Thermal stress in the work place
Upcoming changes to regulations under Part II of the Canada Labour Code
Introducing amendments to regulations under Part II of the Canada Labour Code
On this page
- 1. Introduction
- 2. COHSR Regulations: Thermal stress
- 3. Definitions
- 4. Measuring thermal stress
- 5. TLVs® and action limits
- 6. Heat stress
- 7. Cold stress
- 8. Resources
Alternate format

Thermal stress in the work place
[PDF – 440 KB]
Large print, braille, MP3 (audio), e-text and DAISY formats are available on demand by ordering online or calling 1 800 O-Canada (1-800-622-6232). If you use a teletypewriter (TTY), call 1-800-926-9105.
1. Introduction
Hot and cold work environments are occupational physical hazards and the body undergoes stress when there is a change in the environmental temperature, resulting in thermal stress to workers. Thermal stress is an important health and safety issue that needs to be addressed in a timely manner to avoid catastrophic effects on workers. With an effective thermal stress management program, not only will the worker be satisfied with the work environment, but the company will also have better productivity and less injuries.
Thermal Stress has 2 components: heat stress and cold stress, either of which occurs when the core body temperature is no longer maintained at 36 to 37°CFootnote 1, Footnote 2. It is not the same as thermal comfort. Thermal comfort is when a person feels not too hot or too cold, just comfortableFootnote 2. Depending on the work environment, the body adapts and maintains its temperature so that the employee can function optimally. A body adapts to hot temperatures by sweating and increasing skin blood flow to prevent body temperature from rising while in cold temperatures, the body shivers and reduces skin blood flow to prevent body temperature from decreasingFootnote 2. However, in extreme conditions, the adaptation and maintenance processes are not enough and start to fail causing the body to undergo thermal stress.
Extreme temperature put the body's physiological response under stress such as high temperatures causing heat stress to the workers. In hot environments, the body responds by trying to remove the excess heat in other words it undergoes heat strain. The excess heat is removed from the body via four processes: when the body comes in contact with a cold surface and loses heat via transfer (conduction), when moving air over the skin takes away heat from the body (convection), through radiation and through evaporation of sweatFootnote 1. After a certain point when the heat intake by the body exceeds the body's ability to dissipate heat, the body's ability in removing excess heat is compromised and the core temperature begins to raise in other words heat stress starts to occur. Extremely hot environments include a high temperature and high humidity that together change the actual heat felt by the worker which can eventually lead to heat stress symptoms. Heat stress can then cause multiple symptoms in the body followed by serious and fatal illnesses that require immediate medical attention.
Working in cold environment increases the likelihood of the employee going through cold stress as the body's skin and core temperature begin to decrease below 36 to 37°CFootnote 2. The cold environment includes not only cold air temperature but also wind chill which further decreases the temperature. Additionally, cold stress can also occur when there is cold water immersion for long duration, which also brings down the body's core temperature. The core temperature decreases as the body loses heat to the cold environment through heat loss mechanisms such as conduction and convection. The decrease in core temperature is then followed by varying degrees of injury and illnesses to the worker, which in some cases may be fatal and can cause deathFootnote 2.
Federally regulated work places are governed by the Canadian Occupational Health and Safety Regulations (COHSR). Until recently, extremes of heat or cold were considered physical hazardous substances under Part X of the COHSR without explicitly mentioning thermal stress. However, due to an increasing number of employee and employer concerns relating to exposure to thermal stresses on a regular basis, it became essential to prescribe thermal stress mitigation requirements in amendments to Part X of COHSRFootnote 3.
2. COHSR Regulations: Thermal stress
Thermal stress amendment is included as a subsection in the section 10.19 of Part X (Hazardous Substances) in COHSR, under Part II of the Canada Labour Code. The section will specify heat and cold stress prevention requirements in the work place, with employer and employee responsibilities, for indoor and outdoor exposureFootnote 3.
Part X, section 10.19 on thermal stresses will require as followsFootnote 3:
- To reduce injuries and work time loss related to thermal stress encountered both indoors and outdoors:
- employers, in consultation with the workplace committee, the health and safety representative, or the policy committee as appropriate, must develop and implement procedures for the monitoring and control of thermal stress, which would include the following:
- monitoring requirements of thermal conditions such as cooling power of wind and humidex
- protective clothing and equipment
- administrative controls such as fluid replacement and work practices, work rest cycles, acclimatization, scheduling and organization of work
- engineering controls, such as temporary equipment, shields, insulation and fans to reduce exposure
- employee training to ensure that each employee is familiar with signs and symptoms associated with overexposure to thermal stresses
- internal reporting on any incident associated with exposure to thermal stresses and the treatment provided. The reporting should include the date and time, conditions of work, health symptoms, protective measures, and treatment.
- employers, in consultation with the workplace committee, the health and safety representative, or the policy committee as appropriate, must develop and implement procedures for the monitoring and control of thermal stress, which would include the following:
- Where work is performed indoors an employee shall be kept free from exposure in accordance with the standards below:
- the levels exceeding the Threshold Limit Values (TLVs®) for heat stress exposure listed in the Screening Criteria for TLV® and Action Limit for heat stress exposure, section of the heat stress and strain adopted by the American Conference of Governmental Industrial Hygienists (ACGIH®) in its most recent publication entitled Threshold Limit Values (TLVs®) for Chemical Substances and Physical Agents & Biological Exposure Indices (BEIs®); and
- the levels exceeding the TLVs® listed in the Cold Stress section of the most recent ACGIH® publication entitled Threshold Limit Values (TLVs®) for Chemical Substances and Physical Agents & Biological Exposure Indices (BEIs®). For the purpose of this regulation, ACGIH® TLVs® and action limits are used as reference limit values for heat and cold stress Footnote 4, Footnote 5, Footnote 6. Screening criterion with tables and adjustment factors only exist for heat stress and not cold stress in the ACGIH® booklet. A thing to note here is that the internal reporting system should constitute reporting to the employer or supervisor of any thermal stress incidents and symptoms at workFootnote 3.
This guideline has been developed by Employment and Social Development Canada (ESDC) - Labour Program, to assist federally regulated work place parties that face thermal stress outcomes that are hard to manage and control. The guideline will also be useful for industrial hygiene specialists and health & safety professionals who may have to develop thermal stress prevention program and control measuresFootnote 3.
The guideline can be used by federal workplaces/industries such as postal contractors/employees, long shoring, barge workers, and other outdoor work places which include sport activities, outdoor training and emergency response work placesFootnote 7.
3. Definitions
The definitions below have been summarized from American Society of Heating, Refrigerating, and Air-Conditioning Engineers (ASHRAE) 55 StandardFootnote 8, Footnote 12, Occupational Safety & Health Administration (OSHA)Footnote 9, Footnote 10, Industrial Hygiene BulletinFootnote 11, ACGIH® Footnote 4, Footnote 5, Footnote 6 and National Institute of Occupational Safety and Health (NIOSH)Footnote 1.
Acclimatization: It is the increase in body's physiological adaptation and tolerance to the environmental temperature which occurs over time (ACGIH®).
Action limit (AL): The protective limit for unacclimatized employees and the point where a thermal stress prevention program should be implemented (ACGIH®).
Cold stress: The fall of body core temperature from 36 or 37°C as the body fails in maintaining body heat after being exposed to extremely cold, windy and/or wet conditions. It is associated with multiple cold related illnesses and injuries, some that may be fatal (ACGIH®).
Core temperature: The temperature of the body in the region where the vital organs are present. It is a thermal shell surrounding the vital organs and maintaining their functionality by keeping the temperature around them constant (ACGIH®).
Heat strain: Physiological response of the body to prevent an increase of core body temperature from 36-37°C in extremely hot and/or humid conditions by removing excess heat (ACGIH®).
Heat stress: The net burden of heat experienced by the body when it is exposed to extremely hot environments and causes a rise in body core temperature. The heat burden can cause various health effects and discomfort levels (ACGIH®).
Metabolic rate: It is the rate at which chemical energy is used by the body and converted into heat (ASHRAE 55).
Metabolic work rate: The heat produced by the body as it exerts the energy spent during work (ACGIH®).
Relative humidity: It is the ratio of partial pressure of water vapour to the saturation pressure of water vapour at equal temperature and pressure (ASHRAE 55).
Tdb: Dry bulb temperature. Temperature measured in ambient air in the absence of moisture (NIOSH).
Tg: The globe temperature. Temperature radiated from sources like the sun, structures or machinery (OSHA).
TLVs®: Threshold Limit Values that give the maximum exposure limit for occupational hazards such as physical, chemical and biological hazards (ACGIH®).
Tnwb: The natural wet bulb temperature. Temperature measured by covering the thermometer in a wet cloth and measuring the temperature of the ambient air (NIOSH).
Wet-bulb globe temperature (WBGT): A heat stress index which represents a temperature that includes the total temperature effect or the heat load on humans due to air temperature, humidity, wind and radiation (Industrial Hygiene Bulletin and ACGIH®).4. Measuring thermal stress
Heat stress and cold stress are measured in different ways. When there is a risk of heat hazard exposure causing heat stress in employees, multiple factors are used to calculate the prescribed WGBT. WGBT is first calculated by using the ACGIH® WGBT equations for indoor and outdoor exposure (as provided in the Heat stress and strain section, ACGIH® TLVs® & BEIs® booklet)Footnote 6. The equations use 3 types of temperature in other words the dry bulb temperature Tdb a measure of the ambient temperature, natural wet-bulb temperature Tnwb a measure of the body's ability to cool by the evaporation of perspiration, and the globe temperature TgFootnote 9 a measure of heat intake through radiation. These temperatures already incorporate humidity and wind speed. The calculations then corrected for clothing, work activity level and complexityFootnote 6.
Metabolic work rate is also calculated for heat stress by using work activity levels, height and weight of the worker, in order to identify the appropriate TLV® and action limit on the ACGIH® TLV® graph (as in the Heat stress and strain section of the ACGIH® TLVs® and BEIs® booklet)Footnote 6. Detailed equations, tables and methods can be found in the ACGIH® TLVs® and BEIs® booklet for assessing thermal stress; to be used by a qualified person specialized in thermal stressFootnote 11. A summary of the relevant equations is also given below in Subsection 6.4 for Heat Stress.
For cold stress, there are no equations but the risk for cold stress can be estimated and controls developed based on the tables and requirements provided in the Cold Stress section, ACGIH® TLVs® and BEIs® bookletFootnote 6.
5. TLVs® and action limits
Heat and cold stress in industrial settings are regulated by implementing the ACGIH® TLVs® and Action Limits. Canadian Standards Association (CSA)Footnote 11 and ASHRAE standards are used for thermal comfort and ventilation in indoor offices, not necessarily for thermal stress. These standards are a good resource to use when considering the thermal conditions in indoor office space.
According to CSA standards Z1004-12 – Work place Ergonomics – the comfort level at work is determined by temperature, humidity, wind and work-rest cycleFootnote 13. The optimal temperature range for office comfort should be 23 to 26 °C with 50% relative humidity in summers and 20 to 23.5°C at 50% relative humidity in winterFootnote 13.
ASHRAE 55 Standard -Thermal Environmental Conditions for Human Occupancy specifies the requirements for thermal comfort in indoor work places or a specific area with occupants doing minimal or no physical demanding workFootnote 8. The thermal comfort conditions according to this standard consider the metabolic rate, temperature, humidity, occupants, clothing and wind speedFootnote 8.
ASHRAE 62.1 Standard – Ventilation for Acceptable Indoor Air Quality gives requirements for indoor air ventilation by using factors such as work place type, outdoor air, occupancy and area of work placeFootnote 12. Inadequate ventilation can in some cases contribute to thermal stress in the form of hot, humid and stagnant air or vice versa where the ventilation speed is too high for the work placeFootnote 12.
Thermal Stress TLVs® assume that if all employees are acclimatized to the job task at risk of causing thermal stress, are healthy, not medicated and have good levels of hydration, then at the TLV®, they will not have any adverse effects. In contrast, the Action Limit assumes that the employees are not acclimatized and represents the limit where a thermal stress management program needs to be consideredFootnote 6.
6. Heat stress
Risk factors for thermal heat and cold stress can be either job task related or personal risk factors. The heat and cold tolerance has a high individual variability, however; the risk factors discussed below will help employers in assessing their employees' tolerance levels and the thermal hazard of the job tasks.
6.1 Risk factors
a) Work related factors
The body generates heat when it performs strenuous work. The risk of heat stress is directly associated with the physical exertion required in a given task as well the task duration. More physical exertion required will increase the metabolic rate and body temperature, which, especially in hot environments, will increase the need for removing excess body heat. The frequency of the task will also affect how the body responds to heat stress. Employees doing the same task repeatedly will adapt to the conditions and physical demands and will acclimatize. However, employees who infrequently perform work in hot environments will not be able to adapt and will easily undergo heat stress. More experienced employees can adapt to the work faster or change their work method depending on how they feel in contrast to inexperienced or new employees. Heat stress symptoms experienced by an employee will also be determined by the type of clothing worn by them. Wearing more layers or thicker clothing, will prevent heat loss from the body and increase body core temperature.
b) Personal characteristics
Gender: Generally, women have a lower metabolism rate and low aerobic capacity as compared to men. Women also have a lower rate of sweating than men, altogether which result in a higher body temperature in women than men. Pregnancy is also another factor which plays a role in heat stress management in women where pregnant women are more susceptible to heat related illnessesFootnote 4.
Age: As employees age, their bodily processes slow down and so does the ability to remove excess heat from the body quicklyFootnote 4. It is due to a reduction in blood flow to the skin, sweating, fitness and overall cardiovascular functionFootnote 4. Additionally, older employees also have trouble acclimatizing to the environment quickly compared to those who are younger employees.
Obesity: An obese employee is at a higher risk of undergoing heat stress than a non-obese personFootnote 4. More body weight means that the employee will have a low cardiovascular ability and low physical work capacityFootnote 4. More fat between skin and blood vessels also lowers heat exchange through the skin as the blood flow to the skin decreasesFootnote 4. Additionally, an obese employee may also have a higher base line metabolic rate and more heat will be produced than in a non-obese worker, increasing the internal body and tissue temperatureFootnote 4.
Acclimatization: Given time, a body adapts to the new working conditions and starts to regulate the core temperature according to the new environmentFootnote 4. The amount of time required for acclimatization varies among individuals. Employees who are not acclimatized may experience severe heat stress almost immediately after starting a new job in a work place that is hot. This is because their body cannot replace the water and salts lost due to excessive sweating in the new environment or at the new physical exertion level. Acclimatization can be achieved by slowly introducing the employee to the new task and gradually increasing the intensity and duration of the task so that the body can adapt and regulate heat removal processes like sweating accordingly. After about 4 days of continuous work the body becomes acclimatized to the job task. Unfortunately, if the employee is away from the task for long, acclimatization is reversed and the employee will have to begin as if they were unacclimatizedFootnote 4.
Existing health concerns, medication and/or drug use: Some prescribed medication or recreational drugs and alcohol use can affect the thermoregulation processes of the bodyFootnote 4. Drugs that have an effect on cardiovascular systems, water regulation and the central nervous system, can interfere with hydration systems and removing excess heat from the body. Employees with such prescribed medicines should be monitored routinely and their job tasks should be adjusted accordingly, if possible. Recreational drugs like cocaine, cannabis and hypnotics will also increase risk for heat stressFootnote 2. Employees with skin disease and rash, and chronic health problems such as heart disease, diabetes and respiratory problems will be more susceptible to heat stressFootnote 2.
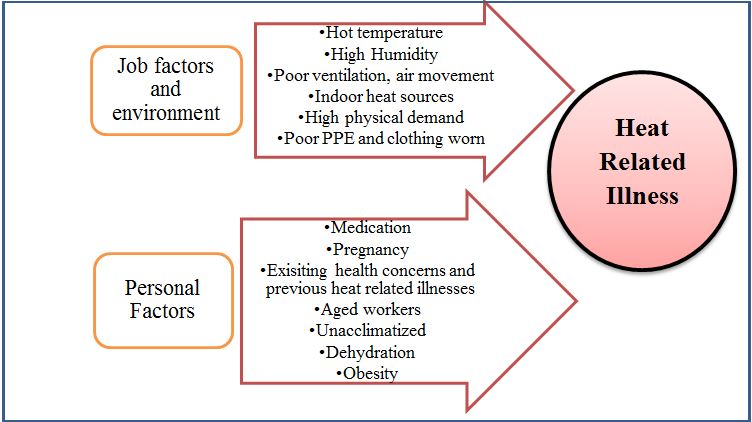
Figure 1 - Text version Heat stress risk factors
Heat Stress Risk Factors adapted from the Criteria for a Recommended Standard: Occupational Exposure to Heat and Hot Environments, NIOSHFootnote 1.
Occupational exposure to heat and hot environments and some prescribed medication or recreational drugs and alcohol use can interfere with hydration system and removing excess heat from the body, which may lead to heat related illnesses.
Job and environment factors include:
- hot temperature
- high humidity
- poor ventilation and air movement
- indoor heat sources
- high physical demand, and
- poor personal protective equipment and clothing being worn.
Personal factors include:
- medication
- pregnancy
- existing health concerns and previous heat related illnesses
- aged employees
- unacclimatized employees
- dehydration, and
- obesity
6.2 Illnesses or disorders
Before severe heat stress begins, the body tries to remove the excess heat. Known as heat strain, this is the deployment of bodily processes such as sweating, blood flow to skin, breathing rate and metabolic rateFootnote 6. However, after some time of exposure these processes may not be long enough to control body temperature and the body begins to overheat and the heat related disorders begin.
a) Heat syncope
Heat syncope or fainting occurs in employees not acclimatized to their working conditions. It occurs when the worker's blood pressure begins to drop, and the blood begins to remain in the lower limbs as posture changes or too much blood goes to the skin.
b) Heat exhaustion
It is directly correlated with dehydration and low salt in the body. As the body gets dehydrated, blood volume falls and the heart is not able to keep up with the demand. Acute symptoms may include dizziness, headaches, irritability and weakness along with high sweating, fast heart beat and nausea/vomiting. Chronic heat exhaustion cause increase risk for kidney stones and gastrointestinal diseases as well as psychological health effects.
c) Heat stroke
Heat Stroke is the most fatal illness due to heat stress. This occurs when the body is unable to regulate the core body temperature in the central nervous system. It can be due to a hot environment or inefficient removal of heat from the body produced by metabolic processes. Symptoms include fainting, loss of consciousness, high body temperature, and red, "flushed" skin, and increased sweating. It is fatal because after the initial symptoms, risk for organ failure and death is very high, as the internal body systems are unable to recuperate after severe heat damage.
d) Dehydration
Sweating is the natural mechanism for the body to remove excess heat however; it is also a main cause for dehydration and loss of salt from the body. Dehydration eventually leads to reduction in blood volume and disruption of normal blood pressure. Prolonged dehydration can also lead to fainting, muscle cramps and gastrointestinal problems. Darkening or more concentrated urine is an indication of the onset of dehydration.
e) Heat cramps
These are muscle cramps and pain that arise when the employee performs their job tasks in an extreme, hot climate. It is a result of dehydration and salt loss from the body and causes cramps in legs, arms and abdomen.
f) Heat rash
It commonly occurs in a hot environment and is shown by red pimples and blisters. It mostly occurs in areas of the body where the sweat is unable to dry off or there is restrictive clothing such as at the neck, elbow creases, groin and breast regionFootnote 9.
g) Hyponatremia
It is result of dehydration, loss of salt and electrolytes or unequal water and salt distribution in the body. Excessive sweating or drinking too much water without enough salts can cause varying degrees of hyponatremia. Symptoms can either be negligible or severe. Some severe symptoms include respiratory distress, pulmonary edema or even death.
h) Rhabdomyolysis
Rhabdomyolysis is a tissue injury in the muscle due to heat and physical stress. It can either show minimal or no symptoms, or serious symptoms. Symptoms can include pain and cramps in muscles, dark urine, weakness and inability to exercise. Other symptoms such as nausea, vomiting, confusion and abdominal pain can also occur generally. It is caused by prolonged and extreme exertion of muscles, high body temperature, medications and use of excessive drugs or supplements in other words it is caused by factors which reduce blood to muscles or injure the musclesFootnote 1.
Treatment
Immediate first aid is required as soon as the early symptoms of heat stress arise. Initial first aid should include:
- removing employees from the hot environment
- keeping employees in shady and cool areas
- giving them cold water or other drinks (no alcoholic or caffeinated beverages), and snacks to prevent dehydration and salt loss as in heat cramps and hyponatremia
- areas with heat rash should be kept clean and dry at all time, and no creams should be applied
When heat exhaustion symptoms start to occur, along with previous first aid tips:
- use ice packs and remove unnecessary clothing to cool down the body
- if the heat exhaustion gets worse, then immediately go to the emergency room
- no more work should be performed by the employee
In case of a heat stroke:
- immediately call 911
- help employee in removing unnecessary clothing
- put ice packs at armpits
- keep the employee in a cool, shady area
- give employee cold drinks
6.3 Assessing risk and decision making process
The decision process below should begin when there is a likelihood of risk for heat stress. It takes into account clothing, the WBGT threshold, analyzing the limits based on clothing and work activity adjustments, heat strain and heat stress management and controls. The decision making figure is an adaptation of the decision matrix provided in the ACGIH® TLVs® and BEIs® bookletFootnote 5, Footnote 6.
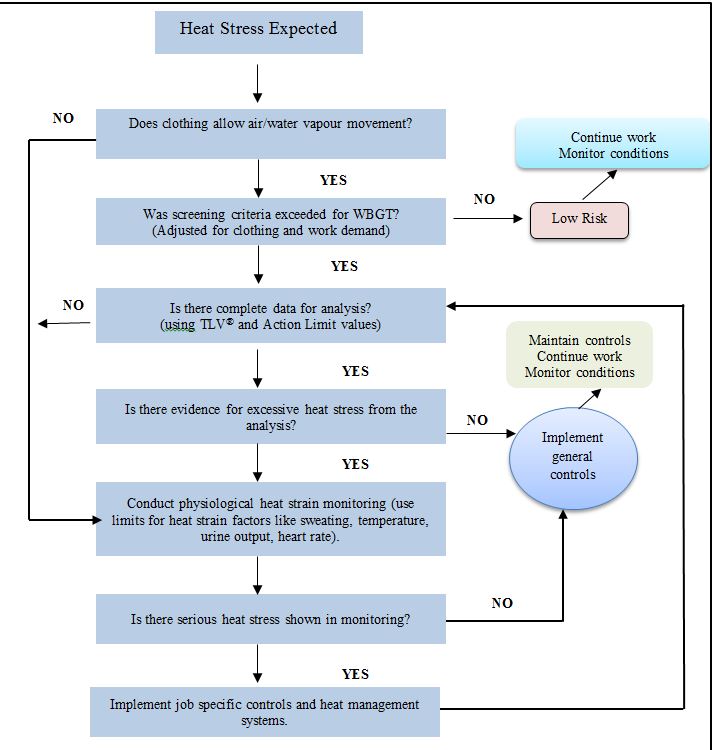
Figure 2 - Text version Decision making and risk assessing process for heat stress
Figure 2: Decision making and risk assessing process for heat stress. The above process should be used in accordance with the tables provided in ACGIH® booklet in assessing risk and implementing the relevant controls and management programFootnote 6.
The decision making and risk assessment process for heat stress begins when there is a likelihood of risk for heat stress, therefore heat stress is expected. It takes into account clothing, the WBGT threshold, analyzing the limits based on clothing and work activity adjustments, heat strain and heat stress management and controls. If the WBGT threshold adjusted for clothing and work demand is not exceeded, the risk is considered low, consequently the work continues but the work conditions are monitored. If there is no evidence for excessive heat stress from the analysis or in monitoring, there is no serious heat stress shown, general controls should be implemented, the work continues, controls should be maintained and conditions of work monitored.
6.4 TLVs® for heat stress
The goal of the heat stress TLV® is to prevent the body core temperature from increasing more than 1 degree from 37°CFootnote 6. It must be noted however that the TLV® does not guarantee complete protection from severe heat related illnesses as they can occur even below the TLV® and there is also the chance of a carry-over effect from the previous day.
TLVs® and action limits for heat stress are obtained by screening for work load and work-rest cycle from table 2 in the Heat stress and strain section of the ACGIH® TLVs® & BEIs® booklet. The table 2 TLVs® from the ACGIH® booklet are more protective as they indicate any risk of heat stress and are only to be used as an initial screening tool and not to prescribe work-rest schedules.
(For more in depth analysis, figure 3 below is used for TLVs® and action limits.) The obtained value is then compared to the adjusted wet bulb globe temperature (WBGT) and metabolic rate (metabolic work rate). The WBGT is calculated using the measurement methods described below, with equations from the Heat stress and strain section of the ACGIH® TLVs® & BEIs® booklet. The effective WBGT used here is a sum of the calculated WBGT and the clothing adjustment factors (from table 1 in the Heat stress and strain section of the ACGIH® TLVs® & BEIs® booklet). The metabolic rate is also calculated using the task specific metabolic rates given in table 3 in the Heat stress and strain section of the ACGIH® TLVs® & BEIs® booklet, and the employee's personal characteristics. To take into account body weight, the metabolic rate from table 3 can be multiplied with employee weight ratio to get the estimated (est) metabolic rate. Following are the equations usedFootnote 4, Footnote 6:
- WBGTamb (indoor) = 0.7 Tnwb + 0.3 Tg
- WBGTamb (outdoor) = 0.7 Tnwb + 0.2 Tg +0.1 Tdb
- WBGTeffective = WBGTambient + Clothing Adjustment Value
- Metabolic rateestimated = (Metabolic expectations (task specific, table 3) multiplied by employee body weight) divided by 70 kg or 154 lbs
In case there are multiple tasks being performed then the time-weighted average (TWA) is calculatedFootnote 14. The calculated WBGTeff, for each task duration is calculated or for one continuous task, and then used to calculate the time-weighted average over a 1 to 2 hour period, where "t" is the time period for each taskFootnote 14. The TWA is not calculated if only one task is being analyzed. The TWA is then compared against the TLVs® and action limits graph.
- TWA-WBGT = [WBGTeffective for task 1 multiplied by t1(the time period for task 1) + WBGTeffective for task 2 multiplied by t2(the time period for task 2) + … + WBGTeffective for task n multiplied by tn (the time period for task n)] divided by the sum of the time periods for each task (t1 + t2 + ... + tn)
- TWA-Metabolic rate (M) = [M for task 1 multiplied by t1(the time period for task 1) + M for task 2 multiplied by t2(the time period for task 2) + … + M for task n multiplied by tn(the time period for task n)] divided by the sum of the time periods for each task (t1 + t2 + ... + tn)
From the figure below, the point where the effective (eff) WBGT and metabolic rate intersect at solid line is the TLV® for that employee in the specific working conditions, whereas intersection at the dotted line is the action limitFootnote 6. If the intersection point where the metabolic rate and WBGTeff is above the TLV® line, then the employee is overexposed as the exposure is above the TLV®.
This screening process is used when the decision making process for heat stress is started. The TLVs® and action limits screening tools also take into account the work intensity, and the work rest schedule. Relevant tables and examples for evaluating heat stress hazards and TLVs®/action limits can be found in the ACGHI® TLVs® & BEIs® bookletFootnote 6.
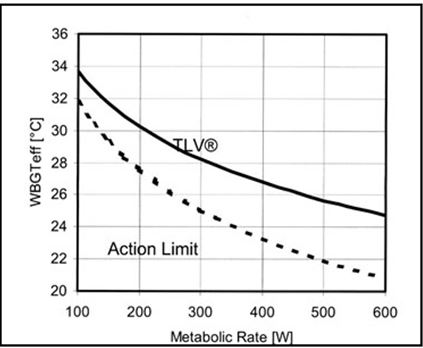
Figure 3 - Text version Threshold Limit Values (TLV)
Figure 3: TLV® (solid line) and Action Limit (dotted) for heat stress specified by the ACGIH®, obtained from OSHA6, Footnote 9.
The figure specifies the TLV® and action limits for heat stress. The solid line represents the TLV® and the dotted line is the action limit. The point where the effective (eff) WBGT and metabolic rate intersect at solid line is the TLV® for that employee in the specific working conditions, whereas intersection at the dotted line is the action limitFootnote 5. If the intersection point where the metabolic rate and WBGTeff is above the TLV® line, then the employee is overexposed as the exposure is above the TLV®.
6.5 Heat stress example
Following is an example of a thermal stress problem at the work place which should be solved by a qualified person using the techniques and equations described above. The adjustment factors and TLVs® have been taken from the Thermal Stress chapter in the ACGIH® TLVs® & BEIs® booklet.
On a hot summer day, a 20 year old, 90kg new internee started his first day as a mail carrier. He worked an 8 hour shift completely outdoors, with an hour break in between for lunch and 2 15 minute breaks as needed. He started his shift at 7am and did not have breakfast but had a cup of coffee. He kept 2 500ml water bottles with him. The employee drove the office van to deliver mail, worked alone and wore double layered clothing as he felt a little feverish. He met a fellow employee for lunch who commented that he looked rather red and offered him water. For 1 hour, he delivered mail by foot to 3 neighbourhoods. During that task, the following temperatures were recorded:
Tdb: 30°C
Tnwb: 26°C
Tg: 28°C
Solution:
We assume here that the tasks are moderate as it requires fast walking for timely delivery and he has a 75 to 100% allocation of work in a work-rest cycle as the worker has 1 hour break only in his 8hr shift. According to table 2 in Heat stress and strain, ACGIH® TLVs® & BEIs® booklet, the initial screening for moderate work showed that the protective TLV® should be 28.0°C while the action limit should be 25.0°C. That immediately shows that there is risk for heat stress as that is a high temperature. We will also calculate the heat stress risk for the 1 hr task as that has the only data available and also as it was a continuous task.
- WBGT
WBGTamb (outdoor) = 0.7 Tnwb + 0.2 Tg +0.1 Tdb
= 0.7(26) + 0.2(28) + 0.1(30) = 26.8°C
Clothing adjustment factor = 3 (Table 1 in heat stress, ACGIH® TLVs® & BEIs® booklet)
WBGTeff = 26.8 + 3 = 29.8°C
- Metabolic rate: According to table 3 in Heat stress and strain section, ACGIH® TLVs® & BEIs® booklet, for moderate work, the TLV® should be 300 Watts. Since, the employee weighs more than the average; the effect of body weight will be taken into account for the metabolic rate estimate.
Metabolic rateestimated = [300 watts (W) multiplied by 90 kilograms (kg)] divided by 70 kilograms (kg) = 385 watts (W)
- Now, using the WBGT and metabolic rate values, the graph in figure 2 above can be used to estimate if the employee is at risk for heat stress.
The point of intersection for WBGT of 29.8°C and metabolic rate of 385 W is above the solid TLV® line which means that the employee is over exposed. Using the metabolic rate, the TLV® for the WBGT for this employee for this task was 27°C, as shown by the graph.
- Work-rest regime:
We assumed the worker has a 75 to 100% work allocation in a work-rest cycle/regime. Based on the WBGT of 29.8°C, the worker should allocate roughly about 25 to 50% of his time to work in a work-rest regime, and use the remaining time to cool down or rest in cooling stations or in shade.
- Facts
- The employee is unacclimatized and did a full time shift on his first day.
- He also wore more layers of clothes than necessary and did not feel well.
- The redness on his face is a sign for early heat stress as his body is trying to cope with the high temperatures.
- He also seems to be dehydrated and did not eat enough to have energy.
- The employee is overexposed to heat stress as his WBGT and metabolic rate is above the TLV®.
- Recommendations
- His WBGT and metabolic work rate must be brought down to the TLV® or even lower.
- Work schedule must begin slowly with part time shifts before he goes into full time work in other words follow an acclimatization plan.
- He must be given training in heat stress management and identification, and first aid in addition to the regular job training.
- He must wear clothes that consider the work and temperature conditions and if he still feels sick then should take a day off before returning to work.
- He must remain hydrated and eat more snacks, with less caffeine to prevent dehydration.
- The work should be balanced between indoor and outdoor tasks.
- He should be given a modified work rest schedule where he gets more breaks in other words his work allocation must follow the calculated WBGT and the TLV®. As per this example, he should work 25 to 50% of his time if he continues to work at moderate work load and current WBGT value. If the administration is able to lower the WBGT, then the table 2 in Heat stress and strain section, ACGIH® TLVs® & BEIs® booklet should be used again as a reference of allocating work and break schedules.
6.6 Controls for hot environment
The most effective controls are engineering controls or elimination/substitution controls followed by administrative controls and finally personal protective equipment (PPE). PPE should be the last resort or should be used as a supplementary control method.
a) Engineering controls
- Reduce work intensity and demand by mechanizing physically demanding tasks by using carts or lifting devices.
- Outside work should be done in the shade, covered areas or otherwise conditioned areas so as to prevent direct heat exposure.
- Cooling stations with proper ventilation should be put up in the work area where employees can take their breaks or take a few minutes to cool down between tasksFootnote 2.
- Indoor work environment should be adequately air conditioned with effective ventilation and local exhausts to remove hot air, and fans should be used where possible, to increase air movement and sweat evaporation.
- Use shields or insulation for indoor equipment that may give off heat.
- Heat sources should be isolated or changed to reduce their heat radiationFootnote 11.
b) Administrative controls
- The job needs to be adjusted according to the working conditions and the employees' personal risk factors.
- Physical demand of the job should be reduced by decreasing the shift length, changing the exertion required on the job, and replacing heavy tasks with light tasksFootnote 2.
- A specialized work-rest schedule should also be made for the employees depending on their job description, environmental conditions, company policies, acclimatization and employee characteristics.
- Employees should be allowed to take breaks or change tasks at any point if they feel too hot or uncomfortable.
- There should be enough employees to equally distribute the task and decrease the load.
- Workstations should be at a reasonable distance from heat sources.
- The work schedule should be adjusted according to the weather conditions, and risky tasks should be scheduled for the cooler times of the day.
- Any rare or unplanned tasks should be monitored and trained employees should be used specifically.
- The work place should make clean drinking water easily available for employees to keep them hydrated.
- An acclimatization program should be in place at work which will allow employees to adapt to the hot work conditions in about 7 to 14 days, and decrease heat related illnesses.
- On anticipated hot sunny days, start work very early and finish the shift before heat conditions worsen in the afternoon.
c) Personal Protective Equipment (PPE)
Clothing worn while working greatly affects the employees WGBT and the maximum heat they can be exposed to, to remain under the TLV®. More information on the required PPE can be obtained from Part XII of the COHSR.
- Use cooling vests or jackets with space for ice packs, compressed air source to cool down air in jackets or coveralls, and cooled supplied air to be used with suitsFootnote 2.
- The employees should not be overdressed in hot environments and they should wear goggles, gloves and hats.
- Take breaks while wearing PPE to prevent heat stress.
d) Prevention techniques
The following techniques should be included in the thermal stress prevention program implemented at a work place.
Medical surveillance: Even though this is not a regulatory requirement, it is a recommended best practice measure for secondary prevention and predicting any future illnesses. Biological factors may affect employee's tolerance to heat and susceptibility to heat related illnesses. Employees should undergo periodic medical surveillance so that any changes to their health or effect of heat exposure can be identified. Initial screening should include an in-depth medical history for existing disease/illness, past surgeries, past and current medication, occupational history and previous heat related illnessesFootnote 1. Employees should also under a heat tolerance test so that their individual tolerance ability can be noted down in regards to their job. This test can include monitoring heart rate, sweat production and body temperature. Regular medical surveillance should include urine analysis, blood pressure trends, and respiratory volume tests which can indicate heat tolerance and level of acclimatizationFootnote 1.
Training: employees should be given regular training so that they are aware of the hazards of the job tasks and heat, and are able to detect signs and symptoms of heat stress in themselves or their fellow employees. The training should also include basic first aid and prevention techniques learning. Employees should be trained on proper maintenance and usage of PPE, an understanding of personal or non-occupational factors that may increase their susceptibility to heat stress, and the importance of complying with the controls and reporting any issues. The training should not only be for new employees but also include experienced employees and supervisors. Supervisors should be trained the same as employees with the addition of acclimatization, monitoring conditions and employees, and emergency procedures.
Personal hygiene: employees should stay hydrated and cool during their work. Employees are also responsible for maintaining a healthy lifestyle so that their tolerance or acclimatization to the job is not adversely affected. They should be aware of their personal health issues and identify any symptoms of heat stress that arise, to their supervisor/manager.
Reporting: employees, supervisors and managers are liable to timely report any incident or symptoms of heat stress at work placeFootnote 3. The reports should be kept up to date and detailed enough to prevent future injuries and illnesses. Employers should also use the buddy system where employees can observe and report any signs or symptoms of heat stress in their fellow worker.
7. Cold stress
7.1 Risk factors
a) Work related factors
The job related physical demand, conditions, duration and frequency greatly determine the risk for cold stress. The conditions can include how cold the surfaces or objects are, how wet the surfaces are and how long is the employee being exposed to the wet and cold. Air temperature along with wind chill and moisture combined create the actual coldness felt by the body. That coldness determines the temperature gradient and how fast the body will lose its heat. Prolonged work done in the extreme cold conditions will increase risk for cold stress injuries, however, if work is done in a regulated work-rest cycle, then the risk is lowered. The type of work conducted also changes susceptibility to cold stress. In cold weather, the work should also not be physically demanding as it may increase the rate of sweating, making the clothing wet and exposing the skin to cold and wet induced conditions.
b) Personal characteristics
Gender: Differences in susceptibility to cold stress due to gender differences relies heavily on anthropometric differences in men and women. Women's hands and fingers are more susceptible to cooling as compared to men due to differences in hand size and blood vessel responses at the skin. Generally, women have a high fat content or high surface area but small body mass as compared to men, due to which insulation and heat loss processes differ in men and women. Women might experience a faster decline in their core temperature than men due to the differences mentioned above.
Age: Heat conservation processes in the body, such as vasoconstriction metabolic heat production, decrease in efficiency with age. Older employees will get tired easily and will not be able to maintain a high metabolic rate for long which will decrease their core temperature faster. Older employees will also have a different sensitivity to cold than younger employees.
Race: A study showed that African American men and women are 2 to 4 times more likely than Caucasians to suffer from frostbiteFootnote 5.
Clothing: The type of clothing worn by the employees will determine their susceptibility to cold stress. The number of layers of clothing insulation required is determined by the metabolic heat requirement, work physical demand and the degree of coldness in the environment. Appropriate clothing insulation can prevent a decrease in body core temperature as it will add to the insulation provided by bodily processes and body fat. Protective clothing against the cold must also include protection for hands, ears, face and head in other words areas where the heat loss is rapid. Employee clothing for cold environments takes into account not only the dry coldness but also moisture and wind, which will change the perception of coldness for the worker.
Activity level: This is a minor factor in thermoregulatory processes. The activity level and physical fitness of employees is important in prolonging the high metabolic rate in employees which will produce heat for a longer time than in less fit employees. It increases the employees' stamina in working in cold environments.
Existing medical conditions, medication and/or drug use: Employees with hypertension, respiratory diseases, diabetes and heart disease will have trouble acclimatizing to the extreme cold weather conditions. Employees that have Raynaud's syndrome or vibration disease will also be more susceptible to cold stressFootnote 2. Such employees will then require regular monitoring, precautions and modified work if possible. Additionally, employees that frequently drink alcohol or take medication such as antidepressants, blood thinners, insulin, amphetamines or recreational drugs will be more susceptible to cold stress induced injuries and illnesses than employees who do not take such substancesFootnote 2.
7.2 Illnesses and injuries due to cold stress
In cold environments, the body tries to prevent excessive heat loss and increase internal body heat. Processes that achieve this goal include vasoconstriction at the skin, shivering and increasing metabolic heat. Soon however, these processes are not enough in preventing body temperature from falling and for cold stress symptoms to start progressing.
a) Hypothermia
As the body's core temperature falls to below 35°C, there is a risk for hypothermia, which can be mild, moderate or severe. It starts off as shivering, slight pain in exposed areas and gradually moves onto more pain, a feeling of numbness, an inability to perform basic tasks, and confusion including denial of feeling cold. Extremely severe symptoms can also appear such as inability to walk or move loss of awareness, unconsciousness, erratic heart rate, breathing failure, pulmonary edema and even death. The symptoms begin to get worse as the body temperature falls. If the body temperature reaches 27°C, unconsciousness occurs. It can eventually be fatal if not treated urgently.
b) Frostbite
Frostbite usually occurs due to contact with cold surfaces or objects, or exposure to extreme cold environments or cold gases. Symptoms might be mild or severe. Mild frostbite is associated with inflammation and pain whereas in severe frostbite, the tissue is damaged, in some cases permanently. This occurs when the tissue temperature approaches and falls below 0°C and the blood vessels get damaged and the circulation is obstructed.
c) Immersion/trench foot
Cold and wet exposures may cause immersion and trench foot. If the employee is continuously exposed to wet conditions with temperature around 10°C, then immersion foot can occur. Immersion foot causes damage to muscle and nerves, hence the symptoms are numbness, tingling, pain and swelling in limbs. The skin also may change colour from red to blue/purple and there is also a chance of gangrene occurring.
Trench foot occurs when the employee is exposed to wet and cold conditions, where the temperature is below 10°C and can go to freezing cold as well.
d) Chilblains
It is a mild injury arising from prolonged exposure to cold air, where temperatures range from 0 to 16°C. The skin will usually be red and swollen, and the employee may feel tingling and some painFootnote 2.
Treatment
As soon as signs of hypothermia become apparent:
- medical attention needs to be given immediately
- the employee should be moved to a warm room as soon as possible and any wet clothing, shoes/boots and wet socks should be removed
- the center of the body such as the neck, head, and abdomen should be warmed first
- if conscious, the employee should be given warm beverages. Alcohol must not be given to warm up
- in case of frostbite, the employee should not walk on frostbitten feet or toes
- the frostbitten parts of the body should be immersed in warm (not hot) water, or the affected area should be warmed using body heat
- the affected area should not be massaged
When there is wet and cold exposure:
- the affected areas should be dried and any wet clothing, shoes/boots and wet socks should be removed
- walking on the affected feet or toes should be avoided
- massaging the affected area should be avoided as it may cause more damage
- in the case of chilblains, the area should be slowly warmed
- creams for inflammation can be applied but the area should not be touched unnecessarily or scratched. Corticosteroid creams are recommended to relieve itching and swelling
7.3 TLVs® for cold stress
Unlike heat stress, cold stress TLV's® do not include screening tables or adjustment factors. The main goal of the Cold Stress TLVs® is to prevent the body core temperature from falling below 36°C and preventing severe cold stress injuries like hypothermia and frostbiteFootnote 5. If the core body temperature falls below 35°C, there is a risk for hypothermia whereas if the tissue temperature falls below 0°C then frostbite occursFootnote 5.
When considering the risk for cold stress, it is important to thoroughly follow through the decision making process discussed below. Hazard assessment should include air temperature and wind chill temperature measurement in quantifying the actual cold temperature perceived by the worker. Using the wind chill temperature with air temperature and wind speeds, the risk of frostbite to employees and how long till frostbite occurs can be predicted. These predictions can be made using tables provided in the Cold Stress section, ACGIH® TLVs® & BEIs® bookletFootnote 6. When conditions fall below -7°C, then the employees should be warned against bare contact with cold surfacesFootnote 6. When the temperature is below -17.5°C, then the employees should be provided with proper warm Personal Protective Equipment (PPE) and use insulated machines or machines which are adapted to be used with PPEFootnote 6.
For manual work, there are specific guidelinesFootnote 6:
- precise work in <16°C and for more than 10 to 20 minutes: Use radiant heaters or warm air jets to keep employee hands warm
- precise work in < -1°C: Handles of the equipment should be insulated
- sedentary work in <16°C: Use gloves
- light work in <4°C: Use gloves
- moderate work in <-7°C: Use gloves
Work place monitoring is required for cold stress management. The monitoring should includeFootnote 6:
- thermometry when temperatures fall below 16°C and if they fall below -1°C, then they should be recorded every 4 hours
- in indoor work places, if the air velocity exceeds 2m/sec then wind speed should be recorded every 4 hours where as in outdoor work places, the air temperature and wind speed should be recorded together when the temperature falls below -1°C
When assessing the risk of cold stress, the ACGIH® booklet should be used for the respective tables. The ACGIH® booklet provides tables (table 2), in the Cold Stress section in the Thermal Stress Chapter, for estimating the metabolic requirements based on the work intensity and requirementsFootnote 6. Those metabolic requirements along with the temperature can be used to estimate the insulation required for the PPE needed by the employees to work in that cold temperature. The clothing insulation required will be in the units of 'clo' which can then be used to estimate the level or layers of insulation required6. Tables 4 and 5 in the Cold Stress section in the ACGIH® booklet quantify risk for frostbite by using wind chill temperature and give the time until frostbite occurs in that temperatureFootnote 6.
7.4 Assessing risk and decision making process
Once there are employee complaints for heat or cold stress symptoms or the working conditions seem like a risk for thermal stress, then a decision making process must be initiated.
Unlike the heat stress documentation in ACGIH®, cold stress TLVs® do not include any screening process and adjustments. Due to this, the risk for cold stress is estimated differently. ACGIH® provides a general risk management process for evaluating cold stress and strain, which has been adapted belowFootnote 6.
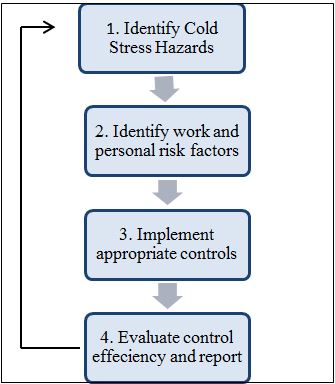
Figure 4 - Text version General risk management process
Figure 4: General Risk Management process flow for Cold Stress exposure reduction, adapted from the Cold Stress section in the ACGIH® TLVs® & BEIs® bookletFootnote 6.
The description of the figure is already provided in the text under the figure (Steps 1 to 4).
As there is no screening or adjustment process, the decision on the probability of cold stress is taken based on temperature measurements, work and personal risk factors, and PPE used. The following steps describe the information in figure 4Footnote 6:
- step 1: Measure weather conditions (temperature, wind chill, rain and snow levels).
- step 2: Identify personal characteristics of the employee such as fitness, body fat, experiences and overall health and work factors such as physical demand, shift duration, shelters, PPE, warming centers, and organization of work.
- step 3: The initial controls should include warming shelters, PPE, food and water, better work-rest schedules for re-warming and changing tasks according to the weather. After that the controls should become more administrative and should include employees in prevention programs by using a buddy system or training them in symptoms of cold stress.
- Buddy systems entail that employees be paired up or work in groups so that they can observe each other for symptoms of thermal stress. This system helps in timely identification of symptoms and first aid.
- step 4: The controls should be supervised and reported periodically so that they can be corrected as needed and if they are not working well, then the process of assessing hazards begins again.
7.5 Cold stress example
The following is an example of a thermal stress problem at the work place which should be solved by a qualified person using the techniques and equations described above. The interpretations of the conditions given in the scenario below are based on the adjustment factors and TLVs® taken from the Thermal stress chapter, section Heat stress and strain, in the ACGIH® TLVs® & BEIs® booklet.
In late January, a 45 year old rail yard worker, with mild hypertension, was working an evening shift from 4pm to 10pm. The temperature that night was -25°C with a wind speed of 5 km/hr (1.4 m/s). He worked on an outside task for about 30 to 45 minutes, while he spent the remaining time of his shift in an indoor setting. After being outdoors, he felt mild pain in his fingers and he was shivering. For most of his shift, he was doing heavy lifting of <40 lbs load, and moving things back and forth. He was wearing steel toe boots, woolen gloves and 1 layer of insulation (1 clo) underneath his winter jacket. He was working in a team of 5 other workers, all dispersed at the yard.
Solution:
- how cold is it?
The first step for screening for risk of cold stress is to determine how cold it is. Using table 4 in the Cold stress section, ACGIH® TLVs® and BEIs® booklet, the wind chill temperature (WCT) is -30°C at the air temperature of -25°C and wind speed of 5 km/hr. This WCT means that there is "increasing risk of frostbite for most people in 10 to 30 minutes of exposure"Footnote 6.
- frostbite risk
Based on the above risk determination through WCT, the employee is at increasing risk when he is completing the outdoor task. Using the temperature parameters, it will take approximately 20 to 30 minutes until cheek frostbite occurs, according to Table 5 in the Cold Stress section, ACGIH® TLVs® & BEIs® booklet. This table shows that there is high risk for freezing to occur in 10 to 30 minutes.
- clothing insulation
Based on the work description provided, we assume here that the employee had moderate work load as he is frequently moving things and is lifting loads <40lbs. Moderate work means that the metabolic requirement is 450 Watts according to Table 2 in the Cold Stress section, ACGIH® TLVs® & BEIs® booklet. 450 Watts means that the metabolic equivalent is 4 to 5, which can then be used to estimate the clothing requirement. From Figure 3 in the Cold Stress section, ACGIH® TLVs® & BEIs® booklet, 4 to 5 metabolic equivalent would equate to1 to 2 clo of clothing insulation at air temperature of -25°C.
- facts
- The employee is at an increasing risk of frostbite if he is exposed 10 to 30 minutes.
- He is already shivering and feels slight pain which means that he is showing early symptoms of hypothermia and moving close to frostbite.
- Working outside for 30 to 45 minutes in 1 clo is risky.
- He is relatively an upper aged worker, has hypertension, and we assume he may be taking some sort of hypertension medication as well.
- He is currently working alone, with fellow employees nearby.
- His gloves are woolen, not waterproof, and he is wearing steel toe boots that do not seem to be insulated.
- recommendations
- Heaters must be used during outdoor and indoor task, and the indoor area must be monitored for temperature periodically.
- He must undergo regular medical surveillance due to his age and hypertension whose medication can affect the perception and tolerance of cold.
- He must take breaks in between his tasks so he is not exposed to the cold for more than 10 minutes at a stretch.
- The task must be adjusted according to the bulkiness of the clothing.
- He must be provided with waterproof gloves and not just woolen gloves, and must wear warm working boots.
- The employees must be paired up if possible in other words use buddy system.
- He should also wear 2 clo or layers of insulation rather than 1 as that is more protective in this situation.
7.6 Controls for cold environment
The most effective control measures are engineering controls or elimination/substitution controls followed by administrative controls and finally personal protective equipment (PPE). PPE should be the last resort or should be used as a supplementary control measure.
The following should be employed at work place depending on the temperature, wind chill, work conditions, employee discomfort and especially if the wind chill temperature falls below -12°C.
a) Engineering controls
The main aim of the engineering controls should be that employees are protected from the cold environment and objects.
- Use enclosures and heated shelters or warming rooms for breaks should be put up where possible and if the temperature is below -7°CFootnote 5.
- The work area should be protected from wind and different types of heaters should be used in work areas to protect employees against cold induced injuriesFootnote 5.
- Any equipment, material or work surfaces that will get cold should be insulated so that the employees do not touch a cold surfaceFootnote 5.
According to the ACGIH®, the design of a refrigerator room should limit the air velocity inside to not exceed 1 m/s with an effective ventilation system, and the employees should be provided with special wind proof clothing according to the air velocity insideFootnote 5.
b) Administrative controls
- A regular work-rest schedule, depending on the employee's task and work intensity should be developed and implemented.
- The employees should have flexibility in taking breaks, if they feel the need to do so, and also in adjusting the work depending on the weather conditions.
- Employees should be encouraged to use heated shelters as soon as they start shivering too much or start having early symptoms of cold stress such as fatigue, irritability, pain etc.
- Majority of the work should be aimed to be completed during the day and the time spent outdoors should be limited.
- New employees should be acclimatized by giving them only part time work. Once the employees are comfortable with the task and PPE, and have adapted to the working conditions, they can be slowly moved to full time work.
- Employees should have variety and balance of tasks that do not include prolonged sitting or standing, nor contact with cold surfaces for long periods of time.
- In addition, if temperature is at or below -12°CFootnote 5:
- Buddy system or supervision should be employed;
- The work rate should not be so high as to cause heavy sweating that will result in wet clothing;
- The weight and bulkiness of clothing should be included in estimating the required work performance and weights to be lifted by the employee.
Note: More details could be obtained in the ACGIH® "Documentation on Cold Stress", under "Work-Warming Regimen"Footnote 5.
c) Personal Protective Equipment (PPE)
PPE is the least desired form of control and should only be used as a supplementary control in addition to the other controls employedFootnote 5,Footnote 6.
- In cold conditions, PPE can include multiple layers of insulated clothing (a least 2 to 3 layers), thick gloves and hats.
- Heating pads can also be worn under regular clothing.
- The PPE needs to be warm, water proof and also protect against wind if possible once the temperature is below -12°C.
- When working outdoors or in the snow, employees should be provided with UV and glare protective goggles.
- Extra clothes and jackets can be worn depending on the type of work and work intensity.
d) Prevention techniques
The following techniques should be included in the thermal stress hazard prevention program implemented at a work place.
Medical surveillance: Even though this is not a regulatory requirement, it is a recommended best practice measure for secondary prevention and predicting any future illnesses. If the external temperature falls below -1°C, then the employees with chronic health conditions or using prescribed medicines affecting body thermoregulation system should be restricted from working and given modified workFootnote 5,Footnote 6. Employees with chronic disease or older employees should undergo regular medical surveillance to update any change in their health which could affect susceptibility to cold stressFootnote 5, Footnote 6.
Training: It should be provided to new and experienced employees periodically and with every change in their tasks. The training should focus on hazards of cold environments, how to prepare for the cold working conditions, first aid, eating, drinking and clothing requirements, warming techniques and safe work practicesFootnote 5, Footnote 6. The employees should also be aware of the signs and symptoms of cold stress induced injuries and illnesses so that they can identify or detect any signs in their fellow employees and alert management in a timely mannerFootnote 5, Footnote 6.
Personal hygiene/health: Employees should keep themselves fit and healthy so that their body is able to adapt to the cold conditionsFootnote 2. Employees should be mindful of their alcohol intake and drugs that they take. They should also keep themselves hydrated by drinking a lot of fluids with enough salt intakes. When they enter a heated shelter, the employees should remove the outer clothing and loosen the remaining clothing for sweat evaporation. The employees should keep an extra change of clothes with them, including extra warm clothes to use in extreme weather conditions or when leaving the heated shelters, if needed.
Reporting: Employees, supervisors and managers are liable to timely report any incident or symptoms of cold stress in employeesFootnote 3. The reports should be kept up to date and detailed enough to prevent future injuries and illnesses. Employers should also use the buddy system where employees can observe and report any signs or symptoms of cold stress in their fellow employee or themselves.
8. Resources
Resources for training or awareness purposes: