Fact sheet: 3 Questions to ask yourself that make difficult conversations about serious illness easier
Talking with your patients about their serious illness is not easy
Where do I start? What do I say?
We all have had that uncomfortable feeling of not knowing what to say or when to say it. Regardless of your role, ask yourself these three questions.
1. Is a treatment or care decision needed?
The answer directs you to the purpose and outcomes of the conversation.
If yes, then you are supporting deciding. Make sure illness is understood and decisions align with a person’s values and goals.
If no, then you are helping with preparing. Prepare a patient and substitute decision makers (SDM) for progressing illness and future decision-making.
2. What do they know?
Up to 70% of people do not understand that their serious illness cannot be cured and is progressive over time. Exploring what the person understands about their illness helps you to know how much and what kind of information to offer.
3. What matters to the person?
There is clear evidence that values and goals guide as few as 10% of clinician recommendations. Helping your patient express their values and goals will keep the person at the centre of the decision.
Benefits
When a seriously ill patient and their substitute decision makers (SDM) are prepared, outcomes are better, distress is less and clinicians have greater professional satisfaction.
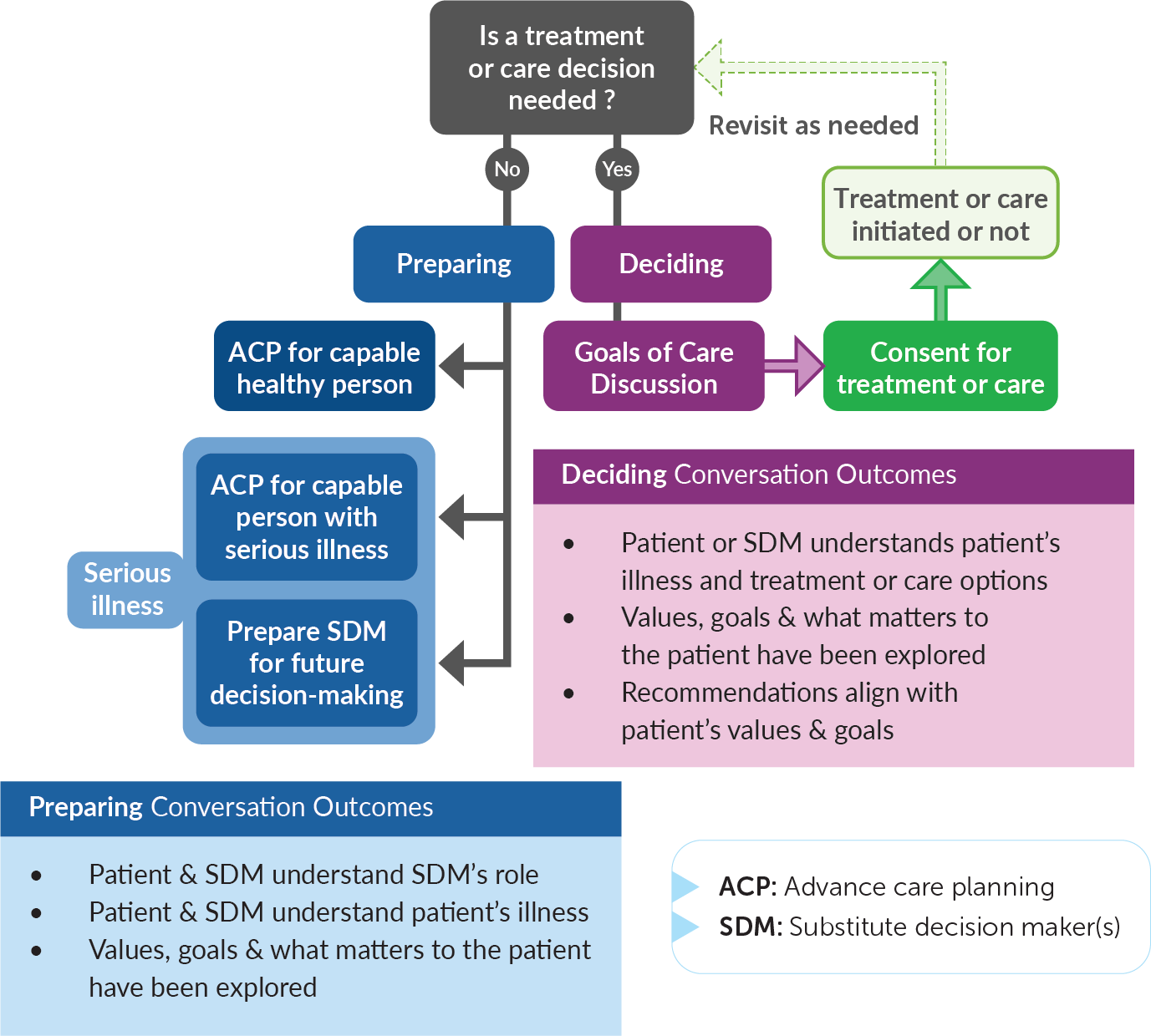
1. Is a treatment or care decision needed?
This algorithm shows how advance care planning (ACP), even for a healthy person, fits in preparing for future health related changes and decision making, as well as the steps required for a treatment or care decision, including goals of care discussions. Below are lists of outcomes for both conversations.
Figure 1. Algorithm – Is a treatment or care decision needed?
Text description
Is treatment or care decision needed?
No
- Preparing
- ACP for capable healthy person
- ACP for capable healthy
- ACP for capable person with serious illness
- Prepare SDM for future decision-making
Yes
- Deciding
- Goals of care discussion
- Consent for treatment or care
- Treatment or care initiated or not
- Revisit Is treatment or care decision needed? as needed
Preparing Conversation Outcomes
- Patient and SDM understand SDM’s role
- Patient and SDM understand patient’s illness
- Values, goals and what matters to the patient have been explored
Deciding Conversation Outcomes
- Patient or SDM understands patient’s illness and treatment or care options
- Values, goals and what matters to the patient have been explored
- Recommendations align with patient’s values and goals
ACP: Advance care planning
SDM: Substitute decision maker(s)
©2022 Dr. Jeff Myers, Dr. Leah Steinberg, Dr. Nadia Incardona, Dr. Jessica Simon & Dr. Justin Sanders. This work is licensed under Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License .
2. What do they know?
Why this is important?
Most Canadians will die from serious illnesses yet most seriously ill people do not appreciate that their illness is progressive and not curable. This means that most of their decisions are inadequately informed. Many clinicians worry that by talking about the illness and its progression, the patient and their SDM will lose hope. Most patients and SDM who have conversations about serious illness however experience less anxiety when they understand their illness and how it will progress.
How to do this?
This is not about teaching a person day-to-day self-management strategies for their illness. This is about the big picture of what to expect. Start by asking: “What do you know or have been told about your illness?” Listen carefully to a person's answer as this will give you a sense of how much and what kind of information to offer. When providing information, share small chunks at a pace that makes sense for the person. Use non-technical language and check that the person understands.
What are the tasks?
When preparing, the tasks are to improve what the patient and substitute decision maker understand about the illness trajectory and what is expected to happen in the future. When deciding, the tasks are to assess for and address any information gaps to ensure the decision is informed.
Preparing
Improve what the patient and SDM understand about the illness trajectory and what is expected to happen in the future.
Figure 2. Graph of the three most common illness trajectories
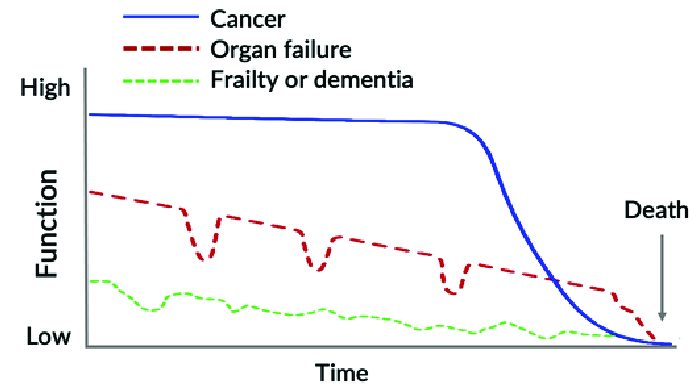
Text description
This figure depicts the three most common illness trajectories represented by horizontal lines on a graph. The top-bottom axis of the graph represents a person’s function, and the left-right axis represents time. The first trajectory is commonly associated with cancer. It shows a relatively horizontal line that represents stability over time. It is followed by a sharp decline, which represents a rapid decrease in function just prior to the dying phase. The second trajectory is commonly associated with organ failure. It has a general slope downwards over time with sporadic episodes of decreased function that returns to near baseline. The third trajectory is commonly associated with frailty or dementia. The line begins at a much lower function level than the other two trajectories. The line is irregularly shaped and has a slow downward slope. This represents inconsistent function levels that is often seen for people with frailty and dementia.
Graph of the three most common illness trajectories. Adapted from Living Well at the End of Life: Adapting Health Care to Serious Chronic Illness in Old Age, J. Lynn and D. Adamson (RAND Health report WP-137, 2003).
Deciding
Assess for and address any information gaps to ensure the decision is informed.
3. What matters to the person?
Why this is important?
Thought Experiment: You were recently diagnosed with a neurodegenerative disorder. You are offered a new medication that halts disease progression for most people. Most however also experience a 30% loss of cognition. Would you take the medication?
The only way you could make a decision for this scenario was to consider and apply what matters to you, or what you value. Ideally, all medical decisions are guided by our patients' own values and goals. Our tasks are to explore these then ensure our recommendations align.
How to do this?
Start by asking, "Given what you know now, when you think about the future, what matters to you? What is most important for us to focus on?”
Remember, the more a person’s values and goals are directly used when decision-making, the more they will feel heard and understood.
What are the tasks?
Preparing
Ensure patients and SDMs have the information that would guide future decision-making. Assist future providers by documenting conversations.
Deciding
Elicit information you can use to determine which treatment or care option to recommend based on how it aligns with the patient’s values and goals.