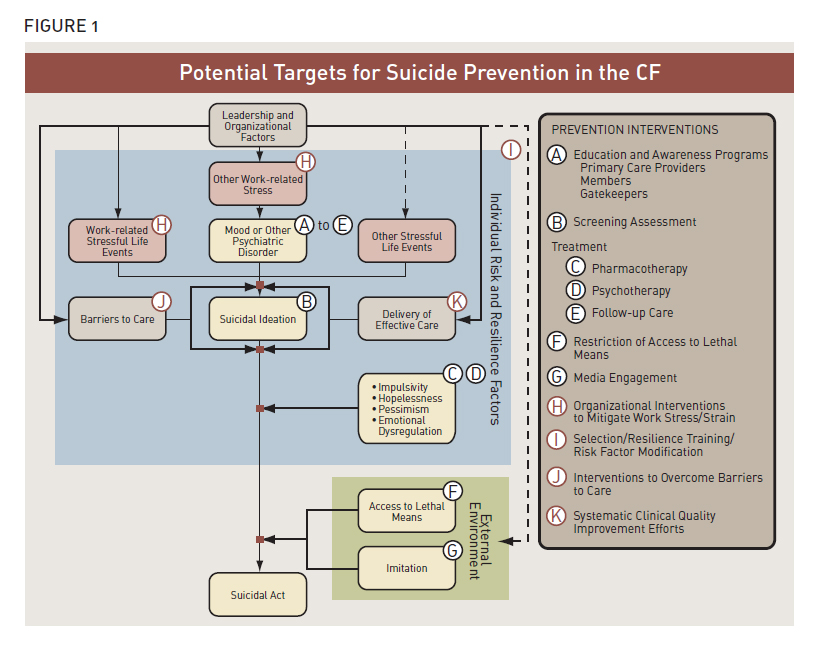
Figure 1: Potential Targets for Suicide Prevention in the CF
Figure 1: Potential Targets for Suicide Prevention in the CF (Text equivalent)
Prevention Interventions
- Education and Awareness Campaigns
- Primary Care Providers
- Members
- Gatekeepers
- Screening Assessment
- (Treatment) Pharmacology
- (Treatment) Psychotherapy
- (Treatment) Follow-up Care
- Restriction of Access to Lethal Means
- Media Engagement
- Organizational Interventions to Mitigate Work Stress/Strain
- Selection / Resilience Training / Risk Factor Modification
- Interventions to Overcome Barriers to Care
- Systematic Clinical Quality Improvement Efforts
Potential Targets for Suicide Prevention in the CF
- Leadership and Organizational Factors
- Individual Risk and Resilience Factors (I)
- Work-related Stressful Life Events (H)
- Other Stressful Life Events
- Other Work-related Stress (H)
- Mood or Other Psychiatric Disorder (A)
- Barriers to Care (J)
- Delivery of Effective Care (K)
- Suicidal Ideation (B)
- Impulsivity (C,D)
- Hopelessness (C,D)
- Pessimism (C,D)
- Emotional Dysregulation (C,D)
- External Environment
- Access to Lethal Means (F)
- Imitation (G)
- Suicidal Act
The Panel accepted that suicide prevention research poses formidable methodological challenges. Truly bias-free studies are close to impossible, and those inclined to doubt will find limitations in any given study. The Panel dealt with this challenge by trying to look at the strength of the literature as a whole instead of focusing on the limitations of any particular study. 3
The Panel also took the unusual stance of endorsing activities as suicide prevention initiatives even in the absence of firm evidence that they prevent suicide. However, this was only done when there was ahighly plausible link to suicide prevention, 4 when the intervention offered other clear benefits to theorganization, and when the potential for harm appeared low.
The Panel’s key findings and recommendations 5 for each of these targets are as follows:
A. Education and awareness programs: Suicide awareness training is what most people think of when they think of suicide prevention. While there is no evidence that it is beneficial as an isolated intervention, the multi-faceted, community-based prevention programs with the strongest evidence of efficacy have included an element of mass education.
In the past, the CF’s mental health and suicide education program had been fragmented and inconsistent. Recently, however, the CF has stood up a Mental Health Education Advisory Committee, and it has expanded its Joint Speakers Bureau as its preferred delivery mechanism. The strategic vision is for members to receive a comprehensive and coherent mental health education and training program across their career and deployment cycle. The Panel recommended that these mechanisms be used to integrate suicide prevention training into the rest of mental health education.
B. Screening and assessment: The CF already screens for suicidal thoughts during its regular Periodic Health Assessments and its pre- and post-deployment screenings. The Panel did not recommend any additional screening for suicidal thoughts. However, the Panel did recommend that the CF consider additional screening for depression in primary care, given evidence that this can contribute to better mental health outcomes. The Panel recommended that the CF follow conventional guidelines for the assessment of suicidal risk in patients with symptoms of mental health problems.
C. Pharmacotherapy: The Panel noted that CF Regular Force members have access to any needed psychiatric medications at no cost. This represents much better access than the average Canadian enjoys. 6 The Panel found that the balance of evidence showed that antidepressants lower suicidal risk. The Panel recommended that the CF follow conventional guidelines for drug treatment of individuals with mental disorders and for suicidal patients in particular.
D. Psychotherapy: CF Regular Force members also have ready access to psychotherapy at no cost. Again, this is far better access than the typical Canadian enjoys. 7 Expansion of the CF’s mental health staff will shortly result in Regular Force members having approximately twice as many mental health providers per capita relative to Canadian civilians. Access to psychotherapy is important because optimal treatment for the common mental disorders that drive suicidal behaviour should include some evidence-based psychotherapy. The Panel recommended that the CF follow conventional guidelines for psychotherapy of individuals with mental disorders. It also recommended that suicidality be specifically targeted with evidence-based psychotherapies, citing evidence that this decreases the risk of suicidal behaviour.
E. Systematic follow-up for high-risk patients: The Panel found some evidence that systematic efforts to assure follow-up of high-risk patients decreased the risk of suicidal behaviours. Moreover, such efforts lead to other favourable outcomes, particularly for depressed patients in primary care settings. Each CF clinic currently has its own approach to ensuring follow-up, but the Panel recommended that the CF consider standardizing this essential process nationwide. The Panel also recommended that the CF consider implementing the US Army’s RESPECT-Mil program for primary care management of depression and PTSD, based on strong evidence of the value of this approach.
CF members receive inpatient psychiatric care through civilian institutions. Limitations in inpatient bed capacity mean that members at significantly increased suicide risk 8 will need to be managed as outpatients. Military environments offer both additional constraints (e.g., less privacy) and additional opportunities (e.g., engagement of the unit leader) relative to the typical community setting. High-risk patients are sometimes managed in their units, watched over by their co-workers (sometimes termed a “buddy watch”). The Panel found this practice to be well-intentioned but problematic, noting the enormous breach of patient confidentiality that it requires. Hence, the Panel recommended that the CF develop best practices for outpatient management of high-risk patients, making it clear that a unit “buddy watch” should be used only as a last resort.
F. Restriction of access to lethal means: The Panel found good evidence that restriction of access to lethal means (e.g., firearms, certain medications) can decrease the risk of suicide. However, additional opportunities for means reduction in the CF appear limited because the means of member suicides are often procured from outside the CF. The Panel did recommend that the CF’s suicide surveillance system better capture information on the means of suicide to identify potential means reduction opportunities. The Panel also recommended that the CF evaluate means reduction through changes in the packaging and dispensing of medications commonly used in suicide (e.g., over-the-counter pain relievers). The Panel also emphasized that means restriction should be part of the management plan for individual high-risk patients managed as outpatients.
G. Media engagement: The Panel identified some evidence that media reporting of suicides can serve as a suicide trigger for suicide-prone individuals. The challenge for the CF is that member suicides are sometimes judged to be newsworthy, particularly when there is a perceived connection to a deployment. The Panel recommended that the CF attempt to engage the media to encourage them to follow conventional guidelines on the reporting of suicide in the media, such as those promulgated by the US Centers for Disease Control.
H. Organizational interventions intended to mitigate work stress/strain (leadership training, programs, policies,etc.): Work stress is a risk factor for mental health problems, and it is a common contributor to suicidal behaviour. The CF has implemented a broad range of organizational policies and programs to mitigate work stress. Examples include the PERSTEMPO policy, the Screening and Reintegration Policy, and the Alternative Dispute Resolution Program. Effective leadership mitigates work stress and hence may have suicide preventive effects.
Failed intimate relationships are a common trigger for suicidal behaviour. The Panel noted that the CF has developed a number of family-friendly policies and programs that are designed to strengthen intimate relationships, potentially mitigating suicide risk. Given that supervisors and others in the unit are likely to know about failed relationships, the Panel identified this as a potential point of intervention for suicide prevention.
Disciplinary action and/or legal problems are another common factor in military suicides, so these again represent another potential point for intervention. The Panel recommended that leader education provide guidance on managing the disciplinary process in ways that mitigate suicide risk. The Panel also recommended that the CF evaluate the US Air Force’s “hands-off” policy for members under investigation. This policy requires that members be “handed off” 9 to their leadership immediately after any investigative interview. Leaders then assess how the member is coping and refer for evaluation or care as needed.
I. Selection, resilience training, and primary risk factor reduction: At recruitment, the CF already screens out those with the most serious mental illnesses, which bring with them a high risk of suicide. Additional screening for those with a history of more minor psychopathology or those who merely have risk factors for these in the future is appealing in principle but unreliable in practice.
The CF is integrating some of the most promising resilience training approaches into its mental health education program. In theory, such training could mitigate suicide risk, but other demonstrated benefits 10 would need to sustain these programs.
The CF also offers evidence-based primary risk factor reduction through its “Strengthening the Forces” health promotion program. These programs target risk factors such as alcohol use disorders, relationship conflict, psychological stress, and anger. The programs may plausibly attenuate suicide risk through risk factor modification.
J. Systematic efforts to overcome barriers to mental health care: Nearly all suicidal individuals have mental health problems, but more than half are not in care at the time they commit suicide. The CF has invested heavily in efforts to overcome the barriers to mental health care over the past 5 to 10 years. These efforts have included:
- Strengthening confidentiality and career protection for members seeking care for mental health or substance abuse problems;
- The development of the innovative Operational Stress Injury Social Support (OSISS) peer support program;
- Dramatically expanding the number of CF mental health professionals;
- Offering up to 10 sessions of free, confidential counselling to CF members or their families through non-CF civilian providers; 11 and
- Reinforcing screening for mental health problems during the regular Periodic Health Assessment and routine pre- and post-deployment screening.
The Panel reviewed evidence that these initiatives are paying off, and it noted that the CF has a robust surveillance system for monitoring barriers to mental health care in garrison using its periodic Health and Lifestyle Information Survey. The Panel supported carrying out a planned in-theatre mental health needs assessment to identify the needs and barriers to care in deployed settings.
K. Systematic efforts to improve the quality of mental health care: Conventional suicide prevention models focus on finding ways to identify suicidal individuals and get them into care, with the assumption being that once there, they will receive optimal treatment. Data from elsewhere shows that this is not a safe assumption: Studies have repeatedly shown that the quality of mental health care that actually gets delivered usually falls short of what experts consider optimal care. Care received by suicide victims tends to be especially inadequate.
The CF’s well-resourced mental health system has eliminated nearly all of the structural problems that plague the delivery of mental health care in civilian settings, so it should be performing better. However, hard data on the quality of care in the CF is lacking: Without such data, systematic efforts to enhance the quality of care are impossible. For this reason, the Panel’s most pivotal recommendation is that the CF take steps to reinforce its infrastructure for quality improvement in mental health care. Each suicide offers the tragic potential to provide valuable lessons for suicide prevention, much as airplane crash investigations help prevent future crashes. Current CF policy requires a Board of Inquiry (BOI) for every CF suicide, but the Panel concluded that the BOI process was a weak and inefficient tool for clinical quality assurance. For this reason, it recommended that the CF do a rapid, standardized health care quality assurance investigation after each suicide.
Conclusions: When broadly framed as above, the CF already has a strong suicide prevention program that compares favourably to those of its closest allies. In particular, it includes almost all of the elements of the US Air Force’s benchmark suicide prevention program (ANNEX B), for which the strongest and most relevant evidence of efficacy exists. It has also implemented (or is in the process of implementing) nearly all of the suicide prevention strategies most consistently identified in the civilian scientific literature. Finally, its approach targets additional factors that are more specific to military organizations.
Nevertheless, the Panel did identify some opportunities for reinforcing the CF’s program, most notably the need to improve its ability to systematically improve the quality of mental health care that it delivers. Given the strength of the CF’s existing program, the Panel’s recommendations represent additional prevention opportunities to exploit as opposed to serious deficiencies to correct.
The Panel emphasized that the responsibility for suicide prevention in the CF needs to be shared among leaders, clinicians, and the rank-and-file. The leader and clinician responsibilities are laid out above. Members need to do what they can to recognize the need for care in others and to help them get into care. Moreover, members have a responsibility to do their best to recognize their own need for care, to actively engage in such care, and to comply with recommended treatment. However, the Panel recognized that mental disorders perversely rob people of the insight, hope, and trust that are needed in order to engage in care. For this reason, the CF’s suicide prevention approach can be framed as an attempt to set up circumstances that favour this essential engagement in care.
Suicide prevention has a strong, intuitive appeal. To the grieving friend or family member, their loved one’s suicide likely appears preventable, particularly when the victim is receiving mental health care. In practice, though, most suicides are not preventable: Quality assurance audits in mental health settings suggest that even for those already in care, only about a quarter of suicides are judged to be preventable.
The Panel identified a number of factors that contribute to the incomplete preventability of suicide, including intrinsic technological limitations in mental health care, the complexities of providing mental health care, the broad range of contributors to suicidal behaviour, and important scientific uncertainties as to how best to treat mental disorders and prevent suicides. While mental health treatments are better than ever, mental illnesses are powerful disorders: Even the best equipped clinicians cannot pry every patient from their grasp.
Thus, the Panel emphasized the need to have reasonable expectations of the CF’s suicide prevention program. Many of the most effective interventions are already in place, so future gains are likely to be modest. For this reason, the Panel felt that the ancillary benefits of the CF’s suicide prevention program (e.g., quality improvement in mental health care) will overshadow its impact on suicide rates.
1 There are so few suicides in women in the CF that is not appropriate to calculate and report their suicide rates.
2 Namely, bipolar (manic-depressive) disorder and psychotic disorders such as schizophrenia.
3 For example, while each study addressing the effectiveness of restriction of access of lethal means had at least some sources of uncontrollable bias, the literature as a whole consistently shows that means reduction can decrease the risk of suicide.
4 For example, the Panel looked for evidence showing that the intervention significantly attenuates an important mediator of suicide, such as depression.
5 All recommendations are summarized in ANNEX A.
6 Coverage for psychiatric medications is uneven for the provincial health plans in Canada. Many individuals have private insurance coverage for medications, but these often have deductibles, co-insurance, or coverage limits.
7 Insurance coverage for psychotherapy is also uneven for most Canadians.
8 For example, those recently discharged from an inpatient facility after a serious suicide attempt.
9 The US Air Force’s choice of ambiguous terminology here is unfortunate: “Hands-off” in this context refers to the transfer of responsibility for the member’s safety from the investigator to the member’s chain of command rather than a “hands-off” approach of non-intervention. Quite to the contrary, the whole point is the active involvement by the chain of command in assuring the member’s safety and wellbeing.
10 Specifically, improvements in performance or wellbeing in response to adversity
11 Access is managed through the Canadian Forces Member Assistance Program (CFMAP).