Final Audit Report - Audit of the Non-Insured Health Benefits Medical Supplies and Equipment, Vision Care and Mental Health - March 2014
Table of Contents
Executive summary
To support First Nations people and Inuit in reaching an overall health status that is comparable with other Canadians, Health Canada's Non-Insured Health Benefits (NIHB) Program provides coverage for a specified range of drugs, dental care, vision care, medical supplies and equipment, short-term crisis intervention mental health counselling, and medical transportation for approximately 926,000 eligible First Nations people and recognized Inuit.
The objective of the audit was to assess the effectiveness of the management control framework for managing and administering the medical supplies and equipment, vision care, and mental health benefits of the Non-Insured Health Benefits Program. The audit was conducted in accordance with the Treasury Board Policy on Internal Audit and the International Standards for the Professional Practices of Internal Auditing. Sufficient and appropriate procedures were performed and evidence gathered to support the audit conclusion.
Strategic direction is provided through the First Nations and Inuit Health Branch (FNIHB) Strategic Plan. The strategic plan is overseen by several committees. Management and administration of the benefits under scope is a shared responsibility between headquarters and regional offices. The 2012 FNIHB Accountability Framework describes the structure and process to support the new accountability relationship between headquarters and the regional offices. Risk management is integrated into practices and is overseen by a Risk Committee with membership from headquarters and the regions. Each benefit has a risk assessment completed with overall risk ratings, mitigating strategies and accountability. Many of the internal control weaknesses identified in the audit report have been identified by management and are recorded in the benefit risk registry.
All three benefits have similar procedures for claims processing; however only the medical supplies and equipment benefit is managed and administered in a systematic and consistent manner. The audit found regional variations in the administration and process of vision care and mental health benefits. As well, once providers for these two benefits have registered with the Department it is not common practice for their professional standing to be re-validated or for their services to be monitored or audited, whereas the providers of medical supplies and equipment benefits are monitored and are subject to audit. Since the department reimburses the providers of vision care and mental health benefits directly, it would be important for the Department to have formal arrangements with the vision care and mental health Providers.
The medical supplies and equipment claims are administered by the third party supplier on a single IT platform (the Health Information and Claims Processing Services system). Vision care claims are managed and administered on region specific system developed by the Department and mental health claims are managed and administered on different databases and Excel spreadsheets in each region. Having a single platform for the vision care and mental health benefits would better support a national approach, improve system controls around processing of claims and provide for more accessible national data.
Currently the NIHB program does not have personal information banks for vision care and mental health benefits which describes the personal information collected on First Nations and Inuit clients in support of these benefit programs. As well, the privacy impact assessments should be refreshed and requirements for safeguarding, storage and handling of personal information should be reviewed with the regions.
The Program is compliant with the Financial Administration Act and the Treasury Board's Policy on Transfer Payments requirements. The Branch should remind Program staff to complete a change request form in order to remove clauses from the contribution agreement templates to support better documentation in the files.
The audit report includes four recommendations that will serve to strengthen the internal controls for managing and administering the vision care and mental health benefits program.
A - Introduction
1. Background
Aboriginal health is a priority shared by the federal, provincial/territorial governments and First Nations and Inuit communities. The Non-Insured Health Benefits Program is a national program that provides coverage to registered First Nations and recognized Inuit to support them in reaching an overall health status that is comparable with other Canadians. The Non-Insured Health Benefits Program provides coverage for a specified range of medically necessary goods and services when they are not otherwise covered through private insurance plans or provincial/territorial and social programs. In cases where a benefit is covered under another plan, the NIHB Program will act to coordinate payment of those benefits. An eligible recipient must be identified as a resident of Canada and one of the following: a registered Indian according to the Indian Act; an Inuk recognized by one of the Inuit Land Claim organizations; or an infant less than one year of age, whose parent is an eligible recipient.
It is the Government of Canada's position that current health programs and services including Non-Insured Health Benefits be provided to First Nations and recognized Inuit on the basis of national policy and not due to any constitutional or other legal obligations. First Nations assert that health benefits are an inherent Aboriginal and Treaty Right and are constitutionally protected.
Medical Supplies and Equipment
Medical supplies and equipment benefits are covered in accordance with the Pharmacy and Medical Supplies and Equipment Policy Framework and benefit level program policies. To access these benefits, clients must obtain a prescription from a prescriber that is recognized by the NIHB Program, and have their prescription filled at a NIHB-approved provider. Items covered under the benefit include hearing aids and repairs, wheelchairs and walkers, medical supplies, such as bandages and dressings, orthotics and custom footwear, pressure garments, prosthetics, oxygen supplies and equipment, and respiratory supplies and equipment. The regions do the prior approvals and headquarters manages and pays the third party supplier. In fiscal year 2012-13, claims processed through the Health Information and Claims Processing Services (HICPS) system reached $31.2 million, plus $899k was processed through contribution agreements with communities.
Vision care
Vision care benefits are covered in accordance with the policies set out in the NIHB Vision Care Policy Framework and are managed and processed by the regional offices. The Program covers: eye examinations (when they are not insured by the province/territory); eyeglasses that are prescribed by a vision care professional; eyeglass repairs; and other vision care benefits such as contact lenses and tints. A vision care provider must be an optometrist or optician who is licensed/certified and in good standing with the regulatory body of the province/territory of practice. Vision care benefits are managed and processed by the regional offices (83 percent) and through contribution agreements (17 percent) with communities. In 2012-13, NIHB vision care expenditures totalled $32.1 million.
Mental Health
The mental health benefit program covers short-term crisis intervention counselling to address at-risk situations. This service is provided by recognized professional therapists when no other service is available to the client. The mental health benefit covers the following services: initial assessment; development of a treatment plan; mental health treatment by an eligible NIHB provider as per NIHB Program directives: individual; conjoint (with a couple); family; or group (with unrelated individuals) counselling sessions; and fees and associated travel costs for the professional mental health therapist when it is deemed cost effective to provide such services in a community. Some communities provide these benefits under contribution agreements. Program activities are managed and monitored by the regions with each region having its own system. In 2012/13, NIHB's mental health expenditures amounted to $13.9 million, including $9.7 million (70 percent) in direct payments and $4.2 million (30 percent) in transfer payments to communities that provide the equivalent services.
| Operating | Contributions | Total by Benefit | |
|---|---|---|---|
| Medical Supplies and Equipment | $ 31,206,640 | $ 899,583 | $ 32,106,223 |
| Vision Care | $ 26,646,047 | $ 5,487,400 | $ 32,133,447 |
| Mental Health | $ 9,697,163 | $ 4,169,608 | $ 13,866,771 |
| Total by Funding Model | $ 67,549,850 | $10,556,591 | $ 78,106,441 |
| Percentage | 86% | 14% | 100% |
2. Audit objective
The objective of the audit was to assess the effectiveness of the management control framework for managing and administering the medical supplies and equipment, vision care, and mental health benefits of the Non-Insured Health Benefits Program.
3. Audit scope
The audit focused on the management controls within the First Nations and Inuit Health Branch (FNIHB) related to governance, risk management and internal controls for administering the medical supplies and equipment, vision care and mental health benefits. The scope included both procurement contracts and transfer payments and covered financial and non-financial information and analysis. Transactions sampled for examination were from the 2012-13 fiscal year and the first half of 2013-14.
4. Audit approach
The audit was conducted in Health Canada's headquarters and principally in two regions: Ontario and Alberta. The choice of these locations was based on expenditure levels and associated risks. Questionnaires were also sent to the other regional offices to validate processes and controls. The principal audit procedures included:
- interviews (in-person and by phone) with key NIHB personnel at Headquarters and in the regional offices; questionnaires on specific items were also sent to the Regions;
- review of documentation on the systems of governance, risk management and internal controls for the three benefits within the audit scope; and
- detailed examination of a sample of fifty payments to service providers and eight to transfer payment recipients for conformity with the Financial Administration Act, Treasury Board's policies on transfer payments, and program eligibility.
5. Statement of conformance
In the professional judgment of the Chief Audit Executive, sufficient and appropriate procedures were performed and evidence gathered to support the accuracy of the audit conclusion. The audit findings and conclusion are based on a comparison of the conditions that existed as of the date of the audit, against established criteria that were agreed upon with management. Further, the evidence was gathered in accordance with the Internal Auditing Standards for the Government of Canada and the International Standards for the Professional Practice of Internal Auditing. The audit conforms to the Internal Auditing Standards for the Government of Canada, as supported by the results of the quality assurance and improvement program.
B - Findings, recommendations and management responses
1. Governance
1.1 Strategic direction
Audit criterion: Strategic direction for medical supplies and equipment, vision care and mental health benefits is established.
The First Nations and Inuit Health Branch (FNIHB) recently approved its Strategic Plan, a long-term guiding document for the Branch. The Plan is focused on improved access and quality of health services; new partnerships to leverage resources through health service integration and adaptation; and increased First Nations and Inuit capacity to deliver health programs and services.
The work of the Branch is operationalized through the Branch Operational Plan and Regional Operational Plan. The non-insured health benefits in scope are included in both plans as they are coordinated nationally but delivered regionally. Furthermore, each benefit is guided by its respective benefit framework and policies which describes the benefit's objectives, client eligibility and processes. Decision-making related to the strategic direction for the non-insured health benefits occurs through the Senior Management Committee and the Regional Executive Forum. These decision-making committees are supported by working-level NIHB committees including the Risk Management Committee and the NIHB Regional Managers Forum, and their sub-benefit working groups.
The FNIHB Senior Management Committee is chaired by the Senior Assistant Deputy Minister with membership including the Assistant Deputy Minister of Regional Operations, Director Generals and Regional Executives. It provides a forum for ongoing management of the Branch and approves the funding allocation. There is a process and formula to allocate funding optimally between the regions. Funding allocation is historically-based but is reviewed every year through a 13-step process. Cost factors impacting on expenditures (that is, epidemics, transportation costs) are used to make adjustments to the overall growth rates to provide a more accurate forecast and determine each region's specific budget allocation.
The Regional Executive Forum is made up of Regional executives and the FNIHB ADM for Regional Operations. It is responsible for carrying out FNIHB's strategy in the Regions. As well, strategic direction for the NIHB Program is provided through numerous committees and processes which form the governance structure. NIHB's progress is monitored by the Branch's Senior Management Committee at mid-year and year-end, and is reported in the Department's Report on Plans and Priorities.
The NIHB Regional Managers Forum is made up of the NIHB regional and Headquarters directors and managers. The Forum meets monthly through conference calls and once a year in person. This forum is also supported by joint committees.
The NIHB Risk Management Committee is chaired by the NIHB's Program Analysis Division. The mandate of the NIHB Risk Management Committee is to develop an accountability framework to manage the risk of inappropriate billing to the Program. The Risk Management Committee includes members from all divisions and benefit areas of the NIHB Directorate, Legal Services, the Portfolio Audit and Accountability Bureau and from the regions and meets quarterly by teleconference.
Each of the benefits under scope also has its own Working Group whose objective is to identify policy gaps and best practices and to report issues to the Regional managers Forum.
In conclusion, strategic direction for medical supplies and equipment, vision care and mental health programs is well established.
1.2 Roles and responsibilities
Audit criterion: Roles and responsibilities for medical supplies and equipment, vision care and mental health programs are documented and understood.
In April 2012, FNIHB developed an accountability framework document. It describes the structure and process to support the new accountability relationship between Headquarters and regional offices. The reorganization was one of the Branch's Economic Action Plan transformation initiatives to improve access and quality of FNIHB-funded health programs and services. The document sets out the division of roles and responsibilities between headquarters and the regions and establishes the formal processes and mechanisms to facilitate implementation and performance measurement. The relationship between headquarters and the regional offices continues to evolve towards the model proposed in the framework document.
The NIHB Director General at headquarters reports to the Senior Assistant Deputy Minister. The Directorate is responsible for national program policy, central coordination, and the provision of support to the regions. Under the Director General are the Program, Policy, and Planning Division, Program Analysis Division, Operational Services and Systems Division, and Benefit Management and Review Services Division.
Program, Policy, and Planning Division is responsible for a range of activities including strategic direction and program policy for NIHB, as well as coordinating the risk management effort and managing the performance reporting process. The Program Analysis Division is responsible for the financial management of the program; provider audit and risk management activities; the negotiation of compensation rates for certain health services provided to the Program; analysis of performance data; production of the NIHB Annual Report; and relationships with provider groups and associations. The Operational Services and Systems Division is responsible for development, maintenance, and management of the key business processes, systems and services required to operate the NIHB Program. This includes management of the Health Information and Claims Processing Services contract and system, and supplier relations including financial controls and accountability, systems and governance issues. The Benefit Management and Review Services Division is a national centre responsible for the review and adjudication of NIHB requests for pharmacy, dental and orthodontic benefits, and providing expert advice and recommendations to FNIHB regions on requests for medical supplies and equipment.
Each Region is led by a Regional Executive who is accountable to FNIHB's Assistant Deputy Minister for Regional Operations, as well as functionally to the Senior Assistant Deputy Minister for the implementation of overall national policy direction and budget management. The regions are responsible for the delivery of vision care and mental health benefits. In each region, the benefits are managed by a regional manager. Regions also have a navigator or helpline to support First Nation and Inuit clients in understanding the existing health services, jurisdictions and the NIHB Program.
Roles and responsibilities for medical supplies and equipment, vision care and mental health benefits are well documented in the FNIHB Accountability Framework.
1.3 Performance measurement strategy
Audit criterion: Management has a strategy to measure the performance for the medical supplies and equipment, vision care and mental health benefit program.
A performance measurement strategy for NIHB is an integral part of managing for results. The organizational objective of NIHB is to provide benefits to clients that: are appropriate to their unique health needs; contribute to the achievement of an overall health status for First Nations and Inuit people that is comparable to that of the Canadian population as a whole; are sustainable from a fiscal and benefit management perspective; and facilitate First Nations/Inuit control at a time and pace of their choosing.
The current elements of the performance measurement strategy are aligned with Health Canada's Program Alignment Architecture for all NIHB benefits. The strategy includes annual indicators for immediate and intermediate outcomes. One immediate outcome being measured by the program is cost-effectiveness and sustainability. It is measured annually by annual growth percentage and ratio of administrative and benefit costs.
In the 2012-13 Departmental Operational Plan the Branch committed to developing performance measures for the three benefits by March 2014. To date, a draft version of performance indicators for medical supplies and equipment has been developed, while measures for vision care and mental health are under development.
The NIHB's Program Analysis Division is responsible for collecting data from the regions at the end of each fiscal year. The Division has the tools to extract national medical supplies and equipment data as it is centrally stored by the third party supplier on the claims processing system. However, NIHB does not have direct access to either vision care or mental health data because each region has its own application and/or database. To mitigate the problem, NIHB relies on financial data gathered from the departmental financial system.
As for benefits managed through contribution agreements data is collected from community recipients. A review and analysis of these activity reports noted a detailed summary of how public funds were spent for health services provided by the recipient. For example, contribution agreements with mental health funding must provide annual reports that include a general overview of the work being done, how the benefits are being delivered, a brief summary of effectiveness, outcomes, any problems encountered and recommendations for improvement. The regional offices could use this information to further inform the overall management of the benefit program.
In conclusion, management has a performance measurement strategy which is in the process of being fully developed and implemented. The program is scheduled for a program evaluation in 2015 which will serve to further strengthen overall program effectiveness.
2. Risk management
2.1 Risk management
Audit criterion: Risks related to administering the benefits are identified, assessed and have mitigating strategies.
Risk management is recognized as a core element of effective public administration. The effective management of risk contributes to improved decision-making, better allocation of resources and, ultimately, better results for First Nations and Inuit. Effective risk management practices can equip the Branch to respond proactively to change and uncertainty by using risk-based approaches and information to enable more effective decision-making.
The Program Policy and Planning Division within NIHB leads the ongoing risk assessment exercise which consists of identifying risks, assessing their potential impact and likelihood of occurrence resulting in an overall risk rating. Risk assessment documentation also indicates implemented and planned mitigation strategies with due dates as well as accountability for each mitigation strategy. Each benefit under scope has its own risk registry. Risks are monitored through a cycle of quarterly reviews by the Risk Management Committee and monthly reviews by the Regional Managers Forum.
Some of the key risks identified for the Medical Supplies and Equipment benefit include: difficulties accessing certain medical supplies and equipment items for clients living in remote areas; the lack of an independent external expert advisory committee; lack of clearly defined pricing for all on medical supplies and equipment items; increased cost-pressures due to emerging medical supplies and equipment technologies; ensuring Program policies align with the expanding scopes of practice of allied health professionals; provider dissatisfaction due to NIHB program documentation requirements; and pressure on NIHB to expand medical supplies and equipment coverage to items not currently covered.
Vision care benefits' risks include: national consistency of coverage; the absence of a national form and process to register providers; the limited measures of Program's performance; risks related to maintaining the evidence-base for the benefit area given the evolving scope of practice of vision care professionals; evolving availability of vision care products via on-line providers; and changing industry standards for prescription duration.
Mental health benefits risks include: national consistency of coverage; limited measures of program performance; regional variations in the application of provider registration policy; lack of detailed policy documentation to support policy coverage decision-making for crisis counselling; lack of ability to conduct post-treatment follow-up with clients; the 'sunsetting' of the funding for the Indian Residential School Program (anticipated impact on NIHB mental health); the evolving scope of practice of mental health care professionals and the evolving industry practices to include emerging technologies like telehealth.
In conclusion, risks related to managing and administering the benefits are identified, assessed and have mitigating strategies.
3. Internal controls
3.1 Claims processing
Audit criterion: There is an effective suite of management controls for claims related to medical supplies and equipment, vision care and mental health benefits.
Medical Supplies and Equipment Suite of Controls
- Contract Governance
- Program and System Controls - including provider registration process and prior approval process
- HICPS claims payment structure
- Pre-payment account verification process - including Next day claim verification
- Post-payment account verification and monitoring
- Provider Audit Program
Medical Supplies and Equipment
Medical supplies and equipment benefits are delivered by recognized medical supply and equipment providers registered with Express Scripts Canada (on contract with Health Canada). The contractor uses the Health Information and Claims Processing Services system to process claims from service providers dispensing benefits to eligible clients. There is a contract (provider agreement) between Express Scripts Canada and the medical supplies and equipment providers which details the terms and conditions under which the provider may submit claims and receive payment for the provision of services.
Claims Processing
In most cases, the NIHB Program must provide prior approval for a claim to be processed. Prior approval decisions are made at the regional level, however there is a national review centre located at headquarters which assists with this determination. Most regions consult the Centre's experts on the eligibility of equipment and associated costs however some regions use their own consultants to conduct the prior approval work. The Review Centre coordinates reviews by 17 consultants with expertise in one of the six specific benefit areas of: audiology; oxygen; orthotics and custom footwear; pressure garments and pressure orthotics; prosthetics; and respiratory. One region typically relies on the advice of a general physician to make very technical benefit decisions.
Express Scripts Canada pays claims and submits a request to NIHB for funding twice a month. NIHB verifies and reconciles the request and forwards it to the Chief Financial Officer Branch for payment. Eighteen medical supplies and equipment transactions were tested for the presence of the required supporting documentation including the eligibility of the item according to the approved benefit list, payment approvals by authorized officers and accuracy of coding. The pre-approval number and the required supporting documentation was on file; the item or treatment requested was on the approved benefit list; payments were made within maximum allowed; payments were approved by an authorized officer for the Cost Centre; and coding was accurate. While no errors were found, there is a risk of over payment. The Health Information and Claims Processing Services system does not have an embedded national pricing policy for most items. Therefore item prices may come from either a national list or a regional list. These price lists are not entered into the system, which means that a regional NIHB analyst may enter any amount up to $10,000 without an automatic system check against a standard item price (unlike the vision care system which has the prices embedded - a hard control). Furthermore, equipment items over the $10,000 threshold must be split and are entered as two different prior approvals making it difficult to monitor higher priced claims. While post-payment verification is done on a small sample of transactions there is no guarantee that it would be included and verified.
The Program is aware of this risk, as evidenced in the risk management documentation. Mitigation measures include plans to establish price files for medical supplies and equipment benefits in the claims processing system. To date, price files have been completed for incontinence products.
Audit Framework
As noted, the contractor performs post-payment verifications as per the terms of the contract with the Department. In addition, NIHB's Program Analysis Division has access to the national data from the claims-processing system to perform its own analysis and monitoring. Audits are conducted by the claims processor on contract however the analysis and selection of audits is directed by NIHB Program Analysis Division at headquarters.
Vision Care
Vision Care Suite of Controls
- Provider registration process and prior approval process
- Program and System Controls
- Vision care regional systems
- Claims payment from regional hub
- Monitoring and audit
Vision care benefits are delivered by optometrists and opticians. Currently the department has registered 6,459 vision care businesses which have multiple eye care providers. In Alberta alone, this represents approximately 35,500 claims annually. The management and processing of vision care benefits are regionally based. As such, providers must register with the regional office. The purpose of registration is to obtain a provider kit which explains the benefit coverage and to obtain the legal address and banking information to facilitate payments. Once registered, the primary interaction between the department and the provider is paying the fee-for-service that pays the provider directly rather than the First Nations or Inuit client. It would be beneficial for the Program to update the benefit guidance to develop a practice to verify registered provider professional status.
Claims Processing
As with all benefits, before a claim can be paid, a prior approval number is issued to the provider. The prior approval process varies somewhat per region. During regional visits it was noted that in Alberta the benefit analyst who issues the Prior Approval also certifies the provider's invoice prior to payment. In Ontario, these duties are segregated: a payment analyst certifies that the invoice matches the prior approval. As well, management reports that in the Ontario region analysts pre-audit each payment, and input payments into the system for uploading to the department's financial system. This additional control allows the program to better track provider activity.
Two regions have per-diem agreements with nine providers to deliver specific services in isolated and remote communities. The other 6,450 providers across the country do not have contracts with the Department. More formal arrangements would allow for better controls related to adhering to the terms and conditions provided to them and stipulating other protections for the Crown such as proper insurance, professional standing and compliance with privacy laws. A formal agreement could also include a clause to allow the right to audit.
The audit tested a sample of 16 regionally managed vision care transactions. The pre-approval number and the required supporting documentation was on file; the item or treatment requested was on the approved benefit list; payments were made within maximum allowed; payments were approved by an authorized officer for the Cost Centre; and coding was accurate. While no errors were found there is no national vision care system, national database or central management of the vision care systems. As a result headquarters has no direct access to uniform and consistent vision care data to perform adequate monitoring.
Audit Framework
In April 2008, headquarters developed a Provider Audit Framework for Vision Care. The intent of the framework is to assist with the prevention and detection of inappropriate billing practices; billing irregularities; validate active licensure of registered providers; determine that services paid for were received by eligible clients; and that providers have retained appropriate documentation to support claims. The framework includes a proposed audit approach and methodology, the lines of enquiry and draft audit criteria, and detailed service provider audit procedures.
Despite a well-documented audit framework, there was no evidence of a structured provider audit plan from headquarters or the regions for vision care (see recommendation 1). While the Framework calls for sample size calculation and random sample selection, the Program Analysis Division performs at most one or two audits per year based on referrals from the regions. For the period of time within the scope of this audit the auditors were not provided the results from any vision care audits conducted.
Mental Health
Mental Health Suite of Controls
- Program and System Controls
- Provider registration process and prior approval process
- Various unique regional systems
- Claims payment from regional hub
- Monitoring and audit
Mental health short term crisis benefits are delivered by psychologists and social workers. Currently the department has registered 1,916 mental health professionals. The management and processing of mental health benefits is regionally based. Similar to vision care, each provider must register with the program however the mental health registration process is more rigorous. In order to become an approved service provider, a professional must submit a request and attach documentation on their experience and qualifications including proof of required education and registration with an appropriate college or a professional association. Applicant documentation submitted is assessed by the program and, if approved, applicants are sent a fee-for-service provider information document which describes the services that may be provided as well as how new clients can be approved based on treatment plan and how to prepare billing.
While Ontario annually requests the professionals' association membership card, the audit did not find evidence that this was a standard practice in all regions. As noted above, maintaining and annually updating documentation on service providers would provide added assurance of continued professional standing.
Claims Processing
As with the other benefits, before a claim can be paid there must be a prior approval however the program automatically pays the initial two sessions to allow the provider to write a treatment plan specific to the needs of the client. The treatment plan, which is to be short term to address a crisis, is reviewed and approved by a mental health expert working for the Department. However each region interprets crisis and short term differently resulting in varying lengths of approved treatment plans and various extensions to previously approved plans. Twenty-three client files were sampled in Alberta and Ontario and it was found that six had received treatment over a span of forty sessions or greater. NIHB staff are of the opinion that 12 to 15 sessions should be the norm, but no guideline exists on the upper threshold number. Beyond 15 sessions, a patient should be referred to community services or the provincial system. Without specific policy guidelines, the concept of crisis counselling is vague, making it difficult to be applied consistently.
During regional visits, it was also noted that in Alberta the benefit analyst who issues the prior approval also certifies the provider's invoice prior to payment. In Ontario, these duties are segregated: a payment analyst certifies that the invoice matches the prior approval. In a sample of 16 mental health transactions, the audit confirmed that: the pre-approval number and the required supporting documentation was on file; the item or treatment requested was on the approved benefit list as per its valid item code; payments were made within maximum and approved by an authorized officer for the Cost Centre; and coding was accurate. However, as noted above, without crisis and short term being defined there is a risk that the benefit is being provided inconsistently between the regions.
Currently, the mental health benefit program has 59 providers hired under per-diem agreements by three regions to deliver specific services in isolated and remote communities. The other 1,857 providers do not have contracts with the Department. As noted, more formal arrangements with the providers would allow for better controls related to adhering to the terms and conditions provided to them and stipulating other protections for the Crown such as proper insurance, professional standing and compliance with privacy laws.
Audit Framework
In April 2008, headquarters developed a Provider Audit Framework for Mental Health. The intent of the framework is the same as with vision care: to assist with the prevention and detection of inappropriate billing practices; billing irregularities; validate active licensure of registered providers; determine that services paid for were received by eligible clients; and that providers have retained appropriate documentation to support claims. The framework includes a proposed audit approach and methodology, the lines of enquiry and draft audit criteria, and detailed service provider audit procedures.
Despite a well-documented framework, there was no evidence of a structured provider audit plan by headquarters or the regions for mental health benefits. While the Framework calls for sample size calculation and random sample selection, the Program Analysis Division performs audits only if they are referred by the regional offices. For the period of time within the scope of this audit the auditors were not provided the results from any mental health audits conducted.
Overall, it was found that the vision care and mental health programs have two operating models with providers for the delivery of the benefits - providers on contract versus providers who have registered without a contract. As noted, none of the fee-for-service Providers are under contract with NIHB. The FNIHB Accountability Framework (2012) noted that management is refocusing regional efforts to putting in place contract services or putting other models in place to reduce pressure on fee for service benefits. However, at the time of the audit, this was not being done yet. As mentioned more formal arrangements with the fee-for-service providers would serve to strengthen controls.
Recommendation 1
It is recommended that the Assistant Deputy Ministers, First Nations and Inuit Health Branch (FNIHB):
- update the benefit management guidelines for vision care and mental health especially as it relates to strengthening controls related to providers; and
- fully implement the provider audit framework for vision care and mental health.
Management response
Building on the NIHB Benefit policies and operational guidelines already in place, the Assistant Deputy Ministers of FNIHB will:
- develop a nationally consistent provider registration agreement (for vision care and mental health providers) which includes the right of the NIHB Program to audit provider billings;
- incorporate provider registration requirements into the benefit Guides;
- implement a provider registration process in these benefit areas; and
- implement a national schedule of provider audits in these benefit areas.
3.2 Privacy
Audit criterion: There are adequate controls to safeguard personal information collected, used and disclosed for the purposes of administering the medical supplies and equipment, vision care and mental health benefits.
The NIHB program collects substantial amounts of personal information for the purpose of providing benefit coverage to its clients. Client numbers, client names, dates of birth, gender, band numbers, residential addresses, diagnoses and treatment plans are some examples of personal information collected by NIHB that must be protected, in compliance with the Privacy Act.
Privacy Training
Health Canada has developed a Non-Insured Health Benefits Privacy Code, which represents a consistent approach to privacy and data protection for personal information collected, used, disclosed and retained by the Program. The objectives of the code are: to set out the NIHB Program's commitments that will ensure responsible and secure handling of personal information collected, used, disclosed and retained for Program delivery, administration and management; and to foster transparency, accountability and increased awareness of the NIHB Program's privacy procedures and practices.
The NIHB Privacy Code applies to all Health Canada employees administering and managing the NIHB Program. Organizations or groups administering NIHB benefits through contribution agreements must comply with privacy requirements found in the schedules and the confidentiality clauses that form part of the Terms and Conditions of the agreement. Health care professionals must respect the privacy codes of their regulatory or licensing bodies.
The NIHB Program has developed an on-line Privacy Training learning tool. Privacy training is mandatory for NIHB employees dealing with personal information. Within the Privacy Training tool there is a Privacy and Contribution Agreements section which provides information to those who administer benefits on behalf of the federal government through contribution agreements. It summarizes their responsibilities regarding the protection of recipients' personal information in accordance with confidentiality clauses in the agreements.
In the regional offices, it was noted that employees would benefit from having a re-fresh on the privacy training as it had been some time since they had received any training on safeguarding personal information. In the Ontario Region, in general, desks were clear of forms that contain personal information, especially after working hours, and cabinets were locked when employees were absent, however, a few exceptions were found. In the Alberta Region, Program staff should be following a clean desk policy and storing sensitive information in locked cabinets. While the two regional office environments are secured as access is limited through access cards, in Alberta the NIHB area can be accessed by employees from other floors making it important to safeguard the personal information (see recommendation 3).
Personal Information Banks
Equally important is the fact that the Department/Program does not have Personal Information Banks for vision care and mental health benefits. Personal Information Banks are descriptions of personal information that are maintained by government institutions about individuals, in support of specific programs and activities. The Privacy Act requires that Personal Information Banks include all personal information that is organized and retrievable by a person's name or by an identifying number, symbol or other particular assigned only to that person. Personal Information Banks must also include personal information that has been or is being used, or is available for use for an administrative purpose.
Privacy Impact Assessments
During 2009-10, NIHB updated its Privacy Impact Assessment on the Health Information and Claims Processing Services system. The internal Audit of NIHB Pharmacy Benefits (June 2011) concluded that the system was compliant with privacy procedures in maintaining the confidentiality of the clients' personal information while administering the Program. Annual Privacy Reviews are completed for the contractors operations for medical supplies and equipment claims that are processed by the contractor.
The audit did find two draft Privacy Impact Assessments that were conducted in the Alberta Region for the mental health system and vision care system. These documents remain in draft format and it is uncertain if the relevant risks were monitored. Many of these risks (rated as low and moderate) are still relevant today. Other regions questioned did not have any privacy impact assessments for the mental health or vision care benefit program.
Recommendation 2
It is recommended that the Assistant Deputy Ministers of the First Nations and Inuit Health Branch (FNIHB) create personal information banks and update the privacy impact assessments for vision care and mental health benefit programs.
Management response
The Assistant Deputy Ministers of FNIHB will ensure that the required Personal Information Banks (PIBs) and Privacy Impact Assessments (PIAs) for vision care and mental health benefits are completed.
3.3 Information systems
Audit criterion: Information systems support the processing of medical supplies and equipment, vision care and mental health benefits.
Medical Supplies and Equipment
The system used for medical supplies and equipment benefits is also used for pharmacy and dental claims and supports the processing of medical supplies and equipment. The system is managed by a claims processor under contract with Health Canada and is used for all medical supplies and equipment claims. Change management controls have been addressed on prior audits of the system with no material findings. An internal audit of NIHB Pharmacy (June 2011) examined security controls and concluded that they were satisfactory. This audit reviewed the contract with the claims processor and interviewed headquarters staff to confirm these controls have been maintained.
Vision Care
The vision care systems are run separately by each region. The vision care system coding was initially developed and implemented by the Ontario Region and the core coding was shared with all Regions, but there are small differences between regions in data formats. These databases are not inter-connected therefore providing less support to the processing of vision care benefits. Consequently there is no national vision care health system, national database or central management of the regional vision care systems and headquarters has no direct access to uniform and consistent vision care data.
The audit team visited two regions and surveyed the other regions and notes that there are no documented change management controls to ensure that changes are managed in accordance with recognized best practices. Specifically, there is no evidence that changes are tested in a controlled environment and are signed off by the business users. Without a formal change management process in place, there is a risk that changes go into production without being tested or approved, which could compromise the integrity of data.
Secondly, systems that manage Protected B information require password changes every 90 days, as per Health Canada's Password Security Order (2007). While access profiles in the Ontario Region for the vision care and mental health systems are defined and managed by an application called NIHB Security Manager, there is access login required. For all other regions, access controls are defined within the vision care system, but there is no requirement for the users to change their password. In addition, passwords are to be constructed using alpha numeric combinations with at least one capital letter and a symbol. The Department would benefit from implementing these controls.
Lastly, for payment and financial reporting purposes, vision care data are transferred into the Department's financial system (SAP). Yet, the system does not provide control totals or reconciliations between the feeder systems and financial data. Without this control, it is difficult to determine if all transactions have been received or acknowledged by the financial system or whether payments are issued more than once.
Some regions report that making enquiries to other regions to ensure that out-of-province clients have not double claimed vision benefits elsewhere within a 24-month period is a manual process that is time-consuming as each region cannot view the other's regional system.
Mental Health
Each region has its own mental health data management system, varying from a simple Excel spreadsheet to an Access database. Like the vision care program, the mental health program has systems that are run separately by each region. These systems were developed individually and are maintained locally. Some regions use Excel spreadsheets, which limits query and reporting capabilities. Consequently there is no national mental health system, national database or central management of the regional mental health systems and headquarters has no direct access to uniform and consistent mental health data. The findings with regards to mental health systems are similar to those made on the vision care system above, namely: control weaknesses around change management; user access and password practices; and the absence of built-in reconciliation features between the management systems and the departmental financial data.
In conclusion, there are control deficiencies in the information systems. Having a single platform for the vision care and mental health benefits would better support a national approach, improve system controls around processing of claims and provide for more accessible and accurate national data.
Recommendation 3
It is recommended that the Assistant Deputy Ministers, First Nations and Inuit Health Branch (FNIHB) address the information and system security matters identified and develop an integrated plan towards a single IT platform for vision care and for mental health.
Management response
The Assistant Deputy Ministers of FNIHB agree to work towards a single IT platform for the vision care and (short term crisis intervention) mental health counselling benefits by including these benefit areas as part of the re-procurement of the national HICPS system.
The Assistant Deputy Ministers of FNIHB will ensure that existing regional IT systems include appropriate controls, and that NIHB regional offices are appropriately secured.
The NIHB Program is committed to protecting client personal information. All NIHB employees (headquarters and regions) must familiarize themselves with the NIHB Privacy Code, and complete privacy training specific to the NIHB Program.
NIHB also has an annual process in which all employees are reminded of their responsibilities with respect to client personal information.
3.4 Contribution agreements
Audit criterion: Contribution contracts are managed in compliance with the Financial Administration Act and Treasury Board's Policy on Transfer Payments.
Some benefits are delivered through transfer payments. Contribution agreements with communities are managed by regional staff. In Ottawa, the Health Funding Arrangements Directorate, which reports to the Assistant Deputy Minister of Regional Operations, provides support to the Regions through policies, guidelines and templates. Until May 2013, Regions had to submit a Change Request Form to the Health Funding Arrangements Directorate if they wished to make changes to any of the standard templates. Since then, change requests may be approved in the Regions.
The community, in conjunction with regional FNIHB staff, writes a work plan towards the delivery of the benefit for inclusion in a contribution agreement. Each region or zone has a Funding Arrangement Unit, responsible for preparing the contribution agreement. Regional managers are responsible for working directly with the communities. These managers can sign agreements up to a pre-determined amount (normally $4M) and can approve the payment release in consultation with Program Managers.
Monitoring of recipient activities is the responsibility of Liaison Officers/Zone Managers. They determine that the recipient complies in particular with the reporting requirements and the terms and conditions of the contribution agreement. They also play a key role in recommending recipient audits or cases where payments should be withheld due to late reporting. Once a year, the Agreement/Recipient Risk Assessment Tool (known as ARRAT) exercise is performed. It is a recipient monitoring tool used throughout FNIHB, which provides general guidance on the level of interaction with communities at higher risk and records particular risks. Data on community activities are collected annually through the community based reporting tool.
Contribution agreements controls tested worked effectively with minor exception. Each contribution agreement sampled had a recipient capacity and readiness assessment completed prior to entering into the agreement for the first time or to upgrade to a more flexible funding model; each had a recipient risk assessment performed over the past year; each had the required reports received from the recipient and approved by FNIHB; each had activities approved that were eligible; and each had payments made in compliance with the requirements of the Financial Administration Act.
The Treasury Board Directive on Transfer Payments has specific requirements relating to transfer payments to Aboriginal recipients and identifies elements that managers responsible for preparing funding agreements are to address in a funding agreement. The Branch has in place a good internal control to ensure the elements are addressed through its change request policy. The policy details the process to be followed if a clause is to be removed from the standard contribution agreement template and expects a change request form to be completed and submitted for approval. If approved, the change request form is left on the contribution agreement file to demonstrate that the element was addressed and considered not required.
The audit tested eight contribution agreements of a total of 59 to verify that the elements identified in the Directive were addressed. There were a few instances where clauses were not included and no change request documentation was found: recognition of federal funding (57 percent); notification to the recipient that the information may be made public (57 percent); and the dispute resolution mechanism (75 percent). There were instances where the official languages clause was missing from the contribution agreement (25 percent) and no change request was found. This clause is optional (to be determined between the Region and the Recipient), however it is mandatory for any Recipient that is delivering services or benefits where there may be an impact on members of either official language group.
Overall, the Program was compliant with the Financial Administration Act and the Treasury Board's Policy on Transfer Payments. It would be beneficial to have the change request forms on file to demonstrate that the elements have been addressed as expected by the policy.
Recommendation 4
It is recommended that the Assistant Deputy Ministers, First Nations and Inuit Health Branch (FNIHB) re-communicate the Change Request Policy so deviations from the standard clauses are documented and approved.
The 2008 Directive on Transfer Payments was integrated into the 2010-11 contribution agreement templates in 2009.
Not all clauses identified in the Directive on Transfer Payments are relevant for FNIHB's contribution agreements. Discretion is provided in the Directive with the inclusion wording such as "at the Minister's discretion," "where appropriate," "are addressed where they are relevant," and "when the Minister deems appropriate" which are referenced in Appendix E (Terms and Conditions for Contributions) and Appendix G (Funding Agreement Provisions for Contributions).
FNIHB contribution agreement templates are standardized for all FNIHB programs. The Assistant Deputy Ministers of FNIHB will issue a reminder to FNIHB staff that deviations from the standard clauses are subject to FNIHB's Change Request Policy for First Nations and Inuit Health Branch Contribution Agreements.
C - Conclusion
The NIHB Program is delivered through a complex network involving service arrangements with health care providers, territorial governments, the private sector, and First Nations and Inuit Benefits. Although the Program is mandated nationally, benefit delivery activities in the benefit areas within the scope of this audit are decentralized.
Overall, the management control framework for the delivery of medical supplies and equipment is appropriate. However, the management control framework for the delivery of vision care and mental health benefits requires improvements. The benefits in scope are well governed and risk managed. The performance measurement strategy, once fully developed for vision care and mental health, will serve to provide the Program with enhanced performance information to guide decision-making.
Going forward, the Program will be well served from reviewing its benefit guidelines for vision care and mental health to implement procedures to have more oversight of the registered providers. The additional provider oversight through more formal arrangements, regional monitoring and headquarters audit will benefit the eligible First Nations and recognized Inuit, the registered providers and the Department as it continues to provide this important health benefit service.
There are controls in place to ensure proper payment release. Controls around the management of medical supplies and equipment benefits, including its information management system are strong. However, this is not the case with the vision care and mental health benefits. The Department will also be well served from developing a single operating platform for vision care and mental health benefits. In addition, regional offices need to develop personal information banks, update privacy impact assessments and monitor the security of personal information kept in office space. Finally the Program was compliant with the Financial Administration Act and the Treasury Board's Policy on Transfer Payments however contribution agreements should demonstrate that all the clauses prescribed by the Treasury Board Directive on Transfer Payments are addressed.
The audit report includes four recommendations that focus on strengthening the internal controls for vision care and mental health benefits.
Appendix A - Lines of enquiry and criteria
| Criteria Title | Audit Criteria |
|---|---|
| Line of Enquiry 1: Governance | |
| 1.1 Strategic direction | Strategic direction for medical supplies and equipment, vision care and mental health benefits is established. |
| 1.2 Roles and responsibilities | Roles and responsibilities for the management of the medical supplies and equipment, vision care and mental health benefits are documented and understood. |
| 1.3 Performance Management Strategy | Management has procedures to measure and report on the performance for the medical supplies and equipment, vision care and mental health benefits. |
| Line of Enquiry 2: Risk management | |
| 2.1 Risk management | Risks related to administering the medical supplies and equipment, vision care and mental health benefits are identified, assessed and have mitigating strategies. |
| Line of Enquiry 3: Internal controls | |
| 3.1 Operationally managed claims processing | There is an effective suite of management controls for managing claims related to the medical supplies and equipment, vision care and mental health benefits. |
| 3.2 Privacy | There are adequate controls to safeguard personal information collected, used and disclosed for the purposes of administering the medical supplies and equipment, vision care and mental health benefits. |
| 3.3 Information systems | Information systems support the processing of medical supplies and equipment, vision care and mental health benefits. |
| 3.4 Contribution agreements | Contribution contracts are managed in compliance with the Financial Administration Act and Treasury Board's Policy on Transfer Payments. |
Appendix B - Scorecard
| Criterion | Rating | Conclusion | Rec # |
|---|---|---|---|
| Governance | |||
| 1.1 Strategic direction | S | Strategic direction is guided by the FNIHB Strategic Plan. The direction for the plan is overseen by several committees. | |
| 1.2 Roles and responsibilities | S | Roles and responsibilities between headquarters and regions are documented in the 2012 Accountability Framework. | |
| 1.3 Performance measurement strategy | NMI | Management has a performance measurement strategy however the indicators for vision care and mental health are yet to be drafted. | |
| Risk Management | |||
| 2.1 Risk management | S | Risks related to managing and administering the three benefits are identified, assessed with mitigating strategies. | |
| Internal Controls | |||
| 3.1 Operationally managed claims processing | NMI MS&E |
There is an effective suite of management controls for medical supplies and equipment. However one of the larger regions relies on a general physician to make very technical benefit decisions. | |
| NI VC |
Regional variation requires a national approach. There is also a need to strengthen provider arrangements and implement the audit framework. | 1 | |
| NI MH |
Regional variation requires a national approach. There is also a need to strengthen provider arrangements and implement the audit framework. | 1 | |
| 3.2 Privacy | S MS&E |
Personal information collected is recorded in personal information banks and controls to safeguard personal information are appropriate. | |
| NI VC |
Updated Privacy Impact Assessments required and personal information banks need to be created. | 2 | |
| NI MH |
Updated Privacy Impact Assessments required and personal information banks need to be created. | 2 | |
| 3.3 Information systems | S MS&E |
Systems controls are found in the contractor's Health Information and Claims Processing Services system. | |
| NI VC |
The benefits management systems are owned and managed locally and are not interconnected between regions. | 3 | |
| NI MH |
Information systems differ from region to region and are inadequate to prevent abuse. | 3 | |
| 3.4 Contribution agreements | NMI MS&E VC MH |
Contribution agreements should demonstrate that all clauses listed in the Treasury Board directive for transfer payments are addressed. | 4 |
S: Satisfactory NMI: Needs Minor Improvement NMO: Needs Moderate Improvement NI: Needs Improvement U: Unsatisfactory UKN: Unknown; Cannot Be Measured MS&E: Medical Supplies and Equipment MH: Mental Health VC: Vision Care |
|||
Appendix C - Program expenditures
| 2011-2012 | 2012-2013 | Yearly Change | |
|---|---|---|---|
| Medical Supplies and Equipment | |||
| Contributions | 852,536 | 899,583 | 47,047 |
| Administration of HICPS | 222,072 | 239,180 | 17,108 |
| Medical and Dental Supplies | 9,334,768 | 9,659,447 | 324,679 |
| Medical Equipment | 20,151,426 | 21,308,013 | 1,156,587 |
| 30,560,802 | 32,106,223 | 1,545,421 | |
| Vision Care | |||
| Contributions | 5,231,683 | 5,487,400 | 255,717 |
| Ophthalmologist, Optician, Optometrist | 24,536,634 | 26,646,047 | 2,109,413 |
| 29,768,317 | 32,133,447 | 2,365,130 | |
| Mental Health | |||
| Contributions | 3,361,357 | 4,169,608 | 808,251 |
| Mental Health Professionals | 8,910,426 | 9,697,163 | 786,737 |
| 12,271,783 | 13,866,771 | 1,594,988 | |
| Total Contributions | 9,445,576 | 10,556,591 | 1,111,015 |
| Total Operating | 63,155,326 | 67,549,850 | 4,394,524 |
| Grand Total | 72,600,902 | 78,106,441 | 5,505,539 |
| Percent Contributions | 13% | 14% | |
| Percent Operating | 87% | 86% | |
Appendix D - Expenditure profile across Canada
Expenditure profile across Canada
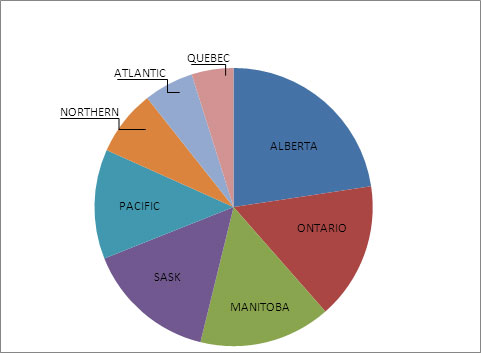
Text description
This pie chart shows the relative size by region of expenditures for the three NIHB benefits under scope, taking into account both contributions and operating activities, averaging the 2011-12 and 2012-13 fiscal years' amounts. The Alberta region has the highest expenditure level with $15,199,691, followed by Ontario with $12,347,103, and Manitoba with $11,869,189. The graphic below breaks down expenditures between contributions and operating activities.
| Average | 2012 Total | 2013 Total | |
|---|---|---|---|
| Contributions | 10,001,083.50 | 9,445,576.00 | 10,556,591.00 |
| NORTHERN | 3,159,406.00 | 3,155,987.00 | 3,162,825.00 |
| ALBERTA | 2,569,849.00 | 2,156,649.00 | 2,983,049.00 |
| PACIFIC | 1,651,093.50 | 1,606,231.00 | 1,695,956.00 |
| ONTARIO | 810,860.00 | 765,812.00 | 855,908.00 |
| MANITOBA | 775,549.50 | 715,000.00 | 836,099.00 |
| SASKATCHEWAN | 505,000.00 | 505,000.00 | 505,000.00 |
| QUEBEC | 323,434.50 | 429,985.00 | 216,884.00 |
| ATLANTIC | 205,891.00 | 110,912.00 | 300,870.00 |
| Operating | 65,225,717.88 | 63,155,326.00 | 67,549,850.00 |
| ALBERTA | 12,629,842.31 | 12,758,327.54 | 12,755,097.31 |
| ONTARIO | 11,536,243.56 | 11,415,015.81 | 11,657,471.31 |
| SASKATCHEWAN | 11,238,321.34 | 10,481,903.87 | 11,994,738.81 |
| MANITOBA | 11,093,640.15 | 10,811,359.27 | 11,375,921.02 |
| PACIFIC | 8,232,846.88 | 8,340,869.35 | 8,124,824.40 |
| ATLANTIC | 4,288,100.94 | 3,571,178.47 | 5,005,023.40 |
| QUEBEC | 3,452,350.13 | 3,115,533.23 | 3,789,167.03 |
| NORTHERN | 2,754,372.59 | 2,661,138.46 | 2,847,606.72 |
| Grand Total | 75,226,801.38 | 72,600,902.00 | 78,106,441.00 |
Page details
- Date modified: