Consultations on the social and economic impacts of ageism in Canada: “What we heard” report
On this page
- Alternate format
- List of abbreviations
- Participating governments
- Acknowledgments
- Executive summary
- Introduction and disclaimer
- Background information on ageism
- Consultation methods
- General experiences with ageism
- Ageism and employment
- Ageism and health and health care
- Ageism and social inclusion
- Ageism and safety and security
- Ageism and media and social media
- Strategies to address ageism
- References
- Annex 1. Summary of consultation participation
- Annex 2. Subpopulation responses
- Annex 3. Programs, initiatives and strategies to address ageism identified in the ageism questionnaire
- Annex 4. Programs, initiatives and strategies to address ageism identified in the roundtable and stakeholder-led consultations
Alternate formats

Consultations on the social and economic impacts of ageism in Canada: “What we heard” report [PDF- 874 KB]
Large print, braille, MP3(audio), e-text and DAISYformats are available on demand by ordering online or calling 1 800 O-Canada (1-800-622-6232). If you use a teletypewriter (TTY), call 1-800-926-9105.
List of abbreviations
- CARP
- Canadian Association of Retired Persons
- CPP/QPP
- Canada Pension Plan/Québec Pension Plan
- FADOQ
- Fédération de l'Âge d'Or du Québec
- FPT
- Federal, Provincial, and Territorial
- GIS
- Guaranteed Income Supplement
- OAS
- Old Age Security
- 2SLGBTQ+
- 2-Spirit, lesbian, gay, bisexual, transgender, queer, and other identities
Participating governments
- Government of Ontario
- Government of Nova Scotia
- Government of New Brunswick
- Government of Manitoba
- Government of British Columbia
- Government of Prince Edward Island
- Government of Saskatchewan
- Government of Alberta
- Government of Newfoundland and Labrador
- Government of Northwest Territories
- Government of Yukon
- Government of Nunavut
- Government of Canada
Québec contributes to the Federal, Provincial and Territorial (FPT) Seniors Forum by sharing expertise, information and best practices. However, it does not subscribe to, or take part in, integrated federal, provincial, and territorial approaches to older adults. The Government of Québec intends to fully assume its responsibilities for older adults in Québec.
1. Acknowledgements
Prepared by Laura Kadowaki, Barbara McMillan, and Kahir Lalji (United Way British Columbia) for the Federal, Provincial and Territorial (FPT) Forum of Ministers Responsible for Seniors. The views expressed in this report may not reflect the official position of a particular jurisdiction.
2. Executive summary
Introduction
The Forum of Federal, Provincial and Territorial (FPT) Ministers Responsible for Seniors (Seniors Forum) has been working to address the social and economic impacts of ageism on older adults in Canada. The World Health Organization defines ageism as “the stereotypes (how we think), prejudice (how we feel) and discrimination (how we act) towards others or oneself based on age.” As a part of the FPT Seniors Forum’s work, feedback was sought from Canadians to better understand the impacts of ageism at the individual level, and at the community level. Participants provided feedback in 2 different ways: 1) by participating in a FPT Seniors Forum led roundtable consultation or a stakeholder-led consultation, or 2) by completing an ageism questionnaire. While ageism can be experienced by people of any age, the focus of the consultations and questionnaire was on ageism directed towards older adults. An older adult was defined as a person aged 55 and up.
As ageism is a complex topic, 5 themes were selected to focus on:
- employment
- health and health care
- social inclusion
- safety and security
- media and social media
Between September and November 2022 a total of 8 FPT Seniors Forum led roundtable consultations and 17 stakeholder-led consultations were hosted across Canada, providing participants with an opportunity to discuss ageism as it related to the 5 theme areas. The ageism questionnaire was available to respondents from August 15 to October 31, 2022, and a total of 2,920 complete responses were received. The questionnaire consisted of a series of close-ended questions, as well as opportunities to share personal stories about the impacts of ageism.
This “What We Heard” report summarizes input received from the FPT Seniors Forum led roundtable consultations and stakeholder-led consultations and the ageism questionnaire. This input will inform a subsequent Policy Options Report, to be submitted to FPT Ministers for their consideration, that will propose approaches, initiatives, and strategies to address ageism in Canada.
General experiences with ageism
In the ageism questionnaire, respondents were asked whether they had ever experienced ageism themselves. Approximately half (48.4%) of respondents responded yes. The most common settings in which respondents reported having experienced or seen ageism were public settings, workplace settings, and health care settings. Furthermore, over two-thirds of questionnaire respondents (69.9%) believed that ageism has increased in Canada since the COVID-19 pandemic began.
Ageism and employment
When discussing ageism and employment in the roundtable and stakeholder-led consultations, participants suggested stereotypical beliefs about older workers were causing significant harm to older workers. Stereotypical beliefs about older workers can make workplaces unwelcoming, contribute to employers not wanting to hire older workers, and cause older workers to doubt their abilities. Furthermore, societal expectations that one should retire at age 65 can cause older workers to feel pressured to retire. Participants also expressed concerns about discriminatory policies and practices in the workplace (for example, lack of accommodations for older workers, being excluded from extended health benefits). Within the context of the COVID-19 pandemic, participants observed how during the shift to remote working, some older workers struggled significantly due to being less familiar with the digital environment and employers not offering adequate supports to adapt to these changes.
In the ageism questionnaire, respondents expressed the most concern about 1) Discrimination against older job seekers in hiring processes, and 2) Older workers being fired, laid off, or forced to retire. These concerns were reflected in the many personal stories shared by respondents about older workers:
- struggling to find employment
- feeling pressured to retire
- being subjected to ageism in the workplace
- being fired, laid off, or forced to retire
Ageism and health and health care
Participants in the roundtable and stakeholder-led discussions were most concerned about ageist attitudes and behaviours by health care providers, and the negative impacts they can have on older adults. Common concerns included older adults being ignored or treated paternalistically, health care providers assuming that symptoms are just due to age, and older adults being denied care or provided with different treatments based on their age. Participants also discussed several barriers to accessing health care services that they viewed as examples of systemic ageism within health care: 1) transportation barriers, 2) telehealth and the digital divide, and 3) language and communication barriers. Finally, participants also discussed how ageism has contributed to the longstanding systemic neglect of long-term care facilities and home care services across Canada.
In the ageism questionnaire, the issues that clearly emerged as the most important concerns for respondents were:
- older adults being viewed as a burden on the health care system
- the lack of action to address issues affecting long-term care facilities or other group living settings
- the lack of action to address issues with general health care services for older adults
Respondents also shared many personal stories that illustrated the negative health impacts of ageist attitudes and behaviours by health care providers. Examples were provided of older adults being misdiagnosed, neglected, or denied treatments. Many respondents who shared a story believed that they or a loved one had received different or poor care because of their age, and that older patients are viewed as disposable or unworthy of receiving care.
Ageism and social inclusion
Roundtable and stakeholder-led consultation participants discussed how ageist attitudes within society hinder the social inclusion of older adults. Participants stated that stereotypical beliefs, ignoring and excluding older adults, and discriminatory actions can make older adults feel disrespected or unwelcome within society. Participants also remarked on how ageism intersects with other forms of prejudice such as sexism, racism, ableism, and homophobia. Participants were concerned about 2 social inclusion issues that had significantly intensified during the COVID-19 pandemic: 1) social isolation and loneliness and 2) the digital divide. Generally, respondents perceived that more resources and supports need to be provided to strengthen social support networks and offer inclusive activities in order to prevent social isolation and loneliness. Participants also emphasized that the assumption by society, government, and organizations that everyone is able to participate digitally is ageist and excludes segments of the older adult population.
Key concerns that were identified in the ageism questionnaire included 1) Government programs, policies and service delivery that do not adequately consider the needs of older adults and 2) The lack of recognition of the contributions that older adults make to society. In the personal stories shared by respondents, the lack of accessible and inclusive community spaces and activities for older adults was the most common theme. Respondents also shared stories about the negative impacts that financial insecurity and the lack of aging in place supports have on the social inclusion of older adults.
Ageism and safety and security
The most commonly discussed safety and security topic at the consultations was senior abuse. Participants believed that ageism contributes to societal beliefs that senior abuse is less important than other types of abuse. Participants also observed there are very limited resources available for responding to these types of crimes and supporting victims. Another concern participants highlighted was that homes and communities are often poorly designed to meet the needs of older adults, with little consideration given to accessibility and safety.
The top safety and security concerns of questionnaire respondents were:
- lack of access to affordable, suitable, and adequate housing for older adults
- physical environments that are not well designed to meet the needs of older adults
- negative views about older adults that can contribute to abuse and neglect
In the personal stories, a major theme was the importance of access to quality affordable housing for older adults. Clear links were made by respondents between housing insecurity and financial insecurity. The stories also illustrated the need for communities to be age-friendly in design and have effective mechanisms in place for reporting senior abuse and ensuring accountability.
Ageism and media and social media
In the roundtable and stakeholder-led discussions, the most prominent topic of discussion was how media and social media perpetuate ageism within society. Older adults are often missing from media and social media, and when they are included, they are usually portrayed stereotypically or negatively. An additional concern raised by the participants is the unintended exclusion of older adults as information, news, and social interactions are shared online.
The top media and social media concerns identified by respondents in the questionnaire were: 1) The lack of representation of older adults and their views in the media, and 2) Discussions or descriptions in media/social media that frame older adults as a burden or drain on society. The stories shared by respondents focused on the stereotypical portrayals and underrepresentation of older adults in media and social media.
Strategies to address ageism
In the ageism questionnaire, the 2 most important theme areas that respondents identified to target for strategies, initiatives, or programs to address ageism were: 1) health and health care, and 2) social inclusion. In the open-ended feedback from the questionnaire and the feedback from the roundtable and stakeholder-led consultations, many of the recommended strategies to address ageism overlapped with the health and health care and social inclusion themes. The main strategies described by consultation participants and questionnaire respondents were:
- implementing campaigns to promote ageism awareness or celebrate aging and the contributions of older adults
- building intergenerational connections through intergenerational programs and housing models
- offering digital technology training to older adults
- increasing funding for non-profit and community-based organizations, which were recognized as providing many social, educational, intergenerational, and aging support programs that promote the social inclusion of older adults
- implementing strategies to prevent the isolation of older adults (for example, outreach, providing information in age-friendly formats, access to public transportation)
- designing age-friendly communities
- developing aging in place supports and innovative housing models as alternatives to long-term care facilities
- reforms to modernize health care systems to better meet the complex health care needs of older adults (for example, improve training on caring for older adults, implement more multidisciplinary care models, increase length of appointments)
- implementing strategies to encourage the hiring and retention of older workers
- promoting positive depictions of older adults in the media and social media
- implementing senior abuse prevention initiatives
Introduction and disclaimer
The Forum of Federal, Provincial and Territorial (FPT) Ministers Responsible for Seniors (Seniors Forum) has been working to address the social and economic impacts of ageism on older adults in Canada. Under the Ageism priority, the Forum has determined a set of deliverables to be issued during their work cycle 2018 to 2021, including this "What We Heard" report. As a part of this work, FPT Seniors Forum led roundtable consultations, stakeholder-led consultations, and a questionnaire were undertaken to better understand the impacts of ageism at the individual level, and at the community level. A Discussion Guide was prepared to provide background information for both consultation participants and questionnaire respondents on the topic of ageism. While ageism can be experienced by people of any age, the focus of the consultations and questionnaire was on ageism directed towards older adults. An older adult was defined as a person aged 55 and up. As ageism is a complex topic, 5 themes were selected to focus on:
- employment
- health and health care
- social inclusion
- safety and security
- media and social media
This “What We Heard” report summarizes input received from the FPT Seniors Forum led roundtable consultations, stakeholder-led consultations, and ageism questionnaire. This input, along with this report, will inform a subsequent Policy Options Report, to be submitted to FPT Ministers for their consideration, that will propose approaches, initiatives, and strategies to address ageism in Canada.
The content of this document does not necessarily represent the views of the Government of Canada, provincial and territorial governments, the Forum of FPT Ministers, participating departments and agencies or government employees.
Background information on ageism
The World Health Organization defines ageism as “the stereotypes (how we think), prejudice (how we feel) and discrimination (how we act) towards others or oneself based on age.”1 Stereotypes are beliefs that are generalized towards a whole group of people. If older adults accept stereotypes and negative views about themselves, self-ageism can occur. Age is just one aspect of a person’s identity, and experiences of ageism can be influenced by other characteristics, such as gender or ethnicity.
Ageism can take many forms. Some examples of ageism include:
- jokes about a person’s age and making fun of older adults in general
- negative or stereotypical portrayals of older adults in the media
- workplace or health care policies that discriminate against older adults
- older adults being patronized, ignored, or insulted, and
- assuming that an older adult is incapable of making their own decisions
Ageism is an important area of study, as research shows it is associated with a number of negative outcomes for older adults, such as reduced longevity, poverty and financial insecurity, poor health outcomes, and loss of self-esteem and confidence.1,2
Consultation methods
Roundtable and stakeholder-led consultations
Roundtable and stakeholder-led consultations: Methods and analysis
Between September and November 2022, FPT Seniors Forum led roundtable consultations and stakeholder-led consultations on ageism were hosted across Canada. Consultations were hosted either virtually or in-person. All consultations addressed ageism as it related to the 5 themes. The following questions guided the discussions for each theme:
- what are the most significant ageism issues related to each of the themes?
- what impacts has the COVID-19 pandemic had on ageism in each of the themes?
- what efforts are currently working to address ageism related to each of the themes?
- what more could be done (for example, new strategies, initiatives, or programs) to best address ageism related to each of the themes, and who should be involved?
The roundtable consultations were hosted by the FPT Seniors Forum and conducted by a contracted facilitator. Stakeholder organizations were also invited to host their own consultations. A Consultation Toolkit was developed and made available to help guide stakeholder organizations that wished to host their own consultations. Notetakers at the roundtable and stakeholder-led consultations recorded key points from the discussions, and the notes were submitted to the FPT Seniors Forum. Analysis of the notes from the roundtable and stakeholder-led consultations was conducted using the qualitative data analysis program NVivo. Key themes were identified from the notes for each topic.
Roundtable and stakeholder-led consultations: sample
A total of 8 FPT Seniors Forum led roundtable consultations were hosted:
- Newfoundland and Labrador
- Alberta
- British Columbia
- Saskatchewan
- Ontario
- Manitoba
- Nova Scotia, New Brunswick, and Prince Edward Island
- Yukon, Northwest Territories, and Nunavut (see Annex 1, Table 1A, for more details)
Seven of the roundtables were conducted virtually and 1 in-person. A total of 108 people participated in the roundtables and the number of participants at each consultation ranged from 8 to 20.
A total of 17 stakeholder-led consultations were also hosted across the country by organizations in:
- British Columbia (n=6)
- Alberta (n=4)
- Ontario (n=2)
- Québec (n=2)
- Manitoba (n=1)
- Nova Scotia (n=1)
- Prince Edward Island (n=1) (refer to Annex 1, Table 1B, for more details)
A total of 457 people participated in the stakeholder-led consultations and the number of participants at each consultation ranged from 6 to 90. Two of the stakeholder-led consultations targeted specific populations of older adults (Indigenous Elders and immigrant older adults). Targeted outreach was conducted by the FPT Seniors Forum to 8 Indigenous organizations to encourage their participation; the FPT Secretariat met virtually with 2 of these organizations to discuss the consultations and anecdotal evidence was received from 1 group, though formal engagement was not conducted.
Roundtable and stakeholder-led consultations: limitations
A few limitations of the consultation approach should be mentioned. The majority of FPT Seniors Forum led roundtables took place virtually, which may have limited the ability of the participants to engage with each other in the discussions. As the stakeholder-led consultations were dependant on the interest of stakeholder groups, some provinces and territories and population groups were underrepresented. In the feedback from stakeholder-led consultation organizers, it was also noted that there was inadequate time to discuss all of the themes and questions at some of the consultations.
Ageism questionnaire
Questionnaire: methods and analysis
The ageism questionnaire was available to respondents from August 15th to October 31st, 2022. The questionnaire was open to anyone with an interest in the topic of ageism and could be answered in English or French. The questionnaire was available online, or a paper survey could be downloaded for printing and filled out and mailed in. A total of 2,920 complete responses were received: 1,387 responses in English (47.5%) and 1,533 responses in French (52.5%). A further 73 stories and submissions were received about ageism via email and the online Share Your Story Platform (53 in English [72.6%], 20 in French [27.4%]).
Descriptive statistics (for example, counts, percentages) were calculated for close-ended questions using the statistical program SPSS. Cross-tabulations were also calculated to present the responses of specific sub-populations. All percentages were rounded to one decimal place. The responses for open-ended questions were analyzed using the qualitative data analysis program NVivo. Key themes were identified from these stories and comments. Due to the large number of stories received, while all were reviewed, it was only possible to include a small number of these in the report. To protect the privacy of respondents, any names of individuals, organizations, or locations were removed from the stories that are included in the report.
Questionnaire: sample characteristics
Questionnaire responses were received from all provinces and territories except for Nunavut. Most of the participants resided in Québec, Ontario, or British Columbia. Table 1 provides a breakdown of the respondents’ province or territory of residence (the total populations of the provinces and territories are also provided for comparison). Based on comments from the respondents, the strong response from Québec (n=1,625, 55.7%) was likely related to efforts by the advocacy organization FADOQ (previously known as Fédération de l'Âge d'Or du Québec) to promote the survey to their members. Three-quarters of the respondents lived in an urban community (n=2,187, 74.9%), one-quarter lived in a rural community (n=714, 24.5%), and a small number (n=19, 0.7%) preferred not to answer.
| Province or territory | Population (2021) | % of Canadian population (2021) | # of respondents | % of respondents |
|---|---|---|---|---|
| Québec | 8,501,833 | 23.0 | 1,625 | 55.7 |
| Ontario | 14,223,942 | 38.5 | 615 | 21.1 |
| British Columbia | 5,000,879 | 13.5 | 295 | 10.1 |
| Alberta | 4,262,635 | 11.5 | 134 | 4.6 |
| Manitoba | 1,342,153 | 3.6 | 74 | 2.5 |
| Nova Scotia | 969,383 | 2.6 | 48 | 1.6 |
| Saskatchewan | 1,132,505 | 3.1 | 39 | 1.3 |
| Newfoundland and Labrador | 510,550 | 1.4 | 21 | 0.7 |
| New Brunswick | 775,610 | 2.1 | 16 | 0.5 |
| Prince Edward Island | 154,331 | 0.4 | 15 | 0.5 |
| Yukon | 40,232 | 0.1 | 7 | 0.2 |
| Northwest Territories | 41,070 | 0.1 | 4 | 0.1 |
| Nunavut | 36,858 | 0.1 | 0 | 0.0 |
- Note: Percentages may not add up to 100% due to rounding.
The questionnaire was open to respondents of all ages. The majority of respondents were aged 55 and up (n=2,685, 92.0%), with the largest number of respondents in the 65 to 74 age group (refer to Figure 1). When asked if they identified with the term “senior” (aîné) or “older adult” (personne âgée), there was no clear preference among respondents (refer to Table 2). However, among English respondents, a larger number preferred the term “older adult” over “senior”, while among French respondents, a larger number preferred the term “senior” (aîné) over “older adult” (personne âgée). Most commonly, respondents identified they were participating in the questionnaire due to having been affected by ageism as an older adult (n=1,280, 43.8%), as someone who had witnessed ageism towards an older adult (n=1,125, 38.5%), or in their role as an unpaid family or friend caregiver or volunteer (n=769, 26.3%) (refer to Table 3).
Figure 1. Age of respondents

- Notes: Percentages may not add up to 100% due to rounding. 6 respondents (0.2%) preferred not to answer.
Figure 1 – Text version
Figure 1 shows a bar graph representing the ages of survey respondents.
- There were 11 respondents aged 18 to 24 representing 0.4% of total respondents
- There were 45 respondents aged 25 to 34 representing 1.5% of total respondents
- There were 60 respondents aged 35 to 44 representing 2.1% of total respondents
- There were 114 respondents aged 45 to 54 representing 3.9% of total respondents
- There were 620 respondents aged 55 to 64 representing 21.2% of total respondents
- There were 1,337 respondents aged 65 to 74 representing 47.2% of total respondents
- There were 616 respondents aged 75 to 84 representing 21.1% of total respondents
- There were 72 respondents aged 85 and older representing 2.5% of total respondents
Underneath the bar graph it is noted that percentages may not add up to 100% due to rounding. It was also noted that 6 respondents (0.2%) preferred not to answer.
| Terminology | Total # of responses | % of total responses | # of English responses | % of English responses | # of French responses | % of French responses |
|---|---|---|---|---|---|---|
| Older adult / personne âgée | 571 | 19.6 | 434 | 31.3 | 137 | 8.9 |
| Senior / aîné | 741 | 25.4 | 218 | 15.7 | 523 | 34.1 |
| Either senior or older adult | 812 | 27.8 | 457 | 32.9 | 355 | 23.2 |
| Other | 129 | 4.4 | 77 | 5.6 | 52 | 3.4 |
| Does not apply | 633 | 21.7 | 187 | 13.5 | 446 | 29.1 |
| Prefer not to answer | 34 | 1.2 | 14 | 1.0 | 20 | 1.3 |
- Notes: Total sample size was 2,920 (1,387 responses in English and 1,533 responses in French). The most preferred “Other” terms were “adult”, “elder”, or “person”. Percentages may not add up to 100% due to rounding.
| Role | Number | Percentage (%) |
|---|---|---|
| Someone who has been affected by ageism as an older adult | 1,280 | 43.8 |
| Someone who has witnessed ageism against older adults | 1,125 | 38.5 |
| A caregiver or a volunteer (not paid for the service provided) | 769 | 26.3 |
| An employee or representative of an organization representing and supporting older adults (for example, advocacy organization, senior centre, community services) | 345 | 11.8 |
| A person paid to be involved in the provision of direct care to older adults in the home, a group living setting (for example, long-term care home, assisted living facility), or other health care settings | 133 | 4.6 |
| A stakeholder/partner from fields such as academia, health administration, finance, law, and/or any level of government (federal, provincial/ territorial, municipal, and Indigenous) | 135 | 4.6 |
| Other | 211 | 7.2 |
| Not applicable or Prefer not to answer | 435 | 14.9 |
- Notes: Percentages do not add up to 100% due to the option to select multiple responses. The most common “Other” response provided was as an “older adult who had not experienced ageism” (n=178).
More females (n=2,064, 70.7%) participated in the questionnaire than males (n=828, 28.4%). A small number of respondents identified as non-binary (n=11, 0.4%), two-spirit (n=2, 0.1%), preferred to self identify (n=2, 0.1%), or preferred not to answer (n=13, 0.4%). Information on the percentage of Indigenous and minority group respondents is summarized in Table 4.
| Respondent group | Number | Percentage (%) |
|---|---|---|
| Person with a disability | 294 | 10.1 |
| Ethno-cultural or a visible minority group | 181 | 6.2 |
| Official language minority community | 131 | 4.5 |
| 2SLGBTQ+ community | 117 | 4.0 |
| Indigenous peoples | 51 | 1.7 |
- Notes: Among Indigenous respondents, 30 identified as Métis citizen, 19 as First Nations, and 2 as Inuk/Inuit. A member of an official minority community is considered to be from a French-speaking community outside Québec or from an English-speaking community in Québec.
Generally, respondents tended to have high levels of education, with about 6 in 10 respondents (n=1,713, 58.7%) having an undergraduate or graduate degree (refer to Table 5).
| Highest level of education completed | Number | Percentage |
|---|---|---|
| Less than high school graduation | 33 | 1.1 |
| High school diploma or equivalent | 275 | 9.4 |
| Apprenticeship or trades certificate or diploma | 104 | 3.6 |
| Some college, CEGEP or university | 389 | 13.3 |
| College, CEGEP, or university certificate | 385 | 13.2 |
| College or university undergraduate degree | 826 | 28.3 |
| Graduate level degree or higher | 887 | 30.4 |
| Prefer not to answer | 21 | 0.7 |
- Notes: Percentages may not add up to 100% due to rounding.
Over two-thirds of respondents were retired (n=1,970 67.5%) (refer to Table 6).
| Employment status | Number | Percentage (%) |
|---|---|---|
| Retired | 1,970 | 67.5 |
| Working full-time | 470 | 16.1 |
| Working part-time | 232 | 7.9 |
| Self-employed | 116 | 4.0 |
| Unemployed | 58 | 2.0 |
| Student | 10 | 0.3 |
| Other | 52 | 1.8 |
| Prefer not to answer | 12 | 0.4 |
- Notes: Percentages may not add up to 100% due to rounding. The most common “Other” responses provided were “On disability or medical leave” (n=26) or a “Family or friend caregiver, homemaker, or volunteer” (n=20).
Questionnaire: limitations
Some limitations of the ageism questionnaire should be noted. First, certain groups of older adults were underrepresented in the questionnaire sample:
- males
- individuals with lower education backgrounds
- the oldest old (considered to be older adults aged 85 and up)
- members of ethno-cultural or visible minority groups
- Indigenous peoples
- older adults from certain provinces and territories
In addition, residents of Québec were significantly overrepresented. Second, due to the questionnaire being primarily accessible online, older adults who do not have access to or prefer not to use the internet were likely underrepresented.
General experiences with ageism
Questionnaire feedback: general experiences with ageism
Questionnaire respondents were asked whether they had ever experienced ageism themselves. A total of 1,413 respondents (48.4%) answered yes (refer to Figure 2). Among older adult respondents there was an age gradient, with a higher proportion of the 55-64 age group (52.6%) reporting experiencing ageism compared to the 65 to 74 (48.4%), 75 to 84 (43.0%), and 85 and up (37.5%) age groups. A higher proportion of female respondents reported having experienced ageism than male respondents (51.9% vs. 39.1%). Compared to the overall sample, a larger proportion of Indigenous (64.7%), ethno-cultural or visible minority (60.8%), 2SLGBTQ+ (62.4%), and people living with a disability (68.0%) also reported having experienced ageism. There was a notable educational gradient, with more individuals with higher levels of education reporting having experienced ageism (refer to Annex 2 for full results for subpopulations). Respondents were also asked whether stereotypes or negative views about aging had ever negatively influenced their perception of themselves. A total of 1,169 respondents (40.0%) responded yes (refer to Figure 3). For the subpopulations, similar patterns were seen for this question as for the previous question (refer to Annex 2).
Figure 2. Have you ever experienced ageism yourself? (n=2,920)

- Notes: 7 respondents (0.2%) preferred not to answer. Percentages may not add up to 100% due to rounding.
Figure 2 – Text version
Figure 2 shows a pie chart that represents responses to the question: “Have you ever experienced ageism yourself?” with n= 2,920 responses.
- A segment of the chart representing 1,413 answers, approximately 48.4% of the total answers, indicated an answer of “Yes”
- A segment of the chart representing 1,090 answers, approximately 37.3% of the total answers, indicated an answer of “No”
- A segment of the chart representing 410 answers, approximately 14.0% of the total answers, indicated an answer of “Not sure”
Underneath the pie chart it is noted that 7 respondents, representing approximately 0.2% of total respondents indicated they prefer not to answer. It is noted that percentages may not add up to 100% due to rounding
Figure 3. Have stereotypes or negative views about aging ever negatively influenced your perception of yourself? (n=2,920)

- Notes: 72 respondents (2.5%) selected “not applicable” or preferred not to answer. Percentages may not add up to 100% due to rounding.
Figure 3 – Text version
Figure 3 shows a pie chart that represents responses to the question: “Have stereotypes or negative views about aging ever influenced your perception of yourself?” with n= 2,920 responses.
- A segment of the chart representing 1,169 answers, approximately 40.0% of the total answers, indicated an answer of “Yes”
- A segment of the chart representing 1,373 answers, approximately 47.0% of the total answers, indicated an answer of “No”
- A segment of the chart representing 306 answers, approximately 10.5% of the total answers, indicated an answer of “Not sure”
Underneath the pie chart it is noted that 72 respondents, representing approximately 2.5% of total respondents indicated they prefer not to answer. It is noted that percentages may not add up to 100% due to rounding.
Among those respondents who were completing the questionnaire on behalf of an older person (n=760), 41.4% (n=315) reported that the older person had experienced ageism and 45.4% (n=345) reported that they thought stereotypes or negative views had impacted the perceptions of that older person (refer to Figures 4 and 5).
Figure 4. If you are completing this questionnaire on behalf of an older person (age 55+), has this person experienced ageism against older persons? (n=760)

- Note: Percentages may not add up to 100% due to rounding.
Figure 4 – Text version
Figure 4 shows a pie chart that represents responses to the question: “If you are completing this questionnaire on behalf of an older person (aged 55+), has this person experienced ageism against older persons?” with n= 760 responses.
- A segment of the chart representing 315 answers, approximately 41.4% of the total answers, indicated an answer of “Yes”
- A segment of the chart representing 352 answers, approximately 46.3% of the total answers, indicated an answer of “No”
- A segment of the chart representing 93 answers, approximately 12.2% of the total answers, indicated an answer of “Not sure”
Underneath the pie chart it is noted that percentages may not add up to 100% due to rounding.
Figure 5. If you are completing this questionnaire on behalf of an older person (age 55+), do you think stereotypes or negative views about aging ever negatively influenced the perception of themselves? (n=760)

- Note: Percentages may not add up to 100% due to rounding.
Figure 5 – Text version
Figure 5 shows a pie chart that represents responses to the question: “If you are completing this questionnaire on behalf of an older person (aged 55+), do you think stereotypes or negative views about aging ever negatively influenced the perception of themselves?” with n= 760 responses.
- A segment of the chart representing 345 answers, approximately 45.4% of the total answers, indicated an answer of “Yes”
- A segment of the chart representing 293 answers, approximately 38.6% of the total answers, indicated an answer of “No”
- A segment of the chart representing 122 answers, approximately 16.1% of the total answers, indicated an answer of “Not sure”
Underneath the pie chart it is noted that percentages may not add up to 100% due to rounding.
When respondents were asked if they had ever seen or been aware of ageism occurring against an older adult, 46.4% (n=1,355) reported they had seen ageism occur first-hand, 33.1% (n=966) reported they had not seen it but were aware of instances of it happening to people they knew, and 20.5% (n=599) reported they had not seen ageism occur and were not aware of it happening to anyone they knew. Respondents most frequently reported having seen or experienced ageism in public settings (39.9%), workplace settings (39.7%), and health care settings (35.0%) (refer to Figure 6).
Figure 6. Have you ever seen or experienced ageism in any of the following settings? (n=2,920)

- Note: Percentages do not add up to 100% due to the option to select multiple responses.
Figure 6 – Text version
Figure 6 shows a bar graph representing survey responses to the question “Have you seen or experienced ageism in any of the following settings ?” with n=2920 responses.
- 1,165 respondents, representing 39.9% of total respondents, indicated they had seen or experienced ageism in a public setting
- 1,160 respondents, representing 39.7% of total respondents, indicated they had seen or experienced ageism in a workplace setting
- 1,023 respondents, representing 35.0% of total respondents, indicated they had seen or experienced ageism in a health care setting
- 966 respondents, representing 33.1% of total respondents, indicated they had seen or experienced ageism in a home or social setting
- 846 respondents, representing 29.0% of total respondents, indicated they had seen or experienced ageism in a long-term care facility or group living setting
- 776 respondents, representing 26.6% of total respondents, indicated they had seen or experienced ageism in a media or social media setting
- 506 respondents, representing 17.3% of total respondents, indicated they had seen or experienced ageism in a government setting
- 49 respondents, representing 1.7% of total respondents, indicated they had seen or experienced ageism in another setting that was not listed
Underneath the bar graph it is noted that percentages may not add up to 100% due to rounding.
Questionnaire feedback: ageism and the COVID-19 pandemic
Figure 7 summarizes responses on the impact the COVID-19 pandemic has had on ageism in Canada. The majority of respondents (81.8%) agreed or strongly agreed the COVID-19 pandemic has brought increased attention to ageism. More than half of respondents agreed or strongly agreed that during the pandemic ageism has increased in health care settings (61.4%), long-term care or group living settings (61.2%), media and social media settings (70.2%), and public places (55.2%). Respondents were more ambivalent about the effects of the pandemic on ageism in the workplace, government, and home or social settings. Most respondents agreed or strongly agreed the pandemic has reduced the social inclusion of older adults (78.2%) and negatively impacted their safety and security (75.9%). Most respondents also agreed or strongly agreed the pandemic has increased intergenerational tensions (62.8%).
Figure 7. Impacts of the COVID-19 pandemic on ageism in Canada

The COVID-19 pandemic has brought increased attention to ageism in Canada.

Ageism has increased in Canada during the COVID-19 pandemic.

Ageism in the workplace has increased during the COVID-19 pandemic.

Ageism in health care settings has increased during the COVID-19 pandemic.

Ageism in long-term care facilities or group living settings has increased during the COVID-19 pandemic.

Ageism in the media and social media has increased during the COVID-19 pandemic.

Ageism in public places (for example, schools, grocery stores, services in general) has increased during the COVID-19 pandemic.
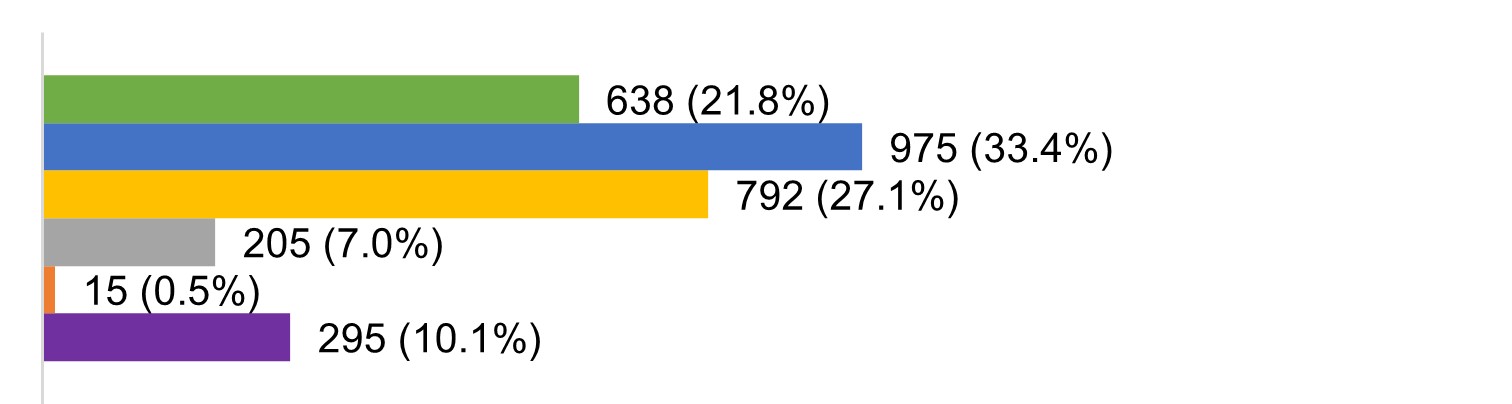
Ageism in government settings (for example, government service centre, government programs, municipal centre) has increased during the COVID-19 pandemic.
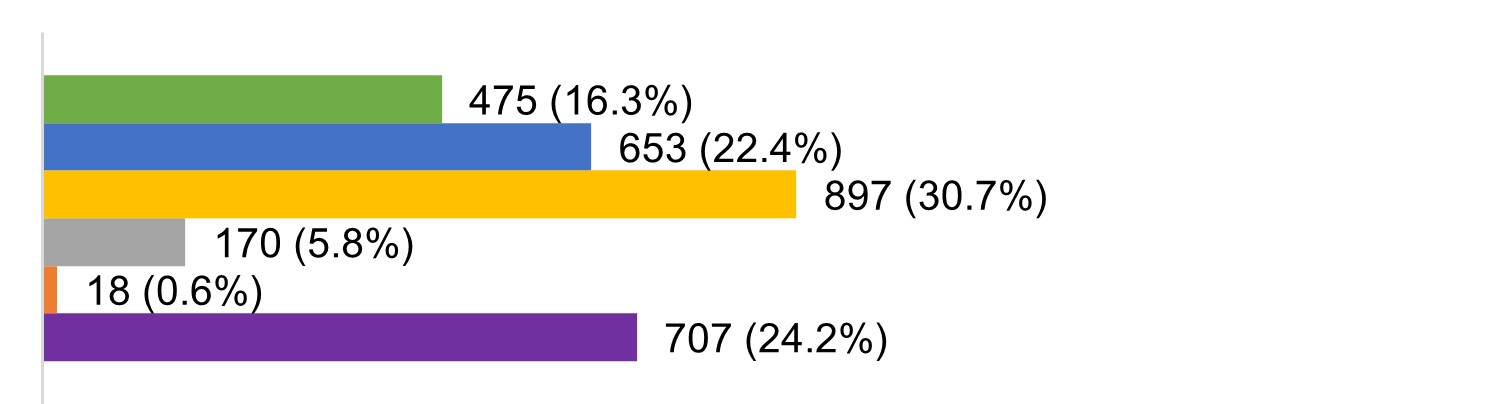
Ageism in the home or social settings has increased during the COVID-19 pandemic.

The COVID-19 pandemic has decreased the social inclusion of older adults in society.

The COVID-19 pandemic has decreased the safety and security of older adults.

The COVID-19 pandemic has resulted in increased intergenerational tensions.

- Note: Percentages may not add up to 100% due to rounding.
Figure 7 – Text version
Figure 7 is a series of bar graphs titled “Impacts of the COVID-19 pandemic on ageism in Canada”. These bar graphs show survey respondents’ answers regarding their level of agreement or disagreement with a series of statements.
- In response to the statement “The COVID-19 pandemic has brought increased attention to ageism in Canada” respondents answered as follows:
- 1,379 respondents, representing 47.2% of total respondents, stated they strongly agreed
- 1,009 respondents, representing 34.6% of total respondents, stated they agreed
- 348 respondents, representing 11.9 % of total respondents, stated they neither agreed nor disagreed
- 109 respondents, representing 3.7% of total respondents, stated they disagreed
- 27 respondents, representing 0.9% of total respondents, stated they strongly disagreed
- 48 respondents, representing 1.6% of total respondents, stated they were unsure or preferred not to answer
- In response to the statement “Ageism has increased in Canada during the COVID-19 pandemic” respondents answered as follows:
- 1,111 respondents, representing 38.0% of total respondents, stated they strongly agreed
- 932 respondents, representing 31.9% of total respondents, stated they agreed
- 566 respondents, representing 19.4 % of total respondents, stated they neither agreed nor disagreed
- 135 respondents representing 4.6% of total respondents, stated they disagreed
- 11 respondents, representing 0.4% of total respondents, stated they strongly disagreed
- 165 respondents, representing 5.7% of total respondents, stated they were unsure or preferred not to answer
- In response to the statement “Ageism in the workplace has increased during the COVID-19 pandemic” respondents answered as follows:
- 407 respondents, representing 13.9% of total respondents, stated they strongly agreed
- 527 respondents, representing 18.0% of total respondents, stated they agreed
- 827 respondents, representing 28.3% of total respondents, stated they neither agreed nor disagreed
- 175 respondents, representing 6.0% of total respondents, stated they disagreed
- 20 respondents, representing 0.7% of total respondents, stated they strongly disagreed
- 964 respondents, representing 33.0% of total respondents, stated they were unsure or preferred not to answer
- In response to the statement “Ageism in healthcare settings has increased during the COVID-19 pandemic” respondents answered as follows:
- 893 respondents, representing 30.6% of total respondents, stated they strongly agreed
- 898 respondents, representing 30.8% of total respondents, stated they agreed
- 547 respondents, representing 18.7% of total respondents, stated they neither agreed nor disagreed
- 132 respondents, representing 4.5% of total respondents, stated they disagreed
- 13 respondents, representing 0.4% of total respondents, stated they strongly disagreed
- 437 respondents, representing 15.0% of total respondents, stated they were unsure or preferred not to answer
- In response to the statement “Ageism in long-term care facilities or group living settings has increased during the COVID-19 pandemic” respondents answered as follows:
- 1,029 respondents, representing 35.2% of total respondents, stated they strongly agreed
- 759 respondents, representing 26.0% of total respondents, stated they agreed
- 458 respondents, representing 15.7% of total respondents, stated they neither agreed nor disagreed
- 100 respondents, representing 3.4% of total respondents, stated they disagreed
- 15 respondents, representing 0.5% of total respondents, stated they strongly disagreed
- 559 respondents, representing 19.1% of total respondents, stated they were unsure or preferred not to answer
- In response to the statement “Ageism in the media and social media has increased during the COVID-19 pandemic” respondents answered as follows:
- 986 respondents, representing 33.8% of total respondents, stated they strongly agreed
- 1,062 respondents, representing 36.4% of total respondents, stated they agreed
- 512 respondents, representing 17.5% of total respondents, stated they neither agreed nor disagreed
- 111 respondents, representing 3.8% of total respondents, stated they disagreed
- 14 respondents, representing 0.5% of total respondents, stated they strongly disagreed
- 235 respondents, representing 8.0% of total respondents, stated they were unsure or preferred not to answer
- In response to the statement “Ageism in public places (for example, schools, grocery stores, services in general) has increased during the COVID-19 pandemic” respondents answered as follows:
- 638 respondents, representing 21.8% of total respondents, stated they strongly agreed
- 975 respondents, representing 33.4% of total respondents, stated they agreed
- 792 respondents, representing 27.1% of total respondents, stated they neither agreed nor disagreed
- 205 respondents, representing 7.0% of total respondents, stated they disagreed
- 15 respondents, representing 0.5% of total respondents, stated they strongly disagreed
- 295 respondents, representing 10.1% of total respondents, stated they were unsure or preferred not to answer
- In response to the statement “Ageism in government settings (for example, government service centre, government programs, municipal centre) has increased during the COVID-19 pandemic” respondents answered as follows:
- 475 respondents, representing 16.3% of total respondents, stated they strongly agreed
- 653 respondents, representing 22.4% of total respondents, stated they agreed
- 897 respondents, representing 30.7% of total respondents, stated they neither agreed nor disagreed
- 170 respondents, representing 5.8% of total respondents, stated they disagreed
- 18 respondents, representing 0.6% of total respondents, stated they strongly disagreed
- 707 respondents, representing 24.2% of total respondents, stated they were unsure or preferred not to answer
- In response to the statement “Ageism in the home or social settings has increased during the COVID-19 pandemic.” respondents answered as follows:
- 467 respondents, representing 16.0% of total respondents, stated they strongly agreed
- 892 respondents, representing 30.5% of total respondents, stated they agreed
- 839 respondents, representing 28.7% of total respondents, stated they neither agreed nor disagreed
- 233 respondents, representing 8.0% of total respondents, stated they disagreed
- 21 respondents, representing 0.7% of total respondents, stated they strongly disagreed
- 468 respondents, representing 16.0% of total respondents, stated they were unsure or preferred not to answer
- In response to the statement “The COVID-19 pandemic has decreased the social inclusion of older adults in society.” respondents answered as follows:
- 1,350 respondents, representing 46.2% of total respondents, stated they strongly agreed
- 934 respondents, representing 32.0% of total respondents, stated they agreed
- 299 respondents, representing 10.2% of total respondents, stated they neither agreed nor disagreed
- 191 respondents, representing 6.5% of total respondents, stated they disagreed
- 37 respondents, representing 1.3% of total respondents, stated they strongly disagreed
- 109 respondents, representing 3.7% of total respondents, stated they were unsure or preferred not to answer
- In response to the statement “The COVID-19 pandemic has decreased the safety and security of older adults.” respondents answered as follows:
- 1,349 respondents, representing 46.2% of total respondents, stated they strongly agreed
- 867 respondents, representing 29.7% of total respondents, stated they agreed
- 328 respondents, representing 11.2% of total respondents, stated they neither agreed nor disagreed
- 216 respondents, representing 7.4% of total respondents, stated they disagreed
- 39 respondents, representing 1.3% of total respondents, stated they strongly disagreed
- 121 respondents, representing 4.1% of total respondents, stated they were unsure or preferred not to answer
- In response to the statement “The COVID-19 pandemic has resulted in increased intergenerational tensions.” respondents answered as follows:
- 897 respondents, representing 30.7% of total respondents, stated they strongly agreed
- 937 respondents, representing 32.1% of total respondents, stated they agreed
- 563 respondents, representing 19.3% of total respondents, stated they neither agreed nor disagreed
- 257 respondents, representing 8.8% of total respondents, stated they disagreed
- 35 respondents, representing 1.2% of total respondents, stated they strongly disagreed
- 231 respondents, representing 7.9% of total respondents, stated they were unsure or preferred not to answer
Underneath the bar graphs it is noted that percentages may not add up to 100% due to rounding.
Ageism and employment
Introduction
An increasing number of older adults are now working in later life. Ageism may prevent older workers from finding a job or remaining in the workforce, and could lead to older workers being treated unfairly in the workplace. Research has shown that employers often believe stereotypes about older workers (for example, older workers are less productive, it is more difficult for older workers to learn new skills), which can lead to age-based discrimination.3 Including older adults in the workforce is good for individuals, businesses, and society. Researchers estimate that increasing the number of older workers in Canada could increase our economic performance by $56 billion.4
Roundtable and stakeholder-led consultation feedback
Societal beliefs about older workers
Common societal beliefs about older workers and retirement were recognized as deterring older adults from participating in the labour force. Within the workplace, participants reported that it is common for employers, managers, and co-workers to believe stereotypes about older workers (for example, older workers are less capable, less productive, unable to use technology, in poor health). These beliefs can make the workplace unwelcoming and contribute to employers not wanting to hire older workers. Self-ageism can occur when older workers begin to accept negative stereotypes about themselves, and this was also identified by participants as an important barrier to participation in the labour force. Participants discussed how stereotypes about older workers or experiencing a layoff or long period of unemployment can lead older adults to lose confidence in themselves and question their ability to contribute as an employee.
Employers not wanting to hire older workers was the most frequent point of discussion by participants, as employers may not want to hire older workers due to:
- stereotypical beliefs about their capabilities
- assumptions that older workers will not stay with the company for long
- concerns that older workers will be more costly
There are nuances to the situation though, with several participants noting that how welcoming employers are to older workers is affected by the physical demands of the job, labour availability, and organizational and occupational culture. Some participants believed that due to the current economic situation and labour shortages, job markets are improving for older workers. However, other participants disagreed, and it was noted that some of the jobs that are becoming available (for example, lower wage jobs, retail) may not be the types of jobs sought by most older workers.
Participants also discussed societal expectations around retirement (for example, retirement at age 65) and how these can deter the participation of older adults in the labour force. Despite increases in life expectancy and changing work environments, participants noted there is still a strong societal expectation that workers will retire by age 65. Older workers must constantly endure comments and questions about retirement from employers, managers, and co-workers, which may cause them to question their capabilities or pressure them to retire. Participants noted employers and co-workers also may exert pressure on older workers to retire by accusing them of taking away job opportunities from younger workers. Furthermore, the idea that older adults should be engaging in unpaid labour during retirement (for example, childcare, volunteering, caregiving) rather than participating in the labour force is a common notion that is promoted within society. Participants acknowledged that many older adults find engaging in these activities rewarding; however, such expectations can be harmful for the older adults who want to, or, out of economic necessity, need to work.
Policies and practices that discriminate against older workers
Participants identified a variety of employment policies and practices that appeared to discriminate against older workers. First, participants highlighted that employers often fail to consider the needs of older workers and as a result do not offer accommodations that will help keep older workers in the workforce. There is a lack of flexible work options available for older adults who, for health, disability, or caregiving reasons, may require accommodations. Some participants also pointed out that more can be done to adapt the workplace environment to meet the needs of older workers (for example, larger keyboards, adaptive devices, ergonomic chairs, louder computer or speaker volume for hearing impaired). Second, concerns were expressed by participants about pension and health insurance policies that discriminate against older workers. For example, it was noted that after age 70 contributions to the CPP are stopped and employers also usually no longer provide extended medical benefits. Third, it was noted that in some occupations, older workers are commonly forced to retire or are laid off by employers when they have reached a certain age. Fourth, employers may exclude older adults from training and advancement opportunities. Fifth, it was observed that for older job seekers, there are fewer skills training and job search programs than for other age groups.
Employment within the context of the COVID-19 pandemic
The most prominent point of discussion regarding the COVID-19 pandemic and employment was the transition to remote working that occurred in many workplaces. While participants emphasized that many older workers are proficient with technology and were able to effectively transition to remote working, it was acknowledged that some older workers struggled significantly with this transition due to being less familiar with computers and the digital environment. This digital divide was a challenge for older workers even before the pandemic; however, the pandemic significantly accelerated the reliance on digital technologies within the workplace. Participants highlighted the institutional ageism that occurred as a result, with little consideration provided to the needs of older workers and a lack of support and training opportunities from employers for older workers. Several participants commented that these workplace changes caused some older adults to accelerate their retirement plans. Furthermore, it was also stated by some participants that the remote working challenges encountered by older workers and stereotypical views about their abilities to use technology led to older workers being pressured to retire or chosen for layoffs.
A second point of discussion among participants was how ageism influenced perceptions of COVID-19 risk in the workplace and policies to mitigate these risks. While COVID-19 is a serious workplace health and safety concern, the blanket classification of all older workers as “high risk” by some employers was a concern. Participants noted that some employers adopted paternalistic approaches towards older workers, for example requesting them to work from home or laying them off to “protect” them. On the other hand, it was also noted that failures by employers to adequately create a safe working environment and mitigate COVID-19 related risks has prevented some older workers from returning to the workplace.
A final point of discussion was that the pandemic did have some positive impacts on employment opportunities for older workers. The option to work remotely has opened up new job opportunities for older workers who desire flexible working arrangements. Several participants also observed there has been an increased demand for labour in some sectors resulting in some employers becoming more willing to hire older workers.
Questionnaire feedback
Additional feedback on ageism and employment was collected through the ageism questionnaire. In the questionnaire, respondents were asked “What do you believe are the most serious ageism issues related to employment?” and were able to select up to 3 options from a list. The issues that were identified as the most significant concerns were:
- discrimination against older jobseekers in hiring processes; and
- older workers being fired, laid off, or forced to retire
Refer to Table 7 for full results.
| Ageism and employment concerns | Number | Percentage |
|---|---|---|
| Discrimination against older jobseekers in hiring processes | 1,446 | 49.5 |
| Older workers being fired, laid off, or forced to retire | 1,116 | 38.2 |
| Ageist attitudes or beliefs about older workers held by employers or managers | 836 | 28.6 |
| Older workers being disrespected or excluded in the workplace | 804 | 27.5 |
| Societal beliefs that older workers take away jobs or promotion opportunities from younger workers | 724 | 24.8 |
| Societal beliefs that older workers should retire at age 65 | 664 | 22.7 |
| Ageist attitudes or beliefs about older workers held by co-workers | 594 | 20.3 |
| Company policies or practices that discriminate against older workers | 464 | 15.9 |
| Ageist attitudes or beliefs about older workers held by self | 145 | 5.0 |
| Other | 29 | 1.0 |
| I don’t believe there are any ageism issues related to employment | 154 | 5.3 |
| Prefer not to answer/Unsure | 188 | 6.4 |
- Notes: % shows the percentage of respondents out of 2,920 who selected the response. Respondents were able to select up to 3 responses, therefore the percentages do not add up to 100%.
A total of 769 comments and stories were also received about ageism and employment via the questionnaire (n=755) and the Share Your Story platform/email (n=14). The most prominent themes identified from the comments and stories were:
- employers not wanting to hire older workers (n=182)
- ageist behaviours and attitudes in the workplace (n=158)
- older workers being fired, laid off, or forced to retire (n=148)
- being pressured to retire (n=108)
These 4 themes also featured prominently in the roundtable and stakeholder-led discussions as described in section 5.2. A short summary of each theme and sample of comments and stories relating to the theme is provided below. An overarching observation across the themes was the intersections between ageism and sexism, with older women particularly likely to experience discrimination in the workplace. Additional themes that emerged from the comments and stories included: the lack of training and advancement opportunities for older workers (n=42); discriminatory policies and practices that deter older workers from participating in the labour force (for example, pension policies, employer health insurance policies) (n=40); the lack of accommodations and flexible work opportunities (n=35); and societal perceptions that older workers are taking jobs away from younger people (n=34).
Employers not wanting to hire older workers
The most common theme in stories and comments was employers not wanting to hire older workers. Many examples were provided of perceived age-based discrimination in hiring processes (for example, employers losing interest in an applicant after they met them in-person, applicant being told off-the-record the employer wanted to hire a younger person). Some respondents reported altering their resume (for example, removing dates, shortening work experience) or their appearance (for example, dying their hair) in an attempt to avoid age-based discrimination in hiring processes.
At some point, I stopped putting dates on my résumé, because I would simply not be called for an interview. Once I stopped putting dates, the interest in my application increased. So I just put 2 and 2 together and came up with ageism.
During the pandemic I was between jobs and I applied for dozens with no success. The response most times was I was overqualified or questioning why would I still want to work. Head hunters told me I was exactly what the client needed to turn the organization around but when I got to the first interview, I could see that I wasn't going to get a second.
Despite extensive experience and stellar credentials and so many vacancies, I had difficulty landing a full-time job and had to take one eventually that was at half the compensation of previous jobs. I was told it was due to my shorter shelf life (I am paraphrasing, but that was the intent of the message).
I was job hunting and emailed an application to a company. I had every qualification and got an invite to interview within hours with many positive remarks about my resume. I got to the interview and the person appeared surprised when she saw me. After a short interview I was told I was not what they were looking for. Everything was fine until she saw me, an older woman, sitting in front of her.
I have seen employer looking at resumes and calculating the approximate age of the applicant and putting resume in the not to interview file.
Older workers being fired, laid off, or forced to retire
Respondents provided many examples of older workers being fired, laid off, or forced into early retirement. In addition to examples of personal experiences and the experiences of friends, family, and co-workers, the specific case of CTV news ending Lisa LaFlamme’s contract was mentioned by multiple respondents.Footnote i Common reasons given for older adults being forced out of their employment included employers wanting to hire younger workers at lower salaries, employers having stereotypical views about the capabilities of older workers, and employers feeling that older workers no longer “fit” with the company culture or image. It was observed by multiple respondents that when layoffs occur at a company, the majority of employees laid off are older workers.
My co-worker and I were let go because we were 'too old' to represent the company. This was not said to us, but reported by another from a board meeting.
I was laid off in July 2021 after the store where I worked closed. Everyone was offered a job at a different store except for me. I was the store manager and the company had several ads for store managers and all other positions in the area. I asked my manager if I could stay on as Assistant Manager or just a team member instead of being laid off but she said no, I would have to re-apply. After getting one month's severance, I knew I didn't have a chance of ever working for that company again.
Our company created a false financial crisis, saying that our division was losing money, when in fact we were keeping some of the other divisions afloat financially. Five of us over the age of 55 were fired without cause in the course of a single morning. No younger people lost their jobs then or later.
My mother was let go from her job at the beginning of the COVID-19 pandemic. Younger, newer staff (less than 1 month experience) were kept on for their 'longevity in the organization', as stated after the fact to another employee.
Ageist behaviours and attitudes in the workplace
Respondents provided many examples of the ageist behaviours and attitudes of co-workers and managers that make older workers feel unwelcome in the workplace. Respondents reported older workers are commonly subjected to ageist attitudes and disrespect by co-workers and managers (for example, name calling, jokes about older workers, assumptions about abilities and competence). Respondents also reported feeling ignored or excluded by their colleagues, both in the workplace during projects and meetings, as well as socially outside of the workplace. Some respondents reported the knowledge and experience of older workers is overlooked or viewed as out-of-date.
As a 63-year-old, white-haired female person, I have found that managers often treat me as if I am incompetent when dealing with technology. They seem to have this preconceived notion that older people don't understand technology.
What I see often occur in workplaces I've been is a lack of respect for older employees (particularly those not in positions of power). These folks are often treated as disposable and given less air time in meetings, fewer responsibilities, and there is less effort on the part of co-workers to include them.
I have heard colleagues in their 30s comment about 'older' staff people being resistant to change or 'not understanding' how straightforward an issue is when the colleagues they are referring to are often more experienced and can see aspects of an issue or additional factors that might need to be considered before implementing change. They are not resisting change, only bringing experience to the discussion to help make the change successful.
I obtained new employment at age 60 and maintained that employment until 70. I had to work very hard to ensure that younger workers did not exclude me in group discussions/social interaction, and to acknowledge that I had assets (skills, experience) that positively contributed to the workplace. A general attitude that as an older person I could not keep up with current practices and would not be open to differing perspectives.
My colleagues make jokes about old women and then tell me how extraordinary I am because I am still able to work. I have one colleague who tells me that I should be sitting at home because that's what her grandmother does.
Being pressured to retire
Over one hundred comments and stories related specifically to the theme of being pressured to retire. Respondents reported co-workers, managers, or human resource professionals constantly asking them when they would retire or suggesting they should retire. In some examples, respondents reported being targeted with mean-spirited comments or it being implied they were taking away opportunities from their younger colleagues. Respondents also provided examples of having their hours reduced, being given unfavourable or difficult assignments, or being bullied or harassed in attempts to force them to retire. In some cases, respondents reported deciding to retire earlier than they would have preferred, due to the pressures being put on them to retire.
Being asked why I don’t retire (on a weekly basis). I’m 56 but have worked for 30 years. I’m eligible to retire but I’m not ready yet. I still feel I have a lot to offer.
The HR department coming to you as soon as you turn 60 and asking when you plan on retiring rather than asking if you enjoy your job and plan on continuing to work because they are glad you are working for them!
A few years ago, my employer made an offer of early retirement. Some employees could not avail themselves of it (financial, social or other reasons); a member of senior management chided them, in front of everyone, for not quitting.
Managers at [my company] would put additional pressures and workloads on older workers trying to force them to quit or become so ill they would miss work and then be pressured to quit. Often managers would get a bonus for having encouraged older workers to take an early retirement package to the point where such a person would buckle under the pressure and quit, often having to go to much lower paying jobs.
Supervisor who asks the question almost every week and sometimes even every day: "When do you plan to retire? You should think about it!" With a young person, the salary would be lower and the number of vacation days fewer. The experience acquired in the company and the quality of the work are not taken into account. It's the volume of work that counts even if you have to go back to do the work.
Ageism and health and health care
Introduction
There is strong evidence that ageism impacts the health of older adults. Ageism may contribute to declines in memory function, increased risk of developing dementia, and decreased life expectancy.5,6,7 Research suggests that ageism can directly affect the health of older adults through 3 main pathways: 1) psychological (for example, ageist attitudes and beliefs become a “self-fulfilling prophecy”); 2) behavioural (for example, negative stereotypes may lead older adults to believe there is no point in engaging in healthy behaviours); and 3) physiological (for example, exposure to negative stereotypes causes stress and triggers cardiovascular stress responses such as increased blood pressure and heartrate).8 Ageism within the health care system may also lead to poor quality health care. For example, health care providers may assume an older adult’s symptoms are a normal part of aging rather than a sign of a health condition.9 Researchers in the United States have estimated that ageism costs their health care system $63 billion annually.10
Roundtable and stakeholder-led consultation feedback
Ageist attitudes and practices within health care
The most frequently discussed concern about health care was how ageist attitudes can impact health care practices and how health care providers treat older adults. Older adult patients being ignored, not listened to, infantilized or spoken to as if they were a child (elderspeak), patronized, or treated paternalistically were common concerns. Multiple participants provided examples of older adults attending medical appointments and the health care provider speaking to their children and ignoring the older adult. Participants also expressed concern about the paternalistic way long-term care residents are treated. For example, the strict visitor restrictions that were put in place to protect long-term care residents during the COVID-19 pandemic were noted to have been implemented without input from residents.
Health care providers holding stereotypical beliefs about older adults (for example, all older adults are frail and dependant) was also a significant concern, with changes in physical and cognitive health commonly assumed to be a natural part of aging. Many participants commented that health care providers do not take the health concerns of older adults seriously and dismiss these concerns as being simply “due to age.” Several participants commented that the limited training given to health care providers on the needs of older patients contributes to these problems. For example, geriatrics training for physicians is often only 1 to 2 weeks long and occurs in a long-term care facility. Some participants also commented that family physicians may be unwilling to take on older adult patients due to assumptions they are in poor health and will take up too much time.
Participants also provided examples of older adults being denied care or provided with different treatments or recommendations based on their age. Older adults were commonly viewed as being lower priority cases for the health care system, particularly when trying to access hospital care. Examples were provided of older adults receiving surgeries or treatments only after convincing their doctors they were fit and/or productive members of society. During the COVID-19 pandemic, several participants commented that discrimination against older adults intensified with triage policies discriminating against people based on their age, and long-term care facilities treated as a lower priority health care setting for resources and personal protective equipment.
In their comments, participants also highlighted how ageist attitudes can intersect with racism, sexism, homophobia, ableism, and other forms of prejudice and discrimination to impact how older adults are treated by health care providers. Previous experiences of discrimination or trauma can also deter older adults from accessing needed medical care. In feedback from First Nations and Métis participants it was stated that health care settings may be traumatic for elders who are survivors of residential schools or the Sixties Scoop.
Systemic barriers to accessing health care
In the roundtable and stakeholder-led consultations, participants discussed a variety of systemic barriers that can prevent older adults from accessing health care services. The most commonly identified were: 1) transportation, 2) telehealth, and 3) language and communication barriers. Participants viewed these barriers as examples of systemic ageism, as health care systems have failed to take into account the needs of older adults and design their services to accommodate them.
Participants identified transportation as a major barrier to accessing health care. While the majority of older adults drive cars, health conditions and changes in physical and cognitive abilities can lead older adults to restrict their driving habits. Participants commented that older adults, and particularly those at more advanced ages, may be uncomfortable driving at night or to unfamiliar places. Some older adults may have decided or been required to stop driving. As a result, older adults may rely on public or accessible transportation, volunteer driver programs, or friends and family to travel to appointments. Transportation was particularly a concern for rural, remote, and Indigenous communities, where there often are limited or no public and accessible transportation options and older adults must travel long distances to access health care services.
Box 1: Travelling to access medical care: feedback from a stakeholder-led consultation
Elders noted that within towns and cities, specifically in (the north of the province), it has been difficult to obtain a long-standing family doctor. Even when a doctor is found, appointments are few and far between, while transportation to and from appointments is another barrier to accessing health care. Specifically, in the north or within smaller communities, Elders must travel a great distance to obtain regular and routine health care, with long waits, and any additional testing or treatment being even further, most often needing overnight accommodation. This is especially difficult to obtain for Elders who may not have access to transportation at any point in time, while a low-income creates an even larger gap, leaving Elders at the mercy of community programming or family members to care for them, taking days off work, investing monies into gas and accommodations rather than securing housing, food, and other necessities.
Participants observed that since the COVID-19 pandemic began, there has been a significant increase in the use of telephone and virtual appointments. While telephone or virtual appointments can address the inconveniences caused by travel, they also can be a barrier to access for older adults who are unfamiliar with/lack access to digital technologies or who live in communities that do not have internet infrastructure or good cellphone reception.
Finally, some participants believed expectations that older adults accessing health care services will have a high level of fluency in English or French, and the lack of translation and interpretation services available to address language and communication barriers, are examples of systemic ageism. Participants in the consultations noted 2 main ways that age amplifies language and communication barriers: 1) Due to cognitive changes that can occur later in life, it may be more difficult to learn a new language and fluency in secondary languages can decline or be lost with age; and 2) Older adults may have had fewer educational opportunities compared to younger generations, and as a result may not have had an opportunity or may find it more difficult to learn English or French. Participants identified immigrants, Indigenous elders, older adults who are deaf or hard of hearing, and members of French or English language minority communities as populations particularly likely to be impacted by language or communication barriers. Language barriers were particularly observed to be a problem for older adults residing in long-term care facilities who may be unable to communicate with the people who are providing them with daily care.
Systemic neglect of long-term care and home care
Participants expressed concerns about all areas of the health care system (acute care, primary care, long-term care, and home care) being under significant stress in recent years (for example, capacity issues, long wait times, challenges accessing needed services). In the discussions, participants particularly focused on how ageism has contributed to the longstanding systemic neglect of long-term care facilities and home care services across Canada. These services are primarily used by older adults, have consistently been underfunded, and the staff providing care in these settings are underpaid. Participants observed that the COVID-19 pandemic has intensified and exposed issues with long-term care and home care. Long-term care facilities received significant attention during the pandemic due to the large number of deaths that occurred in these settings. Inadequate staffing and poor quality of care were key concerns raised by participants. The main concern expressed about home care was that currently services are either unavailable in communities or inadequate to effectively support aging in place. Lack of home care and other community supports (for example, family and friend caregiver supports, transportation, housing) prevents older adults from aging in their communities and pushes them into long-term care facilities.
Questionnaire feedback
Respondents were asked, “What do you believe are the most serious ageism issues related to health and health care?” and were able to select up to 3 options from a list. The issues that clearly emerged as the most important concerns for respondents were:
- older adults being viewed as a burden on the health care system
- the lack of action to address issues affecting long-term care facilities or other group living settings
- the lack of action to address issues with general health care services for seniors (refer to Table 8)
| Ageism and health and health care concerns | Number | Percentage |
|---|---|---|
| Older adults being viewed as a burden on the health care system | 1,928 | 66.0 |
| The lack of action to address issues (for example, staffing, quality of care, underfunding) affecting long-term care facilities or other group living settings | 1,685 | 57.7 |
| The lack of action to address issues with general health care services for seniors (for example, lack of specialists, quality of services for seniors in health care, access to a general practitioner | 1,667 | 57.1 |
| Health care providers assuming medical problems are a natural part of aging | 836 | 28.6 |
| Different treatments being recommended; or treatments being withheld based on a person’s age | 687 | 23.5 |
| Health care providers ignoring, being impatient with, or not wanting to take on older patients | 612 | 21.0 |
| Other | 33 | 1.1 |
| I don’t believe there are any ageism issues related to health and health care | 75 | 2.6 |
| Prefer not to answer | 48 | 1.6 |
- Notes: % shows the percentage of respondents out of 2,920 who selected the response. Respondents were able to select up to 3 responses, therefore the percentages do not add up to 100%.
A total of 861 comments and stories were received about ageism and health and health care via the questionnaire (n=830) and the Share Your Story platform/email (n=31). The most prominent themes identified in the comments and stories were:
- older adults being denied care or provided poor care due to their age (n=229)
- neglect and poor quality of care in long-term care facilities (n=131)
- health care providers assuming medical problems are just due to age (n=110)
- ageism as a contributing factor to challenges finding a family physician (n=73)
These 4 themes overlapped with the consultation findings and are described in greater detail below. Additional themes that emerged from the comments and stories included: older patients being ignored or treated in condescending or infantilizing manners by health care providers (n=69); the lack of publicly funded home care services available to provide an alternative to institutionalization (n=49); gaps in access to health care services, particularly in rural areas (n=39); and perceptions of the public and health care providers that older adults are a burden on the health care system (n=37).
Older adults being denied care or provided poor care due to their age
The most prominent theme that emerged from the stories and comments was that older adults are being denied care or provided with poor care due to their age. Respondents provided multiple examples of situations where screenings, treatments, or surgeries had been denied, delayed, or not recommended for older adult patients. While it is important to acknowledge that these care decisions may have been made for legitimate medical reasons in some cases, respondents perceived them as being due to ageism. Some examples were the result of the ageist actions of individual providers, while others were due to health care policies and processes that discriminate based on age (for example, several respondents noted that mammograms are no longer offered to women after a certain age). Many respondents believed that they or a loved one had received different or poor care because of their age, and that older patients are viewed as disposable or unworthy of receiving care.
I was told at my last mammogram (age 72) that I would receive no more notifications. I replied, ‘Oh do older women not get breast cancer as often?’ The response, ‘Oh, yes, they do, they just die of so many other things as well.’ Disgusting; as our memory fails, we get fewer notifications. We are discardable.
A nurse told me, regarding my mother-in-law, that she (mother-in-law) was a dying patient and her job was to spend her time caring for persons who were going to get better! That was a reality shock as I stared at the 3 dried pools of urine underneath her chair that she had obviously been sitting in for hours!
I’ve been a very active person in my life. I severed my ACL. The surgeon at the time was not really interested in offering me a surgical procedure to address my injury, because he thought that I was too old. He thought basically I would be sitting around in a chair for the rest of my life, and therefore didn’t need my leg to move around anymore. I insisted on having my leg fixed, surgically, and have continued to live a very active life. Can you imagine if I had not been able to be active, the impact of that on my health, and more. This is about doctors having very restrictive use of what they offer patients based on their age.
When my husband suffered a brain bleed, one of his doctors told me that he would never get better because he was 85. This man had been active and fit. He walked our usual 2 miles route a few days before his stroke. He suffered very little physical damage from the stroke. Yet, the hospital never implemented a rehab program and physical therapy was terminated after a few weeks. He could walk with a walker but was not allowed to at the personal care home. The person in charge of rehab there would not discuss a program for him. The system treated him as disposable.
I took my mother-in-law to the hospital emergency when she was 90 years old. By some clerical error, the waiting paper work showed her as 80 years old. When I pointed out the error to a nurse who came into the room to check on her while we were waiting, she cautioned me in a low voice to not say anything as she would receive better care if they thought she was 80 than if they knew she was 90.
Neglect and poor quality of care in long-term care facilities
Neglect and poor quality of care in long-term care facilities and other group living settings was a prominent theme in the comments and stories. Respondents gave examples of residents not being provided with timely assistance to meet basic needs (for example, help going to the bathroom) or being denied basic necessities required for comfort (for example, no air conditioning). While some of the examples pertained specifically to neglect and poor care provided during the lockdown phase of the COVID-19 pandemic (for example, lack of personal protective equipment, high mortality rates, preventing family from visiting), there were many other examples that illustrated poor quality of care in long-term care facilities is a longstanding and ongoing problem. Multiple respondents suggested inadequate staffing levels are a root cause of quality issues. Additional causes suggested in the comments included lack of regulation and government oversight, poor pay and working conditions for staff, and the profit motivations of for-profit providers. Respondents noted that ageism has contributed to the lack of attention and political will to address issues within long-term care facilities.
A senior family member in a private long term care home did not eat or drink for 3 days. No health care professional or family member were contacted or notified. A visiting family member inquired into the senior’s deteriorated health and was told about the lack of food and liquids. The senior spent several weeks in hospital as a result of the neglect. There were no changes in policy at the care home.
I work in different long-term care homes and have witnessed residents not being helped properly at meals due to lack of staffing, residents having to wait 30+ minutes to use the bathroom because of lack of staff, and more.
My mother-in-law was in a care facility for the last 3 years of her life, predating COVID. She was hard of hearing. We got her hearing aids but the care aides did not believe she needed them and also thought she might lose them in the sheets...they didn't want to be held responsible, which we assured them they wouldn't be. One nurse told us it was important she wore the hearing aids because without them, some care aides treated her like 'a vegetable'. She was often left alone for hours in her sometimes very hot room without fluids nearby to drink and without an open window or fan. When we would visit and ask if she'd eaten, no one could tell us if she had or not. She was unable to get herself up or move well in bed which led to bedsores. Though she was in a publicly funded bed in a private facility, it took over 6 months and many bedsores later, for the facility to come up with an alternating air pressure mattress. She wasn't the only one in the home who received poor care.
During the pandemic, tens of thousands of elderly people died in horrific conditions. It brought to light that we don't give a damn if they die. They are given filthy food; the care is not adequate; there are no clear rules on the number of staff/patients; private long-term care facilities are there to make money. If one day I am so sick, I will ask for assistance in dying rather than going to a long-term care facility. Dying with dignity should be a right! Not a wish.
Problems with staffing, staff ratios, and quality of care in long-term care have been going on for decades without being adequately addressed. And government oversight of these agencies has been pitiful, responding only when there are complaints. Regular, unannounced inspections must be done. And more government funding needs to be diverted to aging in place. Most older people fear nursing homes more than death itself.
Health care providers assuming medical problems are just due to age
In many comments and stories respondents described situations where health care providers assumed that the symptoms or medical problems of older adults were simply the result of old age, and thus not worth investigating or treating. Respondents provided examples of medical problems being misdiagnosed or diagnosis being delayed due to these assumptions, in some cases with fatal results. Multiple respondents commented that they had to advocate for their or a loved one’s medical problems to be investigated and taken seriously.
The famous phrase “you know at your age...” I am not a statistic.
I have many senior clients who have shared with me that their health issues are being ignored and not followed up on. They are being told by the general practitioner they have a condition called 'TMB'. When asked what that meant, they are told 'Too Many Birthdays.' This is very sad and disheartening to hear that Doctors are actually saying this.
A friend's husband was told by a doctor that there was nothing he could do for his back pain; it came with old age. He was 56!
Earlier this year I had a medical emergency that resulted in a trip to Emergency. I was in extreme pain, doubled over, barely able to move. The attending physician dismissed, without examination, my symptoms and tried to discharge me. His comment was that ‘at my age’ the cause of my pain was likely cancer. I was discharged but I returned 2 days later with a perforated appendix that required a week in hospital to clear the massive infection. My husband has been dealing with leg pain that is, at times, debilitating. The doctor he saw dismissed the pain as being a part of ageing and did nothing to help him.
Hearing loss [is] not taken seriously, as it's considered part of aging, when it is in fact a health and social issue.
Ageism as a contributing factor to challenges finding a family physician
The shortage of family physicians within Canada was a major concern for the questionnaire respondents. Some respondents stated they had been waiting years for a new family physician. While not all respondents believed their challenges finding a family physician were the result of ageism, others stated family physicians did not want to take on older patients due to the assumed complexity of their health problems. In some cases, respondents had been explicitly told a family physician was not taking on patients of a certain age. Several participants who had recently lost their family physician expressed how stressful and discouraging it was to need to search for a family physician at their age.
The biggest problem is the serious shortage of general practitioners as well as all the health care professionals. At 83 years of age, I am facing the retirement of my GP and being unable to find a replacement. How do I get basic care and have prescriptions filled without clogging up hospital emergency rooms?
I am 70 years old and my husband 83 years old. We have been without a doctor for 3 years. It is incredible and aberrant.
My parents had challenges finding a family doctor. The clinics contacted asked for the age of my parents and advised them that they were not taking new patients beyond a certain age.
My husband and I were dropped from our primary physician's practice. We were told that he had to reduce his practice so a 'lottery' was taken and we won the privilege of trying to find another doctor in our declining years. Not an easy task.
Ageism and social inclusion
Introduction
Social inclusion “describes how a society values all of its citizens, respects their differences, ensures everyone’s basic needs are met, and welcomes and enables full participation in that society.”11 Ageism contributes to the social isolation and feelings of loneliness of older adults.12 Social isolation and loneliness have been linked to negative health outcomes for older adults and increased health care costs.13
Roundtable and stakeholder-led consultation feedback
Ageism and other intersecting forms of prejudice hinder social inclusion
In the roundtable and stakeholder-led consultations, participants identified that ageist attitudes within society can hinder the social inclusion of older adults. Stereotypical beliefs, patronizing behaviours, ignoring and excluding older adults, and discriminatory actions can make older adults feel disrespected or unwelcome within society. The COVID-19 pandemic was viewed by some as intensifying the ageist attitudes and segregated nature of society. Participants also remarked on how ageism can intersect with other forms of prejudice such as sexism, racism, ableism, and homophobia. Box 2 provides an example from the notes of a stakeholder-led consultation of a discussion by participants that illustrates the intersecting nature of ageism. Women, members of Indigenous and racialized communities, people living with disabilities or dementia, and 2SLGBTQ+ older adults were identified by participants as potentially experiencing intersecting forms of prejudice and discrimination later in life. Several participants also highlighted how discrimination and trauma experienced earlier in the life course can impact individuals later in life. For example, discrimination by employers can impact income and pensions later in life.
Box 2: The intersectional nature of ageism: feedback from a stakeholder-led consultation
Age intersects all identities. This is evident in some of the experiences shared by the older participants. One older participant in her 80s, of a smaller stature, and Chinese was pushed aside by a young person as the elevator opens. Even a bystander observed the act to be intentional and mean-spirited. She asked the group whether this was ageism, racism, or sexism. We could not arrive at a definitive answer because she embodies all these identities. Participants commented that in their younger age, they are more resilient in overcoming these "isms" and continuing as usual. In older age, they are more likely to cocoon in and reduce participation in society.
Addressing social isolation and loneliness
Social isolation and loneliness was the most commonly discussed social inclusion topic in the roundtable and stakeholder-led consultations. Some participants commented on changes in family and community structures that they believe have increased the social isolation of older adults (for example, families living farther away from each other, lack of intergenerational contact). The COVID-19 pandemic was viewed as having significantly increased social isolation and loneliness among the older adult population. While the need for public health measures to prevent the spread of COVID-19 was not disputed by participants, some commented that ageism and the desire to “protect” older adults contributed to the development of overly restrictive policies that targeted older adults (for example, restriction of visitors to long-term care).
Generally, it was perceived that more resources and supports need to be provided to strengthen social support networks, enhance intergenerational ties, and offer inclusive activities in order to prevent social isolation and loneliness. Participants highlighted the need to address systemic barriers to the social participation of older adults, including lack of transportation, inadequate incomes to meet basic necessities (let alone participate socially), and language barriers. Furthermore, several participants noted there has been a lack of supports to deal with the mental health concerns (for example, anxiety, depression) and grief caused by the COVID-19 pandemic.
Exclusion of older adults due to the digital divide
The digital divide refers to the gap between individuals who have the ability and resources to access the internet and use digital technologies (for example, computers, smartphones, tablets) and those who do not. The digital divide was discussed extensively in conversations on social inclusion and media and social media at the roundtable and stakeholder-led consultations. As most of the comments made by participants pertained to social inclusion, the digital divide discussions are summarized in this section. Participants at the consultations highlighted that while many older adults are proficient at using digital technologies, older adults are more impacted by the digital divide than younger age groups. Older adults did not grow up using digital technologies and may not have had an opportunity in their personal or work life to acquire the skills necessary to use digital technologies. Participants observed the costs of internet and digital technologies also can be a barrier for low-income older adults. Rural and remote communities, whose populations often include a high proportion of older adults, also may lack the infrastructure necessary for internet access.
Participants asserted that the assumption by society, government, and organizations that everyone is able to participate digitally is ageist and excludes primarily segments of the older adult population. Older adults who do not use digital technologies are excluded from participating in social activities (for example, participating in social media and online activities), communications and important information (for example, information about community events that is only shared online), and accessing services (for example, government forms that must be filled out online, online banking and payment systems, telehealth). Participants highlighted that the COVID-19 pandemic has intensified the digital divide due to the rapid shift to the digital environment, with many social activities, workplaces, and services moving online (and many still remaining online even during the later stages of the pandemic). Participants commented that there has been little support provided to the people who have been left behind by these shifts. Some participants observed though that a positive outcome of the pandemic has been more older adults learning how to use digital technologies, which has opened up new social participation, health, and work options.
Questionnaire feedback
In the questionnaire, respondents were asked “What do you believe are the most serious ageism issues related to social inclusion?” and were able to select up to 3 options from a list. The issues that were identified as respondents’ most significant concerns were:
- government programs, policies and service delivery that do not adequately consider the needs of older adults
- lack of recognition of the contributions that older adults make to society
- lack of supports (financial or programs/education) to assist older adults to participate in society
- older adults being ignored or treated as if invisible (refer to Table 9)
| Ageism and social inclusion concerns | Number | Percentage (%) |
|---|---|---|
| Government programs, policies and service delivery that do not adequately consider the needs of older adults | 1,464 | 50.1 |
| Lack of recognition of the contributions that older adults make to society | 1,446 | 49.5 |
| Lack of supports (financial or programs/education) to assist older adults to participate in society | 1,228 | 42.1 |
| Older adults being ignored or treated as if invisible | 1,212 | 41.5 |
| Ageist attitudes within society that make older adults feel unwelcome or rejected | 1,057 | 36.2 |
| Lack of opportunities for the social inclusion or participation of older adults within society | 813 | 27.8 |
| Other | 43 | 1.5 |
| I don’t believe there are any ageism issues related to the social inclusion of older adults | 84 | 2.9 |
| Prefer not to answer | 43 | 1.5 |
- Notes: % shows the percentage of respondents out of 2,920 who selected the response. Respondents were able to select up to 3 responses therefore the percentages do not add up to 100%.
A total of 619 comments and stories were received about ageism and social inclusion via the questionnaire (n=596) and the Share Your Story platform/emails (n=23). The most prominent themes that emerged from the comments and stories were:
- lack of accessible and inclusive community spaces and activities for older adults (n=105)
- lack of financial security for older Canadians (n=99)
- older adults feeling ignored by society and government (n=88)
- need for aging in place supports (n=64)
These 4 themes are described in greater detail below. While all themes were also discussed in the consultations, financial security issues and the need for aging in place supports were represented more prominently in the questionnaire. Additional themes that emerged from the comments and stories included: ageist attitudes from the public or service providers that make older adults feel unwelcome (n=59); the digital divide (n=49); the negative impacts of the COVID-19 pandemic on the social inclusion of older adults (n=35); the lack of inclusion of older adults within workplaces (n=33); and the need for more intergenerational activities and opportunities for interaction (n=32).
Lack of accessible and inclusive community spaces and activities for older adults
Respondents’ comments and stories illustrated the lack of inclusive community spaces and social and recreational activities for older adults. Respondents expressed concerns about the lack of variety of programming (for example, programming to accommodate a range of interests and abilities) and lack of supports to ensure activities are accessible and inclusive for diverse older adults (for example, low-cost fees, accessible buildings, transportation supports, sharing information in accessible ways). Lack of public transportation options (including accessible transportation) was a frequently highlighted barrier to social participation, particularly in rural areas. Respondents commented both on the need for senior-specific spaces and activities, as well as community spaces and activities that are open to all ages.
At the local community centre no programming was announced/provided for seniors until we (seniors) finally addressed the issue. Recreation staff didn't even consider the need or potential.
It is very difficult for any senior's group to find adequate space (including office space) for seniors' activities. Community centres are mostly built with younger people in mind, and in their running, are reluctant to share that space with seniors. Large centres appearing here and there, may not be sufficiently accessible to seniors, who may not drive and/or don't want to drive on very busy roads sometimes in difficult weather conditions. Everything depends on having a car and being sufficiently mobile.
I live in a rural area where access to programs or recreation is either by walking or by private automobile. Older adults in rural areas often cannot afford a car. The government chooses to rely on rural communities to provide needed transportation to older adults. This means that if an older adult is not well connected to community groups, they face extreme isolation. Rural communities are under serviced by every kind of government program. At the same time these communities are exhibiting great pressure to provide for a growing older population. We need organized help!
How about making programs for seniors a priority in the community at local Community Centres? How about having the local municipal government actually mailing hard copies of available programs for seniors in the community instead of making or expecting that a senior can easily access information online without the help of someone who is computer literate? 90% of info for seniors is now only available online. Most seniors I know grew up with paper and pencil and it has been very difficult to train one’s brain to learn how to navigate and access information online.
Lack of financial security for older Canadians
Another prominent theme that emerged from the comments was the lack of financial security of older Canadians. Respondents stated that many low-income older adults who rely primarily on government pensions and benefits (for example, CPP/QPP, OAS, GIS) do not have the financial resources to have a good quality of life and participate socially (for example, pay for transportation, program fees, and more). Several respondents noted that older women are particularly likely to face poverty in old age due to disadvantages in the labour market (for example, lower pay, unpaid labour as homemakers or family and friend caregivers). Concerns were also raised about the adequacy of income supports for people living with disabilities. Many respondents also expressed concerns about government decisions to only target income benefit increases to specific age-segments of older adults (for example, OAS increases for older adults 75 and up).
I am on a very limited income (due to divorce) and cannot afford to belong to many of the senior groups because of the fees and also the cost of transportation. These circumstances also affect my ability to access fitness programs that would improve my long-term health.
Both of my parents are 65+. My mom was disabled prior to becoming a senior. My dad was laid off because of his age (they called the store he managed the old folks home, a truck accessory business). Neither of my parents can afford life. They exist and scrape by. I wish I could help but I can’t. If you look at a senior couple, living only on CPP and OAS until death, they cannot make it. For them to both eat, 3 times a day, everyday until age 85 at $5 per meal is around $219,000. What about housing, taxes, utilities and heaven forbid a day of something fun? These people built our country and this is how they are treated…. So sad. Everyone should be able to live and not simply exist.
Gender-based analysis is required when it comes to policies, programs, services and benefits as women have not had equal pay for work of equal value. They also live longer and bear the vast majority of unpaid child and elder care. Older single women are the poorest people in Canada. Most of them prefer to age in place but often can’t financially afford to do so.
The Canada OAS and the Canada CPP are inadequate to afford the cost of living and inflation. Especially for 65- to 74-year-old retired seniors who won't get the OAS increase for 75+ year old retired to be enacted in 2023.
I am $40,000 in debt, I've been unemployed for over a year and I can't even find a part-time job. I've had several job interviews but as soon as I walk in I see 'the look' and I know I'm wasting my time being there. I go through the interview anyway, I keep telling myself one day my luck will change, but the outcome is always the same. I requested my CPP this year to help out with what I have left of my savings. If I can't find a job soon, I will have to file for bankruptcy to save payment of about $600 per month on debt to delay homelessness.
Older adults feeling ignored by society and government
Many of the comments and stories related to the theme of older adults feeling ignored by society and government. Respondents provided examples of older adults being ignored in social, retail, or other public settings. Several respondents specifically described feeling “invisible” and being overlooked when in public or in the company of others. Respondents also expressed concerns that the needs of older adults are being ignored by government and that more consultation with older adults, and attention to their needs, is required. Some respondents highlighted the intersections between ageism and sexism, with older women in particular reporting they felt ignored or invisible.
Genuinely feel that no one cares how I feel, think or am physically or mentally. My children tell me their problems, ask me to provide childcare, or shop for them but they never ask how I am or want to spend time with me.
Women become invisible in public. In places that I go to regularly, I am not recognized unless I am accompanied by my husband, who is systematically recognized.
When I go shopping with my 50-year old daughter, almost every time, the clerks turn to her first to offer service and she has to insist that I am the one who requires service. This has been particularly so when shopping for a new car as the sales staff quite literally ignore me until they realize I have the money!
Government completely ignores input by older adults about what services and supports we need. They are patronizing and dismissive or ignore us completely.
Need for aging in place supports
The need for more supports for aging in place was a common theme. Most of the comments and stories specifically referred to the need for more home care; however, additional needed supports were suggested such as family and friend caregiver and home maintenance supports. It was commented by many respondents that allowing older adults to age in place should be the priority, as it is both preferred by most older adults and allows them to remain a part of their community. Several respondents observed that once an older adult is institutionalized it becomes very difficult for them to participate in broader society.
There are not enough supports for older adults and their caregivers to adequately and effectively provide home care. No other options are available, and the out-of-pocket expenses are extremely high. This leaves many families, especially those caring for and living with dementia, to have no other choice but turn to long-term care for support. They don't want or need the 24/7 support, but this is their only option. It is a stressful time for the individual and for families, and often leads to increased behaviours, isolation, and poorer health outcomes.
Home care should be a priority for every political party! The majority of seniors want to stay home as long as possible...but with care if necessary.
We want home care, we are offered retirement homes.
When seniors are removed from their homes due to lack of services they are also removed from society.
Ageism and safety and security
Introduction
Freedom from harm and access to shelter are 2 of the most basic standards for the safety and security of older adults. Ageism is considered a risk factor for and a result of senior abuse and can lead to reports of senior abuse not being believed or taken seriously.14 Ageist policies and practices can also hinder older adults’ access to security, such as secure housing. Houses and neighbourhoods are often poorly designed to meet the needs of older adults.15 Discrimination in the rental market can jeopardize the ability of older adults to access housing.
Roundtable and stakeholder-led consultation feedback
Senior abuse
The most commonly discussed safety and security topics at the consultations were senior abuseFootnote ii and scams and fraud targeting older adults.Footnote iii Participants stated that in cases of senior abuse it often is family members that are the perpetrators and this can make older adults reluctant to report the abuse. Reporting senior abuse can be particularly difficult for recent immigrants who may be dependent on their families or lack the language skills necessary to make a report. Indigenous elders also may be reluctant to report senior abuse due to past experiences of trauma, discrimination, and abuse that lead them to fear retribution from care providers or the repercussions for their family members. Several participants also commented on the lack of safeguards to prevent individuals from taking advantage of older adults if they have power of attorney. Participants believed the COVID-19 pandemic has made older adults more vulnerable to senior abuse and scams and fraud due to isolation and increased reliance on digital technologies.
Participants perceived that ageism contributes to societal beliefs that senior abuse is less important than other types of crimes. In cases of financial abuse, ageism can lead family members to feel entitled to the money of an older adult. Ageism may also lead scammers to view older adults as easy targets. Participants commented on the lack of police resources dedicated to responding to these types of crimes, lack of data collection on cases of senior abuse, lack of shelter spaces for victims of senior abuse, and lack of advocacy and victim support services. For victims of senior abuse and concerned family members or friends, it can be difficult to determine who the abuse can be reported to (for example, police, health care system, bank, social services, and more). Furthermore, it was noted that gaps in legislation around domestic violence, power of attorney, and people in care can prevent the police from effectively responding to cases of senior abuse that may be criminal in nature. Participants stated that stricter banking regulations are also needed to deal with cases of financial abuse and scams and fraud. Police, health care providers, bankers, and frontline services providers were identified by participants as needing better training on how to deal with cases of senior abuse and scams and fraud.
Safe and accessible homes and communities
The need for safe and accessible homes and communities was also discussed by participants at the roundtable and stakeholder-led consultations. Participants highlighted that homes and communities are often designed without consideration given to accessibility and the needs of older adults. Communities need to be designed to be age-friendly and accessible to people living with mobility, hearing, vision, and other forms of disability. Pedestrian safety, in particular, was identified as a concern (for example, ramps and curb cuts to accommodate wheelchairs, adequate lighting at night, sidewalks, snow shoveling). Buildings and homes also were identified by participants as needing to be age-friendly in design. Improved access to quality affordable housing for older adults was recognized by participants as a need in most communities. Some participants also commented on the need for safe and accessible public transportation options for older adults. Finally, emergency preparedness was discussed at one of the consultations as an important priority to ensure the safety of older adults during an emergency.
Questionnaire feedback
Respondents were asked “What do you believe are the most serious ageism issues related to safety and security?” and were able to select up to 3 options from a list. Respondents expressed the most concern about the following safety and security issues:
- lack of access to affordable, suitable, and adequate housing for older adults
- physical environments that are not well designed to meet the needs of older adults
- negative views about older adults that can contribute to abuse and neglect (refer to Table 10)
| Ageism and safety and security concerns | Number | Percentage (%) |
|---|---|---|
| Lack of access to affordable, suitable, and adequate housing for older adults | 1,810 | 62.0 |
| Physical environments (for example, houses, neighbourhoods, communities) that are not well designed to meet the needs of older adults | 1,230 | 42.1 |
| How negative views about older adults contribute to abuse and neglect (for example, assumptions about the mental competence of older adults) | 1,132 | 38.8 |
| Ageist policies and practices that negatively impact the financial security of older adults (for example, employment policies, pension policies) | 1,080 | 37.0 |
| Issues with the systems designed to receive reports, investigate, and/or protect older adults from abuse (for example, paternalistic approaches, poor coordination, lack of clarity around the roles of police and social workers and other professionals) | 1,028 | 35.2 |
| Reports of senior abuse not being believed or treated seriously enough | 948 | 32.5 |
| Other. | 28 | 1.0 |
| I don’t believe there are any ageism issues related to the safety and security of older adults | 42 | 1.4 |
| Prefer not to answer | 74 | 2.5 |
- Notes: % shows the percentage of respondents out of 2,920 who selected the response. Respondents were able to select up to 3 responses therefore the percentages do not add up to 100%.
A total of 512 comments and stories were received about ageism and safety and security via the questionnaire (n=501) and the Share Your Story platform/email (n=11). The most important themes that emerged were:
- access to quality affordable housing (n=74)
- designing communities to be age-friendly (n=68)
- ineffective reporting and accountability mechanisms for senior abuse (n=66)
These 3 themes are described in greater detail below. Additional themes that emerged from the stories included: the lack of financial security of older Canadians (n=62); the need for a continuum of housing options for older adults in the community (n=53); the lack of home care, home maintenance, and other supports required to help older adults age in place (n=44); situations of abuse and neglect in long-term care facilities (n=35); and the negative impacts of assumptions about the competency of older adults and removal of decision-making powers (n=34).
Access to quality affordable housing
A major theme in the stories and comments was the importance of access to quality affordable housing for seniors. Some respondents suggested ageism has contributed to housing insecurity experienced by older adults due to failures to ensure adequate retirement incomes and insufficient age-friendly affordable housing options. Respondents were concerned about both the lack of affordable housing for older adults, as well as the quality and safety of the housing that is available (for example, violent tenants, maintenance problems, bugs). Clear links were made by respondents between housing insecurity and financial insecurity. For older adults who rely primarily on government pensions and benefits (for example, CPP/QPP, OAS, GIS), respondents noted these sources of income are generally inadequate to afford quality housing and an adequate standard of living. Older women and older adults living alone were identified in the comments as particularly likely to experience financial insecurity. Multiple stories and examples were provided of older adults forced to live in unsafe living environments due to the lack of quality affordable housing. Several respondents also highlighted the link between affordable housing and the ability of older adults to age in place.
Access to affordable, suitable and adequate housing for adults is a tremendously dire issue. In considering quality of life, in our community specifically, all of our subsidized housing opportunities are riddled with unsafe patrons of all different ages. Our clients are forced to either live in fear in the only rental they can afford, or live beyond their means and have no additional income for food, medication, transportation, leisure.
My elder sister, in her 70s, has sold her home in a smaller centre to be near immediate medical care and family. However, she has been attempting to get a place in the senior housing units in [a large city] since June 2022 to no avail. She was initially told she would get a place after July 11, 2022. However, when she called to inquire after that date, she was told she would not be getting a place. She has serious heart issues, having had a 5-bypass surgery on her heart in 2018. She has mobility issues and uses a scooter. Trying to find another apartment on the main level of a building that she can afford has been almost impossible for her.
My mother cannot afford to live on her own and so she had to move in with one child and eventually with another child. While her children are happy to share their homes with her...she has lost her sense of independence and choice.
Having applied to [housing provider] I was told that I was the 496th on the waiting list and after checking if I had dropped significantly; to my great surprise, I only went down 3 in 1 year. So, I will have a home in 165 years at this rate. Is this acceptable?
My rent represents 63% of my retirement income so how do you expect me to be able to live decently?
Designing communities to be age-friendly
In their comments and stories, respondents observed the need for communities to be age-friendly in design. Consideration should be given to the needs of older adults when designing physical environments, such as streets, parks, stores, community centres, and more. Respondents commented on the need for outdoor spaces and buildings to include features such as benches, paved walking paths, public washrooms, and curb cuts. Respondents noted quality public transportation options should also be available to facilitate mobility. Some respondents highlighted how age-friendly communities are particularly important for older adults who use mobility devices, such as wheelchairs or walkers. It was noted by respondents that age-friendly communities can enhance the safety and quality of life of older adults and promote their social participation.
In smaller communities, like [my community], there have been improvements in walking paths but there are still areas that are unsafe, not just for seniors, but for others to walk. Wheelchair access is almost nonexistent so anyone using a wheelchair can have difficulty using the sidewalks or entering some of the commercial businesses.
Lack of outdoor seating and public washrooms is a concern for older adults. Plus, with aging infrastructure, little attention was made for people with mobility issues – few level entry businesses, curbs, gravel left on streets from the winter.
Where we live there are 2 retirement homes and yet our sidewalks are not maintained or kept snow and ice free in winter. Older folks are staying inside because they don't feel safe going out in winter.
In my own rural area there is no public transportation available to seniors to attend social gatherings. Seniors in my area are experiencing extreme isolation.
Ineffective reporting and accountability mechanisms for senior abuse
A prominent theme that emerged from the comments and stories was the ineffective reporting and accountability mechanisms in place for when senior abuse occurs. Respondents commented that:
- reports of senior abuse may not be believed or may be treated less seriously than other forms of abuse
- older adults may be reluctant to make reports due to not wanting to report a family member
- reporters may fear reprisals from family or friend caregivers, staff, or management
- there are often no clear mechanisms and structures to ensure accountability when serious abuse or neglect occurs
Even when abuse or neglect is potentially criminal in nature, it was noted by several respondents that the police often are not involved. About half of the comments and stories referred specifically to long-term care and group living settings, and respondents observed that while processes are in place to make complaints, reports often are not addressed appropriately, with little accountability or punishment for offenders or the institution.
It is very difficult to file a complaint against the care received in a long-term care facility. When on a Saturday night, a floor has no attendant or nurse for 2 hours, who to call? The police?
My dad's arm was broken in long term care. I launched a quality investigation and they could not establish how it occurred. He is paralyzed on that side so it had to be caught in his wheelchair or someone moved it without realizing it couldn't be moved.
There are no designated policies in place that protect older adults from abuse, unless it’s in a facility. If I suspect abuse of a child I can contact [organization] and they are mandated to complete an investigation to ensure the child is safe. If I have an older adult being abused in the community, unless it’s significant physical/sexual abuse it is difficult to get police involved.
We phoned about an elder abuse in our community and were told that the person being abused was the only person who could report it. This older adult was emotionally unable to do anything about her son-in-law's abuse but her friends were fearful for her physical and mental safety.
Ageism and media and social media
Introduction
Media plays an important role in shaping the views of a society. Research suggests that older adults are often underrepresented in media and media spreads both negative and positive age-based stereotypes about older adults.2 Media is particularly influential in shaping the views of younger people. This is especially true for those who may have limited contact with older adults in their own personal lives.
Roundtable and stakeholder-led consultation feedback
Perpetuation of ageism by media and social media
In the roundtable and stakeholder-led discussions, the most prominent topic of discussion was how media and social media perpetuate ageism within society. Participants observed that older adults tend to be depicted as a homogenous group and media fails to recognize the diversity of older adult experiences. Negative stereotypes (for example, frail older adults, using canes, unable to use technology) as well as positive stereotypes (for example, retirees living a life of luxury, super-fit older adults running marathons) are spread by the media and social media. Participants also commented on the underrepresentation of older adults within media and social media and the lack of attention paid to their voices and interests. The presence of older women in particular was noticed to be missing. It was also observed by several participants that older adults are rarely depicted on television and in advertising doing normal everyday things (for example, taking the bus).
Participants also commented on the tendency in the news media to focus on negative news stories about older adults. Participants acknowledged the positive role that the news media had played in shining a spotlight on issues affecting older adults during the COVID-19 pandemic, with the neglect of older adults in long-term care facilities a prominent example. However, some participants also voiced the concern that the fixation of the news media on long-term care issues and vulnerable older adults contributes to societal perceptions that all older adults are frail and vulnerable. Participants wished to see more balanced portrayals of older adults and their interests in the news media.
The digitalization of communication and information sharing
A key point of discussion in the roundtable and stakeholder-led consultations was the societal changes that are occurring regarding how people communicate and share information. Digitalization has been rapidly occurring in many areas of society and this trend has been accelerated by the COVID-19 pandemic. As described previously in the social inclusion section, due to the digital divide some segments of the older adult population are increasingly being excluded from society. Participants observed that as news media and information increasingly move online, alternative forms that may be preferred by older adults such as print newspapers and radio are disappearing. Several participants highlighted that more information needs to be made available in languages other than English and French. It was recognized by participants that there are positive sides to social media platforms, such as opportunities to bring together people who are separated by distance or have shared interests. Social media can also be used to build connections between younger and older generations. However, participants also stated that there has been a lack of action to address the misinformation, scams, and ageist jokes and attacks that older adults may be exposed to on social media platforms.
Questionnaire feedback
Respondents were asked “What do you believe are the most serious ageism concerns related to media and social media?” and were able to select up to 3 options from a list. The top 2 concerns identified by respondents were:
- the lack of representation of older adults and their views in the media
- discussions or descriptions in media/social media that frame older adults as a burden or drain on society (refer to Table 11)
| Ageism and media and social media concerns | Number | Percentage (%) |
|---|---|---|
| Lack of representation of older adults and their views in the media | 1,400 | 47.9 |
| Discussions or descriptions in media/social media that frame older adults as a burden or drain on society | 1,003 | 34.3 |
| Discussions in media/social media that frame older adults and younger generations as being in competition with each other for resources (for example, the idea that older generations receive more than their fair share of resources) | 881 | 30.2 |
| Older adults being shown in a negative light or as stereotypes on social media | 837 | 28.7 |
| Older adults being shown in a negative light or as stereotypes in the media | 743 | 25.4 |
| Lack of representation of older adults and their views in social media | 669 | 22.9 |
| Influence of ageism in the media/social media on the attitudes of children and young adults towards older adults | 515 | 17.6 |
| Influence of ageism in the media/social media on the attitudes of older adults towards other older adults or themselves | 261 | 8.9 |
| Other | 23 | 0.8 |
| I don’t believe there are any ageism issues related to media and social media | 167 | 5.7 |
| Prefer not to answer | 166 | 5.7 |
- Notes: % shows the percentage of respondents out of 2,920 who selected the response. Respondents were able to select up to 3 responses therefore the percentages do not add up to 100%.
A total of 348 comments and stories were received about ageism and the media and social media via the questionnaire (n=343) and the Share Your Story platform/email (n=5). In general, stories and comments tended to focus more on the media than social media. The most prominent themes that emerged from the comments and stories were:
- underrepresentation of older adults in media (n=82)
- stereotypical or negative portrayals of older adults in media (n=79)
These themes overlapped significantly with the roundtable and stakeholder-led discussions and are described in more detail below. In their comments and stories, respondents also highlighted the intersections between ageism and sexism, with older women perceived as experiencing more negativity and less representation in media and social media. Additional themes that emerged from the stories and comments included: ageist discourses about older adults in the media and social media (n=43); the use of ageist language (and particularly using the terms “Boomer” and “Okay Boomer” in derogatory ways) (n=25); and ageist jokes and harassment on social media (n=22).
Underrepresentation of older adults in the media
The underrepresentation of older adults in the news, television shows, movies, newspapers, and other forms of media was a concern expressed by respondents. The specific case of CTV news ending anchor Lisa LaFlamme’s contract was mentioned by 45 respondents as an example of perceived ageism. Some respondents also noted the news media tends to pay less attention to events, achievements, and issues of importance to older adults. Several respondents also expressed concern about the tendency of the news media to rely on “experts” rather than seeking the opinions and voices of older adults themselves.
The under-representation of people aged 55 and over in social media and/or television is striking.
Discussions in the media are often 'about' seniors as if they are unable or too feeble to speak for themselves.
If someone as successful as Lisa LaFlamme can get terminated, the issue of discrimination against older women in the media is very serious.
Stereotypical and negative portrayals of older adults in media
In their comments and stories respondents brought attention to both the positive (for example, wealthy, super-active) and negative (for example, frail, helpless, cognitively impaired) stereotypes about older adults that are commonly seen in media. Generally, it was felt that portrayals did not adequately represent the diversity of older adults and their experiences. In particular, respondents expressed concerns about the tendency to portray older adults as being in poor physical and/or mental health. Some respondents also noted that media stories rarely recognize the positives of aging and achievements of older adults and tend to focus more on vulnerability and negatives of the aging experience.
Imagery chosen to portray older adults in the media is often very stigmatizing. The category of 'older adult' is very diverse, in terms of age, culture, ethnicity, they are often lumped together as a homogenous group by the media.
I see a lot of media coverage showing older people: sitting staring out a window, making some crafts like doilies, or sitting around. A lot of older people actually do much more. My father had 40 beehives after he retired and at 84 was selling honey and royal jelly. At 65 I am physically active, practicing yoga daily (better than many in their 30s), enjoying weightlifting & cycling, and I'm working on a PhD!
I am impacted by what I see on the screen and when older women are depicted as having difficulty moving quickly, or as being slow to understand what is happening, I wonder if that's what I'm like. Or if I'm not like that now, will I be in the near future? It's difficult to maintain self esteem when older women are portrayed as out of touch or immobile.
Stories about older people in the media tend to be about overcrowded conditions, lack of care, resources… Long term facilities are always shown in a negative light. The caregivers and health care workers get no love.
Too often, advertising portrays older people as either privileged (with photoshopped photos that are unrealistic) or as financially or physically dependent. Although some older people fall into either of these 2 types, this is not representative of the majority of older people in our society.
Strategies to address ageism
Questionnaire feedback: priorities for addressing ageism
In the ageism questionnaire, respondents were asked what theme area they viewed as the highest priority for the implementation of new strategies, initiatives, or programs to address ageism in Canada. Respondents ranked the theme areas in the following order of priority:
- health and health care (n=1,582, 54.2%)
- social inclusion (n=551, 18.9%)
- safety and security (n=450, 15.4%)
- employment (n=179, 6.1%)
- media and social media (n=132, 4.5%)
Aligning with their identification of health and health care and social inclusion as the most important theme areas, respondents ranked the following 2 strategies as the highest priorities for addressing ageism in Canada:
- investments in health/long-term care services for older adults
- programs that build connections between older and younger generations (refer to Table 12)
| Strategies, initiatives, or programs to address ageism | Number | Percentage (%) |
|---|---|---|
| Investments in health/long-term care services for older adults | 1,321 | 45.2 |
| Programs designed for multiple generations (for example, intergenerational programs) that build connections between older and younger generations | 1,254 | 42.9 |
| Initiatives to encourage employers to hire/retain older workers (for example, wage subsidies, tax credits, hiring grants or programs) | 870 | 29.8 |
| Better education for health care, long-term care, and home care providers on caring for older adults | 851 | 29.1 |
| Increased recognition of the contributions of older adults to society | 680 | 23.3 |
| Reforms to legislation, regulations, and/or voluntary codes of practice to prevent age-based discrimination or promote the inclusion of older people in the workplace | 673 | 23.0 |
| Age-friendly communities | 664 | 22.7 |
| Ageism education and awareness campaigns | 610 | 20.9 |
| Education and awareness campaigns that promote the value of older workers | 547 | 18.7 |
| Programs to prevent senior abuse | 434 | 14.9 |
| Other | 45 | 1.5 |
| Prefer not to answer | 12 | 0.4 |
- Notes: % shows the percentage of respondents out of 2,920 who selected the response. Respondents were able to select up to 3 responses therefore percentages do not add up to 100%.
Roundtable and stakeholder-led consultations and questionnaire feedback: strategies to address ageism in Canada
In the ageism questionnaire, an additional 482 open-ended responses about strategies, programs, or initiatives to address ageism in Canada were received. The most frequently mentioned types of strategies, programs, or initiatives were:
- advocacy, education, and governmental organizations
- innovative aging in place and housing models
- non-profit and community-based organizations and programs
- age-friendly communities
- intergenerational initiatives
- strategies to prevent senior abuse
- aging and ageism awareness campaigns
- strategies to support older workers
Annex 3 lists the strategies, programs, and initiatives that were identified in the ageism questionnaire.
Participants in the roundtable and stakeholder-led consultations also provided feedback on strategies, programs, or initiatives to address ageism. These discussions allowed strategies, programs, and initiatives to be explored in greater depth than in the questionnaire, and tended to focus more on how the strategies could be implemented and who should be involved. Annex 4 lists some of the specific strategies, programs, and initiatives that were identified in the roundtable and stakeholder-led consultations, though it does not capture the full depth of the conversations. Due to the significant overlap for some of the responses received, a combined summary of the identified strategies, programs, and initiatives from the questionnaire and consultations is provided below.
Aging and ageism awareness campaigns
In the consultations and questionnaire feedback, promoting positive views of aging and increasing awareness of ageism were identified as important priorities (see Lists 3A, 3B, and 4A in Annexes 3 and 4). Several non-profit, community-based, and advocacy organizations were stated to be promoting the positives of aging or offering ageism education or awareness activities. Advocacy organizations such as FADOQ (previously known as Fédération de l'Âge d'Or du Québec) and CARP (Canadian Association of Retired Persons) were stated to be promoting the rights and interests of older adults. It was also mentioned that a Canadian Coalition Against Ageism has now been established, which will implement a comprehensive Canada-wide program to combat ageism against older adults, while strengthening, protecting, and promoting their human rights. Several consultation participants stated the need to engage a wide range of partners in campaigns (for example, older adults, schools, researchers, health care system, advocacy organizations, and more) and to identify champions in different fields to help celebrate older adults and promote ageism awareness. Indigenous communities were provided as examples of how communities can respect and honour the contributions of older adults. Consultation participants also highlighted the need to move beyond just awareness and advocate for ageism, age-friendly, and accessibility concerns to be taken into account during policy and program development. In order for this to occur, it was emphasized that it will be important for government and organizations to continue to engage in discussions and consultations with older adults about their needs. The adage “Nothing about us without us” was mentioned by several participants.
Building intergenerational connections
Building intergenerational connections was the most commonly described strategy to address ageism in the roundtable and stakeholder-led consultations and also featured prominently in the ageism questionnaire responses (see Lists 3C and 4B in Annexes 3 and 4). Consultation participants and questionnaire respondents provided a variety of examples of initiatives to connect older adults with younger generations (usually students or children) through social and recreational activities (for example, walking clubs, gardening, cooking classes on social media). Intergenerational volunteering opportunities for both older adults (for example, reading buddies, mentors, living library) and younger people (for example, technology education, practical help, visiting long-term care homes) were also identified. A few consultation participants cautioned though that volunteer activities should recognize the strengths of both younger and older participants and include mutual benefits in order to not perpetuate stereotypes about older adults being frail or dependent. Examples of intergenerational housing models were also provided by consultation participants and questionnaire respondents (for example, homesharing, multigenerational housing, daycare centres located at long-term care facilities).
Strategies to encourage the hiring and retention of older workers
In the roundtable and stakeholder-led consultations, a variety of strategies were identified to encourage the hiring and retention of older workers in the workforce, though older workers were less of a focus in questionnaire responses. Consultation participants and questionnaire respondents identified 7 main types of strategies that could be used to encourage the hiring and retention of older workers (refer to Lists 3D and 4C in Annexes 3 and 4):
- education and awareness campaigns to promote the value of older workers to employers
- providing older workers with the opportunity to mentor or train younger workers
- providing older workers with flexible work options such as reduced hours, part-time work options, or flexible hours
- introducing financial incentives to encourage employers to hire older workers (for example, wage subsidies, government funded placements, and more)
- skills training and job matching programs to support older workers to re-enter the labour force
- introducing policies to make workplaces age-friendly
- reviewing tax and pension policies to identify changes that can encourage working in later life
Strategies to prevent senior abuse
While programs to prevent senior abuse were ranked as a lower priority in the ageism questionnaire, strategies to prevent senior abuse were frequently described as necessary to address ageism in the open-ended questionnaire responses and roundtable and stakeholder-led consultations. The most frequently mentioned strategies were presentations, information sessions, or campaigns to raise public awareness and provide education about senior abuse (refer to Lists 3E and 4D in Annexes 3 and 4). Several consultation participants noted that senior abuse education and information needs to be tailored to meet the needs of the target audience, and examples were provided of educational materials that have been specifically developed for northern and Indigenous communities. Participants also stated the need for integrated approaches to be developed and mentioned a variety of stakeholders who could play a role in preventing senior abuse, including police, banks, libraries, postal workers, health care providers, community-based organizations, and advocacy and senior abuse prevention organizations. Police, in particular, were identified as playing an important role, with participants stating the need for training to be provided to police on senior abuse and relevant legislation to be reviewed to ensure proper penalties for senior abuse that is criminal in nature.
Digital technology education and access programs
While there was limited mention of digital technology education and access programs in the questionnaire responses, in the roundtable and stakeholder-led consultations these were commonly mentioned as a strategy to address the digital divide (refer to List 4E in Annex 4). Digital technology education and access programs can provide training to older adults on how to use digital technologies and may also provide older adults with access to free digital devices and internet. Consultation participants identified non-profit organizations, libraries, and student volunteer programs as commonly delivering these types of programs. Digital technology programs were recognized as a strategy that can address several ageism-related concerns:
- digital technology programs can assist older workers to improve their technology skills and increase their employability
- digital technology programs can promote the social participation of older adults and reduce social isolation, and
- digital technology programs can educate older adults on internet safety and security and reduce the risks of scams and fraud
Promoting positive depictions of older adults in media and social media
In the roundtable and stakeholder-led consultations, promoting more positive depictions of older adults in media and social media was identified as a strategy to reduce ageism (see List 4F in Annex 4). Participants wished to see the voices of older adults and diversity of the older adult population reflected in media and social media. There was a desire for more positive stories and celebration of the achievements of older adults in news media, though it was cautioned by some participants that it is important to maintain a balance and also not fall into promoting super senior stereotypes. In addition to more positive stories in news media, participants also recommended more positive and nuanced portrayals of older adults in television, advertising, and visuals. Participants also mentioned the need for: a) older adults to be involved in the creation of media and social media content, and b) journalists, new anchors, and other media content creators to be educated about ageism.
Age-friendly communities
Age-friendly communities were commonly mentioned in the roundtable and stakeholder-led consultations and in the questionnaire comments as a strategy to address ageism (refer to Lists 3F and 4G in Annexes 3 and 4). In Canada, age-friendly initiatives are often based on the age-friendly cities concept of the World Health Organization’s Global Age-Friendly Cities: A Guide.17 The Age-friendly Communities model consists of 8 core areas:
- outdoor spaces and buildings
- transportation
- housing
- social participation
- respect and social inclusion
- civic participation and employment
- communication and information
- community support and health services.
Support non-profit and community-based organizations
In the comments made by respondents in the ageism questionnaire, it emerged that non-profit and community-based organizations have been at the forefront of efforts to address ageism in Canada. Most social, educational, intergenerational, and aging support programs that were identified as addressing ageism were offered by these types of organizations (refer to List 3G in Annex 3). In the roundtable and stakeholder-led consultations, the important role non-profit and community-based organizations play in supporting the social inclusion of older adults was highlighted (refer to List 4H in Annex 4). Consultation participants observed, however, that these organizations are underfunded and rely on short-term grant funding to offer many programs. The New Horizons for Seniors Program, as well as various provincial and local grants, were noted to be playing an important role in supporting these organizations. Consultation participants recommended that more funding be made available to non-profit and community-based organizations and that governments work with these organizations to determine the most effective ways to provide funding for these programs.
Strategies to prevent the social isolation of older adults
In the roundtable and stakeholder-led consultations, the need to prevent the isolation of older adults was emphasized. Consultation participants observed that in order to ensure the inclusion of older adults within our communities, outreach efforts are needed to encourage older adults to participate socially, promote community connections, and support isolated older adults (refer to List 4I in Annex 4). It was also strongly emphasized by consultation participants that care needs to be taken to communicate information about services and activities to older adults in inclusive and age-friendly ways. Consultation participants highlighted the need to provide information in both digital and non-digital formats (for example, pamphlets, posters, newspaper ads, radio, and more) and also to translate information into other languages. Investing in accessible, convenient, and affordable public transportation options was identified by participants as necessary both to meet the essential needs of older adults (for example, travel to medical appointments, grocery store) as well as for older adults to participate socially. Examples of strategies for improving transportation options for older adults included offering low-cost bus passes, providing on-demand bus services, training staff to be age- and dementia-friendly, and providing transportation for older adults for community events.
Aging in place supports and innovative housing models
Both consultation participants and questionnaire respondents recommended the introduction of more home and community-based supports for aging in place. Expanding access to home care and the range of home care services available was a particular priority. When aging at home is no longer possible, participants and respondents recommended the use of innovative seniors’ care and housing models as alternatives to traditional long-term care facilities (refer to Lists 3H and 4J in Annexes 3 and 4). Multiple questionnaire respondents highlighted seniors’ care models from European (for example, Denmark, Finland, Netherlands, Sweden) and other countries (for example, Japan, USA) that they believed Canada could learn from. Denmark, in particular, was noted to have very generous home and community-based supports for aging in place, as well as innovative housing models that offer alternatives to long-term care facilities.
Reforms to modernize health care systems to better meet the needs of older adults
In the roundtable and stakeholder-led consultations, participants identified several health care reforms necessary to modernize the health care system so it can better meet the needs of older adults and address ageism issues within health care (see List 4K in Annex 4). The most frequently suggested reform was changes to the training of health care providers, with more training required on the health care needs of older adults. Consultation participants stated training is necessary not only for physicians, but also for other health care providers such as nurses and personal support workers. It is also important for health care providers to be encouraged to specialize in geriatrics. In recognition of the fact that older adults often have complex health care needs, participants also recommended more multidisciplinary and one-stop shop care models to be implemented. Several participants also suggested that payment models be revised so family physicians can spend more time with older adult patients. Participants suggested the roles of providers such as nurse practitioners, pharmacists, and paramedics could be expanded. Finally, participants recommended reforms be made so older adults and their family and friend caregivers can more easily navigate the health care system. For example, introducing system navigators or patient advocates and improving referral and discharge processes.
References
- World Health Organization. Global Report on Ageism. Published 2020. Accessed March 26, 2022. https://www.who.int/publications/i/item/9789240016866
- Lagacé M, Mérette M, Navaux J, Rodrigues-Rouleau P. An Examination of the Social and Economic Impacts of Ageism. Federal, Provincial and Territorial Ministers Responsible for Seniors; 2020.
- Harris K, Krygsman S, Waschenko J, Laliberte Rudman D, Pruchno R. Ageism and the older worker: A scoping review. Gerontologist. 2018;58(2):1-14.
- Advisory Council on Economic Growth. Tapping Economic Potential through Broader Workforce Participation. Published 2017. Accessed March 15, 2022. https://www.budget.gc.ca/aceg-ccce/pdf/workforce-marche-travail-eng.pdf
- Levy BR, Zonderman AB, Slade MD, Ferrucci L. Memory Shaped by Age Stereotypes over Time. J Gerontol. 2012;67B(4):432-436.
- Levy BR, Slade MD, Pietrzak RH, Ferrucci L. Positive age beliefs protect against dementia even among elders with high-risk gene. PLoS ONE. 2018;13(2):1-8.
- Levy BR, Slade MD, Kunkel SR, Kasl SV. Longevity increased by positive self-perceptions of aging. J Pers Soc Psychol. 2002;83(2):261-270.
- Levy B. Stereotype Embodiment: A Psychosocial Approach to Aging. Curr Dir Psychol Sci. 2009;18(6):332-336.
- Wyman MF, Shiovitz-Ezra S, Bengel J. Ageism in the Health Care System: Providers, Patients, and Systems. In: Ayalon L, Tesch-Römer C, eds. Contemporary Perspectives on Ageism. International Perspectives on Aging, vol 19. Cham: Springer. 2018: 193-212.
- Levy BR, Slade MD, Chang E-S, Kannoth S, Wang S-Y. Ageism Amplifies Cost and Prevalence of Health Conditions. Gerontologist. 2020;60(1):174-181.
- Employment and Social Development Canada. What We Heard – Report on the Roundtable on Social and Economic Inclusion. Employment and Social Development Canada; 2018.
- Shiovitz-Ezra S, Shemesh J, McDonnell/Naughton M. Pathways from Ageism to Loneliness. In: Ayalon L, Tesch-Römer C, eds. Contemporary Perspectives on Ageism. International Perspectives on Aging, vol 19. Cham: Springer. 2018: 131-148.
- Barnes TL, MacLeod S, Tkatch R, et al. Cumulative effect of loneliness and social isolation on health outcomes among older adults. Aging Ment Health. 2021;1-8. doi:10.1080/13607863.2021.1940096
- Pillemer K, Burnes D, Riffin C, Lachs MS. Elder Abuse: Global Situation, Risk Factors, and Prevention Strategies. Gerontologist. 2016;56(Supplement):S194-S205.
- Ballard EL. Housing. In: Palmore EB, Branch L, Harris D, eds. Encyclopedia of ageism. Routledge. 2005: 176-178.
- World Health Organization. Abuse of older people. Published June 13, 2022. Accessed March 10, 2023. https://www.who.int/news-room/fact-sheets/detail/abuse-of-older-people
- World Health Organization. Global age-friendly cities: A guide. Published 2007. Accessed March 21, 2023. https://www.who.int/publications/i/item/9789241547307
Annex 1. Summary of consultation participation
| Date of roundtable | Provinces or territories covered | Type of roundtable | Number of participants |
|---|---|---|---|
| September 21, 2022 | Newfoundland and Labrador | Virtual | 13 |
| September 28, 2022 | Alberta | In-person | 18 |
| October 5, 2022 | British Columbia | Virtual | 17 |
| October 11, 2022 | Saskatchewan | Virtual | 11 |
| October 13, 2022 | Ontario | Virtual | 20 |
| October 17, 2022 | Nova Scotia, New Brunswick, and Prince Edward Island | Virtual | 10 |
| October 25, 2022 | Manitoba | Virtual | 8 |
| October 27, 2022 | Yukon, Northwest Territories, and Nunavut | Virtual | 11 |
| Organization | City | Province or territory | Number of participants |
|---|---|---|---|
| Age Friendly Edmonton | Edmonton | Alberta | 35 |
| Alberta Native Friendship Centre's Association (ANFCA) | Edmonton | Alberta | 20 |
| City of Calgary on behalf of Age-Friendly Calgary | Calgary | Alberta | 28 |
| Cochrane Family & Community Support Services (FCSS) | Cochrane | Alberta | 38 |
| Age Knowble | Vancouver | British Columbia | 29 |
| BC Association of Community Response Networks (BC CRN) - Surrey, BC | Langley | British Columbia | 6 |
| City of Surrey | Surrey | British Columbia | 9 |
| Lionsview Seniors' Planning Society | North Vancouver | British Columbia | 22 |
| The Pender Harbour Health Centre | Madeira Park | British Columbia | 25 |
| United Way British Columbia | Burnaby | British Columbia | 21 |
| Centre on Aging | Winnipeg | Manitoba | 20 |
| Nova Scotia Centre on Aging, Mount Saint Vincent University | Halifax | Nova Scotia | 15 |
| Neilson Park Creative Centre | Toronto | Ontario | 22 |
| Ontario Association of Social Workers | Toronto | Ontario | 8 |
| PEI Seniors Secretariat | Charlottetown | Prince Edward Island | 7 |
| Table de concertation des aînés du Bas-Saint-Laurent | Rimouski | Québec | 62 |
| Table régionale de concertation des aînés de la Côte-Nord | Forestville | Québec | 90 |
Annex 2. Subpopulation responses
| Sample | Yes | No | Not sure if what they experienced was ageism | Prefer not to answer |
|---|---|---|---|---|
| Full sample | 1,413 (48.4 %) | 1,090 (37.3 %) | 410 (14.0 %) | 7 (0.2 %) |
| 55+ | 1,285 (47.9 %) | 1,013 (37.7 %) | 380 (14.2 %) | 7 (0.3 %) |
| 55 to 64 | 326 (52.6 %) | 221 (35.6 %) | 71 (11.5 %) | 2 (0.3 %) |
| 65 to 74 | 667 (48.4 %) | 504 (36.6 %) | 201 (14.6 %) | 5 (0.4 %) |
| 75 to 84 | 265 (43.0 %) | 254 (41.2 %) | 97 (15.7 %) | 0 (0.0 %) |
| 85+ | 27 (37.5 %) | 34 (47.2 %) | 11 (15.3 %) | 0 (0.0 %) |
| Under 55 | 122 (53.3 %) | 77 (33.6 %) | 30 (13.1 %) | 0 (0.0 %) |
| Females | 1,072 (51.9 %) | 695 (33.7 %) | 291 (14.1 %) | 6 (0.3 %) |
| Males | 324 (39.1 %) | 387 (46.7 %) | 116 (14.0 %) | 1 (0.1 %) |
| Urban | 1,078 (49.3 %) | 810 (37.0 %) | 294 (13.4 %) | 5 (0.2 %) |
| Rural | 329 (46.1 %) | 272 (38.1 %) | 112 (15.7 %) | 1 (0.1 %) |
| Indigenous | 33 (64.7 %) | 12 (23.5 %) | 6 (11.8 %) | 0 (0.0 %) |
| Education – High School or below | 96 (31.2 %) | 159 (51.6 %) | 52 (16.9 %) | 1 (0.3 %) |
| Education – Trades, Certificate, or Some College or University | 384 (43.7 %) | 351 (40.0 %) | 139 (15.8 %) | 4 (0.5 %) |
| Education - Undergraduate Degree | 420 (50.8 %) | 295 (35.7 %) | 110 (13.3 %) | 1 (0.1 %) |
| Education – Graduate Degree | 504 (56.8 %) | 278 (31.3 %) | 105 (11.8 %) | 0 (0.0 %) |
| Ethno-cultural or a visible minority | 110 (60.8 %) | 48 (26.5 %) | 23 (12.7 %) | 0 (0.0 %) |
| 2SLGBTQ+ community | 73 (62.4 %) | 30 (25.6 %) | 14 (12.0 %) | 0 (0.0 %) |
| Person with a disability | 200 (68.0 %) | 56 (19.0 %) | 38 (12.9 %) | 0 (0.0 %) |
| Official language minority community | 62 (47.3 %) | 45 (34.4 %) | 24 (18.3 %) | 0 (0.0 %) |
- Notes: Cells show the number of subpopulation respondents who selected the answer and the corresponding percentage of subpopulation respondents. Rows may not add up to 100% due to rounding.
| Sample | Yes | No | Not sure | Not applicable | Prefer not to answer |
|---|---|---|---|---|---|
| Full sample | 1,169 (40.0 %) | 1,373 (47.0 %) | 306 (10.5 %) | 68 (2.3 %) | 4 (0.1 %) |
| 55+ | 1,038 (38.7 %) | 1,311 (48.8 %) | 290 (10.8 %) | 42 (1.6 %) | 4 (0.1 %) |
| 55 to 64 | 306 (49.4 %) | 230 (37.1 %) | 68 (11.0 %) | 15 (2.4 %) | 1 (0.2 %) |
| 65 to 74 | 560 (40.7 %) | 654 (47.5 %) | 143 (10.4 %) | 19 (1.4 %) | 1 (0.1 %) |
| 75 to 84 | 155 (25.2 %) | 379 (61.5 %) | 72 (11.7 %) | 8 (1.3 %) | 2 (0.3 %) |
| 85+ | 17 (23.6 %) | 48 (66.7 %) | 7 (9.7 %) | 0 (0.0 %) | 0 (0.0 %) |
| Under 55 | 127 (55.5 %) | 61 (26.6 %) | 16 (7.0 %) | 25 (10.9 %) | 0 (0.0 %) |
| Females | 949 (46.0 %) | 840 (40.7 %) | 226 (10.9 %) | 46 (2.2 %) | 3 (0.1 %) |
| Males | 209 (25.2 %) | 525 (63.4 %) | 76 (9.2 %) | 18 (2.2 %) | 0 (0.0 %) |
| Urban | 882 (40.3 %) | 1016 (46.5 %) | 238 (10.9 %) | 49 (2.2 %) | 2 (0.1 %) |
| Rural | 281 (39.4 %) | 346 (48.5 %) | 67 (9.4 %) | 19 (2.7 %) | 1 (0.1 %) |
| Indigenous | 31 (60.8 %) | 15 (29.4 %) | 4 (7.8 %) | 1 (2.0 %) | 0 (0.0 %) |
| Education – High School or Below | 77 (25.0 %) | 182 (59.1 %) | 37 (12.0 %) | 11 (3.6 %) | 1 (0.3 %) |
| Education – Trades, Certificate, or Some College or University | 342 (40.0 %) | 415 (47.3 %) | 97 (11.0 %) | 23 (2.6 %) | 1 (0.1 %) |
| Education - Undergraduate Degree | 334 (40.4 %) | 385 (46.6 %) | 89 (10.8 %) | 18 (2.2 %) | 0 (0.0 %) |
| Education – Graduate Degree | 408 (46.0 %) | 384 (43.3 %) | 82 (9.2 %) | 13 (1.5 %) | 0 (0.0 %) |
| Ethno-cultural or a visible minority | 87 (48.1 %) | 67 (37.0 %) | 23 (12.7 %) | 4 (2.2 %) | 0 (0.0 %) |
| 2SLGBTQ+ community | 64 (54.7 %) | 39 (33.3 %) | 9 (7.7 %) | 5 (4.3 %) | 0 (0.0 %) |
| Person with a disability | 168 (57.1 %) | 85 (28.9 %) | 33 (11.2 %) | 8 (2.7 %) | 0 (0.0 %) |
| Official language minority community | 50 (38.2 %) | 63 (48.1 %) | 16 (12.2 %) | 1 (0.8 %) | 1 (0.8 %) |
- Notes: Cells show the number of subpopulation respondents who selected the answer and the corresponding percentage of subpopulation respondents. Rows may not add up to 100% due to rounding.
| Sample | Yes | No | Not sure |
|---|---|---|---|
| Full sample | 1355 (46.4 %) | 966 (33.1 %) | 599 (20.5 %) |
| 55+ | 1,211 (45.1 %) | 890 (33.1 %) | 584 (21.8 %) |
| Under 55 | 141 (61.6 %) | 73 (31.9 %) | 15 (6.6 %) |
| 55-64 | 344 (55.5 %) | 187 (30.2 %) | 89 (14.4 %) |
| 65-74 | 625 (45.4 %) | 467 (33.9 %) | 285 (20.7 %) |
| 75-84 | 222 (36.0 %) | 212 (34.4 %) | 182 (29.5 %) |
| 85+ | 20 (27.8 %) | 24 (33.3 %) | 28 (38.9 %) |
| Females | 1,032 (50.0 %) | 693 (33.6 %) | 339 (16.4 %) |
| Males | 305 (36.8 %) | 266 (32.1 %) | 257 (31.0 %) |
| Urban | 1,017 (46.5 %) | 729 (33.3 %) | 441 (20.2 %) |
| Rural | 329 (46.1 %) | 232 (32.5 %) | 153 (21.4 %) |
| Indigenous | 31 (60.8 %) | 13 (25.5 %) | 7 (13.7 %) |
| Education – High School or Below | 82 (26.6 %) | 113 (36.7 %) | 113 (36.7 %) |
| Education – Trades, Certificate, or Some College or University | 366 (41.7 %) | 309 (35.2 %) | 203 (23.1 %) |
| Education - Undergraduate Degree | 398 (48.2 %) | 273 (33.1 %) | 155 (18.8 %) |
| Education – Graduate Degree | 502 (56.6 %) | 262 (29.5 %) | 123 (13.9 %) |
| Ethno-cultural or a visible minority | 106 (58.6 %) | 52 (28.7 %) | 23 (12.7 %) |
| 2SLGBTQ+ community | 75 (64.1 %) | 28 (23.9 %) | 14 (12.0 %) |
| Person with a disability | 175 (59.5 %) | 86 (29.3 %) | 33 (11.2 %) |
| Official language minority community | 62 (47.3 %) | 47 (35.9 %) | 22 (16.8 %) |
- Notes: Cells show the number of subpopulation respondents who selected the answer and the corresponding percentage of subpopulation respondents. Rows may not add up to 100% due to rounding.
Annex 3. Programs, initiatives and strategies to address ageism identified in the ageism questionnaire
List 3A: Advocacy, education, and governmental organizations
- Fédération de l'Âge d'Or du Québec (FADOQ) (n=35)
- Canadian Association of Retired Persons (CARP) (n=11)
- Seniors for Social Action (Ontario) (n=9)
- AGE-WELL (n=6)
- Councils on Aging (n=6)
- CanAge (n=4)
- Alzheimer's Societies (n=3)
- University for the Third Age (n=3)
- Saskatoon Council on Aging (n=2)
- Ottawa Council on Aging (n=2)
- International Federation on Aging (n=2)
- Establishment of seniors advocate offices (n=2)
- AQDR (n=2)
- AREQ (n=2)
- AQRP (n=1)
- Association Féministe D'Éducation Et D'Action Sociale (n=1)
- Seniors NL (n=1)
- McMaster Institute for Research on Aging (n=1)
- Elders Take Actions (Courtenay, BC) (n=1)
- Congress of Union Retirees of Canada (n=1)
- Ontario Federation of Union Retirees (n=1)
- B’Nai Brith (n=1)
- City of Kitchener Seniors Advisory Council (n=1)
- Advance Care Planning Canada (n=1)
- BC Health Coalition (n=1)
- Office of the Seniors Advocate of BC (n=1)
- Canadian Civil Liberties Association (n=1)
- Arthritis Society (n=1)
- HelpAge International (n=1)
- ADA Australia (n=1)
- Centre for Better Aging UK (n=1)
- University gerontology departments (n=1)
- ARPA Canada (n=1)
- National Advisory Council on Poverty (n=1)
- Simon Fraser University Gerontology Department (n=1)
- Advocacy Centre for the Elderly (n=1)
- Organization Center of Excellence on Aging in Quebec (n=1)
- Public Health Agency of Canada (n=1)
- Canadian Institutes of Health Research (n=1)
- Canadian Frailty Network (n=1)
- Centre for Aging + Brain Health Innovation (n=1)
- Ontario Centres for Learning, Research and Innovation in Long-Term Care (n=1)
- Brenda Strafford Foundation (n=1)
- National Institute on Aging (n=1)
- Retired Teachers Association (n=1)
- RTOERO Foundation (n=1)
- Disease specific education groups (n=1)
- Seniors advocacy groups (n=1)
- Advocacy from community and religious groups (n=1)
- Tables de concertation des aînés du Québec (n=1)
List 3B: Aging and ageism awareness campaigns (n=30)
- WHO Global Campaign to Combat Ageism (n=8)
- Media campaigns on aging/ageism/recognition of older adults (n=4)
- Ageism Awareness Event (A&O) (n=3)
- Canadian Coalition Against Ageism (n=2)
- Ageism Awareness Workshops (Aging and Society Observatory) (n=1)
- Ageism Awareness Campaign (Rural Development Network) (n=1)
- Australia’s ageism campaign (n=1)
- Saskatchewan Seniors Mechanism Media Monitoring (n=1)
- THIRD ACTion Film Festival (n=1)
- Coordination of action against ageism (n=1)
- Aging film festival (n=1)
- Anti-Ageism in the Workplace campaign (City of Toronto) (n=1)
- Old School Anti-Ageism Clearinghouse (n=1)
- ACT project (Concordia University) (n=1)
- Ageism in the Workplace (Concordia University) (n=1)
- International Day of the Older Person (n=1)
- Let’s Stop Ageism (Alberta Council on Aging) (n=1)
List 3C: Intergenerational initiatives (n=63)
- Intergenerational projects and recreational activities (n=11)
- School programs where children/youth visit with seniors in the community or long-term care facilities (n=7)
- Daycares co-located with long-term care facilities (n=5)
- Intergenerational housing options (n=5)
- Grandparents Day (A&O) (n=3)
- Older adults volunteering in schools (n=3)
- Canada HomeShare Program (n=2)
- Homeshare programs (n=2)
- Mentoring Plus Program (Dalhousie University) (n=2)
- La Maison des Grands-Parents (n=2)
- Little Brothers (n=2)
- Youth volunteering to support seniors (n=2)
- Housing university students in seniors’ residences (examples from Netherlands, Nordic countries) (n=2)
- Aga Khan Residence (Calgary, AB) (n=1)
- Pointe Claire's Aid for Seniors program (n=1)
- Old School Intergenerational Projects (n=1)
- Patty’s Place (Oakville, ON) (n=1)
- The iAM Human Conversation eXchange (McMaster University) (n=1)
- The Neighbourhood Network (n=1)
- Soif de vivre Volunteer Center of the Bay (Friendly Visiting/Phonecall Program) (n=1)
- Aging Activisms Collective (n=1)
- Teen programs co-located with long-term care facilities (n=1)
- New parent programs based in long-term care (n=1)
- Intergenerational penpals (n=1)
- Intergenerational days (n=1)
- Seniors Speaker Bureau (n=1)
- Building intergenerational activities into program curriculums (for example, nursing) (n=1)
- West-end Intergenerational Network (n=1)
List 3D: Strategies to support older workers (n=20)
- Flexible work options (n=2)
- Tax credits for older workers (n=2)
- Job matching websites (n=2)
- Top Sixty Over Sixty (n=2)
- CAFE Employment certification program (n=1)
- Job Start (n=1)
- Encouraging employers to hire older workers (n=1)
- Advertising campaigns on the value of older workers (n=1)
- Make older workers a priority category for hiring (n=1)
- Skills training programs for older workers (n=1)
- Wage subsidies for older workers (n=1)
- Amend policies/legislation so working does not negatively impact pensions (n=1)
- “Third Quarter” program (n=1)
- Opportunities for Employment (n=1)
- Supportive workplace policies (n=1)
- Legislation that prevents forced retirement at 65 (n=1)
List 3E: Strategies to prevent senior abuse (n=59)
- Advertisements about senior abuse (for example, campaigns in Québec, Ontario) (n=9)
- Canadian Network for the Prevention of Elder Abuse (n=6)
- BC Association of Community Response Networks (n=6)
- Alberta Elder Abuse Awareness Council (n=3)
- Elder Abuse Prevention Ontario (n=3)
- Fédération de l'Âge d'Or du Québec (FADOQ) Ainé-Avisé Conference (n=3)
- Senior abuse and scam prevention programs (n=3)
- Cybersecurity or cyberbullying programs (n=3)
- Senior abuse awareness days (n=2)
- It’s Not Right Workshops (n=2)
- ReAct Teams (n=2)
- Fédération de l'Âge d'Or du Québec (FADOQ): “It’s not correct” program (n=2)
- Seniors First BC (n=1)
- Atira (n=1)
- Ontario Elder Abuse Networks (n=1)
- Prevent Elder Abuse Manitoba (n=1)
- Lethbridge Elder Abuse Resource Network (n=1)
- Government action plan to counter mistreatment of older adults 2022-2027 (Québec) (n=1)
- Halton Regional Police Service Burlington outreach and education on frauds and scams (n=1)
- Senior Safety Programs in Nova Scotia (n=1)
- Reform of laws to prevent senior abuse (n=1)
- Senior abuse navigators (n=1)
- Senior abuse telephone line (n=1)
- Training volunteers to identify senior abuse (n=1)
- Educational programs and conferences by law enforcement on seniors’ issues (n=1)
- Monitoring by banks to prevent fraud/abuse (n=1)
- Long-term care training on ageism and senior abuse (n=1)
List 3F: Age-friendly community initiatives (n=73)
- Age-Friendly Communities (n=47)
- Municipalités amies des aînés (MADA) (n=16)
- Québec ami des aînés (QADA) (n=2)
- Accessibility of outdoor settings and built environment (n=4)
- Accessible and age-friendly public transportation (n=2)
- Age-Friendly University Status (n=1)
- Senior-friendly portions at restaurants (n=1)
List 3G: Non-profit and community-based organizations and programs (n=92)
- General community-based organizations (n=15)
- General municipal and community recreational activities and supports (n=10)
- Funding/grants for non-profit and community-based organizations (n=5)
- Senior centres (n=4)
- Healthy Aging CORE Alberta (n=3)
- Saskatchewan Seniors Mechanism (n=3)
- General information and referral programs (n=2)
- Increase Recreation in Seniors (IRIS) (n=2)
- Golden Age Clubs (n=2)
- United Way British Columbia Healthy Aging (n=2)
- Healthy Aging CORE BC (n=2)
- ElderCollege programs (n=2)
- Men’s Sheds (n=2)
- SAGE (n=2)
- Retiree associations (n=1)
- Thompson Seniors Community Resource Council Inc (n=1)
- Alliance of Community Health Centres (n=1)
- Church groups (n=1)
- Edmonton Seniors Coordinating Council (n=1)
- Neilson Park Creative Centre (n=1)
- Autumn Services (n=1)
- Community Development Halton (n=1)
- Senior Games (n=1)
- Elders in Motion (n=1)
- NWT Recreation & Parks Association initiatives (n=1)
- GeriActors and Friends (n=1)
- Carya (n=1)
- Golden Circle Seniors Centre (n=1)
- SOS Program (Service Options for Seniors) (n=1)
- Meals on Wheels (n=1)
- La Belle Gang theatre group (n=1)
- YMCA (n=1)
- Grand River Counsel on Aging (n=1)
- Senior Centres Without Walls (n=1)
- Grande Prairie Friendship Centre (n=1)
- Atwater Library Connect Project (n=1)
- Seniors Serving Seniors Return to Health program (n=1)
- New Horizons for 2S-LGBTQ+ Older Adults (n=1)
- Mauritian Chinese Association of Ontario (n=1)
- Mutual aid of Faubourg Quebec (n=1)
- OVS (n=1)
- The Coalition for Maintenance in the Community (COMACO) (n=1)
- Meaningful Groups (Ontario) (n=1)
- CSARN (Art organization) (n=1)
- Maison de la culture in Montreal (n=1)
- Legions (n=1)
- Probus clubs (n=1)
- South Winnipeg Seniors Resource Council (n=1)
- Traveling library programs (for example, bringing services to retirement homes) (n=1)
- GoBoomerang (n=1)
List 3H: Innovative aging in place and housing models (n=94)
- Models of care/housing for older adults in Nordic/Scandinavian countries (n=10)
- Models of care/housing for older adults in Denmark (n=8)
- Aging in place programs (n=7)
- Improvements to home care (n=6)
- Dementia-friendly communities (n=5)
- Innovative models of long-term care (n=4)
- Greenhouse model (n=4)
- Improve quality of life in long-term care (n=4)
- Program of All-Inclusive Care (PACE) (Burlington, ON) (n=3)
- Butterfly model for long-term care (n=3)
- Models of care/housing for older adults in Japan (n=3)
- Co-housing models (n=3)
- Dementia Villages (n=2)
- Montessori model for long-term care (n=1)
- Small scale long-term care homes (n=1)
- Elim Village Retirement Community (n=1)
- Time Bank Volunteering Models (Switzerland) (n=1)
- Initiatives de travail de milieu auprès des aînés en situation de vulnérabilité (ITMAV) (n=1)
- Knollcrest Lodge (Milverton, ON) (n=1)
- Integrated Home Care Program in Alberta (n=1)
- Family managed home care program in Ontario (n=1)
- Directly managed home care programs in US (n=1)
- Nova Scotia home care program (n=1)
- Toronto seniors ombudsman pilot (n=1)
- MINT memory clinic (n=1)
- City of Toronto pilot with 10 homes (n=1)
- Buurtzorg Neighbourhood Care (n=1)
- Close to Home Program (n=1)
- Better at Home (United Way British Columbia) (n=1)
- CLSCs (n=1)
- Abbeyfield model (n=1)
- Home renovation funds (n=1)
- Paid family caregiver program in Newfoundland and Labrador (n=1)
- Supportive housing (n=1)
- Adult day programs (n=1)
- Social prescribing (n=1)
- ACE (n=1)
- Primary Care Networks (n=1)
- Hub and Spoke program in Peel Region (n=1)
- Community-based palliative care (n=1)
- Subsidized housing programs (n=1)
- Bylaws to allow granny suites (n=1)
- NORC Ambassadors Program (n=1)
- More support for family physicians caring for patients with multiple chronic conditions (n=1)
- More nurse practitioners (n=1)
List 3I: Additional strategies (n=35)
- UN Convention on the Rights of Older Persons (n=3)
- Retirement education and planning (n=2)
- Development of seniors’ strategies (n=2)
- Magazine Bel Age (n=2)
- Increase pensions for older adults (n=2)
- 'Co-designing action-oriented mental health conversations between care providers and aging Canadians in the community' (n=1)
- Age-Friendly Healthcare: Inter-professional Training Program (University of Washington) (n=1)
- Minister of Seniors, Canada (n=1)
- Ministre déléguée à la Santé et aux Aînés (Quebec) (n=1)
- Zoomer magazine (n=1)
- Calgary's Bariatric Program (n=1)
- 2SLGBTQ+ Seniors Toolkit (Toronto) (n=1)
- Research by seniors (n=1)
- Prevent discrimination based on relationship status (n=1)
- Human Rights Code (n=1)
- Accessibility act (n=1)
- European Community Agency for Fundamental Rights (n=1)
- Canadian Charter of Rights and Freedoms (n=1)
- Vulnerable persons law (n=1)
- CBC Marketplace (n=1)
- Introduction of federal dental care program (n=1)
- Older Adult Strategy in Waterloo Wellington (n=1)
- Seniors policies in MRC du Rocher Percé (n=1)
- Education about MAID (n=1)
- Prevent frailty (n=1)
- Restore programs for people with disabilities (n=1)
- Provide technology implementation bundles for older adults (n=1)
- International Organization for Standardization (ISO) TC 314 on Ageing Societies (n=1)
- Cultures that value and honour their seniors for valuable experience (n=1)
Annex 4. Programs, initiatives and strategies to address ageism identified in the roundtable and stakeholder-led consultations
List 4A: Aging and ageism awareness campaigns
- Accessibility, age-friendly, and other aging related lenses for programs and policies
- Ageism education and awareness campaigns
- Campaigns that promote the contributions of older adults (for example value of volunteering, caregiving)
- Campaigns that promote the positives of aging
- Champions to promote aging and older adults
- Community-level coalitions of organizations/groups to address ageism
- Develop an elder video storytelling campaign
- Empower older adults to engage in advocacy and action to call out and challenge ageism
- Forming a seniors union to advocate for older adults
- International older persons day celebrations
- Older Adult Resilience Project
- Opportunities for older adults to share their life story
- Radio theatre clips on ageism (Association franco-yukonnaise)
- Reframing Aging Initiative (USA)
- Saskatchewan Blooming Perennials Initiative
- Senior Islanders of the Year Awards (PEI)
- Third Action Film Festival
List 4B: Intergenerational initiatives
- Adopt-a-Grandparent program in New Brunswick
- CALM programs in schools
- Children/youth volunteering in long-term care
- Co-location of older adult and childrens’ programs/services (for example, daycares in long-term care)
- Connecting Generations Task Force
- CORAH 55+ Community Hub
- Credits for students who take intergenerational courses or do intergenerational volunteering
- Cultural sharing opportunities for Indigenous elders and youth
- Education about aging/ageism in schools and universities
- Intergenerational cooking shows
- Intergenerational housing
- Living libraries
- Media Mentors technology training program
- Multigenerational clubs/groups/community centres
- Intergenerational outdoor programs (for example, gardens, walking programs)
- Port au Port Peninsula senior interviews project
- Programming that incorporates grandchildren
- School programs (for example, pen pals, reading programs)
- Technology training programs
List 4C: Strategies to support older workers
- Accommodations for disabilities, caregiving responsibilities, and more
- Age-friendly business recognition programs/awards (for example,Moosejaw, SK)
- Age-friendly policy lens tool and training for workplaces
- Age-friendly workplace certification (available in the US, similar initiative being introduced in Canada)
- Develop provincial strategies for older workers
- Education/awareness campaigns on the value of older workers
- Encore Careers Research Project
- Government credit for hiring a certain number of mature workers
- Government loans for older adults who want to start a business
- Government of Alberta Taskforce on Aging Workers.
- Include age in workplace equity, diversity, and inclusion policies
- Increase employment/health benefits for older workers
- Internships, work placements, and summer job programs for older workers
- Job matching programs in Edmonston and Moncton, NB and Brandon, MB
- Increased length of EI availability for older workers
- Mentorship programs (such as, older workers mentor younger workers)
- Older worker employment and training programs (for example, Friendship centres, immigrant service organizations, Ontario Society of Senior Citizens Organizations, WorkBC, AARP, Chrysalis, Yukon University, PEI passport to employment)
- Opportunities to earn honorariums or payments for informal work
- Flexible work opportunities (for example, part-time, seasonal, contract, job sharing)
- Project to build age-friendly employer guidelines (Ontario Society of Senior Citizens Organizations)
- Remove mandatory retirement ages
- Research by Nova Scotia Center of Aging on older workers
- Review implications of the duty to accommodate under the Federal Accessibility Act
- Shift mindsets/societal expectations about retirement and work
- Shorter shifts for older workers (particularly in health care, factories, or physically demanding jobs)
- Tax benefits to encourage participation in the labour force
- Top Sixty Over Sixty
- Tourism Industry Association of NS campaign to recruit older workers
- US program “encore.org”
- Wage subsidies
- Wisdom/Vision Keepers Council made up of older workers
List 4D: Strategies to prevent senior abuse
- Affordable legal aid services
- BC Association of Community Response Networks
- BC Council to Reduce Elder Abuse
- Block Watch for seniors
- Bystander Training (Its Not Right: Neighbours, Friends and Family)
- Canadian Network for Prevention of Elder Abuse.
- CPS fraud prevention training
- Cybersafety education
- Education on the concept of entitlement
- Emergency shelters for older adults
- Future Us: A Roadmap to Elder Abuse Prevention
- Interdisciplinary approaches to senior abuse/financial abuse detection and response (for example, police, postal workers, financial institutions, pharmacists, home care, and more)
- Judiciary navigators in community-based organizations such as Friendship Centres
- Police Academy program (Manitoba Association of Senior Centres)
- NWT Senior Society workshops and videos on senior abuse
- Police presentations on scams and fraud (for example, Ontario Provincial Police, RCMP, Winnipeg Police)
- Reforms to banking policies to introduce safeguards
- Review and make amendments to Power of Attorney Act, Personal Directives Act, and Federal Bank Act
- Senior abuse and scam/fraud education and awareness programs (for example, by police, libraries, banks, friendship centres, and more)
- Seniors Safety Society
- Sto:lo Nation "Tales of Singing Bear” DVD on senior abuse
- Telus call protection to help avoid spam/scam calls
- “You and the law” workshops on senior abuse
- Yukon Public Legal Education Association videos on senior abuse in the Northern context
List 4E: Digital technology education and access
- Computers for Schools program (gives computers to non-profits)
- Connected Canadians
- Cyber Seniors
- Digital technology training (for example, at libraries, friendship centres, intergenerational programs, peer programs, employment programs, and more)
- GLUU
- Managing Privacy During Virtual Family Visits: A Toolkit For Care Facility Staff
- New Horizons and United Way funded programs for technology training
- Provision of digital technology in long-term care (for example, Alberta, Northwest Territories)
- Seniors on the Bow – Tech Time
- Yukon Learn (computers for older adults)
List 4F: Media and social media strategies
- Age-positive images & icons – Centre for Ageing Better in the UK
- Education of people working in media/social media on ageism and the positives of aging
- Media and social media campaigns to dispel aging stereotypes
- Opportunities for older adults to collaborate with content creators
- Positive media stories about aging and older adults
- Saskatchewan Seniors Mechanism - Media Monitoring Project
- SNAP Magazine
- Strength-based approaches to storytelling (for example, She is Indigenous campaign)
- Tax credits to encourage media producers to include more age-positive content
- Writing op-eds about the positives of aging
List 4G: Age-friendly community initiatives
- Age Friendly Cochrane
- Age Friendly PEI
- Age friendly training and procedures for hospitals, grocery stores, and other service providers
- Age-friendly communities
- Government funding for age-friendly communities
- Improvements to outdoor settings to enhance walkability (for example, lighting, benches, shoveling snow, and more etc.)
- Modifications to ensure accessibility of buildings and public spaces
- Training on how to influence politicians to adopt age-friendly initiatives (Age-Friendly Summerside and University of California)
- Universal design
List 4H: Non-profit and community-based organizations and programs
- Alberta’s Friendship Centres
- Change New Horizons for Seniors Program funding so a larger proportion can be used for salaries
- Community centres
- Community groups
- Community-based seniors’ services sector in British Columbia
- Dementia-friendly programs
- Drop in lunch and activity programs.
- Government funding for capital investments and infrastructure for seniors’ programs
- Government funding for immigrant service organizations
- Immigrant serving organizations (such as, MOSAIC)
- Lifelong learning programs
- Newcomer Seniors’ Conversation Circles
- Offering online, zoom, and phone programs
- Programming offered by non-profit and community-based organizations (such as, book clubs, community gardens, holiday events, outdoor activities)
- Reform funding for seniors’ programs (for example, more funding, multi-year funding)
- Religious organizations and activities
- Senior Centres Without Walls model
- Seniors Active Living Centres Program funding model (Ontario)
- Senior-specific and age-integrated programs
- STEP program (provides transportation and activities)
List 4I: Strategies to prevent the social isolation of older adults
- Accessible transportation options
- Age-friendly and dementia-friendly training for bus drivers
- COLT: Cochrane On-Demand Local Transit
- Developing seniors resource directories or guides
- Friendly visiting
- Local neighbourhood houses
- Low-cost annual bus passes for older adults (British Columbia)
- Peer support programs
- Programs and activities to build meaningful social connections
- Safety check programs for vulnerable/isolated older adults
- Sentinel Ainé telephone line
- Sharing information in non-digital forms (for example, radio, newspaper, pamphlets, cable news)
- Social prescribing
- Strategies to encourage building and maintaining social networks
- Support from churches, legions, senior centres, community groups, and more. etc.
- Support to navigate transition into retirement
- Telephone reassurance program (Association franco-yukonnaise)
- Training for older adults on how to use public transportation
- Translation of important public information into multiple languages
- UK Campaign to End Loneliness
- Use pharmacists, postal workers, and more, to check-in on and connect older adults with services in the community
List 4J: Innovative aging in place and housing models
- Adult day programs
- Affordable and accessible housing
- Assistive technology in the home to support aging in place
- Community-based seniors services sector in British Columbia
- Co-housing models
- Dementia friendly communities
- Develop a national strategy for elder care for First Nations
- Homeshare models
- Increase access to home care, home support, and expand available services
- Increase access to supports for family and friend caregivers
- Innovative home care model from the Netherlands
- Innovative housing/aging in place models from Denmark
- Intergenerational housing models
- Municipal grants or tax credits for home adaptations
- Netherlands Dementia Village
- Specialized long-term care and assisted living for Indigenous elders (for example, Elders Lodge in Alberta)
- The Caregiving Strategies online courses
List 4K: Health care system reforms to meet the needs of older adults
- Care navigators
- Encourage specialization in geriatrics by health professionals
- Expand the roles of nurse practitioners, pharmacists, paramedics, and more
- Family health teams, one-stop care hubs, and other team-based care models
- Health care models from Denmark and Europe
- Improve referral and discharge pathways
- Increases wages for health care providers working in seniors’ care
- Indigenous health navigators
- Integrated care models (for example, single access point, standardized assessments, matching services to needs, and more)
- Introduce new payment systems for physicians to allow for longer appointments (for example, alternatives to fee-for-service such as salaries or changes to billing)
- Memory clinics (Saskatchewan)
- NavCare.ca – trainers and volunteers
- New Canadians Health Centre
- Patient advocates
- Providing education to health professionals (for example, ageism, age-related changes, dementia care, communicating with older patients)
- Senior-Friendly Care Framework (Regional Geriatric Program of Toronto)
- Streamline the process for immigrant health care workers to obtain credentials
- Update curriculums and textbooks for physicians to improve geriatrics training