Summary of the clinical review of the cases of infant misidentification at Norway House Hospital
Prepared for Health Canada
By: David Creery, MD, MSc, FRCPC, MHSc
Maura Davies, BSc, BEd, MHSA, FCCHL
Revised May 25, 2017
Table of Contents
- Executive Summary
- 1. Introduction
- 2. Methodology
- 3. Background
- 4. Maternal Care in 1975
- 5. Contributing Factors
- 6. Infant and Maternal Identification at Norway House Hospital in 1975
- 7. Infant and Maternal Identification at Norway House Hospital in 2017
- 8. Infant and Maternal Identification at a Tertiary Care Birthing Centre in 2017
- 9. Conclusions
- 10. Recommendations
- 11. Limitations
- 12. Acknowledgments
- Appendices
Download the alternative format
(PDF version, 752 KB, 27 pages)
- Organization: Health Canada
- Type: Report
- Published: 2017-08-08
Executive Summary
In 1975, two pairs of individuals born at Norway House Hospital were misidentified shortly after birth and raised by their non-biological parents. Although the circumstances of the two incidents were different, the major factors that resulted in these errors were similar. Based on a review of documents and interviews with many individuals, it appears that the newborn identification process used at Norway House Hospital in 1975 was insufficient to ensure accurate identification (ID) of infants. The identification band procedure was not used consistently. The identification bands were not routinely placed on the baby in the room where the baby was delivered.
Although Norway House is no longer designated as a birthing centre, a small number of emergency deliveries still occur at the hospital. Practices have changed considerably since 1975, including adoption of Rooming In, whereby the mother and baby are kept in the same room. An infant identification process is now in place, using identification bands. However, current practice at Norway House Hospital still poses some risks for error. Therefore it is recommended that Norway House Hospital and any other Health Canada facility where births occur:
- Implement number-matched four-band mother-infant bracelet system, such as Ident-a-Band®, with two bands on the baby (ankle and wrist);
- Apply identification bands to the infant, mother and mother's partner (if present) in the delivery room immediately after birth, or as quickly as the clinical situation allows;
- Train hospital staff to be highly compliant with the above process, with regular performance audits.
The circumstances involved in these cases had tragic results for the mothers, the babies and their families. There is no way of knowing whether these two incidents were unique.
Review of these incidents was made possible because of the willingness of the individuals most affected to tell their stories. This often brought back painful memories. The reviewers hope that this report provides answers that can help the healing process and lead to practice changes that prevent misidentification of newborns ever happening again at Norway House Hospital or other Health Canada facilities.
This summary report excludes detailed personal information specific to each case, which will be shared with the individuals involved.
1. Introduction
In 2015 Health Canada was informed that DNA tests confirmed that two individuals were raised by their non-biological parents/families after discharge as newborns from Norway House Hospital in 1975. In 2016 Health Canada was informed that DNA tests confirmed that a second switched at birth incident had occurred at the same hospital in 1975Footnote 1. Health Canada responded by stating that it took this issue very seriously and was committed to supporting the individuals and families affected by these traumatic events. On November 21, 2016, the Honourable Jane Philpott, Minister of Health, met with the individuals, their families and representatives to discuss these incidents and to understand the impacts on the men and their families. Health Canada committed to conduct an independent, third-party review of the circumstances that led to these incidents. The Department committed to making the results of this case review public.
This independent review was conducted by Dr. David Creery and Ms. Maura Davies. Dr. Creery is the Medical Director of Patient Safety at the Children's Hospital of Eastern Ontario (CHEO) in Ottawa, Ontario, and an Investigating Coroner in Ontario. Ms. Davies is the former President and CEO of the Saskatoon Health Region and has extensive experience in delivery of health services and patient safety. Dr. Creery and Ms. Davies worked in collaboration with many individuals, including the family physicians for the affected men, who provided insight into Norway House Hospital and community, and who continue to provide support to the men and their families.
The purpose of the Norway House Hospital Case Review was to:
- Identify facts and circumstances with regard to the clinical setting and practices when the births occurred;
- Identify factors that contributed to the errors;
- Identify risks that still exist or could exist at Norway House or other federal health facilities related to patient identification, based on the Norway House Hospital experience.
On October 7, 2016, Health Canada learned that the RCMP would be initiating an investigation into the same cases in Norway House. While the RCMP's activities are independent of the present review, Health Canada committed to fully cooperate with the RCMP investigation.
2. Methodology
Health Canada and the independent reviewers committed to conduct the case review in a manner that was sensitive to and respectful of the affected individuals, their families and communities. The methodology used for the case review was grounded on a systems approach to adverse analysis, as pioneered by the esteemed patient safety leader, Dr. James Reason.
Dr. James Reason is a British psychologist whose analysis of industrial accidents revealed that safety failures are almost never caused by isolated errors by individuals but usually result from multiple smaller errors in environments with serious underlying systems failures (AHRQ, 2015). In this model, first published in 2000, it is acknowledged that human error is inevitable, especially in complex systems such as health care, but that errors can often be prevented if the system is organized to catch errors before they occur. Adverse events occur when safety gaps, many of which are relatively minor in isolation, line up like the holes in a series of pieces of Swiss cheese, allowing a harmful outcome to occur (See Figure 1).
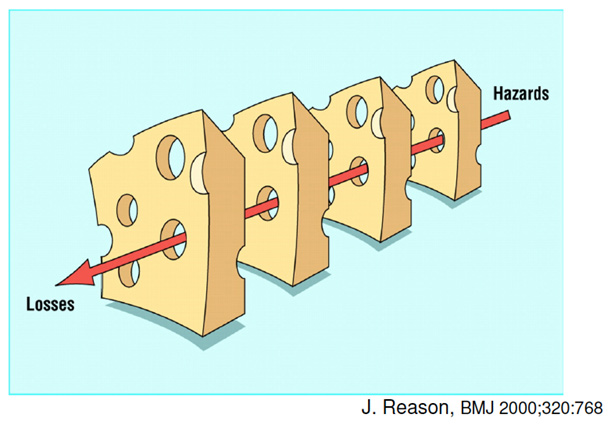
Figure 1 - Text Equivalent
The James Reason Swiss Cheese Model shows that adverse events occur when many safety gaps (which in isolation are relatively minor) line up like the holes in a series of pieces of Swiss cheese.
Using this model as a foundation for the case review meant that the reviewers would be examining many potential factors, including but not limited to human error, which could have contributed to the two incidents, each involving two babies who were misidentified in a small northern hospital in the same year.
The review was designed to involve two phases:
Phase 1
- Chart reviews: The birth records of the four men and the record of their mothers’ hospital stays were reviewed. Particular attention was paid to evidence related to measures taken to identify the infants and extenuating circumstances that may have contributed to misidentification.
- Policy review: Policies related to patient identification at Norway House Hospital and federally-owned hospitals during the period 1970-1980 were sought and compared to processes actually used as documented in the charts reviewed for that period. The policy in place at Thompson Hospital during the same period was examined for comparison purposes. Finally, past practices for infant identification were compared to current standards of practice.
- Document review: Other documents related to Norway House Hospital during the period 1970-1980 were reviewed to assist in understanding local context and possible contributing factors related to the errors.
- Stakeholder interviews: Key stakeholders were interviewed to explore their recollection and knowledge about Norway House Hospital care delivery during 1970-1980 and the circumstances related to the two incidents. Interviewees were to include, subject to their availability and willingness to be interviewed, the four individuals switched at birth, members of their families, current Norway House Hospital clinical and administrative staff, and professional staff involved in the care of the newborns during their hospital stay in 1975.
- Hospital tour: Norway House Hospital was visited to identify the layout of the building and patient flow, with a view to identifying structural and process factors that may have contributed to the errors.
- Root cause analysis: Evidence obtained from the hospital records and other documents and stakeholder interviews were used to:
- Develop a timeline of the events associated with the two errors;
- Identify factors that may have contributed to misidentification;
- Identify additional information that would be helpful in understanding what happened and why.
- Identification of leading practices: Contact was made with The Ottawa Hospital, the Saskatoon Health Region and the Izaak Walton Killam Hospital in Halifax, Nova Scotia. Information related to Accreditation Canada standards and infant misidentification cases registered in the Canadian Patient Safety Institute Global Safety Alerts was also reviewed.
- Preliminary report: A preliminary report was prepared for review by Health Canada. Minor edits were made to the draft report to provide greater clarity and to incorporate additional information gathered through contact with former staff.
- Debriefing with the families: Meetings were held in Winnipeg and Norway House with family members to review the draft findings and identify any errors or additional information to be added to the final report.
- Final report: The report was edited and submitted to Health Canada. Although a great deal of personal health information was examined by the reviewers and individuals consented to being interviewed, efforts have been made to minimize the amount of personal health information in this report.
Phase 2
Based on the preliminary findings from Phase 1, discussion will be held with Health Canada regarding the potential value and feasibility of doing a broader case review of other births at Norway House Hospital. This will need to factor in issues related to patient privacy and confidentiality and the practical and ethical challenges of identifying the second individual in a pair of switched infants, if non-maternity for one individual is found on DNA testing.
3. Background
History of Norway House (based on October 1977 Norway House Hospital Role Study and 1983 Norway House Base Review)
Norway House Hospital (originally known as Norway House Indian Hospital) was built in 1952, replacing an earlier facility. The hospital, which is situated on 17.5 acres on Fort Island in Norway House, was built as a 20-bed acute care general hospital serving the Indigenous populations of Norway House and several other remote rural reserves. The hospital was, and remains, owned and operated by the federal government.
In 1977 the population of Norway House was approximately 3000, consisting of 2300+ Registered Indians, and 575 Metis and others. The Base Review noted that the health care staff working at the hospital were physically, psychologically and philosophically isolated from the community. Health care delivery was described as fragmented. Mental health care for the population was identified as a major issue. Other community health problems included a high rate of violent deaths, poor housing and sanitary systems, limited access to services including transportation and a high turnover of health care professionals, resulting in challenges in continuity of care (Health Canada Base Review, 1983).
At that time, the hospital was designated as a birthing centre. In 1974, 211 of the 303 births by women living in Norway House and the surrounding area occurred at Norway House Hospital. Expectant mothers were expected to live in Norway House for the weeks prior to their expected delivery date. Mothers from other communities were usually housed in boarding rooms, far removed from their families and community supports. Many mothers, especially those living in more remote communities, had little, if any, prenatal care. Complex cases were referred to Winnipeg, although emergency caesarian sections were done at Norway House Hospital.
Up until 1975, the hospital was serviced by physicians under contract with private clinics. During 1976, the hospital was serviced by physicians under individual contracts and a few physicians provided by the Northern Medical Unit (NMU). From January 1977 onward, the NMU has provided all physician and allied health services.
The 1983 Base Review of Norway House Hospital noted that no health care professionals employed at Norway House spoke the local language, even though the 1977 role study recommended an increase in indigenous staff and provision of services in the local language. Opportunities for professional development of staff were very limited. Nursing and physician turnover and staffing shortages were frequent. The average length of stay for a nurse working at Norway House Hospital between 1972 and 1975 was just over one year.
Ancillary staff (i.e. non-professional staff such as aides and orderlies), were usually from the local Indigenous community. They spoke the local language, provided interpreter services and contributed valuable information about patients and their living conditions which assisted the professional staff. (Health Canada Norway House Hospital Role Study 1977).
A 1975 survey of people served by the hospital noted a high level of dissatisfaction with the hospital and a lack of confidence in the treatment provided. (Report on the Norway House Hospital Attitude Survey, 1975) The survey report stated that hospital staff were viewed with suspicion by members of the public, who felt staff lacked appropriate qualifications and gave second rate service. In contrast, another 1975 Health Canada document on Norway House Hospital operations stated that the hospital "appears to be well received by the community" and that the hospital was generally "looked upon as doing a good job" by the people in Norway House and neighbouring communities. (Health Canada Norway House Operations Report, 1975).
In 1983, the hospital operated 12 adult and pediatric beds and 4 cribs, serving a population of 3488. Outpatient services were also provided, including the antepartum clinic. The reduction in beds was attributed to increased use of facilities in Thompson and Winnipeg. Even with the reduction in beds, hospital occupancy was low, which was not unusual in small remote northern facilities. The Base Review was intended to address more efficient utilization of the hospital and hospital resources.
4. Maternal Care in 1975
Information about maternal care at Norway House Hospital in 1975 was obtained through review of documents, interviews with current and former hospital staff, and interviews with women (including three of the mothers involved in these cases) who received care at Norway House Hospital. Based on this information, it appears that in 1975, provision of obstetrical care normally involved (or was supposed to involve) the following:
- The mother was admitted to and laboured in a labour room. She was transferred to the delivery room (case room) when the birth was imminent. If the delivery room was already in use by another mother or if the birth happened quickly, the delivery was done in the labour room (with a curtain separating the mothers sharing the room). After delivery the mother was transferred to the ward;
- High risk patients were transferred to Thompson or Winnipeg prior to delivery. Emergency caesarian sections were done at Norway House Hospital, if required. Mothers and/or newborns requiring urgent specialist care were airlifted by Medivac to the Winnipeg Health Sciences Centre. A Norway House Hospital nurse usually accompanied the patient being transferred;
- Immediately after delivery, the newborn was assessed, assigned an APGARFootnote 2scores, weighed, placed in an incubator or bassinet and taken to the nurseryFootnote 3;
- In the nursery the newborn was placed in a bassinet, which was labeled with the infant's gender and mother's last name. The newborn was bathed, measured and received an identification (ID) bracelet (usually placed on the infant's ankle). The ID bracelet identified the last name of the baby (e.g. Newborn Male Smith) and possibly the mother's first name (the reviewers were not able to confirm this).Footnote 4 The ID band remained on the infant at the time of discharge;
- The infants were brought from the nursery to their mothers for feeding. It was not unusual for breast milk to be supplemented with glucose and water and/or formula. Nursing staff sometimes bottle fed the babies, to allow the mothers to rest and recover, especially if there had been a difficult delivery or if the mother was having difficulty breastfeeding. This meant that some mothers, especially those who were not breastfeeding, had limited contact with their babies during the hospital stay;
- Mother and baby were usually discharged to home after 3-4 days, with a recommendation for follow-up in the local clinic or nursing station.
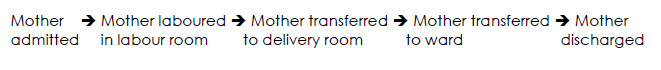
Figure 2 - Text Equivalent
This figure outlines the process map for a mother’s hospital stay. The mother is first admitted and laboured in a labour room. The mother is then transferred to the delivery room. After delivery, the mother is transferred to the ward and then discharged.
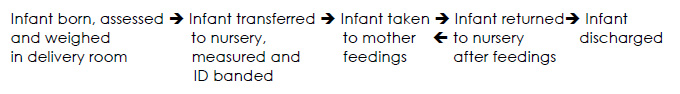
Figure 3 - Text Equivalent
This figure outlines the process map for an infant’s hospital stay. The infant is born, assessed and weighed in the delivery room. The infant is then transferred to the nursery to be measured and ID banded. The infant is taken to the mother for feedings and then returned to the nursery after feedings. Finally, the infant is discharged.
Conflicting reports from different people interviewed during this review about the processes used in 1975 may reflect different recollections of events that occurred more than 40 years ago. The reviewers also believe that the differences in information from various sources probably reflect that practices such as applying and checking ID bands were not consistently used.
It is noted that the birth records and patient charts reviewed as part of the Clinical Review varied considerably in the quality of documentation. In some cases key information (e.g. daily infant weights, reference to breastfeeding) was not recorded. Only one of the four mother's hospital chart contained a completed labour and delivery form. Sometimes information was inaccurate (e.g. length of a newborn recorded as 32 cm). Changes to some records appear to have been made (e.g. changes to the recorded gender and weight of one of the babies). These changes appear to have been made in the same ink and handwriting as the original note and therefore the reviewers assume that the changes were made at or shortly after the time care was recorded.
Although there were patterns in the delivery of care (e.g. administration of ascorbic acid to the newborn on Day 3), there do not appear to have been written policies or standard work describing how some processes e.g. infant identification were to be done. It appears that some important practices e.g. use of infant identification bands were inconsistent and not performed in every case.
With approximately 250-300 births per year, often clustered tightly over a short period of time, the obstetrical service was sometimes very busy, especially if a caesarian section was involved or the unit was short-staffed.
5. Contributing Factors
A cause and effect diagram, also known as a fishbone or Ishikara diagram, is a graphic tool used to display the causes of a given effect. The causes are typically grouped into categories, which can be modified to fit the event under review. In considering the causes of the two infant misidentification events at Norway House Hospital in 1975, the case reviewers grouped the causes into People, Processes, Equipment, and Environment.
To protect the privacy of individuals, some contributing factors specific to each case are not included in this summary report.
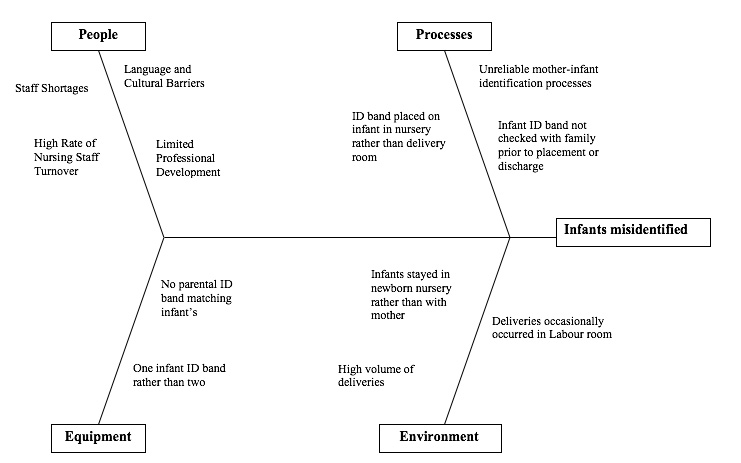
Figure 4 - Text Equivalent
This figure shows a cause and effect (or fishbone) diagram of contributing factors. It shows that, in considering the causes of the two infant misidentification events at Norway House Hospital in 1975, the case reviewers grouped the causes into people, processes, equipment, and environment.
Under people: language and cultural barriers, staff shortages, high rate of nursing staff turnover and limited professional development.
Under processes: unreliable mother-infant identification process; ID band placed on infant in nursery rather than delivery room; and infant ID band not checked with family prior to placement or discharge.
Under equipment: no parental ID band matching infant’s and one infant ID band rather than two.
Under Environment: infants stayed in newborn nursery rather than with mother, deliveries occasionally occurred in the labour room, and high volume of deliveries.
People
- Language and cultural barriers may have been a contributing factor. According to community members and staff working at Norway House Hospital at the time, the nurses working during the period of both events were not of First Nations origin and did not speak the language of the community.
- Compared to now, patients in 1975 were less empowered to raise concerns about their care or to challenge information provided by professional staff. This may have been particularly true for young First Nations women being cared for by non-First Nations staff. Based on interviews with some stakeholders, the reviewers believe that this may have contributed to the Norway House Hospital infant misidentifications, although the extent to which it did so is not known.
- Staff shortages were common at Norway House hospital at the time these events occurred, but it is not known whether staff shortages contributed to these events.
- Nursing staff had a high turnover rate at the time (average length of tenure less than one year). This would create challenges for nursing staff to establish standard processes, and to respond appropriately to unanticipated events such as power outages or periods of high patient census.
- There were limited opportunities for professional development at that time, creating challenges in introducing current leading practices;
Processes
- Infant/mother identification processes were not robust or reliable when these events occurred. The reviewers heard from multiple interviewees that the identity band was not routinely placed on the infant immediately after birth in the room where the infant had been born;
- Interviewees did not recall a standard process for confirming the baby's identity with the mother or another family member prior to the band being placed;
- Only one band (rather than both ankle and wrist bands) was placed, creating a risk for infant misidentification if the band were to fall off (which sometimes occurs, especially in very small infants).
Equipment
- A single, hand-written infant band was placed on the infant. Current leading practice is to have four number-matched bracelets produced - two for the infant, one for the mother and one for the mother's partner.
Environment
- At the time of these events, infants typically stayed in the newborn nursery, not in the mother's room as is the current practice (Rooming In). Infants were taken regularly to the mother's room for feeding and other care, although some bottle-feeding was done by nursing staff. Multiple identification events were needed each day;
- In general, infants were born in the delivery room, which contained only one mother at the time of delivery. In cases where mothers delivered in the same labour room, an additional risk of misidentification occurred;
- The birthing unit of the Norway House Hospital was very busy at the time both events occurred. During the entire month of January 1975, 19 mothers had babies. For the period when the Swanson and Tait babies were born, six babies were born in a 24-hour period. During the entire month of June 1975, 26 mothers had babies. In the Barkman/Monias situation, five babies were born in a 24-hour period. Four of the babies were born within a 12-hour period. This very likely created stresses for staff in terms of adhering to normal protocols. It also resulted in a large number of infants residing in the newborn nursery at the same time, increasing the probability of misidentification.
6. Infant and Mother Identification at Norway House Hospital in 1975
The reviewers were not able to identify and review written policies or procedures specific to infant/mother identification from the period the two cases of misidentification occurred - it is likely none existed at that time. Nurses interviewed by the reviewers had very limited recollection of what constituted standard practice in 1975. Important information was obtained through multiple interviews of women who delivered at Norway House Hospital during this period.
As noted above, the practice in 1975 was that, following delivery of a healthy newborn in the delivery room (i.e. not requiring resuscitation), the infant would be placed in an incubator or bassinet and transported to the nursery to be weighed and measured. According to multiple but not all sources, an identification bracelet, on which the mother's name and the baby's gender would be written, would be placed on the infant's ankle. The infant's bassinet would also be labeled. The ankle bracelet would stay on until the infant was discharged home.
7. Infant and Mother Identification at Norway House Hospital in 2017
The reviewers met with the Nurse in Charge at Norway House, and toured the birthing area. During this tour, information was provided regarding the previous layout of the obstetrical service and the size and location of the nursery.
The number of annual births at Norway House has decreased dramatically over the past few years. In 2016, for example, only 8 babies were born there, and in only one month (February) was more than one infant born. This indicates that the risk for misidentification of babies is currently very low. However, according to staff, there are busier times of the year (usually over the Christmas holidays and during the August festival period), so the potential for infant misidentification still exists. Also, in general terms, events that occur rarely are more difficult to perform with a high degree of reliability.
Currently at Norway House, all deliveries are considered emergencies. If the infant cries immediately, he or she is placed on the mother's chest to allow for bonding. If the infant does not cry immediately, he or she is transferred to the over-bed warmer in the delivery room for resuscitation. Once stable, the infant is wrapped and given to the mother for bonding. The infant is kept in the delivery room until the mother is stable and is having a normal postpartum recovery period. Prior to transfer out of the delivery room, an ankle bracelet written with non-smear marker is placed on the infant's ankle. Sometimes the infant's identification band is stamped with the mother's information using an addressograph. If written with a pen, the band includes the infant's gender, the surname of the mother and the date of birth. The infant's bassinet is also labeled with the infant's gender, surname of mother, weight, length and date and time of birth. There is no infant-specific band placed on the mother or another family member.
In general, infants stay at the mother's bedside except when the mother leaves temporarily, at which time the infant is brought to the nursing desk. Mother and infant are generally kept in hospital for at least 24 hours to ensure both are doing well prior to discharge home. There is currently no designated nursery at Norway House.
8. Infant and Mother Identification at a Tertiary Care Birthing Centre in 2017
An Internet search identified reference to 18 "switched at birth" cases across the world between 1931 and 2015, including a 1971 case in Australia where infant misidentification was attributed to the newborns being placed in the wrong cots.
A review of the Global Safety Alerts database maintained by the Canadian Patient Safety Institute revealed one documented case of switched at birth in a Hong Kong hospital in 2009.
"Two newborns were switched in their cribs. Baby A and B of the same gender and similar weight were born within 35 minutes of each other. They had the correct wrist bands applied in the labour ward and the cribs were labelled correctly, but the babies were placed in the wrong cribs. Two new 2D barcode bracelets were made at the same time and applied to the babies based on the name on the crib and not checking the babies' wristband. The babies were given to the wrong mothers without checking their identification and Mother B noticed that the baby given to her had a bracelet that said Baby A. DNA testing was done to confirm the babies' identities. Key contributing factors included not properly verifying the identity of the baby before applying the identification bracelet and not checking the baby's identity before a procedure."
This Hong Kong incident led to recommendations to streamline the baby identification process and require that baby identification be checked before any procedure.
Additional cases of misidentification have been documented when mothers were given the wrong infant to breastfed.
These cases, as well as other "near misses" have led to a variety of approaches to ensure correct infant identification and linkage of the newborn with the actual mother.
The Ottawa Hospital General Campus Birthing Unit provided information to the reviewers about current leading practices in infant/mother identification. According to the Birthing Unit staff, all routine vaginal deliveries occur in single birthing rooms. When the infant has been delivered and is stable (not requiring resuscitation), he or she is given to the mother for bonding. The nurse then instructs the unit clerk to print off a group of four identification bands, using the unit's computer system. The four bands consist of two for the infant (one on the ankle, one on the wrist), one for the mother (in addition to her regular hospital identification band) and one for the father or designated partner. Prior to the bands being placed, the accuracy of the information is confirmed with mother and mother's partner (if present). If the infant is transferred to the Neonatal Intensive Care Unit (NICU), the bands are attached to the incubator, as some infants are too small to attach the bands to the ankles and wrists.
When the computer system is not working, the Birthing Unit uses a manual system called Ident-a-Band® (See Figure 7). The system consists of four number-matched plastic bands (two large, two small) into which paper tabs are inserted. After identifying information is hand-written on the paper tabs (mother's name, date of birth, gender of baby), they are inserted into the plastic holders. The two smaller bands are placed on the infant (one of the wrist and one on the ankle; see above regarding infants admitted to NICU), and the larger ones are placed on the mother and mother's partner. Accuracy of the information on the band is confirmed by the mother and/or mother's partner prior to placement.
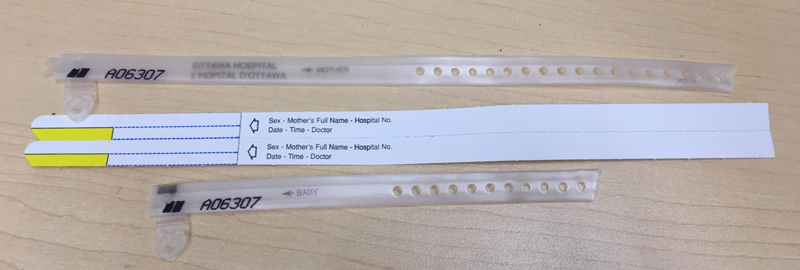
Figure 5 - Text Equivalent
This picture shows the Ident-a-Band® system which consists of four number-matched plastic bands (two large, two small) into which paper tabs are inserted.
A similar approach is used at the Saskatoon Health Region and Izaak Walton Killam Hospital in Halifax. In addition, all three organizations comply with Accreditation Canada standards that require use of two client identifiers (e.g. name and hospital ID number) whenever a procedure is done, medication is given or transitions in care occur.
In addition to using ID bands, some hospitals take fingerprints, footprints, palm prints and/or heel prick blood tests of newborns. In hospitals with advanced bar-coding systems, identification bands with bar codes that link the mother and baby are placed on the mother and newborn, usually immediately at the time of birth. The bar code is scanned as part of robust double checks throughout the care process including discharge. In at least one large organization, the mother signs a form at discharge confirming that the bands on the mother and the baby match and that the mother is being discharged with the right baby.
9. Conclusions
Between January and June 1975, there were two confirmed instances at Norway House Hospital in Manitoba when a pair of male infants were misidentified shortly after birth and were not discharged with their biological parents/family. Although the circumstances were different, the major factors which resulted in these errors were similar. Based on a review of documents and interviews with many individuals, it appears that the newborn identification process used at Norway House Hospital was not sufficiently robust to ensure accurate identification of infants. The identification band process was not used consistently and the identification bands were not put on the baby in the room where the baby was delivered.
Specific details regarding the probable timing and major contributing factors in each case include confidential personal information that will be provided to the individuals involved and are not included in this summary report.
10. Recommendations
It is recommended that Norway House Hospital and any other Health Canada facility where births occur:
- Implement a number-matched four-band mother-infant bracelet system, such as Ident-a-Band®, with two bands on baby (ankle and wrist);
- Implement a standard process such that bands are applied to the infant, the mother and the mother's partner (if present) in the delivery room immediately after birth, or as quickly as the clinical situation allows;
- Train staff to be highly compliant with the above process with regular performance audits.
Based on the findings from this review, and considering that Health Canada is making DNA testing available to individuals who have concerns about the circumstances of their births at Norway House Hospital, the reviewers do not recommend a broader case review of other births that occurred at Norway House Hospital. This conclusion is influenced by absence of evidence of malicious intent, absence of specific requests by other individuals to have their cases reviewed, and the practical limitations of searching for potential misidentified infants. Should circumstances change, e.g. additional requests and DNA evidence from specific individuals, those specific cases should certainly be reviewed.
11. Limitations
A retrospective review of events is always challenging. It is particularly difficult when more than 41 years has passed. Memories fade and key individuals are difficult to reach, may not want to participate or may have died. This review encountered all these challenges. Some individuals immediately affected by the switched at birth incidents were not available to meet with the reviewers.
The reviewers are very grateful to the many people who participated in the review, often sharing stories that brought up painful memories. During the interviews, the reviewers heard that the misidentification of the newborns profoundly affected not only the four men and their parents, but also many members of their extended families. In many cases, talking about these events brought back memories and hurts involving other, sometimes painful, events in their lives as indigenous people. The reviewers attempted to be sensitive and hope that the answers provided in this report contribute to healing. Other processes are underway as part of the Reconciliation process arising from the Truth and Reconciliation Commission Report (2015) and the federal government's commitment to the report recommendations.
The reviewers were able to access many documents, as listed in Appendix 1. As previously noted, the quality of documentation in some of the hospital records was incomplete, inaccurate or hard to decipher.
Despite these limitations, the reviewers are confident that they have completed as thorough a review as possible under the circumstances and have sufficient evidence to provide sound conclusions as to when the switches occurred and why. Throughout the review, the reviewers emphasized that it will never be possible to say with 100% certainty what happened 41 years ago. However, like building a jigsaw puzzle, the reviewers were able to identify and put together sufficient pieces of the puzzle to paint a picture of what probably happened.
12. Acknowledgments
The reviewers would like to thank all the individuals who participated in this review. In particular, we would like to thank members of the families who shared their stories with us. This was not easy for them. We hope that we have provided them with some answers which will help their healing process.
Submitted by:
David Creery, MD, MSc, FRCPC, MHSc
Maura Davies, BSc, BEd, MHSA, FCCHL
Date: May 25, 2017
Appendix 1: Documents Reviewed
Thousands of pages of documents were reviewed as part of this case review, including the Norway House Hospital medical records for the four mothers and their babies. Other documents of particular significance include:
- AHRQ, Patient Safety Primer: Systems Approach accessed at https://psnet.ahrq.gov/primers/primer/21/systems-approach on January 16, 2017
- Canadian Patient Safety Institute Global Safety Alerts, accessed at http://www.patientsafetyinstitute.ca/en/NewsAlerts/Alerts/Pages/default.aspx on January 22, 2017
- Health Canada, A Study of the Hospital Physical Facilities of the Norway House Hospital, Norway House, Manitoba, May 1973
- Health Canada, Base Review of the Norway House Hospital, 1983
- Health Canada, Norway House Hospital Maternity Record of Births August 5, 1971-January 24, 1978
- Health Canada, Norway House Hospital Operational Monthly Reports, July 1973-December 1975
- Health Canada, Norway House Hospital - Plans for Facility Changes, December 1975
- Health Canada, Norway House Hospital Role Study, 1977
- Health Canada, Report on the Norway House Hospital Attitude Survey, March 1975.
https://en.wikipedia.org/wiki/Babies_switched_at_birth accessed February 23, 2017 - http://www.independent.co.uk/life-style/health-and-families/health-news/babies-switched-at-birth-will-not-be-returned-to-their-biological-family-a6738261.html accessed February 23, 2017
- K.A. Wotton and S.M. Macdonald, Obstetrical Care in a Northern Indian Community, Northern Medical Unit, University of Manitoba, 1981
- Reason, J., Human Error: models and management, BMJ, 2000; 320:768.
- Ward, P.D.M, Bagnall, H.J., Cardillo, R., Norway House Hospital Study, September 1975
- Ward, Paul, Report on Norway House Operations, July 14, 1975
- Winnipeg Free Press, In Failing Health, October 28, 2016
Downloaded as http://www.winnipeg freepress.com/local/in-failing-health-399079991.htlm on October 31, 2016
In addition, background information was obtained from the following sources:
- Accreditation Canada, Qmentum Standards for Obstetrics, 2017
- Maureen K. Lux, Separate Beds: A History of Indian Hospitals in Canada, 1920s-1980s, University of Toronto Free Press, Toronto, 2016.
- Royal Commission on Health services v2, Chapter 9: The Meaning of the North, 1965
- Royal Commission on Health Services v2, Chapter 10: Recommendations, 1965
Appendix 2: List of Figures
- Figure 1. James Reason Swiss Cheese Model
- Figure 2. Process Map for Mother's Hospital Stay
- Figure 3. Process Map for Infant's Hospital Stay
- Figure 4. Fishbone Diagram of Contributing Factors
- Figure 5. Ident-a-Band® Bracelets and Inserts