Canada Health Act Annual Report 2023-2024
Table of contents
- Acknowledgements
- Canada Health Act 2023-2024 year in review infographic
- Road to the Canada Health Act
- Chapter 1 - Canada Health Act overview
- Chapter 2 - Administration and compliance
- Chapter 3 – Provincial and territorial health care insurance plans in 2023-2024
- Annex A - Canada Health Act and Extra-Billing and User Charges Information Regulations
- Annex B - Policy interpretation letters
- Annex C - Financial statements of actual amounts of extra-billing and user charges for the period April 1, 2021 to March 31, 2022
- Annex D - Reimbursement action plans and progress reports
- Contact information
- Endnotes
Acknowledgements
Health Canada would like to acknowledge the work and effort that went into producing this Annual Report. It is through the dedication and timely commitment of the following departments of health and their staff that we are able to bring you this report on the administration and operation of the Canada Health Act:
- Newfoundland and Labrador Department of Health and Community Services
- Prince Edward Island Department of Health and Wellness
- Nova Scotia Department of Health and Wellness
- New Brunswick Department of Health
- Quebec Ministry of Health and Social Services
- Ontario Ministry of Health
- Manitoba Health, Seniors, and Long-Term Care
- Saskatchewan Ministry of Health
- Alberta Ministry of Health
- British Columbia Ministry of Health
- Yukon Department of Health and Social Services
- Northwest Territories Department of Health and Social Services
- Nunavut Department of Health
We also greatly appreciate the extensive work effort that was put into this report by our production team, including desktop publishers, translators, editors and concordance experts, printers and staff of Health Canada.
Canada Health Act 2023-2024 year in review infographic

Figure 1 - Text description
- 2024 marked the 40th anniversary of the passage of the Canada Health Act, which received royal assent on April 17, 1984.
- To ensure the Act keeps pace with evolutions in health care delivery, interpretation letters have been issued on several occasions. Most recently, on January 9, 2025, the new Canada Health Act Services Policy was announced and confirms that patients should not be charged for medically necessary physician-equivalent services when provided by other regulated health professionals, such as nurse practitioners, pharmacists, or midwives. The policy comes into effect on April 1, 2026.
- In 2023-2024, the federal government transferred over $49.4 billion to provinces and territories through the Canada Health Transfer, to support them in delivering publicly funded care.
- In 2023–2024, approximately $1 billion was reciprocally billed for insured hospital and physician services provided to residents outside their home jurisdiction, through reciprocal billing agreements in place between the provinces and territories.
- In March 2024, $79.4 million in Canada Health Transfer deductions were levied, including:
- $72.4 million under the Diagnostic Services Policy to NS, NB, QC, MB, SK, AB, and BC for patient charges for medically necessary diagnostic services.
- $6.99 million to NL, NB, ON, and BC for patient charges for other medically necessary surgical services such as abortions, cataract and other day-surgery procedures.
- Based on actions taken to ensure patients do not face charges for medically necessary services, in March 2024, more than $90 million was reimbursed to provinces. More than $175 million has been reimbursed to provinces since
Road to the Canada Health Act
“I came to believe that health services ought not to have a price tag on them, and that people should be able to get whatever health services they required irrespective of their individual capacity to pay.”
- Tommy Douglas, Premier of Saskatchewan 1944-1961, who introduced North America’s first single-payor universal health care program.
Canada's public health insurance system has developed over more than 60 years, shaped by key legislative changes and shifting public expectations. The roots trace back to the introduction of the Hospital Insurance and Diagnostic Services Act (HIDSA) in 1957, which built on the work of Tommy Douglas, widely known as the father of Medicare in Canada, who established universal hospital coverage in Saskatchewan in 1947. The HIDSA created a 50-50 cost-sharing model to encourage provinces and territories (PTs) to establish comprehensive and universal coverage for hospital services. This was followed by the Medical Care Act (MCA) in 1966, which followed a similar approach, encouraging PTs to provide universal coverage for physician services. Under the HIDSA, patient user charges were deducted from payments made by the federal government; however, under the MCA, there was no equivalent reduction for extra-billing by physicians. These cost-sharing agreements helped fund hospital and physician services until the late 1970s.
In 1977, the Federal-Provincial Fiscal Arrangements and Established Programs Financing Act (EPF) changed the way the federal government provided health care funding to the PTs. Under the EPF, the former 50-50 cost-sharing agreements were replaced with a fixed federal per capita contribution. The move to block funding removed the federal government's capacity to withhold partial sums from transfer amounts to PTs that allowed user charges. As a result, the federal government could only transfer the full amount of the block funding or withhold it all, making it harder to enforce compliance and prevent patient charges.
During this time, many provinces started introducing hospital user fees, justifying the charges by claiming that health care funding had been reduced. Some provinces also cited the income from extra-billing during physician payment negotiations to rationalise lower settlements. Consequently, extra-billing was occurring in most provinces during this time, with hospital user charges occurring in six provinces.
In 1979, Justice Emmett Hall, who had previously reviewed Canada's health care system in 1964, was once again tasked by the federal government to assess the state of Canada's publicly funded health insurance programs. His final report, released in 1980, called for a renewed commitment to the principles of Medicare, and warned that extra-billing by doctors and hospital user fees were creating a two-tiered system, undermining universal access to care.
“As a society, we are aware that the trauma of illness, the pain of surgery, the slow decline to death, are burdens enough for the human being to bear without the added burden of medical or hospital bills penalizing the patient at the moment of vulnerability. The Canadian people determined that they should band together to pay medical bills and hospital bills when they were well and income earning. Health services were no longer items to be bought off the shelf and paid for at the checkout stand. Nor was their price to be bargained for at the time they are sought. They were a fundamental need, like education, which Canadians could meet collectively and pay for through taxes.”
- Justice Emmett Hall, excerpted from “Canada’s National-Provincial Health Program for the 1980’s: A Commitment for Renewal”.
Building on Justice Hall's conclusions, a Parliamentary task force on the Federal-Provincial Fiscal Arrangements recommended in 1981 that the federal government combine the HIDSA and MCA into a single program supported by clear criteria that could be monitored and enforced. The task force also recommended that the Minister of National Health and Welfare report annually to Parliament on whether these criteria were being met, including details of any penalties levied against PTs that failed to fully comply. These recommendations were later implemented with the passage of the Canada Health Act.
At the May 1982 meeting of federal, provincial and territorial health ministers, Monique Bégin, the Minister of National Health and Welfare, announced the government's plan to replace the HIDSA and MCA with the Canada Health Act. In her introductory remarks, Minister Bégin stated the proposals put forward as components of the Canada Health Act were meant "to protect, renew and improve our excellent system of health care. They are based on the fundamental principles that the cost of adequate health care should be borne by all Canadians rather than by the sick and that the best possible health care system can only be achieved by all of us working cooperatively to solve problems before they become insoluble and to protect a program at a time when it is vulnerable."
The new Act would combine the four key principles from the previous legislation (public administration, universality, comprehensiveness, portability) and add a fifth condition, accessibility, distinguishing the concept of "universality" from "accessibility", while adding measures to ensure these principles were respected. In her opening statement from the meeting, she emphasized the ministers' pride in Canada's health care system and their commitment to ensuring access for all, recognizing the importance of controlling patient charges to ensure that accessibility.
In order to gain public support for the new legislation and counter negative media campaigns and statements from some medical groups and provincial officials, who saw extra-billing and user charges as legitimate revenue streams, the federal government distributed more than 300,000 copies of "Preserving Universal Medicare: A Government of Canada Position Paper" in July 1983. The paper explained the government's position on Medicare's future, stressing that extra-billing and user charges were a serious threat to the universal access that Medicare was meant to guarantee. The release of the paper sparked significant public engagement, with over 100 meetings held across the country to discuss its contents.
“It is apparent that unless a concerted effort is made to commit ourselves once more to the principles of universal health insurance, the gaps in insurance cover will continue to grow. A choice must now be made. Do we as a nation wish to allow an increasing number of out fellow Canadians to fall through the widening cracks in our health insurance program? Or do we wish in stead to preserve and improve Medicare?”
- Excerpted from “Preserving Universal Medicare – A Government of Canada Position Paper.”
On December 12, 1983, Bill C-3, an Act relating to cash contributions by Canada in respect of insured health services provided under provincial health care insurance plans and amounts payable by Canada in respect of extended health care services and to amend and repeal certain Acts in consequence thereof, which would later be more commonly known as the Canada Health Act, was given first reading in the House of Commons.
“Thanks to Medicare, no one need worry about any financial burden resulting from an unforeseen illness. Since health insurance is a collective program, all Canadians share the cost of medical care for which they could not pay individually…This program is not only for the young, the wealthy and the healthy. It is designed also to help the poor, the old and the chronically ill. The latter group is the one most affected by the charging of direct fees.”
- Senator Jacques Hébert, excerpted from the debate on the enactment of the Canada Health Act, April 11, 1984.
After the Bill's second reading, it was sent to the Standing Committee on Health, Welfare, and Social Affairs for review. Over 130 witnesses appeared before the Committee, which met 17 times between January and March 1984. The Committee submitted its report to the House of Commons on March 21, 1984, and, after several more days of debate, Bill C-3 passed unanimously on April 9, 1984. The Bill was then sent to the Senate and received royal assent on April 17, 1984.
Chapter 1 - Canada Health Act overview
This chapter describes the evolution of Medicare in Canada, as well as the Canada Health Act, its key definitions, requirements, regulations, penalty provisions, and excluded persons and services under the Act. It also outlines interpretation letters from former federal Ministers of Health sent to their provincial and territorial counterparts, all of which followed months of consultation:
- the Honourable Jake Epp provided guidance on the interpretation and implementation of the Act;
- the Honourable Diane Marleau announced the Federal Policy on Private Clinics;
- the Honourable Ginette Petitpas Taylor announced three new Canada Health Act initiatives - the Diagnostic Services Policy, the Reimbursement Policy, and strengthened Canada Health Act reporting; and
- the Honourable Mark Holland announced the Canada Health Act Services Policy.
The evolution of Medicare in Canada
Canada's single-payor public health care insurance system, "Medicare", is financed through a progressive tax system, which allows risks to be pooled and costs to be shared by all Canadians. Our health care insurance system evolved into its present form over more than six decades. Saskatchewan was the first province to establish universal, public hospital insurance in 1947 and, 10 years later, the Government of Canada passed the Hospital Insurance and Diagnostic Services Act (HIDSA), to encourage provinces and territories to provide universal coverage for these services by sharing in their costs. Its unanimous adoption by the federal Parliament launched the largest single program ever undertaken in peace-time Canada and, by 1961, all the provinces and territories had public insurance plans that provided universal access to hospital services. Saskatchewan again pioneered by providing insurance for physician services, beginning in 1962. The Government of Canada enacted the Medical Care Act in 1966, to encourage provinces and territories to provide universal coverage for physician services by sharing in their costs. By 1972, all provincial and territorial insurance plans had been expanded to include physician services.
In 1979, at the request of the federal government, Justice Emmett Hall undertook a review of the state of health services in Canada. In his report, he affirmed that health care services in Canada ranked among the best in the world but warned that extra-billing by doctors and user charges levied by hospitals were creating a two-tiered system that threatened the universal accessibility of care. This report, and the national debate it generated, led to the enactment of the Canada Health Act.
Did You Know?
The Canada Health Act was enacted expressly to protect patients from charges when they access medically necessary physician and hospital services. While the Act has remained largely unchanged over the last four decades, the federal government has issued several policy interpretation letters to ensure the Act's application keeps pace with new circumstances as health care delivery evolves. A description of the four policy interpretation letters issued to date, with the most recent being issued in January 2025, can be found later in this chapter. Copies of these letters can also be found in Annex B of this report.
Passed unanimously in the House of Commons in 1984, the Canada Health Act, Canada's federal health care insurance legislation, codified the national principles which underpin federal funding for hospital and physician services and added prohibitions on the patient charges which threatened to undermine universal access to care.
In Canada, the roles and responsibilities for health are shared between the federal, provincial and territorial governments. The provincial and territorial governments have primary jurisdiction in health care administration and delivery. This includes setting their own priorities, administering their health care budgets and managing their own resources. The federal government, under the Canada Health Act, defines the national principles that are to be reflected in provincial and territorial health care insurance plans.
What is the Canada Health Act?
The Act establishes criteria and conditions related to insured health services and extended health care services that the provinces and territories must fulfill to receive the full federal cash contribution under the Canada Health Transfer (CHT). In fiscal year 2023–2024, the federal government transferred $49,421,000,000 to provinces and territories to support their health care systems. Additional information on federal, provincial and territorial funding arrangements is available by visiting the Department of Finance's website. The aim of the Act is to ensure that all eligible residents of Canadian provinces and territories have reasonable access to medically necessary hospital, physician, and surgical-dental services that require a hospital setting, on a prepaid basis, without charges related to the provision of insured health services.
A copy of the Act is provided in Annex A.
Budget 2024 re-confirmed the federal government's plan, Working Together to Improve Health Care for Canadians, to invest $200 billion to support the health and well-being of Canadians, which includes $25 billion over 10 years in targeted funding through bilateral agreements with provinces and territories to improve access to family health and mental health and substance use services, support the health workforce and modernize health systems. The bilateral agreements also include $9.5 billion for addressing home care, mental health, personal support workers and long-term care.
By March 2024, all provinces and territories had signed their bilateral agreements with the federal government, anchored in fundamental principles, including a mutual commitment to upholding the Canada Health Act. These agreements marked a significant investment in ensuring equitable access to health care services across Canada, fostering collaboration between federal and provincial and territorial authorities to address systemic challenges and enhance health care delivery.
Key definitions under the Canada Health Act (Section 2)
Insured health services are medically necessary hospital, physician and surgical-dental services (performed by a dentist in a hospital, where a hospital is required for the proper performance of the procedures) provided to insured persons, unless those services are provided under another Act of Parliament, or provincial or territorial workers' compensation legislation.
Extended health care services are certain aspects of long-term residential care (nursing home intermediate care and adult residential care services), and the health aspects of home care and ambulatory care services.
Insured persons are eligible residents of a province or territory. A resident of a province is defined in the Act as "… a person lawfully entitled to be or to remain in Canada who makes his home and is ordinarily present in the province, but does not include a tourist, a transient or a visitor to the province…"
Insured hospital services include medically necessary in-patient and out-patient services such as accommodation and meals at the standard or public ward level and preferred accommodation if medically required; nursing services; laboratory, radiological and other diagnostic procedures, together with the necessary interpretations; drugs, biologicals and related preparations when administered in the hospital; use of operating room, case room and anesthetic facilities, including necessary equipment and supplies; medical and surgical equipment and supplies; use of radiotherapy facilities; use of physiotherapy facilities; and services provided by persons who receive remuneration therefor from the hospital.
Insured physician services are medically required services rendered by medical practitioners. Medically required physician services are generally determined by the provincial or territorial health care insurance plan, in consultation with the medical profession.
Insured surgical-dental services are services provided by a dentist in a hospital, where a hospital setting is required for the proper performance of the procedure.
Health care practitioner is a person lawfully entitled under the law of a province to provide health services in the place in which the services are provided by that person.
The Canada Health Act infographic
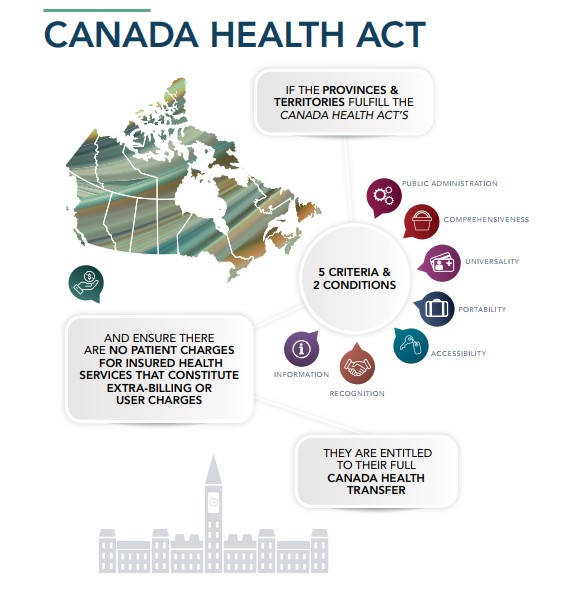
Figure 2 - Text description
If the provinces and territories fulfil the Canada Health Act's 5 criteria and 2 conditions:
- Public administration
- Comprehensiveness
- Universality
- Portability
- Accessibility
- Recognition
- Information
And ensure there are no patient charges for insured health services that constitute extra-billing or user charges they are entitled to their full Canada Health Transfer.
Requirements of the Canada Health Act
The Canada Health Act contains nine requirements that the provinces and territories must fulfill in order to qualify for the full amount of their cash entitlement under the CHT.
They are:
- five program criteria that apply only to insured health services;
- two conditions that apply to insured health services and extended health care services; and
- two provisions, with respect to extra-billing and user charges, that apply only to insured health
The criteria
1.0 Public administration (Section 8)
The public administration criterion of the Canada Health Act requires provincial and territorial health care insurance plans to be administered and operated on a non-profit basis by a public authority, which is accountable to the provincial or territorial government for decision-making on benefit levels and services, and whose records and accounts are publicly audited. However, the criterion does not prevent the public authority from contracting out the services necessary for the administration of the provincial and territorial health care insurance plans, such as the processing of payments to medical practitioners for insured health services.
The public administration criterion pertains only to the administration of provincial and territorial health care insurance plans and does not preclude private facilities or providers from supplying insured health services as long as no insured person is charged in relation to the provision of these insured health services.
2.0 Comprehensiveness (Section 9)
The comprehensiveness criterion requires that the health care insurance plan of a province or territory must cover all insured health services provided by hospitals, physicians or dentists (i.e., surgical-dental services that require a hospital setting).
3.0 Universality (Section 10)
Under the universality criterion, all insured residents of a province or territory must be entitled to the insured health services provided by the provincial or territorial health care insurance plan on uniform terms and conditions. Provinces and territories generally require that residents register with the plan to establish entitlement.
4.0 Portability (Section 11)
Residents moving from one province or territory to another must continue to be covered for health care services insured by the home jurisdiction during any waiting period imposed by the new province or territory of residence (up to three months), before coverage is established in the new jurisdiction. It is the responsibility of residents to inform their province or territory's health care insurance plan that they are leaving and to register with the health care insurance plan of their new province or territory, in order to avoid any gaps in coverage.
Residents who are temporarily absent from their home province or territory, or from Canada, must continue to be covered for insured health services by their home province or territory. If insured persons are temporarily absent in another province or territory, the portability criterion requires that insured health services be paid at the host province's rate. Refer to the Interprovincial Health Insurance Agreement Coordinating Committee section in Chater 2 for additional information on how in-Canada portability is facilitated by the provinces and territories. If insured persons are temporarily out of the country, insured health services are to be paid at the home province's rate. Insured residents must apply to their home provincial or territorial health care insurance plan in order to obtain reimbursement for any insured health services outside Canada.
The portability criterion is intended to permit a person to receive medically necessary services in relation to an urgent or emergent need, when absent on a temporary basis (e.g., business or vacation) but does not entitle residents to seek services or shorter waits for non-urgent or emergent services.
Prior approval by the health care insurance plan in a person's home province or territory may be required before coverage is extended for elective (non-emergency) services to a resident while temporarily absent from their province or territory.
5.0 Accessibility (Section 12)
The intent of the accessibility criterion is to ensure that insured persons in a province or territory have reasonable access to insured hospital, physician, and surgical-dental services that require a hospital setting, on uniform terms and conditions. Access to insured health services should be unimpeded, either directly or indirectly, by charges (extra-billing or user charges) or other means (e.g., discrimination on the basis of age, race, health status, or financial circumstances).
In addition, the health care insurance plan of the province or territory must provide:
- reasonable compensation to physicians and dentists for all the insured health services they provide; and
- payment to hospitals to cover the cost of insured health services.
The conditions
1.0 Information (Section 13[A])
Provincial and territorial governments are required to provide information to the federal Minister of Health as prescribed by regulations under the Act.
2.0 Recognition (Section 13[B])
Provincial and territorial governments are required to recognize the federal financial contributions toward both insured and extended health care services.
The provisions
Extra-Billing and User Charges
The provisions of the Canada Health Act pertaining to extra-billing and user charges for insured health services in a province or territory are outlined in sections 18 to 21. If it can be confirmed that either extra-billing or user charges exist in a province or territory, a mandatory dollar-for-dollar deduction from the CHT payments to that province or territory is required under the Act.
Extra-Billing (Section 18)
Under the Act, extra-billing is defined as a charge by an enrolled medical practitioner or dentist (i.e., a dentist providing insured surgical-dental services when a hospital setting is medically required) to an insured person for an insured health service, which is charged in addition to the amount paid by the provincial or territorial health care insurance plan. For example, if an enrolled physician were to charge a patient any amount for an office visit that is insured by the provincial or territorial health care insurance plan, the amount charged would constitute extra-billing. Extra-billing is seen as a barrier for people seeking medical care, and is contrary to the accessibility criterion.
User Charges (Section 19)
A user charge is defined as any charge for an insured health service, other than extra-billing. This includes any charge levied for insured hospital services, or any non-physician related services provided in conjunction with an insured physician service at a non-hospital facility (e.g., private practice). In other words, if patients were charged a fee as a condition of receiving insured health services, that fee would be considered a user charge. User charges are not permitted under the Act because, as is the case with extra-billing, they constitute a barrier to access.
What is a patient charge?
- If an enrolled medical practitioner or dentist…
- Charges an insured resident…
- For an insured health service…
- An amount in addition to the amount paid by the provincial or territorial health care insurance plan that…is extra-billing.
- Other charges (e.g., for supplies) related to the provision of insured health services…are user charges.
Other elements of the Act
Regulations (Section 22)
Section 22 of the Canada Health Act enables the federal government to make regulations for administering the Act in the following areas:
- defining the services included in the Act's definition of "extended health care services," e.g., nursing home care or home care;
- prescribing which services are excluded from hospital services;
- prescribing the types of information that the federal Minister of Health may reasonably require, as well as the format and submission deadline for the information; and
- prescribing how provinces and territories are required to recognize the CHT in their documents, advertising or promotional materials.
To date, the only regulations in force under the Act are the Extra-billing and User Charges Information Regulations. These Regulations require the provinces and territories to report annually to Health Canada on the amounts of extra-billing and user charges levied. A copy of these Regulations is provided in Annex A.
Penalty provisions of the Canada Health Act
Mandatory Penalty Provisions
Under the Act, provinces and territories that allow extra-billing and user charges are subject to mandatory dollar-for-dollar deductions from the federal transfer payments under the CHT. For example, if it is determined that any amount of extra-billing by physicians has occurred in a province or territory, the federal cash contribution to that province or territory will be reduced by that same amount. Although deductions are usually based on information provided by the province or territory in accordance with the Extra-billing and User Charges Information Regulations, where information is not provided, or is incomplete, Health Canada will make an estimate of the amount of extra-billing and user charges. This process requires consultation with the province or territory concerned. Deductions based on estimates have been made on numerous occasions.
Provincial and territorial financial statements of extra-billing and user charges received during the reporting period are provided in Annex C.
Discretionary Penalty Provisions
Non-compliance with one of the five criteria or two conditions of the Act is subject to a discretionary penalty. The amount of any deduction from CHT payments is based on the magnitude of the non- compliance, and is approved by Cabinet.
The Canada Health Act sets out a consultation process that must be undertaken with the province or territory before discretionary penalties can be levied. To date, the discretionary penalty provisions of the Act have not been used.
Excluded services and persons
Although the Canada Health Act requires that insured health services be provided to insured persons in a manner that is consistent with the criteria and conditions set out in the Act, not all health care services or Canadian residents fall under the scope of the Act.
Excluded services
A number of services provided by hospitals and physicians are not considered medically necessary, and, thus, are not insured under provincial and territorial health care insurance legislation. Uninsured hospital services for which patients may be charged include preferred hospital accommodation (unless prescribed by a physician or when standard ward level accommodation is unavailable), private duty nursing services, parking, and the provision of telephones and televisions. Uninsured physician services for which patients may be charged include telephone advice (unless it is insured by the provincial or territorial health care insurance plan); the provision of medical certificates (e.g., for work, school, insurance purposes); the transfer of medical records; testimony in court; and cosmetic services. Amounts for these services are governed by provincial and territorial Colleges of Physicians, which generally require that charges be reasonable and reflect the cost of services provided.
The definition of "insured health services" excludes services provided to persons under any other Act of Parliament (e.g., certain services provided to veterans) or under the workers' compensation legislation of a province or territory.
In addition to the medically necessary hospital and physician services covered by the Canada Health Act, provinces and territories also provide a wide range of other programs and services, such as prescription drug coverage, non-surgical dental care, ambulance services and optometric services, at their discretion and on their own terms and conditions. These services are often targeted to specific population groups (e.g., seniors, children, and those receiving social assistance), with levels of funding and scope of coverage varying from one province or territory to another.
Excluded persons
The Canada Health Act definition of "insured person" excludes members of the Canadian Armed Forces and persons serving a term of imprisonment within a federal penitentiary. The Government of Canada provides coverage to these groups through separate federal programs.
The exclusion of these persons from insured health service coverage predates the adoption of the Act and is not intended to constitute differences in access to publicly insured health care.
Policy interpretation letters
There are four key policy statements that clarify the federal position on the Canada Health Act. These statements were made in the form of ministerial letters from former federal Ministers of Health to their provincial and territorial counterparts, following months of consultation. Copies of the letters are provided in Annex B of this report.
Epp Letter
In June 1985, approximately one year following the passage of the Canada Health Act in Parliament, former federal Minister of Health and Welfare Jake Epp wrote to his provincial and territorial counterparts to set out and confirm the federal position on the interpretation and implementation of the Act. The letter sets forth statements of federal policy intent that clarify the Act's criteria, conditions and regulatory provisions. The letter highlighted the fundamental change signified by the Canada Health Act, which was the prohibition of all patient charges for insured health services provided to insured residents. The Epp letter remains an important reference for assessing and interpreting compliance with the Act.
Marleau Letter—Federal Policy on Private Clinics
Between February and December of 1994, a series of seven federal, provincial and territorial meetings dealing wholly, or in part, with private clinics took place. At issue was the growth of private clinics providing medically necessary services funded partially by the public system and partially by patients, and their impact on Canada's universal, publicly funded health care system.
At the September 1994 federal, provincial and territorial meeting of Health Ministers in Halifax, all Ministers of Health present, with the exception of Alberta's Health Minister, agreed to "…take whatever steps were required to regulate the development of private clinics in Canada."
Diane Marleau, the federal Minister of Health at the time, wrote to all provincial and territorial Ministers of Health on January 6, 1995, to announce the new Federal Policy on Private Clinics. The Minister's letter provided the federal interpretation of the Canada Health Act as it relates to the issue of facility fees charged directly to patients receiving medically necessary services at private clinics. The letter stated that the definition of hospital contained in the Act includes any facility that provides acute, rehabilitative or chronic care. Thus, when a provincial or territorial health care insurance plan pays the physician fee for a medically necessary service delivered at a private clinic, it must also pay the facility fee or face a deduction from federal transfer payments.
Petitpas Taylor Letter
On August 8, 2018, the former federal Minister of Health, Ginette Petitpas Taylor, wrote to her provincial and territorial counterparts formalizing three new Canada Health Act initiatives – the Diagnostic Services Policy, the Reimbursement Policy, and strengthened Canada Health Act reporting. These initiatives were the subject of discussions between federal, provincial and territorial officials and adjustments were made to the requirements of these initiatives based on feedback received from the provinces and territories.
Diagnostic Services Policy
The Diagnostic Services Policy came into effect on April 1, 2020. This policy is a formalization of the application of the Canada Health Act to diagnostic services. It confirms the longstanding federal position that medically necessary services, including diagnostic services, are insured regardless of the venue where the services are delivered. Under this policy, provinces and territories first reported on patient charges for medically necessary diagnostic services in December 2022 (for any patient charges which occurred during 2020–2021), and these reports were published in the 2022-2023 Canada Health Act Annual Report.
Did You Know?
Since April 1, 2020, any patient charges for medically necessary diagnostic imaging services, such as MRI or CT scans, regardless of where these services are provided (i.e., hospital or private facility), have been considered contrary to the Canada Health Act. If you believe you have been charged inappropriately, you may report these charges to your provincial or territorial health ministry, using the phone numbers provided inside the back cover of this report. You may also contact the Canada Health Act Division of Health Canada at the following coordinates:
Reimbursement Policy
Should a province or territory be subject to a mandatory deduction, the federal Minister of Health has the discretion to provide a reimbursement if the province or territory eliminates the patient charges that led to the deductions within a specified timeframe. The first deductions eligible for reimbursement under the policy were those taken in March 2018.
Strengthened Canada Health Act Reporting
The aim of strengthened Canada Health Act reporting is to ensure Health Canada has the information required to accurately assess compliance with the Act, as well as to increase transparency for Parliament and Canadians on the administration of the Act, and the state of the publicly funded health care insurance system.
Holland Letter - Canada Health Act Services Policy
Following over two years of engagement with provinces and territories, on January 9, 2025, former federal Minister of Health, Mark Holland wrote to his provincial and territorial counterparts, outlining the new Canada Health Act Services Policy, reaffirming the federal government's commitment to protecting the publicly funded health care system and ensuring that all Canadians benefit from innovations in health care delivery without being burdened by patient charges to access these services.
The Canada Health Act Services Policy clarifies the federal position that anyone with a valid health card should not pay for medically necessary services which would be covered by their provincial or territorial health care plan, if provided by a physician. The intention of the policy is to ensure that the hospital and physician services that were insured when the Canada Health Act was enacted in 1984, remain insured in the future, as the health care system evolves.
To give provinces and territories time to consider how best to integrate these services into their health care insurance plans, the policy will come into effect on April 1, 2026.
Once implemented, the provinces and territories will be required to report patient charges related to physician-equivalent services for the first time in December 2028, and if any deductions are required, the first deductions under the policy will be taken in March 2029. These deductions will be eligible for reimbursement under the Canada Health Act Reimbursement Policy provided the province or territory implicated takes steps to eliminate the patient charges and the circumstances that led to them within two years after the deduction occurred.
Did You Know?
Nurse practitioners (NPs) are advanced practice nurses who integrate clinical skills associated with nursing and medicine to independently assess, diagnose, treat and manage a wide range of health conditions in a variety of health care settings, including hospitals, community and continuing care settings. While NP scopes of practice vary across Canada, many provinces and territories are increasingly integrating nurse practitioners into their health care systems as a means of improving access to primary care services overall.
Canada Health Act mythbusters
Myth: All health care in Canada must be publicly delivered.
Fact: The Canada Health Act doesn't forbid the provision of health services by private companies, as long as residents are not charged for insured health services. In fact, many aspects of health care in Canada are delivered privately. Family physicians mostly bill the provincial or territorial health care insurance plan as private contractors. Hospitals are often incorporated private foundations, and many aspects of hospital care (e.g., lab services, housekeeping, and linens) are carried out privately. Lastly, in many provinces and territories, private facilities are contracted to provide services under the health care insurance plan.
Myth: Health care in Canada is free.
Fact: While you may not have to pay upfront when you receive medically necessary services, health care in Canada is not free. Health care in Canada is funded through tax revenues at the provincial, territorial, and federal levels. By spreading the cost of health care across the entire population, everyone is assured of the care they need, without the great financial burden that medical expenses could pose to a family or individual.
If you believe you have been subject to inappropriate patient charges for insured health services please contact your respective province or territory using the information contained in the Contact Information section of the report, or by contacting the Canada Health Act Division at medicare.spb.chad-dlcs.dgps.assurance.maladie@hc-sc.gc.ca.
Myth: I can use my health insurance card to find a shorter waitlist in another province or territory.
Fact: Your health insurance card does not entitle you to seek out shorter waitlists in other provinces or territories. Although you are covered for insured health services during temporary absences from your home province or territory, prior approval may be required before coverage can be used for non-emergency services in another province or territory.
Myth: I'm a Canadian so I am automatically entitled to health care coverage.
Fact: Having Canadian citizenship does not entitle you to health care coverage, rather you must be an eligible resident within a province or territory. Canadians have their part to play in establishing and maintaining their health care coverage. In all provinces and territories, you are required to register for coverage, and then maintain your eligibility by renewing your coverage, and remaining in your home province or territory for a prescribed number of days each year. Although allowance is often made if you leave your home province or territory for school, work, or other reasons, it is important to inform your provincial or territorial health care insurance plan when you will be away for extended periods, and to understand what your responsibilities are in maintaining your coverage.
Myth: My specific medical condition is covered under the Canada Health Act.
Fact: The Canada Health Act is quite a short piece of legislation and lays out standards at a very high level. Specific medical conditions are not named under the Act; rather, it requires provincial and territorial health care insurance plans to cover medically necessary hospital and physician services. Given their role in health care delivery, the decision over which services to cover is made by the province or territory, in consultation with the medical profession.
Myth: I don't need travel insurance within Canada because I'm covered under Medicare.
Fact: This is a very common misconception, and one that could be quite costly under certain circumstances. Medicare ensures that if you leave your province or territory for a few hours, days or weeks, you will still have coverage for emergency medical services. The same is true during moves to other provinces or territories. However, the hospital and physician services covered under the Canada Health Act are not the only services you might need while outside your usual province or territory. Some services that are not covered by the Act (e.g., prescription drug coverage or ambulance services) are highly subsidized for residents, but not for visitors, which is why you should ensure you have adequate coverage whenever you travel or move within the country.
Chapter 2 - Administration and compliance
Administration
In administering the Canada Health Act, the federal Minister of Health (the Minister) is assisted by Health Canada staff and by the Department of Justice.
The Canada Health Act Division
The Canada Health Act Division of Health Canada is responsible for supporting the Minister in the administration of the Canada Health Act. Members of the Division fulfill the following ongoing functions:
- monitoring and analysing provincial and territorial health care insurance plans for compliance with the criteria, conditions, and extra-billing and user charges provisions of the Act;
- conducting issue analysis and policy research to provide strategic advice;
- asking provincial and territorial health ministries to investigate and provide information and clarification when possible compliance issues arise, and, when necessary, recommending corrective action to them in order to ensure the criteria, conditions, and extra-billing and user charges provisions of the Act are upheld;
- informing the federal Minister of Health of possible non-compliance and recommending appropriate action to resolve the issue;
- managing the annual extra-billing and user charges and reimbursement reporting processes;
- disseminating information on the Act and its administration;
- responding to enquiries about the Act and health care insurance issues received by telephone, mail and the Internet, from the public, members of Parliament, federal government departments, other governments, stakeholder organizations and the media;
- developing and maintaining relationships, with health officials in provincial and territorial governments, for information sharing;
- collaborating with provincial and territorial health department representatives through the Interprovincial Health Insurance Agreements Coordinating Committee;
- working with Health Canada Legal Services and Justice Canada on litigation issues that implicate the Act; and
- producing the Canada Health Act Annual Report on the administration and operation of the Act.
Canada Health Act compliance
The Canada Health Act Division monitors the operations of provincial and territorial health care insurance plans in order to provide advice to the Minister on possible non-compliance with the Canada Health Act. Sources for this information include: provincial and territorial government officials and publications; nongovernmental organizations; media reports; and correspondence received from the public.
Staff in the Canada Health Act Division assess issues of concern and complaints on a case-by-case basis. The assessment process involves compiling all facts and information related to the issue and taking appropriate action. Verifying the facts with provincial and territorial health officials sometimes reveals issues that are not directly related to the Act, while others may pertain to the Act but are a result of misunderstanding or miscommunication, such as eligibility for health care insurance coverage and portability of insured health services within and outside Canada. In these instances, matters are generally resolved quickly with provincial or territorial assistance.
In instances where a Canada Health Act issue has been identified and remains after initial enquiries, Division officials ask the jurisdiction in question to investigate the matter and report back. Division staff discuss the issue and its possible resolution with provincial or territorial officials. Only if the issue is not resolved to the satisfaction of the Division after following the aforementioned steps, is it brought to the attention of the federal Minister of Health.
Deductions and reimbursements under the Act
For the most part, provincial and territorial health care insurance plans meet, and often exceed, the requirements of the Canada Health Act. However, some issues and concerns remain. The most prominent of these relate to accessibility issues, and specifically patient charges for medically necessary health and diagnostic services at private clinics.
Diagnostic Services Policy
On April 1, 2020, the Canada Health Act Diagnostic Services Policy (DSP) came into effect. The policy formalized the federal government's longstanding position that all medically necessary physician and hospital services, including diagnostic services, must be covered by provincial and territorial health care insurance plans, regardless of the venue in which they are delivered. The first deductions under the DSP were taken in March 2023. This was the second year provinces and territories were expected to report on these charges, with associated deductions taken in March 2024. These reports, which were submitted to Health Canada in December 2023, pertained to patient charges for diagnostic services that occurred in fiscal year 2021-2022, and can be found in Annex B.
Both Manitoba and British Columbia reported patient charge amounts to Health Canada. In instances where provinces did not report on these charges, estimates of their magnitude were developed using data from the Canadian Agency for Drugs and Technologies in Health's report on private imaging facilities. These estimates were shared with provinces before deductions were taken to give them an opportunity to provide province-specific data. Saskatchewan subsequently provided province-specific data, which was used to inform Health Canada's estimate.
In March 2024, Nova Scotia, New Brunswick, Quebec, Saskatchewan, Manitoba, Alberta and British Columbia, were subject to mandatory dollar-for-dollar deductions, totalling approximately $72.4 million as a result of patient charges for medically necessary diagnostic services. Mandatory deductions under the DSP will continue as long as patients continue to face charges for these services.
Under the Canada Health Act Reimbursement Policy, mandatory Canada Health Transfer (CHT) deductions may be reimbursed to provinces or territories if they implement a Reimbursement Action Plan (RAP) to eliminate the patient charges in question and rectify the circumstances that led to them, within two years of the date of the deduction. Through this process, reimbursements totalling $83,208,629 were provided to Quebec, Manitoba, Alberta and British Columbia as a result of implementing elements in their respective RAPs to improve access and eliminate patient charges for medically necessary diagnostic services.
Quebec, Alberta, and British Columbia received partial reimbursements of past deductions, in recognition of progress made in eliminating patient charges, whereas Manitoba received full reimbursement for successfully implementing their RAP to eliminate these charges. A copy of these RAPs, as well as the current RAP status updates on their implementation, are presented in Annex D of this report.
| Deduction | Reimbursement | |
|---|---|---|
| Nova Scotia | $1,794,635 | - |
| New Brunswick | $1,794,635 | - |
| Quebec | $36,014,132 | $46,728,814Footnote 1 |
| Manitoba | $650 | $354,477Footnote 2 |
| Saskatchewan | $1,084,513 | - |
| Alberta | $20,450,175 | $20,537,796Footnote 3 |
| British Columbia | $11,270,216 | $15,587,542Footnote 4 |
| TOTALS | $72,408,956 | $83,208,629 |
|
||
Other patient charges for medically necessary health services
Newfoundland and Labrador
Based on amounts reported by Newfoundland and Labrador to Health Canada, a deduction of $1,255 was levied against the province's CHT payment in March 2024 in respect of patient charges for insured cataract surgery that occurred in fiscal year 2021–2022. Since 2018, when this issue was first identified, the province has implemented regulatory and policy measures, detailed in its RAP and subsequent status updates, that strengthen its prohibitions against patient charges for insured cataract procedures. Due to the retrospective nature of reporting under the Canada Health Act, and Newfoundland and Labrador's ongoing investigation of patient complaints, the province has continued to identify and report instances of patient charges to Health Canada when they occur. In recognition of the successful implementation of its RAP, and ongoing compliance with the reporting requirements under the Reimbursement Policy, Newfoundland and Labrador qualified for an immediate full reimbursement of $1,255 to offset its March 2024 CHT deduction. Health Canada continues to monitor this issue to ensure continued compliance. A copy of Newfoundland and Labrador's RAP as well the January 2025 status update on its implementation are presented in Annex D of this report.
New Brunswick
During the reporting period, surgical abortion services in New Brunswick were insured under the provincial health care insurance plan but only covered if performed in hospital; procedures provided in a private clinic in Fredericton, which closed in February 2024, were not covered. Prior to the clinic's closing, Health Canada had raised this issue with New Brunswick at the officials' level and Ministerial levels.
Although the province's financial statement of extra-billing and user charges for 2021-2022 indicated a nil amount, there was evidence of ongoing patient charges and Health Canada used data published by the Canadian Institute for Health Information to estimate patient charges for medically necessary surgical abortion services in the amount of $109,275. Since 2020, deductions totalling $444,041 have been levied against New Brunswick's CHT payments in respect of patient charges to access to abortion services. Though the private clinic in New Brunswick is now closed, the retrospective nature of reporting under the Canada Health Act means New Brunswick will face additional CHT deductions for patient charges for medically necessary surgical abortion services levied in 2022-2023 and 2023-2024.
As described in New Brunswick's Reimbursement Action Plan, which can be found in Annex D of this report, this issue has now been resolved and will be reported on in more detail in next year's report.
Ontario
While the Ontario Health Insurance Plan provides coverage for physicians' fees related to abortion services in all settings, including private clinics, during the 2021-2022 reporting period the province only covered facility fees in the four private abortion clinics licensed as Independent Health Facilities (IHF) under the Independent Health Facilities Act (IHFA). In some instances, this led to other clinics charging patients out-of-pocket to access abortion services. Based on amounts reported by Ontario to Health Canada, a deduction of $32,800 was levied against the province's CHT payment in March 2024 in respect of patient charges to access insured abortion services that occurred in fiscal year 2021–2022. At the same time, in recognition of actions taken to eliminate these patient charges, including the introduction of new legislation in 2023, as discussed below, Ontario received partial reimbursement of its March 2022 ($6,560), March 2023 ($32,800), and March 2024 ($32,800) deductions, for a total reimbursement of $43,296.
As reported in its February 2024 Reimbursement Action Plan update, on September 25, 2023, Ontario proclaimed the Integrated Community Health Services Centre Act (ICHSCA), which replaces the IHFA and provides a new framework for the delivery of insured health services in private clinics. The IHSCA maintains the previous legislation's prohibitions on charging facility fees related to the provision of insured health services, while adding prohibitions on refusing access to insured services, or providing preferential access to insured services, based on an insured resident's choice to pay or not pay for an uninsured service. Health Canada continues to engage with Ontario to encourage the province to fulfil the commitment made in its RAP as work is on-going to establish regulations under the new legislation, which is expected to eliminate these patient charges. A copy of Ontario's RAP as well the February 2024 status update on its implementation are presented in Annex D of this report.
British Columbia
Based on amounts reported by British Columbia to Health Canada, a deduction of $6,848,505 was levied against the province's CHT payment in March 2024 for patient charges levied for medically necessary surgical services in fiscal year 2021–2022.
In recognition of the significant strides British Columbia has made in successfully implementing elements of its RAP, to greatly reduce patient charges for medically necessary surgical services, Health Canada authorized a reimbursement of $6,818,207 in March 2024. This represents a partial reimbursement of British Columbia's March 2022, 2023, and 2024 deductions. A copy of British Columbia's RAP and January 2025 status update on its implementation are presented in Annex D of this report.
| Province | Deductions for Diagnostic Services | Deductions for Surgical Services | Deduction Total | Reimbursement Total |
|---|---|---|---|---|
| NL | - | $1,255 | $1,255 | $1,255 |
| NS | $1,794,635 | - | $1,794,635 | - |
| NB | $1,794,635 | $109,275 | $1,903,910 | - |
| QC | $36,014,132 | - | $36,014,132 | $46,728,814 |
| ON | - | $32,800 | $32,800 | $43,296 |
| MB | $650 | - | $650 | $354,477 |
| SK | $1,084,513 | - | $1,084,513 | - |
| AB | $20,450,175 | - | $20,450,175 | $20,538,796 |
| BC | $11,270,216 | $6,848,505 | $18,118,721 | $22,405,749Footnote * |
| Total | $72,408,956 | $6,991,835 | $79,400,791 | $90,072,387 |
Footnotes
|
||||
Additional compliance issues
Enrollment and membership fees at private primary care clinics
Private primary care clinics that charge patients annual membership fees continue to be an issue of concern under the Canada Health Act. In many cases, these clinics provide their members with access to a mix of insured primary care services and uninsured health services (e.g., massage therapy and nutritional services). Typically, the clinics claim that the fees cover a basket of non-insured health services; however, in some cases these fees are also mandatory to access insured health services at the clinic.
When Health Canada becomes aware of such charges, the Department recommends the provinces and territories work with the clinics in question to make clear to insured residents that access to insured health services is not contingent or preferential based on the payment of annual fees for uninsured health services, which may also involve an investigation or audit of the billing practices of the clinic. When investigations or audits occur, Health Canada requests information about the findings and next steps to ensure any inappropriate patients charges have been eliminated. Health Canada also advises that these provinces and territories develop legislation that is clear about patients' access to insured health services and which prohibits out-of-pocket charges to patients.
In 2023, Health Canada reached out to Alberta following media reports of a primary care clinic that appeared to be charging patients for expedited access to insured physician services. Alberta responded that they were in the process of investigating all clinics that had a membership component to their services, including the clinic identified by Health Canada. The province subsequently identified 41 primary care clinics that advertise membership fees to access a mix of insured and uninsured services, and undertook an analysis of seven randomly selected clinics to gain an understanding of their business models and how they operate. While preliminary results of this review found that the membership fees were only to access uninsured services, Alberta informed Health Canada that an audit would be required to ensure these clinics are not operating in contravention of the Canada Health Act. Alberta is currently evaluating next steps concerning all identified membership clinics and Health Canada continues to monitor this issue.
Since 2023, British Columbia has pursued injunctions against two membership-based primary care providers for operating in non-compliance with British Columbia's legislation. Following prolonged consultations, the providers in question changed their business models to come into compliance, prompting British Columbia to drop the respective injunctions. British Columbia continues to monitor the activities of membership-based primary care providers in the province and provides regular updates to Health Canada.
Portability
Physician services received by Quebec residents when out-of-province are not reimbursed at host province rates, which is a requirement of the portability criterion of the Canada Health Act.
For all jurisdictions, except Prince Edward Island and the three territories, the per diem rates for out-of-country hospital services appear lower than home province or territory rates, which is contrary to the requirement of the portability criterion of the Act. These concerns have been raised with the implicated provinces, and Health Canada continues to monitor the issue.
History of deductions, refunds, and reimbursements under the Canada Health Act
The Canada Health Act, which came into force April 17, 1984, reaffirmed the national commitment to the original principles of the Canadian health care system, as embodied in the previous legislation, the Medical Care Act and the Hospital Insurance and Diagnostic Services Act. By putting into place mandatory dollar-for-dollar penalties for extra-billing and user charges, the federal government took steps to eliminate the proliferation of direct charges for hospital and physician services, judged to be restricting the access of many Canadians to health care services due to financial considerations.
Canada Health Act compliance from 1984–1987
During the period 1984 to 1987, subsection 20(5) of the Act provided for deductions in respect of these charges to be refunded to the province if the charges were eliminated before April 1, 1987.
By March 31, 1987, it was determined that all provinces in which patients had been subject to extra-billing and user charges had taken appropriate steps to eliminate them. Accordingly, by June 1987, a total of $244,732,000 in deductions was refunded to New Brunswick, Quebec, Ontario, Manitoba, Saskatchewan, Alberta, and British Columbia.
| PTs | 1984-1985 | 1985-1986 | 1986-1987 | Total |
|---|---|---|---|---|
| NB | $3,078,000 | $3,306,000 | $502,000 | $6,886,000 |
| QC | $7,893,000 | $6,139,000 | - | $14,032,000 |
| ON | $39,996,000 | $53,328,000 | $13,332,000 | $106,656,000 |
| MB | $810,000 | $460,000 | - | $1,270,000 |
| SK | $1,451,000 | $656,000 | - | $2,107,000 |
| AB | $9,936,000 | $11,856,000 | $7,240,000 | $29,032,000 |
| BC | $22,797,000 | $30,620,000 | $31,332,000 | $84,749,000 |
| TOTAL | $85,961,000 | $106,365,000 | $52,406,000 | $244,732,000 |
In the first three years after the enactment of the Canada Health Act, almost $245 million in deductions were taken against federal health transfers to provinces; these deductions were refunded when the provinces effectively eliminated the patient charges that led to them.
Canada Health Act compliance from 1987–2018, by province
Following the Act's initial three-year transition period, during which refunds to provinces and territories for deductions were possible, penalties under the Act did not reoccur until fiscal year 1994–1995. See the chart later in this chapter for penalties occurring from fiscal years 1994–1995 to 2016-2017.
Federal policy on private clinics
In January 1995, federal Minister of Health, the Honourable Diane Marleau, expressed concerns to her provincial and territorial colleagues about the development of two-tiered health care and the emergence of private clinics charging facility fees for medically necessary surgical services. As part of her communication with the provinces and territories, Minister Marleau announced that the provinces and territories would be given more than nine months to eliminate these user charges, but that any province that did not, would face financial penalties under the Act. Accordingly, beginning in November 1995, deductions have been applied to the cash contributions of provinces for noncompliance with the Federal Policy on Private Clinics, which has implicated Newfoundland and Labrador, Nova Scotia, Manitoba, Alberta, and British Columbia, as described below. In addition to deductions taken under the Federal Policy on Private Clinics, Newfoundland and Labrador, Nova Scotia, Quebec, and British Columbia have also taken deductions with respect to physician extra-billing, which is also described below.
Under the Canada Health Act, the term "hospital" includes more than just buildings with a big "H" on them.
Under the 1995 Federal Policy on Private Clinics, the Honourable Diane Marleau, the federal Minister of Health at the time, clarified that the definition of "hospital" set out in the Canada Health Act includes any facility that provides acute, rehabilitative, or chronic care. As such, a hospital also covers health care facilities, such as clinics.
Newfoundland and Labrador
A total of $280,430 was deducted from Newfoundland and Labrador's cash contribution due to facility fees in a private abortion clinic, before these fees were eliminated, effective January 1, 1998.
A deduction of $1,100 was taken from the March 2005 CHT payment to Newfoundland and Labrador as a result of patient charges for an MRI scan in a hospital which occurred during 2002–2003.
From March 2011 to March 2013, deductions totaling $102,249 were taken from CHT payments to Newfoundland and Labrador for extra-billing and user charges, based on charges reported by the province to Health Canada. These charges resulted from services provided by an opted-out dental surgeon who has since left the province.
Nova Scotia
Before it closed in November 2003, deductions totaling $372,135 were made to Nova Scotia's Canada Health and Social Transfer cash contribution for its failure to cover facility charges to patients, while paying the physician fee, at a Halifax clinic. A final deduction of $5,463 was taken from the March 2005 CHT payment to Nova Scotia as a reconciliation of deductions that had already been taken for 2002–2003. A one-time positive adjustment in the amount of $8,121 was made to Nova Scotia's March 2006 CHT payment to reconcile amounts actually charged in respect of extra-billing and user charges with the penalties that had already been levied based on provincial estimates reported for fiscal 2003–2004.
The March 2007 CHT payment to Nova Scotia was reduced by $9,460 in respect of extra-billing during fiscal year 2004–2005. This amount was reported to Health Canada by the province based on the findings of an audit, concluded in 2006, of the billing practices of a Nova Scotia physician.
Quebec
In March 2017, on the basis of amounts of extra-billing and user charges reported by the Quebec Auditor General with respect to accessory fees charged in 2014–2015, the federal Minister estimated a deduction amount of $9,907,229. In light of corrective action the provincial government had already taken to eliminate accessory fees in January 2017, that amount was subsequently returned to Quebec by the Government of Canada.
In March 2018, using the amount of extra-billing and user charges reported by the Quebec Auditor General with respect to accessory fees charged in 2014–2015 as a proxy, the federal Minister estimated a deduction amount of $9,907,229. In light of the legislative changes the provincial government had already implemented to eliminate and prohibit the continuation of accessory fees in January 2017, this amount was subsequently returned to Quebec by the Government of Canada. This reimbursement pre-dated the Reimbursement Policy. Quebec's March 2017 and March 2018 deductions, which, due to reporting timelines under the Act, were taken after patient charges had already been eliminated by the provincial government, served as the inspiration for the Reimbursement Policy.
Manitoba
From November 1995 to December 1998, deductions totaling $2,055,000 were taken due to user charges anticipated by the province at surgical and ophthalmology clinics. However, during fiscal year 2001–2002, a monthly deduction (from October 2001 to March 2002, inclusively) in the amount of $50,033.50 was levied against Manitoba's Canada Health Social Transfer cash contribution on the basis of a financial statement provided by the province. The statement showed that actual amounts charged with respect to user charges for insured health services in fiscal years 1997–1998 and 1998–1999 were greater than the deductions levied on the basis of estimates. This brought total deductions levied against Manitoba to $2,355,201.
Alberta
Deductions of $3,585,000 were made, from November 1995 until June 1996, to Alberta's cash contribution in respect of facility fees charged at clinics providing surgical, ophthalmological and abortion services. On October 1, 1996, Alberta prohibited private surgical clinics from charging patients a facility fee for medically necessary services for which the physician fee was billed to the provincial health care insurance plan.
British Columbia
In the early 1990s, as a result of a dispute between the British Columbia Medical Association and the British Columbia government over compensation, several doctors opted out of the provincial health care insurance plan and began billing their patients directly. Some of these doctors billed their patients at a rate greater than the amount the patients could recover from the provincial health care insurance plan.
This higher amount constituted extra-billing under the Act. Deductions began in May 1994, relating to fiscal year 1992–1993, and continued until extra-billing by physicians was banned when changes to British Columbia's Medicare Protection Act came into effect in September 1995. In total, $2,025,000 was deducted from British Columbia's cash contribution for extra-billing that occurred in the province between 1992–1993 and 1995–1996.
In January 2003, British Columbia provided a financial statement in accordance with the Canada Health Act Extra-billing and User Charges Information Regulations indicating aggregate amounts actually charged with respect to extra-billing and user charges in private surgical clinics during fiscal year 2000–2001, totaling $4,610. Accordingly, a deduction of $4,610 was made to the March 2003 CHST cash contribution.
In 2004, British Columbia did not report to Health Canada the amounts of extra-billing and user charges actually charged during fiscal year 2001–2002. As a result of reports that British Columbia was investigating 55 cases of user charges, a $126,775 deduction was taken from British Columbia's March 2004 CHST payment, based on the amount the federal Minister estimated to have been charged during fiscal year 2001–2002.
Between 2002 and 2017, deductions totaling $1,773,183 were taken from British Columbia's Canada Health Transfer payments in light of patient charges reported by the province to Health Canada. The deduction taken to British Columbia's federal health transfers in March 2013, in respect of fiscal year 2010–2011, was estimated by the federal Minister of Health and represents the aggregate of the amounts reported to Health Canada by British Columbia and those reported publicly as the result of an audit performed by the Medical Services Commission of British Columbia. This methodology was used until fiscal year 2016–2017.
Following collaborative work with Health Canada on an audit project to determine the extent and scope of patient charges in the province, a deduction of $15,861,818 was taken in March 2018 in respect of patient charges during fiscal year 2015–2016. This deduction reflected British Columbia's private clinic audit results, patient complaints, and publicly available evidence of $4.7 million of patient charges to insured residents by enrolled physicians at the Cambie Surgery Centre.
Since the passage of the Act, from April 1984 to March 2024, deductions totaling $276,868,026 have been taken from transfer payments in respect of the extra-billing and user charges provisions of the Act. This amount excludes deductions totaling $244,732,000 that were made between 1984 and 1987, and subsequently refunded to the provinces when extra-billing and user charges were eliminated.
| NL | PE | NS | NB | QC | ON | MB | SK | AB | BC | YT | NT | NU | Total | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1994/95 | - | - | - | - | - | - | - | - | - | $1,982,000 | - | - | - | $1,982,000 |
| 1995/96 | $46,000 | - | $32,000 | - | - | - | $269,000 | - | $2,319,000 | $43,000 | - | - | - | $2,709,000 |
| 1996/97 | $96,000 | - | $72,000 | - | - | - | $588,000 | - | $1,266,000 | - | - | - | - | $2,022,000 |
| 1997/98 | $128,000 | - | $57,000 | - | - | - | $586,000 | - | - | - | - | - | - | $771,000 |
| 1998/99 | $53,000 | - | $38,950 | - | - | - | $612,000 | - | - | - | - | - | - | $703,950 |
| 1999/00 | ($42,570) | - | $61,110 | - | - | - | - | - | - | - | - | - | - | $18,540 |
| 2000/01 | - | - | $57,804 | - | - | - | - | - | - | - | - | - | - | $57,804 |
| 2001/02 | - | - | $35,100 | - | - | - | $300,201 | - | - | - | - | - | - | $335,301 |
| 2002/03 | - | - | $11,052 | - | - | - | - | - | - | $4,610 | - | - | - | $15,662 |
| 2003/04 | - | - | $7,119 | - | - | - | - | - | - | $126,775 | - | - | - | $133,894 |
| 2004/05 | $1,100 | - | $5,463 | - | - | - | - | - | - | $72,464 | - | - | - | $79,027 |
| 2005/06 | - | - | ($8,121) | - | - | - | - | - | - | $29,019 | - | - | - | $20,898 |
| 2006/07 | - | - | $9,460 | - | - | - | - | - | - | $114,850 | - | - | - | $124,310 |
| 2007/08 | - | - | - | - | - | - | - | - | - | $42,113 | - | - | - | $42,113 |
| 2008/09 | - | - | - | - | - | - | - | - | - | $66,195 | - | - | - | $66,195 |
| 2009/10 | - | - | - | - | - | - | - | - | - | $73,925 | - | - | - | $73,925 |
| 2010/11 | $3,577 | - | - | - | - | - | - | - | - | $75,136 | - | - | - | $78,713 |
| 2011/12 | $58,679 | - | - | - | - | - | - | - | - | $33,219 | - | - | - | $91,898 |
| 2012/13 | $50,758 | - | - | - | - | - | - | - | - | $280,019 | - | - | - | $330,777 |
| 2013/14 | ($10,765) | - | - | - | - | - | - | - | - | $224,568 | - | - | - | $213,803 |
| 2014/15 | - | - | - | - | - | - | - | - | - | $241,637 | - | - | - | $241,637 |
| 2015/16 | - | - | - | - | - | - | - | - | - | $204,145 | - | - | - | $204,145 |
| 2016/17 | - | - | - | - | $9,907,229Footnote 1 | - | - | - | - | $184,508 | - | - | - | $10,091,737 |
| 2017/18 | - | - | - | - | $9,907,229Footnote 1 | - | - | - | - | $15,861,818 | - | - | - | $25,769,047 |
| TOTAL: | $383,779 | - | $378,937 | - | $19,814,458Footnote 1 | - | $2,355,201 | - | $3,585,000 | $19,660,001 | - | - | - | 46,177,376 |
Footnotes
|
||||||||||||||
Understanding this chart
The first deductions under the Act were taken during the first three years after the Act's passage and were subsequently refunded. They are described earlier in this chapter and listed in a chart. There were no deductions taken between fiscal year 1987–1988 and 1993–1994.
To date, most deductions have been based on statements of actual extra-billing and user charges, meaning they are made two years after the extra-billing and user charges occurred (for example, deductions taken in fiscal year 2016–2017 would be in respect of patient charges levied in 2014–2015).
In instances where provinces and territories estimate anticipated amounts of extra-billing and user charges for the upcoming year, a deduction was taken in respect of those charges in the fiscal year for which they are estimated.
In addition to forming the basis for most deductions under the Act, the statements of actual extra-billing and user charges provide an opportunity to reconcile any estimated charges with those that actually occurred. These reconciliations form the basis for further modifications to provincial and territorial cash transfers.
Canada Health Act compliance from 2019−present, by province
Reimbursement Policy and Diagnostic Services Policy
As described earlier, two policies were announced in the Petitpas Taylor interpretation letter: the Canada Health Act Reimbursement Policy and the Diagnostic Services Policy (DSP).
The Reimbursement Policy was created to provide a positive incentive for provinces and territories to come into compliance, should they be subject to mandatory penalties as a result of patient charges for insured health services. Since April 1, 2018, the federal Minister of Health has had the discretion to authorise a reimbursement if the province or territory eliminates those charges, and the underlying circumstances which led to the charges, within a specified timeframe. The first deductions eligible for reimbursement under the policy were those taken in March 2018 and since then $175,010,504 in deductions have been reimbursed to provinces as a result of their efforts to eliminate patient charges and the circumstances that led to them.
The DSP, which took effect on April 1, 2020, formalized the longstanding federal position that patient charges for medically necessary diagnostic services are considered extra-billing or user charges under the Act. The policy clarifies that these services are insured, regardless of the venue in which they are delivered, and evidence of patient charges will result in mandatory dollar-for-dollar deductions from provincial and territorial Canada Health Transfer (CHT) payments.
This report marks the second year of deductions taken under the DSP.
Newfoundland and Labrador
In March 2019, a deduction of $1,349 was taken from CHT payments to Newfoundland and Labrador for patient charges for insured cataract surgeries provided at a private ophthalmological clinic that occurred in 2016-2017, based on amounts reported by the province to Health Canada. Similarly, a deduction of $70,819 was taken in March 2020, $4,521 in March 2021, $1,723 in March 2022 and $1,255 in March 2024 in respect of charges for cataract surgeries during 2017-2018, 2018-2019, 2019-2020, and 2021-2022, respectively.
After its March 2019 deduction, Newfoundland and Labrador consulted with Health Canada on a Reimbursement Action Plan (RAP) to eliminate these patient charges. Given the province successfully carried out that plan to eliminated these charges, the province qualified for full reimbursement of its March 2019 deduction, as well as for immediate and full reimbursements of its March 2020, 2021, 2022, and 2024 deductions. Health Canada continues to monitor this issue to ensure ongoing compliance.
Nova Scotia
In March 2023 and March 2024, Nova Scotia was subject to deductions under the DSP, based on estimates made by Health Canada in the amounts of $1,277,659 and $1,794,635, respectively. These deductions were the result of patient charges for medically necessary diagnostic services that occurred in 2020-2021 and 2021-2022, respectively.
As described in Nova Scotia's Reimbursement Action Plan, which can be found in Annex D of this report, the circumstances that led to these deductions have now been addressed, and will be reported on in more detail in next year's report.
New Brunswick
Since March 2020, deductions totaling $444,041 have been taken from New Brunswick's CHT payments for patient charges to access insured abortion services. These deductions include $140,216 taken in March 2020, $64,850 taken in March 2021, March 2022 and March 2023, and $109,275 taken in March 2024, for patient charges that occurred in 2017-2018, 2018-2019, 2019-2020, 2020-2021, and 2021-2022, respectively. The deduction amounts were estimated by Health Canada based on patient charges reported by Clinic 554, the private clinic where the patient charges were occurring, and data published by the Canadian Institute for Health Information. Though Clinic 554 closed in February 2024, the retrospective nature of reporting under the Canada Health Act means that New Brunswick will still face CHT deductions for patient charges that were levied in 2022-2023 and 2023-2024. As described in New Brunswick's Reimbursement Action Plan, which can be found in Annex D of this report, this issue has now been resolved and will be reported on in more detail in next year's report.
In March 2023 and March 2024, New Brunswick was subject to deductions under the DSP, based on estimates made by Health Canada in the amounts of $1,277,659 and $1,794,635, respectively. These deductions were the result of patient charges for medically necessary diagnostic services that occurred in 2020-2021 and 2021-2022, respectively.
As of this reporting period, New Brunswick has not qualified for reimbursement as a result of failing to meet the reporting requirements of the Reimbursement Policy, which include the creation of a RAP, and the accurate reporting of patient charges to Health Canada on an annual basis. However, New Brunswick's March 2024 deduction remains eligible for full reimbursement until March 2026.
Quebec
A deduction of $8,256,024 was taken to Quebec's March 2019 federal health transfer, reflecting patient charges which had occurred prior to the corrective legislative action taken by Quebec to eliminate these charges and was immediately reimbursed. This reimbursement was the first made under the Reimbursement Policy.
In March 2023 and March 2024, Quebec was subject to deductions under the DSP, based on estimates made by Health Canada in the amounts of $41,867,224 and $36,014,132, in respect of patient charges for medically necessary diagnostic services that occurred in 2020-2021 and 2021-2022, respectively. In March 2024, Quebec received a partial reimbursement of its March 2023 and March 2024 CHT deductions totaling $46,728,814, based on the implementation of elements of the province's RAP to improve access and eliminate patient charges, including the introduction of new legislation to reorganize Quebec's health care system, which is expected to improve access to all insured health services.
Ontario
Since March 2021, deductions totaling $86,065 have been taken from Ontario's CHT payments for patient charges to access insured abortion services. These deductions, which are based on amounts of patient charges reported by Ontario to Health Canada, include $13,905 taken in March 2021, $6,560 taken in March 2022, and $32,800 taken in March 2023 and March 2024, for patient charges that occurred in 2018-2019, 2019-2020, 2020-2021 and 2021-2022, respectively. The patient charges represent overhead costs charged to patients seeking abortion services at clinics that did not receive funding under Ontario's Independent Health Facilities Act (IHFA). The IHFA was replaced by new legislation in 2023 (Integrated Community Health Services Centre Act (ICHSCA)), which is expected to eliminate these patient charges. In March 2024, Ontario received a partial reimbursement of its March 2022, March 2023 and March 2024 CHT deductions totaling $43,296, based on the implementation of elements of its RAP to improve access and eliminate patient charges, including the introduction of the ICHSCA.
Manitoba
In March 2023, Manitoba was subject to a deduction of $353,827 under the DSP, based on an estimate made by Health Canada. In March 2024, Manitoba was once again subject to a deduction under the DSP in the amount of $650, based on amounts reported by Manitoba to Health Canada. These deductions were the result of patient charges for medically necessary diagnostic services that occurred in 2020-2021 and 2021-2022, respectively. In March 2024, Manitoba received a full reimbursement of its March 2023 deduction and an immediate reimbursement of its March 2024 deduction for a total reimbursement in the amount of $354,477. This reimbursement was made as a result of the successful implementation of Manitoba's RAP to eliminate patient charges for medically necessary ultrasound scans that were occurring at a private ultrasound clinic.
Saskatchewan
In March 2023 and March 2024, Saskatchewan was subject to deductions under the DSP in the amounts of $742,447 and $1,084,513, respectively, based on estimates made by Health Canada, which were developed using information provided by the province. These deductions were the result of patient charges for medically necessary diagnostic services that occurred in 2020-2021 and 2021-2022, respectively, due to Saskatchewan's Patient Choice Medical Imaging Act, which authorizes private MRI and CT facilities in the province to accept payment directly from patients in exchange for medically necessary imaging services. To date, Saskatchewan has not qualified for reimbursement as a result of failing to meet the reporting requirements of the Reimbursement Policy, namely the creation of a RAP to eliminate the patient charges and the underlying circumstances has allowed them to occur. However, Saskatchewan's March 2023 and 2024 deductions remain eligible for full reimbursement until March 2025 and March 2026, respectively.
Alberta
In March 2023 and 2024, Alberta was subject to deductions under the DSP in the amounts of $13,781,152 and $20,450,175, respectively, based on estimates made by Health Canada. These deductions were the result of patient charges for medically necessary diagnostic services that occurred in 2020-2021 and 2021-2022, respectively. In March 2024, Alberta received a partial reimbursement of its March 2023 and March 2024 CHT deductions totaling $20,538,796, based on the implementation of elements of the province's RAP to improve access and eliminate patient charges, including increased funding and capacity for the provision of medically necessary diagnostic services.
British Columbia
Since 2018, deductions totaling $88,812,438 have been taken from British Columbia's CHT payments for patient charges primarily levied by private clinics for medically necessary surgical services. These deductions include $15,861,818 taken in March 2018, $16,177,259 taken in March 2019, $16,753,833 taken in March 2020, $13,949,979 taken in March 2021, $13,275,823 taken in March 2022, $5,945,221 taken in March 2023 and $6,848,505 taken in March 2024 for patient changes that occurred in 2015-2016, 2016-2017, 2018-2019, 2019-2020, 2020-2021 and 2021-2022, respectively. Since 2019, the deductions have been based on amounts reported by British Columbia to Health Canada, calculated using a similar methodology used by Health Canada to estimate British Columbia's March 2018 CHT deduction.
Further deductions of $17,165,309 and $11,270,216 were taken from British Columbia's March 2023 and March 2024 CHT payments under the DSP as a result of patient charges for medically necessary diagnostic services that occurred in 2020-2021 and 2021-2022, respectively. These deductions were based on amounts reported by British Columbia to Health Canada.
Including amounts deducted in respect of patient charges for medically necessary surgical services, British Columba's March 2024 deduction totalled $18,118,721.
Following its deduction in 2018, British Columbia consulted with Health Canada on a RAP to eliminate patient charges. Because the province successfully carried out many of the elements of that plan, the province received partial reimbursements, including: $16,019,539 in March 2020 (for 2018 and 2019 deductions), $24,509,418 in March 2021 (for 2019, 2020, and 2021 deductions), $20,518,055 in March 2022 (for 2020, 2021, and 2022 deductions), and $15,556,669 in March 2023 (for March 2021, 2022, and 2023 deductions), and $22,405,749 in March 2024 (for March 2022, March 203 and March 2024 deductions). The March 2024 amount represents a reimbursement of $6,818,207 for deductions taken in respect of in surgical charges, and $15,587,542 in respect of deductions taken for diagnostic charges.
Since the Canada Health Act Reimbursement Policy came into effect, $175,010,504 has been reimbursed to provinces, in recognition of their efforts to eliminate patient charges for insured health services.
| NL | NS | NB | QC | ON | MB | SK | AB | BC | TOTALS BY FISCAL YEAR | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
2018-2019 |
Deduction | $1,349 | - | - | $8,256,024 | - | - | - | - | $16,177,259 | $24,434,632 |
| Reimbursement | - | - | - | $8,256,024 | - | - | - | - | - | $8,256,024 | |
2019-2020 |
Deduction | $70,819 | - | $140,216 | - | - | - | - | - | $16,753,833 | $16,964,868 |
| Reimbursement | $72,168 | - | - | - | - | - | - | - | $16,019,539Footnote 1 | $16,091,707 | |
2020-2021 |
Deduction | $4,521 | - | $64,850 | - | $13,905 | - | - | - | $13,949,979 | $14,033,255 |
| Reimbursement | $4,521 | - | - | - | - | - | - | - | $24,509,418Footnote 2 | $24,513,939 | |
2021-2022 |
Deduction | $1,723 | - | $64,850 | - | $6,560 | - | - | - | $13,275,823 | $13,348,956 |
| Reimbursement | $1,723 | - | - | - | - | - | - | - | $20,518,055Footnote 3 | $20,519,778 | |
2022-2023 |
Deduction | - | $1,277,659 | $1,342,509 | $41,867,224 | $32,800 | $353,827 | $742,447 | $13,781,152 | $23,110,530 | $82,508,148 |
| Reimbursement | - | - | - | - | - | - | - | - | $15,556,669Footnote 4 | $15,556,669 | |
2023-2024 |
Deduction | $1,255 | $1,794,635 | $1,903,910 | $36,014,132 | $32,800 | $650 | $1,084,513 | $20,450,175 | $18,118,721 | $79,400,791 |
| Reimbursement | $1,255 | - | - | $46,728,814Footnote 5 | $43,296Footnote 6 | $354,477Footnote 7 | - | $20,538,796Footnote 8 | $22,405,749Footnote 9 | $90,072,387 | |
| TOTAL DEDUCTIONS BY PT | $79,667 | $3,072,294 | $3,516,335 | $86,137,380 | $86,065 | $354,477 | $1,826,960 | $34,231,327 | $101,386,145 | ||
| TOTAL REIMBURSEMENTs BY PT | $79,667 | - | - | $54,984,838 | $43,296 | $354,477 | - | $20,538,796 | $99,009,430 | ||
Deductions are made two years after the extra-billing and user charges occurred (for example, deductions taken in 2023-2024 were in respect of patient charges levied in fiscal year 2021-2022).
|
|||||||||||
Interprovincial Health Insurance Agreements Coordinating Committee
All provinces and territories participate in hospital reciprocal billing agreements, and all, with the exception of Quebec, participate in physician reciprocal billing agreements. These agreements generally ensure that a patient's health care insurance card will be accepted, instead of payment, when the patient receives insured hospital or physician services in another province or territory. The province or territory providing the service will then directly bill the patient's home province at agreed-upon rates. The intent of these agreements is to ensure that insured Canadian residents do not have to pay directly for medically necessary hospital and physician services when they travel within Canada or during the waiting period for coverage to be established after moving to another province or territory. Through these agreements, approximately $1 billion is reciprocally billed across the country each year. While the agreements facilitate the portability criterion of the Canada Health Act, provinces and territories may agree to meet the requirements of the Act through other mechanisms.
The Interprovincial Health Insurance Agreements Coordinating Committee (IHIACC) was formed in 1991 as the authority to oversee the administration of the reciprocal billing agreements and ensure interprovincial/ territorial health care insurance plan coverage in accordance with the Act. IHIACC's mandate also includes analyzing and developing policy recommendations on interprovincial/territorial health care insurance plan coverage issues outside the scope of the Act. The Committee includes members from each province and territory and a non-voting chair from the Canada Health Act Division. The Canada Health Act Division also provides secretariat functions for IHIACC. IHIACC maintains several working groups that support its mandate through the provision of strategic advice and recommendations related to reciprocal billing rates, patient eligibility, and interprovincial/territorial health care coverage policies.
In 2023, IHIACC started preliminary policy work on interprovincial virtual care and simplifying the billing administration of emerging therapies delivered interprovincially (e.g., gene therapies). IHIACC also completed an initial technical review of bone morrow and stem cell transplant billing rates. A revised bone marrow and stem cell rates model is expected to be finalized in 2024-2025 with implementation by 2026-2027.
Chapter 3 – Provincial and territorial health care insurance plans in 2023-2024
The following chapter presents the 13 provincial and territorial health care insurance plans that make up the Canadian publicly funded health insurance system. The purpose of this chapter is to demonstrate clearly and consistently the extent to which provincial and territorial health care insurance plans fulfilled the requirements of the Canada Health Act's program criteria and conditions in 2023-2024.
Officials in the provincial, territorial and federal governments have collaborated to produce the detailed plan overviews contained in Chapter 3. The information that Health Canada requested from the provincial and territorial departments of health for the report consists of two components:
- a narrative description of the provincial or territorial health care system relating to the criteria and conditions of the Act; and
- statistical information related to insured health services.
The narrative component is used to help with the monitoring and compliance of provincial and territorial health care insurance plans with respect to the requirements of the Act, while statistics help to identify current and future trends in the Canadian health care system. While all provinces and territories have submitted detailed descriptive information on their health care insurance plans, Quebec chose not to submit supplemental statistical information which is contained in the tables in this year's report.
To help provinces and territories prepare their submissions to the annual report, Health Canada provided them with the document; Canada Health Act Annual Report 2023-2024: A Guide for Updating Submissions (User's Guide). The User's Guide is designed to help provinces and territories meet Health Canada's reporting requirements. Annual revisions to the guide are based on Health Canada's analysis of health care insurance plan descriptions from previous annual reports and its assessment of emerging issues relating to insured health services.
The process for the Canada Health Act Annual Report 2023-2024 was launched in spring 2024. An updated User's Guide was also sent to the provinces and territories at that time.
Insurance plan descriptions
For the following chapter, provincial and territorial officials were asked to provide a narrative description of their health care insurance plan. The descriptions follow the program criteria areas of the Canada Health Act in order to illustrate how the plans satisfy these criteria. This narrative format also allows each jurisdiction to indicate how it met the Canada Health Act requirement for the recognition of federal contributions that support insured and extended health care services.
Key definitions provided to provinces and territories to guide their submissions to this report
Participating Physician or Dentist is a licensed physician or dentist who is enrolled in a provincial or territorial health care insurance plan.
Non-Participating Physician or Dentist practises completely outside a provincial or territorial health care insurance plan. Neither the physician or dentist nor the patient is eligible for any cost coverage for services rendered or received from the provincial or territorial health care insurance plans. A non-participating physician or dentist may therefore establish their own fees, which are paid directly by the patient.
Opted-out Physician or Dentist is a physician or dentist who is enrolled in the provincial or territorial health care insurance plan but has voluntarily opted out of the plan and will therefore bill their patients directly. These charges can be up to, but not more than, the provincial or territorial amount allowed under the fee schedule agreement. The provincial or territorial health care insurance plans reimburse patients of opted-out physicians or dentists for these charges.
Provincial and territorial health care insurance plan statistics
Over time, the section of the annual report containing the statistical information submitted from the provinces and territories has been simplified and streamlined based on feedback received from provincial and territorial officials, and based on reviews of data quality and availability. The supplemental statistical information tables can be found at the end of each provincial or territorial narrative, except for Quebec
The purpose of the statistical tables is to place the administration and operation of the Canada Health Act in context and to provide a national perspective on trends in the delivery and funding of insured health services in Canada that are within the scope of the Act.
The statistical tables contain resource and cost data for insured hospital, physician and surgical-dental services by province and territory for five consecutive years ending on March 31, 2024. All information was provided by provincial and territorial officials.
Although efforts are made to capture data on a consistent basis, differences exist in the reporting on health care programs and services between provincial and territorial governments. Therefore, comparisons between jurisdictions are not made. Provincial and territorial governments are responsible for the quality and completeness of the data they provide.
Organization of the information
Information in the statistical tables is grouped according to the nine subcategories described below.
Registered Persons: Registered persons are the number of residents registered with the health care insurance plans of each province or territory.
Insured Hospital Services within Own Province or Territory: Statistics in this sub-section relate to the provision of insured hospital services to residents in each province or territory, as well as to visitors from other regions of Canada.
Insured Hospital Services Provided to Residents in Another Province or Territory: This sub-section presents out-of-province or out-of-territory insured hospital services that are paid for by a person's home jurisdiction when they travel to other parts of Canada.
Insured Hospital Services Provided Outside Canada: This represents residents' hospital costs incurred while travelling outside of Canada that are paid for by their home province or territory.
Insured Physician Services within Own Province or Territory: Statistics in this sub-section relate to the provision of insured physician services to residents in each province or territory, as well as to visitors from other regions of Canada.
Insured Physician Services Provided to Residents in Another Province or Territory: This sub-section reports on physician services that are paid by a jurisdiction to other provinces or territories for their visiting residents.
Insured Physician Services Provided Outside Canada: This represents residents' medical costs incurred while travelling outside of Canada that are paid by their home province or territory.
Insured Surgical-Dental Services within Own Province or Territory: The information in this subsection describes insured surgical-dental services provided in each province or territory.
Newfoundland and Labrador
The Department of Health and Community Services (the department) is responsible for setting the overall strategic directions and priorities for the health and community services system throughout Newfoundland and Labrador.
The department works with stakeholders to ensure that high quality, cost effective, and timely health services are available for all Newfoundlanders and Labradorians. The department also works with stakeholders to develop and enhance policies, legislation, provincial standards, and strategies to support individuals, families, and communities to achieve optimal health and well-being. On April 1, 2023, four former Regional Health Authorities and the Newfoundland and Labrador Centre for Health Information were amalgamated to become a single Provincial Health Authority, operating as Newfoundland and Labrador Health Services (NLHS).
The department provides leadership, coordination, monitoring, and support to NLHS, which delivers the majority of publicly funded health services in the province, as well as to other entities that deliver programs and services. This ensures quality, efficiency, and effectiveness in areas such as the administration of health care facilities; access and clinical efficiency; mental health and addictions services; long-term care and community support services; health professional education and training programs; the control, possession, handling, keeping and sale of food and drugs; the preservation and promotion of health; the prevention and control of disease; and public health and the enforcement of public health standards.
With a net annual budget of approximately $3.6 billion, the department accounts for approximately 40 per cent of Newfoundland and Labrador's total budget. In Budget 2023-2024, funding was provided for various programs and initiatives to make significant improvements to mental health and addictions, home and community care, and primary health care. Included in this was approximately $140 million to improve housing stability and prevent homelessness; over $60 million to provide residents with new ways to access cardiovascular services, travelling orthopedic teams, improving access to midwifery services and expanding the scope of practice for health care professionals; $23 million additional funding of health care professional recruitment and retention, and $4.4 million for flexible assertive community treatment teams to provide mental health and addictions services. The 2023-2024 Budget also included approximately $8.0 million in base funding to support the addition of new drug therapies to the Newfoundland and Labrador Prescription Drug Program formulary. An overview of initiatives from the 2023-2024 Budget is available at the Government of Newfoundland and Labrador's website.
In Newfoundland and Labrador, health services are provided to about 530,000 residents. Approximately 22,600 people are employed by NLHS and approximately 231 people are employed by the department.
The purpose of this report is to clearly describe how Newfoundland and Labrador fulfilled the requirements of the Canada Health Act program criteria, conditions, and provisions in 2023-2024.
1.0 Public administration
1.1 Health care insurance plan and public authority
Health care insurance plans managed by the department include the Medical Care Plan (MCP) and the Hospital Insurance Plan (HIP). Both plans are non-profit and publicly administered.
The Medical Care and Hospital Insurance Act (MCHI Act) came into force on October 1, 2016, replacing both the Medical Care Insurance Act, 1999, and the Hospital Insurance Agreement Act. The MCHI Act can be viewed on the Newfoundland and Labrador House of Assembly website.
Under section 5 of the MCHI Act, the Minister of Health and Community Services is required to administer a plan of medical care insurance and hospital insurance for residents of the province. The MCHI Act provides authority to make regulations defining who is a resident, prescribing which services are insured services, and prescribing under what circumstances insured services shall be paid by the Minister.
The MCP facilitates the delivery of comprehensive medical care to all residents of the province by implementing policies, procedures, and systems that permit appropriate compensation to physicians for rendering insured professional services.
The HIP covers insured hospital services received within the province when recommended by a medical practitioner. Eligibility for coverage under the plan is linked with eligibility for the MCP. All beneficiaries of the MCP are automatically entitled to coverage under the HIP.
Both the HIP and the MCP operate in accordance with the provisions of the MCHI Act and related regulations, and in compliance with the Canada Health Act.
The Medical Care Insurance Insured Services Regulations were amended in 2023 to include coverage of medical examinations for persons who are required to have a medical examination for a driver's licence due only to age. No other amendments to the health care insurance plan legislation or regulations were made in 2023-2024.
1.2 Reporting relationship
The Minister is mandated with administering the HIP and the MCP under section 5 of the MCHI Act. The department reports on these plans through the regular legislative processes, as well as through other public reporting mechanisms (e.g., Public Accounts and the Social Services Committee of the House of Assembly).
The Government of Newfoundland and Labrador has a provincial planning and reporting requirement for all government departments, including the Department of Health and Community Services. Under the Transparency and Accountability Act, the department and the six other entities that report to the Minister, including NLHS, produce multi-year performance-based plans. Plans and reports are tabled in the House of Assembly and posted on the department's website.
The 2023-2024 Department of Health and Community Services annual report has been tabled in the House of Assembly.
1.3 Audit of accounts
Each year, the province's Auditor General independently examines provincial Public Accounts. MCP expenditures are considered a part of the Public Accounts. While respecting privacy and personal information, the Auditor General has full and unrestricted access to code-based records of the MCP. There were no Auditor General reviews of the department's programs, services, or MCP expenditures in 2023–2024. The most recent comprehensive audit was a review of the Newfoundland and Labrador Prescription Drug Program in June 2015.
Specific program reviews are executed in accordance with the Office of the Auditor General plan, which is largely driven by risk. In the planning stages of an audit, the department would be notified by receipt of an engagement letter from the Office of the Auditor General, advising that an audit is being planned and requesting any necessary arrangements to execute it.
NLHS is subject to financial statement audits, reviews and compliance audits. A financial statement audit for NLHS is performed in accordance with the Provincial Health Authority Act and the Auditor General Act, 2021. Review engagements are conducted using the Generally Accepted Auditing Standards of the Chartered Professional Accountants of Canada. Various compliance and physician audits are carried out by personnel from the department under the authority of the MCHI Act.
Physician records and professional medical corporation records are reviewed to ensure that the records support the services billed and that the services are insured under the MCP. Beneficiary audits are performed by personnel from the department under the MCHI Act.
2.0 Comprehensiveness
2.1 Insured hospital services
As of March 31, 2024, the Medical Care and Hospital Insurance Act (MCHI Act) and the Hospital Insurance Regulations provided for insured hospital services in Newfoundland and Labrador. No amendments were made to the MCHI Act during this current reporting period concerning insured hospital services. All the hospital services as defined under the Canada Health Act are insured services in Newfoundland and Labrador.
Insured hospital services are provided for in-patients and out-patients in 15 hospitals, 23 community health centres, and 73 community clinics throughout the province. Hospital insured services include:
- accommodations and meals at the standard ward level;
- nursing services;
- laboratory, radiology, and other diagnostic procedures;
- drugs, biologicals, and related preparations;
- medical and surgical supplies;
- operating room, case room, and anaesthetic facilities;
- rehabilitative services (e.g., physiotherapy, occupational therapy, speech language pathology and audiology);
- radiotherapy services (e.g., radiotherapy facilities, radioactive isotopes);
- in-patient, out-patient, and emergency visits; and
- day surgery.
There were no new services added to the schedule of insured hospital services during 2023-2024.
The coverage policy for insured hospital services is linked to the coverage policy for insured medical services. The department manages the process of adding or de-listing a hospital service from the list of insured services based on approval from the Lieutenant-Governor in Council. Public consultation is not a requirement for de-listing a service.
Medical goods and services that are permanently implanted and associated with an insured service are provided free of charge to the patient and are consistent with national standards of practice. Patients retain the right to financially upgrade standard medical goods or services. Standards for medical goods are developed by the hospitals providing those services in consultation with service providers.
In 2023-2024, the department was not aware of any private diagnostic clinics that charge patients for services that would be considered insured if provided in a hospital.
2.2 Insured physician services
As of March 31, 2024, the enabling legislation for insured physician services was the MCHI Act and the relevant regulations continued thereunder, which included the:
- Medical Care Insurance Insured Services Regulations;
- Medical Care Insurance Beneficiaries and Inquiries Regulations; and
- Physicians and Fee Regulations.
As of March 31, 2024, there were 1,295 physicians (alternate payment plan, salaried and fee-for-service) active in practice in the province.
For purposes of the MCHI Act, the following services are covered:
- all services properly and adequately provided by physicians to beneficiaries suffering from an illness requiring medical treatment or advice;
- group immunizations or inoculations carried out by physicians at the request of the appropriate authority;
- diagnostic and therapeutic x-ray and laboratory services in facilities approved by the appropriate authority that are not provided under the MCHI Act and Regulations; and
- medical examinations for persons who are required to undergo a medical examination under paragraph 12(b) of the Highway Traffic Driver Regulations, 1999.
Administration of the influenza vaccine by physicians became temporarily billable under Medical Care Plan (MCP) in October 2020. This measure remained in place throughout 2023-2024.
Physicians can choose not to participate in the MCP as outlined in section 8 of the MCHI Act, namely:
- 8. (3) A practitioner may, in writing, notify the minister of his or her election to collect payments in respect of insured services provided by the practitioner to beneficiaries otherwise than from the minister.
- 8. (4) An election under subsection (3) shall have effect from the first day of the first month beginning after the expiration of 60 days after the date on which the minister receives the notice of election.
- 8. (5) A practitioner who has made an election under subsection (3) may revoke the election by written notice to the minister.
- 8. (6) A revocation of election under subsection (5) shall have effect from the first day of the first month beginning after the expiration of 60 days after the date on which the minister receives the notice of revocation.
- 8. (7) Notwithstanding subsections (4) and (6), the minister may waive the time periods in those subsections where, in his or her opinion, it is reasonable to do so.
As of March 31, 2024, no physicians had opted out of the MCP.
Lieutenant-Governor in Council approval is required to add to or to de-insure a physician service from the list of insured services. This process is managed by the department in consultation with various stakeholders. Public consultation is not a specific requirement.
2.3 Insured surgical-dental services
The provincial Surgical-Dental Program is a component of the MCP. Surgical-dental treatments provided to a beneficiary and carried out in a hospital by a licensed oral surgeon or dentist are covered by the MCP if the treatment is specified in the Surgical-Dental Services Schedule.
The Surgical Dental Program provides insured services under the MCHI Act. An insured service is defined as:
- A medically necessary surgical-dental treatment properly and adequately provided to a beneficiary and carried out in a hospital by a dentist if the treatment is listed in the Surgical-Dental Payment Schedule set by the Minister. The clinical need of the provision and claim of an insured service may be evaluated by the Dental Monitoring Committee of MCP.
Policies on pre-existing conditions necessary to define 'medical necessity' must exist for the specific services to qualify as MCP insured services.
There were 20 dentists and oral surgeons providing insured services under the Surgical-Dental Program as of March 31, 2024.
Dentists and oral surgeons may opt out of the MCP under section 8 of the MCHI Act, as referenced above. These dentists or oral surgeons must advise the patient of their opted-out status, state the fees expected and provide the patient with a written record of services and fees charged. As of March 31, 2024, there were no opted-out dentists or oral surgeons. There was no extra-billing in 2023-2024.
Because the Surgical-Dental Program is a component of the MCP, management of the program is linked to the MCP process regarding changes to the list of insured services.
Any addition of a surgical-dental service to the list of insured services must be approved by the Minister of Health and Community Services. There were no new services added to the list of insured surgical-dental services in 2023-2024.
2.4 Uninsured hospital, physician, and surgical-dental services
Hospital services not covered include:
- preferred accommodation that is not medically required;
- ambulance or other patient transportation before admission or upon discharge;
- private duty nursing arranged by the patient;
- non-medically required x-rays or other services (i.e. for employment or insurance purposes;
- drugs (except anti-rejection drugs for transplant patients and AZT for patients with AIDS) and appliances issued for use after discharge from hospital;
- bedside telephones, radios or television sets for personal, non-teaching use;
- services provided in non-approved Canadian diagnostic imaging facilities;
- in-vitro fertilization and other procreative measures;
- services covered by WorkplaceNL or by other federal or provincial legislation; and
- services relating to therapeutic abortions performed outside Canada or in non-accredited Canadian facilities.
The use of the hospital setting for any services deemed uninsured by the MCP are also uninsured under the HIP for purposes of the MCHI Act. The following is a list of uninsured physician services:
- the dispensation by a physician of medicines, drugs or medical appliances, and the giving or writing of medical prescriptions;
- the preparation by a physician of records, reports or certificates for, or on behalf of, or any communication to, or relating to, a beneficiary;
- any services rendered by a physician to the spouse and children of the physician;
- any service to which a beneficiary is entitled under an Act of the Parliament of Canada, an Act of the Province of Newfoundland and Labrador, an Act of the legislature of any province of Canada, or any law of a country or part of a country;
- the time taken or expenses incurred in travelling to consult a beneficiary;
- ambulance service and other forms of patient transportation;
- acupuncture and all procedures and services related to acupuncture, excluding an initial assessment specifically related to diagnosing the illness proposed to be treated by acupuncture;
- examinations not necessitated by illness or at the request of a third party except as specified;
- plastic or other surgery for purely cosmetic purposes, unless medically indicated;
- laser treatment of telangiectasia;
- testimony in a court;
- visits to optometrists, family physicians, and ophthalmologists solely for determining whether new or replacement glasses or contact lenses are required;
- the fees of a dentist, oral surgeon, or family physician for routine dental extractions performed in hospital;
- fluoride dental treatment for children under four years of age;
- excision of xanthelasma;
- circumcision of newborns;
- hypnotherapy;
- medical examination for drivers, except when these are required due to age only;
- alcohol or drug treatment outside Canada;
- consultation required by hospital regulation;
- therapeutic abortions performed in the province at a non-approved facility;
- in-vitro fertilization and ovarian stimulation and sperm transfer;
- reversal of previous sterilization procedure; and
- other services not within the ambit of section 3 of the Medical Care Insurance Insured Services Regulations.
The MCHI Act provides the Lieutenant-Governor in Council the authority to make regulations prescribing which services are or are not insured services for the purpose of the Act. This would involve consultation with the Newfoundland and Labrador Medical Association or the Newfoundland and Labrador Dental Association. There is no specified requirement for public consultation when delisting a service. No services were de-listed from the MCP during 2023-2024.
3.0 Universality
3.1 Eligibility
Residents of Newfoundland and Labrador are eligible for coverage under the Medical Care and Hospital Insurance Act (MCHI Act). The MCHI Act defines a "resident" as a person who is lawfully entitled to be or to remain in Canada, makes his or her home in the province, and is ordinarily present in the province, but does not include a tourist, transient, or visitor to the province.
The Medical Care Insurance Beneficiaries and Inquiries Regulations identify those residents eligible to receive coverage under the plans. There were no amendments to these regulations during the reporting period. The Medical Care Plan (MCP) has established rules to ensure that the Regulations are applied consistently and fairly in processing applications for coverage. The MCP applies the standard that persons moving to Newfoundland and Labrador from another province become eligible on the first day of the third month following the month of their arrival. Under section 6 of the MCHI Act, every resident of the province is required to register for the MCP in accordance with the regulations. While there is no specified opt-out provision, a person may, in effect, do so by choosing not to register.
Persons not eligible for coverage under the MCP and HIP include:
- students and their dependants already covered by another province or territory;
- dependants of residents if covered by another province or territory;
- refugee claimants and their dependants;
- foreign workers with employment authorizations that do not meet the established criteria;
- international students with student authorizations that do not meet the established criteria;
- foreign seasonal workers, tourists, transients, visitors and their dependants;
- Canadian Armed Forces personnel;
- inmates of federal prisons; and
- armed forces personnel from other countries who are stationed in the province.
If the status of these individuals changes, they must meet the criteria as noted above in order to become eligible. Applicants wishing to appeal an eligibility issue may request a formal file review from the Minister of Health and Community Services.
There were approximately 533,567 people registered as active beneficiaries of the MCP as of March 31, 2024.
3.2 Other categories of individuals
Foreign workers, international students, foreign clergy and dependants of North Atlantic Treaty Organization personnel and applicants for permanent residency are eligible for benefits. Returning repatriated Canadian citizens and their dependants born out-of-country, returning permanent residents who hold valid documentation, holders of Minister's permits, convention refugees, resettled refugees or "persons in need of protection" with valid immigration documents are also eligible, subject to MCP approval. Dependants of MCP beneficiaries in all categories may also be eligible for coverage.
In 2023-2024, Ukrainians entering the Newfoundland and Labrador under the Canada-Ukraine Authorization for Emergency Travel and the Special Family Reunification Sponsorship Pathway are eligible for MCP registration for six-month renewable periods, provided they remain a resident of the province.
4.0 Portability
4.1 Minimum waiting period
Persons who meet the eligibility criteria who are moving to Newfoundland and Labrador from other provinces or territories are entitled to coverage on the first day of the third month following the month of arrival.
Persons arriving from outside Canada to establish residence are entitled to coverage on the day of arrival. The same applies to discharged members of the Canadian Armed Forces, and individuals released from federal penitentiaries. For coverage to be effective, registration is required under the Medical Care Plan (MCP). Immediate coverage is provided to persons from outside Canada authorized to work in the province for one year or more and their eligible dependants, and to international post-secondary students attending a recognized Newfoundland and Labrador educational institution who have a valid study permit entitling them to stay in Canada for more than 365 days and their eligible dependants. This one year Immigration, Refugees and Citizenship Canada work permit requirement has been reduced to a six-month work permit for individuals entering the province under the Newfoundland and Labrador Provincial Nominee Program and the Atlantic Immigration Program. For international health care workers with employment authorizations, the period of employment may be for less than 365 days.
4.2 Coverage during temporary absences in Canada
Newfoundland and Labrador is a party to the Interprovincial Agreement on Eligibility and Portability regarding matters pertaining to portability of insured services in Canada.
Sections 12 and 13 of the Hospital Insurance Regulations denote portability of hospital coverage during absences within Canada. The eligibility policy for insured hospital services is linked to the eligibility policy for insured physician services. No amendments to the Regulations were made in 2023-2024.
Coverage is provided to residents during temporary absences within Canada. The Government of Newfoundland and Labrador has entered into formal agreements (e.g., the Hospital Reciprocal Billing Agreement) with other provinces and territories for the reciprocal billing of insured hospital services. In-patient costs are paid at standard rates approved by the host province or territory. In-patient, high-cost procedures and out-patient services are payable based on national rates agreed to by provincial and territorial health plans through the Interprovincial Health Insurance Agreements Coordinating Committee.
Medical services incurred in all provinces (except Quebec), or territories are paid through the Medical Reciprocal Billing Agreement at host province or territory rates. Claims for medical services received in Quebec are submitted by the patient to the MCP for payment at host province rates.
In order to qualify for out-of-province coverage, a beneficiary must comply with the legislation and the MCP rules regarding residency in Newfoundland and Labrador. Generally, a resident must reside in the province for at least four months in each 12-month period to qualify as a beneficiary. The rules regarding medical and hospital care coverage during absences include the following:
- Before leaving the province for extended periods (more than 30 days), a resident is encouraged to contact the MCP office to obtain an out-of-province coverage certificate (a certificate). For out-of-province trips lasting more than 30 days, a certificate is recommended as proof of a resident's ability to pay for services while outside the province.
- Beneficiaries registered under five-year renewal periods who have resided in the province for longer than 12 months who:
- leave for vacation purposes may receive an initial out-of-province coverage certificate of up to 12 months once every five years. Upon return, beneficiaries are required to reside in the province for a minimum four months; thereafter, certificates will only be issued for up to eight months of coverage for each of the next four years;
- are Newfoundland and Labrador students and who leave the province may receive a certificate, renewable each year, provided they submit proof of full-time enrollment in a recognized educational institution located outside the province; and
- leave the province for employment purposes may receive a certificate for coverage up to 12 months, for up to three consecutive years, renewable annually and subject to verification of employment if required. Workers employed with College of the North Atlantic's campus in Qatar may receive coverage for five consecutive years.
- Persons must not establish residency in another province, territory or country while maintaining coverage under the MCP.
- For out-of-province trips of 30 days or less, an out-of-province coverage certificate is not required but will be issued upon request.
Failure to request out-of-province coverage or failure to abide by the residency rules may result in the resident having to pay for medical or hospital costs incurred outside the province.
Failure to apply for an out-of-province coverage certificate for absences exceeding 30 days, or to meet minimum annual in-province residency requirements, could result in the beneficiary being required to pay for medical or hospital costs they incur outside the province.
Insured residents moving permanently to other parts of Canada are covered up to, and including, the last day of the second month following the month of departure.
No changes to coverage during temporary absences in Canada were made in 2023-2024.
International workers and international students who meet eligibility criteria may qualify for out-of-province coverage within or outside of Canada for up to 182 days during their current 365-day registration period, provided that at no point during that period will their cumulative absence exceed the length of time they have been present in the province.
4.3 Coverage during temporary absences outside Canada
Section 12 of the Hospital Insurance Regulations denotes portability of hospital coverage during absences outside Canada. No amendments were made to the Regulations during the reporting period.
The province provides coverage to residents during temporary absences outside Canada similar to the criteria outlined in 4.2 (above) for absence within other parts of Canada. Out-of-country insured hospital in-patient and out-patient services are covered for emergencies, sudden illness, and elective procedures at established rates listed below. Hospital services are considered under the plan when the insured services are provided by a recognized facility (licensed or approved by the appropriate authority within the state or country in which the facility is located) outside Canada. The maximum amount payable by the MCP for out-of-country in-patient hospital care is $350 per day if the insured services are provided by a community or regional hospital. Where insured services are provided by a tertiary care hospital (i.e. a highly specialized facility), the approved rate is $465 per day. The approved rate for out-patient services is $62 per visit and haemodialysis is $220 per treatment. The approved rates are paid in Canadian funds.
Physician services are covered for emergencies or sudden illness and are also insured for elective services not available in the province or within Canada. Emergency physician services are paid at the same rate as would be paid in Newfoundland and Labrador for the same service. If the elective services are not available in Newfoundland and Labrador, they are usually paid at Ontario rates, or at rates that apply in the province where they are available.
Coverage is immediately discontinued when residents move permanently to other countries.
4.4 Prior approval requirement
Prior approval is not required for medically necessary insured services provided by accredited hospitals or licensed physicians in the other provinces and territories that are billed reciprocally. However, physicians may seek advice on coverage from the MCP so that patients may be made aware of any financial implications.
Prior approval is mandatory in order to receive funding at host country rates if a resident of the province has to seek specialized care outside the country because the insured service is not available in Canada. The referring physician must contact the department for prior approval. If prior approval is granted, the provincial health care insurance plan will pay the costs of insured services necessary for the patient's care at host country rates. Prior approval is not granted for out-of-country treatment or elective services at host country rates if the service is available in the province or elsewhere within Canada. If an individual opts to receive the service outside Canada it will be covered at the provincial rate if available in Newfoundland and Labrador. If the service is not available in Newfoundland and Labrador, it is usually paid at Ontario rates, or at rates that apply in the province where they are available. Applicants wishing to appeal out-of-country coverage may request a formal file review by the Minister.
5.0 Accessibility
5.1 Access to insured health services
Access to insured health services in Newfoundland and Labrador is provided on uniform terms and conditions. Co-insurance charges for insured hospital services and extra-billing by physicians is prohibited in the province.
Section 7 of the Medical Care and Hospital Insurance Act (MCHI Act) outlines that a practitioner who provides insured services, whether or not they have made an election to opt out of participation in the Medical Care Plan (MCP), shall not charge or collect from a beneficiary a fee for those insured services in excess of the amount payable under the MCHI Act and Regulations. A practitioner or other person who contravenes this is guilty of an offence and liable on summary conviction to a fine of up to but not more than $20,000 for each contravention. Cases of extra-billing and user charges may be identified through the audit process described under section 21 of the MCHI Act or may be reported from residents. These instances may be discovered when residents submit claims to the department for reimbursement.
Complaints from residents regarding charges for insured health services are managed by the department. Depending on the circumstance, the department may investigate or refer the matter to the College of Physicians and Surgeons of Newfoundland and Labrador, the regulatory body for physicians in the province, for potential disciplinary action. Residents may also contact the College directly if they feel that they have been subject to improper billing by their physician.
Regarding repayment, section 25 of the MCHI Act provides the Minister with powers to recover overpayments and interest that were discovered via audit. The Minister of Health and Community Services may do this by entering into an agreement with the practitioner or their professional corporation or the Minister may order the practitioner to pay to the Minister the overpaid amount plus interest.
Residents wishing to file a complaint regarding medical care that they have received are encouraged to call or email the Complaints Coordinator at the College (1-709-726-8546 or complaints@cpsnl.ca) or call the MCP general inquiries line (Avalon area: 1-866-449-4459; all other regions:1-800-563-1557).
The department works closely with post-secondary educational institutions within the province to maintain an appropriate supply of health professionals. The province also works with external organizations for health professionals not trained in this province. Targeted recruitment incentives are in place to attract health professionals. Several programs have been established to provide targeted sign-on bonuses, bursaries, opportunities for upgrading, and other incentives for a wide variety of health occupations.
With respect to wait times to access insured health services, the department introduced the Policy for Provision of Cataract Surgery in Non-Hospital Designated Facilities in 2020-2021. By extending the provision of cataract surgeries to include non-hospital facilities, the department aims to increase patient access to cataract surgery and reduce wait times overall. In 2023-2024 there were just over 7,000 cataract procedures approved/delivered by non-hospital facilities.
The new initiatives previously introduced in 2022-2023 to increase surgical capacity to address the backlogs of hip and knee replacement surgeries were expanded in 2023-2024. The second same day discharge hip and knee replacement program started, and the travelling orthopedic surgical team started travelling to a second rural surgical site to perform select hip and knee replacement surgeries. Also, a pilot project in which patients will be admitted overnight for a short-stay and then transition to an outpatient ambulatory rehabilitation clinic for select hip and knee replacement surgeries was introduced. As a result of these initiatives, 570 additional joint replacement surgeries were performed in 2023-2024.
A partnership was established with the University of Ottawa Heart Institute to address the wait list for cardiac surgery, in addition to a fly-in and fly-out program for patients in other regions of the province requiring cardiac catheterization at the tertiary care centre.
A Surgical Task Force was established to look at the surgical backlog and provide meaningful solutions in 2022. In August 2023, Government announced that it will implement all 32 recommendations made by the Provincial Surgical Task Force to reduce the current surgical backlog and surgical wait times in Newfoundland and Labrador. The Health Transformation Surgery Sub-Table has been tasked with overseeing the progress to implement the recommendations.
The provincial government also partnered with the Princess Margaret Cancer Centre in Toronto to send patients for radiation treatment.
5.2 Physician compensation
Physicians in the province are paid via fee-for-service, blended capitation, salary or alternate payment plan. As of March 31, 2024, the legislation governing payments to physicians and dentists for insured services continues to be MCHI Act. While section 7 of the MCHI Act provides that physicians and dentists may not charge for insured services, there is no legislative provisions that speaks to the ability of physicians or dentists to levy block fees for uninsured services. The Newfoundland and Labrador Medical Association (NLMA) has published the Physicians Guide to Non-Insured Services, which provides guidance on third party requested services, other non-insured services, suggested fees and relevant policies.
Compensation agreements are negotiated between the government and the NLMA, on behalf of physicians, and the Newfoundland and Labrador Dental Association (NLDA) on behalf of dentists. A Memorandum of Agreement (MOA) was reached with the NLMA and signed on May 3, 2022. The link to the MOA can be found on the department's website. The current agreement with the NLDA was signed on May 4, 2022 for a four-year term (2022-2026). The signed agreements can also be found online on the department's website.
The MCHI Act authorizes the Minister to appoint auditors to audit the accounts and claims for payment submitted by physicians and dentists. The MCHI Act prescribes the power and duties of auditors, sets out the remedies available and details the processes to be followed. The MCHI Act also details the review and appeal processes available to practitioners.
5.3 Payments to hospitals
The department is responsible for funding NLHS space for ongoing hospital operations and capital acquisitions. Payments are made in accordance with the MCHI Act, the Provincial Health Authority Act and the Financial Administration Act. As part of their accountability to the department, NLHS is required to meet the department's annual reporting requirements, which include submitting an annual budget, pursuant to section 25 of the Provincial Health Authority Act, as well as audited financial statements and other financial and statistical information throughout the year as required.
6.0 Recognition given to federal transfers
Funding provided by the federal government through the Canada Health Transfer and the Canada Social Transfer has been recognized and reported by the Government of Newfoundland and Labrador in the annual provincial budget, through press releases, government websites, and various other documents. For fiscal year 2023–2024, these documents include the Public Accounts and Estimates 2023–2024. The Public Accounts and Estimates, tabled by the Government in the House of Assembly, are publicly available and are shared with Health Canada for information purposes.
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 1. Number as of March 31st | 526,151 | 522,484 | 528,143 | 529,682 | 533,567 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| Public facilities | |||||
| 2. Number | 103 | 106 | 106 | 108 | 111 |
| 3. Payments for insured health services ($) | 1,217,480,996 | 1,188,085,817 | 1,272,143,186 | 1,341,025,273 | 1,702,629,104 |
| Private for-profit facilities | |||||
| 4. Number of private for-profit facilities providing insured health services | 1 | 1 | 3 | 3 | 3 |
| 5. Payments to private for-profit facilities for insured health services ($) | 954,483 | 3,017,568 | 4,432,341 | 5,579,380 | 7,988,301 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 6. Total number of claims, in-patient | 1,685 | 1,387 | 1,160 | 1,293 | 1,821 |
| 7. Total payments, in-patient ($) | 24,194,946 | 19,577,883 | 20,075,920 | 19,353,495 | 40,157,671 |
| 8. Total number of claims, out-patient |
25,216 | 14,646 | 17,004 | 17,322 | 24,552 |
| 9. Total payments, out-patient ($) | 10,558,507 | 6,142,889 | 6,362,269 | 6,937,831 | 10,985,398 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| Pre-approved | |||||
| 10. Total number of claims, pre-approved in-patient | 9 | 9 | 1 | 0 | 1 |
| 11. Total payments, pre-approved in-patient ($) | 313,310 | 3,710,544 | 44,748 | 0 | 37,079 |
| 12. Total number of claims, pre-approved out-patient | 65 | 69 | 5 | 9 | 31 |
| 13. Total payments, pre-approved out-patient ($) | 455,264 | 520,539 | 8,192 | 33,504 | 361,029 |
| Non pre-approved | |||||
| 14. Total number of claims, non pre-approved in-patient | 126 | 33 | 14 | 37 | 40 |
| 15. Total payments, non pre-approved in-patient ($) | 138,708 | 67,200 | 13,530 | 45,920 | 64,210 |
| 16. Total number of claims, non pre-approved out-patient | 335 | 62 | 20 | 68 | 139 |
| 17. Total payments, non pre-approved out-patient ($) | 20,837 | 3,792 | 1,240 | 4,599 | 11,810 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 18. Number of participating physiciansFootnote 1 | 1,307 | 1,383 | 1,398 | 1,401 | 1,295 |
| 19. Number of opted-out physicians | 0 | 0 | 0 | 0 | 0 |
| 20. Number of non-participating physicians |
0 | 0 | 0 | 0 | 0 |
| 21. Total payments for services provided by physicians paid through all payment methods ($) | not available | not available | not available | not available | not available |
| 22. Total payments for services provided by physicians paid through fee-for-service ($) | 320,407,337 | 301,991,513 | 325,013,123 | 353,776,212 | 377,755,493 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 23. Number of services | 127,900 | 84,900 | 84,200 | 117,986 | 121,151 |
| 24. Total payments ($) | 8,714,768 | 6,298,511 | 5,605,881 | 8,104,719 | 8,556,682 |
| Insured physician services provided outside CanadaFootnote 2 | |||||
| Pre-approved | |||||
| 25. Number of pre-approved services | 2,509 | 1,001 | 226 | 609 | 599 |
| 26. Total pre-approved payments ($) | 434,941 | 179,048 | 132,418 | 139,680 | 79,664 |
| Non pre-approved | |||||
| 27. Number of non pre-approved services | not applicable | not available | not available | not available | not available |
| 28. Total non pre-approved payments ($) | not applicable | not available | not available | not available | not available |
| Insured surgical-dental services within own province or territory | |||||
| 29. Number of participating dentists | 17 | 17 | 13 | 19 | 20 |
| 30. Number of opted-out dentists | 0 | 0 | 0 | 0 | 0 |
| 31. Number of non-participating dentists |
0 | 0 | 0 | 0 | 0 |
| 32. Number of services provided | 4,097 | 2,888 | 4,752 | 5,265 | 4,752 |
| 33. Total payments ($) | 713,570 | 416,552 | 900,340 | 1,083,488 | 895,472 |
Footnotes
|
|||||
Prince Edward Island
In Prince Edward Island (PEI) the Department of Health and Wellness is responsible for providing policy, strategic, and fiscal leadership for the health care system.
The Health Services Act, R.S.P.E.I. 1988, Cap. H-1.6 provides the regulatory and administrative frameworks for improvements to the health care system in PEI by:
- mandating the creation of a provincial health plan;
- establishing mechanisms to improve patient safety and support quality improvement processes; and
- creating a Crown corporation (Health PEI) to oversee the delivery of operational health care services.
Within this governance structure Health PEI has the responsibility to:
- provide, or provide for the delivery of, health services;
- operate and manage health facilities;
- manage the financial, human and other resources necessary to provide health services and operate health facilities; and
- perform such other duties as the Minister may direct.
1.0 Public administration
1.1 Health care insurance plan and public authority
The Hospital Services Insurance Plan, under the authority of the Minister of Health and Wellness (the Minister), is the vehicle for delivering hospital care insurance in Prince Edward Island (PEI). The enabling legislation is the Hospital and Diagnostic Services Insurance Act R.S.P.E.I. 1988, Cap. H-8. The Medical Services Insurance Plan provides for insured physician services under the authority of the Health Services Payment Act R.S.P.E.I. 1988, Cap. H-2. Together, the plans insure services as defined under section 2 of the Canada Health Act. The Department of Health and Wellness (the Department) is responsible for providing policy, strategic, and fiscal leadership for the health care system, while Health PEI is responsible for service delivery and the operation of hospitals, health centres, manors and mental health facilities. Health PEI is responsible for the hiring of physicians, while the Public Service Commission of PEI hires nurse practitioners, nurses and all other health related workers.
1.2 Reporting relationship
An annual report is submitted by the Department to the Minister who tables it in the Legislative Assembly. The report provides information about the operating principles of the Department and its legislative responsibilities, as well as an overview and description of the operations of the departmental divisions and statistical highlights for the year. The most recent Health PEI annual report was for the 2022-2023 fiscal year, while the annual report for 2023-2024 is expected to be released later this year.
Health PEI prepares an annual business plan which functions as a formal agreement between Health PEI and the Minister responsible, and documents accomplishments to be achieved over the coming fiscal year. The Health PEI business plan for the 2023-2024 fiscal year was released in September, 2024.
1.3 Audit of accounts
The provincial Auditor General conducts annual audits of the public accounts of PEI. The public accounts of the province include the financial activities, revenues and expenditures of the Department.
The provincial Auditor General, through the Audit Act, R.S.P.E.I. 1988, c A-24, has the discretion to conduct further audit reviews on a comprehensive or program specific basis.
2.0 Comprehensiveness
2.1 Insured hospital services
Insured hospital services are provided under the Hospital and Diagnostic Services Insurance Act. The accompanying Regulations define the insured in-patient and out-patient hospital services available at no charge to a person who is eligible. Insured hospital services include, but are not limited to:
- necessary nursing services;
- laboratory, radiological, and other diagnostic procedures;
- accommodations and meals at a standard ward rate;
- formulary drugs, biologicals, and related preparations prescribed by an attending physician and administered in hospital;
- operating room, case room and anaesthetic facilities;
- routine surgical supplies; and
- radiotherapy and physiotherapy services performed in hospital.
The process to add a new hospital service to the list of insured services involves extensive consultation and negotiation between the Department of Health and Wellness (the Department), Health PEI and key stakeholders. The process involves the development of a business plan which, when approved by the Minister of Health and Wellness, would be taken to Treasury Board for funding approval. Executive Council (Cabinet) has the final authority in adding new services.
2.2 Insured physician services
The enabling legislation that provides for insured physician services is the Health Services Payment Act. Insured physician services are provided by medical practitioners licensed by the College of Physicians and Surgeons. The total number of practicing practitioners who billed the Medical Services Insurance Plan as of March 31, 2024, was 535. This includes all physicians (complement, locums, visiting specialists, and other non-complement physicians). Under section 10 of the Health Services Payment Act, a physician or practitioner who is not a participant in the Medical Services Insurance Plan is not eligible to bill the Plan for services rendered. When a non-participating physician provides a medically required service, section 10(2) requires that physicians advise patients that they are non-participating physicians or practitioners and provide the patient with sufficient information to enable recovery of the cost of services from the Department. Under section 10.1 of the Health Services Payment Act, a participating physician or practitioner may determine, subject to and in accordance with the Regulations and in respect of a particular patient or a particular basic health service, to collect fees outside the Plan or selectively opt out of the Plan. Before the service is rendered, patients must be informed that they will be billed directly for the service. Where practitioners have made that determination, they are required to inform the Minister thereof and the total charge is made to the patient for the service rendered.
As of March 31, 2024, no physicians had opted out of the Medical Services Insurance Plan.
All basic health services rendered by physicians that are medically required are covered by the Medical Services Insurance Plan. These include:
- most physicians' services in the office, at the hospital, or in the patient's home;
- medically necessary surgical services, including the services of anaesthetists and surgical assistants where necessary;
- obstetrical services, including pre-natal and post-natal care, newborn care, or any complications of pregnancy such as miscarriage or caesarean section;
- certain oral surgery procedures performed by an oral surgeon when it is medically required, with prior approval that they be performed in a hospital;
- sterilization procedures, both female and male;
- treatment of fractures and dislocations; and
- certain insured specialist services, when properly referred by an attending physician.
Services that are not covered as insured benefits include:
- specific examinations requested by a third-party (for example, pre-school examinations, employer examination, or insurance medicals);
- travel vaccines;
- preparation of testimony reports, doctor's certifications, etc., required for administrative or legal purposes;
- physician travel time;
- cosmetic surgery not deemed medically necessary;
- materials or drugs used in a physician's office;
- eye glasses or lenses or other appliances such as hearing aids, artificial limbs, or other devices;
- acupuncture and acupressure services;
- services provided outside of a hospital by audiologists, chiropodists, chiropractors, dietitians, homeopaths, naturopaths, optometrists, osteopaths, physiotherapists, podiatrists, psychologists, and services performed by a dentist;
- eye refraction examinations by family physicians; and
- reversal of sterilization process.
The process to add a physician service to the list of insured services involves negotiation between the Department, Health PEI, and the Medical Society of Prince Edward Island (PEI). The process involves development of a business plan which, when approved by the Minister, would be taken to Treasury Board for funding approval. Insured physician services may also be added or deleted as part of the negotiation of a new Master Agreement with the Medical Society of PEI (section 5.2). Cabinet has the final authority in adding new services. While negotiations for a new Master Agreement were underway in 2023-2024, no new insured physician services were added during this time.
2.3 Insured surgical-dental services
Most dental services are not insured under the Medical Services Insurance Plan. Only oral maxillofacial surgeons are paid through the Plan. There are currently three surgeons in that category. Surgical-dental procedures included as basic health services in the Tariff of Fees are covered only when the patient's medical condition requires that they be done in hospital or in an office with prior approval, as confirmed by the attending physician.
Any new surgical-dental services added to the list of insured services covered by the Medical Services Insurance Plan is done through negotiations of the Dental Agreement between the Department, Health PEI, and the Dental Association of PEI. In 2023–2024, no new services were added to the Dental Agreement.
2.4 Uninsured hospital, physician and surgical-dental services
Services not covered by the Medical Services Insurance Plan include:
- services that persons are eligible for under other provincial or federal legislation;
- mileage or travel, unless approved by Health PEI;
- telephone consultation except by internists, palliative care physicians, pediatricians, out-of-province specialists, and orthopedic surgeons, provided the patient was not seen by that physician within three days of the telephone consult;
- examinations required in connection with employment, insurance, education, etc.;
- group examinations, immunizations or inoculations, unless prior approval is received from Health PEI;
- preparation of records, reports, certificates or communications, except a certificate of committal to a psychiatric, drug or alcoholism facility;
- testimony in court;
- travel clinic and expenses;
- surgery for cosmetic purposes unless medically required;
- dental services other than those procedures included as basic health services;
- dressings, drugs, vaccines, biologicals, and related materials;
- eyeglasses and special appliances;
- chiropractic, podiatry, optometry, chiropody, osteopathy, naturopathy, and similar treatments;
- physiotherapy, psychology, and acupuncture except when provided in hospital;
- reversal of sterilization procedures;
- in-vitro fertilization;
- services performed by another person when the supervising physician is not present or not available;
- services rendered by a physician to members of the physician's own household, unless approval is obtained from Health PEI; and
- any other services that the Department may, upon the recommendation of the negotiation process between the Department, Health PEI, and the Medical Society, declare non-insured.
Hospital services not covered by the Hospital Services Insurance Plan include:
- private or special duty nursing at the patient's or family's request;
- preferred accommodation at the patient's request;
- hospital services rendered in connection with surgery purely for cosmetic reasons;
- personal conveniences, such as telephones and televisions;
- drugs, biologicals, and prosthetic and orthotic appliances for use after discharge from hospital; and
- dental extractions, except in cases where the patient must be admitted to hospital for medical reasons with prior approval of Health PEI.
The process to de-insure services covered by the Medical Services Insurance Plan is done in collaboration with the Department, Health PEI, and the Medical Society of PEI. No services were de-insured during the 2023–2024 fiscal year.
All Prince Edward Island residents have equal access to services. Third parties such as private insurers or the Workers' Compensation Board of PEI do not receive priority access to services through additional payment.
PEI has no formal process to monitor compliance; however, feedback from physicians, hospital administrators, medical professionals, and staff allows the Department and Health PEI to monitor usage and service concerns.
3.0 Universality
3.1 Eligibility
The Health Services Payment Act and the Hospital and Diagnostic Services Insurance Act, define eligibility for the Medical Services Insurance Plan and the Hospital Services Insurance Plan respectively. These plans are designed to provide coverage for eligible Prince Edward Island (PEI) residents. A resident is anyone legally entitled to remain in Canada and who makes his or her home and is ordinarily present on an annual basis for at least six months plus a day in PEI. While there is no formal appeal process, an individual can seek clarification regarding their eligibility determination.
All new residents must register with Health PEI in order to become eligible. Persons who establish permanent residence in PEI from elsewhere in Canada will become eligible for insured hospital and medical services on the first day of the third month following the month of arrival. PEI currently does not have a process where a resident can opt out of the health care insurance plan.
Residents who are ineligible for insured hospital and medical services coverage in PEI are those who are eligible for certain services under other federal or provincial government programs, such as members of the Canadian Forces, inmates of federal penitentiaries, and clients of Workers' Compensation or the Department of Veterans Affairs' programs.
Ineligible residents may become eligible in certain circumstances. For example, members of the Canadian Forces become eligible on discharge or completion of rehabilitative leave. Penitentiary inmates become eligible upon release. In such cases, the province where the individual in question was stationed at the time of discharge or release, or release from rehabilitative leave, would provide initial coverage during the customary waiting period of up to three months. Parolees from penitentiaries will be treated in the same manner as discharged prisoners.
New or returning residents must apply for health coverage by completing a registration application from Health PEI. The application is reviewed to ensure that all necessary information is provided. A health card is issued and sent to the resident within two weeks of becoming eligible. Renewal of coverage takes place every five years and residents are notified by mail six weeks before renewal.
The number of residents registered with the Medical Services Insurance Plan and the Health Services Insurance Plan in PEI as of March 31, 2024, was 171,708.
3.2 Other categories of individuals
Foreign students, tourists, transients, or visitors to PEI do not qualify as residents of the province and are, therefore, not eligible for hospital and medical insurance benefits.
Temporary workers, refugees, and Minister's Permit holders are not eligible for hospital and medical insurance benefits.
4.0 Portability
4.1 Minimum waiting period
Insured persons who move to Prince Edward Island (PEI) from another province or territory in Canada are eligible for health insurance on the first day of the third month following the month of arrival in the province.
4.2 Coverage during temporary absences in Canada
Residents absent each year for any reasons must reside in PEI for at least six months plus a day each year in order to be eligible for sudden illness and emergency services while absent from the province, as allowed under section 11 of the Health Services Payment Act Regulations. A person, including a student, who is temporarily absent from the province for up to 182 days in a 12 month period must notify Health PEI before leaving.
PEI participates in the Hospital Reciprocal Billing Agreements and the Medical Reciprocal Billing Agreements along with other jurisdictions across Canada.
4.3 Coverage during temporary absences outside Canada
The Health Services Payment Act is the enabling legislation that defines portability of health insurance during temporary absences outside of Canada, as allowed under section 11 of the Regulations thereunder.
Persons must reside in PEI for at least six months plus a day each year in order to be eligible for sudden illness and emergency services while absent from the province, as allowed under section 11 of the Health Services Payment Act Regulations.
Insured residents may be temporarily out of the country for up to a 12 month period in some circumstances.
Students attending a recognized learning institution in another country must provide proof of enrollment from the educational institution on an annual basis. Students must notify Health PEI upon returning from outside the country.
For PEI residents leaving the country for work purposes for longer than one year, coverage ends the day the person leaves.
For PEI residents travelling outside Canada, coverage for emergency or sudden illness will be provided at PEI rates only, in Canadian currency. Residents are responsible for paying the difference between the full amount charged and the amount paid by Health PEI.
4.4 Prior approval requirement
Prior approval is required from Health PEI before receiving non-emergency, out-of-province medical or hospital services. Island residents seeking such required services may apply for prior approval through a PEI physician. If approval is not granted, a letter can be submitted to Health PEI to appeal a medical insurance decision. Full coverage may be provided for (PEI insured) non-emergency or elective services, provided the physician completes an application to Health PEI. Prior approval is required from the Medical Director of Health PEI to receive out-of-country hospital or medical services not available in Canada.
5.0 Accessibility
5.1 Access to insured health services
Both of Prince Edward Island's (PEI) Hospital Services Insurance Plan and the Medical Services Insurance Plan provide services on uniform terms and conditions on a basis that does not impede or preclude reasonable access to those services by insured persons. While there is no formal complaints process for inappropriate charges, an individual can seek clarification on the appropriateness of any charges through the Department of Health and Wellness (the Department). The Department can be contacted at:
Prince Edward Island Department of Health and Wellness
P.O. Box 2000
Charlottetown, PEI
C1A 7N8
902-368-6414
PEI has a publicly administered and funded health system that guarantees universal access to medically necessary hospital and physician services as required by the Canada Health Act.
The Government of PEI recognizes that the health system must constantly adapt and expand to meet the needs of residents.
Several examples of initiatives and accomplishments from the 2023–2024 fiscal year include:
- Five-year Provincial Health Plan launched, including four priorities:
- keeping our Island healthy;
- a seamless experience: right time, right place, right care;
- to have equitable access, and;
- a healthy and sustainable workforce.
- Physician recruitment: 24 physicians (family physicians and specialists) were hired during the 2023 calendar year.
- Associate physicians and physician assistants are now permitted to be licensed and to practice in PEI, providing more support to physicians and helping to improve access to care for Islanders. One new physician assistant was hired in 2023-2024.
- 9 Nurse Practitioners, 201 registered nurses and 265 Resident care workers, personal care workers, and home support workers were hired between January 2023 and November 2023.
- Seven Patient Medical Homes (PMHs) providing team-based care and improved access to Primary Care services were added, for a current total of 17 PMHs across the province.
- Three primary care access clinics (PCACs) providing additional options for access health care services were added, for a current total of five PCACs across the province.
- The Department of Health and Wellness and Health PEI have partnered with the Department of Transportation and Infrastructure to assist Islanders seeking to apply for PEI health cards, register for the patient registry and register for access to virtual care. These services are now available at Access PEI locations across PEI.
- The number of drugs covered under the provincial formulary was expanded to over 100 new drugs. Out-of-pocket expenses for Islanders accessing necessary drugs through provincial drug programs were reduced.
- A new Mental Health and Additions Emergency Department was launched.
5.2 Physician compensation
A collective bargaining process is used to negotiate physician compensation. Bargaining teams are appointed by both physicians and the government to represent their interests in the process. The current five-year Master Agreement between the Medical Society of PEI, the Department and Health PEI covers the period from April 1, 2024, to March 31, 2029.
Many physicians continue to work on a fee-for-service basis; however, alternate payment plans have been developed and some physicians receive salary, contract and sessional payments. Alternate payment modalities are expanding and seem to be the preference for new graduates. Currently, 74 per cent of PEI's physicians (excluding locums and visiting specialists) are compensated under an alternate payment method (non-fee-for-service) as their primary means of remuneration. These methods include salaried (52 per cent), sessional (13 per cent) and contract for service (9 per cent).
The legislation governing payments to physicians and dentists for insured services is the Health Services Payment Act. Health PEI is responsible for auditing physician claims for compliance with legislative requirements and the Master Agreement tariff, as permitted under the Health Services Payment Act and delegated by the Minister. The Health Services Payment Act allows for audits of physician payments to assist in efficient and effective use of resources. Health PEI's audit rights are affirmed in the Master Agreement with the Medical Society of PEI. Health PEI approved its Practitioner Claims Monitoring, Compliance, and Recovery Policy on December 22, 2015, and continues to conduct physician payment audits on a go-forward basis. The policy information was communicated to physicians in January 2016.
Physicians submit bills for services provided to insured residents to Health PEI's Claims Payment System (CPS). The CPS contains billing rules aligned with the Master Agreement which help to ensure billings which do not meet Master Agreement criteria are rejected or flagged for review. As part of Health PEI's monitoring process, physicians are randomly selected and requested to provide Health PEI with documentation to support sample billings. Overall physician billings are periodically reviewed to identify unusual billing profiles when compared to peers, significant increases in fee code billings and irregularities in the use of new fee codes. Any irregularities discovered may trigger an audit.
The audits include specific steps for:
- risk-ranking physicians based on unusual billing profiles compared to peers and other factors;
- auditing samples of claims documentation in the physician's office;
- statistical extrapolation of results to estimate any recovery of overbillings; and
- communication of audit results and any recovery via a letter to the physician.
The Health Services Payment Act allows for recovery of overpayments and provides for appeal of adjustments to claims. The initial stage for appeal is a discussion with the Executive Director, Medical Affairs or designate. If no agreement can be reached, the matter is appealed to the Health Services Payment Advisory Committee which will provide a recommendation to the Minister.
5.3 Payments to hospitals
Payments (advances) to provincial hospitals and community hospitals for hospital services are approved for disbursement by the Department in line with cash requirements and are subject to approved budget levels.
The usual funding method includes using a global budget adjusted annually to take into consideration increased costs related to such items as labour agreements, drugs, medical supplies, and facility operations.
6.0 Recognition given to federal transfers
The Government of Prince Edward Island (PEI) strives to recognize the federal contributions provided through the Canada Health Transfer whenever appropriate. Over the past year, this has included reference in public documents such as the Province of PEI 2023–2024 Annual Budget and in the 2023–2024 Public Accounts, both of which were tabled in the Legislative Assembly and are publicly available to PEI residents.
It is also the intent of the Department of Health and Wellness to recognize this important contribution in the 2023–2024 Annual Report.
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
| 1. Number as of March 31st | 154,728 | 160,279 | 157,157 | 160,356 | 171,708 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| Public facilities | |||||
| 2. Number | 7 | 7 | 7 | 7 | 7 |
| 3. Payments for insured health services ($) | 235,449,936 | 248,936,875 | 260,481,548 | 277,119,271 | 296,212,423 |
| Private for-profit facilities | |||||
| 4. Number of private for-profit facilities providing insured health services | 0 | 0 | 0 | 0 | 0 |
| 5. Payments to private for-profit facilities for insured health services ($) | 0 | 0 | 0 | 0 | 0 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 6. Total number of claims, in-patient | 2,853 | 2,183 | 1,958 | 2,042 | 2,620 |
| 7. Total payments, in-patient ($) | 30,439,891 | 21,258,749 | 24,442,346 | 26,197,286 | 33,830,752 |
| 8. Total number of claims, out-patient | 19,373 | 13,976 | 14,977 | 15,989 | 17,109 |
| 9. Total payments, out-patient ($) | 8,670,798 | 6,411,393 | 6,281,510 | 7,176,808 | 8,497,819 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| Pre-approved | |||||
| 10. Total number of claims, pre-approved in-patient | 3 | 2 | 1 | 3 | 1 |
| 11. Total payments, pre-approved in-patient ($) | 34,465 | 566,727 | 2,314 | 27,763 | 56,887 |
| 12. Total number of claims, pre-approved out-patient | 6 | 3 | 2 | 0 | 9 |
| 13. Total payments, pre-approved out-patient ($) | 642 | 360,228 | 901 | 0 | 3,082 |
| Non pre-approved | |||||
| 14. Total number of claims, non pre-approved in-patient | 30 | 3 | 13 | 16 | 18 |
| 15. Total payments, non pre-approved in-patient ($) | 110,913 | 567,931 | 82,894 | 132,776 | 126,519 |
| 16. Total number of claims, non pre-approved out-patient | 95 | 12 | 14 | 9 | 0 |
| 17. Total payments, non pre-approved out-patient ($) | 50,255 | 5,012 | 4,368 | 4,033 | 0 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 18. Number of participating physicians | 416 | 409 | 462 | 484 | 535 |
| 19. Number of opted-out physicians | 0 | 0 | 0 | 0 | 0 |
| 20. Number of non-participating physicians |
0 | 0 | 0 | 0 | 0 |
| 21. Total payments for services provided by physicians paid through all payment methods ($) | 85,915,289 | 92,021,323 | 94,718,265 | 98,552,852 | 105,183,955 |
| 22. Total payments for services provided by physicians paid through fee-for-service ($) | 73,456,751 | 75,081,965 | 80,413,122 | 81,757,968 | 86,310,935 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 23. Number of services | 124,520 | 105,503 | 113,185 | 129,002 | 138,109 |
| 24. Total payments ($) | 12,740,969 | 11,041,025 | 11,606,231 | 12,983,065 | 14,479,310 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| Pre-approved | |||||
| 25. Number of pre-approved services | 10 | 241 | 2 | 2 | 58 |
| 26. Total pre-approved payments ($) | 1,641 | 119,191 | 12,887 | 5,093 | 60,974 |
| Non pre-approved | |||||
| 27. Number of non pre-approved services | 262 | 29 | 63 | 118 | 177 |
| 28. Total non pre-approved payments ($) | 59,715 | 2,490 | 8,257 | 9,704 | 15,777 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 29. Number of participating dentists | 4 | 4 | 3 | 3 | 3 |
| 30. Number of opted-out dentists | 0 | 0 | 0 | 0 | 0 |
| 31. Number of non-participating dentists | 0 | 0 | 0 | 0 | 0 |
| 32. Number of services provided | 401 | 451 | 486 | 508 | 496 |
| 33. Total payments ($) | 164,239 | 133,800 | 156,621 | 154,301 | 143,749 |
Nova Scotia
The Nova Scotia Department of Health and Wellness (the Department) vision and mission are:
Vision: Healthy Nova Scotians
Mission: To lead a quality, equitable and sustainable health care system that inspires and promotes the health and well-being of all people in Nova Scotia.
The health and wellness system includes the delivery of health care as well as the prevention of disease and injury and the promotion of health and healthy living. The Health Authorities Act establishes roles and responsibilities of the Department, the Nova Scotia Health Authority, and the IWK Health Centre.
The Department is responsible for providing leadership and ensuring accountability for funding for the health system. The Department includes the Office of Healthcare Professional Recruitment and continues to work alongside the Office of Addictions and Mental Health and the Department of Seniors and Long-term Care.
The Nova Scotia Health Authority and the IWK Health Centre are responsible for governing, managing, and providing health services in the province and engaging with the communities they serve.
Insured services in Nova Scotia cover hospital services and physician services. Services such as home care, long-term care, and pharmaceutical supports are also provided.
Nova Scotia continues to be committed to the delivery of hospital services and medically required services consistent with the principles of the Canada Health Act.
Health system transformation is the priority of the Department in 2023-24. Through the Action for Health strategic plan, government has articulated a multi-year roadmap to transform the health system.
- Action for Health provides a framework, identifying the priorities for the year, in partnership with the Office of Addictions and Mental Health (OAMH), the Office of Healthcare Professionals Recruitment, the Nova Scotia Health Authority (NSHA) and the IWK Health Centre; and
- Outlines solutions for creating a world-class health system that will be ready when Nova Scotians need it, is responsive to their needs and provides reliable care they can count on.
A whole-of-government approach is being taken to deliver Action for Health and it requires integrated, system-wide solutions and investments to change the trajectory of our health system in Nova Scotia. Action for Health focuses on innovation and finding new ways to address long-standing generational issues within the health system.
Additional information related to health care in Nova Scotia may be obtained from the Department of Health and Wellness website.
1.0 Public administration
1.1 Health care insurance plan and public authority
Two plans cover insured health services in Nova Scotia: The Hospital Insurance Plan and the Medical Services Insurance (MSI) Plan which both operate under the Health Services and Insurance Act (HSIA).
The Nova Scotia Department of Health and Wellness (the Department) administers the Hospital Insurance Plan, and the MSI Plan is administered and operated by Medavie Blue Cross (MBC) on behalf of the Minister of Health and Wellness.
Amendments made to the HSIA in fall 2023 provide specific authority to the Minister of Addictions and Mental Health to establish insured health services programs for addictions and mental health.
Section 8 of the HSIA gives the Minister of Health and Wellness and the Minister of Addictions and Mental Health the power to enter into agreements and vary, amend or terminate the same agreements with such person or persons as the Minister deems necessary to establish, implement, and carry out the MSI Plan. An amendment made to the HSIA in fall 2023, which came into force in April 2024, removed a previous requirement for either Minister to obtain approval of Governor in Council before using the authority provided in Section 8.
The Department and MBC entered into a service level agreement in 2005 and negotiated a new agreement in June 2021. Under the agreement, MBC is responsible for operating and administering the MSI and Pharmacare Programs, including health card registration, resident services, payments to physicians, prescription monitoring and pharmacare programs, and ancillary programs such as optometry and prosthetics.
The administration and operation of insured dental services is provided by Green Shield Canada under an agreement with the Department.
The Hospitals Regulations were amended on September 12, 2023, and January 16, 2024, to add two privately-operated eye health centres to the list of approved hospitals, to permit delivery of publicly funded outpatient health services in those facilities.
In 2023-2024, no amendments were made to the Medical Services Insurance Regulations.
1.2 Reporting relationship
- Hospital Insurance
Section 17(1)(i) of the Health Services and Insurance Act, and sections 11(1) and 12(1) of the Hospital Insurance Regulations, under this Act, set out the terms for reporting by hospitals and hospital boards to the Minister of Health and Wellness.
- Medical Insurance
In the service level agreement between MBC and the Department, MBC is obliged to provide reports to the Department under various Statements of Requirements as listed in the contract. MBC is audited every year on various areas of reporting. MBC provides audited financial statements for the fiscal year ending March 31st and the statements are provided within four months of the fiscal year end.
1.3 Audit of accounts
The Auditor General audits the provincial financial statements. Under its service level agreement with the Department, MBC provides audited financial statements of MSI costs to the Department. The Auditor General and the Department have the right to perform audits of the administration of the agreement with MBC.
Within the Physician Services portfolio there are various programs that are audited by third parties that submit financial statements to the Department. This includes financial statements from the Dalhousie Family Medicine training sites and the Practice Ready Assessment program. Additionally, MBC conducts audits of claims submitted by physicians for insured services and of alternative funding contracts as Academic Funding Plans.
On behalf of the Minister of Health and Wellness, the service provider that operates Nova Scotia's out-of-hospital emergency medical services (Emergency Health Services [EHS] 911 Ground Ambulance, EHS Critical Care Transport, and non-emergent EHS Mobile Integrated Health Services) and 811 Telehealth services is required to submit audited financial statements each year and they are due 90 days after March 31st. The Department also receives audited financial statements from various other service providers including Nova Scotia Hearing and Speech Centres and Canadian Blood Services, but there is no set deadline for these statements.
Under section 36(4) of the Health Authorities Act, a health authority is required to submit to the Minister of Health and Wellness, no later than June 30 each year, an audited financial statement for the preceding fiscal year.
In addition to the annual audit of the Provincial Financial Statements, the Auditor General conducts performance audits on a variety of programs. The most recent Auditor General audits on the Department of Health and Wellness were:
- Value For Money: Development of Transitional Care Facilities (February 2024);
- QEII New Generation Project - Halifax Infirmary Expansion and Community Outpatient Centre - Phase II (July 2020);
- QEII New Generation Project – Halifax Infirmary Expansion and Community Outpatient Centre (December 2019, Chapter 2);
For further details please visit the Office of the Auditor General of Nova Scotia's website.
1.4 Designated agency
MBC administers monies to pay physician accounts as per the service agreement with the Department. Physician rates of pay are set based on the Physician Agreement negotiated with Doctors Nova Scotia (the sole negotiating body for physicians in Nova Scotia) and the Clinical Academic Funding Plan, which is negotiated with Doctors Nova Scotia, Dalhousie University, the Nova Scotia Health Authority, and the IWK Health Centre.
MSI is the provincial plan of insured medical services. It is designed to pay for a wide range of medically necessary physicians' services, as well as certain clinical pharmacy, dental and optometric services.
The Department and the Office of the Auditor General, have the right, under the terms of the service level agreement with MBC, to audit all MSI and Pharmacare transactions.
Green Shield Canada administers and has the authority to receive monies to pay dentists under a service level agreement with the Department. The tariff of dental fees is negotiated between the Nova Scotia Dental Association and the Department.
As part of an agreement with the Department, Green Shield Canada also provides monthly, quarterly and annual reports with regard to dental programs in Nova Scotia. This includes hospital dental services when the hospital setting is required for the safe performance of the procedure. These reports address provider claims and payments, program utilization, and audits. A complete list of reports can be obtained from the Department.
MBC is responsible for providing a number of regular and ad hoc reports to the Department pertaining to health card administration, physician claims activity, financial monitoring, provider management, audit activities, and program utilization. These reports are submitted on a monthly, quarterly, or annual basis. A complete list of reports can be obtained from the Department.
2.0 Comprehensiveness
2.1 Insured hospital services
The enabling legislation that provides for insured hospital services in Nova Scotia is the Health Services and Insurance Act. Hospital Insurance Regulations are made pursuant to the Act.
Under the Hospital Services Insurance Plan, in-patient services include:
- accommodation and meals at the standard ward level;
- necessary nursing services;
- laboratory, radiological, and other diagnostic procedures;
- relevant drugs, biologicals and related preparations;
- use of operating room(s), case room(s), and anaesthetic services;
- routine surgical supplies;
- use of radiotherapy and physiotherapy facilities;
- services rendered by persons who receive remuneration therefore from the hospital; and
- blood or therapeutic blood fractions.
Out-patient services include:
- laboratory, radiological, and electroencephalographic examinations;
- diagnostic procedures involving the use of radioactive isotopes;
- use of radiotherapy facilities for the treatment of malignancy;
- use of physiotherapy facilities;
- necessary nursing services;
- specific services and supplies when used for emergency diagnosis and treatment, within 48 hours after an accident;
- blood or therapeutic blood protein fractions;
- specific services and supplies in connection with relevant minor medical and surgical procedures;
- relevant drugs, biologicals and related preparations;
- hospital services, where available, including necessary meals, in connection with a day patient care clinic for the necessary training and instruction of diabetics;
- hemodialysis;
- ultrasonic diagnostic procedures;
- the non-medical component (excluding drugs, biologicals and related preparations) of all other general diagnostic and treatment procedures (excluding dental procedures);
- radiotherapy for non-malignant conditions;
- electrocardiograms;
- psychiatric services which are not medical services;
- services provided by and within Hearing and Speech Nova Scotia;
- home parenteral nutrition;
- equipment for the treatment of erythromelalgia;
- continuous ambulatory peritoneal dialysis; and
- chimeric antigen receptor T-cell (CAR T) therapy.
Each year, the Nova Scotia Health Authority and the IWK Health Centre submit business plans outlining budgets and priorities for the coming year to ensure safe and high-quality access to care. Under the Health Authorities Act, business plans are to be submitted on November 1st every year and are approved by the Minister of Health and Wellness.
2.2 Insured physician services
The legislation covering the provision of insured physician services in Nova Scotia is the Health Services and Insurance Act, sections 3(2), 5, 8, 13, 13A, 17(2), 22, 27–31, 35, and the Medical Services Insurance Regulations.
As of March 31, 2024, 3,022 physicians were paid through the Medical Services Insurance (MSI) Plan.
Physicians retain the ability to opt in or out of the MSI Plan. To opt out, a physician notifies MSI and relinquishes their billing number. MSI reimburses patients who pay the physician directly due to opting out. As of March 31, 2024, no physicians had opted-out of the MSI Plan to pursue this method of remuneration.
Insured services include those that are medically necessary. Payment is provided for the following physicians' services, when medically necessary, which can include:
- services in the physician's office, at the hospital, or in the home;
- all necessary surgical services, including the services of anesthetists and surgical assistants, when necessary;
- complete obstetrical care, including pre-natal care, confinement, caesarean section, post-natal and newborn care, and any complications of pregnancy, such as miscarriage;
- sterilization procedures, both male and female;
- gender-affirming care;
- treatment of fractures and dislocations;
- all necessary referred specialist services, including consultations (Please see the paragraph below on specialist services);
- all necessary diagnostic services except those that are available under the Insured Hospital Services;
- physical examinations, when deemed medically necessary;
- supervision of home dialysis;
- well baby care; and
- pap smears and other preventative measures.
If, in the opinion of the physician, a patient requires the services of a specialist for either consultation or care, a referral to the specialist is made. Payment at the specialist tariff is based on a valid referral by the attending physician.
In 2023–2024, Nova Scotia made permanent virtual care to allow physicians to bill for insured non-procedural services provided over the phone or another virtual platform. This was done through changes in Nova Scotia's 'Provision of Publicly Funded Virtual Health Services' policy.
The Fee Committee is outlined in article 4(d) of the 2023 Physician Agreement. The Fee Committee is a collaborative structure made up of the Department, Nova Scotia Health Authority, and Doctors Nova Scotia. The Committee reviews requests for new fees, amendments to current fees, and for additions, revision, or clarification of the Preamble to the MSI Physician manual. The Fee Committee provides advice and recommendations to the Physician Agreement Management Group on all matters pertaining to the fee schedule, based on consensus and available budget. If the fee is approved, Medavie Blue Cross is directed to add the new fee to the schedule of insured services payable by the MSI Plan.
Public consultations are not generally undertaken when listing or delisting insured medical services.
2.3 Insured surgical-dental services
To provide insured surgical-dental services under the Health Services and Insurance Act, dentists must be registered members of the Nova Scotia Dental Association, must be certified competent in the practice of dental surgery, and must also have privileges from the health authorities to deliver services at specific hospitals. The Health Services and Insurance Act provides that a dentist may choose not to participate in the MSI Plan. To participate, a dentist must register with MSI. A participating dentist who chooses not to participate must advise MSI in writing and is then no longer eligible to submit claims to MSI. In 2023–2024, 17 dentists were paid through the MSI Plan for providing insured surgical-dental services.
Insured surgical-dental services must be provided in a public health care facility, are detailed in the Department Dentists Guide, and are reviewed annually. Services under this program are insured when the condition of the patient is such that it is medically necessary for the procedure to be done in a public hospital and the procedure is of a surgical nature.
Generally included as insured surgical-dental services are extractions (where there exists radiographic evidence of infection or destruction of adjacent tooth and bone and for removal of impacted teeth where there exists radiographic evidence of infection, or destruction of adjacent tooth and bone) and oral and maxillofacial surgery. Requests for an addition to the list of surgical-dental services are accomplished through the Nova Scotia Dental Association, which submits a proposal to the Department. In consultation with experts in the field, the Department renders a decision on the addition of the procedure as an insured service. Public consultations are not undertaken during the consideration of additions to the list of insured services.
Insured services in the "other extraction services" (routine extractions) category are approved for the following groups of patients: cardiac patients, transplant patients, immunocompromised patients, and radiation patients. This is the case only when patients are undergoing active treatment in a hospital setting and the medical procedure must require the removal of teeth in a manner that would otherwise be considered routine extractions. Routine extractions of wisdom teeth and extractions for crowding purposes are not insured under prevention alone.
Currently, there are no known opted-out dentists and no known non-participating dentists providing insured surgical-dental services.
2.4 Uninsured hospital, physician and surgical-dental services
Uninsured hospital services include:
- preferred accommodation at the patient's request;
- telephones;
- televisions;
- drugs and biologicals ordered after discharge from hospital;
- cosmetic surgery;
- reversal of sterilization procedures;
- in-vitro fertilization;
- procedures performed as part of clinical research trials;
- services such as gastric bypass for morbid obesity, breast reduction/augmentation, and newborn circumcision (these services may be insured when approved as special consideration for medical reasons only); and
- services not deemed medically necessary that are required by third parties, such as insurance companies.
Uninsured physician services include:
- services available to residents of Nova Scotia who are covered under any statute or law of any other jurisdiction, either within or outside of Canada;
- diagnostic, preventive, or other physician's services available through the Nova Scotia Hospital Insurance Program, the Department, or other government agencies;
- services at the request of a third party;
- provision of a prescription or a requisition for a diagnostic or therapeutic service provided to a patient without a clinical evaluation;
- physician's services provided to their own families;
- services performed for cosmetic purposes only;
- group immunizations performed without prior approval by MSI;
- acupuncture;
- electrolysis;
- reversal of sterilization;
- in-vitro fertilization;
- provision of travel vaccines;
- newborn circumcision;
- release of tongue tie in newborn;
- removal of cerumen, except in the case of a febrile child;
- treatment of warts or other benign conditions of the skin;
- comprehensive visits when there are no signs, symptoms, or family history of disease or disability;
- services, supplies, and other materials not part of office overhead, including for example, photocopying or other costs associated with transfer of records;
- items such as drugs, dressings, and tray fees;
- physician's advice by telephone, letter, fax or email, with exceptions; and
- mileage or travelling time.
Major third-party agencies currently purchasing medically required health services in Nova Scotia include the Workers' Compensation Board and the Department of National Defence.
All residents of the province are entitled to services covered under the Health Services and Insurance Act. If enhanced goods and services, such as fibreglass casts, are offered as an alternative, the specialist or physician is responsible to ensure that the patient is aware of their responsibility for the cost. Patients are not denied service based on their inability to pay. The province provides alternatives to any of the enhanced goods and services.
The Department carefully reviews all patient complaints or public concerns that may indicate that the general principles of insured services are not being followed.
If a service or procedure is deemed by the Department not to be medically required, it is removed from the physician fee schedule and will no longer be reimbursed to physicians as an insured service. Once a service has been de-insured, all procedures and testing relating to the provision of that service also become de-insured. The same also applies to dental services and hospital services. Public consultations are not undertaken during the determination of medical necessity and de-listing of insured services. Consultation with the Nova Scotia Dental Association has preceded past de-listing of dental services. The last time there was any significant de-listing of services was in 1997.
3.0 Universality
3.1 Eligibility
Eligibility for insured health care services in Nova Scotia is outlined under section 2 of the Hospital Insurance Regulations and the Health Services for Foreign Workers, International Students and Armed Forces Families Regulations, made pursuant to section 17 of the Health Services and Insurance Act. All residents of Nova Scotia are eligible. A resident is defined as anyone who is legally entitled to stay in Canada and who makes their home and is ordinarily present in Nova Scotia. Registration for the hospital and medical insurance plans is voluntary and residents may choose not to register.
In 2023-2024, an individual was considered to be "ordinarily present" in Nova Scotia if they:
- make their permanent home in Nova Scotia;
- are physically present in Nova Scotia for at least 183 days in any calendar year; and
- are not a tourist, transient or visitor.
Residents who are a Canadian citizen or "Permanent Resident" as defined by Immigration, Refugees and Citizenship Canada (IRCC) must be ordinarily present in Nova Scotia to remain eligible.
Children born out-of-country to Nova Scotia residents are eligible for coverage provided their parents meet the Nova Scotia residency requirements.
Individuals moving to Nova Scotia from another Canadian province will normally be eligible for Medical Services Insurance (MSI) on the first day of the third month following the month of their arrival. Individuals moving permanently to Nova Scotia from another country are eligible on the date of their arrival in the province, provided they are Canadian citizens or Permanent Residents as defined by IRCC.
Individuals insured under the Workers' Compensation Act, or any other act of the Legislature or of the Parliament of Canada, or under any statute or law of any other jurisdiction either within or outside of Canada, are not eligible for Hospital Insurance Plan and the MSI Plan coverage (such as members of the Canadian Armed Forces, federal inmates and some classes of refugees). Once an individual is no longer covered under any of the acts, statutes or laws noted above, they are then eligible to apply for and receive Nova Scotia health insurance coverage, provided that they are either a Canadian citizen, a Permanent Resident as defined by IRCC or meet the Nova Scotia residency requirements. An administrative review may be requested for individuals who are deemed ineligible.
In 2023-2024, the total number of residents registered with the health insurance plan was 1,127,280.
The eligibility criteria for Nova Scotia Health Insurance Program policy is under review.
3.2 Other categories of individuals
Other individuals may be eligible for insured health care services in Nova Scotia if they meet specific eligibility criteria listed below:
Immigrants: Individuals moving from another country to live permanently in Nova Scotia are eligible for health care on the date of arrival if they arrive as a Permanent Resident, as determined by IRCC.
Non-Canadians married to Canadian Citizens or Permanent Residents: Individuals who possess the required documentation from IRCC indicating they have applied for permanent residency, will be eligible for coverage on the date of arrival in Nova Scotia (if applied prior to their arrival in Nova Scotia), or the date of application for permanent residency (if applied after their arrival in Nova Scotia). A copy of their marriage certificate is required.
Convention refugees or persons in need of protection: Individuals who possess the required documentation from IRCC indicating they have applied for permanent residency will be eligible for coverage on the date of application for permanent residency.
In 2023-2024, there were 84,764 Permanent Residents registered with the Health Insurance Program.
Refugees: Refugees are eligible once they have been granted Permanent Resident status by IRCC, or if they possess either a work permit or study permit.
Canadian Armed Forces: Spouses, common-law partners and dependants of Canadian Armed Forces members are eligible on the date they become a resident of Nova Scotia.
North Atlantic Treaty Organization (NATO): Spouses, common-law partners and dependants of NATO nation members, other than the United States of America, are eligible on the date they became a resident of Nova Scotia. The member must provide a work permit or letter from their NATO commanding officer and meet all other work permit eligibility requirements in order for their spouse and dependants to be eligible.
Repatriated Canadians: Persons who are Canadian citizens or Permanent Residents are eligible on the date they become a resident of Nova Scotia.
Work Permits: Persons moving to Nova Scotia from outside the country who possess a work permit, or an employment contract with a Nova Scotia employer, are eligible on the date they become a resident of the Province, provided they will be remaining in Nova Scotia for at least one full year and sign a residency declaration. Workers must be physically present in the Nova Scotia for 90 days after arrival and cannot be absent for more than 183 days unless the absence is required for employment reasons. MSI coverage is extended for a maximum of 12 months at a time. Each year, a copy of their renewed immigration document must be presented, and a declaration signed. Spouses, common-law partners and dependants who are legally entitled to remain in Canada are eligible on the same basis as the worker.
Once coverage has terminated, the worker is to be treated as never having qualified for health services coverage and must comply with eligibility requirements before coverage is extended to them, their spouse, common-law partner and dependants.
Religious Workers: Foreign religious workers are eligible for the same coverage as those with work permits. Visitor visas (Case Type 13 or Case Type 10) indicating the person is a religious worker are accepted in place of work permits.
Seasonal Workers: Seasonal workers, their spouses, common-law partners and dependants are eligible for the same coverage as those with work permits provided the permit is valid for at least 12 months.
In 2023-2024, there were 29,251 individuals with work permits covered under the Health Insurance Program.
Study Permits: Individuals moving to Nova Scotia from another country and who possess a study permit are eligible for MSI on the first day of the thirteenth month following the month of their arrival, provided they were physically present in Nova Scotia for 90 days after arrival, and not absent for more than 183 days, unless the absence is a requirement of their studies. MSI coverage is extended for a maximum of 12 months at a time. Each year, a copy of their renewed immigration document must be presented, and a declaration signed. Spouses, common-law partners and dependants who are legally entitled to remain in Canada are eligible on the same basis as the student.
In 2023-2024, there were 3,543 persons with study permits covered under the Health Insurance Program.
Diplomatic Passports and Employees of the Northwest Atlantic Fisheries Organization (NAFO): Individuals holding a diplomatic passport, and employees of NAFO who hold an acceptance document issued by the Department of Foreign Affairs Trade and Development in lieu of a Work Permit, must meet all remaining work permit requirements to be eligible. Spouses, common-law partners and dependants who are legally entitled to remain in Canada are eligible on the same basis as the diplomatic passport holder or NAFO employee.
Temporary Resident Permit (TRP): Individuals granted TRP status by IRCC are not eligible unless they meet the eligibility requirements for residency and a work permit or study permit.
4.0 Portability
4.1 Minimum waiting period
Persons moving to Nova Scotia from another Canadian province or territory will normally be eligible for Medical Services Insurance (MSI) on the first day of the third month following the month of their arrival. There is no waiting period for families of Canadian Armed Forces moving to Nova Scotia.
4.2 Coverage during temporary absences in Canada
The Interprovincial Agreement on Eligibility and Portability is followed in all matters pertaining to the portability of insured services.
Generally, the Nova Scotia MSI Plan provides coverage for residents of Nova Scotia who move to other provinces or territories for up to a period of three months, per the Eligibility and Portability Agreement. Students, and their spouses, common-law partners and dependants, who are temporarily absent from Nova Scotia and in full-time studies at an educational institution may remain eligible for MSI on a yearly basis, or longer based on the documented time required to complete the study program. To qualify for MSI, the student must provide to MSI a letter directly from the educational institution which states that they are registered as a full-time student. MSI coverage will be extended on a yearly basis, or for a longer term, pending receipt of this letter.
Workers who leave Nova Scotia to seek employment elsewhere will still be covered by MSI for up to 12 months, provided they do not establish residence in another province or territory. Services provided to Nova Scotia residents in other provinces or territories are covered by reciprocal agreements. Nova Scotia participates in the Hospital Reciprocal Billing Agreement and the Medical Reciprocal Billing Agreement. Quebec is the only province that does not participate in the Medical Reciprocal Billing Agreement. Nova Scotia pays for services provided by Quebec physicians to Nova Scotia residents at Quebec rates if the services are insured in Nova Scotia. The majority of such claims are received directly from Quebec physicians. In-patient hospital services are paid through the Interprovincial Reciprocal Billing Arrangement at the standard ward rate of the hospital providing the service. Nova Scotia pays the host province rates for insured services in all reciprocal billing situations.
The total amount paid by the plan in 2023-2024 for in-patient and out-patient hospital services received in other provinces and territories was $31,904,317.
Nova Scotia residents remain eligible to receive MSI during vacation outside of the province for up to seven months outside of Canada, and up to six months within Canada, in each calendar year and will continue to be deemed a resident if the following conditions are met:
- the resident communicates to MSI of their absence from Nova Scotia;
- the resident does not establish residency outside Nova Scotia; and
- new or returning residents must be physically present in Nova Scotia for at least 183 days prior to the absence.
4.3 Coverage during temporary absences outside Canada
Nova Scotia adheres to the Agreement on Eligibility and Portability for dealing with insured services for residents temporarily outside Canada. Provided a Nova Scotia resident meets eligibility requirements, out-of-country services will be paid, at a minimum, on the basis of the amount that would have been paid by Nova Scotia for similar services rendered in this province. In order to be covered, procedures of a non-emergency nature must have prior approval before they will be covered by MSI.
In 2023-2024, residents receiving haemodialysis outside Canada were eligible for reimbursement to a maximum of $628.00 per day, provided they submit the official service invoice.
Nova Scotia residents remain eligible to receive MSI during vacation outside Canada for up to seven months in each calendar year and continue to be deemed a resident if the above stated conditions are met.
Students, their spouse, common-law partner and dependants who are temporarily absent from Nova Scotia and in attendance at an educational institution outside Nova Scotia or Canada may remain eligible for MSI on a yearly basis or longer depending on the time required to complete the study program. To qualify for MSI, the student must provide to MSI a letter obtained from the educational institution that verifies the student's attendance there in each year for which MSI coverage is requested. MSI coverage will be extended on a yearly basis, or for a longer term, pending receipt of this letter and documentation of the time required to complete the study program.
Individuals who engage in employment (including volunteering, missionary work, or research) outside Canada, which does not exceed 24 months, are still covered by MSI, providing they have already met the residency requirements.
Foreign workers, their spouses, common-law partners and dependants, are covered for insured services that are received out-of-province.
The total amount spent in 2023-2024 for insured in-patient services provided outside of Canada was $4,889,761. In 2023-2024 there was an increase in utilization based on the number of claims, with at least one high-cost service provided. Nova Scotia does not cover out-patient services out-of-country.
In 2023-2024, the total number of residents registered with the Health Insurance Program was 1,127,280.
4.4 Prior approval requirement
There are two categories of prior approval:
Outside Canada
Prior approval must be obtained if residents wish to be reimbursed for elective services outside Canada. Application for prior approval is made to the medical consultant of the MSI Plan by an appropriate specialist in Nova Scotia on behalf of an insured resident. The medical consultant reviews the terms and conditions and determines whether or not the service is available in the province, or if it can be provided in another province or only out-of-country. The decision of the medical consultant is relayed to the patient's referring specialist. If approval is given to obtain service outside the country, the full cost of that service will be covered under MSI. An administrative review may be requested for individuals who are deemed ineligible.
Outside Nova Scotia and within Canada
Nova Scotia residents who are temporarily away from the province, or medically referred outside the province for insured treatment, are eligible for coverage under the provincial plan. Coverage in Canada is in accordance with the terms and conditions that apply to residents who receive insured services within Nova Scotia. Services must be received in an accredited public hospital and billed reciprocally in accordance with the Interprovincial Reciprocal Billing Agreements.
Nova Scotians who are referred by their healthcare provider for a medically necessary insured service outside Nova Scotia may be eligible for financial assistance. Not all medical services are covered by MSI, and residents cannot self-refer. Application for prior approval is made to the medical consultant of the MSI Plan by an appropriate specialist in Nova Scotia on behalf of an insured resident as described above.
Residents without pre-approval are responsible for all costs not insured by the Health Insurance Program. Pre-approval by MSI is not required for residents who are prepared to pay out-of-pocket for all costs.
All pre-approved medically necessary services that are provided on an in-patient or out-patient basis will be insured at 100%.
Prior approval is required before referring a patient outside Nova Scotia for addiction or psychiatric treatment. Prior approval must be sought through the medical consultant of the MSI Plan, as described above.
5.0 Accessibility
5.1 Access to insured health services
Section 3 of the Health Services and Insurance Act states that "subject to this Act and the regulations, all residents of the Province are entitled to receive insured hospital services from hospitals upon uniform terms and conditions." As well, all residents of the province are insured on uniform terms and conditions in respect of the payment of insured professional services to the extent of the established tariff. There are no user charges or extra charges allowed under the province's plans (Medical Services Insurance [MSI] Plan and Hospital Insurance Plan). In Nova Scotia, there is not a dedicated number or website to report cases of patient charges.
Complaints generally come directly to the Department of Health and Wellness via telephone or e-mail; are received by Medavie Blue Cross and then directed to the Department; or are directed to the College of Physicians and Surgeons of Nova Scotia. Complaints are investigated and addressed.
The Department of Health and Wellness General Inquiry contact information is as follows:
By phone: 902-424-5818
1-800-387-6665 (toll-free in Nova Scotia)
1-800-670-8888 (TTY/TDD)
By mail: Department of Health and Wellness
P.O. Box 488
Halifax, Nova Scotia B3J 2R8
Secure form: https://novascotia.ca/dhw/about/contact/#form
Nova Scotia continually monitors and reviews situations around access to insured health services across Canada to ensure equity of access.
5.2 Physician compensation
The Health Services and Insurance Act governs payment to physicians and dentists for insured services. Physician payments are made in accordance with a negotiated agreement between Doctors Nova Scotia (the sole bargaining agent for physicians) and the Province of Nova Scotia, as represented by the Minister of Health and Wellness.
Fee-for-service is one funding source of payment for physician services, as is physician payments made through alternative payment arrangements. Alternative payment arrangements facilitate the delivery of medical care that may not be compatible with the fee-for-service funding model and/or provide an alternate funding option to support physician remuneration preference in recruitment and retention. One such arrangement, launched with the 2023 Physician Agreement is the Longitudinal Family Medicine model, which provides a contracted funding option for primary care delivery. Additionally, within the academic funding context, payments may include compensation for non-medical activities such as teaching, research, and administration.
Other funding programs such as emergency agreements, sessional funding, and locum funding are also utilized by the province. In Nova Scotia, payment and payment monitoring are part of MSI's deliverables. Section 10 of the 2023 Physician Agreement lays out the Department's right to conduct audits of physicians with respect to insured medical service being claimed. Schedule "K" of the Physician Agreement outlines billing audit processes including an Audit Committee of the Physician Agreement Management Group to review the audit process and make recommendation. Annually, MSI develops an audit plan and conducts monitoring of claims to determine whether:
- the service was an insured service in Nova Scotia;
- the service was performed;
- the service was medically necessary;
- the service was correctly represented in the claim for payment; and
- the service meets the requirements set out in:
- the Preamble of the MSI Physician's Manual; and
- any relevant clarification provided to physicians in the MSI Physicians Bulletin.
Payment rates for dental services in the province are negotiated between the Department and the Nova Scotia Dental Association following a process similar to physician negotiations. Dentists are generally paid on a fee-for-service basis. Pediatric dentists at the IWK Health Centre receive remuneration through an Academic Funding Plan.
5.3 Payments to hospitals
The Department establishes budget targets for health care services. It does this by receiving business plans from the Nova Scotia Health Authority and the IWK Health Centre and other non-district health authority organizations. Approved provincial estimates form the basis on which payments are made to these organizations for service delivery.
The Health Authorities Act establishes the Nova Scotia Health Authority and the IWK Health Centre as the bodies responsible for overseeing the delivery of health services in the province of Nova Scotia and requires them to work collaboratively to do so.
Section 10 of the Health Services and Insurance Act and sections 9 through 13 of the Hospital Insurance Regulations define the terms for payments by the Minister of Health and Wellness to hospitals for insured hospital services.
In 2023-2024, there were 3,442 hospital beds in Nova Scotia (3.21 beds per 1,000 population). Department direct expenditures for insured hospital services were $3,198,287,898.
6.0 Recognition given to federal transfers
In Nova Scotia, the Health Services and Insurance Act acknowledges the federal contribution regarding the cost of insured hospital services and insured health services provided to provincial residents. The residents of Nova Scotia are aware of ongoing federal contributions to Nova Scotia health care through the Canada Health Transfer as well as other federal funds through press releases and media coverage.
The Government of Nova Scotia also recognized the federal contribution under the Canada Health Transfer in various published documents, including the following documents:
- Public Accounts 2023 – 2024, released July 26, 2024; and
- Budget Estimates and Supplementary Detail 2023 – 2024, released March 23, 2023.
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 1. Number as of March 31st | 1,043,849 | 1,062,223 | 1,079,880 | 1,101,152 | 1,127,280 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| Public facilities | |||||
| 2. Number | 35 | 35 | 35 | 35 | 35 |
| 3. Payments for insured health services ($)Footnote 1 |
2,033,885,945 | 2,186,870,916 | 2,220,898,704 | 2,640,425,842 | 3,198,287,898 |
| Private for-profit facilities | |||||
| 4. Number of private for-profit facilities providing insured health servicesFootnote 2 | 0 | 0 | 0 | 0 | 0 |
| 5. Payments to private for-profit facilities for insured health services ($) | not applicable | not applicable | not applicable | not applicable | not applicable |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 6. Total number of claims, in-patient | 1,986 | 1,097 | 1,095 | 1,478 | 1,666 |
| 7. Total payments, in-patient ($) | 21,568,883 | 13,216,509 | 12,194,376 | 17,588,618 | 21,245,680 |
| 8. Total number of claims, out-patient |
38,929 | 28,109 | 31,788 | 28,517 | 28,373 |
| 9. Total payments, out-patient ($) | 15,516,229 | 10,158,207 | 10,143,100 | 10,248,199 | 10,658,637 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| Pre-approved | |||||
| 10. Total number of claims, pre-approved in-patient | not available | not available | not available | not available | not available |
| 11. Total payments, pre-approved in-patient ($) | 7,327,272 | 8,640,992 | 5,036,502 | 1,822,948 | 4,638,557 |
| 12. Total number of claims, pre-approved out-patient | not available | not available | not available | not available | not available |
| 13. Total payments, pre-approved out-patient ($) | not available | not available | not available | not available | not available |
| Non pre-approved | |||||
| 14. Total number of claims, non pre-approved in-patient | not available | not available | not available | not available | not available |
| 15. Total payments, non pre-approved in-patient ($) | 352,994 | 108,240 | 45,825 | 89,887 | 251,204 |
| 16. Total number of claims, non pre-approved out-patient | not available | not available | not available | not available | not available |
| 17. Total payments, non pre-approved out-patient ($) | not available | not available | not available | not available | not available |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 18. Number of participating physicians | 2,801 | 2,803 | 2,906 | 3,033 | 3,022 |
| 19. Number of opted-out physicians | 0 | 0 | 0 | 0 | 0 |
| 20. Number of non-participating physicians |
not applicable | not applicable | not applicable | not applicable | not applicable |
| 21. Total payments for services provided by physicians paid through all payment methods ($) | 834,933,109 | 888,887,594 | 923,670,325 | 968,981,019 | 1,058,437,659 |
| 22. Total payments for services provided by physicians paid through fee-for-service ($) | 352,279,973 | 304,525,329 | 376,406,902 | 391,076,855 | 392,348,830 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 23. Number of services | 226,834 | 176,875 | 199,358 | 318,998 | 192,013 |
| 24. Total payments ($) | 9,522,757 | 6,346,214 | 6,894,731 | 8,937,052 | 8,518,386 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| Pre-approved | |||||
| 25. Number of pre-approved services | 47 | 68 | 75 | 52 | 67 |
| 26. Total pre-approved payments ($) | 110,315 | 168,335 | 101,973 | 35,265 | 325,855 |
| Non pre-approved | |||||
| 27. Number of non pre-approved services | 1,391 | 127 | 295 | 346 | 417 |
| 28. Total non pre-approved payments ($) | 91,170 | 11,046 | 22,283 | 22,444 | 33,562 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 29. Number of participating dentists | 18 | 18 | 18 | 19 | 17 |
| 30. Number of opted-out dentists | 0 | 0 | 0 | 0 | 0 |
| 31. Number of non-participating dentists |
0 | 0 | 0 | 0 | 0 |
| 32. Number of services providedFootnote 3 | 6,381 | 6,303 | 6,732 | 7,172 | 7,972 |
| 33. Total payments ($)Footnote 4 | 1,450,699 | 1,385,924 | 1,208,317 | 1,478,687 | 1,477,409 |
|
|||||
New Brunswick
1.0 Public administration
1.1 Health care insurance plan and public authority
In New Brunswick, the formal name for Medicare is the Medical Services Plan. The Minister of Health (Minister) has the mandate and responsibility for operating and administering the plan by virtue of the Medical Services Payment Act and its Regulations. The Act and Regulations set out who is eligible for Medicare coverage, the rights of the patient, and the responsibilities of the Department of Health (the Department). This Act establishes a Medicare plan and defines which Medicare services are covered and which are excluded. It also stipulates the type of agreements the Department may enter into. As well, it specifies the rights of a medical practitioner; how the amounts to be paid for medical services will be determined; how assessment of accounts for medical services may be made; and confidentiality and privacy issues as they relate to the administration of the Act.
1.2 Reporting relationship
The Medicare and Physician Services Branch of the Department are mandated to administer the Medical Services Plan. The Minister reports to the Legislative Assembly through the Department's annual report and through regular legislative processes.
The Regional Health Authorities Act establishes the regional health authorities (RHA) and sets forth the powers, duties, and responsibilities of the same. The Minister is responsible for the administration of the Act, provides direction to each RHA, and may delegate additional powers, duties, or functions to the RHA.
The Department prepares and submits an annual report to the Legislature and provides information to the Office of the Comptroller for inclusion in their Public Accounts documents. The Minister and Department of Health executive team are accountable to answer questions of members of the Legislature pursuant to those Public Accounts documents. The most current Department of Health Annual Report can be found here.
1.3 Audit of accounts
Three groups have a mandate to audit the Medical Services Plan.
The Office of the Auditor General: In accordance with the Auditor General Act, the Office of the Auditor General conducts the external audit of the accounts of the province of New Brunswick, which includes the financial records of the Department. The Auditor General also conducts management reviews on programs as they see fit. Volume I of the Auditor General's 2023 report presents the result of the performance audit on COVID-19 Pandemic Response and Pandemic Preparedness and Response in Nursing Homes. The report's key findings can be found here.
The Office of the Comptroller: The Comptroller is the chief internal auditor for the province of New Brunswick and provides accounting, audit, and consulting services in accordance with responsibilities and authority set out in the Financial Administration Act. Annual financial statements and supplementary information submitted to the Legislature by the Office of the Comptroller for all publicly funded purposes (including those associated with insured services under the Canada Health Act) can be found here.
Monitoring and Compliance Team: This team is tasked with managing compliance with the Medical Services Payment Act and Regulations, as well as the Negotiated Fee Schedule.
2.0 Comprehensiveness
2.1 Insured hospital services
Legislation providing for insured hospital services as described in the Canada Health Act includes the Hospital Services Act, section 9 of Regulation 84–167, and the Hospital Act. Under Regulation 84–167 of the Hospital Services Act, New Brunswick residents are entitled to the following insured hospital services.
Insured in-patient services include:
- accommodation and meals;
- nursing;
- laboratory/diagnostic procedures;
- drugs;
- the use of facilities (e.g., surgical, radiotherapy, physiotherapy); and
- services provided by professionals within the facility.
Insured out-patient services include:
- laboratory and diagnostic procedures;
- mammography; and
- the hospital component of available out-patient services for maintaining health, preventing disease, and helping diagnose or treat any injury, illness or disability, excluding those related to the provision of drugs or third party diagnostic requests.
There were no amendments made to the above noted Acts or Regulations in 2023-2024.
2.2 Insured physician services
The Medical Services Payment Act and corresponding regulations provide for insured physician services. As of March 31, 2024, there were 1,878 participating physicians in New Brunswick.
A medical practitioner or an oral and maxillofacial surgeon (OMS) who is practising in the province, outside the provisions of the Medical Services Payment Act and its Regulations (opted-out), shall inform any person to whom entitled services are provided that he or she is practising outside the provisions of the Act and its Regulations, and that the person is not entitled to payment under the Medical Services Plan. Further, practitioners can elect to opt out for any given patient only for the total management of the patient's condition under care, including any complications which may develop within a reasonable length of time, and they must advise the patient in advance of rendering service that they are opting out for those services.
An opted-in practitioner who subsequently wishes to change their status and opt out totally can do so by notifying the Department of Health (the Department) of their intention in writing. Their change in status becomes effective from the date of receipt by the Department of such written notification, or from the date specified by the practitioner. No physicians rendering health care services in this fiscal year so chose.
The services which residents are entitled to under Medicare include:
- all entitled services rendered by medical practitioners or oral and maxillofacial surgeons that are medically required.
A physician or the Department may request the addition of a new service. All requests are considered by the New Service Items Committee, which is jointly managed by the New Brunswick Medical Society and the Department. The decision to add a new service is based on conformity to the definition of "medically necessary" and whether the service is considered generally acceptable practice (not experimental) within New Brunswick and Canada. Considerations under the term "medically necessary" include services required for maintaining health, preventing disease and/or diagnosing or treating an injury, illness or disability. No public consultation process is used.
In 2023-2024 the Medical Services Payment Act was amended, consequential to the Health Facilities Act, to further enable a regional health authority to enter into an agreement for the provision of surgical services outside a hospital; and for Medicare to pay the surgeons for the services rendered in these surgical facilities.
2.3 Insured surgical-dental services
Schedule 4 of Regulation 84–20 under the Medical Services Payment Act identifies the insured surgical- dental services that can be provided by a qualified dental practitioner in a hospital, providing the condition of the patient requires services to be rendered in a hospital.
In addition, a general dental practitioner may be paid to assist another dentist for medically required services under some conditions. OMS have access to approximately 290 billing codes. They can admit or discharge patients and perform physical examinations, including those performed in an out-patient setting. OMS may also see patients for consultation in their office for insured services.
As of March 31, 2024, there were 15 dentists and OMS who provided services insured under the Medical Services Plan.
There is not a formally defined process through which new dental services may be added to the list of insured services; however, OMS may approach government with such a request if they deem it appropriate. In 2023-2024 there were no such additions.
2.4 Uninsured hospital, physician and surgical-dental services
Uninsured hospital services include:
- take-home drugs;
- third-party requests for diagnostic services;
- visits to administer drugs;
- vaccines;
- sera or biological products;
- televisions and telephones;
- preferred accommodation at the patient's request; and
- hospital services directly related to services listed under Schedule 2 of the Regulation under the Medical Services Payment Act. Services are not insured if provided to those entitled under other statutes.
The services listed in Schedule 2 of New Brunswick Regulation 84–20 under the Medical Services Payment Act are specifically excluded from the range of entitled medical services under Medicare. They are as follows:
- elective plastic surgery or other services for cosmetic purposes;
- correction of inverted nipple;
- breast augmentation;
- otoplasty for persons over the age of eighteen;
- removal of minor skin lesions, except where the lesions are, or are suspected to be pre-cancerous;
- abortion, unless the abortion is performed in a hospital facility approved by the jurisdiction in which the hospital facility is located;
- surgical assistance for cataract surgery unless such assistance is required because of risk of procedural failure, other than risk inherent in the removal of the cataract itself, due to existence of an illness or other complication;
- medicines, drugs, materials, surgical supplies, or prosthetic devices;
- advice or prescription renewal by telephone which is not specifically provided for in the Schedule of Fees;
- examinations of medical records or certificates at the request of a third party, or other services required by hospital regulations or medical by-laws, except examinations of medical records or certificates as part of a forensic psychiatric assessment ordered by a court;
- dental services provided by a medical practitioner or an oral and maxillofacial surgeon;
- services that are generally accepted within New Brunswick as experimental or that are provided as applied research;
- services that are provided in conjunction with or in relation to the services referred to above;
- testimony in a court or before any other tribunal, except with respect to a forensic psychiatric assessment ordered by a court;
- immunization, examinations, or certificates for purpose of travel, employment, emigration, insurance or at the request of any third party;
- services provided by medical practitioners or oral and maxillofacial surgeons to members of their immediate family;
- psychoanalysis;
- electrocardiogram where not performed by a specialist in internal medicine or paediatrics;
- laboratory procedures not included as part of an examination or consultation fee;
- refractions;
- services provided within the province by medical practitioners, oral and maxillofacial surgeons or dental practitioners for which the fee exceeds the amount payable under this Regulation;
- the fitting and supplying of eye glasses or contact lenses;
- acupuncture;
- complete medical examinations when performed for the purposes of periodic check-up and not for medically necessary purposes;
- circumcision of a newborn;
- reversal of vasectomies;
- second and subsequent injections for impotence;
- reversal of tubal ligations;
- intrauterine insemination;
- bariatric surgery unless the person has a body mass index of 40 or greater or of 35 or greater but less than 40, as well as obesity-related comorbid conditions; and
- venipuncture for purposes of taking blood when performed as a stand-alone procedure in a facility that is not an approved hospital facility.
Dental services not specifically listed in Schedule 4 of the Dental Schedule are not covered by the Medical Services Plan. Those listed in Schedule 2 are considered the only non-insured medical services.
There are no specific policies or guidelines, other than the Medical Services Payment Act and its Regulations, to ensure that charges for uninsured medical goods and services (e.g., fibreglass casts), provided in conjunction with an insured health service, do not compromise reasonable access to insured services.
The decision to de-insure physician or surgical-dental services is based on the conformity of the service to the definition of "medically necessary," a review of medical service plans across the country, and the previous use of the particular service. Once a decision to de-insure is reached, the Medical Services Payment Act dictates that the government may not make any changes to the Regulation until the advice and recommendations of the New Brunswick Medical Society are received or until the period within which the Society was requested by the Minister to furnish advice and make recommendations has expired. Subsequent to receiving their input and resolution of any issues, a regulatory change is completed. Physicians are informed in writing following notification of approval. The public is usually informed through a media release. No public consultation process is used.
In 2023–2024, no services were removed from the insured services list.
3.0 Universality
3.1 Eligibility
Sections 3 and 4 of the Medical Services Payment Act and Regulation 84–20 define eligibility for the health care insurance plan in New Brunswick. Residents are required to complete a Medicare application and provide proof of identity, proof of residency, and proof of Canadian citizenship or a valid Canadian immigration document. A resident is defined as a person lawfully entitled to be, or to remain, in Canada, who makes their home and is ordinarily present in New Brunswick, but does not include a tourist, transient, or visitor to the province.
As at March 31, 2024, there were 845,733 persons actively registered in New Brunswick. Below are the numbers of individuals registered in the requested categories:
All persons entering or returning to New Brunswick (excluding children adopted from outside Canada) have a waiting period before becoming eligible for Medicare coverage. Coverage commences on the first day of the third month following the month of arrival.
Exceptions are as follows:
- Dependents of Canadian Armed Forces personnel or their spouses moving from within or outside Canada to New Brunswick are entitled to first day coverage, provided they are deemed to have established permanent residency in New Brunswick.
- Immigrants or Canadian citizens moving or returning to New Brunswick from outside of Canada are entitled to first day coverage, provided they are deemed to have established permanent residency in the province. Proper documentation is required from Immigration, Refugees, and Citizenship Canada (IRCC). Decisions on coverage and residency are reviewed on a case-by-case basis.
- Non-Canadians who are issued a Study Permit and establish residency in the province, may become a beneficiary on the first day of classes, on the commencement date specified in the study permit or on the date of arrival in New Brunswick, whichever is latest. Proper documentation is required from IRCC as well as proof of enrollment at a New Brunswick university or other approved educational institution.
Residents who were not eligible for Medicare coverage during this reporting period included:
- regular members of the Canadian Armed Forces;
- inmates at federal institutions;
- temporary residents;
- a family member who moves from another province to New Brunswick before other family members move;
- persons who have entered New Brunswick from another province to further their education and who are eligible to receive coverage under the medical services plan of that province; and
- non-Canadians who are issued certain types of Canadian authorization permits.
Persons who are discharged or released in New Brunswick from the Canadian Armed Forces, or a federal penitentiary, become eligible for coverage on the date of their discharge or release. An application must be completed and signed, and the applicant must provide proof of Canadian citizenship, proof of residency and the official date of release.
3.2 Other categories of individuals
Non-Canadian new hires coming to Canada under a work permit must have a permit valid for a minimum of one year (or a combination of permits spanning at least one year and within a few months of each other). The Department of Health also requires a copy of their passport (including a copy of the last entry date stamp if available), and proof of residency in New Brunswick.
Children born out-of-country to Canadian citizens will take the eligibility status of the parent upon return to the province. Proper documentation is required.
Should an individual disagree with a decision of the Department of Health, including a decision respecting eligibility to receive services, they may petition the Insured Services Appeal Committee, which shall provide advice to the Minister.
There were no amendments made to eligibility provisions in 2023-2024.
4.0 Portability
4.1 Minimum waiting period
A person is eligible for New Brunswick Medicare coverage on the first day of the third month following the month permanent residency has been established. The three-month waiting period is legislated under New Brunswick's Medical Services Payment Act. Refer to section 3.1 of this submission for exceptions; there were no amendments made to this section of the Act in 2023-2024.
4.2 Coverage during Temporary Absences within Canada
The legislation that defines portability of health insurance during temporary absences in Canada is the Medical Services Payment Act, Regulation 84–20, subsections 3(4) and 3(5). This portion of the Act was not amended in 2023-2024.
Medicare coverage may be extended upon request in the case of temporary absences to:
- students in full-time attendance at a university or other approved educational institution outside New Brunswick;
- residents temporarily working in another jurisdiction; and
- residents whose employment requires them to travel outside the province.
Students: Those in full-time attendance at a university or other approved educational institution, who leave the province to further their education in another province, will be granted coverage for a 12-month period that is renewable, provided the following terms are met:
- Medicare is contacted once every 12 months;
- permanent residency is not established outside New Brunswick; and
- health insurance coverage is not received elsewhere.
Residents: Residents temporarily employed in another province or territory are granted coverage for up to 12 months, provided the following terms are met:
- permanent residency is not established outside New Brunswick; and
- health insurance coverage is not received elsewhere.
New Brunswick has formal agreements for reciprocal billing arrangements of insured hospital services with all provinces and territories. In addition, New Brunswick has reciprocal agreements with all provinces, except Quebec, for the provision of insured physician services. Services provided by Quebec physicians to New Brunswick residents are paid at Quebec rates provided the service delivered is insured in New Brunswick. The majority of such claims are received directly from Quebec physicians. Any claims submitted directly by a patient are reimbursed to the patient.
4.3 Coverage during temporary absences outside Canada
The legislation that defines portability of health insurance during temporary absences outside Canada is the Medical Services Payment Act, Regulation 84–20, subsections 3(4) and 3(5).
Eligibility for New Brunswick residents temporarily absent outside of Canada is determined in accordance with the Medical Services Payment Act.
Residents temporarily employed outside Canada are granted coverage for 182 days. This may be extended up to 12 months within a three-year period upon approval from the Director of Medicare Operations. Exceptions to this are mobile and contract workers.
Coverage for any absence over 212 days for vacation purposes requires approval from the Director of Medicare Operations. This approval can only be for up to 12 months in duration and will only be granted once every three years.
New Brunswick residents exceeding the 12-month extension must reapply for New Brunswick Medicare upon their return to the province. In this instance, cases are reviewed on a case-by-case basis. Depending on the circumstances, some cases may be eligible for first day coverage while others who have been away from the province slightly beyond the 12-month period may be given a grace period.
Insured residents who receive insured emergency services out-of-country are eligible to be reimbursed $100 per day for in-patient stays and $50 per out-patient visit. The insured resident is reimbursed for physician services associated with the emergency treatment at New Brunswick rates. The difference in rates is the patient's responsibility.
Mobile Workers: Mobile Workers are residents whose employment requires them to travel outside the province (e.g., pilots). The following guidelines must be met to receive Mobile Worker designation.
- applications must be in writing;
- documentation is required as proof of Mobile Worker status (e.g., letter from employer or contract confirming that frequent travel is necessary outside the province):
- a letter from the resident indicating their permanent residence as New Brunswick and detailing the frequency of their return to the province;
- a copy of their New Brunswick driver's license;
- if working outside Canada, a copy of resident's immigration documents that allow them to work outside the country; and
- the worker must return to New Brunswick during their off time.
Mobile Worker status is assigned for a maximum of two years, after which the resident must reapply and submit documentation to confirm a continuation of Mobile Worker status.
Contract Workers: Any New Brunswick resident accepting a contract out-of-country must supply the following information and documentation:
- a letter of request from the New Brunswick resident with their signature, detailing their absence, Medicare number, address, departure and return dates, destination, forwarding address, and reason for absence; and
- a copy of a contractual agreement between employee and employer indicating start and end dates of employment.
Contract Worker status is assigned up to a maximum of two years. Any further requests for contract worker status must be forwarded to the Director of Medicare Eligibility and Claims for approval on an individual basis.
Students: Those in full-time attendance at a university or other approved educational institution in another country will be granted coverage for a 12-month period that is renewable, provided they comply with the following:
- proof of enrollment must be provided from the educational institution on an annual basis;
- Medicare must be contacted once every 12 months;
- permanent residency cannot be established outside New Brunswick; and
- health insurance coverage cannot be received elsewhere.
4.4 Prior approval requirement
Medicare may cover out-of-country services that are not available in Canada on a pre-approval basis only. Residents may opt to seek non-emergency out-of-country services; however, they are responsible for assuming the total cost.
New Brunswick residents may be eligible for reimbursement if they receive elective medical services outside the country, provided the following requirements are met:
- the required service or equivalent, or an alternate service must not be available in Canada;
- the service must be rendered in a hospital listed in the current edition of the American Hospital Association Guide to the Health Care Field (guide to United States hospitals, health care systems, networks, alliances, health organizations, agencies and providers);
- the service must be rendered by a medical doctor; and
- the service must be an accepted method of treatment recognized by the medical community and be regarded by the medical community as scientifically proven in Canada. Experimental procedures are not covered.
Even if the above requirements are met, it is mandatory to request prior approval from Medicare in order to receive coverage. A physician, patient or family member may request prior approval to receive these services outside the country, accompanied by supporting documentation from a Canadian specialist or specialists.
A beneficiary who disagrees with a decision made by Medicare regarding their case or the case of an immediate family member can appeal to the Insured Services Appeal Committee. Beneficiary appeals can include decisions about eligibility, refusal of a claim payment for entitled services or the amount paid on a claim. The Committee is comprised of members from the general public. It meets three to four times a year based on the number of cases. It reviews each case and presents recommendations to the Minister of Health who makes the final decision regarding an appeal.
Out-of-country insured services that are not available in Canada, are non-experimental, and receive prior approval are paid in full. Often the amount payable is negotiated with the provider by Global Medical Management on the province's behalf.
Haemodialysis is exempt from the out-of-country coverage policy. Patients are required to obtain prior approval and Medicare will reimburse the resident at a rate equivalent to the current inter-provincial rate per session.
A New Brunswick patient may choose to receive most insured services paid by Medicare in any public hospital in Canada, without prior approval. Most of these services are covered by Interprovincial Reciprocal Billing Agreements, although some may be billed directly to the host province. Some procedures require prior Medicare approval before a patient will be accepted for treatment in another province (e.g. high cost procedures, residential addictions/mental health services, some plastic procedures etc.). Should such prior approval be required, the attending physician would write to the medical consultant with Medicare, providing pertinent documentation and the reason for the out-of-province referral. Travel is not covered by Medicare, but lodging may be considered if the patient meets Medicare's Hostel Policy criteria.
5.0 Accessibility
5.1 Access to insured health services
New Brunswick's health care system delivers equitable, quality care to the public it serves. As indicated in section 13.1 of Medical Services Payment Act Regulation 84–20, New Brunswick does not permit user fees for insured health services as defined by the Canada Health Act. New Brunswick uses a robust "comment based" approach to identifying individual citizens' concerns on a wide range of health issues. In a typical month in the 2023–2024 fiscal year, the Department of Health received, logged, and responded to 150–200 concerns from individual New Brunswickers on issues including access to primary or specialized care, pharmaceutical approvals, access to services in a citizen's language of choice, wait times for specific services, the structure of specific programs, etc. In the same fiscal year and addition to the above, the Department of Health received 11,154 other pieces of correspondence which were parts of coordinated campaigns (often with common pre-written messaging) respecting issues of widely held public interest. The Department's web page provides several mechanisms to make such comments, including mailing addresses, e-mail addresses, telephone numbers, and a web-based message service.
In addition, in partnership with regional health authorities, the Department of Health is exploring proactive mechanisms to ensure that no fees are levied upon citizens for primary care services offered by New Brunswick based providers.
Sixty-seven requests for patient reimbursement for privately provided services were received in the 2023-2024 fiscal year, ranging from reimbursement for having blood drawn at a private collection site, to reimbursement for MRI at a private facility, to surgical treatment provided by a private provider outside of Canada. In accordance with New Brunswick's legislation described above, these requests were reviewed and determined to not be eligible for reimbursement.
Access in a resident's official language of choice is not a limiting factor, regardless of where a resident receives services in the province.
During the 2023-2024 fiscal year, Department of Health focused on these government priorities through:
- NB Health Link (NBHL), which provides patients without a doctor or nurse practitioner with access to primary care services, expanded to cover every health zone in the province. More than 56,000 patients had access to NBHL on March 31, 2024. NBHL replaced the Patient Connect NB list as the provincial registry for individuals waiting for permanent matching to a family doctor or nurse practitioner.
- Eight more common ailments were added to the list of services that New Brunswick pharmacists are publicly funded to treat. Over 191,000 services have been provided by pharmacists over the past fiscal year. Through a partnership with the New Brunswick College of Pharmacists, six pharmacies were selected to provide service for Group A Strep, asthma, COPD, CVD and diabetes as part of a pilot project.
- The Health Human Resources Branch led or supported eight international recruitment missions leading to over 650 job offers in acute and long-term care.
- The target of 75,000 users accessing MyHealthNB Records was reached by December 2023 (over three months early). There were over 100,000 users at the end of March 2024.
- All long waiting hip and knee surgeries were performed or scheduled as of the end of March 2024.
- The Addiction and Mental Health Helpline (1-866-355-5550) was launched and has taken more than 23,000 calls from the public. The service has provided referrals to government or community services patients who otherwise may have turned to emergency departments.
- In February 2024, Ambulance New Brunswick (ANB) – in partnership with the Department of Health and Grand Manan Village Council – announced the signing of a contract with Voyageur Aviation that will see an air ambulance stationed on the island of Grand Manan in the fall of 2024.
- The New Brunswick Cancer Network is expanding access to quality palliative care training opportunities in New Brunswick. Pallium Canada's Learning Essential Approaches to Palliative Care (LEAP) courses will be provided at no cost to health care providers in regional health authorities, EM/ANB Inc. and the Department of Social Development.
- The mobile X-ray program helped avoid over 700 trips to hospital in the Saint John area, with further expansion across New Brunswick planned in 2024-2025.
- The Provincial Archiving and Communications Systems (PACS) Consolidation team launched Enterprise Imaging in Zone 6 (Acadie-Bathurst) in February, as its first consolidation (pilot) site. Primary users included radiologists, emergency physicians, orthopedic surgeons, PACS administrators and diagnostic imaging technologists.
- The Working Together to Improve Health Care in Canada bilateral funding agreement was signed. This will see the Government of Canada providing more than $313 million to support New Brunswick's three-year action plan to deliver improvements to its health care system.
- Amendments to the Regional Health Authorities Act improved the governance of the regional health authorities and established the Health System Collaboration Council to improve province-wide planning.
- Influenza Protection in Adult Residential Facilities (ARFs) was enhanced. 132 doses of funded Tamiflu (antiviral) were provided to residents of ARFs during influenza outbreaks. In addition, to support Provincial Rapid Outbreak Management Team (PROMT) access during a facility outbreak, funding was provided for pharmacists to assess and prescribe antiviral medication for more vulnerable residents to prevent influenza infection.
- The Health Human Resources branch continued to promote nbhealthjobs.com to build awareness of career and life opportunities in New Brunswick and support the recruitment of health care workers in New Brunswick, other parts of Canada and internationally.
- The Department of Health worked collaboratively with partners to develop an expedited registration process for Canadian trained nurses and internationally educated nurses from 14 countries.
- More than 1,900 joint interventions were conducted between Mobile Crisis Services and police throughout the province. 83 per cent of crises were managed in the community, preventing an emergency department visit or a police apprehension.
- The Clinical Information Solution Transformation, which will be responsible for the implementation of a standardized, integrated Clinical Information Solution (CIS) for New Brunswick, was established.
5.2 Physician compensation
Payments to physicians and dentists are governed under the Medical Services Payment Act, Regulations 84–20, 93–143, and 2002–53.
The methods used to compensate physicians for providing insured health services in New Brunswick are fee-for-service, salary and sessional, alternate payment mechanisms or Family Medicine New Brunswick that may include a blended system.
5.3 Payments to hospitals
The legislative authorities governing payments to hospital facilities in New Brunswick are the Hospital Act, which governs the administration of hospitals, and the Hospital Service Act, which governs the financing of hospitals. The Regional Health Authorities Act provides for the delivery and administration of health services in defined geographic areas within the province.
The Department of Health mainly distributes available funding to New Brunswick's regional health authorities (RHA) through a Current Service Level approach. The funding base of the RHA from the previous year is the starting point to which approved salary increases and a global inflator for non-wage items are added. This applies to all clinical services provided by hospital facilities, as well as support services (e.g., administration, food services, etc.).
Funding for Service New Brunswick, a shared services agency that manages the information technology, materials management, laundry and clinical engineering components of the hospital facilities in New Brunswick, is also based on the Current Service Level approach.
Any requests for funding for new programs or services are submitted to the Deputy Minister of Health for approval. Funding for approved new programs or services is based on requirements identified through discussions between Department of Health and RHA staff. These amounts are added to the RHA funding base once there is agreement on the funding requirements.
6.0 Recognition given to federal transfers
New Brunswick recognizes the federal role regarding its contributions under the Canada Health Transfer in public documentation presented through legislative and administrative processes. Federal transfers are identified in the Main Estimates document and in the Public Accounts of New Brunswick. Both documents are published annually by the New Brunswick government.
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
| 1. Number as of March 31st | 782,398 | 791,138 | 805,375 | 825,607 | 845,733 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
| Public facilities | |||||
|---|---|---|---|---|---|
| 2. Number | 64 | 67 | 67 | 67 | 67 |
| 3. Payments for insured health services ($) | 1,942,617,634 | 1,963,401,676 | 2,077,957,401 | 2,404,681,731 | 2,768,286,676 |
| Private for-profit facilitiesFootnote 1 | |||||
| 4. Number of private for-profit facilities providing insured health services | 0 | 0 | 0 | 0 | 3 |
| 5. Payments to private for-profit facilities for insured health services ($) | 0 | 0 | 0 | 0 | 9,925,348 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 6. Total number of claims, in-patient | 4,506 | 2,514 | 2,666 | 3,270 | 3,708 |
| 7. Total payments, in-patient ($) | 48,739,305 | 33,127,169 | 40,120,459 | 55,393,984 | 75,655,095 |
| 8. Total number of claims, out-patient |
51,004 | 36,183 | 40,591 | 44,751 | 46,223 |
| 9. Total payments, out-patient ($) | 22,677,309 | 14,621,209 | 15,762,984 | 19,659,704 | 22,169,819 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| Pre-approved | |||||
| 10. Total number of claims, pre-approved in-patient | 4 | 10 | 10 | 3 | 1 |
| 11. Total payments, pre-approved in-patient ($) | 273,499 | 26,474 | 32,061 | 11,447 | 700 |
| 12. Total number of claims, pre-approved out-patient |
78 | 12 | 7 | 5 | 2 |
| 13. Total payments, pre-approved out-patient ($) | 1,126,040 | 2,027 | 1,444 | 223 | 12,460 |
| Non pre-approved | |||||
| 14. Total number of claims, non pre-approved in-patient | 74 | 12 | 11 | 35 | 61 |
| 15. Total payments, non pre-approved in-patient ($) | 535,056 | 3,652 | 23,341 | 127,396 | 52,624 |
| 16. Total number of claims, non pre-approved out-patient | 524 | 88 | 110 | 295 | 378 |
| 17. Total payments, non pre-approved out-patient ($) | 972,707 | 160,991 | 174,347 | 304,366 | 384,715 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 18. Number of participating physiciansFootnote 2 | 1,748 | 1,771 | 1,820 | 1,858 | 1,878 |
| 19. Number of opted-out physicians | 0 | 0 | 0 | 0 | 0 |
| 20. Number of non-participating physicians |
0 | 0 | 0 | 0 | 0 |
| 21. Total payments for services provided by physicians paid through all payment methods ($)Footnote 3 | 631,179,766 | 627,284,780 | 689,788,846 | 695,816,914 | 687,559,508 |
| 22. Total payments for services provided by physicians paid through fee-for-service ($) | 405,341,277 | 399,494,993 | 412,058,093 | 418,466,815 | 463,379,314 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 23. Number of services | 212,579 | 159,625 | 189,582 | 214,440 | 219,672 |
| 24. Total payments ($) | 21,681,383 | 15,258,372 | 18,497,994 | 21,823,896 | 23,126,951 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| Pre-approved | |||||
| 25. Number of pre-approved services | 622 | 23 | 37 | 17 | 4 |
| 26. Total pre-approved payments ($) | 103,403 | 6,233 | 18,650 | 4,972 | 10,097 |
| Non pre-approved | |||||
| 27. Number of non pre-approved services | 1,933 | 606 | 643 | 1,354 | 1,525 |
| 28. Total non pre-approved payments ($) | 175,131 | 63,610 | 80,770 | 110,556 | 143,038 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 29. Number of participating dentistsFootnote 4 | 11 | 11 | 12 | 11 | 15 |
| 30. Number of opted-out dentists | not applicable | not applicable | not applicable | not applicable | not applicable |
| 31. Number of non-participating dentists |
not applicable | not applicable | not applicable | not applicable | not applicable |
| 32. Number of services provided | 1,747 | 1,799 | 1,454 | 1,211 | 1,291 |
| 33. Total payments ($) | 331,722 | 357,961 | 298,050 | 358,895 | 364,149 |
|
|||||
Quebec
1.0 Public administration
1.1 Health Insurance Plan and Public Authority
Quebec's hospital insurance plan, the Régime d'assurance hospitalisation du Québec, is administered by the Ministry of Health and Social Services (MSSS).
Quebec's health and drug insurance plans are administered by the Régie de l'assurance maladie du Québec (the Régie), a public body established by the provincial government that reports to the Minister of Health and Social Services.
Through the sound management of the Quebec Health Insurance Plan, the Public Prescription Drug Insurance Plan and assistance programs for the public, the Régie collaborates on access to health care. It also compensates health professionals so that Quebeckers can get the care they need.
1.2 Reporting relationships
The Public Administration Act (CQLR, c A-6.01, hereinafter "PAA") affirms the priority given by the government administration to the quality of services to the public in the development and application of the rules of the public administration. It recognizes the role played by parliamentarians with respect to government action and their contribution to improving services provided for the public while making the government more accountable to the National Assembly. As a result, the PAA establishes a framework for management based on results and transparency.
To ensure the implementation of this management framework, the PAA sets out a number of obligations that must be met by departments and agencies, including the production of a declaration of services to the public if direct services to the public are offered, a multi-year strategic plan, an annual management report, and, in the case of departments, an annual expenditure management plan.
Section 24 of the PAA states that a department or body, including the MSSS and the Régie, must prepare an annual management report. This report must include a presentation of the results related to the objectives set out in the strategic plan, and a declaration by the deputy minister or agency head attesting to the reliability of the data in the report and the related controls, and any other element or information determined by Treasury Board or included in its laws.
In the case of the Régie, the annual management report includes a specific section on the results of the various control measures in place (inspections, investigations and amounts recovered) as well as the activity report on the basic prescription drug insurance plan.
In accordance with section 26 of the PAA, the annual management report of a department, and of the bodies and administrative units under a minister's responsibility, shall be tabled in the National Assembly by the minister concerned within four months after the end of their fiscal year or, if the Assembly is not sitting, within 15 days of resumption.
1.3 Audit of accounts
The Quebec Hospital Insurance Plan and the Quebec Health and Drug Insurance Plans are administered by the public authorities on a non-profit basis.
The books and accounts of the Régie are audited by the Auditor General of Quebec each year and also whenever so ordered by the Government. These reports must accompany the Régie's annual management report.
2.0 ComprehensivenessFootnote i
2.1 Insured hospital services
Insured in-patient services outlined in the Regulation respecting the application of the Hospital Insurance Act (CQLR, c A-28) include the following:
- standard ward accommodation and meals;
- necessary nursing services;
- routine surgical supplies;
- diagnostic services;
- use of operating rooms, delivery rooms and anaesthetic facilities;
- medication;
- prosthetic and orthotic devices that can be integrated with the human body;
- biological products and related preparations;
- use of radiotherapy and physiotherapy facilities;
- services delivered by hospital staff; and
- medically assisted reproduction.
Outpatient services covered by the Regulation respecting the application of the Hospital Insurance Act include the following:
- clinical services for psychiatric care;
- electroshock, insulin therapy and behaviour therapies;
- emergency care;
- minor surgery (day surgery);
- radiotherapy;
- diagnostic services;
- physiotherapy;
- occupational therapy;
- inhalation therapy, audiology, speech therapy and orthoptic services; and
- other services or examinations required under Quebec legislation.
The Ministry of Health and Social Services (MSSS) administers a free ambulance transportation program for people aged 65 and older, in accordance with the parameters described in the Quebec policy on user transportation.
2.2 Insured physician services
Services covered under this plan include medical and surgical services provided by physicians participating in the plan that are medically necessary, except those excluded by regulation.
The Régie de l'assurance maladie du Québec (the Régie) also covers the cost of the following:
- optometric services for people who are under age 18 or 65 and over, and for people who have been recipients of a financial assistance program for at least the past 12 consecutive months;
- dental care for children aged 10 and under and people who have been recipients of a financial assistance program for at least the past 12 consecutive months; and
- acrylic dental prostheses for people who have been recipients of a financial assistance program for at least the past 24 consecutive months and who have prior authorization from the Quebec Minister of Employment and Social Solidarity (MESS).
The Régie also covers the following for "insured persons" within the meaning of the Health Insurance Act (CQLR, c A-29, hereinafter "HIA") who meet the eligibility criteria specific to each program:
- prostheses;
- orthotics;
- orthopedic appliances, such as walking and standing aids;
- walking and posture aids;
- hearing aids and assistive listening devices;
- visual aids; and
- glasses and contact lenses.
This coverage applies only to aids and appliances and related services covered in the regulations. Financial aid is granted for external breast prostheses, ocular prostheses, devices provided to ostomies, and compression bandages and clothing for people with lymphedema.
Coverage for eyeglasses and contact lenses applies exclusively to minors. Fixed financial assistance is provided for the purchase of professionally prescribed eyeglasses or contact lenses for vision correction.
The following services may also be included in accordance with specific criteria and only in specific institutions:
- family planning services set forth by legislation;
- artificial insemination services;
- assisted reproduction services required for In Vitro Fertilization (IVF) purposes; and
- services required for the purpose of fertility preservation set forth by legislation which are provided by a participating physician.
Moreover, with respect to drug insurance, the Régie has covered, since January 1, 1997, in addition to recipients of a financial assistance program and people aged 65 or over, insured persons who would not otherwise have access to a private drug insurance plan. In 2023‒2024, 3.9 million people were covered by the Public Prescription Drug Insurance Plan.
The Régie also covers certain services offered in pharmacies that are reimbursed by the Health Insurance Act, such as vaccinations and certain consultations (minor conditions, no diagnosis).
2.3 Insured surgical-dental services
Services insured under this plan include surgery performed by dental surgeons and specialists in oral and maxillofacial surgery, in a prescribed hospital centre or university institution.
2.4 Uninsured hospital, physician and surgical-dental services
Uninsured hospital services include:
- plastic surgery for purely cosmetic purposes;
- accommodation in a private or semi-private room at the patient's request;
- television;
- telephone;
- drugs and biological products ordered after discharge from hospital; and
- services to which the patient is entitled under the Act respecting industrial accidents and occupational diseases or other federal or provincial legislation.
The following services are not insured:
- any examination or service not related to a process of curing or preventing illness;
- psychoanalysis of any kind, unless such service is delivered in a facility maintained by an institution authorized for such purpose by the MSSS;
- any service provided solely for aesthetic purposes;
- any refractive surgery, except where there is documented failure in respect of corrective lenses and contact lenses for astigmatism of more than 3.00 dioptres or anisometropia of more than 5.00 dioptres;
- any service delivered by a professional to his or her spouse or children;
- any examination, expert appraisal, testimony, certificate or other formality required for legal purposes or by a person other than one who has received an insured service, except in certain cases;
- any visit made for the sole purpose of obtaining the renewal of a prescription;
- any examination, vaccination, immunization or injection where the service is provided to a group or for certain purposes;
- any service delivered by a professional on the basis of an agreement or contract with an employer, association or body;
- any adjustment of eyeglasses or contact lenses;
- any surgical extraction of a tooth or dental fragment performed by a physician, unless such service is provided in a hospital centre in certain cases;
- all acupuncture procedures;
- injection of sclerosing substances and the examination performed at that time;
- mammography used for detection purposes, unless this service is required by a medical prescription in a place designated by the Minister to a recipient 35 years of age or older, provided that the person has not been so examined for one year;
- thermography, tomodensitometry, magnetic resonance imaging and use of radionuclides in vivo in humans, unless these services are delivered in a hospital centre;
- ultrasonography, unless this service is delivered in a hospital centre or by a radiologist or, for obstetrical purposes, in a local community service centre recognized for that purpose;
- optical tomography of the eyeball and confocal scanning laser ophthalmoscopy of the optic nerve, unless these services are delivered in a facility maintained by an institution that operates a hospital or are delivered in association with the delivery, by intravitreal injection, of an antiangiogenic drug for the treatment of certain ocular pathologies;
- any radiological or anaesthetic service provided by a physician if required for providing an uninsured service, with the exception of a dental service provided in a hospital centre or, in the case of radiology, if required by a person other than a physician or dentist;
- any sex reassignment surgery, unless it is provided on the recommendation of a physician specializing in psychiatry and is provided in a hospital centre recognized for this purpose; and
- any services that are not related to pathology and that are delivered by a physician to a patient between 18 and 65 years of age, unless that individual is the holder of a claim booklet, for colour blindness or a refractive error, in order to provide or renew a prescription for eyeglasses or contact lenses.
3.0 Universality
3.1 Eligibility
Registration with the Hospital Insurance Plan is not required. Registration with the Régie de l'assurance maladie du Québec (the Régie) is sufficient to establish an individual's eligibility. Any individual residing or staying in Quebec as defined in the Health Insurance Act (CQLR, c A-29, hereinafter "HIA") must be registered with the Régie to be eligible for hospital services.
A person whose eligibility has been denied or who is dissatisfied with a decision of the Régie may request a review of the decision. The request for a review must be submitted to the Régie in a written notice setting out the reasons for the request. The request must be submitted within the six-month period following the date when the requester was informed of the decision.
As a last resort, within 60 days of being notified of the decision, a person may contest before the Tribunal administrative du Québec the decision for which the person has requested a review.
No relevant amendments to eligibility were made in 2023–2024.
3.2 Other categories of individuals
A person incarcerated in a federal penitentiary does not lose their status as a Quebec resident while in custody. They remain eligible for the Quebec Health Insurance Plan. Health care is provided by the federal government during the period in custody. The incarcerated person is eligible for the Public Prescription Drug Insurance Plan, and the Régie covers the prescription drug costs. On the other hand, if the incarcerated person was not a Quebec resident prior to incarceration, they will become a Quebec resident on their release day if they settle in Quebec.
Certain categories of residents, notably permanent residents under the Immigration Act and people returning to live in Canada, become eligible under the plan following a waiting period of up to three months. The waiting period for eligible individuals from other countries who are recipients of a financial assistance program and hold a claim booklet could be shortened to the date on which financial assistance benefits begin.
Canadian Forces personnel and their family members posted to Quebec from another Canadian province or territory who have status permitting them to settle there are eligible on the date of their arrival. Those who have not acquired Quebec resident status, and inmates of federal penitentiaries, become insured the day they are discharged or released.
Immediate coverage is provided for certain seasonal workers, repatriated Canadians, people from outside Canada who are living in Quebec under an official bursary or internship program of the Ministère de l'Éducation and Ministère de l'Enseignement supérieur (Quebec Department of Education and Quebec Department of Higher Education), people from outside Canada who are eligible under an agreement or accord reached with a country or an international organization, and refugees.
People from outside Canada who have work permits and are living in Quebec for the purpose of holding an office or employment for a period of more than six months may be eligible for the plan following a waiting period of up to three months.
3.2.1 Coverage of children whose migratory status is precarious
On September 22, 2021, An Act respecting mainly the health insurance plan and prescription drug insurance plan eligibility of certain children whose parents' migratory status is precarious came into effect. This law extends health and drug insurance coverage to children born to parents whose migratory status is precarious, who were not eligible until now and who are usually present in Quebec. These children will be eligible for coverage whether or not they were born in Quebec if their presence in the province for more than six months is demonstrated.
4.0 Portability
4.1 Minimum waiting period
People settling in Quebec after moving from another province of Canada are entitled to coverage under the Quebec Health Insurance Plan when they cease to be entitled to benefits from their province of origin, provided they register with the Régie de l'assurance maladie du Québec (the Régie) and meet certain conditions.
4.2 Coverage during temporary absences from Quebec
If living outside Quebec in another province or territory for 183 days or more and provided they so notify the Régie, students and full-time unpaid trainees may retain their status as residents of Quebec:
- students for a maximum of four consecutive calendar years; and
- full-time unpaid trainees for a maximum of two consecutive calendar years.
This is also the case for people living outside Quebec who are temporarily employed or working on contract there. Their resident status can be maintained for no more than two consecutive calendar years.
People who are directly employed or working on contract outside Quebec for a company or corporate body with its headquarters or a place of business in Quebec to which they report directly, or who are employed by the federal government or the Government of Quebec and are posted outside Quebec, or who are working on a contract as self-employed people while their place of business is in Quebec, also retain their status as a resident of the province. The same is true of people who remain outside the province for 183 days or more, but less than 12 months within a calendar year, provided such absence occurs only once every seven years.
People who work abroad as employees of a non-profit organization with its head office in Canada, as part of an international aid and co-operation program recognized by the MSSS, or people who stay abroad under a reciprocal agreement concluded by the MSSS, maintain their eligibility.
Insured persons who leave Quebec to settle in another province or territory of Canada remain eligible for health insurance for up to three months after their departure, but their eligibility for the Quebec drug plan ends on the day of their departure.
However, coverage for insured persons who leave Quebec to permanently move abroad terminates the day of their departure.
4.3 Reimbursement of professional services received outside Quebec
The costs of insured services provided by health professionals to an insured person in another province or territory of Canada are reimbursed for the amount actually paid or at the rate that would have been paid by the Régie for such services in Quebec, whichever is lower. Exceptionally, for the Outaouais region, Quebec has negotiated a permanent arrangement with Ontario to pay Ottawa medical specialists at the Ontario fee rate for specialized services that are not available in the Outaouais region. This agreement came into effect on November 1, 1989. The Régie covers the amount it would have paid for the same services in Quebec. The Centre intégré de services de santé et de services sociaux de l'Outaouais [Outaouais integrated health and social services centre] pays the difference between the cost invoiced by Ontario and the amount initially reimbursed by the Régie. A similar agreement was signed in December 1991 between the Centre de santé Témiscaming [Témiscaming Health Centre] and the North Bay Regional Health Centre.
The service provided must be an insured service within the meaning of the HIA. Services that are experimental in nature are not reimbursed.
4.4 Reimbursement of hospital services received in Canada
Costs for hospital services provided to an insured person in another province or territory of Canada are paid in accordance with the terms and conditions of the Hospital Reciprocal Billing Agreement regarding hospital insurance agreed to by the provinces and territories of Canada. These costs are paid either at the established per diem for hospitalization in a standard ward or in intensive care proposed by the host province and approved by all the provinces and territories or, in cases of outpatient services or expensive procedures, at the approved interprovincial rates. Services that are excluded from interprovincial agreements but covered under the provincial program are reimbursed at the rate in force.
4.5 Reimbursement of hospital services outside Canada
During a temporary stay outside Canada, the Régie reimburses the full cost of emergency hospital services and 75 per cent of the cost in other cases to students enrolled in an educational institution outside Canada; full-time unpaid interns in a university, an institution affiliated with a university, a research institute or a government or international organization; Quebec public servants posted abroad; and employees of a non-profit organization with a head office in Canada that works as part of an international aid or co-operation program recognized by the MSSS. However, when such people go on holiday outside their place of study, training or work, this coverage is no longer in force, and regular coverage for hospital services applies.
Residents of Quebec who are working or studying abroad are covered by the plan in effect in that country when the stay falls under a social security agreement reached between the MSSS and the country in question.
For residents who are not in one of the above situations and receive insured services in a hospital outside Canada, the Régie reimburses the cost of such services, when they become necessary due to an emergency or sudden illness, to a maximum of $100 per day if the patient was hospitalized, including for day surgery, or to a maximum of $50 per day for outpatient services. However, hemodialysis treatments are covered to a maximum of $220 per treatment. The services must be delivered in a hospital, or hospital centre, recognized and accredited by the appropriate authorities. No reimbursements are made for nursing homes, spas or similar establishments.
4.6 Prior approval requirement
To receive full reimbursement for professional and hospital services elsewhere in Canada or in another country, which are insured but not available in Quebec, a written request signed by two physicians with expertise in the field of the pathology of the person on whose behalf the request is made must first be sent to the Régie. The request must be accompanied by a summary of the insured person's medical file, describe the specialized services required by the insured person, attest to the unavailability of said services in Quebec or Canada, and contain information about the treating physician and the name and address of the hospital where the services are to be provided. Following an evaluation of the request by the Régie, authorization to receive the services is either given or denied. No authorization will be given if the service is available in Quebec or if it is an experimental service.
A person whose request has been denied or who is dissatisfied with a decision of the Régie de l'assurance maladie du Québec may request a review of the decision. The request for a review must be submitted to the Régie in a written notice setting out the reasons for the request. The request must be submitted within the six-month period following the date when the requester was informed of the decision.
Within 60 days of being notified of the decision, a person may contest before the Tribunal administrative du Québec the decision for which the person has requested a review.
5.0 Accessibility
5.1 Access to insured health services
Everyone has the right to receive adequate health care services without any kind of discrimination. In Quebec, the Health Insurance Act (CQLR, c A-29, hereinafter "HIA") does not allow user fees to be imposed. It also prohibits any person from demanding or receiving any payment from an insured person for incidental fees related to an insured service, except in cases prescribed by regulation or provided for in an agreement and the conditions mentioned therein. If an insured person thinks that they have been incorrectly billed fees, they may request reimbursement from the Régie de l'assurance maladie du Québec (the Régie), which will determine whether any amounts have been unjustifiably billed. If appropriate, the Régie will reimburse the insured person and will recover the amount reimbursed from the health care professional or the clinic involved. It is also possible to reimburse insured persons who have not made reimbursement requests if the Régie finds that fees have been charged to them illegally.
A situation that appears to be illegal with respect to fees charged to an insured person may also be reported to the Régie which, after verification, will follow up appropriately. These follow-ups may include an inspection or an investigation of the clinics or the professionals involved. Residents who have reason to believe they have been subject to patient charges can contact the Régie.
In more detail, as of March 31, 2024, the health and social services network had 131 institutions: 51 public and 80 private. These institutions administer 1,537 facilities or physical spaces providing health and social services to the Quebec population.
The 51 public institutions are administered by 34 president-CEOs or CEOs. They include integrated centres whose legal name is Centre intégré de santé et de services sociaux (CISSS) [health and social services centre] and Centre intégré universitaire de santé et de services sociaux (CIUSSS) [integrated university health and social services centre], as well as grouped institutions and other institutions that have been neither grouped nor merged.
As of April 1, 2015, each of the 22 integrated centres is the result of the merger of all or some of the public institutions in a given health and social services region, as the case may be, with the health and social services agency. Nine of the 22 integrated centres can call themselves a "centre intégré universitaire de santé et de services sociaux" (CIUSSS) because they are located in a health and social services region in which a university offers a complete predoctoral program of study in medicine, or because they operate a centre designated as a university institute in the field of social services.
For their part, the 29 remaining public institutions are distributed as follows:
- Five university hospital centres (UHC), one university institute, and one institution, which are not attached to an integrated centre but to the Ministry of Health and Social Services (MSSS), and which offer specialized or ultra specialized services beyond the boundaries of their health and social service region, namely:
- Québec City UHC - Université Laval;
- Quebec Heart and Lung Institute - Université Laval;
- Université de Montréal UHC;
- McGill University Health Centre;
- Ste-Justine UHC;
- Montréal Heart Institute; and
- Institut national de psychiatrie légale Philippe-Pinel.
- Five public institutions not targeted or affected by the Act to modify the organization and governance of the health and social services network, in particular by abolishing the regional agencies (chapter O-7.2) (LMRSSS) that serve a Northern or Indigenous population.
- 17 public institutions attached to an integrated centre. These institutions were not merged with other institutions under the LMRSSS but are administered by the board of the integrated centre to which they are attached.
- In addition, as of March 31, 2024, Quebec had 39 public and 6 private facilities under agreement with the mission of a hospital centre providing diagnostic services and general and specialized medical care in the physical health (CHSGS) and mental health (CHPSY: psychiatric care) sectors. As of that date, there were 21,084 beds with hospital center mission: 19,918 beds for general and specialized care (CHSGS) and 1,166 beds for psychiatric care (CHPSY). According to the most recent available data, in Quebec hospital facilities:
- From April 1, 2023, to March 31, 2024, there were 769,272 short-term care admissions and 367,871 day surgery admissions. These admissions accounted for 6,600,029 patient days.
Quebec also has four integrated university health and social services networks (réseaux universitaires intégrés de santé et de services sociaux or RUISSS) which promote co-operation, complementarity and integration of the care, teaching and research missions of the health facilities and universities with which they are affiliated. In addition to the services provided by public facilities, the population also has access to the services of private facilities which offer accommodation, long-term care and other services.
Since 2002, Family Medicine Groups (GMFs) have served as flagships for the organization of front-line health care and services in Quebec. GMFs promote teamwork, collaboration among professions, institutional responsibility to the population, and the development of trust and close collaboration between patients and clinicians. The GMF program provides financial and professional support tailored to the realities of clinicians and the needs of patients, and ensures equitable, patient-centred funding, professional support (nursing personnel, social workers, pharmacists and other health professionals), a more balanced service offer, less burdensome administrative procedures, and mandatory use of electronic health records. These features have the voluntary support of physicians and the benefit of a team funding structure.
The elementary structure of the GMFs ensures that registered patients have reasonable and timely access, as is demonstrated by the use of a measurement of patient attendance at the GMF where they are registered. Also, measures were recently added to the program to engage GMFs in a territorial service offer for patients waiting for a family physician.
As of March 31, 2023, Quebec had nearly 379 GMFs in its territory. On the same date, there were about 50 GMF networks.
5.2 Physician compensation
Physicians are remunerated in accordance with the negotiated fee schedule. The Minister may enter into an agreement with the organizations representing any class of health professional.
The HIA governs the compensation of health professionals (physicians, dentists, optometrists and pharmacists). While the majority of physicians practise within the provincial plan, Quebec allows two other options:
- professionals who have withdrawn from the plan and practise outside the plan, but agree to remuneration according to the provincial fee schedule; and
- non-participating professionals who practise outside the plan, with no reimbursement from the Régie for either them or their patients.
- To become a non-participant, a health professional must notify the Régie by registered or certified mail. The non-participation takes effect the thirtieth (30th) day from the date of mailing, and re-enrollment takes effect the eighth (8th) day following the date of mailing of the notice (Regulation respecting the application of the Health Insurance Act, s. 29).
There are various modes of remuneration:
- Fee for service: Compensation according to the service rates set out in the compensation agreements for each specialty or sector of activities for general practitioners. If the service is performed in the office, the fee is increased by approximately 30 percent to offset office expenses.
- Mixed: Include half-day and full-day rates or daily compensation and fee supplements. For general practitioners, the mixed remuneration includes a fixed fee on an hourly basis plus a percentage of the services performed. This remuneration covers all of the physician's professional activities.
- Fixed fees: Include hourly and half-day rates, as well as daily compensation.
- Salary: Salary = specialists/fixed fees = general practitioners. These two modes of compensation are based on a work week whose number of hours may vary. This method of compensation has not been accessible to new physicians since 2011.
- Lump sum: Lump sum compensation is based on a given amount paid periodically or annually to family physicians (general practitioners) for the care and medical management of a patient, as well as a supplement for the volume of patients registered and the lump sum for family practice.
- Hourly rate: Compensation method applicable in an institution. This method pays for the physician's medical activities over a continuous 60-minute period.
- Supplements (incentive measures): For example, supplements have the effect of increasing compensation in specific circumstances due to the complexity or time required to perform a service. There is also a lump sum payment for on-call duty, to compensate for medical-administrative functions (emergency chief, physician in charge of a GMF), lump sum per patient in the intensive care unit, etc.
- Special incentive measures: Some measures are aimed at encouraging physicians to practise and remain in underserved areas (e.g., isolation allowances, applicable rate of increase, basic pay).
- Establishment laboratory service: This mode governs the rate for the practice of laboratory medicine, which includes the disciplines of biomedicine, nuclear medicine and diagnostic radiology. The physician enters a billing period, the services provided and the number of times these services were rendered.
- According to the most recent data available, in 2023–2024, the Régie paid more than an estimated $8.5 billion for professional services provided to Quebec residents. Professional services (including reimbursements to insured persons and payments to professionals) received outside Quebec were estimated at $52.2 million.
- The Régie is responsible for enforcing health care professional compensation agreements and for controlling compensation paid to health care professionals. It has established a framework that enables it to enhance its controls on the basis of the risks identified, in order to ensure that the compensation paid to health care professionals complies with the terms and conditions in the agreements negotiated. The Régie has various control measures as follows:
Awareness-Raising Mechanisms
The Régie issues notifications to the MSSS with respect to issues and risks associated with controlling the payment of health care professionals on the basis of the agreements negotiated. Thus, based on its analyses, the Régie's findings may result in the issuance of notifications on different issues even if they apply more to medical practice or the organization of services.
Systematic Controls
These measures are aimed at the overall billing of health care professionals or agreement situations. The controls are carried out manually, by computer, by taking samples, or by monitoring. Systematic controls may be followed by specific controls if the Régie deems it necessary to do an in-depth analysis of a situation with a professional or a limited group of professionals (see next section).
Specific Controls (inspections, investigations, service audits performed)
These measures are aimed at the billings of a professional or a limited group of professionals for whom practices have been identified as at risk of being non-compliant or potentially abusive or fraudulent. A specific audit may also be initiated following a complaint or a tip.
The Régie recovers the amounts that have been inappropriately paid by means of a compensation or recovery mechanism.
The Régie has a monitoring mechanism to ensure that professionals with non-compliant, abusive or fraudulent billings are subject to monitoring.
5.3 Payments to hospitals
The MSSS funds hospitals through payments directly related to the cost of insured services provided.
Ontario
Ontario has one of the largest and most complex publicly funded health care systems in the world. Administered by the province's Ministry of Health (MOH), Ontario's health care system was supported by $85.46 billion in spending during 2023-2024.Footnote ii
1.0 Public administration
1.1 Health care insurance plan and public authority
Ontario Health Care and Health Care Planning
The Ontario Health Insurance Plan (OHIP) is administered on a non-profit basis by the Ministry of Health (MOH). OHIP was established in 1972 and is continued under the Health Insurance Act (HIA). Revised Statutes of Ontario, 1990, c. H-6, provide insurance in respect of the cost of insured services provided to Ontario residents (as defined in the HIA) in hospitals and health facilities, and by physicians and other prescribed health care practitioners.
The MOH funds health services to the public through programs such as health insurance, drug benefits, assistive devices, forensic mental health and supportive housing, home and community care services, community and public health, and health promotion and disease prevention. It also regulates hospitals, medical laboratories and specimen collection centres, diagnostic imaging, and emergency health services.
MOH continues to focus resources on delivering services where they are most needed, such as resuming planning for the next phase of Ontario Health (OH) transfers and transformation work.
The transformation will take place over a number of years. It will continue to roll out in carefully planned phases to ensure patient care is not interrupted.
1.2 Reporting relationship
Section 2 of the HIA stipulates that the Minister of Health is responsible for the administration and operation of OHIP and is Ontario's public authority for the purposes of the Canada Health Act.
Annually, the MOH reports on its plans, results and outcomes via a published plan and annual report. The MOH's published plan and annual report are tabled in the legislature and published on the MOH's website.
1.3 Audit of accounts
Every year the Auditor General of Ontario reports on the results of their examination of government resources and administration. The Auditor General's report is tabled by the Speaker of the Legislative Assembly, usually in the fall, at which time it becomes available to the public. Audit reports on select areas of the MOH chosen for review by the Auditor General are included within this annual report, the latest of which was released on December 6, 2023.
The MOH's accounts are published annually in the Public Accounts of Ontario. The 2023-2024 Public Accounts of Ontario were released on September 19, 2024.
The Auditor General of Ontario's 2023 Annual Report was released on December 6, 2023. The following sections made specific reference to the operation of OHIP:Footnote iii
- Value-for-Money Audit: Emergency Departments;Footnote iv
- Value-for-Money Audit: Hospitals in Northern Ontario: Delivery of Timely and Patient-Centred Care;Footnote v
- Follow-Up on Recommendations from 2021 Annual Report Value-for-Money Audits (Chapter 1): Outpatient Surgeries;Footnote vi and
- Follow-Up on Special Reports (Chapter 2): COVID-19 Preparedness and Management – Management of Health-Related COVID-19 Expenditures (Chapter 4).Footnote vii
2.0 Comprehensiveness
2.1 Insured hospital services
Insured in-patient and out-patient hospital services in Ontario are prescribed in sections 7 and 8 of Regulation 552 under the Health Insurance Act (HIA).
In keeping with the provisions of the Canada Health Act, the Ontario Health Insurance Plan (OHIP) insures all medically necessary hospital services. Hospital services are all services that are medically required to be performed in hospital. These are described in the Regulations as follows.
Insured in-patient hospital services include medically required:
- use of operating rooms, obstetrical delivery rooms, and anaesthetic facilities including necessary equipment and supplies;
- necessary nursing services;
- laboratory, radiological, and other diagnostic procedures together with the necessary interpretations for the purpose of maintaining health, preventing disease, and assisting in the diagnosis and treatment of any injury, illness or disability;
- drugs, biologicals and related preparations; and
- accommodation and meals at the standard ward level.
Insured out-patient services include medically required:
- laboratory, radiological, and other diagnostic procedures, together with necessary interpretations;
- use of radiotherapy, occupational therapy, physiotherapy, and speech therapy facilities, where available;
- use of diet counselling services;
- use of the operating room and anaesthetic facilities;
- surgical supplies;
- necessary nursing service;
- supply of drugs, biologicals, and related preparations (subject to some exceptions);
- certain other specified services such as the provision of certain equipment, to hemophiliac patients for use at home; and
- certain specified home-administered drugs.
Each individual hospital service is not specifically listed in Regulation 552; rather, the Regulation lists the above broad categories of services so that new medical and technological advances are automatically included as they become accepted standards of practice in Ontario.
Per the 2012 OMA Representation Rights and Joint Negotiations and Dispute Resolution Agreement, the Ministry of Health (MOH) recognizes the Ontario Medical Association (OMA) as the exclusive representative of physicians practicing in Ontario. Under this agreement and the 2017 Binding Arbitration Framework, the MOH and the OMA are required to negotiate any changes affecting physician compensation in Ontario. This includes changes to insured physician services provided in hospital and listed in the Schedule of Benefits for Physician Services.
Regulatory changes are approved by Cabinet and generally there is a public consultation process by way of Ontario's Regulatory Registry.
There was one regulation change regarding the provision of insured hospital services completed in fiscal year 2023-2024, which amended Regulation 552 under the HIA to authorize payment to physicians for interpretation of diagnostic procedures ordered by nurse practitioners and oral and maxillofacial surgeons within the legislated scope of practice for those professions.
2.2 Insured physician services
Insured physician services are prescribed in Regulation 552 under the HIA. Under Regulation 552 of the HIA, a service provided by a physician in Ontario is an insured service if it is:
- is medically necessary;
- is listed in the Schedule of Benefits for Physician Services; and
- is rendered in such circumstances or under such conditions as specified in the Schedule of Benefits for Physician Services.
Physicians provide insured medical, surgical, and diagnostic services, including primary health care services. Services are provided in a variety of settings, including physicians' offices, community health centres, hospitals, mental health facilities, licensed Integrated Community Health Services Centres, and long-term care homes. Physicians also provide certain insured services virtually, where appropriate.
In general terms, insured physician services include:
- consultations and visits for diagnosis and treatment of medical conditions;
- maternity care;
- anaesthesia;
- counselling and mental health care services;
- immunizations; and
- surgical procedures.
Physicians must be registered to practice medicine in Ontario by the College of Physicians and Surgeons of Ontario (CPSO), and both the patient and physician must be physically located in Ontario when the service is rendered in order for the services provided by an Ontario physician to be covered under OHIP. On July 24, 2023, Ontario approved legislative amendments that enabled inter-jurisdictional mobility for physicians with independent practice certificates in other Canadian provinces and territories, whereby eligible out-of-province physicians now have six months from the point of application with the CPSO to practise in Ontario without a licence.
During 2023-2024, most physicians were paid for all insured services rendered to insured persons directly by OHIP, and a small number of physicians billed the insured person. Physicians who do not bill OHIP directly are commonly referred to as having opted-out of OHIP. When a physician has opted-out of OHIP the physician bills the patient an amount not exceeding the amount payable for the service under the Schedule of Benefits for Physician Services (this was permitted on a 'legacy' basis following proclamation of the Commitment to the Future of Medicare Act [CFMA] in 2004). The patient then recoups that amount from OHIP.
There were approximately 36,224 physicians who submitted claims to OHIP in 2023-2024. This figure includes physicians submitting both fee-for-service claims and physicians included in an alternative payment plan who submitted tracking or shadow-billed claims. There are currently 11 opted-out physicians in Ontario.
The Schedule of Benefits for Physician Services is regularly reviewed and revised to reflect current medical practice and new technologies. As described above, changes to the Schedule of Benefits for Physician Services must be negotiated with the OMA.
Please note that as of fiscal year 2023-2024, all temporary physician payment initiatives related to the COVID-19 pandemic have been discontinued.
2.3 Insured surgical-dental services
In accordance with the Canada Health Act, certain surgical-dental services are prescribed as insured services under Regulation 552 in the HIA and listed in the Schedule of Benefits for Dental Services. The HIA authorizes OHIP to pay for a limited number of procedures when the procedure is performed in a public hospital graded under the Public Hospitals Act as Group A, B, C, or D, by a dental surgeon who has been appointed to the dental staff of the public hospital.
Generally, insured dental services include:
- oral and maxillofacial surgery that would normally be required to be performed in a hospital;
- root resection and apical curettage procedures when performed in association with other insured dental procedures; and
- dental extractions when performed in a hospital for the safety of high-risk patients and if prior approval is obtained from the MOH.
With respect to insured surgical-dental services, the MOH negotiates with the Ontario Dental Association (ODA) when making changes to the Schedule of Benefits for Dental Services.
The required regulatory changes are approved by Cabinet and generally there is a public consultation process by way of Ontario's Regulatory Registry.
In Ontario, in the fiscal year 2023-2024, 927 dentists had active billing numbers and 231 dentists billed OHIP. There were 696 dentists who had active billing numbers but did not bill OHIP. Following proclamation of the CFMA in 2004, dentists are required to submit claims for all insured surgical-dental services to OHIP, i.e., are prohibited from charging the patient for insured services. No dentists are 'opted-out' under 'legacy' provisions.
2.4 Uninsured hospital, physician and surgical-dental services
Uninsured hospital services include but are not limited to:
- private or semi-private accommodation unless no ward room is available and if not prescribed by a physician, oral maxillofacial surgeon, or midwife due to a patient's condition;
- telephones and televisions;
- charges for certain private-duty nursing;
- provision of medications for patients to take home from hospital, with prescribed exceptions; and
- services that are not medically necessary.
Section 24 of Regulation 552 details some specified physician and dental surgical services that are not insured services. Uninsured physician services include:
- services that are not medically necessary;
- services not listed in the Schedule of Benefits for Physician Services;
- "add-ons" to insured services that are considered non-medically necessary and optional upgrades to a basic insured service (e.g., upgraded cataract lenses, specialized testing for cataract surgery, fibreglass casts, etc.); and
- services that meet the circumstances set out in section 24 of Regulation 552. For example, and with some exceptions, a service, including an annual health or annual physical examination, received wholly or partly for the production or completion of a document or transmission of information to a third party (e.g., insurance company, employer, Workplace Safety and Insurance Board [WSIB], etc.) may be uninsured.
Under section 24 of Regulation 552 of the HIA, treatment for a medical condition that is generally accepted within Ontario as experimental is also not insured.
Dental services provided in dentists' private offices are not insured and payment is the responsibility of the individual patient or their private insurer if applicable. Dental services not specifically listed in the Schedule of Benefits for Dental Services are not insured, including such services as prosthetic restorations (fixed bridges and dentures) for the replacement of teeth, orthodontic treatment, fillings, and crowns.
In an effort to uphold requirements under the Canada Health Act to prohibit extra-billing and user charges (EBUC) for insured health care services, Ontario's CFMA provides authority to obtain information and take certain actions related to allegations of EBUC. Specifically, with respect to EBUC, the CFMA makes it illegal:
- for a physician or designated practitioner to charge or accept payment or other benefit for rendering an insured service to an insured person in addition to the amount that is paid by OHIP (subject to a few specified exceptions). Such charges are "unauthorized payments" that are commonly called extra-billing;
- for a physician or designated practitioner to accept payment or benefit for an insured service rendered to an insured person except from OHIP (subject to a few specified exceptions);
- for any person or entity to charge or accept payment or other benefit for an insured service rendered to an insured person except as outlined above or as specified in Regulation 552.
For comprehensive information on the CFMA, please refer to section 5.1.
Under the Integrated Community Health Services Centres Act, 2023 (ICHSCA), which repealed and replaced the Independent Health Facilities Act on September 25, 2023, the MOH provides facility cost funding for services or overhead costs that support, assist or are a necessary adjunct to the provision of insured services rendered in non-hospital health facilities when these costs are not included as part of the insured service. Under the ICHSCA, facility costs are payable only by the MOH or OH to a licensed Integrated Community Health Services Centre, and charges to or receipt of a facility cost payment from a patient or in any other manner is an illegal facility cost.
The MOH reviews all possible violations of the CFMA and ICHSCA that come to its attention. Possible violations come to the MOH's attention from various sources such as patient complaints, the Ontario Patient Ombudsman, the media, advertisements, health care providers and their staff and Members of Provincial Parliament. In some cases, the MOH may also review possible violations of the CFMA and ICHSCA on a proactive basis (i.e., without receiving a complaint tied to a specific patient). If it is found that a patient has paid an unauthorized payment, the MOH ensures that patients are reimbursed in accordance with provisions of the CFMA or the ICHSCA.
Providers and facilities are legally permitted to charge patients for uninsured services, either on a fee-for-service basis, or through a block or annual fee, which covers a group of uninsured services rendered by a physician, practitioner, or hospital over a specified time period.
The MOH does not regulate charges for uninsured services, or for services rendered to uninsured persons nor does the MOH set prices for uninsured services.
The College of Physicians and Surgeons of Ontario (CPSO), the body governing the practice of medicine in Ontario, is responsible for ensuring that charges by physicians for uninsured services, including block fees are in accordance with professional standards of practice. The MOH's interest in block fees is to ensure that they do not create a barrier to accessing insured services, do not include charges for insured services, do not confer preferential access to insured services, or constitute illegal facility fees contrary to Ontario law. However, the MOH does not regulate the amount charged for block fees or the types of uninsured services that may or may not be included in block fees.
The CPSO has established guidelines with respect to charging patients for uninsured services and is responsible for investigating professional practice complaints against physicians, such as for excessive fees. The MOH directs patients who have complaints regarding charges for uninsured services to the CPSO.
3.0 Universality
3.1 Eligibility
Section 11 of the Health Insurance Act (HIA) specifies that every person who is a resident of Ontario is entitled to become an insured person under the Ontario Health Insurance Plan (OHIP) upon application, in accordance with the HIA and the regulations.
To be considered an Ontario resident, Regulation 552 under the HIA, with a few exceptions that are noted in the Regulation, requires that a person must:
- have Canadian citizenship or an immigration status as prescribed in Regulation 552; and
- make their primary place of residence in Ontario; and
- be physically present in Ontario for at least 153 days in the first 183 days after becoming a resident, unless the person is moving to Ontario directly from another province or territory of Canada where the person was insured or meets other limited exceptions; and
- be physically present in Ontario for at least 153 days in any 12-month period, subject to some exceptions.
Individuals who are not eligible for OHIP coverage are those who do not meet the definition of a resident, such as tourists, visitors to the province, and those who do not hold an immigration status as defined in Regulation 522. Services that a person is entitled to receive under federal legislation are not OHIP-insured services. These include services provided to federal penitentiary inmates and Canadian Forces members. Services that a person is entitled to receive under the Workplace Safety and Insurance Act are also not insured services under OHIP.
When it is determined by ServiceOntario that a person is not a resident and is not eligible, or is no longer eligible, for OHIP coverage, a request may be made by the person (or their authorized representative) to the Ministry of Health (MOH) to review the decision. Anyone may request that the MOH review the denial of their OHIP eligibility by making a request in writing to the OHIP Eligibility Review Committee (OERC). Those who do not agree with the OERC's decision regarding their OHIP eligibility may request an appeal by the Health Services Appeal and Review Board.
The HIA provides no authority for MOH or any other person to provide OHIP coverage to persons who are not eligible under Regulation 552 of the HIA.
The MOH is the sole payor for medically necessary OHIP insured physician, hospital, and hospital surgical-dental services. An eligible Ontario resident may not obtain any benefits from another insurance plan for the cost of any insured service that is covered by OHIP. As noted below, the waiting period for the commencement of OHIP coverage was removed in 2020.
Persons who were previously ineligible for OHIP coverage but whose status and/or residency situation has changed may be eligible for coverage for OHIP upon application, subject to the requirements of Regulation 552. There were 14,901,258 valid and active health card users in Ontario as of March 31, 2024.
3.2 Other categories of individuals
The MOH provides health insurance coverage to a limited number of specified categories of individuals in Ontario, other than Canadian citizens and permanent residents or landed immigrants.
These individuals are required to provide acceptable original documentation to support that they meet the definition of resident for the purposes of OHIP coverage in the same manner as Canadian citizens and permanent resident or landed immigrant applicants.
The individuals listed below may be eligible for OHIP coverage in accordance with Regulation 552 of the HIA. Individuals are required to apply in person at ServiceOntario, which has the government-wide mandate for the delivery of front-facing services to the residents of Ontario, including the issuance of the Ontario Photo Health Card.
As of March 19, 2020, the province has removed the three-month waiting period requirement for OHIP coverage to commence.
Applicants for Permanent Residence: These are persons who have submitted an application for permanent resident status to Immigration, Refugees and Citizenship Canada (IRCC), and IRCC has confirmed that the person meets the eligibility requirements to apply for permanent residence in Canada and that the application has not yet been denied.
Protected Persons/Convention Refugees: These are persons who are determined to be Protected Persons/Convention Refugees under the terms of the federal Immigration and Refugee Protection Act (IRPA).
Holders of Temporary Resident Permits: A Temporary Resident Permit is issued to an individual by IRCC when there are compelling reasons to admit an individual into Canada who would otherwise be inadmissible under IRPA. Each Temporary Resident Permit has a case type or numerical designation on the permit that indicates the circumstances allowing the individual entry into Canada. Individuals who hold a permit with a case type of 86, 87, 88, 89, 90, 91, 92, 93, 94, 95 (or 80 for adoption only) are eligible for OHIP coverage.
Foreign Clergy, Temporary Foreign Workers and their Accompanying Family Members: An OHIP-eligible foreign member of the clergy is a person who is sponsored by a religious organization or denomination if the member has finalized an agreement to minister to a religious congregation or group in Ontario for at least six months, as long as the member is legally entitled to stay in Canada.
A temporary foreign worker is eligible for OHIP if the individual has a work permit or other document issued under IRPA that permits the person to work in Canada, and if the person also has a formal agreement in place to work full-time for an employer in Ontario and is working under that agreement for no less than six consecutive months. To be eligible for OHIP, the work permit or other document issued by IRCC, or a letter provided by the employer, must set out the employer's name, state the person's occupation with the employer, and state that the person will be working full-time for an employer in Ontario for no less than six consecutive months.
A self-employed temporary foreign worker is also eligible for OHIP if the individual has been issued a work permit or other document under IRPA that permits the person to work in Canada while self-employed if the self-employment is full-time, the person is working in Ontario, and will continue to do so for no less than six consecutive months.
A spouse and/or dependant (under 22 years of age; or 22 years of age or older if dependent due to a mental or physical disability) of an eligible foreign member of the clergy or an eligible temporary foreign worker is also eligible for OHIP coverage as long as the spouse or dependant is legally entitled to stay in Canada.
Applicants for Canadian Citizenship: These individuals are eligible for OHIP coverage if they have submitted an application for Canadian citizenship under section 5.1 of the federal Citizenship Act, even if the application has not yet been approved, provided that IRCC has confirmed that the person meets the eligibility requirements to apply for citizenship under that section and the application has not yet been denied.
Children Born Out-of-Country: A child born to an OHIP-eligible parent who was transferred from Ontario to receive insured health services that were pre-approved for payment by OHIP is eligible for immediate OHIP coverage provided that the parent was pregnant at the time of departure from Ontario.
Seasonal Agricultural Farm Workers: Are persons who have a Work Permit issued under the Seasonal Agricultural Worker Program administered by the Government of Canada. Due to the special nature of their employment, seasonal agricultural farm workers do not have to meet any other residency requirements.
Holders of Emergency Authorizations: Are persons in Ontario who have been granted an emergency authorization to enter into and remain in Canada for humanitarian reasons for the duration of that authorization or any subsequent authorizations issued for the same reason.
3.3 Premiums
No premiums are required to obtain OHIP coverage. There is an Ontario Health Premium that is collected through the provincial income tax system, but it is not connected to OHIP registration or eligibility in any way. Responsibility for the administration of the Ontario Health Premium lies with the Ontario Ministry of Finance.
4.0 Portability
4.1 Minimum waiting period
Prior to March 19, 2020, in accordance with section 5 of Regulation 552 under the Health Insurance Act (HIA), individuals who moved to Ontario were typically entitled to Ontario Health Insurance Plan (OHIP) coverage three months after establishing residency in the province unless listed as an exception in Regulation 552, or subsection 11(2.1) of the HIA.
Effective March 19, 2020, in response to the COVID-19 pandemic, Regulation 552 under the HIA was amended to remove the waiting period for OHIP for all new and returning residents of Ontario. As such, there is currently no waiting period for OHIP coverage.
4.2 Coverage during temporary absences in Canada
Ontario adheres to the terms of the Interprovincial Agreement on Eligibility and Portability (EPA). Under section 1.6 of Regulation 552, and in accordance with the EPA, an insured person who leaves Ontario temporarily to travel within Canada, without establishing residency in another province or territory, may continue to be covered by OHIP for a period of up to 12 months.
An insured person who temporarily seeks or accepts employment in another province or territory may continue to be covered by OHIP for a period of up to 12 months. If the individual plans to remain outside Ontario beyond the 12-month maximum, they should apply for coverage in the province or territory where that person has been working or seeking work.
As per section 1.8 of Regulation 552, and in accordance with the EPA, insured Ontarians who are temporarily absent from Ontario, but remain within Canada, for full-time enrollment as a student in an academic program in an education institution in another province or territory of Canada are eligible for continuous OHIP coverage for the duration of their continuous full-time studies, provided they do not establish permanent residency elsewhere during this period. To ensure that they maintain continuous OHIP eligibility, a student should provide the Ministry of Health (MOH) with documentation or information from their educational institution confirming registration as a full-time student. Insured family members (spouses and dependents) of students who are studying in another province or territory are also eligible for OHIP while accompanying students for the duration of their studies.
Also, in accordance with sections 1.6 and 1.8 of Regulation 552 of the HIA, most insured residents who want to travel, work or study outside Ontario, but within Canada, and maintain OHIP coverage, must have been physically present in Ontario or been a mobile student or mobile worker for at least 153 days in the last 12-month period immediately prior to departure from Ontario.
Payments for insured out-of-province services are prescribed under sections 28, 28.0.1, 28.0.2, and 29 of Regulation 552 of the HIA. Insured residents who are temporarily outside of Ontario can use their valid Ontario health card to obtain insured physician (except in Quebec) and hospital services generally at no direct cost.
Ontario participates in Reciprocal Hospital Billing Agreements with all other provinces and territories for payment of insured in-patient and out-patient hospital services. For the 2023-2024 year, rates were set and approved by the Interprovincial Health Insurance Agreements Coordinating Committee. Payment for in-patient services depends on the hospital's approved in-patient per diem rate. Payment for out-patient services is at the standard approved out-patient rate.
Ontario is also party to the Reciprocal Medical Billing Agreements with all other provinces and territories, except Quebec (which does not participate in reciprocal medical billing). Ontario residents who have been directly billed for insured physician or hospital services in another province or territory can submit their receipts to MOH for reimbursement. Reimbursement of insured physician services is at the rates payable in the Ontario Schedule of Benefits for Physician Services or the amount billed, whichever is less. Reimbursement of insured hospital services is at the established rates or the amount billed, whichever is less.
Physicians and hospitals are not parties to the Reciprocal Hospital Billing and Reciprocal Medical Billing Agreements and such providers in other provinces and territories may bill Ontario residents directly for services rendered. Ontario residents billed directly may submit claims for reimbursement to OHIP.
Out-of-province (Within Canada)
Out-of-province (but within Canada) authorized laboratory services performed outside of a publicly funded hospital require prior approval of funding in accordance with Section 28.0.2 of Regulation 552. In addition, certain medical services that require prior approval of funding in Ontario (as prescribed in the Schedule of Benefits for Physician Services such as breast reduction and panniculectomy) must be prior approved if the service is sought in another province or territory.
4.3 Coverage during temporary absences outside Canada
Residents may be temporarily outside of Canada for a total of 212 days in any 12-month period after the first 183 days after becoming a resident and still maintain OHIP coverage as long as their primary place of residence remains Ontario.
Extended Absences
Health insurance coverage for insured Ontario residents during extended absences (longer than 212 days) outside Canada is governed by Regulation 552 of the HIA.
The MOH requests that residents apply to MOH to confirm this coverage before their departure and provide documents explaining the reason for their absence.
In accordance with Regulation 552 and MOH policy, most applicants must also have been residents in Ontario for at least 153 days in each of the two consecutive 12-month periods before their expected date of departure.
The length of time that a person can receive continuous Ontario health insurance coverage during an extended absence outside Canada varies depending on the reason for the absence as follows:
| Reason | OHIP coverage |
|---|---|
| Study | Duration of full-time academic studies (unlimited) |
| Work | Five 12-month terms (specific residency requirements must be met for two years between absences) |
| Charitable Worker | Five 12-month terms (specific residency requirements must be met for two years between absences) |
| Vacation/Other | Two 12-month terms (specific residency requirements must be met for five years between absences) |
Spouses and dependants may also qualify for continuous OHIP coverage while accompanying the primary applicant on an extended absence outside Ontario or Canada.
Out-of-country coverage for Ontario residents who are temporarily absent
Regulation 552 under the HIA sets out eligibility criteria and payment authority for funding emergency health care costs incurred by eligible Ontarians who are temporarily absent from Canada, such as for travel, work, and studying.
The provisions under this program provide reimbursement at very limited rates for medical treatment required to treat illnesses, diseases, conditions, or injuries that are acute, unexpected, arose outside of Canada and required immediate treatment.
OHIP reimburses patients at the following rates:
- in-patient hospital expenses at $200/$400 CAD per day for standard in-patient care/intensive in-patient care;
- emergency out-patient hospital services eligible for OHIP coverage up to a maximum of $50 CAD per day or the amount billed – whichever is less; and
- physician services are reimbursed at the rates listed in the Ontario Physician Schedule of Benefits or the amount billed, whichever is less.
These provisions are intended and designed to provide a very limited amount of funding for the medical treatment of insured residents of Ontario if they incur costs related to an unexpected illness, disease, condition or injury that arose while they are outside of Canada and that requires immediate treatment. This program does not fund treatment if the illness, disease, condition, or injury arises before the patient leaves Canada, or if it is not acute or unexpected.
4.4 Prior approval requirement
As set out in Regulation 552 under the HIA, payment for non-emergency health services provided outside of Canada requires written prior approval from the General Manager of OHIP before the services are rendered.
With written prior approval, full funding for out-of-country medical services is paid directly to out-of-country hospitals, health facilities, and physicians as well as laboratories for medically necessary insured services that are not performed in Ontario or, with the exception of laboratory services, for services that cannot be obtained in Ontario without medically significant delay.
For clarity, out-of-country/out-of-province medical services operate as two distinct programs:
- One program is for medical services, where the insured person travels to receive hospital and/or physician services.
- The other program is for laboratory services including genetic testing services where the insured person does not travel. Instead, specimens collected in Ontario are sent to the out-of-country/out-of-province laboratory.
In accordance with the requirements of Regulation 552 under the HIA, the requested out-of-country medical services are eligible for funding as insured services only if they are:
- performed at a licensed hospital or health facility as defined in the Regulation; and
- generally accepted by the medical profession in Ontario as appropriate for a person in the same medical circumstances as the insured person; and
- medically necessary, and either:
- not performed in Ontario by an identical or equivalent procedure; or
- if the identical or equivalent procedure is performed in Ontario, it is medically necessary that the insured person travel outside of Canada to avoid a delay that would result in death, or medically significant irreversible tissue damage; and
- not experimental or for the purposes of research or a survey.
Requests for prior approval of funding must be submitted by an Ontario physician and generally require written confirmation from a specialist, as defined in the Schedule of Benefits, in the type of services for which prior approval has been requested, to confirm that the regulatory criteria for the funding of out-of-country medical services are met. This requirement does not apply to emergency services or services that are within a general practitioner's scope of practice.
Depending on the nature of the service being requested, other requirements in section 28.4 of Regulation 552 may apply.
Funding requirements for laboratory services performed outside Canada are described in section 28.5 of Regulation 552 of the HIA.
In the case of a denial of funding, the referring Ontario physician and the patient are advised that the decision may be reviewed by the MOH if additional medical information is submitted for consideration. Internal reviews may be requested as often as needed, provided new additional supporting medical documentation is submitted. In addition, the patient may appeal an out-of-country funding decision to the Health Services Appeal and Review Board.
5.0 Accessibility
5.1 Access to insured health services
Funding for all insured hospital, physician, health facility and practitioner services provided to insured Ontario residents is in accordance with the Health Insurance Act (HIA) and regulations. Access to insured services without charges is protected under Part II of the Commitment to the Future of Medicare Act (CFMA), "Health Services Accessibility." The CFMA prohibits extra-billing by including a provision that prohibits any physician or designated practitioner from charging or accepting payment or other benefit for rendering an insured service to an insured person for more than the amount that is paid by Ontario Health Insurance Plan (OHIP). The CFMA also prohibits a physician or designated practitioner from accepting payment or benefit for an insured service rendered to an insured person except from OHIP (subject to a few specified exceptions) and prohibits any person or entity from charging or accepting payment or other benefit for an insured service rendered to an insured person except as outlined above or as specified in the regulations.
The CFMA further prohibits queue-jumping through a provision that prohibits any person or entity from paying, charging, or accepting payment or other benefit in exchange for conferring upon an insured person a preference in obtaining access to an insured service. In addition, the CFMA prohibits physicians, practitioners, and hospitals from refusing to provide an insured service if an insured person chooses not to pay a "block" or "annual" fee for uninsured services.
The CFMA contains provincial offence provisions, where individuals and corporations in violation of the Act may be subject to fines set out in the Act.
The Ministry of Health (MOH) reviews all possible contraventions of the CFMA that come to its attention. For situations in which it is determined that an unauthorized payment has occurred, the MOH takes steps to ensure that the amount is repaid to the payee.
For complaints regarding charges for insured services, the CFMA program of the MOH can be reached at 1-888-662-6613 or by email at: protectpublichealthcare@ontario.ca.
Health Card Validation (HCV) assists health care providers with access to information requested for claims payment. HCV allows the provider to determine the point-in-time validity of a patient's Ontario health number (and version code) indicating eligibility or ineligibility for provincially funded health care services, thereby reducing claim rejects. A health care provider may subscribe for validation services if they have a valid and active billing number as assigned by the MOH. If patients require access to insured services and do not have a valid health card in their possession, upon obtaining patient consent, the provider may obtain the necessary information by utilizing the accelerated health number release service provided by ServiceOntario's Health Number Look Up service, which is offered 24 hours a day, 365 days per year to physicians or hospitals registered for this service.
Acute care priority services are designated, highly specialized, hospital-based services that deal with life-threatening conditions such as organ transplants, cancer surgery and treatments, and neurosurgery services. These services are often high-cost and are rapidly growing, which has made access a concern. Generally, these services are managed provincially, on an ongoing basis by continually monitoring demand and adjusting funding as needed.
Acute care priority services include:
- selected cardiovascular services;
- selected neurosurgery services;
- selected cancer services;
- chronic kidney disease services;
- critical care services; and
- organ and tissue donation and transplantation.
Primary Health Care: The various primary health care physician compensation models encourage access to comprehensive primary health care services for Ontario as a whole, as well as for targeted population groups and remote underserviced communities.
Interprofessional care models
Family Health Teams (FHTs) are independent, non-profit organizations that provide interdisciplinary team-based primary health care; they are staffed by providers such as nurse practitioners, nurses, social workers, and dieticians. Physician groups that can affiliate with and participate in FHTs are funded by one of three compensation options: Blended Capitation (such as Family Health Network or Family Health Organization), Complement Based Models (Rural and Northern Physician Group Agreement or other specialized agreements) and Blended Salary Model (for community sponsored FHTs). FHT are located across Ontario, in both urban and rural settings, ranging in size, structure, scope and governance.
Nurse Practitioner-Led Clinics (NPLCs) have been created throughout Ontario to provide comprehensive, accessible and coordinated family health care services by targeting Ontarians who have difficulty accessing primary care. NPLCs are contributing to a number of local and provincial health care priorities by providing faster access to care and collaborating with other community partners to improve quality and better coordinate care for their patients.
Community Health Centres (CHCs) are models of primary health care delivery that play a key role delivering primary health care services to priority populations across Ontario and support the province's overarching efforts to transform primary care. CHCs are not-for-profit community governed organizations with a primary focus to improve the health and well-being of populations who have traditionally faced barriers accessing health services, including those who are low income, new immigrants, those with complex mental health issues and individuals who do not have health insurance. CHCs are mandated to deliver comprehensive primary health care services, health promotion, and disease prevention services to individuals and families. CHCs develop partnerships that focus on broader health and social issues, such as inadequate housing, literacy, pollution, and other social determinants of health.
Indigenous Primary Health Care Organizations (IPHCOs) are Indigenous-governed primary health care organizations that provide a combination of traditional healing, primary care, cultural programs, health promotion programs, community development initiatives, and social support services to First Nations, Métis, and Inuit Communities. IPHCOs are closely modelled after Ontario's Community Health Centres and provide the mechanisms to improve the health and well-being of communities in Ontario facing various barriers in accessing health care. IPHCOs serve as a key contributor to Ontario's commitment to improve and expand access to comprehensive primary care by providing clinical care services, integrated chronic disease prevention and management, family focused maternal/child health care, and addictions counselling and mental health care.
Health Care Connect (HCC) refers Ontarians who are seeking a primary health care provider (family doctor or nurse practitioner) to a provider who is accepting new patients in their community. Insured persons without a primary health care provider who register with HCC may be referred to a family doctor or a nurse practitioner if there is a participating provider who is accepting new patients in their community. HCC is voluntary for both patients and providers and there is no guarantee that a referral will be made for each program registrant.
During 2023-2024, MOH continued to administer various initiatives to improve access to health care services across the province. Ontario's physician supply has been stable for the past number of years due to past medical school expansion. Nevertheless, Ontario's ongoing evidence-informed physician planning recently pointed to the need to adjust medical school enrolment to ensure ongoing and future stability. To that end, Ontario is expanding medical school education in the province, adding 260 undergraduate seats and 449 postgraduate positions over the next five years. 60 per cent of these will be allocated for family medicine training positions.
In addition to physicians, building on previous investments, Ontario is further expanding nursing education by adding 1,000 registered nurse and 500 registered practical nurse education seats at public colleges and universities starting in 2023-2024. Ontario is also adding 150 nurse practitioner education seats starting in 2023-2024.
Ontario also continues to work to enhance the retention and distribution of physicians through a range of measures, such as:
- supporting rural and remote clinical education opportunities for medical students;
- supporting Remote First Nations medical resident training positions to address First Nations primary health care in northern Ontario;
- supporting the Northern Ontario School of Medicine;
- supporting training and assessment programs for International Medical Graduates and other qualified physicians who do not meet certain requirements for practice in Ontario; and
- supporting Ontario Health to help recruit and retain health care professionals in Ontario communities that need them.
There are a number of existing initiatives to improve access across Ontario, including but not limited to the Northern and Rural Recruitment and Retention Initiative, the Northern Physician Retention Initiative, the Northern Health Travel Grant Program, the Learn and Stay Grant, and the Community Commitment Program for Nursing.
Northern and Rural Recruitment and Retention Initiative (NRRRI): The NRRRI supports the recruitment and retention of physicians in rural and northern communities. The NRRRI provides financial recruitment incentives to physicians who establish a fulltime practice in an eligible community. Community eligibility for the NRRRI is based on a Rurality Index for Ontario score of 40 or more. Also eligible are the five Northern Ontario Urban Referral Centres (Thunder Bay, Sudbury, North Bay, Sault Ste. Marie, and Timmins).
Northern Physician Retention Initiative (NPRI): The NPRI provides physicians who have completed a minimum of four years of continuous full-time practice in Northern Ontario with a retention incentive paid at the end of each fiscal year in which they continue to practise full-time in Northern Ontario. NPRI supports retention of physicians in Northern Ontario and encourages them to maintain active hospital privileges. Northern Ontario is defined as the districts of Algoma, Cochrane, Kenora, Manitoulin, Nipissing, Parry Sound, Rainy River, Sudbury, Thunder Bay, and Timiskaming.
Northern Health Travel Grant (NHTG) Program: The NHTG Program helps defray travel-related costs for residents of Northern Ontario who must travel long distances to access OHIP insured medical specialist services, or Ministry funded health care facility-based procedures that are not locally available, within a radius of 100 kilometres. In addition to travel grants based on kilometric rate, the Program provides an accommodation allowance of $100-$550 (dependent on the number of lodging nights) per eligible treatment trip to patients whose one-way road distance to the nearest medical specialist able to render needed care is at least 200 kilometers. In 2017-2018, a $9.9 million enhancement was introduced to move from a $100 flat rate accommodation allowance to a maximum of $550, dependent on the number of medically necessary lodging nights. The NHTG Program also promotes using specialist services located in Northern Ontario, which encourages more specialists to practice and remain in the north.
Learn and Stay Grant: In Spring 2023, Ontario launched the new Learn and Stay Grant for up to 2,500 eligible postsecondary students who enroll in priority programs, such as nursing, and work in underserved communities in the region where they studied after graduation.
Community Commitment Program for Nursing (CCPN): CCPN provides an incentive of $25,000 for up to 3,000 nurses in 2022-2023 and 2023-2024 in exchange for a two-year commitment to work at a hospital, long-term care facility, home and community care agency, primary care service provider and mental health service provider in a high-need area of Ontario.
5.2 Physician compensation
Physicians are paid for the services they provide through a number of mechanisms. Many physician payments are provided through fee-for-service arrangements. Fee-for-service remuneration is based on the Schedule of Benefits for Physician Services a document incorporated by reference into Regulation 552 under the HIA. Other physician payment models include Primary Health Care Models (such as blended capitation models), Alternate Payment Plans, and funding arrangements for physicians in Academic Health Science Centres.
Physicians that belong to these other payment models may also bill fee-for-service when providing services that are outside of the scope of these models.
In fiscal year 2023-2024, 98.9 per cent of primary care physicians received fee-for-service payments from OHIP, but fewer than 22 per cent of them were paid solely on a fee-for-service basis. The majority (greater than 78 per cent) of primary care physicians in Ontario received funding through one of the primary health models: Comprehensive Care, Family Health Group, Family Health Network, Family Health Organization, Community Health Centres, Rural and Northern Physician Group Agreement, Group Health Centre, Blended Salary Model, and specialized agreements.
The MOH negotiates physician compensation with the OMA in accordance with the OMA Representation Rights and Joint Negotiation and Dispute Resolution Agreement. In 2017, the MOH and the OMA ('the parties') successfully negotiated a Binding Arbitration Framework (BAF), an agreement that governs the process for Physician Services Agreement (PSA) negotiations, mediation, and arbitration.
On February 10, 2022, the parties agreed to a memorandum of settlement for a new PSA, which was subsequently ratified by the OMA membership on March 28, 2022. As outlined in the BAF, the parties initiated negotiations in October 2023 to determine physician compensation for the next PSA (2024-2028).
While the parties made good faith efforts to negotiate a price increase for 2024-2025, they mutually agreed to call upon the services of a Board of Arbitration chaired by arbitrator Mr. William Kaplan to resolve their impasse. The Arbitration Board deliberated and ultimately awarded a 9.95 per cent increase for physician services in 2024-2025.
5.3 Payments to hospitals
Ontario hospitals are funded through a combination of global funding, volume-based funding, and Patient-Based Funding—which provides funding on a spectrum between activity-based, and performance-based approaches.
Since April 1, 2012, Ontario shifted hospital funding from a predominantly global budget system towards a patient-based funding (PBF) system. PBF ensures that patients get the right care, at the right place, at the right time, and at the right price. PBF offers an integrated approach to health system funding and puts the patient at the centre through adopting a 'funding follows the patient' principle.
For purposes of funding, publicly funded hospitals are classified based on whether they receive funding through the Growth and Efficiency Model (GEM) or not. In addition, GEM hospitals are further classified based on whether they provide specialized care (e.g., teaching, pediatric) or by their size (e.g. large, medium).
Stand-alone psychiatric and small-sized hospitals do not receive GEM funding. Instead, they rely primarily on global budgets for their operational funding.
Hospital funding sources
Global funding: Non-targeted base funding that is carried over year-to-year. This funding is not tied to the delivery of specific procedures.
Growth and Efficiency Model (GEM) (Formerly Health-Based Allocation Model [HBAM]): HBAM was an evidence-based funding formula that used clinical and financial information to redistribute about $5.135 billion annually among all modeled hospitals, based on the number of patients treated and the complexity of their care. The model also took into account the efficiency of hospitals.
In 2019-2020, the redistribution of HBAM was suspended, pending development of a long-term plan that considers a consolidated approach to address growth in services, which resulted in the introduction of the Growth and Efficiency Model (GEM). GEM is used to allocate incremental growth funding, rather than re-distributing existing funds. This increases the total GEM funding envelope on an annual basis.
Quality Based Procedures (QBP): QBP are episodes of care (e.g., hip/knee replacement surgery, stroke) for which evidence-based best practices have been defined and providers are compensated for providing the services included in the episode based on an established price.
Funding is allocated by assigning a number of cases (volumes) and a provincial price that is specific to identified surgical or medical procedures. The provincial price is adjusted to reflect patient cohort differences at each hospital using a measure of acuity, known as the Case Mix Index (CMI).
The MOH does not place a limit on the number of QBP services that can be provided. QBP volumes are targets based on historical activity and population growth needs. In this patient-based funding model, there is considerable flexibility for hospitals to perform additional (or fewer) volumes, in accordance with QBP volume management policies.
Bundled Care: Like QBP, Bundled Care funding is allocated by an assigned number of cases and a price. However, a Bundled QBP encompasses services that cross providers, specifically including hospital and post-acute community care like home and community care. Bundled QBP provide a single payment for an episode of care across multiple settings and providers, like hip/knee replacement surgery and post-surgical rehabilitation.
Funding is allocated to a Bundle Holder (a health service provider) who is responsible for partnering with and transferring funds to other service providers for surgical care and/or post- acute rehabilitation, providing a more integrated service from the time patients enter hospital for surgery to their recovery at home and in the community. Bundle Holders must ensure that patients are receiving the full scope of care in an integrated pathway, regardless of where the patient lives.
Bundled care is being implemented for hip and knee replacement and shoulder surgery and chronic kidney disease, and is being tested in other clinical areas.
Priority Programs and Services: Funding for life-saving and life-enhancing procedures and specialized services (i.e., cardiovascular, neurosurgery, bariatric, critical care) as well as maternal/newborn health programs.
Funding rates are pre-set, and volume amounts are determined using a number of data points, including historical utilization information, changes in the population of interest for the catchment area, and direct discussions with the hospitals and Ontario Health at the regional level, regarding their respective projections.
Post Construction Operating Plan (PCOP): PCOP funding provides operating funds to hospitals for clinical service and space expansions incurred after the completion of an approved capital project.
PCOP funding may be provided for service volume increases, one-time start up and transition costs, equipment amortization and/or incremental facility costs.
Wait Times: Allocated to support additional diagnostic imaging (e.g., Magnetic Resonance Imaging [MRI] and Computerized Tomography [CT] Hours) and select surgical procedures (price per procedure). Funding allocation is determined based on prior year performance, current capacity and wait lists and in-year reallocations.
Pay for Results (P4R): Provides annual one-time performance-related funding incentives to hospitals to enhance services for all patients seeking emergency department (ED) care. Through this funding, EDs will have the financial means to undertake initiatives specific to their site's needs that will improve their ability to remain open and continue to deliver faster emergency care to the communities they serve.
6.0 Recognition given to federal transfers
The Government of Ontario publicly acknowledged the federal contributions provided through the Canada Health Transfer in its Public Accounts of Ontario 2023-2024.
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 1. Number as of March 31stFootnote 1 | 14,295,514 | 14,525,378 | 14,646,581 | 14,946,151 | 14,901,258 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| Public facilities | |||||
| 2. NumberFootnote 2 | 140 | 141 | 140 | 140 | 140 |
| 3. Payments for insured health services ($)Footnote 3 | 18,400,652,198 | 24,321,059,400 | 23,046,801,683 | 22,707,926,948 | 25,665,132,607 |
| Private for-profit facilities | |||||
| 4. Number of private for-profit facilities providing insured health servicesFootnote 4 | not available | not available | not available | not available | not available |
| 5. Payments to private for-profit facilities for insured health services ($)Footnote 4 | not available | not available | not available | not available | not available |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 6. Total number of claims, in-patient | 5,809 | 4,323 | 5,081 | 5,759 | 5,779 |
| 7. Total payments, in-patient ($) | 54,158,972 | 43,726,985 | 55,073,029 | 65,605,485 | 84,897,394 |
| 8. Total number of claims, out-patient | 119,206 | 104,232 | 134,342 | 124,807 | 119,387 |
| 9. Total payments, out-patient ($) | 45,498,572 | 37,812,107 | 43,000,540 | 44,783,667 | 47,789,190 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| Pre-approved | |||||
| 10. Total number of claims, pre-approved in-patientFootnote 6 | 800 | 435 | 461 | 514 | 623 |
| 11. Total payments, pre-approved in-patient ($)Footnote 6 | 76,038,140 | 32,377,325 | 22,123,444 | 27,072,095 | 37,517,320 |
| 12. Total number of claims, pre-approved out-patient (#) | not applicable | not applicable | not applicable | not applicable | not applicable |
| 13. Total payments, pre-approved out-patient ($) | not applicable | not applicable | not applicable | not applicable | not applicable |
| Non pre-approved | |||||
| 14. Total number of claims, non pre-approved in-patientFootnote 6 | 4,419 | 1,248 | 1,547 | 1,799 | 2,868 |
| 15. Total payments, non pre-approved in-patient ($)Footnote 6 | 3,986,091 | 1,288,096 | 1,559,798 | 1,905,106 | 2,799,190 |
| 16. Total number of claims, non pre-approved out-patientFootnote 6 | 13,891 | 3,453 | 3,571 | 3,279 | 6,097 |
| 17. Total payments, non pre-approved out-patient ($)Footnote 6 | 1,385,304 | 270,470 | 192,141 | 183,162 | 324,021 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 18. Number of participating physicians | 33,245 | 33,562 | 34,798 | 35,340 | 36,224 |
| 19. Number of opted-out physicians | 15 | 14 | 14 | 12 | 11 |
| 20.
Number of non-participating physiciansFootnote 7 |
0 | 0 | 0 | 0 | 0 |
| 21. Total payments for services provided by physicians paid through all payment methods ($)Footnote 8 | 13,910,893,530 | 13,300,206,910 | 14,766,370,330 | 15,631,036,132 | 16,741,513,276 |
| 22. Total payments for services provided by physicians paid through fee-for-service ($) | 9,013,952,400 | 8,375,400,748 | 9,569,959,838 | 10,351,717,146 | 11,012,153,558 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 23. Number of services | 506,698 | 426,823 | 522,370 | 575,212 | 582,740 |
| 24. Total payments ($) | 28,626,840 | 23,229,219 | 28,108,868 | 32,443,283 | 32,763,645 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| Pre-approved | |||||
| 25. Number of pre-approved services | not applicable | not applicable | not applicable | not applicable | not applicable |
| 26. Total pre-approved payments ($) | not applicable | not applicable | not applicable | not applicable | not applicable |
| Non pre-approved | |||||
| 27. Number of non pre-approved servicesFootnote 9 | 79,937 | 20,803 | 35,108 | 23,164 | 33,961 |
| 28. Total non pre-approved payments ($)Footnote 9 | 2,771,990 | 807,589 | 2,774,569 | 1,040,039 | 1,334,441 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 29. Number of participating dentists | 276 | 256 | 253 | 249 | 231 |
| 30. Number of opted-out dentists | not applicable | not applicable | not applicable | not applicable | not applicable |
| 31. Number of non-participating dentists | not applicable | not applicable | not applicable | not applicable | not applicable |
| 32. Number of services provided | 101,668 | 72,476 | 82,795 | 91,879 | 93,405 |
| 33. Total payments ($) | 12,527,790 | 8,337,866 | 9,245,799 | 11,089,599 | 11,101,881 |
|
|||||
Manitoba
Manitoba Health, Seniors and Long-Term Care provides leadership and support to protect, promote, and preserve the health of all Manitobans. Manitoba Health continues efforts to improve access, service delivery, capacity, innovation, sustainability, and improve the health status of Manitobans while reducing health disparities. The roles and responsibilities of the department include policy, program, and standards development; fiscal and program accountability; and evaluation. In addition, some direct services continue to be provided through public health inspections and provincial nursing stations.
1.0 Public administration
1.1 Health care insurance plan and public authority
The Manitoba Health Services Insurance Plan (MHSIP) is administered by Manitoba Health, Seniors, and Long-Term Care (MHSLTC) under The Health Services Insurance Act, C.C.S.M c. H35 (the Act).
The MHSIP is administered to provide insurance for residents of the province in respect of the costs of hospital services, medical services and other health services referred to, or shortly described, in Acts of the Legislature or regulations made thereunder.
The Minister of MHSLTC (the Minister) is responsible for the administration and operation of the MHSIP.
The Minister may enter into contracts and agreements with any person or group that the Minister considers necessary for the purposes of the Act.
The Minister may also make grants to any person or group for the purposes of the Act on such terms and conditions as the minister considers advisable.
The Minister may, in writing, delegate to any person any power, authority, duty or function conferred or imposed upon the Minister under the Act or under the Regulations.
There was one legislative amendment to the Act made in the 2023-2024 fiscal year. Once the amendment is proclaimed into force, personal care home operators will be obliged to provide support for the family councils established by family members of personal care home residents.
In the 2023-2024 fiscal year, the Prosthetic, Orthotic and other Medical Devices Insurance Regulation (M.R. 53/93) made under the Act was amended to provide coverage for insulin pumps, of a type approved by the Minister, for all eligible individuals, who are 18 or older, who have been diagnosed with Type 1 diabetes. The amendment also enabled physicians who are not endocrinologists to request coverage of a pump for patients they are providing care to in relation to the management of their diabetes.
1.2 Reporting requirement
Section 6 of the Act requires the Minister to have audited financial statements of the MHSIP showing separately the expenditures for hospital services, medical services, and other health services. The Minister is required to prepare an annual report, which must include the audited financial statements, and to table the copy of the annual report before the Legislative Assembly within 15 days of receiving it, if the Assembly is in session. If the Assembly is not in session, the report must be tabled within 15 days of the beginning of the next session.
1.3 Audit of accounts
Section 7 of the Act requires that the Office of the Auditor General of Manitoba (or another auditor designated by the Office of the Auditor General of Manitoba) audit the accounts of the MHSIP annually and prepare a report on that audit for the Minister. The most recent audit reported to the Minister and available to the public is for the 2022-2023 fiscal year and is contained in p. 135-137 in the Manitoba Annual Report and Public Accounts, 2023.
2.0 Comprehensiveness
2.1 Insured hospital services
Sections 46 and 47 of the Health Services Insurance Act, as well as the Hospital Services Insurance and Administration Regulation (M.R. 48/93), provide for insured hospital services.
There were no amendments to sections 46 and 47 of the Health Services Insurance Act, C.C.S.M c. H35, or the Hospital Services Insurance and Administration Regulation in 2023-2024.
As of March 31, 2023-2024, there were 96 facilities providing insured hospital services to both in-and out-patients. Hospitals are designated by the Hospitals Designation Regulation (M.R. 47/93) under the Health Services Insurance Act.
Services specified by the Hospital Services Insurance and Administration Regulation (M.R. 48/93) as insured in-patient and out-patient hospital services include:
- accommodation and meals at the standard ward level;
- necessary nursing services;
- laboratory, radiological and other diagnostic procedures;
- drugs, biologics and related preparations;
- routine medical and surgical supplies;
- use of operating room, case room, and anaesthetic facilities; and
- use of radiotherapy, physiotherapy, occupational and speech therapy facilities where available.
The Hospital Services Insurance and Administration Regulation (M.R. 48/93) states that hospital in-patient services include routine medical and surgical supplies, thereby ensuring reasonable access for all residents. The regional health authorities and Manitoba Health, Seniors and Long-Term Care (MHSLTC) monitor compliance.
No additional services were added to the list of insured hospital services in 2023-2024.
MHSLTC for the period of 2023-2024, had no formal evidence, investigations, or actions against any diagnostic clinics where there was an assertion of inappropriate charging of patients for services that would be considered insured if provided in a hospital. MHSLTC does not have any recent or upcoming legislative or regulatory changes in this regard.
Manitoba residents maintain high expectations for quality health care and insist that the best available medical knowledge and service be applied to their personal health situations.
2.2 Insured physician services
The enabling legislation that provides for insured physician services is the Medical Services Insurance Regulation (M.R. 49/93) made under the Health Services Insurance Act (C.C.S.M c. H35).
Physicians providing insured services in Manitoba must be lawfully entitled to practice medicine in Manitoba and be registered and licensed under The Medical Act, R.S.M 1987, c. M90.
As of April 30, 2024, there were 3,334Footnote viii physicians registered in Manitoba, with 3,071 participating in the Manitoba Health Services Insurance Plan.
A physician, by giving notice to the Minister of MHSLTC in writing, may elect to collect the fees other than from the Minister for medical services rendered to insured persons, in accordance with section 91 of The Health Services Insurance Act (C.C.S.M c. H35) and section 5 of the Medical Services Insurance Regulation (M.R. 49/93). The election to opt out of the health care insurance plan takes effect on the first day of the month following a 90-day period from the date the Minister receives the notice.
Before rendering a medical service to an insured person, physicians must give the patient reasonable notice that they propose to collect any fee for the medical service from them or any other person except the Minister. The physician is responsible for submitting a claim to the Minister on the patient's behalf and cannot collect fees more than the benefits payable for the service under the Act or Regulations. No physicians opted-out of the medical plan in 2023-2024.
The range of physician services insured by MHSLTC is listed in the Payments for Insured Medical Services Regulation (M.R. 73/2003), under The Health Services Insurance Act (C.C.S.M c. H35). Coverage is provided for all medically required personal health care services that are not excluded under the Excluded Services Regulation (M.R. 46/93) of The Health Services Insurance Act (C.C.S.M c. H35), rendered to an insured person by a physician.
During fiscal year 2023-2024, several new insured services were added to a revised fee schedule. The Physician's Manual can be found on the MHSLTC website.
The process for a medical service to be added to the list of those covered by MHSLTC is that physicians must put forward a proposal to their specific section of Doctors Manitoba. Doctors Manitoba will negotiate the item, including the fee, with MHSLTC, who may also initiate this process, and may include stakeholder and public consultation.
2.3 Insured surgical-dental services
Insured surgical and dental services are listed in the Hospital Services Insurance and Administration Regulation (M.R. 48/93) under the Health Services Insurance Act (C.C.S.M c. H35). Surgical services are insured when performed by a certified oral and maxillofacial surgeon or a licensed dentist in a hospital, when hospitalization is required for the proper performance of the procedure. This Regulation also provides benefits relating to the cost of insured orthodontic services in cases of cleft lip and/or palate for persons registered under the program by their 18th birthday, when provided by a registered orthodontist.
Providers of dental services, by giving to the Minister at any time notice in writing, may elect to collect their fees directly from the patient in the same manner as physicians in accordance with section 91(1) of the Health Services Insurance Act (C.C.S.M c. H35) and may not charge to, or collect from, an insured person a fee more than the benefits payable under the Act or Regulations. No providers of dental services opted-out in 2023-2024.
For a dental service to be added to the list of insured services, a dentist must put forward a proposal to the Manitoba Dental Association (MDA) for discussion with MHSLTC, which may include stakeholder and public consultation. The MDA negotiates the item and fee with MHSLTC.
2.4 Uninsured hospital, physician and surgical-dental services
The Excluded Services Regulation (M.R. 46/93) made under the Health Services Insurance Act (C.C.S.M c. H35) sets out those services that are not insured. These include:
- examinations and reports for reasons of employment, insurance, attendance at university or camp, or performed at the request of third parties;
- group immunization or other group services except where authorized by MHSLTC;
- services provided by a physician, dentist, chiropractor, or optometrist to him or herself or any dependents;
- preparation of records, reports, certificates, communications and testimony in court;
- mileage or travelling time;
- services provided by psychologists, chiropodists, and other practitioners not provided for in the legislation;
- tattoo removal;
- contact lens fitting;
- reversal of sterilization procedures; and
- psychoanalysis.
The Hospital Services Insurance and Administration Regulation (M.R. 48/93) states that hospital in-patient services includes routine medical and surgical supplies, thereby ensuring reasonable access for all residents. The regional health authorities and MHSLTC monitor compliance.
Third parties such as private insurers or the Workers Compensation Board do not receive priority access to services through additional payment. Manitoba has no formalized process to monitor compliance; however, feedback from physicians, hospital administrators, medical professionals and staff allows regional health authorities and MHSLTC to monitor usage and service concerns.
To de-insure services covered by MHSLTC, the Ministry prepares a submission for approval by Cabinet. The need for public consultation is determined on an individual basis depending on the subject. No services were removed from the list of those insured by MHSLTC in 2023-2024.
3.0 Universality
3.1 Eligibility
The Health Services Insurance Act, C.C.S.M c. H35 (the Act), defines the eligibility of Manitoba residents for coverage under the provincial health care insurance plan.
Subsection 2(1) of the Act states that a resident is a person who is legally entitled to be in Canada, makes his or her home in Manitoba, is physically present in Manitoba for at least six months in a calendar year, and includes any other person classified as a resident in the Regulations, but does not include a person who holds a temporary resident permit under the Immigration and Refugee Protection Act (Canada), unless the Minister of Health (the Minister) determines otherwise, or is a visitor, transient or tourist.
The Residency and Registration Regulation (M.R. 54/93), made under the Act, extends the definition of residency. The extensions are found in subsections 7(1) and 8(1). Section 7(1) allows missionaries, individuals with out-of-country employment and individuals undertaking sabbatical leave to be outside Manitoba for up to two years while still remaining residents of Manitoba. Students are deemed to be Manitoba residents while in full-time attendance at an accredited educational institution. Section 8(1) extends residency to individuals who are legally entitled to work in Manitoba and have a work permit of 12 months or more under the Immigration and Refugee Protection Act (Canada). Additionally, section 8.1.1 of the Residency and Registration Regulation (M.R. 54/93) extends deemed residency to temporary foreign workers (and their dependents) in the province to provide agricultural services based on a work permit, regardless of the duration of their work permit.
No amendments were made to the Residency and Registration Regulation (M.R. 54/93) in 2023-2024.
The Residency and Registration Regulation (M.R. 54/93), section 6, defines Manitoba's waiting period as follows:
"A resident who was a resident of another Canadian province or territory immediately before his or her arrival in Manitoba is not entitled to benefits until the first day of the third month following the month of arrival."
Section 6 of the Residency and Registration Regulation (M.R. 54/93) stipulates that there is no waiting period for dependents of members of the Canadian Armed Forces. There are currently no other waiting periods in Manitoba.
The Manitoba Health Services Insurance Plan (MHSIP) excludes residents covered under any federal plan, including the following federal statutes:
- Aeronautics Act;
- Civilian War-related Benefits Act;
- Government Employees Compensation Act;
- Merchant Seaman Compensation Act;
- National Defence Act;
- Pension Act;
- Veteran's Rehabilitation Act; and
- Federal inmates or those covered under legislation of any other jurisdiction (Excluded Services Regulations subsection 2[2]).
These residents become eligible for health services insurance coverage upon discharge from the Canadian Forces, or in the case of an inmate of a penitentiary, upon discharge if the inmate has no resident dependents. Upon change of status, these persons have one month to register with Manitoba Health, Seniors and Long-Term Care (MHSLTC), as per subsection 2(3) of the Residency and Registration Regulation (M.R. 54/93).
RCMP members are insured persons in Manitoba and are eligible for benefits under the MHSIP.
The process of issuing health insurance cards requires that individuals inform and provide documentation to MHSLTC that they are legally entitled to be in Canada, and that they intend to be physically present in Manitoba for six months in a calendar year. They must also provide a primary residence address in Manitoba. Upon receiving this information, MHSLTC will provide a registration card for the individual and all qualifying dependents.
Manitoba has two health-related numbers: a six-digit alphanumeric registration number assigned to an individual 18 years of age or older who is not classified as a dependent, and the nine-digit Personal Health Information Number (PHIN). The six-digit registration number may be shared by all members of a family including a spouse and dependents, whereas the nine-digit PHIN is used for payment of all medical service claims and hospital services.
As of March 31, 2024, there were 1,450,478 residents registered with the MHSIP, demonstrating an increase of 39,792 new registrations since 2022-2023.
Individuals may appeal decisions of MHSLTC with respect to eligibility before the Manitoba Health Appeal Board, an independent quasi-judicial tribunal established pursuant to the Health Services Insurance Act (C.C.S.M c. H35).
There is no provision for a resident to opt out of the MHSIP.
3.2 Other categories of individuals
Subsection 8(1) of the Residency and Registration Regulation (M.R. 54/93) requires that temporary workers possess a work permit issued by Immigration, Refugees and Citizenship Canada for at least 12 consecutive months, be physically present in Manitoba for six months in a calendar year and be legally entitled to be in Canada before receiving MHSIP coverage.
Subsection 8.1.1 of the Residency and Registration Regulation (M.R. 54/93) extends deemed residency to temporary foreign workers (and their dependents) in the province to provide agricultural services based on a work permit, regardless of the duration of their work permit.
As of March 31, 2024, there were 58,688 work permit holders registered with the MHSIP.
4.0 Portability
4.1 Minimum waiting period
Section 6 of the Residency and Registration Regulation (M.R. 54/93) identifies the waiting period for insured persons from another province or territory. A resident who lived in another Canadian province or territory immediately before arriving in Manitoba is entitled to benefits on the first day of the third month following the month of arrival.
4.2 Coverage during temporary absences in Canada
Subsection 7(1) of the Residency and Registration Regulation (M.R. 54/93) defines the rules for portability of health insurance during temporary absences in Canada.
Students are considered residents and will continue to receive health coverage for the duration of their fulltime enrollment at any accredited educational institution. The additional requirement is that they intend to return and reside in Manitoba after completing their studies.
Manitoba has formal agreements with all Canadian provinces and territories (excluding Quebec) for the reciprocal billing of insured hospital services, made under the Interprovincial Health Insurance Agreements Coordinating Committee (IHIACC).
In-patient costs are paid at standard rates approved by the host province or territory. Payments for in-patient, high-cost procedures, and out-patient services are based on national rates agreed to by provincial and territorial health plans. These include all medically necessary services as well as costs for emergency care.
Except for Quebec, medical physician services incurred in all provinces or territories are paid through a reciprocal billing agreement at host province or territory rates. Claims for physician medical services received in Quebec are submitted by the patient or physician to MHSLTC for payment at host province rates.
4.3 Coverage during temporary absences outside Canada
Subsection 7(1) of the Residency and Registration Regulation (M.R. 54/93) defines the rules for portability of health insurance during temporary absences outside of Canada.
Subsection 7(1)(g) of the Residency and Registration Regulation (M.R. 54/93) extends the period during which a person may be temporarily absent from Manitoba for the purpose of residing outside of Canada from six months to a maximum of seven months in a 12-month period.
Residents on full-time employment contracts outside Canada will receive health services insurance coverage for up to 24 consecutive months. Individuals must return and reside in Manitoba after completing their employment terms. Individuals serving as humanitarian aid workers or missionaries on behalf of a religious organization approved as a registered charity under the Income Tax Act (Canada) will be covered by Manitoba Health, Seniors, and Long-Term Care (MHSLTC) for up to 24 consecutive months. Students are considered residents and will continue to receive health coverage for the duration of their full-time enrollment at an accredited educational institution. The additional requirement is that they intend to return and reside in Manitoba after completing their studies. Residents on sabbatical or educational leave from employment will be covered by MHSLTC for up to 24 consecutive months. These individuals also must return and reside in Manitoba after completing their leave.
Manitoba residents receiving coverage under the provincial health insurance plan who receive medical and hospital services outside of Canada are eligible to be reimbursed at the rates set out in the Medical Services Insurance Regulation (M.R. 49/93) and the Hospital Services Insurance and Administration Regulation (M.R. 48/93), made under the Health Services Insurance Act (C.C.S.M c. H35). Emergency doctors' services outside of Canada are reimbursed at a rate equal to what a Manitoba doctor would receive for a similar service. Emergency hospital care is paid on an average daily rate established by MHSLTC.
4.4 Prior approval requirement
Prior approval is not required for procedures that are covered under the interprovincial reciprocal agreements with other provinces. Prior approval by MHSLTC is required for high-cost items or procedures that are not included in the reciprocal agreements.
To be eligible for reimbursement, all non-emergency hospital and medical care provided outside Canada requires prior approval from MHSLTC. Manitobans requiring medically necessary medical and/or hospital services unavailable in Manitoba or elsewhere in Canada may be eligible for reimbursement of costs incurred outside of Canada, pursuant to the Medical Services Insurance Regulation (M.R. 49/93), by providing MHSLTC with a recommendation from a specialist stating that the patient requires a specific, medically necessary service.
Individuals may appeal decisions of MHSLTC with entitlement to medical benefits before the Manitoba Health Appeal Board, an independent quasi-judicial tribunal established pursuant to the Health Services Insurance Act (C.C.S.M c. H35).
5.0 Accessibility
5.1 Access to insured health services
Manitoba Health, Seniors, and Long-Term Care (MHSLTC) ensures that medical services are equitable and reasonably available to all Manitobans. Effective January 1, 1999, the Surgical Facilities Regulation (M.R. 222/98) under the Health Services Insurance Act came into force to prevent private surgical facilities from charging additional fees for insured medical services.
The Health Services Insurance Act and the Private Hospitals Act include definitions and other provisions to ensure:
- that no charges can be made to individuals who receive insured surgical services, or to anyone else on that person's behalf; and
- that a surgical facility cannot perform procedures requiring overnight stays and thereby function as a private hospital.
The Accessibility for Manitobans Act includes definitions and principles to ensure accessibility by preventing and removing barriers that disable people with respect to receiving health care services including:
- accommodation;
- the built environment, including facilities, building, structures and premises;
- the delivery and receipt of goods, services and information; and
- a prescribed activity or undertaking.
If a Manitoba resident feels that they have been inappropriately charged for a service that is insured under the provincial health insurance plan (i.e., a potential incidence of extra-billing or a user charge), the resident is encouraged to contact Manitoba to report this occurrence at the following:
Manitoba Health, Seniors, and Long-Term Care
Executive Director – Insured Benefits Branch
300 Carlton Street
Winnipeg, MB R3B 3M9
1-800-392-1207
Inquiries are made by the Insured Benefits Branch of MHSLTC into the specifics of the fee(s) charged to assess whether the service provided was an insured service, and any required further action. Generally, contact from MHSLTC to the medical service provider, advising that the provider must reimburse the patient and submit a claim to MHSLTC, is sufficient to address the concern. Further incidents on the part of the same service provider may result in an investigation by MHSLTC Audit and Investigation Unit. Concerns regarding the professional conduct of medical service providers are referred to the appropriate regulatory agency.
MHSLTC remains committed to the principles of Medicare and improving the health status of all Manitobans. In 2023-2024, Manitoba continued to support these commitments through several activities including the following:
Priority Areas for Improvement
Manitoba's health system aims to create a coordinated, provincial approach to health services. This involves aligning regional service delivery organizations to plan and deliver clinical services in an integrated manner to support the province's population.
The provincial health authority (Shared Health) works with all health regions, partners, and local communities to develop and implement a provincial clinical plan that guides improvements to access, quality and patient outcomes for all Manitobans.
The departmental strategic objectives reflect the government priorities listed in the department mandate letters. The re-introduction of mandate letters represents a renewed approach designed to align departmental efforts more closely with government direction.
A plan to address the priority areas has been developed and is guided by the quintuple aims of health care improvement. These aims are closely aligned with government's priorities to reduce emergency department wait times, promote fiscal responsibility, and advance health equity. Together, the quintuple aims and government priorities act as the foundation that have informed the government's six-point action plan, which provides a framework for how improvements are addressed across the health system.
The six-point action plan focuses on addressing the following priority areas to strengthen public health care:
- Access to Services including Primary, Community and Long-term Care and Seniors Care: Building service capacity in the system to improve patient access, wait times and system navigation across the care continuum, in addition to the establishment of an independent senior's advocate to represent seniors' rights and interests.
- Emergency Department Wait Times: Investing in increased care capacity across the acute care system by adding beds to improve patient flow, as well as implementing best practices for patient triage, discharging, and bed management.
- Health Workforce Culture, Retention, Recruitment and Training: Committing to hiring 1000 net new health care workers in fiscal year 2024/2025 (for which over 1,255 net new health care workers have already been hired across the province), addressing vacancies (especially in rural and remote areas), driving recruitment by removing barriers and offering greater incentives, expanding training opportunities and introducing innovative ways of enhancing care.
- Indigenous Health Services: Committing to focused actions, resources, and partnerships with Indigenous communities, including the implementation of the Indigenous Partnership Framework to guide future health work, combat Indigenous-specific racism and build respectful, trusting relationships with Indigenous Peoples.
- System Level Fiscal Stability and Accountability: Ensuring a culture of accountability and efficient use of resources through accountability agreements, regular performance meetings and enhanced reporting requirements.
- Electronic Patient Records and Health Cards: Modernizing electronic patient medical records, increasing reliable digital connectivity, modernizing the health card and related application process, and promoting the use of virtual health technologies to expand access to care.
Activities to implement this plan are underway in all areas of the department and are being monitored with regular progress tracking. For instance, the Health Care Retention and Recruitment Office was formed in 2024 to address health workforce challenges and opportunities. In 2023-2024, the department also implemented monetary incentives and system-level improvements to encourage retention and recruitment of key professional groups, including nursing, support, allied health, physician assistants/clinical assistants and medical residents and interns.
In addition, the department undertook planning for the creation of three new minor injury and illness clinics to improve access to primary care and providing alternatives for care outside of the emergency departments.
In 2023-2024, plans to expand the provincial pharmacare program were developed, resulting in coverage of pre-exposure prophylaxis and birth control for Manitobans.
By focusing on these priorities, government sought to positively impact patient outcomes and experiences, add value to services and ensure system cohesion and accountability.
Facilities
For the 2023-2024 fiscal year, MHSLTC provided strategic guidance, and oversight for capital investment in health care facilities to support the delivery of health care programs in the province. These include investments in new and renovated buildings, facility repairs and upgrades, new or upgraded medical equipment and Information and Communications Technology (ICT).
MHSLTC developed a multi-year capital plan that supports provincial population health objectives, sustainability, and flexibility to adapt to the changing needs of the population and innovative service delivery models. This included analysis and prioritization for capital projects within a fiscally sustainable funding allocation. New capital projects were submitted by Service Delivery Organizations (SDOs) and Regional Health Authorities (RHAs) and carefully reviewed by the provincial health authority, with consideration of funding to current projects in design or construction stages. The scope, timelines and funding limits of the capital plan are defined and implemented in accordance with government mandates and strategic objectives.
Overall, there were approximately 450 capital projects for repair or upgrades to facilities, medical equipment, and ICT infrastructure. For the 2023-2024 fiscal year, total spending for these projects was valued at approximately $616 million.
MHSLTC, provided to government information on the capital plan including forecasting of maintenance requirements, emerging program standards, capital financing, development of appropriate programming, and policy options.
MHSLTC applied policies related to procurement practices, capital planning, funding, and community cost-sharing. Oversight and guidance were provided to ensure that expectations and requirements were known to and complied with by the RHAs and SDOs.
MHSLTC provided funds for upgrades and functional changes to existing facilities in a timely, prioritized sequence. MHSLTC also continued to oversee the annual allocations for safety and security program, medical equipment and ICT renewal which focuses on the execution of a risk-based approach to replacing and upgrading old, obsolete, and failing technical infrastructure. This included the review of the prioritized list of potential projects, monitoring of the projects to completion and review of the expenditures against the approved funding.
Health Professionals
In 2023-2024, the province funded the following complement of medical and nursing professionals registered to practice in Manitoba:
- 3,334 Physicians;
- 260 Physician and Clinical Assistants;
- 338 Nurse Practitioners;
- 13,890 Registered Nurses;
- 1,189 Registered Psychiatric Nurses; and
- 3,949 Licensed Practical Nurses.
The transition to the Regulated Health Professions Act (RHPA), S.M. 2009 c. 15, continues to be a significant undertaking for the province. In January 2014, the RHPA took effect, establishing uniform and consistent regulations for all regulated health professions, with a heightened emphasis on patient safety and accountability. Based on their competence and training, the legislation authorizes regulated health professionals to perform a list of activities and procedures known as reserved acts when providing health care. The RHPA sets out consistent rules and processes for governance, registration, complaints, and discipline, as well as regulation and bylaw-making authority.
Professions that are not currently regulated but wish to become regulated under the RHPA must file an application. To transition from a profession to the RHPA, two regulations are required:
- A practice regulation made by the Lieutenant Governor in Counsel (LGIC) that transitions an existing college and its members under the RHPA or, in the case of a new college, establishes the new college and sets out the reserved acts that members of the profession are authorized to perform.
- A General Regulation made by the governing council of the health profession regulatory college and approved by the LGIC, which sets out the registration requirements, requirements to obtain/renew a certificate of practice, terms and conditions on the performance of reserved acts, continuing competency requirements, standards of practice, member public profile requirements (if a college is required to have public profiles of its members), and requirements re: health profession corporations.
To date, the following five health professions transitioned to regulation under the RHPA.
- Audiologists and Speech Language Pathologists (2013)
- Registered Nurses (2017)
- Physicians, Physician Assistants and Clinical Assistants (2018)
- Paramedics (2020)
- Registered Psychiatric Nurses (2022)
The transition of other health professions to the RHPA will continue to be a focus for the province, as it will have a significant long-term impact on the provincial health workforce.
In 2023-2024, the province provided funding to increase the number of medical and nursing professionals registered in Manitoba as follows:
- Physicians increased by 133 (from 3,201 to 3,334);
- Nurse Practitioners increased by 25 (from 313 to 338);
- Registered Nurses increased by 430Footnote 1 (from 13,460 to 13,890);
- Registered Psychiatric Nurses increased by 19 (from 1,170 to 1,189);
- Licensed Practical Nurses increased by 62 (from 3,887 to 3,949); and
- Physician and Clinical Assistants remained the same at
5.2 Physician compensation
Manitoba continues to employ the following methods of payment for physicians:
- fee-for-service;
- contract;
- blended; and
- sessional.
The Health Services Insurance Act governs remuneration to physicians for insured services. There were no amendments to the Health Services Insurance Act related to physician compensation during the 2023-2024 fiscal year.
Fee-for-service remains the primary method of payment for physician services. Alternate payment arrangements constitute a significant portion of the total compensation to physicians in Manitoba. Alternate-funded physicians are those who receive non-fee-for-service compensation, including through a salary (employment relationship) or those who work on an independent contract basis. Manitoba also uses blended payment methods where appropriate. As well, physicians may receive sessional payments for providing medical services on a time-based arrangement, as well as stipends for on-call and other responsibilities.
Physicians are typically represented by Doctors Manitoba with some exceptions, such as oncologists engaged by CancerCare Manitoba. The most recent Physician Services Agreement (PSA) negotiated with Doctors Manitoba and ratified by physicians August 2023 and took effect retroactively on April 1, 2023. The PSA includes $268 million in increased funding for physician services over its four-year term. Key highlights of the new PSA include the following:
- increased funding for specialty and hospital services to attract more physician coverage for inpatient and emergency department care, and more resources to address surgical and diagnostic backlogs.
- A new funding model for longitudinal family medicine branded as Family Medicine Plus that blend existing volume-based payments with funding for patient panels and time-based stipends. This blended model will offer more predictable funding to stabilize family medicine clinic operations, which will connect more Manitobans with a family doctor. For patients, it will mean more time with their doctor for complicated medical concerns.
- new rural and northern retention and recruitment incentives and additional funding to help stabilize physician coverage in rural hospitals and remote First Nations communities.
- Creation of new extended hour clinics and Minor Injury and Illness clinics to give people more options for care outside of traditional hours.
- permanent funding model for virtual visits, ensuring Manitobans will continue to be able to receive appropriate care by phone or video, if they wish.
The Manitoba Physician's Manual lists all the fee tariff descriptions, rates, rules of application and the dispute resolution process in relation to fee-for-service payments to physicians. This document is the Schedule of Benefits payable to physicians on behalf of insured persons in Manitoba pursuant to the Medical Services Insurance Regulation (M.R. 49/93) under the Health Services Insurance Act (C.C.S.M c. H35).
All fee-for-service claims must be submitted electronically. The submission of paper claims is permitted on a limited basis and only with the prior approval of MHSLTC. Fee-for-service claims must be received within six months of the date upon which the physician rendered the service.
5.3 Payments to hospitals
Division 3.1 of Part 4 of the Health System Governance and Accountability Act (C.C.S.M c. H26.5) sets out the requirements for operating agreements between regional health authorities and the operators of hospitals and personal care homes, defined as "health corporations" under the Act.
Pursuant to the provisions of division 3.1, regional health authorities are prohibited from providing funding to a health corporation for operational purposes unless the parties have entered into a written agreement for this purpose that:
- enables the health services to be provided by the health corporation;
- enables the funding to be provided by the regional health authority for the health services;
- sets out the terms of the agreement; and
- includes a dispute resolution process and remedies for breaches.
If the parties cannot reach an agreement, the Minister of Health, Seniors, and Long-Term Care (MHSLTC) is empowered to resolve the matter or matters in dispute. The Minister's resolution is binding on the parties.
There are three regional health authorities which have hospitals operated by health corporations in their health regions. The regional health authorities have required agreements with health corporations that enable the regional health authority to determine funding based on objective evidence, best practices and criteria that are commonly applied to comparable facilities. In all other regions, the hospitals are operated by regional health authorities. The allocation of resources by regional health authorities for providing hospital services is approved by MHSLTC through the approval of annual operating plans, which the regional health authorities are required to submit for approval pursuant to section 24 of the Health System Governance and Accountability Act (C.C.S.M c. H26.5). Section 23 of the Health System Governance and Accountability Act (C.C.S.M c. H26.5) requires that regional health authorities allocate their resources in accordance with the approved annual operating plan.
Pursuant to subsection 50(2.1) of the Health Services Insurance Act (C.C.S.M c. H35), payments from the Manitoba Health Services Insurance Plan for insured hospital services are to be paid to the regional health authorities. In relation to those hospitals that are not owned and operated by a regional health authority, the regional health authority is required to pay each hospital in accordance with any agreement reached between the regional health authority and the hospital operator.
6.0 Recognition given to federal transfers
Manitoba regularly recognizes the federal role regarding the contributions provided under the Canada Health Transfer in public documents. Federal transfers are identified in the Supplement to the Estimates of Expenditures (Manitoba Budget) document and in the Public Accounts of Manitoba. Both documents are published annually by the Manitoba government.
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 1. Number as of March 31st | 1,372,708Footnote 1 | 1,386,938Footnote 1 | 1,399,093 | 1,428,007 | 1,450,478 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| Public facilities | |||||
| 2. Number | 96 | 96 | 96 | 96 | 96 |
| 3. Payments for insured health services ($) | not available | not available | not available | not available | not available |
| Private for-profit facilities | |||||
| 4. Number of private for-profit facilities providing insured health services | 0 | 0 | 0 | 0 | 0 |
| 5. Payments to private for-profit facilities for insured health services ($) | 0 | 0 | 0 | 0 | 0 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 6. Total number of claims, in-patient | 2,502 | 1,922 | 2,035 | 2,595 | 2,792 |
| 7. Total payments, in-patient ($) | 35,646,832 | 26,464,737 | 29,936,426 | 31,518,984 | 47,403,588 |
| 8. Total number of claims, out-patient |
30,616 | 22,008 | 28,499 | 28,044 | 30,191 |
| 9. Total payments, out-patient ($) | 13,949,642 | 8,894,815 | 9,734,282 | 9,172,772 | 11,687,573 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| Pre-approved | |||||
| 10. Total number of claims, pre-approved in-patient | not available | not available | not available | not available | not available |
| 11. Total payments, pre-approved in-patient ($) | not available | not available | not available | not available | not available |
| 12. Total number of claims, pre-approved out-patient | not available | not available | not available | not available | not available |
| 13. Total payments, pre-approved out-patient ($) | not available | not available | not available | not available | not available |
| Non pre-approved | |||||
| 14. Total number of claims, non pre-approved in-patientFootnote 2 | 567 | 315 | 101 | 168 | 292 |
| 15. Total payments, non pre-approved in-patient ($)Footnote 2 | 1,719,770 | 1,995,854 | 531,287 | 398,706 | 731,062 |
| 16. Total number of claims, non pre-approved out-patientFootnote 2 | 7,718 | 3,650 | 2,130 | 2,821 | 4,452 |
| 17. Total payments, non pre-approved out-patient ($)Footnote 2 | 2,876,572 | 2,868,875 | 935,548 | 804,300 | 1,347,868 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 18. Number of participating physicians | 2,829 | 2,856 | 2,898 | 3,058 | 3,071 |
| 19. Number of opted-out physicians | 0 | 0 | 0 | 0 | 0 |
| 20.
Number of non-participating physicians |
not applicable | not applicable | not applicable | not applicable | not applicable |
| 21. Total payments for services provided by physicians paid through all payment methods ($) | 1,393,152,000 | 1,296,902,000 | 1,345,650,000 | 1,393,999,000 | 1,700,405,612 |
| 22. Total payments for services provided by physicians paid through fee-for-service ($) | 931,517,187 | 876,012,714 | 944,198,207 | 944,854,000 | 1,079,094,612 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 23. Number of services | 251,133 | 185,256 | 228,668 | 231,879 | 272,431 |
| 24. Total payments ($) | 13,440,993 | 9,784,063 | 10,884,233 | 12,003,861 | 14,742,635 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| Pre-approved | |||||
| 25. Number of pre-approved services | not available | not available | not available | not available | not available |
| 26. Total pre-approved payments ($) | not available | not available | not available | not available | not available |
| Non pre-approved | |||||
| 27. Number of non pre-approved services | 5,482 | 3,036 | 723 | 1,565 | 2,658 |
| 28. Total non pre-approved payments ($) | 602,938 | 264,565 | 89,165 | 223,734 | 364,008 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 29. Number of participating dentists | 273 | 235 | 273 | 269 | 283 |
| 30. Number of opted-out dentists | 0 | 0 | 0 | 0 | 0 |
| 31.
Number of non-participating dentists |
473 | 585 | 730 | 775 | 826 |
| 32. Number of services provided | 7,098 | 5,449 | 4,876 | 7,724 | 6,520 |
| 33. Total payments ($) | 2,205,750 | 1,410,459 | 1,382,196 | 2,005,387 | 2,137,444 |
|
|||||
Saskatchewan
Saskatchewan's Ministry of Health (the Ministry) is dedicated to achieving a responsive, integrated, and efficient health system for Saskatchewan people with a focus on better health, better care, better value, and better teams as close to home as possible. The Ministry leads provincial health care strategy and supports innovative approaches to meet the needs of patients and families by putting the patient first and promoting healthy choices and responsible self-care.
There was a major focus on restoring volume for surgical and medical procedures and enhancing access to mental health and addictions services, as well as new investments in capital projects across the province. Saskatchewan also continues to take bold actions to advance its ambitious Health Human Resources Action Plan to recruit, train, incentivize and retain health care professionals.
Within Saskatchewan's health system, and services are provided by the Saskatchewan Health Authority, the Saskatchewan Cancer Agency, the Athabasca Health Authority and affiliated health care organizations, which are supported by eHealth Saskatchewan, 3sHealth (Shared Services Saskatchewan), and a diverse group of professionals, many of whom are in private practice. There are 28 self-regulated health professions in the province, overseen by 26 regulatory bodies. An estimated 48,000 people provide a broad range of services across the health system.
The Ministry works with and supports health system leaders and works with local, regional, provincial, national and international organizations to help ensure all Saskatchewan residents have access to safe, high quality health care.
Visit saskatchewan.ca for more information about Ministry programs and services.
1.0 Public administration
1.1 Health care insurance plan and public authority
The provincial government is responsible for funding and ensuring the provision of insured hospital, physician and surgical-dental services in Saskatchewan. Section 6.1 of the Health Administration Act authorizes that the Saskatchewan Minister of Health (the Minister) may:
- pay part of, or the whole of, the cost of providing health services for any persons or classes of person who may be designated by the Lieutenant Governor-in-Council;
- make grants or loans, or provide subsidies to the provincial health authority, health care organizations or municipalities for providing and operating health services or public health services;
- pay part of, or the whole of, the cost of providing health services in Saskatchewan in which those services are considered by the Minister to be required;
- make grants or provide subsidies to any health agency that the Minister considers necessary; and
- make grants or provide subsidies to stimulate and develop public health research, and to conduct surveys and studies in the area of public health.
Sections 8 and 9 of the Saskatchewan Medical Care Insurance Act provide the authority for the Minister to establish and administer a plan of medical care insurance for residents of Saskatchewan. The Provincial Health Authority Act, implemented in 2017, provided the authority to amalgamate the 12 regional health authorities to a single health authority.
Sections 3 and 9 of the Cancer Agency Act provide the authority for establishing a Saskatchewan Cancer Agency (SCA) and for the Agency to coordinate a program for diagnosing, preventing and treating cancer.
The mandates of the Saskatchewan Ministry of Health (the Ministry), provincial health authority, and the Saskatchewan Cancer Agency are outlined in the Health Administration Act, the Provincial Health Authority Act, and the Cancer Agency Act.
1.2 Reporting relationship
The Ministry is directly accountable, and regularly reports, to the Minister on the funding, and administering the funds, for insured physician, surgical-dental, and hospital services.
Section 36 of the Saskatchewan Medical Care Insurance Act requires that the Minister submit an annual report concerning the medical care insurance plan to the Legislative Assembly.
The Provincial Health Authority Act requires that the provincial health authority submit to the Minister in each fiscal year:
- a report on the activities of the provincial health authority; and
- a detailed, audited set of financial statements.
Pursuant to legislation, the Minister submits these reports and corresponding statements to the Legislative Assembly.
Section 7-4 of the Provincial Health Authority Act requires that the provincial health authority and the SCA submit any reports that the Minister may request from time to time. The provincial health authority and the SCA are required to submit various financial documents and a health service plan to the Ministry.
1.3 Audit of accounts
The Office of the Provincial Auditor for Saskatchewan provides independent assurance (audit reports) and examinations of the Government's management of and accountability practices for the public resources entrusted to it. The Provincial Auditor informs the Legislative Assembly about the reliability of the Government's financial and operational information, the Government's compliance with legislative authorities and the adequacy of the Government's management of public resources. Their reports are available on the Provincial Auditor of Saskatchewan website. The report was released June 5, 2024, and included examinations of the Saskatchewan Health Authority (SHA), 3sHealth (Shared Services Saskatchewan), and the Ministry.
The examination of the Ministry included an audit report on detecting inappropriate physician payments (2024 Report Volume 1, Chapter 12). This report assessed the Ministry's progress on addressing recommendations made in a previous report related to physician billings for insured services.
The Provincial Auditor conducts an annual audit of all government ministries and agencies, including the Ministry. The audit of the Ministry includes a review of Ministry payments including, but not limited to, payments made to the SHA, SCA, and community-based organizations, as well as physicians and dental surgeons for insured physician and surgical-dental services.
Section 7-7 of the Provincial Health Authority Act requires that an independent auditor, who possesses the prescribed qualification and is appointed for that purpose by the SHA and the SCA, audit the accounts of the SHA or the SCA at least once in every fiscal year. The SHA and the SCA must annually submit to the Ministry an audited set of financial statements.
The most recent financial statement audits were for the year ending March 31, 2024. The SHA and SCA each table annual reports in the Saskatchewan Legislature each year which include their audited financial statements. The Government of Saskatchewan tables its audited financial statements (Public Accounts) in the Legislature each year as well. The reports are available to the public directly from each entity and are available on their websites. The annual reporting requirement for the provincial health authority are specified in section 7-5 of the Provincial Health Authority Act.
2.0 Comprehensiveness
2.1 Insured hospital services
Section 2-7 of the Provincial Health Authority Act gives the Saskatchewan Minister of Health (the Minister) the authority to provide funding to the provincial health authority or a health care organization for the purpose of the Act. There were no amendments made to the Act in 2023-2024.
Section 2-9 of the Act permits the Minister to designate facilities including hospitals, special care homes, urgent care centres, and health centres. Section 2-10 allows the Minister to prescribe standards for delivering services in those facilities in the provincial health authority, including health care organizations that have entered into service agreements with the provincial health authority.
The Act sets out the accountability requirements for the provincial health authority and health care organizations. These requirements include, for example, submitting annual financial and health service plans for ministerial approval (section 7-2), and reporting critical incidents (section 8-2). The Minister also has the authority to establish a provincial surgical registry to help manage surgical wait times (section 2-11). The Minister retains authority to inquire into matters (section 8-3), and approve general and practitioner staff by-laws (sections 6-1 to 6-3). The Lieutenant Governor in Council may appoint a public administrator to manage the affairs of the provincial health authority or an affiliate if necessary (section 8-4).
Funding for hospitals is included in the funding provided to the provincial health authority. A comprehensive range of insured services is provided by hospitals. These may include:
- public ward accommodation;
- necessary nursing services;
- the use of operating room and case room facilities;
- required medical and surgical materials and appliances;
- x-ray, laboratory, radiological and other diagnostic procedures;
- radio-therapy facilities;
- anaesthetic agents and the use of anaesthesia equipment;
- physiotherapeutic procedures;
- all drugs, biological and related preparations required for hospitalized patients; and
- services rendered by individuals who receive remuneration from the hospital.
Hospitals are grouped into the following six categories: community or northern, district, regional, provincial, rehabilitation, and field. The hospitals are grouped this way so that people know what they can expect at each hospital. While not all hospitals will offer the same services, reliability and predictability means:
- it is widely understood which services each hospital offers; and
- these services will be provided on a continuous basis, subject to the availability of appropriate health providers.
The provincial health authority has the authority to change the manner in which they deliver insured hospital services based on an assessment of their population health needs, available health providers, and financial resources.
The process for adding a hospital service to the list of services covered by the health care insurance plan involves a comprehensive review, which takes into account such factors as service need, anticipated service volume, health outcomes by the proposed and alternative services, cost and human resource requirements, including availability of providers as well as initial and ongoing competency assurance demands. Typically the provincial health authority initiates the process and, depending on the specific service request, it could include consultations involving several branches within the Ministry of Health as well as external stakeholder groups such as service providers and the public.
The Patient Choice Medical Imaging Act and the Medical Imaging Facilities Licensing Regulations authorize private Magnetic Resonance Imaging (MRI) and Computed Tomography (CT) facilities in Saskatchewan to accept payment directly from patients in exchange for MRI and CT services. However, for every scan that is paid for privately, the Regulations require private providers to provide a second scan, free of charge, to an individual who is waiting on the public list. Private-pay MRI and CT service and its unique two-for-one provision gives patients more options in accessing MRI and CT service and has added capacity to the publicly-funded system at no extra cost to the health system or the patient receiving the reciprocal scan. Along with increases in public capacity through expanded hospital volumes, new MRI and CT scanners, and increased volumes in publicly funded contracts, these privately funded scans and second scans are assisting in the management of diagnostic imaging wait times.
No new hospital services were added to the health care insurance plan in 2023-2024.
2.2 Insured physician services
Sections 8 and 9 of the Saskatchewan Medical Care Insurance Act enable the Minister of Health to establish and administer a plan of medical care insurance for provincial residents. There were no amendments to the Act in 2023-2024. All insured fee items for physicians can be found in the Physician Payment Schedule. As of March 31, 2024, there were 2,907 physicians licensed to practise in the province and eligible to participate in the Medical Care Insurance Plan. Of these, 1,466 (50.4 per cent) were family practitioners and 1,441 (49.6 per cent) were specialists. Physicians may choose not to participate in the Medical Services Plan (known in Saskatchewan legislation as opting-out), but if doing so, they must fully opt out of providing any insured physician services. As per legislation, the non-participating physician must also advise beneficiaries that the physician services to be provided are not insured and that the beneficiary is not entitled to be reimbursed for those services. Written acknowledgement from the beneficiary indicating that they understand the advice given by the physician is also required.
As of March 31, 2024, there was one physician opting-out in Saskatchewan.
Insured physician services are those that are medically necessary, are covered by the Medical Services Plan of the Saskatchewan Ministry of Health, and are listed in the Physician Payment Schedule as prescribed by the Saskatchewan Medical Care Insurance Payment Regulations, 1994 of the Saskatchewan Medical Care Insurance Act.
A process of formal discussion and negotiation between the Ministry's Medical Services Branch and the Saskatchewan Medical Association addresses new insured physician services and definition or assessment rule revisions to existing insured physician services. The Executive Director of the Medical Services Branch manages this process. When the Medical Services Plan covers a new insured physician service, or a change is made to an existing physician service, the changes are reflected in the Physician Payment Schedule. A regulatory amendment to the Saskatchewan Medical Care Insurance Payment Regulations, 1994 is required to provide the authority to pay updated rates to physicians and new insured services.
Although formal public consultations are not held, any member of the public may make recommendations about physician services to be added to the Medical Services Plan.
2.3 Insured surgical-dental services
Dentists may choose to not participate in the Medical Services Plan, but if doing so, they must opt out of providing any insured surgical-dental services. The non-participating dentist must also advise beneficiaries that the surgical-dental services to be provided are not insured and that the beneficiary is not entitled to reimbursement for those services, or advise the beneficiaries to seek services from a dental specialist who is participating. Written acknowledgement from the beneficiary indicating that they understand the advice given by the dentist is also required.
Starting in the fall of 2020, dentists were asked to comply with s. 24(1) of the Saskatchewan Medical Care Insurance Act in regards to formally opting out. Since that time, Medical Services Branch has received 12 formal opt out notices, most of these being received throughout 2023. There are 605 non-participating dentists in Saskatchewan as of August 30, 2024, most of whom are general dentists. Sixty-nine general and specialist dentists provided insured services under the Medical Services Plan.
Insured surgical-dental services are limited to:
- oral or maxillofacial surgery and adjunctive services if provision for payment for the service is included in the dentist payment schedule;
- orthodontic service or nasoalveolar molding treatment services for the care of cleft palate where the beneficiary receiving the service is referred to the dentist by a physician or another dentist;
- the extraction of any teeth necessary to be performed before the provision of heart surgery services, services for chronic renal disease, stem cell transplant services, head or neck cancer services or services for total joint replacement by prosthesis, or resulting from cancer radiation treatment, where:
- the beneficiary is referred to the dentist by a specialist in the field of practice in which the services lie;
- the specialist recommends that payment be made for the service; and
- the Minister approves the payment.
In addition, all dental anaesthetic for beneficiaries under age 14 is publicly funded.
Surgical-dental services can be added to the list of insured services covered under the Medical Services Plan through a process of negotiation with provincial dental surgeons. The Executive Director of the Medical Services Branch manages the process of adding a new service. Although formal public consultations are not held, any member of the public may recommend that surgical-dental services be added to the Medical Services Plan.
As of August 30, 2024, there were approximately 686 practicing dentists and dental surgeons located in all major centres in Saskatchewan. Sixty-nine provided services insured under the Medical Services Plan.
2.4 Uninsured hospital, physician and surgical-dental services
Uninsured hospital, physician, and surgical-dental services in Saskatchewan include:
- in-patient and out-patient hospital services provided for reasons other than medical necessity;
- services prescribed to be an "uninsured service" in legislation;
- the extra cost of private and semi-private hospital accommodation not ordered by a physician;
- physiotherapy and occupational therapy services not provided by or under contract with the provincial health authority;
- services provided by health facilities other than hospitals unless through an agreement with the provincial health authority and licensed under the Health Facilities Licensing Act;
- MRI and CT services, as defined in the Medical Imaging Facilities Licensing Regulations, when performed in a medical imaging facility as defined in the Patient Choice Medical Imaging Act;
- non-emergency insured hospital, physician, or surgical-dental services obtained outside Canada without prior written approval;
- non-medically required elective physician services;
- surgical-dental services that are not medically necessary; and
- services received under other public programs including the Workers' Compensation Act, 1979, the federal Department of Veteran Affairs and the Mental Health Services Act.
As a matter of policy and principle, insured hospital, physician, and surgical-dental services are provided to residents on the basis of assessed clinical need. There are no charges allowed in Saskatchewan for insured hospital, physician, or surgical-dental services. Charges for enhanced medical services or products are permitted only if the medical service or product is not deemed medically necessary and/or not deemed to be an insured service. Compliance is monitored through consultations with the provincial health authority, physicians and dentists, as well as via complaints from members of the public.
Insured hospital services are typically de-insured by the government if they were determined to be no longer medically necessary and/or clinically appropriate. The process involves discussions among stakeholders, practitioners, and officials from the Saskatchewan Ministry of Health.
Insured physician services could be de-insured if they were determined not to be medically required and/or clinically appropriate. The process involves consultations with the Saskatchewan Medical Association and managed by the Executive Director of the Medical Services Branch.
Insured surgical-dental services could be de-insured if they were determined not to be medically necessary and/or clinically appropriate. The process involves discussion and consultation with the dental surgeons of the province and is managed by the Executive Director of the Medical Services Branch.
Formal public consultations about de-insuring hospital, physician or surgical-dental services may be held if warranted. There were no services de-insured during 2023-2024.
3.0 Universality
3.1 Eligibility
The Saskatchewan Medical Care Insurance Act (sections 2 and 12) and the Medical Care Insurance Beneficiary and Administration Regulations define eligibility for insured health services in Saskatchewan. Section 11 of the Act requires that all residents register for provincial health coverage.
While the Regulations set out classes of beneficiaries exempt from insured services under the Act, it is possible for individual residents to request that the Health Registry not issue a provincial health card in certain cases (e.g., for religious reasons).
Eligibility is limited to residents. A "resident" means a person who is legally entitled to remain in Canada, who makes their home and is ordinarily present in Saskatchewan, or any other person declared by the Lieutenant Governor-in-Council to be a resident. Canadian citizens and permanent residents of Canada relocating from within Canada to Saskatchewan are generally eligible for coverage on the first day of the third month following establishment of residency in Saskatchewan. There were no changes to residency requirements in 2023-2024.
Returning Canadian citizens, the families of returning members of the Canadian Forces, and international students, and international workers with valid immigration status are eligible for coverage on establishing residency in Saskatchewan, provided that residency is established before the first day of the third month following their admittance to Canada.
The following persons are not covered under Saskatchewan's Medical Services Plan:
- members of the Canadian Forces, federal inmates, refugee claimants, visitors to the province; and
- persons eligible for coverage from their home province or territory for the period of their stay in Saskatchewan (e.g., students and workers covered under temporary absence provisions from their home province or territory).
Such people become eligible for coverage as follows:
- discharged members of the Canadian Forces, if stationed in or resident in Saskatchewan on their discharge date;
- released federal inmates (this includes those inmates who have completed their sentences in a federal penitentiary and those inmates who have been granted parole and are living in the community); and
- refugee claimants, on receiving Convention Refugee status (immigration documentation is required).
Individuals who are not successful when applying for a provincial health card may appeal the decision by submitting to Health Registries - eHealth Saskatchewan, a Saskatchewan Health Services Card Application—Appeal Form.
The number of persons registered for health services in Saskatchewan on June 30, 2024 was 1,278,382.
3.2 Other categories of individuals
Other categories of individuals who are eligible for insured health service coverage include persons allowed to enter and remain in Canada under authority of a work permit, study permit, or Minister's permit issued by Immigration, Refugees and Citizenship Canada. Their accompanying family may also be eligible for insured health service coverage.
Refugees are eligible on confirmation of Convention status or with a study or work permit, Minister's permit, or permanent resident or landed immigrant record.
People moving to Saskatchewan from outside of Canada may be eligible for Saskatchewan health coverage upon establishing residence in province, if among one of the following groups:
- permanent residents (landed immigrants);
- people discharged from the Canadian Forces;
- non-immigrants who are in Canada in connection with their trade or profession;
- international students;
- returning spouses of Canadian Forces members; and
- returning Canadian citizens.
Applicants for permanent residence are not eligible for health benefits unless they are eligible under one of the above categories. Foreign clergy and NATO individuals are eligible for Saskatchewan health benefits.
4.0 Portability
4.1 Minimum waiting period
In general, insured persons from another province or territory who move to Saskatchewan are eligible on the first day of the third month following establishment of residency. However, where one spouse arrives in advance of the other, the eligibility for the initial arriving spouse is established on either a) the first day of the third month following arrival of the second spouse; or b) the first day of the thirteenth month following the establishment of residency by the first spouse. The second spouse would be eligible on the first day of the third month following arrival.
In 2022–2023, Saskatchewan amended the Medical Care Insurance Beneficiary and Administration Regulations to provide health coverage to individuals arriving from Ukraine as part of Government's commitment to provide services and supports for individuals arriving under the Canada-Ukraine Authorization for Emergency Travel program.
4.2 Coverage during temporary absences in Canada
Section 3 of the Medical Care Insurance Beneficiary and Administration Regulations of the Saskatchewan Medical Care Insurance Act prescribes the portability of health insurance provided to Saskatchewan residents while temporarily absent within Canada.
Residents of Saskatchewan are able to maintain health coverage during a period of temporary absence, conditional upon the registrant's intent to return to Saskatchewan residency.
- Residents of Saskatchewan are required to be physically present in the province for a minimum 5 months over a 12 month period.
- Residents of Saskatchewan who are temporarily absent from the province for more than 7 months are required to submit a request for extended absence as follows:
- education: for the duration of studies at a recognized educational facility (confirmation by the facility of full-time student status and expected graduation date are required);
- employment of up to 12 months in Canada; and
- vacation and travel of up to 12 months.
In 2015–2016, Saskatchewan amended the Medical Care Insurance Beneficiary and Administration Regulations to increase the amount of time residents are allowed to be out-of-province while still maintaining their health care benefits. Residents are now able to maintain health coverage after spending a maximum of seven months outside of Saskatchewan. Residents were only allowed to be absent for a maximum of six months over any 12 month period before their health benefits were discontinued. The amended legislation took effect January 1, 2016.
Section 6.6 of the Health Administration Act provides the authority for paying in-patient hospital services to Saskatchewan beneficiaries temporarily residing outside the province. Section 10 of the Saskatchewan Medical Care Insurance Payment Regulations, 1994, provides payment for physician services to Saskatchewan beneficiaries temporarily residing outside the province but within Canada. No amendments were made to the Act in 2023-2024; however, amendments were made to the Regulations to provide the authority to pay updated rates and new insured services to physicians.
Saskatchewan has bilateral reciprocal billing agreements with all provinces for hospital services. Quebec does not participate in reciprocal billing of physician services.
4.3 Coverage during temporary absences outside Canada
Section 3 of the Medical Care Insurance Beneficiary and Administration Regulations of the Saskatchewan Medical Care Insurance Act prescribes the portability of health insurance provided to Saskatchewan residents who are temporarily absent from Canada.
Residents of Saskatchewan are able to maintain health coverage during a period of temporary absence, conditional upon the registrant's intent to return to Saskatchewan residency.
- Residents of Saskatchewan are required to be physically present in the province for a minimum of 5 months over a 12-month period.
- Residents who are temporarily absent from the province for 7 months or more are required to submit a request for extended absence as follows:
- education: for the duration of studies at a recognized educational facility (confirmation by the facility of full-time student status and expected graduation date are required);
- employment of up to 24 months outside of Canada; and
- vacation and travel of up to 12 months.
Section 3 of the Medical Care Insurance Beneficiary and Administration Regulations provides open-ended temporary absence coverage for persons whose principal place of residence is in Saskatchewan, but who are not able to satisfy the annual five months physical presence requirement because the nature of their employment requires travel from place to place outside Canada (e.g., cruise line workers).
In 2022–2023, Saskatchewan amended the Medical Care Insurance Beneficiary and Administration Regulations to ensure out-of-country employees of the Government of Saskatchewan are not without provincial health coverage.
Section 6.6 of the Health Administration Act provides the authority under which a resident is eligible for health coverage when temporarily outside Canada. In summary, a resident is eligible for medically necessary hospital services at the rate of $100 per in-patient and $50 per out-patient visit per day. No amendments were made to the Regulations in 2023-2024.
4.4 Prior approval requirement
Out-of-Province
The Saskatchewan Ministry of Health covers most hospital and medical out-of-province care received by its residents in Canada through reciprocal billing arrangements. These arrangements mean that residents do not need prior approval and may not be billed for most hospital and medical services received within the publicly funded health care system in other provinces or territories while travelling within Canada. The cost of travel, meals and accommodation are not covered. Prior approval is required for the following services provided out-of-province:
- alcohol and drug, mental health, rehabilitation, problem gambling services, home care, certain rehabilitative services, and services not eligible to be billed reciprocally.
Prior approval from the Saskatchewan Ministry of Health must be obtained by the patient's specialist before the out-of-province services are received.
Out-of-Country
If a Saskatchewan specialist refers a patient outside Canada for treatment not available in Saskatchewan or another province, the referring specialist must obtain prior approval for coverage from the Medical Services Plan of the Saskatchewan Ministry of Health. The Saskatchewan Cancer Agency is consulted for out-of-country cancer treatment requests. If approved, the Saskatchewan Ministry of Health will pay the full cost of treatment, excluding any items that would not be covered in Saskatchewan.
In Saskatchewan, the Health Services Review Committee (HSRC) is an arms-length panel that reviews government decisions made on requests for out-of-province and out-of-country medical coverage, ensuring legislation, policy, and guidelines are followed appropriately.
The Ministry of Health informs eligible applicants of their right to request a review by the HSRC upon denial of their out-of-province or out-of-country coverage request. A person can request a review by the HSRC only if the coverage request was for out-of-province insured medical health services, elective out-of-country insured medical services (physician and hospital care) or community care programs (mental health, alcohol and drug, problem gambling, and rehabilitative services).
If a case is ineligible for HSRC or if HSRC upholds the Saskatchewan Ministry of Health's coverage decision, a person may contact the Provincial Ombudsman for their review.
5.0 Accessibility
5.1 Access to insured health services
To ensure that access to insured hospital, physician, and surgical-dental services is not impeded or precluded by financial barriers, extra-billing by physicians or dental surgeons, and user charges by hospitals for insured health services are not allowed in Saskatchewan.
Pursuant to section 18 (1.1) of the Saskatchewan Medical Care Insurance Act, no physician or other person who provides an insured service to a beneficiary shall demand or accept payment for that service in an amount that he knows exceeds the payment to be made for that service prescribed in the Saskatchewan Medical Care Insurance Payment Regulations, 1994.
With regard to extra-billing and user charges, compliance is monitored through consultations with the provincial health authority, physicians and dentists, as well as complaints from members of the public. The Saskatchewan Ministry of Health's General Inquiry contact information is as follows:
Saskatchewan Ministry of Health
1-800-667-7766
When requests are made by a beneficiary to reimburse monies paid directly to a physician for insured physician services that are extra-billing charges, correspondence is sent to the beneficiary (copying the physician) advising them of section 18 (1.1) of the Saskatchewan Medical Care Insurance Act that a physician must accept the negotiated rate as payment in full for insured services provided to a beneficiary. Once they have received payment from Medical Services Plan for the eligible service(s), reimbursement for any difference in the amount charged by the practitioner and the amount paid by Medical Services should be collected directly from the practitioner. If further complaint is made, the beneficiary is directed to address complaints to the Saskatchewan College of Physicians and Surgeons.
In addition, a private third-party facility must obtain a health facility licence to provide certain insured services (e.g., surgical services) on behalf of the publicly funded health system. The Health Facilities Licensing Act (HFLA) authorizes and prescribes the conditions under which a health facility licence may be issued to a private facility. The HFLA stipulates that a licensee may not charge or permit any other person to charge any fee to any beneficiary for any insured health service as defined under the HFLA.
Legislation prescribes that the Saskatchewan Minister of Health may amend, suspend or cancel a license if, in the opinion of the Minister, the licensee has failed to comply with the above clause.
Persons who have a complaint of an extra-billing and user charge may also raise the concern with the College of Physicians and Surgeons of Saskatchewan. The College has in their bylaws 7.1 Code of Ethics that includes:
- treat all patients with respect; and
- do not exploit them for personal advantage.
Contravention of, or failure to comply with, the Code of Ethics is unbecoming, improper, unprofessional or discreditable conduct for the purposes of the Saskatchewan Medical Care Insurance Act.
The health system continues to strengthen coordination, communication, and referral guidelines to better coordinate services to ensure patients have timely access to the most appropriate specialist and diagnostic services. By reducing the wait time for a consult with a specialist or diagnostic services (such as MRI and CTs), patients will be able to access treatment sooner.
Other Programs and Initiatives to Improve Access
The Family Physician Comprehensive Care Program is intended to support recruitment and retention of family physicians by recognizing those physicians who provide a full range of services to their patients and the continuity of care that result from these comprehensive services.
Leveraging Immediate Non-Urgent Knowledge (LINK) is a provincial telephone consultation service that allows primary care providers to consult with a specialist about serious and/or complex non-urgent patient health concerns. LINK helps patients get answers to their health concerns sooner, prevents unnecessary referrals, and supports better referrals to the right specialist when required.
Specialist wait times can vary for a variety of reasons and can result in two patients with the same condition and acuity having very different wait times. Pooled referrals offer referring physicians and their patients more choices to reduce wait times and improve patient access. Pooled referral systems direct patients to the next available specialist able to treat the patient's condition yet still allow physicians to make direct referrals to a specific specialist using the same referral process.
Saskatchewan's online Specialist Directory makes it easier to find current surgical wait times and information about surgical specialists in Saskatchewan. It can help patients and their family doctors view their options for surgical services and help them to easily identify the most appropriate surgeon for them. One of the many benefits is it can enable patients who are willing to travel to have the surgery more quickly in a location other than their nearest surgical centre.
The Transitional Payment Model (TPM) is a new payment model launched on April 1, 2024, for fee-for-service family physicians aimed at promoting longitudinal care within family medicine and increasing patient access to primary care. The new model is a transitional step between the current fee-for-service and the future goal of a blended capitation model.
5.2 Physician compensation
Section 6 of the Saskatchewan Medical Care Insurance Payment Regulations, 1994, outlines the obligation of the Minister of Health to make payments for insured services in accordance with the Physician Payment Schedule and the Dentist Payment Schedule.
Fee-for-service is the most widely used method of compensating physicians for insured health services in Saskatchewan, although sessional payments, salary, and blended methods are also used. Fee-for-service is the only mechanism used to fund dentists for insured surgical-dental services. Total expenditures for in-province physician services and programs in 2023-2024 amounted to $1.282 billion: $573.8 million for fee-for-service billings; $33.2 million for Specialist Emergency Coverage Programs; and $550.7 million in non-fee-for-service expenditures. There was also an additional $124.7 million for the Clinical Services Fund and other Saskatchewan Medical Association and bursary programs.
The Saskatchewan Joint Medical Professional Review Committee (JMPRC) is a physician peer-review Committee that was established by section 49 of the Saskatchewan Medical Care Insurance Act (1988) to review the billing patterns of Saskatchewan physicians who are directly billing the publicly funded system for insured services. The JMPRC reviews billing patterns of physicians referred by the Director of Professional Review of the Ministry of Health and in cases where they determine that monies have been paid by the Minister inappropriately, they may order recovery from the physician.
Saskatchewan physicians do not charge block fees.
5.3 Payments to hospitals
The Saskatchewan Health Authority (SHA) is provided with a global operating grant and is responsible for allocating the funding it receives to address service needs and priorities identified through its needs assessment processes. The annual operating grant includes status-quo funding levels and other adjustments as outlined in the current year provincial budget. The SHA may receive additional funds for providing specialized hospital programs and services (e.g., acute services including surgical and EMS programs, primary and public health including seniors programs, and mental health and addictions services).
Payments to the SHA for delivering services are made pursuant to section 2-7 of the Provincial Health Authority Act. The legislation provides the authority for the Minister of Health to make grants to the SHA and health care organizations for the purposes of the Act, and to arrange for providing services in any area of Saskatchewan if it is in the public interest to do so.
The SHA provides an annual report on the consolidated financial results of its operations.
6.0 Recognition given to federal transfers
Federal contributions provided through the Canada Health Transfer are publicly acknowledged by the Government of Saskatchewan in:
- the 2023-2024 Provincial Budget and related documents;
- the 2023-2024 Public Accounts; and
- the Quarterly and Mid-Year Financial Reports.
These documents were tabled in the Legislative Assembly and are publicly available to Saskatchewan residents at Saskatchewan.ca. Federal contributions have also been acknowledged in news releases and issue papers, and in speeches and remarks made at various conferences, meetings, and public policy forums.
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 1. Number as of March 31st | 1,216,490Footnote 1 | 1,227,341Footnote 1 | 1,209,615Footnote 1 | 1,261,585Footnote 1 | 1,278,382Footnote 1 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| Public facilities | |||||
| 2. Number | 66 | 66 | 66 | 66 | 66 |
| 3. Payments for insured health services ($)Footnote 2 | 2,141,445,000 | 2,328,971,000 | 2,419,274,000 | 2,533,077,000Footnote 3 | 2,807,688,750 |
| Private for-profit facilities | |||||
| 4. Number of private for-profit facilities providing insured health services | 6 | 8 | 8 | 6 | 6 |
| 5. Payments to private for-profit facilities for insured health services ($) | not availableFootnote 4 | not availableFootnote 4 | not availableFootnote 4 | not availableFootnote 4 | not availableFootnote 4 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 6. Total number of cases, in-patient | 3,991 | 3,362 | 2,854 | 3,191 | 2,898 |
| 7. Total payments, in-patient ($) | 55,922,600 | 64,907,900 | 50,402,300 | 64,153,300 | 66,010,600 |
| 8. Total number of cases, out-patient | 74,539 | 53,521 | 55,133 | 58,807 | 54,876 |
| 9. Total payments, out-patient ($) | 30,332,600 | 20,739,600 | 19,857,600 | 21,886,800 | 23,084,300 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| Pre-approved | |||||
| 10. Total number of cases, pre-approved in-patient | 8 | 0 | 0 | 2 | 4 |
| 11. Total payments, pre-approved in-patient ($) | 1,855,300 | 0 | 0 | 243,000 | 376,100 |
| 12. Total number of cases, pre-approved out-patient | 216 | 22 | 12 | 37 | 15 |
| 13. Total payments, pre-approved out-patient ($) | 1,433,700 | 42,900 | 127,400 | 94,000 | 86,400 |
| Non Pre-approved | |||||
| 14. Total number of cases, non pre-approved in-patient | 283 | 120 | 47 | 118Footnote 6 | 160 |
| 15. Total payments, non pre-approved in-patient ($) | 2,431,900 | 288,117 | 22,900 | 985,800Footnote 6 | 72,700 |
| 16. Total number of cases, non pre-approved out-patient | 920 | 419 | 133 | 249 | 659 |
| 17. Total payments, non pre-approved out-patient ($) | 45,200 | 21,500 | 6,500 | 12,500 | 33,000 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 18. Number of participating physicians | 2,622 | 2,718 | 2,796 | 2,820 | 2,907 |
| 19. Number of opted-out physicians | 0 | 0 | 0 | 0 | 1 |
| 20. Number of non-participating physicians | 0 | 0 | 0 | 0 | 0 |
| 21. Total payments for services provided by physicians paid through all payment methods ($) | 1,050,449,400 | 970,000,400 | 1,178,460,260 | 1,240,000,000 | 1,282,330,000 |
| 22. Total payments for services provided by physicians paid through fee-for-service ($) | 556,434,500Footnote 7 | 437,348,300Footnote 7 | 541,863,260Footnote 7 | 570,245,600Footnote 7 | 573,789,500Footnote 7 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 23. Number of services | 770,674 | 638,087 | 690,676 | 729,095 | 711,340 |
| 24. Total payments ($) | 44,549,700 | 35,554,200 | 38,179,300 | 41,047,600 | 41,331,100 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| Pre-approved | |||||
| 25. Number of pre-approved services | 764 | 145 | 23 | 189 | 190 |
| 26. Total pre-approved payments ($) | 747,889 | 140,442 | 20,445 | 295,300 | 600,400 |
| Non Pre-approved | |||||
| 27. Number of non pre-approved services | 4,817 | 1,627 | 709 | 1,703 | 2,111 |
| 28. Total non pre-approved payments ($) | 289,000 | 93,058 | 41,200 | 156,900 | 139,200 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 29. Number of participating dentists | 76 | 74 | 70 | 65 | 69 |
| 30. Number of opted-out dentists | 0 | 0 | 0 | 17 | 12 |
| 31. Number of non-participating dentists | 1 | 2 | 1 | 499Footnote 8 | 605Footnote 8 |
| 32. Number of services provided | 12,656 | 10,374 | 9,804 | 7,926 | 8,778 |
| 33. Total payments ($) | 1,565,900 | 1,046,000 | 1,197,300 | 1,450,600 | 1,771,200 |
|
|||||
Alberta
The Government of Alberta is refocusing the health care system to prioritize patient care and empower frontline health care workers, including those serving rural, remote and Indigenous communities, to deliver the highest quality health care. In 2023-2024, the Government of Alberta invested in high priority areas including decreasing emergency department wait times, improving EMS wait times, addressing surgical wait times, empowering front-line workers, and providing mental health and addiction supports. More information is available through the Ministry of Health and Ministry of Mental Health and Addiction websites.
1.0 Public administration
1.1 Health care insurance plan and public authority
The Ministry of Health sets policy and direction to achieve a sustainable and accountable health system to promote and protect the health of Albertans. The Ministry of Health administers and operates the Alberta Health Care Insurance Plan (AHCIP). Pursuant to the Health Insurance Premiums Act, the Alberta Health Care Insurance Act (AHCIA) and the Hospitals Act, Alberta residents are eligible to receive insured services under the AHCIP and the Hospitalization Benefits Plan in accordance with the Canada Health Act. Since 1969, the AHCIA, which is available on the Alberta King's Printer website, has regulated the administration and operation of the AHCIP. Section 3 of the AHCIA establishes the AHCIP and designates the Alberta Minister of Health (the Minister) as the public authority responsible for the administration and operation of the AHCIP.
1.2 Reporting relationship
The Minister is accountable for the AHCIP. As the public authority responsible for the AHCIP, the Minister is required to administer and operate the AHCIP on a non-profit basis, in accordance with the AHCIA and the regulations under the Act, to provide benefits for basic health services to all residents of Alberta. The AHCIA and regulations include several accountability measures relating to the administration and operation of the AHCIP, including provisions that enable the Minister to reassess claims for benefits and recover overpayments to practitioners.
The Sustainable Fiscal Planning and Reporting Act (SFPRA) provides a framework for government budgeting and fiscal planning. A ministry annual report is prepared under the direction of the Minister in accordance with the SFPRA and the government's accounting policies. The Ministry of Health 2023-2024 Annual Report, covering the fiscal year April 1, 2023, to March 31, 2024, was released on June 27, 2024.
1.3 Audit of accounts
The Auditor General of Alberta is an independent office responsible for conducting annual financial audits and other audits pertaining to the government's management of public resources. In accordance with Alberta's Auditor General Act, audit reports are tabled with the Legislative Assembly. The Auditor General's report on the audit of the Government of Alberta's consolidated financial statements, which includes the financial transactions and other information of the Ministry of Health, was published on June 27, 2024, in the Government of Alberta's 2023-2024 Annual Report.
The Auditor General's report indicated that the consolidated financial statements present fairly and in all material respects the consolidated financial position and the results of its operations, in accordance with the Canadian public sector accounting standards, for the fiscal year ended March 31, 2024.
2.0 Comprehensiveness
2.1 Insured hospital services
The Hospitals Act, the Operation of Approved Hospitals Regulation (247/1990), the Hospitalization Benefits Regulation (AR 244/1990), the Health Facilities Act (HFA), and the Health Facilities Regulation (AR 208/2000) govern the provision of insured services in hospitals and chartered surgical facilities (CSFs). These are available on the Alberta King's Printer website.
In Alberta, hospital boards (meaning the corporate body or person that owns or operates a hospital, and includes a regional health authority under the Regional Health Authorities Act) (replaced June 21, 2024, by the Provincial Health Agencies Act) are the entities accountable to the Minister for ensuring the provision of insured hospital services. Alberta Health Services (AHS), as Alberta's sole regional health authority, is responsible for operating the majority of the approved hospitals in Alberta.
The publicly funded hospital services provided in approved hospitals in Alberta include all of the hospital services listed in the Canada Health Act. The insured hospital services range from advanced levels of diagnostic and treatment services for in-patients and out-patients, to routine care and management of patients with previously diagnosed chronic conditions. The benefits available to hospital patients in Alberta are set out in the Hospitals Act and the Hospitalization Benefits Regulation.
The list of insured services included in the Hospitals Act and the Hospitalization Benefits Regulation is intended to be both comprehensive and generic, thereby limiting the need for routine review and updating. No new insured hospital services were added during 2023-2024.
Computed Tomography (CT) and Magnetic Resonance Imaging (MRI) diagnostic procedures are publicly funded and provided to eligible Albertans at AHS facilities or AHS-contracted facilities. AHS has a system that sets priorities and manages wait times for these services. If a patient chooses to attend a private diagnostic clinic and self pay for medically required CT and MRI diagnostic procedures, AHS has a process for reimbursement if certain criteria are met.
The Ministry of Health has not made any legislative or regulatory changes to insured hospital services in 2023-2024, including in respect of diagnostic imaging.
2.2 Insured physician services
The Alberta Health Care Insurance Act (AHCIA) establishes the Alberta Health Care Insurance Plan (AHCIP) to provide benefits for basic health services to all residents of Alberta. Physicians, as defined in the AHCIA, are permitted to claim benefits through the AHCIP for providing insured services. Persons referred to in section 20.1 of the AHCIA (discussed further below) are also able to submit claims for benefits through the AHCIP for insured services provided by physicians, subject to meeting certain legislative requirements.
Section 20.1 of the AHCIA authorizes a person (excluding individuals and professional corporations) to submit claims for benefits for an insured service provided by a physician if:
- the Minister has entered into a section 20 agreement or established a section 20 arrangement with that person for the payment of benefits for the insured service on a basis other than a fee-for-service basis;
- the person employs or has entered into a service agreement with the physician to provide the insured service; and,
- the physician was participating in the AHCIP when the insured service was provided.
Examples of possible section 20.1 persons include AHS, or a corporation that owns and operates pharmacies.
The person referred to in section 20.1 has a direct legal relationship with the Minister through the section 20 agreement or arrangement (i.e., a legal right to claim and receive benefits for the provision of insured services by a physician without the physician having to assign the benefits to that person).
Section 20.1(4) provides that the person referred to in section 20.1 has all the duties of a physician with respect to the provision to the Minister of information required to facilitate the handling, assessing, and payment of the claim for benefits. The person referred to in section 20.1 is also subject to the prohibition on extra-billing, the Minister's right to recover amounts, and monitoring and enforcing compliance with the AHCIA. In 2023-2024 there were no section 20 arrangements or agreements with a person referred to in section 20.1.
Alberta had 11,435 physicians participating under the AHCIP as of March 31, 2024. Of these physicians:
- 9,071 physicians claimed benefits exclusively on a fee-for-service basis;
- 1,081 physicians claimed benefits solely through an agreement or arrangement under section 20 of the AHCIA (e.g., through an Alternative Relationship Plan) (see section 5.2 for more details); and,
- the remaining 1,283 physicians claimed benefits from both fee-for-service and through an Alternative Relationship Plan.
As of March 31, 2024, there were six non-participating physicians in the province.
A physician must complete the appropriate registration forms and include a copy of the licence issued to them by the College of Physicians and Surgeons of Alberta (CPSA) before being registered with the AHCIP.
Under section 8 of the AHCIA, all physicians are deemed to participate in the AHCIP. Under section 8(2), a physician may choose to not participate in the AHCIP by taking the following actions at least 180 days prior to the effective date of opting out:
- notifying the Minister of Health in writing indicating the effective date of non-participation;
- publishing a notice of the proposed non-participation in a newspaper having general circulation in the area in which the physician practises; and,
- posting a notice of the proposed non-participation in a part of the physician's office to which patients have access.
Legal requirements are set out in section 8(3) of the AHCIA for a physician who has not previously practised in Alberta and wants to opt out of the AHCIP. Under section 8(3), the physician may choose to not participate in the AHCIP prior to commencing practice by:
- notifying the Minister in writing indicating the date on which the physician will commence non-participating practice; and,
- publishing a notice of the proposed non-participation in a newspaper having general circulation in the area in which the physician intends to practise.
By not participating in the AHCIP, a physician agrees that, commencing on the effective date of opting out, they will not participate in the publicly funded health system. This means that the physician cannot submit a claim for benefits to the AHCIP for payment for providing what would otherwise be insured medical services, and the patient cannot seek reimbursement for any amounts paid by the patient for receiving the medically required services from the non-participating physician.
The Medical Benefits Regulation (AR 84/2006) establishes the benefits payable for insured medical services provided to a resident of Alberta. Descriptions of those insured medical services which are payable on a fee-for-service basis are set out in the Schedule of Medical Benefits.
The Ministry of Health is committed to having a Schedule of Medical Benefits that supports continuous improvement and is responsive to health reform. The Ministry of Health consults with the medical community by engaging with the Alberta Medical Association (AMA), and health services codes are created to ensure the Schedule of Medical Benefits reflects the current standard of practice for physicians within Alberta. There is no broader public consultation. All changes to the Schedule of Medical Benefits require the approval of the Minister of Health.
Virtual care health service codes were permanently added to the Schedule of Medical Benefits on June 9, 2020. In May 2021, the Ministry of Health formed a virtual care working group to explore short-term opportunities with respect to claims for benefits for physicians providing insured medical services virtually. The group included members from AHS, the AMA and the CPSA. Based on the working group's recommendations, the Ministry of Health made enhancements to the Schedule of Medical Benefits in respect of virtual health service codes in January 2022. The Ministry provided the necessary medical bulletins (MED 252/254 and MED 266/268) to the physician community on educating and submitting claims for insured services provided virtually. Effective October 23, 2023, Alberta Health implemented changes to the Schedule of Medical Benefits to enhance delivery of virtual mental health insured services in Alberta. This included, but was not limited to, the creation of new health service codes for delivery of group and family psychotherapy, and complex psychiatric insured services, virtually.
2.3 Insured surgical-dental services
In Alberta, a small number of medically necessary oral surgical and dental procedures are insured through the AHCIP, and are listed in the Schedule of Oral and Maxillofacial Surgery Benefits. In 2023-2024, no updates were made to this schedule
The majority of dental procedures for which benefits are claimed through the AHCIP can only be performed by a dentist certified as an oral and maxillofacial surgeon who meets the requirements stated in the AHCIA. Insured dental-surgical services must be performed in public hospitals or CSFs. Major surgical services, including dental-surgical services as referred to in section 2(2)(b) of the HFA may only be provided in a public hospital. As of March 31, 2024, there were 147 dentists who submitted claims for benefits under the AHCIP for eligible dental procedures in the 2023-2024 fiscal year, and no dentists were non-participants. Routine dental care is not an insured service for which a benefit is payable through the AHCIP.
Although there is no formal agreement with dentists, the Ministry of Health meets with the Alberta Dental Association to discuss changes to the Schedule of Oral and Maxillofacial Surgery Benefits. There is no public consultation. All changes to the Schedule of Oral and Maxillofacial Surgery Benefits require the approval of the Minister of Health.
Under section 7(1) of the AHCIA, all dentists are deemed to participate in the AHCIP. Under section 7(2), a dentist may opt out of the AHCIP by taking the following actions at least 30 days prior to the effective date of opting out:
- notifying the Minister in writing indicating the effective date of nonparticipation;
- publishing a notice of the proposed non-participation in a newspaper having general circulation in the area in which the dentist practises; and,
- posting a notice of the proposed non-participation in a part of the dentist's office to which patients have access.
Legal requirements are set out in section 7(3) of the AHCIA for a dentist who has not previously practised in Alberta and wants to opt out of the AHCIP. Under section 7(3), the dentist may choose to not participate in the AHCIP prior to commencing practice by:
- notifying the Minister in writing indicating the date on which the dentist will commence non-participating practice; and,
- publishing a notice of the proposed non-participation in a newspaper having general circulation in the area in which the dentist intends to practise.
By choosing not to participate in the AHCIP, a dentist agrees that, commencing on the effective date of opting out, they will not participate in the publicly funded health system. This means that the dentist cannot submit a claim for benefits to the AHCIP for payment for providing what would otherwise be insured surgical-dental services and the patient cannot seek reimbursement for any amounts paid by the patient for receiving surgical-dental services from the non-participating dentist.
2.4 Uninsured hospital, physician, and surgical-dental services
Section 4(2) of the Hospitalization Benefits Regulation lists hospital services that are not insured services.
The Preferred Accommodation and Non-Standard Goods or Services Policy (the Policy) describes the Government of Alberta's expectations and requirements of regional health authorities (i.e., AHS) in respect of the provision of preferred accommodation and enhanced or non-standard goods and services. The Policy requires regional health authorities to provide 30 days' advance notice to the Minister of Health's designate regarding the categories of preferred accommodation offered and the charges associated with each category. Regional health authorities are also required to provide 30 days' advance notice to the Minister of Health's designate regarding any goods or services that will be provided as non-standard goods or services. Regional health authorities must also provide information about the associated charge for these goods or services, and when applicable, the criteria or clinical indications that may qualify patients to receive it as a standard good or service.
Section 12(2) of the Alberta Health Care Insurance Regulation (AR 76/2006) lists services that are not considered basic or extended health services unless otherwise approved by the Minister of Health.
Section 4(2) and section 5(2) of the Oral and Maxillofacial Surgery Benefits Regulation (AR 86/2006) indicates no benefits are payable for oral and maxillofacial surgery services provided to an Alberta resident in another province or territory of Canada or outside of Canada if the services provided are not insured services in Alberta.
Services not covered by the AHCIP include (but are not limited to):
- medical-legal services;
- surgical procedures for the alteration of appearance, performed for emotional, psychological, or psychiatric reasons;
- transportation services (including ambulance services);
- prescription drugs, casts, surgical appliances and special bandages (except as provided for in the Schedule of Medical Benefits, the Schedule of Podiatric Surgery Benefits, or the Schedule of Podiatric Benefits);
- clinical pharmacy services;
- routine dental care;
- routine eye examinations for residents 19 to 64 years of age; and,
- third party medical services, such as medicals for employment, insurance, and sports.
Medical services are deleted from the Schedule of Medical Benefits when those services are identified by the medical community as obsolete. The process to engage the medical community is completed through consultation with the AMA and AHS. The AMA is the representative of physicians. AHS is engaged in this decision process in order to understand how changes may impact current service delivery models or the health system at a macro level. No medical services were removed from the Schedule of Medical Benefits in 2023-2024.
3.0 Universality
3.1 Eligibility
Pursuant to the Health Insurance Premiums Act, the Alberta Health Care Insurance Act and the Hospitals Act, Alberta residents are eligible to receive insured services under the Alberta Health Care Insurance Plan (AHCIP) and the Hospitalization Benefits Plan. There were no changes made to eligibility requirements in 2023-2024.
A resident is defined as a person who is lawfully entitled to be or to remain in Canada, who makes the province their home and is ordinarily present in Alberta, and any other person deemed by the regulations to be a resident. The term "resident" does not include a tourist, transient, or visitor to Alberta.
Persons moving permanently to Alberta from outside Canada are eligible for coverage if they have permanent resident status, are returning permanent residents, or are returning Canadian citizens. Persons residing in Alberta on an approved Canada entry document may also be eligible for coverage, and their eligibility is reviewed on a case-by-case basis.
A resident is not entitled to coverage if the resident is a member of the Canadian Armed Forces or a person serving a term of imprisonment in a federal penitentiary as defined in the Corrections and Conditional Release Act. These residents receive health care coverage from the federal government. Spouses or partners and dependants of these residents are provided with coverage if they are Alberta residents.
Individuals released within Alberta from the Canadian Armed Forces or federal penitentiaries, are eligible for coverage effective the date of release, if the ministry is notified within three months. If individuals are released in another part of Canada, they are eligible for coverage on the first day of the third month after becoming a resident of Alberta.
In order to access insured services under the AHCIP and the Hospitalization Benefits Plan, Alberta residents are required to register themselves and their eligible dependants. Family members are registered on the same account. Persons moving to Alberta should apply for coverage within three months of arrival or effective dates may be affected. For persons moving to Alberta from within Canada, their registration is effective on the first day of the third month after they become an Alberta resident. For persons moving to Alberta from outside Canada, their registration is effective the day they become an Alberta resident. The process for registering Albertans requires registrants to provide documentation that proves their identity, legal entitlement to be in Canada, and Alberta residency.
When a cancellation or denial of AHCIP or Hospitalization Benefits Plan coverage is questioned, an individual may contact the Ministry of Health by phone, e-mail, or mail to discuss the issue. If the issue cannot be resolved by front-line staff, it is escalated to a supervisor, then a manager, if needed. The manager will conduct a thorough investigation and send a letter with reasons for the decision, as it relates to legislation.
Pursuant to section 25(1) of the Health Insurance Premiums Act, individuals can choose at any time for themselves and their dependants to not participate in the AHCIP and the Hospitalization Benefits Plan by filing a declaration with the Minister stating an intention to opt out. A declaration to opt out takes effect on the day it is filed and remains in effect for 36 months or until the declaration is revoked by the individual. A new declaration is required every 36 months of non-participation.
As of March 31, 2024, there were 5,333,327 Alberta residents registered with the Ministry of Health for coverage through the AHCIP and the Hospitalization Benefits Plan, and a total of 257 Alberta residents were opted out of the AHCIP and the Hospitalization Benefits Plan.
3.2 Other categories of individuals
Under the Alberta Health Care Insurance Regulation, a person may be deemed a resident for the purpose of AHCIP coverage if they are residing in Alberta to work, study, or are the spouse, partner or dependant of a person who is here to work or study. A similar provision exists in the Hospitalization Benefits Regulation whereby a person who is in full-time attendance at an educational institute, but whose ordinary place of residence is outside of Canada, is deemed to be a resident and eligible to receive Hospitalization Benefits Plan coverage if they intend to remain in Alberta for a period of 12 consecutive months. A Canada entry document such as a Work Permit or Study Permit, is required as proof of their legal entitlement to be, and remain, in Canada. Dependants accompanying temporary residents on a Work or Study Permit must have a Visitor Record (that limits the length of stay) as proof of their legal entitlement to be, and remain, in Canada. Deemed residents must intend on residing in Alberta for 12 months or more. AHCIP coverage is provided to temporary residents and their accompanying dependants who meet all of the eligibility requirements. There were 161,790 people covered by the AHCIP under these conditions as of March 31, 2024.
Individuals who hold a Study Permit that does not indicate a school in Alberta are required to provide proof of registration from the accredited school they are attending. Open or employer-specific Work Permits must be valid for six months or more. Employer-specific Work Permits must state that a company operating in Alberta employs the individual. With the exception of clergy, athletes or members of the British army, individuals with a Visitor Record must be the spouse, partner, or dependant of an eligible resident or deemed resident.
Individuals with a Canada Entry Document that has the remark 'does not confirm resident status', are not eligible for AHCIP coverage. Permanent residents who have proof of permanent resident status and Convention refugees who have a positive Notice of Decision letter are eligible for AHCIP coverage. Refugee claimants are not eligible.
Children of non-entitled residents (e.g., residents on a Visitor Record, with expired permits, or refugee claimants) who were born in Canada and meet residency requirements are eligible for AHCIP and Hospitalization Benefits Plan coverage. Children born to Canadian citizens who are temporarily absent from Alberta (and have maintained their coverage) are also eligible; however, documentation may be required.
Seasonal workers from outside Canada are considered temporary foreign workers. To obtain AHCIP and Hospitalization Benefits Plan coverage, they must meet the definition of deemed resident, have a Work Permit as proof of their legal entitlement to be, and remain, in Canada and intend on residing in Alberta for 12 months or more. Seasonal workers from other provinces retain health coverage from their home province.
Returning Canadians whose Alberta residency has expired must provide evidence of their legal entitlement to be, and remain, in Canada (typically a permanent resident card) and meet residency requirements to be eligible for AHCIP and Hospitalization Benefits Plan coverage. Individuals who have applied for permanent resident status must maintain legal entitlement to be, and remain in Canada, (e.g., a valid Work Permit, Study Permit or Visitor Record) while they await a decision on the permanent resident application. During this period, AHCIP and Hospitalization Benefits Plan coverage may be granted if they meet the eligibility requirements for a deemed resident.
On March 28, 2022, the Government of Alberta established the Ukrainian Evacuee Temporary Health Benefits Program (UETHBP) through a Ministerial Order to provide temporary medical, hospital, health, and supplemental benefits to Ukrainian evacuees who have entered or remained in Canada and Alberta due to armed conflict in the Ukraine, until they qualified or enrolled for coverage under a public (e.g., the AHCIP and the Hospitalization Benefits Plan) or private health insurance, and supplemental benefit plan. Notwithstanding a Ukrainian evacuee's eligibility for AHCIP and Hospitalization Benefits Plan coverage, all evacuees who have entered Canada and Alberta under the federal government's Canada-Ukraine Authorization for Emergency Travel Visa program are eligible to receive temporary health insurance coverage under the UETHBP if they reside in Alberta. As of March 31, 2024, approximately 53,000 Ukrainian evacuees were receiving temporary medical, hospital, health and supplemental benefits under the UETHBP.
4.0 Portability
4.1 Minimum waiting period
Under the Alberta Health Care Insurance Plan (AHCIP) and the Hospitalization Benefits Plan, generally, persons moving permanently to Alberta from another part of Canada are eligible for coverage on the first day of the third month following the date they establish residency in Alberta.
4.2 Coverage during temporary absences in Canada
The AHCIP provides coverage under the Alberta Health Care Insurance Regulation for eligible Alberta residents who temporarily leave Alberta for other parts of Canada. There is a similar provision in the Hospitalization Benefits Plan for coverage for insured hospital services.
A person is considered temporarily absent from Alberta if the person stays in another province or territory for a period that does not exceed 12 consecutive months and where the person intends to return to and maintain permanent residence in Alberta on the conclusion of their stay outside Alberta. Albertan students who attend an accredited school in Canada, and who intend to return to Alberta after completing their studies, maintain their AHCIP and Hospitalization Benefits Plan coverage.
Temporary foreign workers who are deemed residents retain their AHCIP coverage if they travel to another Canadian province for vacation; however, they do not retain their coverage if they leave Alberta to work in another province or if they leave Canada.
Individuals who are routinely absent from Alberta every year normally must spend a cumulative total of 183 days in a 12-month period in Alberta to maintain continuous coverage. Individuals not present in Alberta for the required 183 days may be considered residents of Alberta if they satisfy the Ministry of Health of their permanent and principal place of residence within the province. Individuals may also remain eligible for coverage if, on a recurring basis, they are absent from Alberta for up to 212 days in a 12-month period for the purpose of vacation.
The Ministry of Health participates in Interprovincial Hospital and Medical Reciprocal Billing Agreements. All provinces and territories participate in Hospital Reciprocal Agreements, and all provinces and territories, except Quebec, participate in Medical Reciprocal Agreements. These agreements were established to minimize complex billing processes and to help ensure timely payments to physicians and hospitals when they provide services to residents from other provinces or territories. Under the agreements, where an eligible Albertan receives an insured physician service or hospital service in another participating province or territory, Alberta will reimburse for the insured service provided at the host province's or territory's rates for medical services and the applicable rate for hospital services.
In 2023-2024, no amendments were made to the legislation regarding portability within Canada. More information on coverage during temporary absences outside Canada is available online.
Section 16(1)(a) of the Hospitalization Benefits Regulation addresses payment for goods and services provided outside of Alberta but in Canada to in-patients and out-patients in hospitals. Section 4 of the Medical Benefits Regulation addresses payment of medical services provided by a physician outside of Alberta but within Canada. These sections were not amended in 2023-2024.
4.3 Coverage during temporary absences outside Canada
Pursuant to the Alberta Health Care Insurance Regulation, eligible Alberta residents who are temporarily absent from Canada are covered through the AHCIP. There is a similar provision in the Hospitalization Benefits Regulation.
A person is considered to be temporarily absent from Alberta if the person stays outside Canada for a period that does not exceed six consecutive months, and the person intends to return to and maintain permanent residence in Alberta on the conclusion of their stay outside Alberta.
Individuals who are routinely absent from Alberta every year normally must spend a cumulative total of 183 days in a 12-month period in Alberta to maintain continuous coverage. Exceptions may be considered by the Ministry of Health depending on the individual circumstance. Individuals may also remain eligible for coverage if, on a recurring basis, they are absent from Alberta for up to 212 days in a 12-month period for the purpose of vacation.
Individuals leaving the province temporarily on extended vacations, or for temporary employment, may be eligible for coverage for 24 to 48 consecutive months. Students attending an accredited educational institute outside Canada on a full-time basis are entitled to coverage for the duration of their studies providing they intend to reside in Alberta at the conclusion of their studies.
The maximum amount payable for out-of-country in-patient hospital services is $100 CAD per day (not including day of discharge). The maximum hospital out-patient visit rate is $50 CAD, with a limit of one visit per day. The only exception is haemodialysis received as an out-patient, which is paid at a maximum of $591 CAD per visit, with a limit of one visit per day. Physician and dental specialist or oral surgeon services are paid according to Alberta rates as per the Schedule of Medical Benefits.
The AHCIP does not provide coverage for non-urgent health services received by Albertans when travelling in another country. Only claims for emergency physician and/or hospital services received outside of Canada are eligible for reimbursement. Section 12(2)(I) of the Alberta Health Care Insurance Regulation provides that services provided outside Canada that are available inside Canada (other than services provided in the case of an emergency resulting from an acute and unexpected illness, disease, condition or injury that requires medically required treatment without delay outside Canada) are not insured services. Similarly, section 4(2)(e.1) of the Hospitalization Benefits Regulation provides that services provided by a facility outside of Canada (other than services provided in the case of an emergency resulting from an acute and unexpected illness, disease, condition or injury that requires medically required treatment without delay outside Canada) without the prior approval of the Minister, unless the Minister directs otherwise, are not insured services.
Funding may also be available through the Out-of-Country Health Services Committee (OOCHSC). The OOCHSC reviews applications for payment of expenses for insured medical services and insured hospital services to be provided outside of Canada when:
- the resident is eligible for coverage;
- the resident has endeavored to receive the services in Canada but they are unavailable and all other options in Canada have been exhausted;
- the services are medically necessary and insured;
- the services will be provided in a manner that accords with accepted standards of practice in Alberta; and,
- the services are not part of research study or clinical trial, and are not an experimental service.
The OOCHSC is governed by the Out-of-Country Health Services Regulation when making decisions for payment of such expenses. The OOCHSC can only approve applications that satisfy the application criteria and timelines as set out in the Out-of-Country Health Services Regulation.
Decisions made by the OOCHSC can be appealed. An appeal may be submitted by an Alberta physician or dentist on behalf of the Alberta resident or by the Alberta resident to the Out-of-Country Health Services Appeal Panel (Appeal Panel). The Appeal Panel can only review the information provided in the application to the OOCHSC and cannot review any new information. The Appeal Panel has the authority to confirm, vary or substitute the OOCHSC's decision.
The OOCHSC and the Appeal Panel were established under the Alberta Health Care Insurance Regulation and continue under the Out-of-Country Health Services Regulation (Alta Reg 78/2006).
More information on coverage during temporary absences outside Canada is available online.
Section 16(1)(b) of the Hospitalization Benefits Regulation addresses payment for goods and services provided to residents of Alberta by hospitals or approved facilities outside of Canada. Section 5 of the Medical Benefits Regulation addresses payment of benefits for medical services provided to residents of Alberta by physicians outside Canada. These sections were not amended in 2023-2024.
4.4 Prior approval requirement
Prior approval is not required for elective (non-emergency) insured services in another Canadian province or territory that would be billed under the interprovincial hospital and medical reciprocal agreements. Prior application is required for elective services received in another Canadian province or territory for new and emerging procedures that are not covered under the interprovincial hospital and medical reciprocal agreements for insured services that are medically required, are not experimental, and are not available in Alberta. Prior application is also required for elective services rendered out-of-country and approval may only be given through the OOCHSC for insured services that are medically required, are not experimental, and are not available in Alberta or elsewhere in Canada.
Decisions made by the OOCHSC can be appealed. An Alberta physician or dentist on behalf of the Alberta resident or the Alberta resident may submit appeals to the Appeal Panel. The Appeal Panel reviews the application, the committee's decision, and determines whether to confirm, vary or substitute the OOCHSC decision under appeal.
5.0 Accessibility
5.1 Access to insured health services
The Government of Alberta is committed to meeting the health care needs of all Albertans. To ensure Albertans have the best possible access to primary health care services, the Ministry of Health funds Primary Care Networks (PCNs). Physicians and Alberta Health Services (AHS) are jointly responsible for PCNs through joint venture agreements. In most cases, the physicians' non-profit corporation and AHS enter into a joint venture agreement whereby they agree to operate the PCN. In a small number of cases, AHS and the physicians enter into a joint venture agreement and form a non-profit corporation to operate the PCN. In both cases, the Ministry of Health provides grant funding for the operations of the PCN.
PCNs support inter-disciplinary teams made up of family physicians and other health care professionals who deliver primary health care services for their patients. Each PCN has the flexibility to develop programs and provide services to meet the specific needs of patients. Access to health care services can be limited by geography, hours of operation, and wait times. As of March 31, 2024, there were 39 PCNs operating in Alberta. More than 4 million Albertans were enrolled in a PCN. A total of 4,515 primary care providers (including family physicians, general practitioners, pediatricians, and nurse practitioners), and the full-time equivalent of 1,714 other health care providers were registered providers in PCNs.
Announced in November, 2023 and launched in April 2024, the Government of Alberta's Nurse Practitioner Primary Care Program (NP Program) was established to help stabilize, strengthen, and improve Alberta's primary care system. The program provides publicly funded primary care services to enable Nurse Practitioners (NPs) to offer more health service choices to Albertans and their communities. Through the creation of the NP Program, NPs will be paid to practice comprehensive primary care and operate their own independent clinics, or practice independently in a team-based care setting. They will offer services based on their scope of practice, training and expertise. This will add much-needed capacity to the primary health care system and give Albertans more options to access the care they need. The program is currently accepting applications from eligible NPs, and it is expected that that NPs practicing under this new funding model will begin seeing patients in fall 2024.
Section 9(1) of the Alberta Health Care Insurance Act (AHCIA) prohibits extra-billing by opted-in physicians or dentists [i.e., physicians and dentists participating in the Alberta Health Care Insurance Plan (AHCIP)]. No physician or dentist who participates in the AHCIP and who provides insured services to a resident with coverage under the AHCIP is allowed to charge or collect from any person an amount in addition to the benefits payable by the Minister of Health for those insured services. Section 9(1.1) of the AHCIA contains a similar prohibition for persons referred to in section 20.1 of the AHCIA.
Section 11 of the AHCIA prohibits any person from charging or collecting from any person the following payments, where the amount is in addition to the benefits payable by the Minister of Health for the insured service:
- an amount for any goods or services that are provided as a condition to receiving an insured service provided by a physician or dentist who is participating in the AHCIP; or
- an amount the payment of which is a condition to receiving an insured service provided by a physician or dentist who is participating in the AHCIP.
When an individual questions extra-billing or user charges, they may contact the Ministry of Health staff by mail, phone, fax, or e-mail as follows:
Alberta Health
Attention: Alberta Health Care Insurance Plan
PO Box 1360, Stn Main
Edmonton AB T5J 2N3
Phone: Edmonton: 780-427-1432; Toll free in Alberta: 310-0000 then 780-427-1432
Fax: 780-422-0102
E-mail: health.ahcipmail@gov.ab.ca
(This email address is for general information or non-personal questions regarding the AHCIP)
If the matter cannot be resolved with the physician or dentist through communication or education, it may proceed to a compliance review.
The Ministry of Health monitors and enforces compliance with the AHCIA through a dedicated compliance unit. The unit reviews billing compliance, recovers inappropriately paid funds, and educates on appropriate billing practices. These reviews are conducted pursuant to section 18 of the AHCIA. If a compliance review uncovers evidence of non-compliance with sections 9 or 11 of the AHCIA, then sections 9, 11, 12, 13, and 14 set out the fines and other steps that may be taken by the Minister of Health.
Sections 9(2), 9(2.1), and 9(3) set out the escalating disciplinary actions the Minister may take in response to extra-billing, in addition to any actions taken under sections 13 and/or 14.
Section 11(3) authorizes the Minister to recover from any person who receives a prohibited fee, that amount in a civil action in debt. Where the Minister recovers an amount pursuant to section 11(3), section 11(4) requires the Minister to reimburse the recovered amount to the person who was charged the amount.
Section 12(1) establishes that a physician or dentist who is opted into the AHCIP and provides insured services in circumstances where the physician or dentist knows, or reasonably ought to have known, that a person has been charged an amount in contravention of section 11 shall not receive payment of benefits from the Minister for those insured services. Section 12(1.1) contains a similar prohibition on receiving benefits for a person referred to in section 20.1. Section 12(2) then provides that if benefits have been received in contravention of sections 12(1) or 12(1.1), the sanctions set out in section 9(2) of the AHCIA apply.
Section 13 of the AHCIA sets out the Minister's right to recover amounts received in contravention of sections 9, 10, or 12 by one or more of the following means:
- by withholding those amounts from any benefits payable to the physician, dentist or person referred to in section 20.1;
- by civil action as though those amounts were a debt owing to the Crown in right of Alberta; or,
- pursuant to any agreement between the Minister and the physician, dentist or person referred to in section 20.1 that provides for the repayment of those amounts.
Section 13(3) provides that the Minister must reimburse a person in respect of whom benefits may be paid for any amounts recovered under section 13 that were paid by the person and have not been previously reimbursed.
Section 14 provides that a contravention of sections 9, 10, 11, or 12 is an offence and subject to the fines set.
Membership-based or concierge service clinics potentially restrict access to insured health services. The clinics often provide both insured and uninsured services and charge a fee (annual membership or subscription) for access to the clinic's physicians and other practitioners. The Ministry of Health is currently undertaking a Knowledge of Business project which will inform an audit of clinics operating under these business models. The audits began in early 2024. The Ministry of Health is also reviewing relevant legislation and conducting research on how other jurisdictions are managing similar clinics. The legislation review, jurisdictional research, and audit findings will inform any legislative or regulatory changes that may be required.
To ensure Albertans have access to safe and appropriate health care services, Alberta's Ministry of Health committed to expanding virtual care and digital solutions. Health Canada supports part of this work under a bilateral agreement for approximately $16 million, and an agreement with Canada Health Infoway for $2 million.
The Ministry of Health has identified four strategic priorities for virtual-care delivery in Alberta:
- establish the Provincial eHealth Strategy, inclusive of virtual care;
- expand MyHealth Records information and capabilities;
- development of secure messaging and collaboration services; and,
- develop a privacy and security framework for virtual care.
Health infrastructure is critical to ensuring current and future health care needs are met. The Ministries of Health and Infrastructure, along with AHS, share responsibility for planning and management of Alberta's Health Capital Plan and projects.
The Ministry of Health is responsible for setting strategic directions and implementing health policy, legislation, standards and providing global operating funding to AHS. AHS identifies and prioritizes health service needs requiring capital development. The Government of Alberta supports health infrastructure by funding capital development including capital maintenance and renewal of existing health facilities.
The Ministry of Infrastructure is responsible for the design, construction and delivery of major health capital projects throughout the province. The Ministry of Health provides capital grants to expand continuing care capacity by supporting the development of continuing care spaces for Indigenous, private and not-for-profit organizations, typically through competitive capital grant programs that incentivize infrastructure development in line with strategic needs while ensuring best value for money. The Regional Health Authorities Act and the Hospitals Act also stipulate requirements for the purchase and disposition of assets and properties and the general provisions for health infrastructure.
The Budget 2023 Capital Plan dedicated $4.2 billion over three years to move forward with a number of capital projects, including $237 million to develop additional surgical capacity under Alberta Surgical Initiative program; $84.7 million over three years for the redevelopment of emergency, mental health ICU and laboratory services at the Peter Lougheed Centre (Calgary); $104.7 million to upgrade medical device reprocessing facilities, enhancing sterilization and safety standards; and $529.4 million to maintain and renew health facilities across the province as part of the Capital Maintenance and Renewal Program.
In addition, Budget 2023 provided continued support for ongoing projects, including $69.5 million over three years for the Provincial Pharmacy Central Drug Production and Distribution Centre, $90.6 million over three years for The Norwood Tower at the Gene Zwozdesky Continuing Care Centre, $166.4 million over two years to complete the Calgary Cancer Centre, $320.6 million over three years for the redevelopment and expansion of the Red Deer Regional Hospital Centre, and several other Health capital projects.
5.2 Physician compensation
The AHCIA governs the payment of claims of benefits for the provision of insured medical services by physicians to eligible Alberta residents. In Alberta, the College of Physicians and Surgeons of Alberta (CPSA) enforces standards of practice for physicians charging for uninsured professional services (services which are not insured under the AHCIA), which include rules related to block fees billed by physicians. (i.e., defined by the CPSA as a fixed fee for all designated uninsured services provided during a specified time period).
Under the Oral and Maxillofacial Surgery Benefits Regulation (Alta Reg 86/2006), benefits are payable in accordance with the regulations under the AHCIA for oral and maxillofacial surgery services provided to a resident of Alberta by a dentist.
Physicians are compensated through the AHCIP on a volume-driven, fee-for-service basis or through the use of alternative to fee-for-service compensation models, which are authorized by section 20 of the AHCIA. Examples of alternative compensation models include Clinical Alternative Relationship Plans (ARPs), and Alberta Academic Medicine and Health Services Program master agreements. Some primary care physicians are compensated through a "Blended Capitation Model" which allows physicians to submit certain fee-for-service claims and receive capitation payments though a Clinical ARP.
Clinical ARPs and the Alberta Academic Medicine and Health Services Program master agreements provide alternative compensation models to the traditional fee-for-service basis of compensation. Their purpose is to enhance physician recruitment and retention, team-based approaches to service delivery, access to services, patient satisfaction, and value for money. They also support innovative health care delivery, which will result in better health outcomes. The more predictable funding provided through Clinical ARPs and the Alberta Academic Medicine and Health Services Program master agreements enables physician groups to recruit new physicians and retain their services to support service delivery.
Through Clinical ARPs, the Minister compensates physicians for delivering a defined set of insured medical services to a specific patient population (e.g., people diagnosed with Chronic Obstructive Airways Disease).
There are two Alberta Academic Medicine and Health Services Program master agreements, which include the University of Alberta in the "north sector" master agreement and the University of Calgary in the "south sector" master agreement. The master agreements are multi-party, including the Minister of Health, AHS, the participating physicians, and the respective university. The master agreements include accountability and reporting requirements for AHS, the universities, and the participating physicians. Key performance themes include clinical service delivery, administration and leadership, research productivity, and educational quality. These themes are used to measure performance on an annual basis.
The Government of Alberta and the Alberta Medical Association (AMA) have a long-standing relationship in the form of formal agreements. The Ministry of Health continues to work with physicians and the AMA to address common interests such as quality of care, health care system sustainability, and stability of physician practices. In October 2022, an agreement was executed between the Ministry of Health and the AMA regarding matters relating to compensation for medically required services provided by physicians, and support programs to benefit physicians. The agreement covers the period of April 1, 2022, to March 31, 2026, and outlines annual increases to the rates of benefits payable to physicians on a fee-for-service basis (payable through the Schedule of Medical Benefits) or on an alternative to fee-for-service basis (e.g., through ARPs for providing insured services). The agreement also provides for the continuance or establishment of various physician support programs with associated budgets; and, outlines various initiatives to review existing physician support programs and budgets over the term of the agreement.
To ensure accountability with the AHCIA, the Ministry of Health conducts regular reviews of claims for benefits filed by physicians for their compliance with the AHCIA. The Ministry of Health uses statistical and risk assessment methodologies to identify errors or issues in the claims for benefit that were paid under the AHCIP. Compliance reviews can be initiated for a practitioner or group of practitioners to determine compliance with specific legislative or contractual requirements. Further, a compliance review may be triggered by a specific complaint about a physician from an external party.
5.3 Payments to hospitals
Alberta's public hospitals are operated by boards, which means the corporate body or person that owns or operates a hospital, and includes a regional health authority (i.e., AHS). AHS or non-profit organizations under service agreements with AHS, operate Alberta's public hospitals in accordance with the Hospitals Act and regulations. The Health Facilities Act (HFA) prohibits the operation of private hospitals.
The Regional Health Authorities Act governs the funding of AHS, Alberta's single regional health authority. The Ministry of Health funds AHS through base operating funds provided twice each month. AHS determines funding for individual hospitals and the facility fees for operators of CSFs that are contracted by AHS to provide insured surgical services.
The Hospitals Act and the HFA govern the provision of insured and uninsured surgical services performed in public hospitals and CSFs. The HFA prohibits queue jumping for insured surgical services. Specifically, no person shall give or accept any money or other valuable consideration, pay for or accept payment for enhanced medical goods or services or non-medical goods or services, or provide an uninsured surgical service for the purpose of giving any person priority for the receipt of an insured surgical service. Access to insured surgical services is based on the medical needs of patients and determined by physicians and dentists.
The Minister of Health must approve any proposed service agreement between an operator of a CSF and a regional health authority (i.e., AHS) in order for insured surgical services to be provided in the operator's CSF. The CSF must also be designated by the Minister and accredited by the CPSA.
According to the HFA, the Minister may not approve a proposed agreement between a regional health authority (i.e., AHS) and a CSF operator unless:
- the Minister of Health is satisfied:
- that the provision of insured surgical services as contemplated under the proposed agreement would be consistent with the principles of the Canada Health Act;
- that the proposed agreement indicates performance expectations and related performance measures for the insured surgical services and facility services to be provided; and
- that the proposed agreement contains provisions showing how physicians' compliance with the following will be monitored:
- the Health Professions Act (HPA) and regulations under the HPA;
- the bylaws of the CPSA; and,
- the code of ethics and standards of practice adopted by the council of the CPSA under the HPA.
- the Minister has considered the assessment of the proposed agreement with respect to the factors referred to in section 8(1.1). Pursuant to section 8(1.1), the Minister, or a person designated by the Minister, must assess the proposed agreements against certain factors:
- access to insured surgical services in Alberta;
- quality of care;
- cost effectiveness and other economic considerations in Alberta; and,
- any other factors the Minister considers appropriate.
Pursuant to the terms of the agreement between the regional health authority (i.e., AHS) and the operator of the CSF, the regional health authority agrees to pay the operator a "facility fee". This fee covers the overhead costs of the facility, such as equipment and staffing. Physicians who provide insured surgical services to patients within an accredited CSF submit claims for benefits through the AHCIP. The benefits claimed and paid to the physician are the same regardless of whether the physician provides the insured surgical service in a public hospital setting or in a CSF.
6.0 Recognition given to federal transfers
The Government of Alberta publicly acknowledged and reported the federal contribution provided through the Canada Health Transfer in various public documents, including:
- Budget 2023 – Fiscal Plan;
- 2023-2024 Government of Alberta Annual Report; and,
- Health 2023-2024 Annual Report.
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 1. Number as of March 31st | 4,783,609 | 4,825,270 | 4,913,180 | 5,106,110 | 5,333,327 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| Public facilities | |||||
| 2. Number | 228 | 228 | 231 | 231 | 231 |
| 3. Payments for insured health services ($) | not available | not available | not available | not available | not available |
| Private for-profit facilities | |||||
| 4. Number of private for-profit facilities providing insured health services | not available | not available | not available | not available | not available |
| 5. Payments to private for-profit facilities for insured health services ($) | not available | not available | not available | not available | not available |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 6. Total number of claims, in-patient | 5,872 | 4,479 | 4,956 | 4,951 | 5,145 |
| 7. Total payments, in-patient ($) | 45,985,705 | 34,951,536 | 43,435,985 | 46,820,271 | 59,694,402 |
| 8. Total number of claims, out-patient | 124,744 | 108,778 | 124,788 | 109,168 | 105,631 |
| 9. Total payments, out-patient ($) | 46,258,409 | 38,124,525 | 38,535,537 | 38,219,646 | 40,436,208 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| Pre-approved | |||||
| 10. Total number of claims, pre-approved in-patient | 3,225 | 622 | 1,062 | 1,674 | 1,878 |
| 11. Total payments, pre-approved in-patient ($) | 307,394 | 61,787 | 103,693 | 166,244 | 185,866 |
| 12. Total number of claims, pre-approved out-patient | 3,287 | 457 | 715 | 1,515 | 1,662 |
| 13. Total payments, pre-approved out-patient ($) | 345,422 | 31,455 | 104,682 | 262,768 | 236,212 |
| Non Pre-approved | |||||
| 14. Total number of claims, non pre-approved in-patient | not available | not available | not available | not available | not available |
| 15. Total payments, non pre-approved in-patient ($) | not available | not available | not available | not available | not available |
| 16. Total number of claims, non pre-approved out-patient | not available | not available | not available | not available | not available |
| 17. Total payments, non pre-approved out-patient ($) | not available | not available | not available | not available | not available |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 18. Number of participating physiciansFootnote 5Footnote 6 | 10,618 | 10,631 | 10,816 | 11,085 | 11,435 |
| 19. Number of opted-out physiciansFootnote 7 | 0 | 0 | 0 | 0 | 0 |
| 20. Number of non-participating physicians | 2 | 2 | 2 | 4 | 6 |
| 21. Total payments for services provided by physicians paid through all payment methods ($) | not available | not available | not available | not available | not available |
| 22. Total payments for services provided by physicians paid through fee-for-service ($) | 3,947,765,122 | 3,625,400,111 | 4,035,008,312 | 4,292,864,026 | 4,687,655,606 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 23. Number of services | 726,338 | 597,064 | 684,248 | 599,987 | 901,515 |
| 24. Total payments ($) | 35,406,860 | 27,115,215 | 30,346,947 | 30,795,005 | 31,133,669 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| Pre-approved | |||||
| 25. Number of pre-approved services | 19,339 | 2,450 | 5,133 | 9,057 | not available |
| 26. Total pre-approved payments ($) | 1,653,886 | 201,756 | 463,970 | 716,878 | not available |
| Non Pre-approved | |||||
| 27. Number of non pre-approvedservices | not available | not available | not available | not available | not available |
| 28. Total non pre-approvedFootnote 3 payments ($) | not available | not available | not available | not available | not available |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 29. Number of participating dentists | 219 | 182 | 189 | 166 | 147 |
| 30. Number of opted-out dentistsFootnote 10 | 0 | 0 | 0 | 0 | 0 |
| 31. Number of non-participating dentistsFootnote 10 | 0 | 0 | 0 | 0 | 0 |
| 32. Number of services provided | 46,593 | 49,024 | 60,568 | 68,114 | 74,663 |
| 33. Total payments ($) | 13,967,172 | 15,344,493 | 18,952,367 | 21,482,596 | 23,162,300 |
|
|||||
British Columbia
British Columbia (BC) has a progressive and integrated health care system, which includes a health care insurance plan that provides publicly funded health care services to residents of BC in accordance with the guiding principles of the Canada Health Act. The BC Ministry of Health has overall responsibility for ensuring that quality, appropriate, and timely health care services are available to all BC residents.
This report provides information on BC's publicly funded health system for the period of April 1, 2023, to March 31, 2024. To read more about BC's publicly-funded health system, please refer to the BC Ministry of Health's 2023-2024 – 2025-2026 Service Plan.
1.0 Public administration
1.1 Health care insurance plan and public authority
The Ministry of Health (the Ministry) is obligated under the Medicare Protection Act (MPA) to preserve a publicly managed and fiscally sustainable health care system for British Columbia (BC), and to support access to necessary medical care based on need and not the individual's ability to pay. The Ministry has overall responsibility for ensuring that health services meet the needs of all in BC, through accessible services no matter where you are in the province, and to support timely, high-quality, appropriate, equitable, and cost-effective service delivery. While the Ministry has overall responsibility for the province's health authorities, the health authorities are the organizations primarily responsible for health service delivery. Five regional health authorities deliver a full continuum of health services to meet the needs of the population within their respective geographic regions pursuant to the Health Authorities Act. A sixth health authority, the Provincial Health Services Authority (PHSA) governed by the Societies Act, is responsible for provincial clinical policy, the delivery of provincial clinical services, provincial commercial services, and provincial digital and information management and information technology planning and services.
The Ministry works in partnership with the First Nations, Métis, and urban Indigenous organizations to address the gaps in health outcomes for Indigenous Peoples in BC. The Ministry's relationships with the First Nations Health Authority (FNHA) and the First Nations Health Council have been in place for more than a decade. The FNHA supports the health and wellness of First Nations people in BC, and is responsible for planning, management, service delivery, and funding of First Nations health programs, in partnership with First Nations communities in BC. FNHA receives federal funding to administer the First Nations Health Benefits program, which covers health-related services and supports for BC First Nations to meet medical and dental needs not funded under the Canada Health Act; coverage is provided through partnerships with Pacific Blue Cross, BC PharmaCare, First Nations, and Indigenous Services Canada. The Ministry also works with Métis Nation BC, as demonstrated through the Métis Nation Relationship Accord II (2016), and the BC Association of Aboriginal Friendship Centres, to support the health and wellness of Métis, urban First Nations, and Inuit Peoples in the province. The Ministry recognizes that the implementation of BC's Declaration on the Rights of Indigenous Peoples Act (Declaration Act) is an evolving conversation from the perspectives of the health authorities, the Government of British Columbia, First Nations, Métis, and Inuit People. Relationship building with the acknowledgement of rights holders must be a basic understanding across government, demonstrated through evolving and existing partnerships, and by establishing new pathways where needed and agreed upon. Underpinning this is the ongoing work across health authorities and with other key partners to address Indigenous-specific racism through the recommendations of the In Plain Sight Report.
The BC Medical Services Plan (MSP), which is managed by the Medical Services Commission (MSC) on behalf of the Government of British Columbia, provides health care coverage (including for diagnostic services) to beneficiaries and corresponding payments to medical and health care practitioners.
MSP is administered pursuant to the Medicare Protection Act (MPA). The purpose of the MPA is to preserve a publicly managed and fiscally sustainable health care system for BC, in which access to necessary medical care is based on need and not on an individual's ability to pay. It expressly incorporates the principles of the Canada Health Act.
The MSC reports to the Minister of Health (the Minister), in accordance with the MPA. Under the MPA, the function and legislative mandate of the MSC is to facilitate reasonable access, throughout BC, to quality medical care, health care, and prescribed diagnostic services for British Columbians.
The MSC is a nine-member statutory body comprised of three representatives of the Government of British Columbia, three representatives from the Association of Doctors of BC (known as the Doctors of BC), and three members from the public who have been jointly nominated by the Doctors of BC and the Government of British Columbia to represent beneficiaries.
General hospital services are publicly funded in BC under the Hospital Insurance Act, the Hospital Insurance Act Regulations, the Hospital Act, and the Hospital District Act.
Medically required laboratory services (including in-patient and out-patient laboratory testing) are administered and provided under the Laboratory Services Act (LSA). The Minister is responsible for all matters related to laboratory services (including test review and facility approval processes), governance, accountability, and provision of benefits for all laboratory services in BC. Since the 2015 enactment of the LSA, the Ministry has delegated the delivery of several operational functions (under the LSA) to Provincial Laboratory Medicine Services (previously the BC Agency for Pathology and Laboratory Medicine), a program under the PHSA. The PHSA's mandate is to provide effective provincial oversight, which includes provincial planning, coordination, monitoring, evaluating, and reporting on province-wide results and health outcomes for publicly funded laboratory and pathology services.
The Laboratory Services Regulation (under the LSA) was amended twice in 2023-2024 to expand the range of health professionals and health care organizations that are permitted to order laboratory tests that are covered as benefits under the LSA. On June 19, 2023, amendments were made enabling registered psychiatric nurses and registered nurses in certified practice to order certain laboratory tests as benefits under the LSA, to support the diagnosis of opioid use disorder, and the prevention and management of communicable diseases. Further amendments were made on December 11, 2023, allowing the PHSA to order specified laboratory tests for the purposes of cervical and colon cancer screening.
The Medical and Health Care Services Regulation (under the MPA) was also amended on June 19, 2023, to support the diagnosis of opioid use disorder, in parallel with the Laboratory Services Regulation changes. The amendments to the Medical and Health Care Services Regulation allow registered psychiatric nurses and registered nurses in certified practice to request medically necessary diagnostic services associated with their scope of practice as benefits under the MPA.
In addition, regulatory amendments were made effective March 6, 2024, to introduce digital options into processes under the Laboratory Services Regulation. As a result of the amendments, individuals responding to regulatory actions taken under the LSA may participate in hearings electronically rather than in person, if agreed to by the Minister.
1.2 Reporting relationship
The Ministry provides information on the performance of BC's publicly-funded health care system in its Annual Service Plan Report, with the 2023-2024 Annual Service Plan Report being the relevant publication for this reporting period. The Annual Service Plan Report is released with the Public Accounts by August 31 annually. Tracking and reporting this information is consistent with the Ministry's strategic approach to performance planning and reporting, and it is consistent with requirements contained in the provincial Budget Transparency and Accountability Act. Service Plans and Annual Service Plan Reports can be located on the Government of BC website for the Ministry of Health.
The MSC is accountable to the Government of British Columbia through the Minister. The MSC Annual Report, which provides an annual accounting of the business of the MSC, its advisory committees and other delegated bodies, is published annually for the prior fiscal year.
Regional health authorities and the PHSA have independent boards; however, health authority boards are accountable to the public through the Minister, report to the Minister for required stewardship purposes, and are required to follow directions from the Minister. Each health authority board chair receives a mandate letter from the Minister, which is posted publicly on the health authority's website. Health authority board members are required to sign the health authority's mandate letter, which sets out overarching principles relevant to the entire public sector and the Minister's specific directions on priorities and expectations for each health authority.
The FNHA is not a regional health authority and does not receive a mandate letter due to the unique BC First Nations governance partnership with the Government of British Columbia. Instead, the Ministry and FNHA collaborate from a position of mutual accountability, expectations for work and accountabilities of both the FNHA and the Ministry with respect to the planning, administration, delivery, and monitoring of health services that support First Nations health and wellness in BC.
1.3 Audit of accounts
The Ministry's accounts and financial transactions are subject to audit as follows:
- Internal Audit and Advisory Services, the Government of British Columbia's internal auditor, determines the scope of the internal audits and timing of the audits. Internal Audit and Advisory Services reports can be located on the Government of BC website.
- The Office of the Auditor General (OAG) of BC is responsible for conducting annual financial audits, as well as special audits and reports. The OAG reports its findings to the Legislative Assembly. The OAG initiates its own audits and determines the scope of its audits. The Select Standing Committee on Public Accounts of the Legislative Assembly reviews the recommendations of the OAG.
The OAG's annual audit of the Ministry's accounts and financial transactions are reflected in the OAG's overall review and opinion related to the BC Public Accounts, and can be found on the Government of BC website. The OAG's special audits and reports can be located on the Office of the Auditor General of BC website.
1.4 Designated agency
Since 2005, the Ministry has contracted with service providers to deliver many of the administrative operations of MSP (the province's medical insurance plan) and PharmaCare (the province's drug insurance plan), including responding to inquiries from the public, registering clients and processing medical and pharmaceutical claims from health professionals. These administrative operations are delivered under the Health Insurance BC (HIBC) program, with third parties contracted to operate HIBC. HIBC processes payments for health care services in accordance with payment schedules approved by the MSC and for drug benefit and pharmacy services claims under the Pharmaceutical Services Act. Policy and decision-making functions for these services remain the responsibility of the Ministry.
From 2005 to 2023, HIBC was operated by MAXIMUS Canada under a series of contracts that concluded at the end of the 2022-2023 fiscal year. In August 2022, PBC Solutions Limited (a subsidiary of Pacific Blue Cross Health Benefits Society) was awarded the contract to operate HIBC. The transition from MAXIMUS Canada to PBC Solutions Limited as the operator of HIBC occurred on May 21, 2023.
HIBC is required to comply with all applicable laws, including the:
- Ombudsperson Act;
- Business Practices and Consumer Protection Act;
- Financial Administration Act; and
- Applicable privacy and freedom of information legislation (i.e., the Freedom of Information and Protection of Privacy Act, the Personal Information Protection Act, and the equivalent federal legislation, if applicable).
2.0 Comprehensiveness
2.1 Insured hospital services
The Hospital Act and Hospital Act Regulation provide authority for the Minister of Health (the Minister) to: designate facilities as hospitals and societies as hospital societies; license private long-term care hospitals (also referred to as long-term care homes); approve the bylaws of hospitals; inspect hospitals; and appoint a public administrator. This legislation also establishes broad parameters for the operation of hospitals.
The Hospital Insurance Act and the Hospital Insurance Act Regulations entitle beneficiaries to "general hospital services", define the group of beneficiaries, and set out coverage and other provisions for hospital services. They also provide authority for the Minister to make payments to health authorities for the purpose of operating hospitals.
Medically required hospital services are publicly funded benefits. There is no scheduled or regular process to review publicly funded hospital services, as these services are intended to be inclusive.
All hospital services that were funded in 2022-2023 continued to be funded in 2023-2024.
When medically required, the following are provided as benefits to beneficiaries who are in-patients in a general hospital:
- accommodation and meals at the standard or public ward level;
- necessary nursing service;
- laboratory and radiological procedures and the necessary interpretations, together with such other diagnostic procedures as approved by the Minister in a hospital, for the purpose of maintaining health, preventing disease, and assisting in the diagnosis and treatment of illness, injury, or disability;
- drugs, biologicals, and related preparations, when administered in a general hospital;
- use of operating room, case room and anaesthetic facilities, including necessary equipment and supplies;
- routine surgical supplies;
- use of radiotherapy facilities, where available;
- use of physiotherapy facilities, where available;
- other rehabilitation services, where available; and
- other required services approved by the Minister that are provided by persons who receive remuneration from the hospital.
When medically required, the following are provided as benefits to beneficiaries who are out-patients:
- emergency department services;
- use of operating room facilities;
- equipment and supplies used in medically necessary services provided to the beneficiary, including anaesthetics, sterile supplies, dressings, casts, splints or immobilizers, and bandages;
- meals required during diagnosis and treatment;
- drugs and medications administered in a medically necessary service provided to the beneficiary; and
- any service provided by an employee of the hospital that is approved by the Minister.
When medically required, the following diagnostic services—which are specified in the Medical and Health Care Services Regulation under the Medicare Protection Act (MPA) - are provided as benefits to beneficiaries who are out-patients. Depending on the service, they may be provided at hospitals or privately-owned facilities that the Medical Services Commission (MSC) has approved to charge the public healthcare system for the service, including:
- Diagnostic Radiology, including Computerized Axial Tomography (PDF document);
- Diagnostic Ultrasound (PDF document);
- Nuclear Medicine Scanning (PDF document);
- Polysomnography (PDF document);
- Pulmonary Function (PDF document);
- Electromyography (PDF document); and
- Electroencephalography (PDF document).
Medically required in-patient and out-patient laboratory services are administered and provided as benefits under the Laboratory Services Act (LSA). Outpatient laboratory tests that are funded through the Medical Services Plan (MSP) fee-for-service payment model are listed in the Laboratory Services Outpatient Payment Schedule.
Insured hospital services are provided to beneficiaries without charge, with a few exceptions, such as:
- the incremental cost of preferred medical or surgical supplies/devices/services compared to that which is medically necessary (patients may not be charged for an "enhanced" material, device, or service, if it is provided solely because the standard item is not available at the time the related insured service is rendered);
- non-standard preferred accommodation, when provided at the patient's request (and when not medically required and standard accommodation is available);
- daily fees for long-term care patients receiving long-term care services in extended care or general (acute care) hospitals, or private long-term care hospitals licensed under Part 2 of the Hospital Act. Health authorities and hospital societies are required to follow Home and Community Care policies to determine benefits in such cases); and
- additional exceptions are listed in section 2.4 below.
In accordance with the definition of "benefits" under the MPA, diagnostic services such as magnetic resonance imaging (MRI) and computed tomography (CT) scans are insured benefits only if delivered in a facility approved by the MSC. During 2023-2024, there have been no changes to the legislation or regulations to address patient payments for services in private (not approved) diagnostic facilities.
2.2 Insured physician services
Unless specifically excluded, the following medical services are publicly funded as benefits under the MPA or the LSA:
- medically required services provided to beneficiaries (residents of BC who are enrolled with the MSP in accordance with section 7 of the MPA) by a practitioner who is enrolled with the MSP; and
- medically required diagnostic services performed in an approved diagnostic facility under the supervision of an enrolled physician.
To practise in BC, physicians must be registered and in good standing with the College of Physicians and Surgeons of British Columbia. To receive payment for publicly funded services, they must be enrolled with MSP. In the fiscal year 2023-2024, 12,983 physicians were enrolled with MSP and received payments through fee-for-service. As of March 31, 2024, 4,215 MSP-enrolled physicians have additionally enrolled in the Longitudinal Family Physician Payment Model.
The types of practitioners (in addition to physicians and dentists) who may enrol and provide benefits under MSP include midwives, optometrists, osteopaths, and supplementary benefit practitioners (e.g., chiropractors and massage therapists). Nurse practitioners are not included in this list as they enrol to get a practitioner number, but are not paid directly by MSP under the MPA. Additionally, Registered Nurses in certified practice (RN(C)), Registered Nurses (RN), Registered Psychiatric Nurses (RPN) and Registered Psychiatric Nurses in certified practice (RPN(C)) are authorized to independently refer eligible MSP beneficiaries for selected medically necessary laboratory tests approved as within scope of practice outlined by the British Columbia College of Nurses and Midwives. This program is of particular benefit to patients in communities who do not have an attendant physician or nurse practitioner, but who do have access to nursing care provided by an RN(C), RN, RPN or RPN(C). RN(C)s, RNs, RPNs and RPN(C)s do not submit billing information to MSP; they may only make referrals for approved laboratory services.
For eligible beneficiaries, the Supplementary Benefits Program provides partial payment for acupuncture, massage therapy, physiotherapy, chiropractic, naturopathy, and non-surgical podiatry services. The program contributes $23 towards the cost of each patient visit to a maximum of ten visits per patient per annum summed across the six types of providers. Eligibility for the program is based on income. Income is verified by way of an automated Canada Revenue Agency income verification process that runs once per year. Clients of the Ministry of Social Development and Poverty Reduction may be eligible to receive up to 12 additional visits per year.
Practitioners enrolled in MSP may choose to be "opted-in" or "opted-out". Opted-in practitioners bill MSP directly for MSP benefits provided to MSP beneficiaries. An opted-in practitioner may not bill a patient directly for an insured benefit. Opted-out practitioners bill patients directly for benefits. Enrolled practitioners wishing to opt out of MSP must give written notice to the MSC. In this case, beneficiaries may apply to MSP for reimbursement of the fee for benefits rendered. Under the MPA, an opted-out physician may not charge a patient more for a benefit than the prescribed MSP fee amount.
Unenrolled physicians are not registered with MSP. Consequently, services provided by a physician who is not enrolled or whose enrolment has been cancelled with MSP are not insured and are not reimbursed by MSP. By law, under the MPA, unenrolled physicians in BC may not charge patients more than the MSP amount for an insured benefit that is provided at a hospital, or community care facility, or other setting set out in the MPA.
Under the Physician Master Agreement between the Government of BC, MSC, and the Association of Doctors of BC (Doctors of BC), modifications to the MSC Payment Schedule such as additions, deletions, or fee changes are made by the MSC upon advice from Doctors of BC or the Government of British Columbia. During fiscal year 2023-2024, 41 net new types of services by physicians were added to the MSC Payment Schedule to reflect current practice standards including, for example, the introduction of eight new cardiac surgery fees, two new assist fees, three new fees related to consultations, and three new Medical Assistance in Dying (MAiD) fees.
Additionally, 57 fee items were amended and five changes were made to the preamble or the overall MSC Payment Schedule in fiscal 2023-2024 to provide clarity regarding re-referrals, to include the new statutory holiday for Truth and Reconciliation, and to change the title of the Specialist Services Committee to the Consultant Specialists.
Further, as part of the MSP's monitoring program, eight reviews resulted in the provisional status for the fees being removed, and six reviews resulted in the provisional status being extended to allow for further monitoring.
Also, in response to and planning for the COVID-19 pandemic, amendments to the MSC Payment Schedule were made in 2019-2020, 2020-2021, 2021-2022 and 2022-2023 on a temporary basis to support access to physician services during the pandemic, including virtual care and immunizations. These amendments are still in place.
Temporary fee changes include:
- amending wording in the General Preamble around Telehealth Services to allow the use of "face-to-face" fee codes for consultations, office visits, and non-procedural interventions where no telehealth fees exist, including for telephone calls;
- creating new fees for family physicians (FP) and specialists to support provision of virtual services and communication among practitioners;
- removing the restriction that real-time ultrasound fees may be claimed only when the physician is onsite in the diagnostic facility for the purpose of diagnostic ultrasound supervision;
- amending the list of fees eligible for the Business Cost Premium to include telehealth fees;
- allowing counselling by telephone;
- establishing age-based telehealth fees, corresponding to the existing "face-to-face" fees for FP consultations, visits, and counselling to replace the existing non-age-based telehealth fees;
- establishing fees to support respiratory (including influenza), and COVID-19 immunizations, including COVID-19 immunization advice;
- establishing a COVID-19 perioperative complexity surcharge; and
- establishing an assessment for COVID-19 therapeutics fee.
Longitudinal Family Physician Payment Schedule
Introduced on February 1, 2023, the Longitudinal Family Physician (LFP) Payment Model was developed by the Ministry in consultation with the Doctors of BC and BC Family Doctors. The LFP Payment Model is available to FPs, and their locums, who provide clinic-based, longitudinal, relationship-based, family medicine care to a known panel of patients, aligned with the attributes of a Patient Medical Home.
The LFP Payment Model includes three bases of payments: time, patient-related interactions, and the size and complexity of a physician's patient panel. Changes to the LFP Payment Model are governed by a Memorandum of Understanding between the Government of British Columbia, Doctors of BC and the MSC, and any changes are implemented by mutual agreement between these parties.
The LFP payment schedule can be found here.
2.3 Insured surgical-dental services
In certain circumstances, in-patient or out-patient hospitalization is medically required for the safe and proper completion of surgical-dental services. In such cases, the surgical-dental procedure component is publicly funded if the service falls within the meaning of covered dental or orthodontic services by the Medical and Health Care Services Regulation under the MPA. The hospitalization component is funded by the health authority. Further, dental services that are provided in privately owned/operated surgical facilities under contract with a health authority, and are listed in the Dental Payment Schedule, are insured benefits under MSP. The Medical and Health Care Services Regulation was amended in 2020 to authorize payment for oral and maxillofacial surgical services in relation to a public health emergency, and in BC a declaration of a public health emergency related to COVID-19 was in effect throughout the 2023-2024 reporting period.
Publicly funded surgical-dental procedures include those related to remedying a disorder of the oral cavity or a functional component of mastication. Generally, this includes oral surgery related to trauma, orthognathic surgery, medically required extractions, and surgical treatment of temporomandibular joint dysfunction.
The dental procedures funded by MSP are established through the negotiation of an agreement between the British Columbia Dental Association (BCDA) and the Government of British Columbia. Public consultation is not undertaken. The agreement outlines any changes to surgical-dental benefits during the term of the agreement, including any additional benefit procedures. Additions or changes to the list of benefits are managed by MSP on the advice of the Dentistry Advisory Committee, which consists of representatives from both the Ministry and the BCDA. Additions and changes to the Dental Payment Schedule must be approved by the Dentistry Special Committee (under the MPA). A new 2022-2025 agreement has been negotiated through March 31, 2025.
Any general dentist in good standing with the British Columbia College of Oral Health Professionals who is enrolled in MSP and has hospital privileges may provide surgical-dental benefits in a hospital or other approved facility. There were 196 dentists enrolled with MSP in 2023-2024 (including general dentists, pediatric dental specialists, oral surgeons, oral medicine dental specialists, and orthodontists billing through MSP).
Dentists must register with the British Columbia College of Oral Health Professionals to practise, but they are not required to participate in MSP. If they choose to participate, they must enrol in MSP to receive payment for MSP insured services. Dentists enrolling in MSP may choose to opt out of billing MSP for insured services, instead billing the patient directly. The patient may then submit a claim to MSP for reimbursement of the insured service.
2.4 Uninsured hospital, physician and surgical-dental services
Medical necessity is the criterion for public funding of hospital and medical services. Coverage is excluded for out-patient take-home drugs, and any drugs not clinically approved by the hospital. Procedures not publicly funded under the Hospital Insurance Act and Hospital Insurance Act Regulations include:
- services of medical personnel not employed, privileged, or contracted by a hospital;
- treatment for which WorkSafeBC, the Department of Veterans Affairs, or any other agency is responsible;
- services or treatment that the Minister (or a person designated by the Minister) determines, on a review of the medical evidence, the beneficiary does not require; and
- excluded illnesses or conditions (detailed in section 5.22 of the Hospital Insurance Act Regulations).
Non-publicly funded hospital services also include:
- non-standard preferred accommodation, when provided at the patient's request (and when not medically required and standard accommodation is available);
- the incremental cost of preferred medical or surgical supplies/devices/services compared to that which is medically necessary (patients may not be charged for an "enhanced" material, device, or service, if it is provided solely because the standard item is not available at the time the related insured service is rendered);
- televisions, telephones, and private nursing services;
- dental care that could safely be provided in a dental office, including prosthetic and orthodontic services; and
- other exceptions listed in section 2.1 above.
Health authorities are required by Ministry of Health policy to fund medically necessary transfers between acute care hospitals within BC, but beneficiaries (subject to an income-based exemption) are required to pay a fee to partially off-set costs when an ambulance or contracted alternative service provider is used for transport in other situations, in accordance with the Emergency Health Services Regulation under the Emergency Health Services Act.
Services not covered under MSP include:
- those covered by the Workers Compensation Act or by other federal or other provincial legislation;
- services that are deemed to be not medically required, such as cosmetic surgery solely for the alteration of appearance;
- dental services, except as outlined under benefits;
- routine eye examinations for persons 19 to 64 years of age;
- eyeglasses, hearing aids, and other equipment or appliances;
- prescription drugs (pharmaceutical coverage is provided under PharmaCareFootnote ix);
- acupuncture, chiropractic, massage therapy, naturopathy, physical therapy, and non-surgical podiatry services (except for MSP beneficiaries receiving supplementary benefits);
- preventive services and screening tests not supported by evidence of medical effectiveness (for example, routine annual "complete" physical examinations, whole body CT scans, prostate specific antigen tests, etc.);
- services of counsellors or psychologists;
- medical examinations, certificates, or tests for non-medical purposes, such as those required for:
- driving a motor vehicle;
- employment;
- life insurance;
- school or university;
- recreational and sporting activities;
- immigration purposes;
- in-vitro fertilization; and
- reversal of sterilization procedures (except when the sterilization was originally caused by trauma).
With respect to MSP, the MSC has authority to determine which services are not benefits.
Temporary hospital fee changes were made in response to COVID-19. To remove potential barriers to COVID-19 related health care in acute care hospitals during the COVID-19 health crisis, a temporary policy change in regard to insured hospital services and goods came into effect on May 21, 2020. The Temporary Amendment to Funding of Hospital Services Related to COVID-19 policy provides a fee suspension that impacts only hospital services and goods related to COVID-19 for individuals in BC who are not eligible for MSP coverage (e.g., people who have precarious immigration status), and it aligns with the MSP response to COVID-19. This temporary policy applies to all acute care hospitals in BC, and provides that:
- patients who are not eligible for MSP will not have to pay any fee for medically necessary COVID-19 treatment (i.e., services and goods) in BC hospitals; and
- hospital services and goods that are provided to non-MSP individuals for non-COVID-19 related conditions will remain uninsured.
3.0 Universality
3.1 Eligibility
Section 7 of the Medicare Protection Act (MPA) sets out the Medical Services Plan (MSP) requirement for residents of BC to enrol in MSP. A person must be a resident of BC to be eligible for provincial health care benefits.
Section 1 of the MPA defines a resident as a person who is either deemed to be a resident under regulation, or:
- is a citizen of Canada or is lawfully admitted to Canada for permanent residence;
- makes the person's home in BC; and
- is physically present in BC for at least six months in a calendar year, or for a prescribed shorter period.
"Deemed residents" include individuals such as some holders of permits issued under the federal Immigration and Refugee Protection Act (see section 3.2 of this report) among others, but this does not include a tourist or visitor to BC.
Residents who do not want to participate in the BC's public health care plan may choose to opt out of the publicly funded program. Individuals are required to file an "Election to opt out" statement and submit that statement to the Medical Services Commission (MSC). A statement, once signed, is irrevocable and results in the resident being responsible for paying the entire cost of all hospital, medical, and other health care services they may receive during the 12-month opted-out period. Residents cannot opt out retroactively and must reapply to opt out at the expiry of each 12-month period.
All residents are entitled to medically required hospital and medical care coverage. Those residents who are members of the Canadian Armed Forces and those serving a term of imprisonment in a federal penitentiary, as defined in the Corrections and Conditional Release Act, are eligible for federally funded health insurance. MSP provides first-day coverage to discharged members of the Canadian Armed Forces, as well as to released inmates of federal penitentiaries located in BC.
It is possible for a beneficiary's enrolment to be cancelled by order of the MSC, if the MSC determines that the beneficiary was not eligible for enrolment or the beneficiary has ceased to be a resident. Section 11 of the MPA requires that the beneficiary must be notified that they have a right to a hearing, prior to making an order cancelling a beneficiary's enrolment. If the beneficiary requests a hearing, the hearing is conducted by a delegate of the MSC — either in person or in writing. Decisions of the MSC or its delegates may be judicially reviewed by the Supreme Court of BC.
The number of BC residents registered with MSP, as of the end of the reporting period on March 31, 2024, was 5,847,035.
3.2 Other categories of individuals
Diplomats, holders of study permits and work permits valid for six months or longer (and accompanying spouses and children), applicants for permanent resident status who are the spouse or child of an eligible resident, and individuals who have arrived in BC under the Canada-Ukraine authorization for emergency travel are eligible for enrolment and benefits when they are deemed to be residents under the MPA in accordance with section 2 of the Medical and Health Care Services Regulation of the MPA.
3.3 Premiums
Until January 1, 2020, the MPA and the Medical and Health Care Services Regulation provided authority for the MSC to collect premiums from beneficiaries. As announced by the Government of British Columbia, and further to amendments enacted through the Medicare Protection Amendment Act, 2019, MSP premiums were eliminated for all beneficiaries effective January 1, 2020.
Retroactive premium assistance for premiums incurred prior to January 1, 2020, remains available.
Effective July 2, 2013, Health Canada transferred the funds historically used to pay MSP premiums on behalf of status First Nations residents in BC to the First Nations Health Authority (FNHA). Of this transfer, 25 per cent over the first three years was set aside by FNHA to support the development of new primary care services. The 2013 Agreement Regarding Payments in Lieu of MSP Premiums on behalf of First Nations people resident in the province of BC was successfully renegotiated in 2018, and although the Government of BC eliminated MSP premiums for British Columbians effective January 1, 2020, FNHA continues to receive annual funding from the Ministry to support these primary care services through a joint Ministry of Health-FNHA project/priorities Board.
3.4 International Student Health Fee
As the province has eliminated MSP premiums for British Columbians, an updated payment method helps to ensure international students continue to contribute to, and benefit from, BC health care coverage. Under the updated system, effective September 1, 2019, all international K-12 and post-secondary students began paying a monthly health fee of $37.50. Effective January 2020, the fee was increased to $75 per month upon the elimination of MSP premiums. International students with a study permit valid for a period of six or more months are required to apply for MSP as soon as they arrive in BC. Through this application process, they will be enrolled and then invoiced for the new health fee following the mandatory coverage wait period. Any outstanding International Student Health Fee debt is not a barrier to receiving coverage.
4.0 Portability
4.1 Minimum waiting period
New residents or persons re-establishing residence in BC are eligible for coverage after completing a waiting period that normally consists of the balance of the month in which residence is established, plus two additional months. For example, if an eligible person applies during the month of July, coverage is available October 1. If absences from Canada exceed a total of 30 days during the waiting period, eligibility for coverage may be affected. New residents from other parts of Canada are advised to maintain coverage with their former provincial or territorial health insurance plan during the waiting period.
4.2 Coverage during temporary absences in Canada
Sections 3, 3.1, 4, and 5 of the Medical and Health Care Services Regulation set out the portability provisions for persons temporarily absent from BC regarding publicly funded services.
In general terms, residents who spend part of every year outside BC must be physically present in BC at least six months in a calendar year, and continue to maintain their home in BC, to retain coverage. However, longer term vacationers may qualify for a total absence of up to seven months per calendar year for vacation purposes only, provided they give prior notice to the Medical Services Commission (MSC) and continue to meet the other requirements, such as maintaining their home in BC.
Individuals leaving BC temporarily on extended vacations, or for temporary employment, may be eligible to retain their medical coverage for up to 24 consecutive months provided they receive prior approval of the MSC and meet other requirements of section 4 of the Medical and Health Care Services Regulation. Approval is limited to once in five years for absences exceeding six months in a calendar year. When a beneficiary stays outside BC longer than the approved period, there is a requirement to re-enrol and fulfill a waiting period upon re-establishing residence in the province before coverage can begin. Students and extended family of students attending a recognized school in another province or territory on a full-time basis are entitled to coverage for the duration of their studies.
According to inter-provincial/territorial reciprocal billing arrangements, physicians in other Canadian provinces and territories, except in Quebec (QC), bill their own medical plans directly for services rendered to BC residents who are eligible for Medical Services Plan (MSP) coverage, upon presentation of a valid Personal Health Number or BC Services Card. BC then reimburses the province or territory at the rate of the fee schedule in the province or territory in which services were rendered. For in-patient hospital care, services are paid at the ward rate approved for each hospital by the Assistant Deputy Ministers Policy Advisory Committee. For out-patient services, the payment is at the inter-provincial/territorial reciprocal billing rate. Payment for these services, except for excluded services that are billed to the patient, is handled through inter-provincial/territorial reciprocal billing procedures.
QC does not participate in reciprocal billing agreements for physician services. As a result, claims for services provided to BC beneficiaries by QC physicians are handled individually. When travelling in QC (or outside of Canada), the beneficiary is usually required to pay for medical services and seek reimbursement later from the Government of British Columbia.
BC pays host provinces/territories the approved hospital billing rates and out-patient rates. These rates are recommended by the Interprovincial Health Insurance Agreements Coordinating Committee and approved by provincial-territorial Assistant Deputy Ministers or Deputy Ministers of Health.
4.3 Coverage during temporary absences outside Canada
The provisions that set out the portability of health insurance during temporary absences outside Canada are as follows: section 24 of the Hospital Insurance Act; Division 6 of the Hospital Insurance Act Regulations; sections 5.5 and 29 of the Medicare Protection Act (MPA); and sections 3–5 and 35 of the Medical and Health Care Services Regulation.
Residents who leave BC temporarily to attend school or university are eligible for MSP coverage for the duration of their studies, provided they were physically present in Canada for six of the 12 months immediately preceding departure and are in full-time attendance at a recognized educational facility. Beneficiaries who have been studying outside BC must return to the province by the end of the month following the month in which studies are completed. Any student who will not return to BC within that timeframe is encouraged to contact the MSC.
In some circumstances, while temporarily outside the province for work or vacation, an individual may be deemed an eligible resident during an 'extended absence' of up to 24 consecutive months, once in a five-year period. To qualify, an individual must obtain prior approval for status as a resident during the absence, continue to maintain their home in BC, be physically present in Canada for six of the 12 months immediately preceding departure, and have not been granted an extended absence in the previous five calendar years. In addition, they must not have taken advantage of the additional one-month absence available to vacationers during the year the extended absence begins, or during the calendar year prior to the start of the extended absence. In certain situations, if a person's employment requires them to routinely travel outside of BC for more than six months per calendar year, they can apply to the MSC for approval to maintain their eligibility.
BC residents who are temporarily absent from BC and cannot return due to extenuating health circumstances may be deemed residents for up to an additional 12 months. This also applies to the person's spouse and children provided they are with the person, and they are also residents or deemed residents.
BC residents who are eligible for coverage while temporarily absent from BC may receive reimbursement from MSP for out-of-country medical expenses. Provincial coverage for emergency medical treatment applies to a BC resident who unexpectedly requires medical care while travelling (business, pleasure, study) in another country. MSP provides coverage for out-of-country emergency physician services up to the BC physician fee rates. Reimbursement for out-of-country emergency hospital services is limited to a maximum benefit of $75 per day. Any excess cost is the responsibility of the beneficiary.
Reimbursements are made in Canadian dollars.
4.4 Prior approval requirement
No prior approval is required for medically required procedures that are covered under interprovincial reciprocal agreements with other provinces and territories. Prior approval from the MSC is required for procedures that are excluded under the reciprocal agreements.
The physician services excluded under the Interprovincial Agreements for the Reciprocal Processing of Out-of-Province Medical Claims are:
- surgery for alteration of appearance (cosmetic surgery);
- gender reassignment surgery;
- surgery for reversal of sterilization;
- routine periodic health examinations such as routine eye examinations;
- in-vitro fertilization;
- artificial insemination;
- acupuncture;
- acupressure;
- transcutaneous electro-nerve stimulation;
- moxibustion;
- biofeedback;
- hypnotherapy;
- services to persons covered by other agencies (e.g., Canadian Armed Forces, Workers' Compensation Board, Department of Veterans Affairs, Correctional Services of Canada);
- services requested by a third party;
- team conferences;
- genetic screening and other genetic investigation, including DNA probes;
- procedures still in the experimental/developmental phase; and
- anaesthetic services and surgical assistant services associated with all the foregoing.
All elective (non-emergency) procedures performed outside Canada require approval from the MSC before the procedure is performed, to be eligible for coverage under the publicly funded program. All such applications for provincial coverage are to be submitted to the Ministry of Health (the Ministry) or its designate, Health Insurance BC. The beneficiary is notified of the decision in writing.
If a decision is made to deny the application for funding, the beneficiary may request an administrative review of the denial.
If, after the administrative review is concluded, the application for funding under MSP is denied again, the beneficiary may request a review of the decision. For out-of-country applications, the review is conducted by an MSC Review Panel. The panel consists of three members—one delegate representing the Ministry, one delegate representing the Association of Doctors of BC, and one delegate representing the general public. This tripartite structure ensures that decisions affecting administration of the provincial health care system reflect the best interest of all concerned.
For out-of-province but inside Canada applications, the review is conducted by an advisory committee of the MSC.
5.0 Accessibility
5.1 Access to insured health services
The Medical Services Commission (MSC) has a legislative mandate to protect the integrity and sustainability of the health care system and uphold the Medicare Protection Act (MPA). Section 36 of the MPA gives the MSC the authority to audit private clinics for extra-billing. Extra-billing is the practice of charging beneficiaries for the Medical Services Plan (MSP) benefits, or for matters relating to the rendering of benefits.
On October 1, 2018, the Government of British Columbia brought sections of the MPA that had previously been passed by the Legislative Assembly in 2003 (Bill 92) into force. In general terms, these provisions enhance enforcement powers in relation to extra-billing to better ensure that eligible BC residents (beneficiaries) receive quality public health care based on need, not on ability to pay. These changes uphold the fundamental principles of the MPA, as well as the Canada Health Act.
Several of the MPA provisions were subject to challenge as part of the Cambie Surgeries Corp. v. British Columbia (Attorney General) litigation. On April 6, 2023, the Supreme Court of Canada denied Cambie Surgeries' application for leave to appeal, bringing this proceeding to a conclusion that upheld the validity of the challenged provisions.
Section 45 of the MPA prohibits the sale or issuance of health insurance by private insurers to patients for services that would be a publicly funded benefit. Section 17 prevents extra-billing by prohibiting persons from being charged for, or in relation to, a benefit or for "materials, consultations, procedures, use of an office, clinic or other place or for any other matters that relate to the rendering of a benefit" provided by a practitioner who is enrolled in MSP (and not opted-out).
In 2018, the MPA was amended to strengthen requirements for beneficiaries to be notified of intended charges for services that would be benefits if rendered by a practitioner who is enrolled in MSP. If notice is not provided as required, a person is not liable to pay for the service unless the service was rendered in an emergency, making it impracticable to comply with the notice requirement.
Beneficiaries, as defined in section 1 of the MPA, are eligible for medically required publicly funded health care services. To ensure equal access to all regardless of income, sections 17 and 18 of the MPA limit charges by medical practitioners in most contexts. Similarly, section 15 of the Laboratory Services Act prohibits charging beneficiaries for medically required laboratory services provided at an approved laboratory facility, materials, consultations, procedures or the use of a laboratory facility or specimen collection station, or any other matter related to the provision of a benefit. As well, sections 12 and 13 of the Hospital Insurance Act prohibit extra-billing for hospital services.
If a benefit is provided by an enrolled medical practitioner who has opted-out of MSP, any amount charged which exceeds the amount allowed under the MPA is considered extra-billing and must be refunded. The MSC may apply for an injunction restraining a person from contravening the extra-billing provisions of the MPA.
The Audit and Inspection Committee (AIC) is a panel empowered by section 6 of the MPA, which specifies that such a panel consists of 3 or more persons who represents each of the Association of Doctors of BC (Doctors of BC), beneficiaries and the government. The AIC is currently comprised of: (a) a physician to represent Doctors of BC; (b) a retired physician who represents the government; (c) a non-physician to represent beneficiaries (i.e., the public); and (d) a physician with ties to the College of Physicians and Surgeons of BC to represent beneficiaries.
The MSC has delegated its powers and duties under section 36 of the MPA (i.e., to audit and inspect medical practitioners) to the AIC. On December 1, 2006, section 10 of the Medicare Protection Amendment Act, 2003 was brought into force. This section expanded the audit and inspection powers of the MSC to include the power to audit clinics as corporate entities, rather than just physicians.
The AIC has responsibility for two types of audits: (1) patterns of practice audits which are done to ensure that services billed to MSP have been delivered and billed accurately; and (2) extra-billing audits which focus on whether beneficiaries are being charged for services in contravention of the MPA. The AIC decides whether on-site audits are appropriate, and it outlines the nature and extent of the audits. It also reviews the audit results and makes recommendations to the Chair of the MSC for further appropriate action.
The Billing Integrity Program within the Ministry of Health (the Ministry) develops and analyses practitioners' profiles, monitors trends, and conducts audits for the MSC. Where appropriate, the MSC seeks recovery of inappropriately paid monies in accordance with the MPA.
A hearing is held before a panel of three or more persons who are appointed by the MSC to represent the Doctors of BC, beneficiaries, and government. A panel has authority to make an order for recovery of money and other remedies.
The Ministry and the MSC respond to complaints of extra-billing made by patients and take appropriate actions to correct identified situations. Information regarding the extra-billing review process is available on the Government of BC website. If a beneficiary believes they have been charged inappropriately for an insured medical benefit, they can request a review by completing an extra-billing investigation form. This form is available publicly on the MSP website.
The MSC's audit powers over health care practitioners have been assigned to various special committees. A special committee for each body of health care practitioners has been established. The special committees are the Chiropractic Special Committee; the Dentistry Special Committee; the Massage Therapy Special Committee; the Naturopathy Special Committee; the Optometry Special Committee; the Physical Therapy Special Committee; the Podiatry Special Committee; the Acupuncture Special Committee; and the Midwifery Special Committee.
Each audit results in the submission of a detailed report to the individual Special Committee. Subsequently, the individual Special Committee makes recommendation to the Health Care Practitioners Special Committee for Audit Hearings to assist in determining if recovery should be pursued. Practitioners have a right to be heard before the Health Care Practitioners Special Committee for Audit Hearings makes a determination.
Further, access to publicly funded services continues to be enhanced. The Ministry's focus is on increasing access to team-based quality, comprehensive, culturally safe, and person-and-family-centered primary care for people throughout BC. To support team-based care, the Ministry has implemented or expanded alternate compensation options, in addition to other existing compensation models:
- On February 1, 2023, the Ministry in collaboration with Doctors of BC and BC Family Doctors, announced the development of a new payment model for family physicians (FPs), the Longitudinal Family Physician (LFP) payment model. This payment model is available to all FPs in BC who either are currently or want to provide longitudinal primary care, and as of March 31, 2024, over 4,215 FPs have registered for LFP payments. Work to expand the payment model is ongoing.
- The LFP payment model is part of MSP, and all FPs registered for LFP payments are enrolled with MSP. Payments under LFP are made through MSP.
- The Alternative Payments Program (APP) funds regional health authorities to contract with, or employ, FPs and/or specialists to deliver publicly funded clinical services. The Ministry's Primary Care Division and APP funds a variety of service contracts to support the delivery of primary care services, such as: the Alternative Payments Subsidiary Agreement through the Physician Master Agreement (PMA) provides the framework for clinical contract options: service contracts, salary agreements, and sessional contracts compensate FPs and/or specialists based on time.
- To support Primary Care Networks (PCNs), the Ministry worked with the Doctors of BC to support the continued roll out of the following clinical services contracts to support FPs, including:
- The New to Practice Contract supports FPs establishing a patient panel within a group practice and provides income security while they build their practice. As of March 31, 2024, 246 new FPs have registered for the program across the province.
- The group contract for practicing full-service family physicians compensates based on the time worked and provides incremental payment for the clinic's patient panel size/complexity, as well as for completing quality improvement activities. By November 2023, all the contracts were terminated, with the physicians transitioning to the LFP payment model.
- To further support PCNs, the Ministry has invested in the following:
- Funding new nursing and allied health provider positions in PCNs. In the coming years, integrated teams including nurses and allied health providers are expected to be available in approximately 99 PCNs across the province.
- As of March 31, 2024, 79 PCNs have been launched by the Ministry, covering 85 per cent of Community Health Service Areas and 90 per cent of the provincial population.
- Launching the Nurse in Primary Care Practice program enables the integration of nurses into interdisciplinary teams in family practices and expands a longitudinal and focused primary care clinic's capacity to support a fully optimized scope of practice within the clinical setting.
- In 2020, the Ministry launched a Nurse Practitioner Primary Care Clinic (NPPCC) model of care in which longitudinal team-based care and clinical leadership are provided by nurse practitioners (NPs) working on contract with health authorities. Three NPPCCs opened in 2020 in communities with significant unattached populations. As of January 2024, the clinics have attached approximately 14,650 patients. Research by the University of Victoria School of Nursing indicates that newly attached patients of these clinics experience dramatic improvements in access to care.Footnote x
- Service Contracts for FPs and NPs working at Urgent and Primary Care Centres (UPCCs) – these clinics provide a flexible resource to meet the urgent/episodic, and longitudinal primary care needs of people in communities throughout the province. As of March 31, 2024, 32 UPCCs were operating, with more planned. The target is to have 50 UPCCs operating by 2025. Since the first sites opened in 2018, as of March 31, 2024, UPCCs have collectively had 2.37 million patient visits and have attached approximately 21,920 patients.
- Service Contracts for FPs and NPs working at First Nations Primary Care Centres (FNPCCs) – these clinics deliver primary care to Indigenous patients and their families using integrated western/Indigenous approaches. The main focus is establishing a holistic relationship with First Nations patients and their families as part of the circle of care while providing care in a culturally safe environment. As of March 31, 2024, three FNPCCs are in implementation, with five more in active planning or initial service offering, and three more sites planned. The target is to have 15 FNPCCs operating by 2024-2025.
- Service Contracts for FPs and NPs working at Community Health Centres (CHCs) – CHCs are team-based, community-governed, not-for-profit, multi-sectoral health and social service organizations that deliver culturally safe primary care as well as access to social supports for priority populations. As of March 2024, nine CHCs are open and serving the public, and five CHCs are currently in planning.
- The Ministry has worked with the Ministry of Post-Secondary Education and Future Skills to increase the number of education seats available for NP students at BC's post-secondary institutions to support a team-based model of primary care and improve equitable access to primary care health services in BC. The number of NP students at BC post-secondary institutions reached 100 following the launch of the Thompson Rivers University program in 2023 (with the first students starting in May 2023) and the addition of 20 seats to the University of Victoria program.
- Integrated teams including nurses and allied health providers are expected to be available in PCNs across the province by 2025, at which point PCNs will be in place covering most communities in BC.
- Between when the Government of BC first launched its primary care strategy in 2018 and March 2024, 512,072 individuals were attached to a primary care provider.
- The increase in attached patients reflects the gradual implementation of PCNs, introduction of the Provincial Attachment System and Health Connect Registry, and the opening of several models of care throughout BC.
- Blended capitation models such as Population Based Funding — In 2023-2024, the Ministry funded 10 clinics compensated through two risk adjusted blended capitation models of payment. Population-based funding models compensate full-service group family practices for longitudinal care to a registered population of patients. Under these models, clinics have greater flexibility to determine the best method and team member to provide the required services. Payments are based on the size and complexity of the practice's registered patient panels.
- The Ministry in collaboration with Doctors of BC has also supported blended capitation payments to longitudinal FPs in the form of Community LFP payments. These payments complement fee-for-service (FFS) billings and are adjusted to reflect the size and complexity of the patient panel.
- The Ministry announced the New to Practice Physician Incentives Program on June 15, 2022. The incentives include a signing bonus and medical education debt relief grants and is offered to physicians who recently completed their residency in family medicine. These incentives are intended to promote full-service, longitudinal primary care as an attractive and viable option for newly graduating family medicine residents and for recently new to practice physicians who may be interested. As of March 2024, there were 230 new family physicians committed to providing longitudinal care under the program.
- The Ministry provides funding through the Medical On-Call Availability Program to health authorities to enable them to contract with groups of physicians to provide "on-call" coverage necessary for hospitals to deliver emergency health care services to patients in a reliable, effective, and efficient manner.
- The Ministry provides funding for 24/7 peer support pathways for care providers throughout BC and across the care continuum requiring specialist consultative expertise. Through existing initiatives such as the Rapid Access to Consultative Expertise, Emergency Physician Online Support, and regional care coordination lines, as well as new initiatives focused on rural, remote, and Indigenous communities, the Ministry and its partners continue to work to closing health gaps and improve access to quality health services.
- The Ministry has funded new contracts and availability agreements to expand the range and specialization of 24/7 peer support pathways in BC to provide additional services focused on rural and remote providers requiring consultative expertise. These Real-Time Virtual Support (RVTS) pathways provide immediate access to rural and remote clinicians who have emergency, maternity, pediatric, and critical care expertise and can provide culturally safe, patient-centred care. Examples of RVTS pathways include the Maternity and Babies Advice Line, Child Health Advice in Real-Time Electronically (CHARLiE), and Rural Urgent Doctor in-aid (RUDi) pathways.
- The Ministry has also funded new patient-centred virtual care programs. The existing HealthLink BC 8-1-1 virtual health service has been expanded to offer virtual physician services to patients; in addition to services provided by nurses, dietitians, qualified professionals, pharmacists, and health services navigators.
- Two new services administered by the First Nations Health Authority (FNHA), the First Nations Virtual Doctor of the Day Program and the First Nations Virtual Substance Use and Psychiatry Service, deliver culturally safe, virtually accessible care to First Nations people who have limited access to FPs and NPs, or who require addictions medicine or psychiatric service support. In addition, a Northern Health Virtual Primary and Community Care Clinic has been established by the Northern Health Authority to provide care to people located in the Northern Health region who do not have an FP or NP, or who need care on the weekends, after their health centre is closed.
- The Ministry continues programs under the PMA to enhance the availability and stability of physician services in smaller urban, rural, and remote areas of BC. An outline of these programs can be obtained on the Government of BC website.
Infrastructure and Capital Planning
BC continues to make strategic investments in health sector capital infrastructure. The Ministry invests annually to renew and extend the asset life of existing health facilities, medical and diagnostic equipment, and information management technology at numerous health facilities across BC. The Ministry maintains a long-term capital plan to ensure health infrastructure is maintained and renewed within expected asset lifecycle timelines.
5.2 Physician compensation
The PMA is a formal agreement signed by the Government of BC, the Doctors of BC, and the MSC. The agreement supports ongoing efforts to recruit and retain physicians, while also improving access to FPs, specialists, and health care in rural and remote communities. A new three-year agreement has been signed and is effective April 1, 2022, through to March 31, 2025. Separately, physicians are registered by the College of Physicians and Surgeons of British Columbia, a regulatory body established under the Health Professions Act (HPA).
The Doctors of BC represent the interests of all physicians who receive payment for the medical services they provide to beneficiaries in relation to the PMA. The PMA establishes mechanisms that promote enhanced collaboration and accountabilities between the Government of BC and Doctors of BC through various joint committees. It also provides a formal conflict management process at both the local and provincial levels, and language limiting physician service withdrawals. The role of the health authorities in the planning and delivery of health care services is reinforced in the PMA.
The PMA sets out the compensation and benefit structure for physicians who provide publicly funded medical services whether via FFS, contract, or blended capitation funding models. Through the PMA, the Government of BC also provides targeted financial support for areas such as: rural programs; specialist services; full-service family practice; and shared care models involving FPs, specialists, and other health care professionals.
The PMA provides processes for monitoring and managing the funding established by the MSC under section 25 of the MPA for publicly funded medical services provided by physicians on an FFS basis. Mechanisms for revisions to the MSC Payment Schedule and for the payment of physicians are detailed in the PMA.
Dentists are registered by the British Columbia College of Oral Health Professionals, which is also a body established under the HPA. The Dentistry Master Agreement between the Province and the British Columbia Dental Association (BCDA) covers the following services: dental surgery; oral surgery; orthodontic services; oral medicine; pediatric dental services; and dental technical procedures. BC and the BCDA collaborate through a Dentistry Liaison Committee. The previous three-year agreement expired on March 31, 2022, and a new agreement is in force through March 31, 2025.
Physician compensation for medical services delivered in BC is provided through four different paths: to individual practitioners who submit claims to MSP under FFS or the LFP Payment model; to individual practitioners or physician groups who provide patient services under contract to the Ministry; by health authorities who contract and employ physicians for providing services to patients; and to health authorities and/or physician groups who provide patient services under blended capitation funding models.
The MSC is authorized to monitor the billing and payment of claims to manage expenditures for medical and health care benefits on behalf of MSP beneficiaries. The Ministry's Billing Integrity Program monitors, audits and investigates billing patterns and practices of medical and health care practitioners to detect and deter inappropriate and incorrect billing of MSP claims to MSC. The Billing Integrity Program develops and analyses practitioners' profiles, monitors trends, and conducts audits for the MSC. Further, where appropriate, the MSC seeks recovery of inappropriately paid monies in accordance with the MPA.
5.3 Payments to hospitals
Funding for publicly funded hospital services is included within annual funding allocations to health authorities, as well as specifically targeted funding from time to time. This funding allocation is used to fund the full range of necessary health services for the population of the region (or for specific provincial services, for the population of BC), including the provision of hospital services. Annual funding allocations to health authorities are determined as part of the Ministry's annual budget process. The current year funding allocations and notional out-year allocations are conveyed to health authorities by means of annual funding letters.
The Hospital Insurance Act (including the Hospital Insurance Act Regulations) and the Health Authorities Act govern payments made by the Government of BC to health authorities. These statutes establish the authority of the Minister of Health to make payments to regional health authorities and the Provincial Health Services Authority, and specify in broad terms what services are publicly funded when provided within a hospital and in delivering regional and other health care services.
The BC Tripartite Framework Agreement on First Nation Health Governance and other negotiated agreements provide the basis for the Ministry to provide funding to the First Nations Health Authority. Funding to support the Nisga'a Nation health care services and programs is provided to the Nisga'a Valley Health Authority under the terms of the 1999 Nisga'a Valley Health Board Transitional Funding Agreement.
The Ministry does not specifically fund hospitals directly; instead, health authorities are funded and provide operating budgets to hospitals within their regions to deliver specified services. The exception to this is when funding provided to health authorities (again not directly to hospitals) is targeted for specific priority projects (e.g., to fund wages or to provide operating funding to support large hospital construction projects coming on stream). Since it is specifically targeted, the funding must be reported on separately.
Annual incremental funding is allocated to health authorities using the Ministry's Population Needs-Based Funding model and other funding allocation methodologies (targeted funding allocations directed to specific health authorities, e.g., for wage costs related to collective bargaining). The annual funding allocation to health authorities does not include funding for programs directly operated by the Ministry, such as payments to physicians that occur through MSP and payments for prescription drugs that are covered under PharmaCare.
The accountability mechanisms associated with government funding for hospitals are part of several comprehensive documents that set expectations for health authorities. These include the annual funding letters, annual service plans, mandate letters, and annual bilateral agreements. Taken together, these documents convey the Ministry's broad expectations for health authorities and explain how performance will be monitored in relation to these expectations.
6.0 Recognition given to federal transfers
Funding provided by the federal government through the Canada Health Transfer is recognized and reported by the Government of British Columbia through various government websites and provincial government documents. In 2023–2024, these documents included:
- Estimates, Fiscal Year Ending March 31, 2024 (PDF document);
- Budget and Fiscal Plan 2023-2024 to 2025-2026 (PDF document); and
- Public Accounts, 2023-2024 (PDF document).
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 1. Number as of March 31st | 5,108,915 | 5,249,794 | 5,328,995 | 5,522,934 | 5,847,035 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| Public facilities | |||||
| 2. NumberFootnote 1 | 121 | 120 | 120 | 120 | 119 |
| 3. Payments for insured health services ($)Footnote 2 | not available | not available | not available | not available | not available |
| Private for-profit facilities | |||||
| 4. Number of private for-profit facilities providing insured health services | not available | not available | not available | not available | not available |
| 5. Payments to private for-profit facilities for insured health services ($) | not available | not available | not available | not available | not available |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 6. Total number of claims, in-patient | 5,622 | 3,585 | 3,425 | 3,937 | 8,169 |
| 7. Total payments, in-patient ($) | 59,949,069 | 36,666,159 | 48,688,770 | 43,777,017 | 70,438,677 |
| 8. Total number of claims, out-patient | 83,059 | 57,362 | 64,475 | 70,355 | 73,684 |
| 9. Total payments, out-patient ($) | 31,703,771 | 20,948,446 | 22,212,580 | 25,664,874 | 27,840,227 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| Pre-approved | |||||
| 10. Total number of claims, pre-approved in-patient | 44 | 57 | 30 | 12 | 15 |
| 11. Total payments, pre-approved in-patient ($) | 13,722,925 | 12,008,280 | 7,793,787 | 1,585,790 | 8,683,801 |
| 12. Total number of claims, pre-approved out-patient | not applicable | not applicable | not applicable | not applicable | not applicable |
| 13. Total payments, pre-approved out-patient ($) | not applicable | not applicable | not applicable | not applicable | not applicable |
| Non pre-approved | |||||
| 14. Total number of claims, non pre-approved in-patient | 1,817 | 827 | 248 | 462 | 691 |
| 15. Total payments, non pre-approved in-patient ($) | 740,655 | 378,501 | 101,370 | 151,946 | 279,846 |
| 16. Total number of claims, non pre-approved out-patient | 2,667 | 468 | 436 | 764 | 225 |
| 17. Total payments, non pre-approved out-patient ($) | 6,749,987 | 2,963,462 | 5,181,957 | 8,015,311 | 5,079,548 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 18. Number of participating physiciansFootnote 3 | 11,898 | 11,961 | 12,417 | 12,683 | 12,983 |
| 19. Number of opted-out physicians | 2 | 2 | 2 | 2 | 1 |
| 20.Number of non-participating physicians |
not available | not available | not available | not available | not available |
| 21. Total payments for services provided by physicians paid through all payment methods ($) | not available | not available | not available | not available | not available |
| 22. Total payments for services provided by physicians paid through fee-for-service ($) | 3,618,185,361 | 3,617,937,320 | 3,893,740,877 | 4,049,909,481 | 4,513,685,688 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 23. Number of services | 678,818 | 535,145 | 660,275 | 729,769 | 709,061 |
| 24. Total payments ($) | 35,479,965 | 25,212,412 | 30,781,911 | 33,765,605 | 35,758,266 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| Pre-approved | |||||
| 25. Number of services pre-approved | 3,783 | 3,611 | 3,947 | 2,149 | 538 |
| 26. Total payments pre-approved ($) | 6,512,749 | 5,582,667 | 4,496,066 | 3,059,713 | 1,159,098 |
| Non pre-approved | |||||
| 27. Number of services non pre-approved | 33,681 | 5,070 | 8,749 | 7,114 | 16,176 |
| 28. Total payments non pre-approved ($) | 1,714,922 | 246,382 | 449,423 | 310,088 | 761,399 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 29. Number of participating dentists | 201 | 193 | 204 | 199 | 196 |
| 30. Number of opted-out dentists | not available | not available | not available | not available | not available |
| 31. Number of non-participating dentists |
not available | not available | not available | not available | not available |
| 32. Number of services provided | 64,388 | 59,048 | 65,386 | 66,926 | 72,522 |
| 33. Total payments ($) | 10,243,209 | 9,302,887 | 10,036,091 | 11,262,347 | 12,644,463 |
|
|||||
Yukon
The Government of Yukon is committed to ensuring that Yukoners acquire the skills to live responsible, healthy, and independent lives. The Department of Health and Social Services (HSS) and its Minister are responsible for delivering all insured health care services.
In 2023-2024, HSS continued to work on implementing the recommendations outlined in the Putting People First report, which was created by an Independent Expert Panel following a comprehensive review on health and social services in the Yukon. As part of this work, the Yukon Dental Program was implemented in 2023, which provides up to $1,300 per year in dental care for eligible individuals who earn below a set income level and have no other dental insurance coverage. In addition, HSS has been working to streamline the physician contracting process through new standardized templates and rates. HSS continues to work on implementing the commitments outlined under the 2023 Confidence and Supply Agreement (CASA) made by the current government. This includes planning to expand access to fertility treatments through support for out-of-territory travel and tax rebates, as well as the HSS-run walk-in health care clinic that opened in December of 2023.
1.0 Public administration
1.1 Health care insurance plan and public authority
Insured Health Services (IHS) delivers health care benefits as set out in the Health Care Insurance Plan Act (HCIPA) and Hospital Insurance Services Act (HISA). The objective of IHS is to ensure access to insured physician and hospital services in line with these Acts.
The Government of Yukon delivers insured health benefits according to the HCIPA and the HISA. Both the HCIPA and HISA are administered by the Director of Insured Health Services (the Director). This position is a joint appointment by the Minister and the Commissioner of the Yukon Territory.
Insured health services in the Yukon means those physician services, surgical-dental services, and other services, including the supply of drugs, medical and dental supplies, prostheses, orthotics, appliances and similar devices, as may be described, that are provided to insured persons, but does not include any service that a person is entitled to or eligible for under any other Act, under any law of a province that relates to workers' compensation or under any Act of Parliament of Canada other than the Health Canada Act.
The HCIPA, section 3(2) and section 4, establishes the public authority to operate the health care plan. The HISA, section 3(1) and section 5, establishes the public authority to operate the hospital care plan.
Subject to the HCIPA (section 5), the HISA (section 6), and the Regulations, it is the responsibility of the Director to do the following:
- administer both plans;
- determine eligibility for insured health services;
- establish advisory committees and appoint individuals to assist operations;
- determine the amounts payable for insured health services outside the Yukon;
- conduct surveys and research programs and obtain statistics for such purposes;
- appoint auditors to examine and obtain information from medical records, reports, and accounts; and
- perform any other functions and discharge any other duties assigned by the Minister of Health and Social Services (HSS) under the Act.
Specific to the HISA, the Director has the responsibility to:
- enter into agreements on behalf of the Government of Yukon with hospitals in or outside of Yukon, or with the Government of Canada or any province or an appropriate agency thereof, for the provision of insured services to insured persons; and
- perform any other functions and discharge any other duties assigned to the administrator by the Regulations.
In 2023-2024, there were no amendments to the HCIPA's regulations.
1.2 Reporting relationship
The Department of Health and Social Services is accountable to the Legislative Assembly and the Government of Yukon through the Minister.
Section 6 of the HCIPA and section 7 of the HISA require that the Director submit an annual report on the administration of the two health insurance plans to the Minister. This report, "A Statement of Revenue and Expenditures", is tabled and reviewed in the legislature. The latest version of this report was tabled in the 2023 fall sitting of the Yukon legislature.
1.3 Audit of accounts
The services provided under the Yukon HCIPA and the Yukon HISA are subject to audit by the Office of the Auditor General of Canada. The Auditor General of Canada is the auditor of the Government of Yukon in accordance with section 34 of the Yukon Act. The Auditor General is required to conduct an annual audit of the transactions and consolidated financial statements of the Government of Yukon. Further, the Auditor General must report to the Yukon Legislative Assembly any matter falling within the scope of the audit that should be reported to the Assembly.
Further, section 13(2) of the Hospital Act requires the Yukon Hospital Corporation to submit a report of their operations for that fiscal year to the Minister within six months after the end of each fiscal year. The report is to include the financial statements of the Corporation and the Auditor's report.
2.0 Comprehensiveness
2.1 Insured hospital services
The Hospital Insurance Services Act (HISA), sections 3, 4, 5, 6, and 9, establish authority to provide insured hospital services to insured residents. The Yukon Hospital Insurance Services Ordinance was first passed in 1960 and came into effect April 9, 1960.
Adopted on December 7, 1989, the Hospital Act establishes the responsibility of the legislature and the government to ensure "compliance with appropriate methods of operation and standards of facilities and care." Adopted on November 11, 1994, the annexed Hospital Standards Regulation sets out the conditions under which all hospitals in the territory are to operate. Section 4(1) provides for the Ministerial appointment of one or more investigators to report on the management and administration of a hospital. Section 4(2) requires that the hospital's Board of Trustees establish and maintain a quality assurance program.
In April 1997, the Yukon government assumed responsibility for operating health units in rural Yukon communities from the federal government. These health centres are staffed by one or more nurses and auxiliary staff. In the absence of a physician, primary health care nurses provide daily clinics for medical treatment, community health programs, and 24-hour emergency services in 11 communities throughout the Yukon along with the Whitehorse Health Centre, which offers immunization clinics and pre/postnatal care.
In 2023-2024, insured in-patient and out-patient hospital services were delivered in Whitehorse General Hospital, Watson Lake Community Hospital, and Dawson City Community Hospital. Eleven community health centres across the Yukon provide out-patient hospital services.
In February 2024, amendments were made to the Hospital Insurance Services Regulations that added two new contract hospital locations in Whitehorse, Thomson Centre and Whistle Bend Place, that could be used for the provision of hospital-based insured services.
Pursuant to the Hospital Insurance Services Regulations, section 2(e) and (f), services provided in an approved hospital are insured.
As part of section 5 of the HISA, a Yukon Health Care Insurance Administrator (the Administrator) is appointed by the Commissioner in Executive Council to administer the services under the HISA and supervise staff who are required to administer services in accordance with the HISA.
Section 2(e) defines in-patient insured services as all of the following services to in-patients, namely:
- accommodation and meals at the standard or public ward level;
- necessary nursing service;
- laboratory, radiological, and other diagnostic procedures together with the necessary interpretations to maintain health, prevent disease, and help diagnose and treat injury, illness, or disability;
- drugs, biologicals, and related preparations as provided in Schedule B of the Regulations, when administered in the hospital;
- use of operating room, case room, and anaesthetic facilities, including necessary equipment and supplies;
- routine surgical supplies;
- use of radiotherapy facilities where available;
- use of physiotherapy facilities where available; and
- services rendered by persons who receive remuneration from the hospital.
Section 2(f) of the Hospital Insurance Services Regulations defines "out-patient insured services" as all of the following services to out-patients, when used for emergency diagnosis or treatment within 24 hours of an accident (period may be extended by the Administrator, provided the service could not be obtained within 24 hours of the accident):
- necessary nursing service;
- laboratory, radiological, and other procedures, together with the necessary interpretations for the purpose of assisting in the diagnosis and treatment of an injury;
- drugs, biologicals, and related preparations as provided in Schedule B, when administered in a hospital;
- use of operating room and anaesthetic facilities, including necessary equipment and supplies;
- routine surgical supplies;
- use of radiotherapy facilities where available; and
- use of physiotherapy facilities where available.
All diagnostic services available in the Yukon are provided through the hospitals, including magnetic resonance imaging (MRI) and computerized tomography (CT) scans. There are currently no private clinics providing diagnostic services. For services that are not available in the Yukon, patients receive care out-of-territory, usually in British Columbia or Alberta.
Pursuant to the Hospital Insurance Services Regulations, all in-patient and out-patient services provided in an approved hospital, by hospital employees, are insured services. Standard nursing care, pharmaceuticals, supplies, diagnostic, and operating services are provided. Any new programs or enhancements with significant funding implications or reductions to services or programs require the prior approval of the Minister. This process is managed by the Director of Insured Health Services. Public representation regarding changes in service levels is made through membership on the hospital board.
2.2 Insured physician services
Insured physician services in the Yukon are defined as medically required services rendered by a medical practitioner. Sections 1 to 8 of the Health Care Insurance Plan Act (HCIPA) and sections 2, 3, 7, 10, and 13 of the Health Care Insurance Plan Regulations provide for insured physician services. No amendments were made to the above sections of the Act in 2023-2024 fiscal year.
The HCIPA covers physicians providing medically required services. Physicians cannot opt out of HCIPA and must do the following:
- register for licensure pursuant to the Health Professions Act; and
- maintain licensure, pursuant to the Health Professions Act.
There were 293 physicians participating in HCIPA in 2023-2024. This includes resident physicians, as well as visiting specialists and locum physicians who are licensed to provide care throughout the Yukon. In 2023-2024, there were no physicians practicing in the territory who were providing services outside of the HCIPA.
Section 7 of the Yukon Health Care Insurance Plan Regulations covers payment for medical services. Subsection 4 allows physicians to arrange for payment for insured services on a basis other than fee-for-service. If a physician chooses to do this, they must submit a request in writing to the Director. In 2023–2024, physicians received payment through both fee-for-service and alternative arrangements.
The process of adding a new fee or changing an existing one in the Payment Schedule for the Yukon is supported by a committee structure. This process requires physicians to submit requests in writing to the HCIPA and the Yukon Medical Association (YMA) Fee Liaison Committee. After review, the committee makes a recommendation to the Director of Insured Health Services to either accept or reject the request. This recommendation is then prepared to be presented to the Minister of Health and Social Services for a final decision by the Yukon government. The fees are normally set in accordance with similar fees in other jurisdictions. Once a fee-for-service value has been determined, Yukon physicians are notified of the service and the applicable fee. Public consultation is not required.
New fees can also be implemented through fee negotiation between the YMA and the Department of Health and Social Services.
The current Memorandum of Understanding with the YMA was ratified October 5, 2022, and reflects the values of seamless transitions; access and attachment to primary care; and equity.
2.3 Insured surgical-dental services
Dentists providing insured surgical-dental services under the HCIPA must be licensed pursuant to the Dental Professions Act and bill in accordance with the HCIPA. Dentists providing services to Yukoners outside the territory also bill in accordance with the HCIPA.
Insured dental services are limited to surgical-dental procedures listed in Schedule B of the Health Care Insurance Plan Regulations. The procedures must be performed in a hospital. In 2023-2024, no dentists provided insured surgical-dental services under the HCIPA.
Changes to the list of insured services requires public consultation and amendment by Order-in-Council to Schedule B of the Health Care Insurance Plan Regulations. Coverage decisions are made on the basis of whether or not the service must be provided in hospital under general anaesthesia. The Director administers this process.
There were no new insured surgical-dental services added in 2023-2024.
2.4 Uninsured hospital, physician, and surgical-dental services
Only services prescribed by and rendered in accordance with the HCIPA and Regulations and HISA and Regulations are insured. All other services are uninsured.
Uninsured hospital services include:
- non-resident hospital stays;
- special or private nurses requested by the patient or family;
- additional charges for preferred accommodation unless prescribed by a physician;
- crutches and other such appliances;
- nursing home charges;
- televisions;
- telephones; and
- drugs and biologicals following discharge (these services are not provided by the hospital).
Section 3 of the Yukon HCIPA contains a list of services that are prescribed as non-insured. Uninsured physician services include:
- medical-legal services;
- testimony in court;
- preparation of records, reports, certificates, and communications;
- services or examinations required by a third party;
- services, examinations, or reports for reasons of attending university or camp;
- examination or immunization for the purpose of travel, employment, or emigration;
- cosmetic services;
- services not medically required;
- giving or writing prescriptions;
- the supply of drugs;
- dental care except procedures listed in Schedule B; and
- experimental procedures.
Yukon physicians may bill patients directly for non-insured services. Block fees are not used at this time; however, some physicians bill by service item. Billable services include but are not limited to:
- completing employment forms;
- medical-legal reports;
- transferring records;
- third-party examinations; and
- some elective services.
Payment does not affect patient access to services because not all physicians or clinics bill for these services and other agencies or employers may cover the cost.
Uninsured dental services include procedures considered restorative and procedures that are not performed in a hospital under general anaesthesia.
All Yukon residents have equal access to services. Third parties, such as private insurers or the Worker's Safety and Compensation Board, do not receive priority access to services through additional payment. Purchasing non-insured services, like fiberglass casts, does not delay access to insured services. Insured persons are given treatment options at the time of service.
The Yukon has no formal process to monitor compliance; however, feedback from physicians, hospital administrators, medical professionals, and staff allows the Director to monitor concerns.
The process used to de-insure services covered by HCIPA is as follows:
- Physician services: The HCIPA and the Yukon Medical Association Fee Liaison Committee are responsible for reviewing changes to the payment schedule for the Yukon, including decisions to de-insure services. In consultation with the Yukon Medical Advisor, decisions to de-insure services are based on medical evidence that the service is not medically necessary, is ineffective, or is a potential risk to the patient's health. Once a decision has been made to de-insure a service, all physicians are notified in writing. No physician services were de-insured in the 2023-2024 fiscal year.
- Hospital services: An amendment by Order-in-Council to sections 2(e) and 2(f) of the Yukon Hospital Insurance Services Regulations is required. As of March 31, 2024, no insured in-patient or out-patient hospital services, as provided for in the Regulations, have been de-insured.
- Surgical-dental services: An amendment by Order-in-Council to Schedule B of the Health Care Insurance Plan Regulations is required. A service could be de-insured if deemed not medically necessary or if it's no longer required to be carried out in a hospital under general anaesthesia. The Director manages this process. No surgical-dental services were de-insured in 2023–2024.
3.0 Universality
3.1 Eligibility
Eligibility requirements for insured health services are set out in the Health Care Insurance Plan Act (HCIPA) and Regulations, sections 2 and 4, and the Hospital Insurance Services Act (HISA) and Regulations, sections 2 and 4. There were no amendments to the legislation in 2023-2024.
Every Yukon resident is eligible for and entitled to insured health services on uniform terms. "Resident" is defined according to the Canada Health Act and means a person lawfully entitled to be or to remain in Canada, who makes their home and is ordinarily present in the Yukon, but does not include a tourist, transient, foreign student, or visitor. Pursuant to section 4(1) of the Yukon Health Care Insurance Plan Regulations and the Yukon Hospital Insurance Services Regulations, an insured person is eligible for insured services after midnight on the last day of the second month following the month of arrival to the Yukon. All persons returning to or establishing residency in the Yukon are required to complete this waiting period. The only exceptions are for newborns and children adopted by insured persons, persons arriving to the Yukon through the special program initiated through the Government of Canada in 2015 for the resettlement of Syrian refugees, and members of the Canadian Armed Forces and their families.
The following persons are not eligible for coverage in the Yukon:
- persons entitled to coverage from their home province or territory (e.g., students and workers covered under temporary absence provisions);
- visitors to the Yukon;
- refugee claimants;
- convention refugees;
- inmates in federal penitentiaries;
- study permit holders, unless they are a child and they are listed as the dependent of a person who holds a one year work permit; and
- employment authorizations of less than one year.
The ineligible persons noted previously may become eligible for coverage if they meet one or more of the following conditions:
- establish residency in the Yukon;
- become a permanent resident; or
- for inmates at the Whitehorse Correctional Centre, the day following discharge or release if stationed in or a resident in Yukon.
As of March 31, 2024, there were 46,570 people registered in the Yukon HCIPA.
3.2 Other categories of individuals
The Yukon HCIPA also covers the following groups:
- Children of Yukon residents born outside of Canada: if authorized no waiting period is applied.
- Returning Canadians: a waiting period is applied.
- Permanent Residents: a waiting period is applied.
- Minister's Permit: if authorized, a waiting period is applied.
- Foreign Workers: if holding an employment authorization in excess of twelve months, a waiting period is applied.
- Clergy: if holding an employment authorization, a waiting period is applied.
International students, temporary workers, tourists, transients, or visitors to the Yukon do not qualify as residents of the territory and are not eligible for HCIPA coverage.
4.0 Portability
4.1 Minimum waiting period
Where applicable, the eligibility of all persons is administered in accordance with the Interprovincial Agreement on Eligibility and Portability. Under section 4(1) of both the Health Care Insurance Plan Act Regulations and the Hospital Insurance Services Act Regulations, "an insured person is eligible for and entitled to insured services after midnight on the last day of the second month following the month of arrival to the Territory." All persons entitled to coverage are required to complete the minimum waiting period (see section 3.1 for exceptions).
4.2 Coverage during temporary absences in Canada
The provisions relating to portability of health care insurance during temporary absences outside the Yukon, but within Canada, are defined in sections 5, 6, 7, and 10 of the Yukon Health Care Insurance Plan Regulations and sections 6, 7(1), 7(2), and 9 of the Yukon Hospital Insurance Services Regulations. There were no changes to these Regulations in 2023-2024 that impact coverage during temporary absences in Canada.
The Regulations state that, "where an insured person is absent from the Territory and intends to return, he/she is entitled to insured services during a period of 12 months of continuous absence." Persons leaving the Yukon for more than six months must contact Yukon Insured Health Services (IHS) and complete a Temporary Absence form. Failure to do so may result in cancellation of coverage.
Students attending schools full-time outside the Yukon remain eligible for the duration of their studies. The Director of Insured Health Services (the Director) may approve absences in excess of 12 consecutive months upon receiving a written request from the insured person. Requests for extensions must be renewed yearly and are subject to approval by the Director.
For temporary workers and missionaries, the Director may approve absences in excess of 12 consecutive months upon receiving a written request from the insured person. Requests for extensions must be renewed yearly and are subject to approval by the Director.
The provisions regarding coverage during temporary absences in Canada fully comply with the terms and conditions of the Interprovincial Agreement on Eligibility and Portability effective February 1, 2001. Definitions are consistent in regulations, policies, and procedures.
The Yukon participates fully with the Interprovincial Medical Reciprocal Billing Agreements and Hospital Reciprocal Billing Agreements in place with all other provinces and territories with the exception of Quebec. Persons receiving physician or hospital services in Quebec may be required to pay directly and submit claims to IHS for reimbursement, in accordance with the Health Care Insurance Plan Act (HCIPA). Persons receiving hospital services in Quebec can present a valid health care card and receive services that are billed reciprocally to Yukon on behalf of the patient in accordance with the Hospital Insurance Services Act.
The Hospital Reciprocal Billing Agreements provide for payment of insured in-patient and out-patient hospital services to eligible residents receiving insured services outside the Yukon, but within Canada.
The Medical Reciprocal Billing Agreements provide for payment of insured physician services on behalf of eligible residents receiving insured services outside the Yukon, but within Canada.
Insured services provided to Yukon residents while temporarily absent from the territory are paid at the rates established by the host province.
4.3 Coverage during temporary absences outside Canada
The provisions that define portability of health care insurance to insured persons during temporary absences outside Canada are defined in sections 5, 6, 7, 9, 10, and 11 of the Yukon Health Care Insurance Plan Regulations and sections 6, 7(1), 7(2), and 9 of the Yukon Hospital Insurance Services Regulations. There were no changes to these regulations in 2023-2024 that impact coverage during temporary absences outside Canada.
Sections 5 and 6 state that, where an insured person is absent from the Yukon and intends to return, the person is entitled to insured services during a period of 12 months of continuous absence.
Persons leaving the Yukon for more than six months must contact the HCIPA and complete a Temporary Absence form. Failure to do so may result in cancellation of the coverage.
The provisions for portability of health insurance during out-of-country absences for students, temporary workers, and missionaries are the same as for absences within Canada (see section 4.2 of this report).
Insured physician services provided to eligible Yukon residents temporarily outside the country are paid at rates equivalent to those paid had the service been provided in the Yukon. Reimbursement is made to the insured person or directly to the provider of the insured service, in accordance with the HCIPA.
Insured in-patient hospital services provided to eligible Yukon residents outside Canada are paid at the rate established in the Standard Ward Rates Regulation for the Whitehorse General Hospital. For 2023-2024 the in-patient ward rate was set at $2,208 per day at Whitehorse General Hospital. The rate for the ICU ward at Whitehorse General Hospital was $6,719. These rates are set annually by the Interprovincial Health Insurance Agreements Coordinating Committee (IHIACC).
Insured out-patient hospital services provided to eligible Yukon residents outside Canada are paid at the rate established by the IHIACC.
4.4 Prior approval requirement
There is no legislated requirement that eligible residents must receive approval before seeking elective or emergency hospital or physician services outside the Yukon or Canada.
When treatment is provided outside the Yukon or Canada, plan members will only be reimbursed the amounts as described in Sections 4.2 and 4.3.
Prior approval by the Director is required for full reimbursement of services sought outside of Canada.
5.0 Accessibility
5.1 Access to insured health services
There are no user fees under the Yukon Health Care Insurance Plan Act (HCIPA). All services are provided on a uniform basis and access is not impeded by financial or other barriers. There is no extra-billing in the Yukon for any services covered by HCIPA.
In 2023-2024, the Yukon did not have any private for-profit health care facilities delivering insured health services.
If a patient has a complaint related to physician services, including extra-billing or user charges, they can contact the Yukon Medical Council (YMC). Information on complaints can be found on the YMC's website. The YMC can be reached by phone at 867-667-3774 or by email to ymc@yukon.ca.
Access to hospital or physician services not available locally are provided through the Visiting Specialist Program, Telehealth Program, or the Travel for Medical Treatment Program. These programs reduce delay in receiving necessary services.
To improve access to insured health services, the number of resident specialists working in the Yukon continues to increase to better serve Yukoners. In 2019, the "Find a Family Doctor" program was established to match unattached Yukon residents with family physicians able to take on new patients to their rosters. In early 2023, the program was expanded to "Find a Primary Care Provider" so that nurse practitioners could also start taking on unattached patients.
Insured Health Services provides extended health benefits to eligible Yukon residents which include the Travel for Medical Treatment Program, the Children's Drug and Optical Program, the Chronic Disease and Disability Benefits Program, Pharmacare Program, Extended Benefits Program, and the Yukon Dental Program.
The Yukon Hospital Corporation operates the three hospitals in the territory: Whitehorse General Hospital, Watson Lake Community Hospital, and Dawson City Community Hospital.
5.2 Physician compensation
The Department of Health and Social Services (HSS) seeks its negotiating mandate from the Government of Yukon before entering into negotiations with the Yukon Medical Association (YMA). The YMA and the government each appoint members to the negotiating team. Meetings are held as required until an agreement has been reached. The YMA's negotiating team then seeks approval of the tentative agreement from the YMA membership. HSS seeks ratification of the agreement from the Government of Yukon. The final agreement is signed with the concurrence of both parties.
Payments to physicians and dentists for insured services are governed by the HCIPA and the Health Care Insurance Plan Regulations.
The fee-for-service system is used to reimburse the majority of physicians providing insured services. Other systems of reimbursement include alternative payment arrangements, which are primarily used for specialist services in Whitehorse as well as physician services in rural communities.
5.3 Payments to hospitals
The Government of Yukon funds the Yukon Hospital Corporation (Whitehorse General Hospital, Watson Lake Community Hospital, and Dawson City Community Hospital) through contribution agreements with the HSS. Global operations and maintenance and capital funding levels are negotiated and adjusted based on operational requirements. In addition to the established operations and maintenance and capital funding set out in the agreement, the hospital can submit requests for additional program funding.
Payments made by the health care plan to facilities that provide insured hospital services are governed by the Hospital Insurance Services Plan Act and Regulations. These legislation and regulations organize payments to hospitals for insured services provided to insured persons.
6.0 Recognition given to federal transfers
The Government of Yukon has acknowledged the federal contributions provided through the Canada Health Transfer in its 2023–2024 annual Public Accounts publications, which are available publicly. Section 3(1) (d) and (e) of the Health Care Insurance Plan Act and section 3 of the Hospital Insurance Services Act acknowledge the contribution of the Government of Canada.
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 1. Number as of March 31st | 41,456 | 42,499 | 43,291 | 44,480 | 46,570 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| Public facilitiesFootnote 1 | |||||
| 2. Number (#) | 14 | 14 | 14 | 14 | 14 |
| 3. Payments for insured health services ($) | 88,761,576 | 89,796,881 | 95,644,777 | 113,289,492 | 144,204,570 |
| Private for-profit facilities | |||||
| 4. Number of private for-profit facilities providing insured health services | 0 | 0 | 0 | 0 | 0 |
| 5. Payments to private for-profit facilities for insured health services ($) | 0 | 0 | 0 | 0 | 0 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 6. Total number of claims, in-patient | 1,498 | 1,065 | 1,220 | 1,351 | 1,435 |
| 7. Total payments, in-patient ($) | 24,908,946 | 19,934,836 | 25,461,332 | 27,207,684 | 34,835,394 |
| 8. Total number of claims, out-patient | 15,636 | 13,348 | 14,364 | 16,919 | 20,217 |
| 9. Total payments, out-patient ($) | 5,820,934 | 4,743,896 | 5,489,199 | 6,742,156 | 8,870,909 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| Pre-approved | |||||
| 10. Total number of claims, pre-approved in-patient | not available | not available | not available | not available | not available |
| 11. Total payments, pre-approved in-patient ($) | not available | not available | not available | not available | not available |
| 12. Total number of claims, pre-approved out-patient | not available | not available | not available | not available | not available |
| 13. Total payments, pre-approved out-patient ($) | not available | not available | not available | not available | not available |
| Non pre-approved | |||||
| 14. Total number of claims, non pre-approved in-patient | 7 | < 5 | < 5 | 8 | 10 |
| 15. Total payments, non pre-approved in-patient ($) | 35,883 | 3,990 | 1,060 | 17,445 | 11,449 |
| 16. Total number of claims, non pre-approved out-patient | 62 | 18 | 14 | 30 | 18 |
| 17. Total payments, non pre-approved out-patient ($) | 67,707 | 30,659 | 8,225 | 20,818 | 7,951 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 18. Number of participating physiciansFootnote 4 | 196 | 180 | 226 | 238 | 293 |
| 19. Number of opted-out physicians | 0 | 0 | 0 | 0 | 0 |
| 20. Number of non-participating physicians | 0 | 0 | 0 | 0 | 0 |
| 21. Total payments for services provided by physicians paid through all payment methods ($) | 36,842,094 | 37,615,689 | 40,326,233 | 43,312,409 | 48,931,693 |
| 22. Total payments for services provided by physicians paid through fee-for-service ($) | 26,932,827 | 26,822,341 | 28,480,144 | 30,886,658 | 33,596,211 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 23. Number of services | 71,644 | 35,643 | 59,607 | 62,400 | 50,255 |
| 24. Total payments ($) | 5,505,429 | 2,898,923 | 5,074,446 | 4,996,900 | 4,519,544 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| Pre-approved | |||||
| 25. Number of pre-approved services | not available | not available | not available | not available | not available |
| 26. Total pre-approved payments ($) | not available | not available | not available | not available | not available |
| Non pre-approved | |||||
| 27. Number of non pre-approved services | 5 | not available | not available | not available | <5 |
| 28. Total non pre-approved payments ($)Footnote 3 | 712 | not available | not available | not available | 252 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 29. Number of participating dentists | 0 | 0 | 0 | 0 | 0 |
| 30. Number of opted-out dentists | 0 | 0 | 0 | 0 | 0 |
| 31. Number of non-participating dentists | 0 | 0 | 0 | 0 | 0 |
| 32. Number of services provided | 0 | 0 | 0 | 0 | 0 |
| 33. Total payments ($) | 0 | 0 | 0 | 0 | 0 |
|
|||||
Northwest Territories
The Department of Health and Social Services (the Department) is responsible for setting the strategic direction for the health and social services system through the development of legislation, policy, and standards; establishing approved programs and services; establishing and monitoring system budgets and expenditures; monitoring and evaluating programs and services; and reporting on system outcomes and performance measures. The Department is responsible for ensuring that all statutory functions and requirements are fulfilled, ensuring professionals are appropriately licensed and managing access to health insurance.
The Health and Social Services Authorities are governed by the Northwest Territories Health and Social Services Leadership Council (Leadership Council). Regional Wellness Councils provide advice to the Leadership Council and valuable information on the needs and priorities of the residents in their respective regions. The Leadership Council is responsible to the Minister of Health and Social Services (the Minister) for governing, managing, and providing health and social services in accordance with the plan set out by the Minister.
The Department recognizes that the identification of priorities and the development and delivery of responsive programs and services are best managed in partnership with Indigenous people and communities through an integrated system.
1.0 Public administration
1.1 Health care insurance plan and public authority
The Northwest Territories (NWT) Health Care Plan consists of the NWT Medical Care Plan and the NWT Hospital Insurance Plan.
The public authority responsible for the administration of the NWT Medical Care Plan is the Director of Medical Insurance, appointed by the Minister of Health and Social Services, under s.23(1) of the Medical Care Act. The Minister establishes the Northwest Territories Health and Social Services Authority and the Health and Social Service Authorities' Boards of Management pursuant to s.5(1), s.10(1), and s.10(2) of the Hospital Insurance and Health and Social Services Administration Act. The Hospital Insurance and Health and Social Services Administration Act recognizes, at s.10.3(1), that the Tłı̨chǫ Community Services Agency established by the Tłı̨chǫ Community Services Agency Act is deemed to be a Board of Management. The territorial authority and the boards of management administer the Hospital Insurance Plan; their legislated mandate is to:
- deliver health services, social services, and health and wellness promotional activities within the authority or boards region(s);
- manage, control and operate each health and social service facility for which the authority or board is responsible; and
- manage the financial, human and other resources necessary to perform the authority or board's duties.
There were no amendments made in 2023-2024 to the Medical Care Act or the Hospital Insurance and Health and Social Services Administration Act.
1.2 Reporting relationship
During the reporting period there were three Health and Social Service Authorities: Northwest Territories Health and Social Services Authority (Territorial Authority), Hay River Health and Social Services Authority, and Tłı̨chǫ Community Services Agency.
Territorial Authority affairs are directed by a Territorial Board of Management, the Leadership Council. Six Regional Wellness Councils provide advice to the Leadership Council, which is composed of the Regional Wellness Council chairpersons and the chairperson of the Tłı̨chǫ Community Services Agency and the Deputy Minister of the Department. The Leadership Council is accountable to the Minister.
The three Health and Social Services Authorities are responsible for the delivery of health and social services and for the management, control, and operation of facilities and services throughout the Northwest Territories. The Health and Social Services Authorities are required under legislation to comply with the territorial plan, which is set by the Minister.
The Minister appoints the Director of Medical Insurance who is responsible for administering the Medical Care Act and its Regulations. The Director of Medical Insurance prepares an annual report for the Minister on the operation of the NWT Medical Care Plan. This report can be found within the NWT Health and Social Services Annual Report.Footnote xi
The Minister appoints the Chair of the Leadership Council as well as the chairperson and members of ach Regional Wellness Council. The chairpersons and members of the Regional Wellness Councils may serve for three years and may be re-appointed to serve another term.
The Minister may appoint a Public Administrator to assume the role of a Board of Management in certain circumstances if the Minister feels it is necessary. During 2023-2024, a Public Administrator was in place for the Hay River Health and Social Services Authority. The Public Administrator acts in the place of a Board of Management.
The Tłı̨chǫ Community Services Agency was established under the Tłı̨chǫ Community Services Agency Act as part of the Tłı̨chǫ Land Claims and Self Government Agreement. The Tłı̨chǫ Community Services Agency Act, which is administered by the Minister of Executive and Indigenous Affairs, stipulates that the Tłı̨chǫ Community Services Agency has all the powers, duties and functions of a Board of Management under the Hospital Insurance and Health and Social Services Administration Act. Under the Tłı̨chǫ Community Services Agency Act, each Tłı̨chǫ community government is responsible for appointing one board member and the Minister of Executive and Indigenous Affairs is responsible for appointing the Chairperson following a consultation with the board members. The term for Tłı̨chǫ Community Services Agency board members is maximum of four years with the Chairperson's term being fixed by the Minister of Executive and Indigenous Affairs.
The Director of Medical Insurance and the Boards of Management are responsible to the Minister, as per section 8(1)(b) of the Canada Health Act.
In accordance with the Financial Administration Act and the Hospital Insurance and Health and Social Services Administration Act, there is an obligation to report to the Legislative Assembly on the preceding year's operations and financial position of the Department. Each year the NWT Health and Social Services System Annual Report meets these obligations, as well as meets the obligation to annually report on the operations of the Medical Care Plan.
1.3 Audit of accounts
The Office of the Auditor General of Canada (OAG) audits payments made under the NWT Hospital Insurance Plan and the NWT Medical Care Plan through their annual audit of the Government of the NWT's Public Accounts.
The Hospital Insurance Plan and the Medical Care Plan are administered by the Department. The latest OAG audit was on the 2022-2023 Public Accounts Section I: Consolidated Financial Statements and was completed as of December 19th, 2023. The GNWT, Public Accounts 2022-2023 Section I: Consolidated Financial Statements was published on December 19, 2023.
2.0 Comprehensiveness
2.1 Insured hospital services
Insured hospital services in the Northwest Territories (NWT) are provided under the Hospital Insurance and Health and Social Services Administration Act. No amendments were made to the legislation or regulations in 2023-2024.
During the reporting period, insured hospital services were provided to in-patients and out-patients by 24 facilities throughout the NWT. Consistent with Section 9 of the Canada Health Act, the NWT offers a comprehensive range of insured services to its residents.
Insured in-patient hospital services include:
- meals and accommodation at the standard or public ward level;
- required nursing services;
- laboratory, diagnostic, and imaging services (along with necessary interpretations);
- drugs, biologicals, and other preparations administered in the hospital;
- routine surgical supplies and use of operating room;
- case room and anesthesiology services;
- radiology and rehabilitation therapy (physiotherapy, speech and language pathology therapy, occupational therapy, and audiology);
- psychiatric and psychological services within an approved program; and
- detoxification at approved centers.
Insured out-patient hospital services include:
- laboratory tests;
- diagnostic imaging (including interpretations when needed);
- physiotherapy, speech and language pathology therapy, occupational therapy, and audiology;
- minor medical and surgical procedures and related supplies; and
- psychiatric and psychological services under an approved hospital program.
The Minister of Health and Social Services may approve additions or deletions to insured services provided in the NWT. While there were no changes to insured services in 2023-2024, assessment of additions is accomplished on a case-by-case basis. The Director of Medical Insurance makes such determinations based on the advice of the Medical Advisor. This process is a 'right size' approach, scaling the complexity of decision making to be appropriate to the size of the NWT health and social services system. Public consultation can be carried out through Regional Wellness Councils.
As outlined in the Government of the NWT Medical Travel Policy, travel assistance is provided to residents with a valid NWT Health Care Card who require medically necessary insured services that are not available in their home community.Footnote xii This ensures that residents of the NWT have reasonable access to insured hospital and physician services and that the cost of travel is not a barrier to care.
The NWT does not have any private diagnostic clinics that charge patients for services that would be considered insured if provided in a hospital.
2.2 Insured physician services
The NWT Medical Care Act and the NWT Medical Care Regulations provide for insured physician services. Medically necessary services provided in approved facilities by physicians, nurses, nurse practitioners, and midwives are considered insured services under the NWT Health Care Plan. These professionals are required by legislation to be licensed to practice in the NWT under the Medical Profession Act (physicians), Nursing Profession Act (nurses and nurse practitioners), and Midwifery Profession Act. Amendments to the Medical Profession Regulations under the Medical Profession Act came into force in November 1, 2023 to adopt the Canadian Medical Association's Code of Ethics and Professionalism and NWT-specific Standards of Practice. A new Nursing Profession Act came into force November 1, 2023 (replacing the previous Act), to establish a single regulatory framework for all nurses in the Northwest Territories, establish new nursing designations and update the complaints and discipline process. Work to move the regulation of midwives from the Midwifery Profession Act to profession-specific regulations under the Health and Social Services Professions Act, including modernization of the regulatory framework, was advanced in 2023-2024.
For the period 2023–2024 there were 326 licensed physicians (resident, locum and visiting) active in the NWT.
Physicians may opt out and collect fees other than under the NWT Medical Care Plan by providing written notice to the Director of Medical Insurance. There were no opted-out physicians in the NWT during the reporting period.
The NWT Medical Care Plan insures all medically necessary physician services such as:
- diagnosis and treatment of illness and injury;
- surgery, including anesthetic services;
- obstetrical care, including prenatal and postnatal care; and
- eye examinations, treatment and operations provided by an ophthalmologist.
Services not insured include:
- yearly physicals;
- cosmetic surgery;
- services that are considered experimental;
- prescription drugs;
- physical examinations done at the request of a third party;
- optometry services;
- dental services other than specific procedures related to jaw injury or disease;
- the services of chiropractors, naturopaths, podiatrists, osteopaths, and acupuncture treatments;
- physiotherapy, speech therapy, psychology services, received in a facility that is not an insured out-patient facility (hospital); and
- any service to which a resident is entitled under legislation, e.g., Workers Compensation Act, Public Health Act, or other Territorial or Federal Legislation, including treatment of veterans who are entitled to such treatments as a result of service in the Armed Forces.
The Director of Medical Insurance is responsible for recommending an insured services tariff for services payable by the NWT Medical Care Plan for the Minister's approval. The Minister ultimately determines if services will be added, altered, or removed from the tariff by:
- establishing a medical care plan that provides insured services to insured persons by medical practitioners that will qualify and enable the NWT to receive transfer payments from the Government of Canada under the Canada Health Act; and
- approving the fees and charges itemized in the tariff that may be paid in respect to insured services rendered by medical practitioners in the NWT and the conditions under which fees and charges are payable.
While there were no changes to insured services in 2023-2024, assessment of additions is accomplished on a case-by-case basis. The Director of Medical Insurance makes such determinations based on the advice of the Medical Advisor. This process is a 'right size' approach, scaling the complexity of decision making to be appropriate to the size of the NWT health and social services system. Public consultation is readily available through Regional Wellness Councils.
2.3 Insured surgical-dental services
Licensed oral surgeons may submit claims for insured surgical-dental work in the NWT. The Province of Alberta's Schedule of Oral and Maxillofacial Surgery Benefits is used as a guide.
Dentists are unable to participate in the NWT Medical Care Plan except where medically necessary and when services are delivered in a hospital. Dentists, when delivering services in a hospital, bill third-party insurance providers for dental surgery, and the anaesthetic services are covered under the NWT Medical Care Plan.
The only surgical-dental related procedures, covered under insured services, are for procedures focusing on reconstructive surgery of the face, primarily of the mouth and jaw as a result of trauma or birth defect. Such procedures are not identified as dental surgery but are identified as medically necessary surgery and are subject to physician referral. No procedures were added in 2023-2024 to the list of insured surgical services covered by the NWT Medical Care Plan.
2.4 Uninsured hospital, physician and surgical-dental services
Not all services provided by hospitals, medical practitioners and dentists are covered under the NWT Health Care Plan. Some uninsured services include:
- in-vitro fertilization;
- third party examinations;
- dental services that are not surgical in nature;
- medical-legal services;
- advice or prescriptions done over the phone;
- services rendered to the physician's family; and
- services carried out by people who usually are considered alternative medical care providers such as osteopaths, naturopaths, and chiropractors. Physiotherapy, psychiatry, and psychological therapies are not covered if delivered in a non-approved location.
Prior approval is required for NWT residents to receive items, services, or both, that are generally considered uninsured under the NWT Health Care Plan. A Medical Advisor makes recommendations to the Director of Medical Insurance regarding the appropriateness of the request.
The Workers' Safety and Compensation Commission (WSCC) covers the costs of the services to treat a worker who is injured on the job according to WSCC policy. The policy that covers requirements for entitlement can be found in NWT and Nunavut WSCC, Policy Manual, (Policy 03.02) available on the Workers' Safety and Compensation Commission site.
Changes to the list of uninsured hospital, physician, and surgical-dental services may be made by the Minister. While there were no changes to uninsured services in 2023-2024, assessment of additions is accomplished on a case-by-case basis. The Director of Medical Insurance makes such determinations based on the advice of the Medical Advisor. This process is a 'right size' approach, scaling the complexity of decision making to be appropriate to the size of the NWT health and social services system. Public consultation is available through Regional Wellness Councils.
3.0 Universality
3.1 Eligibility
The Medical Care Act and the Hospital Insurance and Health and Social Services Administration Act define eligibility for the Northwest Territories (NWT) Health Care Plan. The NWT Health Care Plan uses guidelines that are consistent with the legislation and the Interprovincial Agreement on Eligibility and Portability to determine eligibility to fulfill obligations of section 10 in the Canada Health Act.
Every resident is, on the first day of the third month after becoming a resident, eligible for and entitled to payment of benefits in respect of insured services rendered to the resident in accordance with the Medical Care Act and Medical Care Regulations. Military families are exempt from the three-month waiting period and are eligible for coverage their first day in the Territory.
According to the Medical Care Act, a resident is a person lawfully entitled to be or to remain in Canada, who makes their home and is ordinarily present in the NWT, but does not include a tourist, transient, or visitor to the NWT. There were no amendments to the Medical Care Act regarding eligibility made in 2023-2024.
To register for the NWT Health Care Plan, residents fill out an application form and provide relevant supporting documentation (e.g., visa, immigration papers, and proof of residency). Residents may register prior to the date they become eligible. Registration is directly linked to eligibility for coverage and claims are only paid if the client has registered.
Coverage begins when a signed application has been approved.
Residents can opt out of the NWT Health Care Plan if they choose not to register. There is nothing in the Medical Care Act that requires a resident to register for the NWT Health Care Plan. At any time, a resident may advise the NWT Health Care Plan administrator of a wish to opt out of the Plan.
Eligible people are those who have established permanent residency in the NWT, members of the Royal Canadian Mounted Police residing in the NWT, dependents of a member of the Canadian Armed Forces residing in the NWT, returning Canadians or returning Permanent Residents (a person who has immigrated to Canada with permanent resident status through Citizenship and Immigration Canada), and individuals working at a mine site who do not maintain a permanent residence in another province.
Individuals not eligible for NWT health care coverage are members of the Canadian Forces, federal inmates, and new residents who have not completed the minimum waiting period.
In accordance with the Interprovincial Agreement on Eligibility and Portability of Hospital and Medical Care Insurance, residents who have been federal inmates become eligible upon release to the NWT; permanent residents become eligible upon establishment of permanent residency. Returning Canadians are eligible on the first day of arrival in NWT and permanent residents are also eligible on the first day, provided that the NWT is the first jurisdiction they are residing in upon arriving in or returning to Canada.
If an application for an NWT Health Care Card is denied, coverage is denied for a procedure, or if a person is appealing the decision to cancel their NWT Health Care Card, individuals may appeal to the Director of Medical Insurance. Second level and final appeals may be directed to the Deputy Minister of Health and Social Services.
As of March 31, 2024, there were 41,358 individuals registered with the NWT Health Care Plan.
3.2 Other categories of individuals
Holders of employment visas, student visas and, in some cases, visitor visas are covered if they meet the provisions of the Interprovincial Agreement on Eligibility and Portability Agreement and guidelines for NWT Health Care Plan coverage.
Babies born to NWT residents outside of Canada are automatically covered effective on the date of birth, if:
- at least one parent is a Canadian citizen; and
- the parent(s) has:
- approved temporary absence coverage under NWT Health Care Plan; and
- an intended date of return to the NWT.
Foreign students and workers are eligible for coverage if they hold study or work permits valid for a period of 12 months or longer. Those holding permits of less than 12 months are not eligible for coverage.
Permanent residents (landed immigrants) and returning permanent residents, including those with expired residency, are covered on the first day of arrival in the NWT provided the NWT is their first place of residence in Canada, and they intend to reside in the NWT.
Convention refugees are covered, provided they provide appropriate documentation.
The following are not eligible for an NWT Health Care Card as they are not considered residents:
- tourists;
- visitors;
- transients;
- remand clients from other jurisdictions;
- Canadian students, who are not NWT residents, attending an educational institution in the NWT (unless the student intends to establish a permanent residence in the NWT). Permanent residence does not include student housing or living on campus;
- a person who works in the NWT but does not intend to maintain a permanent residence (over 12 months) in the NWT (s.7, Interprovincial Agreement on Eligibility and Portability of Hospital and Medical Care Insurance);
- Temporary Resident Permit (TRP) holders (TRPs are issued by the Federal Immigration Minister and are issued to individuals who, for some reason, do not meet the immigration requirements but are admitted to Canada for compassionate or humanitarian reasons. The duration of the TRP varies but they can be issued for up to three years); and
- individuals without valid documentation from Immigration, Refugees, and Citizenship Canada.
4.0 Portability
4.1 Minimum waiting period
Waiting periods for persons moving to the Northwest Territories (NWT) are consistent with the Interprovincial Agreement on Eligibility and Portability. The waiting period ends the first day of the third month of residency for those moving permanently to the NWT. Military families are exempt from the three- month waiting period and are eligible for coverage their first day in the NWT.
4.2 Coverage during temporary absences in Canada
Section 4(2) of the Medical Care Act provides NWT residents with access to insured health coverage while temporarily out of the NWT but still in Canada, consistent with section 11(1) (b)(i) of the Canada Health Act. The Department of Health and Social Services (the Department) adheres to the Interprovincial Agreement on Eligibility and Portability. No amendments were made in 2023-2024 to the Medical Care Act.
NWT residents may be covered for up to one year of temporary absence for work, travel or holidays. Full-time students attending post-secondary school are covered. The full cost of insured services is paid for all services received in other Canadian jurisdictions. The criterion for Temporary Absence is that the individual must be physically present in the NWT for a period of 153 days in a calendar year to maintain residency.
When a valid NWT Health Care Card is produced, most doctor visits and hospital services are billed directly to the Department. During the reporting period, approximately $46.8 million dollars were paid out for hospital in-patient and out-patient services in other provinces and territories. Reimbursement guidelines exist for patients having to pay up front for medically necessary services.
The NWT participates in both the Hospital Reciprocal Billing Agreement and the Medical Reciprocal Billing Agreement with other jurisdictions (except Quebec).
4.3 Coverage during temporary absences outside Canada
As per section 4(3) of the Medical Care Act and section 11(1)(b) (ii) of the Canada Health Act, the NWT provides reimbursement for NWT residents who require medically necessary services while temporarily outside Canada. No amendments were made in 2023-2024 to the Medical Care Act.
Individuals are required to pay up front and seek reimbursement upon their return to the NWT. Costs for eligible services, including in-patient services, out-patient services, and hemodialysis rendered outside Canada, will be reimbursed up to the amounts payable in the NWT.
Residents temporarily out of Canada may receive coverage for up to one year; however, prior approval as well as documentation proving the NWT will be the individual's permanent residence upon return is required. Returning Canadians are covered on the first day of arrival in the NWT. Documentation is required to validate the first day of arrival. Permanent residents (Landed immigrants) are covered on the first day of arrival in the NWT, with appropriate documentation from Immigration, Refugees and Citizenship Canada, provided the NWT is their first place of residence in Canada and they intend to reside here. Foreign workers holding a valid closed work permit are eligible for coverage on the first day they are present in the NWT. Live-in care givers with a work permit that lists the NWT as the location of employment are eligible for first day coverage. Military families are also eligible for first day coverage.
4.4 Prior approval requirement
Prior approval is required for elective services rendered in other provinces and outside Canada. All services from private facilities require prior approval.
First level appeals of decisions may be sent to the Director of Medical Insurance. Second level appeals are considered by the Deputy Minister of Health and Social Services. The decision of the Deputy Minister is final.
5.0 Accessibility
5.1 Access to insured health services
The Northwest Territories (NWT) provides NWT residents with assistance to access medically necessary insured services not available in their home community consistent with section 12(1)(a) of the Canada Health Act.Footnote xiii
Extra-billing is not permitted in the NWT, in adherence to section 18 of the Canada Health Act and section 14(1) of the Medical Care Act. The only exception is if a medical practitioner opts out of the NWT Medical Care Plan and collects his or her own fees. Extra-billing did not occur in 2023-2024.
User charges are also not permitted under section 14(2) of the Medical Care Act unless the medical practitioner has opted-out of the NWT Medical Care Plan, collects his or her own fees, and gives reasonable notice of the intention to collect fees.
The Medical Care Act includes a provision to allow the Minister of Health and Social Services to establish a Benefits Appeal Committee that could address any matter referred to it by the Minister, including complaints where a physician engaged in extra-billing and charged user fees. This committee has not been established.
Complaints of extra-billing or user charges can be made to:
The Health Services Administration Office, Health and Social Services
Bag #9
Inuvik NT, X0E 0T0
by phone at: 1-800-661-0830 or 1-867-678-8050
or by Fax at: 1-867-777-3197
5.2 Physician compensation
The Department of Health and Social Services (the Department), in consultation with the NWT Medical Association, sets physician compensation. Generally, family and specialist practitioners are compensated through contractual agreements with the Government of NWT, while the remaining practitioners are compensated on a fee-for-service basis. Fee-for-service rates in the NWT are itemized in the Insured Services Tariff approved by the Minister in accordance with the Medical Care Act.
Under the Medical Care Act, the Minister may appoint medical and financial inspectors who shall, under the direction of the Director, inspect, examine, and audit books, accounts, reports, and medical records maintained in hospitals, health facilities, offices of medical practitioners, and other health care facilities respecting patients who are receiving or who have received insured services. The Director may reassess an account for insured services submitted by a medical practitioner and make any appropriate adjustment in the amount paid to the medical practitioner in respect of the insured services.
5.3 Payments to hospitals
Contribution agreements between the Department and the Boards of Management dictate payments made to hospitals. Government budgets, resources, and levels of services offered determine the allocated amounts.
Payments for the provision of insured hospital services are governed under the Hospital Insurance and Health and Social Services Administration Act and the Financial Administration Act. A comprehensive budget is developed to fund hospitals in the NWT.
6.0 Recognition given to federal transfers
Federal funding from the Canada Health Transfer has been recognized and reported by the Government of the Northwest Territories (GNWT) through the following documents: GNWT, Public Accounts 2022-2023Section I: Consolidated Financial Statements (published December 2023), and GNWT, 2024-2025 Main Estimates (published May 2024).
The Public Accounts contain the consolidated financial statements of the GNWT, audited by the Auditor General of Canada, and are presented annually to the Legislative Assembly. The Main Estimates are also presented annually to the Legislative Assembly.
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 1. Number as of March 31st | 42,501 | 43,211 | 43,902 | 41,131 | 41,917 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| Public facilities | |||||
| 2. Number | 23 | 23 | 23 | 23 | 24 |
| 3. Payments for insured health services ($)Footnote 1 | 98,439,727 | 107,379,830 | 108,887,913 | 113,092,978 | 130,136,474 |
| Private for-profit facilities | |||||
| 4. Number of private for-profit facilities providing insured health services | 0 | 0 | 0 | 0 | 0 |
| 5. Payments to private for-profit facilities for insured health services($) | not applicable | not applicable | not applicable | not applicable | not applicable |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 6. Total number of claims, in-patient | 1,451 | 1,215 | 1,422 | 1,432 | 1,684 |
| 7. Total payments, in-patient ($) | 21,691,553 | 21,005,854 | 23,539,221 | 26,701,796 | 36,575,030 |
| 8. Total number of claims, out-patient | 14,719 | 11,536 | 13,005 | 15,476 | 19,393 |
| 9. Total payments, out-patient ($) | 7,118,914 | 5,214,017 | 5,916,399 | 7,466,578 | 10,260,952 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| Pre-approved | |||||
| 10. Total number of claims, pre-approved in-patient | 0 | 0 | 0 | 0 | 0 |
| 11. Total payments, pre-approved in-patient ($) | 0 | 0 | 0 | 0 | 0 |
| 12. Total number of claims, pre-approved out-patient |
2 | 0 | 8 | 0 | 0 |
| 13. Total payments, pre-approved out-patient ($) | 5,253 | 0 | 12,329 | 0 | 0 |
| Non pre-approved | |||||
| 14. Total number of claims, non pre-approved in-patient | 8 | 2 | 3 | 3 | 4 |
| 15. Total payments, non pre-approved in-patient ($) | 34,544 | 38,039 | 9,557 | 237,272 | 13,092 |
| 16. Total number of claims, non pre-approved out-patient | 27 | 1 | 2 | 9 | 14 |
| 17. Total payments, non pre-approved out-patient ($) | 10,892 | 359 | 2,873 | 4,985 | 21,432 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 18. Number of participating physiciansFootnote 2 | 421 | 390 | 439 | 373 | 326 |
| 19. Number of opted-out physicians | 0 | 0 | 0 | 0 | 0 |
| 20. Number of not participating physicians | 0 | 0 | 0 | 0 | 0 |
| 21. Total payments for services provided by physicians paid through all payment methods ($)Footnote 3 | 59,307,947 | 69,731,726 | 69,149,635 | 79,766,508 | 78,178,001 |
| 22. Total payments for services provided by physicians paid through fee-for-service ($) | 1,327,593 | 1,791,787 | 1,998,842 | 1,960,751 | 1,854,548 |
| Pre-approved | |||||
|---|---|---|---|---|---|
| 23. Number of services | 66,422 | 52,523 | 59,097 | 60,852 | 85,716 |
| 24. Total payments ($) | 7,366,537 | 6,586,069 | 7,207,778 | 8,402,981 | 9,626,598 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| Pre-approved | |||||
| 25. Number of pre-approved services | 0 | 0 | 0 | 0 | 0 |
| 26. Total pre-approved payments ($) | 0 | 0 | 0 | 0 | 0 |
| Non Pre-approved | |||||
| 27. Number of non pre-approved services | 51 | 2 | 13 | 20 | 18 |
| 28. Total non pre-approved payments ($) | 14,389 | 580 | 5,764 | 12,108 | 4,583 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 29. Number of participating dentists | not applicable | not applicable | not applicable | not applicable | not applicable |
| 30. Number of opted-out dentists | not applicable | not applicable | not applicable | not applicable | not applicable |
| 31. Number of non-participating dentists | not applicable | not applicable | not applicable | not applicable | not applicable |
| 32. Number of services provided | not applicable | not applicable | not applicable | not applicable | not applicable |
| 33. Total payments ($) | not applicable | not applicable | not applicable | not applicable | not applicable |
|
|||||
Nunavut
The Department of Health (the Department) faces many unique challenges when providing for the health and well-being of Nunavummiut. Of a total population of 40,758 approximately one third of the population is under the age of 15 yearsFootnote xiv,Footnote xv. The territory is made up of 25 communities located across three time zones and divided into three regions: the Qikiqtani (or Baffin), the Kivalliq and the Kitikmeot.
The Government of Nunavut incorporates Inuit Societal Values into program and policy development, as well as into service design and delivery. The delivery of health services in Nunavut is based on a primary health care model. Nunavut's primary health care providers are family physicians, nurse practitioners, midwives, community health nurses, and other allied health professionals.
In 2023-2024, the territorial operations and maintenance budget for the Department was $479,490,000 including supplementary appropriationsFootnote xvi. One third of the Department's total operational budget was spent on costs associated with medical travel and treatment provided in out-of-territory facilities. Nunavut is a vast territory with a low population density and limited health infrastructure, therefore, access to a range of hospital and specialist services often requires that residents be sent out-of-territory for care.
In 2023-2024, a total of $32,454,000 was allocated to the Department for capital projectsFootnote xvii. The Department's 2023-2024 capital projects include the construction of the long-term care facility in Rankin Inlet and the new Nunavut Recovery Centre (Aqqusariaq) in Iqaluit.
1.0 Public administration
1.1 Health care insurance plan and public authority
The Health Care Insurance Plans of Nunavut, including physician and hospital services, are administered by the Department of Health (the Department) on a non-profit basis.
The Medical Care Act (NWT, 1988 and as duplicated for Nunavut by section 29 of the Nunavut Act, 1999) governs the entitlement to and payment of benefits for insured medical services.
The Hospital Insurance and Health and Social Services Administration Act (NWT, 1988 and as duplicated for Nunavut by section 29 of the Nunavut Act, 1999) enables the establishment of hospital and other health services.
The Department is responsible for delivering health care services to Nunavummiut, including the operation of community health centres, regional health centres, and a hospital. There are three regional offices that manage the delivery of health services at a regional level. Iqaluit operations are administered separately. The Government of Nunavut opted for decentralization to regional offices to support front-line workers and community-based delivery of a wide range of health programs and services.
1.2 Reporting relationship
Legislation governing the administration of health services in Nunavut was carried over from the Northwest Territories (as Nunavut statutes) pursuant to the Nunavut Act. The Medical Care Act governs who is covered by the Nunavut Health Care Plan and the payment of benefits for insured medical services. Section 23(1) of the Medical Care Act requires the Minister responsible for the Act to appoint a Director of Medical Insurance.
The Director is responsible for the administration of the Act and its Regulations. Section 24 requires the Director to submit an annual report on the operation of the Nunavut Health Care Plan to the Minister for tabling in the Legislative Assembly. The Operation of the Medical Care Plan (PDF document) from the Director of Medical Insurance was submitted and is available on the Legislative Assembly website.
1.3 Audit of accounts
The Auditor General of Canada is the auditor of the Government of Nunavut in accordance with section 30.1 of the Financial Administration Act (Nunavut, 1999). The Auditor General is required to conduct an annual audit of the consolidated financial statements of the Government of Nunavut. The most recent audit of the Government of Nunavut's public accounts was completed June 2024, for the fiscal year 2022-2023. The Independent Auditor's Report to Nunavut's Legislative Assembly can be found on page 19 of the Government of Nunavut's Report of Public Accounts.
2.0 Comprehensiveness
2.1 Insured hospital services
Insured hospital services are provided in Nunavut under the authority of the Hospital Insurance and Health and Social Services Administration Act and Regulations, sections 2 to 4. No amendments were made to the Act or Regulations in 2023-2024.
In 2023-2024, insured hospital services were delivered in 27 facilities across Nunavut including:
- one general hospital (Iqaluit);
- two regional health facilities (Rankin Inlet and Cambridge Bay);
- 22 community health centres; and
- two public health facilities (Iqaluit and Rankin Inlet). Rehabilitative treatment is available through the Timimut Ikajuksivik Centre located at Qikiqtani General Hospital (QGH) or via contracted services in other regions.
The QGH is currently the only acute care facility in Nunavut, accredited by Accreditation Canada, providing a range of in-and out-patient hospital services as defined by the Canada Health Act. QGH offers 24-hour emergency services, in-patient care (including obstetrics, pediatrics, and palliative care), surgical services, laboratory services, diagnostic imaging, respiratory therapy, rehabilitation services, and health information management services.
Currently, Rankin Inlet is providing 24-hour care for in-patients; out-patients receive care by on-call staff. Cambridge Bay is providing daily clinic hours, and emergency care is available, on-call, 24-hours a day. There are also a limited number of birthing beds at both facilities.
Other community health centres provide primary care services, inclusive of public health services, out-patient services, and urgent treatment services.
Public health services are provided at public health clinics located in Rankin Inlet and Iqaluit. Public health programing is provided in the remaining communities through the local health centre. The Department of Health (the Department) also operates a Family Practice Clinic in Iqaluit. This clinic operates as part of the primary care program at QGH.
The Department is responsible for authorizing, licensing, inspecting, and supervising all health facilities in the territory.
Insured in-patient hospital services include:
- accommodation and meals at the standard ward level;
- necessary nursing services;
- laboratory, radiological and other diagnostic procedures, together with the necessary interpretations;
- drugs, biological and related preparations prescribed by a physician and administered in hospital;
- routine surgical supplies;
- use of operating room, case-room, and anaesthetic facilities;
- use of radiotherapy and physiotherapy services where available;
- psychiatric services provided under an approved program; and
- services rendered by persons who are paid by the hospital.
Out-patient services include:
- laboratory tests and diagnostic imaging, including interpretations, when requested by a physician and performed in an out-patient facility or in an approved hospital;
- hospital services in connection with most minor medical and surgical procedures;
- physiotherapy, occupational therapy, limited audiology and speech therapy services in an out-patient facility or in an approved hospital; and
- psychiatric services provided under an approved hospital program.
The Department makes the determination to add publicly funded insured hospital services based on the availability of appropriate resources, equipment, and overall feasibility in accordance with financial guidelines set by the Department and with the approval of the Financial Management Board. The Commissioner of Nunavut, with their authority, may also make regulations prescribing insured services. No new services were added in 2023-2024 to the list of insured hospital services.
2.2 Insured physician services
The Medical Care Act, section 3(1), and Medical Care Regulations, section 3, provide for insured physician services in Nunavut. No amendments were made to the Act or Regulation in 2023-2024. The Nursing Professions Act allows for licensure of nurse practitioners in Nunavut; this permits nurses to deliver insured services in Nunavut. The new Nursing Professions Act came into force December 5, 2023.
Upon initial registration, physicians must be in good standing with a College of Physicians and Surgeons from a Canadian jurisdiction to be licensed to practice in Nunavut. The Government of Nunavut's Medical Registration Committee currently manages this process for Nunavut physicians. Nunavut recruits and contracts its own family physicians and accesses specialist services primarily from its main referral centres in Ottawa, Edmonton, Winnipeg, and Yellowknife. There are 40.5 family physician positions, which are covered by a combination of locums and full-time physicians. Recruitment of full-time family physicians has become an increasing challenge and remains a high priority for the Department. In 2023-2024, family physicians provided over 11, 255 days of service across the territory.
Of the 40.5 full-time family physician positions in Nunavut, 24.5 are in the Qikiqtaaluk region; 11 in the Kivalliq region; and five in the Kitikmeot region. There are also three general surgeon positions, three general practitioner anesthetist positions, four pediatrician positions, and two obstetrician-gynecologist positions at QGH. Visiting specialists, general practitioners, and locums also provide insured physician services; these arrangements are made by the Department's Medical Affairs division, in consultation with regional leadership.
Physicians can elect to collect fees other than those under the Medical Care Plan as per section 12(2) (a) or (b) of the Medical Care Act by notifying the Director of Medical Insurance (the Director) in writing. An election can be revoked on the first day of the following month after a letter to that effect is delivered to the Director. In 2023-2024, no physicians provided written notice of this election. All physicians practicing in Nunavut are under contract with the Department. In 2023-2024, 179 physicians provided services in Nunavut.
Insured physician services refer to all services rendered by medical practitioners that are medically required. Where insured services are unavailable in some places in Nunavut, the patient is referred to another jurisdiction to obtain the insured service. Nunavut has health service agreements with medical and treatment centres in Ottawa, Winnipeg, Churchill, Yellowknife, and Edmonton. These are the out-of-territory sites to which Nunavut mainly refers its patients to access medical services not available within the territory.
The following is a list of common insured categories as per Nunavut's Medical Care Regulations. Services provided under these categories are considered insured if the medically required diagnosis and/or treatment is provided in-territory or out-of-territory.
- anesthesiology;
- cardio-thoracic and vascular surgery;
- dermatology;
- general practitioner;
- gynecology;
- general surgery;
- internal medicine;
- neurology;
- obstetrics;
- ophthalmology;
- otolaryngology;
- orthopedics;
- pediatrics;
- plastic surgery (not cosmetic);
- psychiatry;
- radiology;
- trans-related surgeries; and
- urology.
The addition or deletion of insured physician services requires government approval. For this, the Director would become involved in negotiations with a collective group of physicians to discuss the service. Then the decision of the group would be presented to Cabinet for approval. No insured physician services were added or removed in 2023-2024.
2.3 Insured surgical-dental services
Dentists providing insured surgical-dental services under the Nunavut Health Care Plan must be licensed pursuant to the Dental Profession Act (NWT, 1988 and as duplicated for Nunavut by section 29 of the Nunavut Act, 1999). Billing numbers are provided for billing the Plan regarding the provision of insured dental services.
Insured dental services are limited to those dental-surgical procedures scheduled in the Dental Profession Regulations, requiring the unique capabilities of a hospital for their performance; for example, orthognathic surgery. The Department insures all dental-surgical services outlined in provincial/territorial reciprocal billing agreements. Oral surgeons are brought to Nunavut on a regular basis, but on rare occasions, for medically complicated situations, patients are flown out of the territory. Dentists travelling to Nunavut to deliver services are under contract with the Government of Nunavut and do not have the option to opt-out.
The addition of new surgical-dental services to the list of insured services requires government approval. No new services were added to the list in 2023-24.
2.4 Uninsured hospital, physician, and surgical-dental services
Services provided under the Workers' Compensation Act (NWT, 1988 and as duplicated for Nunavut by section 29 of the Nunavut Act, 1999) or other acts of Canada, except the Canada Health Act, are excluded.
Services provided by physicians that are not insured include:
- yearly physicals for people between 11 and 64 years of age (physicals for those under 10 or 65+ are insured);
- cosmetic surgery;
- services that are considered experimental;
- prescription drugs;
- physical examinations done at the request of a third party;
- optometric services;
- dental services other than specific procedures related to jaw injury or disease;
- the services of chiropractors, naturopaths, podiatrists, osteopaths, and acupuncture treatments; and
- physiotherapy, speech therapy, and psychology services received in a facility that is not an insured out-patient facility (hospital).
Services not covered in a hospital include:
- hospital charges above the standard ward rate for private or semi-private accommodation;
- services that are not medically required, such as cosmetic surgery;
- services that are considered experimental;
- ambulance charges (except inter-hospital transfers);
- dental services, other than specific procedures related to jaw injury or disease; and
- alcohol and drug rehabilitation, without prior approval.
In 2023-2024, the Qikiqtani General Hospital charged a $3,219 per diem rate for services provided for non-Canadian resident stays. The in-patient rate charged in Rankin Inlet and Cambridge Bay was $1,808 per day.
When residents are sent out-of-territory for services, the Department relies on the policies and procedures guiding that particular jurisdiction when they provide services to Nunavut residents that could result in additional costs, only to the extent that these costs are covered by Nunavut's Medical Insurance Plan (see section 4.2 below). Any query or complaint is handled on an individual basis with the jurisdiction involved.
The Department also administers the Non-Insured Health Benefits (NIHB) Program, on behalf of Indigenous Services Canada, for Inuit and First Nations residents in Nunavut. NIHB covers a co-payment for medical travel, accommodations and meals at boarding homes (in Ottawa, Winnipeg, Churchill, Edmonton, Yellowknife and Iqaluit), prescription drugs, dental treatment, vision care, medical supplies and prostheses, and a number of other incidental services.
3.0 Universality
3.1 Eligibility
Eligibility for the Nunavut Health Care Plan is briefly defined under sections 3(1), (2), and (3) of the Medical Care Act. The Department of Health (the Department) also adheres to the Interprovincial Agreement on Eligibility and Portability, as well as internal guidelines. No amendments were made to the Act or Medical Care Regulations in 2023-2024.
Subject to these provisions, every Nunavut resident is eligible for and entitled to insured health services on uniform terms and conditions. A resident means a person lawfully entitled to be in or to remain in Canada, who makes their home and is ordinarily present in Nunavut, but does not include a tourist, transient or visitor to Nunavut. Eligible residents receive a health card with a unique health care number.
Registration requirements include a completed application form and supporting documentation. A health care card is issued to each resident. To streamline document processing, a staggered renewal process is used. No premiums exist. Coverage under the Nunavut Medical Insurance Plan is linked to verification of registration, although every effort is made to ensure registration occurs when a coverage issue arises for an eligible resident. For non-residents, a valid health care card from their home province or territory is required.
Coverage generally begins the first day of the third month after arrival in Nunavut, but first-day coverage is provided under a number of circumstances, for example, newborns whose mothers or fathers are eligible for coverage. Permanent residents (landed immigrants), returning Canadians, repatriated Canadians, returning permanent residents, and non-Canadians who have been issued an employment visa for a period of 12 months or more, are also granted first-day coverage.
Members of the Canadian Armed Forces and inmates of a federal penitentiary are not eligible for registration. These groups are granted first-day coverage under the Nunavut Health Care Plan upon discharge.
Pursuant to section 7 of the Interprovincial Agreement on Eligibility and Portability, individuals in Nunavut who are temporarily absent from their home province or territory and who are not establishing residency in Nunavut remain covered by their home provincial or territorial health insurance plans for up to one year.
On March 31, 2024, 42,153 individuals were registered with the Nunavut Health Care Plan, an increase of 828 from the previous year. There are no formal provisions for Nunavut residents to opt-out of the Nunavut Health Care Plan, and no legislated appeals process, or policy related to appeals of residency or coverage decisions.
3.2 Other categories of individuals
Categories of individuals not eligible for coverage include:
- non-Canadian holders of employment visas of less than 12 months;
- foreign students with visas of less than 12 months;
- transient and seasonal workers;
- refugees and immigrants; and
- individuals holding a Minister's Permit (with the possible exception of those holding a temporary resident permit who may be reviewed on a case-by-case basis).
Children born out-of-country to Canadian citizens are covered only when they return to Nunavut. Returning residents (whose residency has expired) would be covered if proof of residency is provided.
When unique circumstances occur, assessments are done on an individual basis. This is consistent with section 15 of the Northwest Territories' Guidelines for Health Care Plan Registration, which was adopted by Nunavut in 1999.
4.0 Portability
4.1 Minimum waiting period
Consistent with section 3 of the Interprovincial Agreement on Eligibility and Portability, the waiting period before coverage begins for individuals moving within Canada is three months, or the first day of the third month following the establishment of residency in a new province or territory, or the first day of the third month when an individual, who has been temporarily absent from his or her home province, decides to take up permanent residency in Nunavut.
4.2 Coverage during temporary absences in Canada
The Medical Care Act, section 4(2), prescribes the benefits payable where insured medical services are provided outside Nunavut, but within Canada. The Hospital Insurance and Health and Social Services Administration Act, sections 5(d) and 28(1)(j)(o), provide the authority for the Minister of Health to enter into agreements with other jurisdictions to provide health services to Nunavut residents, and the terms and conditions of payment. No legislative or regulatory changes were made in 2023-2024 with respect to coverage outside Nunavut.
Students studying outside Nunavut must notify the Department of Health (the Department) and provide proof of enrollment to ensure continuing coverage. Requests for extensions must be renewed yearly and are subject to approval by the Director of Medical Insurance (the Director). Temporary absences for work, vacation, or other reasons for up to one year are approved by the Director upon receipt of a written request from the insured person. The Director may approve absences in excess of 12 continuous months upon receiving a written request from the insured individual.
The provisions regarding coverage during temporary absences in Canada fully comply with the terms and conditions of the Interprovincial Agreement on Eligibility and Portability. Nunavut participates in physician and hospital reciprocal billing. As well, health service agreements are in place with Ontario, Manitoba, Alberta, and the Northwest Territories. The Hospital Reciprocal Billing Agreements provide payment of in-patient and out-patient hospital services to eligible Nunavut residents receiving insured services out-of-territory. High-cost procedure rates, newborn rates, and out-patient rates are based on those established by the Interprovincial Health Insurance Agreements Coordinating Committee. The Physician Reciprocal Billing Agreements provide payment of insured physician services on behalf of eligible Nunavut residents receiving insured services out-of-territory. Payment is made to the host province or territory at the rates established by that province or territory.
4.3 Coverage during temporary absences outside Canada
The Medical Care Act, section 4(3), prescribes the benefits payable where insured medical services are provided outside Canada. The Hospital Insurance and Health and Social Services Administration Act, section 28(1)(j)(o), provides the authority for the Minister to set the terms and conditions of payment for services provided to Nunavut residents outside Canada. No amendments were made in 2023-2024 to either Act respectively. Nunavut residents are granted coverage for up to one year if they are temporarily out of the country for any reason, although they must give prior notice in writing. No exceptions are made to this process for specific categories of individuals as all cases are addressed individually. For services provided to residents who have been referred out-of-country for highly specialized procedures unavailable in Nunavut and Canada, Nunavut will pay the full cost. For 2023-2024, for emergency services, the payment for hospital services is $3,219 per day and for out-patient care it is $361 per day.
Insured physician services provided to eligible residents temporarily outside the country are paid at rates equivalent to those paid had that service been provided in the territory. Reimbursement is made to the insured individual or directly to the provider of the insured service.
4.4 Prior approval requirement
Prior approval is required to receive reimbursement for elective services provided in private facilities in Canada or in any facility outside the country. There are no processes related to pre-approval appeals for out-of-jurisdiction coverage.
5.0 Accessibility
5.1 Access to insured health services
The Medical Care Act, section 14, prohibits extra-billing by physicians unless the medical practitioner has made an election to collect fees other than those under the Medical Care Plan that is still in effect. Access to insured services is provided on uniform terms and conditions. To break down the barrier posed by distance and cost of travel, the Government of Nunavut provides medical travel assistance. Interpretation services in Inuktut are also provided to patients. The Department of Health (the Department) does not have a specific complaints office solely for extra-billing. However, the Department has other mechanisms for Nunavummiut to register concerns regarding their health care service and can be reached at:
Nunavut Health Insurance Programs Office
Department of Health
Box 889
Rankin Inlet, NU
X0C 0G0
Toll Free: 1 800-661-0833
Concerns raised regarding extra-billing that have occurred within Nunavut are fully investigated and addressed with disciplinary action if warranted. If extra-billing has occurred out-of-territory, it is up to the jurisdiction where it has occurred to investigate and address.
The Qikiqtani General Hospital, a site of Iqaluit Health Services is currently the only acute care hospital facility in Nunavut. The hospital has a total of 20 beds available for acute, medical, surgical, pediatric, rehabilitative, palliative, and chronic care services. There are also four birthing rooms, two post anesthesia care beds, and five-day surgery beds. The facility provides in-patient, out-patient, and 24-hour emergency services. On-site physicians provide emergency services on rotation. Medical services provided include: an ambulatory care/out-patient clinic emergency trauma response and stabilization services, pediatric services, and general medical, maternity, and palliative care. On-site specialists include pediatrics, general surgery, and gynecology. Visiting specialist services provided include ophthalmology, urology, orthopedics otolaryngology, and dental surgery under general anaesthesia and conscious sedation. Patients requiring complex specialized surgeries are sent to other jurisdictions. Diagnostic services include digital diagnostic imaging, laboratory, electrocardiogram, and CT scans.
Outside of Iqaluit, out-patient and 24-hour emergency nursing services are provided by local health centres in Nunavut's 24 other communities.
Nunavut has three continuing care centres located in Gjoa Haven, Igloolik and Cambridge Bay. These facilities provide full-time nursing and personal care to adults. The Gjoa Haven and Igloolik facilities have 10 beds each, and the Cambridge Bay facility has 8 beds.
Nunavut has agreements in place with a number of out-of-territory regional health authorities and specific facilities to provide medical specialists and other visiting health practitioner services. The following specialist services were provided in Nunavut during 2023-2024 under the visiting specialists program: ophthalmology, orthopedics, internal medicine, otolaryngology, neurology, rheumatology, dermatology, gynecology, urology, respirology, cardiology, total joint assessment clinic, sleep study, oral surgery, plastic surgery, and allergist. Visiting specialist clinics are scheduled in advance and are offered on specific weeks throughout the year. Due to COVID-19 restrictions, in-person specialist clinics were reduced, canceled, or postponed in response to COVID-19 outbreaks. Virtual care was used whenever feasible.
Nunavut's Telehealth network, linking all 25 communities, allows for the delivery of a broad range of services over distances including specialist consultation services such as dermatology, psychiatry and internal medicine; rehabilitation services; regularly scheduled counseling sessions; family visitation; and continuing medical education. The long-term goal is to integrate Telehealth into the primary care delivery system, enabling residents of Nunavut greater access to a broader range of service options, and allowing service providers and communities to use existing resources more effectively.
For services and equipment unavailable in Nunavut, patients are referred to other jurisdictions.
5.2 Physician compensation
All full-time physicians in Nunavut work under contract with the Department of Health (the Department). The Medical Care Act section 5.1(1) states "the Director, in accordance with this Act and the regulations, may enter into agreements, as the Director considers necessary, for services, including insured services, provided on an other than fee-for-service basis". The terms of the contracts are set by the Department. Visiting consultants are paid a daily contract rate for their professional services. Rates vary based on services rendered. The Department complies with the Financial Administration Act and Financial Administration Manual in monitoring or auditing remuneration.
5.3 Payments to hospitals
Funding for the Qikiqtani General Hospital, regional health facilities, and community health centres is provided through the Government of Nunavut's budget process.
6.0 Recognition given to federal transfers
Nunavummiut are aware of ongoing federal contributions through press releases and media coverage. The Government of Nunavut has also recognized the federal contribution provided through the Canada Health Transfer in various published documents. For fiscal year 2023-2024, they included the 2023-2024 Fiscal and Economic Indicators and the 2024-2027 Government of Nunavut and Territorial Corporations Business Plan.
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 1. Number as of March 31stFootnote 1 | 38,997 | 39,945 | 40,586 | 41,325 | 42,153 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| Public facilities | |||||
| 2. Number | 28 | 28 | 28 | 27 | 27 |
| 3. Payments for insured health services ($) |
not available | not available | not available | not available | not available |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
| Private for-profit facilities | |||||
| 4. Number of private for-profit facilities providing insured health services | 0 | 0 | 0 | 0 | 0 |
| 5. Payments to private for-profit facilities for insured health services ($) | 0 | 0 | 0 | 0 | 0 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 6. Total number of claims, in-patient | 4,139 | 4,204 | 4,043 | 3,766 | 4,043 |
| 7. Total payments, in-patient ($) | 48,802,196 | 49,827,272 | 44,278,952 | 49,289,353 | 57,964,442 |
| 8. Total number of claims, out-patient |
28,096 | 23,583 | 23,836 | 24,328 | 26,747 |
| 9. Total payments, out-patient ($) | 12,961,710 | 10,538,570 | 10,424,441 | 11,373,874 | 14,596,673 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| Pre-approved | |||||
| 10. Total number of claims, pre-approved in-patient | not available | 0 | 0 | 0 | 0 |
| 11. Total payments, pre-approved in-patient ($) | not available | 0 | 0 | 0 | 0 |
| 12. Total number of claims, pre-approved out-patient | not available | 15 | 20 | 30 | 9 |
| 13. Total payments, pre-approved out-patient ($)Footnote * | not available | 16,377 | 16,830 | 37,851 | 11,194 |
| Non pre-approved | |||||
| 14. Total number of claims, non pre-approved in-patient | not available | 0 | 0 | 0 | 0 |
| 15. Total payments, non pre-approved in-patient ($) | not available | 0 | 0 | 0 | 0 |
| 16. Total number of claims, non pre-approved out-patient | not available | 0 | 0 | 0 | 0 |
| 17. Total payments, non pre-approved out-patient ($) | not available | 0 | 0 | 0 | 0 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 18. Number of participating physicians | 177Footnote 3 | 138Footnote 3 | 127Footnote 3 | 170Footnote 3 | 142Footnote 3 |
| 19. Number of opted-out physicians | 0 | 0 | 0 | 0 | 0 |
| 20.
Number of non-participating physicians |
0 | 0 | 0 | 0 | 0 |
| 21. Total payments for services provided by physicians paid through all payment methods ($) | not available | not available | not available | not available | not available |
| 22. Total payments for services provided by physicians paid through fee-for-service ($)Footnote 4 | 870,135 | 801,070 | 0 | 0 | 0 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| 23. Number of services | 128,069 | 113,217 | 122,616 | 136,168 | 142,780 |
| 24. Total payments ($) | 10,208,947 | 9,127,352 | 9,454,239 | 10,561,554 | 10,694,238 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|---|---|
| Pre-approved | |||||
| 25. Number of pre-approved services | not applicable | 0 | 0 | 0 | 0 |
| 26. Total pre-approved payments ($) | not applicable | 0 | 0 | 0 | 0 |
| Non pre-approved | |||||
| 27. Number of non pre-approved services | 11 | 0 | 0 | 2 | 2 |
| 28. Total non pre-approved payments ($) | 678 | 0 | 0 | 181 | 153 |
| 2019-2020 | 2020-2021 | 2021-2022 | 2022-2023 | 2023-2024 | |
| 29. Number of participating dentists | not available | not available | not available | not available | not available |
| 30. Number of opted-out dentists | not available | not available | not available | not available | not available |
| 31.
Number of non-participating dentists |
not available | not available | not available | not available | not available |
| 32. Number of services provided | not available | not available | not available | not available | not available |
| 33. Total payments ($) | not available | not available | not available | not available | not available |
|
|||||
Annex A - Canada Health Act and Extra-Billing and User Charges Information Regulations
This annex provides the reader with an office consolidation of the Canada Health Act and the Extra-billing and User Charges Information Regulations. An office consolidation is a rendering of the original Act, which includes any amendments that have been made since the Act's passage. The only regulations in force under the Act are the Extra-billing and User Charges Information Regulations. These Regulations require the provinces and territories to provide estimates of extra-billing and user charges prior to the beginning of each fiscal year so that appropriate penalties can be levied, as well as financial statements showing the amounts actually charged so that reconciliations with any estimated charges can be made. These Regulations are also presented in an office consolidation format. This unofficial consolidation is not necessarily current and is provided for the convenience of the reader only. For the official text of the Canada Health Act, please contact Justice Canada.
Links to Canada Health Act and Regulations:
Annex B - Policy interpretation letters
There are four key policy statements that clarify the federal position on the Canada Health Act. These statements were made in the form of ministerial letters from federal Health Ministers to their provincial and territorial counterparts.
[Following is the text of the letter sent on June 18, 1985, to all provincial and territorial Ministers of Health by the Honourable Jake Epp, federal Minister of Health and Welfare. (Note: Minister Epp sent the French equivalent of this letter to Quebec on July 15, 1985.) ]
June 18, 1985
Ottawa, K1A 0K9
Dear Minister:
Having consulted with all provincial and territorial Ministers of Health over the past several months, both individually and at the meeting in Winnipeg on May 16 and 17, I would like to confirm for you my intentions regarding the interpretation and implementation of the Canada Health Act. I would particularly appreciate if you could provide me with a written indication of your views on the attached proposals for regulations in order that I may act to have these officially put in place as soon as conveniently possible. Also, I will write to you further with regard to the material I will need to prepare the required annual report to Parliament.
As indicated at our meeting in Winnipeg, I intend to honour and respect provincial jurisdiction and authority in matters pertaining to health and the provision of health care services. I am persuaded, by conviction and experience, that more can be achieved through harmony and collaboration than through discord and confrontation.
With regard to the Canada Health Act, I can only conclude from our discussions that we together share a public trust and are mutually and equally committed to the maintenance and improvement of a universal, comprehensive, accessible and portable health insurance system, operated under public auspices for the benefit of all residents of Canada.
Our discussions have reinforced my belief that you require sufficient flexibility and administrative versatility to operate and administer your health care insurance plans. You know far better than I ever can, the needs and priorities of your residents, in light of geographic and economic considerations. Moreover, it is essential that provinces have the freedom to exercise their primary responsibility for the provision of personal health care services.
At the same time, I have come away from our discussions sensing a desire to sustain a positive federal involvement and role—both financial and otherwise—to support and assist provinces in their efforts dedicated to the fundamental objectives of the health care system: protecting, promoting and restoring the physical and mental well-being of Canadians. As a group, provincial/territorial Health Ministers accept a co-operative partnership with the federal government based primarily on the contributions it authorizes for purposes of providing insured and extended health care services.
I might also say that the Canada Health Act does not respond to challenges facing the health care system. I look forward to working collaboratively with you as we address challenges such as rapidly advancing medical technology and an aging population and strive to develop health promotion strategies and health care delivery alternatives.
Returning to the immediate challenge of implementing the Canada Health Act, I want to set forth some reasonably comprehensive statements of federal policy intent, beginning with each of the criteria contained in the Act.
Public Administration
This criterion is generally accepted. The intent is that the provincial health care insurance plans be administered by a public authority, accountable to the provincial government for decision-making on benefit levels and services, and whose records and accounts are publicly audited.
Comprehensiveness
The intent of the Canada Health Act is neither to expand nor contract the range of insured services covered under previous federal legislation. The range of insured services encompasses medically necessary hospital care, physician services and surgical-dental services which require a hospital for their proper performance. Hospital plans are expected to cover in-patient and out-patient hospital services associated with the provision of acute, rehabilitative and chronic care. As regards physician services, the range of insured services generally encompasses medically required services rendered by licensed medical practitioners as well as surgical-dental procedures that require a hospital for proper performance. Services rendered by other health care practitioners, except those required to provide necessary hospital services, are not subject to the Act's criteria.
Within these broad parameters, provinces, along with medical professionals, have the prerogative and responsibility for interpreting what physician services are medically necessary. As well, provinces determine which hospitals and hospital services are required to provide acute, rehabilitative or chronic care.
Universality
The intent of the Canada Health Act is to ensure that all bonafide residents of all provinces be entitled to coverage and to the benefits under one of the twelve provincial/territorial health care insurance plans. However, eligible residents do have the option not to participate under a provincial plan should they elect to do so.
The Agreement on Eligibility and Portability provides some helpful guidelines with respect to the determination of residency status and arrangements for obtaining and maintaining coverage. Its provisions are compatible with the Canada Health Act.
I want to say a few words about premiums. Unquestionably, provinces have the right to levy taxes and the Canada Health Act does not infringe upon that right. A premium scheme per se is not precluded by the Act, provided that the provincial health care insurance plan is operated and administered in a manner that does not deny coverage or preclude access to necessary hospital and physician services to bonafide residents of a province. Administrative arrangements should be such that residents are not precluded from or do not forego coverage by reason of an inability to pay premiums.
I am acutely aware of problems faced by some provinces in regard to tourists and visitors who may require health services while travelling in Canada. I will be undertaking a review of the current practices and procedures with my Cabinet colleagues, the Minister of External Affairs, and the Minister of Employment and Immigration, to ensure all reasonable means are taken to inform prospective visitors to Canada of the need to protect themselves with adequate health insurance coverage before entering the country.
In summary, I believe all of us as Ministers of Health are committed to the objective of ensuring that all duly qualified residents of a province obtain and retain entitlement to insured health services on uniform terms and conditions.
Portability
The intent of the portability provisions of the Canada Health Act is to provide insured persons continuing protection under their provincial health care insurance plan when they are temporarily absent from their province of residence or when moving from province to province. While temporarily in another province of Canada, bonafide residents should not be subject to out-of-pocket costs or charges for necessary hospital and physician services. Providers should be assured of reasonable levels of payment in respect of the cost of those services.
Insofar as insured services received while outside of Canada are concerned, the intent is to assure reasonable indemnification in respect of the cost of necessary emergency hospital or physician services or for referred services not available in a province or in neighbouring provinces. Generally speaking, payment formulae tied to what would have been paid for similar services in a province would be acceptable for purposes of the Canada Health Act.
In my discussions with provincial/territorial Ministers, I detected a desire to achieve these portability objectives and to minimize the difficulties that Canadians may encounter when moving or travelling about in Canada. In order that Canadians may maintain their health insurance coverage and obtain benefits or services without undue impediment, I believe that all provincial/territorial Health Ministers are interested in seeing these services provided more efficiently and economically.
Significant progress has been made over the past few years by way of reciprocal arrangements which contribute to the achievement of the in-Canada portability objectives of the Canada Health Act. These arrangements do not interfere with the rights and prerogatives of provinces to determine and provide the coverage for services rendered in another province. Likewise, they do not deter provinces from exercising reasonable controls through prior approval mechanisms for elective procedures. I recognize that work remains to be done respecting interprovincial payment arrangements to achieve this objective, especially as it pertains to physician services.
I appreciate that all difficulties cannot be resolved overnight and that provincial plans will require sufficient time to meet the objective of ensuring no direct charges to patients for necessary hospital and physician services provided in other provinces.
For necessary services provided out-of-Canada, I am confident that we can establish acceptable standards of indemnification for essential physician and hospital services. The legislation does not define a particular formula and I would be pleased to have your views.
In order that our efforts can progress in a coordinated manner, I would propose that the Federal-Provincial Advisory Committee on Institutional and Medical Services be charged with examining various options and recommending arrangements to achieve the objectives within one year.
Reasonable Accessibility
The Act is fairly clear with respect to certain aspects of accessibility. The Act seeks to discourage all point-of-service charges for insured services provided to insured persons and to prevent adverse discrimination against any population group with respect to charges for, or necessary use of, insured services. At the same time, the Act accents a partnership between the providers of insured services and provincial plans, requiring that provincial plans have in place reasonable systems of payment or compensation for their medical practitioners in order to ensure reasonable access to users. I want to emphasize my intention to respect provincial prerogatives regarding the organization, licensing, supply, distribution of health manpower, as well as the resource allocation and priorities for health services. I want to assure you that the reasonable access provision will not be used to intervene or interfere directly in matters such as the physical and geographic availability of services or provincial governance of the institutions and professions that provide insured services. Inevitably, major issues or concerns regarding access to health care services will come to my attention. I want to assure you that my Ministry will work through and with provincial/territorial Ministers in addressing such matters.
My aim in communicating my intentions with respect to the criteria in the Canada Health Act is to allow us to work together in developing our national health insurance scheme. Through continuing dialogue, open and willing exchange of information and mutually understood rules of the road, I believe that we can implement the Canada Health Act without acrimony and conflict. It is my preference that provincial/territorial Ministers themselves be given an opportunity to interpret and apply the criteria of the Canada Health Act to their respective health care insurance plans. At the same time, I believe that all provincial/territorial Health Ministers understand and respect my accountability to the Parliament of Canada, including an annual report on the operation of provincial health care insurance plans with regard to these fundamental criteria.
Conditions
This leads me to the conditions related to the recognition of federal contributions and to the provision of information, both of which may be specified in regulations. In these matters, I will be guided by the following principles:
- to make as few regulations as possible and only if absolutely necessary;
- to rely on the goodwill of Ministers to afford appropriate recognition of Canada's role and contribution and to provide necessary information voluntarily for purposes of administering the Act and reporting to Parliament;
- to employ consultation processes and mutually beneficial information exchanges as the preferred ways and means of implementing and administering the Canada Health Act;
- to use existing means of exchanging information of mutual benefit to all our governments.
Regarding recognition by provincial/territorial governments of federal health contributions, I am satisfied that we can easily agree on appropriate recognition, in the normal course of events. The best form of recognition in my view is the demonstration to the public that as Ministers of Health we are working together in the interests of the taxpayer and patient.
In regard to information, I remain committed to maintaining and improving national data systems on a collaborative and co-operative basis. These systems serve many purposes and provide governments, as well as other agencies, organizations, and the general public, with essential data about our health care system and the health status of our population. I foresee a continuing, co-operative partnership committed to maintaining and improving health information systems in such areas as morbidity, mortality, health status, health services operations, utilization, health care costs and financing.
I firmly believe that the federal government need not regulate these matters. Accordingly, I do not intend to use the regulatory authority respecting information requirements under the Canada Health Act to expand, modify or change these broad-based data systems and exchanges. In order to keep information flows related to the Canada Health Act to an economical minimum, I see only two specific and essential information transfer mechanisms:
- estimates and statements on extra-billing and user charges;
- an annual provincial statement (perhaps in the form of a letter to me) to be submitted approximately six months after the completion of each fiscal year, describing the respective provincial health care insurance plan's operations as they relate to the criteria and conditions of the Canada Health Act.
Concerning Item 1 above, I propose to put in place on-going regulations that are identical in content to those that have been accepted for 1985-86. Draft regulations are attached as Annex I. To assist with the preparation of the "annual provincial statement" referred to in Item 2 above, I have developed the general guidelines attached as Annex II. Beyond these specific exchanges, I am confident that voluntary, mutually beneficial exchange of such subjects as Acts, regulations and program descriptions will continue.
One matter brought up in the course of our earlier meetings, is the question of whether estimates or deductions of user charges and extra-billing should be based on "amounts charged" or "amounts collected". The Act clearly states that deductions are to be based on amounts charged. However, with respect to user fees, certain provincial plans appear to pay these charges indirectly on behalf of certain individuals. Where a provincial plan demonstrates that it reimburses providers for amounts charged but not collected, say in respect of social assistance recipients or unpaid accounts, consideration will be given to adjusting estimates/deductions accordingly.
I want to emphasize that where a provincial plan does authorize user charges, the entire scheme must be consistent with the intent of the reasonable accessibility criterion as set forth [in this letter].
Regulations
Aside from the recognition and information regulations referred to above, the Act provides for regulations concerning hospital services exclusions and regulations defining extended health care services.
As you know, the Act provides that there must be consultation and agreement of each and every province with respect to such regulations. My consultations with you have brought to light few concerns with the attached draft set of Exclusions from Hospital Services Regulations.
Likewise, I did not sense concerns with proposals for regulations defining Extended Health Care Services. These help provide greater clarity for provinces to interpret and administer current plans and programs. They do not alter significantly or substantially those that have been in force for eight years under Part VI of the Federal Post-Secondary Education and Health Contributions Act (1977). It may well be, however, as we begin to examine the future challenges to health care that we should re-examine these definitions.
This letter strives to set out flexible, reasonable and clear ground rules to facilitate provincial, as much as federal, administration of the Canada Health Act. It encompasses many complex matters including criteria interpretations, federal policy concerning conditions and proposed regulations. I realize, of course, that a letter of this sort cannot cover every single matter of concern to every provincial Minister of Health. Continuing dialogue and communication are essential.
In conclusion, may I express my appreciation for your assistance in bringing about what I believe is a generally accepted concurrence of views in respect of interpretation and implementation. As I mentioned at the outset of this letter, I would appreciate an early written indication of your views on the proposals for regulations appended to this letter. It is my intention to write to you in the near future with regard to the voluntary information exchanges which we have discussed in relation to administering the Act and reporting to Parliament.
Yours truly,
Jake Epp
Attachments
[Following is the text of the letter sent on January 6, 1995, to all provincial and territorial Ministers of Health by the federal Minister of Health, the Honourable Diane Marleau.]
January 6, 1995
Dear Minister:
RE: Canada Health Act
The Canada Health Act has been in force now for just over a decade. The principles set out in the Act (public administration, comprehensiveness, universality, portability and accessibility) continue to enjoy the support of all provincial and territorial governments. This support is shared by the vast majority of Canadians. At a time when there is concern about the potential erosion of the publicly funded and publicly administered health care system, it is vital to safeguard these principles.
As was evident and a concern to many of us at the recent Halifax meeting, a trend toward divergent interpretations of the Act is developing. While I will deal with other issues at the end of this letter, my primary concern is with private clinics and facility fees. The issue of private clinics is not new to us as Ministers of Health; it formed an important part of our discussions in Halifax last year. For reasons I will set out below, I am convinced that the growth of a second tier of health care facilities providing medically necessary services that operate, totally or in large part, outside the publicly funded and publicly administered system, presents a serious threat to Canada's health care system.
Specifically, and most immediately, I believe the facility fees charged by private clinics for medically necessary services are a major problem which must be dealt with firmly. It is my position that such fees constitute user charges and, as such, contravene the principle of accessibility set out in the Canada Health Act.
While there is no definition of facility fees in federal or most provincial legislation, the term, generally speaking, refers to amounts charged for non-physician (or "hospital") services provided at clinics and not reimbursed by the province. Where these fees are charged for medically necessary services in clinics which receive funding for these services under a provincial health insurance plan, they constitute a financial barrier to access. As a result, they violate the user charge provision of the Act (section 19).
Facility fees are objectionable because they impede access to medically necessary services. Moreover, when clinics which receive public funds for medically necessary services also charge facility fees, people who can afford the fees are being directly subsidized by all other Canadians. This subsidization of two-tier health care is unacceptable.
The formal basis for my position on facility fees is twofold. The first is a matter of policy. In the context of contemporary health care delivery, an interpretation which permits facility fees for medically necessary services so long as the provincial health insurance plan covers physician fees runs counter to the spirit and intent of the Act. While the appropriate pro-vision of many physician services at one time required an overnight stay in a hospital, advances in medical technology and the trend toward providing medical services in more accessible settings has made it possible to offer a wide range of medical procedures on an out-patient basis or outside of full-service hospitals. The accessibility criterion in the Act, of which the user charge provision is just a specific example, was clearly intended to ensure that Canadian residents receive all medically necessary care without financial or other barriers and regardless of venue. It must continue to mean that as the nature of medical practice evolves.
Second, as a matter of legal interpretation, the definition of "hospital" set out in the Act includes any facility which provides acute, rehabilitative or chronic care. This definition covers those health care facilities known as "clinics". As a matter of both policy and legal interpretation, therefore, where a provincial plan pays the physician fee for a medically necessary service delivered at a clinic, it must also pay for the related hospital services provided or face deductions for user charges.
I recognize that this interpretation will necessitate some changes in provinces where clinics currently charge facility fees for medically necessary services. As I do not wish to cause undue hardship to those provinces, I will commence enforcement of this interpretation as of October 15, 1995. This will allow the provinces the time to put into place the necessary legislative or regulatory framework. As of October 15, 1995, I will proceed to deduct from transfer payments any amounts charged for facility fees in respect of medically necessary services, as mandated by section 20 of the Canada Health Act. I believe this provides a reasonable transition period, given that all provinces have been aware of my concerns with respect to private clinics for some time, and given the promising headway already made by the Federal/Provincial/Territorial Advisory Committee on Health Services, which has been working for some time now on the issue of private clinics.
I want to make it clear that my intent is not to preclude the use of clinics to provide medically necessary services. I realize that in many situations they are a cost-effective way to deliver services, often in a technologically advanced manner. However, it is my intention to ensure that medically necessary services are provided on uniform terms and conditions, wherever they are offered. The principles of the Canada Health Act are supple enough to accommodate the evolution of medical science and of health care delivery. This evolution must not lead, however, to a two-tier system of health care.
I indicated earlier in this letter that, while user charges for medically necessary services are my most immediate concern, I am also concerned about the more general issues raised by the proliferation of private clinics. In particular, I am concerned about their potential to restrict access by Canadian residents to medically necessary services by eroding our publicly funded system. These concerns were reflected in the policy statement which resulted from the Halifax meeting. Ministers of Health present, with the exception of the Alberta Minister, agreed to:
- take whatever steps are required to regulate the development of private clinics in Canada, and to maintain a high quality, publicly funded medicare system.
Private clinics raise several concerns for the federal government, concerns which provinces share. These relate to:
- weakened public support for the tax funded and publicly administered system;
- the diminished ability of governments to control costs once they have shifted from the public to the private sector;
- the possibility, supported by the experience of other jurisdictions, that private facilities will concentrate on easy procedures, leaving public facilities to handle more complicated, costly cases; and
- the ability of private facilities to offer financial incentives to health care providers that could draw them away from the public system—resources may also be devoted to features which attract consumers, without in any way contributing to the quality of care.
The only way to deal effectively with these concerns is to regulate the operation of private clinics.
I now call on Ministers in provinces which have not already done so to introduce regulatory frameworks to govern the operation of private clinics. I would emphasize that, while my immediate concern is the elimination of user charges, it is equally important that these regulatory frameworks be put in place to ensure reasonable access to medically necessary services and to support the viability of the publicly funded and administered system in the future. I do not feel the implementation of such frameworks should be long delayed.
I welcome any questions you may have with respect to my position on private clinics and facility fees. My officials are willing to meet with yours at any time to discuss these matters. I believe that our officials need to focus their attention, in the coming weeks, on the broader concerns about private clinics referred to above.
As I mentioned at the beginning of this letter, divergent interpretations of the Canada Health Act apply to a number of other practices. It is always my preference that matters of interpretation of the Act be resolved by finding a Federal/Provincial/Territorial consensus consistent with its fundamental principles. I have therefore encouraged F/P/T consultations in all cases where there are disagreements. In situations such as out-of-province or out-of-country coverage, I remain committed to following through on these consultative processes as long as they continue to promise a satisfactory conclusion in a reasonable time.
In closing, I would like to quote Mr. Justice Emmett M. Hall. In 1980, he reminded us:
"we, as a society, are aware that the trauma of illness, the pain of surgery, the slow decline to death, are burdens enough for the human being to bear without the added burden of medical or hospital bills penalizing the patient at the moment of vulnerability."
I trust that, mindful of these words, we will continue to work together to ensure the survival, and renewal, of what is perhaps our finest social project.
As the issues addressed in this letter are of great concern to Canadians, I intend to make this letter publicly available once all provincial Health Ministers have received it.
Yours sincerely,
Diane Marleau
Minister of Health
[Following is the text of the letter sent on August 8, 2018, to all provincial and territorial Ministers of Health by the federal Minister of Health, the Honourable Ginette Petitpas Taylor.]
Dear Minister,
It was a pleasure to see you recently at our Federal/Provincial/Territorial Health Ministers' Meeting in Winnipeg. As I have explained, when I was appointed as federal Health Minister, the Prime Minister tasked me with promoting and defending the Canada Health Act and quite specifically with eliminating patient charges for services that should be publicly insured. As you are aware, I have taken this responsibility seriously.
Following our conversations earlier this year, I was pleased to hear that all provinces and territories participated in officials' level discussions convened by Health Canada this Spring. We fine-tuned our approach based on the feedback provided in a series of multi- and bilateral meetings.
The purpose of this letter is to formally advise that I am proceeding with the three Canada Health Act initiatives I discussed with you. Taken together, the Diagnostic Services Policy, the Reimbursement Policy, and strengthened reporting, will provide me with tools to effectively administer the Act in the interest of all Canadians.
Diagnostic Services Policy
One of the overarching objectives of the Canada Health Act is to ensure that Canadians have access to medically necessary care based on their health needs and not their ability or willingness to pay. However, in many jurisdictions patients are charged for medically necessary diagnostic services provided at private clinics. Since the inception of the Canada Health Act, the federal position has always been that all medically necessary physician and hospital services – including diagnostic services – must be covered by provincial and territorial health insurance plans.
If an authorized provider has referred a patient for a medically necessary diagnostic test, the status of the procedure as a publicly insured service should not change simply because the service is delivered in a private clinic rather than in a hospital. I do not accept the premise that since some patients are willing to pay for expedited access to medically necessary services, they should be provided with a venue to do so. This practice results in patients jumping the queue twice – first, for the diagnostic service itself and then for any follow-up care that may be required. Simply put, this is not fair and goes against the fundamental principle of Canadian health care – that is, that access should be based on health need, not on the ability or willingness, to pay.
The Canada Health Act does not preclude the private delivery of insured services. Many insured health services are provided to Canadians in private clinics and are paid for by the provincial or territorial health insurance plan. As long as there are no patient charges, provinces and territories can provide insured services as they best see fit. However, my clarification of the status of medically necessary diagnostic services through this letter means, in effect, that any charges to patients for these services will be considered to be in contravention of the Canada Health Act.
I fully appreciate that it may take time in some jurisdictions to align provincial and territorial systems with the Diagnostic Services Policy. As I indicated in Winnipeg, the policy will not take effect until April 1, 2020 and reporting on any patient charges for diagnostic services will begin in December 2022 (for the fiscal year 2020-21). That would mean, in accordance with the Canada Health Act, that any Canada Health Transfer deductions would only be made in March 2023. If, in the interim, a jurisdiction has eliminated patient charges for diagnostic services, that jurisdiction would be eligible for reimbursement of deducted funds through the new Reimbursement Policy.
Reimbursement Policy
The Canada Health Act was enacted to eliminate the unfair practice of patient charges. The Act is clear – when a province allows patient charges, mandatory deductions to federal transfer payments must be made. During the first three years of the Canada Health Act, a provision in the Act allowed deductions to be refunded if the jurisdiction took the necessary steps to eliminate patient charges for services which should be publicly insured. This proved effective, and by 1987, patient charges were eliminated for most hospital and physician services across Canada. However, when this refund provision expired, the incentive structure under the Act went from a positive one, to a purely negative one. I believe this needs to change.
With the aim of emulating the success of the original refund provision, I am introducing a new Reimbursement Policy. Going forward, provinces and territories would be eligible to be reimbursed for deductions taken in respect of patient charges, should they demonstrate they have taken action to remove these barriers to access. The attached document provides details on the scope and application of the Policy. Any deductions made starting from March 2018 will be eligible for reimbursement under this Policy.
Strengthened Reporting
Finally, in order to ensure that I have the information needed to administer the Act in an even-handed manner and in order to report to Canadians on the state of their publicly funded health care insurance system, reporting from provinces and territories to Health Canada and from Health Canada to Canadians will be strengthened and standardized. Details, which were discussed with your officials this past Spring, will be communicated by my Deputy in the coming weeks. Again, respecting that a new approach cannot be instituted overnight, we will phase in the new reporting measures.
Canadians are rightfully proud of their health care system and have high expectations that their governments will work together to protect their access to it. I am confident these initiatives will help us meet that challenge and will safeguard our universal health care system for future generations.
I have appreciated our discussions to date and look forward to ongoing collaboration.
Yours sincerely,
The Honourable Ginette Petitpas Taylor, P.C., M.P.
Reimbursement Policy for Provinces and Territories - Subject to Deductions under the Canada Health Act (the Reimbursement Policy)
Background
A fundamental premise of the Canadian health care system is that Canadians should have access to medically necessary physician and hospital services unimpeded by financial or other barriers. The Canada Health Act (CHA) was enacted in response to a growing concern that access to publicly insured health care services was increasingly undermined by point of service charges to patients.
The CHA established the conditions and criteria provinces must meet in order to qualify for their full cash contribution under the Canada Health Transfer (CHT). The Act also established discretionary and mandatory deductions for violations of the CHA principles and the extra-billing and user charges (EBUC) provisions of the Act, respectively. The Minister is required to make dollar-for-dollar deductions to a province's or territory's (PT's) CHT payments when EBUC are permitted. The intent of the CHA with respect to deductions is to encourage compliance with the Act and its objective of ensuring Canadians' access to health care services on uniform terms and conditions and without financial barriers.
At the time the CHA came into force, many jurisdictions had legal frameworks for public health insurance which either explicitly allowed EBUC to be levied on patients, or, by convention, had permitted such fees to become entrenched in their health care systems. In view of these factors, it was acknowledged that it would take time for PTs to align their systems with the values and requirements of the CHA. The Act, therefore, included a provision for the first three years (1984-1987) which, in effect, provided refunds of amounts deducted from federal transfers for EBUC violations once the PT succeeded in eliminating EBUC.
PTs adopted legislation governing their public health insurance systems which mirrored, and in most cases went well beyond, the requirements of the CHA. As a result, over $244 million was refunded to seven PTs in respect of patient charges levied in the 1984-1987 period. The advent of the CHA, including the refund provision, helped eliminate EBUC for a considerable period of time in most parts of the country and in most care settings.
Time for a new Reimbursement Policy
Despite provisions discouraging or prohibiting EBUC in both federal and PT legislation, there are still instances of patients paying for access to insured health care services in some jurisdictions. As was the case in 1984, these charges put at risk the fundamental value of universal access to health care.
Some jurisdictions have been active in investigating allegations of patient charges, adopting legislative and regulatory measures to deter EBUC, ensuring that patients are reimbursed and that providers or institutions who contravene PT law (and the CHA) are disciplined. These governments are to be commended for their vigilance on behalf of patients.
Given the success of the original refund provision of the CHA in eliminating EBUC, the federal government is implementing a new Reimbursement Policy for Provinces and Territories Subject to Deductions under the Canada Health Act (the Reimbursement Policy). Under this new policy, if a province or territory is subject to a deduction, the federal Minister of Health has the discretion to provide a reimbursement if the PT comes into compliance with the Act by the end of the calendar year.
Current process
Under the CHA's Extra-billing and User Charges Information Regulations (the Regulations), PTs are obligated to report to Health Canada on EBUC occurring within their jurisdiction. This takes the form of a financial statement submitted each year, by December 16, which describes any EBUC activity occurring in the fiscal year two years previous. If the Minister does not receive a statement, or believes the information was not provided in accordance with the Regulations, the Act obligates the Minister to estimate an amount after consultation with the PT. The CHT payments to the jurisdiction are then reduced by a corresponding amount in March of the following year.
Working together to eliminate patient charges
The objective of the Reimbursement Policy is to work collaboratively with PTs subject to a CHT deduction to ultimately eliminate these patient charges. When a PT is informed it will be subject to a CHT deduction for EBUC (typically in January/February), the conditions for reimbursement will also be outlined. In instances where the PT has already eliminated patient charges and a sufficient period of time has elapsed to assure Health Canada that the circumstances that led to these charges have been addressed, reimbursement may be made immediately. Where such charges are ongoing, Health Canada will work with PT officials on the elements of an action plan to meet the conditions for reimbursement. Action plans, and PT progress on meeting them, will be published in the Canada Health Act Annual Report.
To be considered for reimbursement, the jurisdiction would need to demonstrate it has followed through on the agreed upon action plan within the specified time period – typically 12 months but no more than two years following the initial deduction. Because the circumstances leading to deductions will vary from province to province, so will the action plans. Nonetheless, it is expected that all action plans will require the PT to submit the following documents to Health Canada in the January following the deduction:
- A financial statement of any EBUC levied in the jurisdiction since the deduction
- A report on the steps the jurisdiction has taken to eliminate EBUC, and how these charges have been addressed
- An attestation as to the completeness and accuracy of the information submitted
Upon review of the jurisdiction's report, if the Minister is satisfied that the elements of the action plan have been fulfilled, the PT would receive a reimbursement. However, if the Minister is not satisfied that the conditions were fulfilled, no reimbursement would occur and the deduction amount would be forfeited. Following an initial deduction and reimbursement cycle, if the Minister remains satisfied that appropriate action has been taken, the Reimbursement Policy would allow for the immediate reimbursement of subsequent CHT deductions.
In order to qualify for continued consideration under the Reimbursement Policy, a PT must also comply with the regular reporting requirements set out in the Regulations and submit an accurate EBUC financial statement to Health Canada in the December following the CHT deduction and commit to doing so on an annual basis going forward.
[Following is the text of the letter sent on January 9, 2025, to all provincial and territorial Ministers of Health by the federal Minister of Health, the Honourable Mark Holland.]
To all Provincial and Territorial Ministers of Health
Dear Ministers:
Evolutions in health care delivery have the potential to improve how care is provided to meet the health care needs of people in Canada. It is clear from discussions to date that all governments support advances that help to ensure Canadians can get the care they need, when they need it.
In 2023, the Prime Minister and Premiers agreed on shared health priorities to deliver real results to Canadians, supported by additional federal health investments of close to $200 billion over 10 years. I am pleased that we have worked together to sign bilateral agreements with all jurisdictions. The Working Together to Improve Health Care for Canadians Plan emphasizes the importance of upholding the Canada Health Act (CHA) to protect Canada's publicly funded health care system.
A key aspect in upholding these principles is to ensure that patients do not face charges for medically necessary care when a service would otherwise be covered if provided by a physician. When innovations are introduced into our health care system, it is important to ensure that they benefit all Canadians equally. Unfortunately, over the past few years we have seen that this is not the case in all circumstances and is resulting in patients being charged for medically necessary care.
Physician-equivalent services and the core basket of services
There has been an expansion in scopes of practice for many regulated health care professionals (e.g. nurse practitioners, pharmacists, midwives) to better utilize the full extent of their competencies, knowledge and skills to increase access to needed care. This now permits these professionals to deliver some of the same services that would normally be insured if provided by a physician. In no area has this been more evident than in team-based primary care where nurse practitioners, in particular, are being integrated more fully into the primary care system, greatly increasing access for Canadians while helping to relieve pressure.
Nurse practitioners are now able to practise autonomously—diagnosing, treating, prescribing and referring patients—mirroring many of the tasks of a primary care physician, and in some cases, becoming the sole primary care provider for many Canadians, particularly in rural and remote communities. These developments support the CHA's objective of reasonable access to medically necessary care.
However, increasingly, there are reports of the growth of patient charges arising from health care professionals offering medically necessary services to Canadians on a private pay basis. If left unchecked, more and more Canadians could be required to pay to access care services that would otherwise be insured if delivered by a physician.
CHA Services Policy
I want to acknowledge the work of the provinces and territories in increasing patients' access to care through expanding the scope of practice of health care professionals, such as pharmacists and nurse practitioners. I also want to ensure access to these services remains based on medical need, and not a patient's ability or willingness to pay.
As such, when the CHA Services Policy is implemented, patient charges for medically necessary services, whether provided by a physician or other health care professional providing physician-equivalent services, will be considered extra-billing and user charges under the CHA.
The purpose of this policy is not to expand the core basket of services insured under the CHA. It is, instead, to maintain the basket by ensuring patients are not charged for services that would otherwise be provided without charges if delivered by a physician. As such, this policy does not include regulated health providers who had an overlapping scope of practice with physicians prior to the enactment of the CHA in 1984, and whose services were not considered insured at that time. The core basket of insured services remains the same regardless of who is providing the provincially or territorially regulated services.
Implementation
In order to give provincial and territorial governments sufficient time to review the administration of their health care plans and make any necessary adjustments, the CHA Services Policy will come into effect on April 1, 2026.
The federal government will work with provinces and territories on developing measures to collect the information required to implement this policy in an open and transparent manner. To collect the information required to respect the reporting obligations under the CHA's Extra-Billing and User Charges Information Regulations, the provinces and territories will be required to report patient charges under this new policy for the first time in December 2028.
I would like to underline that the federal goal of the CHA is not to levy penalties, but to ensure access to medically necessary care. Therefore, any deductions made under the policy will be eligible for reimbursement under the CHA Reimbursement Policy, once patient charges and the circumstances that led to them are eliminated.
I would also like to take the opportunity to commend all provinces and territories for the significant work undertaken to date to integrate virtual care services, delivered by physicians, into their health insurance plans. I encourage all jurisdictions to continue down this path. I look forward to the opportunity to further discussing the integration of virtual care at our upcoming Health Ministers' Meeting.
I am also aware that, in some cases, private surgical clinics are offering patients opportunities to jump the queue for surgical procedures that are not an emergency (e.g. cataract surgery, knee or hip replacements, hernia repair) by accessing care outside their home province or territory for a fee. I am concerned that this practice could undermine the fundamental principle of Medicare, where access to care should be based on health need rather than the ability or willingness to pay. That is why I have directed departmental officials to continue working with you to closely monitor this issue.
Our publicly funded health care system is dynamic, and can benefit from innovation while remaining true to the fundamental principle of Medicare. By embracing positive evolution while ensuring access based on need, I am confident we can keep delivering improvements in the health care system that will benefit all Canadians.
Please accept my best wishes.
Yours sincerely,
The Honourable Mark Holland, P.C., M.P.
Annex C - Financial statements of actual amounts of extra-billing and user charges for the period April 1, 2021 to March 31, 2022
The Canada Health Act and Extra-billing and User Charges Information Regulations require provinces/territories to report annually to the federal Minister of Health. This report takes the form of a financial statement of actual amounts of extra-billing and user charges levied in the province/territory for the fiscal year in question, along with an explanation regarding the method used to determine the reported amount as indicated in below.
The information reported in the financial statements may be used to determine amounts deducted from the Canada Health Transfer payments of a province/territory where extra-billing and user charges are occurring. However, pursuant to Section 20 of the Act, the federal Minister of Health may estimate amounts of extra-billing and user charges levied, if there is evidence that the information reported in the financial statement does not accurately reflect amounts actually charged to patients in the province or territory.
Under the Act, extra-billing is defined as a charge by an enrolled physician or dentist to an insured person for an insured service in addition to the amount paid by the provincial/territorial health care insurance plan.
Under the Act, a user charge is defined as any charge for an insured health service, other than extra-billing. This includes any charge levied for insured hospital services, provided in hospital or at a non-hospital facility (e.g., private surgical or diagnostic clinic), or any non-physician related services provided in conjunction with an insured physician service at a non-hospital facility (e.g., private surgical or diagnostic clinic or private practice).
While Quebec did not submit a financial statement in the standard form provided, amounts of extra-billing and user charges levied in the province during 2021-2022 was confirmed in the form of a letter, which is reproduced in this annex.
- N.B. Charges may be levied for accommodation and meal costs related to a patient who, in the opinion of the attending physician, is a permanent resident in a hospital or other chronic care institution as per the limitation of Section 19 (2). Charges related to this limitation should not be included in the financial statement.
Newfoundland and Labrador
Canada Health Act
Financial statement of actual amounts of extra-billing and user charges
For the period April 1, 2021 to March 31, 2022
- Amounts of extra-billing
Extra-billing is defined as a charge by an enrolled physician or dentist to an insured person for an insured service in addition to the amount paid by the provincial/territorial health insurance plan.
- Amount of extra-billing levied by enrolled physicians and dentists for insured health services: $ NIL
- Amounts of user charges
A user charge is defined as any charge for an insured health service, other than extra-billing. This includes any charge levied for insured hospital services, provided in hospital or at a non-hospital facility (e.g., private surgical or diagnostic clinic), or any non-physician related services provided in conjunction with an insured physician service at a non-hospital facility (e.g., private surgical or diagnostic clinic or private practice).
- Amount of user charges levied for medically necessary diagnostic services: $ NIL
- Amount of user charges levied for all other insured services: $ 1,254.88
- N.B. Charges may be levied for accommodation and meal costs related to a patient who, in the opinion of the attending physician, is a permanent resident in a hospital or other chronic care institution as per the limitation of Section 19 (2). Charges related to this limitation should not be included in the financial statement.
Total for extra-billing and user charges $ 1,254.88
- Description of method used to determine amounts of extra-billing and user charges
The following information should be included in the description of the method used to determine the amounts of extra-billing and user charges (EBUC) reported, including if a NIL amount is submitted:
- Name of applicable pieces of PT legislation that prohibit extra-billing and user charges (including facility fees).
Please use as much space as needed below.
In Newfoundland and Labrador, the Department of Health and Community Services (HCS) administers the Medical Care Plan (MCP). Subsection 7(1) of the Medical Care and Hospital Insurance Act states that a practitioner shall not charge or collect from a beneficiary a fee for those insured services in excess of the amounts payable under this Act and the regulations. Administration of the Medical Care Plan, including deterrence of extra-billing, is in accordance with the Act and the associated regulations. Of particular note are the Medical Care Insurance Insured Services Regulations, NLR 21/96 (the "Regulations").
Section 25 of the Medical Care and Hospital Insurance Act provides the Minister with powers to recover overpayments and interest that were discovered via audit. The Minister of Health and Community Services may do this by entering into an agreement with the practitioner to pay to the Minister the overpaid amount plus interest.
On June 15, 2018, an amendment was made to section 3 of the Medical Care Insurance Insured Services Regulations to clarify that "the medically necessary removal and replacement of a cataractous lens by any procedure is an insured service and shall be performed in a hospital or a facility designated by the Lieutenant-Governor in Council."
On January 12, 2021, two non-hospital facilities were approved to provide insured cataract surgery. A third was designated in April 2022. The Provision of Cataract Surgery in Non-Hospital Facilities Policy outlines the requirements for these designated non-hospital facilities.
At this time, section 3 of the Medical Care Insurance Insured Services Regulations insures diagnostic and therapeutic X-ray and laboratory services only when they are provided in facilities approved by the commission which are not provided under the Medical Care and Hospital Insurance Act and regulations made under that Act. There are no such facilities approved within Newfoundland and Labrador to deliver diagnostic and therapeutic x-ray and laboratory services.
- Details about the process used to investigate extra-billing and user charges (e.g., proactive regular audits of provider billings; reactive investigations triggered by patient complaints, media reports or other sources).
Please use as much space as needed below.
HCS conducts regular audits of provider billings. No instances of extra-billing or user charges (EBUC) were identified during the relevant period through the regular auditing process. Cases of EBUC may be identified through the audit process described under section 21 of the Medical Care and Hospital Insurance Act or may be reported by beneficiaries. These instances may be discovered when beneficiaries submit claims for reimbursement to the Medical Care Plan (MCP) or make enquiries for services when payment is requested.
Complaints from beneficiaries regarding charges for insured health services are managed by the Department. Depending on the circumstance, the Department may investigate or refer the matter to the College of Physicians and Surgeons of Newfoundland and Labrador, the regulatory body for physicians in the province, for potential disciplinary action. Beneficiaries may also contact the College directly.
- A summary of any extra-billing and user charges investigations during the fiscal year including:
- Number of investigations
- Nature of each investigation (e.g., physician billing audits; patient triggered investigations; private clinic audits; third party report findings (e.g., Auditor General))
- Confirmed cases and dollar amounts of extra-billing and user charges.
- Any amounts reimbursed to patients.
Please use as much space as needed below.
Cataract Surgery
In 2017-2018, HCS received complaints from beneficiaries for charges associated with cataract surgery. HCS issued a Public Service Announcement on February 7, 2018 inviting individuals to contact HCS with suspected instances of EBUC related to cataract surgery in an effort to better understand the issue. HCS officials tracked calls and emails, and analysed documents provided by patients. Where appropriate to do so, billings to MCP were examined.
On February 20, 2020, HCS published a Public Advisory on the Reimbursement Process for Cataract Surgeries. To be eligible for reimbursement of fees paid for cataract surgery, patients must submit documents indicating that insured cataract surgery was paid for outside of a hospital or designated facility before June 15, 2018. Patients who had previously submitted documents indicating eligibility for reimbursement were contacted by HCS to arrange payment. HCS also identified other beneficiaries that could be eligible for reimbursement but whose supporting documents were inconclusive or unavailable. HCS invited these individuals to submit documents for review to determine eligibility.
Despite the requirement for services to be provided prior to June 15, 2018 for reimbursement, HCS does receive enquiries for reimbursement for services received after June 15, 2018. To better understand this issue, HCS invites these patients to provide such documents for review. Through this process, HCS identified user charges for one patient for procedures completed on both eyes during this reporting period. Supporting documentation provided by the patient supports the medical necessity of these procedures. However, the patient was charged for "Custom Premium Vision Correction". In addition to non-insured upgraded lenses, the patient was charged $2,445 per eye for non-insured diagnostic tests, femtosecond laser, a three-year "laser enhancement plan", as well as a post-surgical refractive lens kit. All invoices provided for the procedure stated that the procedure was "not medically necessary", a "vision upgrade", "optional", "non-insured". There was no charge for the removal of the lens.
Given the above, the amount of user charges identified for cataract surgery during this reporting period is $627.44 X 2 = $1,254.88. Please note that there has been an increase from the amount awarded from $574.47 per eye to $627.44 based on increased amounts payable to ophthalmologists under the Memorandum of Agreement between government and the Newfoundland and Labrador Medical Association effective December 2021.
No reimbursements were made for cataract surgeries performed during the reporting year.
- Details on mechanisms to deter patient extra-billing and user charges (e.g., provider fines; plan payment withholding; provider/patient education initiatives; loss of facility accreditation).
Please use as much space as needed below.
Section 7 of the Medical Care and Hospital Insurance Act outlines that a practitioner who provides insured services, whether or not he or she has made an election to opt out of participation in the MCP, shall not charge or collect from a beneficiary a fee for those insured services in excess of the amount payable under the Act and the regulations. A practitioner or other person who contravenes this is guilty of an offence and liable on summary conviction to a fine of up to, but not more than $20,000 for each contravention.
The Medical Care and Hospital Insurance Act authorizes the Minister to appoint auditors to audit the accounts and claims for payments submitted by physicians and dentists. The Act prescribes the power and duties of auditors, sets out the remedies available and details the processes to be followed. The Act also details the review and appeal processes available to practitioners. Individual providers are randomly selected on a biweekly basis for audit.
On January 12, 2021, two non-hospital facilities were approved to provide insured cataract surgery. A third facility was designated in April 2022. The Provision of Cataract Surgery in Non-Hospital Facilities Policy outlines the requirements for these designated non-hospital facilities. Section 14.1 of the policy specifically deals with expectations regarding EBUC, which are prohibited. The ophthalmologist has a duty to make sure that the patient understands that all insured services are available without any charge to the patient. Non-hospital facilities must provide an itemized list of services billed to the patient to ensure clarity between insured and billable non-insured services. A Patient Information Sheet on cataract surgery is provided in Annex B of the above policy. Non-hospital designated facilities must post the Patient Information Sheet in visible areas for public viewing. They must also provide a copy of this information sheet to all patients who are receiving cataract surgery in a non-hospital designated facility for patient signature.
The Lieutenant-Governor in Council has the authority to suspend or cancel a non-hospital facility's designation status if the non-hospital facility fails to comply with the above policy.
The Department of Health and Community Services conducted a review in 2022 of the provincial allocation of out-of-hospital cataract surgery and the Policy for the Provision of Cataract Surgery in Non-Hospital Designated Facilities. This review included a calculation of Total Predicted Regional Demand (TPRD) for cataract surgery in each region of the province, as well as evaluating wait lists, national benchmarks for wait times, and adherence to the policy by designated facilities. As a result of this evaluation, the Department has approved a one-time increase of 3,300 procedures to the regional caps on cataract surgery in designated facilities. This increase will be in place from October 1, 2022 until March 31, 2024 (18 months total with 1,100 performed in the second half of 2022-2023 and 2,200 performed in 2023-2024). Budget 2023 provided a further 1,500 procedures and this, plus the baseline number of procedures (3,500) provided each year to designated facilities across the province brings the total out-of-hospital procedures for 2023-24 to 7,200 (3,500 + 2,200 + 1,500). The Department anticipates that funding more out-of-hospital cataract procedures will increase patient access to insured cataract surgery.
Prince Edward Island
Canada Health Act
Financial statement of actual amounts of extra-billing and user charges
For the period April 1, 2021 to March 31, 2022
- Amounts of extra-billing
Extra-billing is defined as a charge by an enrolled physician or dentist to an insured person for an insured service in addition to the amount paid by the provincial/territorial health insurance plan.
- Amount of extra-billing levied by enrolled physicians and dentists for insured health services: $ NIL
- Amounts of user charges
A user charge is defined as any charge for an insured health service, other than extra-billing. This includes any charge levied for insured hospital services, provided in hospital or at a non-hospital facility (e.g., private surgical or diagnostic clinic), or any non-physician related services provided in conjunction with an insured physician service at a non-hospital facility (e.g., private surgical or diagnostic clinic or private practice).
- Amount of user charges levied for insured services: $ NIL
- Amount of user charges levied for all other insured services: $ NIL
- N.B. Charges may be levied for accommodation and meal costs related to a patient who, in the opinion of the attending physician, is a permanent resident in a hospital or other chronic care institution as per the limitation of Section 19 (2). Charges related to this limitation should not be included in the financial statement.
Total for extra-billing and user charges $ NIL
- Description of method used to determine amounts of extra-billing and user charges
The following information should be included in the description of the method used to determine the amounts of extra-billing and user charges (EBUC) reported, including if a NIL amount is submitted:
- Name of applicable pieces of PT legislation that prohibit extra-billing and user charges (including facility fees).
Please use as much space as needed below.
Extra-billing is not permitted, as per the Province of Prince Edward Island's Health Services Payment Act.
PEI's Hospital and Diagnostic Services Insurance Act (HDSIA) does not explicitly prohibit user charges for insured health services. However, there are a number of sections in the HDSIA Regulations that infer that user charges would be prohibited, as described below.
1(e) "insured services" means the hospital and diagnostic services to which a person is entitled under this Act and regulations;
9(1) Entitlement to receive insured services (1) Subject to this Act and the regulations, all residents of the province are entitled to receive insured services upon uniform terms and conditions.
10(d) Minister, further functions and powers: to approve or disapprove charges made to all patients by hospitals in Prince Edward Island to which payments are made under the plan of hospital care insurance;
11 Regulations (1) The Lieutenant Governor in Council may make regulations
(r) approving the charges that may be made for private and semi-private wards in hospitals;
(t) approving the charges for insured services that mat be made by a hospital directly to the patient
Hospital and Diagnostic Services Insurance Regulations:
1.1(l): "insured services" means, subject to subsection (2), the in-patient and out-patient hospital services available to an entitled person without charge, as determined by the Minister but does not include any services to which a person is entitled, and for which a person is eligible, under any law mentioned in Schedule B;
6. Direct charge to patient (1) An approved hospital shall make a direct charge in respect of the patient who is an entitled person for the difference between the per diem cost of providing insured services and the hospital charges approved by the Minister for private or semi-private accommodation and for any other services which are not insured services requested by or on behalf of the patient.
- Details about the process used to investigate extra-billing and user charges (e.g., proactive regular audits of provider billings; reactive investigations triggered by patient complaints, media reports or other sources).
Please use as much space as needed below.
The process used would be reactive investigations triggered by patient complaints, media reports or other government entities.
Health PEI administers a system of internal controls when reviewing physician billings, and investigates irregularities in billing. Physicians are subject to internal audit of billing practices to ensure all amounts billed to Health PEI are appropriate.
Annual financial results for Health PEI are reviewed to identify irregularities and significant variances. This includes a review of revenues to identify any new revenue items (i.e.; user charges). These revenues are also subject to review by the Auditor General.
The Province of Prince Edward Island offers several avenues for patients and the general public to provide feedback and complaints, including a patient feedback link on the Health PEI website. The Minister of Health and Wellness, the CEO of Health PEI and staff can also be contacted by anyone who may have been subject to any extra-billing or user charges. Health PEI follows up on any complaints, including those around billing practices.
- A summary of any extra-billing and user charges investigations during the fiscal year including:
- Number of investigations
- Nature of each investigation (e.g., physician billing audits; patient triggered investigations; private clinic audits; third party report findings (e.g., Auditor General))
- Confirmed cases and dollar amounts of extra-billing and user charges.
- Any amounts reimbursed to patients.
Please use as much space needed bellow.
Throughout the year, HPEI conducted analysis of financials as it relates to extra-billing as noted above. There were no findings of extra-billing.
- Details on mechanisms to deter patient extra-billing and user charges (e.g., provider fines; plan payment withholding; provider/patient education initiatives; loss of facility accreditation).
Please use as much space as needed below.
Provider Education through the Medicare Office and the Prince Edward Island Health Authority.
Nova Scotia
Canada Health Act
Financial statement of actual amounts of extra-billing and user charges
For the period April 1, 2021 to March 31, 2022
- Amounts of extra-billing
Extra-billing is defined as a charge by an enrolled physician or dentist to an insured person for an insured service in addition to the amount paid by the provincial/territorial health insurance plan.
- Amount of extra-billing levied by enrolled physicians and dentists for insured health services: $ 0
- Amounts of user charges
A user charge is defined as any charge for an insured health service, other than extra-billing. This includes any charge levied for insured hospital services, provided in hospital or at a non-hospital facility (e.g., private surgical or diagnostic clinic), or any non-physician related services provided in conjunction with an insured physician service at a non-hospital facility (e.g., private surgical or diagnostic clinic or private practice).
- Amount of user charges levied for medically necessary diagnostic services: $ 0
- Amount of user charges levied for all other insured services: $ 0
- N.B. Charges may be levied for accommodation and meal costs related to a patient who, in the opinion of the attending physician, is a permanent resident in a hospital or other chronic care institution as per the limitation of Section 19 (2). Charges related to this limitation should not be included in the financial statement.
Total for extra-billing and user charges $ 0
- Description of method used to determine amounts of extra-billing and user charges
The following information should be included in the description of the method used to determine the amounts of extra-billing and user charges (EBUC) reported, including if a NIL amount is submitted:
- Name of applicable pieces of PT legislation that prohibit extra-billing and user charges (including facility fees).
Please use as much space as needed below.
With respect to extra-billing, Nova Scotia's Health Services and Insurance Act (HSIA) provides:
29 (1) Where a provider renders an insured professional service to a resident, the provider shall be entitled to receive in respect of that service only the fee or compensation provided in the tariff of fees or other system of payment established pursuant to Section 13.
- Details about the process used to investigate extra-billing and user charges (e.g., proactive regular audits of provider billings; reactive investigations triggered by patient complaints, media reports or other sources).
Please use as much space as needed below.
Nova Scotia relies on a complaints-based system where concerns are brought to the attention of the Minister on a case-by-case basis. Complaints are directed to the Department of Health and Wellness via telephone or email; are received by Medavie Blue Cross and then directed to the Department; or are directed to the College of Physicians and Surgeons of Nova Scotia. All complaints are investigated and addressed.
- A summary of any extra-billing and user charges investigations during the fiscal year including:
- Number of investigations
- Nature of each investigation (e.g., physician billing audits; patient triggered investigations; private clinic audits; third party report findings (e.g., Auditor General))
- Confirmed cases and dollar amounts of extra-billing and user charges.
- Any amounts reimbursed to patients.
Please use as much space needed bellow or add extra pages as necessary.
There were no EBUC investigations to report in the 2021-2022 fiscal year. As stated in the 2020-2021 report, Nova Scotia has no legislative authority to audit private clinics.
- Details on mechanisms to deter patient extra-billing and user charges (e.g., provider fines; plan payment withholding; provider/patient education initiatives; loss of facility accreditation).
Please use as much space as needed below.
Under the HSIA, a breach of provision 29 (1) could constitute an offense subject to criminal prosecution:
35 (1) Any person who violates this Act or the regulations or willfully makes a false statement in any report or form required to enable a payment to be made under the Hospital Insurance Plan, the Insured Prescription Drug Plan or the M.S.I Plan is guilty of an offence and liable on summary conviction to a fine of not more than ten thousand dollars for a first offence and for a subsequent offence to a fine of not more than twenty thousand dollars.
New Brunswick
Canada Health Act
Financial statement of actual amounts of extra-billing and user charges
For the period April 1, 2021 to March 31, 2022
- Amounts of extra-billing
Extra-billing is defined as a charge by an enrolled physician or dentist to an insured person for an insured service in addition to the amount paid by the provincial/territorial health insurance plan.
- Amount of extra-billing levied by enrolled physicians and dentists for insured health services. $ 0
- Amounts of user charges
A user charge is defined as any charge for an insured health service, other than extra-billing. This includes any charge levied for insured hospital services, provided in hospital or at a non-hospital facility (e.g., private surgical or diagnostic clinic), or any non-physician related services provided in conjunction with an insured physician service at a non-hospital facility (e.g., private surgical or diagnostic clinic or private practice).
- Amount of user charges levied for medically necessary diagnostic services: $ 0
- Amount of user charges levied for insured services: $ 0
- N.B. Charges may be levied for accommodation and meal costs related to a patient who, in the opinion of the attending physician, is a permanent resident in a hospital or other chronic care institution as per the limitation of Section 19 (2). Charges related to this limitation should not be included in the financial statement.
Total for extra-billing and user charges $ 0
- Description of method used to determine amounts of extra-billing and user charges
The following information should be included in the description of the method used to determine the amounts of extra-billing and user charges (EBUC) reported, including if a NIL amount is submitted.
- Name of applicable pieces of PT legislation that prohibit extra-billing and user charges (including facility fees).
Please use as much space as needed below.
New Brunswick's Medical Services Payment Act and its Regulations (MSPA) describe mechanisms creating a health system which is Publicly Administered, Comprehensive, Universally available to its beneficiaries, Portable, and Accessible. It defines who may receive or provide an entitled service and how fee schedules are determined and prohibits extra-billing or user charges for any such service remunerated through the Medicare Branch.
Some providers may choose to practise outside the MSPA. The MSPA establishes a wall between the publicly funded system (which meets the principles outlined above) and entrepreneurial private business, prohibiting any practitioner payments which exceed the established fee schedules, and payments to private hospitals. It also establishes a private practitioner's duty to inform prospective patients.
- Section 2.01 of the Act prohibits payments for private services when furnished by a practitioner who (at the time services are provided) is practising outside the provisions of the Act and Regulations, or if the services were furnished in a private hospital facility.
- Sub-paragraph 3.iv of the Act recognizes that a practitioner may elect to practise his or her profession outside the Act and Regulations, and thereby assumes an obligation under section 5.1 to inform their patients that any services would not be entitled for payment within New Brunswick's publicly funded health system.
- Schedule 2 of the Regulation describes services which are ineligible for payment under the Act, paragraph (n.1) specifically prohibits payments to practitioners within New Brunswick whose fee exceeds the amount payable under the Regulation.
- Schedule 3 of the Regulation provides the wording of an agreement to be signed by the practitioner that they would accept funds provided by the Medicare Branch as payment in full for any entitled services for which they submit an account and make no further claim for reimbursement with respect to that service.
- Details about the process used to investigate extra-billing and user charges (e.g., proactive regular audits of provider billings; reactive investigations triggered by patient complaints, media reports or other sources).
Please use as much space as needed below.
New Brunswick uses a robust "comment based" approach to identifying individual citizens' concerns on a wide range of health issues. In a typical month in the 2018-2019 fiscal year the Department of Health received, logged, and responded to 150-200 concerns from individual New Brunswickers on issues including access to primary or specialized care, pharmaceutical approvals, access to services in a citizen's language of choice, wait times for specific services, the structure of specific programs, etc.
The Department's web page provides several mechanisms to make such comments, including mailing addresses, e-mail addresses, telephone numbers, and a web-based message service.
In 2021-2022, ten requests for reimbursement were submitted to the Department for consideration. All were rejected, whether following preliminary review or further investigation.
- A summary of any extra-billing and user charges investigations during the fiscal year including:
- Number of investigations. 10
- Nature of each investigation (e.g., physician billing audits; patient triggered investigations; private clinic audits; third party report findings (e.g., Auditor General)).
- Each of these investigations originated as patient requests for reimbursement for services they had paid for in private facilities in New Brunswick. The reviews were conducted by the Medicare Branch of the Department of Health.
- Two requests were rejected because they referred to services which Medicare does not cover in any circumstance.
- Four requests were rejected because they contravened section 2.01 of the Medicare Services Payment Act.
- Four requests were rejected because they contravened Regulation 84-20, Schedule 2 (p.1) of the Medicare Services Payment Act.
- Confirmed cases and dollar amounts of extra-billing and user charges.
- The Department of Health cannot independently confirm the amounts which these individuals may have paid to private providers but can only rely on the figures provided by the individuals in their requests.
- The sum of all reimbursements requested in these fourteen instances was $9,515.
- Any amounts reimbursed to patients.
- As described above, all the requests for reimbursement contravened provisions of either the Medical Services Payment Act itself, or its Regulation.
- No reimbursement was provided to patients.
- Details on mechanisms to deter patient extra-billing and user charges (e.g., provider fines; plan payment withholding; provider/patient education initiatives; loss of facility accreditation).
Please use as much space as needed below.
New Brunswick's Medical Services Payment Act and its Regulations (MSPA) describe mechanisms creating a health system which is Publicly Administered, Comprehensive, Universally available to its beneficiaries, Portable, and Accessible. It defines who may receive or provide an entitled service and how fee schedules are determined and prohibits extra-billing or user charges for any such service remunerated through the Medicare Branch.
Some providers may choose to practise outside the MSPA. The MSPA establishes a wall between the publicly funded system (which meets the principles outlined above) and entrepreneurial private business, prohibiting any practitioner payments which exceed the established fee schedules, and payments to private hospitals. It also establishes a private practitioner's duty to inform prospective patients.
- Schedule 2 of the Regulation describes services which are ineligible for payment under the Act, paragraph (n.1) specifically prohibits payments to practitioners within New Brunswick whose fee exceeds the amount payable under the Regulation.
- Schedule 3 of the Regulation provides the wording of an agreement to be signed by the practitioner that they would accept funds provided by the Medicare Branch as payment in full for any entitled services for which they submit an account and make no further claim for reimbursement with respect to that service.
Quebec
[The following represents Quebec's financial statement of extra-billing and user charges levied during 2021-2022, which was communicated in a January 30, 2024, exchange between officials.]
Dear Sir:
I am writing in response to your email dated November 6, 2023. It contains a request for an accounting of the total amount of extra-billing, user charges and patient charges for medically required diagnostic services in the 2021–2022 fiscal year.
In Quebec, the health insurance plan is regulated by the Health Insurance Act. The Act does not allow user charges to be imposed. In addition, it prohibits any person from demanding or receiving any payment of incidental fees for an insured service, except in cases prescribed by regulation or provided for in an agreement.
Regarding diagnostic services, once again, please note that medically required examinations are fully covered by the public health care system and are available to Quebec patients in public hospitals. Access is therefore free and universal for all Quebecers. Your organization's estimates of patient billing, based on a questionable calculation method, therefore do not paint a realistic picture of the situation in Quebec. There are no circumstances in which I could agree that they are valid.
Moreover, the Ministère de la Santé et des Services sociaux has provided Health Canada with information on current and future measures relating to diagnostic examinations in Quebec, in particular under the Act to make the health and social services system more effective and the contracts signed between public hospitals and private clinics to improve access to publicly funded health care services. Canada has stated that it will reimburse Quebec 50% of the deduction applied to Quebec's March 2023 Canada Health Transfer (CHT) payment ($41,867,224) and 50% of the deduction that would be applied to the March 2024 CHT payment ($36,014,132), for a total reimbursement of $38,940,678. This reimbursement represents only half of the cut arbitrarily applied to the Quebec CHT payment, and I find it difficult to make sense of this percentage that your organization has set unilaterally and without basis. In this respect, Quebec considers that the information provided is more than sufficient and reiterates that it believes it is entitled to full reimbursement of the sums due to it.
Moreover, the Government of Quebec is accountable to the National Assembly and the people of Quebec with respect to how its health care system is run. Quebec will continue to fulfill this responsibility to Quebecers, who are the ultimate arbiters as to the quality and accessibility of the health care services provided to them.
I encourage you to consult the public information in the 2021–2022 annual management report of the Ministère de la Santé et des Services sociaux, tabled in the National Assembly, which provides an accounting of how Quebec manages its health care system.
Yours sincerely
Valérie Fontaine, Director
Ontario
Canada Health Act
Financial statement of actual amounts of extra-billing and user charges
For the period April 1, 2021 to March 31, 2022
- Amounts of extra-billing
Extra-billing is defined as a charge by an enrolled physician or dentist to an insured person for an insured service in addition to the amount paid by the provincial/territorial health insurance plan.
- Amount of extra-billing levied by enrolled physicians and dentists for insured health services: $ 0
- Amounts of user charges
A user charge is defined as any charge for an insured health service, other than extra-billing. This includes any charge levied for insured hospital services, provided in hospital or at a non-hospital facility (e.g., private surgical or diagnostic clinic), or any non-physician related services provided in conjunction with an insured physician service at a non-hospital facility (e.g., private surgical or diagnostic clinic or private practice).
- Amount of user charges levied for medically necessary diagnostic services: $ 0
- Amount of user charges levied for insured services: $ 32,800
- N.B. Charges may be levied for accommodation and meal costs related to a patient who, in the opinion of the attending physician, is a permanent resident in a hospital or other chronic care institution as per the limitation of Section 19 (2). Charges related to this limitation should not be included in the financial statement.
Total for extra-billing and user charges $ 32,800
- Description of method used to determine amounts of extra-billing and user charges
The following information should be included in the description of the method used to determine the amounts of extra-billing and user charges (EBUC) reported, including if a NIL amount is submitted:
- Name of applicable pieces of PT legislation that prohibit extra-billing and user charges (including facility fees).
Please use as much space as needed below.
The Ontario Health Insurance Plan (OHIP) and all insured services are set out under the Health Insurance Act (HIA) and its Regulations.
In Ontario, from April 1, 2021 to March 31, 2022, two pieces of legislation prohibited any person or entity from charging for all or part of an OHIP-insured service rendered to an insured person or for overhead charges related to the provision of insured services (i.e. EBUC, including illegal facility fees) and were as follows:
- The Commitment to the Future of Medicare Act (CFMA) prohibits any person or entity from charging unauthorized payments for all or part of an OHIP-insured service rendered to an insured person. Such charges include extra-billing (i.e. charges to insured persons for insured physician and dental-surgical services) and user charges (i.e. charges to insured persons for non-physician/dental-surgical services provided in conjunction with insured services at a hospital or health facility).
The CFMA also prohibits providers and other entities from providing preferred access to an insured service conditional on the payment of a fee, which is called queue-jumping, and from making the provision of an insured service conditional on paying a block fee for uninsured services.
The CFMA applies regardless of the type of facility or setting in which a service is rendered.
- The Independent Health Facilities Act* (IHFA) prohibits any person from charging or accepting payment of facility fees unless charged and paid in accordance with the Act (e.g., facility fees are only payable by the Minister or Ontario Health, only in respect of services provided in licensed facilities, etc.). A facility fee is a charge, fee or payment in respect of a service or operating cost that supports, assists or is a necessary adjunct to an OHIP-insured service, and is not part of the insured service.
Regardless of whether an insured service is provided in a licensed Independent Health Facility (IHF) or any other private, community-based setting, a charge or payment in respect of a service or operating cost that supports, assists and/or is a necessary adjunct to an insured service, but is not part of the insured service, and that is not charged/paid in compliance with the IHFA is an illegal facility fee.
*On September 25, 2023, the IHFA was replaced by the Integrated Community Health Services Centres Act, however, this legislation was not in force during the 2021-2022 EBUC reporting period and has no impact on this annual report.
Through a dedicated program (CFMA Program), the Ontario Ministry of Health (the ministry) reviews all possible cases of EBUC brought to its attention. Charging facility fees contrary to the IHFA may also be considered to be EBUC and therefore, the ministry's CFMA Program also reviews allegations of illegal facility fees under the IHFA in conjunction with the ministry's IHF program.
The above mechanisms in place prohibit EBUC for medically necessary diagnostic services.
If, as a result of a review, it is determined that a patient has paid an unauthorized payment (i.e. extra-billing) and/or user charge, the ministry ensures that the full amount is reimbursed to the patient.
- Details about the process used to investigate extra-billing and user charges (e.g., proactive regular audits of provider billings; reactive investigations triggered by patient complaints, media reports or other sources).
Please use as much space needed bellow or add extra pages as necessary.
As noted above, the ministry reviews all possible instances of EBUC that come to its attention. Patient complaints regarding possible EBUC and questions from the public are received mostly via a dedicated toll-free number and email address. Information regarding possible EBUC arises primarily from patient complaints; however, the ministry may also review possible violations that are brought to its attention by other sources such as Health Canada, MPPs, the media, advertisements, etc. The ministry also conducts proactive reviews, without external prompts.
All inquiries from patients and other sources regarding out-of-pocket charges for insured services are responded to, and patients are provided with an opportunity to request that the ministry open a CFMA review. The ministry may also assess the complaint/concern independently to determine whether or not a general CFMA review should be opened (i.e., was the service charged for clearly insured or is further review required?). If it is determined that EBUC may have occurred, according to CFMA Program policy, patients are asked to complete a CFMA Program form for the ministry to open a specific review and advised that if they do not wish to initiate a specific review, they may request a general review.
As part of a review, the ministry requests relevant records and/or information from providers under authority of the CFMA (e.g., medical and/or hospital/facility records related to the service the patient was charged for, copies of all invoices and receipts, a breakdown of any patient charges, etc.). Once the requested information has been received, it is reviewed by CFMA Program staff in order to determine whether a specific service provided to a patient was insured. In almost all cases, ministry medical advisors are consulted for assistance in interpreting medical records. Staff may also consult with other areas of the ministry.
The ministry can and does review possible EBUC on a proactive basis (i.e., without receiving a patient-specific complaint). As noted above, reviews often require examinations of specific patient records to determine whether a specific service provided to a patient was insured, and therefore, without a specific patient complaint, the ministry primarily undertakes these reviews for the purposes of provider education, seeking information regarding general practices and policies to ensure their compliance with Ontario legislation.
If the ministry finds through a CFMA review that a patient has paid an illegal extra-billing fee or user charge, the ministry ensures that the full amount is reimbursed to the patient.
- A summary of any extra-billing and user charges investigations during the fiscal year including:
- Number of investigations.
- Nature of each investigation (e.g., physician billing audits; patient triggered investigations; private clinic audits; third party report findings (e.g., Auditor General)).
- Confirmed cases and dollar amounts of extra-billing and user charges.
- Any amounts reimbursed to patients.
Please use as much space as needed bellow.
In FY 2021-2022, the ministry conducted 91 reviews of potential EBUC under the CFMA.
88 of the reviews in FY 2021-2022 were patient-initiated and 3 were non-patient specific and/or initiated by other sources, and 54 of them resulted in a determination that a patient was not charged for all or part of an insured services under Ontario legislation and regulations.
| # of reviews | Nature of review |
|---|---|
| 88 | Patient-Initiated |
| 3 | Non-Patient Specific and/or Initiated by Other Sources (e.g. Other Ministry Area, MPP Referred, Concerned Citizen, etc.) : |
| 91 | Total |
When the ministry finds, through a CFMA review, that a patient has paid an illegal extra-billing fee or user charge, the ministry ensures that the full amount is reimbursed to patients. 37 of the 91 reviews in FY 2021-2022 resulted in a determination that a patient was charged for an insured service contrary to Ontario legislation and each of these patients was reimbursed in full.
Included in this reporting period is the specification of diagnostic services where a patient was charged but, further to the CFMA review, the diagnostic service was determined to be an insured service and the patient was reimbursed in full.
A breakdown of these reviews is as follows:
| # of Reviews | Nature of review | # of patients reimbursed/charge withdrawn | Charge type | Charge per service | Total amount charged | Total amount reimbursed |
|---|---|---|---|---|---|---|
| 4 | Patient initiated | 4 | Extra-billing | $200-$508.50 | $1,560.50 | $1,560.50 |
| 30 | Patient initiated | 30 | User Charges | $20-$5,085 | $15,933.95 | $15,933.95 |
| 3 | Patient initiated | 3 | Diagnostic Services | $73.72-$550 | $1,173.72 | $1,173.72 |
| 37 | Total # of Reviews Involving Confirmed EBUC (Including Facility Fees) | Total Amount Charged and Reimbursed for Confirmed Reviews | $18,668.17 | $18,668.17 | ||
Therefore, Ontario is reporting $nil for extra-billing charges for FY 2021-2022.
Abortion Clinics
At the request of Health Canada and/or other stakeholders, the ministry has undertaken several proactive reviews of private abortion clinics not currently funded under the IHFA over the last few years. None of these reviews occurred in the 2021-2022 EBUC reporting period. All private clinics (that were/are no funded by the ministry under the IHFA/ICHSCA) known to the ministry have been reviewed at least once in the past five years, and four out of five have been reviewed twice in that timeframe.
In accordance with Health Canada's position that these reviews suggest payment of a block fee (101 out of 120 patients), and despite the fact that the ministry takes a contrary position, user charges in the amount of $6,560 for each of the five abortion clinics are being reported for FY 2021-2022 totalling $32,800.
- Details on mechanisms to deter patient extra-billing and user charges (e.g., provider fines; plan payment withholding; provider/patient education initiatives; loss of facility accreditation).
Please use as much space as needed below.
Through a dedicated program (CFMA Program), the Ontario Ministry of Health (the ministry) reviews all possible cases of EBUC brought to its attention.
The ministry takes steps to prevent EBUC by maintaining a webpage which provides public information regarding the CFMA, including what is prohibited under the Act (i.e., extra-billing, queue-jumping, illegal block fees), how to determine if a patient has been charged for an insured service or for access to an insured service, and how to contact the ministry via a dedicated toll-free number and email address in order to open an review or ask a question regarding a possible CFMA violation.
The ministry also regularly undertakes proactive CFMA reviews that are not tied to a specific patient complaint. In many cases, these investigations are done for the purposes of provider education, in order for the ministry to communicate its obligations under the Canada Health Act (CHA) and requirements for providers under the CFMA and IHFA, and to ensure that providers' billing practices comply with Ontario legislation. The ministry has also in the past undertaken patient education initiatives to increase awareness among members of the general public about the protections under the CFMA and to encourage filing of valid complaints to the CFMA program so that reviews can be initiated.
In rare but serious cases where the person or entity fails to comply with a CFMA review without just cause (e.g., if a provider or entity fails to provide the ministry with requested information relevant to the determination of whether or not EBUC has occurred), the Act authorizes the ministry to suspend all OHIP payments to the person or entity pending receipt of the requested information.
Manitoba
Canada Health Act
Financial statement of actual amounts of extra-billing and user charges
For the period April 1, 2021 to March 31, 2022
- Amounts of extra-billing
Extra-billing is defined as a charge by an enrolled physician or dentist to an insured person for an insured service in addition to the amount paid by the provincial/territorial health insurance plan.
- Amount of extra-billing levied by enrolled physicians and dentists for insured health services: $ 0
- Amounts of user charges
A user charge is defined as any charge for an insured health service, other than extra-billing. This includes any charge levied for insured hospital services, provided in hospital or at a non-hospital facility (e.g., private surgical or diagnostic clinic), or any non-physician related services provided in conjunction with an insured physician service at a non-hospital facility (e.g., private surgical or diagnostic clinic or private practice).
- Amount of user charges levied for medically necessary diagnostic services: $ 650
- Amount of user charges levied for all other insured services: $ 0
- N.B. Charges may be levied for accommodation and meal costs related to a patient who, in the opinion of the attending physician, is a permanent resident in a hospital or other chronic care institution as per the limitation of Section 19 (2). Charges related to this limitation should not be included in the financial statement.
Total for extra-billing and user charges $ 650
- Description of method used to determine amounts of extra-billing and user charges
The following information should be included in the description of the method used to determine the amounts of extra-billing and user charges (EBUC) reported, including if a NIL amount is submitted:
- Name of applicable pieces of PT legislation that prohibit extra-billing and user charges (including facility fees).
Please use as much space as needed below.
- The Health Services Insurance Act and Regulations made under the Act
- Details about the process used to investigate extra-billing and user charges (e.g., proactive regular audits of provider billings; reactive investigations triggered by patient complaints, media reports or other sources).
Please use as much space as needed below.
- In the event that a Manitoba resident feels that they have been inappropriately charged for a service that is insured under the provincial health insurance plan (i.e., a potential incidence of extra-billing or a user charge), or of a report or allegation of extra-billing or user charges, the department will investigate the complaint, report or allegation appropriately. Residents may contact Manitoba Health, Seniors and Long-Term Care (MHSLTC) to report such occurrences through any of the contact coordinates listed on our website, including our Audit and Investigation Fraud Line.
- The Insured Benefits Branch of MHSLTC examines the specifics of any fee charged to assess whether the service provided was an insured service.
- Generally, in the event that there has been a fee charged that could be considered an instance of extra-billing or a user charge, MHSLTC contacts the medical service provider advising that the provider must reimburse the patient and submit a claim to MHSLTC. This is sufficient to address the concern. Further incidents on the part of the same service provider could result in an investigation by MHSLTC's Audit and Investigation Unit.
- MHSLTC learned of one medically necessary diagnostic service charge by a private clinic during the reporting period. MHSLTC sent a formal letter instructing the Prota Clinic to stop charging patients for medically necessary ultrasound services. Since issuing the letter, MHSLTC has not identified any additional patients charged by the clinic.
- A summary of any extra-billing and user charges investigations during the fiscal year including:
- Number of investigations. One
- Nature of each investigation (e.g., physician billing audits; patient triggered investigations; private clinic audits; third party report findings (e.g., Auditor General)). Above b)
- Confirmed cases and dollar amounts of extra-billing and user charges. n/a
- Any amounts reimbursed to patients. n/a
- Details on mechanisms to deter patient extra-billing and user charges (e.g., provider fines; plan payment withholding; provider/patient education initiatives; loss of facility accreditation).
Please use as much space as needed below.
- Routine audits of practitioner billings;
- The Health Services Insurance Act prohibits extra-billing for insured services and outlines penalties to deter regional health authorities, hospitals, medical practitioner etc.
Saskatchewan
Canada Health Act
Financial statement of actual amounts of extra-billing and user charges
For the period April 1, 2021 to March 31, 2022
- Amounts of extra-billing
Extra-billing is defined as a charge by an enrolled physician or dentist to an insured person for an insured service in addition to the amount paid by the provincial/territorial health insurance plan.
- Amount of extra-billing levied by enrolled physicians and dentists for insured health services: $ 0
- Amounts of user charges
A user charge is defined as any charge for an insured health service, other than extra-billing. This includes any charge levied for insured hospital services, provided in hospital or at a non-hospital facility (e.g., private surgical or diagnostic clinic), or any non-physician related services provided in conjunction with an insured physician service at a non-hospital facility (e.g., private surgical or diagnostic clinic or private practice).
- Amount of user charges levied for medically necessary diagnostic services: $ 0
- Amount of user charges levied for insured services: $ 0
- N.B. Charges may be levied for accommodation and meal costs related to a patient who, in the opinion of the attending physician, is a permanent resident in a hospital or other chronic care institution as per the limitation of Section 19 (2). Charges related to this limitation should not be included in the financial statement.
Total for extra-billing and user charges $ 0
- Description of method used to determine amounts of extra-billing and user charges
The following information should be included in the description of the method used to determine the amounts of extra-billing and user charges (EBUC) reported, including if a NIL amount is submitted:
- Name of applicable pieces of PT legislation that prohibit extra-billing and user charges (including facility fees).
Please use as much space as needed below.
The Saskatchewan Medical Care Insurance Act precludes physicians/dentists who provide insured services from charging patients more than the amount paid for that service under the Act, unless the physician/dentist has opted out entirely from receiving payments under the Act. Notice must also be given to the province where a physician/dentist opts out. No notices have been received for the reporting period.
The Saskatchewan Medical Care Insurance Act includes provisions which indicate that any amount that a physician who provides insured services requires a beneficiary to pay or to have paid as a condition of receiving an insured service which exceeds the amount to be paid for that service under the Act, is considered to be a charge.
The Health Facilities Licensing Act precludes any licensee from charging or permitting any other person to charge any fee to any beneficiary for any insured health service performed at the health facility.
- Details about the process used to investigate extra-billing and user charges (e.g., proactive regular audits of provider billings; reactive investigations triggered by patient complaints, media reports or other sources).
Please use as much space as needed below.
With regards to extra-billing, compliance is monitored through consultations with the provincial health authority, physicians and dentists, as well as complaints from members of the public.
When requests are made by a beneficiary seeking reimbursement of monies paid directly to a physician for insured physician services that are extra-billing charges, correspondence is sent to the beneficiary (copying the physician) advising them of Section 18 (1.1) of the Saskatchewan Medical Care Insurance Payment Act that a physician must accept the negotiated rate as payment in full for insured services provided to a beneficiary. Once the physician has received payment from Medical Services for the eligible service(s), reimbursement for any difference in the amount charged by the practitioner and the amount paid by Medical Services should be collected directly from the practitioner. If a further complaint is made, the beneficiary is directed to address complaints to the Saskatchewan College of Physicians and Surgeons.
Persons who have a complaint of an extra-billing charge may raise the concern with the College of Physicians and Surgeons of Saskatchewan. Section 7.1 (Code of Ethics) in the College's bylaws notes the following:
- Treat all patients with respect; do not exploit them for personal advantage. Contravention of, or failure to comply with, the code of ethics is unbecoming, improper, unprofessional or discreditable conduct for the purposes of the Medical Care Insurance Act.
With regards to user charges, compliance is monitored through consultations with the provincial health authority, physicians and dentists, as well as complaints from members of the public.
Persons who have a complaint of user charges may raise the concern with the College of Physicians and Surgeons of Saskatchewan. Section 7.1 (Code of Ethics) in the College's bylaws notes the following:
- Treat all patients with respect; do not exploit them for personal advantage. Contravention of, or failure to comply with, the code of ethics is unbecoming, improper, unprofessional or discreditable conduct for the purposes of the Medical Care Insurance Act.
- A summary of any extra-billing and user charges investigations during the fiscal year including:
- Number of investigations.
- Nature of each investigation (e.g., physician billing audits; patient triggered investigations; private clinic audits; third party report findings (e.g., Auditor General)).Confirmed cases and dollar amounts of extra-billing and user charges.
- Confirmed cases and dollar amounts of extra-billing and user charges.
- Any amounts reimbursed to patients.
Please use as much space as needed bellow.
For the 2021-2022 fiscal year Saskatchewan is reporting $0 in extra-billing. Saskatchewan has no information that extra-billing charges have been levied during the reporting period.
For the 2021-2022 fiscal year Saskatchewan is reporting $0 in User Charges. Saskatchewan has no information that user charges have been levied during the reporting period. Saskatchewan is not aware of charges being levied for insured services provided in a hospital. Nor is Saskatchewan aware of any additional charges for insured services being levied in a physician clinic as defined in the federal private clinics policy.
Please note that MRI and CT scans performed under The Patient Choice Medical Imaging Act (PCMIA) are not reported as these services are non-insured services under The Saskatchewan Medical Care Insurance Act, and are authorized under the PCMIA and The Medical Imaging Facilities Licensing Regulations.
The private-pay MRI/CT service with its unique two-for-one provision gives patients more options in accessing MRI/CT services and has added capacity to the publicly-funded system at no extra cost to the health system or the patient on the public waitlist receiving the reciprocal scan. Along with increases in public capacity, through expanded hospital volumes, new MRI and CT scanners, and increased volumes in publicly funded contracts, these privately funded scans and second scans are assisting in the management of MRI/CT wait times. They increase overall system capacity for less complex cases, thereby freeing up capacity in hospitals to perform more complex exams.
- Details on mechanisms to deter patient extra-billing and user charges (e.g., provider fines; plan payment withholding; provider/patient education initiatives; loss of facility accreditation).
Please use as much space as needed below.
The Saskatchewan Medical Care Insurance Act and the Health Facilities Licensing Act stipulate monetary penalties for individuals guilty of contravening the Act(s), including extra-billing and user charges of insured health services.
Alberta
Canada Health Act
Financial statement of actual amounts of extra-billing and user charges
For the period April 1, 2021 to March 31, 2022
- Amounts of extra-billing
Extra-billing is defined as a charge by an enrolled physician or dentist to an insured person for an insured service in addition to the amount paid by the provincial/territorial health insurance plan.
- Amount of extra-billing levied by enrolled physicians and dentists for insured health services: $ 0
- Amounts of user charges
A user charge is defined as any charge for an insured health service, other than extra-billing. This includes any charge levied for insured hospital services, provided in hospital or at a non-hospital facility (e.g., private surgical or diagnostic clinic), or any non-physician related services provided in conjunction with an insured physician service at a non-hospital facility (e.g., private surgical or diagnostic clinic or private practice).
- Amount of user charges levied for medically necessary diagnostic services: $ 0
- Amount of user charges levied for all other insured services: $ 0
- N.B. Charges may be levied for accommodation and meal costs related to a patient who, in the opinion of the attending physician, is a permanent resident in a hospital or other chronic care institution as per the limitation of Section 19 (2). Charges related to this limitation should not be included in the financial statement.
Total for extra-billing and user charges $ 0
- Description of method used to determine amounts of extra-billing and user charges
The following information should be included in the description of the method used to determine the amounts of extra-billing and user charges (EBUC) reported, including if a NIL amount is submitted:
- Name of applicable pieces of PT legislation that prohibit extra-billing and user charges (including facility fees).
Please use as much space as needed below.
Alberta Health has conducted audits and compliance reviews in accordance with the authority and the provisions of the Alberta Health Care Insurance Act (AHCIA) that mirrors the fundamental principles of the Canada Health Act.
The AHCIA prohibits EBUC in the following sections and imposes penalties as follows:
- Section 9(1), Extra-billing, holds that "No Physician or dentist who is opted into the Plan [Alberta Health Care Insurance Plan] who provides insured services to a person shall charge or collect from any person an amount in addition to the benefits payable by the Minister for those insured services."
- Section 11(1), Other prohibited fees, prescribes that "No person shall charge or collect from any person (a) an amount for any goods or services that are provided as a condition to receiving an insured service provided by a physician or dentist who is opted in to the Plan, or (b) an amount the payment of which is a condition to receiving an insured service provided by a physician or dentist who is opted into the Plan where the amount is in addition to the benefits payable by the Minister for the insured service."
- Section 26(1) (2), Prohibitions, hold that an insurer (carrier, employer, corporation or unincorporated group that administers a self-insurance plan) shall not enter into, issue, maintain in force or renew a contract or initiate or renew a self-insurance plan under which any resident or group of residents is provided with any prepaid basic health services or extended health services or indemnification for all or part of the cost of any basic health services or extended health services.
- Details about the process used to investigate extra-billing and user charges (e.g., proactive regular audits of provider billings; reactive investigations triggered by patient complaints, media reports or other sources).
Please use as much space as needed below.
- Sections 18 and 39 of the AHCIA authorize Alberta Health to reassess claims and conduct audits and compliance reviews after the Minister has paid a claim. Such audits and reviews allow Alberta Health personnel to enter premises and examine practitioner records to gather evidence, which Alberta Health can use to determine EBUC that falls under the AHCIA.
- Alberta Health does not report on audits and/or compliance reviews that are not yet concluded.
- If patients in Alberta have questions or concerns regarding extra-billing or user charges they can direct their inquiries to Alberta Health. The primary mechanisms of inquiry or complaint are:
- Contacting the Alberta Health Care Insurance plan (AHCIP) by phone, fax, mail or email.
- The Alberta Health TIPS line. Patients can call to express concerns and those that are physician or claims related will be directed to the Claims Specialist
- The Statement of Benefits Paid (SOBP) phone line. The SOBP is a list of practitioner services a patient receives during a specified period that have been paid for by the AHCIP. The statement lists dates, general types of service, physician names, and the amount paid to the physicians. Albertans who find health services on their SOBP that they do not recognize can outline the discrepancies and return the SOBP to Alberta Health for investigation.
- Additionally, Alberta Health staff may investigate claims if billing irregularities are noticed as that are being processed.
- A summary of any extra-billing and user charges investigations during the fiscal year including:
- Number of investigations.
- Nature of each investigation (e.g., physician billing audits; patient triggered investigations; private clinic audits; third party report findings (e.g., Auditor General)).
- Confirmed cases and dollar amounts of extra-billing and user charges.
- Any amounts reimbursed to patients.
Please use as much space as needed bellow.
Alberta Health does not report on audit and/or compliance reviews that are not yet concluded.
In 2021-2022, the Business Expertise Team responded to 0 complaints of possible extra-billing from Albertans.
- Details on mechanisms to deter patient extra-billing and user charges (e.g., provider fines; plan payment withholding; provider/patient education initiatives; loss of facility accreditation).
Please use as much space as needed below
Alberta Health uses the following mechanisms to deter EBUC:
- Sections 9(2), 11(3) and (4), 12(1), 13(3) and 14(1) of the AHCIA prescribe that the Minister may send warnings to practitioners, refer contraventions to practitioners' professional regulators, opt practitioners out of the Plan, recover benefits paid, recover and reimburse amounts charged or collected as other prohibited fees, or apply fines.
- Alberta Health issued Bulletin Med 184 on May 25, 2016 to provide information to physicians and billing staff about prohibited billing activities under the AHCIA. This bulletin is available online here.
- Alberta Health uses a risk-based planning process to identify potential areas of inappropriate billing under the AHCIA. Based on this process, high risk subjects for audit and/or a compliance review are selected. The scope of review includes all physicians and other practitioners receiving compensation through the Plan on a fee-for-service-basis or through Alternative Relationship Plans. Payments to hospitals are not in scope.
British Columbia
Canada Health Act
Financial statement of actual amounts of extra-billing and user charges
For the period April 1, 2021 to March 31, 2022
- Amounts of extra-billing
Extra-billing is defined as a charge by an enrolled physician or dentist to an insured person for an insured service in addition to the amount paid by the provincial/territorial health insurance plan.
- Amount of extra-billing levied by enrolled physicians and dentists for insured health services:
- Based on Health Canada Methodology (See Appendix A): $6,817,360.00
- Charges Based on Unresolved Patient Complaints: $ 0
- Cases Found to be Non-Compliant with Cambie Injunction (see Appendix B): $ 31,144.87
Total: $6,848,504.87
- Amounts of user charges
A user charge is defined as any charge for an insured health service, other than extra-billing. This includes any charge levied for insured hospital services, provided in hospital or at a non-hospital facility (e.g., private surgical or diagnostic clinic), or any non-physician related services provided in conjunction with an insured physician service at a non-hospital facility (e.g., private surgical or diagnostic clinic or private practice).
- Amount of user charges levied for medically necessary diagnostic services (Appendix D): $ 11,270,216
- Amount of user charges levied for all other insured services: $ 0
- N.B. Charges may be levied for accommodation and meal costs related to a patient who, in the opinion of the attending physician, is a permanent resident in a hospital or other chronic care institution as per the limitation of Section 19 (2). Charges related to this limitation should not be included in the financial statement.
Total for extra-billing and user charges $ 18,118,720.87
- Description of method used to determine amounts of extra-billing and user charges
The following information should be included in the description of the method used to determine the amounts of extra-billing and user charges (EBUC) reported, including if a NIL amount is submitted:
- Name of applicable pieces of PT legislation that prohibit extra-billing and user charges (including facility fees).
Please use as much space as needed below.
The Medicare Protection Act (MPA) sets out the requirements for insured medical services (also known as benefits) provided to residents of British Columbia (BC). The MPA establishes rules regarding billing for services provided by physicians who are enrolled with the Medical Services Plan (MSP). The MPA also prohibits anyone from charging patients for "materials, consultations, procedures, use of an office, clinic, or for any other matters that relate to the rendering of a benefit" unless specifically permitted by the Medical Services Commission (MSC).
The Canada Health Act (CHA) establishes criteria that provinces must meet with respect to "insured health services" (which include any medically required services of hospitals and medical practitioners) in order to receive full federal transfer payments. The CHA explicitly prohibits user fees and extra-billing of patients for insured services and requires the federal government to deduct an amount equal to such charges from transfer payments to a province involved.
- Details about the process used to investigate extra-billing and user charges (e.g., proactive regular audits of provider billings; reactive investigations triggered by patient complaints, media reports or other sources).
Please use as much space as needed below.
Beneficiary and Diagnostic Services Branch:
The Beneficiary and Diagnostic Services Branch of the BC Ministry of Health (the Ministry) receives correspondence from beneficiaries reporting instances of potential extra-billing and user charges. Ministry staff review and respond to all correspondence on behalf of the MSC, including the use of medical consultants to review medical records. In cases where there is potential extra-billing, letters are sent out to the clinics or individual physicians requesting clarification for any charges as well as reimbursement to beneficiaries in case of erroneous billing, extra-billing or user charges.
Billing Integrity Program, Audit and Investigations Branch:
In 2017, Health Canada and the Ministry agreed upon a methodology to determine the extent and nature of patient extra-billing in BC, outlined in a Terms of Reference and Letter of Agreement. Since this agreement, the Ministry has completed twelve audits of private surgical clinics, including Cambie Surgeries Corporation. The results of these audits were shared with Health Canada in accordance with the signed agreement.
Starting in April 2022, for Health Canada reporting period 2020-2021, the Ministry is required to report extra-billing attributed to private diagnostic facilities. A diagnostic audit framework is under development and the Ministry will commence audits of these facilities once S.18.1 of the MPA is enacted. Currently there are 12 private diagnostic facilities operating in BC. One of these facilities, False Creek Surgical Centre, was previously audited by the Ministry. The Ministry has plans to conduct three private diagnostic facility audits per year, until audits of the 11 remaining facilities have been completed.
The purpose of these audits is two-fold:
- To monitor and assess compliance with the MPA, and
- To help determine an accurate estimate of the extent of extra-billing in the province.
The Ministry will provide the final audit reports for individual clinics and/or providers to Health Canada subject to any redactions required to comply with the Freedom of Information and Personal Privacy Act. The Ministry is working through concerns and legalities around posting summarized versions of audit reports online. The Ministry will be adding communication resources for this work and recruitment to staff these positions will be undertaken in the short term. Their first order of priority will be to make sure this is completed and posted in a timely manner.
Subject to clarification from the Court, the Ministry is committed to full transparency and will continue to work with Health Canada in reviewing audit findings as the work is completed. Monthly conference calls to discuss extra-billing and other pertinent matters including audit findings have been re-established.
- A summary of any extra-billing and user charges investigations during the fiscal year including:
- Number of investigations
- Nature of each investigation (e.g., physician billing audits; patient triggered investigations; private clinic audits; third party report findings (e.g., Auditor General)).
- Confirmed cases and dollar amounts of extra-billing and user charges.
- Any amounts reimbursed to patients.
Please use as much space as needed below.
There were no patient complaints submitted inn 2021-2022. This year appears to be an anomaly, as patient complaints resumed in 2022-2023.
Injunction Data Reporting for 2021-2022
As a term of the December 2020 injunction, private clinics who provided surgeries pursuant to the injunction were required to maintain adequate records to permit the MSC to determine that those surgeries are in accordance with the court order and make those records available to the MSC on demand.
In accordance with this term of the injunction, on February 5, 2021, the MSC issued letters to 50 Non-Hospital Medical Surgical Facilities requesting monthly reporting of data, for the term of the interim order, to ensure compliance with the interim order. On June 3, 2021, a second round of letters was sent to 13 clinics who failed to respond to the first letter.
It was determined that 102 cases (surgeries) were determined to be non-compliant with the injunction, with 69 cases, up to March 31, 2021 being reported in BC's 2020-2021 EBUC report. The remaining 33 cases, from April 1, 2021 and September 30, 2021, are included in this year's extra-billing and user charges report for 2021-2022 (see Appendix B).
- Details on mechanisms to deter patient extra-billing and user charges (e.g., provider fines; plan payment withholding; provider/patient education initiatives; loss of facility accreditation).
Please use as much space as needed below.
In October 2018, BC brought the remaining provisions of the Medicare Protection Amendment Act Bill 92 (2003) into force to address the province's ability to respond to extra-billing and to bring BC in compliance with the CHA.
The key changes to the MPA resulting from Bill 92 include:
- Offence provisions for practitioners and/or clinics who contravene extra-billing; fines of up to $10,000 for a first offence and up to $20,000 for a second or subsequent offence;
- Ability for the MSC to cancel the enrolment of a practitioner for "cause";
- A beneficiary (or person who pays for service) is entitled to a refund for an amount that is paid contrary to the extra-billing provisions contained in the MPA;
- The MSC may reimburse a beneficiary (or the person who paid for an insured service) in exchange for assigning the claim arising due to extra-billing, and pursue the debt against the person who improperly charged for the service;
- Clarification on general limits on extra-billing by enrolled practitioners; and
- An increase in the scope of the limits on extra-billing by non-enrolled medical practitioners.
To date, the powers to lay fines and reimburse beneficiaries have not been exercised, due to injunctions that have been in place. However, given the successful outcome through two levels of provincial court and the Supreme Court of Canada, the province is currently working to operationalize these powers.
Currently, the regional Health Authorities (HAs) monitor the surgical contracts for compliance with all provisions. Since implementation in September 2018, the HAs have not terminated any contracts with private surgical clinics over performance or compliance issues. The Ministry is confident that the agreements are being followed by the physicians and HAs. Overall, the Ministry views this current productive dynamic between HAs and clinics (formerly providing private services) as demonstrative of the value of contractual arrangement to bring private surgical services back into the public system. This approach simultaneously eliminates extra-billing practices and enhances the capacity of the public health system to provide needed patient care.
The Ministry works closely with the MSC to ensure that operational processes are designed to protect patients from extra-billing. The Ministry processes patient complaints and investigates allegations of extra-billing to determine whether extra-billing has taken place. Where possible, throughout the investigation, the Ministry seeks to resolve the complaint by communication and education with the physician.
Yukon
Canada Health Act
Financial statement of actual amounts of extra-billing and user charges
For the period April 1, 2021 to March 31, 2022
- Amounts of extra-billing
Extra-billing is defined as a charge by an enrolled physician or dentist to an insured person for an insured service in addition to the amount paid by the provincial/territorial health insurance plan.
- Amount of extra-billing levied by enrolled physicians and dentists for insured health services: $ 0
- Amounts of user charges
A user charge is defined as any charge for an insured health service, other than extra-billing. This includes any charge levied for insured hospital services, provided in hospital or at a non-hospital facility (e.g., private surgical or diagnostic clinic), or any non-physician related services provided in conjunction with an insured physician service at a non-hospital facility (e.g., private surgical or diagnostic clinic or private practice).
- Amount of user charges levied for medically necessary diagnostic services: $ 0
- Amount of user charges levied for all other insured services: $ 0
- N.B. Charges may be levied for accommodation and meal costs related to a patient who, in the opinion of the attending physician, is a permanent resident in a hospital or other chronic care institution as per the limitation of Section 19 (2). Charges related to this limitation should not be included in the financial statement.
Total for extra-billing and user charges $ 0
- Description of method used to determine amounts of extra-billing and user charges
The following information should be included in the description of the method used to determine the amounts of extra-billing and user charges (EBUC) reported, including if a NIL amount is submitted:
- Name of applicable pieces of PT legislation that prohibit extra-billing and user charges (including facility fees).
Please use as much space as needed below.
There are no user fees or co-insurance charges for Insured Health Services under the Yukon Health Care Insurance Plan or the Yukon Hospital Insurance Plan. All services are provided on a uniform basis and are not impeded by financial or other barriers. There is no extra-billing in Yukon for any services covered by the plans.
The Yukon Health Care Insurance Plan Act defines Insured Health Services as:
"those physician services, surgical-dental services, and other health services including the supply of drugs, medical and dental supplies, prostheses…"
In FY 2021-2022, Yukon did not have any private for-profit health care facilities delivering insured health services. Information submitted excludes government-operated continuing care facilities in Yukon.
- Details about the process used to investigate extra-billing and user charges (e.g., proactive regular audits of provider billings; reactive investigations triggered by patient complaints, media reports or other sources).
Please use as much space as needed below.
Regular audits of physician claims along with reactive investigations triggered by client and/or other physician complaints. Annual audit of the programs by the Auditor General.
- A summary of any extra-billing and user charges investigations during the fiscal year including:
- Number of investigations. 0
- Nature of each investigation (e.g., physician billing audits; patient triggered investigations; private clinic audits; third party report findings (e.g., Auditor General)). N/A
- Confirmed cases and dollar amounts of extra-billing and user charges. 0
- Any amounts reimbursed to patients. 0
Please use as much space needed bellow or add extra pages as necessary.
- Details on mechanisms to deter patient extra-billing and user charges (e.g., provider fines; plan payment withholding; provider/patient education initiatives; loss of facility accreditation).
Please use as much space as needed below.
The preamble to the Yukon Physician Fee Guide contains the following:
"No fee above or in addition to the Payment Schedule may be charged to either YHCIP (Yukon Health Care Insurance Plan) or to the patient for insured health services."
Northwest Territories
Canada Health Act
Financial statement of actual amounts of extra-billing and user charges
For the period April 1, 2021 to March 31, 2022
- Amounts of extra-billing
Extra-billing is defined as a charge by an enrolled physician or dentist to an insured person for an insured service in addition to the amount paid by the provincial/territorial health insurance plan.
- Amount of extra-billing levied by enrolled physicians and dentists for insured health services: $ 0
- Amounts of user charges
A user charge is defined as any charge for an insured health service, other than extra-billing. This includes any charge levied for insured hospital services, provided in hospital or at a non-hospital facility (e.g., private surgical or diagnostic clinic), or any non-physician related services provided in conjunction with an insured physician service at a non-hospital facility (e.g., private surgical or diagnostic clinic or private practice).
- Amount of user charges levied for medically necessary diagnostic services: $ 0
- Amount of user charges levied for all other insured services: $ 0
- N.B. Charges may be levied for accommodation and meal costs related to a patient who, in the opinion of the attending physician, is a permanent resident in a hospital or other chronic care institution as per the limitation of Section 19 (2). Charges related to this limitation should not be included in the financial statement.
Total for extra-billing and user charges $ 0
- Description of method used to determine amounts of extra-billing and user charges
The following information should be included in the description of the method used to determine the amounts of extra-billing and user charges (EBUC) reported, including if a NIL amount is submitted:
- Name of applicable pieces of PT legislation that prohibit extra-billing and user charges (including facility fees).
Please use as much space as needed below.
There are two pieces of legislation in the Northwest Territories which prohibit extra-billing and user charges. Section 14(1) of the Northwest Territories Medical Care Act states that: "No medical practitioner shall charge to or collect from an insured person a fee in excess of the benefit in respect of the insured service, unless the medical practitioner has made an election that is still in effect." In addition, section 8(2) of the Hospital Insurance Regulations under the Hospital Insurance and Health and Social Services Administration Act also states that: "The rate payable to a hospital or federal hospital that is situated in a province or territory participating under the federal Act (i.e. Canada Health Act) shall not exceed the rate established for the hospital by that province or territory, less the authorized charge." Therefore, residents of the NWT are protected from extra-billing and charges when receiving insured services both within the territory, and when receiving insured services outside the territory under a reciprocal billing agreement.
- Details about the process used to investigate extra-billing and user charges (e.g., proactive regular audits of provider billings; reactive investigations triggered by patient complaints, media reports or other sources).
Please use as much space as needed below.
Medical Care Act 8. (1) (2) (3) (4)
8.(1) The Director may reassess an account for insured services submitted by a medical practitioner, where, as a result of an inspection under section 7, it appears to the Director that (a) all or part of the insured services were not in fact rendered; (b) all or part of the insured services were not medically necessary; (c) all or part of the insured services were not provided in accordance with accepted professional standards and practice; or (d) the nature of the insured services is misrepresented.
(2) Where the Director makes a reassessment under subsection (1), the Director may make any appropriate adjustment in the amount paid to the medical practitioner in respect of the insured services.
(3) If the amount paid to a medical practitioner for insured services was in excess of the benefit payable under the adjustment referred to in subsection (2), the difference between the amount paid and the adjusted amount constitutes a debt to the Government of the Northwest Territories and the Director may recover the amount from the medical practitioner (a) by withholding from benefits payable to the medical practitioner an amount equivalent to the difference between the amount paid and the adjusted amount; (b) by civil action; or (c) pursuant to an agreement between the Director and the medical practitioner providing for the payment of the amount.
(4) If the amount paid to a medical practitioner for insured services was less than the benefit payable under the adjustment referred to in subsection (2), the Director shall pay to the medical practitioner an amount equal to the difference between the amount paid and the adjusted amount.
The NWT has a "complaint-based" system in place, and takes steps to respond to concerns and improve care and services for NWT residents. When a resident has a concern or issue with the care they have received they are first encouraged to speak with their local health provider. If the issue is not resolved they are encouraged to contact their designated Patient Representative to help address the issue and file a formal complaint.
The Medical Care Act includes a provision to allow the Minister of Health and Social Services (the Minister) to establish a Benefits Appeal Committee that could address any matter referred to it by the Minister, including complaints where a physician engaged in extra-billing and charged user fees. At present, there has been no need to establish this committee, because almost all physicians are compensated through contractual agreements with the Government of the NWT.
No audits completed. Mostly salaried physicians
All but two physicians in the NWT are on contract with the NT Health Authority and do not bill fee for service. The two NWT Fee for Service Physicians and all visiting specialists use the services of local NWT billing clerks who bill the appropriate fees according to the NWT fee tariff.
- A summary of any extra-billing and user charges investigations during the fiscal year including:
- Number of investigations. Zero
- Nature of each investigation (e.g., physician billing audits; patient triggered investigations; private clinic audits; third party report findings (e.g., Auditor General)). N/A
- Confirmed cases and dollar amounts of extra-billing and user charges. $0
- Any amounts reimbursed to patients. $0
Please use as much space as needed below.
- Details on mechanisms to deter patient extra-billing and user charges (e.g., provider fines; plan payment withholding; provider/patient education initiatives; loss of facility accreditation).
Please use as much space as needed below.
Mostly salaried physicians
All but two physicians in the NWT are on contract with the NT Health Authority and do not bill fee for service. The two NWT Fee for Service Physicians and all visiting specialists use the services of local NWT billing clerks who bill the appropriate fees according to the NWT fee tariff.
Nunavut
Canada Health Act
Financial statement of actual amounts of extra-billing and user charges
For the period April 1, 2021 to March 31, 2022
- Amounts of extra-billing
Extra-billing is defined as a charge by an enrolled physician or dentist to an insured person for an insured service in addition to the amount paid by the provincial/territorial health insurance plan.
- Amount of extra-billing levied by enrolled physicians and dentists for insured health services: $ 0
- Amounts of user charges
A user charge is defined as any charge for an insured health service, other than extra-billing. This includes any charge levied for insured hospital services, provided in hospital or at a non-hospital facility (e.g., private surgical or diagnostic clinic), or any non-physician related services provided in conjunction with an insured physician service at a non-hospital facility (e.g., private surgical or diagnostic clinic or private practice).
- Amount of user charges levied for medically necessary diagnostic services: $ 0
- Amount of user charges levied for all other insured services: $ 0
- N.B. Charges may be levied for accommodation and meal costs related to a patient who, in the opinion of the attending physician, is a permanent resident in a hospital or other chronic care institution as per the limitation of Section 19 (2). Charges related to this limitation should not be included in the financial statement.
Total for extra-billing and user charges $ 0
- Description of method used to determine amounts of extra-billing and user charges
The following information should be included in the description of the method used to determine the amounts of extra-billing and user charges (EBUC) reported, including if a NIL amount is submitted:
- Name of applicable pieces of PT legislation that prohibit extra-billing and user charges (including facility fees).
Please use as much space as needed below.
NIL
- Details about the process used to investigate extra-billing and user charges (e.g., proactive regular audits of provider billings; reactive investigations triggered by patient complaints, media reports or other sources).
Please use as much space as needed below.
NIL
- A summary of any extra-billing and user charges investigations during the fiscal year including:
- Number of investigations.
- Nature of each investigation (e.g., physician billing audits; patient triggered investigations; private clinic audits; third party report findings (e.g., Auditor General)).
- Confirmed cases and dollar amounts of extra-billing and user charges.
- Any amounts reimbursed to patients.
Please use as much space needed below.
NIL
- Details on mechanisms to deter patient extra-billing and user charges (e.g., provider fines; plan payment withholding; provider/patient education initiatives; loss of facility accreditation).
Please use as much space as needed below.
NIL
Annex D - Reimbursement action plans and progress reports
Under the Reimbursement Policy, provinces and territories (PT) subject to a Canada Health Transfer (CHT) deduction as a result of patient charges are eligible for reimbursement should they demonstrate action has been taken to come into compliance with the Canada Health Act and the patient charges have been eliminated.
Following a CHT deduction as a result of patient charges, Health Canada officials work collaboratively with PT officials to reach a mutually agreed upon Action Plan. Given the circumstances leading to deductions will vary by jurisdiction, so too will the conditions for reimbursement, and the resulting Action Plans. However, the overarching objective of the Reimbursement Policy is the effective elimination of patient charges.
In addition to the Reimbursement Action Plan, PTs must submit annual progress reports to Health Canada that outline the degree to which the plan has been implemented. Upon review of the jurisdiction's report, if Health Canada is satisfied that key elements of the Action Plan have been fulfilled, the PT could receive a partial or full reimbursement. Following an initial deduction and reimbursement cycle, if Health Canada remains satisfied that patient charges have been eliminated, the Reimbursement Policy allows for the immediate reimbursement of subsequent CHT deductions.
Action plans, and PT progress reports on meeting their plans, are published on the following pages.
For further details on the Reimbursement Policy please refer to Annex C which includes the full text.
[Following is the text of the Newfoundland and Labrador's Reimbursement Action Plan and January 2025 Status Update]
Newfoundland and Labrador Reimbursement Action Plan
Background
In the winter of 2017-2018, the Department of Health and Community Services (HCS) received phone calls from Medical Care Plan (MCP) beneficiaries complaining that they had paid out of pocket for cataract surgery.
Investigation
In February 2018, HCS issued a Public Service Announcement (PSA) in an effort to identify beneficiaries in the province who felt that they had been billed inappropriately for insured cataract surgery and created a hotline for reporting of such instances.
- The hotline received over 600 calls after the PSA was launched.
- Documentation was provided by 73 callers confirming that cataract surgery was performed and paid for out of pocket.
- It was determined that the callers who produced documentation paid varying totals from approximately $1,000 to $4,000 total per eye.
- Two of these 73 cases fell within the 2016-2017 fiscal year, which resulted in a $1,349 deduction to NL's Canada Health Transfer in March 2019, as per the Canada Health Act.
- HCS continues to receive calls and documents regarding cataract surgery paid out of pocket by MCP beneficiaries.
Corrective action through patient reimbursement and further investigation
HCS plans to reimburse patients for the excision of the cataract and intraocular lens replacement at a rate of $574.47 per eye when patients can produce documents verifying that they have paid for cataract surgery in a private clinic until June 15, 2018. The amount of $574.47 represents the professional fees billable for the excision of the cataract ($473.09) and insertion of the intraocular lens ($101.38). HCS is not reimbursing the costs of non-insured services associated with providing cataract surgery in a private clinic.
- The callers without documentation will not be included in the totals for extra-billing and user charges reporting under the Canada Health Act as there is insufficient evidence to demonstrate that the patients paid out of pocket for cataract surgery.
- To date, HCS has not further contacted callers who have not provided documentation. However, HCS will review the cataract phone line results, directly reaching out to any patients who may meet criteria for reimbursement but did not submit the relevant documents.
- To ensure that reimbursement is available to eligible patients who have not yet been identified, HCS plans to issue a news release regarding reimbursement for insured professional fees in a further attempt to identify patients who may have paid charges associated with cataract surgery in the private clinic setting.
Legal declaration
On March 28, 2018, in Jackman v. Newfoundland and Labrador, the Applicants filed an application for declaratory relief with the Supreme Court of Newfoundland and Labrador, General Division, on three matters:
- That there is no legislative prohibition to removing a cataractous lens in a private office.
- That the removal of a cataractous lens by an ophthalmologist in a private office is a non-insured service.
- That a supplementary list of services, when provided by an ophthalmologist in a private clinic, are non-insured services.
On March 6, 2019, Justice Goodridge declared that:
- Prior to June 15, 2018, there was no legislative prohibition to removing a cataractous lens in a private office.
- Prior to June 15, 2018, the removal of a cataractous lens by an ophthalmologist in a private clinic was an insured service.
- The supplementary list of services provided are non-insured services when provided in a private clinic.
Corrective action through legislative and policy amendments
- On June 15, 2018, legislative amendments were filed in order to clarify the type of cataract surgery that is insured under MCP and where those surgeries could occur. Section 4(1)(x.1) of the Medical Care Insurance Insured Services Regulations which stated that non-insured services included those not otherwise authorized or grandfathered into private clinics as of a certain date, was subject to different interpretations in Jackman v. Newfoundland and Labrador.
- Recognizing the difficulties in interpretation of this particular clause, the section was later repealed and replaced on June 15, 2018, with: 3. (2) For greater certainty, the medically necessary removal and replacement of a cataractous lens by any procedure is an insured service and shall be performed in a hospital or a facility designated by the Lieutenant-Governor in Council (Reg. 47/18).
- On January 30, 2019, HCS announced that cataract surgery would be available in private offices throughout the province in the near future.
- HCS worked with the Newfoundland and Labrador Medical Association (NLMA) to establish, on April 17, 2019, Schedule O: Cataract Surgery Service Fees in Non-Hospital Designated Facilities. This schedule is an amendment to the 2013-2017 Memorandum of Agreement between the Government of Newfoundland and Labrador and the NLMA.
- As part of the transition to include cataract surgery in private offices, HCS will be working with the Regional Health Authorities to establish a central intake process with the objective of improving wait times for cataract surgery across the province.
- HCS is continuing to undertake the necessary steps towards establishing a policy to designate non-hospital facilities that will include, but is not limited to, issues concerning patient safety and facility accreditation.
- HCS is also considering introducing broader legislation for the transitioning of other hospital-based procedures.
- HCS is investigating models to prevent extra-billing and user charges related to cataract surgery.
- Providers operating out of designated facilities will be required to inform patients that they are not required to purchase any additional optional add-on services which are uninsured.
- HCS plans to publish guidelines for physicians and patients outlining insured costs associated with cataract surgery in a plain language format.
- As of January 1, 2019, HCS has adopted the aspheric lens as the new standard, ensuring that patients will no longer be billed for the basic lens associated with cataract surgery.
Conclusion
This action plan was created as part of the Reimbursement Policy under the Canada Health Act and with the intention of eliminating patient charges for medically necessary cataract surgery. These efforts have been made in hopes of obtaining a reimbursement for Canada Health Transfer deductions in the amount of $1,349 taken in March 2019 for fiscal year 2016-2017, and in hopes of obtaining an immediate reimbursement for deductions resulting from the remaining patient charges that occurred in subsequent fiscal years.
January 2025 status report, implementation of Newfoundland and Labrador's Reimbursement Action Plan
Summary of actions
Starting in late 2017, the Department of Health and Community Services (HCS) began receiving phone calls from Medical Care Plan (MCP) beneficiaries complaining about out-of-pocket charges being levied for cataract surgery. In February 2018, HCS issued a Public Service Announcement (PSA) and created a Cataract Surgery Information Line in an effort to identify beneficiaries who may have been billed inappropriately for insured cataract surgery.
On June 15, 2018, amendments to the Medical Care Insurance Insured Services Regulations were introduced to clarify that "the medically necessary removal and replacement of a cataractous lens by any procedure is an insured service and shall be performed in a hospital or a facility designated by the Lieutenant-Governor in Council".
As of January 1, 2019, HCS adopted the aspheric lens as the new standard for cataract surgery, ensuring that patients would no longer be billed for this lens when inserted during insured cataract procedures.
In January 2019, HCS announced that cataract surgery would be available in private offices throughout the province in the near future. In April 2019, an Amending Agreement to add Schedule "O" to the 2013- 2017 Memorandum of Agreement was signed by HCS and the Newfoundland and Labrador Medical Association (NLMA). Schedule "O" outlines an agreement between HCS and the NLMA with respect to service fees for cataract surgeries performed in designated facilities. In January 2021, the Lieutenant- Governor in Council designated two non-hospital facilities to provide insured cataract surgery. A third facility was designated in April 2022.
In February of 2020, a PSA was issued to outline a Reimbursement Process for Cataract Surgeries.
The Department of Health and Community Services conducted a review in 2022 of the provincial allocation of out-of-hospital cataract surgery and the Policy for the Provision of Cataract Surgery in Non- Hospital Designated Facilities. This review included a calculation of Total Predicted Regional Demand (TPRD) for cataract surgery in each region of the province, as well as evaluating wait lists, national benchmarks for wait times, and adherence to the policy by designated facilities.
As a result of that evaluation, the Department approved an increase of 3,300 procedures to the regional caps on cataract surgery in designated facilities from October 1, 2022 until March 31, 2024 (18 months total with 1,100 performed in the second half of 2022-23 and 2,200 performed in 2023-24). Budget 2023 provided a further 1,500 procedures and thus the total out-of-hospital procedures for 2023-24 was brought to 7,200 (3,500 + 2,200 + 1,500).
In July 2024, the Department and the Newfoundland and Labrador Medical Association, on behalf of the three Non-Hospital Designated Facilities, negotiated an agreement to further supplement the 3,500 procedures performed out of hospital under Schedule 'O'. An additional 3,200 procedures are allocated annually at the same facility fee as Schedule 'O' and an additional 2,100 procedures at a reduced facility fee. This brings the annual number of procedures going forward to 8,800. As well, the Provincial Health Authority is working to complete a Provincial Central Intake Process, after which, the caps on procedures out of hospital will be removed. The Department anticipates that funding more out-of-hospital cataract procedures will increase patient access to insured cataract surgery.
Corrective action through patient reimbursement and further investigation
Following the 2018 PSA, HCS issued another PSA on the Reimbursement Process for Cataract Surgeries on February 20, 2020. As part of this process, HCS established a dedicated phone line (1-844-957-1401) and email address(cataract@gov.nl.ca) for patients. HCS also directly contacted individuals who had previously reached out to HCS via the Cataract Surgery Information Line of 2018. As part of the Reimbursement Process, HCS reviewed information provided from new patients that had not previously contacted HCS until the 2020 PSA was released. HCS is now reporting a total of $132,574.42 in user charges identified for 135 individuals and $127,532.34 paid to 130 individuals for procedures performed prior to the legislative amendments introduced on June 15, 2018. This total of $132,574.42 represents the professional fees for cataract surgery for 134 patients and includes an extra-billing amount of $650 identified for one patient. Not all patients who contacted HCS were eligible for reimbursement. There were several reasons patients did not meet the eligibility criteria for reimbursement. For example, under the Reimbursement Process, June 15, 2018 was established as the cut-off date for reimbursement. This date coincided with the coming into force of the legislative amendments. As such, patients whose procedures were performed after June 15, 2018, were not eligible for reimbursement, and therefore have not been reimbursed. In other instances where a claim was denied, the documentation submitted by the patient may not have provided sufficient evidence that the service provided was an insured cataract procedure.
While the reimbursement cut-off date has passed, the review process remains open. HCS continues to review documents submitted by patients and report any instances of patient user charges.
In 2024, Medical Services, HCS received requests from two individuals regarding reimbursement of charges associated with eye procedures. One enquiry included documents for review for procedures on both eyes. The request was also accompanied by a document from the treating clinic indicating that the patient was diagnosed with cataracts but opted for a non-insured lens to be implanted into both eyes (i.e. Refractive Lens Exchange). The correspondence provided went on to describe that "Cataract Surgery is covered by the provincial healthcare plan (MCP) using a standard monofocal lens". The patient was subsequently charged $6,095 for "Premium Vision Correction". The itemized invoice lists a breakdown of this amount into costs associated with the non-insured lens, laser system, non-insured diagnostics, a 3 year laser enhancement plan, as well as a post-surgical refractive lens kit. There was no charge for removal of the natural lens. As in past years, the invoice included strong language that the procedure was not insured by NL's public health care plans and "not eligible for MCP reimbursement". The itemized invoice indicated that the service was considered a "vision upgrade" with the role of the procedure "to provide the best refractive outcome" and that the procedure does not "reduce the wait times for surgery". Details of this patient enquiry will be included in the Financial Statement of Actual Amounts of Extra-Billing and User Charges 2023-2024.
Medical Services has not received any new enquiries of this nature since March 2024.
Proactive action through Policy for New Non-Hospital Designated Facilities
In 2020, HCS developed the Policy for the Provision of Cataract Surgery in Non-Hospital Designated Facilities (updated in July 2024), which outlines the requirements and expectations for these facilities. Section 14.1 of the policy specifically deals with expectations regarding extra-billing and user charges, which are prohibited. The ophthalmologist has a duty to make sure that the patient understands that all insured services are available without any charge (to the patient). Non-hospital designated facilities must provide an itemized list of services billed to ensure clarity between insured and billable non-insured services. Non-hospital designated facilities must also post a Patient Information Sheet in visible areas for public viewing in their offices and patients receiving cataract surgery must also receive and sign a copy to indicate their understanding. HCS will investigate any patient complaints of suspected extra-billing or user charges.
The Lieutenant-Governor in Council has the authority to suspend or cancel a non-hospital facility's designation status if the non-hospital designated facility has failed to comply with the policy.
[Following is the text of the Nova Scotia's 2025 Reimbursement Action Plan]
Nova Scotia's Reimbursement Action Plan regarding Diagnostic Services
This document describes actions being taken in Nova Scotia to eliminate patient charges for medically necessary diagnostic services.
Background
Nova Scotia continues to invest in its publicly funded healthcare system and continues to focus on providing diagnostic imaging services within the public system. In fiscal year 2024-2025, Nova Scotia's budget included increase investment of more than $19 million in Diagnostic Imaging. Significant work is underway, guided by Nova Scotia's Action for Health plan, to advance a robust public health system including improvements to access to diagnostic imaging services through measures to reduce wait times.
Nova Scotia has expanded diagnostic services capacity through a 5 -year strategy to improve quality, safety and access. In May 2024, Government announced four new magnetic resonance imaging (MRI) machines in the Province. In addition to investing in new, modernized equipment, the strategy includes:
- A provincial centralized electronic referral system;
- Hiring additional medical radiation technologists;
- New provincial quality control standards;
- New, patient-centred processes for cancellation and rebooking of
In the three years since implementing Action for Health, Nova Scotia has seen a 20% increase in MRI volumes, a 31% increase in CT volumes, and a 26% increase in ultrasound volume. Nova Scotia has prioritized improving patient wait times to a target of within 60 days across MRI, CT and ultrasound services.
Nova Scotia has one private clinic (HealthView Medical Imaging) in the province which operates both MRI and ultrasound services in a private capacity. This clinic was identified by Health Canada during the 2020-2021 extra-billing and user charges reporting period as providing medically necessary diagnostic imaging services. Health Canada has estimated the clinic's billings for medically necessary services as follows:
- $1,277,659 for 2023-2024 (due to billings in 2020-2021)
- $1,794,635 for 2024-2025 (due to billings in 2021-2022)
Corrective action to be taken
In addition to investing in new equipment and staff, Nova Scotia's strategy to increase access includes new partnerships with service providers across the health system. In 2024, the Nova Scotia Health Authority (NSHA) entered into a five-year, $7.6-million agreement with Healthview Medical Imaging to provide publicly funded MRI and ultrasound scans services agreement that will increase public access and address patient extra-billing and user charges. This equates to at least 1,500 more MRI and 1,000 more Ultrasound appointments each year.
Key provisions under the agreement related to Canada Health Act requirements and Health Canada's Diagnostic Services Policy include:
- The clinic is required to comply in all respects with the provisions of the Canada Health Act and all relevant federal and provincial legislation.
- Referrals to Healthview under the agreement are made by the NSHA based on publicly managed triage and scheduling processes. Patients do not self-refer.
- The clinic cannot charge any patient any amount in relation to the services being
- Patient access is prioritized based on triage and scheduling considerations, access cannot be prioritized based on an ability or willingness to pay out of pocket, and the clinic shall not give any person priority over referred NSH patients to receive services.
Nova Scotia's new single-entry intake model for managing and coordinating referrals was introduced in 2023 and is mandatory for some health care providers. This model is supported by an electronic referral tool, a surgical central intake office / centralized waitlist, and diagnostic imaging central queue. The new model allows referral routing to occur based on the best information and evidence available, including patient preferences regarding service location. A small number of patient referrals may occur outside of the single-entry intake model while it continues to be rolled out; however, the improved referral process that provides faster access to care and improved patient awareness of their referral status, in combination with the contractual inability for the clinic to charge referred NSHA patients to receive services, is expected to make the likelihood of patient charges occurring for medically necessary services low.
In addition to meeting its the minimum contracted volume, the NSHA will have the option of purchasing additional services from the clinic as needed to meet wait time targets. If this is not required, the clinic may have additional capacity and is permitted to continue to offer its diagnostic services privately, including to patients not covered by the Canada Health Act (i.e. for research, worker's compensation, or Canadian Armed Forces clients). These volume commitments are expected to match the capacity of the clinic's ability to provide services.
Nova Scotia's DSP Reimbursement Plan is intended to discourage insured patients against seeking private services while also acknowledging the clinic's business model to provide for uninsured services.
Evaluation and monitoring
Provisions under the agreement between the NSHA and Healthview will allow monitoring of the number of patients referred to the clinic and the timeliness and quality of the services provided to them. In implementing this reimbursement action plan, Nova Scotia will monitor that information, and will also incorporate upcoming results of the 2024 Statistics Canada survey on private diagnostic imaging clinics, which is intended to provide reliable data regarding the activities of private clinics to provinces. It is anticipated that the data from the 2024 Statistics Canada survey will identify whether any patient charges are occurring, and indicate the need for possible need for further action in Nova Scotia to address patient charges.
Information will continue to be provided to Health Canada through the Canada Health Act Annual Report and reporting on Extra-billing and User Charges.
[Following is the text of the New Brunswick's 2025 Reimbursement Action Plan]
New Brunswick Abortion Reimbursement Action Plan Outline, January 2025
Background
In New Brunswick, patients seeking medically necessary surgical abortions faced financial barriers due to Regulation 84-20 under the Medical Services Payment Act. This regulation only covered abortions performed at specific hospitals (Chaleur Regional, Moncton, and Dr. Georges-L.-Dumont) and excluded private clinics like Clinic 554. As a result, patients who sought services at private clinics had to pay out of pocket, creating financial barriers, particularly for those who could not afford the costs.
Prior to changes, paragraph (a.1) of Schedule 2 in Regulation 84-20 stated that abortions could only be covered if performed in an approved hospital facility within the province. If the procedure took place in a private clinic, it was not considered an entitled service under the provincial health plan.
Investigation and reporting
Since Clinic 554 is now closed and New Brunswick does not collect financial data from private clinics, the province cannot provide specific information on patient charges for services previously offered at the clinic. Instead, New Brunswick will use data from the Induced Abortions in Canada survey, compiled by the Canadian Institutes of Health Information (CIHI), which includes information from Clinic 554 before it closed. This data will be submitted to Health Canada, noting it reflects services prior to the clinic's closure.
Corrective action to be taken
On November 7, 2024, New Brunswick expanded coverage for surgical abortion services by repealing paragraph (a.1) of Schedule 2 of Regulation 84-20. This change allows surgical abortions at private clinics to be reimbursed under the provincial Medicare plan, removing out-of-pocket costs for patients.
In fall 2022, amendments to the Regional Health Authorities Act, the Medical Services Payment Act and related regulations were made to enable insured surgical services outside hospitals. The Health Facilities Act was then established in 2023 and sets rules for publicly funded surgical facilities, including agreements with regional health authorities, ministerial approval, and accreditation.
The Department of Health will continue to collaborate with stakeholders to determine how these services will be delivered in the community.
Conclusion
These changes are aligned with the Canada Health Act and will help New Brunswick receive reimbursement for Canada Health Transfer deductions. Medicare will now fully cover medically necessary abortions, whether performed in a hospital or health facility. Further efforts will focus on improving service delivery and increasing access to abortion services across the province.
[Following is a description of Quebec's Reimbursement Action Plan to eliminate patient charges for medically necessary diagnostic scans, which was communicated in a December 14, 2023 exchange between officials, and February 6, 2025 Status Update.]
Quebec Reimbursement Action Plan to eliminate patient charges for medically necessary diagnostic scans
Bill 15, an Act to make the health and social services system more efficient, which has been completed in the Quebec National Assembly, reiterates the responsibility of the public health and social services network to ensure the provision of medically required services to meet the social and health needs and specific characteristics of the Quebec population, particularly diagnostic services.
To this end, the Act provides that the presidents and chief executive officers of the institutions shall create conditions favourable to access to general and specialized medical services, to their continuity and to their networking, in conjunction with the territorial departments of family medicine and specialized medicine, paying particular attention to the accessibility of:
- diagnostic technical platforms for all doctors;
- clinical information, including the results of diagnostic examinations such as laboratory and medical imaging tests, drug profiles and case summaries.
This legislative provision shows that the Quebec government is continuing its work to ensure that these services remain covered by its public system.
It is therefore with a view to offering Quebecers better access to the right healthcare professional at the right time, and to ensuring a better response to the needs of the population through better control of needs and supply, that Bill 15 provides for the creation of Santé Québec, whose mandate will include overseeing and coordinating the activities of private establishments and certain other service providers.
Secondly, we confirm that the contracts established between private clinics and public establishments include the scope of the measures taken and that the medically necessary services rendered by private clinics under these contracts do not entail any additional costs for patients.
In addition, in order to improve access to specialized medical services, Santé Québec may propose to the Minister that a Santé Québec establishment that carries on hospital activities be associated with the operator of one of the following businesses in order to entrust it with the provision of certain specialized medical services to users of the establishment.
Before accepting Santé Québec's proposal, the Minister must be of the opinion that it is likely to improve access to the specialized medical services concerned and that it will not affect the capacity of the public health and social services network, particularly with regard to the workforce required to operate this network. It is also required to take into account the efficiency and effectiveness gains resulting from the implementation of this proposal.
This mechanism will strengthen both the effectiveness and accessibility of the network, as well as the Minister's decision-making power, thereby ensuring that no costs are incurred by users, in compliance with the Act respecting health services and social services.
In addition, the law also requires user satisfaction to be measured, so that services can be rapidly adapted accordingly. A national users' committee will be set up with responsibility for harmonising the practices of users' committees in institutions and making recommendations to the Board of Directors of Santé Québec. The law also provides for the addition of a national complaints commissioner. This will ensure that the Minister is effectively informed if a patient finds himself in a position where he has to pay for medically required services himself.
February 2025 Status Update, Implementation of Quebec's Reimbursement Action Plan
I am writing further to your letter of January 31, in which you informed us of a possible cut to the Canada Health Transfer, in connection with an estimate of out-of-pocket expenses incurred by patients for diagnostic services obtained in private clinics. Quebec acknowledges the estimated amount of $35,249,525.
As you mentioned, Quebec is making numerous efforts to improve the efficiency of the public healthcare system on its territory. The Act respecting the governance of the health and social services system, as well as the contracts signed between hospitals in the health and social services network, are all examples of Quebec's determination to ensure the provision of medically required services to meet the social and health needs and specific characteristics of the Quebec population, particularly diagnostic services.
Similarly, the Plan pour mettre en œuvre les changements nécessaires en santé, launched on March 29 by the Quebec government, is based on the vision of offering all Quebecers a patient experience focused on accessibility, quality of care and value.
As previously mentioned, Quebec has no data on the fees that certain citizens voluntarily choose to pay for the private provision of diagnostic services. We also have serious reservations about the method used to determine the out-of-pocket expenses incurred by Quebec citizens for diagnostic services.
[Following is the text of the Ontario's Reimbursement Action Plan and February 2025 Status Update which was communicated in a February 10, 2025 exchange between officials]
Ontario Reimbursement Action Plan
Background
Ontario's Extra-Billing and User Charges (EBUC) legislative framework
Ontario recognizes that medicare is a fundamental Canadian value and its preservation is essential for the health of Ontarians, now and in the future. Ontario continues to support the prohibition of two-tier medicine, extra-billing and user fees in accordance with the Canada Health Act (CHA) and is committed to ensuring that accessibility is a central principle of medicare in Ontario.
The Health Insurance Act (HIA), the Independent Health Facilities Act (IHFA) and the Commitment to the Future of Medicare Act (CFMA) comprise the legislative framework through which Ontario actively protects insured persons from extra-billing and user charges (EBUC).
The Ontario Health Insurance Plan (OHIP) and all insured services are set out under the HIA and its regulations.
Commitment to the Future of Medicare Act (CFMA):
The CFMA prohibits any person or entity from charging unauthorized payments for all or part of an OHIP-insured service rendered to an insured person. Such charges include extra-billing (i.e. charges to insured persons for insured physician and dental-surgical services) and user charges (i.e. charges to insured persons for non-physician/dental surgical services provided in conjunction with insured services at a hospital).
The CFMA also prohibits providers and other entities from providing preferred access to an insured service conditional on the payment of a fee, which is called queue-jumping, and from making the provision of an insured service conditional on paying a block fee for uninsured services.
The CFMA applies regardless of the type of facility or setting in which a service is rendered.
Independent Health Facilities Act (IHFA):
The IHFA prohibits any person from charging facility fees except in accordance with the Act. A facility fee is a charge, fee or payment in respect of a service or operating cost that supports, assists and/or is a necessary adjunct to an OHIP-insured service and is not part of the insured service.
Regardless of whether an insured service is provided in a licensed IHF or any other community setting, a charge or payment in respect of a service or operating cost that supports, assists and/or is a necessary adjunct to an insured service, but is not part of the insured service, that is not in compliance with the IHFA is an illegal facility fee.
CFMA program
Through a dedicated program (CFMA Program), the Ontario Ministry of Health (the ministry) reviews all possible cases of EBUC brought to its attention. Charging facility fees contrary to the IHFA may also have implications under the CFMA, and therefore, the ministry's CFMA Program also reviews allegations of illegal facility fees under the IHFA in conjunction with the ministry's IHF program. If, as a result of a review, it is determined that a patient has paid an unauthorized payment (i.e. extra-billing) and/or user charge, the ministry ensures that the full amount is reimbursed to the patient.
Abortion services in Ontario
As noted above, the current Ontario legislative framework (HIA, CFMA, and IHFA) protects insured persons from being charged for OHIP-insured services and for the associated overhead/facility fee costs of providing such services.
In Ontario, physician services associated with both surgical and medical abortions are insured under OHIP regardless of the setting where the services are provided. The "overhead" or "facility" costs associated with medical abortions are included in the fee paid by OHIP for the insured physician service, and Mifegymiso, the drug used in the performance of medical abortions, is also publicly funded. The overhead/facility costs associated with performing surgical abortions in hospitals are insured hospital services funded through a hospital's global budget.
The ministry also licenses and funds four non-hospital clinics for the overhead/facility costs associated with surgical abortion services under the IHFA. There are other non-hospital surgical abortion clinics operating in Ontario that are not licensed and funded for overhead/facility costs under the IHFA. These clinics do not receive any funding from the ministry for the facility fee (overhead) component of the service.
Under provincial legislation, patients cannot be charged for insured physician services or insured hospital services (CFMA) or for the cost of premises, equipment, supplies or personnel used to perform insured services (IHFA), regardless of the setting in which the services are received (e.g., non-hospital clinic licensed under the IHFA, nonhospital/non-IHFA-licensed clinic).
Additionally, the ministry promptly reviews all potential contraventions of the HIA, CFMA and IHFA that come to its attention. This is important to ensure that all patients are not charged for insured health care services.
Issue
Health Canada has expressed concerns that some non-hospital surgical abortion clinics in Ontario may be charging patients mandatory fees ("clinic" or "block" fees) in order to access insured surgical abortion services contrary to the CHA.
Health Canada's specific concerns are based, in part, on inquiries conducted by Health Canada staff members posing as patients who were told by clinic staff that they would be required to pay a mandatory fee ("clinic" or "block" fee) in order to access insured surgical abortion services or where clinic websites were not clear with respect to fees.
Additionally, Health Canada made a deduction to Ontario's March 2021 Canada Health Transfer (CHT) in the amount of $13,905 to reflect user charges found at one nonhospital surgical abortion clinic, as reported on Ontario's FY 2018-2019 EBUC report.
To address the concerns raised by Health Canada with respect to abortion services dating back several years, Ontario has conducted CFMA reviews into several private abortion clinics to ensure that their fee policies are in compliance with Ontario legislation.
Investigation
Ontario has taken extensive efforts to address Health Canada's concerns with respect to insured abortion services in Ontario.
Since 2017, the ministry has undertaken 9 proactive reviews of five private surgical abortion clinics in Ontario, four of which were initiated in response to concerns raised by Health Canada.
Based on the reviews undertaken, with the exception of one clinic, the ministry identified no instances of EBUC.
Additionally, the ministry has received very few complaints directly from patients who have been charged in association with insured surgical abortion services in Ontario. In addition to the proactive investigations noted above, since 2003, the ministry has undertaken only five other investigations associated with specific patient complaints related to charges by community-based abortion clinics. In all cases, no cases of EBUC were identified. As a result of Health Canada's concerns, the ministry promptly opened new reviews under the CFMA into two of the three clinics in question. The ministry had already recently concluded a review of the third clinic.
| The timeline of the investigations | Clinic A
2018-2019 |
Clinic B
2019-2020 |
Clinic C
2019-2020 |
|---|---|---|---|
| Describe the investigation process for each clinic, including details regarding: | |||
| The nature of the clinic-level service data requested by ON and provided by each clinic | OHIP claims data | 60 medical records and all patient materials provided by clinic | 60 medical records and all patient materials provided by clinic |
| When the services described by this data were provided to patients | April 2018 - March 2019 | October 2017 - October 2019 | October 2017 - October 2019 |
| The methodology used to analyze that data | Average of illegal facility fees charged to patients ($4) by the # of abortions performed | Reviewed patient records (60) and all patient materials (website, posted, provided) | Reviewed patient records (60) and all patient materials (website, posted, provided) |
| Summarize the findings of the investigations: | |||
| What was the nature of the fees charged by each clinic? | $40-$50 facility fee for piece of equipment used in association with surgical abortion | Of the 60 patients for whom records were requested, 9 patients receiving insured surgical abortions did not pay a clinic fee | Of the 60 patients for whom records were requested, 10 patients paid no fees and 1 patient declined to pay a block fee for uninsured services and instead paid only a "dispensing fee" for medications |
| How many patients were charged, and what proportion of patients at each clinic paid fees? | 296 | See above | See above |
| Extra-billing and User Charges | Ontario reported a net amount of $13,905 for user charges on its FY2018-2019 EBUC report | No evidence of extra-billing and user charges | No evidence of extra-billing and user charges |
| Patient information | n/a | The ministry requested their list of fees for uninsured services, other information made available to ensure that patients understand that they can access insured abortion services without charge. | The ministry requested revision of list of fees for uninsured services, the information provided to patients after booking, any other information made available to ensure that patients understand that they can access insured abortion services without charge. |
| Summary | The ministry has since received confirmation from the clinic that they have ceased charging patients for equipment. Additionally, the clinic is no longer providing surgical abortion services. | The ministry has since received confirmation from the clinic that they have updated patient information as requested. | The ministry has since received confirmation from the clinic that they have updated patient information as requested. |
Corrective action taken
Remodeling abortion care in Ontario
Ontario is committed to revisiting the current framework for the funding of insured surgical abortion services in Ontario. The changing landscape and complexity of the current funding model for abortion services in Ontario provides an opportunity to consider options to enhance provision of care across different health service delivery settings for abortion services beyond those currently funded by the ministry.
An appropriate assessment of service delivery options, with an eye to funding all surgical abortion service providers/facilities, would need to be taken with consideration of the potential impact to patients, currently funded service providers, as well as the special nature of abortion services.
Ontario has specific legislation to ensure safe access to abortion care, the Safe Access to Abortion Services Act, 2017. This legislation protects the safety, security, health and privacy of patients and abortion service providers in their health service delivery settings and homes.
Any updates to the funding of abortion services in Ontario would need to carefully consider the safe access zones and the unique nature of abortion services.
Conclusion
Ontario trusts that Health Canada will accept the significant efforts being made by Ontario to ensure that the abortion landscape in Ontario protects patients from facing barriers in accessing insured abortion services and that these efforts will be recognized by Health Canada by way of a reimbursement of the March 2021 CHT deduction.
February 2025 status report, implementation of Ontario's Reimbursement Action Plan
Last year's Reimbursement Action Plan update included mention of the Integrated Community Health Services Centre Act, which was introduced to address wait times for essential health services, enhance guardrails to integrate community surgical and diagnostic centres into the health system, and enhance quality standards and oversight while protecting the stability of doctors, nurses and other health-care workers in public hospitals and other health-care settings.
This work has progressed, increasing access and reducing wait times for needed surgical and diagnostic services. Addressing wait times was, and continues to be a top priority, and Ontario is doing this while protecting access to these insured services.
Once this work is completed, Ontario will be better positioned to turn its attention to addressing the structural funding concerns brought forward by Health Canada at private abortion clinics specifically. At that time, a thorough assessment of service delivery options needs to occur in order to adequately consider the special nature of abortion services, the potential impact to service providers, and, most importantly, the potential impact to patients.
While you are already aware that through its reviews under the Commitment to the Future of Medicare Act, Ontario has educated private abortion clinics and directed them to amend their patient-facing materials and websites to clearly state that patients are able to access Ontario Health Insurance Plan (OHIP)-insured abortion services at the clinic at no cost, and that opting out of a block fee does not prevent patients from accessing these services. I am happy to report that currently, all four private abortion clinics in Ontario clearly state on their websites that patients are able to access OHIP-insured abortion services at their clinic at no cost. Further, three of those clinics clearly state that opting out of a block fee does not prevent patients from accessing these services.
While this is an interim step towards addressing Health Canada's concerns, please rest assured that Ontario remains committed to specifically addressing the structural funding concerns and will continue to provide updates to Health Canada as this work progresses.
[Following is the text of the Manitoba Reimbursement Action Plan to eliminate patient charges for medically necessary diagnostic scans and February 2025 Status Update ]
Manitoba Diagnostic Services Policy Reimbursement Action Plan
This document summarises efforts by Manitoba to eliminate patient charges for medically necessary diagnostic services.
Background
- In Manitoba, one private clinic (the Prota Clinic) was charging patients for medically necessary ultrasound and echocardiogram services.
Investigation and reporting
- The Manitoba Health, Seniors and Long-term Care (MHSLTC) learned of one medically necessary diagnostic service charge by a private clinic during the 2021-2022 reporting period. MHSLTC learned of the event after receiving a call to its billing inquiry line from a patient who was charged for the service.
- As a result, Manitoba reported $650 in user charges levied in respect of accessing medically necessary diagnostic services to Health Canada for the reporting period. The cost of the service was obtained by MHSLTC from the patient and verified by contacting the Prota Clinic.
Corrective action taken and monitoring compliance
- MHSLTC sent a formal letter on July 14, 2023, instructing the Prota Clinic to stop charging patients for medically necessary ultrasound services. Since issuing the letter, MHSLTC has not identified any additional patients charged by the clinic. MHSLTC does not have a contract with Prota Clinic to provide services, however the Clinic is an approved facility by MHSLTC to provide x-ray services.
- In the event that a Manitoba resident feels that they have been inappropriately charged for a service that is insured under the provincial health insurance plan (i.e., a potential incidence of extra-billing or a user charge), or of a report or allegation of extra-billing or user charges, the department will investigate the complaint, report or allegation appropriately. Residents may contact MHSLTC to report such occurrences through any of the contact coordinates listed on our website, including our Audit and Investigation Fraud Line.
- The Insured Benefits Branch of MHSLTC examines the specifics of any fee charged to assess whether the service provided was an insured service.
- Generally, in the event that there has been a fee charged that could be considered an instance of extra-billing or a user charge, MHSLTC contacts the medical service provider advising that the provider must reimburse the patient and submit a claim to MHSLTC. This is sufficient to address the concern. Further incidents on the part of the same service provider could result in an investigation by MHSLTC's Audit and Investigation Unit.
February 2025 status update, implementation of Manitoba's Reimbursement Action Plan
This document summarises efforts by Manitoba to eliminate patient charges for medically necessary diagnostic services.
Background
- The Insured Benefits Branch of the Department of Manitoba Health, Seniors and Long-Term Care (MHSLTC) addresses concerns from the public in the event they have been charged for a medical service that they feel should have been an insured benefit not paid for out-of-pocket.
- In the 2022-23 fiscal year, MHSLTC did not receive any complaints or concerns from the public regarding extra-billing or user charges.
Investigation and reporting
- If a Manitoba resident feels that they have been inappropriately charged for a service that is insured under the provincial health insurance plan (i.e., a potential incidence of extra-billing or a user charge), or of a report or allegation of extra-billing or user charges, the department will investigate the complaint, report or allegation appropriately.
- Residents may contact MHSLTC to report such occurrences through any of the contact coordinates listed on our website, including our Audit and Investigation Fraud Line.
- Under Section 2 of the Claims Information Regulation, made under the Health Services Insurance Act (HSIA), the Minister of Health can request the billing and financial records of a practitioner that has made a claim for payment of services provided to insured persons.
- A practitioner has 60 days to comply with the request form the Minister of Health.
Corrective taken and monitoring compliance
- The Insured Benefits Branch of MHSLTC examines the specifics of any fee charged to assess whether the service provided was an insured service.
- If it is determined that there has been a fee charged that could be considered an instance of extra-billing or a user charge, MHSLTC contacts the medical service provider advising that the provider must reimburse the patient and submit a claim to MHSLTC. This is sufficient to address the concern. Further incidents on the part of the same service provider could result in an investigation by MHSLTC's Audit and Investigation Unit.
[Following is a description of Alberta's Reimbursement Action Plan to eliminate patient charges for medically necessary diagnostic scans, which was communicated in a January 11, 2024 exchange between officials, and February 2025 Status Update ]
Alberta Reimbursement Action Plan to eliminate patient charges for medically necessary diagnostic scans
In general, Alberta Health uses a proactive, risk-based planning process to identify potential areas of inappropriate billing under the Alberta Health Care Insurance Act. This process includes provisions to address non-compliance with respect to extra-billing and prohibited fees by any person. Should an Albertan suspect inappropriate billing has occurred, they are invited to submit a complaint to Alberta Health; all complaints regarding suspicious behaviour for inappropriate billing are investigated. For the 2021-2022 fiscal year, no substantiated cases of extra-billing were identified through inquiries made by Albertans nor through Statements of Benefits Paid.
Regarding Alberta's 2023 Canada Health Transfer deduction related to the Diagnostic Services Policy, Alberta Health has developed a plan to ensure compliance with the Canada Health Act, and we are working to address the issue of patient charges for medically necessary diagnostic imaging. To this end, Alberta Health has completed a legislative gap analysis and is developing policy options to address this issue.
In Alberta, diagnostic imaging services such as CT, MRI and PET scans, are publicly funded through Alberta Health Services (AHS). These services are not identified as "insured services" in Alberta's Schedule of Medical Benefits, which lists the medical services that Alberta considers "insured health services" for the purposes of the Canada Health Act. Although diagnostic imaging services may not strictly be identified by Alberta as "insured health services", they are still publicly funded and meet the overarching goal of the Canada Health Act, which requires that medically necessary diagnostic imaging be funded through provincial and territorial health insurance plans.
Further, AHS provides diagnostic imaging services within facilities owned and operated by AHS, as well as through contracts with community-based private diagnostic imaging facilities. Diagnostic imaging services provided in AHS facilities are publicly funded, and there is no charge to a patient to receive these services. Albertans may also receive publicly funded diagnostic imaging services in a community setting outside of an AHS facility by using an AHS-contracted private diagnostic imaging provider. Again, there is no charge to a patient when receiving diagnostic imaging services in an AHS-contracted facility. Albertans with a physician referral who choose privately purchased diagnostic imaging services over publicly funded diagnostic imaging services can also apply to AHS to be reimbursed for the cost if medical urgency is demonstrated.
As noted in previous correspondence, AHS has a reimbursement policy for patients who have paid privately for diagnostic imaging in instances where the public sector may not be able to provide the same service in a clinically appropriate timeframe. Once AHS receives a reimbursement claim with supporting documentation, it makes a reimbursement decision based on:
- The clinical need for the scan, as identified by the referring physician;
- The original scan request being submitted to AHS;
- The requested scan being prioritized based on AHS diagnostic imaging prioritization and indication guidelines; and
- The scan not being scheduled in an appropriate timeframe, based on documented clinical presentation and urgency, despite documented efforts made to expedite the request with AHS by the referring physician.
To address wait times for diagnostic imaging, additional public funding has been included in the last few budgets. Budget 2023 provided a $12 million funding increase so that AHS can perform 41,000 more CT scans, for an annual total of 540,000, and 12,000 more MRI scans, for an annual total of 255,000.
Alberta's government has also allocated funding for diagnostic imaging under the Shared Health Priorities Bilateral Funding Agreement. This funding will increase the number of publicly funded scans at community-based diagnostic imaging facilities to reduce wait times and ensure access to publicly funded scans for all Albertans. Over three years, this funding will lead to approximately 100,000 additional advanced diagnostic imaging scans.
February 2025 status report, implementation of Alberta's Reimbursement Action Plan
Should any person suspect inappropriate billing has occurred they are invited to submit a complaint to Alberta Health through a public-facing email (mibranch@gov.ab.ca). Complaints regarding suspicious behaviour for inappropriate billing are investigated and evaluated for non-compliance with the Alberta Health Care Insurance Act, including extra-billing and user charges prohibitions. For the 2022-2023 fiscal year, there was one case of extra-billing identified through a complaint made by an Albertan, for which they were reimbursed by the physician following an inquiry made by Alberta Health.
Alberta Health has made significant strides to advance its Reimbursement Action Plan by increasing access to publicly funded diagnostic services and additional investments above the annual budget allocation. Beyond the $45 million of federal funding under the Canada-Alberta Agreement to Work Together to Improve Health Care for Canadians and increase capacity to conduct MRI and CT scans, Alberta Health has initiated an additional $13.8 million innovation grant to Alberta Health Services to equip eligible MRIs with artificial intelligence, increasing the efficiency of those machines by reducing the time it takes to complete a scan, and conducting more scans as a result. Alberta Health will continue exploring options to replace outdated equipment, improve intake and scheduling processes, and create electronic order entry systems to streamline referrals and wait times.
Alberta Health also continues to make access to publicly funded healthcare a priority by addressing issues identified by Health Canada while assessing changes that may be required to support Canada Health Act compliance. Alberta Health is exploring options to continue enabling access to medically necessary diagnostic imaging services while implementing the new provincial healthcare provision strategy.
Alberta Health remains committed to ensuring universal access to medically necessary services, including ongoing audits of clinics offering annual memberships for access to uninsured services. The purpose of these audits is to examine service provision, confirm compliance with the Alberta Health Care Insurance Act and Canada Health Act (CHA) and consider future policy changes.
Alberta Health has conducted a jurisdictional scan, policy reviews, legislative reviews, and is currently analyzing options to address extra-billing and user charges monitoring to support CHA compliance.
[Following is the text of the British Columbia Extra-Billing Elimination Action Plan and January 2025 status update]
British Columbia's Extra-billing Elimination Action Plan
This report outlines British Columbia's (BC) Action Plan to address extra-billing. Central to the plan is the implementation of Bill 92, the amendment to the BC Medicare Protection Act (Appendix A), which strengthens the province's legislative provisions against extra-billing.
Background
The Canada Health Act requires the Federal Government to impose financial penalties on provinces where extra-billing has occurred. As a result, BC has been subject to reductions in the amount it receives under the Canada Health Transfer. Previous federal deductions reported by BC to Health Canada have been approximately $200,000 per year. In 2017-2018, the Ministry of Health (MoH) audited three private clinics. Based on the audits, Health Canada estimated that extra-billing in BC for the 2015-2016 fiscal year was $15.9 million and as a result, BC's federal health funding was reduced by that amount.
In the spring of 2018, BC's Minister of Health announced, in part to bring BC in compliance with the Canada Health Act, that the Government would bring into force the remaining provisions of the 2003 Bill 92 to address the province's ability to respond to and address extra-billing. Most of these provisions came into force on October 1, 2018. The key changes include:
- New offence provisions for practitioners and/or clinics related to contravention of the extra-billing provisions in the Medicare Protection Act (Act), including fines of up to $10,000 for a first offence and up to $20,000 for a second or subsequent offence; (s. 46(5.1) and (5.2))
- The ability for the Medical Services Commission to cancel the enrolment of a practitioner for "cause", if the practitioner: (a) contravenes; (b) attempts to contravene; or (c) authorizes, assists or allows someone else to contravene, the extra-billing provisions in the Act; (s. 15)
- A beneficiary (or the person who pays for the service) is entitled to a refund for an amount that is paid contrary to the extra-billing provisions contained in the Act; (s. 20)
- The Medical Services Commission may pay a beneficiary (or the person who paid for an insured service) in exchange for assigning the claim arising due to extra-billing, and pursue the debt against the person who improperly charged for the service; (s. 21)
- The general limits on extra-billing by enrolled practitioners have been clarified; (s. 17) and
- There is an increase in the scope of the limits on extra-billing by non-enrolled medical practitioners. (s. 18)
In addition to the above changes, Bill 92 includes a prohibition for charging in relation to diagnostic services (s. 18.1). This provision is scheduled to take effect on April 1, 2019.
Bringing into force these provisions serves to strengthen enforcement against extra-billing and reinforces the province's commitment to universal public health care.
The enforceability of the Bill 92 provisions has been challenged in Court in Cambie Surgeries Corporate v. British Columbia (Attorney General). On November 23, 2018, the BC Supreme Court issued an injunction enjoining the enforcement of the extra-billing provisions in the Act until June 1, 2019 or further order of the Court (the Court Order). BC is appealing this decision.
Since BC's announcement to bring into force Bill 92, a number of steps have been taken. The following provides a summary of the province's approach to implementation.
Physician/clinic notification
A letter serving notice of the changes was issued to all registered medical practitioners, accredited diagnostic facilities and private surgical clinics on September 10, 2018 (Appendix B). These letters were sent via registered mail to ensure there is a record of them being delivered.
Sections of the BC government website aimed at medical practitioners – Practitioner-Specific Information – have been updated to articulate the changes that have been made. This includes an FAQ document for practitioners, as well as contact information for further questions (Appendix C).
Partners/Stakeholders
Briefings were conducted prior to October 1, 2018, with various associations including: Doctors of BC, the BC College of Physicians and Surgeons, the Canadian Medical Protective Association and the Vice Presidents of Medicine for the Health Authorities, to ensure awareness around the legislative changes and new expectations.
Public awareness
On April 4, 2018, the MoH issued a press release announcing the province would be bringing into force the remaining provisions of Bill 92, effective October 1, 2018. An additional press release was issued on September 7, 2018, providing an overall update on Bill 92 and reporting a six-month extension to April 1, 2019 of the Medicare Protection Act measures applicable to diagnostic services.
A number of relevant sections of the BC government website aimed at the public have been updated to prominently feature alerts that will link patients directly, through multiple paths, to information concerning extra-billing. These include:
- On the BC government's Health homepage, the language under Popular Topics has been amended to indicate that extra-billing information is available under the MSP for BC Residents webpage. This page has an alert button that takes patients directly to information about extra-billing.
- Additional links to extra-billing information can be accessed from the homepage, under Health Care Complaints, and under Medical Services Plan.
Applicable patient information on the changes to the Medicare Protection Act and the ability to seek reimbursement from the Medical Services Commission is profiled at Additional Fees and Charges. Updates also include an FAQ document for patients, as well as contact information for further questions (Appendix D).
The MoH will monitor ongoing patient inquiries and consider additional formats to make information available to the public, as required.
Health authority contracts
Currently, there are ten contracts between Health Authorities and private clinics for surgical services. The MoH issued a letter on September 13, 2018 notifying all Health Authorities of expectations about contracting between Health Authorities and private clinics for the provision of medical services (Appendix E). This included a requirement for all Health Authorities to amend their current surgical services contracts with private clinics to include termination provisions in the event of extra-billing. As a requirement of the amended contracts, medical practitioners and clinics have been required to sign compliance statements (Appendix F). This letter of expectations was revised following the Court Order (Appendix G), as was the compliance statement – which is now referred to as a "notice to physician" (Appendix H).
Medical Services Commission – Compliance and monitoring
The MoH has developed a series of operational processes to protect patients from extra-billing. However, due to the recent Court Order, the Ministry is not able to implement these processes at this time. These processes include: processing complaints, investigating allegations and making a determination as to whether extra-billing has taken place. Once the Ministry is able to move forward, these processes will enable the Medical Services Commission to reimburse beneficiaries directly, assume debt on behalf of a beneficiary and recover the charge from the practitioner and/or clinic. In addition, once enforcement is not prohibited by the Court Order, extra-billing offences may be referred to the MoH's Audit and Investigations Branch and the Special Investigations Unit for the purpose of recommending charges and penalties, where appropriate. As noted above, the Ministry is appealing the recent Court Order and will be seeking for the injunction to be overturned.
Diagnostic imaging and laboratory services
On August 8, 2018, the Honourable Ginette Petitpas Taylor, Minister of Health Canada, wrote to BC Minister of Health, Adrian Dix, regarding the Federal Government's Diagnostic Services Policy. In the letter, Minister Petitpas Taylor stated:
"I fully appreciate that it may take time in some jurisdictions to align provincial and territorial systems with the Diagnostic Services Policy. As I indicated in Winnipeg, the policy will not take effect until April 1, 2020, and reporting on any patient charges for diagnostic services will begin in December 2022 (for the fiscal year 2020-2021.) That would mean, in accordance with the Canada Health Act, that any Canada Health transfer deductions would only be made in March 2023. If in the interim, a jurisdiction has eliminated patient charges for diagnostic services, that jurisdiction would be eligible for reimbursement of deducted funds through the new Reimbursement Policy."
Further, on September 20, 2018, Deputy Minister of Health Canada, Simon Kennedy emailed all of the provinces and territories on the issue of the diagnostic services. In his email, it stated:
"You will note the Minister has indicated that the Diagnostic Services Policy will take full effect from April 1, 2020. This policy is a clarification of the application of the CHA to diagnostic services. It confirms the federal position that medically necessary diagnostic services are insured services, regardless of the venue where the services are delivered. This means that provinces and territories not currently reporting to Health Canada on patient charges in respect of medically necessary diagnostic services will be required to do so as of December 2022 (for the fiscal year 2020-2021). This extended phase-in period is to allow any jurisdiction where patient charges for diagnostic services are permitted to make the changes necessary to align with the Policy. Naturally, moving earlier than 2020-2021 to eliminate such charges is strongly encouraged."
BC is committed to addressing patient charges for diagnostic services. To that end, in March 2018, the BC Surgical and Diagnostic Imaging Strategy was announced which seeks to provide faster access and to reduce wait times for all medical imaging modalities within the province. The priority focus for 2018-2019 was providing faster access to magnetic resonance imaging (MRI), which included by performing 37,000 more MRI exams by the end of March 2019, establishing a centralized intake and pooled referrals approach (where appropriate) and to reduce wait times for high priority patients. To support these initiatives, $11 million in additional funding was made available to the Health Authorities.
- MRI Volumes
- In 2018-2019, the target number of publicly-funded MRI exams performed is 225,000.
- This is approximately 35,000 more MRI exams performed than in 2017-2018.
- Year-to-Date (Period 6, up to September 20, 2018), BC has performed 103,683 MRI publicly-funded MRI exams, which is:
- 971 above the 2018-2019 YTD Period 6 target; and
- 25,607 more MRI exams performed compared to 2017-2018 YTD Period 6.
- MRI Inventory
- There are 31 MRI units in the province operating over 800 hours per week.
- There is an expected deployment of 9 net new MRI units over the next two years. There may be more net new MRI units as further business cases are approved by the Ministry.
- The 9 net new MRI units include 2 private MRI clinics that were recently purchased by Fraser Health Authority and the new clinics will start seeing patients in early 2019.
- There are no active contracts between Health Authorities and private clinics to perform MRI exams, but there are 7 contracts that are ready for demand if needed.
- HHR Recruitment and Retention
- All Health Authorities, except Northern Health Authority, were able to recruit more MRI technologists to meet their needs. This includes the addition of 17 MRI technologists in the Lower Mainland.
- The Northern Health Authority has had issues with recruiting and retaining MRI technologists. To secure MRI technologists coverage, they are contracting with an out-of-province agency for locums, aggressively recruiting for full-time FTEs (three positions currently posted), and investigating other options to overcome the shortage, such as working with other Health Authorities to share resources.
BC believes the above steps will address the demand for medically necessary MRIs in the province. In addition, as of April 1, 2019, BC will bring into effect Section 18.1 of the Medicare Protection Act, which will make it illegal for a medical practitioner to charge for diagnostic imaging. This will deter the private delivery of the service and provide greater protection to patients being charged for medically necessary diagnostic services.
With regard to the Laboratory Services Act, the Ministry plans to bring forward in the fall/winter of 2019-2020 a proposed series of consequential amendments for Cabinet to consider. These changes are not anticipated to be material in nature; rather, they are to ensure elements in the Laboratory Services Act are consistent with the updated Medicare Protection Act.
Audits of private clinics
The MoH has completed three audits of private clinics – False Creek Healthcare Centre, Seafield Surgical Centre, and Okanagan Health Surgical Centre. The results of these audits were shared with Health Canada in accordance with the agreement signed by our respective ministers in 2017.
The MoH has established an audit unit that is responsible for the ongoing audit of existing private surgical centers, and in the 2018-2019 fiscal year is aiming to complete a further three audits, subject to impediments due to the Court Order, bringing the total completed and underway to ten, including Cambie. The clinics are selected on a risk-based approach, taking into account factors such as complaints made by patients, types of services offered, number of physicians providing services and evidence from clinics' websites that they extra bill.
The purpose of the audits is two-fold:
- To monitor and assess compliance with the Medicare Protection Act, and
- To help determine an accurate estimate of the extent of extra-billing in the province.
Subject to clarification from the Court, the MoH is committed to full transparency and will continue to work with Health Canada in reviewing audit findings as the work is completed. Going forward, it is suggested that the monthly conference calls to discuss audit findings are re-established.
Reporting requirements
BC commits to submitting a complete and accurate 2016-2017 extra-billing and user charges financial statement to Health Canada in December 2018, per the reporting requirements set out in the Canada Health Act and Regulations.
As per the Reimbursement Policy, BC also commits to submitting a January 2019 report to Health Canada, assessing the degree to which the elements of the Action Plan have been completed. This report will include:
- A financial statement of any EBUC levied in BC since the March 2018 deduction;
- A report on the steps BC has taken to eliminate EBUC, and how these charges have been addressed; and
- An attestation as to the completeness and accuracy of the information submitted.
Conclusion
In summary, BC's MoH is appealing the Court Order to be able to use the Bill 92 provisions, and, if successful, will monitor and assess the impact of the implementation of Bill 92. BC's MoH will also determine whether further changes to policy and/or legislation are warranted to address extra-billing. By moving forward with the above noted actions, BC believes it has taken the necessary steps to address extra-billing within the province and is seeking reimbursement from Health Canada for the 2018-2019 $15.9 million penalty.
January 2025 status report, implementation of British Columbia's Extra-billing Elimination Action Plan
Pursuant to sections 18 and 19 of the Canada Health Act (CHA), we submit the January 2025 status update to British Columbia's extra-billing Reimbursement Action Plan.
This status update demonstrates B.C.'s ongoing commitment to upholding the principles of the CHA under challenging circumstances. This report is submitted with the reiterated expectation that steps are taken under the federal Reimbursement Policy to reimburse B.C. for all extra-billing penalties levied to date, including any penalty that may arise from the filing related to practices in effect in 2022-2023.
In September 2020, the Province saw a successful outcome in the landmark Cambie Surgeries Corporation (Cambie) litigation.
The appeal was heard in June 2021, with a decision rendered by the BC Court of Appeal, on July 15, 2022, which upheld that of the BC Supreme Court in favour of the province.
On April 6, 2023, the Supreme Court of Canada denied Cambie's application for leave to appeal, bringing this ongoing proceeding to a successful conclusion.
This successful outcome, through two levels of provincial court and the Supreme Court of Canada, highlights the considerable effort and resources that B.C. has contributed to uphold the values of our publicly funded healthcare system.
It is important to emphasize that during the 2022-2023 reporting year, the province took all actions reasonably within its power to enforce the provisions of the Medicare Protection Act (MPA) and uphold the principles of the CHA.
Background
In October 2018, B.C. brought the remaining provisions of the Medicare Protection Amendment Act Bill 92 (2003) into force to address the province's ability to respond to extra-billing and to bring B.C. into compliance with the CHA.
The key changes to the MPA resulting from Bill 92 include:
- Offence provisions for practitioners and/or clinics who contravene extra-billing; fines of up to $10,000 for a first offence and up to $20,000 for a second or subsequent offence*;
- Ability for the Medical Services Commission (the Commission) to cancel the enrolment of a practitioner in the Medical Services Plan (MSP) for "cause";
- Entitlement to a refund for a beneficiary (or person who pays for service) for an amount that is paid contrary to the extra-billing provisions contained in the MPA;
- Ability for the Commission to:
- reimburse a beneficiary (or the person who paid for an insured service) in exchange for assigning the claim arising due to extra-billing, and
- pursue the debt against the practitioner who improperly charged for the service*;
- General limits on extra-billing by MSP-enrolled practitioners have been clarified, and
- The increase of the scope of limits on extra-billing by non-MSP enrolled medical
Public awareness
The Ministry has provided patients with a description of benefits and a link to the description of extra-billing at the webpage: www.gov.bc.ca/MSP/BC residents benefits
The Ministry also has a description of extra-billing along with the form for submitting a request for investigation for patients who believe themselves to have been extra billed: www.gov.bc.ca/MSP/BC residents benefits/additional charges
Links to the description of extra-billing and the form are also available with the description(s) of:
- Services Covered by the MSP:
- Services Not Covered by MSP:
British Columbians have the right to expect that they will not be asked by physicians to pay out of pocket for insured services.
The Ministry believes that its communication strategy has been effective in reducing the frequency of these situations and remains committed to working towards their elimination. The Ministry routinely receives tips or information from members so the public who believe a physician, clinic, or company may be extra-billing. The Ministry monitors ongoing patient inquiries and will make additional information available to the public, as required.
Physician/clinic notification
Sections of the B.C. government website aimed at medical practitioners have been updated and added to the Ministry's main landing page. The Ministry believes this will:
- Raise awareness amongst physicians about information being communicated to patients regarding appropriate and inappropriate billing, and
- Allow physicians to better understand patient expectations for appropriate billing.
The MSC has clarified website information regarding physician enrolment status: www.gov.bc.ca/MSP physician enrollment status. This information outlines, for physicians and their patients, the implications of physician de-enrollment from MSP.
Federal Diagnostic Services Policy
On April 1, 2020, the federal Diagnostic Services Policy (DSP) came into effect, clarifying the federal government's position that medically necessary diagnostic services, regardless of the venue in which they are delivered, are considered insured services under the CHA, and must be covered by provincial and territorial health insurance plans.
Medical necessity for diagnostic imaging is determined when a patient receives a referral or requisition from a medical practitioner for the test or procedure.
Medically necessary diagnostic services encompass a range of scanning modalities, including MRI, CT, ultrasounds, and echocardiograms. Accordingly, any patient charges levied for these services must be included in the annual extra-billing and user charges reporting to Health Canada.
B.C. is anticipating a decision to bring section 18.1 of the MPA into force following the recent Provincial Election and swearing in of a new Cabinet, including a new Minister of Health.
Implementation of section 18.1 would expand the current prohibition against approved diagnostic facilities charging for medically necessary diagnostic services, which are considered benefits under the MPA or the Hospital Insurance Act, to include those without MSC approval. This would cause charges to a beneficiary in relation to medically necessary diagnostic services provided at any diagnostic facility in B.C. to be prohibited in almost all cases.
MSC– Compliance and monitoring
On behalf of the Commission, the Ministry processes patient complaints and investigates allegations of extra-billing to determine whether extra-billing has taken place. Where possible, throughout the investigation, the Ministry seeks to resolve the complaint through communication and education with the physician.
In 2022-2023 there were 7 patient complaints where extra-billing was determined to have likely occurred.
The Ministry and the Commission continue to work closely to enforce the MPA and ensure that operational processes designed to protect patients from extra-billing are effective. Examples of the success of this relationship include two injunctions filed in 2022-2023 against private clinics/companies providing patient care in B.C.: TELUS Health and Harrison Healthcare Inc.
In February 2022, the Ministry asked the Commission to review and consider companies' business and service models. This request was in an effort to confirm these entities were not providing priority access to MSP insured services, independent of acuity, because a patient also paid a fee to the organization. This practice would not be consistent with the CHA and/or the MPA.
The Commission is aware of numerous entities that are offering patient care through the delivery of 'bundled services', that is, charging a monthly or annual fee for health services. These fees are often marketed as preventative or supplementary healthcare services (e.g. dieticians, kinesiologists, etc.), however, physician participation in these paid-pay plans has raised concerns for the Commission around expedited access to insured services.
The Commission continues to contact known, and any new entities brought to its attention through referral and investigation. These include corporations, bricks and mortar health care clinics, and independent practitioners. These communications have produced various results – from immediate steps to come into compliance with the MPA, to continued dispute (and communications) regarding the intent of the fees.
On December 1, 2022, the Commission filed a petition in the BC Supreme Court to seek an injunction against TELUS Health, alleging that it was charging for the TELUS Health LifePlus program contrary to the MPA. In April 2023, TELUS Health demonstrated to the satisfaction of the Commission that it would make the necessary changes to the LifePlus program to come into compliance with the MPA.
On February 1, 2023, the Commission filed a petition in the BC Supreme Court to seek an injunction against Harrison Healthcare Inc. and Harrison Healthcare (BC) Inc., alleging that it was charging for services contrary to the MPA. This litigation remained ongoing at the close of 2023, but was successfully brought to a closely shortly thereafter with Harrison Healthcare making the necessary changes to come into compliance with the MPA.
Health Authority (HA) surgical contracts
B.C. has seen success in curbing extra-billing through government contracts with private clinics. B.C. is committed to curbing extra-billing and user charges in the province to enhance publicly funded health care.
In 2022-2023, HAs contracted with 11 facilities to perform surgeries. All private surgical centres that hold contracts with HAs are required to be accredited by the Non-Hospital Medical and Surgical Facilities Accreditation Program (NHMSFAP) of the College of Physicians and Surgeons of B.C. (CPSBC) and must be approved by the Commission to bill MSP for publicly funded surgeries.
The Ministry issued a letter on September 13, 2018, notifying all HAs of expectations ("letter of expectation") regarding contracting between HAs and private clinics for the provision of medical services. This letter of expectation included a requirement for all HAs to amend their current surgical services contracts with private clinics to include termination provisions in the event of extra-billing. As a requirement of the amended contracts, medical practitioners and clinics have been required to sign compliance statements. The compliance statement to physicians requires acknowledgement by physicians of the termination provisions in the contract between the HA and their clinic pertaining to extra-billing. These provisions apply to the physician's service under contract (MSP-insured services) as well as services undertaken by the physician in clinics outside of the contract (the latter would include MSP-insured services provided at the clinic).
Physicians can only provide contracted surgical services once the compliance statement is signed. The letter of expectation and compliance statements were revised following the November 23, 2018, BC Supreme Court injunction prohibiting the enforcement of the extra-billing provisions (s. 17, 18, and 45 of the MPA).
Currently, regional HAs in B.C. monitor the surgical contracts for compliance with all provisions. Since implementation in September 2018, no HA contract with a private surgical clinic has been terminated over performance or compliance issues. The Ministry is confident that the agreements are being followed by the physicians and HAs.
Overall, the Ministry views this current productive dynamic between HAs and clinics (formerly providing private services) as demonstrative of the value of a contractual arrangement to bring private surgical services back into the public system. This approach simultaneously eliminates extra-billing practices and enhances the capacity of the public health system to provide needed patient care. See the section for data on the number of surgeries performed under HA contracts with private clinics.
In 2022-2023, the HAs had contracts to perform surgical procedures with the following:
Fraser Health Authority (FHA)
- New Westminster Surgical Centre
- Valley Surgery Centre
Interior Health Authority (IHA)
- Kamloops Surgical Centre
- Okanagan Health Surgical Centre
Provincial Health Services Authority (PHSA)
- Anesthesia for Dentistry Clinic
Northern Health Authority (NHA)
- Prince George Surgery Centre
Vancouver Island Health Authority (VIHA)
- Seafield Surgical Centre
- View Royal Surgical Centre
Vancouver Coastal Health Authority (VCHA)
- ASC Vancouver Surgical Centre
- Lasik MD Vancouver Hornby
Contracts with the following entities ended in 2022/23:
- ASC Vancouver Surgical Centre (VCHA)
- Prince George Surgery Centre (NHA)
In April 2022, the Province purchased View Royal Surgical Centre and Seafield Surgical Centre.
For fiscal year 2022-2023, B.C. confirms that False Creek Healthcare Centre has entered into contracts with two Has, valued at $4.91 million:
- VCHA, for the period May 1, 2020, to March 31, 2023, for an amount of $2.54 million
- FHA, for the period March 3, 2020, to March 31, 2023, for an amount of $2.37 million.
These contracts are anticipated to eliminate extra- billing at False Creek Healthcare Centre, which has been identified as a significant source of extra-billing in previous years.
The total amount paid by HAs in 2022-2023 to private clinics for acute care services was $23.8 million; 0.18% of the $13.6 billion HAs reported spending in acute care over the same time period.Footnote xviii
B.C. Surgical and diagnostic imaging strategy
On May 7, 2020, the Province announced its commitment to Surgical Renewal, which was a $250 million action plan launched in response to the COVID-19 pandemic. In addition to the initial investment, on September 9, 2020, the Province announced operating funding of up to $1.6 billion and capital funding of $150 million in 2020-2021 to respond to the health-care requirements related to the COVID-19 pandemic response. Of this amount, approximately $187.5 million was allocated to support enhanced surgical capacity, including additional nursing staff and operating room costs.
Outside of the Surgical Renewal investments, Budget 2022 included $303 million in new base budget funding over the next three years to continue the strategy to reduce wait lists for surgery and diagnostic imaging.Footnote xix
In Year 3 of Surgical Renewal, (fiscal year 2022-2023), there were 339,908 scheduled and unscheduled surgeries performed in B.C., amounting to a 3.7 percent increase over 2021-2022 (Year 2 of Surgical Renewal) and a 6.5 percent increase over the pre-pandemic years of 2019-2020.
The key to achieving the mandate above is maximizing surgical capacity. In B.C., as in other provinces, this includes private surgical centres. Contracting with these centres increases publicly funded access for patients whose surgical day procedures can be done safely and efficiently in the community, leaving our hospital capacity for more complex surgeries and procedures. Under contract arrangements with clinics in the province, 13,021 surgeries were performed in 2022-2023; compared to the following:
- 16,777 surgeries in 2021-2022,
- 13,862 surgeries in 2020-2021, and
- 12,336 surgeries in 2019-2020.
This decrease in surgical volumes in 2022-2023 relates to the ending of two contracts and the purchase of two private surgical clinics by HA in B.C.
As an estimate of the impact, we would note that the Ministry has increased HA contracts, or extended additional contracts, to private surgical clinics found previously to be extra-billing.
These contract additions should eliminate an approximate equivalent in private billing. With these contracts, the HAs have moved from short term to multi-year terms of service (while maintaining termination clauses should extra-billing occur). The stability of these contract arrangements will keep former private capacity in the public system in a sustainable manner.
In addition to these steps, B.C. is committed to increasing public system capacity within HAs. This includes opening new operating rooms and extending the operating hours for others in our hospitals.
In 2022-2023, operating rooms ran 26,877Footnote xx more hours compared to 2021-2022, 45,033Footnote xxi more hours compared to 2020-2021, and 31,219Footnote xxii more hours compared to 2019-2020.
The purchase of the View Royal Surgical Centre and the Seafield Surgical Centre resulted in VIHA performing an additional 3,376 surgeries and 2,997 colonoscopies and other GI endoscopies in 2022-2023.
Through the purchase of private clinics and by negotiating contracts with private clinics to provide MSP-insured beneficiary services instead of extra-billing for the same services, B.C. continues to demonstrate its commitment to addressing patient extra-billing, as defined under the CHA.
Gastrointestinal (GI) endoscopy surgical contracting
In 2022-2023, three facilities were contracted by HAs to perform GI endoscopy procedures, including:
- New Westminster Surgical Centre (FHA),
- GI Research Institute (VCHA), and
- View Royal Surgical Centre (VIHA).
Similar to surgical contracts with HAs, all private GI surgical centres that hold contracts with HAs are required to be accredited through the NHMSFAP with the CPSBC and must also be approved by the Commission to bill MSP for publicly funded surgeries.
In 2022-2023, a total of 7,384 colonoscopy and other GI endoscopy procedures were performed in private surgical centres at no cost to patients. In comparison, 10,101 procedures were performed at private clinics in 2021-2022 and 7,672 in 2020-2021. The decrease in volumes in 2022-2023 is related to the purchase of the View Royal Surgical Centre by the Island Health Authority in 2022.
Medical imaging contracts
Medical imaging services can be performed within the medical imaging department of a hospital or at a Community Imaging Clinic (CIC). In order to perform diagnostic imaging services in B.C., a medical imaging facility must be accredited for those specific imaging modalities by the Diagnostic Accreditation Program (DAP) of the CPSBC.
Additionally, all outpatient medical imaging clinics must be approved by the Advisory Committee on Diagnostic Facilities, an advisory committee to the Commission, to provide publicly insured services and bill the MSP for such services. In compliance with provincial legislation, a diagnostic facility approved by the Commission must not charge a beneficiary for a medically necessary insured benefit, such as MRI; only HAs are approved to provide publicly funded MRI exams. The purpose of the legislation is to preserve a publicly managed and fiscally sustainable health care system in B.C. in which access to necessary medical care is based on need and not on an individual's ability to pay.
Since 2020-2021, VCHA and FHA have accessed exams on publicly owned MRI research units to deliver additional exams within their health authority's region. This has enabled the HAs to complete more exams locally on underutilized research units that are publicly owned.
In 2021, VCHA purchased and converted a privately owned MRI clinic in Vancouver to a facility owned and operated by the health authority.
In 2018-2019, FHA purchased two privately owned CICs, located in Surrey and in Abbotsford, with existing MRI units.
To continue to improve access and reduce wait times for patients, provincial health authorities are exploring contracts with CICs for medically necessary MRI and CT exams. A requirement within the contracts will be that there are no extra-billing practices at the facility, in alignment with the MPA and CHA.
Additionally, BC Cancer is contracted with private PET-CT providers, in B.C. and in the United States, to serve cancer patients in a timely manner when waitlists are impacted or when equipment experiences unexpected downtime.
Medical imaging volumes
In 2022-2023, HAs in B.C. conducted 299,061 MRI exams and 923,990 CT exams. This is 46,534 more MRI exams and 118,406 more CT exams compared to pre-pandemic volumes in fiscal year 2019-2020. Despite increased volumes year over year, the backlog of waitlisted patients for imaging services continues to grow with an estimated 84,050 exams waiting for MRI and 102,990 exams waiting for CT as of period 5, 2024-2025.
Imaging equipment
B.C. currently operates 43 MRI units, 73 CT units, and 4 PET-CT units across the province. This is 10.1 MRI and 13.8 CT units per million population in 2022-2023, which is well below the Organisation for Economic Co-operation and Development averages of 19.4 MRI and 29.9 CT units per million population.
To support medical imaging in B.C., the Ministry established a Provincial Medical Imaging Office in the PHSA in early 2024. The key objectives of the provincial office this fiscal year are to model wait time targets by health authority facility for MRI and CT, to improve access and wait times, work with regional health authorities on a capital investment priority framework, digitize the ordering to imaging workflow, and to develop an overarching medical imaging strategy for B.C. to improve access to publicly funded medical imaging services across the province.
The Canada Drug Agency (CDA) tracks medical imaging equipment across Canada and drafted a report on equipment needs to reduce wait times across the country. The report shared with the Ministry, titled 'Optimal units per capita to achieve priority wait times for CT, MRI, and PET-CT', indicated that as of 2022-2023, B.C. would require an additional 50 MRI, 88 CT, and 9 PET-CT units. The CDA estimates that by 2030, and in order to serve the growing and aging population of the province, B.C. will require a total of 116 MRI, 181 CT, and 16 PET-CT units.
Significant investments are needed to address the shortage of imaging equipment as the requirement to replace aging equipment beyond their 15-year lifecycles continues to be considered. An added impact is the need to address shortages of Radiologists and specialized Imaging Technologists (e.g.: Medical Radiation Technologists, MRI Technologists, Sonographers, etc.) to effectively deliver publicly funded medical imaging services with reduced wait times.
MRI at Community Imaging Clinics (CICs)
In late 2023, the Commission advised three privately owned CICs operating MRI units and other imaging modalities that they would no longer be able to bill the MSP for services provided to beneficiaries if they continued to operate private-pay MRI services for medically necessary MRI. Those clinics have all ceased providing privately paid MRI services to beneficiaries.
Private CICs form a vital part of the health system in B.C. and the majority comply with the Medicare Protection Act and Canada Health Act to maintain their good standing with the Commission in order to continue billing the MSP for medically necessary imaging provided to beneficiaries.
Health Human Resources (HHR)
B.C.'s health workforce
- In B.C., Canada, and around the world, health needs are becoming more complex and demand for healthcare services is growing.
- In response to increasing demand, B.C.'s health workforce continues to grow – thanks in part to key investments through B.C.'s Health Human Resources (HHR) Strategy and eight strategic repositioning initiatives:
- Primary Care
- Seniors Care
- Mental Health and Substance Use
- Cancer Care
- Ambulance
- Hospitals
- Surgical
- Diagnostics
- Some highlights of workforce growth in the last year include:
- Over 9,000 nurses newly registered or were reinstated between January and October 2024 and the nursing workforce grew by more than 1,000.
- The physician workforce grew by over 550 (January to September 2024).
- Health authorities hired more than 2,800 registered nurses and registered psychiatric nurses and more than 800 licensed practical nurses through external competitions between January and August 2024.
B.C.'s Health Human Resources (HHR) strategy
- On September 29, 2022, the Ministry released B.C.'s HHR Strategy with nearly $1 billion in new funding over three years to support its implementation.
- The HHR Strategy envisions a health system that puts people first – fostering workplace satisfaction and innovation to ensure health services are accessible to everybody in B.C., now and in the future.
- This vision is advanced through 70 actions organized around four cornerstones: retain, redesign, recruit, and train.
- In Fiscal Year 2024-2025 (April 1, 2024 – March 31, 2025, year two of implementation), HLTH and partners have made major progress across all four cornerstones of the HHR Strategy with 53 of 70 actions complete or underway as of December 31, 2024.
- Some key achievements from Fiscal Year 2024-2025 include:
- Full implementation of the relational security model at 26 sites identified in partnership with the BC Nurses Union and Health Authorities.
- The creation of a new provincial psychological health and safety resource team.
- Expansion of the provincial rural retention incentive for 2024-2025 whereby all regular all regular (not casual) eligible health authority employees in 74 eligible communities receive up to $2,000 per quarter, pro-rated against productive hours (straight time and overtime).
- Preliminary implementation of minimum Nurse to Patient Ratios in B.C.'s hospital settings including funding for nursing incentives, new graduate bursaries, tuition credits, expanded training opportunities, and new staffing lines.
- Continuation and expansion of funding to reduce barriers to practice for internationally educated nurses, occupational therapists, physiotherapists, medical laboratory assistants, and physicians.
- Expansion of the Health Career Access Program (HCAP) into mental health and substance use settings.
- Expansion of bursaries and tuition credits for students enrolled in priority programs and for indigenous students in select healthcare programs.
Laboratory services
Medically required laboratory services are publicly funded under the Laboratory Services Act (LSA). The Minister is responsible for all matters related to laboratory services including the facility approval process, governance, accountability and provision of benefits for all laboratory services in the province. The Agency for Pathology and Laboratory Medicine is now a program under the Provincial Health Services Authority (PHSA). The Agency's mandate is to provide laboratory system oversight and to ensure that clinical laboratory services are sustainable, quality driven, innovative, and support British Columbia's residents and clinicians with access to laboratory services. Since April 1, 2019 PHSA accepted accountability for operational functions assigned by the Ministry to support the LSA.
Ministry of Health service provider – Health insurance BC
In August 2022, Pacific Blue Cross, doing business as PBC Solutions (PBCS) was awarded the contract to provide HIBC Services on behalf of the Ministry. The Ministry has been working closely with PBCS and the incumbent service provider Maximus BC, to ensure a smooth transition of HIBC Services, resources, and technology.
Under the agreement, PBC Solutions will administer the MSP, PharmaCare, and laboratory programs (including responding to public inquiries, registering clients, and processing medical and pharmaceutical claims from health professionals). Policy and decision-making functions will continue to remain with the Ministry.
Audits of private clinics
In 2017, Health Canada and the Ministry agreed upon a methodology to determine the extent and nature of patient extra-billing in B.C., outlined in a Terms of Reference and Letter of Agreement. Since this agreement, the Ministry has completed 12 audits of private surgical clinics, including Cambie Surgeries Corporation. The results of these audits were shared with Health Canada in accordance with the signed agreement.
Since April 2022, for Health Canada reporting period 2020-2021, the Ministry is required to report extra-billing attributed to private diagnostic facilities. A diagnostic audit framework has been developed, pending a decision on the implementation of s. 18.1 of the MPA.
The purpose of these audits is two-fold:
- To monitor and assess compliance with the MPA, and
- To help determine an accurate estimate of the extent of extra-billing in the
The Ministry will provide the final audit reports for individual clinics and/or providers to Health Canada subject to any redactions required to comply with the Freedom of Information and Personal Privacy Act. The Ministry is working through concerns and legalities around posting summarized versions of audit reports online. The Ministry will be adding communication resources for this work and will recruit staff for these positions. Their first order of priority will be to make sure audits are completed and posted in a timely manner.
Subject to clarification from the Court, the Ministry is committed to full transparency and will continue to work with Health Canada in reviewing audit findings as the work is completed.
Monthly meetings with BC staff and Health Canada staff to discuss extra-billing and other pertinent matters including audit findings remain ongoing.
Reporting requirements
B.C. is submitting a complete and accurate 2022-2023 extra-billing and user charges financial statement to Health Canada as per the reporting requirements set out in the CHA and Regulations.
B.C. is reporting a total of $23,537,756 in extra-billing and user charges that occurred in 2022-2023 according to the agreed-on reporting methodology.
Conclusion
In summary, B.C. is continuing to take all actions within its power to strengthen the public health care system, eliminate extra-billing, and ensure full compliance with the CHA. The specific steps and strategies to reach this goal will evolve to address changing circumstances but B.C.'s multi-pronged and robust approach backed by significant resources will stay constant.
Given the successful outcome of the Cambie Surgeries litigation, B.C. will continue to focus on audit and enforcement and deterring extra-billing, as well as ongoing efforts to educate both the public and medical community in the province. We believe this status update demonstrates the robust commitment of our province in upholding the principles of the CHA under challenging circumstances.
By moving forward with the above noted actions, B.C. has taken the necessary steps to address extra-billing within the province and is seeking reimbursement from Health Canada for the 2022-2023 penalty of $23,537,756.10.
It is our expectation that steps be taken under the authority of the federal Reimbursement Policy to reimburse B.C. for all extra-billing penalties levied to date, including any balance of Canada Health Transfer funds eligible for reimbursement previously withheld by the Federal Government and any penalty that may arise from the filing related to practices in effect in 2022-2023.
Statement of attestation
I attest that the above information captures the full extent of the Ministry of Health's efforts to eliminate extra-billing and ensure full compliance with the CHA and its Regulations and applicable provincial/territorial legislation.
Rob Byers
Assistant Deputy Minister and Executive Financial Officer
Ministry of Health British Columbia
Contact information
Contact information is provided below for residents who believe they may have been subject to inappropriate patient charges for insured health services.
Refer to Chapter 1 for key definitions under the Canada Health Act. For detailed information on what health services are insured under provincial or territorial health insurance plans, refer to section 2.0- Comprehensiveness, under each provincial and territorial section.
Newfoundland and Labrador
MCP General Inquiries Line
1-866-449-4459 (Avalon area)
1-800-563-1557 (all other regions)
Prince Edward Island
Prince Edward Island Department of Health and Wellness
P.O. Box 2000
Charlottetown, PEI
C1A 7N8
1-902-368-6414
Nova Scotia
Department of Health and Wellness
P.O. Box 488
Halifax, NS
B3J 2R8
1-902-424-5818
1-800-387-6665 (toll-free in Nova Scotia)
1-800-670-8888 (TTY/TDD)
https://novascotia.ca/dhw/about/contact/#form
New Brunswick
Contact the New Brunswick Department of Health
Quebec
Ontario
Commitment to the Future of Medicare Act Program
1-888-662-6613
protectpublichealthcare@ontario.ca
Manitoba
Manitoba Health, Seniors, and Long-Term Care
300 Carlton Street
Winnipeg, MB
R3B 3M9
1-800-392-1207
Saskatchewan
Saskatchewan Ministry of Health
1-800-667-7766
info@health.gov.sk.ca
Alberta
Alberta Health
Attention: Alberta Health Care Insurance Plan
P.O. Box 1360, Stn Main
Edmonton, AB
T5J 2N3
1-780-427-1432 (Edmonton)
1-310-0000 then 780-427-1432 (toll-free in Alberta)
780-422-0102 (fax)
health.ahcipmail@gov.ab.ca
British Columbia
Yukon
867-667-5111
ymc@yukon.ca
https://www.yukonmedicalcouncil.ca/index.php/public/complaint-process
Northwest Territories
Health Services Administration Office, Health and Social Services
Bag#9
Inuvik, NT
X0E OTO
1-800-661-0830 or1-867-678-8050
1-867-777-3197 (fax)
Nunavut
Nunavut Health Insurance Programs Office
Department of Health
Box 889
Rankin Inlet, NU
X0C 0G0
1-800-661-0833 (toll free)
NHIP@gov.nu.ca
Endnotes
- Footnote 1
-
Correction for 2022-2023: Registered Nurses increased by 177 (from 13,283 to 13,460), not the previously reported increase of 566 (from 13,283 to 13,849).
- Endnote 1
-
https://www.ramq.gouv.qc.ca/en/citizens/health-insurance/medical-services
- Endnote 2
-
This number includes the activities of the Ministries of Health and Long-Term Care. On June 20, 2019, Ontario announced changes to its Cabinet that included the creation of the Ministry of Health and the Ministry of Long-Term Care. As such, the Ministry of Health and Long-Term Care are referred to as the Ministry of Health (MOH) throughout this report.
- Endnote 3
-
https://www.auditor.on.ca/en/content/annualreports/arbyyear/ar2023.html
- Endnote 4
-
https://www.auditor.on.ca/en/content/annualreports/arreports/en23/AR_emergencydepts_en23.pdf
- Endnote 5
-
https://www.auditor.on.ca/en/content/annualreports/arreports/en23/AR_hospitalsnorth_en23.pdf
- Endnote 6
-
https://www.auditor.on.ca/en/content/annualreports/arreports/en23/1-16FU_outpatient_en23.pdf
- Endnote 7
-
https://www.auditor.on.ca/en/content/annualreports/arreports/en23/2-01FU_COVIDmgmtexpenditures_en23.pdf
- Endnote 8
-
Provided by the College of Physicians and Surgeons of Manitoba: number of licensed physicians practicing in Manitoba, aligning with academic graduation period of April 30, 2024.
- Endnote 9
-
See section 2.1 for information on insured drugs, etc., for hospital in-patients and out-patients.
- Endnote 10
-
Contandriopoulos, D, K Bertoni and G.K. Randhawa 2022. Developmental Evaluation of NPPCCs. Interim report - September 2022.
- Endnote 11
-
The report for 2023-2024 can be found here: nthssa_-_annual_report_-_2023-24_-_final_-_web.pdf
- Endnote 12
-
https://www.hss.gov.nt.ca/en/services/medical-travel/medical-travel-policy
- Endnote 13
-
Details on Medical Travel policy can be found here: https://www.hss.gov.nt.ca/en/services/medical-travel/medical-travel-policy
- Endnote 14
-
https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1710000901&request_locale=en
- Endnote 15
-
https://www12.statcan.gc.ca/census-recensement/index-eng.cfm
- Endnote 16
-
Supplementary Appropriation (Operations and Maintenance), No. 1, 2023-2024. om_supp_1_2023-24_-_english.pdf (gov.nu.ca)
- Endnote 17
-
2023–2024 Capital Estimates, Department of Finance. capital_supp_1_-_2023-2024_-_english.pdf (gov.nu.ca)
- Endnote 18
-
2022-2023 audited HA financial statements
- Endnote 19
- Endnote 20
-
Source: AW. Report: Surgical Activity Monitoring by HA - OR Hours - MOH - FY2122 P13 - v01(Urgent 4 Weeks).pdf
- Endnote 21
-
Source: AW. Report: MOH - Total OR Hours by Health Authority and Urgency - 10 - FY1617 to FY2021 - v01.pdf
- Endnote 22
-
Source: AW. Report: Surgical Activity Monitoring by HA - 02ez - OR Hours - MOH - FY2223 P13 - v02 (Urgent 4 Weeks).pdf