Extreme heat and human health: For pharmacists and pharmacist technicians
Download the alternative format
(PDF format, 517 Kb, 2 pages)
- Organization: Health Canada
- Date published: 2024
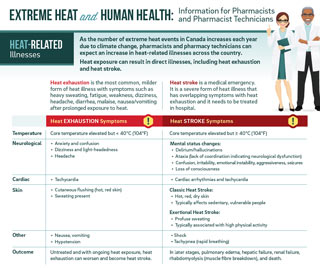
Heat-Related Illnesses
As the number of extreme heat events in Canada increases each year due to climate change, pharmacists and pharmacy technicians can expect an increase in heat-related illnesses across the country.
Heat exposure can result in direct illnesses, including heat exhaustion and heat stroke.
Heat exhaustion is the most common, moderate form of heat illness with symptoms such as heavy sweating, fatigue, weakness, dizziness, headache, diarrhea, malaise, nausea/vomiting after exposure to heat.
Heat stroke is a medical emergency. It is a severe form of heat illness that has overlapping symptoms with heat exhaustion and it needs to be treated in hospital.
| Heat Exhaustion Symptoms | Heat Stroke Symptoms | |
|---|---|---|
| Temperature | Core temperature elevated but < 40°C (104°F) | Core temperature ≥ 40°C (104°F) |
| Neurological |
|
|
| Cardiac |
|
|
| Skin |
|
|
| Other |
|
|
| Outcome | Untreated and with ongoing heat exposure, heat exhaustion can worsen and become heat stroke. | In later stages, pulmonary edema, hepatic failure, renal failure, rhabdomyolysis (muscle fibre breakdown), and death. |
At-Risk Populations
Many of the risk factors that can increase the susceptibility to heat-related illness and death are interrelated. Some pre-existing conditions are exacerbated by exposure to heat and increase a person's vulnerability to heat-related illness.
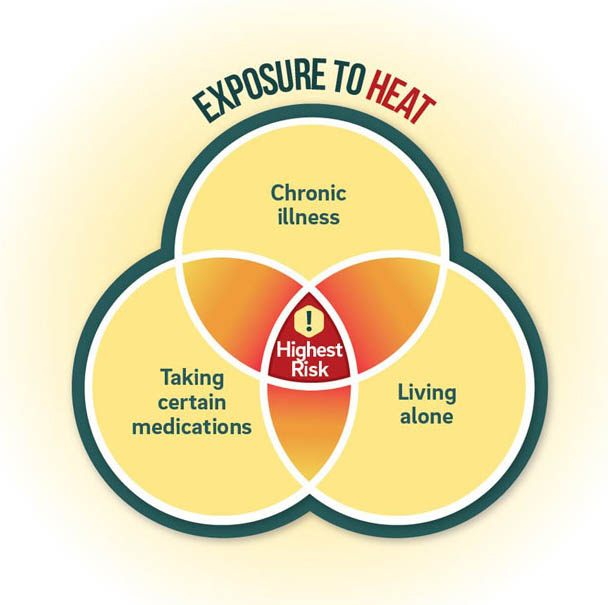
Text Description
A Venn diagram, with three overlapping circles, demonstrates three risk factors associated with increased susceptibility to heat-related illnesses: having a chronic illness, taking certain medications and living alone. When two of these risk factors overlap, they are at a higher risk, and where all three risk factors overlap a person is at the highest risk.
Populations disproportionately affected by heat include:
- Older adults and children
- Those who are pregnant
- Athletes & people who are active in heat (such as outdoor workers)
- People with cardiovascular illnesses (including hypertension), obesity, diabetes, respiratory illnesses, renal disease, neurological disease, and mental health disorders including addictions
- People who are malnourished or dehydrated
- People who have a history of heat illness or an active sunburn
- People living alone & people who are socially isolated
- People with lower socioeconomic status
Heat-Risk Factors Associated with Medications
Various drugs and medications are known to interfere with the body's thermoregulatory mechanisms, predisposing the person to heat illness.
Note: There is no straightforward relationship between the consumption of a drug and a resultant hyperthermic state. Heat stroke may occur in those who are not on any medications. Heat stroke episodes can be due to a physiological condition that predisposes a patient to heat hypersensitivity (e.g., poor hydration), and may not be associated with any drug(s) in question. Secondly, there are various drugs that can induce a hyperthermic state in the absence of extreme environmental heat or exercise.
Any medication with the potential to affect the following can put someone at a higher risk of heat illness:
- The hypothalamus, and the body temperature set-point
- Heat perception, leading to behavioural change (avoidance)
- Cardiac output
- Peripheral vasodilation
- Sweat rate
- Renal function
- Body hydration
- Electrolyte status
Some examples of drug classes include:
- Antipsychotics/ Neuroleptics
- Antidepressants
- Lithium
- Anti-epileptics
- Anti-Alzheimer's agents (Cholinesterase inhibitors)
- Anti-Parkinson's agents
- Diuretics
- Nitrate vasodilators
- ACE inhibitors
- Calcium channel blockers & beta blockers
Prevention of Heat-Related Illnesses
- Drink water before having the sensation of thirst, drink MORE when it is hot
- Lower consumption of alcohol, if possible
- Do not increase consumption of caffeine
- Wear light-coloured, loose-fitting, breathable clothing and wear a hat
- Reduce strenuous activity (e.g., reduce duration & intensity of activity),
- Be active during cooler parts of day or move activities to a cooler area
- Spend more time in air conditioned spaces, use cool showers/baths as alternative if air conditioning is not available
- Mist the skin with cool water to cool down when hot
- Seek medical attention, as needed
Recommendations for Pharmacists and Technicians during Extreme Heat Events
- Recognize early signs of heat illnesses and direct patients to appropriate medical care.
- Discuss safe handling of medications sensitive to heat.
- Identify patients more at risk during extreme heat events.
- Identify medication history or prescribed medications that may exacerbate heat-related conditions.
- Provide Health Canada heat health information to patients, especially those prescribed medications that may increase their vulnerability to heat related illnesses. Resources can be found online and ordered at Canada.ca
Extreme Heat Events Guidelines: Technical Guide for Health Care Workers: https://www.canada.ca/en/health-canada/services/environmental-workplace-health/reports-publications/climate-change-health/extreme-heat-events-guidelines-technical-guide-health-care-workers.html