Seniors' Falls in Canada: Second Report
To promote and protect the health of canadians through leadership, partnership, innovation and action in public health.
For readers interested in the PDF version, the document is available for downloading or viewing:
Seniors' Falls in Canada: Second Report (PDF document - 2.1 MB - 52 pages)
Table of Contents
- Executive Summary
- Preface: How this report is organized
- 1.0 Introduction
- 2.0 The scope of the problem
- 3.0 Risk factors for falls and fall-related injuries among seniors
- 4.0 Best practices for the prevention of falls
- 5.0 Stepping up fall prevention in Canada
- Appendix A: Distribution of CCHS sample with injury related to a fall by key demographic variables, age 65+, Canada, 2005 and 2003
- Appendix B: Factors associated with an increased risk of falling among older adults
- References
Executive Summary
Injury in Canada is a serious public health concern. It is a leading cause of hospitalization for children, young adults and seniors, and it is a major cause of disability and death. Falls remain the leading cause of injury-related hospitalizations among Canadian seniors, and between 20% and 30% of seniors fall each year. Falls and associated outcomes not only harm the injured individuals but also affect family, friends, care providers and the health care system. However, we do know that these personal and economic costs can be avoided through injury prevention activities.
To this end, this report provides policy makers, researchers, community programmers and practitioners with current national information to prevent falls among seniors. It offers an update of our knowledge of falls, injuries and hospitalizations among Canadian adults aged 65 and over, and provides a picture of changes over time. The data used in this report were taken from the Canadian Community Health Survey, the Hospital Morbidity Database and Canadian Vital Statistics Footnote 31 Footnote 159 Footnote 160.
The data show a continued, but also increasing, need for effective falls interventions initiatives targeted at older adults. Among Canadian seniors, falls remain the leading cause of injury-related hospitalizations, and absolute numbers are on the rise. Falls can lead to negative mental health outcomes such as fear of falling, loss of autonomy and greater isolation, confusion, immobilization and depression. In addition to the negative physical and mental health consequences of falling, there are significant associated financial costs, estimated at $2 billion annually, a value 3.7 times greater than that for younger adults Footnote 156.
Results from the data analysis indicate that self-reported injuries due to falls are increasing, specifically by 43% between 2003 and 2009/2010. The majority of falls resulted in broken or fractured bones, and over one third of fall-related hospitalizations among seniors were associated with a hip fracture. Fracture-induced physical limitations augment the need for support on the part of older adults themselves and their caregivers, and increases pressure on Canadian health care systems.
When hospitalization data are examined, the results show that seniors who are hospitalized for a fall remain in hospital an average of nine days longer than those hospitalized for any cause. This discrepancy highlights the disproportionate health care costs of fall-related injuries in comparison to other causes of hospitalization. Even more worrying is that the number of deaths due to falls increased by 65% from 2003 to 2008.
The report also presents risk factors for falls among seniors, which are numerous, complex and interactive. These factors are categorized as biological/intrinsic, behavioural, environmental and social/economic. Each older person may face a unique combination of risk factors according to his or her life circumstances, health status, health behaviours, economic situation, social supports and environment. Factors that put seniors at risk of falls include chronic and acute health conditions, balance or gait deficits, sensory factors, inadequate nutrition, social isolation, as well as factors related to the built and social environment.
Evidence shows that preventing falls requires interventions that target more than one risk factor. Specifically, the evidence supports comprehensive individual assessment followed by multifactorial, evidence-based practices. Fall prevention guidelines may be useful to assess individual risks, behaviours and challenges, and to establish standards that minimize the number and impact of falls. Further, interventions need to be tailored to the individual's health status, situation and environment.
The research literature on risk factors for falls and on best practices in fall prevention reveals a number of research gaps. In particular, there is a lack of knowledge around the efficacy of fall prevention practices for subpopulations of Canadian seniors. Given that 50% of falls that result in hospitalization occur in the home and the same percentage of seniors are discharged to a home setting, the report also serves to highlight the importance of developing and evaluating tools for seniors and their families to plan for safely aging in place.
Falls among seniors are preventable; however, their multifactorial nature means that addressing this growing public health problem is a shared responsibility. Progress in the prevention of falls and their resulting injuries requires continued multisectoral collaboration, including governments, health care providers, non-government organizations, care associations and services, as well as Canadians themselves. Over the years, Canada has laid a foundation for good health and well-being across the life course Footnote 123. However, as our population ages, focused efforts on fall prevention will be required to maintain and improve the quality of life and well-being of seniors and to ensure that they continue to contribute and participate in society.
The Public Health Agency of Canada (PHAC) has a history of playing a strong coordinating role with respect to fall prevention among seniors in Canada. Working collaboratively with stakeholders, PHAC aims to increase the capacity of those who work with seniors to plan, implement and evaluate evidence-based injury prevention programs. To target the unique needs of seniors in preventing injuries due to falls, PHAC has undertaken several activities in public education, community-based programming and policy development. Examples include numerous publications aimed at helping seniors and their families to reduce the occurrence and impact of falls. PHAC has also advanced the Age-Friendly Communities concept in Canada and internationally as a way to facilitate healthy and supportive environments for older adults.
In Canada, there is an increased understanding of what puts seniors at risk of falling and what kind of fall prevention interventions work, for whom and in what setting. Healthy aging is about creating conditions for individuals to make choices and engage in behaviours that prevent falls. Given Canada's aging population, it is anticipated that falls will continue to be a public health problem, especially if collaborative action is not taken. In stepping up our coordinated efforts against falls, Canadians are working together to create a healthier environment in which to live and thrive.
Preface: How this report is organized
Chapter 1
Introduction, presents the report's objectives, definitions and main data sources used.
Chapter 2
The scope of the problem, offers a comprehensive overview of data on fall-related injuries, hospitalizations and deaths among Canadians aged 65 and over.
Chapter 3
Risk factors for falls and fall-related injuries among seniors, provides the latest evidence regarding risks of falls from widely adopted guidelines, and it reviews recent studies on the prevention of falls. The information is organized under biological/intrinsic, behavioural, environmental and social/economic risk factors.
Chapter 4
Best practices for the prevention of falls, summarizes current guidelines and best practices for the prevention of falls and fall-related injuries with a focus on multifactorial approaches.
Chapter 5
Stepping up fall prevention in Canada, discusses national activities to reduce falls among seniors and areas for potential improvement and further collaboration.
1.0 Introduction
Unintentional injuries represent a significant public health issue for Canadians at all stages of the life course. Injury is a leading cause of hospitalization for children, young adults and seniors, and it is a major cause of disability and death in Canada Footnote 156. Injuries and associated outcomes not only harm the afflicted individuals, but also affect family, friends, care providers and the health care system. In 2004, for example, the total economic burden of injury in Canada was estimated at $19.8 billion Footnote 156. We do know that these personal and economic costs can be avoided, however, through injury prevention activities.
Falls remain the leading cause of injury-related hospitalizations among Canadian seniors Footnote 28. It is estimated that between 20% and 30% of seniors fall each year. For example, data from the Canadian Community Health Survey - Healthy Aging indicate that 20% of seniors living in the community reported a fall, with a higher prevalence among older seniors, i.e., over 80 years Footnote 162. Research suggests that falls are the direct cause of 95% of all hip fractures, leading to death in 20% of cases Footnote 78 Footnote 81 Footnote 178. Falls also appear to be a catalyst for the transition to long-term care. Research shows that over one third of seniors who are hospitalized for a fall are discharged to long-term care, which is almost double the proportion who were living in that kind of care when they fell Footnote 147. Falls can also lead to negative mental health outcomes, such as fear of falling, loss of autonomy and greater isolation, confusion, immobilization and depression. In addition to the negative physical and mental health consequences of falling, there are significant associated financial costs. In 2004, the direct costs associated with falls among seniors in Canada were estimated at over $2 billion. The cost of falls for Canadian seniors (per capita) was 3.7 times greater than that for individuals between the ages of 25 and 64 years Footnote 156.
In 2011, an estimated 5 million Canadians, or 15% of the population, were 65 years of age or older Footnote 161. This number is expected to double in the next 25 years and reach 10.47 million seniors by 2036. Given this shift towards an older demographic, the release of this report is timely, as it presents data on the rates of falls, information on risk factors, and evidence-based interventions to prevent falls among seniors.
This report is an update of the Report on Seniors' Falls in Canada Footnote 125 and provides policy makers, researchers, community programmers and practitioners with current national information to prevent falls among seniors. Specifically, it updates our knowledge of the nature and severity of falls among Canadian adults aged 65 and over, and provides a picture of changes over time. The report also re-examines risk factors for falls and fall-related injuries in older adults and reviews the effectiveness of multifactorial interventions to prevent falls.
National information is provided through analysis of the following data:
- Epidemiological evidence on seniors' falls focusing on self-reported data from Statistics Canada - Canadian Community Health Survey Footnote 159;
- Hospitalization data from the Canadian Institute for Health Information - Hospital Morbidity Database Footnote 31; and
- Mortality data from Statistics Canada - Canadian Vital Statistics Footnote 160.
The following content is also included in the report:
- Information on multifaceted risks for falls among seniors;
- Evidence-based best practices for the prevention of falls and injury from falls; and
- Considerations that will have an impact on national fall prevention efforts.
1.1 Seniors' falls – Definitions
All statistics and information reported in this document refer to Canadians aged 65 and over unless otherwise stated. Terms such as senior, older adult and older person all refer to this age group.
A fall is often defined as a sudden and unintentional change in position resulting in an individual landing at a lower level such as on an object, the floor, or the ground, with or without injury Footnote 170. Different data sets define falls in various ways. These are described under each section.
Age standardization for this report was calculated by proportionally adjusting annual figures to the standard 1991 Canadian population aged 65 and over.
2.0 The scope of the problem
A comprehensive description of the magnitude and nature of seniors' falls and related injuries in Canada was derived from an analysis of three data sources:
- Epidemiological evidence on falls highlighting seniors' self-reported data from the Canadian Community Health Survey (CCHS) Footnote 159;
- Hospitalization data from the Canadian Institute for Health Information (CIHI) Hospital Morbidity Database (HMDB) for all seniors, then more specifically for seniors in residential care Footnote 31; and
- Mortality data from Statistics Canada's Canadian Vital Statistics Footnote 160.
The reader should be cautious when comparing data on falls among data sources as each data source analyzed for this report has its own definition of what constitutes a fall. These definitions are influenced by the nature of the data collection methods, for example, self-report versus hospital records. It is equally important to recognize the limitations associated with any data source, including the inherent potential for data errors and the impact of changes in the International Classification of Diseases on hospitalization and mortality data.
2.1 What seniors report about falls and related injuries
This section provides national estimates based on data from the CCHS from seniors aged 65 and over who indicated that they had had at least one injury in the previous 12 months that was both serious enough to limit normal activities the day after the injury occurred and was the result of a fall. Included are estimates of the number of cases and rates of injurious falls, types of injury, types of activity and places where treatment was sought. Where sample size permitted, results are presented by sex and age group.
The Canadian Community Health Survey Footnote 159 Footnote 162
The CCHS is a cross-sectional survey that collects information about health status, health care utilization and health determinants, representing approximately 98% of the population aged 12 and older. The CCHS collects data from household residents in Canada's provinces and territories. People living on Indian reserves or Crown lands, residents of institutions, full-time members of the Canadian Armed Forces and residents of certain remote regions are excluded. Coverage is lower in the north where the population is more likely to be living in remote regions not captured by the CCHS Footnote 159. The exclusion of institutional residents should be noted as particularly pertinent for this analysis. Data are collected from a complex, multi-stage stratified sample of approximately 65,000 individuals annually from across Canada (Statistics Canada, 2010)Footnote a . The data for this report are based on three cycles of CCHS data - cycle 2.1 (2003), cycle 3.1 (2005) and data for the period 2009/2010Footnote b .
2.1.1 Definitions and data
With regard to the CCHS data, a fall is "defined" by the respondents when they indicate, first, that they suffered an injury in the previous year serious enough to limit their normal activities and, second, that the injury was the result of a fall.
The CCHS collects data about only the most serious injury resulting from a fall in the previous 12 months, thus information about individuals who experienced more than one fall or who fell but were not injured is not captured.
The term cases referred to in this section refers to the number of persons reporting a fall-related injury in the previous 12 months. The term rate refers to the number of persons who reported a fall-related injury in the previous 12 months per 1,000 persons in the population (of those aged 65 and over).
2.1.2 Findings
Of the total CCHS sample aged 65 and over, Table 1 compares those who did not report an injury related to a fall in the previous 12 months with those who did report such an injury. Presented in these data are population estimates, the proportion of respondents within a series of key demographic variables and the 95% confidence interval (CI) for the proportionsFootnote c .
In 2009/2010, 256,011 older Canadians reported experiencing a fall-related injury. In comparison to those without a fall-related injury, they were more likely to be female (63.6% compared with 54.3%) and less likely to be aged 74 or younger (47.5% compared with 57.7%). There were also statistically significant differences found by marital status. Among those with a fall-related injury, 55.9% were married, compared with 63.6% without a fall-related injury.
Additionally, 31.0% of those with a fall-related injury were widowed, compared with 23.6% of those without a fall-related injury. Difference in marital status is likely tied to differences in age, in that older individuals were more likely to be widowed. Education was only significantly different among those with less than secondary school graduation. A total of 30.0% of those with an injury related to a fall were in this education group, compared with 34.1% of those without an injury related to a fall. There were no differences observed in the proportions by household income group.
Data from 2003 and 2005 are presented in Appendix A.
| Without a Fall-related Injury | With a Fall-related Injury | |||||||
|---|---|---|---|---|---|---|---|---|
| Pop. Estimate Footnote 1.1 | % | 95% Confidence Interval | Pop. Estimate | % | 95% Confidence Interval | |||
| Lower | Upper Footnote 1.3 | Lower | Upper Footnote 1.2Footnote 1.3 | |||||
| Sex | ||||||||
| Male | 1,918,788 | 45.7 | 45.5 | 45.9 | 93,090 | 36.4 | 33.0 | 39.8* |
| Female | 2,279,216 | 54.3 | 54.1 | 54.5 | 162,921 | 63.6 | 60.2 | 67.0* |
| Age | ||||||||
| 65-69 | 1,415,712 | 33.7 | 32.8 | 34.6 | 74,185 | 29.0 | 25.5 | 32.5* |
| 70-74 | 1,005,525 | 24.0 | 23.1 | 24.8 | 47,348 | 18.5 | 16.0 | 21.0* |
| 75-79 | 841,906 | 20.1 | 19.4 | 20.7 | 55,126 | 21.5 | 18.1 | 25.0 |
| 80-84 | 570,275 | 13.6 | 12.9 | 14.2 | 36,653 | 14.3 | 11.7 | 16.9 |
| 85-89 | 273,249 | 6.5 | 6.1 | 6.9 | 32,484 | 12.7 | 9.4 | 16.0* |
| 90+ | 91,336 | 2.2 | 1.9 | 2.5 | 10,215 | 4.0 | 2.4 | 5.6E |
| Marital Status | ||||||||
| Married | 2,670,783 | 63.6 | 62.7 | 64.6 | 143,006 | 55.9 | 52.9 | 58.8* |
| Widowed | 989,597 | 23.6 | 22.9 | 24.3 | 79,415 | 31.0 | 28.3 | 33.7* |
| Separated/Divorced | 342,082 | 8.1 | 7.7 | 8.6 | 23,245 | 9.1 | 7.0 | 11.2 |
| Single, never-married | 185,020 | 4.4 | 4.0 | 4.8 | 10,344 | 4.0 | 2.9 | 5.2 |
| Not stated Footnote 1.4 | 10,521 | 0.3 | 0.1 | 0.4E | 0 | 0.0 | 0.0 | 0.0 |
| Education Footnote 1.5 | ||||||||
| Less than secondary school graduation | 1,433,432 | 34.1 | 33.2 | 35.1 | 76,714 | 30.0 | 26.7 | 33.2* |
| Secondary school graduation | 618,242 | 14.7 | 14.2 | 15.3 | 41,275 | 16.1 | 13.1 | 19.2 |
| Some post-secondary | 227,552 | 5.4 | 5.0 | 5.8 | 15,901 | 6.2 | 4.1 | 8.3E |
| Post-secondary graduation | 1,763,707 | 42.0 | 41.0 | 43.0 | 112,140 | 43.8 | 39.8 | 47.8 |
| Not stated | 155,070 | 3.7 | 3.3 | 4.1 | 9,981 | 3.9 | 2.3 | 5.5E |
| Household Income Footnote 1.6 | ||||||||
| Less than $15,000 | 203,691 | 4.9 | 4.4 | 5.3 | 16,958 | 6.6 | 5.3 | 7.9 |
| $15,000-$29,999 | 921,973 | 22.0 | 21.3 | 22.6 | 56,344 | 22.0 | 18.8 | 25.2 |
| $30,000-$49,999 | 949,721 | 22.6 | 21.8 | 23.5 | 52,055 | 20.3 | 16.8 | 23.9 |
| $50,000-$79,999 | 694,477 | 16.5 | 15.8 | 17.3 | 44,556 | 17.4 | 13.8 | 21.0 |
| $80,000 or more | 513,709 | 12.2 | 11.4 | 13.0 | 34,593 | 13.5 | 10.1 | 16.9 |
| Not stated | 914,432 | 21.8 | 21.1 | 22.5 | 51,505 | 20.1 | 17.1 | 23.1 |
Figure 1 presents estimates of cases and rates of fall-related injuries based on self-reports from CCHS samples for 2003, 2005 and 2009/2010. The data show that in 2003, there were 178,755 older Canadians who reported an injury related to a fall, which translates to a rate of 47.2 per 1,000 population (95% CI 43.0 to 51.5). In 2009/2010, this number had increased significantly to 256,011 with a rate of 57.5 per 1,000 (95% CI 52.5 to 62.4). This represents a 43% increase in the number of individuals who reported a fall-related injury from 2003 to 2009/2010.
Figure 1: Estimated cases and rates (per 1,000) of injuries resulting from a fall, age 65+, Canada, 2003, 2005, 2009/2010 (95% CIs shown) Footnote 159
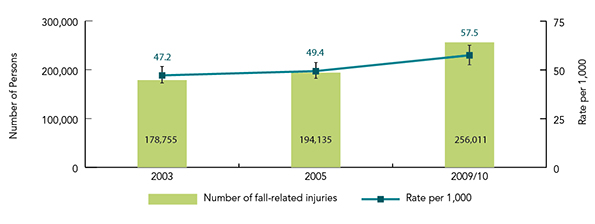
Text Equivalent - Figure 1
Figure 1 is a bar graph illustrating estimated cases and rates, per 1,000, of injuries resulting from a fall for Canadians 65 years of age and over for 2003, 2005 and 2009/2010. 95% Confidence Intervals are indicated.
| Year | Number of fall-related injuries | Rate per 1,000 | Lower Confidence Interval | Upper Confidence Interval |
|---|---|---|---|---|
| 2003 | 178,755 | 47.2 | 43.0 | 51.5 |
| 2005 | 194,135 | 49.4 | 45.3 | 53.5 |
| 2009/2010 | 256,011 | 57.5 | 52.5 | 62.4 |
Figure 2 shows rates of self-reported injuries related to a fall by sex and survey year. The data indicated significantly higher rates among females than males for each survey year. A significant increase in the rate of fall-related injuries among older males was observed in 2009/2010 in comparison to previous years.
Figure 2: Estimated rates (per 1,000) of injuries resulting from a fall by sex, age 65+, Canada, 2003, 2005, 2009/10 (95% CIs shown) Footnote 159

Text Equivalent - Figure 2
Figure 2 is a bar graph of estimated rates per 1,000 of injuries resulting from a fall, by sex for Canadians 65 years of age and over for the years 2003, 2005 and 2009/2010. 95% confidence intervals are indicated.
| Year | Male Rate | Lower Confidence Interval | Upper Confidence Interval | Female Rate | Lower Confidence Interval | Upper Confidence Interval |
|---|---|---|---|---|---|---|
| 2003 | 33.4 | 28.9 | 37.9 | 58.0 | 51.9 | 64.2 |
| 2005 | 34.9 | 30.4 | 39.5 | 61.0 | 55.0 | 67.0 |
| 2009/2010 | 46.3 | 40.3 | 52.3 | 66.7 | 60.1 | 73.3 |
Figure 3 shows the general trend of increasing rates of self-reported injuries due to falls with age. In 2009/10, the rates among Canadians aged 85 to 89 and 90 and older were significantly higher than among Canadians aged 65 to 69.
Figure 3: Estimated rates (per 1,000) of injuries resulting from a fall by age group, age 65+, Canada, 2009/10 (95% CIs shown) Footnote 159
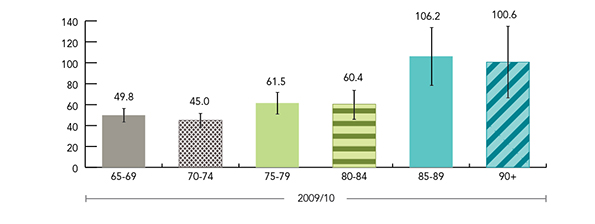
Text Equivalent - Figure 3
Figure 3 is a bar graph indicating estimated rates per 1,000 of self-reported injuries due to falls broken down by age group for Canadians 65 years of age and older over 2009/2010. 95% confidence intervals are indicated.
| Age Range | 2009/10 fall rate | Lower Confidence Intervals | Upper Confidence Intervals |
|---|---|---|---|
| 65 to 69 | 49.8 | 43.1 | 56.5 |
| 70 to 74 | 45.0 | 38.1 | 51.9 |
| 75 to 79 | 61.5 | 50.9 | 72.0 |
| 80 to 84 | 60.4 | 47.0 | 73.8 |
| 85 to 89 | 106.2 | 78.5 | 134.0 |
| 90 and older | 100.6 | 66.01 | 135.2 |
Figure 4 shows that, of the age groups sampled by the CCHS, the rates of both self-reported fall-related injuries and injuries due to any cause were highest among those 12 to 24 years of age within each CCHS survey cycle. Rates of fall-related injuries are shown to decrease in midlife and then increase in older adulthood. Specifically, in 2009/2010, rates of self-reported fall-related injuries were 105.2 per 1,000 among those 12 to 24 years, decreased to 46.8 per 1,000 among those 25 to 64 years, and subsequently increased to 57.5 per 1,000 among those 65 aged years or older. The data indicate that fall-related injuries account for a greater proportion of all injuries among seniors in comparison to all other examined age groups.
Figure 4: Estimated rates of injuries from all causes vs. injuries due to a fall by age group, age 12+, Canada, 2003, 2005, 2009/10 (95% CIs shown) Footnote 159
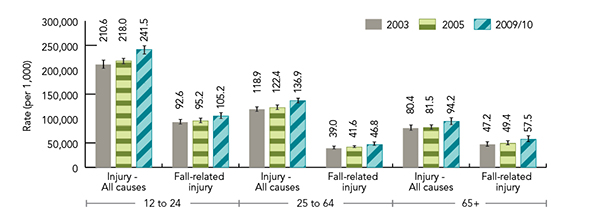
Text Equivalent - Figure 4
Figure 4 is a bar graph of estimated rates of injuries resulting from all causes versus injuries resulting from a fall for Canadians 12 to 24, 25 to 64 and those 65 years of age and over. The graph presents data from 2003, 2005 and 2009/2010. 95% confidence intervals are indicated.
| Year | 12 to 24 years of age, injuries from all causes | 12 to 24 years of age with fall-related injury | 25 to 64 years of age, injuries from all causes | 25 to 64 years of age with fall-related injury | 65 years of age and over, injuries from all causes | 65 years of age and over with fall-related injury |
|---|---|---|---|---|---|---|
| 2003 | 210.6 | 92.6 | 118.9 | 39.0 | 80.4 | 47.2 |
| 2005 | 218.0 | 95.2 | 122.4 | 41.6 | 81.5 | 49.4 |
| 2009/2010 | 241.5 | 105.2 | 136.9 | 46.8 | 94.2 | 57.5 |
Falls among seniors compared with those among children and youth
Unintentional fall-related injuries among children and youth are associated with risk factors that are different from those that are present in falls among seniors. Among children, injurious falls may result from falls from bunk beds or a play structure Footnote 168. Among adolescents, alcohol and risk-taking behaviour are often implicated in the occurrence of falls Footnote 155.
Figure 5 shows that in 2009/2010 walking on a surface other than snow and ice was stated most often as the activity involved in self-reported injuries related to a fall among those aged 65 and older. This type of activity was cited in 45% of injuries relating to falls and represented 115,569 individuals (95% CI 103,164 to 127,974). Walking on snow or ice was the second most frequently cited activity in all survey years followed by going up or down stairs or steps.
Figure 5: Activity associated with fall-related injury, age 65+, Canada, 2009/10 Footnote 159
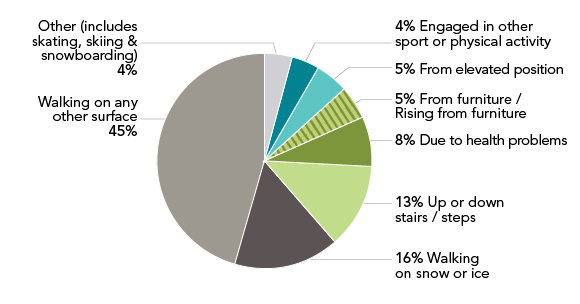
Text Equivalent - Figure 5
Figure 5 is a pie chart diagram illustrating activity associated with fall-related injury among Canadians 65 years of age and over in 2009/2010.
45% resulted from walking on a surface other than snow and ice
16% resulted from walking on snow or ice
13% resulted from walking up or down stairs or steps
8% resulted from health problems
5% resulted from furniture or rising from furniture
5% resulted from an elevated position
4% resulted from engagement of other sport or physical activity, and finally
4% resulted from other activity including skating, skiing & snowboarding
Figure 6 presents the part of the body that was injured as reported by seniors who experienced an injury as a result of a fall. The majority of injuries were to the shoulder or upper arm (17%) followed by the knee or lower leg (15%). The ankle and foot were cited third most frequently (10%).
Figure 6: Body part affected by fall-related injury, age 65+, Canada, 2009/10 Footnote 159
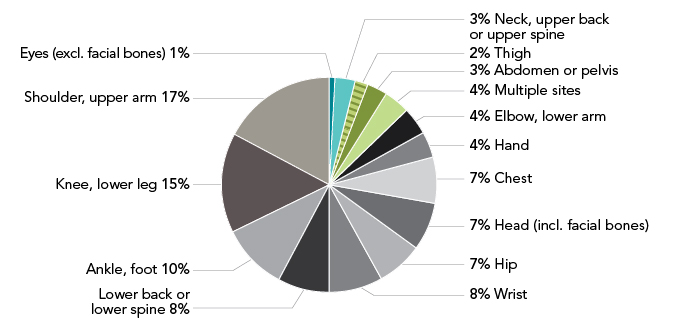
Text Equivalent - Figure 6
Figure 6 is a pie chart indicating the body part affected by fall-related injury for Canadians 65 years of age and over in 2009/2010:
17% were to the shoulder or upper arm
15% were to the knee or lower leg
10% were to the ankle or foot
8% were to the lower back or lower spine
8% were to the wrist
7% were to the hip
7% were to the head, including facial bones
7% were to the chest
4% were to the hand
4% were to the elbow or lower arm
4% were to multiple sites
3% were to the abdomen or pelvis
3% were to the neck, upper back or upper spine
2% were to the thigh, and finally
1% were to eyes, excluding facial bones
Figure 7 shows that the majority of injuries resulting from a fall were broken or fractured bones (35%) followed by sprains or strains (30%) and scrapes, bruises or blisters (19%). This finding highlights the importance of bone health in preventing fall-related injuries among seniors.
Figure 7: Type of fall-related injury, age 65+, Canada 2009/10 Footnote 159
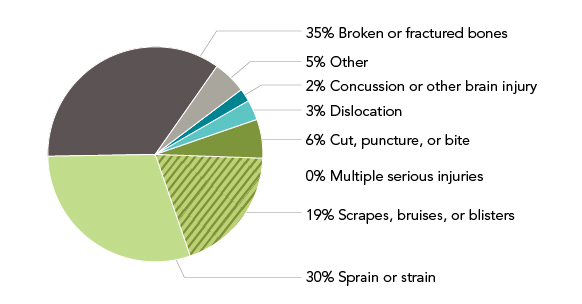
Text Equivalent - Figure 7
Figure 7 is a pie chart depicting types of reported fall-related injuries in 2009/2010 among Canadians 65 years of age and over:
35% resulted in broken or fractured bones
30% resulted in sprain or strain
19% resulted in scrapes, bruises, or blisters
6% resulted in a cut, puncture or bite
5% resulted in other types of injury
3% resulted in dislocation
2% resulted in concussion or other brain injury, and finally
0% resulted in multiple serious injuries
Falls as a cause of traumatic brain injury (TBI)
Falls are the leading cause of head injury hospitalizations among children and youth as well as among adults over 60 years Footnote 29. Head impact is common in falls, particularly in forward falls Footnote 142. Resultant head injuries and TBIs are important outcomes of falls among older adults that contribute to morbidity Footnote 140.
Figure 8 indicates that individuals aged 65 or older who reported that they sought medical treatment within 48 hours after an injury related to a fall were most likely to seek treatment in an emergency room (67%). This was followed in all survey years by those who sought treatment in a doctor's office (16%) and a clinic (7%).
Figure 8: Type of treatment sought for fall-related injury, age 65+, Canada, 2009/10 Footnote 159
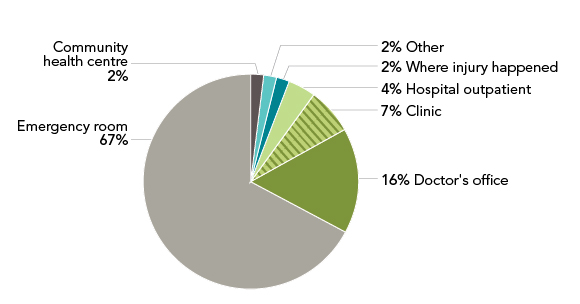
Text Equivalent - Figure 8
Figure 8 is a pie chart that shows the location of treatment for fall-related injuries among Canadians 65 years of age and over in 2009/2010:
67% sought treatment in an emergency room
16% sought treatment at a doctor's office
7% sought treatment at a clinic
4% sought treatment as hospital outpatients
2% sought treatment at the site where injury occurred
2% sought treatment at a community health centre, and finally
2% sought treatment through other means
2.1.3 Summary
In 2009/2010, 256,011 Canadians aged 65 and older reported a fall-related injury, translating to a rate of 57.5 per 1,000. Compared with those who did not experience a fall-related injury, they were more likely to be female, more likely to be older (i.e., 85+) and less likely to be married. Comparing data from several years shows a trend towards increases in the number and rates of older adults experiencing an injury as a result of a fall. While females continue to report higher rates of fall-related injuries than males, when multiple survey years are compared there appears to be a trend towards increasing rates among males. Forty-six percent of older Canadians who sustained an injury due to a fall reported that they were walking when the injury occurred, signalling the interaction with the environment, as discussed in later chapters. The majority of these injuries were broken or fractured bones. This finding highlights the importance of promoting bone health in preventing fall-related injuries among seniors. With regard to seeking medical treatment, 67% of respondents sought treatment at an emergency room, highlighting the impact of falls on the health care system.
2.2 What hospitalization data tell us about seniors' falls
The analyses provided in this section are based on the HMDB, at CIHI. They include fall-related hospitalization cases and rates, length of hospital stay, injury type, place of occurrence of fall, and differences by age group and sex for seniors aged 65 and over, for the fiscal years 2006/2007 through 2010/2011 (i.e., five years)Footnote d .
Hospital Morbidity Database
The HMDB is a national dataset that houses administrative, clinical and demographic information on inpatient separations from acute care hospitals. Discharge data are received from all acute care facilities across Canada. Responsibility for the HMDB was taken on by CIHI from Statistics Canada in 1995 during a transfer of several databasesFootnote 31.
2.2.1 Definitions and data
International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10)
The ICD-10 refers to an international standard, developed by the World Health Organization, for reporting on clinical diagnoses. ICD-10-CA is an enhanced version of ICD-10 developed by CIHI for morbidity classification in CanadaFootnote 30.
In the succeeding analyses, fall-related hospitalizations were defined as hospitalizations in acute care hospitals in Canada involving an unintentional fall as defined by select ICD-10-CA codes. The variable was calculated by examining all diagnosis codes in the discharge records associated with a given episode of care. External Cause of Injury codes used to identify unintentional falls were ICD-10-CA codes W00-W19 Footnote 30.
This section uses the HMDB data pertaining to acute care hospitalizations for falls among persons 65 years and over in Canada. Fall-related hospitalizations for a specific population are a good estimate of all falls resulting in serious injury for that population. However, this data source does not capture information on injurious falls of lesser severity, which may be treated at hospital emergency departments or physicians' offices, or falls for which medical treatment was not sought.
The Report on Seniors' Falls in CanadaFootnote 125 presented analyses using discharge counts in which each hospital discharge is counted as a case, even those representing transfers for the same fall injury. For this report, the methodology has been updated to use episodes of care in which all discharges, including transfers related to a given injury, are counted as a single case. This distinction is important as it can affect the reported number of cases, the length of stay and the resource utilization associated with falls. Specifically, the rates of falls calculated using discharge counts tend to be higher than the rates calculated using episodes of care. This can lead to overestimation of the demand for care for those being discharged from hospital and underestimation of the resource utilization involved in treating falls in acute care hospitals (i.e., length of stay). Thus, shifting from discharge counts to episode of care provides a more comprehensive view of the extent of acute care involved in treating fall-related hospitalizations. This report adopted a linkage methodology that has been employed in previous studies using administrative data to explore falls in seniors Footnote 27 Footnote 146 Footnote 147.
2.2.2 Findings
Figure 9 shows the trend in fall-related hospital cases and rates for those aged 65 and over in Canada during 2006/2007 through 2010/2011. Overall, the total number of fall-related hospitalizations increased from 67,899 in 2006/2007 to 78,330 in 2010/2011. This represents a 15% increase in the number of individuals who were hospitalized as a result of falls during that period. Despite this observed increase, the crude rate of fall-related hospitalizations remained relatively constant over the five-year period, ranging from 15.6 per 1,000 population in 2006/2007 to 16.1 per 1,000 population in 2010/2011. Therefore, the number of fall-related hospitalizations appears to have increased because of increased numbers of older adults in the Canadian population.
Figure 9: Number and rates of fall-related hospitalizations, age 65+, Canada, by fiscal year (crude and age standardized) Footnote 31
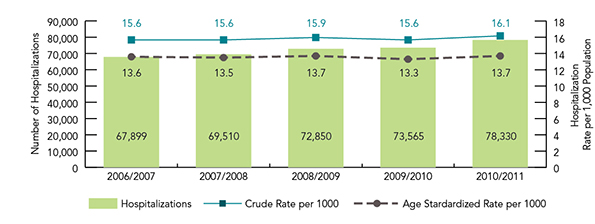
Text Equivalent - Figure 9
Figure 9 is a bar graph which indicates fall-related hospitalizations and rates for Canadians 65 years of age and over for the period spanning fiscal year 2006/2007 to 2010/2011. The data is depicted at a crude rate per 1000 and an age-standardized rate per 1,000.
| Fiscal Year | Hospitalizations | Age Standardized Rate per 1,000 | Crude Rate per 1,000 |
|---|---|---|---|
| 2006/2007 | 67,899 | 13.6 | 15.6 |
| 2007/2008 | 69,510 | 13.5 | 15.6 |
| 2008/2009 | 72,850 | 13.7 | 15.9 |
| 2009/2010 | 73,565 | 13.3 | 15.6 |
| 2010/2011 | 78,330 | 13.7 | 16.1 |
Figure 10 shows fall-related hospitalizations as a percent of all injury hospitalizations for seniors age 65 and over. Each year, fall-related hospitalizations account for about 85% of injury hospitalizations for seniors.
Figure 10: Fall-related hospitalizations as a percent of all injury-related hospitalizations, age 65+, Canada, by fiscal year Footnote 31
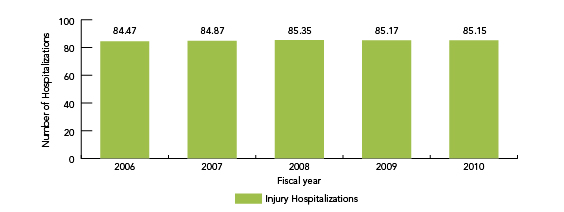
Text Equivalent - Figure 10
Figure 10 is a bar graph that depicts fall-related hospitalizations as a percent of all injury-related hospitalizations by fiscal year, for Canadians 65 years of age and over:
| Fiscal Year | % of Fall-related Hospitalizations |
|---|---|
| 2006/2007 | 84.5 |
| 2007/2008 | 84.9 |
| 2008/2009 | 85.4 |
| 2009/2010 | 85.2 |
| 2010/2011 | 85.1 |
Figure 11 shows that men and women both had increasing rates of fall-related hospitalization with age but that females appeared to have an increased rate of falls relative to males as age increases. As discussed in Chapter 3, females are at greater risk of osteoporosis, which partly accounts for the increase in the risk of fracture as a consequence of a fall and therefore the impact on hospitalizations.
Figure 11: Fall-related hospitalization rates, by sex and age group, age 65+, Canada, fiscal year 2010/11 Footnote 31
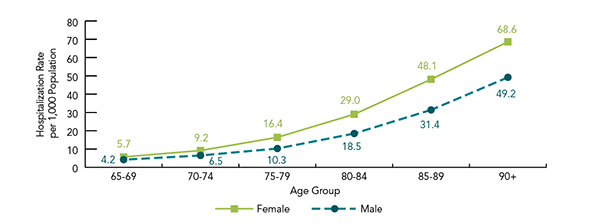
Text Equivalent - Figure 11
Figure 11 is a line graph that depicts fall-related hospitalization rates by sex and age group for Canadians 65 years of age and over in fiscal year 2010/2011:
| Age Group | Female fall-related hospitalization | Male fall-related hospitalization |
|---|---|---|
| 65-69 | 5.7 | 4.2 |
| 70-74 | 9.2 | 6.5 |
| 75-79 | 16.4 | 10.3 |
| 80-84 | 29.0 | 18.5 |
| 85-89 | 48.1 | 31.4 |
| 90 and over | 68.6 | 49.2 |
Figure 12 shows that as age increased so did the length of hospital stay for fall-related events. The longest stays for fall-related hospitalizations tended to be for those aged 90 years and older, and these increased slightly from 22 days in 2006/07 to 24 days in 2010/11. The data also show little variation over the five years studied for all age groups.
Figure 12: Average length of stay (LOS) of fall-related hospitalizations, by age group, Canada, by fiscal year Footnote 31
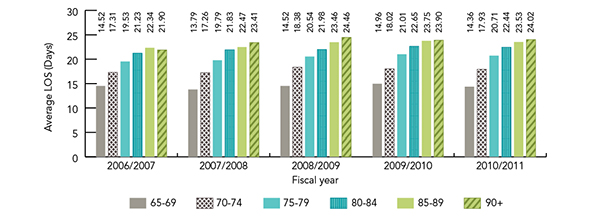
Text Equivalent - Figure 12
Figure 12 is a bar graph indicating the average length of stay per case for fall-related hospitalizations. The information is presented by age group for Canadians 65 years of age and over and by fiscal years 2006/2007, 2007/2008, 2008/2009, 2009/2010, 2010/2011.
| Length of stay by age group (in years) | 2006/2007 | 2007/2008 | 2008/2009 | 2009/2010 | 2010/2011 |
|---|---|---|---|---|---|
| 65-69 | 14.52 days | 13.79 days | 14.52 days | 14.96 days | 14.36 days |
| 70-74 | 17.31 days | 17.26 days | 18.38 days | 18.02 days | 17.93 days |
| 75-79 | 19.53 days | 19.79 days | 20.54 days | 21.01 days | 20.71 days |
| 80-84 | 21.23 days | 21.83 days | 21.98 days | 22.65 days | 22.44 days |
| 85-89 | 22.34 days | 22.47 days | 23.46 days | 23.75 days | 23.53 days |
| 90 and over | 21.90 days | 23.41 days | 24.46 days | 23.90 days | 24.02 days |
Long hospital stays
This analysis of average length of stay shows that seniors who fell and were admitted to hospital spent an average of approximately three weeks (i.e., 22 days) in hospital. To put this into perspective, in 2010/2011 seniors admitted for any cause spent an average of 12 days in hospital. Therefore, the average length of stay resulting from falls among seniors is ten days longer than among seniors admitted for any cause, highlighting the disproportionate health care costs of fall-related injuries in comparison to other causes of hospitalization among seniors.
Figure 13 illustrates that in the period from 2006/07 to 2010/11, the average length of hospital stay for a fall-related hospitalization was about nine days longer than the average length of stay for all causes of hospitalization for seniors aged 65 and over. The average length of stay for both falls and all causes showed little change over the study period.
Figure 13: Average length of stay (LOS) of fall-related hospitalizations (FRH) and all-causes hospitalizations, age 65+, Canada, by fiscal year Footnote 31
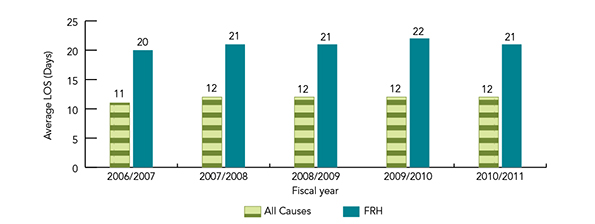
Text Equivalent - Figure 13
Figure 13 is a bar graph comparing average length of stay for fall-related hospitalizations to hospitalizations for all other causes for Canadians 65 years of age and over. The data covers fiscal years 2006/2007, 2007/2008, 2008/2009, 2009/2010, 2010/2011.
| Fiscal Year | All Cause Hospital Stay | Fall-related Hospital Stay |
|---|---|---|
| 2006/2007 | 11 days | 20 days |
| 2007/2008 | 12 days | 21 days |
| 2008/2009 | 12 days | 21 days |
| 2009/2010 | 12 days | 22 days |
| 2010/2011 | 12 days | 21 days |
Figure 14 shows the number and percentage of fall-related hospitalizations associated with a hip fracture for seniors aged 65 and over. The data indicate that, in each year, approximately 35% of fall-related hospitalizations for seniors aged 65 and over involved a hip fracture. Hip fractures related to a fall accounted for 95% of all hip fractures among seniors aged 65 and over Footnote 146.
Figure 14: Number and percentage of fall-related hospitalizations (FRH) associated with hip fracture, age 65+, Canada, by fiscal year Footnote 31
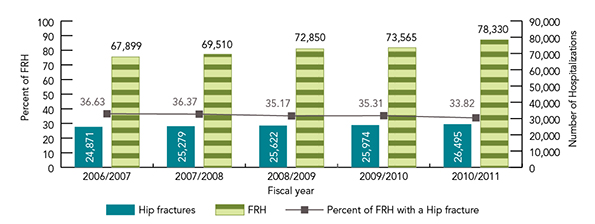
Text Equivalent - Figure 14
Figure 14 provides information on the number and percentage of fall-related hospitalizations associated with a hip fracture among Canadians 65 years of age and over, presented by fiscal year.
| Fiscal Year | Number of fall-related hospitalizations | Number of hip fractures | Percentage of fall-related hospitalizations with a hip fracture |
|---|---|---|---|
| 2006/2007 | 67,899 | 24,871 | 36.6% |
| 2007/2008 | 69,510 | 25,279 | 36.4% |
| 2008/2009 | 72,850 | 25,622 | 35.1% |
| 2009/2010 | 73,565 | 25,974 | 35.3% |
| 2010/2011 | 78,330 | 26,495 | 33.8% |
Figure 15 shows the place of occurrence of the fall for fall-related hospitalizations among seniors aged 65 and over. The results indicate that half of such hospitalizations stemmed from a fall occurring at home. Falls that occurred in residential care accounted for 17% of all fall-related hospitalizations.
Figure 15: Fall-related hospitalizations, by place of occurrence of fall, age 65+, Canada, pooled across all fiscal years Footnote 31
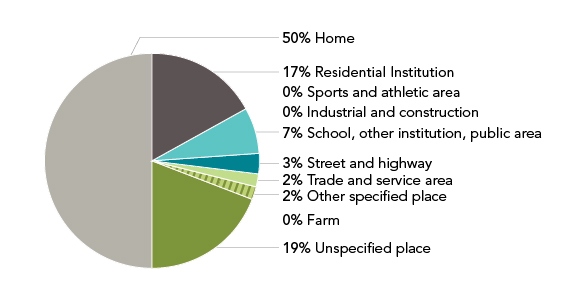
Text Equivalent - Figure 15
Figure 15 is a pie chart depicting the location where a fall occurred resulting in hospitalization. The data covers the period from fiscal year 2006/2007 to 2010/2011 for Canadians 65 years of age and over.
50% occurred at home
19% occurred in an unspecified place
17% occurred in a residential institution
7% occurred in school, other institution or public area
3% occurred on a street or highway
2% occurred in a trade and service area
2% occurred at other specified place
0% occurred on a farm
0% occurred at an industrial and construction setting, and finally
0% occurred at a sports and athletic area
2.2.3 Summary
Canadian fall-related hospitalization data for all seniors were analyzed for the years 2006/2007 through 2010/2011. The crude rates of hospitalization among seniors remained relatively constant over the five years analyzed. The rates among females were higher than among males, a difference that increased with age. Across data collection periods, the average length of stay in hospitals remained reasonably constant year over year and was greatest among seniors 90 years of age and older. Seniors who were hospitalized because of a fall spent approximately three weeks in hospital, three times more than the average hospital stay in Canada among all ages. Half of the falls that led to hospitalizations occurred in the home.
2.3 What hospitalization data tell us about falls among seniors in residential care
The information in this section is based on the data from the HMDB pertaining to acute care hospitalizations for falls among adults aged 65 years and older living in residential care facilities in Canada (for information about the HMDB, see section 2.2).
The analyses provided in this section include fall-related hospitalization cases and rates, length of hospital stay, injury type, place of occurrence of fall, and differences by age group and sex for seniors aged 65 and over, for the fiscal years 2006/2007 through 2010/2011 (i.e., five years).
2.3.1 Definitions and data
The definitions and data cautions stated in section 2.2.1 also apply to this section, which uses the same data source, further narrowed by selection for residential care. Residential care encompasses a range of living options for people, primarily seniors, with different support needs and is also known as long-term care, nursing home or complex care Footnote 31. The episode of care methodology was also used for the analyses that follow and is also described in section 2.2.1 of this report.
Because the population living in residential care versus at home is unclear, rates (crude and standardized) could not be calculated.
Adults living in residential institutions tend to have more complex health challenges, such as advanced dementia, multiple chronic health conditions and limited mobility. These characteristics put this population at greater risk of falling and sustaining a fall-related injury Footnote 175.
Residential care
This section includes hospitalization data for persons for whom "place of occurrence" of the fall was designated as "Residential Institution," and the place they were "transferred from" to hospital was "Chronic Care Facility," "Nursing Home" or "Home for the Aged". Only residents of care facilities who were aged 65 years and over were included.
2.3.2 Findings
Figure 16 shows the number of hospitalizations due to falls for seniors living in residential care versus those living at home. In 2006, there were 10,805 fall-related hospitalizations among seniors living in residential care as compared with 57,094 fall-related hospitalizations among community-dwelling seniors. In 2010, these values increased to 12,884 (increase of 19%) and 65,446, respectively (increase of 15%).
Figure 16: Fall-related hospitalizations for residential care vs. home, age 65+, Canada, by fiscal year Footnote 31
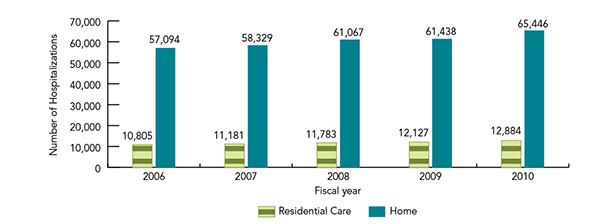
Text Equivalent - Figure 16
Figure 16 is a bar graph depicting the number of fall-related hospitalizations in residential care versus those living at home among Canadians 65 years of age and over, by fiscal year.
| Fiscal Year | Fall-related hospitalizations in residential care | Fall-related hospitalizations for those living at home |
|---|---|---|
| 2006 | 10,805 | 57,094 |
| 2007 | 11,181 | 58,329 |
| 2008 | 11,783 | 61,067 |
| 2009 | 12,127 | 61,438 |
| 2010 | 12,884 | 65,446 |
Figure 17 indicates that, in general, the number of fall-related hospitalizations increased with age. Fall-related hospitalizations of those living at home and in residential care were more frequent among women than men, and this difference increased with age.
Figure 17: Fall-related hospitalizations for residential care vs. home, by sex and age group, age 65+, Canada, fiscal year 2010/11 Footnote 31

Text Equivalent - Figure 17
Figure 17 is a line graph comparing fall-related hospitalizations for Canadians 65 years of age and over in residential care settings versus home care settings for fiscal year 2010/2011. The data is broken down by age group and gender.
| Age Group | Female residential fall-related hospitalizations | Male residential fall-related hospitalizations | Female home fall-related hospitalizations | Male home fall-related hospitalizations |
|---|---|---|---|---|
| 65-69 | 169 | 111 | 4,218 | 2,926 |
| 70-74 | 311 | 203 | 5,115 | 3,197 |
| 75-79 | 823 | 384 | 7,384 | 3,874 |
| 80-84 | 1,844 | 697 | 9,947 | 4,626 |
| 85-89 | 3,038 | 867 | 10,361 | 3,953 |
| 90 and over | 3,666 | 771 | 7,561 | 2,284 |
Sex differences in the older adult population
Throughout this report, population-level data on the frequency of falls, fall-related hospitalizations and deaths due to falls among older Canadians are presented. A key consideration in interpreting these data is that the proportion of females in the population in comparison to males increases with age. Thus, what might seem to be an increase in the frequency of falls among females relative to males may actually be a result of a difference in the population structure. When appropriate, sex-specific rates have been presented to help clarify these effects.
Figure 18 shows that for those living in residential care, the average length of stay for fall-related hospitalizations remained relatively constant with age. This is in contrast to those at home, whose average length of stay for fall-related hospitalizations increased with age. This difference may reflect delays in arranging community or other support services for home-based seniors after discharge Footnote 147.
Figure 18: Fall-related hospitalizations for residential care vs. home, average length of stay by age group, Canada, 2010/2011 Footnote 31

Text Equivalent - Figure 18
Figure 18 is a bar graph depicting length of stay for fall-related hospitalizations for Canadians 65 years of age and over living in residential care compared to those living at home in fiscal year 2010/2011. The data is broken down by age group.
| Age Group | Average length of fall-related hospitalization stay for residential-care dwelling seniors | Average length of fall-related hospitalization stay for home-dwelling seniors |
|---|---|---|
| 65-69 | 16.2 days | 14.3 days |
| 70-74 | 22.3 days | 17.7 days |
| 75-79 | 19.4 days | 20.9 days |
| 80-84 | 18.6 days | 23.1 days |
| 85-90 | 18.7 days | 24.8 days |
| 90 and over | 18.5 days | 26.5 days |
Figure 19 indicates that fall-related hospitalizations among patients living in residential care were associated with more hip fractures (59%) than such hospitalizations among seniors not living in residential care (32%).
Figure 19: Percentage of fall-related hospitalizations (FRH) associated with hip fracture, residential care vs. home, age 65+, Canada, 2010/2011 Footnote 31

Text Equivalent - Figure 19
Figure 19 is a bar graph indicating that, of Canadians 65 years of age and over in 2010/2011, seniors in residential care account for 58.64% of fall-related hospitalizations associated with hip fracture versus 32.46% of those living at home.
2.3.3 Summary
Between 2006 and 2010, fall-related hospitalizations among seniors living in residential care increased by approximately 19% to 12,884 cases. In general, fall-related hospitalizations increased with age and were more common among females than males. While longer hospital stays were associated with increased age among those living in the community, length of stay in hospital for those living in residential care appeared relatively constant across older age groups. This difference may reflect delays in arranging community or other support services for home-based seniors after discharge Footnote 147. Hospitalizations for hip fractures were more common among residents of residential care than among seniors living at home, possibly because of the increased number of comorbidities.
2.4 What mortality data tell us about deaths due to falls
The analyses provided in this section present data from Canadian Vital Statistics on all direct deaths due to falls among those aged 65 and over. These analyses include differences by place of injury, sex and age groups as well as trends over time.
Canadian Vital Statistics, Death Database
The information in this section is based on data from Statistics Canada's Canadian Vital Statistics, Death Database, from 2003-2008Footnote 160 .
Conversion of ICD 9 to ICD 10 coding affects analysis of data on fall-related deaths
Cause of death for this report was captured through the use of ICD-10. Comparing the figures presented in this report with those of previous studies on fall-related deaths could be affected by changes that took place in the year 2000, with the change in coding from ICD-9 to ICD-10. In particular, "accidental falls" as a "cause of death" category was dramatically affected by the implementation of ICD-10. Included under the ICD-9 group of codes for accidental falls was a code for "fracture, cause unspecified." This external cause of death was not included in the ICD-10 category of codes for falls but, rather, was included as a code under another category, "exposure to unspecified factor." For this analysis, only ICD-10 codes were used. Statistics Canada has used ICD-10 exclusively since 2000 Footnote 31.
2.4.1 Definitions and data
This section:
- Includes data on direct deaths, equivalent to the "underlying cause of death" as indicated on the medical certificate of death;
- Excludes indirect deaths, in which a fall may have eventually led to death but was not the underlying cause of death;
- Excludes deaths of non-residents of Canada, deaths of residents of Canada with unknown province or territory of residence, and deaths for which the age of the deceased was unknown; and
- Shows 95% CIs where appropriate.
2.4.2 Findings
Figure 20 shows there was a rise in both the number of deaths and the age-standardized mortality rate due to falls between 2003 and 2008. In 2008, 2,691 deaths among seniors were due to a fall. When trends over time are considered, statistically significant differences were noted in the age-standardized mortality rate between 2003 (3.5 per 10,000) and 2008 (4.7 per 10,000).
Figure 20: Number of deaths and age-standardized mortality rate due to falls, age 65+, Canada, 2003-2008 (95% CIs shown) Footnote 160
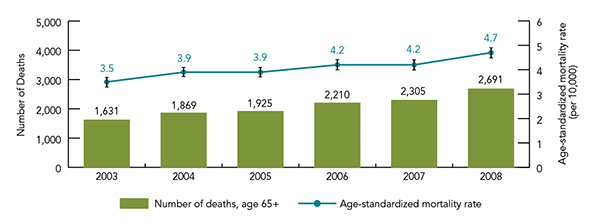
Text Equivalent - Figure 20
Figure 20 is a bar graph indicating the number of deaths and age-standardized mortality rate due to falls among Canadians 65 years of age and over for 2003, 2004, 2005, 2006, 2007, 2008. 95% confidence intervals are indicated.
| Year | Number of deaths among Canadians 65 years of age and over | Age-standardized mortality rate per 10,000 |
|---|---|---|
| 2003 | 1,631 | 3.5 |
| 2004 | 1,869 | 3.9 |
| 2005 | 1,925 | 3.9 |
| 2006 | 2,210 | 4.2 |
| 2007 | 2,305 | 4.2 |
| 2008 | 2,691 | 4.7 |
Figure 21 indicates that, with the exception of 2005, the number of deaths climbed with each successive increase in age category.
Figure 21: Number of deaths due to falls by age group, age 65+, Canada, 2003-2008 Footnote 160
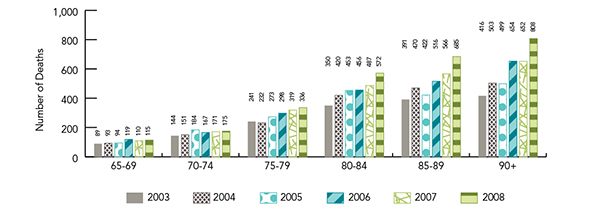
Text Equivalent - Figure 21
Figure 21 is a bar graph indicating the number of deaths due to falls by age group among Canadians 65 years of age and over for 2003 to 2008.
| Age Group | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 |
|---|---|---|---|---|---|---|
| 65-69 | 89 | 93 | 94 | 119 | 110 | 115 |
| 70-74 | 144 | 151 | 184 | 167 | 171 | 175 |
| 75-79 | 241 | 232 | 273 | 298 | 319 | 336 |
| 80-84 | 350 | 420 | 453 | 456 | 487 | 572 |
| 85-89 | 391 | 470 | 422 | 516 | 566 | 685 |
| 90 and over | 416 | 503 | 499 | 654 | 652 | 808 |
Figure 22 shows that age-specific mortality rates were consistent with the trends shown in the data presented above, with rates of death due to falls rising with each successive increase in age group.
Figure 22: Age-specific mortality rate for deaths due to falls (per 10,000), age 65+, Canada, 2003-2008 (95% CIs shown) Footnote 160
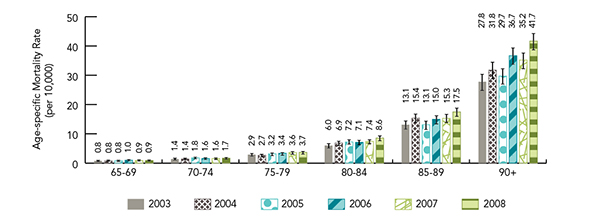
Text Equivalent - Figure 22
Figure 22 is a bar graph indicating the age-specific mortality rate for deaths due to falls per 10,000 for Canadians 65 years of age and over for 2003 to 2008. 95% confidence intervals are shown.
| Age Group | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 |
|---|---|---|---|---|---|---|
| 65-69 | 0.8 | 0.8 | 0.8 | 1.0 | 0.9 | 0.9 |
| 70-74 | 1.4 | 1.4 | 1.8 | 1.6 | 1.6 | 1.7 |
| 75-79 | 2.9 | 2.7 | 3.2 | 3.4 | 3.6 | 3.7 |
| 80-84 | 6.0 | 6.9 | 7.2 | 7.1 | 7.4 | 8.6 |
| 85-89 | 13.1 | 15.4 | 13.1 | 15.0 | 15.3 | 17.5 |
| 90 and over | 27.8 | 31.8 | 29.7 | 36.7 | 35.2 | 41.7 |
Figure 23 shows that age-standardized mortality rates generally increased among both males and females between 2003 and 2008. While the number of deaths due to falls was higher among females, the age- and sex-standardized mortality rates were significantly higher among males.
Figure 23: Number of deaths and age-standardized mortality rate for deaths due to falls (per 10,000), by sex, age 65+, Canada, 2003-2008 (95% CIs shown) Footnote 160

Text Equivalent - Figure 23
Figure 23 is a bar graph indicating the number of deaths and age-standardized mortality rate for deaths due to falls, per 10,000, by sex among Canadians 65 years of age and over for 2003 to 2008.
| Year | Female Deaths | Male Deaths | Female Mortality Rate | Male Mortality Rate |
|---|---|---|---|---|
| 2003 | 880 | 751 | 2.9 | 4.5 |
| 2004 | 1,073 | 796 | 3.3 | 4.6 |
| 2005 | 1,044 | 881 | 3.2 | 4.9 |
| 2006 | 1,242 | 968 | 3.6 | 5.2 |
| 2007 | 1,289 | 1,016 | 3.6 | 5.2 |
| 2008 | 1,515 | 1,176 | 4.1 | 5.7 |
2.4.3 Summary
Mortality data from Statistics Canada were analyzed for all direct deaths due to falls among those age 65 and over for the years 2003 to 2008. The results show a steady rise in both the number of deaths due to falls (65%) and the age-standardized mortality rate between 2003 and 2008. In general, the number of deaths climbed with each successive increase in age category. Age-specific mortality rates were consistent with these trends – rates of deaths due to falls rose with each successive increase in age group. In fact, each increase in age group resulted in a rate approximately twice that of the previous group. Although the number of deaths due to falls was shown to be higher among females, the age- and sex-standardized mortality rates were significantly higher among males.
3.0 Risk factors for falls and fall-related injuries among seniors
The previous chapter highlighted the socio-demographic and epidemiological evidence on fall-related injuries among seniors in Canada. This chapter focuses on current knowledge about fall risks. The information presented in this chapter was summarized from several well-known guidelines and from a review of the academic literature on risk factors for falls and fall-related injuries among seniors.
In addition to a thorough electronic search of PubMed, the following resources were consulted:
- Registered Nurses' Association of Ontario. Prevention of falls and fall injuries in the older adult (2005 updated and 2011 supplement) Footnote 134.
- American Geriatrics Society and British Geriatrics Society (AGS/BGS). Clinical practice guideline for the prevention of falls in older adults (2010) Footnote 118.
- Canadian Fall Prevention Education Collaborative. Canadian Falls Prevention Curriculum© (2012 updates to workshop, E-learning courses and associated materials) Footnote 26.
- Safer Healthcare Now. Reducing falls and injuries from falls: Getting started kit (2010) Footnote 138.
- National Institute for Clinical Excellence. Clinical practice guideline for the assessment and prevention of falls in older people (2004) Footnote 112.
3.1 Risk factors - Complex and interactive
Most falls occur as a result of compounding factors that combine and overwhelm an older person's ability to maintain or regain his or her balance. These factors typically represent a complex interaction of biological, behavioural, environmental and socio-economic conditions termed "risk factors". Research has identified numerous conditions that differentiate between older persons who fall and those who do not fall. Each older person may face a unique combination of risk factors based on life circumstances, health status, health behaviours, economic situation, social supports and the environment. Understanding what puts a person at risk of falling is a critical step in reducing falls and fall-related injuries among older Canadians.
The broad set of conditions that have been demonstrated to increase the risk of falling among older persons can be categorized as biological/intrinsic, behavioural, environmental and social/economic (see Appendix B). These risk factors do not exist in isolation but are instead complex and interactive.
The order in which the following risk categories is presented is not based on their relative importance but, instead, in accordance with their presentation in Scott, Dukeshire, et al. Footnote 143, and then specific factors are addressed alphabetically.
3.2 Biological or intrinsic risk factors
Biological or intrinsic risk factors include those pertaining to the human body and are related to the natural aging process, as well as the effects of chronic or acute health conditions. In 2008/2009, 20% of Canadian seniors in the household population reported at least one fall; falling was even more prevalent among older ages (i.e., 80 years and over) Footnote 162 . The following conditions often associated with aging are contributors to falling:
- Acute illness: Symptoms of acute illness such as weakness, pain, fever, nausea and dizziness can increase the risk of falling Footnote 102. For example, one study found that infections, in particular urinary tract infections, were a precipitating factor in 8% of falls Footnote 82. Furthermore, the effects of medications taken to treat the condition or symptoms can also increase the risk of falling Footnote 169.
- Balance and gait deficits: Balance impairments result when there are changes to the normal functioning of the systems underlying postural control, which can involve biomechanical, sensory and cognitive changes Footnote 76. Changes to these systems result in context-specific instabilities that may lead to falls Footnote 76. Research consistently shows that balance deficits are significantly linked to risk of falling among older adults Footnote 110 Footnote 112 Footnote 118 Footnote 169 Footnote 171 Footnote 172. Similarly, a number of studies have found that variability in one's gait (e.g., timing, placement) is a risk factor for falling Footnote 68 Footnote 98.
- Chronic conditions and disabilities: A wide range of chronic conditions can increase an individual's risk of falls, including neurological disorders such as Parkinson's disease Footnote 4 Footnote 5 Footnote 166 Footnote 179, diabetes Footnote 21, arthritis Footnote 165, cardiovascular disease Footnote 38 Footnote 43, end-stage renal disease Footnote 1, chronic obstructive pulmonary disorder Footnote 8 Footnote 9 or the effects of a stroke Footnote 24 Footnote 88 Footnote 153. These chronic conditions result in physical limitations that affect one's mobility, gait and balance. For example, in samples of community-dwelling individuals with Parkinson's disease, estimates show that over 60% of participants fell at least once each year Footnote 4 Footnote 179, and the risk of a fracture has been shown to be approximately twice that of comparable older persons who fall Footnote 57. Furthermore, complications related to diabetes, such as neuropathy, retinopathy and nephropathy, likely contribute to an increased risk of falls Footnote 21.
Other chronic conditions include bowel or bladder incontinence and urgency, which can lead to rushing and frequent trips to the bathroom. A recent meta-analysis conducted by Bloch et al. found a strong link between taking laxatives and falls Footnote 17, such that patients taking laxatives were twice as likely to fall as those not taking them. Similarly, foot disorders such as corns, bunions, toe deformities, ulcers and general pain can contribute to balance and gait difficulties Footnote 107.
While osteoporosis, characterized by low bone mass and the deterioration of bone tissue, does not affect the risk of falling per se, it does increase the risk of fractures from a fall Footnote 41. Older women are at greater risk of osteoporosis than men, and the prevalence increases with age. A recent analysis of CCHS data found that, in 2008, 19% of women and 3% of men aged 50 and older reported receiving a diagnosis of osteoporosis Footnote 56. Low bone mass in the absence of a clinical diagnosis of osteoporosis may also be a risk factor for fracture. Research estimates that at least one in three women and one in five men will suffer from an osteoporotic fracture during their lifetime Footnote 104 Footnote 105. These fracture patients are at extremely high risk of re-fracture if their condition is left untreated Footnote 117. Thus, even a minor fall or injury can lead to a fracture for someone with osteoporosis, highlighting the importance of fall prevention. - Cognitive impairments: For those older people with dementia or other cognitive impairments, the risk of falling and sustaining a fall injury is two to three times that of older people without cognitive impairments Footnote 65. Cognitive impairments affect one's ability to anticipate and adapt to environmental stimuli to maintain or restore balance Footnote 67. In addition, researchers are beginning to explore the link between dementia, gait instability and falls Footnote 5 Footnote 150. These symptoms may be further compounded by the side effects of medications taken to manage behavioural problems that can accompany dementia. A state of mental confusion or disorientation, also referred to as delirium, has also been shown to increase the risk of falls. Delirium may result from acute infection, medication, dehydration, sensory impairment, emotional distress etc Footnote 77 Footnote 87. Research has found that normal age-related cognitive changes can also affect balance, for example, through delays in switching attention from an ongoing cognitive task to the task of responding to an unexpected loss of balance Footnote 101.
- Low vision: Changes to vision, such as decreases in visual field sensitivity, acuity, contrast sensitivity and stereopsis, are associated with aging and increase the risk of falls Footnote 95. For example, a systematic review of risk factors found that older adults with low vision were 2.5 times more likely to fall than older adults without visual deficits Footnote 118. Indirectly, changes in vision are linked to a decrease in physical activity, which is another risk factor for falling Footnote 131. Low vision can impede one's ability to walk safely because one cannot detect hazards in the environment. Low vision can also affect the ability to maintain balance Footnote 131. In 2006, more than 240,000 Canadians over the age of 75 reported experiencing vision loss Footnote 20.
Visual attention and gaze behaviour can also affect the risk of falling for seniors. For example, seniors are less likely than young adults to look at a handrail upon entering an unfamiliar environment and less likely to direct visual attention to changes in the location of obstacles around them. Seniors at high risk of falling were found to exhibit different gaze behaviour in comparison to low-risk subjects, suggesting that the strategy used to gather visuospatial information during walking may affect the risk of falling Footnote 34. - Muscle weakness and reduced physical fitness: Decreases in muscle strength and endurance can leave one unable to prevent a slip, trip or stumble from becoming a fall Footnote 109. The panel of the American Geriatrics Society, British Geriatrics Society and American Academy of Orthopaedic Surgeons found muscle weakness to be the most important risk factor, increasing the risk of a fall by four to five times Footnote 118. Furthermore, weakness in the lower extremities was found to be a risk factor for fall-related hip fractures Footnote 109 Footnote 151.
3.3 Behavioural risk factors
Behavioural risk factors for falling include actions, emotions or choices of the individual.
- Assistive devices: Assistive devices can promote independence and mobility and may prevent falls if properly used and safely maintained Footnote 7. However, lack of maintenance, malfunction, inappropriate fit or overreliance on the device can turn an assistive device into a fall hazard. For example, cane tips can become worn, wheels on walkers and wheelchairs can become loose, or equipment can be too heavy or the wrong height Footnote 6. In addition, feeling uneasy when using assistive devices has been linked to falling Footnote 19.
- Excessive alcohol: Research has found an association between alcohol use and falls and fall-related injury. In one study of adults 18 years and older, 22% of patients seen in an emergency department for a fall tested positive for alcohol; the percentage as well as the degree of blood alcohol levels decreased with ageFootnote 84 . In addition, alcohol may interact with certain drugs to increase the risk of falls by producing changes in awareness, balance and gait.
- Fear of falling: Fear of falling is itself an important risk factor for future falls Footnote 141 Footnote 165. A recent analysis of data from the Canadian household population showed that 34% of Canadians over the age of 65 were worried or concerned about falling in the future Footnote 162. A fear of falling may lead to a decrease in physical activity, which in turn leads to muscle weakness and poor balance, and poorer self-reported health Footnote 172 Footnote 141. Among older Canadians who reported a fear of falling in the future, 44% limited their activities on the basis of that concern Footnote 162. It is important to note that fear of falling can result from falls that are not injurious and thus not captured in the CCHS. Fear of falling may be reduced through home-based exercise and multifactorial fall prevention programs as well as through community-based tai chi offered in a group format Footnote 182.
- Footwear and clothing: Features of footwear that have been linked to fall risk include soles that are too thick, a tread that is too smooth, and shoes with heels that are too high and/or too narrow Footnote 106 Footnote 167. Research has also shown that footwear designs may improve postural stability through, for example, balance-enhancing insoles Footnote 121. Clothing that is too long may impede walking or clothing made from slippery fabric, such as satin, can lead to older people sliding off furniture Footnote 157. In addition, clothing that is difficult to put on may cause a person with reduced mobility to lose his or her balance and fall while dressing.
- History of previous falls: Prior falls are one of the strongest predictors of future falls Footnote 118 Footnote 172. Research has shown that older adults who experience one or more falls are three times more likely to fall again within the following year compared with older adults with no history of falls Footnote 118. A history of falling is considered a behavioural risk factor when one chooses not to seek information on ways to reduce risk or chooses not to take action to reduce the risk, even when safeguards proven to be effective are known.
- Inadequate diet: The relationship between diet and falls has long been suspected but only recently has been studied. It is reasonable to expect that dehydration and/or malnutrition from poor diets and inadequate fluid could lead to physical weakness, fatigue and frailty. Recent research found that malnourished older adults who presented to the emergency department were more likely to report falling within the previous six months Footnote 174. In 2008/2009 an estimated 34% of Canadian seniors in private households were at nutritional risk, a concept that lies on a continuum between nutritional health and malnutrition Footnote 129.
- Medications: Systematic reviews of the evidence have illustrated a strong association between the occurrence of falls and fractures in older people and the use of certain medications, particularly psychotropic (medications that alter mood), sedative (medications that induce calm) and hypnotic (medications that induce sleep) medications, such as benzodiazepines, antidepressants and antipsychotics Footnote 18 Footnote 66. Cadario & Scott found that medications that cause drowsiness, dizziness, hypotension, Parkinsonian effects, ataxia/gait disturbance or visual disturbances increase an older person's risk of falling Footnote 22. Furthermore, any drug that decreases bone density or increases the risk of bleeding can increase the risk and severity of injury from a fall Footnote 22. Older adults taking more than three to four medications seem to be at higher risk of falls Footnote 89.
- Risk-taking behaviour: Among older persons, risk-taking behaviours can lead to an increase in falls and fall-related injuries. A behaviour is considered risk-taking when a discrepancy exists between the risk associated with the activity and the abilities of the individual engaging in that activity. For an older person, behaviours such as climbing ladders, standing on unsteady chairs, paying little attention to the surrounding environment or walking without a mobility aid when one is needed are all risk-taking behaviours that lead to falls and injuries Footnote 136.
- Vitamin D: Vitamin D has been linked to bone and muscle strength Footnote 70 Footnote 71. Recently, researchers have found that vitamin D supplementation alone and combined with calcium may reduce the risk of falls Footnote 15 Footnote 79 Footnote 83 Footnote 111. Other research shows that vitamin D supplementation only reduces falls among those with vitamin D deficiency Footnote 58.
3.4 Social and economic risk factors
The connection between social determinants and one's health, level of disability, development of chronic conditions, longevity and cognitive function has been well established and is widely accepted Footnote 45 Footnote 97 Footnote 169. Despite the fact that a direct relationship between falls and social and economic factors is not well established there are some data linking these factors and falls Footnote 46.
- Social networks: While the available evidence shows an indirect relationship between social networks and falls through poor health, isolation, depression and disabilities Footnote 14 Footnote 53 Footnote 128, there is growing evidence for direct links between social factors and fall risk. One study of over 6,500 Caucasian women aged 70 years and older showed a positive relationship between strong family networks and lower fall rates Footnote 47. In addition, a recent meta-analysis by Bloch et al. demonstrated a protective effect of marriage against falling in patients over 80 years of age Footnote 16. Evidence on the protective effect of marriage against falling is supported by the self-report data presented in Chapter 2, in which married older adults were less likely to report a fall. Peel, Bartlett & McClure found that being married, living in current residence for five years or more, using proactive coping strategies in response to stress, having a higher level of life satisfaction, and engagement in social activities in older age all had a protective effect on preventing hip fractures due to falls Footnote 120. This may be indicative of the risk presented by social isolation in general.
- Socio-economic status: Existing research suggests a relationship between low socio-economic status and risk of falls Footnote 135 Footnote 177. A number of explanations for this finding have been proposed, including the association of low socio-economic status with poor environment, poor diet and barriers in accessing health care services Footnote 180. Another contributing factor may be low education and low health literacy, which prevent individuals from benefiting from web-based or printed resources on strategies for preventing falls.
3.5 Environmental risk factors
Environmental risk factors are those factors associated with the physical environment, such as the design of a building, entrances and outdoor spaces, and the type of furniture and other objects in the rooms. Some earlier research has demonstrated that 40-60% of falls are related to environmental hazards Footnote 50. However, a recent systematic review did not establish a consistent association between environmental hazards and falls, which may reflect the difficulty in isolating environmental contributors from other factors that impair balance Footnote 48. Some studies have shown that the risk of falls results from an interaction between an older person's mobility, physical abilities or risk-taking behaviour and their exposure to physical environmental hazards Footnote 48 Footnote 94. Environmental factors may work together to create a risk condition that increases the likelihood of falls among seniors.
CSA Group's Inclusive Design for an Aging Population is intended to promote the application of design guidelines that inform the creation of products, services and environments that are accessible to an aging population. This standard offers principles and concepts that provide the tools necessary to appropriately identify and address the needs of older adults Footnote 39.
- Factors in the community: Community hazards are often related to design standards, and building codes may not take into account the needs of older persons Footnote 44. Examples include poor stair design, inadequate lighting, the lack of handrails, the lack of curb ramps and rest areas, uneven pavement due to sidewalk cracks or tree roots, and obstacles on sidewalks that impede safe passage, such as sidewalk furniture, bike racks, grates and store signage Footnote 54 Footnote 169. Unsafe stair design is particularly problematic for those with low vision or mobility problems. Hazards related to stairs include uneven steps, stairs without contrasting edges, lack of handrails, poor handrail design (e.g., inappropriate height), stairs in need of repair and stairs that are slippery from rain, snow or moss Footnote 99 Footnote 119. As people age, they may experience changes in gait pattern, strength, vision and balance, which, when combined with unstable walking surfaces, can result in an increased risk of falls in the winter Footnote 11 Footnote 12 Footnote 13. Chapter 2 showed that 46% of self-reported injurious falls were associated with walking on surfaces other than snow or ice.
Falls may also occur in a hospital setting, some studies reporting that falls represent a significant proportion of in-hospital accidents Footnote 63. For example, an analysis of Australian data showed that 90% of in-hospital accidents were falls, and most occurred among older patients Footnote 59. In an attempt to estimate the costs associated with falls in hospitals in Canada, Zecevic and colleagues found that the hospital costs for those seriously injured in falls in an acute care setting were $30,696 greater than the costs for those who did not fall Footnote 181. - Factors in the living environment: Researchers and practitioners often consider environmental hazards in the home the most common environmental risk factor for falls Footnote 90. Home hazards that have been demonstrated to increase the risk of falling for older people include throw rugs and loose, worn or deep pile carpets; electrical cords in walkways; raised door sills; cluttered floors; poor lighting; slippery floors; poorly designed tubs, toilets and fixtures in the bathroom; no aids or poorly installed aids such as grab bars or hand rails; and pets that get under foot Footnote 51 Footnote 73 Footnote 114 Footnote 127 Footnote 137 Footnote 165 Footnote 173 Footnote 176. This is of particular concern given that the CCHS data in Chapter 2 showed that half of all falls occur in the home. In residential care or institutional settings, additional hazards that increase the risk of falling include beds that are too high, carpet and cluttered rooms and hallways Footnote 82 Footnote 169. Finally, moving to a new location may be sufficient to increase fall risk because of the unfamiliarity of a new environment Footnote 10 Footnote 130.
- Weather and climate: Weather conditions may also increase the risk of falls if appropriate precautionary measures are not taken. In Canada, both temperature and precipitation are factors that can lead to wet or icy surfaces and increase the risk of falling Footnote 55 Footnote 75. Winter weather conditions increase the risk of slips and falls as snow and ice can reduce underfoot traction, making it difficult for all pedestrians to maintain balance and execute effective balance recovery strategies Footnote 2. Freezing and accumulation of precipitation can also create barriers to safe access to roadways, sidewalks and buildings. These risks are exacerbated when pedestrians increase their walking speed because of the physical discomfort of exposure to cold Footnote 91. Winter weather conditions are also problematic on entry into buildings, as wet footwear can lead to slips on smooth indoor flooring Footnote 132. Such conditions can also prevent effective use of assistive devices, as gait stabilizers such as canes and walkers are more likely to slip and tires on wheelchairs and scooters can lose traction or become obstructed.
3.6 Summary
The scientific literature and existing practice guidelines report that falls among seniors result from a complex interaction of risk factors. These risk factors can be categorized as biological/intrinsic, behavioural, environmental and social/economic. Aging is associated with changes in physical and cognitive function that may increase the risk of falls. However, the risk of falling may be mitigated by evidence-based programming and/or interventions.
4.0 Best practices for the prevention of falls
Over the past decade, research on best practices in fall prevention has flourished. As a result, more detailed information now exists about what works, for whom and in what setting. The majority of available systematic reviews agree that, in most cases, the best approach to fall prevention among older adults includes a multifactorial falls risk assessment and a subsequent management program tailored to an individual's risk factors and setting Footnote 23 Footnote 33 Footnote 58 Footnote 103 Footnote 118. Single interventions have also been shown to be effective, particularly for healthier older adults who have a limited number of risk factors. For example, a recent systematic review found that exercise alone was five times more effective in fall prevention for older adults living in the community than the multifactorial interventions evaluated in other studies Footnote 122. The following is an overview of multifactorial best practices for fall prevention, which also identifies single interventions that are components of the multifactorial interventions. The review reflects the current evidence and clinical expertise for community and institutional settings. This information was gathered through a review of the academic literature and by consulting resources identified by experts in fall prevention.
4.1 Initial risk assessment
The first step in fall prevention is to conduct a multifactorial risk assessment (see Figure 24). The AGS and BGS recommend that primary health care providers ask all older adults at least once a year about falls, the frequency of falling and any difficulties in gait and balance Footnote 118. According to the recommendation, any older person who presents with an acute fall (fall with an injury), has difficulty with gait or balance, or reports two or more falls in the previous 12 months warrants a comprehensive risk assessment. For those without a reported fall or with a single fall in the previous 12 months, a comprehensive assessment is not required, unless the older adult has difficulties with gait or balance.
Figure 24: Multifactorial risk assessment of falls among seniorsFootnote 118
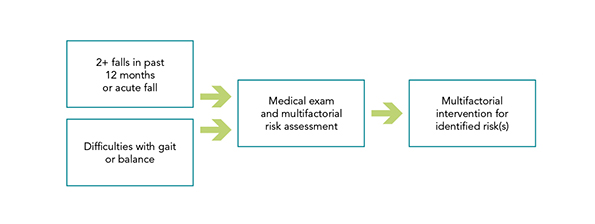
Text Equivalent - Figure 24
Figure 24 is a schematic diagram showing the progression of a multifactorial risk assessment of falls among seniors. In summary, if a senior has either more than 2 falls in the past 12 months or had an acute fall or has gait/balance difficulties, they should undergo a medical exam and multifactorial risk assessment. This would be followed by a multifactorial intervention for any identified risk.
4.1.1 Components of a comprehensive assessment
A comprehensive clinical assessment can determine the risk of falls, identify the risk factors and assist in identifying the most appropriate tailored interventions. The 2011 AGS/BGS guidelines Footnote 118 recommend that the following components be included in a comprehensive clinical assessment:
- Medical history, physical examination, cognitive and functional assessment;
- History of falls; taking multiple medications (particularly psychotropic medications); problems with gait, balance and mobility; impaired vision; other neurological impairments; reduced muscle strength; problems with heart rate and rhythm; postural hypotension; foot problems and incorrect footwear; environmental hazards.
The assessment may be carried out by a single clinician or, alternatively, several clinicians, such as physicians, nurse practitioners, physical therapists, occupational therapists or pharmacists, may complete the components most relevant to their expertise.
4.2 Multifactorial interventions
Multifactorial interventions are focused interventions that target multiple risk factors identified during a comprehensive risk assessment. Risk factors for seniors often differ according to health and social circumstances, which typically reflect where they live (i.e., in private homes in the community or institutional settings). Recent research highlights the importance of settings-based interventions Footnote 23 Footnote 58. The reasons for falls among community-dwelling seniors are typically different from those of seniors living in institutional settings. In turn, the nature of effective interventions differs between community-dwelling and non-community-dwelling seniors. Thus, the findings for evidence-based multifactorial interventions are presented by setting, and the interventions themselves are presented in alphabetical order.
4.2.1 Components of successful multifactorial approaches for community-based settings
- Assistive devices and other protective equipment: The appropriate use of assistive devices is important for those with gait and balance deficits. It is recommended that clinical expertise be sought for the appropriate assessment of equipment needs. For older adults living in climates with snow and ice, an anti-slip shoe device worn in icy conditions has been shown to reduce falls Footnote 58 Footnote 118. Research has shown that this footwear may perform well on some surfaces but poorly on others Footnote 55 Footnote 62. For example, cleated footwear may be hazardous when walking indoors on hard, smooth surfaces Footnote 62. Seniors may avoid using assistive devices because of lack of information, inconvenience, the bulkiness of the device or the stigma associated with using assistive devices.
- Clinical disease management, including chronic and acute illness: Appropriate treatment of medical conditions, including visual problems, cardiovascular disorders and hypotension has been demonstrated to reduce falls Footnote 58 Footnote 118. The existence of multiple chronic conditions often requires multiple drugs, increasing the probability of drug interactions which, in turn, may lead to increased risk of falls.
- Education: Education of older adults and their care providers is important for implementation and sustained use of fall prevention strategies. Many effective programs include opportunities for older adults to access fall prevention resources (e.g., durable medical equipment, local exercise programs) and to take specific actions that maintain or improve health or build fall prevention skills (e.g., transferring safely into the bathtub, learning how to use mobility devices) Footnote 118. The Canadian Falls Prevention Curriculum© for health care professionals and community leaders has been shown to have a positive impact on practice and to enhance implementation of evidence-based fall prevention Footnote 144.
- Environmental modification: For older adults with mobility or sensory problems or those who are prone to falling, it is recommended that a health care professional perform an environmental assessment for required modification as part of a multifactorial intervention. The intervention should include modifications of environmental fall risks identified in the home, and both evaluation of daily activities and intervention to promote their safe performance Footnote 118. A systematic review and meta-analysis demonstrated a 21% reduction in falls across all studies and a 39% reduction among high-risk older adults following environmental modification Footnote 35. Occupational therapists may play a role in preventing falls through environmental modification Footnote 40.
- Exercise programs: Research has demonstrated that exercise is effective for community-dwelling older people and should be included in a multifactorial approach Footnote 108 Footnote 152. Exercises that target balance, gait and strength training are most effective and can be offered in supervised groups or performed individually Footnote 58 Footnote 118.
A recent systematic review examined 54 exercise programs designed to prevent falls in older adults and developed the following recommendations for exercise-based interventions Footnote 152:- Exercise must provide a moderate or high challenge to balance;
- Exercise must be of a sufficient dose to have an effect;
- Ongoing exercise is necessary;
- Fall prevention exercise should be targeted at the general community as well as those at high risk of falls;
- Fall prevention exercise may be undertaken in a group or home-based setting;
- Walking training may be included in addition to balance training, but high risk individuals should not be prescribed brisk walking programs;
- Strength training may be included in addition to balance training;
- Exercise providers should make referrals for other risk factors to be addressed.
- Medication review and modification: Having routine reviews, adjustments and removal of unnecessary medication under the supervision of a physician or pharmacist may be effective in reducing falls. Some psychotropic medications, including those taken for sleep, anxiety or the treatment of depression, have been shown to significantly increase the risk of falls. Gradual, supervised withdrawal from these medications has been shown to reduce falling among older adults Footnote 58 Footnote 118.
- Nutrition and supplements: Good nutrition is essential for good health Footnote 70. In particular, older adults require sufficient protein to maintain muscle strength and adequate hydration, particularly in the summer months. In addition, nutritional supplements are sometimes required. Poor nutrition and dehydration cause poor physical reaction at the time of an injury, as well as acting as an impediment to recovery Footnote 117 Footnote 70 Footnote 80 Footnote 42. The AGS recommends vitamin D as a daily supplement for all older adults at risk of falls, or with either a known or suspected vitamin D deficiency Footnote 118. Researchers have found that vitamin D combined with calcium reduces the risk of falls and that this impact is most profound when an older person is deficient in vitamin D Footnote 111 Footnote 83 Footnote 52 Footnote 108.
- Vision referral and correction: All vision concerns or problems should be formally assessed, and any remediable visual abnormalities should be treated, particularly cataracts Footnote 58 Footnote 118. Seniors with chronic and degenerative eye disease such as age-related macular degeneration and diabetic retinopathy may be referred to the Canadian National Institute for the Blind for vision rehabilitation services to develop the orientation and mobility skills that will allow them to navigate their environment safely and to ensure that their living environment is free of falling hazards Footnote 32.
4.2.2 Components of successful multifactorial approaches for residential care settingsFootnote f
- Assistive devices and other protective equipment: Research has been done on the effectiveness of hip protectors among individuals in residential care Footnote 36. Hip protectors are padded garments designed to reduce the impact to the hip that results from falling. Hip protectors are not designed to prevent falling but can instead prevent injury resulting from a fall. The design features of hip protectors vary considerably among makes and, until recently, there were no established guidelines for assessing their effectiveness Footnote 85. This may explain why the research findings to date have been mixed, and there is currently no evidence to support universal use of hip protectors by older adults in residential care Footnote 134. The design features of the hip protector and the individual's health status are among the factors that may be taken into consideration when determining the appropriateness of hip protectors Footnote 25.
- Education: The education of long-term care staff has had mixed results: some evidence supports the effectiveness of health care team training in awareness and prevention strategies, although several multifactorial studies failed to show a significant reduction in falls Footnote 118.
- Environmental modification: The results of environmental modification on reducing falls in a residential care setting have been mixed. Of the studies that included environmental modification as part of a multicomponent intervention, half of the studies supported its effectiveness while the other half did not Footnote 118. Currently, there are no data to support environmental modification as an independent intervention Footnote 118. New research has shown that low stiffness flooring can reduce the impact of falls by up to 50% without impairing balance Footnote 86.
- Exercise programs: Results relating to the effectiveness of exercise in reducing the rate of falls and risk of falling among seniors living in residential care are inconsistent. Some studies have found a greater risk of falls with exercise, whereas others show a reduction of falls with exercise. These differences may be attributed to differences in levels of frailty and cognitive function, as well as differences in sample sizes among studies Footnote 118. According to the AGS and BGS, there are currently no clinical randomized controlled trials to recommend the use of customized exercise protocols for the prevention of falls in long-term care settings Footnote 118. Fall prevention interventions that include an exercise component for individuals in residential care should carefully assess each individual's capacity and suitability, because exercise interventions may increase the risk of falls Footnote 23.
- Medication review and modification: Targeting inappropriate medications may be effective in reducing falls in residential care Footnote 23 Footnote 118. Review and modification of medications, particularly medications that alter mood (i.e., psychotropics), have been demonstrated to significantly reduce the rate of falling Footnote 74.
- Nutrition and supplements: There is strong evidence for vitamin D supplementation for seniors in residential care who have known vitamin D deficiency Footnote 52. Vitamin D supplementation should also be considered for those at risk of falls who reside in long-term care Footnote 83 Footnote 118.
- Other interventions: Other interventions shown to be clinically relevant include staff training for skills such as safer transferring techniques, creating multidisciplinary teams and promoting commitment among staff to fall prevention Footnote 49.
- Vision referral and correction: If patients report problems or concerns, their vision should be formally assessed, and any remediable visual abnormalities should be treated, particularly cataracts Footnote 118.
4.2.3 Components of successful multifactorial approaches for acute care settings
The research on fall prevention in acute care is sparse. The majority of available studies suffer from small samples and insufficiently described data Footnote 72. Two reviews of current evidence, however, did find that targeting multiple risk factors and supervised exercise are effective for long stay (greater than three weeks) patients Footnote 23 Footnote 116. Studies also show that there is no evidence to support the use of physical or pharmaceutical restraints to reduce falls and that these restraints may actually lead to falls Footnote 69. It has been suggested that the use of restraints be kept to a minimum, never used as a substitute for individualized assessment or supervision, and frequently reviewed Footnote 116. Another recommendation for acute care settings is patient education on fall risk Footnote 64. Acute care settings that establish senior friendly processes may reduce unnecessary adverse events such as falls Footnote 149.
Accreditation Canada provides organizations with an external review process in order to evaluate and improve services, including fall prevention strategies Footnote 3. Recently, Accreditation Canada designated fall prevention and management as a Required Organizational Practice, requiring health care teams to implement and evaluate a fall prevention strategy to minimize patient falls Footnote 3.
4.3 Summary
On the basis of a review of the scientific literature, there is evidence for the effectiveness of combining multifactorial risk assessments with multifactorial interventions that address factors associated with health and environment among seniors. These interventions typically include exercise programs with a focus on balance, gait and weight training. Multifactorial approaches that target the risk factors identified in Chapter 3 and that tailor interventions to individuals' health needs and environment can reduce the incidence of falls. Innovative approaches that leverage new technology (e.g., compliant flooring) have the potential to reduce the impact of falling.
5.0 Stepping up fall prevention in Canada
5.1 Why is an updated report on falls needed?
As evidenced by the data summarized in this report, falls among seniors continue to be a public health concern. However, responsibility for preventing falls is shared across jurisdictions, caregivers and individuals. As the population of Canadians aged 65+ increases from 14% in 2009 to an estimated almost 25% of the total population by 2036 Footnote 163, coordinated efforts can make a huge impact on reducing the effect of falls on older Canadians and minimizing the burden associated with health care costs. It is important that accurate data be available to assist stakeholders by identifying potential areas for improvement in the frequency and outcomes associated with falls among seniors.
Notwithstanding the significant indirect cost of falls to the lives of seniors and their families, direct health care costs associated with injurious falls in this population were estimated at over $2 billion in 2004 Footnote 156. The cost of falls for Canadian seniors (per capita) was 3.7 times greater than that of individuals between the ages of 25 and 64 years.
In 2005, the Report on Seniors' Falls in Canada provided the first national overview of fall-related hospitalizations, deaths and self-reported injuries for older Canadians Footnote 125. The data contained within this second edition of the report provide an update to our knowledge of the nature and severity of seniors' falls and paint a picture of changes over time. Secondly, the report re-examines risk factors for falls and fall-related injuries in older adults and presents the effectiveness of multifactorial interventions to prevent falls.
5.2 Examining the findings
This report mined several data sources to capture the current impact of falls in Canada. While there are recognized limitations to the data available (see Chapter 2 for specific disclaimers), there are some particular findings on self-reported falls (as opposed to hospitalization records) that should be noted:
- Rates of self-reported injuries due to falls increased significantly from 2003 to 2009/2010;
- Rates of self-reported fall-related injuries were higher in older age groups (i.e., over 85 years);
- The majority of self-reported fall-related injuries resulted in broken or fractured bones; and
- Respondents with a fall-related injury were:
- more likely to be female (although the rate among males is on the rise);
- more likely to be older (i.e., 85+); and
- less likely to be married.
An analysis of hospitalization records showed the following:
- Length of hospital stays related to a fall-related injury increased with age;
- Over one third of fall-related hospitalizations among seniors were associated with a hip fracture;
- Half of fall-related hospitalizations among seniors resulted from falls at home; and
- Hospitalizations resulting from falls in residential care were associated with longer stays in hospital than those that occurred at home.
The Canadian data related to deaths due to falls revealed the following:
- The age-standardized mortality rate due to falls has increased significantly since 2003;
- The frequency of deaths and the age-standardized mortality rates due to falls were highest among the oldest seniors; and
- While the number of deaths due to falls was higher among females, the age- and sex-standardized mortality rates were significantly higher among males.
In examining the data presented in Chapter 2 of this report, it is important to recognize that the self-report data and the hospitalization data focus on fall-related injuries as opposed to the prevalence of non-injurious falls. If a CCHS respondent fell but was not injured, the data would not be captured in this analysis. Similarly, if a respondent was injured as a result of a fall and was not hospitalized, the data would not be captured in the HMDB. Thus, the analysis presented in this report may underestimate the number of falls by Canadian seniors.
The data related to self-reported fall-related injuries revealed that the most frequent site of injury was the shoulder or upper arm (17%) followed by the knee or lower leg (15%). According to the self-report data, injuries to the hip accounted for 7% of fall-related injuries (Figure 6). The hospitalization data, on the other hand, showed that approximately 35% of fall-related hospitalizations were associated with a hip fracture (Figure 14). It is likely that self-reported fall-related injuries captured by the CCHS were, on the whole, less severe than those requiring hospitalization. In particular, not all individuals who reported a fall-related injury in the CCHS sought medical attention, and of those who did 67% sought treatment at an emergency room (Figure 8).
When comparing fall-related injuries and hospitalizations among seniors from year to year, there were many similarities. A striking difference, however, was noted in the increased mortality rates due to falls among Canadian seniors over time. Possible explanations of the difference may be an increase in the severity of the falls in recent years. Alternatively, given that risk of falls increases for each successive age category within the older adult population (Figure 21 and 22), it seems reasonable to suspect that these year-over-year changes could stem from an increase in the number of seniors in the oldest-old category (i.e., 85+).
5.3 Managing the risk factors
The risk factors for falls among seniors are numerous, complex and interactive. These factors can be broadly categorized as biological/intrinsic, behavioural, environmental and social/economic. Aging is associated with changes in biological, behavioural and social factors that can lead to changes in how seniors interact with their environments. These risk factors alone and in combination may increase the risk of falls. This is important to take into consideration in fall prevention programming, as the information presented in Chapter 4 demonstrates a relationship between environmental and physical risk factors for falls among seniors.
Biologic/intrinsic risk factors are important elements of a successful fall prevention approach. Falls can result in negative health outcomes, both psychological (e.g., loss of autonomy, confusion, depression) and physical (e.g., injury, disability, death). To further complicate matters, social isolation among older adults has been associated with an increased number of falls Footnote 113. While the available evidence shows an indirect relationship between social networks and falls through poor health, depression and disabilities, there is growing evidence for direct links between social factors and fall risk.
Nutritional deficiencies and lack of physical activity are factors that have been demonstrated to be associated with risk of falling. There are currently a number of investments that support Canadians in making healthy lifestyle choices. References such as Eating Well with Canada's Food Guide and Eating Well with Canada's Guide for First Nations, Inuit and Métis are provided by the Government of Canada to help Canadians meet their needs for vitamins, minerals and other nutrients; reduce their risk of nutrition-related chronic disease; and contribute to overall health and vitality. These guidelines underpin nutrition and health policies, standards, education programs and meal planning initiatives across the country. The most recent edition of the guide includes specific recommendations for seniors.
Data on injuries due to falls in the CCHS demonstrated that walking was the most frequent activity undertaken at the time of falling and was a significantly higher risk than that posed by either sports activities or stairs. Sixteen percent of these incidents were linked to icy surfaces; however 45% were associated with walking on non-icy surfaces (see Figure 5). The data are not specific enough to determine whether there is a predominant surface type involved in the non-icy category. The findings highlight the importance of interventions that help strengthen resiliency and core balance to mitigate imbalance and injury, addressing the risk factors of balance and gait deficits as well as muscle weakness. A number of studies have shown that exercise programs and restorative care are important interventions to help prevent falls (see Chapter 4). The most effective exercise programs appear to be those suited to the level of mobility of the older adult: notably those involving strength and posture building, smooth movements and gentle stretching, such as tai chi. Canada's Physical Activity Guide to Healthy Active Living for Older Adults and the Physical Activity Tips for Older Adults guide are important tools for achieving better health by making physical activity an important part of daily living. In addition, promising technologies now exist to help assess the risk of imbalance and can also be used as part of a multifactorial exercise program, such as electronic balance boards, videogaming products and handrail cueing systems Footnote 100 Footnote 148. Evidence suggests that programs may be used both as a pre-emptive strategy before an initial fall occurs, as well as a post-discharge tool (both hospital and emergency room) to prevent readmission Footnote 37 Footnote 139.
General weather changes associated with a northern climate also increase fall risks, such as weather extremes causing cracked pavement or large piles of fallen leaves obscuring visibility and posing an obstacle. Inherent to our Canadian landscape, ice, sleet and snow present a risk for falling. While anti-slip shoes can be effective in reducing falls in icy conditions Footnote 58, they may actually increase the risk when individuals use them to walk on other surfaces Footnote 132. It would be of interest to explore the role of anti-slip and other assistive devices in preventing falls in the broader context of an entire journey, notably their safety in and out of entryways or other interior surfaces in addition to their effectiveness in a cold exterior, as the footwear may not be suitable for both.
There has been a significant amount of literature on practices to improve seniors' environments to reduce falls (see Chapter 4). Some proposed approaches have been alternative flooring and modified stairs. Building codes may play an important role in implementing environmental interventions to reduce falls among seniors. Environmental risk factors may also be addressed through outdoor civic planning activities such as city snow removal and sidewalk sanding, as well as street crossing and curb design Footnote 92 Footnote 133.
Addressing falls may not be achieved by targeting only one risk factor. Instead, comprehensive evaluations followed by multifactorial, evidence-based practices are important for fall prevention among seniors. Setting practices, standards, and management and assessment applications can contribute to fall prevention activities in Canada. Fall prevention guidelines may be useful to assess individual risks, behaviours and challenges, and to establish standards that minimize the number and impact of falls. As well, guidelines can involve various sectors in reducing individual and community risk factors. Interventions also need to be tailored to the client's specific environment, as evidenced by the data showing that risk factors, location, place of injury and types of fall varied depending on the setting (see Chapter 2). To assist with this, Accreditation Canada offers services for organizations and health care teams to improve fall prevention strategies Footnote 3. In addition, the e-learning Canadian Falls Prevention Curriculum© was developed with funding from the Government of Canada for those working with older adults in long-term care, acute care and home care to acquire the knowledge and skills needed to apply an evidence-based approach to the prevention of falls and fall-related injuries Footnote 26.
5.4 Identified research gaps
This report is a summary of available data, literature and existing knowledge in the area of falls, fall-related injuries and fall prevention among seniors. It does not assess the validity of or recommend existing fall prevention approaches above any other. In their Cochrane review on fall prevention, Gillespie and colleagues noted that effective and validated falls interventions should be sourced from well-conducted, controlled trials Footnote 58. The report also does not validate prospective interventions or assess the relative importance of risk factors. However, in its development several gaps in knowledge surrounding fall prevention were noted.
As we have seen, much of the data available indicates high fall rates among women, whether they reside at home or in long-term care. These findings could be further explored with the knowledge that, on average, women live longer and there are more women in residential care, which may potentially be skewing the data. However, studies may still continue to reflect a higher incidence of falls and injury among women because of the increased likelihood of predisposing factors, such as osteoporosis, which presents another area of potential study.
The data suggests that there is a significant difference between younger old versus older old, and a difference between the sexes within these subpopulations. Narrowing down the risk categories more specifically by age and sex may shed light on how to better target fall prevention activities.
The data analysis also identified a need for heightened surveillance of falls while individuals are receiving health services in home care and/or in hospitals, as the primary focus to date has been on falls in residential care. While long-term care data are valuable, the report has shown that the majority of seniors do not reside in residential care facilities and that the majority of falls occur in the home (see Chapter 2). Evaluation of the effectiveness of the fall prevention materials available to plan for aging in place would also be important. Additional research assessing potential differences between rural and urban home settings may strengthen effective approaches.
There are also promising new approaches and interventions that are in their infancy and have yet to be assessed for efficacy, so have not been included in this report in any detail. Over the coming years, it will be important to monitor developments on how new technologies and assistive devices can be used to prevent falls. In addition, the shift from individual- to population-level interventions will need to be evaluated for effectiveness and may shed light on environmental risk factors, for example the WHO Safe Communities and Age-Friendly Communities projects.
5.5 Working together to build strength
Falls among older Canadians continue to be a public safety concern, and their wide-reaching consequences will only increase if the trend continues. Preventing falls among seniors is a shared responsibility and can only be achieved through continued multisectoral collaboration, including governments, health care providers, non-government organizations, care associations and services, as well as Canadians themselves.
Over the years, Canada has laid a foundation for good health and well-being across the life course Footnote 123. However as our population ages, fall prevention will continue to be an important public health issue for which focused efforts are required to maintain and improve the quality of life and well-being of seniors, ensuring that they continue to contribute and participate in society.
At the Public Health Agency of Canada (PHAC), our role is to promote the health of Canadians and to prevent and control diseases and injury through leadership, partnership, innovation and action in public health. Helping Canadians to make healthier choices is a shared responsibility. We work together with multiple levels of government, with stakeholders and researchers in order to encourage a sustained approach to health promotion that is based on the best available evidence. Injury prevention is a key public health concern, and PHAC has been the focal point at the federal level for seniors' falls.
PHAC has a history of playing a strong coordinating role with respect to fall prevention among seniors in Canada. To target the unique needs of seniors in preventing injuries due to falls, PHAC has undertaken several activities in public education, community-based programming and policy development. Working collaboratively with stakeholders, PHAC aims to increase the capacity of those who work with seniors to plan, implement and evaluate evidence-based injury prevention programs. Through the Canadian Best Practices Portal, PHAC provides program planners and public health practitioners with a comprehensive listing of resources for planning, implementing and evaluating programs designed to promote health and prevent chronic disease and injuries.
In addition, PHAC has developed a number of publications aimed at helping seniors and their families to reduce the occurrence and impact of falls. These publications are detailed below:
- Bruno and Alice - A Love Story in Twelve Parts About Seniors and Safety is a series of stories that offer insight into some of the personal preventive measures seniors can take to make their environment safer and prevent injuries. The goal of this publication is to promote a greater awareness of the issue of injury prevention for seniors. Over the last 14 years, this product has been converted into braille and audio formats, as well as adapted into a radio show and several theatre productions.
- If You Fall or Witness a Fall, Do You Know What to Do? is a pamphlet that provides important information to seniors and those working with seniors on the steps to take if they fall or witness a fall.
- You Can Prevent Falls! is a pamphlet that focuses on how seniors can prevent falls by making the needed adjustments to their homes and lifestyles, by eating well, staying fit and using devices that will facilitate their daily lives while keeping them safe.
- (The) Safe Living Guide - A Guide to Home Safety and Seniors is an award-winning publication that presents ideas on how to prevent injuries in and around the home. It provides information in the form of check lists, fact sheets and tips, as well as a resource section.
- Stay Safe! (poster) is an illustration of a senior's living room and contains 14 dangers that can cause seniors to fall or injure themselves.
- What to Do After a Fall… (poster) is an informative illustration detailing the steps to take after a fall or after witnessing a fall.
- 12 Steps to Stair Safety at Home is a one-page checklist that reminds seniors of the common hazards in stairways and the proper ways to set up and use their stairs.
As a way to facilitate healthy and supportive environments for older Canadians, PHAC actively promotes the Age-Friendly Communities (AFC) concept in Canada. Features of AFC include sidewalks that are well lit and kept in good shape, outdoor areas and public buildings that are safe and accessible, and housing that is safe and well designed for seniors. As key elements of a community's physical environment, outdoor spaces and buildings, and houses in particular, have a strong influence on personal mobility and safety from injury Footnote 180. Canadian communities are increasingly adopting AFC strategies to proactively prevent injury among seniors.
The Canadian Institute of Health Research (CIHR)'s Institute of Aging supports and promotes activities aimed at preventive strategies and lifestyle interventions. CIHR has supported a number of research projects focusing on the prevention of falls and associated injuries among seniors. In the Institute's view, these activities must integrate the biological, psychological, social and environmental determinants of health and wellness, while shedding light on the trajectory of aging in the individual. An integrative approach is crucial in order to truly comprehend not only each of these dimensions individually but also the dynamics and synergies among them. To this end, CIHR has continued its support for the Canadian Longitudinal Study on Aging (CLSA). The CLSA follows men and women aged 45 to 85 for a period of 20 years to better understand the aging process and the factors that shape the way we age, and to use that knowledge to improve the health of Canadians. CIHR has also made investments in research that explores and evaluates fall prevention practices.
Fall prevention initiatives and strategies are taking place in all provinces and territories and at the national level. To enhance the collaborative understanding of these initiatives, a National Fall Prevention Workshop was held at the 2010 Canadian Injury Prevention and Safety Promotion Conference Footnote 126. The objectives were to bring together federal, provincial and territorial leads interested in collaborating on evidence-based, clinically relevant programming, policy and practice to reduce the risk of falls and related injuries among older adults in Canada; to present model strategic fall prevention plan components; and to discuss current best practices and their application. Jurisdictions that reported having access to data were able to demonstrate a positive relationship between their fall prevention programs and a reduction in falls and fall-related injuries, although it was noted that lack of data and surveillance at the setting made it difficult to evaluate programs rigorously. Networks and coalitions were frequently referred to as an important medium for professionals to communicate about implementing fall prevention programming, while the education of health care providers was identified as a priority. Standardizing and integrating fall prevention training into postsecondary education was considered an important next step.
Effective fall prevention is a collaborative effort that pins its success on multifactorial intervention. In addition to government action, Canadians themselves can take and are taking action to prevent seniors' falls. Adoption of AFC strategies, active involvement in building code and civil planning, and proactive seniors' organizations are all good examples of Canadian achievements in this area. Public education campaigns are also a crucial tool to help seniors help themselves. Reaching seniors with awareness and education programs involves using various tools and methods of communication, such as information sessions with presentations, question and answer sessions, discussion periods and printed materials (pamphlets, newsletters). Group sessions can also be advantageous, as they encourage socialization, idea sharing and peer support. Together we are working towards better identifying causes, risks and concerns around falls, with the aim of reducing fall rates more effectively.
5.6 Summary
As a result of societal changes and the progress made in areas such as public health, health care, living conditions, social norms and individual choices, Canada has a vibrant aging society and one of the highest life expectancies in the world. Over the years, Canada has laid a foundation for good health and well-being across the life course Footnote 123. However as our population ages, fall prevention will continue to be a significant public health issue for which focused efforts are required to maintain and improve the quality of life and well-being of seniors.
The updated information contained in this report is essential for the design of effective fall prevention programs in Canada. Though falls are the most common cause of injuries among seniors, they are largely preventable through evidence-based interventions. In Canada there is an increased understanding of what puts seniors at risk of falling and what kind of fall prevention interventions work, for whom and in what setting. Promotion of healthy aging is about creating conditions for individuals to make choices and engage in behaviours that support fall prevention. In stepping up our coordinated efforts against falls, Canadians are working together to create a healthier environment in which to live and thrive.
Appendices
Appendix A: Distribution of CCHS sample with injury related to a fall by key demographic variables, age 65+, Canada, 2005 and 2003
| Injury Related to a Fall, 2005 | Injury Related to a Fall, 2003 | |||||||
|---|---|---|---|---|---|---|---|---|
| Pop. Estimate Footnote g | % | 95% Confidence Interval | Pop. Estimate Footnote i | % | 95% Confidence Interval | |||
| Lower | Upper Footnote h | Lower | Upper Footnote h | |||||
| Sex | ||||||||
| Male | 61,034 | 31.4 | 28.1 | 34.8 | 55,373 | 31.0 | 27.6 | 34.3 |
| Female | 133,102 | 68.6 | 65.2 | 71.9 | 123,382 | 69.0 | 65.7 | 72.4 |
| Age | ||||||||
| 65-69 | 49,181 | 25.3 | 21.8 | 28.9 | 39,440 | 22.1 | 19.2 | 24.9 |
| 70-74 | 41,277 | 21.3 | 18.6 | 23.9 | 44,527 | 24.9 | 21.4 | 28.4 |
| 75-79 | 46,186 | 23.8 | 20.2 | 27.4 | 45,098 | 25.2 | 20.8 | 29.6 |
| 80-84 | 29,353 | 15.1 | 12.6 | 17.6 | 27,838 | 15.6 | 13.5 | 17.6 |
| 85-89 | 20,099 | 10.4 | 8.1 | 12.6 | 17,200 | 9.6 | 7.4 | 11.8 |
| 90+ | 8,040 | 4.1 | 2.8 | 5.5 | 4,652 | 2.6 | 1.2 | 4.0E |
| Marital Status | ||||||||
| Married | 100,592 | 51.8 | 47.4 | 56.2 | 87,476 | 48.9 | 44.8 | 53.0 |
| Widowed | 69,984 | 36.0 | 32.3 | 39.8 | 67,497 | 37.8 | 34.1 | 41.4 |
| Separated/Divorced | 14,570 | 7.5 | 5.8 | 9.2 | 14,616 | 8.2 | 5.7 | 10.6 |
| Single, never-married | 8,907 | 4.6 | 3.2 | 6.0 | 8,619 | 4.8 | 3.2 | 6.5E |
| Not stated | (F) Footnote j | (F) | ||||||
| Education | ||||||||
| Less than secondary school graduation | 76,403 | 39.4 | 35.0 | 43.7 | 71,252 | 39.9 | 36.4 | 43.3 |
| Secondary school graduation | 28,856 | 14.9 | 11.5 | 18.2 | 32,191 | 18.0 | 14.8 | 21.2 |
| Some post-secondary | 11,481 | 5.9 | 4.1 | 7.7E | 11,042 | 6.2 | 3.8 | 8.5E |
| Post-secondary graduation | 72,526 | 37.4 | 33.7 | 41.0 | 61,206 | 34.2 | 31.0 | 37.5 |
| Not stated | (F) | 3,063 | 1.7 | 0.8 | 2.6E | |||
| Household Income | ||||||||
| Less than $15,000 | 22,584 | 11.6 | 9.8 | 13.5 | 26,799 | 15.0 | 12.9 | 17.1 |
| $15,000-$29,999 | 48,861 | 25.2 | 22.4 | 27.9 | 44,867 | 25.1 | 21.9 | 28.3 |
| $30,000-$49,999 | 38,953 | 20.1 | 17.3 | 22.8 | 38,138 | 21.3 | 17.7 | 25.0 |
| $50,000-$79,999 | 24,512 | 12.6 | 10.2 | 15.1 | 20,924 | 11.7 | 8.8 | 14.6 |
| $80,000 or more | 14,000 | 7.2 | 5.2 | 9.2 | 14,712 | 8.2 | 5.1 | 11.3E |
| Not stated | 45,225 | 23.3 | 19.1 | 27.5 | 33,315 | 18.6 | 15.7 | 21.6 |
Appendix B: Factors associated with an increased risk of falling among older adults
| Biological/Intrinsic | Behavioural | Social & Economic | Environmental |
|---|---|---|---|
|
|
|
|
Updated from: Scott, Dukeshire, Gallagher, & Scanlan Footnote 143.