What we heard: Strengthening Canada's approach to substance use issues

Download the alternative format
(PDF format, 1,339 KB, 38 pages)
Organization: Health Canada
Date published: 2019-07-09
Table of Contents
- 1. Introduction
- 2. Stigma and Discrimination
- 3. Understanding Problematic Substance Use
- 4. Accessing Services and Support
- 5. Services that Better Meet the Needs of Individuals and Groups
- 6. Community Safety and the Criminal Justice System
- 7. Addressing Problematic Alcohol Use
- 8. Conclusion and Next Steps
- Appendix A – What We Asked: List of Questions from the Online Questionnaire
- Appendix B – Who We Heard From
1. Introduction
Canada is currently facing the most severe public health crisis in recent history, with annual mortality rates from drug-related overdose deaths exceeding those seen at the peak of the HIV epidemic. 11,577 Canadians lost their lives to opioid-related overdose between January 2016 and December 2018. The Government of Canada has taken steps to respond decisively to this crisis, including quickly addressing key gaps in federal drug policy. For example, we streamlined the application process for supervised consumption sites, launched campaigns to raise awareness of the stigma faced by people who use drugs, and provided $150M in funding to provinces and territories to increase their substance use treatment capacity.
However, opioid overdoses and other harms associated with problematic substance use continue to negatively impact Canadians. The Canadian Drugs and Substances Strategy guides federal action to address substance use issues, including the federal response to the opioid crisis, and measures to address the problematic use of other substances such as cannabis and alcohol. We know that more can be done to better meet the needs of Canadians, their loved ones and their communities.
To that end, a 90-day consultation was launched on September 5, 2018, to gather ideas on potential next steps under the Canadian Drugs and Substances Strategy.
The consultation was primarily conducted through an online questionnaire (Appendix A) and a "Tell us your story" tool which allowed Canadians to share their personal experiences with drug and substance use. The online consultation was supplemented by in-person workshops held in Halifax, Toronto, Ottawa, and Winnipeg, which were attended by over 200 participants and drug policy stakeholders, including those with lived experience. Additional information on the in-person workshops is included in Appendix B.
More than 1,600 responses to the consultation were received. We would like to thank those who took the time to participate. Many respondents shared details of their personal challenges with problematic substance use, including for some, the tragic loss of someone close to them.
Overview of Themes
A number of common themes emerged in the responses received Footnote 1. This report presents the feedback we received under each of the themes.
- We heard from many respondents that stigma and discrimination towards people who use drugs act as barriers to effectively addressing substance use issues in Canada. On the other hand, a few respondents told us that stigma can be an effective deterrent to substance use in the first place.
- Respondents told us that there is a need to improve our understanding of problematic substance use by strengthening the evidence base and conducting more research on underlying causes. We also heard that effectively addressing problematic substance use requires an understanding that we must address its root causes including mental health, and issues such as financial insecurity and a lack of stable housing.
- We heard that access to treatment in Canada is impeded by many factors including long wait lists and high costs. Many respondents called for increased access to particular treatment options including medication assisted treatments, while others preferred non-medication approaches. We heard that there are not enough harm reduction or high quality treatment services across the country, particularly in rural and remote areas. A small number of respondents told us that instead of focusing on harm reduction, we should focus our efforts on prevention and treatment.
- We heard that there is no “one-size fits all approach” to addressing substance use and that services need to be better tailored to meet the needs of individuals and groups. We heard that culture, race, gender, sexuality and age all need to be considered, and that communities should also have a voice in designing services that meet their needs.
- Respondents also provided their views on how Canada’s criminal justice system deals with substance use. Suggestions ranged from strengthening Canada’s capacity to prevent drug trafficking, reducing or eliminating criminal penalties for people who use drugs, diverting people with substance use disorders away from the criminal justice system and towards health care and other support programs, and increasing collaboration between public health and law enforcement officials, to calls for harsher penalties for substance related offenses and the stricter regulation of substances.
- Finally, we heard that the federal government should do more to minimize the harms caused by problematic alcohol use, including increasing awareness, legislative and regulatory changes, and developing a national alcohol strategy.
- Footnote 1
-
As the respondents did not represent a nationally representative sample (demographic information on respondents is included in Appendix B), the consultation feedback cannot be interpreted as reflecting the views of all Canadians or the spectrum of opinions regarding substance use in Canada. For the purposes of this report, “many” can be interpreted to mean greater than 20% of respondents, “some” means between 10-20%, a “small” number is less than 10%, and a “few” is less than 2%.
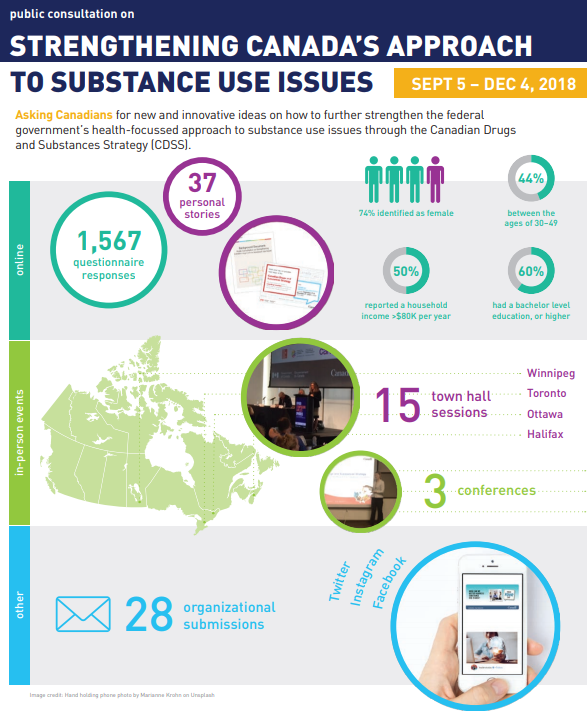
Infographic - Text Equivalent
This infographic provides a visual narrative of the engagement activities for the Canadian Drugs and Substances Strategy.
Public consultation on strengthening Canada’s approach to substance use issues (Sept 5 – Dec 4, 2018)
Asking Canadians for new and innovative ideas on how to further strengthen the federal government’s health-focused approach to substance use issues through the Canadian Drugs and Substances Strategy (CDSS).
Online
1567 questionnaire responses
37 personal stories
Background document and postcards advertising the consultation
74% of respondents identified as female
50% of respondents reported a household income of greater than $80,000 per year
44% of respondents were between the ages of 30 and 49
66% of respondents had a bachelor level education, or higher
In-person events
Map of Canada showing where the in-person consultation sessions took place. There were a total of 15 in person consultation sessions with stakeholders in Winnipeg, Toronto, Ottawa and Halifax.
Two photographs of government officials presenting information.
Three conferences
Other
28 organizational submissions
Twitter, Facebook, Instagram
Image of a hand holding a phone with screen showing consultation web page
Image credit: Hand holding phone photo by Marianne Krohn on Unsplash
Government of Canada, Canada wordmark
2. Stigma and Discrimination
Stigma can be defined as the negative attitudes directed toward a group of people due to their circumstances in life, while discrimination is the behaviour that results from these negative attitudes. Stigma and discrimination are cross cutting issues that were consistently raised in response to the consultation questions, and have impacts on all other themes raised in this consultation.
Many respondents told us about the negative impacts caused by stigma towards people who use drugs and other substances. In contrast, a small number of respondents told us that stigma can be an effective deterrent from using substances in the first place.
We heard that stigma is a barrier to people seeking treatment and other services and can prevent people from receiving necessary care.
There is no way I would ever admit to a doctor if I used illegal drugs. First rule is don't admit it, even if your health is at risk. You might have your kids taken away, or go to jail; never mind being patronized by someone who probably does not know anything about it. That is an issue.
We heard that the fear of judgement by others can lead to feelings of shame and make people unwilling to access harm reduction or treatment services such as methadone clinics or needle exchanges.
We also heard that stigma can lead to riskier substance use, such as using alone, sometimes with tragic consequences.
My 27 year old son who was brilliant and employed died alone in his truck from heroin laced with fentanyl…End the stigma and shame so they don't use alone.
People literally die because they are stigmatized. They use alone because they cannot share with their family or friends their drug use. They do not access services or seek help from workers/community members/physicians/hospital staff because they fear they will be judged, seen as other, refused services due to their drug use.
Some respondents told us that people aren't compassionate to people who have substance use disorders or don't form trusting relationships with them.
We heard that education and awareness activities should be implemented in as many places as possible including schools and workplaces. Respondents told us that education on substance use should be started in elementary or high schools, in order to overcome stigma at an early age, and/or teach the harms and benefits of substance use. We heard that the public, government workers, counsellors, teachers, health care providers and law enforcement officials all need to be better educated on substance use.
Stigma is still one of the largest barriers to people accessing support and treatment. Increasing awareness to healthcare providers on the experiences of people with stigma and providing appropriate training on approaches and solutions to eliminate stigma would be valuable, as well as training on trauma-informed care. This should be developed in collaboration with people who have lived or living experience with substance use.
When asked which kinds of messages would work best to help Canadians understand the serious harms that can result from stigma around substance use, respondents told us that sharing the stories of people who use drugs or are in recovery would help reduce stigma by humanizing problematic substance use. We also heard that messages should focus on helping people understand that problematic substance use is a health issue, not a personal choice or a moral failing, that it can happen to anyone. We heard that there are underlying issues that cause problematic substance use, such as mental health issues, poverty, trauma, and chronic pain.
When asked how we can best act to reduce stigma across the country, most respondents said we should engage with people who use drugs to help them share their stories and experiences with stigma with the public. Many respondents also supported information campaigns by non-governmental organizations, celebrities, social media influencers, etc. and information campaigns by government.
Addiction does not discriminate, it is extremely powerful, and addicts are not bad people. We unfortunately have chosen drugs as a way to cope, and they have brought negative consequences and behaviours. Once we reach a point where we are willing to get help, and battle our addiction, we can become contributing members of society. Please instead of judging, try and help and show some love and tolerance.
3. Understanding Problematic Substance Use
This section summarizes feedback related to improving the understanding of problematic substance use through research and evidence and the recognition of its root causes.
Research and Evidence
Many respondents told us that there is a need for more data on people who use drugs, including their demographics (e.g. race, age, gender), their mental health status, their personal histories, and their socio-economic status.
Some respondents told us that there is a need for data on access to treatment and support services, as well as evidence that the current treatments are effective. A small number of respondents called for data on wait times for treatment.
Some respondents identified the need for more research into psychedelic drugs to treat mental health and substance use disorders. A small number of respondents expressed concern about a lack of data on cannabis, including the benefits and harms associated with its use.
Some respondents said that research and evidence was needed to clarify prescription guidelines and practices, for example the use of opioids for chronic and acute pain.
The need for research into substance use, including on its underlying biological causes and risk factors, was raised by some respondents. Respondents also called for research on the effects of psychoactive substances, the role of mental health in substance use disorders, and whether there is a link between childhood use of drugs that affect the central nervous system and the development of substance use disorders later in life.
A small number of respondents stated that overdose data could be improved by providing more detail on things such as the drugs involved, the pattern of use (e.g. recreational), the frequency of occurrence, and the long term health impacts on survivors.
Other data gaps identified by respondents include information on the type of drugs being used, information on where drugs are coming from, information on the costs of drugs, and data on community needs related to substance use, such as the scope and nature of substance use in rural areas. A few respondents said there is a lack of information on the costs associated with problematic substance use.
Many respondents called for more timely information sharing between groups already collecting data in order to share access to the most current information regarding substance use. Some suggested that Canada needs a mechanism to pool information from a variety of sources in real time and create a system that could be easily accessible. There were also suggestions for information sharing between doctors and pharmacists to keep tabs on which prescriptions are being filled by patients and where/how often.
When asked how we could better identify emerging substance use patterns as early as possible, many people told us that we should better leverage the expertise of people on the frontlines who have the most current information about drug types in circulation and issues being experienced. This includes people who use drugs, and their families and friends, frontline workers, physicians and other healthcare professionals, and law enforcement officials.
In addition, some respondents told us that an early warning system regarding dangerous drugs would be useful. This data could be enhanced by providing services to test drugs for contamination and adulteration.
Other suggestions included improving community-based data collection. This would allow officials to identify substance use trends and to understand the needs of communities. Studies of school-aged populations were also suggested as a way to enable the earlier identification of factors that may contribute to problematic substance use later in life.
It begins with data surveillance. We need to monitor and look for trends among people who use substances. We should find that there are many external factors that can be addressed…. taking a preventative lens that is evidence-informed will be more cost effective for society and the healthcare system, as well as reduce the personal burden for those struggling with substances.
A very small number of respondents suggested scanning social media to identify trends, with a few specifically mentioning the dark web.
Addressing Root Causes
Respondents told us we should focus on preventing problematic substance use from occurring in the first place. Many respondents stressed the importance of good mental health to prevent problematic substance use. We were told that mental health care should be more accessible, with many calling for full mental health coverage through provincial and territorial health plans. Other suggestions included mental health care workers in schools, and more funding for social workers and case workers. We also heard about increased feelings of stress or being overwhelmed due to the accelerated pace of modern life and factors such as a lack of work/life balance or the false sense of connection or unrealistic expectations caused by social media. To address this, respondents told us about the importance of improving community connectedness and increasing hope, factors that strengthen resilience and protect mental health.
The importance of housing was mentioned by many respondents, with many calling for increased affordable housing with social supports. We heard that financial challenges can make people less likely to get necessary health care, including treatment for mental health issues, and that this may make someone more vulnerable to problematic substance use.
When asked about initiatives that would improve the social determinants of health that influence substance use, many people mentioned the need for income supports, with some suggesting that a guaranteed minimum income would help those who are struggling to meet their basic needs. A small number of respondents called for the more widespread adoption of a housing first approach, including wraparound services.
Guaranteed minimum income is a system of payments by a government to eligible citizens, intended to ensure that all citizens or families have sufficient income to live.
Housing First involves rapidly moving people experiencing homelessness - particularly chronic homelessness- from the street or emergency shelters into stable long term housing, with supports. The goal is to encourage housing stability, improved quality of life and foster self-sufficiency.
Folks who are marginalized, discriminated against, excluded, poor, and homeless need their social and health needs met before addressing the substance use issues - substance use isn't the cause of their vulnerability it's the symptom. Address the cause.
We heard about the needs for parental and prenatal programming, particularly for low-income families, including free childcare, so children and families have access to quality care and parents can participate in the workforce.
While a few respondents told us that stricter parenting alone would prevent teens from substance use, many respondents called for funding for programs that keep teens meaningfully busy and connected to their communities, such as after-school programs, community sports, and apprenticeships.
Education, recreational services, and career opportunities seem like the three biggest factors for at-risk youth in particular: essentially, being able to carve out an encouraging potential path for life success (and life enjoyment!).
Finally, many respondents mentioned the importance of education about substance use for youth, parents, healthcare providers and the general public, to raise awareness of potential risks and ways to minimize those risks. In particular, we heard about the importance of providing youth with factual, non-judgemental information about substance use. Others said that more facts about the risk factors related to substance use would allow for earlier identification of potential problems by family members, friends, teachers, doctors, youth workers and others.
4. Accessing Services and Support
This section summarizes feedback related to accessing services and supports related to problematic substance use.
Treatment
The most common thing we heard through the consultation was that there are not enough treatment services and those that are in place have long wait lists making it difficult for people to access treatment when they decide they are ready. Many people told us that the cost of treatment acts as a barrier, mentioning the high costs of private treatment facilities, medications, or counselling services. People told us that this should be addressed with more public funding and/or insurance coverage for treatment services.
In general, funding for working people (especially the working and lower middle class) to take time away and go spend time in a healing or recovery centre without financial penalty and risk of losing their housing or jobs... This measure is critical in increasing accessibility to treatment options. Currently, unless you are on Income Assistance or have a stellar benefits package, it is very difficult financially to take that kind of time to make the commitment to yourself and your wellness.
Many people told us that the logistics of seeking treatment, such as having to arrange child care or time off of work, also act as barriers to treatment. For example, we heard that having 9am-5pm Monday-to-Friday hours for outpatient services makes it difficult for people to seek treatment while also maintaining their employment or other responsibilities.
We also heard about the frustration of trying to navigate the treatment system, which some told us was fragmented and disorganized. Examples included the need to make regular calls to maintain a spot on treatment waiting lists, and the need to complete complicated and extensive intake assessments at each stage of the process (e.g., detox, inpatient treatment, outpatient treatment). We heard that there is a need to better integrate treatment of problematic substance use with other healthcare services, particularly mental health care and primary care, in order to better address concurrent disorders.
…existing systems are a disparate jumble of clinics, charities, hospital services, and more, and very few of these coordinate effectively with each other; effective coordination requires very capable and committed communicators in these organizations to unite their services. Facilitating this communication is a key element of improving treatment access.
When I was calling [a] place for information, some centres refused to talk to me because I was not the person with the addiction. I was told he had to reach bottom, which may be death, and when he wanted information bad enough he could phone.
Respondents also told us that the requirement not to use substances for a period of days or weeks prior to entering treatment was a barrier for many. We also heard that the fact that some treatment facilities require complete abstinence or limit the use of other substances such as tobacco acts as a barrier to treatment.
Addiction is the only medical condition where you get kicked out of the treatment program for having the disease that you want treated. We would never kick a diabetic out of the hospital because they didn't adhere to their diet!
Many respondents called for the increased availability of a range of treatment options. While some called for increased access to medication-assisted treatments such as buprenorphine/naloxone or prescription heroin (diacetylmorphine), a few respondents said that they did not support medication-assisted treatments, such as methadone, with many of those stating that abstinence should be the end goal. In contrast, some respondents expressed concern about treatment programs, such as 12-step models, that focus on abstinence. Respondents also said that poly-substance use (using more than one substance at a time) should be better addressed in treatment programs.
A few respondents called for mandatory treatment services, particularly for youth, with some stating that people with substance use disorders may not be capable of making decisions about their treatment needs. A few respondents expressed concern about privacy policies that prevented parents or other family members from being informed of their loved ones’ interactions with the health care system, including any prescriptions they may have been given.
Many respondents told us about the need for more treatment and harm reduction services closer to their homes, particularly outside of urban centres. We heard about the challenges associated with having to travel long distances to access services, including difficulties finding transportation.
Getting to appointments is an issue. Finding transportation is difficult for many clients, which may make it hard for them to get to a pharmacy to pick up methadone before the pharmacy closes, or to make it to doctor appointments on time. Because it's difficult to find a family doctor, some clients end up living in a place that's hours away from their health care provider, which is a huge barrier for someone who needs frequent contact with their doctor. This is even an even worse issue for rural clients.
Other concerns included the need for better training for health care providers on available treatment options, screening, early identification, and referral for substance use treatment. A small number of respondents said that more health care providers should be permitted to prescribe medications to treat substance use disorders.
We also heard about the need to provide sensitivity training to health care professionals and front line workers on how to work with people who use drugs. It was suggested that this would make people who use drugs more comfortable and therefore more likely to seek out help and stick with treatment when they are ready.
The largest barrier is poorly educated staff providing treatment according to outdated theories. Addiction treatment is a clinical specialty that requires clinicians who are well educated and able to include the latest research perspectives in their practice.
Finally, some respondents told us they are concerned about the lack of standards or accreditation for treatment facilities across the country. In addition, some respondents expressed concern about the efficacy of treatment models and/or the lack of well-trained staff. To address this, respondents asked for government oversight or accreditation to ensure minimum standards are met.
It is super difficult to get in to treatment. And then when you arrive, you're often searched - told to change into a hospital gown, have your belongings removed. You're not allowed to smoke- your crutch is removed without your consent. But you have to. You feel like a criminal again: and with your years of being judged, excluded, ashamed - this may not be your first time here - you have failed…again..: You want to leave. So you leave. Because often the attitudes of the people there are not welcoming. And they are not based on best evidence. You have a very strong culture of AA and medicalization that focus either on choice /god / a life of personal punishment or a program that heavily focuses on medication and short term support. At least in some places, people can now be on OAT and still go to recovery care. But that isn't the norm.
Harm Reduction
We heard from some respondents that existing harm reduction services (e.g., supervised consumption sites and needle exchanges) need to be scaled up to better meet the needs of Canadians. Respondents told us that there should be increased access to supervised consumption sites across Canada, particularly outside of urban centres, with some respondents stating that supervised consumption sites should be available in every province. Some respondents told us that the process for establishing supervised consumption sites should be more straightforward. In addition, many respondents told us that harm reduction services should be provided in different settings (e.g., hospitals, pharmacies, community health centers) and that they should support different modes of consumption, such as inhalation, in order to reach more people and reduce drug related harms, including overdoses. A small number of respondents told us that there should be more harm reduction options for stimulants, including equipment such as pipes, filters and needles. We also heard about the need for drug checking services in order to allow people to make informed choices about whether or not to use their drugs, or to use them in safer ways. On the other hand, a small number of respondents told us that enough has been done in the area of harm reduction already and that the federal government should focus its efforts on prevention and treatment.
A small number of respondents told us that people who use drugs should be provided with safer alternatives to the contaminated drug supply, such as prescription drugs.
Respondents told us that education and awareness are important aspects of harm reduction. We heard about the need to inform health care providers about harm reduction, to educate people who use drugs on harm reduction options, and to educate the general public about its importance in order to improve understanding and acceptance of harm reduction services.
Education on lower-risk substance use PERIOD. That means, of ALL substances. What is safe, what is harmful, what mixtures shouldn't happen, what do you do if you take too much of something, who can you talk to? Etc.
I think it could be important to educate the general public on harm reduction. In a lot of cases people with no experience with addiction or harm reduction don't understand it, why it is important and they may look at it as enabling. The more knowledge and education that we can share on the topic the more communities will understand the importance of it.
Social Supports and "Wrap-Around Care"
We heard from many respondents about the importance of social supports and wrap-around care for people who use drugs. Respondents told us that addressing problematic substance use in isolation from all other factors in a person's life (including housing stability, friends and family, childcare and mental wellness) is setting them up for failure. Several noted that integration of a person's family in the after-care preparation and reintegration process is often neglected, leaving children, spouses, and parents at a loss when they try to support their loved one.
One of the primary barriers that I face as an outreach support worker that deals with marginalized populations is the issue of identification. Many of these individuals have no ID at all and the way the system is set up it is almost impossible to get ID especially when they have no money. Without ID they are unable to get social services support, a bank account or even into addiction treatment.
Very few programs are accommodating to people with children and it can often mean that children remain in care, and when people are out of treatment and most vulnerable, they do not have support in caring for their children.
5. Services that Better Meet the Needs of Individuals and Groups
This section summarized feedback related to tailoring services to the needs of individuals and groups.
Services for Indigenous Peoples
We heard about the need to scale up Indigenous-led, culturally safe approaches, with many citing the Honouring our Strengths: A Renewed Framework to Address Substance Use Issues Among First Nations People in Canada as a successful model.
Honouring our Strengths: A Renewed Framework to Address Substance Use Issues Among First Nations People in Canada is a national framework to address substance use issues among First Nations people in Canada. It outlines a continuum of care and provides guidance on an approach to community development that prioritizes mental health and well-being and relies upon community and cultural strengths.
Many respondents called for the root causes of problematic substance use to be addressed within Indigenous communities, such as inadequate infrastructure (e.g., housing, drinking water), food insecurity, a lack of recreational and educational opportunities for youth, the loss of language and connection to the land and the inter-generational trauma caused by residential schools.
Addressing social determinants of substance use seems like the best route: investing more in education, work opportunities, counselling services, culturally appropriate rehabilitation programs, and overall investment into being able to live out indigenous cultural identity seem like some of the most affirming ways to preventatively and currently address substance use.
We heard that there should be more support for traditional and land based treatment approaches built upon the distinct cultural touchstones of First Nations, Inuit, and Métis communities. In addition, we heard that services should be improved or expanded within Indigenous communities so that people don't have to leave their homes to access things such as education, treatment or harm reduction services.
Inuit have developed innovative models that work for Inuit …By being trauma-informed and grounding participants in pride for Inuit language and culture… The solutions are there, but they need to be scaled up, and adequately and securely funded.
We heard that different approaches are needed for Indigenous peoples living on-reserve or in their traditional communities and those Indigenous people living in urban areas. A number of respondents suggested the use of mentorship or peer-support programs for Indigenous youth to decrease isolation and promote community identity, including for youth that need to move to urban areas to attend school.
We also heard that access to treatment can be complicated by jurisdictional issues. For example, it was mentioned that federal funding generally supports on reserve programs, which may not be accessible to individuals that currently live off reserve.
When asked about what could be learned from Indigenous approaches to problematic substance use, we heard about the need for a greater focus on community connection and emotional and mental well-being.
Indigenous initiatives use a holistic approach that addresses people's pride in themselves, including cultural pride. They tend to be strengths-based, building on what the person can do, rather than the western model which focuses on what is wrong with the person and the person's need to be "fixed". Healing is not the same as fixing. Healing implies restoring balance with the community and the universe.
Meeting the Needs of Pain Patients
The response to the opioid crisis and public and media attention around the role of prescription opioids in Canada's opioid crisis, have led to changes in the ways that opioids are prescribed. We heard that chronic pain patients sometimes have trouble accessing medications and other forms of care necessary to treat their condition. Many respondents told us that health care professionals do not spend enough time with pain patients to adequately discuss their conditions, and the range of treatment options that may be available, which can lead to inadequate care and the misperception that a patient is seeking drugs instead of being recognized as genuinely in pain and in need of treatment. We also heard about the need for more frequent follow-up and monitoring of patients so that treatment can be modified and adapted as needed.
Respondents cautioned against a "one-size fits all" approach to pain management, noting that health care providers should listen to patients to understand their individual needs, and to recommend treatments that work for them, including opioids for those who need them.
The decision to prescribe opiates- or any other medication- should be a personal decision between a patient and his doctor with no one else playing any part in it.
Respondents told us about the need to develop comprehensive approaches to pain management that include non-opioid alternatives, such as physiotherapy, acupuncture, cannabis and concomitant psychological supports. Many respondents told us that these alternatives should be covered under provincial and territorial health care plans to the same extent as opioids and other pharmaceuticals.
Many respondents called for more health care resources to be dedicated to helping patients manage their pain. Some suggested that pain management clinics should be established and that there should be better access to practitioners who are specialized in pain management. We also heard that the way healthcare providers are paid should be changed so that they can spend more time with patients.
A small number of respondents strongly advocated for awareness campaigns and media reports to clarify that in the context of the opioid crisis, pain patients often have very different needs, challenges and barriers to services than other groups.
Tailoring Approaches to the Needs of Specific Populations
We heard that there is a need to tailor approaches to substance use to the needs of specific populations that may be at risk of experiencing substance use related harms due to underlying social or economic factors.
Many respondents told us that we should work with communities that may be at risk of developing problematic substance use to develop programs and strategies that meet their specific needs by considering factors such as the impacts of sex, gender, race, age, and culturally-specific understandings of healing and wellness.
We heard that we should speak to people who live and work in these communities such as health care workers and peer support workers from community organizations, establish community liaisons, and get advice from people who use drugs or with lived experience with drug and substance use issues.
Without the active and supported involvement of people with lived experience, we run the risk of once again not developing and implementing strong and effective public policies that will be effective and supportive for at-risk populations.
Understand the differences between these groups, and build the program to directly address these differences. Interface with intervention groups that are already active with these populations.
We heard that some groups face more barriers to treatment than other Canadians for reasons including financial insecurity, a lack of stable housing, disability, trauma, and experiences of stigma and discrimination that may be compounded by the intersection of more than one stigmatized identity (e.g., sexual orientation, a person who uses drugs). To help address this, respondents called for tailored and trauma-informed community based programs, increased mental health supports, and mobile treatment services that reach out to people who need help instead of waiting for them to seek it. We were told that supportive spaces and options for LGBTQ2, women, youth, and sex workers are critical.
I think that everyone has different issues and yet the same…We just need to find places where people can feel comfortable and stay connected to their religion and culture, to help address the issues. LGBTQ+ would feel more comfortable and share more common experiences in a facility designed specifically for them than one that is mostly 30-60 year old men.
There is a gap in service when youth turn 18, and youth ages 18-24 (or 18-29) lack appropriate services. Youth who are 19 are often not a good fit for adult services and programs, however there are no other options. Addiction programs should expand their youth services to serve youth age 19-24 as these clients are often a better fit for youth services and would benefit from continued care as they continue to be at a high risk age.
We also heard that health and social service providers (including governments, the health care system, and civil society organizations) should be better connected to prevent people from falling through the cracks and that more support should be provided upon a person's first interaction with the justice or medical system.
6. Community Safety and the Criminal Justice System
This section summarizes feedback related to improving community safety and crime prevention, changes to the way Canada's criminal justice system approaches people with problematic substance use, and collaboration between public health and law enforcement officials.
Community Safety
Some respondents called for increased efforts to prevent the importation of controlled substances into Canada. While most respondents did not expand upon how to achieve this, a few provided specific recommendations including focusing on ports of entry, increasing staffing and resources at borders, monitoring the postal system and working with other governments.
Some respondents told us that law enforcement should focus on organized crime groups that produce and import drugs into Canada, with some suggesting that money laundering should be targeted to reduce the profits of the illegal drug business.
A few respondents suggested education could improve community safety, for example by educating jailed drug dealers about the effects drugs have on their clientele and exposing the underbelly of drug trafficking and exploitation.
A small number of respondents provided specific suggestions of initiatives that law enforcement could take to better address current priorities, including collaborating with international law enforcement partners, addressing the sale of illegal substances on the internet or "darknet", reducing access to drug paraphernalia, increasing community policing, increasing surveillance activities and tackling instances of corruption within the law enforcement system.
Criminal Justice Approaches to Problematic Substance Use
Consultation respondents provided many suggestions on how to adapt Canada's criminal justice system to better address problematic substance use.
Many respondents commented that criminal penalties for substance use-related offenses should be reduced or eliminated, including the decriminalization of possession of small amounts of drugs for personal use, and/or for the legalization and regulation of currently illegal substances. A small number of respondents mentioned the approach that Portugal has taken to problematic substance use, which eliminates criminal sanctions for substance use while reallocating enforcement funding to treatment and prevention. In contrast, many respondents called for the tougher regulation of alcohol and a few respondents expressed concern about the potential impacts of cannabis legalization.
We heard from some respondents that there should be harsher penalties. While some of these respondents did not specify, most stated that harsher penalties should be for high-level drug dealers, especially fentanyl dealers. Other respondents called for harsher penalties for people dealing to minors, or stated that more severe penalties would deter others from becoming dealers. A small number of respondents said there should be harsher penalties for possession of illegal substances. Specific suggestions included longer jail sentences for trafficking, homicide charges or automatic life sentences for trafficking fentanyl, a 3 strikes rule, keeping dealers in solitary confinement, releasing drug dealer names to the media, and minimum sentences for trafficking.
At the same time, many respondents told us that treatment for problematic substance use should be provided as an alternative to criminal charges and jail time.
Some responders suggested that diversion models should be developed where individuals with substance use disorder would be directed towards treatment and other health and social supports to break the cycle of repeated drug use and incarceration. Others called for drug treatment courts, or expanding the range of offenses eligible for drug treatment courts or other diversion programs.
Drug treatment courts provide an alternative to incarceration by offering drug-involved adult offenders who meet specified criteria an opportunity to complete a drug treatment program.
Prison time is probably the worst possible way to deal with substance addiction. However, it is a great method to ensure people have no other non-substance options left in their lives.
Some respondents called for more substance use treatment services to be provided to individuals in prison or on probation. We heard that there should be more support for people who use drugs following their release from prison, including social supports (e.g., housing, employment support) to help reduce substance use and the risks of returning to prison.
Other suggestions included implementing more restorative approaches, with a focus on addressing the root causes of crime; not making abstinence a requirement for drug treatment courts; and reforming parole so people who use drugs are not restricted from using harm reduction services upon their release.
A small number of respondents called for increased awareness of the Good Samaritan Drug Overdose Act among law enforcement, or changes to broaden its applicability.
The Good Samaritan Drug Overdose Act provides some legal protection for people who witness or experience an overdose and call 9-1-1 for help.
And while the Good Samaritan Drug Overdose Act was passed in 2017.…people who use drugs have indicated that they are still deterred from calling 911 to report an overdose because emergency dispatchers continue to dispatch police in response to calls reporting a suspected overdose, the list of offences for which one cannot be charged is far too limited, or the law does not protect people in prison from institutional charges.
Models of Collaboration between Law Enforcement and Public Health Officials
Many respondents told us that collaboration between the criminal justice system, and specifically law enforcement, with the health care community (e.g., social workers, nurses, doctors) should be improved. Specific examples of potential collaboration included teaming up police officers with mental health nurses and/or social workers for day-to-day policing activities. There were many calls to improve training and education for law enforcement and justice officials in public health related areas such as stigma and racism, trauma, human rights, harm reduction and treatment, with some suggestions for joint training between law enforcement and public health.
7. Addressing Problematic Alcohol Use
Many respondents recognized that problematic alcohol use in Canada is a significant issue with higher costs and harms than other substances. While we heard that problematic alcohol use shares many of the same causes as other problematic substance use, many of the challenges are the result of the normalization of problematic alcohol use.
By far the biggest issue when it comes to substance use … is the widespread and far reaching normalization of alcohol consumption in so many segments of culture and society.
We heard that alcohol use is seen as socially acceptable and is linked to "having a good time" and celebrations. Many respondents expressed concerns regarding excessive drinking among youth, including the "party culture" at colleges, universities and sports games. Respondents also told us that alcohol is affordable and widely available.
Alcohol is offered everywhere you go. If you are trying to quit drinking or have an alcohol use disorder, you cannot escape.
Many respondents told us that the normalization of problematic alcohol use is supported by the high prevalence of inescapable advertising and marketing of alcohol, including efforts that target women and youth.
Alcohol is blatantly and aggressively normalized and advertised whereas other substances have a zero tolerance policy regarding advertisement and marketing.
We also heard that alcohol is often used as a coping mechanism to deal with stress, disappointment, trauma, and other mental health issues. Some respondents cited the role of parents in modeling alcohol use, and the role of genetics and intergenerational trauma in contributing to problematic alcohol use in youth.
Actions to Address Problematic Alcohol Use
Many respondents recommended that the federal government take action at the national level to address alcohol related harms, including implementing a national alcohol strategy, passing federal legislation (i.e., an "Alcohol Act"), and/or putting in place a comprehensive public health approach to alcohol similar to cannabis and tobacco. Some respondents suggested any such approach should not be influenced by the alcohol industry.
To help prevent youth from engaging in problematic alcohol use, some respondents recommended school-based prevention programs to teach resiliency and positive coping skills. Others suggested including information about the risks and harms of problematic alcohol use in school curriculum.
The more I knew about drugs when I was younger, the more I wanted to stay away from them - conversely we learn nothing about how alcohol affects the body and that can be detrimental to youth because it is so acceptable in our society to over-consume.
A small number of respondents recommended implementing the "Iceland model" to reducing alcohol use - a data-driven, community-based prevention model that engages youth in recreation and encourages positive parental involvement.
To address problematic alcohol use at the population-level, it was recommended that the federal government implement evidence-based practices, such as the World Health Organization's "Best Buys" to reduce the harmful use of alcohol which include: controlling affordability of alcohol through pricing and taxation, regulating the physical availability of alcohol, and placing strict controls on marketing and advertising of alcohol. In particular, many respondents suggested restricting alcohol marketing and advertisement, including addressing social media.
The Best Buys are recommendations from the World Health Organization regarding the most cost-effective, evidence-based interventions to reduce the harmful use of alcohol.
Many respondents suggested raising awareness of Canada’s Low-Risk Alcohol Drinking Guidelines and a “standard drink”, as well as risks and harms of alcohol use, such as cancer and family and sexual violence, through health warnings or standard drink labels and targeting messaging for specific demographics (i.e., youth, women).
In my community and networks, I see a culture of consumption and poor understanding of what it means to drink moderately or at low risk.
On the other hand, two industry organizations raised concerns related to labelling, including the need to ensure that information is balanced and complete, as well as suggesting that the federal government explore alternative approaches to consumer education. An industry association also indicated that existing marketing and advertisement restrictions are sufficient and that they do not support price or taxation increases.
Similar to other substances, we heard about the need to increase access to treatment services for alcohol use disorder, including reducing wait-times, increasing access to medically-assisted treatment, and early screening and interventions. Some respondents suggested moving away from abstinence-based approaches; however, others acknowledged that abstinence-based approaches were successful for some people, particularly when combined with access to support services like affordable housing.
Many respondents also urged the government to increase harm reduction efforts, including increasing support for and expanding managed alcohol programs that integrate housing and broader healthcare services. Finally, a small number of respondents indicated the need for increased research and surveillance on problematic alcohol use in Canada.
8. Conclusion and Next Steps
It is clear that problematic substance use is a complex issue. At its core are longstanding challenges such as poverty, housing instability and mental health, which Canadians will continue to grapple with for some time. We know that there is more that can be done to prevent problematic substance use, to provide better treatment for those in need, and to help reduce the associated harms to individuals, families and communities across Canada.
The Government of Canada would like to thank all of those who participated in this consultation, which has provided us with practical suggestions to make inroads into this important issue. Respondents have made it clear through their comments that there is no one-size-fits-all solution to substance use issues, and progress requires close collaboration between governments, the medical community, public health officials, law enforcement, Indigenous peoples, and all stakeholder groups, including people who use drugs.
We will closely review and consider the ideas and experiences shared through this process, as well as inputs from other sources, as we move forward with a public-health focussed approach to problematic substance use under the Canadian Drugs and Substances Strategy.
People who use drugs deserve access to evidence-based treatment and respect as much as your families and businesses do. Let’s come together in our common humanity and find ways to mitigate the risks that some community members are concerned about, while also providing respect, compassion and evidence-based treatment for those suffering with substance use disorder. Each of those affected is somebody’s someone.
Appendix A – What We Asked: List of Questions from the Online Questionnaire
- What sorts of circumstances do you see within your networks, communities or in society that you think contribute to problematic substance use?
- Have you seen or experienced programs, practices or models at the local or regional level that could be expanded, or implemented more broadly, to improve circumstances or social determinants of health that influence substance use?
- What needs to change to make sure that opioid medications are being provided and used appropriately, based on the needs of each patient?
- How can we make sure that those who require prescription opioids to manage their pain have access to them, without judgement or discrimination?
- Which kinds of messages would work best to help Canadians understand the serious harms that can result from stigma around substance use?
- How can we best act to reduce stigma across the country? (you may select more than one answer)
- Information campaigns by governments
- Information campaigns by non-governmental organizations, celebrities, social media influencers, etc.
- Engagement with people who use drugs to help them share their stories and experiences with stigma with the public
- Other(s) (please write your answer in the text box below)
- What would you recommend to improve substance use treatment services in Canada?
- What obstacles or barriers do people face when they want to access treatment in Canada?
- The federal government has been focussed on removing regulatory barriers to effective treatment. For example, we have recently made it easier for treatment providers to prescribe medications such as methadone for people with opioid use disorder. Are there other regulatory barriers to treatment that the federal government should look at, in order to help increase access to evidence-based treatment in Canada?
- In addition to current harm reduction initiatives – such as supervised consumption sites, needle exchange programs – what other harm reduction services should governments consider implementing in Canada?
- Many harm reduction tools focus on opioid use disorder (e.g., naloxone). How can the federal government develop harm reduction tools to address a broader range of substances, such as stimulant drugs (e.g., methamphetamines, cocaine)?
- How can we better bring public health and law enforcement together to explore ways to reduce the cycle of involvement for people who use substances with the criminal justice system?
- What further steps can the federal government take to better address current regulation and enforcement priorities, such as addressing organized drug crime and the dangerous illegal drugs like fentanyl being brought into Canada?
- Recognizing Indigenous rights and self-determination, how can all governments work together to address the high rates of problematic substance use faced by some Indigenous communities?
- What can we learn from Indigenous approaches to problematic substance use, such as using holistic approaches, that may help inform activities under the CDSS?
- How can governments, and the health, social, and law enforcement sectors design more effective substance use policies and programs for at-risk populations?
- What are effective policies and programs to help improve access to prevention, treatment, and harm reduction services for at-risk populations?
- What urgent gaps related to substance use (in terms of data, surveillance, and/or research) need to be addressed in Canada?
- How can we use research tools to better identify emerging substance use issues as early as possible?
- We look forward to continuing to work together as a country to address substance use issues from a health perspective. If you have any additional comments or ideas on potential next steps in the CDSS, please include them below.
Appendix B – Who We Heard From
Background on the In- Person Consultation Workshops
At the end of November 2018, in-person consultation workshops were held in Ottawa (November 1 and November 27), Toronto (November 26), Winnipeg (November 27-28) and Halifax (November 28-29), in order to gather input from individuals and stakeholders who might not otherwise participate in the online consultation.
The workshops focused on particular themes of the consultation, tailored to the interests of stakeholders in a particular region. Themes included: moving forward with prevention; increasing access to evidence-based treatment; expanding harm reduction services and reducing stigma; law enforcement and justice, alcohol policy, and addressing methamphetamine use.
Feedback from the in-person workshops was collected on a “not for attribution” basis, summarized into notes and rolled up into this report.
Detailed Demographic Information of Online Consultation Respondents
Note: Demographic information was only collected for online questionnaire respondents.
(For all the figures below, n= total number of responses, NR = no response (i.e., "Prefer not to answer", or blank).
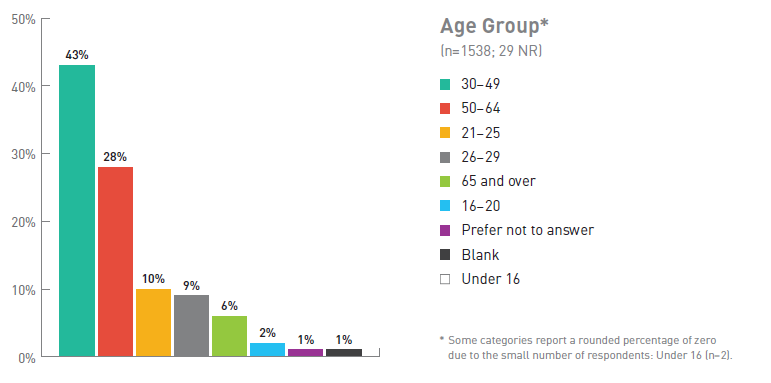
Figure 1. Breakdown of Respondents by Age Group
| Age Breakdown | Number of respondents (%) (No response =29) |
|---|---|
| 30-49 | 43 |
| 50-64 | 28 |
| 21-25 | 10 |
| 26-29 | 9 |
| 65 and over | 6 |
| 16-20 | 2 |
| Prefer not to answer | 1 |
| Blank | 1 |
| Under 16 | 0Footnote * |
| Total number of respondents | 1538 |
|
|
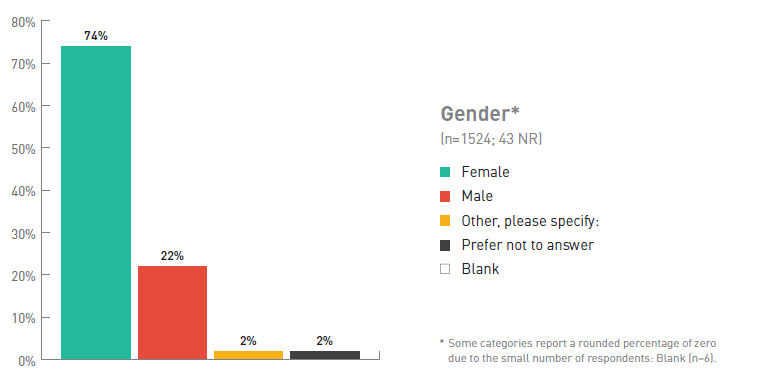
Figure 2. Breakdown of Respondents by Gender
| Gender | Number of respondents (%) (No response = 43) |
|---|---|
| Female | 74 |
| Male | 22 |
| Other, please specify | 2 |
| Prefer not to answer | 2 |
| Blank | 0 Footnote * |
| Total number of respondents | 1524 |
|
|
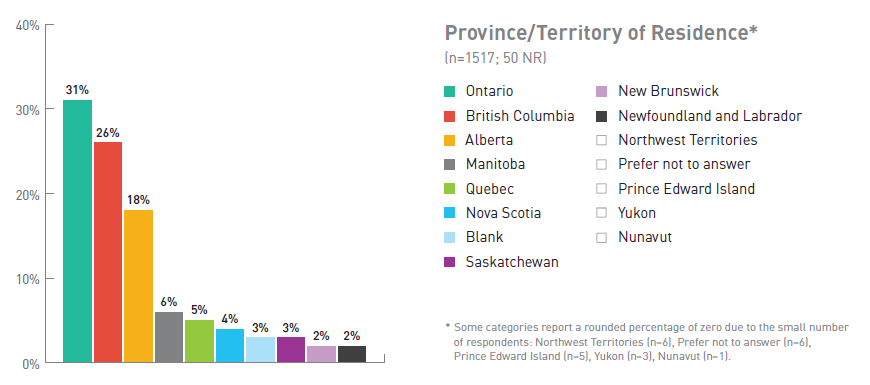
Figure 3. Breakdown of Respondents by Province/Territory of Residence
| Province/territory | Number of respondents (%) (No response = 50) |
|---|---|
| Ontario | 31 |
| British Columbia | 26 |
| Alberta | 18 |
| Manitoba | 6 |
| Quebec | 5 |
| Nova Scotia | 4 |
| Blank | 3 |
| Saskatchewan | 3 |
| New Brunswick | 2 |
| Newfoundland and Labrador | 2 |
| Northwest Territories | 0 Footnote * |
| Prefer not to answer | 0 Footnote * |
| Prince Edward Island | 0 Footnote * |
| Yukon | 0 Footnote * |
| Nunavut | 0 Footnote * |
| Total number of respondents | 1517 |
|
|
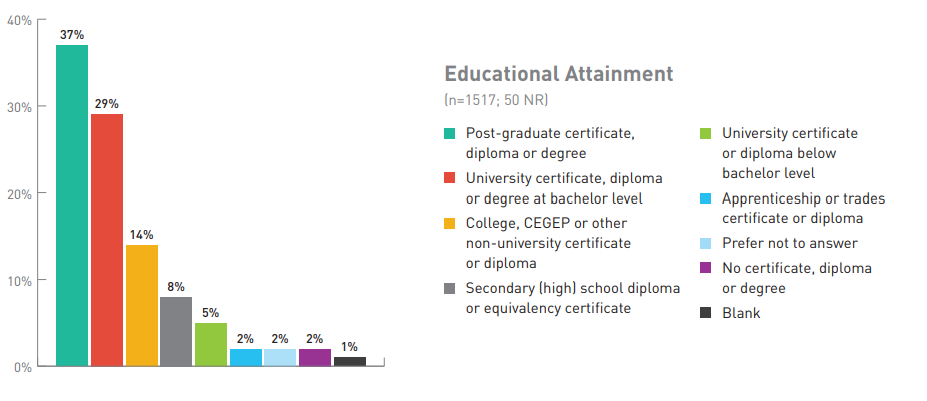
Figure 4. Breakdown of Respondents by Educational Attainment
| Education level | Number of respondents (%) (No response = 50) |
|---|---|
| Post-graduate certificate, diploma or degree | 37 |
| University certificate, diploma or degree at bachelor level | 29 |
| College, CEGEP or other non-university certificate or diploma | 14 |
| Secondary (high) school diploma or equivalency certificate | 8 |
| University certificate or diploma below bachelor level | 5 |
| Apprenticeship or trades certificate or diploma | 2 |
| Prefer not to answer | 2 |
| No certificate, diploma or degree | 2 |
| Blank | 1 |
| Total number of respondents | 1517 |
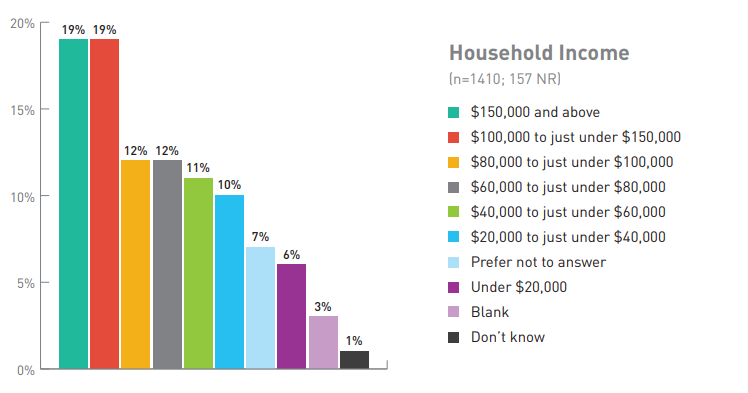
Figure 5. Breakdown of Respondents by Household Income
| Household Income | Number of respondents (%) (No response = 157) |
|---|---|
| $150,000 and above | 19 |
| $100,000 to just under $150,000 | 19 |
| $80,000 to just under $100,000 | 12 |
| $60,000 to just under $80,000 | 12 |
| $40,000 to just under $60,000 | 11 |
| $20,000 to just under $40,000 | 10 |
| Prefer not to answer | 7 |
| Under $20,000 | 6 |
| Blank | 3 |
| Don't know | 1 |
| Total number of respondents | 1410 |
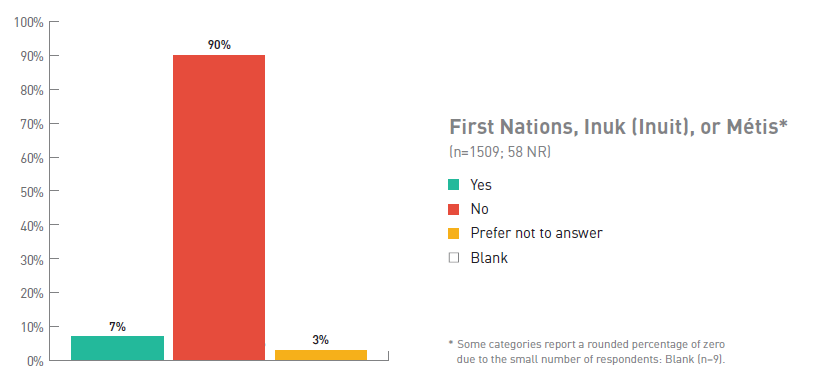
Figure 6. Respondents Identifying as First Nations, Inuk or Métis
| First Nations, Inuk or Métis | Number of respondents (%) (No response = 58) |
|---|---|
| Yes | 7 |
| No | 90 |
| Prefer not to answer | 3 |
| Blank | 0 Footnote * |
| Total number of respondents | 1509 |
|
|
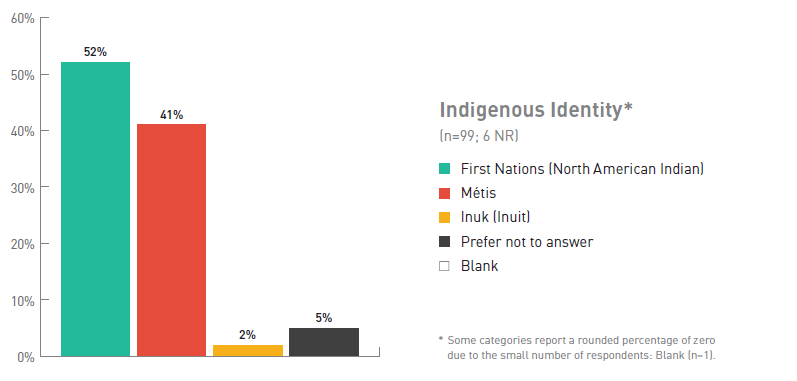
Figure 7. Breakdown of Respondents by Indigenous Identity
| Indigenous Identity | Number of respondents (%), (No response = 6) |
|---|---|
| First Nations (North American Indian) | 52 |
| Métis | 41 |
| Inuk (Inuit) | 2 |
| Prefer not to answer | 5 |
| Blank | 0 Footnote * |
| Total number of respondents | 99 |
|
|