Government of Canada Actions on Opioids: 2016 and 2017
Download the alternative format
(PDF - 516 Kb)
Organization: Health Canada
Type: Publication
Published: 2017-11-15
Canada is in the midst of a crisis. In 2016, there were more than 2,800 suspected opioid-related deaths in Canada and preliminary data for 2017 suggest that we will almost certainly surpass 3,000 Canadian lives lost. Governments, non-government organizations, health and public safety professionals, and individual Canadians across the country have been responding to this crisis in an effort to save lives.
The roots of this crisis are complex and no one actor has the power to change the current course of events – we must all work together to do better for Canadians. The Government of Canada is coordinating a whole-of-government approach that is grounded in compassion and evidence. This report provides an overview of the actions taken by the Government of Canada since early 2016 to address the opioid crisis.
Overview of Current Opioid Situation in Canada
Problematic substance use and illegal drugs have long presented health and safety challenges in Canada. Recently, however, there has been a dramatic rise in the number of overdoses and deaths as a result of problematic opioid use. New data, only recently available, is helping to bring the overall picture in Canada into focus. In 2016 there were more than 2,800 suspected opioid-related deaths in Canada and preliminary data for 2017 suggest that we will almost certainly surpass 3,000 Canadian lives lost.
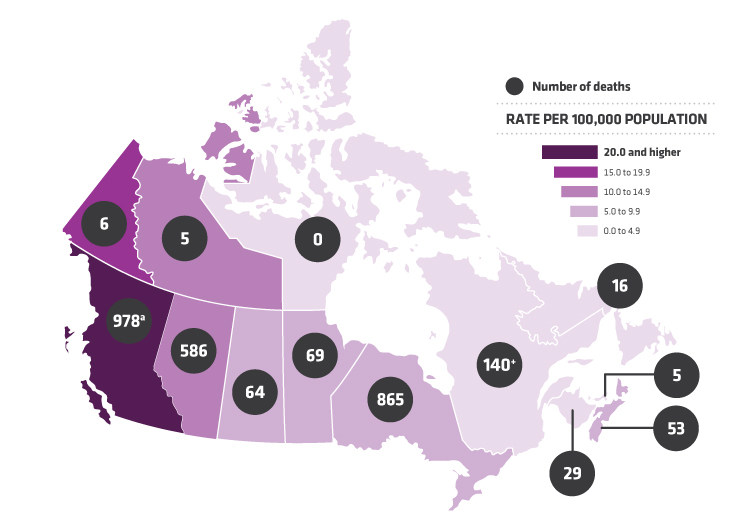
a) British Columbia reports unintentional deaths related to all illicit drugs including, but not limited to, opioids.
+) Expected to rise
Text equivalent
| Provinces and territories | Number | Rate per 100,000 population |
|---|---|---|
| British Columbia (note: reports on unintentional deaths related to all illicit drugs, including but not limited, to opioids) |
978 | 20.0 and up |
| Alberta | 586 | 10.0 to 14.9 |
| Saskatchewan | 64 | 5.0 to 9.9 |
| Manitoba | 69 | 5.0 to 9.9 |
| Ontario | 865 | 5.0 to 9.9 |
| Quebec (expected to rise) |
140 | 0.0 to 4.9 |
| New Brunswick | 29 | 0.0 to 4.9 |
| Nova Scotia | 53 | 5.0 to 9.9 |
| Prince Edward Island | 5 | 0.0 to 4.9 |
| Newfoundland and Labrador | 16 | 0.0 to 4.9 |
| Yukon | 6 | 15.0 to 19.9 |
| Northwest Territories | 5 | 10.0 to 14.9 |
| Nunavut | 0 | 0.0 to 4.9 |
| Total | 2816 | |
a) British Columbia reports unintentional deaths related to all illicit drugs including, but not limited to, opioids. |
||
British Columbia has been at the forefront of this crisis, declaring a public health emergency in April 2016. However, the impact of the crisis is now being felt, to varying degrees, in many communities across the country - from inner cities to suburbs as well as in northern and rural communities and in First Nation communities. Problematic substance use has historically been viewed as a problem for a certain segment of society and has long been stigmatized. But the current opioid crisis has highlighted that problematic substance use is a public health tragedy affecting all socio-economic, gender and age groups. It is affecting elderly people and youth in their prime, as well as adults from all walks of life.
One contributing factor to the current crisis has been the growth in the use of opioids for medical treatment. Beginning in the mid-2000's, rates of prescription high-dose opioid dispensing began to rise significantly in Canada. While the medical needs of patients, including which prescription drugs they should be taking, are best determined by a patient and their physician, we know that opioid pain medications are being overprescribed in Canada. Canadians are the 2nd highest per capita consumers of opioids in the world, after the United States. Those with lived and living experience have reported that prescription opioid use can lead to dependence for some individuals. Some of these people turn to less safe alternatives, including illegal drugs, once prescribed medications are no longer available to them.
Fentanyl, which is fifty to one hundred times more potent than morphine, is a legitimate pharmaceutical used to treat severe pain. However, illegally produced fentanyl and fentanyl analogues, are now being found in Canada. These toxic drugs, many of which are coming from overseas, are making their way to the street in a pure form, pressed into counterfeit drugs or mixed into other illegal drugs, given their comparatively low cost. These drugs have significantly contributed to the overdose epidemic. The number of times fentanyl or an analogue has been identified in samples submitted by law enforcement to Health Canada laboratories has increased by more than 2000% since fentanyl was first encountered in Canada in 2012. From the beginning of 2016 to the beginning of 2017, the number of deaths in Canada involving fentanyl more than doubled.
Tragically, many overdoses and deaths associated with fentanyl are accidental. Many Canadians have unknowingly taken this toxic drug and have then experienced an overdose. And while the proportion of overdose deaths associated with fentanyl continues to grow, Canada is now seeing carfentanil, an even more deadly opioid, enter the illegal drug market.
In 2016, just over half of all overdose deaths in Canada were associated with fentanyl or its analogues.
Harder to measure is the toll this crisis is taking on individuals, and on families and communities who are left behind to carry on, as well as first responders who are working tirelessly to save lives.
Shared Response
No one level of government or single sector can address this complex social, health and safety issue alone. Reversing the trajectory of the current overdose epidemic is a shared responsibility and requires collaborative action by many stakeholder groups and all levels of government across health, public safety, social, legal and economic sectors.
The immediate and personal effects of this crisis are most profoundly felt by individuals, families and communities. Provincial and territorial governments have been actively responding to the needs of their populations. Almost all jurisdictions have their own strategies in place or in development, and have struck committees to manage the situation. Almost all are looking to address prescribing practices in some manner and many have increased access to opioid agonist treatment options, with others examining the issue. Take-home naloxone kits are readily available in most jurisdictions at pharmacies or from health authorities, often free of charge. Links to provincial and territorial web pages with additional information can be found at the end of this report.
Municipalities and local public health officials are also working on solutions that work best for their communities. Health professionals, mental health experts, law enforcement and other stakeholders are contributing to the response on the ground and are continuously looking at what more they can do. Most notably, people who use drugs as well as the families and communities directly impacted by problematic substance use are sharing their powerful messages and lessons they have learned, which is critical to the success of any response to this crisis.
To help catalyze action, a number of organizations joined the Joint Statement of Action to Address the Opioid Crisis which initially included 129 commitments in November 2016, but has since grown to 202, with over 80 organizations signed on. The Canadian Centre on Substance Use and Addiction is tracking progress against these commitments, and has released an annual report which provides an update on these important actions undertaken by non-governmental organizations and stakeholders.
Focussing here on federal actions by no means diminishes the work of others. This report is meant to review actions that the federal government has contributed to the collective opioid crisis response and to look forward to up-coming areas of action.
Federal Response
The Government of Canada is committed to protecting the health and safety of all Canadians through a comprehensive, compassionate, collaborative and evidence-based approach to addressing problematic substance use.
As evidence of the current crisis began to mount, the Government of Canada initiated actions to respond directly to the needs of affected jurisdictions and communities. To guide these actions, the Government reconfirmed the commitment to a comprehensive, whole-of-government approach to problematic substance use. In December 2016, the Government replaced the National Anti-Drug Strategy, which relied heavily on enforcement action, with the Canadian Drugs and Substances Strategy which takes a public health approach to problematic substance use and emphasizes compassion and collaboration between sectors. This new approach recognizes that there are powerful social factors in play that require health and social service responses, alongside ones aimed at reducing the supply of illegal drugs. Reflecting this, the Government of Canada has taken a coordinated approach to address the crisis, with actions and commitments coming from across numerous federal departments and agencies.
Since early 2016, Government of Canada officials have worked to leave no stone unturned in identifying solutions. The result has been actions from numerous departments that have resulted in:
- a change in approach to problematic substance use generally, to provide a greater focus on public health;
- greater coordination among partners, to ensure we have not left gaps and that our initiatives are working together;
- changes in legislation and regulations, to address barriers to services or treatment options and gaps in our enforcement authorities;
- enhanced or targeted compliance and enforcement measures, to address illegal activities with drugs;
- new or refocused programming and increased funding to provide needed services; and,
- collaborative efforts to build a more robust evidence base, to inform actions and identify new trends.
Leadership and Coordination
Changing our Approach
The Government of Canada is committed to taking a new approach to addressing problematic substance use – one that emphasizes compassion and that appropriately balances public health considerations with those of public safety.
This approach was formalized with the announcement of the Canadian Drugs and Substances Strategy (CDSS) in December 2016. This new strategy restores harm reduction as a pillar, alongside prevention, treatment and enforcement, and is supported by a strong foundation of evidence. While efforts to fully elaborate the strategy are ongoing, harm reduction and building the evidence base have formed a significant part of the Government of Canada's response to the crisis, as described in this report.
Harm reduction: measures that reduce the negative effects of drugs and substances on individuals and communities, including stigma.
In the 2017 Budget, the Government of Canada announced an investment of $100 million over five years, and $22.7 million ongoing, to support national measures associated with the CDSS and to respond to the opioid crisis. The Government also provided $10 million in urgent support to the Province of British Columbia and $6 million to the Province of Alberta to assist with their responses to the overwhelming effects of the opioid crises in those jurisdictions. Five million dollars is being given to the Province of Manitoba for targeted health care improvements to respond to critical needs including the opioid crisis.
Leadership
- Announced new Canadian Drugs and Substances Strategy
- $100M/5 years and $22.7M ongoing to address drugs and opioids
Working Together
During a crisis, rapid response is important, but it is also critical to ensure that actions taken by all partners do not inadvertently create new gaps or undermine other actions. The Government of Canada has been working to provide this coordinating function.
In November 2016, the Opioid Conference and Opioid Summit were cohosted by the then Minister of Health, the Honourable Jane Philpott and the Ontario Minister of Health and Long-Term Care, the Honourable Eric Hoskins. The Conference was a national dialogue on actions needed to address and reduce the harms related to opioids in Canada. It involved service providers, stakeholders, non-government organizations, researchers and people with lived and living experiences. The Summit brought together over 30 organizations and nine provincial/territorial ministries of health willing to make a commitment to action, resulting in theJoint Statement of Action to Address the Opioid Crisis.
The current and former federal Ministers of Health have hosted a number of roundtable discussions since July 2017 with people who have been directly impacted by the crisis, including front line workers and people with lived and living experiences to discuss root causes of problematic opioid use, barriers to seeking support, best practices and ways to address stigma.
Two senior-level Federal/Provincial/Territorial (F/P/T) tables have been created and are advancing efforts on the opioid crisis. The F/P/T Special Advisory Committee (SAC) on the Epidemic of Opioid Overdoses was established in December 2016 as a time-limited mechanism to focus on urgent issues related to the crisis. It is also the mechanism that supports the Council of Chief Medical Officers of Health in delivering on its commitments in the Joint Statement of Action. The SAC has been meeting regularly on prevention, treatment and harm reduction efforts across Canada and is focussing on improving opioid data and surveillance to better inform overdose response efforts. The F/P/T Committee on Problematic Substance Use and Harms was established in February 2017 to develop policies and strategies on problematic substance use and associated harms, with an immediate focus on actions to address the opioid crisis.
At the federal level, a Deputy Ministers Task Force, with representation from a broad range of federal departments and agencies, was struck in April 2017 to provide senior oversight and direction for the Government of Canada's response to the opioid crisis.
Working Together
- Opioid Conference and Summit
- Joint Statement of Action to Address the Opioid Crisis
- Roundtable discussions with those directly affected
- Federal/provincial/territorial committees established
- Government of Canada Deputy Ministers Task Force
Beyond Canada's Borders
The opioid crisis is not solely a Canadian issue. The United States (US) is also grappling with high rates of opioid use and overdose deaths. Opioids have been a focus of working level, bilateral cooperation with the US and others and, more officially, are part of the trilateral discussions with the US and Mexico through the recently established North American Dialogue on Drug Policy. The Dialogue is a means to exchange information on drug trends, increase trilateral coordination on drug policy, and develop actions that our governments can take to protect our citizens from harmful drugs and drug trafficking.
Canada is also working closely with China and other international partners to disrupt the export of illegally produced fentanyl. China has recently listed a number of fentanyl analogues as controlled substances under Chinese law and the Royal Canadian Mounted Police (RCMP) and the Chinese Ministry of Public Security are working together to combat the flow of illegal fentanyl and other opioids into Canada. As a result, it is reported that there has been a reduction in the exportation of some fentanyl analogues from China.
Further, the RCMP Federal Policing Program is working in close collaboration with US law enforcement counterparts, particularly the Drug Enforcement Administration and Homeland Security Investigations, to share best practices and lessons learned.
Beyond Canada's Borders
- North American Dialogue on Drug Policy
- Bilateral discussions with US and China
Legislation and Regulation
The Government of Canada has legislative and regulatory tools at our disposal which we have used or amended to respond to the crisis.
Legislative Changes
The Controlled Drugs and Substances Act (CDSA) controls substances that can alter mental processes and may produce harm to health and society. It aims to protect public health and maintain public safety by prohibiting activities with controlled substances unless they are authorized by Health Canada for legitimate medical, scientific or industrial use.
To more effectively and appropriately respond to the opioid crisis, the Government of Canada moved quickly to make changes to the CDSA and other Acts which were adopted by Parliament in May 2017. Many of those changes, described here, came into effect immediately.
Consistent with the Government of Canada's commitment to harm reduction, the legislative changes support the establishment of supervised consumption sites (SCS) by streamlining application requirements to obtain the exemption to the CDSA that is needed to operate a site. This is in recognition of the evidence that shows that, when properly established and maintained, SCS save lives and improve health. Prior to the introduction of the changes, two SCS in Canada were exempted, both in Vancouver. As of November 2017, there are now over 25 approved sites across the country, many of which are now open and providing a place for people to use their drugs under the supervision of trained personnel and offering linkages to other health and social services. This includes approval for the first sites offering oral, intranasal and inhalation services.
To make it more difficult to manufacture illegal drugs in Canada, changes were also made to make it illegal to import unregistered pill presses into Canada, and to possess, transport, import or sell anything intending to be used to traffic or produce any controlled substance without authorization. This is intended to help law enforcement take early action against suspected illegal drug production, including, for example, the production of counterfeit pharmaceutical tablets that contain fentanyl.
Temporary accelerated scheduling is another change made under the CDSA that allows the Minister of Health to quickly control a new and dangerous substance that is not subject to the CDSA. The substance can be quickly scheduled, pending a comprehensive review and decision on permanent scheduling.
To address the issue of fentanyl crossing the border into Canada by way of multiple small packages being sent through international mail, changes were also made to the Customs Act and the Proceeds of Crime (Money Laundering) and Terrorist Financing Act. The amendments allow border officials to open small mail items weighing 30 grams or less, in order to detain or seize illegal substances (such as fentanyl). Now international mail of any weight can be opened, when there are reasonable grounds to suspect the item contains prohibited, controlled or regulated goods.
Parliament also passed the Good Samaritan Drug Overdose Act, a Private Member's Bill, in May 2017. This legislation provides some legal protection for individuals who seek emergency help during an overdose. The goal is to encourage people to make a call to help save a life by reducing the fear of police attending overdose events.

Justice Canada continues to review changes in the criminal justice system and sentencing reforms over the past decade, including working with federal, provincial, and territorial Ministers responsible for justice, and other stakeholders, to explore possible legislative proposals that could enhance judicial discretion and allow courts to impose just sentences that take into account offenders' life circumstances.
Legislative Changes
- Streamlined application requirements for supervised consumption sites
- Require registration to import pill presses
- Ability to quickly control new dangerous substances entering the illegal market
- Allow opening of mail weighing 30g or less if suspected of containing unauthorized controlled substances
- Legal protections for individuals who seek help during an overdose
Regulatory Actions
Regulations under the CDSA and the Food and Drugs Act provide other tools that the Government of Canada has used to address the opioid crisis.
In March 2016, Health Canada made naloxone available without a prescription. Naloxone can be used in emergency situations to temporarily reverse the effects of an opioid overdose, thus preventing deaths. By removing it from the prescription drug list, naloxone kits can now be accessed by health providers, first responders, schools, bars and individuals who feel they may need one. Health Canada also expedited the approval of the easier-to-use nasal spray version of the drug in Canada in October 2016.
A number of recent regulatory actions aim to increase access to treatment options. Following regulatory amendments, as of September 2016, physicians are once again allowed to apply to Health Canada's Special Access Program to request access to medical grade heroin to treat certain patients with chronic relapsing opioid dependence. Further regulations now allow the import of certain listed medications, for urgent public health needs, not yet authorized in Canada, but authorized for sale in the United States, the European Union or Switzerland when certain conditions are met (June 2017). Health Canada has also enlisted the expertise of the Canadian Research Initiative in Substance Misuse (CRISM) to lead a national stakeholder consultation on whether the current exemption requirements for methadone prescribers pose an unnecessary barrier to access to treatment for opioid use disorder (August 2017).
Other regulatory actions are designed to minimize risks associated with opioids. For example, in November 2016, Health Canada made it harder to access six chemicals used to make fentanyl by scheduling them under the CDSA. And in June 2017, the department proposed amendments to the Food and Drug Regulations that would enable the Minister of Health to require pharmaceutical manufacturers to have in place a risk management plan to monitor and mitigate risks associated with their opioid products, once they are on the market. The proposed amendments would also require that a patient information handout and a warning sticker be provided with the sale of a prescription opioid.
Regulatory Actions:
- Naloxone available without a prescription
- Expedited approval of nasal spray version of naloxone
- Physicians able to apply to Health Canada to request access to medical grade heroin for their patients
- Import of medications approved elsewhere for urgent public health needs
- Made it harder to access six fentanyl precursor chemicals
Compliance and Enforcement
Compliance and enforcement activities help ensure conformity with federal laws and regulations. Under the CDSS, enforcement activities aim to address illegal production and trafficking and the diversion of drugs from legitimate uses.
Targeting illegal opioids has been established as a Federal Policing national priority. The RCMP has implemented a national operational strategy targeting synthetic opioid importers, distributors, manufacturers and traffickers and established the Organized Crime Joint Operations Centre with the Canada Border Services Agency (CBSA) and Canada Post. The goal is to detect, disrupt and dismantle criminal networks and help keep illegal fentanyl out of Canada.
The CBSA is also piloting designated safe examination areas in certain air cargo courier and postal facilities. These areas are equipped with modified procedures, infrastructure as well as detection and personal protective equipment to allow for the safe and efficient examination of goods suspected to contain toxic substances such as illegal fentanyl. An additional pilot has been launched to test a designated safe sampling area in border operations. This facility allows for on-site testing and analysis of suspected products by chemists using state-of-the-art equipment. Networked communication with the CBSA Forensic Laboratory supports real-time identification, interdiction and the eventual prosecution of those responsible for smuggling these substances.
To reduce the risk of diversion of prescription medication to the illegal market, Health Canada inspectors conduct compliance and enforcement activities to ensure that regulatory requirements are met, to educate regulated parties about the proper storage of controlled substances, and to address unauthorised actions by regulated parties, such as companies and pharmacies. For example, Health Canada's CDSA inspectors carry out over 700 inspections each year.
Compliance and Enforcement
- RCMP national operational strategy for synthetic opioids implemented
- CBSA pilot projects to examine goods suspected of containing toxic substances at the border
- 700+ inspections by Health Canada of regulated parties to help prevent diversion
Programs
The Government of Canada, through the CDSS, supports ongoing work in the areas of prevention, treatment, harm reduction, enforcement and improving evidence. Existing programs are continuing their work, with an annual budget of $114.1 million per year, and are also focussing their efforts to address the opioid crisis. The new funding announced in Budget 2017, in the amount of $100 million over 5 years, with $22.7 million ongoing, bolsters these programs and supports new federal initiatives.
Public Health
Treatment for problematic opioid use is a crucial component of our collective response to this crisis. The provision of treatment services largely falls under the jurisdiction of provincial and territorial governments. To that end, the Government of Canada has committed $5 billion to provinces and territories over ten years to improve access to mental health and addiction services for Canadians.
The Government of Canada committed $5 billion to provinces and territories over ten years to improve access to mental health and addiction services for Canadians.
Health Canada's Substance Use and Addictions Program (SUAP) provides financial support to provinces, territories, non-governmental organizations and key stakeholders to strengthen responses to drug and substance use issues in Canada in the area of health promotion, prevention, harm reduction and treatment. Through SUAP, a variety of projects have been undertaken to address problematic opioid use, including McMaster University's update of the Canadian Guideline for Safe and Effective Use of Opioids for Chronic Non-Cancer Pain, released in May 2017, that provides recommendations for physicians on the appropriate use of opioids. In June, 2017, a SUAP call for proposals was launched to address substance use issues related to licit and illicit psychoactive substances, with a particular focus on opioids.
Part of the additional funding for the CDSS includes $30 million over five years for the Public Health Agency of Canada to fund community-based initiatives to reduce rates of hepatitis C and HIV among people who use drugs. The new Harm Reduction Fund will be targeted to areas where there are high rates of drug use and infectious diseases and will facilitate access to harm reduction measures.
Through the Canadian Institutes of Health Research (CIHR), the Government of Canada supported the CRISM's development of the National Guideline for the Clinical Management of Opioid Use Disorder. The federal government will continue to support the research network in its efforts to disseminate and implement this Guideline.
Public Health Programming:
- $5B/10 years to provinces and territories for mental health and addiction services
- Substance Use and Addictions Program call for proposals with focus on opioids
- New funding for community-based initiatives to reduce rates of hepatitis C and HIV among people who use drugs
First Nations and Inuit Communities
The Government of Canada supports community-based health program delivery to First Nations on-reserve and to Inuit communities. We also provide primary care services on-reserve in remote and isolated areas, where provincial services are not readily available and supplementary health benefits to eligible First Nations and Inuit, regardless of their residence. The Government of Canada continues to work with Indigenous and provincial and territorial partners to provide effective, sustainable, and culturally appropriate health programs and services to improve health outcomes.
Each year, the Government of Canada provides more than $350 million to support the mental wellness needs of First Nations and Inuit communities. Programming includes mental health promotion, problematic substance use and suicide prevention, life promotion, crisis response services, treatment and after-care and supports for eligible former students of Indian Residential Schools and their families. These investments are being guided by the First Nations Mental Wellness Continuum Framework and the National Inuit Suicide Prevention Strategy, developed with and by our First Nations and Inuit partners. Available problematic substance use services include a network of 44 federally-funded treatment centres, as well as prevention services in the majority of First Nations and Inuit communities across Canada. In 2015-16, these treatment centres registered over 3,600 client admissions to inpatient care, in addition to community-based opioid agonist treatment programs. Health Canada is currently funding over thirty opioid agonist therapy sites, and is working with First Nations partners to increase opioid agonist treatment with comprehensive care (e.g. counselling, social services, health services) at an additional nine sites in the coming year.
The Government of Canada is providing naloxone nasal spray for remote and isolated communities through nursing stations to provide timely access to at-risk clients and their families, until the product is available at local retail pharmacies. For remote and isolated communities, naloxone injection is listed as a "must stock" medicine in the Nursing Station Formulary. We are also working with existing provincial public health programs to distribute take-home naloxone injection kits to high-risk clients for opioid overdose.
Through the Non-Insured Health Benefits Program (NIHB), the Government of Canada provides continued coverage for opioid agonist therapies including buprenorphine/naloxone, methadone and other treatments to First Nations and Inuit clients. Since 2013, the Program has had system-level opioid dose limits to prevent unsafe dose escalations, and engages with prescribers who have clients on higher doses, to encourage a slow taper to a safer dose. Additionally, NIHB monitors opioid prescribing patterns and provides feedback to prescribers who prescribe at rates that are higher than their peers, and has a client-level Prescription Monitoring Program to promote safe use of prescribed opioids among clients at-risk.
Programming for First Nations and Inuit
- Working with Indigenous, provincial and territorial partners to provide culturally appropriate services
- Increasing access to opioid agonist treatment in some First Nations communities
- Supporting efforts to promote harm reduction initiatives based on the unique needs of First Nations and Inuit communities, including the availability of naloxone
Public Security and Safety
In existence since 2004, the Department of Justice's Drug Treatment Court Funding Program (DTCFP) continues to fund the development, delivery and evaluation of drug treatment courts in Canada. Drug treatment courts represent a concerted effort to break the cycle of drug use and criminal recidivism. They focus on facilitating treatment for those in the criminal justice system who meet specified criteria and provide an alternative to incarceration by offering an opportunity to complete a drug treatment program. In keeping with the comprehensive, collaborative and compassionate approach to drug policy, the DTCFP is looking to support models of collaboration that focus on therapeutic approaches leading to off-ramps from the criminal justice system.
In the area of prevention, the Correctional Service of Canada (CSC) has developed educational materials for offenders and has rolled out a national project to provide inmates being released with access to a take-home naloxone kit. This population could be particularly vulnerable to overdosing if their tolerance to opioids has diminished while incarcerated. Furthermore, CSC staff have access to naloxone nasal spray to treat opioid overdoses in federal correctional facilities.
Similarly, the RCMP has distributed naloxone nasal spray kits nationally, to be carried by on-duty operational members and employees that are at risk of accidental exposure, and who may be required to provide first aid treatment to citizens in an emergency situation if an opioid overdose is suspected. The CBSA has also distributed naloxone nasal spray kits and training to all operational areas where there is a risk of accidental contact with opioids to staff, or where first aid may be required as a result of opioid exposure.
Internally, much work has been done to develop occupational health and safety policies and procedures to guide the RCMP, CSC and CBSA officers about the safe handling of highly toxic substances including the use of appropriate personal protective equipment.
Public Security and Safety Programming
- Educational materials for offenders
- Take home naloxone kits for inmates being released
- Naloxone available to RCMP and CBSA staff
- Occupational health and safety policies and procedures for handling of highly toxic substances (RCMP, CSC and CBSA)
Beyond the programs specifically designed to address substance issues, federal strategies and initiatives are in place to address social conditions and mental wellness which have an influence on problematic substance use. This includes the Government of Canada's renewed Homelessness Partnering Strategy, which received an investment of $2.1 billion over 11 years in the 2017 Federal Budget. The Government of Canada is also committed to developing a Poverty Reduction Strategy, and we financially support the Mental Health Commission of Canada, which released a Mental Health Strategy for Canada in 2012.
Knowledge, Information Sharing and Education
One of the obstacles to addressing the opioid crisis was the initial lack of information at a national level, and in many cases, at provincial and regional levels. Data is being collected in different ways by different people measuring different things. Improving epidemiological surveillance is one of the key priorities of the F/P/T Special Advisory Committee on the Epidemic of Opioid Overdoses. To this end, under the leadership of the Chief Public Health Officer of Canada and the Chief Medical Officer of Health in Nova Scotia, in early 2017 F/P/T governments agreed to common case definitions and a uniform reporting template for apparent opioid-related death surveillance. In addition, at the request of some provinces, through the SAC, the Public Health Agency of Canada has deployed field epidemiologists to eight provinces and territories, with more to follow, to assist with data collection.
As a result of this close collaboration with provincial and territorial partners, there is now increased opioid data collection and public quarterly reporting providing details on opioid-related deaths in Canada by type of substance involved, age, sex and region. Federal health portfolio organizations are also working with other partners including the Canadian Institute for Health Information (CIHI) and Statistics Canada to provide an integrated national picture of opioid-related deaths and harms. This improved data helps inform and coordinate responses to the opioid crisis across the country. It is also consistent with the Government of Canada's commitment to an evidence-based drug policy. Federal, provincial and territorial governments will continue to collaborate on enhanced data reporting, including on other related harms.
The CIHR launched a request for applications in September 2017 to support new knowledge syntheses to increase our understanding of issues associated with the opioid crisis. To facilitate the exchange of information, the CIHR has also hosted two knowledge exchange events with health professionals, mental health experts, researchers and representatives of provincial/territorial governments to discuss data and policy and legal frameworks, with another exchange to be held on November 16, 2017 on the implementation of the National Guideline for the Clinical Management of Opioid Use Disorder.
In 2014, the CIHR established a pan-Canadian network on problematic substance use called the Canadian Research Initiative in Substance Misuse (CRISM). This research network is composed four large regional nodes that connect researchers, service providers, decision makers and people with lived and living experience from across Canada. Since its inception, CRISM has conducted significant work to provide research evidence on issues related to problematic opioid use. This includes for example the conduct of a national clinical trial to compare methadone and buprenorphine/naloxone for the treatment of opioid use disorder.
In September 2017, the CRISM received $7.5 million in additional funding from the CIHR to inform how best to implement practical research interventions to prevent opioid overdoses, treat those living with opioid dependence, and promote harm reduction. This research investment will enhance the development of evidence-based practices that can be used by those dealing with this crisis on the ground in communities across Canada.
To better understand the level of knowledge that Canadians have about opioids, and their willingness and ability to act in the event of an overdose, Statistics Canada is conducting a Survey on Opioid Awareness. Results from the survey will be released in January 2018.
Health Canada's Drug Analysis Service (DAS) provides scientific and technical services to help Canadian law enforcement agencies in their activities involving illegal drugs. In December 2016, Health Canada used this information to begin providing real-time drug alerts to provincial and territorial health authorities about emerging potent illegal drugs identified from substances submitted for analysis from their region. It has issued over 100 such alerts since that time. In addition, DAS provides quarterly summary reports, which are available online, on the substances identified in the samples seized by Canadian law enforcement agencies. DAS officials continue to work with clients, both traditional and new, to identify other ways it can share its unique information and capacity to help address the crisis.
With regard to public education, the Government of Canada continues to raise awareness among Canadians about the harms associated with problematic substance use, with a focus on the risks of problematic opioid use. Public education campaigns and outreach initiatives since May 2017 have included providing Canadians with information online at Canada.ca/Opioids related to the opioid crisis and the Government's response (e.g. Good Samaritan Drug Overdose Act and naloxone), a series of videos including one on fentanyl, and posters about calling 9-1-1 to help someone experiencing an overdose in high traffic locations in various Canadian cities. Products are targeted at a variety of audiences, including people who use drugs occasionally, people with substance use disorders, people who use prescription opioids, as well as teens and their parents.
Our efforts to raise awareness of the risks associated with problematic opioid use and opioid-related overdoses included outreach and communication to music festivals, major events, and on university and college campuses throughout the summer and fall 2017. Finally, a new online toolkit, released in August 2017, provides a central repository for a variety of awareness materials, including infographics, videos, and maps on mortality data and surveillance.
Knowledge, Information Sharing and Education:
- Quarterly reporting on opioid-related deaths
- Public Health Agency of Canada deployed epidemiologists in 8 provinces and territories to assist with data collection (more to be placed)
- CIHR knowledge synthesis request for applications
- $7.5M in new funding to the Canadian Research Initiative in Substance Misuse
- 100+ alerts to provincial/territorial health authorities and law enforcement about emerging illegal drugs in their region
- Online quarterly reports on what Health Canada is finding in seized drugs
- Outreach to summer music festivals and events and university and colleges
- Online information tool kit
Looking forward
Governments, non-government organizations, health and public safety professionals and individual Canadians across the country have accomplished much in the past year, but there is still a lot of work to do. Despite efforts to date, the number of overdoses in Canada continues to rise.
We recognize that more needs to be done to improve access to treatment. The Government of Canada will continue to work with provinces and territories to identify barriers to treatment and to explore how to remove them. For example,a Notice To Interested Parties has been issued to seek feedback on a proposal to remove some restrictions to diacetylmorphine (heroin) so that it can be part of a comprehensive list of treatment options for opioid use disorder. We will also continue to work within our mandate to facilitate access to therapies and treatment services for the populations we serve. This includes working with First Nations partners to increase opioid agonist treatment with comprehensive care at an additional nine sites in the coming year.
We have heard from those with lived and living experience about how people who use drugs are often viewed negatively – as though they are not like average Canadians, that they caused their own problems, or that they are simply not trying hard enough to "get over" their problems. This stigma not only fails to recognize problematic substance use as the health issue that it is, but it serves to further marginalize and isolate individuals who most need treatment and health and social services. While the conversation is beginning to change, stigma remains one of the biggest barriers to care.
The Government of Canada will continue to engage broadly with those with lived and living experiences to address this issue. Within government, we will make better linkages between social programs and supports and treatment for people who use drugs, including for individuals participating in federally supported drug treatment courts. We will work with partners to raise awareness about the impact that stigma related to opioid use has in our communities. And we will also fund peer support programs to work with organizations that help people who use drugs.
We also know that while some progress has been made in the area of data, we still have gaps and the depth of our evidence remains a concern. The structures that have been set up will continue to improve the evidence base, as we explore more permanent ways to collect and monitor data. This will help us identify future drug issues as they emerge, allowing us to respond earlier.
The Government of Canada will continue to work with our partners to identify and encourage innovative approaches including exploring new ways to use and share data to help those on the front lines. We will also undertake exercises to determine how recently-developed internal occupational health policies and procedures about the safe handling of highly toxic drugs are working, and can share best practices more broadly. And, we will look at innovative ways to support drug checking services, starting with authorizing these services at supervised consumption sites and funding pilot projects at these sites. The government will also work with provinces and territories on a streamlined protocol for temporary overdose prevention sites where a province or territory has identified an urgent public health need.
The Government of Canada will also work with partners across the country, including people with lived and living experiences to identify gaps, barriers and solutions, as we further elaborate the Canadian Drugs and Substances Strategy, to ensure we are well positioned to continue to respond to the current crisis and any future challenge that may arise.
Future Actions
- Remove regulatory barriers to treatment and harm reduction measures
- Support innovative approaches
- Increase access to opioid agonist treatment in some First Nations communities
- Take steps to address stigma related to opioid use
- Improve reporting of overdoses
Further updates on federal activities can be found on the Government of Canada's opioid web page.
Links to Provincial and Territorial webpages:
- British Columbia
- Alberta
- Saskatchewan
- Manitoba
- Ontario
- Quebec
- Newfoundland and Labrador
- New Brunswick
- Nova Scotia
- Prince Edward Island
- Yukon
- Northwest territories
- Nunavut
Government of Canada Actions on Opioids: 2016 and 2017
Summary of Actions to Date
Leadership
- Announced new Canadian Drugs and Substances Strategy
- $100M/5 years and $22.7M ongoing to address drugs and opioids
Working Together
- Opioid Conference and Summit
- Joint Statement of Action to Address the Opioid Crisis
- Roundtable discussions with those directly affected
- Federal/provincial/territorial committees established
- Government of Canada Deputy Ministers Task Force
Beyond Canada's Borders
- North American Dialogue on Drug Policy
- Bilateral discussions with US and China
Legislative Changes
- Streamlined application requirements for supervised consumption sites
- Require registration to import pill presses
- Ability to quickly control new dangerous substances entering the illegal market
- Allow opening of mail weighing 30g or less if suspected of containing unauthorized controlled substances
- Legal protections for individuals who seek help during an overdose
Regulatory Actions
- Naloxone available without a prescription
- Expedited approval of nasal spray version of naloxone
- Physicians able to apply to Health Canada to request access to medical grade heroin for their patients
- Import of medications approved elsewhere for urgent public health needs
- Made it harder to access six fentanyl precursor chemicals
Compliance and Enforcement
- RCMP national operational strategy for synthetic opioids implemented
- CBSA pilot projects to examine goods suspected of containing toxic substances at the border
- 700+ inspections by Health Canada of regulated parties to help prevent diversion
Public Health Programming
- $5B/10 years to provinces and territories for mental health and addiction services
- Substance Use and Addictions Program call for proposals with focus on opioids
- New funding for community-based initiatives to reduce rates of hepatitis C and HIV among people who use drugs
Programming for First Nations and Inuit
- Working with Indigenous, provincial and territorial partners to provide culturally appropriate services
- Increasing access to opioid agonist treatment in some First Nations communities
- Supporting efforts to promote harm reduction initiatives based on the unique needs of First Nations and Inuit communities, including the availability of naloxone
Public Security and Safety Programming
- Educational materials for offenders
- Take home naloxone kits for inmates being released
- Naloxone available to RCMP and CBSA staff
- Occupational health and safety policies and procedures for handling of highly toxic substances (RCMP, CSC and CBSA)
Knowledge, Information Sharing and Education
- Quarterly reporting on opioid-related deaths
- Public Health Agency of Canada deployed epidemiologists in 8 provinces and territories to assist with data collection (more to be placed)
- CIHR knowledge synthesis request for applications
- $7.5M in new funding to the Canadian Research Initiative in Substance Misuse
- 100+ alerts to provincial/territorial health authorities and law enforcement about emerging illegal drugs in their region
- Online quarterly reports on what Health Canada is finding in seized drugs
- Outreach to summer music festivals and events and university and colleges
- Online information tool kit