Heat Alert and Response Systems to Protect Health: Best Practices Guidebook
To receive more information about climate change and health activities at Health Canada, please contact: Climatinfo@hc-sc.gc.ca

HC Pub.: 110209
Cat.: H129-9/2011E
ISBN: 978-1-100-19671-8
Acknowledgements
- Davidge, Andrew (GHK International [Canada] Ltd.)
- Dobilas, Geoff (GHK International [Canada] Ltd.)
- Ebi, Kristie L. (Stanford University and Carnegie Institution)
- Fedos, Peter (Surrey Extreme Weather Response Coordinator)
- Hamel, Stephan (New Brunswick Public Health)
- Hersi, Hibak (City of Vancouver)
- King, Norman (Direction de santé publique de l'Agence de la santé et des services sociaux de Montréal)
- Lefebvre, Luc (Direction de santé publique de l'Agence de la santé et des services sociaux de Montréal)
- Luber, George (United States Centers for Disease Control and Prevention)
- McInnes, Judith (Department of Epidemiology and Preventive Medicine, Monash University)
- Morris-Oswald, Toni (Manitoba Health and Healthy Living)
- Pacheco, Elaine (Toronto Public Health)
- Paszkowski, Dawn E. (University of British Columbia)
- Pratt, James (James Pratt Consulting)
- Price, Karine (Direction de santé publique de l'Agence de la santé et des services sociaux de Montréal)
- Richters, Karina (City of Windsor)
- Robinson, Martha (Ottawa Public Health)
- Roy, Lucie-Andrée (Direction de santé publique de l'Agence de la santé et des services sociaux de Montréal)
- Ruf, Fred (Outsourcing Services Inc.)
- Sénécal, Ghyslaine (Agence de la santé et des services sociaux de Montréal)
- Shapiro, Howard (Toronto Public Health)
- Smargiassi, Audrey (Air pollution, climatic changes and health research chair, University of Montréal)
- Sullivan, Sue (Canadian Public Health Association)
Table of Contents
- Foreword
- 1 Introduction
- 2 Risks to Canadians from Extreme Heat
- 3 Preparing for the Health Impacts of Extreme Heat
- 3.4 Developing an Alert Protocol
- 3.5 Developing a Response Plan
- 3.6 Supporting a Heat Alert and Response System with Communication Activities
- 3.7 Improving Heat Alert and Response Systems Through Evaluation
- 3.8 Preventative Action: Reducing Urban Heat
- Appendices
- Appendix A--Questionnaires
- Appendix B--Integration of Extreme Heat into the Assiniboine Regional Health Authority Disaster and Emergency Response Plan
- Appendix C--Information Resources for Developing a Heat Alert and Response System Plan
- Appendix D--Examples of Alert Triggers Used by Canadian Communities
- References
Foreword
Extreme heat poses growing risks to the health of Canadians. Public health and emergency management officials in several Canadian communities are developing interventions to reduce heat-health risks and to prepare for the expected increase in the frequency, duration and severity of extreme heat events due to climate change. To help Canadians protect themselves and their families, health authorities are seeking information about the most effective public health interventions to assist those at risk. A range of actions to safeguard health are being taken, but many remain untested. In support of these efforts, Health Canada is taking action to help Canadians and their communities become more resilient in the face of a changing climate. As more communities in Canada begin to develop systems to reduce risks to health from extreme heat, they will require effective strategies to protect health.
A key adaptation step to protect people from extreme heat events is the development and implementation of Heat Alert and Response System(s) (HARS) by public health and emergency management officials. Heat Alert and Response Systems to Protect Health: Best Practices Guidebook provides an overview of health risks from extreme heat and offers evidence-based strategies for alerting health authorities and the public when hazardous conditions arise. It is intended for use by policymakers, planners and service providers involved in protecting citizens from extreme heat events. The Guidebook is designed to help develop interventions tailored to the needs of a specific community. To this end, the Guidebook provides:

- information on extreme heat events and the potential health risks to Canadians, including those most vulnerable to the impacts
- guidance on assessing heat-health vulnerabilities and adaptation options for a community or a region
- guidance on developing a HARS that addresses heat-health vulnerabilities at population and community levels
- a framework for evaluating the effectiveness of HARS
- examples of preventative measures to reduce ambient temperatures in urban environments
- examples and case studies of interventions drawn from communities across Canada and internationally
The information in this document was developed with support from a range of governmental and non-governmental partners, including experts and stakeholders responsible for providing assistance to vulnerable Canadians during heat emergencies. Lessons learned, as well as best practices for organizing community HARS, are provided to help public health and emergency management officials, in partnership with non-government community organizations, protect the health of Canadians from extreme heat.
1. Introduction
"Heat is an environmental and occupational hazard. The prevention of deaths in the community caused by extreme high temperatures (heat waves) is now an issue of public health concern."
- R.S. Kovats and S. Hajat, 2008, p. 41Footnote 6
Even though heat-related deaths are preventable, extreme heat eventsFootnote a have been associated with sudden, short-term increases in mortality, especially among older adults, those who are chronically ill and socially disadvantaged people.Footnote 6Footnote 9 Increases in morbidity are also observedFootnote 13,Footnote 14; however, they are not as well documented.Footnote 15 As a result, these events have the potential to stress existing health and social services, thereby impacting the provision of these services to the public. Extreme heat events also result in high economic costs to society. It is estimated that the 2003 European extreme heat event cost the affected countries 10 billion euros due to the combined effects of drought, heat stress and fire, resulting in losses in farming, livestock and forestry.Footnote 16
1.1 Overview of Heat Alert and Response Systems
The effects of heat on the health of Canadians will depend upon actions taken by public health and emergency management officials, community health and social service providers, and by individuals to prepare for and respond to the impacts. Research suggests that the health effects of extreme heat are a function ofFootnote 6:
- the duration and severity of an extreme heat event
- when an extreme heat event occurs in the season
- the sensitivity of the population
- the ability of a community to respond during extreme heat events
- actions taken by officials and individuals, particularly the most vulnerable, to manage the risks
To prepare for extreme heat events, some communities in Canada and internationally have developed Heat Alert and Response System(s) (HARS).Footnote 17 These systems have the following core elements described in detail in Section 3:
Community Mobilization and Engagement-- Requires a coordinating agency to prepare the community for the upcoming heat season by identifying community needs, recruiting stakeholders and developing plans to implement a HARS.
Alert Protocol-- Identifies weather conditions that could result in increased morbidity and mortality in the region. The protocol is used to alert the public, as well as government officials and stakeholders, who then take pre-determined actions to protect health.
Community Response Plan-- Facilitates actions by individuals to protect themselves during periods of extreme heat by directing public health interventions aimed at reaching vulnerable individuals who require assistance.

Communication Plan-- Raises awareness about the impacts that heat may have on health, and provides advice through media releases, interviews and websites on how to reduce health risks.
Evaluation Plan-- Assesses HARS activities and facilitates improvements. Aims to evaluate the extent to which implemented measures are timely, relevant, effective, meet local priorities, and contribute to the reduction of health impacts.
A HARS is most effective when it is delivered in conjunction with preventative actions that provide long-term and sustainable protection from extreme heat events (Figure 1).
Figure 1: Community HARS and preventative actions to reduce heat-health risks
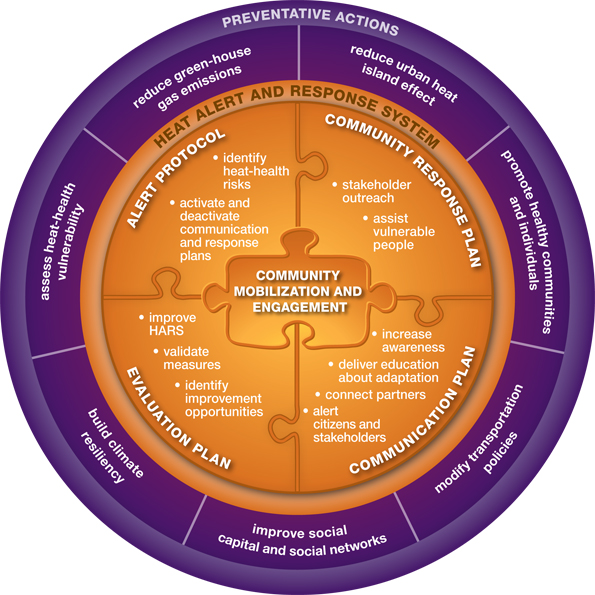
Figure 1: Community HARS and preventative actions to reduce heat-health risks
The figure includes information pertaining to the different components of a Community HARS with preventative actions to reduce heat-health risks. The figure is a circle with four layers. Under the broad category of "Preventative Actions" (layer 1, outer layer), there are seven specific actions (layer 2: reduce urban heat island effect, promote healthy communities and individuals, modify transportation policies, improve social capital and social networks, build climate resiliency, assess heat-health vulnerability and reduce green-house gases. The "Heat Alert and Response System" (layer 3) has 5 core elements (layer 4) that is depicted as five puzzle pieces: Alert Protocol, Community Response Plan, Communications Plan, Evaluation Plan and Community Mobilization and Engagement. Specifically:
- The Alert Protocol specifies to identify heat-health risks and activate and deactivate the communication and response plans.
- The Community Response Plan actions include the need to be involved in stakeholder outreach and assist vulnerable people.
- The Communication Plan highlights the need to increase awareness, deliver education about adaptation, connect partners, and alert citizens and stakeholders.
- The Evaluation Plan actions are to improve HARS, validate measures, and identify improvement opportunities.
- Community Mobilization and Engagement is important for all other core elements and overlaps with Alert Protocol, Community Response Plan, Communication Plan, and Evaluation Plan.
There is a wide disparity across Canada in the measures being used to protect the health of citizens. Measures range from disseminating health protection advice through websites during extreme heat events to full community outreach and response efforts to assist heat-vulnerable populations.Footnote 18Footnote 19 To adapt to extreme heat events, communities need a systematic application of best practices in the development, implementation and evaluation of HARS.
1.2 How the Guidebook Was Developed
Few formal evaluations of HARS in Canada and internationally have been completed. Consequently, the advice and best practices provided in this Guidebook draw from a variety of sources. A literature review was conducted of studies related to:
- climate change and health adaptation
- development and implementation of HARS
- urban heat island mitigation
- communication of heat-health risks to the public
- evaluation of public health programs
The objective was to document the types of measures available to communities to protect citizens through HARS and through preventative actions. The review drew its analysis from original data sources, published and grey literature, and included both peer-reviewed scientific publications and a variety of technical and government reports. Information was obtained from both domestic and international sources; however, international literature was included only when it had a Canadian component or when it provided a theoretical or methodological basis for the analysis that was applicable to the Canadian context.
Expert input was collected from a HARS Advisory Committee, established to guide a Health Canada initiative to develop heat-resilient individuals and communities in Canada. The committee consisted of experts with knowledge and professional experience in the development and implementation of HARS, climate change and health adaptation, public health and emergency management, the needs of heat-vulnerable populations and occupational health. The Guidebook was reviewed by issue experts and public health and emergency management officials in Canada.
The Guidebook also draws from the experiences of Health Canada's four Canadian communities that piloted the development of a HARS from the ground up (Winnipeg, Manitoba; a rural region in Manitoba, within the Assiniboine Regional Health Authority [ARHA]; Windsor, Ontario; Fredericton, New Brunswick).Footnote b These communities used the findings from table-top exercises and heat-health vulnerability assessments to inform their HARS. The Guidebook is supplemented with information from the experiences and evaluation findings of select Canadian communities that currently have a HARS (e.g. Hamilton, Sudbury, Toronto, Ottawa, Kingston, Frontenac, Lennox & Addington in Ontario, and Montréal in Quebec).
2 Risks to Canadians from Extreme Heat
2.1 Relationship Between Heat and Health
The human body tries to maintain a normal core temperature of about 37°C/99°F by constantly regulating the balance of heat gain with heat loss.Footnote 20 Excessive atmospheric temperature in combination with high humidity, radiant solar load and/or metabolic workload (especially without moderate air movement) can overwhelm the body's capacity to thermoregulate and cool itself.Footnote 21
Over-exposure to extreme heat and/or over-exertion for a person's age and/or physical condition in such environments can lead to excessive stress on the body that may result in moderate heat illnesses, such as heat rash, edema, loss of consciousness, cramps and exhaustion. This exposure can also lead to life-threatening heat stroke that may result in severe and long-lasting consequences.Footnote 21 During periods of extreme heat, people may also succumb to underlying health conditions (e.g. respiratory, cardiovascular) that are heat sensitive.

Analysis of morbidity and mortality data from previous extreme heat events reveals that the following population groups are more vulnerable due to underlying risk factors:
- older adultsFootnote 11
- infants and young childrenFootnote 24
- people with chronic illnesses (e.g. psychiatric illnesses) or who are physically impairedFootnote 10
- people taking certain medications that affect heat sensitivity by interfering with the body's cooling functions or water/salt retention (e.g. antihypertensives,Footnote 25 antidepressants,Footnote 26 antipsychotics,Footnote 26Footnote 27 anti-Parkinson's agentsFootnote 27)
- socially disadvantaged individuals (e.g. low-income earners,Footnote 23 homeless people,Footnote 28 people living aloneFootnote 10)
- newcomers to Canada and transient populations
- certain occupational groups (e.g. farmers, construction workers, miners, tree planters)Footnote 30
- those who are physically activeFootnote 13Footnote 33
Early summer extreme heat events generally result in higher health impacts than those occurring later in the summer.Footnote 34 Most people who are regularly exposed to high temperatures become acclimatized to hot environments.Footnote 34Footnote 35 However, the body's ability to acclimatize may be limited for some people, such as those with heart disease,Footnote 36Footnote 37 older adultsFootnote 37 and young children.Footnote 37 Acclimatization is due to physiological adaptation in both cardiovascular and sweating systems.Footnote 38 The benefits of acclimatization lessen as a person's exposure to high temperatures decreases.Footnote 39
Health risks from extreme heat are well documented. Many international and Canadian studies show that daily mortality rates increase when temperatures rise above certain levels.Footnote 40Footnote 41 Recent analysis of the 2009 extreme heat event in British Columbia, an eight-day period where temperatures reached as high as 34.4ºC/93.9ºF (measured at the Vancouver International Airport), suggests that it contributed to 156 excess deaths in the province's lower mainland area.Footnote 42
A historical analysis of annual average mortality associated with extreme heat from 1954 to 2000 found that Montréal, Toronto, Ottawa and Windsor experienced an annual average of 121, 120, 41 and 37 excess deaths, respectively, over this time frame.Footnote 43 In addition, some studies also show a correlation between elevated temperatures and increases in morbidity.Footnote 13 Smaller communities (e.g. rural) also face heat-health impacts.Footnote 44 These impacts are harder to measure due to lower population densities in the communities and consequently fewer deaths.Footnote 45

To further understand the relationship between heat and health in Canada, temperature-mortality curves were developed for Winnipeg, Windsor, Hamilton, Toronto and Fredericton (Figure 2). The curves show that temperature is a health risk in all cities examined and that the temperature-mortality relationship varies among them. For example, in Hamilton relative mortality above 100% (average mortality for June, July and August of each year) was observed at a daily maximum temperature of 26ºC/79ºF, while in Windsor it was detected at 30ºC/86ºF. The rate at which deaths occur as temperatures increase is also variable. In Fredericton, the increase in relative mortality was greater as temperatures increased when compared with Windsor (demonstrated by the slope of the curve in Figure 2). Similar results have been shown for 8 regions in QuebecFootnote 40 and for 15 cities in Europe.Footnote 7 These differences are frequently attributed to local adaptive capacity, differences in vulnerable populations and local climate.Footnote 7 These findings are consistent with published reports that also demonstrate variability between regions, cities and within neighbourhoods.Footnote 7Footnote 47
Daily maximum temperatures during June, July and August from 1986 to 2005 were correlated with all non-traumatic deaths using the Generalized Additive Statistical Model.Footnote 48Footnote 49Footnote cFootnote d
Figure 2: Relationship between daily maximum temperatures in June, July and August, and all non-traumatic deaths for selected Canadian cities, 1986-2005
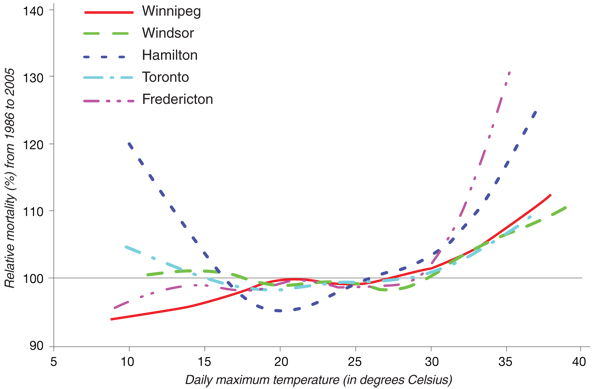
Figure 2: Relationship between daily maximum temperatures in June, July and August, and all non-traumatic deaths for selected Canadian cities, 1986-2005
A graph illustrates the relationships between daily maximum temperatures in June, July and August, and all non-traumatic deaths for selected Canadian cities, 1986-2005. Trend lines demonstrate that temperature is a health risk in all five cities examined and that the temperature-mortality relationship varies among them. Relative mortality above 100% was detected at 27°C/81°F in Winnipeg, 30°C/86°F in Windsor, 26°C/79°F in Hamilton, and 29°C/84°F in Toronto and Fredericton. A sharp increase in the percentage of relative mortality occurs for all cities examined at a daily maximum temperature of approximately 26°C/79°F. No sharp increase in mortality exists for daily maximum temperatures below 26°C/79°F, with the exception of one city; percentage relative mortality in Hamilton increases sharply at temperatures below 16°C/61°F.
Source: Adapted from B. Casati and A. Yagouti, in press.Footnote 50
Heat impacts on health are worse if high temperatures persist over several days and throughout the night. Elevated nighttime temperatures prevent relief from daytime heat and contribute to additional heat stress.Footnote 51 Some regions in urban areas, known as urban heat islands (Section 3.8), trap daytime heat and cool down slower than outside temperatures. The type (e.g. design) and location of a building can have a major influence on individual heat exposure. For example, indoor temperatures can be higher in taller buildings.Footnote 55 Figure 3 illustrates how indoor temperatures in a duplex can remain high even though outdoor temperatures decrease at night.
Figure 3: Comparison between temperatures in a Montréal duplex and in the ambient environment, July 7-9, 2010
Concordia University (Montréal) conducted a study on the indoor thermal conditions in 55 Montréal dwellings to better understand the impact of the urban heat island on indoor conditions during extreme heat. Indoor temperatures (green solid line) measured on the second floor of a two-storey building located on Montréal Island, from July 7 to 9, 2010, are graphed along with outdoor temperatures measured at Montréal's Pierre Elliott Trudeau Airport (orange dashed line). The graph demonstrates that on both days the indoor temperatures reached levels above 34ºC/93ºF. In addition, the lack of cooling at night was detected (shaded areas). The indoor temperature stayed above 31ºC/88ºF while the outdoor temperature was much cooler (about 24ºC/75ºF).
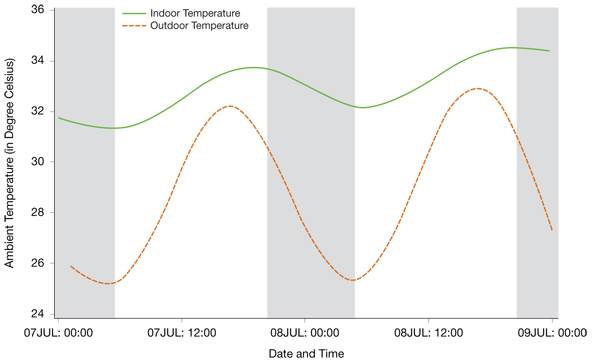
Figure 3: Comparison between temperatures in a Montréal duplex and in the ambient environment, July 7-9, 2010
The graph is a comparison between temperatures in a Montréal duplex and in the ambient environment. Different colour lines indicate indoor temperature (green solid line) and outdoor temperature (orange dotted line) over a two day period, July 7-9, 2010. During the daytime, for both days, ambient indoor temperature reached levels above 34°C/93°F. At night, ambient indoor temperature stayed above 31°C/88°F, thus demonstrating a lack of indoor nighttime cooling. Alternatively, outdoor ambient temperatures exhibited a greater fluctuation over the two day period; temperatures dropped to 24°C/75°F at night and rose to a maximum of 32°C/90°F during the day.
Source: Adapted from K. Park, et al., 2011.Footnote 58
An analysis of temperature trends by Environment Canada revealed that between 1971 and 2000, 29 southern Ontario communities experienced 10 to 15 days annually with temperatures over 30°C/86°F. Another five communities had between 15 to 25 days annually with temperatures over 30°C/86°F.Footnote 59 Some years had more hot days; for example, in 2005, temperatures over 30°C/86°F were recorded in Windsor and Toronto for 47 and 35 days, respectively. Temperature projections (Figure 4) indicate that the number of days with temperatures above 30°C/86°F in Toronto, Winnipeg and Fredericton are expected to almost double between 2041 and 2070. In Windsor, they are expected to more than triple between 2071 and 2100. The projected increase in warm nights will also limit nighttime relief from the heat.
The increased number of extreme heat events resulting from climate change will impact the health of Canadians unless more adaptation efforts are made. For example, without further actions to manage the risks, projections suggest that there will be an increase of 150 excess deaths annually by 2020 in Quebec, 550 excess deaths by 2050 and 1,400 by 2080.Footnote 60 The actual number of deaths may be even higher due to population aging and a general increase in heat vulnerability.Footnote 61
Figure 4: Historical and projected number of hot days and warm nights for selected cities in CanadaFootnote e
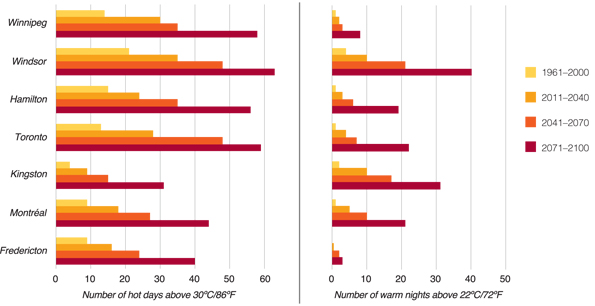
Figure 4: Historical and projected number of hot days and warm nights for selected cities in Canada
Two bar charts show the number of hot days and warm nights, respectively, for seven Canadian cities (Fredericton, Montréal, Kingston, Toronto, Hamilton, Windsor, Winnipeg). The numbers are based on the observed temperature data between 1961 and 2000, and projected for 2011-2040, 2041-2070 and 2071-2100 using Canadian climate models (Scenario A2).
Bar chart for hot days above 30ºC/86ºF reads:
- 1961-2000: Fredericton = 9, Montreal = 9, Kingston = 4, Toronto = 13, Hamilton = 15, Windsor = 22, Winnipeg = 14
- 2011-2040: Fredericton = 16, Montreal = 18, Kingston = 9, Toronto = 28, Hamilton = 24, Windsor = 35, Winnipeg = 30
- 2041-2070: Fredericton = 24, Montreal = 27, Kingston = 15, Toronto = 48, Hamilton = 36, Windsor = 48, Winnipeg 35
- 2071-2100: Fredericton = 40, Montreal = 44, Kingston = 32, Toronto = 59, Hamilton = 56, Windsor = 64, Winnipeg = 58
Bar chart for warm nights above 22ºC/72ºF reads:
- 1961-2000: Fredericton = 0, Montreal = 2, Kingston = 3, Toronto = 2, Hamilton = 2, Windsor = 5, Winnipeg = 2
- 2011-2040: Fredericton = 1, Montreal = 6, Kingston = 10, Toronto = 5, Hamilton = 4, Windsor = 10, Winnipeg = 3
- 2041-2070: Fredericton = 3, Montreal = 10, Kingston = 17, Toronto = 7, Hamilton = 7, Windsor = 22, Winnipeg 4
- 2071-2100: Fredericton = 4, Montreal = 22, Kingston = 32, Toronto = 22, Hamilton = 19, Windsor = 40, Winnipeg = 8.
Source: B. Casati and A. Yagouti, in press.Footnote 50
2.2 Impacts of Air Pollution and Extreme Heat on Health
The health effects of exposure to both air pollution and extreme heat are of concern to public health authorities. There are complex relationships between high atmospheric temperatures, air pollution levels, types of air pollutants, individual behaviours and measures to protect the public. According to the Canadian Medical Association, in 2008 there were 21,000 deaths in Canada associated with the effects of air pollution alone.Footnote 62 Limited evidence suggests that combined exposures to air pollution and extreme heat result in synergistic impacts on health.Footnote 63 Air pollution and extreme heat could combine to impact health in three main ways:
Environmentally--High ambient temperatures increase the formation of air pollutants, such as ground-level ozone.Footnote 63Footnote 64 Air quality can also be affected by forest fires, which occur more often in warmer and dryer climatic conditions.Footnote 65Footnote 66 People exposed to ash and smoke from fires often experience eye irritation and respiratory irritation, leading to bronchitis.Footnote 63Footnote 67
Physiologically--Reduced pulmonary function or heart rate variability due to ozone or particulate matter pollution may lead to inadequate tissue oxygenation, especially under increased cardiovascular stress associated with an increase in thermoregulatory demands.Footnote 68Footnote 69 Compromised respiratory function due to air pollution may also interfere with cardiovascular function during heat stress.Footnote 63
Behaviourally--Individual behaviour during extreme heat events may put people at higher risk to air pollution. People are likely to spend more time outside or leave their windows open, resulting in higher exposure to outdoor pollutants.

Wildfires in Osoyoos, British Columbia, 2003
Properly designed measures to protect people from air pollution and extreme heat can result in immediate health co-benefits for Canadians. For example, reducing ambient temperatures by developing parks to provide shade and dissipate heat through evaporation and transpiration can lead to greater levels of physical activity if they include more walking and biking paths as alternative transportation routes. This can contribute to reduced air pollution and active Canadians, both of which are associated with positive health outcomes.Footnote 70Footnote 71
3 Preparing for the Health Impacts of Extreme Heat
The combined influences of increasing urbanization, an aging population, and a projected increase in the exposure of Canadians to hotter temperatures due to climate change will likely be associated with negative impacts on population health in the absence of further adaptations.Footnote 72 Currently, many communities in Canada and the United States are unprepared to deal with such events.Footnote 53Footnote 73 Many people who are most vulnerable to heat-health risks do not take protective actions during extreme heat. They may not believe their health is at risk or not know about the measures that should be taken.Footnote 29Footnote 77Footnote 78
Health Canada recommends the development and implementation of HARS to prevent, prepare for and respond to health risks from extreme heat.
HARS reduce heat-related morbidity and mortality during extreme heat by alerting the public about the risks, directing the community response to help vulnerable populations, and providing individuals with information and other resources to help them take protective actions before and during an extreme heat event.Footnote 73Footnote 79 The health risks associated with extreme heat events are most effectively reduced by:

- identifying target population groups and areas by conducting vulnerability assessments
- ensuring that a HARS plan is designed to address local needs and priorities
- engaging stakeholders who are best positioned to add value to a HARS
- issuing alerts with a community-specific trigger that is developed based on relationships between heat and health
- providing response measures that reduce heat-health risks and meet the needs of those most vulnerable to heat
- choosing communication strategies that increase awareness and change behaviours
- monitoring HARS activities and evaluating them at the end of the heat season
- implementing long-term preventative actions that reduce heat exposure and negative health outcomes
The following sections of the Guidebook provide information on core elements of HARS and their effective implementation. Given that Canadian communities are diverse (e.g. demographic makeup, population density, unique capacities to issue alerts and mobilize a response), the Guidebook offers multiple approaches that can be adapted to address heat-health risks. Relevant examples of actions to protect health from the experiences of communities in Canada and elsewhere are highlighted to offer useful approaches and tools for public health and emergency management officials.
3.1 Heat Alert and Response Systems to Protect Health
Alert systems that warn of impending dangerous conditions can be used to mobilize community resources to assist people in need. Well-targeted messages and outreach strategies can be effective in raising awareness of heat-health risks and result in behavioural change.Footnote 82 Evaluations of existing HARS, though few in number, demonstrate that these systems help protect people from illness and death associated with extreme heat events.Footnote 79 Analyses of past extreme heat events that resulted in the loss of life suggest that the lack of intervention plans and limited coordination between social services and health organizations were likely major contributing factors to negative health outcomes.Footnote 6

HARS require coordinated actions by government authorities at regional and local levels. Involvement of private sector participants and community groups is also crucial for reaching out to vulnerable groups.Footnote 73 The core HARS elements include:
- community mobilization and engagement
- an alert protocol
- a community response plan
- a communication plan
- an evaluation plan
Table 1 presents the core elements and preventative actions identified in select national and international HARS plans and guidance documents.
Core elements of HARS are implemented at different times. Some activities take place over the whole year (e.g. delivery of preventative actions, stakeholder education and awareness) while others take place during a specific time frame (e.g. public education and awareness, weather surveillance and analysis, evaluation) (Figure 5). The start and end dates for the heat season are determined by the local climate and the possibility of an extreme heat event occurring based on historical climate data and trends.
Weather forecasts are monitored daily during the months when extreme heat may pose a health risk.
When extreme heat is imminent, designated officials determine if the community-specific heat alert triggers have been reached and whether risks to health warrant activation of the HARS. If an alert is issued, internal and external partners are notified through pre-set communication activities, the public is informed of heat-health risks, and community response measures to assist heat-vulnerable people are often put into place.
Continued analysis of weather forecasts determines when weather conditions no longer pose a threat to health. The alert is deactivated through internal and external notifications, followed by a post-event debrief and evaluation. The weather monitoring continues until extreme heat is forecasted again and the HARS is reactivated, or until extreme heat events are unlikely to occur.
Figure 5: Timeline for implementation of core HARS elements and preventative actions
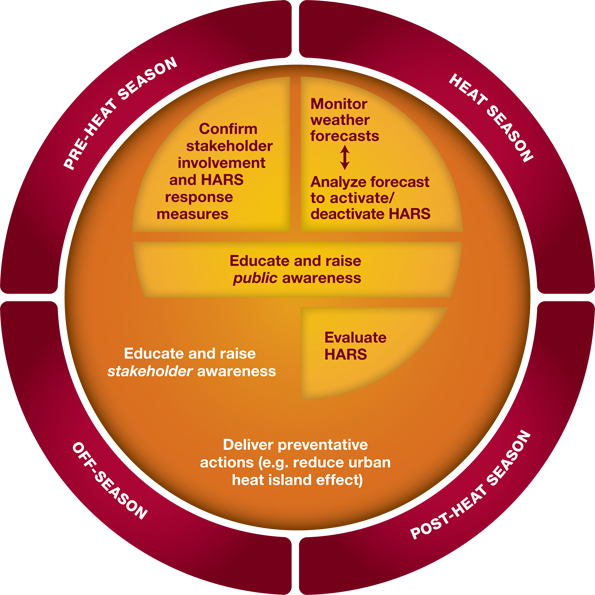
Figure 5: Timeline for implementation of core HARS elements and preventative action
Figure is showing a timeline for implementation of core HARS elements and preventative actions. The figure is divided in four seasons (listed in the outer layer of a circular diagram) within which preventative actions are carried out (described in the inner layer of the circular diagram). The seasons are: Pre-Heat Season, Heat Season, Post-Heat Season and Off-Season. Some actions take place during a specific time period, while others occur throughout the year. In the Pre-Heat Season, actions are to confirm stakeholder involvement and HARS response measures. In the Heat Season, actions are to monitor weather forecasts and analyze the forecast to activate/deactivate HARS. Both the Pre-Heat Season and Heat Season actions are to educate and raise public awareness. During the Post-Heat Season action is to evaluate HARS. Throughout the year, actions are to educate and raise stakeholder awareness and deliver preventative actions (e.g. reduce urban heat island effect).
| WHO | EuroHEAT | U.S. EPA | Australia | England | Canadian Communities | |
|---|---|---|---|---|---|---|
| Community mobilization and engagement--Requires a coordinating agency to prepare the community for the upcoming heat season by identifying community needs, recruiting stakeholders and developing plans to implement a HARS. | ||||||
| Identify a principal coordinating agency | X | X | X | X | X | X |
| Engage broad stakeholders | X | X | X | X | X | X |
| Organize and develop HARS | X | X | X | X | X | X |
| Mobilize community | X | X | X | X | X | X |
| Lead pre-heat season preparations | X | X | X | X | X | X |
| Alert protocol--Identifies weather conditions that could result in increased morbidity and mortality in the region. The protocol is used to alert the public, as well as government officials and stakeholders, who then take pre-determined actions to protect health. | ||||||
| Establish formal alert protocol | X | X | X | X | X | X |
| Reflect local weather conditions | X | X | X | X | X | X |
| Reflect heat-health vulnerabilities | X | X | X | X | X | X |
| Include activation protocol | X | X | X | X | X | X |
| Include deactivation protocol | X | |||||
| Community response plan--Facilitates actions by individuals to protect themselves during periods of extreme heat by directing public health interventions aimed at reaching vulnerable individuals who require assistance. | ||||||
| Establish formal community response plan | X | X | X | X | X | X |
| Include measures tailored to the needs of vulnerable populations | X | X | X | X | X | X |
| Stakeholder driven | X | X | X | X | X | X |
| Communication plan--Raises awareness about the impacts that heat may have on health and provides advice through media releases, interviews and websites on how to reduce health risks. | ||||||
| Establish formal communication plan | X | X | X | X | X | X |
| Develop pre-season education and awareness campaign | X | X | X | X | X | X |
| Identify and plan to address contradictory messages | X | X | X | X | X | |
| Include audience-specific heat-health messages and outreach strategies | X | X | X | X | X | |
| Evaluation plan--Assesses HARS activities and facilitates improvements. Aims to evaluate the extent to which implemented measures are timely, relevant, effective and meet local priorities and contribute to the reduction of health impacts. | ||||||
| Establish formal evaluation plan | X | X | X | X | X | X |
| Implement real-time health surveillance | X | X | X | X | ||
| Hold end-of-season evaluation | X | X | X | X | X | |
| Preventative action: reducing the urban heat island--Addresses heat-health risks through measures designed to reduce urban heat. | ||||||
| Investigate the urban heat island effect | X | X | X | X | ||
| Plan long-term (e.g. implement urban heat island mitigation measures) | X | X | X | X | X | |
3.2 Assessing Vulnerability to the Health Impacts of Extreme Heat
The vulnerability of individuals and communities to the health impacts of extreme heat varies according to the physiological sensitivity of the population, rates of exposure to these events, and the availability of programs and activities that directly or indirectly lower heat-health risks.
Identification of individual- and community-level vulnerabilities before the heat season is necessary to address the rapid onset of heat illnesses and analyze measures to protect health.Footnote 9 These assessments determine existing levels of risk, increase understanding of individual and community vulnerabilities, and direct actions to improve resiliency through the implementation of HARS.Footnote 4 Assessments also gauge community and individual capacity to adapt in the future, and identify responses needed to reduce adverse health impacts. Understanding vulnerability is an iterative process. Assessments improve with increased community involvement and processes that integrate the latest scientific research findings and health data. However, in Canada few formal heat-health vulnerability assessments have been conducted.Footnote g
Vulnerability to the health impacts of extreme heat can often be traced to a combination of factors operating at both individual and community levels.Footnote 10Footnote 83 These includeFootnote 23Footnote 84Footnote 85:
Individual factors
- No air conditioner--or not using it during extreme heat events
- Poor health status--chronic illness, need for medications that increase heat-health risks, dependence on caregiver, poor level of fitness, immobility, cognitive impairment
- Social isolation--limited access to heat-health information and services
- Low income--utility bill arrears, concerns with costs associated with running an air conditioner and accessing other cooling options, living in older housing that may gain heat and retain it even when outdoor temperatures decrease
- Dangerous behaviours during extreme heat events--strenuous physical activity, inadequate hydration, inappropriate clothing
- Type and location of place of work and/or residence--people in occupations with exposure to high temperatures or those living on higher residential floors without air conditioning
Community factors
- Local climate--frequency, length and severity of extreme heat events, humidity levels, nighttime temperatures, seasonal weather variability
- Community design--urban form (e.g. street orientation, building height and density), human activities (e.g. industrial processes, driving) and building materials (e.g. black roofs, concrete surfaces)Footnote 86Footnote 87
- Community characteristics and events--air pollution, outdoor events, influx of tourists
- Limited availability and accessibility of services to cope with extreme heat-- public transportation, drinking fountains, health services, community outreach services, easy-to-access cooling options (e.g. places with air conditioning, community pools)Footnote 22
- Safety and security of citizens--perceived or real threats to personal safety that limit measures taken by individuals to escape the heat (e.g. opening windows, going to cool places)Footnote 88Footnote 89
To help communities assess vulnerability to extreme heat events, Health Canada developed a guidance document, Adapting to Extreme Heat Events: Guidelines for Assessing Health Vulnerability.Footnote 90 Examples of the proposed methods and key tasks relating to six assessment steps are provided in Figure 6. Throughout the assessment, stakeholders should be engaged to provide neighbourhood-level information about the conditions that make specific groups more vulnerable to extreme heat. They can also help identify effective adaption measures to safeguard health, and strategies to overcome barriers to action that individuals and specific population groups may face. A sample partner questionnaire for assessing heat-health vulnerability that Health Canada developed for its pilot communities is provided in Appendix A.
Figure 6: Steps for conducting an extreme heat and health vulnerability assessment
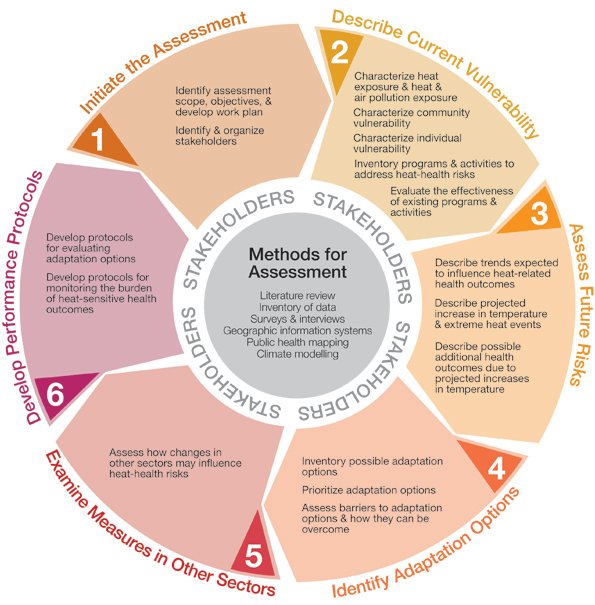
Figure 6: Steps for conducting an extreme heat and health vulnerability assessment
A circular figure illustrates how the assessment guidelines are broken-down into six steps. The objective of the each step is shown on the outside of the parameter of the circle: step 1) initiate the assessment, step: 2) Describe current vulnerability, step 3) assess future risk, step 4) identify adaptation options, step 5) examine measures in other sectors, step 6) develop performance protocols. The individual tasks associated with each steps' objective are included in boxes that form a ring in the circular figure. The task listed for each step read: step 1) identify assessment scope, objectives, and work plan; identify and organize stakeholders: step 2) characterize heat exposure, and heat and air pollution exposure; characterise community vulnerability; characterise individual vulnerability; inventory programs and activities to address heat-health risks; evaluate the effectiveness of existing programs and activities: step 3) describe trends expected to influence heat-related health outcomes; describe projected increase in temperature and heat; describe possible additional health outcomes due to projected increases in temperature: step 4) inventory possible adaptation options; prioritize adaptation options; assess barriers to adaptation options and how they can be overcome: step 5) assess how changes in other sectors may influence heat-health outcomes: step 6) develop protocols for evaluating adaptation options; develop protocols for monitoring the burden of heat-sensitive health outcomes. In the centre of the circular figure, the following research methods that may be applied during an assessment are listed: literature reviews, expert judgement, GIS Climate modelling, surveys, interviews, and public health mapping. Stakeholders are also located in the center of the circular figure to signify that they have an essential role throughout the assessment process.
Source: Reprinted from Health Canada, Adapting to Extreme Heat Events: Guidelines for Assessing Health Vulnerability, 2011.Footnote 90
3.3 Tips for Getting Started
To develop a HARS, it is important to identify an organization that will be responsible for leading the initiative. The lead organization coordinates overall development of the plan, engages partners and assumes the role of, or picks a local champion. The lead agency needs to be clearly identified to all participants. The stakeholders should understand their respective roles and responsibilities and be engaged in all stages of plan development. HARS plans will often differ among municipalities as they take account of the findings of vulnerability assessments related to community-specific needs and characteristics (e.g. regional climate, heat-vulnerable populations, budgetary allocations, organization of public health and emergency management officials, and environments affecting community heat exposure). They are also often integrated into, and complement, existing public health and emergency plans (Appendix B).
3.3.1 Developing a Heat Alert and Response System
Communities should develop a formal HARS plan that provides implementation guidance for alert, response, communication and evaluation components with information onFootnote 72:
- ultimate goals and intermediate objectives
- timelines for HARS activities
- geographic region of coverage
- lead organization
- vulnerable populations and stakeholders
- responsibilities of each partner (e.g. financial, response measures)
- mechanisms for coordinating activities and disseminating information among the lead organization, internal partners, community partners and the public
- back-up response plans for extreme heat and other emergencies (e.g. electricity shut-offs, water shortages)
- steps for phased HARS implementation
- evaluation plans with data requirements and methodologies
- processes and responsibilities for maintaining and updating the HARS plan
Challenges may arise during the initial stages of HARS development (Box 1). To help communities, a wide range of resources is available including guidance for conducting vulnerability assessments, information for health care practitioners on diagnosing and treating heat illnesses, tools for developing HARS communication strategies, and community- and region-specific meteorological and health data (Appendix C).
Box 1: Examples of anticipated challenges during HARS development
- limited human and financial resources
- conflicting priorities of public health and emergency management officials
- data accessibility and limitations (e.g. heat-related morbidity and mortality, accessibility to meteorological forecasts)
- engaging stakeholders and maintaining their interest in heat-health activities
- stakeholder information needs (e.g. data on temperature-mortality relationships, cost-effectiveness of interventions, tailored heat-health messaging products)
- obtaining senior management support for development and approval of a HARS
- coordinating stakeholders, municipal departments and levels of government
- limited understanding of heat-health risks among the public, community health officials and health care providers
3.3.2 Engaging Stakeholders
HARS efforts are most effective when local health officials, social service providers, voluntary agencies and weather service officials are engaged at the planning stages.Footnote 6Footnote 74Footnote 91 For example, representatives from emergency planning organizations, home care services, poverty and literacy agencies, homeless services, tourism centres, and active living and faith-based organizations are needed to ensure that the HARS plan includes partners that are integral to heat-health protection efforts in the community (Figure 7).
Figure 7: Examples of government and community partners participating in the Toronto Hot Weather Response Plan
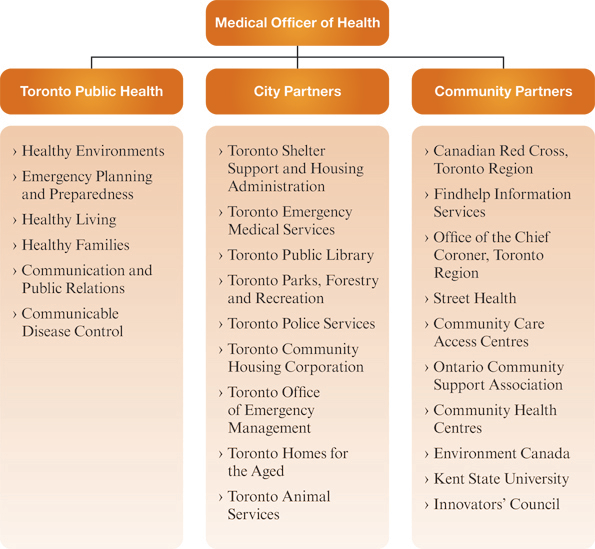
Figure 7: Examples of government and community partners participating in the Toronto Hot Weather Response Plan
A figure provides examples of government and community partners participating in the Toronto Hot Weather Response Plan. A branched diagram lists different partners. At the top is the Medical Officer of Health. The Medical Officer of Health is linked to Toronto Public Health, City Partners and Community Partners. Toronto Public Health partners include: Healthy Environments, Emergency Planning and Preparedness, Healthy Living, Healthy Families, Communication and Public Relations, and Communicable Disease Control. City Partners include: Toronto Shelter Support and Housing Administration, Toronto Emergency Medical Services, Toronto Public Library, Toronto Parks, Forestry and Recreation, Toronto Police Services, Toronto Community Housing Corporation, Toronto Office of Emergency Management, Toronto Homes for the Aged, and Toronto Animal Services. Community Partners include: Canadian Red Cross (Toronto Region), Findhelp Information Services, Office of the Chief Coroner (Toronto Region), Street Health, Community Care Access Centres, Ontario Community Support Association, Community Health Centres, Environment Canada, Kent State University, and Innovators' Council.
Source: Toronto Public Health, 2009.Footnote 92

A stakeholder engagement plan should be developed and followed early in the process (Figure 8). The interest and engagement of stakeholders should be maintained and their contributions acknowledged by keeping them informed of important developments at each stage of the project. This can be achieved through face-to-face meetings, e-mail updates, the provision of detailed notes, and/or involvement in the decision-making process. Pre-season discussions with key stakeholders offer an opportunity to gather input to validate or modify existing HARS protocols.
To facilitate engagement, partners should be provided with information about the nature and magnitude of risks to health from extreme heat, the potential impacts of climate change, and examples of adaptations that other jurisdictions have used successfully. Many non-professionals may not be familiar with professional jargon or wording and may require an audience-appropriate orientation and education support. Questions about HARS development that can be expected from stakeholders include:

- Why develop a HARS now, and why take action on heat over other natural hazards?
- What is the risk to health in our community from extreme heat events (past data: number of hot days, humidex values)?
- What are the projections for extreme heat events in the future for our community?
- What trigger should be used to issue heat alerts?
- What public messages should be used?
- Who are most vulnerable to the heat-health impacts in our community and where are they located?
- How can vulnerable groups be reached?
- What role could my organization play in responding to or preparing the community for extreme heat events?
- How will the HARS be maintained over the long term?
It is important to recognize information gaps and provide material in a timely manner that will help address important questions so the HARS can be improved and the credibility of the process maintained.
Figure 8: HARS stakeholder engagement approach
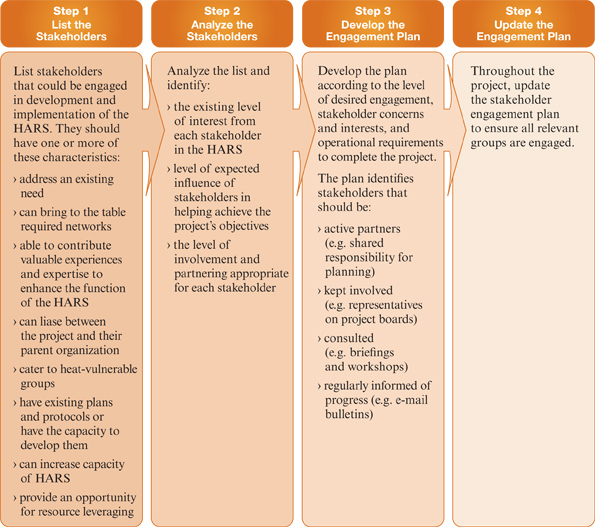
Figure 8: HARS stakeholder engagement approach
A figure describes four steps in a HARS stakeholder engagement approach. The steps are listed in separate adjacent boxes along the top and descriptions for each is shown below in sub-boxes.
- Step 1: List the Stakeholders. List the stakeholders that could be engaged in development and implementation of the HARS. They should have one or more of these characteristics: address an existing need, can bring to the table required networks, able to contribute valuable experiences and expertise to enhance the function of the HARS, can liaise between the project and their partner organization, cater to heat-vulnerable groups, have existing plans and protocols or have the capacity to develop them, can increase capacity of HARS, provide an opportunity for resource leveraging.
- Step 2: Analyze the Stakeholders. Analyze the list and identify: the existing level of interest from each stakeholder in the HARS, level of expected influence of stakeholders in helping achieve the project's objectives, the level of involvement and partnering appropriate for each stakeholder.
- Step 3: Develop the Engagement Plan. Develop the plan according to the level of desired engagement, stakeholder concerns and interests, and operational requirements to complete the project. The plan identifies stakeholders that should be: active partners (e.g. shared responsibility for planning), kept involved (e.g. representatives on project boards), consulted (e.g. briefings and workshops), regularly informed of progress (e.g. e-mail bulletins).
- Step 4: Update the Engagement Plan. Throughout the project, update the stakeholder engagement plan to ensure all relevant groups are engaged.
Source: Adapted from Ebi, K. L. et al., 2011.Footnote 93
Case Study 1
How Fredericton Developed a Heat Alert and Response System from the Ground Up
The City of Fredericton, New Brunswick (N.B.), is one of four Health Canada pilot communities that introduced a HARS in 2009. The specific HARS objectives were to:

- develop partnerships with local stakeholders to support their engagement
- develop heat alert and response protocols
- increase public awareness of heat-health risks and change behaviours
- increase community support to at-risk populations during heat episodes
- identify best practices for communication and share information among agencies to reduce heat-health risks among the public
Early in the development stages, a lead organization (N.B. Department of Health, Health Protection Branch) was identified and a project coordinator was assigned to supervise and roll out the HARS. A core group of stakeholders was recruited, including the District Medical Officer of Health, Canadian Red Cross, the N.B. Emergency Measures Organization, Environment Canada, Meals on Wheels, and the N.B. Home Support Association. To gain their interest on heat-health issues and HARS development, stakeholders were provided with health and environment data, including:
- Environment Canada data demonstrating that Fredericton has historically experienced a higher number of days (along with the central portion of the province) with humidex values above 35 compared with other regions in the Maritimes
- mortality curves demonstrating strong relationships between non-traumatic deaths, temperature and humidex
- temperature projections showing that by 2041 the number of days in Fredericton with temperatures above 30°C/86°F is expected to double
- experiences of other communities (e.g. Europe in 2003 and Chicago in 1995) demonstrating potentially severe detrimental heat-health outcomes
The lead agency established a HARS Advisory Committee to provide guidance on how to develop the HARS, including a public education program to reduce morbidity and mortality during extreme heat events. Regular committee meetings, e-mail updates, telephone discussions and personal contact with the individuals representing organizations were necessary to keep everyone engaged and focused. Information provided by community partners on the needs of the target audiences, availability of data and information resources, identification of community-specific risk factors and educational opportunities helped shape development of the HARS.
Partners gave one-on-one training to their clients about heat-health risks and the HARS. They also distributed material directly to heat-vulnerable people, including older adults, homeless people, and people living alone with mental illnesses or physical limitations. The City of Fredericton also played a key role in the awareness campaign by including heat-health information on their website and in water utility bills mailed in the spring to 16,000 households in the city. In addition, a direct link to heat-health resources is displayed on the City of Fredericton homepage during the summer months. When an alert is issued a message is disseminated for its duration and a press release is sent to news agencies.
For more information on the Fredericton HARS, visit www.fredericton.ca/heatalert.
3.4 Developing an Alert Protocol
Weather alert systems have proven effective in reducing morbidity and mortality from a range of weather hazards.Footnote 94 In many Canadian and international jurisdictions, public health and emergency management decision-makers use rapid communication systems to alert the public, as well as health and social services agencies, of impending hazardous weather conditions so that actions can be taken to protect health.Footnote 29
3.4.1 Identifying an Alert Trigger
Alert triggers protect human health when they are based on knowledge of community- and region-specific weather conditions that result in increased heat-related morbidity and mortality.
- S. Hajat, et al., 2010; S. Hajat and T. Kosatsky, 2009Footnote 41Footnote 95Footnote 125
An alert trigger should be based on a physiological definition of an extreme heat event--one in which the intensity and duration of the event is associated with increased morbidity and mortality of a specific population.Footnote 9 The alert trigger is usually a communityspecific numerical value derived by one or more meteorological parameters (e.g. temperature, humidity) that are forecasted to last for one or more days.Footnote 96 It is determined by:
- extreme heat event timing, intensity and duration
- forecasted maximum and/or minimum temperature and/or humidex
- synergistic risks to health from other meteorological conditions (e.g. air quality)
- contributing factors (e.g. power outages, water shortages)
An alert trigger approach that is transferable to all communities and is most effective in accurately identifying different levels of health risk has not been identified in the literature to date.Footnote 41Footnote 95Footnote h Few communities in Canada and elsewhere have systematically examined the association between the trigger they are using and resultant health outcomes, or other measures of effectiveness.Footnote 41 To help communities identify an alert trigger approach for their unique needs, some strengths and weaknesses of select triggers used in Canada and internationally are highlighted in Table 2.

Communities should choose a trigger approach for their HARS that is best able to contribute to a reduction in heat-health impacts. Whatever approach is adopted, it should allow sufficient lead time to activate outreach and response plans as well as advise stakeholders and the public of an extreme heat event at least one or two days before it occurs.Footnote 96 In addition, the trigger should reflect community needs, response capacities, existing public health standards and requirements, specific vulnerabilities (e.g. cities with cooler average temperatures, less air conditioning and higher population densityFootnote 99Footnote 100), and changing population demographics and needs. This will ensure that the trigger is effective and guards against the development of public apathy associated with activating an alert too often.Footnote 81Footnote 95
| Strengths | Weaknesses |
|---|---|
| Trigger: Temperature--In Canada, air temperatures are measured at Environment Canada's meteorological stations and reported in degrees Celsius. | |
|
|
| Trigger: Humidex--Environment Canada defines humidex as "an index (a computed value as opposed to something measured) devised to describe how hot or humid weather feels to the average person. The humidex combines the temperature and humidity into one number to reflect the perceived temperature."Footnote 101Footnote 102Footnote j | |
|
|
| Trigger: Temperature and/or humidex in combination with daily morbidity and/or mortality-- Hospital admissions and coronary reports are factored into the decision-making process to trigger an alert or upgrade to a higher alert level. | |
|
|
| Trigger: Humidex and/or temperature in combination with air pollution--Measure of thermal discomfort is combined with air quality to trigger an alert. Currently, single pollutant measurements are often used to initiate or upgrade an alert. The Air Quality Health Index (AQHI) measures a combination of three pollutants known to impact human health. It is a non-threshold scale and does not have a specific national advisory level, although an advisory system is available to jurisdictions through Environment Canada. | |
|
|
| Trigger: Spatial synoptic classification of air masses--This system classifies air masses from dry to moist tropical air and identifies the most dangerous to health based on historical mortality data. | |
|
|
| Trigger: Wet Bulb Globe Temperature (WBGT) index--Considers four environmental factors: temperature, humidity, radiant load and air movement, and integrates them into one index that is used to call alerts. | |
|
|
| Trigger: Heat Index (HI)--A "measure of how hot it really feels when the relative humidity is added to the actual air temperature" and is reported in degrees Fahrenheit.Footnote 110Footnote k | |
|
|
An alert system may include more than one trigger to allow for activation of different levels of community response. Some systems include:
- a trigger to notify key partners (e.g. heat watch)
- a trigger to notify a broader range of stakeholders, often accompanied by a public alert (e.g. heat warning)
- an enhanced trigger (e.g. heat emergency) to initiate an aggressive community response to help people requiring assistance
A range of community response measures (e.g. water distribution, opening of cooling facilities, outreach to the most vulnerable) may be initiated to help heat-vulnerable people cope with extreme heat (Section 3.5).Footnote 92 Triggers that result in a frequent change in alert levels or a higher alerting level being reached for only one day often present operational difficulties and should be adjusted.Footnote 111

In Canada, the wording used for issuing heat alerts and triggers are diverse (Appendix D). This can lead to confusion among the public in adjacent communities and among public health officials in regions with similar climatic conditions. Greater alignment of wording and triggers, when supported by heat-health outcome data, will improve the practical implementation and effectiveness of community HARS. To communicate graduated heat-health risks to the public through alert systems, some communities (e.g. Hamilton, Fredericton, Windsor) are using heat meters (Box 2), which raise awareness that risks to health increase with temperature. This approach is also used in forest fire prevention campaigns (Box 2, D).
Weather conditions that may not meet alerting requirements can also be dangerous to health. These conditions may become more common with climate change and warmer summers may result in an increased state of exhaustion in heat-vulnerable people.Footnote 96Footnote 115 Therefore, engaging in broad awareness activities is essential to minimize risk even when alerts are not issued.
Box 2: Graduated alert systems used to communicate risks
A: The City of Fredericton uses Level 1, Level 2 and Level 3 to communicate heat-health risks.

Source: City of Fredericton and Government of New Brunswick.Footnote 112
B: The City of Hamilton uses "Monitoring," Stage 1, Stage 2 and Stage 3 to communicate heat-health risks.

Source: City of Hamilton, Ont.Footnote 113
C: The Marine Corps Logistics Base uses a flag warning system to communicate heat-health risks.

Source: Marine Corps Logistics Base, Albany, New York.Footnote 114
D: Canadian Forest Service (Natural Resources Canada) developed Canadian Forest Fire Danger Rating System used to communicate forest fire risks.

Source: Natural Resources Canada.
Box 2: Graduated alert systems used to communicate risks
A figure is shown describing the Montreal HARS activation and deactivation decision flowchart. Activation of the prevention and protection plan occurs in the event of extreme heat. This is a "Seasonal watch" level which is in effect from May 15 to September 30, 2011. The DSP issues a press release to CSSSs to appear in weekly newspapers.
A Heat warning is issued and an "Active watch" level is reached when the temperature is greater than or equal to thirty degrees Celsius and humidex is greater than or equal to 40. The DS-EUS issues advisories to the public on how to prevent negative health effects. CSSSs implement increased surveillance and prevention measures for vulnerable patients.
A forecast of at least 3 consecutive days of maximum temperature greater than or equal to thirty-three degrees Celsius (weighted average) and minimum temperature of greater than or equal to twenty degrees Celsius (weighted average) or at least 2 consecutive nights with minimum temperature of greater than or equal to twenty-five degrees Celsius triggers an "Alert level. The DSP-EMO notifies partners of the situation to put them on alert. Partners include Joint, Environment Canada, DSP-Emergency Management Office, Health Agencies, the City of Montréal, and Emergency Health Services.
Monitoring of weather conditions and the health surveillance data occurs. The following questions are asked: did weather conditions meet the extreme heat criteria for at least two days, and is Environment Canada weather forecast maintained or is an increase in morbidity and mortality detected using health surveillance data? If the answers are no, then monitoring of weather conditions and the health surveillance data continues. If the answers are yes, then a teleconference is held with neighbouring DSPs the Agence and SCACs to share information on the weather, health and other aggravating factors. An "Intervention level" has been reached and activities set out in the Emergency Response Plan are carried out. Activities include: Management of overcrowding in emergency rooms, Impact management in health care institutions, Health watch, Measures put in place by the Montréal Civil Security Centre, Management of the increase in ambulance transport, Management of fatalities if there is an excess, Communication management, and a Door-to door campaign.
The following question is asked before a "Demobilization" level is reached; that is: Did weather conditions and anticipated levels in the health surveillance data return to normal? If yes Return to "Seasonal watch" or "Active watch" level and the "Demobilization" level. If the answer is no, activities set out in the emergency response plan continue to be carried out.
3.4.2 Calling Alerts
The alert protocol, as defined by set criteria, identifies the lead agency or person responsible for issuing an alert, outlines communication activities, and specifies the deactivation point where meteorological conditions are no longer a health threat. When meteorological and other relevant conditions meet alerting requirements, the lead agency employs pre-identified activities to communicate weather forecasts and health risks to the public and partnering community agencies (Section 3.6). In many communities, it is the public health authority (e.g. Medical Officer of Health) that is responsible for making the decision to issue a heat alert, upgrading to higher stages of an alert and issuing a deactivation notice.Footnote 92Footnote 112Footnote 116
When developing an alert protocol, it is important to consider that the first extreme heat event and ones that occur early in the season are the most dangerous to health.Footnote 122Footnote 123 Therefore, earlier warnings can be used to prime the public and prepare the community.Footnote 81
When deciding whether to move to a higher alert level, some communities consider additional factors that may also be included in the notification. For example:
- surveillance data showing increases in morbidity and mortalityFootnote 96:
- daily deaths (e.g. daily activity of funeral homes)
- daily calls to health information lines
- daily ambulance calls
- daily emergency room visits
- occupancy rate of emergency room beds
- increased risk of forest fires and/or poor air quality
- likelihood of an electrical emergency, existing blackouts or rotating power outages
- drinking water availability
- nighttime temperatures (cooler evenings can offer nighttime relief for the population)
- likelihood of heat-vulnerable people being left alone
- reduced capacity of health care providers to respond due to other commitments, disease outbreaks, or labour disputes
- time of the week (weekends may affect staff availability)
- time of the season (peak vacation periods may effect staff availability)
- major outdoor events (e.g. concerts, sporting events)
- expected influx of visitors
As heat-related mortality may peak only a few days after exposure to high temperatures,Footnote 124 public health authorities need to consider the state of readiness in a community and the capacity to mobilize a response over an extended period of time.
When a heat alert is issued, weather conditions should continue to be monitored to determine when heat no longer poses a health risk. Once conditions are no longer a threat to public health, the alert should be deactivated, along with the response measures that were taken. To account for any "lag effect" in health impacts and ensure that the deactivation of an alert is not premature, some communities continue heat-alert activities for a few days after extreme heat conditions expire.Footnote 73Footnote 111Footnote 116Footnote 125 In addition, following the alert deactivation, some authorities continue to encourage residents to take extra care when exposed to heat, warn about retention of heat in homes with no air conditioning and highlight the need to continue to pay close attention to those at risk.Footnote 126
Figure 9: Montréal HARS activation and deactivation decision flowchartFootnote l
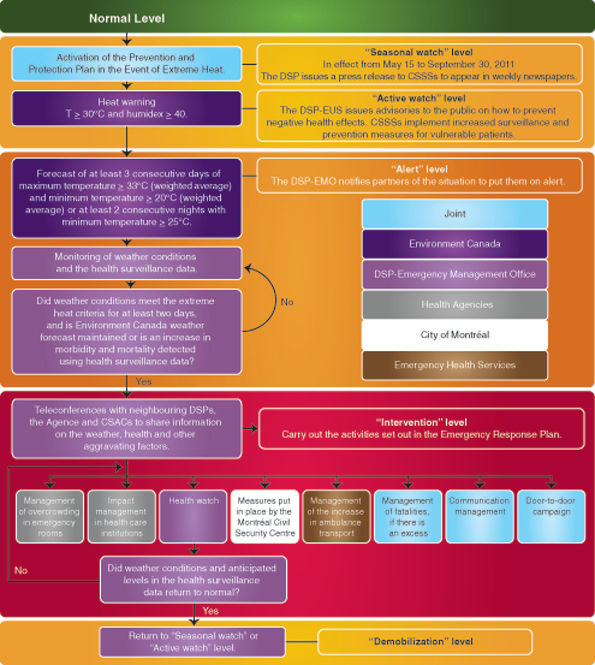
Figure 9: Montréal HARS activation and deactivation decision flowchart
A figure is shown describing the Montreal HARS activation and deactivation decision flowchart. Activation of the prevention and protection plan occurs in the event of extreme heat. This is a "Seasonal watch" level which is in effect from May 15 to September 30, 2011. The DSP issues a press release to CSSSs to appear in weekly newspapers.
A Heat warning is issued and an "Active watch" level is reached when the temperature is greater than or equal to thirty degrees Celsius and humidex is greater than or equal to 40. The DS-EUS issues advisories to the public on how to prevent negative health effects. CSSSs implement increased surveillance and prevention measures for vulnerable patients.
A forecast of at least 3 consecutive days of maximum temperature greater than or equal to thirty-three degrees Celsius (weighted average) and minimum temperature of greater than or equal to twenty degrees Celsius (weighted average) or at least 2 consecutive nights with minimum temperature of greater than or equal to twenty-five degrees Celsius triggers an "Alert level. The DSP-EMO notifies partners of the situation to put them on alert. Partners include Joint, Environment Canada, DSP-Emergency Management Office, Health Agencies, the City of Montréal, and Emergency Health Services.
Monitoring of weather conditions and the health surveillance data occurs. The following questions are asked: did weather conditions meet the extreme heat criteria for at least two days, and is Environment Canada weather forecast maintained or is an increase in morbidity and mortality detected using health surveillance data? If the answers are no, then monitoring of weather conditions and the health surveillance data continues. If the answers are yes, then a teleconference is held with neighbouring DSPs the Agence and SCACs to share information on the weather, health and other aggravating factors. An "Intervention level" has been reached and activities set out in the Emergency Response Plan are carried out. Activities include: Management of overcrowding in emergency rooms, Impact management in health care institutions, Health watch, Measures put in place by the Montréal Civil Security Centre, Management of the increase in ambulance transport, Management of fatalities if there is an excess, Communication management, and a Door-to door campaign.
The following question is asked before a "Demobilization" level is reached; that is: Did weather conditions and anticipated levels in the health surveillance data return to normal? If yes Return to "Seasonal watch" or "Active watch" level and the "Demobilization" level. If the answer is no, activities set out in the emergency response plan continue to be carried out.
Source: Agence de la santé et des services sociaux de Montréal (Bureau des mesures d'urgence de la Direction de santé publique de l'Agence et coordination des mesures d'urgence et sécurité civile de l'Agence); Plan régional sociosanitaire de prévention et protection en cas de chaleur accablante et de chaleur extrême (2011). Footnote 179
Case Study 2
How Winnipeg Chose its Heat Alert and Response System Alert Triggers
Winnipeg, Manitoba, developed a multi-level alert protocol with multiple triggers as part of its HARS. The alert levels include:
- Heat Pre-Alert--communication only to internal partners
- Heat Alert 1--communication to the public and community stakeholders, as well as initiation of some response measures if required
- Heat Alert 2--activation of some response measures and enhanced messaging
- Heat Alert 3--delivery of aggressive response measures, more targeted messaging and increased community mobilization
The Winnipeg HARS Advisory Committee, which is responsible for guiding the development of the HARS, established a Heat Scientific Group led by the provincial Medical Officer of Health (Environmental Health). The Group includes officials from provincial public health, the Winnipeg Regional Health Authority, Environment Canada, provincial communications office and provincial health emergency management. Its mandate includes evaluating existing evidence demonstrating that heat is a health risk in Manitoba (rural and urban), identifying HARS best practices and deciding on alert triggers. To develop appropriate triggers, multiple factors were considered, including humidity and temperature, the location of vulnerable populations, accuracy of weather forecasts, and existing capacity for surveillance of heat illnesses. Historical data and their correlation with mortality were also examined.
Source: Government of Manitoba
Through this process, the Group decided that a heat alert would be issued when specific temperature or humidex triggers were reached. Humidex was chosen because of its physiological relevance and its known correlation with mortality. Humidity reduces the ability of a body to cool through sweat evaporation. It is also a measure of perceived temperature that is widely understood in Canada. Humidex is not currently forecasted by Environment Canada publicly; however, the Weather Network does provide this service. Temperature was also chosen as the basis of a second trigger because, although it is less physiologically relevant, longer historical records of temperature exist in Manitoba and it is forecasted with higher accuracy than humidex.
The specific triggers for issuing alerts using humidex and temperature were based in part upon evidence of the correlation between these two variables and daily deaths in Winnipeg (Figure 10). The triggers also account for nighttime temperatures by identifying minimum, in addition to maximum trigger values, that have to be reached to issue each alert level. The alert protocol takes into consideration the intensity and duration of the extreme heat event and the lack of certainty associated with forecasts. Greater weight is placed on occuring weather conditions, rather than forecasted values, in the decision to activate higher alert levels.Footnote m
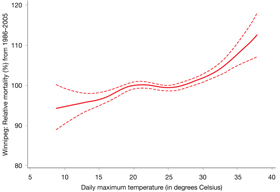
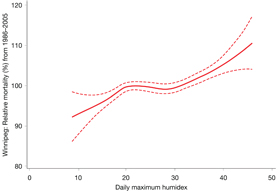
Figure 10: Association between non-traumatic daily deaths and maximum daily temperatures (A) or humidex (B) in Winnipeg, 1986-2005
The figure is two adjacent graphs (A and B) showing the association between non-traumatic daily deaths and maximum daily temperatures (graph A) or humidex (graph B) in Winnipeg, 1986-2005. The y-axis is relative mortality (%) from 1986-2005 in Winnipeg. The x-axes is daily maximum temperature (graph A) and daily maximum humidex (graph B). A single best fit curve (thick solid red line) and 95% confidence intervals (two thin dotted lines) are shown on each graph. In graph A, relative mortality reaches 100% when temperature is approximately 20°C/68°F. Relative mortality steadily rises above 100% with temperature when the temperature reaches 26°C/79°F. A similar correlation is seen in graph B for daily maximum humidex. Relative mortality reaches 100% at humidex 20. Relative mortality steadily rises above 100% with humidex when the humidex reaches 30.
Source: Adapted from B. Casati and A. Yagouti, in press.Footnote 50
Before any notifications of a heat alert are made, a risk assessment is conducted that considers environmental parameters, as well as any additional information about health outcomes during extreme heat events. For example, this may include identification of impacts of heat on health from real-time surveillance and anecdotal reports of heat-related incidents by front-line medical staff, private physicians and community workers, among others.
The alert is deactivated when the forecast no longer meets the trigger criteria and the lead provincial Medical Officer of Health and Manitoba Health's Office of Disaster Management decide that heat is no longer a health risk. The efficiency and accuracy of the triggers will be evaluated at the end of each extreme heat event and each heat season and, if necessary, will be re-calibrated to reflect experiential knowledge, optimize the use of resources and maximize the public's responsiveness and adaptation to extreme heat events.
For more information on the Manitoba HARS, visit www.gov.mb.ca/health/publichealth/environmentalhealth/heat.html
3.5 Developing a Response Plan
A HARS response plan has the ultimate objectives of directing public health interventions to vulnerable people who require assistance and facilitating actions by individuals to protect themselves during extreme heat. Measures in a response plan should be based on the relationship between heat and human health, which is defined by existing risk factors, the potentially rapid onset of heat illness and death, and specific challenges faced by heat-vulnerable groups.Footnote 9
A response plan provides information on the actions that the lead agency and community partners will take to reduce heat-related morbidity and mortality when an extreme heat event is forecasted and action is triggered.
- J. McInnes, et al., 2008Footnote 9
There is no one-size-fits-all solution for developing a community response plan. The involvement of many government agencies and non-governmental organizations with knowledge of the specific needs and vulnerabilities of different population groups is required. An effective response plan relies on the outreach capacity of stakeholders. It is also tailored to the specific needs of a community and its vulnerable populations. A timely response requires that measures to protect health can be activated when alerting conditions are forecasted and the trigger is reached--before extreme heat arrives.Footnote 73
A response plan should include measures needed to overcome obstacles that people face when trying to take protective measures. Obstacles could include obtaining information about current weather conditions or accessing cooling facilities (Table 3). Response plans should consider the ability of first responders and caregivers to reach vulnerable populations.
| Heat-Vulnerable Groups | Examples of Challenges |
|---|---|
| Older adultsFootnote 11 |
|
| Infants and young childrenFootnote 24 |
|
| People with chronic illness or who are physically impairedFootnote 10 |
|
Socially disadvantaged individuals and communities:
|
|
| Newcomers to Canada and transient populations, such as tourists |
|
| Occupational groups |
|
| The physically activeFootnote 30 ,Footnote 31 |
|
Source: Reprinted from Health Canada, Communicating the Health Risks of Extreme Heat Events: Toolkit for Public
Health and Emergency Management Officials, 2011.Footnote 132
When choosing response measures, priority should be placed on actions that are most effective in reducing heat-health risks (e.g. staying cool and hydrated, checking on those at risk).Footnote 9,Footnote 133 Many measures are available to communities to use as part of their response plans. Box 3 highlights measures that have been drawn from analysis of HARS community response plans in Canada and elsewhere, the experiences of Health Canada's pilot communities, as well as workshops and consultations with experts.
Box 3: Possible HARS community response measuresFootnote o
Before an extreme heat event and during seasonal readiness
- Identify heat-vulnerable populations and target groups
- Meet with key community partners to review and plan for the upcoming heat season
- Perform real-time surveillance of heat-health impacts (e.g. mortality rates, emergency calls and visits, calls to hotlines, records from health care providers)
- Incorporate preparations for extreme heat events as part of normal hospital emergency and pandemic planning
- Schedule deployment of public health staff to cover extreme heat emergencies
- Plan for summer vacations by identifying and educating substitute staff to ensure adequate coordination of activities and communications
- Offer in-service training for public health staff
- Offer education and training to residential building managers of heat-vulnerable groups
- Update and coordinate dissemination of resources for HARS implementation
- Develop plans for possible brown- and black-outs
- Identify measures to help heat-vulnerable people manage higher electrical bills from running an air conditioner during extreme heat events
- Provide rebates and subsidies on fansFootnote p and air conditioners
- Offer registration services to receive notifications or home visits during alerts (family members may want to register those at risk or people can register themselves)
- Develop a "buddy" and/or Neighbourhood Watch program
- Plan to provide drinking water (e.g. install water fountains, identify portable water stations, identify water options for homeless shelters)
- Plan to offer cooling options (e.g. splash pads, reflective pools, community parks, community swimming pools)
- Identify cooling facilities and ensure that they are equipped with provisions (Section 3.5.1)
- Identify transportation options to get people to and from cooling facilities
- Encourage healthy life-style choices (e.g. healthy food options, physical activity, social interactions)
- Distribute information to community service providers (e.g. street outreach) and issue public service announcements with reminders about health risks from extreme heat
During an extreme heat alert

- Coordinate financial and volunteer resources
- Organize press conferences to get messages out to the public
- Closely monitor heat-related morbidity and mortality
- Open well-identified cooling facilities (e.g. public libraries, facilities already catering to heat-vulnerable people)
- Extend hours of air-conditioned facilities and places where people are likely to seek heat relief (e.g. swimming pools)
- Open cooling shelters with overnight capabilities
- Provide cooling rooms in residences and apartment buildings, especially if they cater to heat-vulnerable people
- Provide portable water stations and/or distribute drinking water to homeless shelters
- Provide maps with locations and hours of operation of cooling facilities and drinking water stations
- Reduce the cost of swimming at community pools or make it free
- Offer movie tickets to air-conditioned theatres at reduced cost or for free
- Provide transportation support to and from cooling facilities (e.g. bus tickets, taxi cards [may require pre-registering])
- Provide financial assistance for utility bills
- Check on pre-registered heat-vulnerable people (visit, telephone call)
- Open telephone lines (e.g. 211, 311, 811, "Heatline") to provide advice to the public
- Deliver services to specific heat-vulnerable groups (e.g. outreach to the homeless)
- Distribute umbrellas or wide-brimmed and breathable hats to those in need
- Modify or cancel scheduled sports and outdoor events at daycares, summer camps, etc.
- Modify work-rest cycles for workers exposed to extreme heat
- Activate response plan(s) in hospitals and personal care homes
- Increase staff:
- re-deploy emergency response and public health workers to respond to heat-health emergencies
- address the needs of volunteers who could be from heat-vulnerable groups (e.g. provide an air-conditioned environment and assign tasks that are not strenuous)
- assign lifeguards at lakes and beaches to prevent drowning accidents
- ensure police presence in neighbourhoods with high crime rates to encourage people to go to cooler places
Source: Response measures are based on recommended actions and those being taken by Canadian and international communities.Footnote 9Footnote 72Footnote 80Footnote 112Footnote 116Footnote 119Footnote 134
3.5.1 Cooling Facilities
Using air conditioning or visiting cool environments can be highly effective in minimizing heat fatalities--especially for people with chronic conditions or those taking medications that interfere with thermoregulation.Footnote 10Footnote 11 Despite its benefits, air conditioning may contribute to an increase in greenhouse gases and air pollution if the energy consumed is from burning fossil fuels.Footnote 137 It therefore should not be relied on as the only solution for addressing risks to health from extreme heat in a community. Long-term preventative actions are necessary to address heat-health risks in a sustainable manner (Section 3.8).
Many Canadians do not have air conditioning in their homes.Footnote 138 For this reason, some communities offer cooling facilities as part of their response measures (e.g. Toronto, Hamilton, Montréal, Ottawa). These include air-conditioned places or recreation facilities such as:
- libraries
- recreational or community centres
- city halls
- places of worship
- senior centres or legions
- bingo halls
- shelters
- cool rooms in apartment buildings established by landlords
- museums
- shopping malls
- movie theatres
- swimming pools
- spray pads
- public beaches or tree-shaded parks
When appropriate, cooling facilities should have back-up energy sources in case of power failures, as well as provide access to:
- drinking water
- cots, if needed
- medical supplies
- heat-health education material
- trained staff or volunteers who have excellent interpersonal skills, can recognize signs and symptoms of heat illnesses and who know actions to take in case of illness
- a safe and secure environment
Research has revealed some limitations in the effectiveness of community cooling centres in reducing heat-health risks among the most vulnerable older adults.Footnote 23Footnote 80 To successfully reduce morbidity and mortality, cooling facilities should be made available during extreme heat eventsFootnote 23Footnote 139 and be supported by:
- rigorous outreach strategies (Section 3.6, Box 4)Footnote 139Footnote 140
- accessibility features
- provision of amenities tailored to the unique needs of the visitors (e.g. older adults, homeless people, parents with children, pet owners)
- location in areas frequented by people requiring cooling
- convenient hours of operation
- the use of existing facilities known by and already catering to vulnerable people
The use of cooling facilities should be carefully evaluated and the results applied to improve their use.
Case Study 3
Community Response to Extreme Heat Events in the City of Ottawa
A Heat and Smog Action Plan, passed by Council in 2004, formalized a community response to extreme heat events in the City of Ottawa, Ontario. One goal of the Plan is to ensure the safety of heat-vulnerable groups in Ottawa by delivering timely emergency response measures when needed. During heat alerts, city officials work with a range of community service organizations to protect vulnerable populations by:
- distributing heat alert and heat warning notifications to targeted service providers by e-mail and fax
- converting all lane swims to leisure swims in city pools
- recommending places the public can go to cool down (e.g. city wading pools, splash pads, beaches, libraries, community centres)
- partnering with a local movie theatre that provides free and discounted movie tickets at a location that is easily accessible by public transportation
- deploying a street outreach van (through the Salvation Army) to offer water to homeless people and transportation to local shelters
- offering information via a 311 telephone service for inquiries, including contact with a public health nurse
- assigning public health nurses to visit heat-vulnerable populations living in high-rise buildings to ensure they are able to access cool environments. These visited buildings are identified in advance based on resident makeup (i.e. high number of seniors and young children, rooming houses, low income, lack of air conditioning)
- distributing fans to rooming house residents
- encouraging city departments (e.g. road crews, maintenance workers) to follow outdoor heat guidelines

Through its website and exchange with service providers, the City provides or supports community response measures before and during extreme heat events. It offers a Hot Weather Resource Kit that includes:
- "Beat the Heat This Summer!"--information on response measures implemented by the city and where people can go to cool down; includes a media backgrounder on a heat alert and a news release, and is available in 51 languages
- sample of a heat warning
- "What to Do in a Heat Wave"--information for the public on how to stay cool and hydrated
- "Screening Tool for Heat Illness" lists heat-illness risk factors and symptoms, and provides information on actions that should be taken to protect health
- individual handouts on heat stroke, dehydration, sunburn, medications and heat-related illnesses, fan facts
- links to information on park locations, pool schedules, summer safety for pets, working in hot environments
- "Extreme Hot Weather Initiative--Information Brochure for Service Providers to the Homeless"
- "Surviving Summer Power Outages During Heat Waves"
The city's outreach and response efforts have been integrated into the activities of many community organizations. These organizations also take action on their own during extreme heat events. For example, the Ottawa Carleton Ultimate Association reminds players to take extra breaks, drink plenty of fluids, and seek out or bring shade to the game. The rules of the game are modified during a heat alert to ensure safety of the players by permitting heat-related substitutions and increasing the number of timeouts per period from 2 to 3 and increasing their duration from 70 seconds to 120 seconds.
For more information on the City of Ottawa HARS, visit http://ottawa.ca/en/health_safety/living/outdoor/hot/index.html.
Case Study 4
How a Rural Community in Manitoba Reduces Impacts on Health from Extreme Heat
Developing a HARS in a rural region in Manitoba within the Assiniboine Regional Health Authority (ARHA), required that health officials address challenges common to smaller communities and build on existing capacity. Establishing a temperature--mortality relationship was not feasible due to the large geographic area and low population density that limited the amount of data for the analysis.
Despite this, mortality curves of other neighbouring communities, including Winnipeg and Brandon, and historical temperature data for ARHA, provided sufficient evidence to demonstrate heat-health risks and support the development of a HARS. With support from the provincial and regional Medical Officers of Health, multiple partners were engaged to help with this task. This included disaster and emergency management officials, municipal government officials (e.g. mayor, chief administrative officer, local emergency management officers), Meals on Wheels, service providers for seniors, and Manitoba Housing.
An assessment of vulnerability through consultation with community groups helped to develop the ARHA HARS and prioritize community response measures. The assessment revealed that during the heat season, ARHA experienced an influx of visitors (e.g. golfers, campers, children attending camps); therefore, special efforts were needed to reduce the negative health impacts on these individuals as well as permanent residents from extreme heat events. Stakeholder consultations revealed challenges with providing cooling options because of a limited number of easily accessible air-conditioned buildings. In addition, issuing timely alerts was found to be difficult because of weekly media deadlines and limited local media coverage. As a result, response measures were identified to specifically address these challenges, build on existing strengths, and focus on increasing collaboration between the regional health authority and municipal planning staff. The ARHA HARS model focusses on:
- integrating the HARS into the ARHA Disaster Emergency Response Plan to ensure a robust and coordinated response
- ensuring that residents of long-term care facilities have access to air conditioning in common rooms
- establishing an alternate meal plan (cold plates) during alerts in long-term care facilities
- encouraging implementation of alternative work hours for some occupational groups (e.g. construction workers), where staff work evenings or nights to avoid intense heat during the day
- working with Manitoba Health to issue heat alerts and warnings to residents, schools, daycares, recreational groups, volunteer support groups, transient populations (e.g. campers) and sporting events
- developing response plans for Home Care clients which includes an assessment of the client's home environment and a care management plan for use if they should exhibit signs of heat illness
- contacting municipal departments, as required, to encourage appropriate preparations (e.g. check emergency response equipment such as fans, generators, back-up communications capability)
- using Emergency Medical Services staff to conduct home safety checks through the ARHA Home, Health, and Safety Check Program, thereby providing older adults with information on how to stay cool in hot weather, copies of heat-health fact sheets, and a directory of health-related services available within their local community
- putting volunteers on stand-by to assist at cooling facilities and with drinking water distribution
- arranging for health care staff to support individuals and communities, as required, throughout the region during extreme heat events

Strong community support and participation in the HARS, the use of volunteer networks and the existence of local health practitioners who personally know those at risk have been instrumental in the innovative approach public health officials have taken to reduce impacts from extreme heat.
For more information on the ARHA HARS, visit www.assiniboine-rha.ca/index.php/news/plans_view/disaster_plan/.
3.6 Supporting a Heat Alert and Response System with Communication Activities
"Considerably more education is needed of the public and of the responsible agencies about the dangers associated with heatwaves and about the appropriate responses."
- K.L. Ebi and G.A. Meehl, 2007, p. 11Footnote 141
Effective communication of heat alerts and measures to reduce health risks is a fundamental requirement for successful HARS. Heat-health communication campaigns aim to increase knowledge of dangers from extreme heat and to influence individuals to adopt protective behaviours. Communication activities need to be delivered before and during the heat season and during extreme heat events through media (mass/broadcast and targeted), interpersonal networks and community events.Footnote 132
Several authorities in Canada and internationally provide heat-health education materials to help people minimize risks from extreme heat (e.g. Toronto, Hamilton, Montréal; United States Centers for Disease Control and Prevention). Despite these efforts, research suggests that many people are not acting on the information they receive urging them to take actions to reduce health risks.Footnote 29Footnote 78Footnote 142 Many factors may contribute to this, including poor perception of heat-health risks, a general focus of the media on a few vulnerable groups and confusion in existing heat-health messages.Footnote 29 Inconsistent messaging in heat-health campaigns (e.g. fact sheets, media releases, websites) between different public health jurisdictions, or arising from other health promotion campaigns (e.g. West Nile virus, air quality, sun safety, environmental initiatives, physical activity), might be partially responsible for challenges experienced in affecting behavioural change.Footnote 17Footnote 29Footnote 132
To increase the effectiveness of heat-health communication campaigns, collaboration is needed among different communities, stakeholders, public health, emergency management and municipal officials to deliver consistent, audience-appropriate and easily understood messages. Best communication practices to influence behaviours have been identified in Communicating the Health Risks of Extreme Heat Events: Toolkit for Public Health and Emergency Management Officials.Footnote 132 Many strategies identified in Table 4 should be used to inform the development of a HARS communication plan and supporting materials for individual communities. These strategies are based on leading research and practices used by communities to communicate with vulnerable populations through health promotion campaigns.
| Older adults |
|---|
|
| Infants and young children |
|
| People with chronic illness or who are physically impaired |
|
| Socially disadvantaged individuals and communities (e.g. low income, homeless, living alone) |
|
| Newcomers to Canada and transient populations such as tourists |
|
| Occupational groups |
|
| Physically active persons |
|
3.6.1 Before the Heat Season
A communication plan should be developed to engage new partners and increase the awareness of stakeholders (e.g. care providers, health care workers, help phone line staff) and the media.Footnote 7 Audience-appropriate information packages on HARS, heat-health risks and actions to take during alerts (e.g. fridge magnets, downloadable resources, websites, e-mail templates, presentations, train-the-trainer packages) should be developed or updated for the upcoming heat season. End-of-season evaluations of a HARS (Section 3.7), which may involve community meetings and workshops to address challenges, offer the opportunity to revise communication materials, and to continue increasing information and building awareness among stakeholders and the public. Attention should be given to "branding" communication products, using simple and easy-to-remember messages and website names, and ensuring that materials are tailored to specific audiences.
Common messages in most targeted heat-health communication materials relate to:
- methods to prepare for extreme heat
- community-appropriate options to minimize health risks
- signs and symptoms of heat-health impacts
- importance of staying cool and hydrated through community- and audience-specific services
- details on where to get additional information or help

For effective communication of alerts, choose a simple system such as:
- colours from the traffic light (green, yellow or amber, red) (Box 2)Footnote 146
- a level or stage system (e.g. Level 1, Level 2), along with wording that the population understands
For example, the City of Hamilton uses "heat advisory," "heat warning" and "heat alert" to describe three stages of alert.Footnote 113 Other Canadian communities use different wording, such as "extreme heat alert," "humidex advisory," or "heat emergency" (Appendix D).
Communication campaigns are more likely to change behaviours when health education about preventing and identifying heat risks is repeated in advance;Footnote 6 therefore, before the start of a heat season it is essential to develop and deliver a pre-season awareness campaign (e.g. a Blitz Day). For example, Toronto Public Health provides information to the public and to community organizations that play a role in assisting the most vulnerable.Footnote 92 HARS communication campaigns should:
- highlight the objectives of the HARS
- provide information on recent improvements or modifications to the system
- emphasize available resources for the public and stakeholders
- engage the media in preparing for the upcoming heat season
- expand community partnerships
- spike interest in heat-health issues
Before the heat season, it is important to identify partnerships to optimize resource use and effective delivery of heat-health communication products. For example, the City of Windsor partnered with the Windsor Utilities Commission (WUC) to reach residents at higher risk of heat illness and death with educational materials. As part of these efforts, Street Health Help and local food banks distribute reusable water bottles printed with information on WUC services and heat-health messages to residents of Windsor experiencing socio-economic challenges.Footnote 119
3.6.2 During the Heat Season
The heat season is the time to build on the momentum in education and outreach activities gained through the pre-season awareness campaign. A summer with hotter-than-average temperatures will often result in greater interest and receptivity of the public and stakeholders to heat-health messages.
Active communication about HARS with partners through bulletins, e-mail updates, media interviews, community meetings and website postings should continue. Awareness can be raised by providing reminders and regular updates about the impacts that heat has on health. In addition, activities should focus on educating the public and stakeholders about audience-specific needs, as well as effective practices to prepare for extreme heat events and minimize risks to health. It is important to ensure that social service and health care providers are well informed and supportive of the HARS. People who are counselled by a trusted health care professional about risks to health from extreme heat events will be more likely to recognize their personal vulnerability and to adopt protective actions.Footnote 78
Providing information on available response measures and incentives, such as locations of water fountains and cooling options (e.g. tree-shaded areas, swimming pools, splash pads, cooling facilities), rebates on air conditioners, subsidies for utility bills and transportation options is also important. Measures to help reduce barriers to action need to be publicized and details provided on where more information can be obtained (e.g. websites, 211, 311, 811 phone numbers). This will prepare the public by reinforcing key messages about actions that should be taken to get ready for extreme heat events. For example:
- advise people to ensure that air conditioners are working properly
- promote healthy living and good hydration practices and offer suggestions on how people should make them a routine
- raise awareness that special precautions (stay cool, hydrated and check on most vulnerable) should be taken during extreme heat events, especially if it is the first event of the season, which can have the most impact on human healthFootnote 34
- promote the use of long-term residential adaptation strategies, such as:
- planting deciduous trees in front of south- and west-facing windows to block the sun
- choosing light-coloured paint for the outside of the house
- improving ventilation options (e.g. installing windows that open and safety bars if safety is an issue)
- improving insulation
Communication tools and aids to increase the understanding and retention of different alert stages (Box 2) should be provided to the public. Develop tools that can be used as reminders (e.g. refrigerator magnets, websites, tailored fact sheets, posters, presentation decks) and align heat-health communication strategies with existing community practices.
Figure 11: Communication tools developed by the City of Hamilton, Ontario, and Moreland City Council, Australia
A : "Cool Down Here " sign used to indicate cooling centres.

Source: City of Hamilton, Ont., 2009Footnote 113.
B : A cell from a storyboard, "Keeping your cool in a heatwave," to communicate heat-health messages.
Source: Moreland City Council, Australia, 2010.Footnote 147 .
Figure 11: Communication tools developed by the City of Hamilton, Ontario, and Moreland City Council, Australia
(A) The words "Cool Down Here" are shown through an open door above a welcome mat. Above the door is a city of Hamilton logo, and below the door are the words "A Community Heat Response Initiative."
(B) A dual image cartoon cell from a story board. The left side of the cell show two adults speaking with a doctor. The right side of the cell shows a baby and a dog in a car during a sunny day. To indicate that this action is dangerous a large red circle with a line through it is superimposed over the car.
3.6.3 During an Extreme Heat Event
The most important objective of communication activities during an extreme heat event is to influence individuals--particularly vulnerable populations--to take protective measures. To remind people about the different alert stages, the use of simple wording understood by the local population is important. Include a visual heat scale that provides more than one call to action to increase understanding of the system (Box 2).
When a decision is made to issue an alert, stakeholders (especially service providers that cater to heat-vulnerable populations) and the public should be notified using a pre-identified communication plan (e.g. press releases, electronic and print media, service providers [e.g. agencies for seniors], as well as health networks). Direct and timely communication activities will ensure that response measures (e.g. water distribution, opening of cooling facilities) are properly delivered. Updating websites and issuing media releases with information on heat-health risks, preventative actions and available community response measures (e.g. cooling facilities [Box 4], financial assistance with utility bills, free access to public swimming pools) will provide the public with easily accessible information through the alert notification. Communication materials should have clear information about specific actions to take to reduce heat-health risks. During an extreme heat event, it is also important to notify neighbouring communities of the alert to increase coordination between the jurisdictions.
Box 4: Communication strategies for the successful use of cooling facilities
- Highlight the existence of cooling facilities well before an extreme heat event occursFootnote 98Footnote 148
- Provide a clear description of the cooling facilities (i.e. who they are for, what type of services visitors are likely to receive, whether pets are welcome)
- Identify credible messengers for each target group to deliver informationFootnote 149
- Use multiple communication channels to reach those who should be using the cooling facilities
- Educate the public about heat-health risks and the importance of cooling during an extreme heat event
- Reach "shut-ins" (e.g. those with limited social interaction) and those with a false sense of safety, which could prevent them from taking protective actionsFootnote 150
- Educate the public on the signs used to identify cooling facilities (e.g. "Cool Down Here" sign developed by the City of Hamilton, Figure 11, A)Footnote 113 and on their locations
- Encourage friends, neighbours, relatives and volunteers ("buddies") to actively seek out people in need of cooling and to help them stay healthy in the heatFootnote 78Footnote 140
- Encourage the public to welcome family and neighbours when they need a place to cool offFootnote 140
Public awareness can be increased with pre-selected messages from heat-health education campaigns delivered using several communication channels (e.g. media, road/construction signs, faith-based organizations, health care professionals). This campaign should reinforce key messages to stay cool, hydrated and check on the most vulnerable. Pre-selected messages for heat-health communication includeFootnote 132 :

- "Heat illnesses are preventable."
- "Take a break from the heat by spending a few hours in a cool place. It could be a tree-shaded area, swimming facility or an air-conditioned spot such as a public building, shopping mall, grocery store, place of worship or public library."
- "Reschedule or plan outdoor activities during cooler parts of the day."
- "Drink plenty of cool liquids, especially water, before you feel thirsty to decrease your risk of dehydration. Thirst is not a good indicator of dehydration."
- "Frequently visit neighbours, friends and older family members, especially those who are chronically ill, to make sure that they are cool and hydrated."
When it is determined that weather conditions are no longer a health risk, deactivation of the alert should be communicated to the public and stakeholders. At this stage, additional messages may be required to raise awareness about indirect health hazards. For example, messages about the dangers of food spoilage may be needed, especially if the extreme heat event occurred at the same time as a power outage.
Case Study 5
How Windsor-Essex Communicates Heat-Health Risks to the Public

As part of HARS development, Windsor-Essex, Ontario, emphasized development and implementation of its communication campaign. Early in the process, marketing experts were consulted to examine heat-health communication activities in the city and in other communities with existing HARS. This information gathered helped identify heat-health communication goals and outreach strategies. It was also used to develop a STAY COOL Windsor-Essex logo that brands the city's communication activities. Additional tools being used to raise awareness are shown in Figure 12.
Figure 12: Branding of the HARS

Figure 12: Branding of the HARS
(A) Co-branded water bottle – A water bottle with the Windsor and Essex County "Stay Cool" logo.
(B) Fridge magnet - A fridge magnet that contains images and gives tips to stay cool. Beside an image of a glass - it says "drink plenty of water." Beside an image of a hat – it says "wear a hat and light-weight loose fitting clothing." Beside an image of a shower head - it says "take a cool bath or shower."
(C) Pharmacy bag inserts with the Windsor and Essex County "Stay Cool" logo. The insert says: When it's too hot outside, protect yourself."
(D) Place mats with the Windsor and Essex County "Stay Cool" logo. On the placement is a description of the Windsor and Essex County Heat Alert Response System, and tips to stay cool. P48, Figure 12D
Source: City of Windsor, Ont., 2010.
Through extensive consultations with stakeholders, including officials from the City of Detroit, and a review of best communication practices, the City of Windsor developed a number of outreach strategies to support three priority communication goals:
Goal 1: Inform residents and visitors of the effects of extreme heat and the actions required to reduce the risks.
Outreach strategies
- Inform media of heat alerts and provide information products
- Establish a hub for communicating and sharing information on heat-alert activities with stakeholders in addition to the website and 211 services
- Complete an audit of existing heat alert communication practices to determine lessons learned
- Use an e-mail blast that will notify anyone who signed up that a heat alert has been issued with an embedded website link for more information
Goal 2: Educate residents and visitors about extreme heat events and the measures being taken to protect them from health risks.
Outreach strategies
- Launch an education campaign
- Inform city residents and visitors about who will issue heat alerts and where to find out if a heat alert has been called
- Extend the reach of communication materials through the development of strategic partnerships
- Develop a media plan that considers mass media and includes targeted communication activities
Goal 3: Educate emergency responders and service providers about key indicators of an extreme heat event and the necessary policies and procedures for responding to or identifying health effects.
Outreach strategies
- Host train-the-trainer events to educate community partners on available educational tools and key messages
- Gain support for expanded participation by community partners during heat alerts (e.g. open cooling facilities, check on heat-vulnerable populations)
In early communication efforts during development of its HARS, Windsor implemented a targeted approach to reach the public and engage stakeholders. For example, it published two advertisements in the Summer Activity Guide that included heat-health information tailored to the general public and to those caring for infants and young children. Print advertisements were also placed in the summer editions of Windsor Parent Magazine and Retirement Living, which are free to the public. In 2011, the Windsor Essex County Health Unit drafted articles on heat and heat-illnesses that local papers and magazines included in their publications. Other outreach strategies completed in 2011 included pharmacy labels to reach people taking medications that could put them at risk, business cards with heat-health information for the physically active, colouring place mats for young children and fridge magnets for older adults. Partnerships developed through HARS will help to increase the effectiveness of messages delivered to the public.
For more information on the Windsor HARS, visit www.staycoolwindsor-essex.com.
3.7 Improving Heat Alert and Response Systems Through Evaluation
Create an evaluation plan during HARS development to integrate opportunities for data gathering in the implementation phase and ensure continuous measurement for longer-term program improvement.
- R.S. Kovats and L.E. Kristie, 2006Footnote 97
Performance measurement and evaluation can provide information about whether specific HARS elements are successful, and identify system strengths, weaknesses and opportunities for improvement.Footnote 7Footnote 97 Evaluation has traditionally been used as a way to refine and improve program delivery, and allow for adjustments to respond to the evolving needs and priorities of a community.Footnote 151 Few formal evaluations of HARS have been conducted and limited published information exists on methods for conducting such analysis.Footnote 7Footnote 29Footnote 97Footnote 134Footnote 142 However, guidance and conceptual frameworks that have been developed for public health program evaluation provide tools that can be used to investigate HARS performance.Footnote q Consultations with Health Canada's four pilot communities also informed the development of recommendations in this section. The sample partner survey provided in Appendix A was used by the pilot communities in their end-of-season HARS evaluation
3.7.1 Evaluation Design
Depending on the focus of the evaluation, two main categories of investigation should be consideredFootnote 151Footnote 155:
- Process evaluation--Determines if the HARS has been carried out as planned and whether each component of the system has been operating effectively.
- Outcome evaluation--Focusses on the impact of the program based upon the goals and objectives of the HARS.
An evaluation should be focussed on issues of greatest concern to partners and stakeholders, while being as simple and cost-effective as possible.Footnote 155Footnote 156 Informal feedback from stakeholders and target audiences, as well as observations about HARS performance from lead agencies, may be used for the evaluation; however, this type of data is often incomplete and may be biased. Formal evaluations are most credible and useful when information is gathered using a mix of qualitative (e.g. focus groups, in-depth interviews, open-ended survey questions) and quantitative methods (e.g. surveys, process tracking forms and records, large data sets). The most appropriate indicators and methodologies for data collection can be identified when the evaluation design addresses the following:
- evaluation goals
- data availability
- types of tools and measures needed for data collection
- frequency of data collection and optimal time frame to collect the data
- organizations responsible for data collection and analysis
A collaborative approach to the evaluation process, including identifying the core objectives, is essential.Footnote 97Footnote 157 Using this approach, partners and stakeholders contribute to the evaluation through their knowledge of individual and community-level vulnerabilities, target audiences for outreach activities, and existing information gaps.Footnote 152Footnote 155 Figure 13 provides a HARS schematic that can be used when designing an evaluation. It shows the links between core elements of a HARS and its ultimate goal.Footnote 97Footnote 157 The schematic can guide the evaluation process by highlighting how the HARS operates and by identifying program leads with their roles and responsibilities.
Figure 13: Schematic demonstrating links between core elements of HARS and ultimate goal
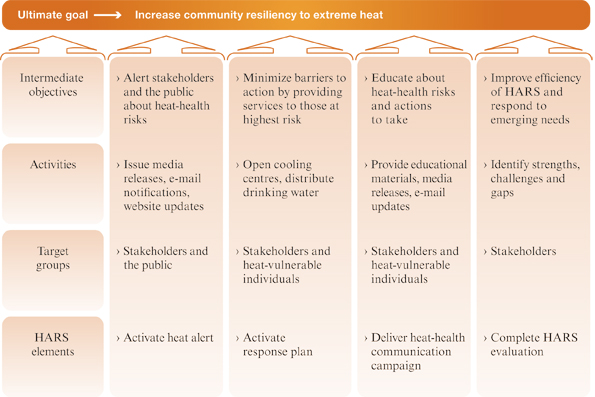
Figure 13: Schematic demonstrating links between core elements of HARS and ultimate goal
The figure is a schematic demonstrating links between core elements of HARS and the ultimate HARS goal (increase community resilience to extreme heat). The figure can be used when designing an evaluation and it lists the four HARS elements and for each, includes descriptions that pertain to target groups, activities and intermediate objectives.
- For activating the heat alert, target groups include stakeholders and the public, activities are to issue media releases, e-mail notifications and website updates and intermediate objectives are to alert stakeholders and the public about heat-health risks.
- For activating the response plan, target groups include stakeholders and heat-vulnerable individuals, activities are to open cooling centres and distribute drinking water and intermediate objectives are to minimize barriers to action by providing services to those at highest risk.
- To deliver the heat-health communication campaign, target groups include stakeholders and heat-vulnerable individuals, activities are to provide educational materials, media releases, and e-mail updates and intermediate objectives are to educate about heat-health risks and actions to take.
- To complete HARS evaluation, target groups are stakeholders, activities are to identify strengths, challenges and gaps and intermediate objectives are to improve efficiency of HARS and respond to emerging needs.
3.7.2 Process Evaluation
A HARS process evaluation should focus on gathering data during implementation to assess program-specific issues of relevance and performance as well as design and delivery. The evaluation should address pre-identified questions using a set of indicators (Table 5).
To acquire information for process evaluation, include data sources such as:
- financial reporting information
- post-extreme heat event and end-of-season debriefs
- interviews
- meteorological data
- meeting summaries
- website usage statistics and other inquiries received
- table-top exercises (Box 6)Footnote 159
Box 6: Understanding community resilience to extreme heat through table-top exercises
An extreme heat event table-top exercise is an opportunity to simulate an emergency situation in an informal, stress-free environment. It provides a community with valuable insights regarding how to strengthen its HARS.
Fredericton, Windsor, Winnipeg and the Assiniboine Regional Health Authority undertook extreme heat event table-top exercises in 2010 to identify and address gaps in the development of their respective HARS plans. Participants in the exercises included health and social service providers, first responders, emergency response personnel and other governmental and non-governmental organizations with a role in planning for and responding to extreme heat events. The focus of the exercises was on training and familiarization with roles, procedures and responsibilities, and the discussion of general problems and lessons learned in the context of an extreme heat emergency scenario. The results of these exercises are being used to inform implementation of new HARS in these communities.
3.7.3 Outcome Evaluation
An outcome evaluation is most appropriate for a well-developed HARS that has made progress toward intermediate objectives and ultimate goals. This type of evaluation should focus on program effectiveness by measuring changes in heat-related morbidity and mortality and the impact of public health interventions on awareness, knowledge, understanding and behavioural change. Outcome evaluations may need more resources because they require several years of observation, the establishment of baseline data, access to hospitalization and annual mortality data, and the expertise of an epidemiologist to conduct the analysis. Due to the complexity of measuring public health outcomes and program attribution, the methodology is less developed.Footnote 7 Potential indicators may include:
- number of daily heat-related deaths relative to historical baseline
- number of daily emergency calls during extreme heat events
- number of daily emergency room visits and hospitalizations during extreme heat events
- changes in health protective behaviours of at-risk populationsFootnote r
- changes in public awareness, knowledge and beliefs
- changes in service utilization
| Evaluation question | Potential indicators | |
|---|---|---|
| Operational Costs | What resources are used to operate the HARS? |
|
| Alert Protocol | Were the alerts issued efficiently? |
|
| Are extreme heat events forecasted and monitored accurately? |
|
|
| Response Plan | How involved were stakeholders with implementing response measures? |
|
| Did stakeholders follow the response plan and find it helpful? |
|
|
| Are response measures being used by the public (e.g. cooling facilities)? |
|
|
| Communication Plan | Were key messages and services provided to the public? |
|
| Was the target population aware of HARS and its key messages? |
|
|
| Did the target population understand and follow key messages? |
|
Source: Developed based on Canadian and international resources.Footnote 7Footnote 9Footnote 97Footnote 153Footnote 158Footnote 159
A detailed analysis of heat-health outcomes based on only a few years of implementation of a HARS will likely convey a limited understanding of program impact and effectiveness. A comparison between two extreme heat events, each with unique characteristics, is not sufficient to evaluate the effectiveness of a HARS.Footnote 123 However, evaluations of data based on only a few years of implementation of a HARS will help contribute to baseline data and may indicate early trends.
Currently, the health impacts of extreme heat events in Canada are not well documented for most communities and regions. In efforts to address this, the Canadian Disaster Database, provided by Public Safety Canada, compiles information on over 900 major natural, technological and conflict events that have directly affected Canadians in the past century, including extreme heat events.Footnote s Better monitoring of the health impacts of extreme heat will help to identify where effective measures should be implemented to reduce future morbidity and mortality.
3.7.4 Evaluation Results
It is critical that the conclusions and recommendations from an evaluation are shared with key partners and stakeholders in a timely manner to help inform decision-making and identify opportunities for improving performance.Footnote 159 Updates to HARS should be clearly communicated to partners every time a change is implemented.Footnote 111 In disseminating evaluation results and lessons learned, it is important to understand the audience and translate findings into clear and concise actionable tasks. The partnerships formed under a HARS are generally voluntary, and a well-designed evaluation will add credibility and strengthen relationships with partners.

Case Study 6
Evaluation of the Montréal Heat Plan Communication ProgramFootnote t
The City of Montréal has had a HARS in place for over 10 years. In 2007, Montréal Public Health conducted an evaluation of its Heat Plan Communication Program with a focus on three main areas:
- Message dissemination was evaluated by visiting distribution locations of promotional material and by conducting media monitoring. The evaluation assessed:
- effectiveness of communication vehicles by reviewing the availability of promotional material (i.e. cards, posters) at the distribution locations
- electronic and print media for coordination of coverage with Environment Canada heat warnings and inclusion of prevention messages
- Exposure of audiences to prevention messages and their impact on knowledge and protective behaviours during extreme heat events was evaluated by a telephone survey of people 65 or older to examine:
- exposure to prevention messages
- correlation between exposure, knowledge and protective behaviours
- Comprehension, acceptability and feasibility of the recommended heat-health prevention messages among older adults at high risk was evaluated through focus groups with people 65 or older (all but one living in non-air conditioned homes). The focus groups examined:
- physical discomfort levels as an indication of heat stress, willingness to ask for help, resources to adequately deal with extreme heat events
- choices of adaptive responses during extreme heat events
- evaluation of promotional material and heat-health messages

The result of this evaluation led to modification of Montreal's HARS communication tools (e.g. promotional material largely distributed to older adults). Certain messages were not retained in the new material. For example, the message to avoid alcohol, caffeine and soft drinks is no longer included because the participants in the focus groups did not view it as acceptable, and scientific support for this message is not solid. Participants did not view checking the temperature in their homes as being realistic and therefore this message was also removed. The message to wear light clothing and a hat was followed by the vast majority of seniors, regardless of their exposure to preventative messages; thus, it was not deemed to be useful.
The revisions to the outreach materials allowed for greater focus on three main messages: Seek out air-conditioned spaces, Drink a lot of water and Reduce physical activity. Finally, two other messages were maintained in the promotional material--"Let someone know how you are on a regular basis" and "Take cool showers or baths as often as needed or cool off using a damp facecloth." This latter recommendation was judged most useful by people without air conditioning and who have mobility challenges.
For more information on the Montréal HARS, visit www.dsp.santemontreal.qc.ca/ index.php?id=523&tx_wfqbe_pi1[uid]=1023.
3.8 Preventative Action: Reducing Urban Heat
"In the long term, improved urban planning, building design, energy and transport policies will ultimately reduce heat exposure."
- World Health Organization--Europe, 2009, p. ixFootnote 7
Health impacts from heat are not limited to extreme heat events that trigger an alert. Prolonged hot temperatures that do not trigger an alert can still result in mortality.Footnote 115 To combat this threat, a preventative approach is required that supports broader community health benefits, reduces vulnerability, and minimizes the overall burden of summertime and extreme heat events.Footnote 41Footnote 115Footnote 160 This long-term planning should include climate change mitigation measures, actions to reduce heat exposure by minimizing the urban heat island, and plans to strengthen the resiliency of communities to the impacts of climate change.Footnote 160 These can be accomplished by reducing greenhouse gas emissions, lowering community surface and air temperatures by planting trees for shade, and using building and infrastructure materials that store less heat and increase surface reflectivity.
3.8.1 The Urban Heat Island
An urban heat island is a built-up area that experiences higher temperatures than nearby rural areas. Urban centres and industrial areas tend to be built from darker, non-reflective and waterproof materials that absorb solar radiation and slowly release it as heat, resulting in average air temperatures approximately 3°C/5°F higher than those in surrounding areas (Figure 14). The impact of urban heat islands is strongest on hot, clear and calm days when the intensity of daytime heat can increase the surface temperature of the built environment.Footnote 161 The effect is most pronounced at night where temperatures have been recorded as much as 12°C/22°F higher than in nearby rural areas. This effect prevents nighttime relief from heat and contributes to additional morbidity and mortality.Footnote 53Footnote 74Footnote 161
The urban heat island is often not uniform across a city. Micro-urban heat islands can put some residents at higher risk during extreme heat.Footnote 47Footnote 56Footnote 161 Several factors contribute to the formation of an urban heat island and microclimates, including:
- a decrease in natural land cover (e.g. soil, rock, water, vegetation) that absorbs solar energy and releases it as water vapour through a cooling process called evapotranspirationFootnote 162 (e.g. in New York City, the lack of urban vegetation, particularly mature trees, is a key contributor to the urban heat islandFootnote 163)
- an increase in impervious, exposed and dry surfaces (e.g. roadways, sidewalks, buildings, infrastructure) that reduce water infiltration into the earth and absorb heatFootnote 161
- the physical components of the urban form (e.g. street orientation and width, building height and density, construction materials) that can trap reflected radiation, interfere with natural air movement and slow down the rate at which cities coolFootnote 53Footnote 57
- human activities such as driving, the production of waste heat from building ventilation and industrial processesFootnote 86Footnote 161Footnote 162
Figure 14: Variations between ambient temperatures in urban and rural areas
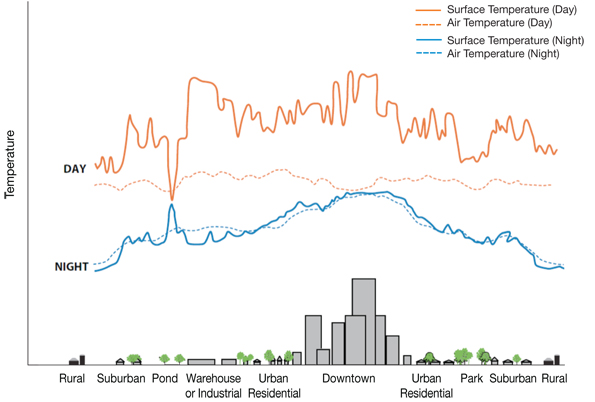
Figure 14: Variations between ambient temperatures in urban and rural areas
Figure illustrates the day and nighttime surface temperatures and the day and nighttime air temperatures across various types of built environments, including rural, suburban, pond or park, warehouse or industrial, urban residential and downtown environments. This figure shows a large increase in daytime surface temperatures in the industrial and downtown environments. Smaller increases in daytime surface temperatures are also seen in the suburban and urban residential environments. In contrast the daytime air temperatures remain constant in all environment types. The nighttime surface temperatures show a similar pattern as the daytime surface temperatures, with the largest increase in the downtown and smaller increases in urban residential environments. The nighttime air temperatures mirror the nighttime surface temperatures with the hottest space in the downtown (built up area).
Source: United States Environmental Protection Agency, 2009.Footnote 161
3.8.2 Reducing the Urban Heat Island
Although the urban heat island is a well-documented phenomenon, many Canadian municipalities do not incorporate measures to reduce it into their urban and land-use planning.Footnote 86Footnote 162 Most Canadian urban centres also face pressures from increased densification, urban sprawl, decaying infrastructureFootnote 164Footnote 165 and the needs of an aging population. If left unaddressed, urban centres will be faced with compounding risks from climate change,Footnote 166Footnote 167 including heat-health risks from an increase in frequency, length and severity of extreme heat events and secondary heat exposure resulting from the urban heat island.Footnote 40Footnote 57Footnote 167 A number of measures have been identified to build cooler and more heat resilient communities that can be implemented by building owners, urban planners and/or the entire community (Table 6).
| Reduction measure | Description and co-benefits | Implementation strategies |
|---|---|---|
| High albedoFootnote u and emissivityFootnote v materials |
|
|
| Green infrastructure |
|
|
| Mixed land-use to increase urban vegetation |
|
|
| Urban geometry |
|
|
| Reduce human-made (i.e. anthropogenic) heat sources |
|
|
Source: Examples of urban heat island reduction measures are based on actions by Canadian and international communities.Footnote 15Footnote 57Footnote 86Footnote 161Footnote 168Footnote 171
3.8.3 Co-benefits for Communities
The health, safety and well-being of people are linked to the quality of liveable environments, based upon their natural, built, social and cultural features.Footnote 74Footnote 172 Urban heat island mitigation is not a stand-alone issue. Changes in urban and land-use planning policies to reduce urban heat islands complement efforts to improve air quality and promote healthier communities.Footnote 168Footnote 175 Urban heat island mitigation measures could support other environmental and health benefits. Examples include:
Improved building design can reduce the need for air conditioning and may also improve indoor air quality and lower greenhouse gas emissions.Footnote 57Footnote 168
Increased green space and urban parkland can provide shade, dissipate heat and improve storm-water management and the quality of life for urban residents. Space for recreational walking or cycling can lead to positive impacts on cardiovascular disease and lowering the risk of diabetes by reducing obesity.Footnote 57Footnote 70Footnote 172Footnote 176
Increased accessibility to public transportation and pedestrian-friendly transit can reduce personal vehicle use and can provide options for some people who are heat-vulnerable (e.g. older adults, people with mobility challenges) to access cool places and maintain independence. This will also help reduce greenhouse gas emissions, increase physical activity, improve air quality and facilitate community engagement.Footnote 15

All levels of government have a role to play in implementing effective urban heat island mitigation measures. Municipalities have the greatest opportunity to adapt infrastructure to climate change, given their jurisdictional responsibility: over approximately two-thirds of all roads in Canada, waste disposal, sewage systems, land and building taxation and the regulation of land use.Footnote 166 Provinces also play an important role as many define the scope of and provide direction to planning authorities at municipal levels (e.g. Ontario Growth Plan for the Greater Golden Horseshoe area).Footnote 86 The federal government supports municipal initiatives to improve air, water and soil quality, and promotes the use of renewable energy and sustainable transportation services through programs such as the Green Municipal Fund. Government programs provide an opportunity to influence urban planning and design through capital spending (e.g. infrastructure, transit) and planning powers (e.g. bylaws, regulations).
Broad collaboration among officials and experts is required to successfully integrate urban heat island mitigation considerations into city planning decisions. Public health officials can promote a preventative approach to address heat-health risks by engaging with land-use and building planners; local and regional officials involved in transportation, parks, forestry; and public works sectors.
Appendices
Appendix A--Questionnaires
Sample Partner Questionnaire for Assessing Heat-Health Vulnerability
A facilitated session can be organized to gather information for a vulnerability assessment. This questionnaire is designed to help better understand partners' knowledge of heat-health risks and heat-vulnerable groups, existing services to minimize heat-health risks, and their vision for the future.
Engaging Stakeholders and Partners
1. Who needs to be involved in an assessment of vulnerability to the health impacts of extreme heat events in your community?
Understanding Vulnerability
2. Which of the following groups does your organization provide services to? (check all that apply)
- Older adults
- Infants and/or young children
- Individuals with chronic illnesses (e.g. diabetes, heart or respiratory conditions)
- Individuals unable to move or change positions by themselves
- Individuals taking certain medications (such as for mental health)
- Individuals who are socio-economically disadvantaged (such as homeless people)
- Newcomers to Canada / the community
- General public
- Other (please specify)
3. Do you currently provide information about the health effects of extreme heat to your clients? (check only one)
- Yes
- No
4. Who is vulnerable to extreme heat events in your community?
5. Does your organization know where individuals who have an increased risk of health complications from heat are located in your community? (check only one)
- Yes
- No
6. What characteristics make your community vulnerable or resilient to extreme heat events? (please explain)
7. What government or non-government programs or activities are in place in your community to manage existing heat-health risks? How effective are they? Who is the lead for the respective program?
8. Currently, what limitations and capacity issues are there for reducing heat-health risks?
Gauging the Ability to Plan and Respond to Extreme Heat Events
9. Describe how health risks from extreme heat may change in the future.
10. What options exist to reduce current and future heat-related risks to health?
11. What challenges exist for future efforts to reduce heat-health risks?
Sample Target Population Questionnaire
The sample target population questionnaire is designed to help better understand public awareness of heat warnings and perception of heat-health risks.
1. Over the past several summers, were you aware of extreme heat warnings?
- Yes
- No (if no, proceed to 8)
2. How did you hear about the warning? (select all that apply)
- Radio
- Television
- Newspaper
- Friend/Relative
- Social services person
- Internet
- Other
3. What recommendations were made to help people deal with the heat? (select all the apply)
- Avoid outdoors/sun
- Drink more liquids
- Find an air-conditioned location
- Use air conditioning at home
- Dress appropriately
- Check on neighbours / those at risk
- I didn't listen / don't remember
- Other
4. Did you do anything different on the days with extreme heat warning?
- Yes (if yes, proceed to 5a and omit 5b)
- No (if no, proceed to 5b)
5a. What did you do? (select all that apply)
- Avoided outdoors/sun
- Drank more liquids
- Found an air-conditioned location
- Used air conditioning at home
- Dressed appropriately
- Checked on neighbours / those at risk
- Other
5b. Why not? (select all that apply)
- Heat is not dangerous to me
- Too much of an inconvenience
- I wasn't concerned / There is always a warning about heat
- I didn't understand what to do / I was confused by the messaging
- Other
6. How seriously do you take warning about extreme heat?
- Very seriously
- Somewhat seriously
- Not seriously at all
7. Do you think there is a proper number of warnings and alerts for extreme heat each summer?
- There are too many
- There are too few
- There are the right amount
8. What do you use to cool your home? (select all that apply)
- Central air conditioning
- Window air-conditioning unit
- Fan
- Nothing
9. If you do not use air conditioning, was it due to financial considerations?
- Yes
- No
- Don't remember
10. How do you usually get your local news? (select all that apply)
- Radio
- Television
- Newspaper
- Internet
- Other
- N/A
11. Are you male or female?
- Male
- Female
12. What is your racial or ethnic background? (modify to reflect your community demographics)
13. What is your age?
- under 18
- 18-29
- 30-41
- 42-53
- 54-65
- Over 65
14. What is your approximate annual income?
- Under $20,000
- $20,000-$40,000
- $40,000-$60,000
- $60,000-$80,000
- $80,000-$100,000
- Over $100,000
Source: Adapted from Sheridan, 2007Footnote 142 and Kalkstein. Re-printed with permission of Springer Science+Business Media.
Sample Partner Survey: End-of-Season Heat Alert and Response System Evaluation
The sample partner survey can be used to evaluate HARS and better understand the relationships developed under HARS, partner satisfaction and recommended improvements.
Partnerships
1. To what extent do you agree or disagree that:
- Your organization established new relationships with partners to address extreme heat events.
- Strongly disagree
- Disagree
- Undecided
- Agree
- Strongly agree
- Your organization strengthened relationships with partners to address extreme heat events.
- Strongly disagree
- Disagree
- Undecided
- Agree
- Strongly agree
- Your HARS partnerships are effective.
- Strongly disagree
- Disagree
- Undecided
- Agree
- Strongly agree
- Your HARS partnerships will last.
- Strongly disagree
- Disagree
- Undecided
- Agree
- Strongly agree
2. How could your partnerships be improved?
Resources
3. To what extent do you agree or disagree that your HARS has all the needed resources.
- Strongly disagree
- Disagree
- Undecided
- Agree
- Strongly agree
- If you disagree, what additional resources are needed?
Benefits
4. To what extent do you agree or disagree that because of HARS:
- You are now better informed about the effects of extreme heat on health.
- Strongly disagree
- Disagree
- Undecided
- Agree
- Strongly agree
- You are better informed about what makes people vulnerable to extreme heat.
- Strongly disagree
- Disagree
- Undecided
- Agree
- Strongly agree
- Your organization benefited.
- Strongly disagree
- Disagree
- Undecided
- Agree
- Strongly agree
- Your organization helped prevent heat illnesses.
- Strongly disagree
- Disagree
- Undecided
- Agree
- Strongly agree
Outreach
5. To what extent do you agree or disagree that the communication developed through HARS were effective in reaching your audience.
- Strongly disagree
- Disagree
- Undecided
- Agree
- Strongly agree
- What aspects of the communication were most effective?
- What aspects of the communication were least effective? How could they be improved?
6. What actions did your organization undertake to help prevent heat illnesses?
Efficiency
7. To what extent do you agree or disagree that:
- HARS was implemented as planned.
- Strongly disagree
- Disagree
- Undecided
- Agree
- Strongly agree
If you disagree, what were the differences, why did they happen, and what was learned from them?
- HARS was effective.
- Strongly disagree
- Disagree
- Undecided
- Agree
- Strongly agree
If you disagree, how could HARS efficiency be improved?
Appendix B--Integration of Extreme Heat into the Assiniboine Regional Health Authority Disaster and Emergency Response Plan
Regional Action Plan--Severe Heat Emergency
Heat Alert--Regional response will be activated with the notification of a heat alert issued by Manitoba Health to the Assiniboine Regional Health Authority. The Heat Alert plan is designed to limit the effects of heat within the region.
Three-level system:
Heat Alert 1:
- Provide notice to all programs and services that a heat alert has been issued.
- Initiate daily Heat Alert Status Reports to report heat-related illness to Manitoba Health as required.
- Respond to media requests for information, sharing information from the Heat-Health Fact Sheet.
Heat Alert 2:
- Actions under Heat Alert 1.
- Consider activation of Corporate Incident Command Structure based on expected event duration.
- Ensure that community-based clients receive Heat-Health Fact Sheet.
- Post Heat-Health Fact Sheet to regional websites.
- Recommend to staff, clients and the public that they take precautions to reduce the impacts of the heat. Distribution of the Regional Newsletter.
- Ensure facilities are monitoring indoor temperatures.
- Provide for cooling areas or adequate rest periods for staff/clients.
- Consider use of the Alternate Meal Plan based on site-specific needs.
- Recommend limiting use of non-essential appliances that generate heat while promoting proper use of air conditioners and fans.
Heat Alert 3:
- Actions under Heat Alert 1 and 2.
- Implement Alternate Meal Plan based on site-specific needs.
- Consider staff scheduling to accommodate the use of needed laundry/kitchen services to cooler nighttime hours to help maintain internal temperatures.
- Work within programs and services to promote and distribute heat fact sheets to community settings or events.
- Report heat-related concerns to Manitoba Health (increases in related illness, inability to maintain services or programs due to staffing or infrastructure).
Post-Event:
- Coordinate a post-event debriefing as required.
- Notify all programs and services when the heat event has ended.
- Maintain monitoring for a post-event period as heat-related illness may still be present though temperatures have begun to cool.
Appendix C--Information Resources for Developing a Heat Alert and Response System Plan
There are a number of additional resources available to inform the planning process. This information can help address knowledge gaps, provide answers to common questions, and educate stakeholders on the need for and benefits of a HARS.
Government of Canada
Health Canada
- Extreme Heat and Health Resources
www.healthcanada.gc.ca/cc- Communicating the Health Risks of Extreme Heat Events: Toolkit for Public Health and Emergency Management Officials
- Audience Specific Public Heat-Health Brochures
- Extreme Heat Events Guidelines: Technical Guide for Health Care Workers
- Extreme Heat Events Guidelines: User Guide for Health Care Workers and Health Administrators
- Adapting to Extreme Heat Events: Guidelines for Assessing Health Vulnerability
Environment Canada
- National Climate Data and Information Archive (official climate and weather observation for Canada)
http://climate.weather.gc.ca/ - Air Quality Health Index (information tool to protect health)
www.airhealth.ca
Natural Resources Canada
- Canadian Centre for Remote Sensing (space-based science and satellite data)
http://www.nrcan.gc.ca/node/9309 - The Atlas of Canada (online climate information)
http://atlas.nrcan.gc.ca/site/english/index.html
Public Safety Canada
- Canadian Disaster Database (historical information on disasters)
www.publicsafety.gc.ca/prg/em/cdd/index-eng.aspx
Statistics Canada
- Population Health Surveys (including the Canadian Community Health Survey, National Population Health Survey, Canadian Health Measures Survey, and Health Services Access Survey)
https://www.statcan.gc.ca/eng/survey/household/3225 - Vital Statistics - Death Database (information on cause of death)
www.statcan.gc.ca/cgi-bin/imdb/p2SV.pl?Function=getSurvey&SDDS=3233&lang=en&db= imdb&adm=8&dis=2
International Organizations with Information on HARS
Australia
- Heatwave Plan for Victoria: Protecting Health and Reducing Harm from Heatwaves
www.health.vic.gov.au/environment/downloads/heatwaveplan_vic.pdf
United Kingdom
- Heatwave Plan for England: Protecting Health and Reducing Harm from Extreme Heat and Heatwaves
www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/documents/digitalasset/dh_127235.pdf
United States Environmental Protection Agency
- Excessive Heat Events Guidebook
www.epa.gov/heatisland/about/pdf/EHEguide_final.pdf
World Health Organization--Europe
- Heat-Health Action Plans: Guidance
www.euro.who.int/document/e91347.pdf - Improving Public Health Responses to Extreme Weather/Heat-Waves-- EuroHEAT: Technical Summary
www.euro.who.int/__data/assets/pdf_file/0010/95914/E92474.pdf - Public Health Advice on Preventing Health Effects of Heat
www.euro.who.int/__data/assets/pdf_file/0007/147265/Heat_information_sheet.pdf
Examples of Canadian Communities with a HARS
City of Fredericton
- Heat Alert and Response System
www.fredericton.ca/en/environment/2010mar30heatalertmain.asp
City of Greater Sudbury
- Hot Weather Response Plan - For Public Release
www.greatersudbury.ca/content/div_emergprep/documents/hot_weather_response_plan_2010.pdf
City of Hamilton
- City of Hamilton's Heat Response
https://www.hamilton.ca/public-health/health-topics/heat-alerts-heat-related-illness
Ville de Montréal
- Heat and extreme heat
https://www.santemontreal.qc.ca/en/heat/
City of Ottawa
- Hot Weather
http://www.ottawapublichealth.ca/en/professionals-and-partners/hot-weather-resource-kit-for-service-providers.aspx
City of Toronto
- Heat Alerts and Extreme Heat Alerts
https://www1.toronto.ca/wps/portal/contentonly?vgnextoid=b95f614ba4353410VgnVCM10000071d60f89RCRD&vgnextchannel=09c6e03bb8d1e310VgnVCM10000071d60f89RCRD
City of Vancouver
- Vancouver, it's hot
http://vancouver.ca/people-programs/hot-weather.aspx
City of Windsor
- Stay Cool Windsor-Essex
https://www.wechu.org/
City of Winnipeg
- Heat and Your Health
www.gov.mb.ca/health/publichealth/environmentalhealth/heat.html
Kingston, Frontenac and Lennox & Addington
- KFL&A Public Health
www.kflapublichealth.ca/Content.aspx?ThemeId=1&CategoryId=125&TopicId=91&ContentId=563
Region of Peel
- Hot Weather - Peel Public Health - Region of Peel
www.hotweatherinpeel.ca
The Regional Municipality of Halton
- Heat Alert
www.halton.ca/cms/One.aspx?portalId=8310&pageId=13692
Region of Waterloo
- Region of Waterloo - Extreme Weather
http://chd.region.waterloo.on.ca/en/healthyLivingHealthProtection/Extreme-Weather.asp
Assiniboine Region
- ARHA Disaster and Emergency Response Plan
https://ottawa.ca/en/residents/emergency-services/emergency-preparedness
| City/Region | Name | Triggers |
|---|---|---|
| Halton Region, Ont. | Heat Alert | Humidex advisory (humidex of 40) is issued by Environment Canada |
| Hamilton, Ont. | Heat Advisory (Stage 1) | Maximum humidex is 40 or greater for 1 day |
| Heat Warning (Stage 2) | Maximum humidex is 40 or greater for 2 or more days | |
| Heat Alert (Stage 3) | Maximum humidex is 40 or greater for 4 or more days or Maximum humidex is 45 or greater for 1 or more days |
|
| Kingston, Frontenac and Lennox & Addington, Ont. | Heat Alert (Level 1) | Humidex of 36 or 36ºC/97ºF for 2 consecutive days with no Smog Advisory |
| Heat Warning (Level 2) | Humidex of 36 or 36ºC/97ºF for 2 consecutive days with a Smog Advisory or Humidex 40 or 40°C/104°F for 2 consecutive days with no Smog Advisory |
|
| Heat Emergency (Level 3) | Humidex of 36 or 36ºC/97ºF with contributing factors (power outage, water failure, etc.) or Humidex of 40 or 40°C/104°F for 2 consecutive days with a Smog Advisory or Humidex of 45 or 45°C/113°F for 2 consecutive days |
|
| Montréal, Que. | Active Watch | Humidex of 40 or greater and 30°C/86°F |
| Alert | Forecast of maximum temperature of 33°C/91°F (weighted average) and minimum temperature of 20°C/84°F (weighted average) for at least 3 consecutive days or At least 2 consecutive nights with minimum temperature of 25°C/77°F or greater |
|
| Intervention | Triggered by extreme heat indicators that reach (or have a confirmed forecast to reach) the predicted levels specified for a heat alert or when there is a deterioration of health watch data (increases in excess number of deaths or emergency room consultations and ambulance transports shown by daily surveillance data) | |
| Ottawa, Ont. | Heat Alert | Maximum humidex is 36 or greater for 2 consecutive days |
| Heat Warning | Maximum humidex is 40 or greater for at least 2 consecutive days | |
| Heat Emergency | Maximum humidex is 45 or greater or When extreme weather and situational conditions will result in significant health consequences |
|
| Region of Waterloo, Ont. | Humidex Advisory | Maximum temperature is 30°C/86°F or greater and Maximum humidex value is 40 or greater |
| Sudbury, Ont. | Heat Advisory | Humidex of 36 is forecasted for at least 2 consecutive days |
| Heat Alert | Humidex of 40 is forecasted for at least 2 consecutive days or Humidex of 36 is forecasted for at least 2 consecutive days with a Smog Alert |
|
| Extreme Heat Alert | Humidex of 45 is forecasted for at least 2 consecutive days or Humidex of 40 is forecasted for at least 2 consecutive days with a Smog Alert |
|
| Toronto, Ont. | Heat Alert | An oppressive air mass is forecast and the likelihood of excess weather-related mortality exceeds 65% |
| Extreme Heat Alert | An oppressive air mass is forecast and the likelihood of excess weather-related mortality exceeds 90% |