Safety Code 35: Safety Procedures for the Installation, Use and Control of X-ray Equipment in Large Medical Radiological Facilities (2024)
Consumer and Clinical Radiation Protection Bureau
Environmental and Radiation Health Sciences Directorate
Healthy Environments and Consumer Safety Branch
Health Canada
2024
Table of contents
- Explanatory notes
- Introduction
- Principal objectives of the safety code
- Section A: Responsibilities and protection
- Section B: Facility and equipment requirements
- Section C: Quality assurance program
- Appendix I: Dose limits for occupational ionizing radiation exposures
- Appendix II: Shielding information checklist templates
- Appendix III: NCRP #49 methodology for calculation of shielding requirements for diagnostic X-ray installations
- Appendix IV: Shielding guides for storage of radiographic film
- Appendix V: Federal/provincial/territorial radiation safety agencies
- Appendix VI: Facility radiation protection checklist
- Appendix VII: Radiation measurement units
- Acknowledgements
- References
Explanatory notes
This document is one of a series of safety codes prepared by Health Canada to set out requirements for the safe use of radiation-emitting equipment.
This safety code has been prepared to provide specific guidance to large medical radiological facilities where diagnostic and interventional radiological procedures are routinely performed using radiographic, radioscopic or computed tomography equipment. Large facilities generally operate more than one type of radiological equipment, or have several suites of the same type of equipment. Most hospitals and computed tomography facilities fall within this category.
This safety code does not address radiation protection for dental and mammography facilities. For these facilities refer to Health Canada publications Safety Code 30: Radiation Protection in Dentistry – Recommended safety procedures for the use of dental X-ray equipment, and Safety Code 36: Radiation Protection and Quality Standards in Mammography - Safety Procedures for the Installation, Use and Control of Mammographic X-ray Equipment. Portions of this safety code may also be used as radiation protection guidance for small radiological facilities (such as chiropractic, podiatry, physical therapy, and bone densitometry) upon consultation with an expert in radiation protection.
The requirements and recommendations of this safety code do not apply to radiation therapy facilities and the equipment used in radiotherapy, including radiation therapy simulators, for localization and treatment planning.
This 2024 revision of the safety code replaces the revision published in 2008. This revision includes specific updates on patient shielding, occupational dose limit for the lens of the eye, and declaration of pregnancy by patients and operators.
The information in this safety code is intended for owners of healthcare equipment, physicians, technologists, medical physicists and other personnel concerned with equipment performance, image quality and the radiation safety of the facility.
Safety codes provide radiation protection guidance, information and advice. Health Canada's safety codes are sometimes referenced in regulations, standards and policies of other authorities, such as federal, provincial or territorial government departments and agencies. In those situations, the applicable department or regulatory authority determines how compliance with the safety code is verified. For example, Safety Code 35 is referenced in the Canada Occupational Health and Safety Regulations for the instruction and guidance of persons employed in Federal Public Service departments and agencies, as well as those whose employers are under the jurisdiction of the Canada Labour Code.
Rules governing the safe installation and use of X-ray equipment, as well as protocols and safety requirements for operators, may be established through provincial and territorial legislation, professional orders and associations. This may include requirements relating to who can perform specific actions or fulfill the roles and responsibilities outlined in this safety code. In some cases, provincial/territorial authorities may also reference Health Canada safety codes. The authorities listed in Appendix V should be contacted for details of the regulatory requirements of individual provinces and territories and to determine the applicability of this safety code.
The words must and should in this safety code have been chosen with purpose. The word must indicates a requirement that is essential to meet the currently accepted standards of protection, while should indicates an advisory recommendation that is highly desirable and is to be implemented where applicable.
In a field in which technology is advancing rapidly and where unexpected and unique problems continually occur, this safety code cannot cover all possible situations. Blind adherence to rules cannot substitute for the exercise of sound judgement. Recommendations may be modified in unusual circumstances, but only upon the advice of experts in radiation protection. This safety code will be reviewed and revised from time to time, and a particular requirement may be reconsidered at any time, if it becomes necessary to cover an unforeseen situation. Interpretation or elaboration on any point can be obtained by contacting the Consumer and Clinical Radiation Protection Bureau, Health Canada.
Introduction
Diagnostic and interventional radiology are an essential part of present day medical practice. Advances in X-ray imaging technology, together with developments in digital technology have had a significant impact on the practice of radiology. This includes improvements in image quality, reductions in dose and a broader range of available applications resulting in better patient diagnosis and treatment. However, the basic principles of X-ray image formation and the risks associated with X-ray exposures remain unchanged. X-rays have the potential for damaging healthy cells and tissues, and therefore all medical procedures employing X-ray equipment must be carefully managed. In all facilities and for all equipment types, procedures must be in place in order to ensure that exposures to patients, staff and the public are kept as low as reasonably achievable.
Diagnostic X-rays account for the major portion of man-made radiation exposure to the general population. Although individual doses associated with conventional radiography are usually small, examinations involving computed tomography and radioscopy can be significantly higher. However, with well-designed, installed and maintained X-ray equipment, and through use of proper procedures by trained operators, unnecessary exposure to patients can be reduced significantly, with no decrease in the value of medical information derived. To the extent that patient exposure is reduced, there is, in general, a decrease in the exposure to the equipment operators and other health care personnel.
The need for radiation protection exists because exposure to ionizing radiation can result in deleterious effects that manifest themselves not only in the exposed individuals but in their descendants as well. These effects are called somatic and genetic effects, respectively. Somatic effects are characterized by observable changes occurring in the body organs of the exposed individual. These changes may appear within a time frame of a few hours to many years, depending on the amount and duration of exposure to the individual. Genetic effects are an equal cause for concern at the lower doses used in diagnostic radiology. Although the radiation dose may be small and appear to cause no observable damage, the probability of chromosomal damage in the germ cells, with the consequence of mutations giving rise to genetic defects, can make such doses significant for large populations.
Since it is not possible to measure carcinogenic effects at low doses, estimates of the incidences of radiation effects at low doses are based on linear extrapolation from relatively high doses. Due to the uncertainties with respect to radiological risk, a radiation protection risk model assumes that the health risk from radiation exposure is proportional to dose. This is called the linear no-threshold hypothesis. Since the projected effect of a low dose increases the incidence of a deleterious effect only minimally above the naturally occurring level, it is impossible to prove by observation either the validity or falsity of this hypothesis. However, the linear no-threshold hypothesis has been widely adopted in radiological protection and has led to the formulation of the ALARA (As Low As Reasonably Achievable) principle. The ALARA principle is an approach to radiation protection to manage and control exposures to radiation workers and the general public to as low as is reasonable, taking into account social and economic factors.
In radiology, there are four main aspects of radiation protection to be considered. First, patients should not be subjected to unnecessary radiographic procedures. This means that the procedures are ordered with justification, including clinical examination, and when the diagnostic information cannot be obtained otherwise. Second, when a procedure is required, it is essential that the patient be protected from excessive radiation exposure during the examination. Third, it is necessary that personnel within the facility be protected from excessive exposure to radiation during the course of their work. Finally, personnel and the general public in the vicinity of such facilities require adequate protection.
While regulatory dose limits have been established for radiation workers and the general public, these limits do not apply to doses received by a patient undergoing medical X-ray procedures. For patients, the risk associated with the exposure to radiation must always be weighed against the clinical benefit of an accurate diagnosis or treatment. There must always be a conscious effort to reduce patient doses to the lowest practical level consistent with optimal quality of diagnostic information. Through close cooperation between medical professionals, technologists, medical physicists, and other support staff it is possible to achieve an effective radiation protection program and maintain a high quality medical imaging service.
Principal objectives of the safety code
This safety code is concerned with the protection of all individuals who may be exposed to radiation emitted by X-ray equipment used in a large radiological facility. The aim of this safety code is to provide radiological facilities with the necessary information to achieve the following principal objectives:
- to minimize patient exposure to ionizing radiation while ensuring the necessary diagnostic information is obtained and treatment provided
- to ensure adequate protection of personnel operating X-ray equipment
- to ensure adequate protection of other personnel and the general public in the vicinity of areas where X-ray equipment is used
To assist personnel in achieving these objectives, this safety code:
- sets out relative responsibilities of the owner, the X-ray equipment operator, the responsible user, the medical physicist or radiation safety officer, the referring physician, the information systems specialist, and the repair and maintenance personnel
- presents practices and procedures to minimize doses from X-ray equipment to operators and the public
- presents practices and procedures for minimizing radiation doses to patients while maintaining adequate image quality
- presents practices and procedures for ensuring the X-ray equipment is used in a safe manner
- provides information on facility design and shielding requirements
- specifies minimum standards of construction and performance for X-ray equipment
- supplies information required to implement and operate a quality assurance program for the facility
- provides a list of acceptance tests and quality control tests for various types of X-ray equipment and their accessories; and
- provides a schedule for performing quality control tests
This safety code is composed of three sections:
Section A: Responsibilities and protection
This section sets out the responsibilities of the owner, responsible user, operators and other staff for the safe installation, operation and control of the equipment, and sets out practices to minimize radiation doses to patients, staff and the public.
Section B: Facility and equipment requirements
This section sets out requirements for the facility design and minimum equipment construction and performance standards.
Section C: Quality assurance program
This section sets out requirements for quality assurance programs including acceptance testing and quality control procedures.
Section A: Responsibilities and protection
A.1.0 Responsibility of personnel
Although staff responsibilities described below are grouped separately, to obtain the optimal level of radiation safety and image quality, it is imperative that full cooperation exists among all concerned parties.
A.1.1 Owner
The owner is ultimately responsible for the radiation safety of the facility. It is the responsibility of the owner to ensure that the equipment and the facilities in which such equipment is installed and used meet all applicable radiation safety standards, and that a radiation safety program is developed, implemented and maintained for the facility. The owner may delegate this responsibility to qualified staff. How this responsibility is delegated will depend upon the number of staff members, the nature of the operation, and on the number of X-ray equipment owned. In any event, the owner must ensure that one or more qualified persons are designated to carry out the roles described below.
A.1.2 Responsible user
The main role of the responsible user is to monitor and manage the radiation safety program of the facility including personnel requirements, equipment performance and safety procedures and to communicate program information with the appropriate staff. There must be at least one person designated as the responsible user. If the responsible user also performs patient examinations, then all of the requirements listed in section A.1.3 for the X-ray equipment operator must also be met. The responsible user must:
- possess qualifications for operating the equipment required by any applicable federal, provincial, or territorial regulations or statutes and be certified according to a recognized standard, such as
- for physicians, the Royal College of Physicians and Surgeons of Canada or by the Collège des médecins du Québec, or
- for technologists, the Canadian Association of Medical Radiation Technologists or l'Ordre des technologues en radiologie du Québec
- acquire re-qualification or refresher training according to any applicable federal, provincial, or territorial regulations or statutes and according to a recognized standard, such as
- for physicians, the Royal College of Physicians and Surgeons of Canada or by the Collège des médecins du Québec, or
- for technologists, the Canadian Association of Medical Radiation Technologists or l'Ordre des technologues en radiologie du Québec
- ensure that the X-ray equipment, image processing equipment, and auxiliary equipment function correctly and are maintained properly by implementing and maintaining an effective imaging quality assurance program for the facility, including quality control testing, establishing diagnostic reference levels, and record keeping
- ensure that the equipment is used correctly, and maintained properly, by competent personnel who are properly trained in the safe operation of the equipment
- ensure that inexperienced personnel, including students, operate the equipment only under the direct supervision of a licensed, certified, and experienced X-ray equipment operator until competence in a given clinical procedure is achieved, at which time supervision should be indirectly provided by a supervisor available on-site when needed
- establish documented safe operating procedures for the equipment and ensure that operating staff are adequately instructed in them
- promulgate documented rules of radiation safety and ensure that staff are made aware of them through training
- ensure an investigation is completed of any known or suspected exposures received by personnel that are
- unusually higher than the usual dose received by that individual, or
- in excess of 1/20th of the dose limit for radiation workers, specified in Appendix I
- ensure that radiation levels in controlled and uncontrolled areas are below the maximum permissible limits such that the annual dose limits to radiation workers and the public, given in Appendix I, will not be exceeded
- ensure that an effective communication system is maintained between X-ray equipment operators, referring physicians, medical physicists/Radiation Safety Officers and information systems specialists to discuss all matters related to radiation protection of patients and workers; and
- ensure that the Medical Physicist/Radiation Safety Officer and all operators are provided with a copy of this safety code
A.1.3 X-ray equipment operator
All X-ray equipment operators have the responsibility of carrying out prescribed radiological procedures in a manner which does not cause any unnecessary exposures to patients, themselves and other workers in the facility. Depending on the type of radiological procedure, the equipment may be operated by a physician, a physician/practitioner or a radiation technologist.
All operators must:
- possess qualifications required by any applicable federal, provincial, or territorial regulations or statutes and be certified according to a recognized standard, such as
- for physicians, the Royal College of Physicians and Surgeons of Canada or by the Collège des médecins du Québec, or
- for technologists, the Canadian Association of Medical Radiation Technologists or l'Ordre des technologues en radiologie du Québec
- acquire re-qualification or refresher training according to any applicable federal, provincial, or territorial regulations or statutes and according to a recognized standard, such as
- for physicians, the Royal College of Physicians and Surgeons of Canada or by the Collège des médecins du Québec, or
- for technologists, the Canadian Association of Medical Radiation Technologists or l'Ordre des technologues en radiologie du Québec
- have documented training in
- the safe operation of the X-ray equipment and accessories used in the facility
- the radiological procedure being performed, iii) patient positioning for accurate localization of regions of interest
- all manufacturer-specified quality assurance procedures, if necessary; and
- radiation protection procedures and measures
- be familiar with, and have access to, the manufacturer's operator manual for the specific equipment used in the facility
- recognize the radiation hazards associated with their work and take measures to minimize them
- monitor their radiation exposures with the use of a personal dosimeter, if they are likely to receive a dose in excess of 1/20th of the dose limit to radiation workers specified in Appendix I
- have a thorough understanding of safe working methods and appropriate techniques and procedures, including the appropriate use of personal protective equipment
- have document clinical training, in accordance to federal, provincial, or territorial statutes and regulations and any relevant professional standards, on new radiological procedures before commencing independent work on patients
- strive to eliminate unnecessary radiographic procedures by reducing the number of retakes, and reducing all patient radiation exposures to the lowest practical values
- participate fully in the established quality assurance program for the facility, including reporting any change in equipment performance to the responsible user; and
- understand the recommendations of this safety code
A.1.4 Medical physicist/radiation safety officer
There must be a Medical Physicist or Radiation Safety Officer to act as an advisor on all radiation protection aspects during the initial stages of construction of the facility, installation of the equipment, and during subsequent operations. Medical physicists are health care professionals with specialized training in the medical applications of physics. A radiation safety officer is the title commonly assigned to a radiation safety specialist who routinely manages a facilities radiation protection program.
The medical physicist /radiation safety officer must:
- possess qualifications required by any applicable federal, provincial, or territorial regulations or statutes and be certified according to a recognized standard, such as
- for medical physicists, the Canadian College of Physicists in Medicine
- acquire re-qualification or refresher training according to any applicable federal, provincial, or territorial regulations or statutes and according to a recognized standard, such as
- for medical physicists, the Canadian College of Physicists in Medicine
- ensure that the installation complies with all applicable regulatory requirements, by
- assessing the radiation safety of an installation at the time of planning and/or construction of the facility, or when modifications are planned and/or being made to an existing facility
- registering the equipment with the appropriate agency when new equipment is purchased, and
- setting periodic scheduled inspections for the facility. In some jurisdictions, the agency responsible for inspections has the mandate for setting inspection schedules
- establish safe working conditions according to the recommendations of this safety code and the statutory requirements of federal, provincial, or territorial legislation, where applicable
- ensure that established safety procedures are being followed and report any non compliance to the responsible user
- review the safety procedures periodically and update them to ensure optimum patient and operator safety
- instruct X-ray equipment operators and other personnel participating in X-ray procedures in proper radiation protection practices
- carry out routine checks of equipment and facility safety features and radiation surveys
- ensure that appropriate radiation survey instruments are available, in good working condition, and properly calibrated
- keep records of radiation surveys, including summaries of corrective measures recommended and/or instituted (refer to section B.5.1)
- declare who is to be considered an occupationally exposed person (i.e. personnel who may receive a radiation dose in excess of 1/20th of the recommended dose limit for a radiation worker, as specified in Appendix I)
- organize participation in a personnel radiation monitoring service, such as that provided by the National Dosimetry Services, Health Canada, Ottawa, Ontario K1A 1C1
- ensure that all occupationally exposed persons wear personal dosimeters during radiological procedures or when occupational exposures are likely;
- review, manage and maintain records of occupational exposures received by personnel
- investigate each known or suspected case of excessive or abnormal exposure to patients and staff to determine the cause and to take remedial steps to prevent its recurrence
- participate in the establishment of diagnostic reference levels; and
- understand the recommendations of this safety code
A.1.5 Referring physician/practitioner
The referring physician/practitioner is the individual authorised to prescribe diagnostic or interventional X-ray procedures. The main responsibility of the referring physician/practitioner is to ensure that the use of X-rays is justified. In some jurisdictions, a registered nurse or nurse practitioner may be authorised by legislation to order X-ray examination. In such cases, the responsibilities of the referring physician/practitioner listed below would apply to those individuals. It is recommended to contact the appropriate provincial or territorial radiation safety agencies, listed in Appendix V, for information on any applicable provincial or territorial statutes or regulations.
The referring physician/practitioner must:
- possess qualifications required by any relevant federal, provincial, or territorial regulations or statutes and be licensed according to a recognized standard such as
- the Royal College of Physicians and Surgeons of Canada or by the Collège des médecins du Québec
- acquire re-qualification or refresher training according to any applicable federal, provincial, or territorial regulations or statutes and according to a recognized standard, such as
- for physicians, the Royal College of Physicians and Surgeons of Canada or by the Collège des médecins du Québec
- prescribe an X-ray examination based on professional experience, judgement and common sense
- give consideration to alternative, non X-ray utilizing, examinations
and should:- be confident that the procedure will improve the patient diagnosis and/or treatment sufficiently in comparison with alternate, non X-ray utilizing, methods of diagnosis and/or treatment
- be aware of the risks associated with X-ray procedures
A.1.6 Information systems specialist
Facilities performing digital image processing should have access to an individual who is trained and experienced in maintenance and quality control of information technology software and hardware such as those for PACS and teleradiology equipment. Depending on the facility, the individual may be on-site or available upon request. The required qualification of this individual will depend highly on the type of facility and the type of equipment used in the facility. In all situations, the information systems specialist must ensure confidentiality of patient records.
The information systems specialist should:
- be educated and experienced in information technology
- possess equipment-specific training provided by manufacturers, where available
- be knowledgeable of networking concepts such as DICOM and HL7
- be familiar with the workflow of the facility
- understand the policies and procedures in place within the facility
- understand the importance of and the requirements for an information systems quality assurance program
- communicate with staff any changes/upgrades made to the information management equipment hardware or software and the resulting consequences on the operating procedures of the facility
A.1.7 Repair and maintenance personnel
The repair and maintenance personnel are individuals authorised to perform hardware and software repairs and maintenance on X-ray generators, control systems, imaging systems and their operating software. Depending on the facility, these individuals may be on-site or available upon request, but in general, this function is sometime contracted to an outside organization, or to the equipment manufacturer. The required qualification of this individual will depend highly on the type of facility and the type of equipment used in the facility.
The repair and maintenance personnel should:
- have knowledge and training in
- repair and maintenance of radiological imaging equipment, and
- radiation protection principles and procedures
- ensure that, after a repair or maintenance procedure, the equipment meets the required regulatory standards or manufacturer' specifications
- ensure that all repair and maintenance procedures are properly recorded and communicated to the responsible user and other appropriate staff
- report any non compliance with the established safety procedures to the responsible user
- review the maintenance procedures periodically and update them to ensure optimum patient and operator safety
- communicate, if necessary, to staff the need for the appropriate acceptance testing, baseline setting and quality control testing; and
- follow manufacturers' recommendations for the repair and maintenance of equipment
A.2.0 Procedures for minimizing radiation exposure to personnel
The required and recommended procedures outlined in this section are primarily directed toward occupational health protection. However, adherence to these will also, in many instances, provide protection to visitors and other individuals in the vicinity of an X-ray facility. The safe work practices and procedures should be regarded as a minimum, to be augmented with additional requirements, when warranted, to cover special circumstances in particular facilities.
To achieve optimal safety, responsible users and equipment operators must make every reasonable effort to keep exposures to themselves and to other personnel as far below the limits specified in Appendix I as reasonably achievable.
A.2.1 General requirements and recommendations
- An X-ray room must not be used for more than one radiological investigation simultaneously.
- Except for those persons whose presence is essential, all persons must leave the room when the irradiation is carried out.
- Personnel must, at all times, keep as far away from the X-ray beam as practicable. Direct radiation exposure of personnel by the primary X-ray beam must never be allowed.
- Deliberate irradiation of an individual for training purposes or equipment evaluation must never occur.
- All personnel must use available protective devices (refer to section B.4.1).
- All operators of X-ray equipment, together with personnel (i.e., nurses) who routinely participate in radiological procedures, and others, likely to receive a radiation dose in excess of 1/20th of the dose limit to radiation workers specified in Appendix I, must be declared radiation workers and monitor their radiation exposures with the use of a personal dosimeter.
- Personal dosimeters must be worn and stored according to the recommendations of the dosimetry service provider. When a protective apron is worn, the personal dosimeter must be worn under the apron. If extremities are likely to be exposed to significantly higher doses, additional dosimeters should be worn at those locations on the body.
- All personal dosimetry records must be maintained for the lifetime of the facility.
- If an employer is notified of a radiation worker's pregnancy, they must take appropriate steps to ensure that the employee's work duties during the remainder of the pregnancy are compatible with the recommended dose limits as stated in Appendix I. Depending on the type of facility and on the type of work being performed by the employee, it may not be necessary to remove a pregnant person from their duties of operating the X-ray equipment. It is recommended that the decision to remove a pregnant person from any radiological duties include consideration of the radiation exposure risks associated with the employee's duties, as determined by a medical physicist or a radiation safety officer.
- Where there is a need to support weak patients or to support or comfort children, holding devices should be used. If parents, escorts or other personnel are called to assist, they must be provided with protective aprons and gloves, and be positioned so as to avoid the X-ray beam. No person should regularly perform these duties.
- All entrance doors to an X-ray room should be kept closed while a patient is in the room and must be closed while making an X-ray exposure.
- X-ray machines which are energized and ready to produce radiation must not be left unattended.
A.2.2 Requirements and recommendations for operation of mobile equipment
- Mobile units should be used only if the condition of the patient is such as to make it inadvisable for the examination to be carried out with a stationary unit in the main X-ray department.
- During operation, the X-ray beam should be directed away from occupied areas if at all possible, and every effort must be made to ensure that this beam does not irradiate any other persons in the vicinity of the patient.
- The operator must not stand in the direction of the direct beam and must be least 3 metres from the X-ray tube unless wearing personal protective equipment or standing behind a leaded shield.
- In a capacitor discharge unit, after an X-ray irradiation has been made, there is a residual charge left in the capacitors. The residual charge can give rise to a "dark current" and result in X-ray emission even though the irradiation switch is not activated. Therefore, the residual charge must be fully discharged before the unit is left unattended.
A.2.3 Requirements and recommendations for operation of radiographic equipment
- The irradiation should, as a general rule, be controlled from the control panel located in a shielded area. Operators should remain in the shielded area. In the case of special techniques where the operator is required to control the irradiation while at the side of the patient, appropriate protective clothing, in accordance with the requirements of section B.4.1, must be worn.
- The operator must have a clear view of the patient during every X-ray examination and must be able to communicate with the patient and/or attendants without leaving the control booth.
- Radiographic cassettes must never be held by hand during an irradiation.
A.2.4 Requirements and recommendations for operation of radioscopic equipment
- All persons, with the possible exception of the patient, required to be in the room during radioscopy and spot film operation associated with the radioscopic operation must wear protective aprons. Lead shields or curtains mounted on the radioscopic unit are not a sufficient substitute for the wearing of personal protective clothing such as lead aprons.
- Protective gauntlets should be worn by the radiologist during palpation in every radioscopic examination. During radioscopy, palpation with the hand should be kept to a minimum.
- All radioscopic examinations should be carried out as rapidly as possible using minimum dose rates and X-ray field size.
- For each type of radioscopic procedure, an assessment should be made of the physical positions of all personnel to ensure ease of operation of the equipment, visibility of the display, and protection from the radiation field.
A.2.4.1 Requirements and recommendations for performing angiography
Angiography is potentially one of the greatest sources of exposure to personnel in radiology, since it requires the presence of a considerable number of personnel close to the patient, radioscopy for extended periods of time and multiple radiographic exposures. For such procedures, all personnel must be aware of the radiation hazards involved and make every effort to adhere to the following requirements and recommendations.
- Full use must be made of the protective devices provided with X-ray equipment such as shielded panels, drapes, bucky slot covers, ceiling-suspended lead acrylic screens, etc.
- The patient is the largest source of scatter radiation. To avoid this scatter, operate the equipment with the tube under the patient and, if the tube is horizontal, stand on the side of the image receptor.
- All personnel must wear protective clothing and personnel dosimeters. Protective glasses should also be worn.
- All personnel who are not required to be immediately adjacent to the patient during the procedure must stand back as far as possible from the patient, while still able to effectively carry out their duties and, if at all possible, should stand behind a protective shield.
- Special shields in addition to the protective devices provided with the machine should be used.
A.3.0 Procedures for minimizing radiation exposure to patients
The largest single contributor of man-made radiation exposure to the population is dental and medical radiography. In total, such use of X-rays can account for more than 90 % of the total man-made radiation dose to the general population.
The risk to the individual patient from a single radiographic examination is very low. However, the risk to a population is increased by increasing the frequency of radiographic examinations and by increasing the number of persons undergoing such examinations. To protect patients from unnecessary radiation exposure, it is important to ensure that X-ray examinations are justified. This includes minimizing the number of radiographs taken for an examination to the number necessary for the clinical need, and ensuring optimization of the doses associated with the examinations.
Required and recommended procedures designed to protect the patient, outlined in this section, are directed toward the physician/practitioner, radiologist, and technologist. They are intended to provide guidelines for elimination of unnecessary radiological examinations and for optimizing doses to patients when radiological examinations are necessary.
A.3.1 Guidelines for the prescription of X-ray examinations
Unnecessary radiation exposures of patients can be significantly reduced by ensuring that all examinations are clinically justified. This can be done by adhering, as much as possible, to certain basic recommendations. These recommendations are presented below.
- The prescription of an X-ray examination of a patient should be based on clinical evaluation of the patient and should be for the purpose of obtaining diagnostic information or patient treatment.
- X-ray examinations should not be performed if there has been no prior clinical examination of the patient.
- Radiological screening must not be performed unless it has been proven that the benefit to the individual examined or the population as a whole is sufficient enough to warrant its use.
- It should be determined whether there have been any previous X-ray examinations which would make further examination unnecessary, or allow for the ordering of an abbreviated examination. Relevant previous images or reports should be examined along with a clinical evaluation of the patient.
- When a patient is transferred from one physician or hospital to another any relevant images or reports should accompany the patient and should be reviewed by the consulting physician.
- When prescribing a radiological examination, the physician should specify precisely the clinical indications and information required.
- The number of radiographic views required in an examination must be kept to the minimum practicable, consistent with the clinical objectives of the examination.
- Before performing X-ray examinations with the potential to directly irradiate the abdomen or pelvic area, patients of child bearing age should be informed of potential risks to a foetus. When an X-ray examination is being performed on a person that has disclosed a potential or confirmed pregnancy, the operator must take care to minimize exposure to the foetus, while also ensuring the required diagnostic information is obtained. The guidelines in section A.3.4 for radiological examinations of pregnant patients should be followed.
- If a radiograph contains the required information, repeat procedures must not be prescribed simply because the radiograph is not of the "best" diagnostic quality.
- Specialized studies should be undertaken only by, or in close collaboration with a qualified radiologist.
- A patient's clinical records should include details of X-ray examinations carried out.
More specific guidance for the prescription of imaging examinations is available from the Canadian Association of Radiologists (CAR) in their Diagnostic Imaging Referral Guidelines. These guidelines provide recommendations on the appropriateness of imaging investigations for the purpose of clinical diagnosis and management of specific clinical/diagnostic problems. The objective of these guidelines is to aid the referring physician/practitioner to select the appropriate imaging investigation and thereby reduce unnecessary imaging by eliminating imaging that is not likely to be of diagnostic assistance to a particular patient and by suggesting alternative procedures that do not use ionizing radiation but offering comparable diagnostic testing accuracy.
A.3.2 Guidelines for carrying out X-ray examinations
Next to elimination of unjustified X-ray examinations, the most significant factor in reducing patient exposure is ensuring that examinations are performed with optimized techniques following ALARA principle. It is possible, for example, to obtain a series of diagnostically-acceptable radiographs and have the patient exposures vary widely because of choice of technique and loading factors used. It is the responsibility of the operator and radiologist to be aware of this and to know how to carry out a prescribed examination with the lowest possible exposure to the patient.
The requirements and recommendations that follow are intended to provide guidance to the operator and radiologist in exercising their responsibility toward reduction of patient exposure.
A.3.2.1 General requirements and recommendations
- The operator must not perform any examination that has not been prescribed.
- The exposure of the patient must be kept to the lowest practicable value, consistent with clinical objectives and without loss of essential diagnostic information. To achieve this, techniques appropriate to the equipment available should be used.
- Particular care, consistent with the recommendations of section A.3.4, must be taken when radiological examinations of pregnant or potentially pregnant patients are carried out.
- The X-ray beam must be well-collimated to restrict it as much as is practicable to the area of diagnostic interest.
- The X-ray beam size must be limited to the size of the image receptor or smaller.
- For systems with multiple AEC sensors, the AEC sensor(s) covering the area of diagnostic interest should be selected.
- Techniques should be used to limit the exposure of radiosensitive tissues and organs, particularly for children (see section A.3.3).
- The focal spot-to-skin distance should be as large as possible, consistent with good radiographic technique.
- Radiological examinations of infants and children should only be performed using techniques and loading factors that have been modified for patient size and age.
- For very young children, special devices should be employed to restrict movement.
- Full details of the radiological procedures carried out should be noted on the patient's clinical records.
- All images captured, whether on film or on digital imaging systems, must remain with the patient study unless they are rejected by the operator for valid predefined quality issues. All rejected images must be collected for use during routine rejection analysis. The facility must have a program established to prevent the total loss of any images without review for reject analysis.
- Patient shielding should be avoided if it has the potential to unintentionally fall within the X-ray field of the image. This may negatively impact the examination (e.g., by introducing artifacts or obscuring anatomy) and result in repeat examinations and additional radiation exposure to the patient.
- In general, while all X-ray examinations must continue to be justified and optimized, the usage of patient shielding in medical imaging is not recommended unless there are clear benefits. Therefore:
- Shielding should not be used when it interferes with imaging and visualization of the anatomy
- Jurisdictional authorities of facilities should develop policies for patient shielding. Such policies should consider the specific technologies used at the facility, and be based on the use of patient shielding only for examinations where it will significantly contribute to minimizing dose to radiosensitive tissues and organs while not interfering with the required diagnostic information of the examination
- The following organizations may provide guidance that may be used to aid in assessing the need for patient shielding:
- the Canadian Organization of Medical Physicists (COMP)
- the Canadian Association of Radiologists (CAR)
- the Canadian Association of Medical Radiation Technologists (CAMRT)
- Provincial or Territorial radiation safety agencies or organizations
A.3.2.2 Requirements and recommendations for radiographic procedures
- The edges of the X-ray beam should be seen on all X-ray images to ensure that no more than the desired area has been irradiated. The selected image receptor and X-ray field size collimated onto it should be as small as possible, consistent with the objectives of the examination.
- For film-based imaging (when the implementation of digital radiography is not feasible), the most sensitive screen-film combination, consistent with diagnostically-acceptable results, should be used.
- To ensure that patient exposure is kept to a minimum, consistent with image quality, full advantage should be taken of a combination of techniques, such as:
- use of an anti-scatter grid or air gap between the patient and the image receptor
- use of the optimum focal spot-to-image receptor distance appropriate to the examination
- use of the highest X-ray tube voltage which produces images of good quality
- use of automatic exposure control devices designed to keep all irradiations and repeat irradiations to a minimum
- The operator of the X-ray equipment should evaluate the resulting images to verify that the techniques being used are producing diagnostic quality images and that the X-ray equipment is functioning correctly.
- To avoid the necessity of retakes, it is particularly important before taking a long series of images that a single preliminary image of the series should be taken to verify correctness of settings.
A.3.2.3 Requirements and recommendations for radioscopic procedures
- In view of the relatively high exposure that results from radioscopy, such procedures should only be carried out when an equivalent result cannot be obtained from radiography. Radioscopy must not be used as a substitute for radiography.
- Equipment operators must be trained in radioscopic procedures before carrying out radioscopy on patients. Training must meet with pertinent provincial/regional regulations. Continuing professional development must meet with the requirements of the Maintenance of Certification Program of the Royal College of Physicians and Surgeons of Canada.
- Where included in the scope of practice of technologists, a technologist who has been properly trained in radioscopic procedures can perform radioscopy on patients. It is recommended to consult provincial or territorial statutes and regulations governing the scope of practice of medical technologists.
- All radioscopic procedures should be carried out as rapidly as possible with the smallest practical X-ray field sizes.
- When operating equipment with automatic brightness control, the operator must monitor the X-ray tube current and voltage since both can rise to high values without the knowledge of the operator, particularly if the gain of the intensifier is decreased.
- When performing radioscopy, the operator must at all times, have a clear line of sight to the output display.
- Mobile radioscopic equipment should only be used for examinations where it is impractical to transfer patients to a permanent radioscopic installation.
- Cine fluorography produces the highest patient doses in diagnostic radiography because the X-ray tube voltage and current used are generally higher than those used in radioscopy. Therefore, this technique should not be used unless significant medical benefit is expected.
A.3.2.4 Requirements and recommendations for angiography
- Exposure to the patient's eyes and thyroid can result during neurological examinations, such as cerebral angiography and cardiac catheterization and angiography. The technique of the procedure should take into consideration the risk to the eyes and thyroid.
- To reduce doses to patient, keep irradiation time to a minimum.
- If possible, use an increased tube filtration to reduce low energy X-rays, and use a lower time frequency in pulse radioscopy.
- Keep the X-ray tube as far from the patient as possible and the image receptor as close to the patient as possible.
- For children and small adults, the grid should be removed when acceptable diagnostic image quality can be maintained without it since this will reduce the dose.
- Use magnification mode with caution as it may increase the dose to the patient.
- Use cine-run only as long as necessary, and if possible, use automated injection systems.
- If the procedure is long, reposition the tube so that the same area of skin is not subjected to X-ray beam.
- Facilities should have documented, for each type of interventional procedure, a statement on the radiographic images (projections, number and loading factors), radioscopy time, air kerma rates and resulting cumulative skin doses and skin sites associated with the various part of the interventional procedure.
A.3.2.5 Requirements and recommendations for computed tomography procedures
- The number of slices produced and the overlap between adjacent scans should be kept to the minimum practicable, consistent with clinical objectives of the examination.
A.3.3 Guidelines for reduction of dose to sensitive tissues
Ionizing radiation can produce gene mutations and chromosomal aberrations in cells. For cells that divide rapidly, deleterious radiation effects are more likely since mutations may be passed on to the cell progeny. Certain tissues may be more sensitive to the effects of radiation (e.g., rapidly dividing cells) and these are referred to as radiosensitive tissues or sensitive tissues. The relative risk of developing cancer due to exposure to a sensitive tissue or organ is described in ICRP 103 (ICRP 2007)Footnote 11. When considering the risk associated with radiation exposure to sensitive tissues, one must also consider the fraction of the tissue or organ that is exposed and the tissue weighting available in ICRP 103.
Reproductive organs (gonads) were previously considered highly sensitive tissues for which fetal and gonadal shielding were recommended, however the gonadal tissue weighting factor was reduced in ICRP 103.
In particular, individuals performing X-ray examinations of patients must pay special attention to the following factors that are important for reducing doses to sensitive organs:
- Correct primary collimation of the X-ray beam. It is not sufficient merely to limit the beam to the size of the image receptor. Care must be taken to further restrict the beam to only the region of the patient's body that is of diagnostic interest. Irradiation of any part of the body outside that region contributes nothing to the objective of the examination and only increases the dose to the body.
- Examinations of children and adolescents. X-ray examinations of young children and adolescents whose body tissues are developing should not be performed unless a condition exists such that the benefit of the diagnostic information outweighs the radiation risk.
- Appropriate selection of loading factors and technique. An appropriate selection of tube voltage, current and filtration is important to minimize the dose to the patient while maintaining acceptable diagnostic quality of the image.
- Sensitivity of imaging system. Doses are related to the sensitivity of the imaging system. Thus, an increase in the sensitivity of the imaging system reduces the dose; conversely, decreasing the sensitivity increases the dose. It is therefore very important to maintain the sensitivity of the imaging system at its optimum value and to be alert for any significant deterioration.
- Routine gonadal shielding should not be used. Recent evidence (including a reduction in the ICRP tissue weighting factor of the gonads relative to other tissues from 0.2 to 0.08 in ICRP 103) has demonstrated that use of gonadal and fetal shields shows negligible benefit to either the patient or their offspring (ICRP 2007, ACOG 2017) Footnote 11 Footnote 3. Furthermore, patient shielding of the gonads may reduce the effectiveness of an exam by obscuring anatomy of interest, reducing image quality, or interfering with automatic exposure control (Fawcett et al., Frantzen et al., Lee et al., ACR 2017)Footnote 7 Footnote 8 Footnote 20 Footnote 4. See section A.3.2.1 for guidance on patient shielding.
A.3.4 Guidelines for radiological examinations of pregnant persons
Radiological examinations of the pelvic area of a pregnant person may potentially irradiate the foetus. The dose to a foetus from most correctly performed diagnostic procedures has not been shown to increase the risk of prenatal or postnatal death, developmental damage, or impairment of mental development. The lifetime risk of developing cancer due to in-utero exposure is similar to that from exposure in early-childhood (ICRP 2007)Footnote 11. As this risk is low, radiological examinations of a pregnant person can be performed if the benefit outweighs this risk.
Regardless of pregnancy status, radiography examinations should only be carried out using a well-collimated X-ray beam (see section A.3.2.1). For X-ray examinations with the potential to irradiate the abdomen or pelvis, patients should be informed of the potential risks to a foetus. If a patient discloses a pregnancy or potential pregnancy, the following recommendations apply to their X-ray examinations:
- Only justified investigations should be taken in the case of pregnant or suspected pregnant patients. In some circumstances, it may be acceptable to postpone an X-ray examination until after the pregnancy.
- Where radiological examinations of the pelvic area or abdomen are justified, specialized or alternate protocols should be used where appropriate to optimize the dose to the patient to the absolute minimum possible while ensuring the necessary diagnostic information can be obtained.
- If a radiological examination is required in which the pelvic area is directly exposed, the prone position should be used when possible. This has the effect of shielding the foetus from the softer X-rays and hence reducing the foetal dose.
A.3.5 Diagnostic reference levels (DRLs)
A.3.5.1 Introduction
Doses for medical diagnostic procedures can vary widely between equipment and facilities. Numerous surveys have demonstrated that, for typical procedures, the difference in radiation doses can be as wide as a factor of 50 to 100. For interventional procedures, this difference can be even wider. In diagnostic radiology, the use of surface air kerma limits is not sufficient since these dose limits are usually set at a level high enough so that any doses greater than the limit is clearly unacceptable, but this limit does not help in optimising patient doses. For this reason, the concept of Diagnostic Reference Levels (DRLs) is introduced, instead of using maximum dose limits.
The purpose of DRLs is to promote a better control of patient exposures to X-rays. This control must be related to the clinical purpose of the examination. DRLs must not be seen as limits but instead as guidance to optimise doses during procedures. DRLs are based on typical examinations of standardized patient or phantom sizes, and for a broad type of equipment. While it is expected that facilities should be able to attain these levels when performing procedures using good methodologies, it is not expected that all patients should receive these dose levels but that the average of the patient population should. DRLs are useful where a large reduction in patient doses may be achieved, such as for computed tomography (CT) procedures, where a large reduction in collective doses may be achieved, such as for chest X-rays, or where a dose reduction will result in a large reduction in risk, such as for paediatric procedures. However, interventional procedures are not going to be addressed at this time since it is difficult to establish DRLs for them due to the variability in techniques, the frequency of procedures, the difficulty in dose measurement, and the lack of published data.
A.3.5.2 Application
The tables shown in section A.3.5.3, list representative ranges of DRLs for radiographic procedures, performed on adults and children, radioscopic procedures and CT procedures. It is obvious that not all facilities will perform all of the listed procedures. Therefore, each facility should establish DRLs for those procedures relevant to them and where the number of patients undergoing the procedures is sufficiently high. A facility may set DRLs for other procedures not presented in the tables but which are being performed. At least one procedure should be evaluated for each X-ray equipment.
DRL measurements can be performed in two different ways; with a phantom specifically designed for the procedure, or using patients. In general, it is preferable to use phantoms since the measurements can be more easily replicated and offer more flexibility in the type of procedures which can be performed. Appropriate phantom, such as phantoms for chest, lumbar spine and abdomen representing a patient thickness, in the PA projection, of 23 cm are acceptable for DRL measurements, as long as they are consistently used. DRLs for CT are based on the weighted CT Dose Index, or CTDIw which can be determined by using CT Dosimetry Phantoms, described in Table 22, section C.3.6.3.
When patients are be used to establish DRLs, measurements should be done only on patients whose individual weight is 70 ± 20 kg, and the average weight measurement of the patients should be 70 ± 5 kg. It is recommended that the minimum sample size for a specific procedures or equipment be 10 patients. Patients should not be used for paediatric procedures.
Entrance surface doses for establishing DRLs can be measured using thermoluminescent dosimeters (TLDs) placed on the tube side of the patient, by using dose area product (DAP) meters, or through information retrieved from the Radiology Information System (RIS), or other means. The use of DAP is more practical since the whole procedure is recorded and their use is less complicated than TLDs, while with the use of RIS, the patient weight may not be available.
The values presented in section A.3.5.3 are provided to facilities for guidance. The values presented are dependent of patient size and, as such, a facility will need to evaluate whether their patient population falls within the range of patient size for the procedure. While this safety code recommends representative DRLs, a hospital or clinic can set their own local DRLs if enough data is available. The facility should create a list of reference doses for their patient population and use these values within their quality assurance program. DRL values should be reviewed from time to time to assess their appropriateness. It is recommended that this review be done annually.
Radiological facilities which fall under provincial or territorial jurisdiction should contact the responsible agency in their respective region for information on any provincial or territorial statutory or regulatory requirements concerning dose limits. A listing of these responsible agencies is provided in Appendix V.
DRL values must not be used for comparison with individual patients. The values should be compared only with the average of a collection of patients of a specific weight. The evaluation of conformity with DRLs should be done at the X-ray room level or X-ray equipment type, i.e., mobiles, CT. For each examination under consideration, the mean patient doses for each room should be compared to the DRL for the examination. If the mean dose is found to significantly and consistently exceed the suggested DRL, an investigation of the performance of the equipment, the radiological technique used, and the methodology of dose measurement should be done in order to reduce patient doses. It is recommended that this action level be set at a defined proportion (i.e., 25% of the mean) and at least twice the standard error of the mean of the measurements.
A.3.5.3 Recommended DRL values
Table 1 presents representative DRL values for radiographic procedures performed on adults. Table 2 presents DRL values for a 5 year old child along with the mean body thicknesses for each examination. It should be noted that the range of values provided for the entrance surface dose is reflective of the variation of values found in published data. Representative DRLs for radioscopic and CT examinations are shown in Table 3 and Table 4 respectively.
| Examination | Entrance surface dose (mGy) |
|---|---|
| Chest (PA) | 0.2 - 0.3 |
| Chest (LAT) | 0.7 - 1.5 |
| Thoracic Spine (AP) | 5 - 8 |
| Thoracic Spine (LAT) | 7 - 10 |
| Lumbar Spine (AP) | 7 - 10 |
| Lumbar Spine (LAT) | 15 - 30 |
| Abdomen (AP) | 7 - 15 |
| Pelvis (AP) | 5 - 10 |
| Skull (AP) | 4 - 5 |
| Skull (LAT) | 2 - 3 |
| Examination | Mean body thickness (cm) (Hart et al.)Footnote 9 |
Entrance surface dose (mGy) |
|---|---|---|
| Chest (AP/PA) | 13.4 | 0.05 - 0.15 |
| Chest (LAT) | 18.8 | 0.15 - 0.25 |
| Abdomen (AP/PA) | 13.6 | 0.5 - 1.0 |
| Pelvis (AP/PA) | 13.7 | 0.6 - 1.0 |
| Skull (AP) | 17.8 | 1.0 - 2.0 |
| Skull (LAT) | 13.8 | 0.8 - 1.5 |
| Examination | Dose area product (Gycm2) |
|---|---|
| Abdominal Radioscopy | 20 - 70 |
| Barium Enema | 30 - 60 |
| Coronary Angiography | 35 - 75 |
| Examination | CTDIw (mGy) | Dose length product (mGy cm) |
|---|---|---|
| Head | 60 | 930 - 1300 |
| Face and Sinuses | 35 | 360 |
| Chest | 30 | 580 - 650 |
| Abdomen - Pelvis | 35 | 560 - 1100 |
| Liver and Spleen | 35 | 470 - 920 |
Section B: Facility and equipment requirements
B.1.0 Facility requirements
B.1.1 General criteria
In the planning of any medical X-ray facility the main priority is to ensure that persons in the vicinity of the facility are not exposed to levels of radiations which surpass the current regulatory exposure limits. Appropriate steps must be taken to ensure adequate shielding is present to meet the following requirements:
- the radiation levels in controlled areas that are occupied routinely by radiation workers must be such that no radiation worker is occupationally exposed to more than 20 mSv per year; and
- the radiation levels in uncontrolled areas must be such that no person receives more than 1mSv per year
Appendix I provides a detailed description of the regulatory dose limits. For medical X-ray imaging facilities, controlled areas are typically in the immediate areas where X-ray equipment is used such as the procedure room and X-ray control booths. The workers in these areas are primarily equipment operators such as radiologists and radiation technologists who are trained in the proper use of the equipment and in radiation protection. Uncontrolled areas are those occupied by individuals such as patients, visitors to the facility, and employees who do not work routinely with or around radiation sources (NCRP 2004)Footnote 23.
In general, attention to the basic principles of distance, time and shielding are required to determine shielding needs.
B.1.2 Design and plan of X-ray facility
In the early stages of designing and planning a medical X-ray facility, three steps should be taken to ensure adequate shielding is in place to provide the necessary level of radiation protection:
- preparation of facility plans
- considerations for room design and layout
- determination of parameters governing shielding requirements
B.1.2.1 Preparation of facility plan
In order to determine the shielding requirements for an X-ray facility a floor plan must be prepared, clearly identifying the following components:
- The dimensions and shape of the room where the X-ray equipment is operated and the physical orientation of the room (a mark indicating North).
- The location where the X-ray equipment is planned to be placed and the range of movement of the X-ray tubes.
- The location of the control booth, if applicable.
- The location, use, occupancy level and accessibility of adjacent rooms, as well as rooms above and below the facility.
- The designation of the adjacent rooms, whether to be designated as a controlled or uncontrolled area. Controlled areas, mainly occupied by radiation workers, are subject to the limit of 20 mSv per year, whereas uncontrolled areas, mainly occupied by non-radiation workers, are subject to the limit of 1 mSv per year. In uncontrolled areas, where radiation sensitive populations are present, such as paediatric wards, a constraint level of 0.30 mSv per year should be used.
- The location where image processing is performed, i.e., location of darkrooms, film storage area, computer workstations.
- The position of all windows, doors, louvers, etc., that may affect radiation protection requirements.
- The planned and existing materials used to construct the walls, floor, ceiling, and the control booth, and their thicknesses including additional materials currently being used, or planned for use, as radiation shielding barriers.
- The application of the protective barriers. Will the intervening shield between the X-ray tube and the occupied area act as a primary or as a secondary protective barrier, i.e., will the barrier be required to attenuate the direct X-ray beam or stray radiation only?
B.1.2.2 Considerations for room design and layout
When designing the layout of the X-ray facility, the following general recommendations must be considered.
- Radiology rooms, with stationary X-ray equipment, which can be accessed from public areas should be equipped with a self-closing door, and must be identified with warning signs incorporating the X-ray warning symbol and the words "Unauthorized Entry Prohibited". Acceptable forms of the X-ray warning symbol are given in the Radiation Emitting Devices Regulations for Diagnostic X-ray Equipment (Schedule II, Part XII).Footnote 25
- Mobile X-ray equipment used routinely in one location must be considered as a fixed installation and the shielding needs for the equipment and room must be determined accordingly.
- The rooms containing the X-ray equipment should be designed to provide adequate working space to the equipment operator and to allow for ease of patient movement.
- The X-ray equipment should be positioned in the room in such a way that, during an irradiation, no one can enter the room without the knowledge of the equipment operator.
- The X-ray beam must always be directed toward adequately shielded areas. Particular attention must be paid to the adequacy of shielding for chest radiography using wall mounted image receptors.
- Whenever possible, the X-ray beam and scattered radiation must be absorbed as close as possible to the patient or scatterer.
- A control booth must be provided for the protection of the operator, if applicable, for the type of equipment. The control booth, and the viewing window, must have shielding properties such that no operator is occupationally exposed to more than 0.4 mSv/week. The ALARA principle requires that additional shielding be specified in the design to further reduce operator exposure, wherever this can reasonably be done. Mobile protective screens must not be considered adequate as a control booth for radiological procedures.
- The control booth should be located in an area, whenever possible, such that the radiation has to be scattered at least twice before entering the booth.
- Shielding must be constructed to form an unbroken barrier and if lead is used, it should be adequately supported to prevent "creeping".
B.1.2.3 Determination of parameters governing structural shielding requirements
The thickness of the shielding material, such as lead, concrete, or gypsum wallboard, required to reduce radiation levels to the recommended dose limits can be determined through calculations. In general, the radiation exposure to individuals depends primarily on the amount of radiation produced by the source, the distance between the exposed person and the source of the radiation, the amount of time that an individual spends in the irradiated area, and the amount of protective shielding between the individual and the radiation source.
The parameters listed below must be considered for the calculation of barrier thicknesses. Allowance should be made for possible future changes in anyone or all of these parameters, including increases in use and occupancy factors, in operating tube voltage and workload, as well as modifications in techniques that may require ancillary equipment.
-
The maximum X-ray Workload, (W) or the workload distribution.
The workload is a measure of the operational time or the amount of use of the X-ray equipment. A workload distribution indicates the workload across a range of operating voltages. The workload and workload spectrum can be determined by recording the operating voltage and current-time product of each irradiation taken in each X-ray suite over a set period of time (i.e., week). For irradiations made under Automatic Exposure Control, the operating voltage, procedure type and patient thickness should be recorded to be used later to estimate the current-time product. If actual workload values are not available, Table 5 presents estimated total workloads for various medical X-ray facilities (NCRP 2004) Footnote 23
Table 5: Typical workloads (NCRP 2004)Footnote 23 Total workload per patient
(mA min/patient)Typical number of patients
(per 40 hour week)Total workload per week
(mA min/week)Average Busy Average Busy Radiographic Room
(chest)0.6 120 160 75 100 Radiographic Room
(other)1.9 120 160 240 320 Dedicated Chest Room 0.22 200 400 50 100 R and FFootnote aRoom
(radioscopic system)13 20 30 260 400 R and FFootnote aRoom
(radiographic system)1.5 25 40 40 40 Angiography Room
(cardiac)160 20 30 3,200 4,800 Angiography Room
(other vascular)64 20 30 1,300 2,000 - Footnote a
-
R and F is a room that contains equipment for both radiography and radioscopy (fluoroscopy).
-
The occupancy factor (T)
The Occupancy factor is the fraction of time that the area under consideration is occupied by the individual (employee or public) who spends the most time at that location while the X-ray equipment is operating. The following table present recommended occupancy factors.
Table 6: Occupancy factors Factor Location T=1 Administrative offices and receptionist areas, laboratories, pharmacies and other areas fully occupied by an individual, attended waiting rooms, children's indoor play areas, adjacent X-ray rooms, image viewing areas, nurses' stations, X-ray control rooms, living quarters. T=1/2 Rooms used for patient examinations and treatments. T=1/5 Corridors, patient rooms, staff lounges, staff rest rooms. T=1/8 Corridor doors. T=1/20 Public toilets, unattended vending areas, storage rooms, outdoor areas with seating, unattended waiting rooms, patient holding areas. T=1/40 Outdoor areas with only transient pedestrian or vehicular traffic, unattended parking lots, vehicular drop off areas (unattended), attics, stairways, unattended elevators, janitor's closets. -
The use factor (U)
The use factor, is the fraction of the workload during which the X-ray beam is pointed in the direction under consideration. The following table presents recommended use factors.
Table 7: Use Factor for primary barrier Factor Location Primary barrier U=1 Floors of radiation rooms, walls containing a vertical image receptor; any other walls, doors or ceiling areas routinely exposed to the direct radiation beam. U=1/4 Doors and wall areas of radiation rooms not routinely exposed to the direct radiation beam. U= 1/16 Ceiling areas of radiation rooms not routinely exposed to the direct radiation beam. Secondary barrier U=1 The use factor for secondary protective barriers is always taken to be 1.
B.1.3 Shielding calculations
Shielding calculations must be made for both primary and secondary protective barriers. Primary protective barriers provide shielding from the direct X-ray beam and therefore must be placed in such an orientation as to intersect the X-ray beam. Secondary protective barriers are required to provide shielding from scattered and leakage X-rays.
Comprehensive shielding calculations for large radiological facilities should only be performed by individuals with current knowledge of structural shielding design and the acceptable methods of performing these calculations. It is recommended that shielding calculations be performed using the methodology presented in the National Council on Radiation Protection and Measurements (NCRP) Report No. 147: Structural Shielding Design for Medical X-ray Imaging Facilities (NCRP 2004)Footnote 23. However, it must be noted that the shielding design goals specified in NCRP Report 147 are not adopted in this safety code. The shielding design goal values may be lower but must not exceed the limits set out in section B.1.1 for controlled and uncontrolled areas. Due to the extensiveness of the information, the methodology of NCRP 147, including equations, tables and figures, is not provided in this safety code. Alternatively, the methodology presented in NCRP Report No. 49 (NCRP 1976)Footnote 21 is also acceptable and presented in Appendix III.
Under the methodology used in NCRP Report 147, the following are assumptions made in the shielding calculation:
- The attenuation of the radiation beam by the patient is neglected.
- The incidence of the radiation beam is always perpendicular to the barrier being evaluated.
- The calculation does not take into account the presence of materials in the path of the radiation other than the specified shielding material.
- The leakage radiation from the X-ray equipment is assumed to be an air kerma of 0.876 mGy h-1.
- The minimum distance to the occupied area from a shielded wall is assumed to be 0.3 m.
The information outlined in sections B.1.1 and B.1.2 along with the final plans of the installation must be submitted for reviewed by the appropriate responsible government agency. For installations under federal jurisdiction, the responsible agency is the Consumer and Clinical Radiation Protection Bureau, Health Canada, Ottawa, Ontario K1A 1C1. Radiological facilities that fall under provincial or territorial jurisdiction should contact the responsible agency in their respective province or territory listed in Appendix V.
B.1.3.1 Radiographic films
Film storage containers must be adequately shielded to ensure that excessive exposure of film by X-rays does not occur. Sufficient film shielding must be in place to reduce the radiation level to stored film to less than 0.1 mGy over the storage period of the film. The values presented in Appendix IV are very conservative but will protect films from radiation exposure for most circumstances. Once films are loaded into cassettes, radiation exposure levels should be less than 0.5 µGy and the resulting increase in the base-plus-fog should be less than 0.05 O.D. Refer to Appendix IV for storage guides for radiographic film.
B.1.3.2 Radiographic X-ray equipment and dedicated chest radiographic equipment
Primary and secondary shielding must be provided for radiographic equipment where the tube can be manipulated in several directions. The walls and floor where the X-ray tube can be directed are considered primary barriers whereas the other walls and ceiling are secondary barriers. The primary barrier includes the wall behind the vertical image receptor, or "wall or chest bucky", and the floor under the radiographic table. For dedicated chest radiographic equipment, the wall behind the image receptor is considered a primary barrier.
The X-ray tube should never be directed towards the control booth. Therefore the walls of the control booth are calculated as secondary barriers. The information required for calculation of the shielding of radiographic X-ray equipment and dedicated chest radiographic equipment is found in Table AII.1 of Appendix II.
B.1.3.3 Radioscopic X-ray equipment and angiographic X-ray equipment
The design of radioscopic X-ray equipment is such that only secondary shielding must be provided for these types of systems. However, in systems where an X-ray tube for radiography is also present, the shielding for this X-ray tube must be evaluated independently, as in section B.1.3.2. When equipment include more than one X-ray tube, such as in cardiac systems, the shielding calculation must take into account each X-ray tube independently. The information required for calculation of the shielding of radioscopic X-ray equipment is found in Table AII.2 of Appendix II.
B.1.3.4 Computed tomography equipment
The design of computer tomography equipment is such that only secondary shielding must be provided. The calculation of shielding for CT rooms should not rely on workload values as defined in section B.1.2.3 and therefore it is recommended that shielding requirements be calculated using the methodology of NCRP 147 for CT equipment. The information required for calculation of the shielding of CT equipment is found in Table AII.3 of Appendix II.
B.2.0 Medical X-ray equipment requirements
B.2.1 Regulatory requirements for medical X-ray equipment
All new, used, and refurbished medical X-ray equipment, and accessories for such equipment, which are sold, imported or distributed in Canada, must conform to the requirements of the Radiation Emitting Devices ActFootnote 24, the Food and Drugs Act and their promulgated regulations. These are the Radiation Emitting Devices RegulationsFootnote 25 and the Medical Devices Regulations. The Radiation Emitting Devices Regulations specify standards for information, labelling, construction and performance of equipment, with respect to radiation safety. Schedule II, Part XII of the Radiation Emitting Devices Regulations addresses medical X-ray equipment. The Medical Devices Regulations encompass all other safety considerations and the question of efficacy for all medical X-ray equipment sold in Canada. It is the responsibility of the manufacturer or distributor to ensure that the equipment conforms to the requirements of these regulations. In addition, X-ray equipment must meet any applicable requirements under provincial or territorial jurisdictions for such equipment. The Canadian Standards Association and provincial electrical utility should be consulted for further information.
B.2.2 Equipment purchasing
The purchase of medical imaging equipment is one of the most significant expenditures of an imaging facility. It is therefore essential to ensure that the desired design and level of performance are being obtained in a cost-effective manner. Below is an outline of the recommended process for purchasing medical imaging equipment.
B.2.2.1 Needs analysis
A needs analysis must be performed to identify the type and specifications of equipment required to meet the clinical X-ray imaging needs. When performing a needs analysis, the main points which should be considered are the types of investigations that the facility intends to perform with the equipment, and the level of performance needed from the equipment. Other points which should to be addressed are whether the staff of the facility possesses the expertise to use the equipment, whether adequate space is available for installation of the new equipment, and the date on which the equipment must be installed and operational at the facility. All staff members who will be routinely using the equipment should be consulted for input at this stage.
B.2.2.2 Equipment specifications
Equipment specifications must be prepared with full knowledge of the clinical needs and operational conditions, as well as manufacturer's specifications, and regulatory requirements. Equipment specifications supplied to the vendor should identify the type of X-ray equipment needed and the types of clinical procedures intended to be performed with the equipment. It should also identify all system components and provide a complete description of the design, construction and performance features of each component. The level of performance should be such that most manufacturers should be able to meet these performance requirements with readily available components and product lines. All relevant requirements stated in this safety code and any further requirements as specified by the agency responsible for the facility should also be addressed in the equipment specifications. Any electrical, mechanical and environmental conditions which may affect the performance of the equipment should also be included.
The equipment specifications should also include other relevant information such as the details concerning the equipment installation and calibration by the vendor and the associated deadlines, the type of warranty and service plan needed, and whether training of staff is required from the manufacturer. In general, the equipment specifications must identity all criteria which must be met for acceptance of the equipment.
Testing equipment required to perform daily to monthly quality control procedures, which are not already available, must be purchased at the same time as the X-ray unit.
B.2.2.3 Analysis of vendor quotation and the purchase contract
Vendor quotations must be thoroughly reviewed to ensure that the vendor supplied equipment specifications address the identified needs of the facility. The vendor's quotation should include the installation and calibration of the equipment, warrantees, delivery time, maintenance plans, quality control testing equipment, staff training and all other criteria included in the purchasers equipment specifications.
The purchase contract should set out all items and conditions of the purchase specified in the equipment specifications and vendor's quotation which have been agreed upon by the purchaser and vendor. All conditions for acceptance of the equipment must be clearly specified, as well as, action to be taken if conditions for acceptance are not met. A detailed and concise purchase contract will ensure the delivery of equipment in a timely and cost-effective manner.
B.2.2.4 Acceptance testing
Acceptance testing must be performed prior to any clinical use of the equipment. Acceptance testing is a process to verify compliance with the performance specifications of the X-ray equipment as written in the purchase contract. It must also verify that the equipment performance meets the manufacturer's specifications and complies with federal and provincial or territorial regulations. It is recommended that acceptance testing be performed by, or under the supervision of, a medical physicist, with in-depth knowledge of the particular type of X-ray equipment and the relevant regulations. This individual must be independent of the manufacturer.
Acceptance testing of a medical X-ray system includes several major steps. They are:
- the verification that delivered components or systems correspond to what was ordered
- the verification of the system mechanical integrity and stability, including safety mechanisms, automatic patient release, power drives, interlocks
- the verification of electrical installation, including electrical safety, power line fluctuation
- the verification of X-ray performance; and
- the verification of imaging or diagnostic performance
More detailed information on acceptance testing of radiographic, radioscopic and CT equipment is available in publications from the International Electrotechnical Commission (IEC 1999), (IEC 2004), (IEC 2006)Footnote 13 Footnote 15 Footnote 16.
X-ray performance tests performed during the acceptance testing should also reflect the requirements described in section B.2.5. The results from the acceptance testing should be used to establish baseline values and limits of acceptance on operational performance of the X-ray equipment. These baseline values and limits are essential to the quality assurance program.
B.2.3 Existing medical X-ray equipment
Whenever possible, existing medical X-ray equipment should be upgraded to incorporate as many as possible of the safety and performance features required of new medical X-ray equipment, as specified in the Radiation Emitting Devices RegulationsFootnote 25 in effect at that time. It should be noted that it is a requirement of the Radiation Emitting Devices Act that replacements for any component or subassembly of an X-ray machine, for which a construction or performance standard has been specified in the Regulations applicable to the class of X-ray equipment, must comply with the standards in effect at the time of replacement.
B.2.4 Retrofitting with computed radiography (CR) and digital radiography (DR) systems
When purchasing a CR system for a new or existing X-ray system or an after market DR detector to be installed on an existing system, both CR and DR systems must meet the requirements of the Radiation Emitting Devices Act and Regulations, as well as the Food and Drugs Act and the Medical Devices Regulations. Furthermore, the existing X-ray system, onto which the CR or DR systems is fitted, must meet the current requirements of Part XII of the Radiation Emitting Devices RegulationsFootnote 25. CR and DR image receptors must only be installed on X-ray systems which have an automatic means of controlling exposures, such as an automatic exposure control. The system must be calibrated to reflect the sensitivity of the digital receptor. For radiography, it is recommended that the detector pitch be equal or better than 200 µm, and the system radiation sensitivity should be greater than an equivalent 200 speed film screen system for equivalent diagnostic images.
B.2.5 Equipment specific requirements
Construction and performance requirements are listed below for radiographic, radioscopic and CT equipment. The Radiation Emitting Devices Regulations, Part XII (Diagnostic X-ray Equipment)Footnote 25 should be referred to for more detailed information on each requirement including, for some requirements, measurement conditions and methodologies.
B.2.5.1 General requirements
The following requirements must be met by all radiographic, radioscopic, and CT equipment. It is important to note that these requirements are reflective of the requirements of Part XII, Diagnostic X-ray Equipment, Radiation Emitting Devices RegulationsFootnote 25, effective at the time of publication of this safety code. Therefore any future amendments to the regulations may also affect the requirements of this section.
- Warning Signs—The X-ray control panel must bear a permanent, visible and legible sign warning that hazardous X-rays are emitted when the equipment is in operation and prohibit unauthorized use.
- Markings—All controls, meters, lights and other indicators relevant to the operation of the equipment must be readily discernible and clearly labelled or marked as to function.
- Mechanical Stability—The X-ray tube must be securely fixed and correctly aligned within the X-ray tube housing. In the case of CT equipment, the X-ray tube housing must be securely fixed and correctly aligned within the CT gantry. The X-ray source assembly and patient support must maintain their required positions without excessive drift or vibration during operation.
- Indicator Lights—There must be readily discernible, separate indicators on the control panel that indicate:
- when the control panel is energized and the machine is ready to produce X-rays
- when X-rays are being produced
- if an automatic exposure control is provided, when that mode of operation is selected
- if an automatic exposure control mode is not selected or does not exist, the selected loading factors to the operator before an irradiation; and
- if the equipment is battery powered, whether the battery is adequately charged for proper operation of the equipment
- Indication of Loading Factors—Medical X-ray equipment having adjustable loading factors must incorporate meters or other indicators on the control panel that enable determination of the X-ray tube voltage, X-ray tube current and time, or combinations of these. For equipment having non-adjustable loading factors, permanent marks or labels may be used to indicate these parameters. The loading factors must be displayed before, during and after the irradiation is complete.
- Irradiation Control—There must be an irradiation switch, controlling timer or other mechanism to initiate and terminate X-ray production.
- Controlling Timer—When the equipment is equipped with a controlling timer it must be constructed so that
- it can automatically terminate an irradiation on completion of a preset irradiation time, on attainment of a preset current time product value, or on completion of a preset number of X-ray pulses
- it permits the operator to terminate an irradiation at any time
- it automatically resets itself to its original setting or to zero on termination of an irradiation, and
- when it is at zero, at the off position or at an unmarked setting, an irradiation cannot occur
- X-ray Tube Shielding—The X-ray tube must be enclosed in a shielded housing. The shielding of the housing must be such that the leakage radiation from the X-ray source assembly shall not exceed an air kerma rate of 1.0 mGy/h at a distance of 1 m away from the focal spot, when operated at the nominal X-ray tube conditions of loading corresponding to the maximum specified energy input in one hour and, when the equipment is not in the loading state, 20 µGy/h at a distance of 5 cm from any accessible surface.
- X-ray Beam Filtration—There must be radiation-absorbing filters that provide a degree of attenuation such that the first Half-Value Layer (HVL) of aluminum is not less than the values shown in Table 8 for a selected X-ray tube voltage. For other X-ray tube voltages, the HVL of the radiation beam must be calculated by linear interpolation from that Table. This requirement applies only to radiographic and radioscopic equipment. For CT equipment see section B.2.5.4(5) below.
| X-ray tube voltage (kV) | Half-value layer of aluminum (mm) |
|---|---|
| 70 | 2.5 |
| 80 | 2.9 |
| 90 | 3.2 |
| 100 | 3.6 |
| 110 | 3.9 |
| 120 | 4.3 |
| 130 | 4.7 |
| 140 | 5.0 |
| 150 | 5.4 |
B.2.5.2 Radiographic equipment requirements
-
Radiation Output Reproducibility—For any combination of operating loading factors, the coefficient of variation of any ten consecutive radiation irradiation measurements, taken at the same source to detector distance within a time period of one hour, is no greater than 0.05, and each of the ten irradiation measurements is 15% of the mean value of the ten measurements.
The coefficient of variation is the ratio of the standard deviation to the mean value of a series of measurements calculated by using the following equation:

Equation B-1: Text Equivalent
The coefficient of variation is equal to the estimated standard deviation divided by the mean value of the measurements. That is, C is equal to 1 divided by X bar, all times the square root of the following: the sum of the square of the difference between each Xi and X bar, divided by n-1.
Where
- C is the coefficient of variation
- S is the estimated standard deviation
- Xi is the value of the ith measurement
- X bar is the mean value of the measurements; and
- n is the number of measurements
-
Radiation Output Linearity—For any preselected value of X-ray tube voltage, within an applicable range, the quotient of the average air kerma measurement divided by the indicated current time product obtained at two applicable settings must not differ by more than 0.10 times their sum, that is,
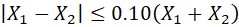
Equation B-2: Text Equivalent
To ensure radiation output linearity, the magnitude of the difference between X1 and X2 must be less than or equal to one tenth of the sum of X1 and X2.
where X1 and X2 are quotients of the average air kermas measurement divided by the current time product at two applicable settings of X-ray tube current or X-ray tube current-time product.
- Irradiation Switch—When the equipment is equipped with an irradiation switch it must require continuous pressure by the operator to emit X-rays.
- Automatic Exposure Control—For film-based systems, the automatic exposure control device shall perform in such a way that the variation of optical density in the resultant radiograms shall not exceed the value of
- 0.15 when the X-ray tube voltage is variable and the thickness of the irradiated object is constant
- 0.20 when the thickness of the irradiated object is variable and the X-ray tube voltage is constant
- 0.20 when the thickness of the irradiated object and the X-ray tube voltage are both variable, and
- 0.10 when the thickness of the irradiated object and the X-ray tube voltage are both constant
For digital systems, the performance of the automatic exposure control must be assessed according to the manufacturer's procedures and must be within the manufacturer's specifications. It is recommended that the automatic exposure control should perform in such a way that the variation in the mean linearized data on a constant region of interest does not exceed 20% for constant X-ray tube voltage and constant thickness of the irradiated object, when the X-ray system is operated in conditions representative of the typical clinical use. Compliance is checked by ensuring that the ratio of the highest and the lowest measured values is less than or equal to 1.2 or within the manufacturer's specifications.
- Current-Time Product Limit—There must be a means to ensure that where the X-ray tube voltage is 50 kV or more, the current time product does not exceed 600 mAs per irradiation.
- Accuracy of Loading Factors—The loading factors must not deviate from the selected value, for any combination of loading factors, by more than
- 10% for X-ray tube voltage
- 20% for X-ray tube current
- 10% + 1 ms for loading time, and
- 10% + 0.2 mAs for current-time product
- Minimum Irradiation Time Capability—The controlling timer or automatic exposure control device must have a minimum irradiation time capability of 1/60 s or the time required to deliver a current-time product of 5 mAs, whichever is greater.
- Beam Limiting Devices—The X-ray tube housing must be equipped with a beam limiting device that enables stepless adjustment of the size of the X-ray field. The minimum X-ray field size permitted by the beam limiting device shall not exceed 5 cm by 5 cm at a focal spot to image receptor distance of 100 cm.
- Radiation Field and Light Field Alignment—The beam limiting device must incorporate an X-ray field indicator which uses light to visually define the X-ray field so that the limits of the X-ray field are visible under the ambient lighting condition in an X-ray room. When the X-ray beam axis is perpendicular to the image receptor plane, the separation between the perimeter of the visually defined field and that of the X-ray field does not exceed 2% of the focal spot to image receptor distance.
- Focal Spot Marking—The location of the focal spot must be clearly and accurately marked on the X-ray tube housing. In the case of dual focal spot X-ray tubes, the location of the mark should be midway between the centres of the two focal spots.
B.2.5.3 Radioscopic equipment requirements
- Accuracy of Loading Factors—The loading factors must not deviate from the selected value, for any combination of loading factors, by more than
- 10% for X-ray tube voltage
- 20% for X-ray tube current
- Visual Indicators—The equipment must have visual indicators which continuously display the X-ray tube voltage and the X-ray tube current.
- Protective Shielding of Image Intensifier—Radioscopic equipment must be constructed to include an X-ray image intensifier that includes protective shielding such that for any focal spot to image receptor distance, the entire cross section of the X-ray beam is intercepted within the primary protective shielding. Also, the radioscopic X-ray tube must not be capable of emitting X-rays unless the protective shielding is in place to intercept the X-ray beam.
- Focal Spot-to-Skin Distance—The equipment must be equipped with a device that limits the focal spot to skin distance. The focal spot to skin distance must not be less than 30 cm for mobile equipment, 38 cm for stationary equipment, 20 cm, for radioscopic equipment designed for special applications that would be impossible at 30 cm or 38 cm. In the case of small-format, low-intensity radioscopic equipment, the minimum focal spot to skin distance is the distance at which the equipment is capable of delivering an air kerma rate of 50 mGy/min.
- Irradiation Switch—The radioscopic irradiation switch must require continuous pressure by the operator for the entire period of any irradiation and enable the operator to terminate the recording of serial radioscopic images at anytime.
- Chronometer—Radioscopic equipment must be equipped with a chronometer that indicates the amount of time that the equipment has been emitting X-rays and can be reset to zero or any other selected value.
- High-level Irradiation Control—High-level irradiation control must be activated by a separate means that requires continuous pressure by the operator to emit X-rays. An audible signal must be emitted when the high-level irradiation control is in use.
- Maximum Air Kerma Rates—The following maximum air kerma rates apply to radioscopic equipment except during recording of radioscopic images:
- 50 mGy/min for equipment not equipped with an automatic intensity control
- 100 mGy/min for equipment equipped with an automatic intensity control; and
- 150 mGy/min for equipment equipped with both an automatic intensity control and a high-level irradiation control and the high-level irradiation control is activated
- Transmitted/Scatter Radiation from Imaging Assembly— The radiation resulting from the transmission of the X-ray beam through, or scattered from the entrance window of the radioscopic imaging assembly must not exceed an air kerma rate of 2 mGy/h for an entrance air kerma rate of 1 Gy/min.
- Last Image Hold—Radioscopic equipment must be equipped with a last image hold system which keeps on display the last radioscopic image obtained.
B.2.5.4 Computed tomography equipment requirements
- Irradiation Control—Initiation or continuation of irradiation must be possible only from the control panel.
- Visual Indications—All CT conditions of operation such as the section thickness, pitch factor, and filtration to be used during a scan series must be indicated prior to the initiation of a scan or scan series. On equipment having all or some of these CT conditions of operation at fixed values, this requirement may be met by permanent markings. Indication of CT conditions of operation must be visible from any position from which scan initiation is possible.
- Emergency Termination of Motorized Movements and Loading—An emergency stop switch must be in place on or near the patient support and/or gantry to immediately terminate the motion of the equipment and the emission of X-rays.
- Focal Spot to Skin Distance—The minimum focal spot to skin distance must be at least 15 cm.
-
X-ray Beam Quality—Fixed added filters must be used to provide a degree of attenuation such that the first Half-Value Layer (HVL) of aluminum is not less than the values shown in Table 9 for a selected X-ray tube voltage. For intermediate X-ray tube voltages, the HVL of the radiation beam must be calculated by linear interpolation from that Table. For X-ray tube voltages which are less than 60 kV or greater than 140 kV, the HVL of the radiation beam must be calculated by linear extrapolation from that Table.
Table 9: Minimum half-value layers of aluminum for given X-ray tube voltages X-ray tube voltage (kV) Half-value layer of aluminum (mm) 60 1.9 70 2.1 80 2.4 90 2.7 100 3.0 110 3.4 120 3.8 130 4.2 140 4.6 - Preview Image—A preview image must be provided on which the operator may set up the tomographic sections to be taken. The reference lines indicating these sections must not differ from the true position by more than 2 mm with the gantry in vertical position.
- Light Field—A light field must be provided for marking the tomographic section or reference plane. The light must be visible under ambient light conditions of up to 500 lx. The width of the light field must not exceed 3 mm, measured in the centre of the gantry opening, and the coincidence of the centre of the light field and the centre of the tomographic plane must be within 2 mm. If more than one tomographic section is acquired at a time, the accompanying documentation must describe the position of the light field in reference to the tomographic section.
- Motion of Patient Support—For motions of the patient support beginning at a typical starting position, and continuing to a position which is the lesser of the maximum selectable scan increment or 30 cm, and returning to the starting position, the deviation between the actual and the indicated distances must not exceed 1 mm. This test must be performed with a load not exceeding 135 kg evenly distributed across the patient support. Measurements of actual versus indicated distances may be taken anywhere along the travel.
- Accuracy of Recorded Examination Data—In normal use the information indicating the orientation of the displayed image with respect to the patient must be displayed with each image.
B.2.5.5 Dose and image quality information for computed tomography equipment
The initial or baseline dose and image information required to assess the continuing performance of a CT X-ray system is normally obtained from the manufacturer at the time of purchase. For existing equipment, baseline values should be established by a medical physicist.
The following safety and technical information regarding the X-ray dose delivered by the radiation beam must be determined: (US CFR 1020.33), (IEC 2002)Footnote 27 Footnote 14.
- The CT conditions of operation used to obtain the dose and imaging performance information required below (sections B.2.5.5(2) and B.2.5.5(3))
- Dose information, separate for systems used to image the head and/or image the body must be provided. All dose measurements must be performed with the CT dosimetry phantom placed on the patient couch or support device without additional attenuating materials present.
Dose information must be given in terms of the Computed Tomography Dose Index (CTDI100), which is the integral of the dose profile produced in a single axial scan along a line perpendicular to the tomographic plane (from -50 mm to +50 mm) and divided by the product of the number of tomographic sections N and the nominal tomographic section thickness T, that is,

Equation B-3: Text Equivalent
The equation for Computed Tomography Dose Index, CTDI100 is equal to the integral of D(z) from z equal to -50 mm to +50 mm divided by N and T.
where
- z is the position along a line perpendicular to the tomographic plane
- D(z) is the dose at position z perpendicular to the tomographic plane, where doses are reported as absorbed dose to air
- N is the number of tomographic sections produced in a single axial scan of the X-ray source, and
- T is the nominal tomographic section thickness
This definition assumes that the dose profile is centred on z = 0.
The following data must be provided:
- The CTDI100 must be provided at the following locations in the dosimetry phantom:
- along the axis of rotation of the phantom
- along a line parallel to the axis of rotation and 1.0 cm interior to the surface of the phantom with the phantom positioned so that CTDI100 is the maximum obtainable at that depth
- along lines parallel to the axis of rotation and 1.0 cm interior to the surface of the phantom at positions 90, 180 and 270 degrees from the position in B.2.5.5(2)(a)(ii) above. The CT conditions of operation must be the typical values suggested by the manufacturer for CT of the head or body. The location of the position where the CTDI100 is maximum as specified in B.2.5.5(2)(a)(ii) must be given by the manufacturer with respect to the housing of the scanning mechanism or other readily identifiable part of the CT scanner in such a manner as to permit placement of the dosimetry phantom in this orientation
- The CTDI100 in the centre location of the dosimetry phantom for each selectable CT condition of operation that varies either the rate or duration of irradiation or the nominal tomographic section thickness. This CTDI100 must be presented as a value that is normalized to the CTDI100 in the centre location of the dosimetry phantom from section B.2.5.5(2)(a), with the CTDI100 of B.2.5.5(2)(a) having a value of 1. As a single CT condition of operation is changed all other independent CT condition of operation shall be maintained at the typical values described in B.2.5.5(2)(a). These data shall encompass the range of each CT condition of operation stated by the manufacturer as appropriate. When more than three selections of a CT condition of operation are available, the normalized CTDI100 must be provided, at least for the minimum, maximum and one mid-range value of the CT condition of operation.
- The CTDI100 at the location coincident with the maximum CTDI100 at 1.0 cm interior to the surface of the dosimetry phantom for each selectable peak X-ray tube voltage. When more than three selections of the peak X-ray tube voltage are available, the normalized CTDI100 must be provided at least for the minimum, maximum and one mid-range value that is normalized to the maximum CTDI100 located at 1.0 cm interior to the surface of the dosimetry phantom from B.2.5.5(2)(a) above, with the CTDI100 of B.2.5.5(2)(a) having a value of 1.
- The dose profile in the centre location of the dosimetry phantom for each selectable nominal tomographic section thickness. When more than three selections of nominal tomographic section thicknesses are available, the information must be provided, at least, for the minimum, maximum, and mid-range value of nominal tomographic section thickness. The dose profile must be presented on the same graph and to the same scale as the corresponding sensitivity profile required by B.2.5.5(3)(d).
- a statement of the maximum deviation from the values given in the information provided according to B.2.5.5(2)(a) to B.2.5.5(2)(d). Deviation of actual values may not exceed these limits.
- Imaging performance information, listed below, must be provided for the CT conditions of operation used to provide the information required in B.2.5.5(2)(a). All other aspects of data collection, including the X-ray attenuation properties of the material in the tomographic section, shall be similar to those used to provide the dose information required in B.2.5.5(2)(a). For any CT X-ray system designed to image both the head and body, separate imaging performance information must be provided for each application.
-
A statement of the noise. Noise is defined as the standard deviation of the fluctuation in CT number. It can be quantified in HU or expressed as a percentage of the linear attenuation coefficient for water using the following formula:
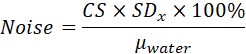
Equation B-4: Text Equivalent
Noise in a CT image is equal to the product of CS, SDx, and 100%, divided by the linear attenuation coefficient of water.
where
- CS is the contrast scale, defined below
- SDx is the measured standard deviation of the CT number of picture elements in a specified region of interest of the CT image, and
- µwater is the linear attenuation coefficient for water
The contrast scale is defined as the change in linear attenuation coefficient per CT number relative to water and the value of the contrast scale must be within preset acceptable limits. It is approximately equal to 2 x 10-4 cm-1HU-1 for beam energies of 100-140 kV. It is calculated from the following equation:

Equation B-5: Text Equivalent
The CT contrast scale is equal to the difference between the linear attenuation coefficients for the material of interest and water divided by the difference between the CT numbers for the material of interest and water.
where
- µx is the linear attenuation coefficient for the material of interest
- µwater is the linear attenuation coefficient for water
- CTx is the CT number for the material of interest, and
- CTw is the CT number for water
The computed tomography number, or CT number, represents the mean X-ray attenuation associated with discrete areas of the CT image, and is expressed in Hounsfield units, where the scale is defined so that water and air have values of 0 and -1000 respectively, and is following the relationship:
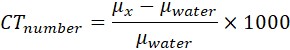
Equation B-6: Text Equivalent
The CT number is equal to the difference between the linear attenuations of a material of interest and water, divided by the linear attenuation of water and the result multiplied by 1000.
where
- µx is the linear attenuation coefficient for the material of interest, and
- µwater is the linear attenuation coefficient for water
- A graphical presentation of the modulation transfer function (MTF) for the same image processing and display mode as that used in the statement of the noise.
- A statement of the nominal tomographic section thickness at the centre of the imaged section.
- A graphical presentation of the sensitivity profile at the centre of the imaged section for each selectable nominal tomographic section thickness for which the dose profile is given according to section B.2.5.5(2)(d).
- A description of the phantom or device and test protocol or procedure including analysis of errors used to obtain the information referred to in B.2.5.5 (3)(a),(b),(c),(d).
-
-
Diagnostic reference levels are described using CTDIw which is the weighted CTDI100. CTDIw is defined as:

Equation B-7: Text Equivalent
The weighted CTDI is equal to the sum of one third of the CTDI100 in the centre of the phantom and two thirds of the average CTDI100 values measured in the periphery of the phantom.
where
- CTDI100(centre) is the value in the centre of the phantom, and
- CTDI100(peripheral) is the value measured in the periphery of the phantom
This CTDIw must be displayed on the operators console, reflecting the type of examination selected, head or body, and the CT conditions of operation.
-
The dose-length product (DLP) is also used as an indicator of overall exposure for a complete examination in order to allow comparison of performance against a reference dose value set for the purpose of promoting optimization of patient protection. The DLP is calculated as:
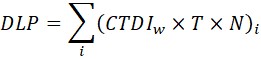
Equation B-8: Text Equivalent
The Dose-Length Product (DLP) is equal to the sum of products of the weighted CTDI, CT slice thickness, and the number of CT slices. The sum is for all CT scan sequences in an examination.
where
- i represents each scan sequence forming part of an examination
- CTDIw is the weighted CTDI
- T is the slice thickness, and
- N is the number of slices in the sequence
B.3.0 Image processing systems
Image processing includes both film and digital processing of radiological images. Film processing systems have been extensively used in the past. Recently with advances in digital technology, digital image processing systems are being used in many radiological facilities. No matter the type of system used, optimization of image quality at an acceptable dose to the patient is a priority for radiological facilities. This is achieved by ensuring image processing is an integral component of the facility's quality assurance program.
B.3.1 Film-based systems
The ability to produce a radiograph of satisfactory diagnostic quality at an acceptable dose to the patient depends on the technique used when performing the examination, the appropriate selection of loading factors, the film-screen employed, the handling and processing of the film, and on the conditions of viewing the image. Good image quality requires proper darkroom techniques, routine processor quality control monitoring, and careful adherence to film and processor manufacturers' instructions.
B.3.1.1 X-ray film
X-ray films are sensitive to light, heat, humidity, chemical contamination, mechanical stress and X-radiation. Unexposed film must be stored in such manners that it is protected from stray radiation, chemical fumes and light. The level of optical density from the base material and film fog from all causes must not be greater than 0.30 O.D.
Generally, X-ray films should be stored on edge, in an area away from chemical fumes, at temperatures in the range of 10°C to 21°C and humidity between 30% and 60%. The film manufacturers' instructions must be followed. Sealed film packages must be allowed to reach room temperature before opening to prevent condensation on the films.
Loaded cassettes must be stored in an area shielded from exposure to radiation. Radiation exposures to stored film must be limited to 0.1 mGy and, for loaded cassettes, to 0.5 µGy.
This area is usually in or near the X-ray room. The location of loaded and unexposed cassettes must be clearly marked. The area should be large enough to accommodate the required supply of cassettes needed during the operation of the facility.
B.3.1.2 Cassette and screen
Cassettes or screens in poor conditions will impair diagnostic quality. Problems are caused by dirty or damaged screens, warped cassettes, fatigue of foam compression material or closure mechanism, light leaks, and poor film-screen contact. Cassettes should be checked regularly for wear and cleanliness and any damaged cassettes should be replaced.
Manufacturers' recommended screen cleaner should be used. To avoid artifacts caused by dirt and dust, the intensifying screens and cassettes should be cleaned at least monthly. The intensifying screens should be inspected with an ultraviolet light to find dust particles. Cleaning tools include a screen cleaner with antistatic solution, lint-free cloths, compressed air, and a camel hair brush. Cassettes and screens should be numbered for identification and matching, both inside the cassette and on the outside of the cassette.
B.3.1.3 Darkroom
With the exception of daylight automatic image processors not requiring darkrooms, automatic film processors require properly designed darkrooms. While specific details may vary from installation to installation, all darkrooms must include certain basic features:
- The room must be light-tight. Particular attention must be paid to the door seal and the mounting of the film processor if the film insertion to the processor is done through a wall. The darkroom should incorporate a lockable door or double doors to ensure light-tightness when undeveloped films are being handled. A film strip exposed to an optical density of 1.2 units must not show an increase in optical density greater than 0.05 units in two minutes exposure to the darkroom light environment.
- If the darkroom is adjacent to a radiographic room, the film storage container must be adequately shielded to ensure that excessive exposure of film by X-rays does not occur. Sufficient film shielding must be in place to reduce the radiation level to the film to 0.1 mGy and to the loaded cassettes to 0.5 µGy.
- A warning light should be located outside the darkroom, at the entrance, to indicate when the room is in use. The warning light is not required if the door is locked when it is closed.
- Safelights, fitted with bulbs of intensity not greater than 15 watts, must be provided above the work areas inside the darkroom. The safelight must have filters appropriate to the specifications of the film used and must be positioned at distances greater than 1 metre from work areas to minimize film fogging.
- The darkroom should be under positive pressure so that chemical fumes and dust are not sucked into the room when the door is opened. The processor should be vented to the outside. The number of air changes must be high enough for the processor to operate properly and not create a hazardous situation for personnel.
Cleanliness in the darkroom and of the screens and cassettes is essential. It is important to maintain the cleanest environment possible in order to minimize any artifacts caused by dirt, dust, or improper handling of film. An ultraviolet light should be used to find dust areas around the darkroom. No one should eat or drink in the darkroom area. All working surfaces, tops of counters and the floor should be cleaned regularly, at least once a day. Tops of cabinets, vents, light fixtures and any other areas which can collect dust should be cleaned on a regular basis. The ventilation system should be checked to make sure that no dust is carried from it to the inside the darkroom; any filter should be changed on a regular basis. Chemicals should not be mixed inside the darkroom since this operation can result in chemical splashes onto the equipment or working surfaces. Personnel should wear personal protection devices (gloves, masks, etc.) when handling chemicals.
To avoid putting fingerprints on the film and to avoid dirtying the screens, it is important to wash hands frequently with soap that does not leave any residue. Clutter which may collect dust should be eliminated. Corrugated cardboard boxes containing film boxes, chemicals, and other supplies should not be stored or opened inside the darkroom as they will create a lot of dust. The boxes should be opened outside the darkroom, and films and supplies carried inside. Any articles of clothing made of loose fibres or which are static generating, such as wool, silk, some cottons or cotton blend fabrics, should not be worn in the darkroom or should be covered with a laboratory coat.
B.3.1.4 Film processing
Improper or careless processing of exposed radiographic films can result in films of poor diagnostic image quality and consequently increase the possibility of wrong diagnosis or requests for repeat X-ray examinations. To achieve full development, the film must be processed in chemically fresh developer, at the correct temperature and for sufficient time to ensure that the silver in exposed silver halide crystals in the film emulsion is completely reduced. If this is not done, the blackening of the film will not be optimum and the tendency will be to increase radiation exposure to achieve proper image density.
Other factors can also affect the quality of the processed film. These include cleanliness of the processing system, film immersion time, and the efficiency of the rinsing. To ensure proper processing of films certain basic procedures must be followed:
- The only acceptable method to monitor the operation of an automated image processor is with the use of a sensitometer to produce repeatable light exposure of the film and with the use of a densitometer to monitor the processed sensitometric film. Processor monitoring must be done each operational day when the processor is started and has stabilized, and at additional times after the processor has been cleaned, or after fresh chemicals have been added. The processor must be given sufficient time to stabilize, before processing patient radiographs.
- Manufacturers' instructions with respect to strength of solution, temperature and time must be followed to ensure optimum development.
- Developing solutions must be replenished as necessary and must be changed or recycled regularly, as required. This should be done often enough to avoid oxidation of the developing solutions. Even unused developer deteriorates with time. Processing chemicals must be protected from freezing. Manufacturers' instructions must be followed in storing chemicals to avoid oxidation. Any chemicals showing signs of oxidation or sedimentation must not be used.
- Fixer must be adequately removed from the processed films. Manufacturers' instructions for film wash must be followed. Fixer retention tests must be done on a regular basis. The fixer is responsible for stopping the development process by removing silver halide crystals remaining on the film. Insufficient washing of films for the removal of fixer will result in staining of films and compromise film storage time.
- Cleanliness is extremely important for reducing film artifacts. The film transport mechanisms of film processors must be cleaned frequently. Abrasive cloths or cleaners should never be used on processors.
- Film processors must be maintained regularly, according to manufacturers' instructions. The accuracy of the processor thermometer should be checked regularly against a nonmercury thermometer. The digital processor thermometer should be accurate to within 0.5°
- When film processing volume is less than 50 films per day, it may not be possible to adequately control chemical concentrations and activity. In this situation, flood replenishment should be used to better control chemical concentrations.
- When film processing volume is at least 50 films per day, a volume replenishment system is generally used which replenishes processing solutions each time a film is fed into the processor. Manufacturers' specifications for replenishment of processor solutions should be followed.
X-ray film processing generates silver containing wastes. Silver containing chemicals must not be disposed of directly into the sewer system. These chemicals must be collected and released to the appropriate waste management agency for disposal and/or recycling. The management of silver containing waste must be carried out in accordance to provincial and municipal requirements.
B.3.1.5 Viewbox
The conditions of viewboxes must be checked regularly along with the conditions under which radiologists and other health care professionals examine radiograms since this may influence diagnostic accuracy. Problems with improper illumination due to the non-uniformity of fluorescent tubes or degradation and discolouration of the viewing surface must be corrected.
B.3.2 Digital imaging systems
As an increasing number of imaging modalities are being introduced based on digital technology, imaging facilities are migrating from film-based to filmless digital imaging systems. Digital images can be acquired using either computed radiography or digital radiography systems. Computed radiography systems, or CR systems, consist of a cassette, an imaging plate and imaging plate reader. The CR cassette, loaded with an imaging plate, is positioned in the X-ray system, as it is done with film cassettes. Upon X-ray exposure, the imaging plate, which contains a photostimulable storage phosphor, stores the latent image. The imaging plate is then read and a digital image is produced. For digital radiography systems, or DR systems, the image receptor is a flat panel detector which converts the X-ray signal into an electronic signal carrying the image information. The electronic signal is sent to a digital image processor and the image is displayed almost instantaneously. Digital imaging systems together with systems for storage and communication of digital images have the potential to significantly improve patient care by increasing the efficiency of patient examinations, facilitating rapid electronic communication between health care providers, both within and outside a facility, and ultimately increasing patient throughput.
Quality control testing of digital image systems is essential. Verification of the proper functioning of the X-ray imaging equipment along with appropriate selection of technique and loading factors remains essential for obtaining a satisfactory image at a minimal dose to the patient. For digital systems, specific quality control testing must also be performed on the image acquisition, storage, communication and display systems. In section C of this safety code, some general quality control tests have been included for digital imaging systems. In addition to these test, all equipment- specific, manufacturer specified tests must also be performed.
B.3.2.1 Computed radiography imaging plates
Computed radiography (CR) imaging plates are reusable and can be exposed, read and erased repeatedly. For this reason, it is necessary to evaluate the conditions of imaging plates on a regular basis. With normal use, the accumulation of dust, dirt, scratches and cracks may reduce image quality. Exposure to chemical agents, such as non-approved imaging plate cleaners, handling with dirty or wet hands or contact with hand lotions are all possible causes of imaging plate damage. It is recommended that a log book be maintained to track the physical conditions of all imaging plates and cassette assemblies. The cleaning frequency depends on patient volume, plate handling, and the frequency at which artifacts are perceived. In general, a weekly visual inspection for dust and dirt is recommended. The imaging plates must be cleaned monthly following manufacturer recommended procedures and using manufacturer recommended cleaners. Cleaner must not be poured directly onto the plates as this may cause staining.
B.3.2.2 CR cassette
Under normal conditions of use, dust and dirt can accumulate on cassettes. It is recommended that a log book be maintained to track the physical conditions of all cassettes. In general, a weekly visual inspection for dust and dirt is recommended and monthly cleaning of CR cassettes following manufacturer recommended procedures and using manufacturer recommended cleaners. The outside of the cassette can easily be cleaned with water and soap or a non-aggressive cleaner. The inside must not be cleaned with soap and water, since soap residue may be left on the protective coating after cleaning.
B.3.2.3 Electronic display devices
The performance of medical electronic display devices must be checked routinely. The cleanliness of the display surface must be maintained. Manufacturer recommended cleaners and cleaning procedures must be followed. The performance of the display must be verified using test patterns designed for evaluating various characteristics of display performance (AAPM, 2005)Footnote 2. An overall assessment should be made daily prior to clinical use. It is recommended that geometric distortion, luminance and resolution be evaluated monthly and a detailed evaluation be performed annually by a medical physicist.
B.3.2.4 Picture archiving and communications system
In digital imaging, a system must be in place to manage patient images so that secure storage and timely retrieval of images is possible. Picture Archiving and Communications System (PACS) is one such system which is widely used in radiology. A PACS in an imaging facility connects digital image acquisition devices with a systems which can store, retrieve and display digital images within and outside the facility. The transition to PACS requires a significant amount of planning, time and resources. However, once established, a PACS offers a number of advantages such as improved productivity, widespread, simultaneous access to images and image manipulation. Radiologists are able to interpret more cases in shorter periods of time, resulting in shorter waiting times for patients and quicker access to results by the referring physicians. However, attention must be given to ensure that the quality of patient images is maintained and that patient information is not lost or unintentionally altered. Such situations can lead to repeat radiological examinations and misdiagnoses of patients.
B.3.2.5 PACS implementation
When deciding whether to implement a PACS, a number of key issues should be addressed. A PACS is a very high capital investment. It requires resources for hardware, software and additional staff such as a PACS administrator and any consultants which may be necessary. Early in the planning stages of a PACS, parties should be consulted from all areas which will be affected by the changes. This should include departmental administrators, PACS specialists, medical physicists, radiologists, technologists, referring physicians and any existing information technology (IT) staff. The information obtained during the consultation should be used to perform an intensive cost/benefit analysis prior to making a decision. Early consulting with all involved parties will facilitate the clinical acceptance of the system.
When deciding upon the specifications of a PACS system the following key components should be considered.
- Insist on Digital Imaging and Communications in Medicine (DICOM) compliance. The DICOM standard facilitates interoperability of medical imaging equipment.
- Ensure that all systems can be integrated. This includes systems such as the Hospital Information System (HIS), the Radiology Information System (RIS), the PACS, image acquisition equipment, printers, and any reporting systems. To ensure ease of integration between systems, equipment should support the "Integrating the Healthcare Enterprise" (IHE) Technical Framework. The IHE is an initiative to promote and support the integration of information systems in the healthcare enterprise to improve the workflow by facilitating communication between systems from different vendors. Information being transferred from one system to another will remove the need to re-enter information independently into each system and thus avoid inconsistencies, redundancies and unavailability of the data.
- Security of patient information must be a priority. Only authorized individuals must be able to access patient data and images. Security measures must be established to control access to patient information as well as to track all activities which are performed on the data. This includes monitoring who accesses information, when the information is accessed, and what changes are made to the information. Authorized system users must understand the importance of keeping system passwords confidential.
- Automated features should be included in the design of the system to facilitate more rapid workflow. For example, a feature should be available which pre-fetches prior studies of the individual to allow for comparison with the current study being interpreted.
- The system should adapt to the user. For example, the graphical interface on the display should adapt to the preferences of the individual signing into the system.
- A system must be in place for quick and efficient error correction. Files containing incorrect information may quickly become lost and unretrievable. On a regular basis, the systems should ensure agreement between the list of studies planned for a work period, the studies performed at the modalities, and the studies interpreted by the radiologists. This will minimize lost cases and ensure incorrectly filed data is quickly identifiable.
- Fault Tolerance. When working with a digital imaging and reporting system, attention must be given to ensure system availability. Critical patient data must be available whenever needed. This is especially important in operating rooms and emergency departments. When purchasing equipment for imaging or information systems, the vendor must guarantee the level of availability of their system. System down times, for upgrades and maintenance must be well planned so as not to interfere with the workflow of the facility. Depending on the type of facility and the workload, purchasers may require the vendor to guarantee as much as 99.999% availability. It must be determined if it is acceptable for the whole system or parts of the system to be down at any time and the duration of the time. Penalties and conditions for not meeting the uptime and downtime guarantees must be clearly stated and agreed upon with the vendor.
- Disaster Recovery. The facility should establish a disaster recovery plan in case of component failure or catastrophic events. The disaster recovery plan should consist of documented policies and procedures identifying primary and backup people and their responsibilities and a description of the actions necessary to restore operations. A critical component of disaster recovery is the continuous backing up and maintenance of data at an off-site location.
- In order for a PACS system to work, it should be based upon, and designed to reflect, a proven, effective workflow. Purchasers must ensure the vendor understands the facility workflow and provides a system which does not disrupt the workflow. PACS systems based upon flawed work flows will carry over all of the existing problems.
- When deciding upon the network and storage requirements of an imaging or information system it is important not to limit the systems to only the current needs of the facility. The system should be scalable to allow for future growth of the system. The system capacity should be based upon the following points:
- the current modalities from which studies are acquired
- the average number of images per study by modality
- the number of pixels and bit depth of the image; iv) number of studies performed each year; v) projected procedure growth volume; vi) modalities to be added in the future; and vii) other sites/facilities to be added to the system in the future
B.3.2.6 Teleradiology
Teleradiology is the electronic transmission of radiological images from one location to another for the purposes of interpretation and/or consultation. Through teleradiology, digital images and patient information can be accessed electronically from multiple sites simultaneously. The benefits of teleradiology include more efficient delivery of patient care and the ability to provide radiological services to facilities in remote areas which do not have radiologists available on-site.
Since teleradiology involves the acquisition and interpretation of patient images at different sites, it is important that policies and procedures be in place at all locations to ensure image quality is optimized and comparable among all facilities accessing patient images. This is especially important when official authenticated written interpretations are made through teleradiology.
-
Teleradiology Quality Assurance—The Canadian Association of Radiologists has produced guidelines for facilities performing teleradiology. Some of the main points of that document relevant to this safety code are listed below (CAR, 1999)Footnote 6.
When used for rendering the official authenticated interpretation of images, the receiving location must conform to the following requirements:
- Images acquired digitally by an imaging device must be displayed in their full native matrix size and bit depth. If this is not possible, display software must be used that allows the user to "pan" over the entire image when displayed in its full matrix size.
- Images obtained through post processing of the original image must not be used to the exclusion of the original images themselves. They must only be used to support the interpretation process.
- Digital images may be "captured" using a frame grabber interfaced to a secondary (analog) device, such as a display monitor on a console being used to display the original images acquired digitally. Such images captured from displayed versions of the original images must only be permitted to be used when there is no other means of displaying the original images themselves. When this is the case, the matrix size of the captured images must not be less than the matrix size of the original images, and the bit depth must be 8 bits or equal to that of the original images.
- Images captured from a film scanning device must have:
- an acquisition or digitization system which enables spatial resolution of a minimum of 2.5 lp/mm and acquisition of 10 bit grey scale
- a display system which enables spatial resolution of a minimum of 2.5 lp/mm and display of 8 bit grey scale
- Image Management (for static images only)—Teleradiology systems are imaging systems that require the use of image management for optimal performance. All systems must include the following:
- An integrity-checking mechanism, either in software or using a manual process, to ensure that all transmitted information from the site of origin is received intact by the receiving site.
- Capability for the selection of the image sequence for transmission and display at all receiving sites.
- Annotation capabilities for use at the transmitting station that must identify the patient accurately and unambiguously. This may include patient name, identification number, date and time of examination, film markers, institution of origin, type of examination, degree of compression (if used) and a brief patient history. This information should be bundled with the image file but may also be transmitted by other secure means.
- The transmitting site should have provision for interactive window and level and/or brightness and contrast.
- Provision for the selection of appropriate compression for improved transmission rates and reduced archiving/storage requirements.
- Image storage at either the transmitting or receiving site as well as transmission must be arranged such that patient confidentiality is maintained and that the system is secure.
- The provider must ensure that the image quality is the same at the transmitting site and receiving site(s).
- Transmission of Images and Patient Data—Communications protocols, file formats and compression must conform to the current DICOM 3.0 network standards.
- Display Capabilities—Display workstations employed for teleradiology systems must provide the following characteristics:
- Luminance of the grey scale monitors must be at least comparable to the workstations used for acquisition.
- Display stations for digitized radiographic films, and digital radiography must include:
- brightness and contrast and/or interactive window and level function
- a magnification function
- the capability of rotating and flipping the displayed images
- the capability of accurate linear measurements; and
- the capability of inverting the grey scale values of the displayed image
- Display stations for CT must accurately reproduce the original study and be equipped with similar functional capabilities as the workstation used for acquisition.
- Patient Database—For radiological images transmitted by teleradiology, a database must be available, at both the transmitting and receiving site to serve as a basis for future integrity checking and audits. The data base must include:
- patient name, identification number and date
- type of examination
- types of images
- number of images
- image acquisition and sending sites (if different); and
- date and time of transmission
- Security—Teleradiology systems must provide network and/or software protocols to protect the confidentiality of the patient's record(s), image(s), interpretation(s) and other data and insure that the system is secure and used only on an as needed basis by those authorized by the patient according to provincial or territorial privacy of information legislation and Canadian Medical Association guidelines.
- Storage of Records—The legal requirements for the storage and retention of images and reports will vary from province to province and the providers of the teleradiology service are responsible for adhering to these requirements. Images stored at either site must meet the jurisdictional requirements of the transmitting site. Images interpreted off-site need not be stored at the receiving facility provided that they are stored at the transmitting site. However, if images are retained at the receiving site, the retention period of that jurisdiction must also be met. The policy on record retention must be in writing.
- Documentation—Communication is a critical component of teleradiology. Physicians interpreting teleradiology examinations must render reports in accordance with the CAR Standards of Communication.
-
Quality Control for Teleradiology—It must be stressed that the images at the receiving site can only be as good as the images captured at the transmission end. It is imperative that an imaging physician must be at the transmitting site on a regular basis to ensure that the equipment is functioning properly and that the technologists are adequately supervised and trained. Both the transmitting and receiving sites must have documented policies and procedures for monitoring and evaluating the effective management, safety, proper performance of imaging, transmitting, receiving and display equipment.
A test image, such as the SMPTE, or its equivalent, must be captured and transmitted at least weekly to test the overall operation of the system. As a dynamic range test, both the 0/5% and the 95/100% areas must be seen as distinct from the respective adjacent 0% and 100% areas.
-
Quality Improvement—The use of teleradiology does not reduce the responsibilities for the management and supervision of radiological medicine. Procedures must be systematically monitored and evaluated as part of the overall quality improvement program of the facility. Monitoring must include the evaluation of the accuracy of the interpretations as well as the appropriateness of the examination. Incidences of complications and adverse events must be reviewed to identify opportunities to improve patient care.
The use of teleradiology must be documented. Periodic reviews must be made for the appropriateness, problems and quality of the transmitted data. The data must be collected in a manner which complies with the statutory and regulatory peer-review procedures to protect the confidentiality of the peer-review/patient data.
B.4.0 Other equipment
Consideration must be given to other equipment, such as those used for personnel protection and equipment testing, which are necessary for ensuring the radiation safety of a radiological facility. Personnel protective clothing must provide adequate protection without being unduly restrictive and heavy. All test equipment must be properly maintained and carefully stored.
B.4.1 Protective equipment
- Protective lead aprons for patients and operators must provide attenuation equivalent to at least
- 0.25 mm of lead, for examinations where the peak X-ray tube voltage is 100 kV or less
- 0.35 mm of lead, for examinations where the peak X-ray tube voltage is greater than 100 kV and less than 150 kV, and
- 0.5 mm of lead, for examinations where the peak X-ray tube voltages is 150 kV or greater
- For interventional procedures, where no other protective devices are used, full wrap around type protective gowns of 0.50 mm Pb in the front panels and 0.25 mm Pb in the back panels are recommended.
- For interventional procedures, protective thyroid shields with an equivalent of 0.50 mm Pb are recommended.
- For interventional procedures, close-fitting protective glasses for the eyes with an equivalent of 0.75 mm Pb are recommended.
- Protective gloves or gauntlets must possess at least a 0.25 mm Pb equivalency. These protections must be provided throughout the glove, including fingers and wrist.
- The lead equivalent thickness of the protective material used must be permanently and clearly marked on all protective equipment and apparel.
- Ceiling-mounted lead acrylic screens and moveable shields should provide protection equivalent to at least 0.50 mm Pb. The attenuation value must be marked on all protective screens and shields.
- All protective equipment must be tested on a yearly basis for integrity and results must be included in the quality control test records.
- Defective equipment must be removed from clinical use.
- Protective equipment must be stored and maintained according to manufacturers' instructions.
B.4.2 Test equipment
- All equipment used for acceptance and quality control testing must be evaluated for their functioning and performance on a regular basis.
- All sensitometric and densitometric equipment, dose meters, tube voltage meters should be calibrated on a regular basis according to manufacturers' recommendations.
- All phantoms and other equipment used for the assessment of image quality, dose and system performance should be checked for damage or any condition which may affect their use.
- Test equipment should be stored away from heat, direct sunlight, and high humidity. They must be operated following manufacturers' recommendations.
B.5.0 Radiation protection surveys
A radiation protection survey is an evaluation, conducted by an expert, of the radiation safety of a radiological facility. The survey is intended to demonstrate that the X-ray and auxiliary equipment function properly and according to applicable standards, and that the equipment is installed and used in a way which provides maximum radiation safety for operators, patients and others. Safety measures such as protective equipment and shielding are also examined to ensure that they are present and provide the required protection. It is important, therefore, that X-ray facilities are inspected at regular intervals.
B.5.1 General procedures
Routine operation of any new installation or an installation which has undergone modifications should be deferred until a complete survey has been made by an expert. The expert is an individual who is qualified by education and experience to perform advanced or complex procedures in radiation protection that generally are beyond the capabilities of most personnel within the facility. These procedures include evaluation of the facility design to ensure adequate shielding is in place, inspection and evaluation of the performance of X-ray equipment and accessories, and evaluation and recommendation of radiation protection programs. The owner of the facility (or another delegated staff member such as the Radiation Protection/Safety Officer) must contact the appropriate regulatory agency to ascertain inspection and acceptance testing procedures in that jurisdiction. Some jurisdictions may require that the facility be declared in compliance with applicable governmental regulations prior to operations.
For a new facility, it is particularly advantageous to make visual inspections during construction, to ensure compliance with specifications and to identify faulty material or workmanship, since deficiencies can be remedied more economically at this stage than later. Such inspections should include determination of thickness of lead and/or concrete thickness and density, degree of overlap between lead sheets or between lead and other barriers, as well as thickness and density of leaded glass used in viewing windows.
For existing installations, a survey must be carried out after any changes are made, which might produce a radiation hazard. This includes alteration of protective barriers, equipment modification and replacement, changes in operating procedures, or increased workloads.
Finally, radiation protection surveys must be carried out at regularly scheduled intervals during routine operations to detect problems due to equipment failure or any long-term trends toward a decrease in the level of radiation safety. The frequency at which radiation protection surveys are to be conducted is dependant on the type of facility, the type of equipment used and the type of examinations performed. Facilities should contact the applicable regulatory authority to establish the survey schedule.
The results of such surveys, including conclusions drawn by the expert, must be submitted to the owner or responsible user in a written report. All such reports must be retained by the owner or responsible user. For federal facilities, radiation survey reports should be maintained for 5 years and personnel dosimetry records for the lifetime of the facility.
B.5.2 Survey report
The survey report must present, in a clear systematic way, details and results of the measurements carried out, as well as the conclusions drawn and recommendations made by the surveyor. Any unusual findings about the equipment itself, the facility or operating procedures, which could affect the safety of operators or other persons in the vicinity of the X-ray facility must be clearly identified.
The survey report must include the following:
- a sketch of the facility, showing the location of the X-ray equipment and control booth within the facility as well as the nature and occupancy of the areas adjoining the facility
- identification of the X-ray equipment (i.e., the name of the manufacturer, model designation and serial number of the generator, control, X-ray tube assembly, X-ray table, etc. as applicable) and the date, or at least approximate date manufactured
- the method of support of the X-ray tube assembly (i.e., floor-to-ceiling tube stand, ceiling suspended over-table tube, etc.)
- observations of the operational conditions (both electrical and mechanical) of the X-ray equipment at the time of the survey
- the actual or estimated total workload of the facility, as well as the workload apportioned into various X-ray beam directions and procedures used, etc.
- results of radiation measurements carried out both inside and outside the controlled area under "typical" operating conditions. The locations at which the measurements are made
- an assessment of the condition of patient restraints, protective aprons, gloves, mobile protective barriers and other protective devices
- an estimate of potential exposures to personnel and general public in or around the facility
- an evaluation of the X-ray performance and the imaging or diagnostic performance (this may include performing applicable quality control tests from sections C.3.1 to C.3.6
- a summary of typical loading factors used and a measurement of the total filtration in the X-ray beam
- an assessment of radiological techniques from the point of view of radiation safety and an assessment of the Diagnostic Reference Levels for the facility. Attention must be drawn to any practices which are or could be detrimental to the patient or to personnel working in the facility. Recommendations of improved or safer techniques should be made in such cases
- results of investigations of any unusually high exposures from previous personnel dosimetry reports and recommendations on whether other persons should be included in the personnel dosimetry service
- a review of the facilities quality assurance program to ensure it exists and is maintained, including quality control testing records; and
- recommendations regarding the need for a follow-up survey
B.6.0 Disposal of X-ray equipment
When X-ray equipment is considered for disposal, an assessment should be made as to whether the equipment can be refurbished and/or recycled. Communication with the manufacturer or supplier of the equipment should be made as to whether the equipment or components of the equipment can be recycled or returned. Once the decision has been made to dispose of X-ray equipment, an assessment must be made to determine if any equipment components contain hazardous materials. For example the X-ray tube may contain polychlorinated biphenyls (PCBs) and lead may be present in the X-ray tube housing. To ensure equipment is not unsafely operated after disposal, it should be made inoperable before disposing. The cables that power the equipment and other electrical connections should be disconnected and removed. It is recommended that radiological facilities, under provincial or territorial jurisdiction contact the responsible agency in their respective province or territory for further information. A listing of these responsible agencies is provided in Appendix V.
Section C: Quality assurance program
C.1.0 Introduction
All radiological facilities must develop and maintain an effective quality assurance program. Quality assurance in radiology is defined as the planned and organized actions necessary to provide adequate confidence that the X-ray equipment and its related components reliably produce diagnostic information of satisfactory quality with minimum doses to the patients and staff. A quality assurance program includes quality control procedures for the monitoring and testing of X-ray equipment and related components, and administrative methodologies to ensure that monitoring, evaluation and corrective actions are properly performed. The owner of an X-ray facility has the responsibility of establishing a quality assurance program which examines all practices of the facility which effect:
- Information Quality—to ensure all diagnostic information produced provide for accurate clinical assessment
- Clinical Efficiency—to ensure all steps leading to accurate diagnosis and intervention are taken and the information is made available in a timely fashion to the patient's physicians or primary medical professionals; and
- Patient Dose—to ensure that the X-ray examination is performed with the lowest possible radiation dose to the patient consistent with clinical imaging requirements
C.1.1 Goals of the quality assurance program
The ultimate goal of a quality assurance program is to ensure accurate and timely diagnosis and treatment at the minimum dose to the patient and staff. In order to have a successful quality assurance program it is essential that equipment is in proper working condition and all staff members understand the goals of the program and are committed to the implementation of the program through full participation.
Information obtained from X-ray equipment must be of utmost quality to ensure accurate diagnosis and treatment. If critical elements are missing or artifacts are added to images, the image is considered to be of poor quality. The consequence of poor quality diagnostic information may be incorrect diagnosis resulting in repeat radiographic procedures, unnecessary radiation doses to the patient, delayed or improper patient treatment and increased cost.
C.1.2 Costs-benefits of the quality assurance program
The initial implementation and the general operation of a quality assurance program will involve cost in both money and time from staff. However, savings from the operation of the program will offset some of these costs. For some facilities, there may be a reduction in the overall operating costs.
C.1.2.1 Costs of quality assurance program
Some of the costs associated to the quality assurance program are as follow:
- Personnel—The staff will be required to perform new duties, which include generating test images for the X-ray equipment and record keeping.
- Test Equipment—Test equipment to perform quality control tests, such as phantoms, will be required. However, the cost of such equipment is small compared to the cost of the X-ray imaging unit and it may be used for several X-ray systems. It would not be necessary to purchase some of the test equipment if the facility decides to have some of the quality control tests performed by an external organization or individual, who would then be responsible for providing their own test equipment.
- Test Images—For film-based systems, and CR and DR systems using laser printers, 2 to 5% of films used by a facility may be required for the performance of sensitometry, phantom imaging, equipment and test imaging.
- External Organizations—If the facility does not have the capacity to perform internally all quality control tests, it may choose to contract an external organization or individual to perform some of these tests and equipment assessments. In addition, the facility may retain the service of a medical physicist as an advisor during implementation and for consultation during operation of the facility.
C.1.2.2 Benefits of quality assurance program
In addition to improved diagnostic quality some of the savings associated with the quality assurance program are as follow:
- Film and Processing Chemicals—For film-based systems, and CR and DR systems using laser printers, a decrease in the number of retakes may result in the reduction in the number of films and processing chemicals used.
- Equipment—The reduction in the number of retakes will lead to a reduction in workloads which in turn will put less stress on X-ray equipment and image processors. Problems with equipment may be diagnosed earlier before more serious and costly problems occur thus reducing down time and equipment service costs.
- Patient Flow—The reduction in the number of repeats, and better image quality will allow efficient use of time for both responsible users and the X-ray equipment operators. This will result in better predictability of scheduling and possibly greater patient throughput.
C.1.3 Implementation of quality assurance program
The implementation of a quality assurance program need not be complicated. It consists in establishing quality control procedures for the equipment along with an administrative methodology to ensure that monitoring, evaluation and corrective actions are properly performed.
C.1.3.1 Policies and guidelines development
One useful step is to develop a series of policies and guidelines where various issues are addressed. The following list presents some of these policies and guidelines. Each facility may require different sets of policies and guidelines depending on the type of work being performed and the organizational structure of the facility. These policies should be established by management with participation from staff. It is recommended that all safety policies, procedures and processes be reviewed by a Joint Health and Safety Committee. The policies should be present in the Quality Assurance (QA) manual. The following information should be readily available to radiology staff:
- Radiology Personnel
- A list of staff and an outline of their duties, authority and responsibilities
- Policies for Minimizing Radiation Exposure to X-ray Operators and Staff
- Policy for minimizing exposure to pregnant workers
- Policy for holding patients
- Policy for the presence of individuals in the X-ray room during procedures
- Policy for training/orientation program for X-ray equipment operators
- Policy for the proper use and maintenance of X-ray equipment
- Policy for personnel radiation dosimetry monitoring
- Policy for the use of protective devices and radiation protection equipment
- Policy for the maintenance and testing of radiation protection devices and equipment
- Policies for Minimizing Radiation Exposure to Patients Policy for carrying out X-ray examinations.
- Policy for the radiological examination of pregnant patients
- Policy for the use of protective devices and radiation protection equipment
- Policy for patient positioning (positioning manual)
- Policy for exposure loading factors (technique charts)
- Policy for the quality acceptance of diagnostic radiograms
- Policy for a reject analysis of radiographic images
- Guidelines for Equipment Quality Control (QC) Testing
- Guidelines listing all X-ray equipment and system components to be tested
- Guidelines for all equipment parameters to be measured and the frequency of monitoring (schedule) for each X-ray system and system component
- Guidelines for the performance standards for each equipment tested and the specific performance tolerance limits expected for each QC test
- Guidelines for the measurement of each parameter and recording of the data
- Guidelines to evaluate the test data and to take the corrective action necessary to maintain equipment optimum performance
- Guidelines for patient exposure measurements (ESEs, DRLs)
- Guidelines for the calibration and maintenance of radiation measuring equipment and other test equipment
- Policies for the Acquisition of New X-ray Imaging Equipment
- Policy for a needs analysis
- Policy for equipment specification writing
- Policy for equipment acceptance testing
- Policy for equipment appraisal and replacement
- Policy for Record Keeping
- Policy for the review of the QA Program
- Policy for the review of the QC Procedures
- Policy for the retention of records (patient information, QC test results, survey reports, personal dosimetry records)
C.1.3.2 Establishment of quality control procedures
The following four steps must be included for the establishment of quality control procedures:
- Equipment Operation—It is essential that the X-ray equipment and image processing equipment function properly before a quality assurance program is implemented. Manufacturers and vendors should provide proper operating characteristics for their equipment. For film-based systems, films and processing must meet manufacturers' speed and contrast values. For CR and DR systems, the imaging system must be properly calibrated with the X-ray systems. This may involve replacement, repair, upgrading or calibration of the equipment.
- Baseline Performance—Baseline performance values of X-ray equipment and image processing system must be established after verifying that the equipment functions properly. This baseline performance will be used to diagnose any changes in equipment performance. It is important to keep records of equipment operation data and baseline performance measurements. These records will be needed to diagnose any changes in image quality. Baselines values must be determined when new equipment is introduced into the facility, when there are changes in components which effect image quality and patient dose and also when testing equipment is changed.
- Reference Test Image—To evaluate image quality a reference test image is needed. This reference test image is made by using the X-ray equipment, image processing system and a quality control phantom and will be used for comparison of quality control test images.
- Result Evaluation and Action Levels—An effective quality control monitoring program includes not only a routine quality control testing schedule, data recording and record keeping, but also test result evaluation, such as determination of acceptable or unacceptable limits of equipment operation coupled with a list of corrective actions that may be required. A set of limits should be established which indicates a level of operation outside of which the system or the function should be closely monitored but where no immediate action is required. Another set of limits should also be established where immediate remedial action must be taken.
C.1.3.3 Establishment of administrative procedures
The following administrative procedures must be included in the establishment of an effective quality assurance program.
- Responsibility—Although the owner of the facility is ultimately responsible for the implementation and operation of the quality assurance program, to obtain the optimal level of radiation safety and quality diagnostic information, it is imperative that full cooperation exists among all concerned parties. Staff members may be assigned duties with regard to equipment monitoring, record keeping and general operations of the quality assurance program. It is essential that the level of responsibilities and involvement of the owner and staff be clearly identified, communicated and understood.
- Record Keeping—It is essential that measurements and information gathered for the quality assurance program is clearly documented and readily available for evaluation. As far as practicable, recorded data should be indicated as data points on a control chart for each day the measurement is made. For example, it includes the densitometric results of the sensitometric film strips, and the charting of temperature for the film processor. In this form, trends can be more easily detected. A log book or other easily identifiable method of recording must be used.
- Evaluation of Data—Recorded data should be evaluated immediately and necessary actions taken.
- Limits of Acceptability of Data—Upper and lower limits of acceptability of recorded data must be determined and documented. When these limits are reached, corrective actions must be taken. For example, they can be the range of acceptable temperatures for the film processor. These limits should be set such that they are just within the range allowable before diagnostically significant image changes are evident. They should not be so restrictive that they exceed the capability of the equipment, or that frequent corrective actions are taken without any evidence of problems. These limits should be reviewed from time to time, especially when major components of the X-ray system are replaced or repaired.
- Testing frequency—Testing frequency must be such that a balance is reached between the cost of testing, disruption to the operation of the facility and the maintenance of quality. The frequency of testing should be increased if the equipment exhibits significant changes between scheduled quality control tests, or if the equipment is used for exceptionally high volume of procedures. Additional testing should be performed if the results of testing fall outside of limits of acceptability for the tests, or after any corrective actions are made. Equipment must be retested after service to any part which may affect the image density, image quality or radiation output from the X-ray tube. The quality control program should not be discontinued if the results indicate relatively stable equipment performance. The purpose of a quality control program is to control quality, and periodic measurement of equipment performance is essential.
- Corrective Actions—There must be established repair and calibration procedures to deal with significant problems. A decision tree system should be developed to provide guidance to deal with events such as equipment failure and to deal with circumstances when equipment performance deviates beyond the set limits. A list of individuals having the authority to stop operation of an X-ray unit should be established. The decision tree should include the following steps:
- repeat the test to confirm
- what to do if repeated test confirms performance failure
- what to do if test fails only marginally
- what to do if test shows a history of failure; and
- what to do if test fails substantially
C.2.0 Acceptance testing
Acceptance testing is a process to verify compliance with the performance specifications of the X-ray equipment as written in the purchase contract and that the equipment performance complies with federal and provincial or territorial regulations. It is recommended that acceptance testing be performed by a medical physicist, or other individuals, with knowledge of the particular type of X-ray equipment and the relevant regulations prior to any clinical use of the equipment. The owner may wish to have acceptance testing performed by an individual or organization independent of the manufacturer.
Acceptance testing of a medical X-ray system includes several major steps. They are:
- the verification that delivered components or systems correspond to what was ordered
- the verification of the system mechanical integrity and stability, including safety mechanisms, automatic patient release, power drives, interlocks
- the verification of electrical installation, including electrical safety and power line fluctuation
- the verification of X-ray performance; and
- the verification of imaging or diagnostic performance
The results from the acceptance testing should be used to set baseline values and acceptance limits on operational performance of the X-ray equipment. These baseline values and limits are essential to the quality assurance program.
C.2.1 Acceptance testing evaluation
Acceptance testing for radiographic, radioscopic and CT equipment should evaluate at least the following items below. Not all equipment will be subject to the full set of tests. The type of equipment and its configuration will dictate the sets of tests to be performed. More detailed information on acceptance testing on radiographic, radioscopic and CT equipment is available from the International Electrotechnical Commission (IEC 1999), (IEC 2004), (IEC 2006)Footnote 13 Footnote 15 Footnote 16.
| Items under evaluation for acceptance testing | Film-based system | CR system | DR system | Radioscopic system | CT system |
|---|---|---|---|---|---|
| 1.0 Identification | |||||
| 1.1 Initial Inspection and Inventory | Yes | Yes | Yes | Yes | Yes |
| 1.2 Inspection of Documentation | Yes | Yes | Yes | Yes | Yes |
| 2.0 Visual and functional texts | |||||
| 2.1 Mechanical Properties | Yes | Yes | Yes | Yes | Yes |
| 2.2 Safety Systems | Yes | Yes | Yes | Yes | Yes |
| 3.0 Performance evaluation (X-ray generator) | |||||
| 3.1 X-ray Tube Voltage | Yes | Yes | Yes | Yes | Yes |
| 3.2 Current Time Product | Yes | Yes | Yes | No | No |
| 3.3 Loading Time | Yes | Yes | Yes | No | No |
| 3.4 Radioscopic Timer and Chronometer | No | No | No | Yes | No |
| 3.5 Beam Limitation and Indication | Yes | Yes | Yes | Yes | Yes |
| 3.6 X-ray Beam Filtration | Yes | Yes | Yes | Yes | No |
| 3.7 Automatic Exposure Control | Yes | Yes | Yes | No | No |
| 3.8 Automatic Intensity Control | No | No | No | Yes | No |
| 3.9 Radiation Output | Yes | Yes | Yes | Yes | No |
| 3.10 Maximum Air Kerma Rate | No | No | No | Yes | No |
| 3.11 Phantom (Entrance) Dose (Rate) | Yes | Yes | Yes | Yes | Yes |
| 4.0 Performance evaluation (image receptor) | |||||
| 4.1 Exposure Index | No | Yes | Yes | No | No |
| 4.2 Dynamic Range | No | Yes | Yes | No | No |
| 4.3 Spatial Resolution | Yes | Yes | Yes | Yes | Yes |
| 4.4 Contrast Detectability | Yes | Yes | Yes | Yes | Yes |
| 4.5 Uniformity | No | Yes | Yes | No | Yes |
| 4.6 Artifacts | Yes | Yes | Yes | Yes | Yes |
| 4.7 Digital Detector Residual Image | No | Yes | Yes | No | No |
| 4.8 Noise | No | Yes | Yes | No | Yes |
| 4.9 Modulation Transfer Function | No | Yes | Yes | No | No |
| 4.10 Mean CT Numbers (calibration and linearity) | No | No | No | No | Yes |
| 4.11 Tomographic Section Thickness | No | No | No | No | Yes |
| 4.12 Axial Patient Positioning Accuracy | No | No | No | No | Yes |
| 4.13 Positioning of Patient Support | No | No | No | No | Yes |
C.3.0 Quality control testing
Procedures and equipment
Quality control testing must be carried out during routine operation of a radiological facility. This section sets out the required and recommended quality control tests, the associated test equipment and testing frequencies.
Quality control testing of a medical X-ray system includes several major steps. They are:
- the verification of the system mechanical integrity and stability, including safety mechanisms, automatic patient release, power drives, interlocks
- the verification of the performance of ancillary equipment such as film processors and display units
- the verification of X-ray performance; and
- the verification of imaging or diagnostic performance, including assessments of dose
Test equipment required to perform daily to monthly quality control tests, must be readily available to the individuals responsible for performing these tests. All test equipment must be calibrated and verified to be operating accurately. Individuals performing quality control tests must be trained in the proper operation of the test equipment and in performing the tests.
In the following sections, the descriptive text for each test indicates whether performance of the test is required or recommended. In addition, not all equipment will be subject to the full set of tests listed in the following sections. For example, for film-based systems, the evaluation of noise is not necessary since this item is for the evaluation of digital systems. The type of imaging system, whether film-based, CR, DR, radioscopic or CT, to which the quality control tests apply is identified. Note that both radiographic and radioscopic imaging equipment employing CR and DR digital image acquisition technologies must perform the required tests listed for these systems. Alternative tests can be performed in place of those specified if it can be shown that the test is capable of verifying the necessary parameter or performance.
C.3.1 Daily quality control testing
C.3.1.1 Quality control tests list
Daily quality control tests are listed in Table 11. The imaging systems to which the tests are applicable, and the test numbers corresponding to those in section C.3.1.2, are provided.
| Quality control procedures under evaluation | Film-based system | CR system | DR system | Radioscopic system | CT system |
|---|---|---|---|---|---|
| Daily quality control tests | |||||
| Equipment Warm-up | D1 | D1 | D1 | D1 | D1 |
| Meters Operation | D2 | D2 | D2 | D2 | D2 |
| Equipment Conditions | D3 | D3 | D3 | D3 | D3 |
| System Movements | N/A | N/A | N/A | D4 | N/A |
| Darkroom Cleanliness | D5 | N/A | N/A | D5 | N/A |
| Film Processor Function | D6 | N/A | N/A | D6 | N/A |
| Overall Visual Assessment of Electronic Display Devices | N/A | D7 | D7 | D7 | D7 |
C.3.1.2 Daily quality control tests
Daily Quality Control Tests. Daily Quality Control tests must be performed at the beginning of each day before commencing patient examinations.
-
D1
-
Equipment Warm-up—The manufacturer's recommended warm up procedure must be followed. The warm up procedure must be repeated if the equipment is left idle for an extended period of time. It is important to note that all components of the imaging system which are routinely used must be warmed up, including computer display devices and printers.
-
D2
-
Meters Operation—Meters and visual and audible indicators should be checked for proper function.
-
D3
-
Equipment Conditions—X-ray equipment conditions should be visually inspected for loose or broken components and cleanliness. The X-ray source assembly should be checked for motion or vibration during operation. Visual inspection should also be conducted of all other components of the imaging systems.
-
D4
-
System Movement—System movement should be checked for proper function. For systems where the X-ray source is below the table, verify the performance of the power assist and locks by moving the tower in all directions. For systems where the X-ray source is above the table, verify the motion of the X-ray tube assembly.
-
D5
-
Darkroom Cleanliness—In order to maintain the cleanliness of the darkroom all working surfaces, tops of counters and the floor should be cleaned daily. Dust and debris can more easily be seen using a UV-B lamp.
-
D6
-
Film Processor Function—Film processor function must be evaluated every morning before performing clinical examinations, after the processor has been turned on and has reached the required development temperature; and at other times as required, such as after a replenishment rate change. Facilities operating spotfilm equipment must also perform the following quality control tests on the film processing system.
- The film processing solution levels must be checked to ensure agreement with the manufacturers' recommended baseline levels for the particular processor and film type, for the given number of films processed daily.
- The displayed processor temperature must be checked to ensure agreement with the manufacturers' recommended baseline level for the particular processor and film used.
- Sensitometric strip processing must be performed in order to monitor the performance of the image processing system.
- The base plus fog must be within + 0.05 of the established operating level
- The mid-density must be within ± 0.15 of the established operating level
- The density difference must be within ± 0.15 of the established operating level
-
D7
-
Overall Visual Assessment of Electronic Display Devices—The performance of electronic display devices used for interpretation of clinical images must be assessed. Displaying the image of a test pattern, an assessment must be made of the general image quality and for the presence of artifacts. The SMPTE or the TG18-QC test patterns can be used for this test and should be displayed using the software routinely used to display clinical images. It is recommended that the test pattern image be viewed from a distance of 30 cm from the front of the display device. The results of the assessment must be within established limits.
C.3.1.3 Daily quality control test equipment
Test equipment for the daily quality control testing are listed in Table 12.
| Item | Equipment | Systems | Reference |
|---|---|---|---|
| 1 | Phantom (if needed for manufacturer's recommended warm up procedure) | FS, CR, DR, RA, SF, CT | D1 |
| 2 | Ultraviolet Light | FS, SF | D5 |
| 3 | Sensitometer (21 steps optical attenuator with densities ranging from approximately 0.00 to 4.80 in steps of 0.15) Accuracy: ± 0.02 log exposure units Reproducibility: ± 0.02 log exposure units |
FS, SF | D6 |
| 4 | Densitometer Accuracy: ± 0.02 O.D. at 1.0 O.D. Reproducibility: ± 0.01 O.D. at 1.0 O.D. |
FS, SF | D6 |
| 5 | Test Pattern Image (ex.: SMPTE or TG18-QC) | CR, DR, RA, CT | D7 |
Note: FS: Film Screen, CR: Computed Radiography, DR: Digital Radiography, RA: Radioscopy, SF: Spotfilm, CT: Computed Tomography |
|||
C.3.2 Weekly quality control testing
C.3.2.1 Quality control tests list
Weekly quality control tests are listed in Table 13. The imaging systems to which the tests are applicable, and the test numbers corresponding to those in section C.3.2.2, are provided.
| Quality control procedures under evaluation | Film-based system | CR system | DR system | Radioscopic system | CT system |
|---|---|---|---|---|---|
| Weekly quality control tests | |||||
| Visual Inspection of Cleanliness of Imaging Systems | W1 | W1 | W1 | W1 | W1 |
| Viewboxes Condition | W2 | W2 | W2 | W2 | W2 |
| Laser Film Printer Operation | N/A | W3 | W3 | W3 | W3 |
| CT Number Accuracy | N/A | N/A | N/A | N/A | W4 |
| CT Noise | N/A | N/A | N/A | N/A | W5 |
| CT Uniformity | N/A | N/A | N/A | N/A | W6 |
| Digital Subtraction Angiography System Performance | N/A | N/A | N/A | W7 | N/A |
C.3.2.2 Weekly Quality Control Tests
-
W1
-
Visual Inspection of Cleanliness of Imaging Systems—Imaging systems must be inspected for dust and dirt on or near the image reception area where they may negatively affect image quality. For CR systems, the imaging plates must be inspected. The imaging plate loading and unloading mechanism must be cleaned and lubricated if necessary. The image receptors for direct-capture systems must be kept clean of dust, dirt and other items which may come into contact with them. Laser scanning digitizers must also be checked for cleanliness.
-
W2
-
Viewboxes Condition—Viewboxes must be inspected visually for cleanliness, viewing area discolouration and improper illumination.
-
W3
-
Laser Film Printer Operation—The quality of images obtained from the laser film printer must be checked. Depending on the system, this may or may not require using pre-established window and level settings on the display. Ensure that the viewbox used to assess printed films has sufficient luminance. The SMPTE, TG18-QC and TG18-PQC test patterns should be used. A hardcopy image of the test pattern must meet the following criteria:
- the 5% patch must be just visible inside of the 0% patch
- the 95% patch must be just visible inside the 100%patch
- no geometrical distortion upon visual inspection
- no artifacts upon visual inspection
-
W4
-
CT Number Accuracy—An evaluation of the accuracy of the CT number of water must be made. Using a uniform water phantom, the mean CT number of water and the standard deviation, within a large region of interest, must remain within the established baseline and acceptable limits of variation. The CT number for water must be in the range of 0 ± 4HU. For quantitative CT application, a phantom containing the material of interest for the particular application should be used for this test. It is recommended that this test be performed at two CT conditions of operation, one representing a typical axial head scan and one representing a typical axial body scan.
-
W5
-
CT Noise—A measurement of CT noise must be made. Noise is given by the variation of CT numbers from a mean value in a defined area in the image of a uniform phantom. Its magnitude is equal to the standard deviation of the CT number values within the region of interest. For noise evaluation, the diameter of the region of interest should represent 40% of the diameter of the uniform phantom image. Noise can be quantified in HU or expressed as a percentage of the linear attenuation coefficient for water (see section B.2.5.5). The noise in a CT system must not deviate from the established baseline value by more than ± 10% or 0.2 HU, whichever is larger. The established baseline noise levels in a CT system should not deviate from the manufacturer specified noise value by more than ± 15%. It is recommended that this test be performed at two CT conditions of operation, one representing a typical axial head scan and one representing a typical axial body scan.
-
W6
-
CT Uniformity—Uniformity is defined as the consistency of the CT numbers of an image of a homogeneous material across the scan field. Uniformity is calculated using the following equation:
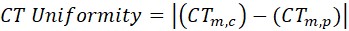
Equation C-1: Text Equivalent
The uniformity of a CT image of a homogeneous material is equal to the magnitude of the difference between the mean CT numbers at the centre and periphery of the image.
where
- CTm,c is the mean CT number in the centre of the image
- CTm,p is the mean CT number at the periphery of the image
The mean CT number must be determined for 5 regions of interest, one in the centre and 4 at the peripheries of the phantom. The diameter of each region of interest should represent 10% of the diameter of the phantom.
The difference between the mean CT number at the centre of the phantom and the periphery must not exceed 2 HU from the established baseline values. The baseline uniformity of the CT number for water must not be greater than ± 5 HU from the centre of the phantom to the periphery. It is recommended that this test be performed at two CT conditions of operation, one representing a typical axial head scan and one representing a typical axial body scan.
-
W7
-
Digital Subtraction Angiography System Performance—Following equipment warm up and prior to clinical use, the image quality of the DSA system should be evaluated using a phantom containing image quality test objects
C.3.2.3 Weekly quality control test equipment
Test equipment for the weekly quality control testing are listed in Table 14.
| Item | Equipment | Systems | Reference |
|---|---|---|---|
| 1 | Test Pattern Image | CR, DR, RA, CT | W3 |
| 2 | Water Filled Uniform Phantom | CT | W4, W5, W6 |
| 3 | Digital Subtraction Angiography Image Quality Phantom | RA | W7 |
C.3.3 Monthly quality control testing
C.3.3.1 Quality control tests list
Monthly quality control tests are listed in Table 15. The imaging systems to which the tests are applicable, and the test numbers corresponding to those in section C.3.3.2, are provided.
| Quality control procedures under Evaluation | Film-based system | CR system | DR system | Radioscopic system | CT system |
|---|---|---|---|---|---|
| Monthly quality control tests | |||||
| Cassette, Screen, and Imaging Plate Cleaning | M1 | M1 | N/A | M1 | N/A |
| Darkroom Temperature and Humidity Conditions | M2 | N/A | N/A | M2 | N/A |
| Darkroom Light Conditions | M3 | N/A | N/A | M3 | N/A |
| Film Processor Operation | M4 | N/A | N/A | M4 | N/A |
| Retake Analysis | M5 | M5 | M5 | N/A | N/A |
| Electronic Display Device Performance | M6 | M6 | M6 | M6 | M6 |
| Laser Film Printer Operation | M7 | M7 | M7 | M7 | M7 |
| CT Tomographic Section Thickness | N/A | N/A | N/A | N/A | M8 |
| Calibration of CT Number | N/A | N/A | N/A | N/A | M9 |
| CT Number Linearity | N/A | N/A | N/A | N/A | M10 |
C.3.3.2 Monthly quality control tests
-
M1
-
Cassette, Screen and Imaging Plate Cleaning—Cassettes, screens and imaging plates must be cleaned and inspected for damage. Manufacturer recommended cleaners and cleaning procedures should be used. An inspection for dust particles should be done with an ultraviolet light. Cassettes must be checked for cleanliness, wear, warping, fatigue of foam compression material and closure mechanism, light leaks.
-
M2
-
Darkroom Temperature and Humidity Conditions—A monthly check of the darkroom temperature and humidity should be conducted. The temperature should be between 18°C and 23°C and the humidity between 40% and 60%.
-
M3
-
Darkroom Light Conditions— A weekly visual test must be performed in the darkroom to ensure the room is light tight. Particular attention must be paid to the door seal and the mounting of the film processor, if the film insertion to the processor is done through a wall. The assessment of darkroom light conditions should be made after a 10 to 15 minute period of adaptation to the dark conditions with safelights turned off.
-
M4
-
Film Processor Operation—Facilities performing spotfilm must also perform quality control tests on the film processing system.
- The accuracy of the processor temperature display must be checked against a non-mercury thermometer. The processor developer temperature should be accurate to within 0.5°C.
- The replenishment rate must be compared with the manufacturers' recommended baseline level for the particular processor and film type, for the given number of films processed daily and for the method of processing.
- All processing solutions should be changed and processor solution tanks cleaned.
- Fixer retention tests should be performed to ensure fixer is adequately removed from processed films according to established baseline levels.
-
M5
-
Retake Analysis—Facilities must maintain records of every retake, including the reason for the retake along with any corrective actions. An analysis must be done of the retake records to identify and correct any trends or repeated errors. The retake rate should be less than 5%, not including quality control films. If images contain some patient diagnostic information, they should be maintained in the patient file.
-
M6
-
Electronic Display Device Performance—The performance of all electronic display devices used to view images from digital systems, as well as those obtained through scanning of radiographic films, must be checked using a test pattern such as the SMPTE or a TG18 test pattern. For closed systems, where a suitable test pattern is not available on the system, a test pattern generator equipped with the appropriate test patterns must be utilized. Where a system does not have the capability to display an externally provided pattern, the manufacturer recommended quality control procedures must be followed. The quality control procedures and acceptance criteria recommended by the AAPM (AAPM 2005)Footnote 2 should be used.
-
M7
-
Laser Film Printer Operation—The quality of images obtained from the laser film printer must be checked. Depending on the system, this may or may not require using pre-established window and level settings on the display. Ensure that the viewbox used to assess printed films has sufficient luminance. The SMPTE, TG18-QC and TG18-PQC test patterns should be used. A hardcopy image of the test pattern must meet the following criteria:
- the 5% patch must be just visible inside of the 0% patch
- the 95% patch must be just visible inside the 100% patch
- the optical density of various patches (for example 0%, 10%, 40% and 90%) must be within acceptable limits from the established baseline values, for the particular film used at the facility
- no geometrical distortion greater than ± 1 mm
- no artifacts upon visual inspection
-
M8
-
CT Tomographic Section Thickness—An evaluation of the tomographic section thickness must be made. Measurement of the tomographic section thickness are made with a test device containing one or two ramps positioned at an angle to the scan plane. For nominal tomographic section thicknesses of 2 mm or more, the measured tomographic section thickness must not vary by more than ± 1 mm from the established baseline tomographic section thickness. For nominal tomographic section thicknesses of 2 mm to 1 mm, the measured tomographic section thickness must not vary by more than ± 50% from the established baseline tomographic section thickness. For nominal tomographic section thicknesses of less than 1 mm, the measured tomographic section thickness must not vary by more than ± 0.5 mm from the established baseline tomographic section thickness. For multislice CT equipment, this test must be performed for both outer tomographic sections and one inner tomographic section. For helical scanning, a test device consisting of a thin disk or bead, mounted in a medium, should be used. The linear attenuation coefficient should be equal to or greater than that of aluminum so that the resulting signal-to-noise ratio is high. Upon scanning of this test device, the tomographic section is defined as the full width at half maximum of the sensitivity profile as a function of the z position.
-
M9
-
Calibration of CT number—At all clinically used voltage settings, the mean CT number and standard deviation should be measured. The mean CT number and standard deviation should be calculated for a 2-3 cm2 area of water and air in the reconstructed image. The same location should be used each time this test is performed. The CT number for water must be 0 ± 4 HU. The CT number for air must be -1000 ± 10 HU.
-
M10
-
CT number linearity—At all clinically used voltage settings, the CT number linearity should be assessed. The CT number linearity should be assessed by scanning a phantom containing uniform objects of known materials with a wide range of CT numbers. The measured CT numbers of the materials should be compared with the nominal values provided by the phantom manufacturer and with previously measured values. The measured values must remain within established limits for the CT scanner.
C.3.3.3 Monthly quality control tests equipment
Test equipment for the monthly quality control testing are listed in Table 16.
| Item | Equipment | Systems | Reference |
|---|---|---|---|
| 1 | Ultraviolet Light | FS, SF | M1 |
| 2 | Hygrometer | FS, SF | M2 |
| 3 | Thermometer (non-mercury) Accuracy: ± 0.3°C Reproducibility: ± 0.1°C |
FS, SF | M2, M4 |
| 4 | Fixer Retention Test Kit | FS, SF | M4 |
| 5 | Test pattern(s) for evaluation of electronic display device performance and laser film printer (ex. SMPTE, TG18-QC, TG18-PQC) | FS, CR, DR, RA, SF, CT | M6, M7 |
| 6 | Densitometer Accuracy: ± 0.02 O.D. at 1.0 O.D. Reproducibility: ± 0.01 O.D. at 1.0 O.D. |
CR, DR, RA, CT | M7 |
| 7 | Ruler | FS, CR, DR, RA, SF, CT | M7 |
| 8 | Test device containing ramps, thin disk or beads | CT | M8 |
| 9 | Water filled uniform phantom | CT | M9 |
| 10 | Phantom with imbedded uniform objects of known materials | CT | M10 |
C.3.4 Quarterly quality control testing
C.3.4.1 Quality control tests list
Quarterly quality control tests are listed in Table 17. The imaging systems to which the tests are applicable, and the test numbers corresponding to those in section C.3.4.2, are provided.
| Quality control procedures under evaluation | Film-based system | CR system | DR system | Radioscopic system | CT system |
|---|---|---|---|---|---|
| Quarterly quality control tests | |||||
| Collimator Operation | Q1 | Q1 | Q1 | Q1 | N/A |
| Interlocks | Q2 | Q2 | Q2 | Q2 | Q2 |
| Table Angulation and Motion | N/A | N/A | N/A | Q3 | N/A |
| Compression Devices Operation | N/A | N/A | N/A | Q4 | N/A |
| Chronometer Operation | N/A | N/A | N/A | Q5 | N/A |
| Protective Devices | N/A | N/A | N/A | Q6 | N/A |
| Park Position Interrupt | N/A | N/A | N/A | Q7 | N/A |
| CT Patient Support Movement | N/A | N/A | N/A | N/A | Q8 |
| CT Spatial Resolution | N/A | N/A | N/A | N/A | Q9 |
| CT Low Contrast Detectability | N/A | N/A | N/A | N/A | Q10 |
C.3.4.2 Quarterly quality control tests
-
Q1
-
Collimator Operation—Using each collimating option, a test should be performed to ensure smooth collimator blade motion. If applicable, vary the SID to assure the collimator tracks (i.e., automatically maintain the field size) as the SID changes.
-
Q2
-
Interlocks—If there are interlocks on the door(s), they must be tested to ensure that they prevent the X-ray equipment from producing radiation when the door is open. For radioscopic equipment, it must not be possible to activate the X-ray tube unless the entire radioscopic beam is intercepted by the image receptor.
-
Q3
-
Table Angulation and Motion—The table should move freely to the upright position and stop at the appropriate spot. The table angle indicator and the actual table angle should coincide to within 2 degrees.
-
Q4
-
Compression Devices Operation—Check that available compression devices easily move in and out of the X-ray beam and function correctly.
-
Q5
-
Chronometer Operation—The chronometer accuracy should be verified with a stopwatch.
-
Q6
-
Protective Devices for Radioscopic Equipment—A protective curtain or drape, of at least 0.25 mm lead equivalence at 100 kV, must be in place and move freely so that it can be placed between the patient and any personnel in the radioscopic room. Lead drapes should be affixed to the image intensifier (under table systems) and have no creases or gaps that may subject the operator to unnecessary scatter radiation. If the unit is an under table radioscopic system, check that the shield covering the cassette holder entrance during radioscopy is working as intended. The shield should provide the equivalent protection of at least 0.5 mm of lead at 100 kV.
-
Q7
-
Park Position Interrupt—When the image receptor is in the parked position, it should not be possible to energize the X-ray tube. This may be checked while wearing a lead apron and depressing the radioscopic irradiation switch to see if the system is activated.
-
Q8
-
CT Patient Support Movement—The accuracy of the patient support movement ensures that the desired volume of the patient is scanned. This becomes important when performing contiguous scans where the scan interval equals the scan width to image an entire volume of the patient. If the scan interval is larger than the scan width, then gaps are present in the imaged volume. If the scan interval is smaller than the scan width, then the scans will overlap. The measured patient support movement must be within ± 1 mm of the intended movement when the patient support moves both into and out of the gantry. To simulate the weight of the patient, a phantom or other weights (not exceeding 135 kg) must be place on the support when performing this test.
-
Q9
-
CT Spatial Resolution—The spatial resolution must be tested, with the CT conditions of operation of the scanner, using one of the following three methods. The recommended method of measuring the spatial resolution is using the modulation transfer function curve, obtained from the Fourier transform of the point-spread function. The test device is a high contrast wire, typically 2 mm in diameter or less, placed in a tube of minimally attenuating material. The measurement of the 50% point and the 10% point of the MTF curve must be within 0.5 lp/cm or ± 15% of the established baseline value, whichever is greater.
A quantitative measurement of modulation can be made using a bar pattern test device which contains line-pair patterns of different spatial frequencies. Using region of interest measurements, individual points along the MTF curve can be obtained. When measurements are made using a test object with line-pair patterns of varying spatial frequency or by noting the spatial frequency at which the measured modulation transfer function drops to 5%, the limiting high contrast resolution should be 5 line pairs per centimetre or more.
An alternate method is through visual assessment using a test device consisting of a repeated pattern of holes, bars or lines. When measuring the limiting high contrast resolution using a phantom for high contrast resolution having sets of test objects of equal diameters and spacing, the high contrast resolution must be 1 mm or less.
-
Q10
-
CT Low Contrast Detectability—Measurements should be made of the low contrast detectability to ensure it is within established limits. Low contrast detectability is typically specified as the smallest sized object at a specified contrast level to the background which can seen in a particular phantom when imaged under specified conditions. The phantom used for this test should have objects with less than 1% or 10 HU contrast to the surrounding material. The limiting detectability should be measured with the reconstruction algorithm of the scanner which is routinely used, as well as other clinically relevant reconstruction algorithms. The baseline performance level must be stated for a given phantom at specific scan conditions, including radiation dose, viewing conditions, and visualization criteria. It should be noted that this visual test for establishing low contrast detectability is subjective since it depends on a number of factors including the visual acuity of the observers and ambient lighting conditions.
C.3.4.3 Quarterly quality control tests equipment
Test equipment for the quarterly quality control testing are listed in Table 18.
| Item | Equipment | Systems | Reference |
|---|---|---|---|
| 1 | Stopwatch | RA | Q5 |
| 2 | Dosimeter Accuracy: ± 5% Reproducibility: ± 1% |
RA | Q6 |
| 3 | Weight (not exceeding 135 kg) | CT | Q8 |
| 4 | Ruler | CT | Q8 |
| 5 | Pre-packaged film (ex. "Ready Pack") | CT | Q8 |
| 6 | Needle (for puncturing holes in film) | CT | Q8 |
| 7 | CT Spatial Resolution Test Device | CT | Q9 |
| 8 | CT Spatial Resolution Test Device | CT | Q10 |
C.3.5 Semi-annual quality control testing
C.3.5.1 Quality control tests list
Semi-annual quality control tests are listed in Table 19. The imaging systems to which the tests are applicable, and the test numbers corresponding to those in section C.3.5.2, are provided.
| Quality control procedures under evaluation | Film-based system | CR system | DR system | Radioscopic system | CT system |
|---|---|---|---|---|---|
| Semi-annual quality control tests | |||||
| CT Laser Light Accuracy | N/A | N/A | N/A | N/A | SY1 |
CT Accuracy of Automatic Positioning of Tomographic Plane |
N/A | N/A | N/A | N/A | SY2 |
| CT Accuracy of Gantry Tilt | N/A | N/A | N/A | N/A | SY3 |
| CT Patient Dose | N/A | N/A | N/A | N/A | SY4 |
C.3.5.2 Semi-annual quality control tests
-
SY1
-
CT Laser Light Accuracy—Laser light accuracy must be determined for both axial scan localization lights, which indicate the location of the radiation beam relative to the external anatomical structures of the patient, and the sagittal and coronal scan localization lights, which centre the anatomic structure of interest in the scan field of view.
- Axial Scan Localization Lights—Axial scan localization light accuracy is tested either by imaging a thin wire (approximately 1 mm diameter) or by using a needle to puncture holes in film at the positions of the laser lights and exposing the film using the smallest available scan width. The difference between the exposed areas on the film and the locations of the pin pricks must be less than ± 2 mm.
- Isocentre Alignment and Sagittal and Coronal Scan Localization Lights—Place a thin absorber (pencil) centred in the tomographic plane at the intersection of the sagittal and coronal positioning light fields. The intersection of the sagittal and coronal scan localization lights must indicate the centre of the field of view. The midline of the table should be coincident with the sagittal scan alignment light. The results must be within the manufacturer's recommended values and tolerances. A limit of ± 5 mm should be achievable.
-
SY2
-
CT Accuracy of Automatic Positioning of Tomographic Plane (using the scanned projection radiograph/scout localization)—The location of the scan plane prescribed by using the scanned projection radiograph must be within ± 2 mm of the actual scan plane.
-
SY3
-
CT Accuracy of Gantry Tilt—The accuracy of the indicated CT gantry tilt should be verified. When performing non-orthogonal scans, it is important to ensure that the physical tilt of the gantry corresponds to the tilt angle indicated on the CT display. This is generally done by exposing film placed upright and parallel to the sagittal laser at various gantry tilt angles. At least 3 irradiations need to be made on the film: no tilt (0 degrees) and each of the extreme angles. The angles measured on the film should correspond with the computer display to within ± 3 degrees.
-
SY4
-
Patient Dose—The CTDI100 must be determined for both head and body scanning techniques, using the CT dosimetry phantom placed on the patient support without any additional attenuating material present. For each technique, the CTDI100 must be determined at the centre and periphery of the phantom as well as in air using the manufacturer's recommended techniques and setting. The values of CTDI100 are used to calculate CTDIw which must be within ± 20% of the established baseline values and the manufacturer's specifications when a fixed technique is used. It is highly recommended to strive for an agreement with manufacturers' specification of ± 10%. This test should be performed by a medical physicist.
C.3.5.3 Semi-annual quality control tests equipment
Test equipment for the semi-annual quality control testing are listed in Table 20.
| Item | Equipment | Systems | Reference |
|---|---|---|---|
| 1 | Thin wire | CT | SY1, SY2 |
| 2 | Pre-packaged film (ex. "Ready Pack") | CT | SY1, SY3 |
| 3 | Sharp needle (for puncturing holes in film) | CT | SY1 |
| 4 | Pencil | CT | SY1 |
| 5 | Ruler | CT | SY1 |
| 6 | Protractor | CT | SY3 |
| 7 | CT Dosimetry Phantom—Head Circular cylinder constructed of polymethyl methacrylate Density 1.19 ± 0.01gm/cm3, length 14 cm, diameter 16 cm |
CT | SY4 |
| 8 | CT Dosimetry Phantom—Body Circular cylinder constructed of polymethyl methacrylate Density 1.19 ± 0.01gm/cm3, length 14 cm, diameter 32 cm |
CT | SY4 |
| 9 | Dosimeter and CT Dose Probes | CT | SY4 |
C.3.6 Annual quality control testing
C.3.6.1 Quality control tests list
Annual quality control tests are listed in Table 21. The imaging systems to which the tests are applicable, and the test numbers corresponding to those in section C.3.6.2, are provided.
| Quality control procedures under evaluation | Film-based system | CR system | DR system | Radioscopic system | CT system |
|---|---|---|---|---|---|
| Annual quality control tests | |||||
| Safelight Test | Y1 | N/A | N/A | Y1 | N/A |
| Film/Screen Contact | Y2 | N/A | N/A | Y2 | N/A |
| Accuracy of Loading Factors | Y3 | Y3 | Y3 | Y3 | N/A |
| Radiation Output Reproducibility | Y4 | Y4 | Y4 | Y4 | N/A |
| Radiation Output Linearity | Y5 | Y5 | Y5 | Y5 | N/A |
| X-ray Beam Filtration | Y6 | Y6 | Y6 | Y6 | N/A |
| Automatic Exposure Control | Y7 | Y7 | Y7 | Y7 | N/A |
| X-ray Field and Light Field Alignment | Y8 | Y8 | Y8 | Y8 | N/A |
| X-ray Beam Collimation | Y9 | Y9 | Y9 | Y9 | N/A |
| Grid Performance | Y10 | Y10 | Y10 | Y10 | N/A |
| Response Function | N/A | Y11 | Y11 | N/A | N/A |
| Exposure Index | N/A | Y12 | Y12 | N/A | N/A |
| Dynamic Range | Y13 | Y13 | Y13 | Y13 | N/A |
| Noise, Uniformity and Image Artifacts | N/A | Y14 | Y14 | N/A | N/A |
| Spatial Resolution | Y15 | Y15 | Y15 | Y15 | N/A |
| Contrast Detectability | Y16 | Y16 | Y16 | Y16 | N/A |
| Digital Detector Residual Images | N/A | Y17 | Y17 | N/A | N/A |
| Phantom Dose Measurements | Y18 | Y18 | Y18 | Y18 | N/A |
| Typical Image Intensifier Air Kerma Rate | N/A | N/A | N/A | Y19 | N/A |
| Maximum Image Intensifier Air Kerma Rate | N/A | N/A | N/A | Y20 | N/A |
| Automatic Intensity Control | N/A | N/A | N/A | Y21 | N/A |
| Image Lag | N/A | N/A | N/A | Y22 | N/A |
| CT Number Dependence on Phantom Position | N/A | N/A | N/A | N/A | Y23 |
| CT Radiation Dose Profile | N/A | N/A | N/A | N/A | Y24 |
| CT Radiation Dose—Scout Localisation Image | N/A | N/A | N/A | N/A | Y25 |
| Viewboxes | Y26 | Y26 | Y26 | Y26 | Y26 |
| Electronic Display Device Performance | N/A | Y27 | Y27 | Y27 | Y27 |
| Integrity of Protective Equipment | Y28 | Y28 | Y28 | Y28 | Y28 |
| General Preventive Maintenance | Y29 | Y29 | Y29 | Y29 | Y29 |
C.3.6.2 Annual quality control tests
-
Y1
-
Safelight Test—An evaluation must be made of the effects of the safelight on film optical density. A film strip exposed to an optical density of 1.2 units must not show an increase in optical density greater than 0.05 units in two minutes exposure to the darkroom light environment. Facilities performing spotfilm must also perform this quality control test.
-
Y2
-
Screen/Film Contact—All cassettes used in the facility must be tested for screen/film contact. Large areas of poor contact that are not eliminated by screen cleaning and remain in the same location during subsequent tests should be replaced. Facilities performing spotfilm must also perform this quality control test.
-
Y3
-
Accuracy of Loading Factors—For any combination of loading factors, the X-ray tube voltage must not deviate from the selected value, by more than 10%, the loading time must not deviate from the selected value by more than (10% + 1 ms), the X-ray tube current, must not deviate from the selected by more than 20%, and the current-time product must not deviate from the selected value by more than (10% + 0.2 mAs).
-
Y4
-
Radiation Output Reproducibility—The X-ray tube radiation output shall be high enough to minimize irradiation time to eliminate perceptible motion artifacts. For any combination of operating loading parameters, the coefficient of variation of any ten consecutive irradiation measurements, taken at the same source to detector distance within a time period of one hour, is no greater than 0.05, and each of the ten irradiation measurements is within 15% of the mean value of the ten measurements
-
Y5
-
Radiation Output Linearity—For any pre-selected value of X-ray tube voltage, the quotient of the average air kerma measurement divided by the indicated current time product obtained at two settings of X-ray tube current or X-ray tube current-time product must not differ by more than 0.10 times their sum, that is,
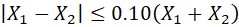
Equation C-2: Text Equivalent
To ensure radiation output linearity, the magnitude of the difference between X1 and X2 must be less than or equal to one tenth of the sum of X1 and X2.
where X1 and X2 are average air kermas (exposures) per current time product. The values of X1 and X2 must be determined at:
- if the X-ray tube current is selected in discrete steps, any two consecutive X-ray tube current settings
- if the X-ray tube current selection is continuous, any two X-ray tube current settings that differ by a factor of 2 or less
- if the current time product is selected in discrete steps, any two consecutive current time product settings; or
- if the current time product selection is continuous, any two current time product settings that differ by a factor of 2 or less
-
Y6
-
X-ray Beam Filtration—The first half-value layer of aluminum must be measured. The measured values must not be less than the values shown in Table 8 in subsection B.2.5.1 for a selected X-ray tube voltage.
-
Y7
-
Automatic Exposure Control—For film-based systems, the automatic exposure control must be evaluated to ensure it performs in such a way that the variation in optical density in the resultant radiograms does not exceed the value of:
- 0.15 when the X-ray tube voltage is variable and the thickness of the irradiated object is constant
- 0.20 when the thickness of the irradiated object is variable and the X-ray tube voltage is constant
- 0.20 when the thickness of the irradiated object and the X-ray tube voltage are both variable, and
- 0.10 when the thickness of the irradiated object and the X-ray tube voltage are both constant
For digital systems, the performance of the automatic exposure control must be assessed according to the manufacturer's procedures and must be within the manufacturer's specifications. It is recommended that the automatic exposure control should perform in such a way that the variation in the mean linearized data on a constant region of interest does not exceed 20% for constant X-ray tube voltage and constant thickness of the irradiated object, when the X-ray system is operated in conditions representative of the typical clinical use. Compliance is checked by ensuring that the ratio of the highest and the lowest measured values is less than or equal to 1.2 or within the manufacturer's specifications.
-
Y8
-
Light Field and X-ray Field Alignment—The alignment of the light localizer, designed to define the outline of the X-ray field, with the X-ray field must be verified. In the plane of the image receptor, the misalignment, of the edges of the visually defined field with the edges of the X-ray field must not exceed 2% of the focal spot to image receptor distance.
-
Y9
-
X-ray Beam Collimation—
- An evaluation of the beam limiting device must be made to ensure that the equipment is capable of aligning the centre of the X-ray field with the centre of the image reception area to within 2% of the focal spot to image receptor distance.
- Radiographic X-ray equipment that has a positive beam limiting system must prevent the emission of X-rays until the beam limiting device is adjusted so that
- the dimensions of the X-ray field do not exceed those of the image reception area, or the selected portion of that area, by more than 3% of the focal spot to image receptor distance, and
- the sum of the absolute values of the differences in the dimensions of the X-ray field and the image reception area, or the selected portion of that area, does not exceed 4% of the focal spot to image receptor distance
- Radioscopic equipment equipped with a spotfilm device must have a mechanism that, when the X-ray beam axis is perpendicular to the image reception plane, permits the perimeter of the X-ray field to be aligned with that of the selected portion of the image reception area so that
- the dimensions of the X-ray field differ from the corresponding dimensions of the image reception area by a distance that does not exceed 3% of the focal spot to image receptor distance, and
- the sum of the absolute values of the differences in the dimensions between the X-ray field size and the image reception area does not exceed 4% of the focal spot to image receptor distance
-
Y10
-
Grid Performance—Grid performance, including movement and uniformity, must be checked annually.
-
Y11
-
Response Function—For digital X-ray imaging systems, the response function of the detector should be assessed. The manufacturer specified relationship between the system response (mean pixel value in a standard region of interest) and exposure to the image receptor, over a range of tube loadings, should be confirmed to be within established limits. The manufacturer's recommended testing procedure should be followed.
-
Y12
-
Exposure Index—For digital X-ray imaging systems, the accuracy and reproducibility of the exposure index, as a function of the dose to the image receptor, must be evaluated. The manufacturer's recommended testing procedure must be followed and the results must be within established limits.
-
Y13
-
Dynamic Range—For film screen systems, a high purity step wedge should be used to monitor the performance of the X-ray generator. When using a 11-step wedge, the acceptable variation in film density should be ± 1 step from the established baseline density, or when using a 21-step wedge, the acceptable variation in film density should be ± 2 steps from the established baseline density. For digital systems, the dynamic range is a measure of the maximum difference in attenuation that the system can simultaneously image, without loss of information due to saturation of pixels. A test object consisting of an attenuating plate terminated with a step wedge of 12 steps should be used. The number of non saturated steps or the thickness of the smallest non saturated step should be within established limits.
-
Y14
-
Noise, Uniformity and Image Artifacts—An assessment must be made of noise, uniformity and image artifacts. The Signal-to-Noise Ratio (SNR) should be calculated by measuring the mean pixel value and standard deviation in a region of interest within the image. The standard deviation of signal values should be determined for three different locations, at the centre, at the top, and at the side of the image. The size of the region of interest should equal approximately 10% of the area of the phantom. The test should be done using homogeneous phantoms having thicknesses representative of patient thickness. The measured noise value must be within established limits. The uniformity of the signal across the different regions of interest at the periphery and the centre of the phantom must be within established limits. Images must be assessed to ensure that unacceptable artifacts are not present.
-
Y15
-
Spatial Resolution—An evaluation must be of the spatial resolution of the equipment. Spatial resolution is the ability to resolve objects in a resultant image when the difference in the attenuation between the objects and the background is large compared to noise. The manufacturer's recommended test procedures must be followed. For each mode of operation, the spatial resolution must within established limits.
-
Y16
-
Contrast Detectability—An evaluation should be made of contrast detectability. The contrast detectability is the ability to resolve different objects from the background when the difference in attenuation between the objects and the background is small compared to noise. The manufacturer's recommended test procedures should be followed. For each mode of operation, the contrast resolution should be within established limits. For DSA applications, it is recommended to use a phantom with contrast levels representative of clinically used iodine contrast levels.
-
Y17
-
Digital Detector Residual Image—There must not be any visible residual image from a previous exposure. The manufacturer's recommended test procedure should be followed.
-
Y18
-
Phantom Dose Measurements—Entrance skin air kerma measurement for frequently performed examinations must be within established limits. Measurements should be performed using the equipment geometry and loading conditions representative of those used clinically. Dose values obtained should be used for the annual review of the facilities Diagnostic Reference values.
-
Y19
-
Typical Air Kerma Rate of Radioscopic Equipment— Using a uniform phantom place on the patient support, measurements of the typical entrance air kerma rate, including backscatter, should be made for all geometries and modes of operation used clinically. The values should be within established levels.
-
Y20
-
Maximum Air Kerma Rate of Radioscopic Equipment—Radioscopic equipment, other than when recording images, must not operate at any combination of X-ray tube voltage and X-ray tube current that results in an air kerma rate that exceeds
- 50 mGy/min when the equipment is not fitted with an automatic intensity control
- 100 mGy/min when the equipment is fitted with an automatic intensity control, and
- 150 mGy/min when the equipment is fitted with both an automatic intensity control and a high level irradiation control when the latter is activated
The image intensifier must be protected with sufficient (approximately 6 mm) lead sheets when performing this test.
-
Y21
-
Automatic Intensity Control—An evaluation must be made of the automatic intensity control system of radioscopic systems. The automatic intensity control system is designed to maintain the rate of the X-ray exposure to the image intensifier with changes in thickness and composition of the anatomical region being imaged. Place a dosimeter between a homogenous phantom and the X-ray source. Double the phantom thickness and repeat the exposure. The exposure measurement should be approximately double the first measurement.
-
Y22
-
Image Lag—An evaluation of the image lag should be made to ensure the performance of the TV camera does not cause unnecessary smearing of the radioscopic image. Radioscopic systems used for cardiac catheterization and interventional procedures must have a high frame rate to provide sufficient temporal resolution required by such procedures. Viewing the image of a rotating test tool, the radioscopic system should be able to visualize a wire of diameter 0.013 inch or smaller.
This test should be repeated using cine cameras and digital recorders to ensure that these systems are delivering optimal image quality.
-
Y23
-
CT number dependence on phantom position—The CT number for water must not vary by more than ± 5 HU when the position of a water filled phantom is varied over clinically relevant positions on the patient support.
-
Y24
-
CT Radiation Dose Profile—The collimation of the radiation beam should be assessed to ensure it does not exceed the prescribed scan width. Scan width is typically defined as the full width half maximum (FWHM) of the radiation dose profile. For each available scan width, the FWHM of the radiation dose profile should not exceed the prescribed scan width by more than manufacturer's specifications. The FWHM of the radiation dose profile can be measured either directly from the density profile of the resultant film or computed from the digital profile upon digitization of the image.
-
Y25
-
CT Radiation Dose–Scan Projection Radiograph/Scout Localization Image—The dose delivered from a scout localization image, which is a scanned projection radiograph, must remain within ± 20% of the nominal value. Changes in this dose can be indicative of problems with collimation or patient support movement. The technique and loading factors used to obtain the scout localization image must be recorded, so that identical test conditions can be used for subsequent tests. It is recommended that this test be performed semi-annually, but must be performed at least annually.
-
Y26
-
Viewboxes—All viewboxes must be tested for compliance with the following requirements. Ensure all viewboxes have been turned on for a minimum of 30 minutes before obtaining measurements.
- Luminance. Luminance is the amount of light emitted or scattered by a surface. The view box luminance should be at least 2,500 nits (cd/m2)
- Light Output Uniformity. The light output from the viewboxes should be uniform to within 10%. Measurements should not be made near the edges of the viewbox (within 1 to 2 inches), where luminance values may be quite low
- Light Output Homogeneity. The light output homogeneity between a bank of viewboxes should be uniform to within 20% of the mean
- Ambient Light Control. The ambient light within the reading room must be less than 50 lux. A value of 5-10 lux is recommended
-
Y27
-
Electronic Display Device Performance—The performance of all electronic display devices used for the interpretation of clinical images and guidance during interventional procedures must be verified using a test pattern such as the SMPTE or TG18 test patterns. For closed systems, where a suitable test pattern is not available on the system, a test pattern generator equipped with the appropriate test patterns must be utilized. Where a system does not have the capability to display an externally provided pattern, the manufacturer recommended quality control procedures must be followed. The annual quality control tests recommended by the American Association of Physicists in MedicineFootnote 2 (AAPM, 2005), including test procedures and acceptance criteria should be used. An evaluation should be made of geometric distortion, reflection, luminance response, luminance dependencies, resolution, noise, veiling glare and chromaticity. The display system must be warmed up prior to testing and attention must be given to the ensure ambient light levels are appropriate and representative of condition under which clinical images are viewed. A viewing distance of 30 cm is recommended.
-
Y28
-
Integrity of Protective Equipment—All personnel's protective equipment must be examined using radiographic or radioscopic equipment to ensure they are not defective. Lead aprons where the total defective area is greater than 670 mm2 are not acceptable. Personnel protective equipment having a defect in the vicinity of the thyroid or the reproductive organs which is larger than the equivalent of a 5 mm diameter circle must not be used. Personal judgement should be used when small defects are located along the edges of the protective equipment and when defects are due to stitching of the equipment. All protective equipment, when not in use, should be stored in accordance to the manufacturers' recommendations.
-
Y29
-
General Preventive Maintenance—Preventive maintenance of the X-ray equipment and accessories is necessary to prolong the life of the equipment. An annual inspection must be conducted for structural integrity, cleanliness, ease of movement of all components and any other procedures recommended by the manufacturers.
C.3.6.3 Annual quality control tests equipment
Test equipment for annual quality control testing are listed in Table 22.
| Item | Equipment | Systems | Reference |
|---|---|---|---|
| 1 | Densitometer Accuracy: ± 0.02 O.D. at 1.0 O.D. Reproducibility: ± 0.01 O.D. at 1.0 O.D. |
FS, SF | Y1, Y7, Y13 |
| 2 | Stopwatch | FS, SF | Y1 |
| 3 | Film/screen contact test tool | FS, SF | Y2 |
| 4 | Non-invasive X-ray tube voltage meter Accuracy: ± 1.5 kV Reproducibility: ± 0.5 kV |
FS, CR DR, SF | Y3 |
| 5 | Irradiation time meter Accuracy: ± 5% Reproducibility: ± 1% |
FS, CR DR, SF | Y3 |
| 6 | Current meter Accuracy: ± 1% Reproducibility: < 0.5% |
FS, CR, DR, SF | Y3 |
| 7 | Dosimeter Accuracy: ± 5% Reproducibility: ± 1% CT dose probes - scout localization dose |
FS, CR, DR, RA | Y4, Y5, Y6, Y11, Y12, Y18, Y19, Y20, Y21, Y25 |
| 8 | Aluminum filter (> 99.9% purity) Accuracy: 1% thickness |
FS, CR, DR | Y6, Y17 |
| 9 | Multiple sheets of uniform, tissue equivalent attenuator (covering range of clinical patient thicknesses) | FS, CR, DR, RA, SF | Y7, Y10, Y11, Y12, Y13, Y14, Y15, Y16, Y17, Y19,Y21 |
| 10 | Metallic markers | FS, CR, DR, RA, SF | Y8 |
| 11 | Ruler | FS, CR, DR, RA, SF | Y8, Y9, Y28 |
| 12 | X-ray Beam Alignment test tool | FS, CR, DR, RA, SF | Y9 |
| 13 | Stepwedge | FS, CR, DR, RA, SF | Y13 |
| 14 | Spatial Resolution test tool (specific for type of equipment) |
FS, CR, DR, RA, SF | Y15 |
| 15 | Contrast Detectability test tool (specific for type of equipment) |
FS, CR, DR, RA, SF | Y16 |
| 16 | Phantom for evaluation of Entrance Surface Dose | FS, CR, DR, RA, SF | Y18 |
| 17 | 6 mm lead sheet | RA | Y20 |
| 18 | Rotatable spoke test tool pattern (steel wires of diameter ranging from 0.005 inches to 0.022 inches, rotatable at 30 rpm) |
RA | Y22 |
| 19 | Electric motor capable of producing 30 rpm | RA | Y22 |
| 20 | Water filled uniform phantom | CT | Y23 |
| 21 | Pre-packed film (ex. "Ready Pack") | CT | Y24 |
| 22 | Scanning Microdensitometer | CT | Y24 |
| 23 | CT Dosimetry Phantom - Head Circular cylinder constructed of polymethyl methacrylate Density 1.19 ± 0.01 gm/cm3, length 14 cm, diameter 16 cm |
CT | Y25 |
| 24 | CT Dosimetry Phantom - Body Circular cylinder constructed of polymethyl methacrylate Density 1.19 ± 0.01 gm/cm3, length 14 cm, diameter 32 cm |
CT | Y25 |
| 25 | CT Dose Probes | CT | Y25 |
| 26 | Light meter (for measurement of luminance and illuminance) Accuracy: ± 10% Reproducibility: ± 5% |
FS, CR, DR, SF, CT | Y26 |
| 27 | Test patterns (for evaluation of electronic display system) (ex. TG18) | CR, DR, RA, CT | Y27 |
Appendix I: Dose limits for occupational ionizing radiation exposures
For the purpose of this safety code, individuals may be classified in one of two categories: (1) radiation workers, individuals who are occupationally exposed to X-rays and (2) members of the public. The dose limits are given for both categories in Table AI.1. These dose limits are based on the latest recommendations of the International Commission on Radiological Protection (ICRP) as specified in ICRP Publications 103 (ICRP 2007)Footnote 11 and 118 (ICRP 2012)Footnote 12.
Dose limits for radiation workers apply only to irradiation resulting directly from their occupation and do not include radiation exposure from other sources, such as medical diagnosis and background radiation.
| Applicable body organ or tissue | Radiation workers | Members of the Public |
|---|---|---|
| Whole Body | 20 mSv effective dose per year averaged over a defined 5 year period (i.e. a limit of 100 mSv in 5 years) and 50 mSv in any single year. | 1 mSv effective dose |
| Lens of the eye | 20 mSv equivalent dose per year averaged over a defined 5 year period and 50 mSv in any single year. | 15 mSv |
| Skin | 500 mSv equivalent dose | 50 mSv equivalent dose |
| Hands and feet | 500 mSv equivalent dose | - |
- It is emphasized that any irradiation involves some degree of risk and the levels suggested in this Appendix are maximum values. All doses must be kept as low as reasonably achievable and any unnecessary radiation exposure must be avoided.
- The ICRP does not recommend discrimination in the dose limits between different biological sexes of persons of reproductive capacity, if the dose is received at an approximately regular rate.
- For occupationally exposed persons, once pregnancy has been voluntarily declared, the foetus must be protected from X-ray exposure. This includes an effective dose limit of 4 mSv for the remainder of the pregnancy, from all sources of radiation.
- Under the scope of this document, occupational exposures to pregnant persons arise mainly from scattered X-radiation. In this case, the most effective method of monitoring exposures to the foetus, is to measure the equivalent dose to the surface of the abdomen using a personal dosimeter.
- For technologists-in-training and students, the recommended dose limits for members of the public should apply.
- For the skin, the equivalent dose is averaged over its whole area. In situations where tissue effects are possible, the recommended equivalent dose limit for the skin is 500 mSv and is averaged over areas of no more than 1 cm2.
- Some provincial or territorial jurisdictions may have different dose limits for some workers. The appropriate agency, listed in Appendix V, should be consulted to determine the dose limits in effect in a particular jurisdiction.
Appendix II: Shielding information checklist templates
| Information required for radiographic X-ray systems | |
|---|---|
| Description | Yes/No |
| Floor plan (scaled blueprint or sketch) including: | |
| Dimensions of the X-ray room, and location of the control booth if present | |
| Location(s) of the X-ray tube, X-ray table, wall mounted imaging device, CR reader, etc. | |
| Direction(s) of the radiation beam during normal operation | |
| Distance(s) between the areas to be shielded and the operational position of the X-ray tube | |
| Location of the control panel and irradiation switch | |
| Identification of all adjacent rooms, including those rooms located above and below, e.g., offices, storage rooms, crawl spaces, etc. | |
| The designation of the area to be shielded, controlled area (for radiation workers), or uncontrolled area (for non-radiation workers and the public) | |
| The Occupancy and Use factors for the areas to be shielded | |
| Medical X-ray equipment | |
| Manufacturer, brand name and model number of the X-ray system(s) | |
| Maximum selectable tube voltage (kV) | |
| Maximum selectable tube current (mA) or maximum selectable tube current time product (mAs) | |
| Maximum selectable irradiation time (sec) | |
| For film screen system: the manufacturer, type and speed of film screen combination used | |
| For CR system: the manufacturer and brand name of CR reader and storage phosphor system used | |
| Equipment workload | |
| Number of patients per week | |
| Average tube voltage per procedure (kV) | |
| Average current time product per patient (mAs) | |
| Information required for radioscopic X-ray systems | |
|---|---|
| Description | Yes/No |
| Floor plan (scaled blueprint or sketch) including: | |
| Dimensions of the X-ray room, and location of the control booth if present | |
| Location(s) of the X-ray tube, X-ray table, image receptor, image display units, etc. | |
| Direction(s) of the radiation beam during normal operation | |
| Distance(s) between the areas to be shielded and the operational position of the X-ray tube | |
| Location of the control panel and irradiation switches | |
| Identification of all adjacent rooms, including those rooms located above and below, e.g., offices, storage rooms, crawl spaces, etc. | |
| The designation of the area to be shielded, controlled area (for radiation workers), or uncontrolled area (for non-radiation workers and the public) | |
| The Occupancy factor for the areas to be shielded | |
| Medical X-ray equipment | |
| Manufacturer, brand name and model number of the X-ray system(s) | |
| Maximum tube voltage (kV) | |
| Maximum tube current time product (mAs) | |
| Number of X-ray tubes on the system | |
| Equipment workload | |
| Number of patients per week | |
| Average tube voltage per procedure (kV) | |
| Average current time product per patient (mAs) | |
| Information required for CT systems | |
|---|---|
| Description | Yes/No |
| Floor plan (scaled blueprint or sketch) including: | |
| Dimensions of the X-ray room, and location of the control booth | |
| Location(s) of the gantry, patient support, etc. | |
| Distance(s) between the areas to be shielded and the position of the gantry | |
| Location of the control panel and irradiation control | |
| Identification of all adjacent rooms, including those rooms located above and below, e.g., offices, storage rooms, crawl spaces, etc. | |
| The designation of the area to be shielded, controlled area (for radiation workers), or uncontrolled area (for non-radiation workers and the public) | |
| The Occupancy factor for the areas to be shielded | |
| Medical X-ray equipment | |
| Manufacturer, brand name and model number of the CT system | |
| Maximum tube voltage (kV) | |
| Maximum tube current time product (mAs) | |
| Isodose curve for the system (to be provided by the manufacturer) | |
| Equipment workload | |
| Number of patients per procedure type per week | |
| Average tube voltage per procedure (kV) | |
| CTDI100 and DLP values, if known | |
Appendix III: NCRP #49 Methodology for calculation of shielding requirements for diagnostic X-ray installations
This appendix presents the methodology of NCRP #49 for determining the shielding necessary in a diagnostic X-ray installation. The required thickness of shielding can be calculated using the formulae contained in this Appendix, in conjunction with Figures 1 to 3 and the answers to the following questions:
- What is the distance between the nearest point of the area to be shielding and the mean operational position of the X-ray tube?
- Is the area to be designated as a controlled or uncontrolled area, i.e., will the area be occupied by radiation workers (subject to the limit of 20 mSv per year) or non-radiation workers (subject to the limit of 1 mSv per year)?
- What will be/is the occupancy factor (T) of the area? The occupancy factor is defined as the time an area is normally occupied, expressed as a fraction of the working week. (If not accurately known, use Table 6 in section B.1.2.3 of this safety code).
- Will the intervening shield between the X-ray tube and the occupied area act as a primary or secondary protective barrier, i.e., will the barrier be required to attenuate the direct useful beam or stray (leakage and scattered) radiation only?
- What will be the use factor (U) of the required protective barrier? The use factor is defined as the fraction of the operational time during which the useful beam will be/is directed at the barrier or area under consideration. (If not accurately known, use Table 7 in section B.1.2.3 of this safety code).
- What will be/is the workload (W) of the X-ray unit? The workload indicates the operational time of an X-ray machine expressed in terms of milliampere-minutes per week.
- What will be/is the maximum and average operating tube potential, and output?
Formulae for calculation of shielding requirements
The thickness of shielding required can be calculated using the formulae given below. This method requires knowing the Workload W, in mA-minutes per week, the use factor U, the occupancy factor T and the distance d, in metres, from the source to the occupied area.
This method involves computation of an average value for the exposure per unit workload at unit distance, K, (in R/mA-min at 1 metre) and then using the curves shown in Figures AIII.1 and AIII.2 and to determine the thickness of lead or concrete required to reduce radiation levels to the required value.
1. Primary protective barriers
For primary protective barriers, the value K can be computed from the following equation:
where

Equation AIII-1: Text Equivalent
The value K is equal to the product of P and d-squared divided by the product of W, U, and T.
- P = maximum permissible weekly exposure expressed in R/week. For controlled areas P = 0.04 R/week; for uncontrolled areas P = 0.002 R/week
- d = distance in metres from the target to the primary area
- W = workload in mA-min/week
- U = use factor
- T = occupancy factor
- K = exposure per unit workload at unit distance, in R/mA-min at 1 metre
Example: Determine the thickness of primary barrier required to protect a controlled area 3 metres from the target of a 150 kVp diagnostic unit having a weekly workload of 2000 mA-min. The wall has a use factor of 1 and the occupancy factor of the area beyond the wall is 1.
For this case,
- P = 0.04 R
- d = 3 m
- W = 2000 mA-min
- U = 1
- T = 1
Using the above equation,
- K = (0.04 × 32)/(2000×1×1)
- = 0.36/2000
- = 0.00018
- = 1.8×10-4
The 150 kVp curves of Figures AIII.1 and AIII.2, respectively show that the required barrier thickness is 2.65 mm of lead or 23.5 cm of concrete.

Figure AIII.1: Attenuation in lead of X-rays from 50 to 150 kVp
The minimum half-value layer of aluminum, measurement without the compression paddle in place, calculated by the equation "HVL (mm of Aluminum) greater than or equal to, X-ray Tube Voltage (kV) divided by 100".

Figure AIII.2: Attenuation in concrete of X-rays generated at 50 to 150 kVp
This graph presents the attenuation of 50, 70, 100, 125 and 150 kVp X-rays as a function of concrete thickness. The vertical axis is logarithmic and represents K, the quotient of exposure at a unit distance and workload in units of Roentgens per milliampere-minute (R per mA-min at 1 metre). The horizontal axis represent the thickness of concrete in centimetres (cm). The graph shows that logarithm of K decreases as the thickness of concrete increases.
2. Secondary protective barriers
Secondary protective barriers are required to provide shielding against both leakage and scattered radiation. Since these two types of radiation are of different qualities, it is necessary to determine the barrier thickness requirements for each separately. If the computed barrier thicknesses for leakage and scatter radiations are about the same, one half-value layer should be added to the larger one to obtain the total secondary barrier thickness. If the computed leakage and scattering thicknesses differ by at least three half-value layers, the larger of the two will be adequate.
2.1 Barrier against leakage radiation
To determine the barrier thickness required to protect against leakage radiation it is necessary to calculate the transmission factor, B, required to reduce the weekly exposure to P. For a diagnostic-type tube housing, where the maximum allowable leakage from the housing is 0.115 roentgen per hour at 1 metre, the transmission factor is given by the following formula:
where

Equation AIII-2: Text Equivalent
The transmission factor is equal to 522 times the product of I, P, and d-squared divided by the product of W and T.
- P = maximum permissible weekly exposure expressed in R/week. For controlled areas P = 0.04 R/week; for uncontrolled areas P = 0.002 R/week
- d = distance in metres from the tube housing to the secondary barrier
- I = tube current in milliamperes
- W = workload in mA-min/week
- T = occupancy factor
Having calculated the transmission factor, B, the barrier thickness, as a number of half-value layers or tenth-value layers, can be determined from Figure AIII.3. The required barrier thickness in millimeters of lead or centimeters of concrete can be obtained from Table AIII.1, for the appropriate energy.
Example: Determine the thickness of barrier required to protect a controlled area 2 metres from the housing of a 100 kVp diagnostic unit having a weekly workload of 2000 mA-min. Assume that the tube operates at 5 mA and that the area in question has an occupancy factor of 1.
For this case,
- P = 0.04 R
- d = 2 m
- W = 2000 mA-min
- T = 1
- I = 5 mA
Using the above equation,
- B = (522×5×0.04×22)/(2000×1)
- = 4176/2000
- = 0.209
From Figure AIII.3, a transmission of 0.209 corresponds to 2.4 HVL's or 0.7 TVL's. From Table AIII.1 the HVL for 100 kVp is 0.27 mm lead or 1.6 cm concrete. Therefore, the required barrier thickness for protection against leakage radiation is
- (2.4 x 0.27) = 0.6 mm lead
- (2.4 x 1.6) = 3.84 cm concrete
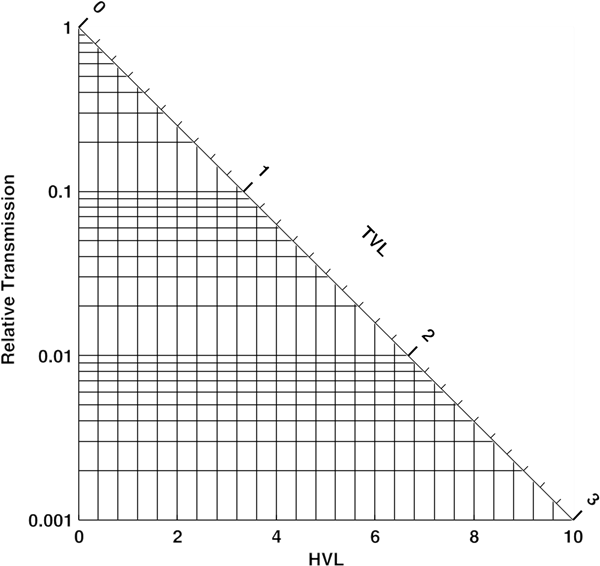
Figure AIII.3: Relationship between the transmission factor B and the number of half-value layers, N, or tenth-value layers, n
This triangular graph presents the relationship between the transmission factor B and the number of half-values, N or tenth-values layers, n of a barrier. The vertical axis is logarithmic and represents the relative transmission factor, B. The horizontal axis represents the number of half-value layers, N. The diagonal axis represents the number of tenth-value layers, n. The graph shows that as the transmission factor increases, the corresponding number of half-value layers or tenth-value layers decrease.
| Tube potential | Attenuation material | |||
|---|---|---|---|---|
| Lead (mm) | Concrete (cm) | |||
| kVp | HVL | TVL | HVL | TVL |
| 50 | 0.06 | 0.17 | 0.43 | 1.5 |
| 70 | 0.17 | 0.52 | 0.84 | 2.8 |
| 85 | 0.22 | 0.73 | 1.25 | 4.5 |
| 100 | 0.27 | 0.88 | 1.60 | 5.3 |
| 125 | 0.28 | 0.93 | 2.00 | 6.6 |
| 150 | 0.30 | 0.99 | 2.24 | 7.4 |
| 200 | 0.52 | 1.70 | 2.50 | 8.4 |
| 250 | 0.88 | 2.90 | 2.80 | 9.4 |
| 300 | 1.47 | 4.80 | 3.10 | 10.4 |
| Thickness | Thickness weight in pounds for 1 square foot section | ||
|---|---|---|---|
| Inches | Millimetre equivalent | Nominal weight | Actual weight |
| 1/64 | 0.40 | 1 | 0.92 |
| 3/128 | 0.60 | 1 1/2 | 1.38 |
| 1/32 | 0.79 | 2 | 1.85 |
| 5/128 | 1.00 | 2 1/2 | 2.31 |
| 3/64 | 1.19 | 3 | 2.76 |
| 7/128 | 1.39 | 3 1/2 | 3.22 |
| - | 1.50 | - | 3.48 |
| 1/16 | 1.58 | 4 | 3.69 |
| 5/64 | 1.98 | 5 | 4.60 |
| 3/32 | 2.38 | 6 | 5.53 |
| - | 2.50 | - | 5.80 |
| - | 3.00 | - | 6.98 |
| 1/8 | 3.17 | 8 | 7.38 |
| 5/32 | 3.97 | 10 | 9.22 |
| 3/16 | 4.76 | 12 | 11.06 |
| 7/32 | 5.55 | 14 | 12.90 |
| 1/4 | 6.35 | 16 | 14.75 |
| 1/3 | 8.47 | 20 | 19.66 |
| 2/5 | 10.76 | 24 | 23.60 |
| 1/2 | 12.70 | 30 | 29.50 |
| 2/3 | 16.93 | 40 | 39.33 |
| 1 | 25.40 | 60 | 59.00 |
Notes:
|
|||
2.2 Barrier against scatter radiation
Scattered radiation has a much lower exposure rate than that of the incident beam and usually is of lower energy. However, for X-ray equipment operating below 500 kVp it is usually assumed that the scattered X-rays have the same barrier penetrating capability as the primary beam. For X-rays generated at kVp's of less than 500 kV, the values for K can be determined from the following formula:

Equation AIII-3: Text Equivalent
The value K is equal to 400 times the product of P, d-squared, and D-squared divided by the product of a, W, T, and F.
where
- K = exposure per unit workload at 1 metre, expressed in R per mA-min at 1 m
- P = maximum permissible weekly exposure rate expressed in R/week. For controlled areas P = 0.04 R/week; for uncontrolled areas P = 0.002 R/week
- d = distance in metres from the target to the scatterer
- D = distance in metres from the scatterer to the secondary barrier
- a = ratio of scattered to incident exposure (tabulated in Table AIII.3)
- W = workload in mA-min/week
- T = occupancy factor
- F = field are in cm2
Having computed K from the above equation, the curves shown in Figures AIII.1 and AIII.2 are then used to determine the thickness of lead or concrete required in the same way as for the primary barrier.
If the barrier thickness for leakage and for scattered radiation differ by at least 1 TVL, the thicker of them will be adequate. If they differ by less than 1 TVL, 1 HVL should be added to the thicker one to obtain the required total secondary barrier thickness.
| Tube potential kVp | Scattering angle (from central axis of beam) | |||||
|---|---|---|---|---|---|---|
| 30o | 45o | 60o | 90o | 120o | 135o | |
| 50 | 0.0005 | 0.0002 | 0.00025 | 0.00035 | 0.0008 | 0.0010 |
| 70 | 0.00065 | 0.00035 | 0.00035 | 0.0005 | 0.0010 | 0.0013 |
| 85 | 0.0012 | 0.0007 | 0.0007 | 0.0009 | 0.0015 | 0.0017 |
| 100 | 0.0015 | 0.0012 | 0.0012 | 0.0013 | 0.0020 | 0.0022 |
| 125 | 0.0018 | 0.0015 | 0.0015 | 0.0015 | 0.0023 | 0.0025 |
| 150 | 0.0020 | 0.0016 | 0.0016 | 0.0016 | 0.0024 | 0.0026 |
| 200 | 0.0024 | 0.0020 | 0.0019 | 0.0019 | 0.0027 | 0.0028 |
| 250 | 0.0025 | 0.0021 | 0.0019 | 0.0019 | 0.0027 | 0.0028 |
| 300 | 0.0026 | 0.0022 | 0.0020 | 0.0019 | 0.0026 | 0.0028 |
Appendix IV: Shielding guides for storage of radiographic film
To reduce the radiation level to the film to 1.75 µGy (0.2 mR) for weekly workloads of:
- 500 mA-sec at 100 kV
- 200 mA-sec at 125 kV
- 100 mA-sec at 150 kV
Table AIV.1 presents the amount of shielding required to reduce radiation level to 1.75 µGy. In general, for most facilities, the storage time for secondary barriers is adequate.
| Distance from X-ray tube to stored film | ||||||||
|---|---|---|---|---|---|---|---|---|
| 2.0 m | 3.0 m | 4.0 m | 5.0 m | |||||
| Lead (mm) | concrete (cm) | Lead (mm) | concrete (cm) | Lead (mm) | concrete (cm) | Lead (mm) | concrete (cm) | |
| Storage time for primary barriers | ||||||||
| 1 day | 1.6 | 15.2 | 1.3 | 12.6 | 1.1 | 10.9 | 1.0 | 9.6 |
| 1 week | 2.3 | 20.4 | 1.9 | 17.9 | 1.7 | 15.9 | 1.5 | 14.5 |
| 1 month | 2.8 | 24.8 | 2.5 | 22.3 | 2.3 | 20.4 | 2.1 | 19.0 |
| 1 year | 3.9 | 33.0 | 3.6 | 30.5 | 3.3 | 28.6 | 3.1 | 27.0 |
| Storage time for secondary barriers | ||||||||
| 1 day | 0.2 | 1.5 | 0.1 | 1.0 | -- | -- | -- | -- |
| 1 week | 0.6 | 5.4 | 0.3 | 2.5 | 0.2 | 1.5 | 0.1 | 1.0 |
| 1 month | 1.0 | 9.6 | 0.7 | 7.1 | 0.5 | 5.4 | 0.4 | 3.7 |
| 1 year | 2.1 | 17.5 | 1.7 | 14.8 | 1.5 | 13.0 | 1.3 | 11.6 |
Appendix V: Federal/provincial/territorial radiation safety agencies
Federal government
Consumer and Clinical Radiation Protection Bureau, Health Canada
(Responsible for the interpretation of safety codes, and administration of Radiation Emitting Devices Act and its Regulations)
E-mail: ccrpb-pcrpcc@hc-sc.gc.ca
Website: https://www.canada.ca/en/health-canada/corporate/contact-us/consumer-clinical-radiation-protection-bureau.html
Medical Devices Directorate, Health Canada
(Responsible for the licensing of medical devices and administration of the Food and Drugs Act and Medical Devices Regulations)
E-mail: mdb_enquiries@hc-sc.gc.ca
Website: https://www.canada.ca/en/health-canada/services/drugs-health-products/medical-devices.html
Labour Program, Employment and Social Development Canada
(Federal Authority responsible for administration of the Canada Labour Code and Canada Occupational Health and Safety Regulations)
Contact: https://www.canada.ca/en/employment-social-development/services/labour-contact.html
Website: https://www.canada.ca/en/services/jobs/workplace/health-safety.html
British Columbia
Senior Manager, Risk Analysis Unit
WorkSafeBC
E-mail: Colin.Murray@worksafebc.com or riskanalysisunit@worksafebc.com
Website: http://worksafebc.com/en
Alberta
OHS Specialized Professional Services
Alberta Jobs, Economy and Trade
E-mail: LBR.RadiationProgram@gov.ab.ca
Website: https://www.alberta.ca/register-radiation-equipment.aspx
Saskatchewan
Manager, Health Standards
Ministry of Labour Relations & Workplace Safety
E-mail: brent.preston@gov.sk.ca
Website: https://www.saskatchewan.ca/business/safety-in-the-workplace/hazards-and-prevention/radiation
Manitoba
Head, Radiation Protection and Imaging Physics
Medical Physics Division
CancerCare Manitoba
E-mail: ifife@cancercare.mb.ca
Website: https://www.cancercare.mb.ca/Research/medical-physics/radiation-protection-services
Ontario (for issues related to patient and public safety)
Manager, Licensing & X-Ray Inspection Services (XRIS)
Long-Term Care Inspections Branch
Ontario Ministry of Health & Long-Term Care
E-mail: Barbara.Parisotto@ontario.ca
Website: http://www.health.gov.on.ca/en/
Ontario (for issues related to worker safety)
Senior Manager, Radiation Protection Services
Occupational Health and Safety Branch
Ministry of Labour, Immigration, Training and Skills Development
E-mail: madelaine.fedorowich@ontario.ca
Website: http://www.labour.gov.on.ca/
Quebec
Conseillère en prévention-inspection
Direction générale de la gouvernance et du conseil stratégique en prévention (DGGCSP)
Commission des normes, de l'équité, de la santé et de la sécurité du travail
E-mail: evelyne.bouvier@cnesst.gouv.qc.ca
Website: https://www.cnesst.gouv.qc.ca/en
New Brunswick
WorkSafeNB
Prevention Division
Manager – Ergonomics & Occupational Hygiene
E-mail: prevention@ws-ts.nb.ca or roberto.sgrosso@ws-ts.nb.ca
Website: https://www.worksafenb.ca/
Nova Scotia
Occupational Health and Safety Engineer
Department of Labour, Skills and Immigration
Toll Free 1-800-952-2687 (24 hrs)
E-mail: colleen.rodgerson@novascotia.ca
Website: https://novascotia.ca/lae/healthandsafety/
Prince Edward Island
Prince Edward Island Provincial Coordinator
Workers Compensation Board of Prince Edward Island
E-mail: kmacneil@wcb.pe.ca or jwhalen@gov.pe.ca
Website: http://www.wcb.pe.ca
Newfoundland and Labrador
Manager, Occupational Health
Occupational Health and Safety Division
E-mail: nwilson@gov.nl.ca
Website: https://www.gov.nl.ca/dgsnl/department/branches/divisions/ohs/
Northwest Territories and Nunavut
Occupational Health and Safety
Government of the Northwest Territories
E-mail: gnwt_ohs@gov.nt.ca
Website: https://my.hr.gov.nt.ca/health-safety
Yukon Territory
Manager, Occupational Hygiene Services
Workers' Safety and Compensation Board
E-mail: robert.rees@wcb.yk.ca
Website: https://www.wcb.yk.ca/
Appendix VI: Facility radiation protection checklist
| Description | Yes / No | Reference Subsection | |||
|---|---|---|---|---|---|
| Personnel Qualifications and Responsibilities | |||||
| Do all personnel possess the required qualifications to carry out all of their responsibilities? | A.1.0 | ||||
| Owner: | A.1.1 | ||||
| Responsible User: | A.1.2 | ||||
| X-ray Equipment Operator: | A.1.3 | ||||
| Medical Physicist/Radiation Safety Officer: | A.1.4 | ||||
| Referring Physician/Practitioner: | A.1.5 | ||||
| Information Systems Specialist: | A.1.6 | ||||
| Repair and Maintenance Personnel: | A.1.7 | ||||
| Procedures for Minimizing Radiation Exposure to Personnel | |||||
| In general, are all required and recommended procedures for minimizing exposures to personnel in place and being followed? | A.2.0 | ||||
Are all personnel who are likely to receive more than 1/20th of the dose to a radiation worker declared radiation workers and monitored with a personal dosimeter? If yes, are the dosimeters: worn properly? read at an appropriate frequency? |
A.2.1 | ||||
| Are personnel exposures within regulatory limits? | A.2.1 | ||||
| Are personal protective equipment available to all staff? | A.2.1 | ||||
Does the facility use mobile equipment? If yes, are the requirements and recommendations of section A.2.2 being followed? |
A.2.2 | ||||
| In general, are all required and recommended procedures for operation of radiographic equipment in place and being followed? | A.2.3 | ||||
When operating radioscopic equipment, are measures taken to protect personnel? Protective clothing worn by staff Minimizing duration of exposures Started Assessment of positioning of personnel during examinations |
A.2.4 | ||||
| Procedures for Minimizing Radiation Exposure to Patients | |||||
| In general, are the guidelines for the prescription of X-ray examinations being followed? | A.3.1 | ||||
| Are medical exposures justified by taking into account the benefits and risks of alternate procedures that do not use ionizing radiation but offer comparable information? | A.3.1 | ||||
| Are previous radiographs or reports consulted prior to prescribing additional radiological examinations? | A.3.1 | ||||
| In general, are the guidelines for radiological examinations of pregnant persons being followed? | A.3.4 | ||||
| Are radiological procedures causing exposure of the abdomen or pelvis of persons who are pregnant avoided unless there are strong clinical reasons for such examinations? | A.3.4 | ||||
| Are radiological procedures causing exposure of the abdomen or pelvis of persons of reproductive capacity planned to deliver the minimum dose to any embryo or foetus? | A.3.4 | ||||
| In general, are all required and recommended procedures for carrying out X-ray examinations in place and being followed? | A.3.2 | ||||
| Are patients treated only when the appropriate prescription is provided by a medical practitioner? | A.3.2.1 | ||||
| Do equipment operators select techniques and loading factors such that their combination produces the minimum patient exposure consistent with acceptable image quality and the clinical purpose of the examination? | A.3.2.1 | ||||
| Is adequate patient shielding available and used where appropriate and practicable? | A.3.2.1 | ||||
| In general, are all required and recommended procedures for carrying out radiographic examinations in place and being followed? | A.3.2.2 | ||||
| For each type of interventional procedure, is there documented information available outlining the radiographic films (projections, number and loading factors), radioscopy time, air kerma rates and resulting cumulative skin doses and skin sites associated with the various part of the interventional procedure? | A.3.2.3 | ||||
| In general, are practices and procedures in place for carrying out CT procedures? | A.3.2.5 | ||||
Are efforts made to reduce the dose to sensitive tissues? Correct collimation of X-ray beam? Attention to X-ray examinations of children and adolescents? Appropriate selection of loading factors and technique? Attention to sensitivity of imaging system? |
A.3.3 | ||||
Have Diagnostic Reference Levels been established and documented? If yes, are the DRLs established using phantoms? Or patients? |
A.3.5 | ||||
| Facility Requirements | |||||
| Is shielding adequate such that the dose rates outside the controlled areas meet the regulatory dose limits for the public? | B.1.1 | ||||
| Are routine measurements of exposure rates in areas adjacent to the radiology rooms made by the staff or qualified experts? | B.1.1 | ||||
| Is there an up-to-date floor plan available containing the information required in subsection B.1.2.1? | B.1.2 | ||||
| Are controlled areas identified by appropriate warning signs? | B1.2.2 | ||||
| Are warning signs in the language(s) of the local population? | B1.2.2 | ||||
| Is access restricted in controlled areas? | B1.2.2 | ||||
| Is adequate information provided to visitors entering controlled areas? | A.2.0 | ||||
| Are the parameters governing structural shielding requirements know and documented for all of the X-ray equipment in the facility? | B.1.2.3 | ||||
| Were the facility layout and construction approved by appropriate regulatory authorities? | B.1.3 | ||||
| Have any modifications been made to the facility? | B.1.3 | ||||
| If modifications have been made to the facility, was a safety assessment performed by a qualified expert prior to the modifications being made? | B.1.3 | ||||
| Were shielding calculations performed by a qualified expert? | B.1.3 | ||||
| Does the facility meet all applicable federal, provincial or territorial regulatory requirements? | B.1.3 | ||||
| Equipment Requirements | |||||
| Does the equipment meet all applicable regulatory requirements? | B.2.1 | ||||
| Was acceptance testing performed on all equipment at time of purchase prior to clinical use? | B.2.2.4 | ||||
| Were results from acceptance testing used to set baseline values and limits on operational performance of the X-ray equipment? | B.2.2.4 | ||||
| Equipment Information | |||||
| Type of X-ray Equipment | Manufacturer | Model Designation | Serial Number | Date of Manufacture | Weekly Workload |
| Equipment Requirements | |||||
At time of purchase, did all new, used and refurbished medical equipment confirmed to meet the: Radiation Emitting Devices Regulations? Medical Devices Regulations? |
B.2.1 | ||||
| Is existing equipment periodically assessed for the possibility of upgrading to improve safety and performance? | B.2.3 | ||||
| Do all equipment meet the necessary construction and performance requirements? | B.2.5 | ||||
| General Requirements | B.2.5.1 | ||||
| Radiographic Equipment | B.2.5.2 | ||||
| Radioscopic Equipment | B.2.5.3 | ||||
| CT Equipment | B.2.5.4 | ||||
| Have the dose and image quality information for CT equipment been obtained from the manufacturer or established by a medical physicist? | B.2.5.5 | ||||
| Image Processing Systems | |||||
| Are the recommendations for film processing systems followed at the facility? | B.3.1 | ||||
| X-ray Film Storage | B.3.1.1 | ||||
| Cassette and Screen Maintenance | B.3.1.2 | ||||
| Darkroom Conditions | B.3.1.3 | ||||
| Film Processing | B.3.1.4 | ||||
| Viewboxes Conditions | B.3.1.5 | ||||
| Is the management of silver containing waste carried out in accordance to provincial and municipal requirements? | B.3.1.4 | ||||
Does the facility perform digital image processing? If yes, what types of digital image acquisition systems are used? CR Systems: DR Systems: |
B.3.2 | ||||
| For the digital imaging systems, is the manufacturer-specified quality control program being followed? | B.3.2 | ||||
Does the facility possess a PACS? If Yes,
|
B.3.2.4 | ||||
| Does the facility perform teleradiology? | B.3.2.6 | ||||
| If yes, does the facility follow the CAR Guidelines for Teleradiology? | B.3.2.6 | ||||
| Radiation Protection Surveys | |||||
| Does the facility undergo Radiation Protection Surveys at regular intervals? | B.5.0 | ||||
| Are copies of past Radiation Protection Survey reports retained and available if needed? | B.5.1 | ||||
| Do survey reports include all of the necessary information? | B.5.2 | ||||
Were there any incidents or accidents at the facility? If yes, were incident and/or accident investigation reports prepared? If yes, were incidents and/or accidents reported to the appropriate federal, provincial or territorial agencies? |
B.5.2 | ||||
| Were safety assessments reviewed or made based on knowledge gained from an incident and/or accident at this facility or other similar facilities? | B.5.2 | ||||
| Quality Assurance Program | |||||
| Is there a documented quality assurance program at this facility? | C.1.0 | ||||
| Are policies and guidelines developed and available? | C.1.3.1 | ||||
| Is the establishment of quality control and administrative procedures documented? | C.1.3.2 C.1.3.3 |
||||
| Is equipment used for quality control testing calibrated? | C.3.0 | ||||
| Is equipment used for daily quality control testing available on-site at the facility? | C.3.0 | ||||
| Are individuals trained in the proper operation of quality control test equipment? | C.3.0 | ||||
| Does the facility quality assurance program include the required tests of this safety code or their equivalent? | |||||
| For Film-based Radiographic Equipment | C.3.1-C.3.6 | ||||
| For Digital Radiographic Equipment | C.3.1-C.3.6 | ||||
| For Radioscopic Equipment | C.3.1-C.3.6 | ||||
| For CT Equipment | C.3.1-C.3.6 | ||||
| Does the facility Quality Assurance program follow the recommended frequency of testing of this safety code? | |||||
| ...for Daily Quality Control Testing | C.3.1 | ||||
| ...for Weekly Quality Control Testing | C.3.2 | ||||
| ...for Monthly Quality Control Testing | C.3.3 | ||||
| ...for Quarterly Quality Control Testing | C.3.4 | ||||
| ...for Semi-Annual Quality Control Testing | C.3.5 | ||||
| ...for Annual Quality Control Testing | C.3.6 | ||||
Appendix VII: Radiation measurement units
Exposure
Following the lead of the International Electrotechnical Commission, the air kerma (in gray, Gy) replaces the exposure (in roentgen, R) as the measure of exposure. The relationship between the two units is as follows:
- 1 Gy ~ 115 R
- 1 mGy ~ 115 mR
- 1 R ~ 8.73 mGy
- 1 mR ~ 8.73 µGy
Absorbed dose
The gray (Gy) replaces the rad (rad) as the unit of absorbed dose. The relationship between the two units is as follows:
- 1 Gy ~ 100 rad
- 1 mGy ~ 100 mrad
- 1 rad ~ 10 mGy
- 1 mrad ~ 10 µGy
Equivalent dose
The sievert (Sv) replaces the rem (rem) as the unit of equivalent dose. The relationship between the two units is as follows:
- 1 Sv ~ 100 rem
- 1 mSv ~ 100 mrem
- 1 rem ~ 10 mSv
- 1 mrem ~ 10 µSv
Note: m = milli = 10-3; µ = micro = 10-6
Acknowledgements
This document reflects the work of many individuals. The 2008 version was prepared and compiled by Mr. Christian Lavoie and Ms. Narine Martel of the Medical X-ray and Mammography Division, Consumer and Clinical Radiation Protection Bureau. Appreciation is expressed to Mr. Yani Picard and other members of the Medical X-ray and Mammography Division for their assistance and advice during the preparation of this code. Revisions published in 2024 were prepared and compiled by Dr. Sarah Cuddy-Walsh, Dr. Narjes Moghadam, and Mr. Richard Smith of the Ionizing and Acoustic Radiation Physical Sciences Division, Consumer and Clinical Radiation Protection Bureau.
The contributions of the following organizations, agencies and associations whose comments and suggestions helped in the preparation of this code are gratefully acknowledged:
Alberta Cancer Board
Alberta College of Medical Diagnostic and Therapeutic Technologists
Alberta Employment, Immigration and Industry
Association des physiciens et ingénieurs biomédicaux du Québec
Association Québécoise des Physicien(ne)s médicaux cliniques
British Columbia Centre for Disease Control
Canadian Association of Medical Radiation Technologists
Canadian Association of Radiologists
Canadian Nuclear Safety Commission
Canadian Organization of Medical Physicists
Cancercare Manitoba
College of Physicians and Surgeons of Alberta
Department of National Defence
Federal Provincial and Territorial Radiation Protection Committee
Hôpital Dr G.-L Dumont, Moncton, New Brunswick
Indigenous Services Canada
Ontario Association of Medical Radiation Technologists
Ontario Safety Association for Community and Healthcare
Queen Elizabeth Hospital, Charlottetown, Prince Edward Island
Saskatchewan Association of Health Organizations
Vancouver General Hospital, British Columbia
WorkSafe BC
Workers' Compensation Board Northwest Territories and Nunavut
References
- Footnote 1
-
AAPM (2002). American Association of Physicists in Medicine. Quality Control in Diagnostic Radiology, AAPM Report No. 74 (Medical Physics Publishing, Madison, Wisconsin).
- Footnote 2
-
AAPM (2005). American Association of Physicists in Medicine. Assessment of Display Performance for Medical Imaging Systems, AAPM On-Line Report No. 03 (American Association of Physicists in Medicine Task Group 18 Imaging Informatics Subcommittee).
- Footnote 3
-
ACOG (2017). American College of Obstetricians and Gynecologists' Committee on Obstetric Practice. Committee opinion no. 723: Guidelines for diagnostic imaging during pregnancy and lactation. Obstet Gynecol. 2017;130(4):933-934.
- Footnote 4
-
ACR (2017). American College of Radiology. ACR-AAPM-SIIM-SPR Practice Parameter for Digital Radiography. Resolution 40.
- Footnote 5
-
Aldrich JE, Bilawich A, Mayo JR. Radiation Doses to Patients Receiving Computed Tomography Examinations in British Columbia. Can Assoc Radiol J 2006; 57(2):79-85.
- Footnote 6
-
CAR (1999). Canadian Association of Radiologists. CAR Standards and Guidelines for Teleradiology.
- Footnote 7
-
Fawcett SL and Barter SJ. The use of gonad shielding in paediatric hip and pelvis radiographs. BJR; 82: 363-370; 2009.
- Footnote 8
-
Frantzen MJ, Robben S, Postma AA, et al. Gonad shielding in paediatric pelvic radiography: disadvantages prevail over benefit. Imaging Insights; 3(1): 23-32; 2012.
- Footnote 9
-
Hart D, Wall BF, Shrimpton PC, Bungay D and Dance DR. 2000 Reference Doses and Patient Size in Paediatric Radiology, NRPBR318 (NRPB, Chilton).
- Footnote 10
-
IAEA (1996). International Atomic Energy Agency. International Basic Safety Standards Protection against Ionizing Radiation and for the Safety of Radiation Sources. Safety Series No. 115 (IAEA, Vienna).
- Footnote 11
-
ICRP (2007). International Commission on Radiological Protection. The 2007 Recommendations of the International Commission on Radiological Protection. ICRP Publication 103, Annals of the ICRP 37 (2-4).
- Footnote 12
-
ICRP (2012). International Commission on Radiological Protection. ICRP Statement on Tissue Reactions / Early and Late Effects of Radiation in Normal Tissues and Organs – Threshold Doses for Tissue Reactions in a Radiation Protection Context. ICRP Publication 118, Annals of the ICRP 41(1/2).
- Footnote 13
-
IEC (1999). International Electrotechnical Commission. Evaluation and routine testing in medical imaging departments – Part 3-1: Acceptance tests – Imaging performance of X-ray equipment for radiographic and radioscopic equipment, 1st, IEC 61223-3-1.
- Footnote 14
-
IEC (2002). International Electrotechnical Commission. Medical Electrical Equipment: Particular Requirements for the Safety of X-ray Equipment for Computed Tomography, 2nd, 1st amendment IEC 60601-2-44.
- Footnote 15
-
IEC (2004). International Electrotechnical Commission. Evaluation and routine testing in medical imaging departments – Part 3-5: Acceptance tests – Imaging performance of computed tomography X-ray equipment, 1st, corrigendum 2006, IEC 61223-3-5.
- Footnote 16
-
IEC (2006). International Electrotechnical Commission. Evaluation and Routine Testing in Medical Imaging Departments – Part 2-6: Constancy tests – Imaging performance of computed tomography X- ray equipment, 2nd, IEC 61223-2-6.
- Footnote 17
-
IEC (2008). International Electrotechnical Commission. Medical electrical equipment – Part 1-3: General requirements for basic safety and essential performance – Collateral Standard: Radiation protection in diagnostic X-ray, 2nd, IEC 60601-1-3.
- Footnote 18
-
IPEM (2004). Institute of Physics and Engineering in Medicine. Guidance on the Establishment and Use of Diagnostic Reference Levels for Medical X-ray Examinations, IPEM Report 88 (Fairmount House, York).
- Footnote 19
-
IPEM(2005). Institute of Physics and Engineering in Medicine. Recommended Standards for Routine Performance Testing of Diagnostic Imaging Equipment, IPEM Report 91 (Fairmount House, York).
- Footnote 20
-
Lee MC, Lloyd J, and Solomito MJ. Poor utility of gonadal shielding for pediatric pelvic radiographs. Orthopedics; 40(4): e623-e627; 2017.
- Footnote 21
-
NCRP (1976). National Council on Radiation Protection and Measurement. Structural Shielding Design and Evaluation for Medical Use of X-rays and Gamma Rays of Energies Up to 10 MeV, NCRP Report No. 49 (National Council on Radiation Protection and Measurements, Bethesda, Maryland).
- Footnote 22
-
NCRP (1988). National Council on Radiation Protection and Measurement. Quality Assurance for Diagnostic Imaging, NCRP Report No. 99 (National Council on Radiation Protection and Measurements, Bethesda, Maryland).
- Footnote 23
-
NCRP (2004). National Council on Radiation Protection and Measurement. Structural Shielding Design for Medical X-ray Imaging Facilities, NCRP Report No. 147 (National Council on Radiation Protection and Measurements, Bethesda, Maryland).
- Footnote 24
-
Radiation Emitting Devices Act, R. S., C.34.
- Footnote 25
-
Radiation Emitting Devices Regulation, C.R.C., c. 1370, s. 3, Part XII Diagnostic X-ray Equipment.
- Footnote 26
-
Shrimpton PC, Hillier MC, Lewis MA, Dunn M. Doses from computed tomography examinations in the UK – 2003 review. Report NRPB – W67. Chilton (UK); NRPB;2004.
- Footnote 27
-
US Code of Federal Regulations 1020.33, Computed Tomography (CT) Regulations, Title 21, Volume 8, Revised as of April 1, 2006.