Surgeon General's Mental Health Strategy: Unique Opportunities within the CAF Mental Health System
The CAF currently has a very strong and comprehensive mental health system that delivers high-quality care. Key factors unique to the CAF environment, however, permit the continued improvement of our system. We will focus our efforts over the next five years in related areas to continue to meet the evolving needs of CAF members—now and in the future.
Shared Responsibility
A balance between the patient, the chain of command and the health system is essential to high-quality mental health care. The CAF can have a significant influence on all three to ensure that they are working closely together in order to achieve:
- an efficient and effective health system focused on high-quality health outcomes
- actively involved patients that personally invest in their health care
- a supportive and engaged chain of command
To achieve this ideal interaction, we must manage patient concerns and right to personal privacy, health professionals’ legal obligation to not disclose personal information, and the chain of command’s responsibility for the health and well-being of those under its command.
This triad of care calls for CAF leaders to visibly take measures to combat stigma, encourage prevention and education programs, openly talk about mental illness in the workplace, seek ways to improve mental health among their personnel, work closely with the medical community and support those who need help.
It is critical that health professionals protect the privacy of their patients’ health information while also involving the chain of command, where appropriate, in the care of their patients. Military health professionals must understand the occupational complexity and unique operational demands on our patients, and have regular and open communication with the chain of command. Above all, they must deliver high-quality, evidence-based health care through optimal multidisciplinary collaboration.
The assignment of medical employment limitations is imperative for good communication with the chain of command, as well as to protect patients and enable their recovery. They must be timely, clear, and practical without disclosing diagnosis or treatment. They communicate prognosis to the chain of command and help inform the best approach to supporting the member.
Patients are the most important part of this triad of care and must be actively involved in their own care. Those who follow their treatment plans, follow up with their mental health team as required, and are open and honest with their care providers and chain of command have the greatest chance of successful recovery.
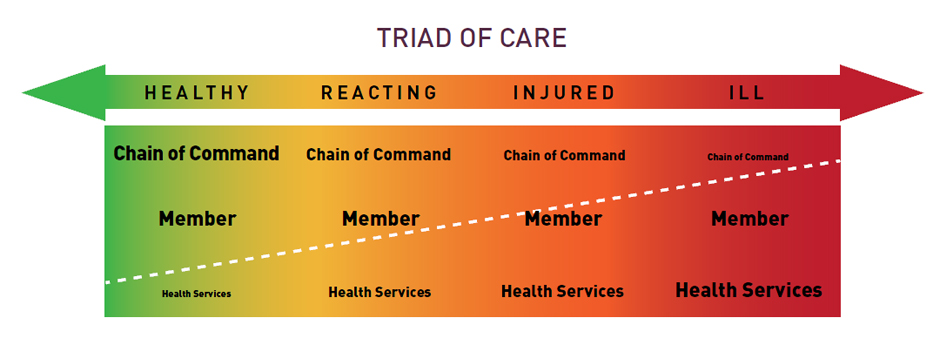
Triad of Care
Triad of Care (Text Equivalent)
| Healthy (green) | Reacting (yellow) | Injured (orange) | Ill (red) |
|---|---|---|---|
| Chain of Command | Chain of Command | Chain of Command | Chain of Command |
| Member | Member | Member | Member |
| Health Services | Health Services | Health Services | Health Services |
Primary Care / Mental Health Integration
Mental health cannot be isolated from physical health. The two are physiologically linked, yet in many ways, they are artificially separated in the Canadian health care system. The CAF health system is, in contrast, specifically established to ensure a close partnership between mental health professionals and primary care teams. Even when mental health and primary care clinics are physically separated, open and clear communication is facilitated by a common chain of command and clinical leadership.
At a fall 2012 symposium, Base/Wing surgeons universally agreed that it was important to strengthen the connection between mental health and primary care in order to ensure comprehensive and integrated care plans. Where it was working well, the overwhelming reason was strong clinical leadership in both domains. It was also clear that sharing the mental health notes with the primary care team was critical to establishing a comprehensive diagnosis and treatment plan.
Performance Measurement and Quality Improvement
Performance measurement and quality improvement (PM&QI) are essential for all health systems, and CF H Svcs Gp is well situated to deliver high-quality care consistent with best practices. Given CAF’s unique role as employer, insurer and deliverer of health services, additional investments in PM&QI will directly lead to enhanced quality of care and health system productivity, as well as decreases in other health care expenses. We measure wait times and patient satisfaction, yet we still share the same challenges of all health systems with measuring health outcomes.
Improving the efficiency and efficacy of care is especially crucial in the context of rapidly increasing health care costs and increasing fiscal austerity. In contrast to civilian health systems, this goal is greatly facilitated by having all CAF health system elements under the control of a single health authority. This permits us to more rapidly and readily determine optimal processes of care and to implement quality improvement measures. Recent developments in measuring expected treatment response will enable a much more robust assessment of patient outcomes and help clinicians tailor treatment to individual needs.
Investment in our PM&QI system will support a more efficient and effective mental health system that improves quality of care.
Mental Health Education
Prevention through education is essential to helping personnel manage stresses and enhance performance, as well as to recognize early indicators of distress and to facilitate care-seeking. CAF mental health education aims to overcome barriers to mental health care, increase mental health literacy, decrease stigma, and enhance well-being and performance in response to occupational and other stressors. Our program aims to demystify mental health treatment and highlight the well-resourced, evidence-based services available to CAF members. While CAF attitudes toward care-seeking have improved significantly in the past decade, there is still work to be done to further reduce stigma and other barriers to care. For example, R2MR is being tailored to address the special needs of the Royal Canadian Navy, the Royal Canadian Air Force, and specific occupations.
Clinical Competency Training
As medical knowledge evolves and promising new therapies emerge, we must ensure that our clinicians remain current with the most up-to-date, evidence-based treatment in order that CAF members receive leading edge health care. This can be achieved through such measures as collective training, conferences and workshops, teaching in academic centres, and research. We must also continually pursue ways of optimizing technological developments.
With the development of the Canadian Forces Health Information System (CFHIS), we have dramatically improved our ability to capture patient information with each visit. In time we will be able to use this information to better capture the prevalence of various health conditions. With further investment, CFHIS can become a data warehouse to provide senior leadership with a proactive understanding of the health of the CAF population.
Programs versus Services
CF H Svcs Gp’s broad range of high-quality services delivers excellent health care, but it must be integrated into more structured programs. For example, several services are available for treating addictions, and many educational tools and services are available for suicide prevention. We can enhance these services as they are consolidated and structured into programs.
Mental Health Program
A mental health program consists of more than just the health services available in a CF Health Services Centre. It consists of a framework that includes quality assurance, performance measurement and effective communication. The core components of a mental health program are:
- an assigned Program Leader
- a clear set of priorities and expected deliverables
- clear and concise guiding policies
- a focus on primary, secondary and tertiary prevention
- an evidence-based approach to assessment and treatment
- quality assurance/improvement processes
- a performance measurement framework
- a communication framework for patients, care providers and the chain of command
- an overarching focus on research
Research
Through health surveillance, the CAF knows more about the mental health of its workforce than any other large employer in Canada. Elements of the Surgeon General Health Research Program will help increase our understanding of mental health in the CAF and answer such questions as:
- What is the impact of leaders on the mental health of subordinates, deployed and in-garrison?
- What is the overall impact of mental health on CAF workplace productivity and safety?
- What is the impact of the post-deployment screening program?
- What is the effectiveness of the R2MR program?
- Which treatments are effective or ineffective in specific populations?
Military Families
Military families are often referred to as “the strength behind the uniform.” A family member’s knowledge of mental illness and of abnormal indicators to look for in their loved ones returning from operations is essential for early diagnosis and treatment of operational stress injuries. Families are therefore part of our mental health strategy, including our R2MR program.
MFRCs across Canada, the United States, and Europe provide extensive programs and services including mental health prevention, support and intervention services such as assessment and short-term counselling. MFRC staff are very familiar with community supports and services that offer families more options to meet their mental health needs. Some of these include the Family Road to Mental Readiness Program, Family Liaison Officers, Casualty Support Child Care, tailored programs for children and youth, community referrals, a 24-hour Family Information Line, a 24/7 telephone advisory and referral service through CFMAP, and www.FamilyForce.ca.
Geographic isolation, postings, frequent absences on duty, high-risk deployments and unpredictability are aspects of military life that put stress on members and their families and may contribute to mental illness. DND and the CAF have implemented many initiatives over the past few years to better support military families. Some of the most common and significant stresses are outside the control and jurisdiction of DND and the federal government, such as access to family health care or loss of spousal employment subsequent to a posting.
Local MFRCs and partner organizations have worked diligently to raise awareness and understanding among service providers about the unique stressors of the military life, and how communities can improve their programs and services to better address the mental health needs of CAF families.
Given the impact of family mental health on CAF members, it is in the CAF’s interest to strongly support the establishment of community health and other services for families within the parameters of constitutional, legal and mandate constraints.

Groups with Different Considerations
The CAF mental health system was established based on CAF needs identified more than 10 years ago. The past decade’s high-intensity operations and changing circumstances have, however, highlighted several groups of people that face different barriers to mental health care.
One such group is the Reserve Force. Under the Total Force concept, our Reserve Force population has contributed heavily to every domestic and international operation. Although data does not indicate a difference in the prevalence of mental illness among Reservists, some of them face unique barriers to care such as distance to access mental health clinics, concern about getting Class B contracts, relative isolation from colleagues who share the same deployment experience and the demands of being a part of both the military and civilian communities. Our mental health system is robust but we must work with VAC, our community partners, charitable organizations, and others to better meet the needs of Reservists.
Other groups, such as those who work in special operations, signals intelligence or image analysis personnel, do not have the normal rotation cycles of large Joint Task Force units. Special aspects of their work can be extremely stressful and may potentially harm their mental health. In some cases, barriers to care may be both real and perceived due to the sensitivity of their missions and the information they deal with, but we must ensure that their mental health care is as comprehensive as it is for all other CAF members.
The majority of the Canadian public is only familiar with large CAF missions such as Afghanistan or Haiti. Few realize that operations are occurring every day in Canada and in small high-risk missions around the world. Among others, examples include search and rescue, maritime patrol drug interdiction, arctic patrol, and United Nations military observers. These operations may place lives at risk, but the CAF members involved often do not undergo the same pre- and post-deployment screening that large deploying contingents do.
Finally, CAF health care providers not only deliver care in Canada every day, but also put their own lives at risk to care for others on deployment where they may see more death and trauma than their colleagues in other arms of the CAF. While health care providers formally have the same access to health care as other CAF members, their dedication to duty, expectations for them to continue providing care to others or privacy concerns may present barriers to their own care. We must be vigilant in ensuring that they are also looked after.