Report on housing needs of seniors
On this page
- Participating governments
- Acknowledgements
- Executive summary
- 1. Introduction
- 2. Background
- 3. Methodology
- 4. Seniors’ historical housing needs in Canada
- 5. Seniors in core housing need in Canada in 2016
- 6. Beyond seniors core housing need
- 7. The meaning of “home” and “age friendly communities”
- 8. Selected Canadian initiatives
- 9. Selected International Initiatives
- 10. Conclusion
- Appendix A: A classification of housing for seniors1
- Appendix B: Financial supports for home repair, renovations and adaptations
- References
- Glossary
Alternate formats

Report on housing needs of seniors [PDF - 787 KB]
Large print, braille, MP3 (audio), e-text and DAISY formats are available on demand by ordering online or calling 1 800 O-Canada (1-800-622-6232). If you use a teletypewriter (TTY), call 1-800-926-9105.
Participating governments
- Government of Ontario
- Government of Québec*
- Government of Nova Scotia
- Government of New Brunswick
- Government of Manitoba
- Government of British Columbia
- Government of Prince Edward Island
- Government of Saskatchewan
- Government of Alberta
- Government of Newfoundland and Labrador
- Government of Northwest Territories
- Government of Yukon
- Government of Nunavut
- Government of Canada
- * Québec contributes to the Federal/Provincial/Territorial Seniors Forum by sharing expertise, information and best practices. However, it does not subscribe to, or take part in, integrated federal, provincial, and territorial approaches to seniors. The Government of Québec intends to fully assume its responsibilities for seniors in Québec.
The views expressed in this report may not reflect the official position of a particular jurisdiction.
Acknowledgements
Prepared by Dr. John Puxty, Professor Mark W. Rosenberg, Dr. Lisa Carver and Professor Barbara Crow, Queen’s University Network of Aging Researchers (QUNAR) for the Federal, Provincial and Territorial (FPT) Forum of Ministers Responsible for Seniors. The views expressed in this report may not reflect the official position of a particular jurisdiction.
In support of work on the topic of Aging in Community, the Federal/Provincial/Territorial (FPT) Forum of Ministers Responsible for Seniors developed two documents:
- A Report on Housing Needs of Seniors
- A Report on Core Community Supports to Age in Community
These reports should be reviewed and considered together.
Executive summary
During the September 2017 meeting in St John’s, Newfoundland and Labrador, Federal, Provincial and Territorial (FPT) Ministers Responsible for Seniors (FPT Seniors Forum) approved aging in community as a key priority. In making this decision, the FPT Seniors Forum commissioned this report on core housing need.
Canada’s almost six million seniors represent a complex and dynamic cohort, with diverse living arrangements and housing needs. Within this context, it is generally understood that most seniors desire to age in community.Footnote 1 However, as individuals age their needs and capabilities can change and they may experience challenges in finding suitable housing to accommodate their changing needs and services. These challenges may include difficulty in finding affordable housing; ability to afford necessary adaptive changes; limited access, or barriers to, mobility aids; and/or potential gaps in availability of appropriate supportive services such as home care. This suite of needs is referred to as the “integrated housing needs” of seniors and when these needs are satisfied seniors can successfully “age in community”.
According to the Canada Mortgage and Housing Corporation (CMHC), a household is living in acceptable housing when it is:
- adequate (does not need major repairs)
- suitable (has enough bedrooms for the household); and
- affordable (costs less than 30% of before-tax income)
A household is living below standards when one or more of the conditions listed above are not met.
A household is in core housing need when their housing is not acceptable and the household does not have enough income to meet expenses of an acceptable alternative.
This report provides a snapshot of the core housing need for seniors and senior-led households (when possible by gender, age and region). The report then expands the study of seniors’ housing needs to include aspects not covered in the core housing need definition, such as accessibility, safety and environmental sustainability. In addition, this report offers an overview of current Canadian and international initiatives that assist seniors in addressing their integrated housing needs. It also examines the potential linkages between the housing market conditions in Canada and integrated housing needs. Within this context, the main types of housing initiatives that assist seniors living with mobility impairments or a broader range of disabilities, including financial initiatives to address housing needs, are examined. While the focus of this report is on seniors’ integrated housing need, it is important to note the connection between the various housing options available to seniors and the care continuum. Housing options range from living independently in a single-family dwelling to living in a residential care facility with 24/7 nursing and other forms of care. Between the two extremes, there are numerous combinations of housing, medical and non-medical care. For example, there are many seniors living in their own homes or in apartments with some level of home care.
Background
Seniors (those 65 years of age and over) are the fastest growing age group in Canada. In 2016, there were 5,935,635 seniors, who represented 16.9% of the total population in Canada and this percentage is expected to increase to 24% by 2036.
The 2016 Census reported that 93.2% of seniors lived in private dwellings (house, apartment or moveable dwelling) while 6.8% lived in collective dwellings, such as residences for senior citizens, long-term care (LTC) facilities or health care related facilities.
Approximately 25% of Canadian households are led by people over the age of 65 years, 75% of these households are owned and 25% rent accommodation. The largest proportion of these senior-led households are couples without children; the second largest group is single women. In 2016, 2.2 million Canadians lived in multigenerational housing, 349,350 of whom were aged 65 and over.
Housing moves by seniors can be characterized as either “lifestyle,” “planned,” or “crisis,” each of which is typically underpinned by a number of “push” (for example, death of a spouse) or “pull” factors (for example. a desire to be closer to children and grandchildren). Seniors are less likely to move than the general population. In 2016 only 5.5% of seniors 65 to 74 years old and 4.7% of those 75 years and older had moved compared to 13.0 % of the general population in the previous year. Seniors who are widows and those who are divorced or separated are more likely to move. Seniors who are renting their homes are twice as likely to move compared to seniors who are homeowners (14% versus 7% respectively).
Integrated housing need
Core housing need
The percentage of senior households in Canada living in core housing need fell between 2001 and 2006 and thereafter remained stable at around 14%. However, Saskatchewan and to a lesser extent Alberta continued to see increases after 2006. Since 2011, Saskatchewan has had the highest provincial proportion of senior households in core housing need followed closely by Ontario, Alberta and British Columbia. In recent years, the sharp rise in housing costs that affected senior renter households living in census metropolitan areas (CMAs) in Ontario, Saskatchewan, Alberta and British Columbia may have contributed to increasing the number of households in core housing need.
According to the 2016 census, almost a quarter of seniors lived below standardsFootnote 2 (24.9%) regardless of their housing arrangement. Individually or in combination, affordability issues were most common (19.4%) followed by adequacy issues (4.6%) and then suitability issues (2.6%). Core housing need (42.8%) and in particular affordability (39.7%) issues were common in households of seniors living alone.
In 2016, Saskatchewan was the province with the highest percentage of senior-led households in core housing need. Ontario, however, had many more households in core housing need, accounting for almost 46% of core housing need in Canada. Among the territories, Nunavut had the highest percentage of senior-led households in core housing need reflecting longstanding shortages and the high cost of housing. In addition, senior-led households in census metropolitan areas (CMAs) were more likely to be in core housing need than those in small towns and rural areas (non-CMA/Census Agglomeration (CAs)). Vancouver and Toronto were the two major metropolitan areas with the highest rates of senior-led households in core housing need in 2016.
Those living in core housing need tend to have significantly lower average incomes. Senior women are more likely to live alone and have low incomes and therefore are more likely to live in core housing need. In fact, in 2016, 57.4% of seniors living in core housing need consisted of women who lived alone. Additionally, in 2016, most seniors with core housing need lived in apartments and were renters.
Beyond core housing need
Housing developments often lack basic consideration of good environmental design (steps, ramps, railing, lighting, safety features, etc.). Seniors’ housing built between the 1960s and 1990s is often unable to accommodate newer independence technologies such as motorized scooters and bulky electric wheelchairs that need to be plugged in.
As seniors age, they are more likely to face disability, to find that their disability creates difficulties for them, and that they need help. Without informal and formal support (for example, homecare), older people with disabilities are among those who are most likely to want or need to find alternative forms of housing.
Aging in community includes making sure the environment, especially the home, is functional and meets the changing needs of seniors (HomeStars, 2017). Home renovations and adaptions can be implemented to improve safety and accessibility. Modifications can enhance seniors’ overall functioning and well-being (Boland et al., 2017). Home modifications can help seniors age at home and may prevent the need to move to other locations.
The meaning of “home” and “age-friendly communities”
It is important to understand the meaning of home from a senior’s perspective to inform service providers and stakeholders in responding to integrated housing needs.
According to the World Health Organization (WHO), the physical and social environments are key determinants of whether people can remain healthy, independent and autonomous as they age. As such, in an Age-Friendly Community (AFC), the physical and social aspects of a community are designed to improve the health and well-being of older adults.
Across Canada, many communities have taken part in AFC development activities at various levels in order to support active aging and aging in place. Through these activities, participating communities have taken action to improve their level of “age-friendliness”, and learned how to integrate an aging perspective into urban planning, and create age friendly spaces and environments.
Canadian housing options for seniors
Across Canada, the for-profit and the not-for-profit sectors, often in conjunction with local governments and incentives from other levels of government, have developed a variety of housing options that try to capture the meaning of home and the spirit of AFCs. The options include: Mainstream Housing, Naturally Occurring Retirement Communities (NORCs), Independent Living and Active Lifestyle Accommodation (inclusive of home share, life lease, cooperatives and flex housing), Assisted Living / Supportive Housing Accommodation, and Seniors Residences and LTC accommodations.
New buildings and homes that follow principles of universal design can provide spaces that are more easily accessible and a barrier-free environment, which enhances the ability to perform daily activities independently (Carr, 2013 and Crews & Zavotka, 2006). There are also specific housing needs for seniors with dementia.
Beyond building new housing, home modifications are another alternative for addressing some integrated housing needs. Research, however, has shown that two barriers to this option are lack of knowledge among seniors to carry out home modifications and the lack of resources to carry them out. Where governments in Canada and other jurisdictions have created funding mechanisms for home modifications, they have aided in aging in community.
International housing initiatives
The need for alternative forms of housing for seniors is not unique to Canada. Especially across Europe and the United States, other jurisdictions have experimented with various forms of housing to address the needs of seniors. Examples include Lifetime Neighbourhoods (United Kingdom), Co-Housing Communities (Denmark), Producer Driven/Resident Driven Seniors Homes (Finland), Apartments for Life (the Netherlands), Homeshare (France) and Villages (United States).
Conclusion
The main findings of the report indicate:
- there is a need to increase the supply of housing for seniors overall, with options that consider the range of health needs and income status of seniors
- senior women are more likely to live alone and have low incomes, and therefore are more likely to live in core housing need
- strategies should continue to be sought to incentivize builders, planners and purchasers to incorporate features of universal design for future adaptability and accessibility into new builds and renovations
- strategies should continue to encourage and promote production of more diverse and affordable housing options, since the national and international evidence reviewed demonstrates that no one housing option is preferable to seniors and all of the options reviewed had positive benefits in sustaining the well-being of seniors
- from the examples identified, the well-being of seniors can be improved through all levels of government encouraging and promoting inclusion of age-friendly principles into all future building and space design policy and planning. Overall, to implement Age-Friendly Communities, there needs to be adaptations and transformation among home design, neighborhood design, city planning, transportation, and health and home-care services
Considerations for further study that all levels of government can encourage, promote and/or increase:
- mixed-use developments with housing located near services and amenities to reduce some of the accessibility and transportation barriers that currently exist
- allow construction of smaller units such as accessory dwelling units for those wishing to down-size, reduce housing costs or house a live-in caregiver
- develop housing suitable for intergenerational living
- retrofitting of existing homes to improve accessibility
- construction of affordable rental units especially in suburban settings; and
- coordinate housing adaptations and community supportive services delivery to increases availability of supportive living options as a viable alternative to LTC
- housing for Indigenous seniors
There is still a need for the creation of a robust knowledge exchange strategy to increase awareness of and access to evidence-informed best practices and models of housing options for seniors in Canada. In addition, further research is needed to understand what motivates seniors to consider various housing options and what deters them. Overall, addressing the core housing need and integrated housing needs of seniors will require adaptations and transformation with respect to home design, neighborhood design, city planning, transportation, and health and home-care services among all levels of government – in consultation with seniors and stakeholders.
1. Introduction
During their September 2017 meeting, Federal, Provincial and Territorial (FPT) Ministers Responsible for Seniors (FPT Seniors Forum) approved aging in community as a key priority. Between spring 2018 and spring 2020, the FPT Seniors Forum will analyze and report on aging in community on the following 3 key related areas:
- housing needs for seniors
- community supports to facilitate seniors’ aging in community; and
- policy options to facilitate aging in community
The purpose of this report is to address the first area of examination, namely, the housing needs for seniors.
Canada’s almost six million seniors represent a complex and dynamic cohort, with diverse living arrangements and housing needs. Within this context, it is generally understood that most seniors desire to age in place.Footnote 3 However, as individuals age their needs and capabilities can change and they may experience a challenge in finding suitable housing to accommodate their changing needs and services. These challenges may include difficulty in finding affordable housing; ability to afford necessary adaptive changes; limited access or barriers to the use of mobility aids and/or potential gaps in availability of appropriate supportive services such as home care. This suite of needs is referred to as the “integrated core housing need" of seniors and when these needs are satisfied seniors can successfully “age in community” (Figure 1).
According to the Canada Mortgage and Housing Corporation a household is living in acceptable housing when it is:
- adequate (does not need major repairs)
- suitable (has enough bedrooms for the household); and
- affordable (costs less than 30% of before-tax income)
A household is living below standards when one or more of the conditions listed above are not met.
A household is in Core Housing Need when their housing is not acceptable and the household does not have enough income to meet expenses of an acceptable alternative.
Throughout the remainder of this report a distinction is drawn between core housing need and integrated housing needs where the former is treated as integral component of the broader concept of integrated housing needs.
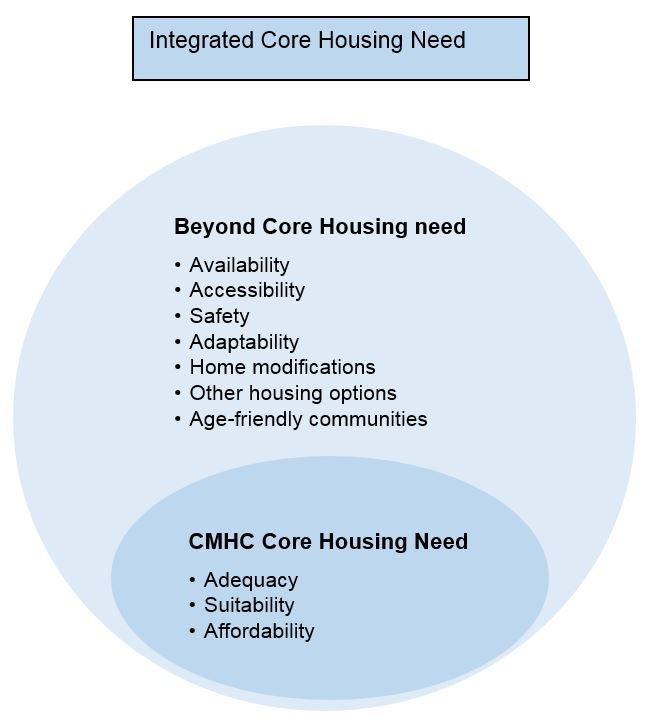
Figure 1 - Text version
The diagram is of two circles one within the other.
The smallest circle indicates the elements that need to exist for a senior to be in ‘core housing need’. These include: adequacy, suitability and affordability.
The larger circle indicates the elements that are beyond core housing need. These include: accessibility, availability, safety, adaptability, home modifications, other housing options and age-friendly communities.
The two circles together represent the relationship between core housing need and integrated housing need.
This report, therefore, provides a national picture of seniors’ integrated housing needs (when possible by gender, age and region). In addition, the report offers an overview of current Canadian and international initiatives that assist seniors in addressing integrated housing needs. It also examines the potential linkages between the housing market conditions in Canada and seniors’ integrated core housing need. Within this context, the main types of housing initiatives that assist seniors living with mobility impairments or a broader range of disabilities, including financial initiatives to address housing needs, are examined. While the focus of this report is on seniors’ integrated housing need, it is important to note the connection between the various housing options available to seniors and the care continuum. Housing options range from living independently in a single family dwelling to living in a residential care facility with 24/7 nursing and other forms of care. Between the two extremes there are numerous combinations of housing, medical and non-medical care. For example, there are many seniors living in their own homes or in apartments with some level of home care.
This report builds on work undertaken by the FPT Seniors Forum on ‘Planning for Aging in Place’ from 2013 to 2016, which included the development and dissemination of a series of tools, factsheets and videos to support and inform an individual’s plans for aging in place, which can be found on Promoting the labour force participation of older Canadians - Canada.ca.
2. Background
Seniors (those 65 years of age and over) are the fastest growing age group in Canada. In 2016, there were 5,935,635 seniors, who represented 16.9% of the total population in Canada and this percentage is expected to increase to 24% by 2036 (Statistics Canada 2016, Federation of Canadian Municipalities, 2015).
Approximately 25% of Canadian households are led by people over the age of 65 years. 75% of these households are home owners and 25% are renters (Statistics Canada, 2016b). The largest proportion of these older adult-led households are couples without children and the second largest group is one-person female-led households (Statistics Canada, 2017). In 2016, 2.2 million Canadians lived in multigenerational housing, 349,350 of whom were aged 65 and over. The fastest growing housing arrangement is multigenerational housing (Statistics Canada, 2017). It is also worth noting that seniors’ specific housing needs (within a continuum of housing options) have evolved over time and as they do, the options available to seniors need to evolve as well.
Seniors wish to continue to live independently for as long as possible in their home and community (Chiu, 2016). There are several reported benefits to living independently including increased physical, mental, and social capacities. Continued successful aging in place over a 14 year longitudinal study was associated with a reduced incidence of depression symptoms among seniors (Kendig, Gong, Cannon & Browning, 2017). Additionally, it reduces the emotional and physical hardships associated with leaving a familiar place (Federation of Canadian Municipalities, 2015). Aging in place allows seniors to maintain social networks with family members, friends and community members and maintain personal identity. Supporting seniors to age in place with appropriate support services potentially avoids the high costs associated with acute care such as emergency room visits and hospital admissions (Chiu, 2016).
Seniors are less likely to move than the general population. In 2016 only 5.5% of seniors 65-74 years old and 4.7% of those 75 years and older had moved in the past year compared to 13.0 % of the general population (Statistics Canada 2016). Seniors who are widows and those who are divorced or separated are more likely to move (Lin, 2005). Seniors who are renting their home are twice as likely to move compared to seniors who are homeowners (14% versus 7% respectively) (Lin, 2005).
Housing moves by seniors can be characterized as either “lifestyle,” “planned,” or “crisis,” each of which is typically underpinned by several “push” or “pull” factors (see Figure 2). These relate to changes in the individual’s circumstances or specific “trigger points” linked to an individual’s health. Push factors include difficulties with maintaining the home or garden, the cost of energy bills associated with a larger or older home, or difficulties with steps or stairs (linked to the increased risk of falls). Pull factors include the accessibility of local shops and services (often framed in terms of reliance on a car) or a desire to move closer to other family members.
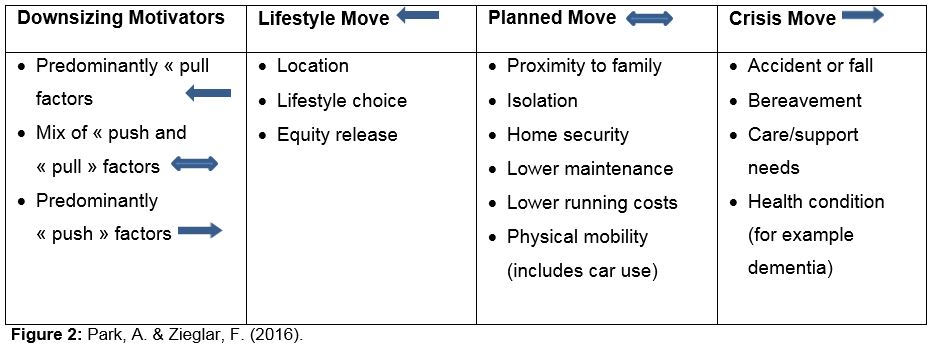
Figure 2 - Text version
The diagram shows that housing moves made by seniors are motivated by a “lifestyle” change, a “planned” change or a “crisis”. The change in location occurs as a result of factors that push, pull or both push and pull the residents. A lifestyle move occur as a result of pull factors: location, lifestyle choice or equity release. A planned move occurs as a result of push and pull factors: proximity to family, isolation, home security, lower maintenance, lower running costs and physical mobility (includes car use).
For many seniors, several factors seem to delay the decision to move, often until a crisis is present or imminent. These include: a strong emotional attachment to one’s existing home; a desire to sustain social networks within the immediate community (particularly neighbours); the potential disruption and costs associated with moving; a human tendency to defer planning for the future (and ignore or discount potential or real changes in physical mobility or health); a fear that an unknown future dwelling may not match up to expectations; and, perhaps a lack of availability of alternative affordable and/or attractive housing and/or downsizing options.
3. Methodology
The findings and information included in this report are based on data from the Canada Mortgage and Housing Corporation (CMHC) (based on the 2016 Census), which was used to examine the current integrated housing needs of seniors. In addition, other key surveys, such as the Canadian Survey on Disability and the Canadian Community Health Survey (CCHS) were utilized for the purposes of this report. While the Census data are reported directly as they appear in the Census, some of the CMHC data are compiled from various data sets created by the CMHC based on their data and data from the Census. The numbers and percentages reported from Statistics Canada surveys (for example, the CCHS) are the weighted data to provide estimates that reflect the senior’s population of Canada taking into account the specific limitations of the surveys. For more information about the weighting procedures used by Statistics Canada and the limitations of any of the surveys, used in this report, one should consult the free online reports provided by Statistics Canada and the relevant technical reports provided by CMHC to explain its data products
This report is also based on an extensive review of key FPT reports/initiatives. Examples of types of policies or initiatives examined include, at the federal level, the National Housing Strategy, as well as an overview of selectedFootnote 4 provincial and territorial initiatives that address integrated housing needs. An overview of academic and non-governmental literature was conducted in order to identify Canadian initiatives that go beyond core housing need. This included an examination of relevant international literature identifying promising international initiatives. A glossary of terms has been developed and is included at the end of the report.
A final challenge was that there is no agreed upon terminology among the provinces and territories or internationally about the various types of housing being offered to seniors along the continuum from living in one’s own house or apartment to living in an institutional setting and receiving long-term care. Throughout the report, the names of the housing examples from the provinces and territories or internationally are used unchanged. In Appendix A, the examples have been categorized as independent housing, assisted living and long-term care.
4. Seniors’ historical housing needs in Canada
The percentage of senior households in Canada living in core housing need fell between 2001 and 2006 and thereafter remained stable at around 14% (Figure 3). However, Saskatchewan and to a lesser extent Alberta continued to see increases after 2006. Since 2011 Saskatchewan has had the highest provincial proportion of senior households in core housing need followed closely followed by Ontario, Alberta and British Columbia (Figure 3). The robust economy in these provinces has until recently resulted in major growth in housing value on the homeowner and rental markets alike. The sharp rise in housing costs that affected senior renter households living in census metropolitan areas (CMAs) in Ontario, Saskatchewan, Alberta and British Columbia may have contributed to increasing the number of households in core housing need.
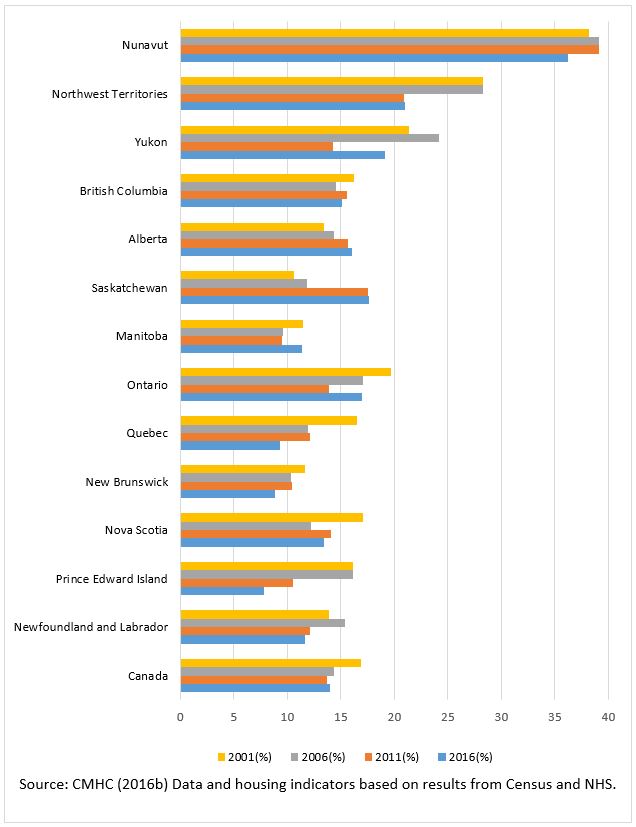
Figure 3 - Text version
Percentage of Senior Households in Core Housing Need in Canada and in each of the provinces and territories. Based on CMHC data from four census years: 2001, 2006, 2011 and 2016.
| Jurisdiction | 2001 | 2006 | 2011 | 2016 |
|---|---|---|---|---|
| Canada | 14.0 | 13.7 | 14.4 | 16.9 |
| Newfoundland and Labrador | 11.6 | 12.1 | 15.4 | 13.9 |
| Prince Edward Island | 7.8 | 10.5 | 16.1 | 16.1 |
| Nova Scotia | 13.4 | 14.1 | 12.2 | 17.1 |
| New Brunswick | 8.8 | 10.4 | 10.3 | 11.6 |
| Quebec | 9.3 | 12.1 | 11.9 | 16.5 |
| Ontario | 17.0 | 13.9 | 17.1 | 19.7 |
| Manitoba | 11.4 | 9.5 | 9.6 | 11.5 |
| Saskatchewan | 17.6 | 17.5 | 11.8 | 10.6 |
| Alberta | 16.0 | 15.7 | 14.4 | 13.4 |
| British Columbia | 15.1 | 15.6 | 14.5 | 16.2 |
| Yukon | 19.1 | 14.3 | 24.2 | 21.4 |
| Northwest Territories | 21.0 | 20.9 | 28.3 | 28.3 |
| Nunavut | 36.2 | 39.1 | 39.1 | 38.2 |
5. Seniors in core housing need in Canada in 2016
According to the 2016 census (Table 1), almost a quarter of seniors lived below standards, for example. either not adequate, suitable or affordable (24.9%) regardless of their housing arrangement. Individually or in combination, affordability issues were most common (19.4%) followed by adequacy issues (4.6%) and then suitability issues (2.6%). Core housing need (42.8%) and in particular affordability (39.7%) issues were common in households of seniors living alone. Single seniors living with their offspring, other relatives or non-relatives had higher rates of adequacy and suitability concerns (Table 1).
| Housing arrangement | Number in 2016 Census | Adequacy issue (does not need major repairs) | Suitability issue (enough bedrooms) | Affordability issue (<30% before tax income) | Living below standards |
|---|---|---|---|---|---|
| Any | 5,379,270 | 4.6% | 2.6% | 19.4% | 24.9% |
| Senior living alone | 1,398,540 | 5.4% | N/A | 39.7% | 42.8% |
| Seniors living in private households of 2 or more persons | 3,980,725 | 4.4% | 3.5% | 12.2% | 18.6% |
| Senior couple living alone | 2,934,225 | 3.5% | 1.1% | 11.8% | 15.6% |
| Senior couple living with son or daughter | 422,170 | 5.5% | 6.0% | 10.0% | 19.6% |
| Solitary senior living with son or daughter | 247, 690 | 8.7% | 10.3% | 17.8% | 32.0% |
| Solitary senior with other relative or non-relative | 376,635 | 6.7% | 15.1% | 14.5% | 31.2% |
- Source: Statistics Canada (2016)
In contrast to Table 1 where seniors live in a household where the person who maintains it might be a senior or non-senior, in Table 2 the focus is only on senior-led households thus explaining the difference in numbers and percentages. In 2016, Saskatchewan was the province with the highest percentage of senior-led households in core housing need. Ontario, however, had many more households with core housing need, accounting for almost 46% of all core housing need in Canada. Among the territories, Nunavut had the highest percentage of senior-led households in core housing need reflecting longstanding shortages and the high cost of housing (Figure 3 and Table 2).
| Geography | Total households led by seniors | Households in core housing need | |
|---|---|---|---|
| Total numbers | Total numbers | Percentage | |
| Canada | 3,399,250 | 477,025 | 14.0% |
| Newfoundland and Labrador | 61,220 | 7,115 | 11.6% |
| Prince Edward Island | 16,615 | 1,300 | 7.8% |
| Nova Scotia | 113,115 | 15,115 | 13.4% |
| New Brunswick | 89,125 | 7,825 | 8.8% |
| Quebec | 881,315 | 81,950 | 9.3% |
| Ontario | 1,275,165 | 217,305 | 17.0% |
| Manitoba | 115,475 | 13,210 | 11.4% |
| Saskatchewan | 97,515 | 17,130 | 17.6% |
| Alberta | 271,670 | 43,580 | 16.0% |
| British Columbia | 472,660 | 71,285 | 15.1% |
| Yukon | 2,540 | 485 | 19.1% |
| Northwest Territories | 2,020 | 425 | 21.0% |
| Nunavut | 815 | 295 | 36.2% |
- Source: CMHC (Census-based housing indicators and data)
Data from the 2016 census found that senior-led households in CMAs were more likely to be in core housing need than those in small towns and rural areas (non-CMA/Census Agglomeration (CAs)). Vancouver and Toronto were the two major metropolitan areas with the highest rates of senior-led households in core housing need (Table 3a).
| Item | Geography | Senior-led households | Households in core housing need | |
|---|---|---|---|---|
| Total numbers | Total numbers | Percentage | ||
| 1 | Canada | 3,399,250 | 477,025 | 14.0% |
| 2 | Total-Non-CMA/CA Canada | 682,380 | 72,770 | 10.7% |
| 3 | All CA Total Canada | 496,905 | 46,325 | 9.3% |
| 4 | Total- CMA Canada | 2,219,970 | 357,910 | 16.1% |
| 5 | St. John's | 18,350 | 2,920 | 15.9% |
| 6 | Halifax | 38,755 | 6,060 | 15.6% |
| 7 | Moncton | 15,080 | 1,480 | 9.8% |
| 8 | Saint John | 13,540 | 1,070 | 7.9% |
| 9 | Saguenay | 20,075 | 360 | 1.8% |
| 10 | Québec | 91,655 | 9,135 | 10.0% |
| 11 | Sherbrooke | 24,400 | 770 | 3.2% |
| 12 | Trois-Rivières | 20,230 | 340 | 1.7% |
| 13 | Montréal | 396,505 | 53,735 | 13.6% |
| 14 | Ottawa – Gatineau | 114,915 | 16,140 | 14.0% |
| 15 | Kingston | 18,655 | 2,670 | 14.3% |
| 16 | Belleville | 12,365 | 1,950 | 15.8% |
| 17 | Peterborough | 15,535 | 2,430 | 15.6% |
| 18 | Oshawa | 32,205 | 5,400 | 16.8% |
| 19 | Toronto | 458,885 | 107,195 | 23.4% |
| 20 | Hamilton | 79,200 | 11,360 | 14.3% |
| 21 | St. Catharines - Niagara | 52,905 | 7,065 | 13.4% |
| 22 | Kitchener - Cambridge - Waterloo | 43,180 | 6,790 | 15.7% |
| 23 | Brantford | 13,825 | 2,150 | 15.6% |
| 24 | Guelph | 13,220 | 1,955 | 14.8% |
| 25 | London | 51,470 | 6,965 | 13.5% |
| 26 | Windsor | 34,670 | 3,455 | 10.0% |
| 27 | Barrie | 15,710 | 2,845 | 18.1% |
| 28 | Greater Sudbury / Grand Sudbury | 18,610 | 2,680 | 14.4% |
| 29 | Thunder Bay | 14,900 | 1,920 | 12.9% |
| 30 | Winnipeg | 71,715 | 9,025 | 12.6% |
| 31 | Regina | 19,755 | 3,280 | 16.6% |
| 32 | Saskatoon | 22,475 | 3,575 | 15.9% |
| 33 | Lethbridge | 10,595 | 1,255 | 11.8% |
| 34 | Calgary | 83,250 | 14,155 | 17.0% |
| 35 | Edmonton | 90,610 | 15,350 | 16.9% |
| 36 | Kelowna | 21,565 | 2,405 | 11.2% |
| 37 | Abbotsford - Mission | 15,050 | 2,010 | 13.4% |
| 38 | Vancouver | 210,595 | 41,575 | 19.7% |
| 39 | Victoria | 45,520 | 6,440 | 14.1% |
- Source: CMHC (Census-based housing indicators and data)
| Item | Geography | Senior-led households | Households in core housing need | |
|---|---|---|---|---|
| Total numbers | Total numbers | Percentage | ||
| 1 | Canada | 3,399,250 | 477,025 | 14.0% |
| 2 | Charlottetown | 7,320 | 485 | 6.6% |
| 3 | Whitehorse | 1,955 | 340 | 17.4% |
| 4 | Yellowknife | 660 | 120 | 18.2% |
| 5 | Iqaluit | 145 | 30 | 20.7% |
- Source: CMHC (Census-based housing indicators and data)
As discussed in the next section, Beyond Seniors Core Housing Need, this report also outlines rental/housing costs as an issue to consider.
Those living in core housing need tend to have significantly lower average incomes. Senior women are more likely to live alone and have low incomes and therefore are more likely to live in core housing need. In fact, in 2016, 57.4% of seniors living in core housing need consisted of women who lived alone (Table 4). Additionally, in 2016, most seniors with core housing need lived in apartments and were renters (Table 5, Canada Mortgage and Housing Corporation, 2016b).
| Household Type | Total - households led by senior | Households in core housing need | |
|---|---|---|---|
| Total numbers | Total numbers | Percentage | |
| All senior-led households | 3,399,260 | 477,030 | 14.0% |
| Senior female, one-person households | 938,030 | 256,535 | 27.3% |
| Senior male, one-person households | 428,810 | 100,075 | 23.3% |
| Senior households consisting of a couple without children | 1,458,710 | 64,880 | 4.4% |
| Senior households consisting of a couple with children | 226,490 | 10,745 | 4.7% |
| Senior households consisting of female lone-parent family | 167,525 | 26,330 | 15.7% |
| Senior households consisting of male lone-parent family | 48,150 | 6,375 | 13.2% |
| Other types of households | 131,545 | 12,090 | 9.2% |
- Source: CMHC (Census-based housing indicators and data)
| Ownership Type | All senior households | Senior households in core housing need | |
|---|---|---|---|
| Total numbers | Percentage | ||
| Total – Tenure | 3,399,250 | 477025 | 14.0% |
| Owned | 2,538,030 | 194705 | 7.7% |
| Rented | 861,225 | 282320 | 32.8% |
6. Beyond seniors core housing need
In this part of the report, the analysis goes beyond the criteria used by CMHC to define affordability, suitability and adequacy to consider supply, appropriately designed seniors’ rental housing and collective housing that offers limited forms of care and the particular needs of seniors with disabilities. It also addresses issues of safety, adaptability and environmental sustainability.
Affordability
As noted previously, the affordability criterion for core housing need is defined by a shelter-cost-to-gross income ratio of less than 30%. While not directly related to core housing need, there are many extra costs that seniors may bear, especially those seniors with chronic health conditions and functional limitations requiring some assistance in usual daily activities. Out of pocket health expenses are higher for seniors and they are more likely to incur some costs for assistance in activities of daily living. This financial burden is augmented by the fact that generally retirement is associated with a reduction in disposal income and in non-durable consumption (MacDonald, Andrews and Brown 2008).
Appropriately designed, suitably located, and affordable rental housing represents an important housing option for seniors who are either unable to afford or are uninterested in personal home ownership. However, the supply of affordable, suitable and adequate rental housing in Canada has dwindled as the private sector has shifted focus, and as governments have reduced their investment in social housing. However, since 2010, there has been an increase in the number of rental unit starts as a percentage of all housing starts across Canada. In the last year for which annual data were available (2016), the number of rental unit starts across Canada was 36,574 or 20.2% of all starts according to CMHC’s 2017 Canadian Housing Observer. While there is no agreed upon optimal mix of housing and rental units, one widely held view is that the lack of supply of rental units is driving up the cost of existing units and driving down vacancy rates in many communities across the country (FCM 2014.)
The current short-term positive trend in the number of rental unit starts should, however, be viewed with caution for two reasons. First, the number of overall starts has been highly variable over the years, not necessarily reflecting the growth in the population of Canada or demand for housing of all types (see Figure4). Second, there is a great deal of variability in local housing markets. For example, in the Toronto CMA, the number of rental unit starts as a percentage of all starts was only 8.8%. In Vancouver the number of rental unit starts as a percentage of all starts was 27.4% and in the Montreal CMA, the number of rental unit starts as a percentage of all starts was 43.8% in 2018 (CMHC Starts and Completions Survey accessed January 2019).
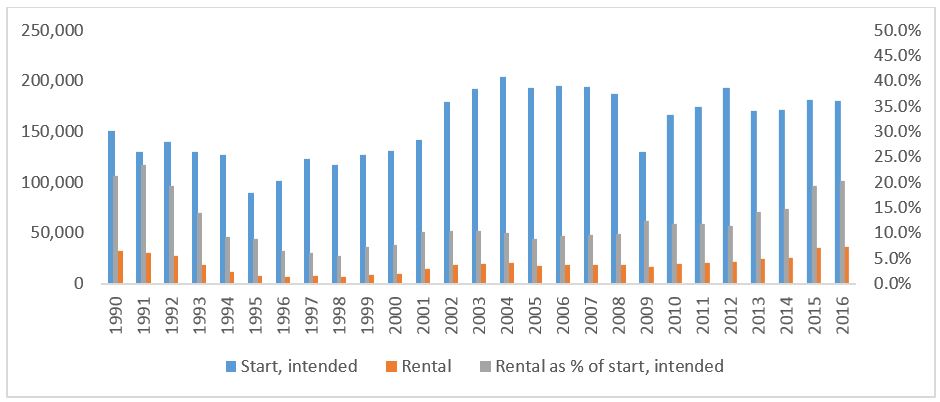
Figure 4 - Text version
Total number of housing construction starts, rentals and rentals as a percentage of total housing construction starts from 1990 to 2016 based on data from the Canada Mortgage and Housing Corporation.
| Year | Construction starts by intended market | Rentals | Rental as a percent of all construction starts |
|---|---|---|---|
| 1990 | 150,620 | 32,201 | 21.4% |
| 1991 | 130,094 | 30,495 | 23.4% |
| 1992 | 140,162 | 27,197 | 19.4% |
| 1993 | 129,988 | 18,193 | 14.0% |
| 1994 | 127,346 | 11,698 | 9.2% |
| 1995 | 89,526 | 7,998 | 8.9% |
| 1996 | 101,804 | 6,643 | 6.5% |
| 1997 | 123,221 | 7,559 | 6.1% |
| 1998 | 116,793 | 6,531 | 5.6% |
| 1999 | 127,103 | 9,276 | 7.3% |
| 2000 | 131,052 | 10,155 | 7.7% |
| 2001 | 142,280 | 14,681 | 10.3% |
| 2002 | 179,124 | 18,841 | 10.5% |
| 2003 | 191,911 | 19,939 | 10.4% |
| 2004 | 204,389 | 20,343 | 10.0% |
| 2005 | 193,471 | 17,210 | 8.9% |
| 2006 | 195,024 | 18,518 | 9.5% |
| 2007 | 193,744 | 18,605 | 9.6% |
| 2008 | 187,368 | 18,265 | 9.7% |
| 2009 | 130,369 | 16,237 | 12.5% |
| 2010 | 166,175 | 19,735 | 11.9% |
| 2011 | 174,351 | 20,721 | 11.9% |
| 2012 | 193,563 | 21,990 | 11.4% |
| 2013 | 170,134 | 24,267 | 14.3% |
| 2014 | 171,843 | 25,308 | 14.7% |
| 2015 | 181,597 | 35,136 | 19.3% |
| 2016 | 180,647 | 36,574 | 20.2% |
- Source: CMHC (2017) Canadian Housing Observer (downloaded 17 January 2019)
The combination of a rapidly expanding seniors’ population, limited investment in private purpose-built rental housing, and progressively declining government-funded social housing in most provinces from the mid-1990s until recently has resulted in long and growing wait lists for social housing and housing subsidies. In Ontario alone, the number of households waiting for rent-geared-to-income housing in 2015 was 171,360 and the seniors’ share of the wait list was 32%, up from 22% in 2003 (Monsebraaten, 2016). Ontario’s Housing Services Corporation (HSC) also estimates that one-quarter of all households on Ontario’s social housing wait lists are led by seniors, reaching as high as 50% in some communities (HSC, 2012).
Another indicator of the relationship between supply, demand and cost of rental housing for seniors can be found in Table 6, from the CMHC Seniors Housing Survey as reported in the Canadian Housing Observer (downloaded 17 January 2019). The table shows the number of standard spaces, the vacancy rate of standard spaces and the average rent for standard spaces (Table 6)Footnote 5. In 2016, 179,676 rental units were defined as standard spaces by CMHC with Québec having almost double the number of standard spaces compared to Ontario, and Newfoundland having more standard spaces than any other province in Atlantic Canada. Ontario has the second highest vacancy rate of standard spaces while Québec has the third lowest vacancy rate of standard spaces and Newfoundland has the highest vacancy rate of standard spaces. While Ontario has the highest average rent for standard spaces, British Columbia has the second lowest average rent for standard space.
Table 6: The number, vacancy rate and average rent for standard spaces in Canada and the Provinces, 2018.
| Area | Standard spaces | Vacancy rate of standard spaces (%) | Average rent for standard bachelor/private rooms with meals included in rent ($) |
|---|---|---|---|
| CanadaFootnote 6 | 185,088 | 8.2 | 2,320 |
| Newfoundland and Labrador | 1,547 | 20 | 2 772 |
| Prince Edward Island | 584 | 8.4 | 3 339 |
| Nova Scotia | 1,216 | 6.2 | 2 946 |
| New Brunswick | 2,117 | 9.3 | 2 654 |
| Quebec | 99,329 | 6.9 | 1 643 |
| Ontario | 43,983 | 10.4 | 3 038 |
| Manitoba | 4,022 | 4.8 | 2 212 |
| Saskatchewan | 5,099 | 15.4 | 2 749 |
| Alberta | 8,213 | 15.4 | 2 780 |
| British Columbia | 18,978 | 3 | 2 250 |
- Source: CMHC (2018) Canadian Housing Observer (downloaded 27 March 2019)
Collective dwellings intended for seniors, including seniors’ residences and LTC facilities, are an essential but costly component of the housing continuum, intended for older Canadians experiencing serious and often chronic limitations in health or mobility. Addressing the need for affordable housing that offers varying levels of support is one of the most pressing challenges facing governments today. The 2016 Census counted 455,690 seniors ages 65 and over or 6.8% of all seniors living in collective dwellings (the vast majority of which were health care and related facilities). Of this number, 163,300 lived in residences for senior citizens, 156,915 lived in nursing homes, 82,360 in facilities that were a mix of nursing home and residence for seniors and 12,955 lived in other forms of residential care facilities.
The proportion of seniors living in a collective dwelling has been declining in Canada over the last 30 years.
Suitability (including disabilities and mobility impairment)
As per the CMHC definition, suitability is determined based upon whether the dwelling had enough bedrooms according to the household’s size and composition. Using this definition, the incidence of suitability problems is relatively low for seniors, unless the senior is sharing a household other than as part of a couple (Table 1) where it rises up to 15.1%.
From the integrated housing needs perspective, even though many provinces allow certain rental housing stock to be designated specifically for older adults as “seniors’ housing”, there may be few if any requirements for seniors’ rental housing to be legitimately designated to accommodate seniors. As a result, a growing number of these apartment buildings or complexes are actually not meeting the physical needs of many older adults (particularly those older adults with some degree of physical impairment). A study of rental housing units built for seniors use within Nova Scotia in the last decade under an Affordable Housing Initiative noted the following concerns by seniors: lack of shared space for social interaction; absence of accessibility and adaptive feature; and issues of difficulties with transportation and accessing usual amenities (Leviten-Reid and Lake 2016).
Adequacy
CMHC housing adequacy is assessed based on the dwelling condition not being reported in need of major repairs. Solitary seniors living with offspring or other relatives or non-relatives were most likely to have higher reported adequacy issues (Table 1). Taking into account integrated housing needs, housing might also be considered inadequate if it requires major adaptations to meet the needs of seniors as disabilities increase with age (Figure 5, Tables 7, 8, 9). Table 7 also highlights how ageing increasingly becomes the explanation for activity limitations with age, while Tables 8 and 9 highlight that, regardless of the reasons for a person’s disability, as they age, they are more likely to find that their disability creates difficulties for them and that they need help (Table 9). Without informal and formal support (for example, homecare), and housing adaptations, older people with disabilities are among those who are most likely to want or will need to find alternative forms of housing.
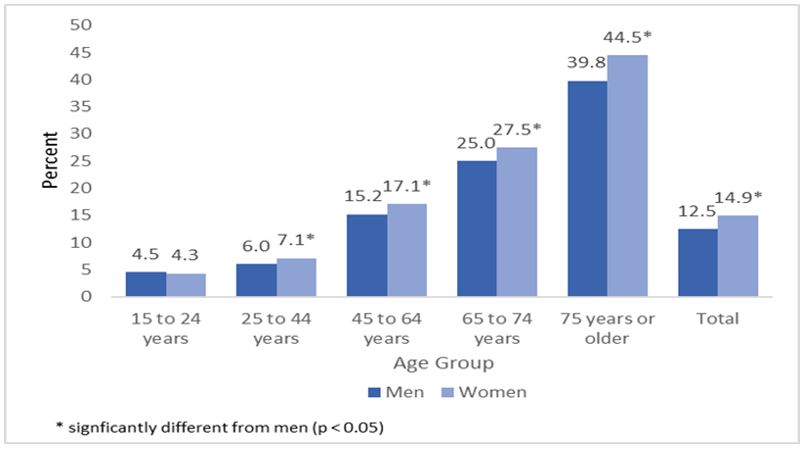
Figure 5 - Text version
The frequency of disability expressed as a percentage of the total population of men and women in age groups.
| Age group | Men | Women |
|---|---|---|
| 15 to 24 years | 4.5% | 4.3% |
| 25 to 44 years | 6.0% | 7.1% |
| 45 to 64 years | 15.2% | 17.1% |
| 65 to 74 years | 25.0% | 27.5% |
| 75 years or older | 39.8% | 44.5% |
| Total | 12.5% | 14.9% |
| Cause of limited activity | Injury | Disease or illness | Ageing | Existed at birth | Work conditions | Other | Total number |
|---|---|---|---|---|---|---|---|
| Age | Percentage | Percentage | Percentage | Percentage | Percentage | Percentage | |
| 45 to 49 years | 28.5 | 26 | 13 | 8.6 | 11.2 | 12.7 | 713,035 |
| 50 to 54 years | 25.5 | 28.4 | 17.6 | 7.7 | 11.4 | 9.4 | 969,889 |
| 55 to 59 years | 24.3 | 29.8 | 20.3 | 7.7 | 10.5 | 7.3 | 1,004,647 |
| 60 to 64 years | 22 | 31 | 24.7 | 6.6 | 9.8 | 5.9 | 942,339 |
| 65 to 69 years | 16.6 | 33.2 | 30.4 | 4.9 | 9.3 | 5.6 | 776,546 |
| 70 to 74 years | 13 | 33.1 | 37.9 | 4.5 | 7.6 | 3.9 | 595,234 |
| 75 to 79 years | 10.8 | 30.4 | 44 | 4.5 | 6.3 | 4 | 499,605 |
| 80 years or more | 8.9 | 25.6 | 56.1 | 2.4 | 3.9 | 3.1 | 72,5830 |
| Total | 22.3 | 26.9 | 20.3 | 10.3 | 8.5 | 11.6 | 9,464,804 |
- Source: Statistics Canada (2013/2014). Canadian Community Health Survey
| Do you have difficulty with activities | Sometimes | Often | Never | Total number |
|---|---|---|---|---|
| Age | Percentage | Percentage | Percentage | |
| 45 to 49 years | 15.1 | 7.5 | 77.4 | 2,332,300 |
| 50 to 54 years | 17.3 | 11.1 | 71.6 | 2,703,641 |
| 55 to 59 years | 20.1 | 12.3 | 67.6 | 2,573,686 |
| 60 to 64 years | 22.7 | 14.6 | 62.7 | 2,178,169 |
| 65 to 69 years | 23 | 15.3 | 61.7 | 1,818,742 |
| 70 to 74 years | 25.4 | 16.1 | 58.5 | 1,298,506 |
| 75 to 79 years | 26.7 | 22.8 | 50.5 | 942,513 |
| 80 years or more | 27.8 | 33 | 39.2 | 1,125,608 |
| Total | 15.7 | 9.4 | 74.9 | 29,967,274 |
- Source: Statistics Canada (2013/2014) Canadian Community Health Survey
| Help needed for tasks | Total | ||
|---|---|---|---|
| Yes | No | Number | |
| Age | Percentage | Percentage | |
| 45 to 49 years | 6.6 | 93.4 | 2,333,347 |
| 50 to 54 years | 9.5 | 90.5 | 2,705,375 |
| 55 to 59 years | 10.1 | 89.9 | 2,573,467 |
| 60 to 64 years | 10.2 | 89.8 | 2,180,032 |
| 65 to 69 years | 11.9 | 88.1 | 1,819,689 |
| 70 to 74 years | 15.5 | 84.5 | 1,298,557 |
| 75 to 79 years | 23.2 | 76.8 | 944,302.4 |
| 80 years or more | 44 | 56 | 1,128,743 |
| Total | 9.5 | 90.5 | 29,948,569 |
- Source: Statistics Canada (2013/2014) Canadian Community Health Survey.
Accessibility, adaptability, environmental sustainability and safety
Aging, disability and housing can also be linked to accessibility, adaptability, environmental sustainability and safety. One-quarter of Canadian seniors report they often have difficulty with one or more activities including hearing, seeing, communicating, walking, climbing stairs, bending, learning or other similar activities. A number of these functional limitations are potentially mitigated through environmental changes and adaptations (Hans-Werner et al 2009; Park, Han, Kim, & Dunkle, 2015).
Housing often lacks basic consideration of good environmental design (steps, ramps, railing, lighting, safety features, etc.) and location relative to the kinds of services that seniors commonly need. Seniors’ housing built between the 1960s and 1990s is now often unable to accommodate newer independence technologies such as motorized scooters and bulky electric wheelchairs that need to be plugged in.
Aging in place includes making sure the environment, especially the home, is functional and meets the changing needs of seniors (HomeStars, 2017). Home renovations and adaptions can be implemented to improve safety and accessibility. Modifications can enhance seniors overall functioning and well-being (Boland et al., 2017). Home modifications might be effective in helping seniors age at home and may prevent the need to move to other locations.
The 2012 General Social Survey (GSS) on Caregiving and Care Receiving provides a picture of the general adequacy of senior’s households regarding accessibility and adaptations (CMHC, 2017 Research Insight July).
- About one quarter (24%) of households and one third (32%) of senior households had an accessible entrance, with either a level, no-step entrance or a ramp. A large proportion of survey respondents 65 years and older claimed their homes had doorways wide enough for a wheelchair (70%), easy-to-open doors including lever handles (53%) and grab bars in the bathroom (41%)
- Seniors’ apartments, whether in low-rise or high-rise buildings, were much more likely than detached, semi-detached or row houses to have an accessible entry, and also to have other accessibility features. About 19% of seniors in single-detached dwellings reported having accessible entries compared to 33% of those in multi-unit dwellings, 62% in low-rise apartments and 89% in high-rises
- More than half (55%) of seniors requiring a wheelchair, mechanical support or aid from other people as a result of mobility limitations lacked an accessible entrance in their homes
- Seniors who recently moved were more likely to have accessible features in their homes. For example, 58% of recent movers (in residence less than one year) had an accessible entrance compared to 26% of those who had been in their homes for 10 or more years
Certain assistive technologies, such as motorized scooters, can also help seniors age in place by allowing them to remain in their homes as long as possible. Home technology can support aging in place by assisting seniors with functional impairments, communication challenges or need for monitoring of chronic diseases (Peek et al., 2014). Technology has also been shown to help alleviate social isolation, depression, anxiety and loneliness. However, individuals’ use and acceptance of technology to support aging in place varies. Overall, seniors express several concerns with using home technology to help facilitate aging in place (Peek et al., 2014). For example, they report concerns about cost, difficulty in its use, false alarms and forgetting or losing portable technology (Peek et al., 2014). Furthermore, seniors might view use of technology as an indicator for decline in function (Reeder et al., 2013).
7. The meaning of “home” and “age friendly communities”
It is important to understand the meaning of home from a senior’s perspective in order to inform service providers and stakeholders in responding to integrated housing needs. For example, an age-friendly pilot project in Québec conducted focus groups with seniors, caregivers, and service providers to better understand the meaning of “home.” (Bigonnesse & Beaulieu & Garon, 2014). They considered three aspects of the home: 1) the physical factors that include the physical components of the house and the community, 2) the social factors that includes the home as a place for socialization; and 3) the individual factors, that include behavioural, cognitive and emotional aspects. Physical aspects of the home and lack of access to affordable housing services and resources was a concern among seniors who participated in this pilot project. It was important for seniors to perceive the setting of their homes as safe, and that they could be gradually adapted or modified as they age. Findings showed that seniors preferred to live in a safe community near services and amenities such as grocery stores and health clinics (Bigonnesse et al., 2014). In a 2017 research study conducted in Edmonton, Alberta, the research showed that low-income immigrants and refugees between the ages of 55 and 92 would prefer to live within walking distance to grocery stores, pharmacies, medical clinics, amenities, and social activities in their community. Furthermore, they did not want to live near a commercial area, an industrial area or bars as they would not feel safe. Several also mentioned willingness to live near a shopping mall to help them stay mobile (Keenan, 2017). Another study also showed that it is also important for low-income seniors to live in walking distance to a grocery store, their doctor, a pharmacy and a bus stop (Barrett, 2013).
In relation to the social aspects of the home, seniors felt it was important to have social connections with their neighbours and other community members. Age-Friendly Communities (AFCs) should therefore promote public gathering spaces for seniors such as senior community centres. Seniors also preferred to live in spaces of appropriate sizes where they can socialise and gather with friends and families (Bigonnesse et al., 2014). The Bigonnesse et al. study also showed that seniors pride themselves in completing daily activities and taking care of their home. Thus, it is important for AFCs to promote home maintenance services that are accessible and affordable (Bigonnesse et al., 2014).
8. Selected Canadian initiatives
8.1 Housing options
There are various types of existing housing options available to meet the integrated housing needs of seniors in Canada including: Mainstream Housing, Naturally Occurring Retirement Communities, Independent Living and Active Lifestyle accommodation (inclusive of home share, life lease, cooperatives and flex housing), Assisted Living / Supportive Housing accommodation, and Seniors Residential and Long-Term Care accommodations) (Ministry of Municipal Affairs and Housing, 2014; Hashim et al., 2014). These options are described below with examples.
- Mainstream housing is a housing model where seniors stay in their usual homes or downsize to ground-oriented options (for example, one-level floor plans usually on a ground level), apartments or condominiums which are not specifically intended for seniors. These dwellings are generally at the market rate. An example of a modified housing model is in La Crete, Alberta, where bungalows are designed specifically for seniors. They have wider doors and a walk-in shower stall and are priced at the lower end of the market rate (Hashim et al., 2014).
- Naturally Occurring Retirement Communities (NORCS) are examples of mainstream housing that are not specifically built for seniors but have a large proportion of senior residents. The term NORC was coined in the United States in the early 1980s to describe a geographic area that has naturally developed a high concentration of older residents. This phenomenon is due to seniors remaining in their own homes as they age, or because they have congregated to an area after retirement or downsizing. The NORC-Supportive Service Program (NORC-SSP) model was developed in United States to wrap around these naturally occurring groups of seniors, and to help them remain living independently for as long as possible (Bedney et al., 2010). They offer supportive services in the home or immediate community, which address the social determinants that are not typically managed through government programs: social connections and supports; care navigation; nutrition and exercise, among others. While the model does provide some direct health care services, it is largely a preventative health model with the goal of increasing access to ancillary supports that slow down the need for more extensive home care, at the same time as providing opportunities for seniors to meaningfully participate in their communities.
OASIS Senior Supportive Living Inc. in Kingston, Ontario, is an example of a NORC SSP. OASIS was established by a grassroots group of seniors as tenants in an ordinary apartment building of mid-range rent in the Kingston area market. This regular rental apartment building had a high proportion of units occupied by seniors. With a small but growing number of frail seniors, they co-created a partnership model between seniors, the landlord and the South East Ontario Local Health Integration Network (LHIN). The landlord agreed to provide and modify space within the building for a common dining and recreational space for use by seniors and supported by voluntarism by seniors. Funding was provided by the South East Ontario LHIN to provide onsite coordination of supportive services tailored to what the seniors needed and wanted to enable them to stay in their homes and age in place. - Independent living and active lifestyle accommodation are a seniors-only housing option that combines accommodations and amenities. These can vary from single detached homes to apartment buildings. An example of an independent living accommodation is shared home ownership where a house is shared among individuals each with their own room and share common areas such as the kitchen. This type of housing allows seniors to remain in their communities and be surrounded by friends and families. Services can also be provided at lower costs due to the efficiency of multiple seniors in one home. An example of this type of housing is Solterra Co-housing in Bracebridge, Ontario where four to six seniors share ownership of a home and each home has a staff member that provides meal preparation, shopping, and housekeeping.
- Another example of independent living accommodation is a not-for-profit housing option called Abbeyfield houses, whish is a form of co-housing in which residents live in one house and each have their own room and bathroom but share common areas. This type of housing is generally for low-income seniors since the house is run on a not-for-profit basis. There are Abbeyfield houses in Caledon and Ottawa, Ontario where a manager does regular cleaning and maintenance, prepares meals, and provides support to residents. The rent each month covers the cost for accommodation, utilities and meals (Hashim et al., 2014).
- Life lease housing is another independent living housing option in Canada that is usually managed by non-profit organizations and is specifically for seniors who can live independently (Ontario Ministry of Municipal Affairs and Housing, 2014). Life lease units can be houses or apartments and are generally priced lower than others in the area. There are several types of life lease agreements. These agreements are governed by contract law which may vary from province to province. Seniors first pay an entrance fee to the landlord or trustee to become a tenant of a life lease unit and then pay a monthly maintenance fee. In some instances, a redemption fee is payable to the estate at the time the life lease ends. Seniors typically choose this housing option due to affordability, low maintenance, and access to services offered by the non-profit organizations. With life leasing, seniors do not own the property but have the right to own the housing unit (Ontario Ministry of Municipal Affairs and Housing, 2014).
- Supportive housing housing options that often include design features for safety and accessibility, as well as providing support services such as counselling, personal support and assistance with medication, recreational activities, housekeeping, and meal preparation. It is important to note that the terminology used to define supportive housing varies widely across Canada (for example, planners in British Columbia use the term ‘assisted living’ as equivalent to supportive housing in Manitoba; while in Alberta these dwellings are called residential facilities, in Ontario Long Term Care Homes, a term used elsewhere to define Personal Care Homes or Nursing Homes).
Data from Statistics Canada’s 2007 General Social Survey (GSS) showed that about 7% of seniors live in supportive housing. Of those aged 45+, 62% said they would consider moving into supportive housing later in life (Canada Mortgage and Housing Corporation, 2016c). Data also showed that renters aged 75+ were more interested in supportive housing than homeowners.
A study of supportive housing use in Winnipeg, Manitoba noted that 10% of new admissions to Personal Care Homes (PCH) (nursing homes) were similar in terms of functional needs to new admission to supportive housing (Doupe et al., 2016). The supportive housing tenants typically received: help with meals, laundry, and light housekeeping; 24-hour on-site access to assistance to complete personal tasks like bathing, dressing, and grooming; and some (but not 24-hour) professional home care services as deemed to make them eligible by the home care program. The primary difference between the PCH residents was they had lower income, or their informal caregivers had health challenges themselves. In terms of government/health region contributions, the median annual cost for a resident in a PCH was $45,348 vs in supportive care of $14,400. The cost to the resident in a PCH was $15,444 vs $19,500 for a supportive housing tenant. This suggests that removing cost disincentives for the supportive housing tenant and family may potentially avoid or delay the need for a more expensive PCH placement in some instances.
Residence Parc Jarry in Montreal, Quebec is an example of supportive housing where a private developer converted an abandoned home to a residence for seniors. Half of the units are below the market rate and the other half are at the market rate. This is an example of how current houses can be converted to affordable housing for seniors (Hashim et al., 2014).
In an Alberta study, residents living in a senior supportive housing facility located on the Red Deer College Campus in Red Deer were asked to rate their satisfaction with the built environment. The residents particularly valued design features that accommodated mobility devices and having accessible showers which helps them maintain their functional independence. However, respondents were not as satisfied with the lighting of the built environment. Many of the respondents lived in the community near the facility previously and had family members that live close to the facility so were able to preserve social networks.
Other examples of creating a supportive living model without relocation include the Georgian Village in Simcoe County, Ontario, which offers a continuum-of-care campus to enable residents to move between levels of care without having to move to a new facility if their care needs change. In addition to providing a variety of housing options, there is a strong focus on socialization, a flexible series of support options, promoting of voluntarism and a readily accessible community hub with a range of amenities including a health clinic, pharmacy, fitness centre, library, chapel, recreational areas, bistro and shops.
The Assisted Living Southwest Ontario’s (ALSO) model is a “hub and spoke” model. ALSO offers a basket of supports for daily living to clients living in several supportive housing sites across Windsor (for example, “hubs”), as well as individuals in their own homes within a given geographic radius from the supportive housing sites (for example, spokes). ALSO locates staff in each of the hubs to flexibly support clients, with 24/7 availability.Footnote 7 - Retirement residences are usually privately owned, and residents are responsible for all or most costs. Accommodation in most retirement residences includes different sized units and common areas, which include a dining room and lounge. Residences that are targeting more affluent seniors may include other amenities such as recreational facilities, swimming pools, libraries, and gift shops. The Ultimate Goal Retirement Village in Lewisporte, Newfoundland is an example of an affordable retirement residence where all units are below the market rent and some units are funded by the Affordable Housing Program (AHP).
Seniors’ lodges offer rooms, meals, services and recreational opportunities for independent seniors. Community-based services may help offer these amenities and opportunities. The Seniors’ Lodge Program is unique to Alberta, and has been serving low-income seniors needing safe, suitable, and affordable accommodation for over 50 years. Each local housing provider sets their own lodge rates, and rates vary between regions. Regardless of the monthly lodge rate, each resident must be left with at least $315 in monthly disposable income. - Long-Term Care accommodation is a housing option for seniors who require 24-hour support and assistance in daily living activities as well as nursing supervision and care. Unlike many of the other housing options reviewed, it is generally the case that access to LTC homes requires an assessment through a provincial/territorial health system. Examples are individuals living with moderate to severe Alzheimer’s disease. LTC homes offer more personal care and support compared to that offered in retirement residences or supportive housing. There is generally a co-pay requirement for publicly-funded facilities. LTC homes are subject to government regulation and often require an operating license. Accommodation may be shared with more than two residents in a room or a private room.
8.2 Home modifications
In British Columbia, there is a Home Renovation Tax Credit for Seniors and Persons with Disabilities assists individuals 65 years or older and persons with disabilities with the cost of certain home renovations to improve accessibility and safety in the home.
British Columbia also offers the Rehabilitation Assistance Program On-Reserve, which provides financial assistance to Band Councils and Band members to repair substandard homes to a minimum level of health and safety and to improve the accessibility of housing for people with disabilities.
Alberta introduced the Seniors Home Adaptation and Repair Program (SHARP) in 2016. SHARP is a low-interest home equity loan program to help senior homeowners finance home repairs, adaptations and renovations. Examples include but are not limited to; plumbing, heating, electrical, tree removal, windows, roof repairs, widening doorways and stair lifts. SHARP allows seniors to use their home equity to remain in their homes and maintain their independence. Eligible seniors can apply for a low-interest home equity loan with the Government of Alberta to cover repairs, adaptations, and/or renovations to their primary residence. In addition to government programs to support home modifications, the private and non-private sector can provide new innovative opportunities to help older adults modify their homes to fit their changing needs as they age.
In New Brunswick, the Minor Home Repairs Grant is available to low-income residents over 65 years old, and offsets the cost of renovations focused on fall prevention, such as ramps and repairs to home entry, handrails, grab bars, improved lighting, non-slip and non-skid floor surfaces, and repairs to flooring.
In the United States, there are a number of programs that help reduce the cost of home modifications for older homeowners. For example, federally funded HOME or Community Development Block Grant programs provide loans for accessibility modifications. The U.S. Department of Agriculture also provides loans and grants for home modifications for rural owners aged 62 and over with very low income (Baker et al., 2014). There are also non-profit organizations such as Rebuilding Together that help low-income, older, and disabled homeowners maintain their homes through partners and volunteers (Baker et al., 2014). It is important to provide seniors with information on how renovations can benefit them in the future and on tax benefits that are available for aging in place renovations.
Tax credits can also be implemented for builders and homeowners to facilitate universal design features. For example, Ohio’s Livable Homes Tax Credit provides income tax credits to builders who construct accessible homes and to homeowners who add accessible features. At the federal level and in Ontario, governments had tax credits in place in the past but because of lack of uptake especially among low income seniors, the tax credits were ended.Footnote 8
At the local level, there are also examples of programs to encourage home modifications. In Vancouver, there is a building bylaw that requires all new housing to have various universal design elements. These include: a barrier-free or adaptable shower; wide stairs, halls, and doors; reachable switches and outlets; a fully accessible bathroom on the ground floor; installation of kitchen sink drainpipes at a lower height; and lever-style door handles (Baker et al., 2014). Additionally, the City of Ottawa has a home renovation program funded through the federal/provincial Investment in Affordable Housing (IAH) program that provides funding to low-income seniors to modify their homes (Federation of Canadian Municipalities, 2015).
Secondary Suites are an option available to homeowners to make use of property to create an income stream and create a housing option for seniors. They offer the opportunity for affordable accommodation to seniors in neighbourhoods where they might not otherwise be able to afford to live. For example, the City of Kingston, Ontario, has a grant program that helps homeowners with the costs of developing a secondary suite that is contingent on offering affordable rental space for a specified time (City of Kingston, 2018).
In Appendix B, there is a list of financial supports for home repair, renovations and adaptations.
8.3 Housing options for vulnerable seniors with dementia
Special consideration should be given to housing options for vulnerable seniors with dementia. The home environment can contribute to the overall well-being of vulnerable seniors living with dementia. When enhancing the comfort and quality of life among seniors with dementia, the environment should consider the physical, emotional, and psychosocial well-being of individuals (Canada Mortgage and Housing Corporation, 2014). Familiarity is also extremely important for people living with dementia since one of their coping mechanisms is to rely on familiar places and routines (Canada Mortgage and Housing Corporation, 2014).
In Canada, Adult Day Programs provide supervised recreation activities outside of a person’s home. The purpose of these programs is to help people with dementia remain connected in their community. They offer meals, assistance with daily living, transportation and dementia appropriate activities. Adult Day Programs may be collated within residential homes or long-term care facilities where access to some health care professional services may also be readily available (Canada Mortgage and Housing Corporation, 2014).
There are also various housing models to support seniors living with dementia, which include the Green House model, the Planetree Model, and GENTLECARE (Canada Mortgage and Housing Corporation, 2015). The Green House model combines small homes where care is provided by consistent staff in a family type setting. The Sherbrooke Community Centre in Saskatchewan is an example of this type of model. The Planetree Model focuses on a holistic approach that meets the needs of an individual’s body, mind, and spirit. Conventional medicine is combined with complementary therapies. The Donald Berman Maimonides Geriatric Centre in Quebec is an example of this type of model. Lastly, GENTLECARE supports the existing functional abilities of an individual rather than forcing the individual to adapt to new changes. Delta View Adult Day Program, Assisted Living and Life Enrichment Centre in British Columbia is an example of this type of model.
9. Selected international initiatives
9.1 Housing options
- Lifetime neighbourhoods: The United Kingdom has adopted the concept of Lifetime Neighbourhoods where the built environment is created in a way that is inclusive for people of all ages and abilities. These neighbourhoods offer a variety of services and aim to be accessible and safe (Harding, 2007). Although this concept has not yet been fully adopted in neighbourhood design, it has potential to promote the well-being and social inclusion for seniors
- Co-housing communities: In Denmark, the concept of co-housing communities was first established. The primary aim of this housing model is to promote social connectedness among residents to reduce loneliness (Pedersen, 2015; Brenton, 2017). This concept combines privacy with social interaction where members in the community support each other to encourage aging in place (Canadian Senior Cohousing Society, 2016). For example, members may choose to run errands together, cook together, or take walks together (Canadian Senior Cohousing Society, 2016). With co-housing communities, houses are built as clusters or single-story rows centred around shared spaces such as gardens and walkways. Residents collaborate with each other to manage activities and shared spaces. A Danish study found that residents made the decision to move to a co-housing facility because houses required less maintenance and the community promoted social connectedness. Results showed that 95% of residents were satisfied with their co-housing community (Pedersen, 2015)
- Producer driven / resident driven senior homes: In Finland, there are four senior housing concepts that either represent a producer driven or a resident driven approach. One article presented a comparative analysis of the four housing concepts (Pirinen, 2016). Aktiivikoti and the Virkkula Senior Village are housing concepts developed for seniors (producer driven) whereas Ars Longa and Loppukiri are developed by seniors (resident driven). Aktiivikoti are homes with added features that promote accessibility and safety. These features include: sound insulation, elevators with automatic doors, and fire alarms. The houses are also built near amenities, services, and public transportation (Pirinen, 2016). The Virkkula Senior Village is another housing concept for rural areas. Many senior houses are built in a village-like community and centred around a larger building that provides services and amenities to all residents. This model allows services to be delivered more efficiently due to the higher concentration of seniors in one area (Pirinen, 2016). Ars Longa is the third housing concept that is mainly targeted to specific professional groups such as artistic seniors or senior economists. The main distinguisher of Ars Longa is that the houses are rentals, which may be ideal for seniors with low or unstable income (Pirinen, 2016). Loppukiri is the final housing concept in which residents manage and provide services. The goals of this model are to promote social connectedness and to allow seniors to live in a more communal way (Pirinen, 2016)
- Apartments for Life: In the Netherlands, is an Apartments for Life concept where individuals and couples aged 55 and over can buy or rent units (Glass, 2014). Universal design is adopted in each unit and care is provided to individuals once they eventually require health related assistance. This model relies heavily on volunteering and as a result is 10% to 20% less expensive than institutional care. The housing model is specifically designed to prevent seniors from relocating even when their health starts to deteriorate as they age (Glass, 2014)
- Homeshare: In Europe, particularly France, Homeshare is an intergenerational housing option where a senior homeowner rents out a room to a younger individual at a very low cost (Garland, 2018). In exchange, the younger individual, typically a university student, supports the senior with daily tasks such as shopping, cooking, or cleaning. Evaluation of homeshares in Spain found that 93% of seniors and 99% of university students benefited from this living arrangement (Labit & Dubost, 2016)
- Villages: In the United States, there is a housing model known as “Villages” where volunteers and staff provide adults aged 50 and over with services such as transportation, grocery shopping, housekeeping, and referrals to community services. Membership is low cost and most villages provide subsidies to those of low-income. Furthermore, residents can benefit from villages while remaining in their own homes (Scharlach & Graham & Lehning, 2011). An example of this housing is the Village-to-Village network in Boston, Massachusetts where neighbourhoods contain a large proportion of seniors, with community supports that provide affordable services including transportation, home repairs, and medical care (Hashim, Pacini, Starr, SHS Consulting, & CBCL Limited, 2014)
9.2 Home modifications
A study in the UK analysed the effectiveness of home modifications and how people experience adaptations (Centre for Ageing Better, 2018). The decision to make home adaptations is often due to common triggers, including an event such as a fall. However, the need for home adaptations is often associated with vulnerability and loss of independence. Therefore, many seniors delay making modifications to their home until a specific event, such as a fall, occurs. There needs to be a wider understanding of the benefits of home modifications and encouragement of positive messaging surrounding home modifications to promote making changes earlier.
This study also found that there is a lack of knowledge on how to access home modifications, with many participants obtaining information from family members or friends with previous experiences. It was suggested that local services and health services collaborate to provide accurate and up to date information of locally available services and funding support. It was also found that the best outcomes are achieved when individuals, families, and caregivers are involved during the entire decision-making process of what individuals hope to achieve from home adaptations.
Participants in this study said that it took time to adjust to their new adaptations, but many expressed positive experiences. For example, one participant said, “It means independence. I don’t have to ask for help. I find it very hard to ask for help. I mean, everybody has got busy lives. They haven’t got time to be bothering on with you. If you can manage yourself, then it’s half the battle” (Centre for Ageing Better, 2018, p. 14). Another person stated, “In terms of there being a problem and in terms of me falling as much, I don’t fall so much now. It just gives away now and then, but because I’ve got all sorts of grab rails and things like that I’m able to cope a lot better” (Centre for Ageing Better, 2018, p. 14). It was also suggested government guidance be provided on outcome measures to better evaluate the impacts of home adaptations (Centre for Ageing Better, 2018).
9.3 Universal design
The design and planning of the built environment may augment or hinder how well the individual adapts to aging and age-related disease processes. The concept of universal design is to design an environment in a way that meets the needs of a wide range of individual needs (Persson et al., 2015). It aims to provide accessible features, without stigmatization, that can benefit everyone who uses the features (Carr, 2013). For the aging population, universal design can provide a barrier-free and accessible environment, which enhances their ability to perform daily activities independently (Crews & Zavotka, 2006). Examples of universal design features that help prevent falls and injuries include: grab bars in showers or tub, no slip flooring, and a no step door entry (Crews & Zavotka, 2006). Moving to or adapting one’s existing family home with universal design features can increase independence and promote aging in place.
New buildings and homes could be developed with standard requirements that enable aging in place, and governments could update policies regarding construction and housing regulations. A case study in Sweden analysed the living environment of rental senior apartments and found that living spaces with a low universal design score were associated with more falls particularly in the kitchen and bedroom (Bamzar, 2018). Although universal design can enhance the built environment, there are some limitations in its use including: lack of education among planners and architects, gaps in building standards and the cost of implementation.
9.4 Housing options for vulnerable seniors with dementia
In the Netherlands, there is the dementia village called De Hogeweyk (Glass, 2014). Residents live in small houses with six to seven bedrooms, two bathrooms, and a kitchen. The unique concept of De Hogeweyk is that residents can choose to live with others who share common interests and live in a home where the decoration aligns with their personal tastes. Residents or family members fill out questionnaires regarding interests and then the organizers put individuals together in a house with similar interests. This model could be adapted to Canada but may be difficult due to a highly diverse population. The grounds of De Hogeweyk also have restaurants, a hair salon, grocery stores, a theatre etc. with trained staff as employees of these businesses. With this model, residents live their lives as independently and safely as possible (Glass, 2014).
Information and communication technologies can also support seniors living with dementia to age in place. In Europe, there is a project called ACTION (Assisting Carers Using Telematics Interventions to Meet Older People’s Needs) that supports seniors with chronic conditions such as Alzheimer’s and their family caregivers (Connelly, Ur Rehman Laghari, Mokhtari, & Falk, 2014). This program promotes aging in place by providing seniors and their caregivers with access to education, information, and support in their homes utilizing a combination of familiar technologies (for example, the carers' own TV and remote-control units,) and additional technologies, (for example, video reception/transmission, fast computer processors and access to interactive communication). Results from this project showed that caregivers were more confident in their abilities to take care of an individual with a chronic condition. They also liked that ACTION allowed them to connect with other family members in the same situation and health care professionals during an emergency.
10. Conclusion
This paper has examined core housing need and integrated housing needs for seniors in Canada and has outlined key FPT initiatives that help address these needs.
The main findings of the report are:
- That there is a need to increase the supply of housing for seniors overall and various options that take into account the range of health needs and income status of seniors. The type of housing required by individuals would vary depending on these factors
- Senior women are more likely to live alone and have low incomes and therefore are more likely to live in core housing need
- In 2016, most seniors with core housing need lived in apartments and were renters
- Strategies should continue to be sought to incentivize builders, planners and purchasers to incorporate features of universal design for future adaptability and accessibility into new builds and renovations
- Strategies should be evolved to encourage and promote production of more diverse and affordable housing options since the national and international evidence reviewed demonstrates that no one housing option is preferable to seniors and all of the options reviewed had positive benefits in sustaining the well-being of seniors
- From the examples identified, the well-being of seniors can be improved through all levels of government encouraging and promoting inclusion of age-friendly principles into all future building and space design policy and planning. Overall, to implement age-friendly communities, there needs to be adaptations and transformation among home design, neighborhood design, city planning, transportation, and health and home-care services
What has not been addressed in this report and requires further study, is how all levels of government can encourage, promote and/or increase:
- Mixed-use developments with housing located near services and amenities to reduce some of the accessibility and transportation barriers that currently exist;
- Allow construction of smaller units such as accessory dwelling units for those wishing to down-size, reduce housing costs or house a live-in caregiver
- Develop housing suitable for intergenerational living
- Retrofitting of existing homes to improve accessibility
- Construction of affordable rental units especially in suburban settings; and
- Coordinate housing adaptations and community supportive services delivery to increases availability of supportive living options as a viable alternative to LTC
- Housing for indigenous seniors
There is still a need for the creation of a robust knowledge exchange strategy to increase awareness of and access to evidence-informed best practices and models of housing options for seniors in Canada. In addition, further research is needed to understand what motivates seniors to consider various housing options and what deters them. Overall, addressing the core housing need and integrated housing needs of seniors will require adaptations and transformation among home design, neighborhood design, city planning, transportation, and health and home-care services among all levels of government – in consultation with seniors and stakeholders.
Appendix A: A Classification of housing for seniors
| Provincial name | Province | Independent housing | Assisted living | Long-term care |
|---|---|---|---|---|
| Mainsteam Housing | Alberta | yes | no | no |
| OASIS | Ontario | yes | no | no |
| Solterra | Ontario | yes | no | no |
| Abbeyfield Housing | Ontario | yes | no | no |
| Life Lease Housing | Ontario | yes | no | no |
| Assisted Living | British Columbia | no | yes | no |
| Personal Care Homes | Manitoba | no | no | yes |
| Supportive Housing | Manitoba | no | yes | no |
| Residential Facilities/Supportive Housing | Alberta | no | yes | no |
| Long Term Care Homes | Ontario | no | no | yes |
| Residence Parc Jarry | Quebec | no | yes | no |
| Georgian Village | Ontario | no | yes | no |
| Assisted Living Southwest Ontario’s (ALSO) | Ontario | no | yes | no |
| Ultimate Goal Retirement Village | Newfoundland | no | yes | no |
| Seniors’ Lodge Program | Alberta | no | yes | no |
| Green House Model – Sherbrooke Community Centre | Saskatchewan | no | no | yes |
| Planetree Model - Donald Berman Maimonides Geriatric Centre | Quebec | no | no | yes |
| GENTLECARE - Delta View Adult Day Program, Assisted Living and Life Enrichment Centre | British Columbia | no | no | yes |
| Centres d’hébergement et de soins de longue durée (CHSLD) | Quebec | no | no | yes |
| Name | Country | Independent housing | Assisted living | Long-term care |
|---|---|---|---|---|
| Lifetime Neighbourhoods | United Kingdom | yes | no | no |
| Co-housing Communties | Denmark | yes | no | no |
| Resident Driven Housing - Loppukiri | Finland | yes | no | no |
| Producer Driven Housing - Aktiivikoti | Finland | yes | no | no |
| Virkkula Senior Village | Finland | yes | no | no |
| Ars Longa | Finland | yes | no | no |
| Apartments for Life | Netherlands | yes | no | no |
| Homeshares | France | yes | no | no |
| Homeshares | Spain | yes | no | no |
| Village – Village-to- Village | United States | no | yes | no |
| Dementia Villages - De Hogeweyk | Netherlands | no | no | yes |
- The identified types of housing are those named in the report. It is assumed that some or all three types of housing exist in every province and territory. The list follows the order in which they appear in the report for ease of reading and should not be interpreted as any form of ranking.
- Independent Housing: Either individual units or congregate housing where seniors live together but no formal organized services are provided. Normally the units are owned by an organization (for-profit or not-for profit) or by the seniors as a group.
- Assisted Living: Where seniors live together but in separate units (rooms or apartments) owned by an organization (for-profit or not-for profit) and formal services are provided (for example, meals, recreational activities, transportation, some health care services, etc.).
- Long-term Care: Where seniors live together normally in separate units (rooms) owned by an organization (for-profit, not-for profit or municipal) and received 24 hour per day on-call nursing and all other services.
Appendix B: Financial supports for home repair, renovations and adaptations
Jurisdiction: Alberta
Rural coverage
No
Program
The Seniors Home Adaptation and Repair Program is a low-interest home equity loan program to help senior homeowners finance home repairs, adaptations and renovations. Examples include but are not limited to; plumbing, heating, electrical, tree removal, windows, roof repairs, widening doorways and stair lifts. A grant of up to $5000 annually is available to seniors with low income who do not qualify for a loan and who have essential home repairs.
Jurisdiction: British Columbia
Rural coverage
No
Program
Home Improvement Assistance Programs help seniors make their homes safer, more accessible, and more energy efficient. They include:
The Home Renovation Tax Credit for Seniors and Persons with Disabilities assists individuals 65 years or older and persons with disabilities with the cost of certain home renovations to improve accessibility and safety in the home. Citizen are eligible to claim the credit for the year if on the last day of the tax year if they are: a resident of B.C., and a senior or a family member living with a senior, or a person with a disability or a family member living with a person with a disability (for 2016 and later tax years).
EfficiencyBC offers financial incentives, information and support to help households and businesses save energy and reduce greenhouse gas (GHG) emissions by switching to high-efficiency heating equipment and making building-envelope improvements.
Home Adaptations for Independence helps low-income seniors and people with disabilities finance home modifications for accessible, safe and independent living. To be eligible, citizen must be a British Columbia resident with limited income and assets. The citizen or someone in its household must have a permanent disability or loss of ability. The adaptations request should directly address the limitations or loss of ability. BC Housing compares applications against three types of eligibility criteria: applicants, properties and adaptations.
Residential Rehabilitation Assistance Program On-Reserve offers financial assistance to Band Councils and Band members to repair substandard homes to a minimum level of health and safety and to improve the accessibility of housing for people with disabilities.
Jurisdiction: Manitoba
Rural coverage
No
Program
Secondary Suite Program. The Secondary Suite program provides financial help to eligible homeowners for the construction of a secondary suite.
Jurisdiction: New Brunswick
Rural coverage
No
Program
The New Brunswick Seniors’ Home Renovation Tax Credit is a refundable personal income tax credit for seniors and family members who live with them.
Minor Home Repairs Grant available to New Brunswick residents over 65 years old with a total household income at or below the low income seniors benefits limits. The repairs that are covered are focused on fall prevention, such as ramps and repairs to home entry, handrails, grab bars, improved lighting, non-slip and non-skid floor surfaces, and repairs to flooring. The total amount available is $1500 per household.
Federal / Provincial Repair Program provides adaptations to the home for low income seniors who have difficulty with activities of daily living, provides for limited modifications to accommodate an aging parent, and repairs, rehabilitates or improves dwellings to a minimum level of health and safety.
Jurisdiction: Newfoundland and Labrador
Rural coverage
No
Program
The NL Housing Corporation offers a Home Modification Program to help low income homeowners (with an annual income of less than $46,500) who apply and require accessibility modifications for their house to help them age in place are eligible.
The Provincial Home Repair Program. assists low income homeowners who require repairs to their house in order to help them age in place.
Jurisdiction: Northwest Territories
Rural coverage
No
Program
NWT Housing Corporation offers several programs streams that can support seniors to complete maintenance, repairs and renovations, or mobility updates to their homes:
Accessibility Modifications Low-income homeowners with disabilities may be eligible for up to $100,000 to carry out modifications to their home to improve accessibility and support independent living, including: wheelchair access ramps; the installation of grab bars in bathrooms; and creating better access to bathtubs, showers, and the kitchen. Modifications must be directly related to the disability of the homeowner or a family member residing in the unit.
NWT Housing Corporation (NWTHC) offers several programs streams that can support seniors to complete maintenance, repairs and renovations, or mobility updates to their homes.
- Repair Programs: Homeowners may apply at any time for assistance, but timelines for home repairs depend on factors such as tendering, winter road delivery, and barge
- Major Repairs: The NWTHC provides forgivable loans of up to $100,000 to low-income homeowners to subsidize necessary major renovations and repairs of their home. The amount of assistance that may be provided depends on the income of the homeowner and the estimated cost of the required repairs
- Preventative Maintenance: The NWTHC provides assistance for preventative maintenance and minor repairs. Applicants can apply for up to $3,000 on an annual basis for preventative maintenance such as: furnace check-ups; electric inspections; servicing of smoke and carbon monoxide detectors; and Inspection of sewage and water tanks; maintenance of water pumps, light fixtures and receptacles; and repair of minor problems of the roof and/or ceiling
- Emergency Repairs: For those seniors in need of emergency repairs, the Securing Assistance for Emergencies provides up to $10,000 to address urgent health and safety issues
Jurisdiction: Nova Scotia
Rural coverage
Yes
Program
Housing Nova Scotia has a number of programs designed for older adults to adapt their home, make repairs, and rent assistance.
Home Adaptations for Seniors' Independence. This program helps homeowners pay for home adaptations so seniors with low incomes can stay in their homes independently for longer periods of time
The Senior Citizens Assistance Program. This program provides assistance to senior homeowners (age 65+) who would like to remain in their own homes, but cannot afford necessary repairs
Public Housing for Seniors. This program provides affordable rental housing to seniors (age 58 and older) with low incomes. Rent is determined by your annual income
Jurisdiction: Nunavut
Rural coverage
Yes
Program
Senior Citizens Home Repair Program The Senior Citizen Home Repair Program (SCHRP) provides assistance to senior citizens (60+) throughout Nunavut who need to repair and/or adapt their homes in order to ensure their continued safe occupancy, and/or to assist with difficulties they encounter with daily living activities. The assistance comes in the form of a grant, to a maximum amount of $15,000, plus freight costs.
Jurisdiction: Ontario
Rural coverage
Yes
Program
Home and Vehicle Modification Program is available to those with a disability that restricts their mobility to make modifications to their homes in order to help them to continue living in their homes, avoid job loss, and participate in their communities. Applicants must have tried to access all other public or private funding before applying for this program; live in Ontario; qualify financially; and; have a substantial ongoing or reoccurring impairment that is expected to last at least one year. This impairment must impede mobility and result in substantial restriction in the activities of daily living.
Jurisdiction: Prince Edward Island
Rural coverage
Yes
Program
Seniors Safe @ Home Program helps to cover adaptations of the home in order to improve its accessibility to continue living there. This program provides between $1,000 and $5,000 in assistance to help with the cost (depending on income). Eligibility is restricted to those 60 or over with an annual net income (combined with your spouse) no greater than $50,000.
Seniors Home Repair Program helps with the cost of small home repairs up to 50% of the cost to a maximum of $2,000 in assistance for eligible repairs like a roof, windows, doors, or furnace. Eligibility is restricted to those 60 or over with an annual net income (combined with your spouse) no greater than $35,000.
Jurisdiction: Quebec
Rural coverage
No
Program
Shelter Allowance Program supplementary financial assistance of up to $80 per month for low-income households that must spend too much of their income on housing. Those 50 or over who live alone or those in a couple where one of the partners is aged 50 or over are eligible.
Jurisdiction: Saskatchewan
Rural coverage
No
Program
The Emergency Repair Program offers financial assistance to help low-income homeowners complete emergency repairs to make their homes safe. Eligible homeowners may receive up to $12,000. Eligible clients must own the property to be repaired and occupy it as their primary residence; require an urgent repair to their property (for example replacing a furnace during the winter months); and have an annual household income and household assets at or below the limits established by Saskatchewan Housing Corporation.
Home Repair Program - Adaptation for Independence provides financial assistance to low-income homeowners or rental property owners to make a home more accessible for a person with a housing related disability. Eligible homeowners and rental property owners may receive a forgivable loan of up to $23,000. Eligibility for homeowners: own and occupy the property as their primary residence; have a household member with a housing-related disability; and have annual household income and asset levels at or below the limits established by Saskatchewan Housing Corporation. Modifications must be identified by a qualified health practitioner.
Jurisdiction: Yukon
Rural coverage
Yes. Available in some but not all rural communities
Program
The Home Repair Loan provides financial support in the form of a loan, subsidized loan or grant to complete home renovations including those related to accessibility.
References
Baker, K., Baldwin, P., Donahue, K., Flynn, A., Herbert, C., La Jeunesse, E., Will, A. (2014). Housing America’s Older Adults—Meeting the Needs of an Aging Population (PDF format, 4.81 MB)
Bamzar, R. (2018). Assessing the quality of the indoor environment of senior housing for a better mobility: a Swedish case study. Journal of Housing and the Built Environment, 1-38
Barrett, E. J. (2013). The Needs of Elders in Public Housing: Policy Considerations in the Era of Mixed-Income Redevelopment. Journal of Aging & Social Policy, 25(3), 218–233
Bedney, B. J., Goldberg, R. B., & Josephson, K. (2010). Aging in Place in Naturally Occurring Retirement Communities: Transforming Aging Through Supportive Service Programs. Journal of Housing For the Elderly, 24(3-4), 304–321
Bigonnesse, C., Beaulieu, M., & Garon, S. (2014). Meaning of Home in Later Life as a Concept to Understand Older Adults’ Housing Needs: Results from the 7 Age-Friendly Cities Pilot Project in Québec. Journal of Housing For the Elderly, 28(4), 357–382
Boland, L., Légaré, F., Perez, M. M. B., Menear, M., Garvelink, M. M., McIsaac, D. I., Stacey, D. (2017). Impact of home care versus alternative locations of care on elder health outcomes: an overview of systematic reviews. BMC Geriatrics, 17(1)
Brenton, M., & Housing Learning & Improvement Network. (2017). Community Building for Old Age: Breaking New Ground The UK’s first senior cohousing community, High Barnet (PDF format, 2.82 MB)
Canada Mortgage and Housing Corporation. (2000). Supportive Housing for Seniors.
Canada Mortgage and Housing Corporation. (2008). Community indicators for an aging population.
Canada Mortgage and Housing Corporation. (2014). Housing Options for People Living with Dementia, Volume I.
Canada Mortgage and Housing Corporation. (2015). Housing Options for People Living with Dementia, Volume 2.
Canada Mortgage and Housing Corporation. (2016a). Analysis of Housing Choices and Changing Housing Needs of Seniors and Pre-seniors by Age Group.
Canada Mortgage and Housing Corporation. (2016b). 2011 Census/National Housing Survey Housing Series: Issue 9 – The Housing Conditions of Canada’s Senior Households
Canada Mortgage and Housing Corporation. (2016c). Determinants of Seniors’ Housing Choices—Part II.
Canadian Mortgage and Housing Corporation. (2017). Accessibility of Canadian Seniors’ Home Research Insight, July 2017.
Canadian Senior Cohousing Society. (2016). Innovating Seniors Housing: The Complete Guide to Cohousing (PDF format, 1.92MB)
Carr, K., Weir, P. L., Azar, D., & Azar, N. R. (2013b). Universal Design: A Step toward Successful Aging. Journal of Aging Research, 2013, 1–8.
Centers for Disease Control and Prevention. (2009, October 15). Healthy Places Terminology.
Centre for Ageing Better. (2018). Homes that help: A personal and professional perspective on home adaptations (PDF format, 3.39 MB).
Chiu, P. (2016). Reframing "Aging in Place" to "Aging in Community": Exploring Innovative Models to Support Aging in Place in British Columbia.
Core Housing Need, 2016 Census.
Crews, D. E., and Zavotka, S. (2006). Aging, Disability, and Frailty: Implications for Universal Design. Journal of Physiological Anthropology, 25(1), 113–118.
Doupe M, Finlayson G, Khan S, Yogendran M, Schultz J, McDougall C, Kulbalba C. Supportive Housing for Seniors: Reform Implications for Manitoba’s Older Adult Continuum of Care. Winnipeg, MB, Manitoba Centre for Health Policy, Spring 2016.
Federation of Canadian Municipalities (FCM). 2014. “Fixing Canada’s Housing Crunch.”
Federation of Canadian Municipalities. (2015). Seniors and Housing: The Challenge Ahead.
Friesen, S., Brémault-Phillips, S., Rudrum, L., & Rogers, L. G. (2016). Environmental Design That Supports Healthy Aging: Evaluating a New Supportive Living Facility. Journal of Housing For the Elderly, 30(1), 18–34.
Garland, E. (2018). Learning from Intergenerational Housing Projects in the USA.
Glass, A. P. (2014). Innovative Seniors Housing and Care Models: What We Can Learn from the Netherlands. Seniors Housing & Care Journal, 22(1), 74-81.
Government of Canada. (2012). Action Plan for Seniors.
Harding, E. (2007, November). Towards Lifetime Neighbourhoods: Designing sustainable communities for all.
Hashim, J., Pacini, A., Starr, E., SHS Consulting, & CBCL Limited. (2014). City of St. John's Seniors Housing Research Project.
HomeStars. (2017). Insights Forum 2017 Aging in Place Report.
Housing Services Corporation (HSC). 2012. Social Housing End Dates in Ontario: Assessing Impacts and Promoting Good Practices.
Keenan, L. (2017). Low Income Immigrant and Refuge Seniors: Housing and Health Needs Assessment.
Kendig, H., Gong, C. H., Cannon, L., & Browning, C. (2017). Preferences and Predictors of Aging in Place: Longitudinal Evidence from Melbourne, Australia. Journal of Housing For the Elderly, 31(3), 259–271.
Labit, A., and Dubost, N. (2016). Housing and ageing in France and Germany: the intergenerational solution. Housing, Care and Support, 19(2), 45–54.
Leviton-Reid, C. and Lake, A. Building Affordable Rental housing for Seniors: Policy Insights from Canada. Journal of housing for the Elderly 2016, 30(3), 253-270
Lin, J. Statistics Canada. (2005). The Housing Transitions of Seniors. Canadian Social Trends. Catalogue no. 11-008.
MacDonald, D A, Andrews, D. and Brown, R. L. 2008. Basic Living Expenses for the Canadian Elderly.
Monsebraaten, L. (2016, May 25). Ontario’s affordable housing wait list grows. The Star.
Ontario Ministry of Municipal Affairs and Housing. (2014). Life Lease Housing Resource Guide.
Park, A. & Ziegler, F. (2016). A Home for Life? A Critical Perspective on Housing Choice for “Downsizers” in the UK. Architecture_MPS , 9 (2) pp. 1-21. 10.14324/111.444.amps.2016v9i2.001.
Park, S., Han, Y., Kim, B., & Dunkle, R. E. (2015). Aging in Place of Vulnerable Older Adults: Person–Environment Fit Perspective. Journal of Applied Gerontology, 36(11), 1327–1350.
Pedersen, M. (2015). Senior co-housing communities in Denmark. Journal of Housing for the Elderly, 29(1-2), 126-145.
Peek, S. T., Wouters, E. J., Van Hoof, J., Luijkx, K. G., Boeije, H. R., & Vrijhoef, H. J. (2014). Factors influencing acceptance of teCore Housing Needology for aging in place: A systematic review. International Journal of Medical Informatics, 83(4), 235–248.
Persson, H., Åhman, H., Yngling, A. A., & Gulliksen, J. (2014). Universal design, inclusive design, accessible design, design for all: different concepts—one goal? On the concept of accessibility—historical, methodological and philosophical aspects. Universal Access in the Information Society, 14(4), 505–526.
Pirinen, A. (2016). Housing Concepts For and By the Elderly: From Subjects of Design to a Design Resource. Journal of Housing For the Elderly, 30(4), 412–429.
Reeder, B., Meyer, E., Lazar, A., Chaudhuri, S., Thompson, H. J., & Demiris, G. (2013). Framing the evidence for health smart homes and home-based consumer health teCore Housing Needologies as a public health intervention for independent aging: A systematic review. International Journal of Medical Informatics, 82(7), 565–579.
Scharlach, A., Graham, C., & Lehning, A. (2011). The "Village" Model: A Consumer-Driven Approach for Aging in Place. The Gerontologist, 52(3), 418–427.
Statistics Canada. (2013). Canadian Survey on Disability.
Statistics Canada. (2015, November 30). Figure 2.5: Distribution of the total population by age group, observed (1921 to 2013) and projected (2014 to 2063) according to the low-growth (L), medium-growth (M1) and high-growth (H) scenarios, Canada [Illustration].
Statistics Canada. (2016). Age and Sex Highlight Tables, 2016 Census. Statistics Canada.
Statistics Canada, (2016b) Census of Population, Statistics Canada Catalogue no. 98-400-X2016234
Statistics Canada. (2017, February 8). Families, households and marital status: Key results from the 2016 Census. Retrieved November 8, 2018.
The Co-operative Housing Federation of Canda. (2009). The Dunning Report: Dimensions of Core Housing Need in Canada – Second Edition.
Wahl, H., Fange, A., Oswald, F., Gitlin, L. N., & Iwarsson, S. (2009). The Home Environment and Disability-Related Outcomes in Aging Individuals: What Is the Empirical Evidence? The Gerontologist, 49(3), 355–367.
What We Heard: Shaping Canada’s National Housing Strategy. Conference Board of Canada 2016
Wiles, J. L., Leibing, A., Guberman, N., Reeve, J., & Allen, R. E. S. (2011). The Meaning of "Aging in Place" to Older People. The Gerontologist, 52(3), 357–366.
World Health Organization (2007) Global Age-Friendly Cities: A Guide. Geneva: World Health Organization
Glossary
Acceptable housing— is Adequate (does not need major repairs); Suitable (has enough bedrooms for the household); and Affordable (costs less than 30% of before-tax income).
Accessible housing—Housing that has been built, renovated or modified to enable independent living by people with disabilities. Accessibility can include architectural design, features such as modified furniture, shelves and cupboards, and electronic control devices.
Accessory apartment—A self-contained unit separate from the principal dwelling, usually in a single-detached home. A garden suite, for example, a self-contained dwelling without a basement built on a lot with an existing house, is a form of secondary unit.
Adaptable housing—Housing that has been designed to meet the changing needs of residents. This can include flexible design or universal design, as well as design that allows legal secondary suites to be created when needed.
Adequate housing—Housing that does not require any major repairs, according to residents. According to CMHC, A dwelling is adequate if, according to its residents, it does not require major repairs. Major repairs include those to defective plumbing or electrical wiring, or structural repairs to walls, floors or ceilings.
Affordable housing—Housing that costs less than 30% of before-tax household income. According to CMHC, A dwelling is affordable if the shelter costs for the dwelling are less than 30% of total before-tax household income. Shelter costs include the following:
- for renters, rent and payments for electricity, fuel, water and other municipal services; and
- for owners, mortgage payments (principal and interest), property taxes, and any condominium fees along with payments for electricity, fuel, water and other municipal services
Age-friendly community—A community that supports the health, participation and security of all, regardless of age, including features such as the availability of different housing options and transportation options, neighbourhood walkability, access to services for older residents, safety and opportunities to engage in social and civic activities.
Aging in place—The ability to stay in the same home a person has lived in while he or she ages, or to stay in the same community in housing that offers extra support services to meet growing needs.
Assisted living in the community—Homes in the community in which personal services such as bathing, dressing and food preparation are provided.
Co-housing—Housing complexes with shared common facilities and individually owned private dwellings, usually designed for physical accessibility and social sustainability.
Collective housing - Refers to a dwelling of a commercial, institutional or communal nature. This includes seniors’ residences and LTC facilities.
Core housing need— A household is in core housing need if it does not live in acceptable housing, and it does not have enough income to meet expenses of an acceptable alternative. Acceptable housing is:
- Adequate (does not need of major repairs)
- Suitable (has enough bedrooms for the household)
- Affordable (costs less than 30% of before-tax income)
Home renovations for independent living—Simple improvements to extend the usefulness of a home, such as ramps or grab bars.
Housing below standards - Housing below standards refers to housing that falls short of at least one of the adequacy, affordability and suitability housing standards.
Integrated housing need: Is housing need that goes beyond the CMHC definition of core housing need. It includes being able to afford necessary adaptive changes to offset limited accessibility or barriers to the use of mobility aids as well as potential gaps in availability of necessary levels of supportive services such as home care so that a senior can “age in place”.
Long-term care facilities —Residential facilities that provide full living and medical support for aging residents. From Health Canada’s perspective, there is no distinction between a nursing home and a long-term care facility. Other terms are sometimes used in different PTs (for example, personal care homes in Manitoba – although “personal care homes” does not have the same meaning in Saskatchewan – and Centres d’hébergement et de soins de longue durée in Québec).
Mainstream housing - Mainstream housing is a housing model where seniors stay in their usual homes or downsize to ground-oriented options (for example, one-level floor plans usually on a ground level), apartments or condominiums which are not specifically intended for seniors.
Secondary suites—See Accessory apartment.
Senior-led household – For the purposes of this report Senior-led household is the same as a Senior-Maintainer Household, which refers to whether a person residing in the household who is 65 and older, is responsible for paying the rent, or the mortgage, or the taxes, or the electricity or other services or utilities. Where a number of people may contribute to the payments, more than one person in the household may be identified as a household maintainer.
Shared housing - Homes in which a family member or caregiver can share living space with older residents who need more attention.
Space - A space is a residential area that is rented out. Examples of spaces include one half of a semi-private unit, a private or bachelor unit, a one-bedroom unit and a two-bedroom unit. In most cases, a space is the same as a unit. The exception is the case where a unit has been divided to rent to multiple residents. Semi-private and ward units are an example of this. Unless otherwise indicated, data for spaces are for all unit types.
Standard space - A space where the resident does not receive high-level care (that is, the resident receives less than 1.5 hours of care per day) or is not required to pay an extra amount to receive high-level care. Regional terms for this type of space may vary across the country.
Standard housing—Housing that is suitable for able aging adults until their needs grow more demanding.
Suitable housing—Housing that has enough bedrooms for the size and makeup of resident households, according to National Occupancy Standards (NOS) requirements.
Suitability – According to CMHC, A dwelling is considered suitable if it has enough bedrooms, as derived by the National Occupancy Standard:
- A maximum of two persons per bedroom
- Household members, of any age, living as part of a married or common-law couple share a bedroom with their spouse or common-law partner
- Lone parents, of any age, have a separate bedroom
- Household members aged 18 or over have a separate bedroom, except those living as part of a married or common-law couple
- Household members under 18 years of age of the same sex share a bedroom, except lone parents and those living as part of a married or common-law couple
- Household members under 5 years of age of the opposite sex share a bedroom if doing so would reduce the suitable number of bedrooms. This situation would arise only in households with an odd number of males under 18, an odd number of females under 18, and at least one female and one male under the age of 5
An exception is a household consisting of one individual living alone. Such a household would not need a bedroom (for example, the individual may live in a studio apartment and be considered to be living in suitable accommodations).
Supportive living—Homes in which older residents can live with the support of care assistants who attend to cleaning, shopping and similar chores.
Visitable housing—Housing that enables everyone to enter a house, move independently and use a bathroom on the entrance level, including three basic access features:
- A zero-step entry
- A clear opening width of 810 mm (32 in.) on all interior doors (including bathrooms) on the entry floor
- A half-bath (preferably a full bath) with a 1,500-mm (60-in.) turning radius on the entry floor
Universal design—An approach to building design or community planning to produce buildings, products and environments that are inherently accessible to older people, people with disabilities and people without disabilities.