Surgeon General's Mental Health Strategy: CAF Mental Health Programs and Services
The CAF was sensitized to the psychological impact of operations as members returned from missions such as those in the former Yugoslavia, Somalia, Rwanda and Afghanistan. While the CAF is now internationally recognized for its operational excellence, the cost has included an increased prevalence of chronic psychological injuries that has required a strong commitment from the CAF to manage.
The CF H Svcs Gp has been in a constant state of evolutionary and revolutionary change, starting with the major resource reductions of Operation PHOENIX in the mid-90s, followed by the reform and reinvestment of the Rx2000 project, and finally, the many new initiatives and resources since the beginning of combat operations in Afghanistan in 2006. All changes were directed by CAF leadership and the final result is our current health system, which delivers a relatively outstanding standard of comprehensive, high-quality care.
In the CAF Ombudsman’s 2012 review entitled Fortitude Under Fatigue: Assessing the Delivery of Care for Operational Stress Injuries that Canadian Forces Members Need and Deserve, Mr. Pierre Daigle commends the CAF for significant improvements over the past decade, and is quoted as saying “I was pleased to see that care and treatment for Canadian Armed Forces members suffering from an operational stress injury has improved since 2008 and is far superior to that which existed in 2002.
”
The Rx2000 reform provided the foundation for our current system. It arose from the 1999 Chief Review Services’ evaluation of the CF Medical Services which noted significant concerns in many areas of health services, and was informed by findings from the Croatia Board of Inquiry, the Lowell Thomas Report, and the McLellan Report on Care of the Injured. The CAF mental health system was further enhanced since 2006 by such measures as the expert panels on mental health-related issues, the Road to Mental Readiness (R2MR) program, expanded mental health research efforts, telemental health, virtual reality exposure capabilities, and others.
The CF H Svcs Gp now has a comprehensive mental health system that consists of strategic, operational and tactical programs and services. The Directorate of Mental Health provides national coordination, strategic assessment and oversight whereas operational delivery of clinical services is carried out through 1 and 4 Health Services Groups. Our mental health system is based on high-quality health surveillance and research to better understand the risks and needs of our population, understand how to improve its health, and improve treatment of illness. We focus on prevention through education and strive to deliver the best possible care. These programs and services essentially cover three components:
- UNDERSTAND: Health surveillance and mental health research
- EDUCATE: Mental health education and training
- CARE: Clinical programs and services
CAF Mental Health Programs and Services - A Historical Perspective
- 2013-2014
-
- Mental Health Survey (Statistics Canada) on the prevalence of mental illness in the CAF
- CF H Svcs Gp - Health and Lifestyle Information Survey of Canadian Forces personnel
- CF H Svcs Gp - OSI ccupational Outcomes Study
- CF H Svcs Gp - mTBI Outcomes Study
- 2012
-
- CF H Svcs Gp - CF Expert Panel on Family Violence
- Mental Health Commission of Canada – Changing Directions, Changing Lives: The Mental Health Strategy for Canada
- Office of the Auditor General Report to the House of Commons – (Chapter 4) Transition of Ill and Injured Military Personnel to Civilian Life
- Ombudsman Report – Reserved Care: A Follow Up into the Treatment of Injured Reservists
- Ombudsman Report – Fortitude Under Fatigue: Assessing the Delivery of Care for Operational Stress Injuries that CF Members Need and Deserve
- Increase of $11.4 M in mental health funding
- 2011
-
- CF H Svcs Gp - OSI Incidence Study
- 2010
-
- Haiti Operations
- Surgeon General's Health Research Strategy
- CF H Svcs Gp - CF Expert Panel on Suicide Prevention
- 2009
-
- CF Mental Health Care Initiative finalized
- 2008
-
- Ombudsman Special Report – Reserved Care: An Investigation into the Treatment of Injured Reservists
- Ombudsman Report – A Long Road to Recovery: Battling Operational Stress Injuries
- CF H Svcs Gp – CF Expert Panel on Mild Traumatic Brain Injury
- CF H Svcs Gp – Health and Lifestyle Information Survey of Canadian Forces personnel
- 2007
-
- Office of the Auditor General Report to the House of Commons - Military Health Care
- Road to Mental Readiness Program was initiated
- 2006
-
- Standing Senate Committee on Social Affairs, Science and Technology - Out of the Shadows at Last: Transforming Mental Health, Mental Illness and Addiction Services in Canada
- 2004
-
- Ombudsman Report - An Analysis of the CF Experience with Third Level Decompression After Deployment
- Bosnia Deployment
- CF Health Services - Health and Lifestyle Information Survey of Canadian Forces personnel
- 2003
-
- Rx2000 CF Mental Health Care Initiative began
- 2002
-
- Enhanced Post-Deployment Screening Program was put in place
- Mental Health Survey (Statistics Canada) on the prevalence of mental illness in the CAF
- Ombudsman Review of DND/CF Actions on Operational Stress Injuries
- Ombudsman Special Report: Systemic Treatment of CF Members with PTSD
- 2001-2013
-
- Afghanistan Operations
- 2001
-
- OSI Social Support (OSISS) - a peer support network was established
- 2000
-
- CF Health Services - Health and Lifestyle Information Survey of Canadian Forces personnel
- 1999
-
- Chief Review Services - Review of CF Medical Services
- Kosovo Operations
- 1995
-
- Op PHOENIX (a rationalization of CF H Svcs)
- Former Yugoslavia (Bosnia Croatia) Operations
- 1992-1993
-
- Rwanda Operations
- Somalia Operations
- 1990
-
- First Gulf War Operations

Understand
Clinical Research
There are many existing mental health treatments but some are limited in efficacy. The mental health challenges affecting our unique military population require that we maintain close health surveillance and remain on the leading edge of research in order to safely and scientifically integrate new therapies into our existing mental health programs. Along with our allies, we continue to contribute to the scientific literature and conduct research on a number of critical topics, including:
- reducing self-termination of care and increasing tolerance to therapies
- expanding understanding of the psychological underpinnings of PTSD
- identifying potential biological markers for PTSD
- exploring novel therapeutic modalities and their applicability to our unique population, such as:
- virtual reality-based exposure therapy
- transcranial magnetic stimulation
- neuro-feedback
- validating our multidisciplinary approach to PTSD treatment
Population-based Mental Health Surveillance, Research and Analysis
Ongoing, detailed information on the incidence, prevalence and impact of mental health problems is essential to guide all facets of the CF H Svcs Gp mental health system. This information directs research, assists with resource allocation and contributes to the evaluation of mental health programs and services.
As with all health research, the mental health research program is a component of the Surgeon General’s Health Research Program. All research related to mental health is reviewed by the Director of Mental Health (DMH) prior to approval by the Surgeon General. The Surgeon General’s Health Research Board’s mandate is to identify critical science and technology requirements in order to engage individuals and organizations in research, technology analysis and development, engineering, and evaluation solutions.
The committed group of DMH research professionals works on behalf of the CAF to prioritize and conduct essential mental health research with the support of the Directorate of Force Health Protection. The CF H Svcs Gp also relies on close collaboration with Defence Research and Development Canada (DRDC), the Canadian Institute for Military and Veteran Health Research (CIMVHR) and its university network members, and our military allies.
Examples of current research:
- 2013 CAF Cross-sectional Mental Health Survey: This survey of approximately 9,000 Regular Force and Reserve Force personnel is conducted by Statistics Canada, focusing on the mental health impact of the Afghanistan mission and the performance of the CAF mental health system.
- OSI Incidence and Outcomes Study: This study looks at OSI diagnoses and occupational outcomes in a random sample of those deployed in support of the mission in Afghanistan from 2001 to 2008.
- Group Randomized Trial of ROAD TO MENTAL READINESS (R2MR) in CAF Recruits: This study randomizes over 1,000 CAF recruits to receive R2MR training or a control intervention. It will evaluate the effect of R2MR on well-being, stress, strain, and attitudes towards mental health care.

Medical Professional Technical Suicide Reviews
Although mental health care audits show that most suicides are not preventable, the loss of any member of the CAF is tragic, and losing someone to suicide is difficult for everyone. As with any loss of life, it is imperative that we learn from these events and do everything possible to prevent them. That is why since 2010, the Chief of Defence Staff (CDS) has directed the conduct of a medical review after every suicide to ensure that any indicated improvements are initiated rapidly to optimize prevention. Conducted by both a medical officer and a mental health specialist, these reviews are initiated within one week of a death being verified as a suicide, and recommendations must be presented to the Surgeon General within 30 days thereafter. The report is also made available to assist the conduct of suicide-related Boards of Inquiry.
During 2011 and 2012, the CF H Svcs Gp completed a Medical Professional Technical Suicide Review (MPTSR) on 90 percent of completed suicides, resulting in over 100 recommendations grouped into four key areas: Clinical Care, Policy, Education and Leadership. These were reviewed and have already helped improve the CAF suicide prevention program and health care system.

Educate
The Road to Mental Readiness
The Road to Mental Readiness (R2MR) is an evidence-based mental health training and education program developed by CF H Svcs Gp to increase mental health literacy and enhance resilience. R2MR is based on the principles of sports psychology and is designed to demystify mental illness, provide individuals with tools for dealing with stressful situations and reduce the risk of developing mental illness. It was introduced in 2007 and has since evolved into a robust program that uses the Mental Health Continuum Model as a foundation for improving CAF members’ understanding of mental health and mental illness. It provides a context for the common and reversible distress that many personnel experience during their careers. The mental health continuum was adopted from the United States Marine Corps and adapted for use in the CAF. Although there are clear diagnostic criteria for mental illness, there is also a continuum that exists between the state of good mental health and a diagnosed mental illness. It has proven to be an excellent tool to understand varying levels of mental health and how people transition from healthy to ill.
This continuum illustrates changes in mood, sense of humour, sleep, energy level and social interaction to indicate where people are in the continuum of mental health. Everyone would ideally be in the green zone but normal stressors can move people into the yellow or orange zone. The R2MR program teaches people how to best manage these normal changes and to recognize when they need help.
| Healthy (green) |
Reacting (yellow) |
Injured (orange) |
Ill (red) |
|---|---|---|---|
| Normal mood fluctuations. Calm and takes things in stride. |
Irritable / impatient. Nervous. Sadness / overwhelmed. |
Anger. Anxiety. Pervasively sad/hopeless. |
Angry outbursts / aggression. Excessive anxiety / panic attacks. Depressed / suicidal thoughts. |
| Good sense of humour. Performing well. In control mentally. |
Displaced sarcasm. Procrastination. Forgetfulness. |
Negative attitude. Poor performance / workaholic. Poor concentration / decisions. |
Overt insubordination. Can't perform duties, control behaviour or concentrate. |
| Normal sleep patterns. Few sleep difficulties. |
Trouble sleeping. Intrusive thoughts. Nightmares. |
Restless disturbed sleep. Recurrent images / nightmares. |
Can't fall asleep or stay asleep. Sleeping too much or too little. |
| Physically well. Good energy level. |
Muscle tension / headaches. Low energy. |
Increased aches and pains. Increased fatique. |
Physical illnesses. Constant fatique. |
| Physically and socially active. |
Decreased activity / socializing. | Avoidance. Withdrawal. |
Not going out or answering the phone. |
| No/limited alcohol use/gambling | Regular but controlled alcohol use/gambling to cope. | Increased alcohol use/gambling - hard to control negative consequences. | Frequent alcohol or gambling use - inability to control with severe consequences. |
*The MHCM provides a guideline to identify signs that may indicate further assessment from a qualified medical / mental health professional is required.
R2MR encompasses the entire package of resilience and mental health training that is embedded throughout CAF members’ careers, including the deployment cycle. It is designed to ensure that the most appropriate training is provided to prepare CAF members mentally for the challenges they may encounter. All CAF personnel are now provided mental health education during Basic Training, throughout leadership courses as they progress during their careers, and at key points before and after they deploy on military operations. The R2MR model provides insight into the varying levels of mental health issues and offers guidance on the appropriate support depending on the severity of the condition.
The goal of R2MR training is to improve well-being and short-term performance, while mitigating any negative long-term mental health problems for both CAF personnel and their families. This is accomplished by teaching early identification of signs and symptoms of mental illness; the importance of peer and leadership support; appropriate leader actions; barriers to seeking mental health care (including stigma); and available mental health resources. Resilience skills, including tactical breathing, mental rehearsal, goal-setting, and self-talk, are also taught, mentored and cued to improve the ability of CAF members and their families to manage both operational and non-operational stresses.
The CF H Svcs Gp’s Directorate of Force Health Protection also provides the Strengthening the Forces health promotion program. This important program provides awareness and prevention education and skill development in areas such as suicide intervention, anger and stress management, healthy relationships, family violence, and addictions.
The education of CAF personnel and their families is not the sole responsibility of the CF H Svcs Gp and must therefore be well coordinated among all relevant CAF elements. R2MR is the foundational mental health education program, but harmonization and coordination of all mental health education and training is conducted by the Mental Health Education Advisory Committee, which is chaired by the Director of Mental Health. Members include representatives from all environments and training centres, the Chaplain branch, the Directorate of Military Family Services, the Directorate of Military Personnel Operational Research and Analysis, and Defence Research and Development Canada.
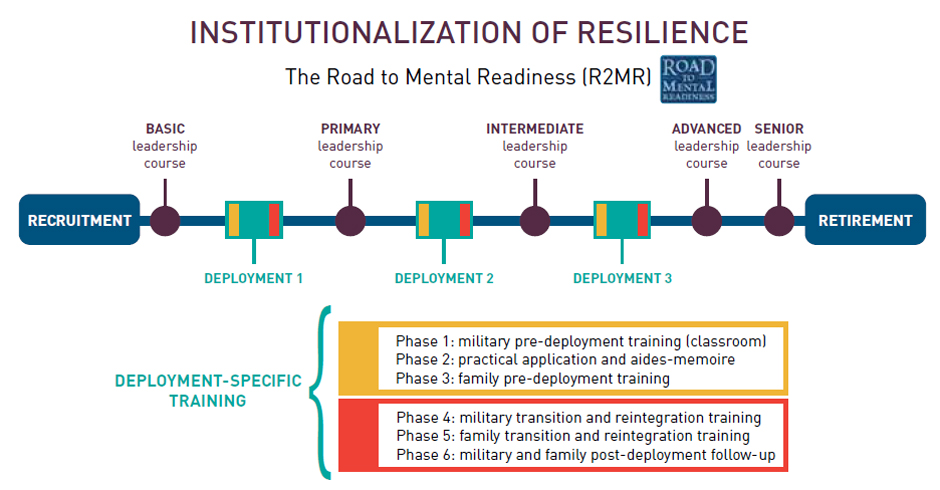
Institutionalization of Resilience - The Road to Mental Readiness (R2MR)
Institutionalization of Resilience - The Road to Mental Readiness (R2MR) (Text Equivalent)
Career Span:
- Recruitment
- BASIC (leadership course)
- DEPLOYMENT 1
- PRIMARY (leadership course)
- DEPLOYMENT 2
- INTERMEDIATE (leadership course)
- DEPLOYMENT 3
- ADVANCED (leadership course)
- SENIOR (leadership course)
- RETIREMENT
Deployment-specific training:
- Phase 1: military pre-deployment training (classroom)
- Phase 2: practical application and aides-memoire
- Phase 3: family pre-deployment training
- Phase 4: military transition and reintegration training
- Phase 5: family transition and reintegration training
- Phase 6: military and family post-deployment follow-up
The goal of R2MR training is to improve well-being and short-term performance, while mitigating any negative long-term mental health problems for both CAF personnel and their families. This is accomplished by teaching early identification of signs and symptoms of mental illness; the importance of peer and leadership support; appropriate leader actions; barriers to seeking mental health care (including stigma); and available mental health resources. Resilience skills, including tactical breathing, mental rehearsal, goal-setting, and self-talk, are also taught, mentored and cued to improve the ability of CAF members and their families to manage both operational and non-operational stresses.
The CF H Svcs Gp’s Directorate of Force Health Protection also provides the Strengthening the Forces health promotion program. This important program provides awareness and prevention education and skill development in areas such as suicide intervention, anger and stress management, healthy relationships, family violence, and addictions.
The education of CAF personnel and their families is not the sole responsibility of the CF H Svcs Gp and must therefore be well coordinated among all relevant CAF elements. R2MR is the foundational mental health education program, but harmonization and coordination of all mental health education and training is conducted by the Mental Health Education Advisory Committee, which is chaired by the Director of Mental Health. Members include representatives from all environments and training centres, the Chaplain branch, the Directorate of Military Family Services, the Directorate of Military Personnel Operational Research and Analysis, and Defence Research and Development Canada.
Care
Tactical-level clinical programs and services are delivered through 19 CF Health Services Centres and 16 Detachments at bases across Canada and in Europe. These Centres vary in size depending on the supported formation, base, wing, station or unit. The smallest clinics provide only psychosocial services, while the larger ones offer a variety of programs to meet all mental health needs of CAF members.
Mental health care is guided by evidence-based best practices and is delivered through multidisciplinary teams that include primary care clinicians, mental health nurses, psychiatrists, psychologists, social workers, occupational therapists, addictions counsellors and mental health chaplains. Current staff levels and the target of 447 established positions represents the highest ratio of providers to service members in NATO. In addition, there are over 2,000 civilian health care providers on the Blue Cross™ provider list who offer varying levels of care to our members across Canada.
The CF H Svcs Gp offers comprehensive treatment to CAF personnel, including unlimited psychotherapy and access to medication as required. When in-patient care is necessary, the CF H Svcs Gp has long-standing relationships with civilian health care facilities. Integration with the civilian health care system is essential to continuity of care for those referred to external providers, as well as to collaborate in shared research efforts.
As in the civilian community, a great deal of mental health care is delivered to CAF members by primary care clinicians. The CF H Svcs Gp is structured on a primary care delivery model in which all personnel receive care through a multidisciplinary health care team in a Care Delivery Unit (CDU). The CDU team works collaboratively with patients to assess their needs and to provide and coordinate care in support of complete wellness. In many cases, the first point of contact for CAF personnel who are experiencing mental health difficulties is their primary care team, which will either provide the required assistance or refer the member to the most appropriate care provider.
CAF personnel undergoing periodic health assessments and deployment-related medical screenings in primary care are also routinely asked questions pertaining to operational stress reactions, depression, addictions, suicide and other mental health conditions. These routine screening questions support the earliest possible identification of emerging concerns, while providing an opportunity for all CAF members to have a discussion with their care provider about mental health and well-being.
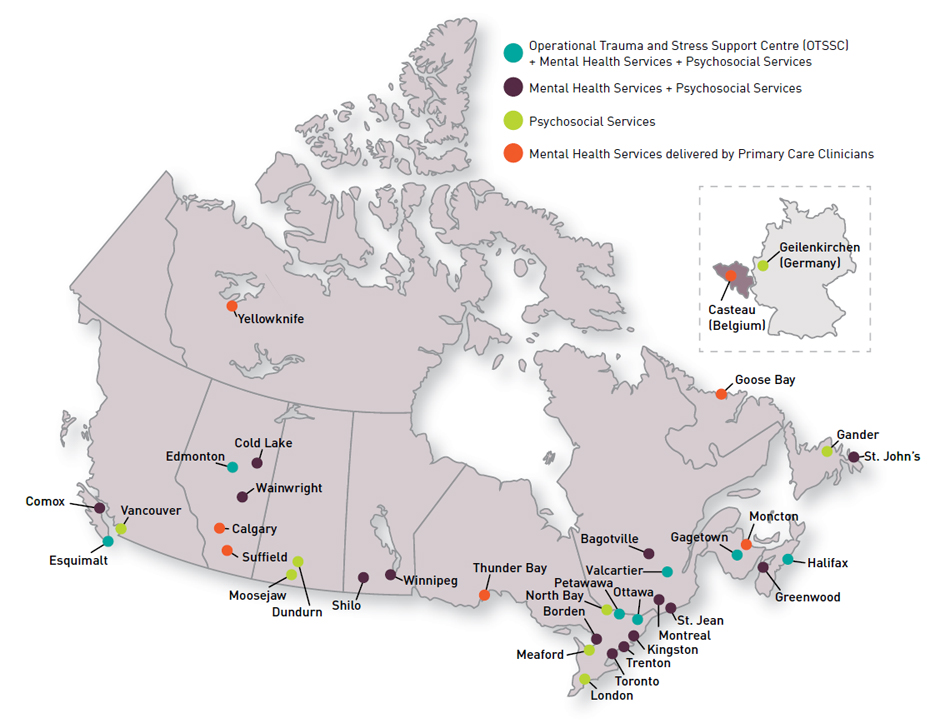
Mental Health Services Across Canada
Mental Health Services Across Canada (Text Equivalent)
Operational Trauma and Stress Support Centre (OTSSC) + Mental Health Services + Psychosocial Services:
- Esquimalt (British Columbia)
- Edmonton (Alberta)
- Ottawa (Ontario)
- Petawawa (Ontario)
- Valcartier (Quebec)
- Gagetown (New Brunswick)
- Halifax (Nova Scotia)
Mental Health Services + Psychosocial Services:
- Comox (British Columbia)
- Cold Lake (Alberta)
- Wainwright (Alberta)
- Shilo (Manitoba
- Winnipeg (Manitoba)
- Borden (Ontario)
- Kingston (Ontario)
- Toronto (Ontario)
- Trenton (Ontario)
- Bagotville (Quebec)
- Montreal (Quebec)
- St. Jean (Quebec)
- Greenwood (Nova Scotia)
- St. John's (Newfoundland and Labrador)
Psychosocial Services:
- Vancouver (British Columbia)
- Moosejaw (Saskatchewan)
- Dundurn (Saskatchewan)
- London (Ontario)
- Meaford (Ontario)
- North Bay (Ontario)
- Gander (Newfoundland and Labrador)
- Geilenkirchen (Germany)
Mental Health Services delivered by Primary Care Clinician:
- Calgary (Alberta)
- Suffield (Alberta)
- Thunder Bay (Ontario)
- Moncton (New Brunswick)
- Goose Bay (Newfoundland and Labrador)
- Yellowknife (Northwest Territories)
- Casteau (Belgium)
Psychosocial Services
Psychosocial Services provide first-line mental health care that CAF members may access directly without a physician’s referral. They are closely integrated with the CDU. Services include individual, couple, and family counselling to military personnel and their families; crisis management; addictions awareness; administrative support for processes such as compassionate and contingency cost moves; and deployment-related screenings. They are available at all CF Health Services Centres.
Mental Health Services
Mental Health Services are specialized services structured to provide multidisciplinary, evidence-based care, and require a referral from a physician. These secondary programs are provided by larger centres with regional support responsibilities. Delivery of mental health services is organized around a grouping of programs:
- General Mental Health Program: The General Mental Health Program provides assessment and individual and group treatment for those suffering from mental illnesses, such as depression, anxiety or PTSD, that are not attributable to deployed operations.
- Addictions Treatment Program: The Addictions Treatment Program provides assessment and treatment of individuals experiencing dependence or problem usage with alcohol, drugs or other compulsive behaviours. If in-patient treatment is required, it is provided by community resources external to CF H Svcs Gp. Service members are offered a one-year follow-up after treatment. Wherever addictions treatment services are not available within the CF H Svcs Gp, CAF members are referred to the appropriate civilian resource.
Dr. Fiona McGregor, Past President of the Canadian Psychiatric Association (CPA) stated: “The CAF is right to take pride in its mental health program which has been recognized by its NATO allies and civilian organizations.
”
Operational Trauma and Stress Support Centres
Operational Trauma and Stress Support Centre (OTSSC) programs are specialized mental health services with regional support responsibilities that ensure comprehensive and consistent assessment and treatment of patients with operational stress injuries using evidence-based best practices. The seven OTSSCs are located in Edmonton, Esquimalt, Gagetown, Halifax, Ottawa, Petawawa and Valcartier. They also conduct educational outreach and research in addition to their primary mandate for assessment and treatment.
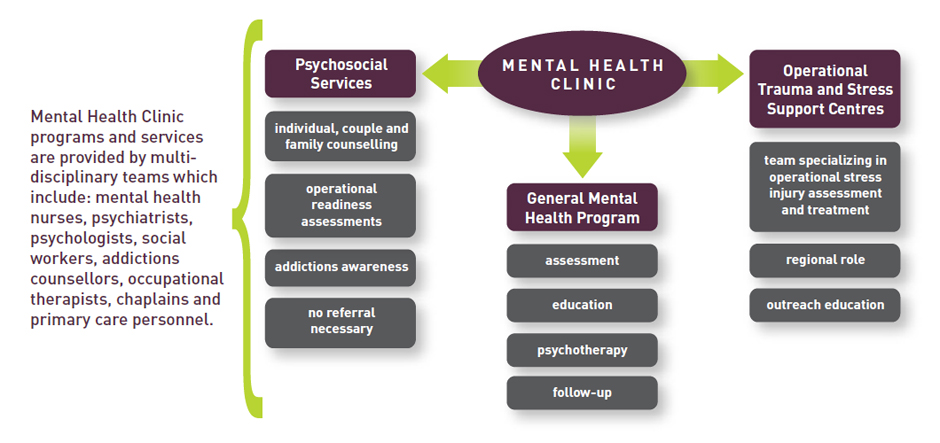
Mental Health Clinic Programs and Services.
Mental Health Clinic Programs and Services (Text Equivalent)
Mental Health Clinic:
- Psychosocial Services
- individual, couple and family counselling
- operational readiness assessments
- addictions awareness
- no referral necessary
- General Mental Health Program
- assessment
- education
- psychotherapy
- follow-up
- Operational Trauma and Stress Support Centres
- team specializing in operational stress injury assessment and treatment
- regional role
- outreach education
* Mental Health Clinic programs and services are provided by multi-disciplinary teams which include: mental health nurses, psychiatrists, psychologists, social workers, addictions counsellors, occupational therapists, chaplains and primary care personnel.
After attending an American Psychiatric Association conference, Senator Romeo Dallaire, Chair of the Senate Committee on Veterans Affairs, noted that: “… Canada’s program on operational stress injury was held as the example to be applied in the United States and, they hope, in other countries.
”
In addition to in-garrison mental health care, each deployment is provided mental health support ranging from a medic and a General Duty Military Officer, to a mental health specialist team. CAF members have the opportunity to consult with mental health clinicians in-theatre as well as during the transition from the theatre of operations to home. Members deployed to high-stress operations longer than 90 days participate in a Third Location Decompression (TLD) program, where they are encouraged to speak to a mental health professional and raise any concerns they may have. All CAF personnel returning from international operations of 60 or more days undergo the Enhanced Post-Deployment Screening (EPDS) process between three and six months after their return to Canada. This screening tool assists us in highlighting any difficulties returning members may have with mental health or simply with adjusting to life in garrison and within their family unit. It also assists us in connecting them with the appropriate resources. The chain of command plays a critical role in this process by ensuring that all deployed personnel complete their EPDS, in order to support an early identification of reintegration challenges and mental health issues.
Individuals are continually encouraged to seek help throughout the deployment cycle. One half of those who require mental health follow-up have already sought some level of care on their own by the time they complete the EPDS. In order to further reduce barriers to care, referrals can be made directly from theatre or TLD to the member’s local CF Health Services Centre in order to ensure a smooth transition and continuity of care.
Coping with psychosocial and mental health problems can be challenging for CAF members and their families for many reasons and in many ways. CF H Svcs Gp does not have the mandate to provide care directly to family members of CAF personnel. It is recognized, however, that families play a crucial role in a member’s mental health. We can therefore provide mental health services to families when it is a necessary component of the member’s treatment or care. The mental health system provides member-focused family care because there is considerable evidence and professional consensus that family involvement in the treatment process can improve outcomes.
Two successive presidents of the Canadian Psychiatric Association were hosted in November 2012 at Petawawa Health Services Centre by mental health staff. “We were very pleased to have the opportunity to experience the realities of the Canadian Armed Forces and its medical system. Both myself and past-president, Dr. Fiona McGregor, were impressed with what we saw.
” said Dr. Suzane Renaud, President of the CPA. “
” We recognize the sacrifices that soldiers make and are pleased to see a comprehensive mental health system in place to support them.
In particular, the CAF mental health system offers a truly interdisciplinary approach to care with mental health practitioners, such as primary care clinicians, psychiatrists, social workers, mental health nurses, addictions counsellors and chaplains, working as a team to treat patients. As well, the CF H Svcs Gp’s electronic records system and its accredited status through Accreditation Canada are truly impressive.

Additional Programs Available to CAF Members
Canadian Forces Member Assistance Program (CFMAP)
CFMAP is a 24/7 toll-free telephone advisory and referral service for all CAF personnel and their families, and can provide short-term, confidential, external counselling for those in need. 1-800-268-7708.
Strengthening the Forces
Strengthening the Forces is the CAF health promotion program and includes awareness and prevention initiatives in areas such as suicide intervention, anger and stress management, healthy relationships, family violence prevention, and addictions.
Operational Stress Injury Social Support (OSISS)
OSISS is a peer-based support program for CAF members, veterans and their families who are coping with an operational stress injury.
Chaplains
As trained religious and spiritual caregivers, CAF chaplains contribute significantly to the spiritual and mental health care of CAF members and their families. They are on-call 24/7 to support members in need and provide support and advice to the chain of command and care providers.
Military Family Services
Military Family Services manages the Military Family Services Program, the Dependent Education Management Program, and addresses issues that affect the quality of life of families on behalf of the Department of National Defence and the CAF. It provides funding and oversight of the Military Family Resource Centres (MFRC) that are located at Bases and Wings across Canada, the United States and Europe. They also provide a 24/7 Family Information Line (1-800-866-4546) that offers bilingual, confidential information and referrals (including mental health) by trained counsellors, an online portal to MRFC, and information useful to all military families.
Veterans Affairs Canada (VAC)
VAC offers a wide range of services and benefits for Veterans, CAF members and Royal Canadian Mounted Police (RCMP) members living with a mental health condition, and their families. It aims to ensure a seamless transition from military to civilian life.
Directorate of Casualty Support Management (DCSM)
DCSM provides policy oversight and manages non-clinical support programs for the ill and injured, as well as transition services for all CAF members. The provision of support services for currently serving and former CAF ill and injured personnel, their families, and the families of the fallen, is done through Integrated Personnel Support Centres (IPSC) and satellites providing services at over 30 locations across Canada.