Adverse Events Following Immunization (AEFI) Quarterly Report for 2015 – Q2
Safety assessment summary for Quarter 2:
- No vaccine safety signals were identified in Quarter 2 of 2015.
- All AEFI reports describing a serious event were reviewed and most found either to be expected (based on known vaccine-related adverse reactions) or to have alternate explanations not related to vaccination.
- As in recent quarterly reports, the total count of AEFI reports received remains lower than seen in historic data, reflecting a gap in reporting from some jurisdictions that are implementing electronic reporting systems.
Preamble
Vaccines are closely monitored in Canada at all phases of the vaccine product ‘life cycle’ from discovery through market authorization (pre-market) and beyond, as people begin using them (post-market). Many stakeholders are involved in various activities related to vaccine safety assessment and monitoring including the federal government, provincial, territorial and local public health authorities, health care providers, vaccine industry and the public. The Public Health Agency of Canada (the Agency) conducts vigilant post-market safety surveillance through a national reporting system, the Canadian Adverse Events Following Immunization Surveillance System (CAEFISS).
An Adverse Event Following Immunization (AEFI) is defined as any untoward medical occurrence which follows immunization and which does not necessarily have a causal relationship with the usage of the vaccine. The adverse event may be any unfavorable or unintended sign, abnormal laboratory finding, symptom or disease. Serious AEFI are those which are life-threatening, result in hospitalization or a prolongation of hospitalization, result in persistent or significant disability, or where the outcome is a birth defect or death.
The primary purpose of vaccine post market surveillance is to detect safety concerns. These concerns include a possible increase in the severity or frequency of expected AEFIs, or occurrence of one or more unexpected events (i.e. an event that is not consistent with Canadian product information or labelling). This allows immunization providers and public health immunization program providers to take public health action at the level of the:
- individual (e.g. further investigation to confirm a diagnosis and determine possible causes, consultation to rule out allergy to one or more vaccine components, or evaluate whether or not to give subsequent doses of a vaccine), and/or
- immunization program (e.g. investigation of a cluster of adverse events, review of procedures to ensure that vaccine storage requirements have been strictly followed, or consider a change in policy to adopt a less reactogenic vaccine).
The Agency also shares AEFI data with Health Canada, the vaccine regulator in Canada, to enable regulatory action related to vaccines marketed in Canada. These actions may include issuing communications to immunization providers or the public regarding the safety concern or requiring additional information or investigation by the vaccine distributor.
Vaccine safety surveillance reports summarizing CAEFISS data are released by the Agency on a routine basis. The Quarterly Reports summarize all AEFI reports received by the Agency from January 1st to March 31st (Quarter 1), April 1st to June 30th (Quarter 2), July 1st to September 30th(Quarter 3) and October 1st to December 31st (Quarter 4), regardless of the date the vaccine was given. In addition, the Quarter 4 Report provides cumulative data spanning the entire year and contains a more detailed review of any concerns that may have been observed in the earlier reports.
In order to provide a general idea of how the data may vary from year to year, each Quarter’s data are shown along with an average of the preceding prior years’ Quarterly data (in other words, the data in this quarter, Quarter 2, are shown along with the average Quarter 2 data from previous years). However, because these data reflect reports received in the particular quarter, and not necessarily when the vaccine was given, they can be subject to wide variations depending on when and how reports are received, processed and forwarded by provincial/territorial public health authorities. Therefore the ability to compare and interpret patterns in these data are limited and the purpose of this report is to provide only a data snapshot.
Notes on interpretation: AEFI reports submitted to the Public Health Agency of Canada represent a suspicion, opinion or observation by the reporter as opposed to an assertion or proof that the vaccine may have caused the event. For most events, a clear causal relationship is difficult to establish. Additional limitations to AEFI report data include varied reporting standards and underreporting, lack of certainty regarding the diagnostic validity of a reported event, missing information regarding other potential causes, and other reporting biases.
Results Highlighted for Quarter 2 of 2015
Counts included in this Quarterly Report (Q2) include reports received from April 1st to Jun 30th, 2015 and comparisons are made to the average number of reports received in the same quarter over the previous four years (2011-2014). The reports analysed were extracted from the CAEFISS database on June 30th, 2015 by the Public Health Agency of Canada (the Agency).
Number of AEFI and Serious AEFI Reports
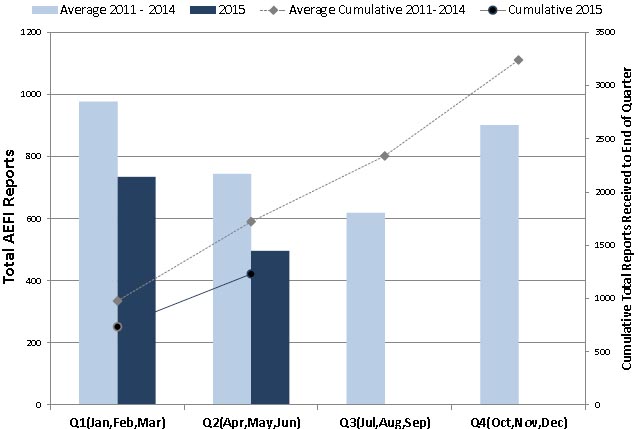
Figure 1: Total AEFI Reports by Quarter and cumulative to end of each Quarter: 2015 vs. average for 2011-2014
A total of 496 AEFI reports were received by the Agency in Q2 of 2015. During Quarter 2 of 2011, 2012, 2013 and 2014 the Agency received an average of 744 (range: 455-884) reports. The main reason for the drop continues to be related to delayed report transmission from one or more provinces and territories to the Agency over the past few years, for technical reasons related to implementing new electronic databases. Nevertheless, all reports are reviewed and analysed in their reporting jurisdictions and any concerns are communicated via provincial/territorial focal points on the pan-Canadian Vaccine Vigilance Working Group (VVWG). Therefore these delays do not substantially affect overall vaccine safety monitoring in Canada.
Text Equivalent
This is a combination bar and line graph. The bars show the total number of AEFI reports received each calendar quarter(Q) with Q1 encompassing January, February and March, Q2 April, May and Jun, Q3 July, August and September and Q4 October, November and December. The line shows the accumulated total reports to the end of each quarter. The primary y-axis on the left hand side of the graph is for the bar graph and shows the total count for each quarter, ranging from 0-1200. The secondary y-axis on the right hand side of the graph is for the line graph and shows the accumulated total count to the end of each quarter, ranging from 0 to 3500. The x-axis is quarter and ranges from Q1 to Q4. Two time periods are depicted on the graph.
The light bars show the average total reports each quarter from 2011 to 2014: 977 in Q1, 744 in Q2, 619 in Q3 and 902 in Q4. The dotted line shows the average cumulative total reports received by the end of each quarter for the same four years: 977 in Q1, 1721 by the end of Q2, 2340 by the end of Q3 and 3242 by the end of Q4.
A second, dark bar for Q1 and Q2 only, shows the total reports received in 2015: 741 during Q1 and 496 during Q2. The solid line starts with a dot for Q1, showing that a cumulative total of 741 reports were received by the end of Q1, 2015, and ends by a dot for Q2, showing a cumulative total of 1237 reports received by the end of Q2, 2015.
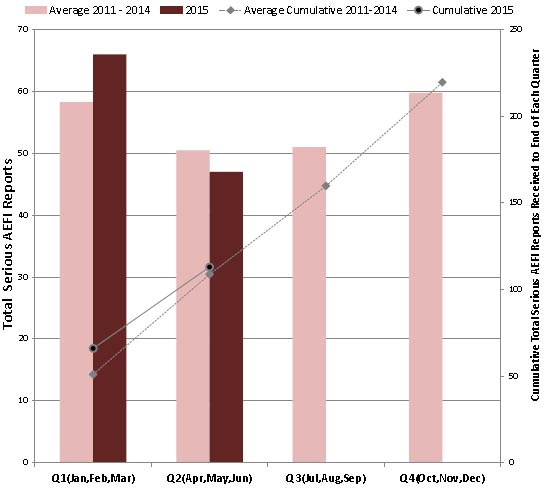
Figure 2: Total serious AEFI reports by Quarter and cumulative to end of each Quarter: 2015 vs. average for 2011-2014.
A total of 47 AEFI reports received by the Agency in Q2 of 2015 were classified as serious (9.5% of all AEFI reports). During Quarter 2 for 2011, 2012, 2013 and 2014 the Agency received an an average of 51 (range: 39-59) serious AEFI reports representing from 5.7 – 8.6% of all AEFI reports received in Quarter 2 for these years.
Text Equivalent
This is a combination bar and line graph. The bars show the total number of serious AEFI reports received each calendar quarter(Q) with Q1 encompassing January, February and March, Q2 April, May and Jun, Q3 July, August and September and Q4 October, November and December. The line shows the accumulated total reports to the end of each quarter. The primary y-axis on the left hand side of the graph is for the bar graph and shows the total count for each quarter, ranging from 0-70. The secondary y-axis on the right hand side of the graph is for the line graph and shows the total count to the end of each quarter, ranging from 0 to 250. The x-axis is quarter and ranges from Q1 to Q4. Two time periods are depicted on the graph.
The light bars show the average total reports each quarter for 2011 to 2014: 58 in Q1, 51 in Q2, 51 in Q3 and 60 in Q4. The dotted line shows the average cumulative total reports received by the end of each quarter for the same years: 58 for Q1, 109 by the end of Q2, 160 by the end of Q3 and 220 by the end of Q4.
The dark bar shows the total reports received each quarter for 2015: one bar at 68 for Q1 and one at 47 for Q2. The solid line shows that a cumulative total of 68 and 115 reports were received by the end of Q1, and Q2, 2015, respectively.
Frequency of Serious and Non-serious AEFI Reports by Age Group
Again in Quarter 2, there were changes in the age distribution for serious AEFI reports received relative to previous years. As shown in Table 1, the proportion of all serious AEFI reports for children one to less than two years of age was higher in Quarter 2 of 2015 than the previous four year average (19 versus 13). This change may be due in part to the recent implementation of new hexavalent vaccines (DTaP-IPV-HB-Hib), which typically have increased AEFI reporting rates. (See Table 3 below).
| Age Group | Serious Adverse Events (SAE) | Non-serious Adverse Events (non-SAE) | ||
|---|---|---|---|---|
| 2015 | Mean for 2011-2014 | 2015 | Mean for 2011-2014 | |
| Unknown | 0 | 1 | 4 | 1 |
| 65+ years | 0 | 4 | 50 | 42 |
| 18-<65 years | 2 | 6 | 160 | 182 |
| 7-<18 years | 4 | 4 | 93 | 113 |
| 2-<7 years | 8 | 7 | 38 | 95 |
| 1-<2 years | 14 | 16 | 59 | 130 |
| 0-<1 year | 19 | 13 | 45 | 121 |
Type of AEFI Reported by Level of Seriousness
The main type of AEFI reported by level of seriousness for Quarter 2 of 2015 compared to the 2011-2014 average is shown in Table 2. As in previous years, neurologic events (most often seizure) followed by systemic events (i.e., events involving many body systems often accompanied by fever), were the most frequently reported serious AEFIs in Quarter 2 of 2015.
| Main AEFI reported | Number of Serious Adverse Event Reports | Number of Non-serious Adverse Event Reports | ||
|---|---|---|---|---|
| 2015 | Average for 2011-14 | 2015 | Average for 2011-14 | |
| Reaction at or near the vaccination site | 2 | 7 | 207 | 255 |
| Allergic or allergic-like events | 0 | 2 | 44 | 78 |
| Neurologic events | 17 | 22 | 12 | 26 |
| Rash only | 0 | 1 | 97 | 156 |
| Other events specified on the CAEFISS form | 5 | 6 | 19 | 33 |
| Systemic events | 12 | 10 | 39 | 71 |
| Vaccination anxiety related events | 0 | 0 | 6 | 7 |
| Miscellaneous other events | 11 | 5 | 25 | 56 |
| Vaccination error without an associated AEFI | 0 | 0 | 0 | 13 |
Most common vaccines administered in AEFI Reports
Table 3 lists the most commonly administered vaccines among AEFI reports received for Quarter 2 of 2015 relative to the average for Quarter 2 of 2011-2014. The most notable change, as pointed out above, was a higher number of serious AEFI reports following several vaccines including DTaP-HB-IPV-Hib, PneuC and Rota, and of non-serious AEFI following zoster, all having increased distribution. As newly introduced vaccines, their use is greater in recent quarters relative to the average that includes older quarters.
| Vaccines administered | Number of Serious Adverse Event (SAE) Reports Received | Number of Non-Serious Adverse Event (non-SAE) Reports Received | ||
|---|---|---|---|---|
| 2015 | Average for 2011-14 | 2015 | Average for 2011-14 | |
Table 3 Footnotes
Totals add up to more than the total number of reports as one report may involve more than one vaccine. DTaP-HB-IPV-Hib - Combined Diphtheria and Tetanus Toxoids, Acellular Pertussis, Hepatitis B (recombinant), Inactivated Poliomyelitis and adsorbed conjugated Haemophilus influenzae type b. DTaP-Hib - Diphtheria and Tetanus Toxoids, acellular Pertussis, Haemophilus influenzae type b. DTaP-IPV - Component Pertussis vaccine and Diphtheria and Tetanus Toxoids adsorbed, combined with Inactivated Poliomyelitis vaccine. DTaP-IPV-Hib - Diphtheria and Tetanus Toxoids and Acellular Pertussis Vaccine Adsorbed, Combined with Inactivated Poliomyelitis Vaccine and Haemophilus b Conjugate Vaccine. |
||||
| Cholera-Ecoli oral (Chol-Ecol-O) | 0 | <1 | 2 | 3 |
| DTaP-HB-IPV-Hib | 15 | 4 | 31 | 47 |
| DTaP-Hib | 1 | <1 | 0 | <1 |
| DTaP-IPV | 2 | 1 | 12 | 43 |
| DTaP-IPV-Hib | 5 | 10 | 35 | 117 |
| HA (Hepatitis A) | 0 | <1 | 9 | 15 |
| HA-Typh (HA Typhoid) | 0 | 0 | 2 | 2 |
| HAHB (Hepatitis A Hepatitis B) | 0 | 1 | 21 | 27 |
| HB (Hepatitis B) | 1 | 2 | 35 | 48 |
| HPV (Human Papilloma Virus) | 0 | 2 | 28 | 48 |
| Hib (Hemophilus influenza type b) | 0 | <1 | 5 | 2 |
| Inf (Influenza) | 11 | 9 | 52 | 99 |
| MMR | 7 | 10 | 49 | 107 |
| MMR-Var (MMR-Varicella) | 8 | 8 | 28 | 29 |
| Men (Meningococcal) | 1 | <1 | 0 | 0 |
| Men-B | 0 | 0 | 13 | <1 |
| MenC (Men Conjugate) | 14 | 15 | 60 | 130 |
| MenP (Men Polysaccharide) | 0 | <1 | 1 | 0 |
| Pneu (Pneumococcal) | 0 | <1 | 3 | 0 |
| PneuC (Pneu Conjugate) | 25 | 19 | 56 | 156 |
| PneuP(Pneu Polysaccharide) | 1 | 5 | 41 | 36 |
| Rota(Rota virus) | 15 | 6 | 19 | 34 |
| Rab (Rabies) | 0 | 0 | 4 | 10 |
| Td (Tetanus diphtheria | 0 | <1 | 9 | 16 |
| Td-IPV (Adult Tetanus Inactivated Polio) | 0 | 0 | 1 | 3 |
| Tdap (Adult Tetanus diphtheria acellular Pertussis) | 1 | 2 | 44 | 72 |
| Tdap-IPVTable 3 Footnote * | 1 | 0 | 11 | 18 |
| Var (Varicella) | 4 | 6 | 20 | 81 |
| YF (Yellow Fever) | 0 | <1 | 4 | 5 |
| Zos (Zoster) | 0 | <1 | 58 | 17 |
Summary
This Quarter 2 report of four planned for 2015 is based on reports of adverse events received at the Agency from provincial/territorial public health authorities and active, pediatric hospital based surveillance. Detailed evaluation of the reports and reporting patterns in collaboration with provincial/territorial vaccine safety focal points on the VVWG and Health Canada have not identified any vaccine safety signals of concern. The tables and figures in this report provide a snapshot of the data reviewed and provide an overview of vaccine safety reporting in Canada.