Horizontal Evaluation of the Canadian Drugs and Substances Strategy: Evaluation Report
Final report
August 2023
Prepared by the Office of Audit and Evaluation
Health Canada and the Public Health Agency of Canada
Table of contents
List of acronyms
- 2SLGBTQIA+
- Two-Spirit, Lesbian, Gay, Bisexual, Transgender, Queer and/or Questioning, Intersex, Asexual, and additional sexual orientations and gender identities
- CADS
- Canadian Alcohol and Drugs Survey
- ADM
- Assistant Deputy Minister
- BC
- British Columbia
- BSO
- Border services officer
- CBSA
- Canada Border Services Agency
- CCSA
- Canadian Centre on Substance Use and Addiction
- CDSA
- Controlled Drugs and Substances Act
- CDSS
- Canadian Drugs and Substances Strategy
- CHIRPP
- Canadian Hospitals Injury Reporting and Prevention Program
- CIHI
- Canadian Institute for Health Information
- CIHR
- Canadian Institutes of Health Research
- CNS
- Central nervous system
- CND
- UN Commission on Narcotic Drugs
- CPADS
- Canadian Postsecondary Education Alcohol and Drug use Survey
- CRA
- Canada Revenue Agency
- CRISM
- Canadian Research Initiative in Substance Misuse
- CSAR
- Centre for Surveillance and Applied Research
- CSC
- Correctional Service Canada
- CTADS
- Canadian Student Tobacco, Alcohol and Drugs Survey
- CSTADS
- Canadian Student Tobacco, Alcohol and Drugs Survey
- DAS
- Drug Analysis Services
- DG
- Director General
- DTC
- Drug Treatment Court
- DTCFP
- Drug Treatment Court Funding Program
- ETF
- Emergency Treatment Fund
- FASD
- Fetal Alcohol Spectrum Disorder
- FINTRAC
- Financial Transactions and Reports Analysis Centre of Canada
- FP
- Federal Policing
- FPT
- Federal/Provincial/Territorial
- FY
- Fiscal Year
- G&Cs
- Grants and Contributions
- GAC
- Global Affairs Canada
- HC
- Health Canada
- HPFB
- Health Products and Food Branch
- HRF
- Harm Reduction Fund
- IEWG
- Interdepartmental evaluation working group
- iOAT
- Injection opioid agonist treatment
- ISC
- Indigenous Services Canada
- JUS
- Department of Justice Canada
- M
- Million
- NADS
- National Anti-Drug Strategy
- OAE
- Office of Audit and Evaluation
- OAT
- Opioid agonist therapy
- OPTIMA
- A Pragmatic Randomized Control Trial Comparing Models of Care in the Management of Prescription Opioid Misuse
- OUD
- Opioid Use Disorder
- PBC
- Parole Board of Canada
- PHAC
- Public Health Agency of Canada
- PMERC
- Performance Measurement, Evaluation and Results Committee
- PPDU
- Problematic Prescription Drug Use
- PPSC
- Public Prosecution Service of Canada
- PS
- Public Safety Canada
- PSPC
- Public Services and Procurement Canada
- PT
- Provincial/Territorial
- PWLLE
- Persons with Lived and Living Experience
- PWUDs
- People who use drugs
- QoL
- Quality of Life
- RCMP
- Royal Canadian Mounted Police
- SCS
- Supervised Consumption Sites
- SDG
- Sustainable Development Goals
- SGBA+
- Sex and Gender Based Analysis Plus
- StatsCan
- Statistics Canada
- STBBI
- Sexually transmitted and blood-borne infections
- SUAP
- Substance Use and Addictions Program
Executive summary
Profile and evaluation scope
Canada is experiencing an unprecedented rate of substance use-related deaths and harms due to a number of complex, interrelated factors. The Canadian Drugs and Substances Strategy (CDSS), which was first announced in 2016, sets out the federal government's comprehensive, collaborative, compassionate, and evidence-based approach to drug policy that focuses on substance use as a public health issue. The CDSS replaced the National Anti-Drug Strategy (NADS), which was established in 2006, and the lead changed from the Department of Justice to Health Canada. From 2017 to 2022, Health Canada coordinated federal investments and activities across the full spectrum of legal and illegal substances under 4 pillars: prevention, treatment, harm reduction, and enforcement. In 2018, the federal government launched the "Addressing the Opioid Crisis" initiative (the Opioid Initiative), a complementary horizontal initiative that received some reallocated funding from the CDSS. The CDSS and the Opioid Initiative are overseen by the Minister of Mental Health and Addictions and Associate Minister of Health, as of 2020-21. Health Canada (HC) is the lead department for both initiatives and supported by 15 other federal departments and agencies.
This evaluation looked at all funded partners' activities from 2017-18 to 2021-22 under both horizontal initiatives and focused on progress made toward delivering on Pillar objectives and shared outcomes (see Figure 1), including HC's Substance Use and Addictions Program (SUAP) and PHAC's Harm Reduction Fund activities to address Financial Administration Act requirements. However, activities related to tobacco and cannabis, including SUAP projects for these substances, were excluded from this evaluation as there were separate evaluations assessing activities related to these 2 substances.

Figure 1 - Text description
Executive Summary: This diagram shows four boxes representing each CDSS pillar: prevention, treatment, harm reduction and enforcement. Underneath the four boxes lays a rectangle which represents the evidence-base as supporting the four pillars. The diagram also defines the pillar’s expected outcomes as follows:
- Prevention: Canadians make better-informed choices around substances use and risks to reduce harms
- Treatment: Treatment and recovery services and systems are easily accessible, comprehensive, and appropriately tailored to the needs of individuals.
- Harm Reduction: Reduction in risk-taking behavior among people who use drugs or substances.
- Enforcement: Decreased diversion of drugs away from authorized activities and reduced size and profitability of the illegal drug market.
- Evidence Base: Data and research evidence on drugs, and emerging drug trends, are used by members of the federal Health Portfolio and their partners.
On the right hand side of the four pillar boxes shows a fifth box outlining the Addressing the Opioid Crisis Horizontal Initiative themes.
- Theme 1: Additional prevention and treatment interventions
- Theme 2: Addressing stigma
- Theme 3: Taking action at Canada’s border
- Theme 4: Enhancing the evidence base
What we found
Overall, the CDSS and Opioid Initiative have helped to frame substance use as a public health matter and contributed to expanding access to harm reduction and treatment services across Canada through regulatory actions, the SUAP and other activities funded through ISC's Mental Wellness Program, among others. Despite notable efforts to reduce and minimize opioid-related harms and deaths, the number of substance use-related harms and deaths continue to be alarming. The COVID-19 pandemic has also exacerbated the overdose crisis due to increased substance use in isolation, reduced access to support services, and a more potent and toxic illegal drug supply. Increased feelings of isolation, stress, and anxiety have also played a significant role increasing harms related to alcohol use.
Recognizing that the COVID-19 pandemic has had an unprecedented impact on substance use trends during the evaluation period, the CDSS quickly adapted its interventions to address the rise in overdoses through various initiatives, including regulatory actions. However, given the urgency of the crisis, prevention activities and collaboration to address the root causes of substance use were limited and much of the Strategy's focus has consequently been on illegal drugs. While the overdose crisis should continue to be a priority, evidence strongly suggests that other substances could be better addressed under the CDSS. Specifically, given the long-term health and economic impacts linked to alcohol, alcohol use was identified as a gap in the Strategy and as an area of risk and need that requires prevention efforts, including targeted approaches for specific populations like youth.
Moreover, the CDSS has supported ongoing efforts to decrease diversion of drugs through regulatory actions like the accelerated scheduling of novel precursor chemicals, compliance promotion, and compliance and enforcement actions in relation to licensed dealers and pharmacies. However, the increasing toxicity of illegal drugs in Canada is an ongoing issue that is not only leading to an increase in overdoses, but also further complicating the federal government's ability to address the crisis through public health and public safety efforts. Specifically, there are challenges with respect to the increasing illegal importation of precursor chemicals used in the production of illegal drugs in Canada and the regulatory regime's capacity to keep pace with the composition of chemicals produced and sold by organized crime groups.
Finally, the federal government has made significant progress in supporting the development of a wide range of evidence-based tools for members of the federal Health Portfolio and their partners, including treatment guidelines for opioid use disorders. However, gaps were identified in surveillance and data monitoring, in particular with respect to disaggregated surveillance data. There is also limited information, such as a lack of baseline data and targets, to effectively measure the Strategy's impact in addressing drug and substance use as a health and social issue.
The evaluation also examined the CDSS governance structure and found that, despite positive collaboration between horizontal partners, there are still challenges within the structure that limit effective coordination. Opportunities for improvement included clarifying the program mandate and roles and responsibilities of each partner, increasing engagement and discussion opportunities for other federal partners and stakeholders to ensure all views are included, and providing meeting materials earlier to allow other government departments to meet their internal briefing needs.
In terms of external engagement, the establishment of the Persons with Lived and Living Experience (PWLLE) Council was a key success. However, greater representation of people along the spectrum of substance use treatment and recovery is needed. Representation of people with more diverse backgrounds is also necessary, including more meaningful engagement with Indigenous communities and partners.
Recommendations
- Address the prevalence of alcohol use and harms [Health Canada and PHAC].
- Enhance prevention and outreach efforts for higher-risk groups to address the root causes of substance use [Health Canada and PHAC].
- Contribute towards addressing evidence gaps to get a more comprehensive national and regional picture of substance use issues and the domestic illegal drug supply, as well as a better understanding of the impact of services and supports [Health Canada and PHAC, in collaboration with all CDSS partners].
- Enhance the performance measurement strategy to align better with the CDSS's outcomes, including a review of performance indicators to focus more on the impacts of activities [Health Canada, in collaboration with all CDSS partners].
- Review the governance structure to clarify roles and responsibilities, and streamline it where possible, while still facilitating ongoing information sharing between partners and all levels of government [Health Canada, in collaboration with all CDSS partners].
- Work to better understand the domestic illegal drug supply, including its growing toxicity, and the tools that are needed to support more effective law, border, and health responses [RCMP and Public Safety Canada, in collaboration with Health Canada and CBSA.
Evaluation description
Description of the horizontal initiatives
About the Strategy
The Canadian Drugs and Substances Strategy (CDSS), which was announced in December 2016, is the Government of Canada's national and public health-based approach to substance use policy. It replaced the National Anti-Drug Strategy (NADS), which was launched in 2006. Harm reduction was added as a key pillar of the strategy, alongside prevention, treatment, and enforcement. These pillars were also to be supported by a strong evidence base. The CDSS covers a broad range of legal and illegal substances, including cannabis, alcohol, and opioids, among others. In 2018, the federal government launched the "Addressing the Opioid Crisis" initiative (the Opioid Initiative), a complementary horizontal initiative that received some reallocated funding from the CDSS. The CDSS and the Opioid Initiative are overseen by the Minister of Mental Health and Addictions and Associate Minister of Health, as of 2020-21. Health Canada (HC) is the lead department for both initiatives and supported by 15 other federal departments and agencies.
Federal partners
- Canada Border Services Agency (CBSA)
- Canada Revenue Agency (CRA)
- Canadian Institutes of Health Research (CIHR)
- Correctional Service Canada (CSC)
- Justice Canada (JUS)
- Financial Transactions and Reports Analysis Centre of Canada (FINTRAC)
- Global Affairs Canada (GAC)
- Indigenous Services Canada (ISC)
- Parole Board of Canada (PBC)
- Public Health Agency of Canada (PHAC)
- Public Prosecution Service of Canada (PPSC)
- Public Safety Canada (PS)
- Public Services and Procurement Canada (PSPC)
- Royal Canadian Mounted Police (RCMP)
- Statistics Canada (StatsCan)
Strategy context
The evaluation focused on funding allocated to the CDSS from Budget 2017 and the Opioid Initiative from Budget 2018. Between fiscal year 2017-18 and FY 2021-22, approximately $698.20 million was allocated in planned spending across the 2 initiatives. Subsequent federal budgets made further funding commitments to address the overdose crisis, in addition to these initiatives (see Figure 2). In total, between 2017 and 2022, over $800 million was allocated across several federal departments to directly address the overdose crisis, including funding for the CDSS and the Opioid Initiative, as well as for complementary programs and activities.Footnote 1. While these additional funding sources and complementary programs are outside the scope of the evaluation, they directly affect substance use policy, since the CDSS is the guiding framework for the Government of Canada's response to the toxic drug and overdose crisis.

Figure 2 - Text description
This image shows a timeline of federal funding allocated across departments for the overdose crisis between 2017 and 2022, presented from left to right.
- Budget 2017:
- Canadian Drugs and Substances Strategy
- Urgent Support to Provinces and Territories
- Budget 2018:
- Addressing the Opioid Crisis
- Emergency Treatment Fund
- Budget 2019:
- Funding for Actions to Protect Canadians and Prevent Overdose Deaths
- 2020 Fall Economic Statement
- Budget 2021:
- Addressing the Opioid Crisis
- Budget 2022
Financial summary
Over the past 5 fiscal years of the CDSS (2017-18 to 2021-22), the Strategy spent a total of $741.66 (120% of planned amount) across all pillars, excluding internal services costs. Over the past 4 fiscal years of the Opioid Initiative (2018-19 to 2021-22), it spent $78.46M (97% of the planned amount) across all themes, excluding internal service costs. See Annex B for a breakdown of planned spending versus actual spending for both horizontal initiatives, by fiscal year and by organization.

Figure 3 - Text description
This graph is a horizontal bar chart showing the CDSS actual spending by pillar. It shows the percentage of total actual spending from fiscal years 2017-18 to 2021-22 by pillar as follows:
| Category | Spending | Percentage of total actual spending | Partners |
|---|---|---|---|
| Enforcement | $432.69 million | 58% | HC, CBSA, CRA, CSC, GAC, FINTRAC, PBC, PPSC, PS, PSPC, RCMP |
| Prevention | $134.18 million | 18% | HC, ISC, RCMP |
| Treatment | $93.06 million | 13% | CIHR, ISC, JUS |
| Harm Reduction | $61.60 million | 8% | HC, ISC, PHAC |
| Evidence Base | $20.14 million | 3% | HC, PHAC, CIHR |
Amounts exclude internal service costs and lead role.

Figure 4 - Text description
This graph is a horizontal bar chart showing the Opioid Initiative actual spending by theme. It shows the percentage of total actual spending from fiscal years 2018-19 to 2021-22 by theme as follows:
| Category | Spending | Percentage of total actual spending | Partners |
|---|---|---|---|
| Addressing prevention and treatment interventions | $25.99 million | 33% | HC |
| Addressing stigma | $19.31 million | 25% | HC, PS |
| Taking action at Canada's borders | $19.30 million | 25% | CBSA, PS |
| Enhancing the evidence base | $13.86 million | 18% | PHAC, Statcan |
Amounts exclude internal service costs and lead role.
Evaluation approach
Scope
The evaluation was conducted to assess the impact of CDSS activities from 2017-18 to 2021-22 and Opioid Initiative activities from 2018-19 to 2021-22. It was led by Health Canada and PHAC's Office of Audit and Evaluation, in collaboration with funded partners. The evaluation focused on all pillars covering a range of activities including grants and contributions (G&Cs) programs. In particular, the Substance Use and Addictions Program (SUAP), and the Harm Reduction Fund were included to address Financial Administration Act requirements. However, activities related to tobacco and cannabis, including SUAP projects for these substances, were excluded from this evaluation as there were separate evaluations assessing activities related to these 2 substances.
Evaluation questions
- What progress has been made towards delivering on prevention, treatment, harm reduction, and enforcement objectives?
- Were resources used efficiently and effectively? Are the strategy's resources directed towards the greatest areas of risk and need?
- Is there governance in place to support effective collaboration among horizontal partners in support of the prevention, treatment, harm reduction, and enforcement objectives?
- Is there governance in place to support effective collaboration with external partners and stakeholders in support of the prevention, treatment, harm reduction, and enforcement objectives?
Findings in the report are presented by each Pillar's expected outcomes, as defined in the latest available logic model (see Annex C). This is followed by an impact assessment of the shared long-term outcomes and a summary of governance and engagement. Findings related to evidence, resources, and areas of greatest risk and need are discussed throughout.
For evaluation methodology, limitations and related mitigation strategies, and evaluation governance, see Annex A.
Evaluation findings
Prevention
Key takeaways
Over the past 5 fiscal years, Health Canada, under the CDSS and the Opioid Initiative, has raised awareness of substance related harms through national public advertising campaigns, educational engagements, international and national health awareness days or weeks, social media, and community-led projects funded by the SUAP. Still, there is more work to be done to generate behavioural changes among Canadians to prevent substance use-related harms. There are also opportunities to improve Health Canada's collaborative efforts to address the root causes of substance use. Data gaps have impeded assessment of progress for other federal partners funded under the Prevention Pillar.
Short-term outcome 1: Increase knowledge to help Canadians make informed choices and reduce risks and harms of drug and substance use.
Public education campaigns
Health Canada's national public education campaigns on substance use appear to have widespread reach. From fall 2018 to spring 2022, Health Canada ran a 5-phase national advertising campaign focused on 3 topics: opioid awareness, awareness of the harms of substance use stigma, and the Good Samaritan Drug Overdose Act.
The 2020-21 campaign surpassed its targets, with 98.9 million ad impressions and increased opioid-related web traffic on Canada.ca by 60%.Footnote 2. The 2021-22 campaign had a relatively smaller reach with 42.4 million impressions. Health Canada staff clarified that the lower count was due to that phase of the campaign taking a more targeted focus on young and middle-aged men, particularly men in trades, as surveillance data shows that this is the group experiencing the highest rates of opioid overdoses and substance use in Canada.Footnote 3 However, disaggregated data is not available to describe the reach to subgroups of the Canadian population, such as reach by age group, gender, or other identity factors.
| Survey response | 2021 | 2019 | 2017 |
|---|---|---|---|
| Certain or pretty sure what opioids are | 67% | 69% | 63% |
| Not at all familiar with at least 1 of the opioids listed | 21% | 16% | 18% |
| Very aware of Canada's opioid crisis | 19% | 25% | 28% |
| Felt the opioid crisis is very or somewhat serious in their community | 61% | 70% | 65% |
While these campaigns appeared to be widely distributed, knowledge of drug and substance use risks and harms among people in Canada remains largely unchanged over the past 5 years. Health Canada commissioned a series of public opinion research studies that have shown minimal changes in public opioid awareness since 2017. According to the 2021 follow up study of a representative sample of Canadians aged 13 and older, awareness of opioids and their risks has remained fairly stable, with a slight peak in 2019 (see Table 1).
The surveys in the research studies did not have a question about awareness of federal public education campaigns, although some focus group participants in the 2019 study shared without being prompted that they had seen Government of Canada public education ads about opioids.Footnote 6. While a few external representatives interviewed for the evaluation mentioned seeing federal public awareness campaigns, a similar proportion of interviewees from community and regional organizations or governments did not feel the campaigns were sufficiently visible. Many interviewees, including several Health Canada representatives, flagged gaps in public awareness activities for substances other than opioids, most notably for alcohol.
Finally, several internal and external interviewees identified a need to improve substance use prevention strategies targeting youth and children. However, it should be noted that Health Canada has been running the Know More Opioids Footnote 7 awareness program for youth since April 2018 (see the following section). Additionally, although not funded under the CDSS Prevention Pillar, PHAC developed a set of resources for preventing substance-related harms among Canadian youth through action within school communities. In August 2021, PHAC published a policy paper Footnote 8 that describes issues related to youth substance use from a public health perspective and published a "Blueprint for Action" Footnote 9 that outlines practical approaches for schools and community organizations to prevent substance-related harms among youth.
Public engagement activities
As a federal partner funded under the Prevention Pillar of the CDSS, the RCMP's Federal Policing (FP) program developed education products to increase awareness of drugs and illegal substances among stakeholders, conducted outreach and engagement efforts, and built new partnerships.Footnote 10
The RCMP committed to meeting 5 performance indicators related to increasing awareness of drugs and illegal substances. For example, in the first 3 years of the evaluation period, the RCMP met its target of 50% with respect to the percentage of partners and stakeholders demonstrating increased awareness of illegal drugs. Moreover, regarding the number of awareness products developed, the RCMP reported meeting its target of 5 products once in the past 5 years, missing their target by only 1 for most years. Despite this, they were still able to produce a total of 20 drug-related awareness products over the evaluation period, including presentations, fact sheets, and news reports on topics such as suspicious chemical precursor transactions, illegal synthetic drug labs, methamphetamine, and fentanyl. Finally, for the indicator of number of stakeholders reached, the RCMP successfully achieved its target every year (see Figure 5). It should be noted that the 2019-20 numbers are much higher than those reported in previous years, given that this sum includes internal website downloads relating to several synthetic drug products. As such the number of downloads does not necessarily represent the unique number of stakeholders reached.
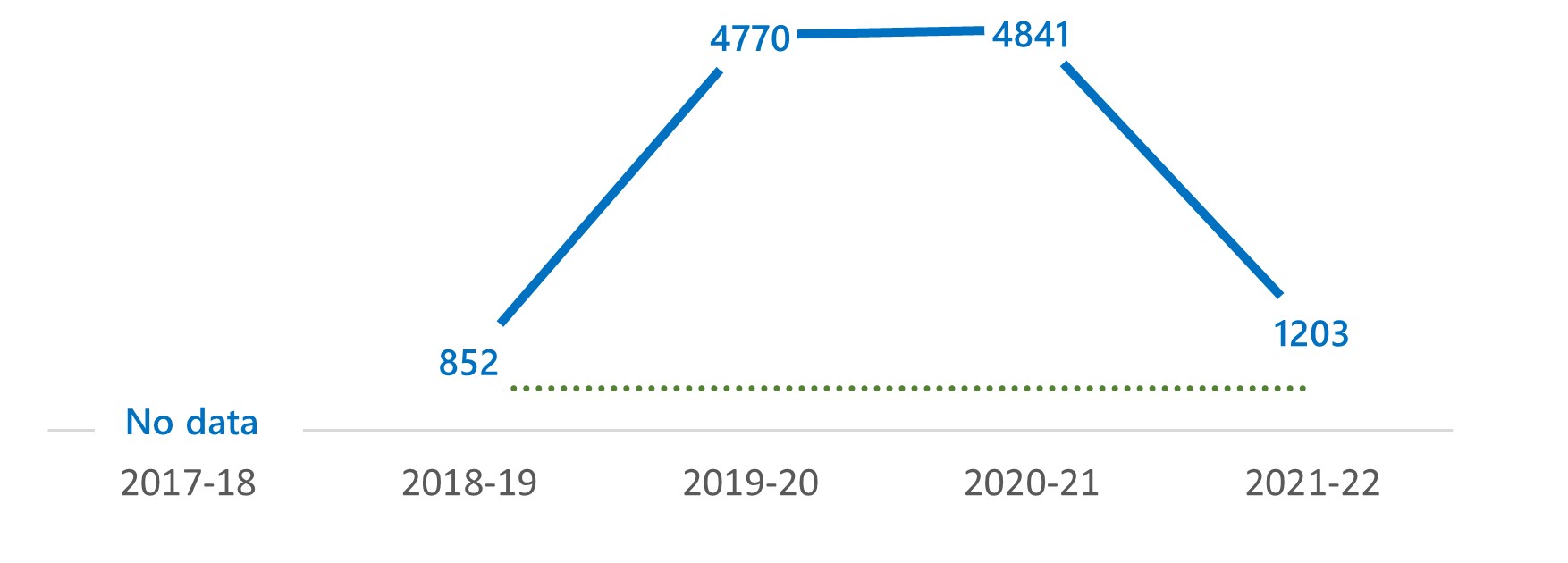
Figure 5 - Text description
Figure 5 is a line graph showing the number of stakeholders reached through RCMP public engagement activities by fiscal year between 2017-18 and 2021-22:
- 2017-18: No data
- 2018-19: 852
- 2019-20: 4770
- 2020-21: 4841
- 2021-22: 1203
- No target
Meanwhile, as part of the Opioid Initiative, Health Canada implemented the "Know More: Opioid public awareness" program targeting Canadian students and youth. Between April 2018 and June 2022, the "Know More" program was involved in 1,148 high school sessions, 68 post-secondary school events, and 43 events and festivals, resulting in over 169,900 participant interactionsFootnote 11. In 2020, the program was adapted for virtual formats in light of pandemic-related public health measures, further expanding its reach of the program.Footnote 12 However, there were no post-event evaluations to measure changes in attitudes or awareness among program participants.
Substance Use and Addictions Program
What is SUAP?
The Substance Use and Addictions Program (SUAP) is a Health Canada G&Cs program that supports the CDSS, the Cannabis Program, and Canada's Tobacco Strategy.
SUAP funds community-led pilot projects to develop evidence or proof of concept for innovative service delivery models to prevent or address substance related harms.
SUAP projects target Canadians at greatest substance use risk or who may face barriers accessing services, including racialized and Indigenous populations, young adults and youth, various gender and 2SLGBTQIA+ populations, and people who face housing insecurity or are street-involved.
From 2017-18 to 2021-22, Health Canada reported spending nearly $96 million for the CDSS and another $26 million for the Opioid Initiative through SUAP G&Cs. The SUAP funds projects across Canada to help prevent, reduce, or treat the harms associated with range of controlled drugs and substances. While SUAP funding is categorized under the Prevention Pillar for reporting purposes, SUAP projects also address outcomes under Treatment and Harm Reduction. SUAP does not allocate or track funding by CDSS pillar as the program is also funded through other initiatives and budget commitments beyond the CDSS.
Currently, in 2023, SUAP funds approximately 290 active projects, with 15% focused on prevention. It should be noted that about 9% of SUAP projects focus on tobacco and cannabis and are out of scope for the evaluation. According to program reporting for fiscal year 2021-22, SUAP's 138 controlled substances projects demonstrated extensive reach and impact on knowledge and awareness among its various target audiences. In the most recent reporting period, SUAP projects developed 59,558 awareness and education products and provided 38,753 learning opportunities, though these included projects related to cannabis and tobacco which were out of scope for this evaluation. Educational products and services were accessed 9.7 million times by people in Canada. Finally, 54% of controlled substances projects met their targets to generate intent among their audiences to use the knowledge and skills they acquired in relation to substance use.
Short-term outcome 2: Increase awareness and collaboration to address the root causes of substance use.
Collaboration with federal partners
Health Canada collaborated with a range of federal organizations, including those not funded under the CDSS, to address root causes and social determinants of health that influence levels of substance use and substance use-related harms, including homelessness, trauma, and mental illness.
For example, housing is an important social determinant of health as rates of addiction and co-occurring mental health challenges are higher among those experiencing chronic homelessness.Footnote 13 Furthermore, people who use substances are at a higher risk of becoming homelessFootnote 14,Footnote 15 due to policies, social norms, and stigma regarding substance use and mental health. To this effect, Health Canada works with Infrastructure Canada, an unfunded CDSS partner, in CDSS working groups and governance committees. Infrastructure Canada oversees a community-based national homelessness strategy that includes considerations for substance use prevention and treatment.Footnote 16 Nonetheless, there appear to be mixed views on the extent to which the CDSS has increased awareness and collaboration to address the root causes of substance use. Many interviewees, including over a third of external interviewees, felt that the CDSS has not advanced this issue.
In interviews with CDSS federal partners, a few interviewees described good interdepartmental collaboration on addressing root causes or social determinants of substance use. However, several internal and external interviews talked about challenges due to conflicting or uncoordinated roles. In a similar vein, a few internal and external interviewees described challenges arising from prevention activities being the purview of provincial, territorial, or municipal governments, not the federal government. See the Governance and Engagement section for further discussion on intergovernmental and external collaborations.
The most cited area for improvement was around collaboration to address homelessness and mental illness. Correspondingly, several interviewees described opportunities to implement prevention interventions using an intersectional approach, such as linking to mental health or counselling programs, or through joint policy initiatives.
Opioid use risk management
Prescription opioids are an important option for management of chronic pain, a health issue that affects an estimated 1 in 5 people in Canada.Footnote 17 However, harmful use of opioids can lead to opioid use disorders (OUD). Personal and social factors, such as trauma and fragmented mental health care, can increase likelihood of development of OUD and worsen opioid-related harms.Footnote 18,Footnote 19,Footnote 20,Footnote 21.
Adverse outcomes of substance use, unintentional overdose, and death resulting from inappropriate prescribing, and harmful use of opioids have emerged as major public health problems. In response to these challenges, Health Canada has conducted a variety of activities to promote and monitor the safety and effectiveness of prescription opioid products, including patient and health care professional education and awareness.
In 2018, Health Canada amended the Food and Drug RegulationsFootnote 22 to prevent and mitigate risks from prescription opioid-related harms through various initiatives, including the requirement for manufacturers to submit a mandatory Canadian Specific Opioid-targeted Risk Management Plan (CSO-tRMP) for prescription opioidsFootnote 23, and the requirement for a warning sticker and patient information handoutFootnote 24 to be provided with prescription opioids at the time of dispensing.
During the evaluation, Health Canada exceeded its CDSS performance indicator target in terms of the percentage of pharmacies inspected that are deemed to be compliant with the CDSA and its regulationsfor all fiscal years except 2018-19 and 2019-20 (see Figure 6). This may be due to compliance framework updates introduced in 2017-18, which meant pharmacies needed time to adjust to the new requirements. Furthermore, the target was not met in 2019-20 due to Health Canada's continued focus on the inspection of pharmacies with a history of non-compliance. This risk-based, targeted inspection approach led to a lower percentage of industry compliance than planned.

Figure 6 - Text description
Figure 6 is a line graph showing the percentage of pharmacies inspected deemed to be compliant with the CDSA and its regulations by fiscal year between 2017-18 and 2021-22:
- 2017-18: 87%
- 2018-19: 75%
- 2019-20: 67%
- 2020-21: 84%
- 2021-22: 83%
- Target: 80%
First Nations and Inuit Mental Wellness Program
ISC used Prevention Pillar funding to support prevention, harm reduction, and treatment activities and services in First Nations and Inuit communities. These include substance use case management supports for prescription drugs, prevention, and training activities. At this time, no information on the performance of the Mental Wellness Program is available since ISC does not have indicators under the Prevention Pillar. Additionally, it should be noted that an evaluation of ISC's Mental Wellness Program is currently underway.
Medium-term outcome 1: Canadians make better informed choices around substance use and risks to reduce harms.
Recent surveillance data shows that rates of substance use were relatively stable until the pandemic, although behaviours associated with higher risks of harms had increased. The 2019 Canadian Alcohol and Drugs Survey (CADS) found that consumption of illegal drugs among people in Canada remains low with only about 4% having used at least 1 illegal drug, though this proportion is relatively unchanged when compared to results from the 2017 Canadian Tobacco, Alcohol and Drugs Survey (CTADS).Footnote 25 The 2019 survey also found that alcohol continues to be the most consumed substance in Canada. Meanwhile, rates of higher-risk use of substances and associated harms appear to have increased since 2017, particularly for young adults (see Table 2).
It is important to note that these surveys predate the COVID-19 pandemic, which posed significant challenges to individuals and to the health care system and led to increased substance use and likely heightened substance-related harms. Recent surveillance data shows that opioid-related hospitalizations and deaths in Canada have increased significantly since 2020.Footnote 26 A 2021 PHAC survey also found that many respondents had increased their substance use during the pandemic.Footnote 27
| Survey question | % of population | |
|---|---|---|
| Exceeding low-risk drinking guidelines - chronic |
2019 | 2017 |
| Overall population | 17.6% | 16.1% |
| Age 20-24 | 26.2% | 24.1% |
| Problematic use of stimulants | 2019 | 2017 |
| Overall population | 0.8% | 0.3% |
| Age 20-24 | 4.8% | 1.9% |
| Problematic use of any pharmaceuticals | 2019 | 2017 |
| Overall population | 1.6% | 1.2% |
| Age 20-24 | 5.5% | 3.6% |
| Any drug harm to self | 2019 | 2017 |
| Overall population | 4.5% | 4.1% |
| Age 20-24 | 13.8% | 10.1% |
Health Canada-commissioned research studies also found that people have continued to engage in opioid use behaviour that increases risk of harm. In 2021, a third (34%) of study respondents who reported use of non-prescribed opioids said they obtained them from a relative or friend who has a prescription, a 4% decrease from 2017.Footnote 31 Notably, only two-thirds (65%) of respondents in 2021 said they "definitely would no longer take non-prescribed opioids if they discovered they contained fentanyl," a 4% increase since 2017. Other questions related to risk behaviours, such as safe storage of opioids and appropriate medication disposal, also remained relatively stable between 2017 and 2021.
These minimal changes since 2017 to rates of high-risk substance use suggest further prevention efforts are required. Several interviewees, particularly federal partners, described opportunities to increase use of policy measures to change substance use outcomes. They cite the success of tobacco regulations and the opportunity to apply similar measures to reduce harmful consumption of other substances, particularly alcohol. however, challenges in changing substance use outcomes are not unique to the CDSS. Studies increasingly show that an individual's intent and ability to address harmful substance use is affected by inequities and differences in lived experiences. As such, public health interventions tend to be more effective when they focus on changing the physical, material, and social environments, rather than individual behaviour.Footnote 32
Area of risk and need: Harms from alcohol use
Alcohol is the second leading cause of death from substance use in Canada after tobacco. Footnote 33, Footnote 34 Research from 2023 found that, in Canada, alcohol use incurs higher costs and harms than other substances. This includes health care costs, criminal justice system costs, losses in productivity, and other direct costs (see Figure 7). Footnote 35 Yet, interviewees and scientific literature note challenges to preventing alcohol use-related harms due to the normalization of alcohol and the lack of awareness of its harms. Footnote 36
Research and interviews reveal policy opportunities to prevent some of the health and social costs of alcohol use. Participants in a 2018 consultation held by Health Canada made several suggestions, including the following:Footnote 37
- Increasing awareness of alcohol harms, including alcohol-impaired driving;
- Instituting legislative and regulatory changes that control the affordability and availability of alcohol;
- Developing a national alcohol strategy; and
- Restricting alcohol marketing and advertisements, including through social media.
It is important to note that alcohol harms do not have an equal impact on everyone. Alcohol use and related health and psychosocial effects vary by sex, gender, and social determinants of health. For example, research has found women and females assigned at birth are more at risk than men and males assigned at birth to face alcohol-related harms due to biological differences in susceptibility to intoxication and disease, and to alcohol-related violence against women.Footnote 38 Future prevention and awareness efforts need to take into account the differential impacts in the harms associated with alcohol consumption between different populations. Finally, the federal government received a failing grade (37%) in the Canadian Alcohol Policy Evaluation's (CAPE) most recent assessment of the effectiveness of government policies in reducing alcohol-related harms in Canada and identified several recommendations to improve their score, including the development of an alcohol strategy.Footnote 39

Source: Canadian Substance Use Costs and Harms Scientific Working Group (www.csuch.ca/explore-the-data) CNS = Central Nervous System
Figure 7 - Text description
Figure 7 is a stacked bar chart graph that shows the total costs (in billions) related to substance use in Canada from 2007 to 2020, by substance and cost type. Each stacked bar represents a substance, and each stack bar is broken down by cost type. Cost types are labelled by colour and are represented as follows for each substance:
| Substance | Health care costs | Lost productivity costs | Criminal justice costs | Other direct costs | Total cost |
|---|---|---|---|---|---|
| Alcohol | $6.27 billion | $7.87 billion | $3.97 billion | $1.57 billion | $19.67 billion (40.09%) |
| Tobacco | $5.43 billion | $5.25 billion | $5.5 million | $471.1 million | $11.15 billion (22.74%) |
| Cannabis | $380.6 million | $490.9 million | $1.07 billion | $443 million | $2.38 billion (4.85%) |
| Opioids | $519.0 million | $5.26 billion | $1.18 billion | $163.2 million | $7.07 billion (14.42%) |
| Other Central Nervous System (CNS) depressants | $240.6 million | $489.6 million | $344.8 million | $294.2 million | $1.37 billion (2.79%) |
| Cocaine | $184.3 million | $1.41 billion | $2.41 billion | $149 million | $4.16 billion (8.48%) |
| Other Central Nervous System (CNS) stimulants | $359.1 million | $1.54 billion | $928.9 million | $200.5 million | $3.03 billion (6.18%) |
| Other substances | $25 million | $57.2 million | $117.3 million | $20.7 million | $0.22 billion (0.45%) |
Treatment
Key takeaways
Overall, evidence shows that the CDSS and Opioid Initiative have expanded access to evidence-based treatment services and systems, though inequities still exist in terms of accessibility to treatment. Specifically, interviews and documents identified a number of barriers to accessing treatment and pointed to a need for more integrated and recovery-focused care.
Short-term outcome 3: Federal actions support the expansion of evidence-based treatment services and systems.
Emergency Treatment Fund
It should be noted that provinces and territories (PT) are primarily responsible for the delivery of treatment services, but that the Government of Canada provides some substance use services and supports to certain federal client populations, including First Nations people living on reserves, Inuit, Canadian Armed Forces members, veterans, and federally incarcerated populations.
Though not funded under the CDSS or Opioid Initiative, the establishment of Health Canada's Emergency Treatment Fund (ETF) contributed towards Treatment Pillar objectives during the evaluation period. The ETF was announced as part of Budget 2018 funding to provide additional support to help address the opioid overdose crisis.
ETF provided 1-time emergency funding of $150M for provinces and territories (PT) to improve access to evidence-based treatment services over 3 years, which when cost-matched by provinces and territories, was expected to result in an investment of over $300M.Footnote 40 Interviewed provincial and territorial representatives noted an appreciation for the funding provided through the ETF, which supported an overall increase in access to treatment services. According to annual reports from PTs, ETF investments have improved access to treatment services across Canada, with reports indicating that progress has been made on the following issues:
- Reducing treatment wait times;
- Increasing the number of treatment beds;
- Increasing Rapid Access Addiction Medicine clinics;
- Improving access to culturally appropriate care for Indigenous communities;
- Expanding access to virtual supports;
- Supporting providers through training opportunities;
- Addressing methamphetamine use; and
- Improving health systems and building community-level capacity.
Substance Use and Addictions Program
Health Canada also helped to increase availability of Opioid agonist therapy (OAT) in communities across Canada through the SUAP. For example, SUAP funding helped open the first injection Opioid Agonist Treatment (iOAT) clinic in New Brunswick and enabled the clinic to double its intake target and capacity within the first year of receiving funding. Opioid agonist therapy (OAT) is a form of therapy for opioid users that consists of injection of lower-potency opioids such as methadone, Suboxone (buprenorphine-naloxone), and Sublocade (injectable buprenorphine).
Interviewees also highlighted how SUAP has expanded access to treatment services at the community level throughout multiple jurisdictions. It should be noted that interviewees often did not distinguish treatment from harm reduction, but rather spoke of their activities and impacts in relation to one another. Among the 92 new SUAP projects in 2021, 9% focused on treatment, which included 3 projects explicitly focused on treatment and 2 OAT projects.
Overall, internal, and external interviewees agreed that federal actions have supported the expansion of evidence-based treatment services and systems through the ETF and SUAP funding, but that the sustainability of services and research activities is largely dependant on federal funding which is time-limited.
Highlight: COVID-19 rapid response
In May 2020, CIHR provided the Canadian Research Initiative in Substance Misuse (CRISM) with $1 million to undertake urgent activities to support people who use drugs (PWUDs), decision-makers and care providers in light of COVID-19. This included the creation of 6 national guidance documents and a rapid assessment of the challenges faced by PWUDs during the COVID-19 pandemic to guide future policy decisions
Enhancing the evidence base for treatment
While only a very small proportion of internal and external interviewees spoke about evidence around substance use treatment, a few internal and external interviewees observed successes in expanding such evidence under the CDSS. The most cited examples were tied to work by the CRISM, including their development of national guidelines, large clinical trials, and rapid response evidence documents during the pandemic.
Supporting treatment guideline development
The CDSS also supported the development of treatment guidelines for health care providers, including clinical guidelines for OAT and national treatment guidelines for opioid use disorders, and delivered it to physicians across Canada. The guidelines provide health care professionals with recommendations on managing opioid use and were developed through extensive consultations with experts and people with lived experience.
In addition to CDSS funding, CIHR provided $17 million in new funding in 2022 to support the next phase of CRISM (Phase II) and launched 2 new funding opportunities to support the creation of a Network Coordinating Centre to support and coordinate governance, training, capacity building and knowledge mobilization across CRISM; as well as an Indigenous Engagement Platform to support Indigenous engagement across the CRISM Network.
A Pragmatic Randomized Control Trial Comparing Models of Care in the Management of Prescription Opioid Misuse (OPTIMA)
OPTIMA is the first randomized clinical trial to compare the relative effectiveness of buprenorphine naloxone (flexible take-home doses) versus methadone (daily witnessed ingestion) models of OAT for people who use drugs in real-world clinical settings. Results from the OPTIMA not only provide valuable evidence around treatment effectiveness of OAT for those with prescription opioid use disorders, but resulting publications are expected to generate additional evidence on issues of patient retention in treatment, best practices around administration of OAT, and cover other important areas like mental health, cost effectiveness of OAT, and overdose data related to different treatment options.Footnote 41
Since the completion of the trial in March 2020, the CRISM Network has continued to target key stakeholder groups, including PWLLE who are seeking OAT, health care providers and key stakeholders involved in policy and programs for opioid use disorder care, and community advocacy groups in substance use, for knowledge mobilization and dissemination activities related to the trial findings.
Alcohol policy and intervention research
In March 2022, under the CDSS, the CIHR in partnership with the Canadian Cancer Society, funded 20 research projects to expand the evidence base and to inform practical policies and interventions to reduce alcohol-related harms in Canada. This research is expected to generate data and evidence that will increase the knowledge base on alcohol-related harms and how to prevent and treat them, as well as inform future larger-scale research projects.Footnote 42
Nonetheless, a few academics and subject matter expert interviewees cited the need for enhanced national standards, guidelines, and strategies to guide the use of treatment evidence. A few CDSS federal partners also described gaps in treatment evidence, particularly in research on populations disproportionally affected by substance-related harms.
Medium-term outcome 2: Treatment and recovery services and systems are easily accessible, comprehensive and appropriately tailored to the needs of individuals.
Drug Treatment Courts (DTCs)
DTCs provide an alternative to incarceration by offering the offender an opportunity to participate in a court-monitored and community-based drug treatment program. DTCs are supported under the CDSS and funded under the Justice Canada administered Drug Treatment Court Funding Program (DTCFP). In 2021-22, 69% of participants stayed in federally-funded DTC programs for more than 6 months, exceeding the expected target of 50%. While the expected target was not met in the first 2 years of the CDSS, there was a steady increase in the DTC participant retention rate, indicating that the program is achieving its intended goals under the Strategy to support alternative ways of responding to the causes and consequences of drug-related offenses (see Figure 8).

Figure 8 - Text description
Figure 8 is a line graph showing the drug treatment court participant retention rate (in percentage), by fiscal year between 2017-18 and 2021-22:
- 2017-18: 37%
- 2018-19: 46%
- 2019-20: 58%
- 2020-21: 68%
- 2021-22: 69%
- Target: 50%
However, certain groups, including women, Indigenous, and racialized Canadians, are seen as being underrepresented in DTC programs. A recent evaluation of Justice Canada's DTC Funding Program found that some stakeholders would like to see greater flexibility in the eligibility criteria, as well as increased use of experimentation. These findings led to a recommendation to consider ways to support DTCs in efforts to include groups who may be under-represented or experiencing barriers to access.Footnote 43
While not specifically funded under the CDSS, PPSC is also a key component of DTCs. Specifically, PPSC prosecutors work with judges, defence counsel, treatment providers, and others to collaboratively address the issues raised by the conduct of offenders appearing before these courts. In some cases, PPSC agrees to reduce sentences for traffickers with substance use disorders who have demonstrated that they are addressing their disorder through treatment, as well as the continued option of attending the DTC.Footnote 44
Expanding access to treatment for First Nations and Inuit communities
Indigenous populations in Canada are disproportionately affected by the overdose crisis and the use of opioids and other substances. ISC has been an instrumental partner in supporting the Strategy's treatment objectives as they relate to expanding access to services and supports for First Nations and Inuit communities in Canada.
Specifically, ISC supports a number of ongoing activities including treatment centre accreditation and certification incentive funding for substance use workers. Moreover, the CDSS also provided the initial funding for Mental Wellness Team pilots and continues to provide $2 million in ongoing funding for the Mental Wellness Program. In addition to these activities, ISC also supports OAT wraparound services in First Nations and Inuit communities. Wraparound services work to address underlying or associated issues through counselling and traditional practices. While barriers to accessing treatment still exist, there was a significant increase in the number of sites funded by ISC that offer OAT wraparound services after the first year of CDSS funding, and then a steady increase in subsequent years during the evaluation period (see Figure 9). As indicated by interviewees, this funding was important in leveraging other sources of funding to support wraparound services. Interviews also indicate that funding has been impactful in raising awareness about harm reduction and increasing availability of services. Highlights from interviews include bulk purchases of Naloxone when availability was limited, the launch of OAT wraparound services, and related training for staff.
![Figure 9: Number of sites [funded by ISC] offering OAT wraparound services, 2017-18 to 2020-21](/content/dam/hc-sc/images/corporate/transparency/corporate-management-reporting/evaluation/canadian-drugs-substances-strategy/fig9-en.jpg)
Figure 9 - Text description
Figure 9 is a line graph showing the number of sites (funded by Indigenous Services Canada) offering opioid agonist therapy (OAT) wraparound services by fiscal year between 2017-18 and 2021-22:
- 2017-18: 15 sites
- 2018-19: 58 sites
- 2019-20: 68 sites
- 2020-21: 72 sites
- 2021-22: 72 sites
It should be noted that the same indicator related to OAT sites and their results are reported by ISC under the Harm Reduction Pillar, as funding and activities support both Pillars' objectives. Moreover, ISC-supported OAT sites are funded through multiple funding sources in addition to the CDSS, including Budget 2018, provincial funding, and internal regional reallocations. Therefore, the impact of ISC-funded OAT sites cannot be entirely attributed to the CDSS. Indicators and funding for other treatment partners intersect and may support activities under other pillars.
Finally, from 2017 to 2022, Justice Canada's Youth Justice Fund supported numerous projects across the country for youth involved in the youth justice system and who have substance use issues, many of which supported Indigenous organizations and initiatives.
Recovery-oriented care
Several interviewees spoke about the need for more integrated and recovery-oriented care. For example, both internal and external interviewees noted a gap in the Strategy when it comes to recovery, highlighting that federal actions have been more focused on harm reduction than addressing the root causes of substance use. One interviewee noted that "people need to hear stories of hope that recovery is possible". Similarly, many interviewees agreed that there is a need for more integrated care, one that takes mental health and other social determinants of health, such as housing, into consideration. Interviewees also noted the positive linkage between harm reduction and wraparound services as a pathway to treatment and recovery, supporting a continuum of care.
Barriers impeding access to treatment
While activities and results show that progress has been made in making treatment and recovery services more accessible, interviewees and documents noted that regional disparities in the availability of services and supports bring challenges in providing equitable access to treatment services across Canada, especially for marginalized groups.
Recognizing that PTs are primarily responsible for the delivery of treatment services, many interviewees emphasized the need for more resources to address increasing treatment demands, and the need for more medical education focused on substance use and addiction treatment, including recruitment of addiction specialists and counsellors. Several other systemic barriers that create inequitable access to treatment were also identified in the literature and by interviewees, including stigma, location and distance of services, lack of culturally appropriate treatment, long wait times, cost of services. In addition, evidence from interviews and literature show that COVID-19 had significant negative impacts on substance use and access to health care during the pandemic, leading to a combination of increased use and reduced services. In response to treatment challenges brought forward by the COVID-19 pandemic, Health Canada has implemented a number of regulatory actions that have removed some barriers to accessing drugs for the treatment of opioid use disorders, such as authorizing pharmacists to prescribe controlled substances. Other regulatory actions will be discussed further in the following section on Harm Reduction.
Harm reduction
Key takeaways
The CDSS and Opioid Initiative have helped to expand the availability of harm reduction services, including supervised consumption sites and safer supply projects, through funding support and legislative and regulatory activities; however, evidence shows disparities in access to harm reduction services. There appears to be widespread awareness of the negative impacts of stigma on people who use drugs; nonetheless, substance use stigma persists, indicating the need for further education of the public, health care workers, and law enforcement.
Short-term outcome 4: Increase awareness of harm reduction principles and services for a wide variety of drugs and substances.
Some external interviewees spoke about how there is now widespread recognition of and support for harm reduction work in Canada. Many credit the federal government and the CDSS for driving the recent shift toward taking a public health approach to substance use, of which harm reduction is an important pillar. Population-based surveys appear to support this view. A series of public opinion research studies between 2017 and 2021 show a consistently high proportion of the Canadian public view the opioid overdose crisis as a public health issue, with around 3 quarters of survey respondents agreeing.
Naloxone, also called Narcan, is a medication and an evidence-based harm reduction measure that can help prevent death from opioid overdose. In 2021, nearly half (47%) of survey respondents were aware of what naloxone is and what it's used for and about a quarter (26%) knew where to get naloxone, although less than a fifth of respondents (18%) said they knew how to administer naloxone.Footnote 45
Finally, as previously discussed under the Prevention Pillar, Health Canada ran a multi-year digital advertising campaign to raise awareness of harm reduction measures, the negative consequences of substance use stigma, and the Good Samaritan Drug Overdose Act. These campaigns have reached millions of people in Canada.
Table 3: Key types of harm reduction measures
Safer Supply
This is a general service to prevent overdoses and death by providing people who use drugs with access to pharmaceutical-grade medications as a safer alternative to drugs obtained through the toxic illegal drug supply.Footnote 46 This also includes distribution of sterile drug use equipment to reduce the risk of transmitting bloodborne infections.Footnote 47
Take-Home Naloxone
Naloxone is a life-saving medication that can temporarily reverse the effects of opioid overdoses. Naloxone kits are available at many pharmacies without need for prescription and can be obtained from community-based organizations.Footnote 48
Drug Checking Services
These are services that test drugs and offer people who use drugs information on the composition of drugs in their possession.
Supervised Consumption Site (SCS)
This kind of site provides a safe space for people to bring their own drugs to use in the presence of trained staff to prevent accidental overdoses and reduce the spread of bloodborne infections.Footnote 49 SCSs operate under an exemption at the discretion of the Minister of Health in each province and territory.
Short-term outcome 5: Increase awareness of, and begin to reduce the negative impacts of stigma towards people who use drugs.
Stigmatization of people who use substances continues to be one of the greatest barriers for people to seek help and stay recovered.Footnote 50,Footnote 51Moreover, according to the Chief Public Health Officer of Canada's 2019 Report on the State of Public Health in Canada, stigma is an important contributor to social and health inequities.Footnote 52 The evaluation found that federal campaigns and resources to address stigma have broad reach, and that awareness of substance use stigma is generally high. Nonetheless, stigmatizing attitudes persist in Canadian society.
Anti-Stigma Public Education Campaign
Since 2018-19, Health Canada has sought to end stigma against people who use opioids through a widespread and highly visible national advertising campaign. According to public reporting, the digital campaign received more than 167 million views, including incomplete views, between 2018-19 and 2021-22.Footnote 53,Footnote 54,Footnote 55,Footnote 56 In 2020, Health Canada launched the Stigma Gallery, a website that shares stories from people with lived and living experience of substance use, to address stigma around substance use. Reducing stigma was also a key theme in Health Canada's "Know More" substance use education tour for youth and young adults in Canada.
Additionally, Health Canada provided SUAP funding to non-profit organizations to develop and implement public education to address substance use stigma (see Table 4).
| Funding Recipient | Key Activities |
|---|---|
| Canadian Centre for Substance Use and Addictions (CCSA) | Stigma Ends with Me Workshops and development of the "Overcoming Stigma through Language Primer". |
| Community Addictions Peer Support Association | Public education and community engagement activities and development of a national public engagement tool. |
| Moms Stop the Harm | In-person and online support workshops and support groups for families with relatives who have a substance use disorder. |
Recent survey evidence reveals that most people in Canada now recognize the negative impacts of substance use stigma. The evaluation following Health Canada's anti-stigma campaign in 2019 found that 57% of respondents believe that stigma creates a barrier to seeking treatment for substance use disorders.Footnote 57Similarly, Health Canada's 2021 public opinion research found that people were generally aware that stigma exists against people who use drugs and that it can limit people from seeking help, though these results were relatively unchanged compared to a previous survey from 2019.Footnote 58 Despite high levels of awareness of stigma, respondents to both the 2019 and 2021 surveys expressed conflicting personal beliefs, with many agreeing with stigmatizing misconceptions that blame substance use disorder on individual behaviour while also agreeing to statements expressing sympathy with people who use opioids. Focus group results revealed that people who held stigmatizing views often had difficulty recognizing that their views perpetuated stigma.Footnote 59
Interviews with representatives of regional and community-based organizations shared concerns about persistent stigmatizing beliefs among the Canadian public. A few people felt that stigma is particularly concentrated among groups that are already at a great disadvantage due to systemic discrimination. For instance,1 interviewee described how those dying from the overdose crisis are being "seen as disposable people and their lives are not valued," which impedes action to help more disadvantaged groups.
Resources and Training for Professional Groups
Substance use stigma can result in health, social, and justice policies and programs that discriminate against people with substance use disorders. This can lead to lower quality of support and care and further marginalization, such as through criminalization and refusal of employment.Footnote 60,Footnote 61,Footnote 62,Footnote 63
Under the CDSS and the Opioid Initiative, the federal government has made progress on addressing substance use stigma among government stakeholders, health care professionals, and law enforcement.
Under the Opioid Initiative, Public Safety Canada (PS) developed and launched a Drug Stigma Awareness Training for law enforcement personnel in Canada. PS collaborated with CCSA to promote this training and raise awareness of the impacts of stigma among law enforcement.Footnote 64However, there is limited information on the impact of these activities on reducing stigma in law enforcement personnel. Public data are available only from 2021-22, where PS reported that 7.9% of Canadian frontline police service members have completed the Drug Stigma Awareness Training. This is significantly less than the completion target of 25%. PS asserts this is largely due to law enforcement being preoccupied with pandemic-related priorities.
Since 2018, PS has hosted the Law Enforcement Roundtable on Drugs involving Canadian and international public safety partners across the country and with invited international guests. At the 2018 Roundtable, attendees and panelists acknowledged the negative impacts of stigma in the medical and law enforcement communities.Footnote 65 Roundtables in subsequent years included discussions of the need for local law enforcement to build relationships with community partners to connect people to health and social services and to ultimately reduce overdose harms, which was seen as an improvement in law enforcement attitudes.Footnote 66,Footnote 67
Although PHAC did not receive funding under the Addressing Stigma theme of the Opioid Initiative, the Agency worked with Health Canada to develop anti-stigma tools and resources for health professionals.Footnote 68 In 2020, PHAC published "A Primer to Reduce Substance Use Stigma in the Canadian Health System" which outlined the impacts of substance use stigma on quality of clinical care and on patient wellbeing. The primer then provided resources to help health care professionals advocate for and adopt non-stigmatizing practices.Footnote 69
Finally, there are examples of recent efforts within federal departments to address stigma in government publications and policies. In 2018, as part of the Drug Stigma Awareness Training, PS established a national law enforcement working group to advise the department on the development and deployment of a national awareness strategy and to identify ways to support de-stigmatization approaches.Footnote 70 As previously noted, progress on this was impeded by law enforcement's focus on supporting government responses to the COVID-19 pandemic and, in some jurisdictions, natural disasters. Meanwhile, Health Canada has been updating their communications products to remove stigmatizing language. For example, while initial CDSS documents used terms such as 'problematic substance use' and 'illicit supply,' Health Canada staff now acknowledge these terms as stigmatizing and have removed and replaced the terms in newer publications and communications products relating to substance use.
Medium-term outcome 3: Increased uptake of community-based harm reduction programs and services across Canada.
Federal funding for community-based projects
Substance Use and Addictions Program
Much of the SUAP funding went to community and regional organizations running harm reduction-themed projects to address the opioid overdose crisis and other substance related harms. These projects have increased the availability of and access to important harm reduction services, including for those groups at greatest risk or who may face additional barriers to access.
Over half of all active SUAP projects focus on harm reduction. These include safer supply projects, drug checking services, overdose prevention and response training, distribution of naloxone kits, support for peer first responders and peer networks, and activities to reduce stigma in the health care system.Footnote 71,Footnote 72,Footnote 73,Footnote 74 Additionally, in fiscal year 2021-22, SUAP also funded a National Safer Supply Community of Practice, an initiative with the goal of facilitating "knowledge exchange, skill-sharing, and capacity building to scale up and support safer supply programs and prescribers across Canada."Footnote 75
Clients on the impact of Safer Supply
"Changed my life, otherwise I [would] still be in jail. Can access health system now. Have money to buy Xmas gifts. Health conditions improved. Gained weight, relationships are better. [Provider] saved my life."
"No [more] overdoses, I used to overdose almost every other day."
"…I feel I've genuinely found a way [to] actually be alive again…actually living and having a glimpse of a future. The money I save, the help I get, the fact that I've been able to stay clean from almost every other substance I used to struggle with… grateful I found [this program] when I did…"
Safer supply projects represent an important priority for SUAP, as the majority of CDSS-supported SUAP funding goes to these projects. As of April 2023, SUAP has supported 31 Safer Supply pilot projects across Canada, representing total funding of over $100.8 million since 2017. Currently, SUAP supports 29 Safer Supply pilot projects across Canada, representing a total funding commitment of over $96.4 million. According to the most recent internal program results report from 2021-22, 18 SUAP-funded Safer Supply projects serviced 2,540 clients and developed 938 knowledge and learning products. In 2022-23, SUAP funded an additional 11 new Safer Supply projects.
Evidence is being collected on the impact of SUAP projects in reducing harm. In 2019, CIHR directed CDSS funding to support 14 research teams through the "Evaluation of Interventions to Address the Opioid Crisis" funding opportunity. Their goal is to synthesize evidence of promising health interventions and practices to address the opioid crisis. Research related to the Harm Reduction Pillar focused primarily on the effectiveness of take-home naloxone programs. One research study identified "robust evidence that overdose education and naloxone distribution programs produce long-term knowledge improvement regarding opioid overdose, improve attitudes towards naloxone, provide sufficient training for participants to manage overdoses safely and effectively, and effectively reduce opioid-related mortality in community settings."Footnote 77 Two other studies confirmed the benefits of naloxone distribution programs to avert opioid overdose deaths, though one flagged challenges in accessibility for people in rural areas due to stigma, and the need for complementary services.
In 2020-21, Health Canada contracted a preliminary qualitative assessment of 10 SUAP-funded Safer Supply projects. This assessment found that program clients and staff reported improvements across a number of health and socioeconomic outcomes, such improved health, improved quality of life and stability, and accessing housing and employment.Footnote 78 Qualitative findings emphasized best practices like wraparound care, community and peer involvement, implementation of service processes, and ensuring inclusivity and accessibility. The main challenge appeared to be the limited effect of pharmaceutical alternatives to the highly potent fentanyl to which some participants have become tolerant. This means that the available dosages of safer alternatives may not be effective in managing withdrawal from fentanyl. Programs also cited logistical and capacity challenges due to the high demand for safer supply services relative to the limited availability of medications and staff.
Finally, in 2021, CIHR funded research grants for evaluations of the program implementation and short-term health impacts of SUAP-funded safer supply pilot projects, and 4 regional assessments of the public health impact of supervised consumption sites (SCSs) on clients and the public before, during, and after the COVID-19 pandemic.Footnote 79 The 2021-22 Supervised Consumption Sites (SCSs) Evaluation's End-of-Grant Virtual Workshop took place in October 2022. The 4 regional projects funded through this initiative evaluated several facets of the dual crises (COVID-19 and the national overdose crisis), including usage and uptake patterns, barriers to access, flexible formats, holistic and integrated care, advocacy, and resourcing. At the end-of-grant workshop, research findings were shared alongside the perspectives and expertise of knowledge users, which provided a comprehensive view of the topic and enhancing the potential impact of the findings. Knowledge shared through this event can be used to support evidence-based decisions to help ensure safe and consistent delivery of SCSs in both regular and adverse public health environments.
Harm Reduction Fund
PHAC has helped expand and increase uptake of services through its Harm Reduction Fund (HRF) G&Cs program. The HRF supports community-based efforts to reduce sexually transmitted and blood-borne infections (STBBI) like hepatitis C virus and human immunodeficiency virus (HIV) among people who use and share inhalation or injection equipment to use drugs.
As of 2019-20, HRF projects have provided harm reduction services to over 35,000 people. An initial assessment of the HRF found that 80% of targets set out in project objectives were being met, nearly met or had been exceeded.Footnote 80 These projects were reviewed by a diverse committee of PWLLE including representatives from LGBTQ2+ and Indigenous communities, health professionals, and peer educators.
Legislative and regulatory activities
From October 2017 to end of March 2022, there have been over 3.5 million visits to SCSs in Canada, with over 256,000 unique clients.Footnote 81 Most SCS clientele are male and a third are in the 30-39 age group. Surveillance data has found these are the demographics most likely to use opioids and experience opioid use harms.Footnote 82 Sites reported reversing over 39,000 overdoses and making over 117,000 referrals to health and social services, including mental health support, medical care, and housing. As a result, SCSs have reduced overdose harms and saved thousands of lives in Canada.
In 2017-18, following the launch of the CDSS, Health Canada streamlined applications for exemptions under the CDSA to allow SCSs to operate. These legislative changes have led to a significant increase in availability of SCS services, particularly for populations that need them most. Following this change, the number of SCSs in Canada increased from only 1 in late 2015 to 38 sites offering services as of April 2023. While only 56% of applications for an exemption to operate a SCS received a decision within service standards in 2017-18, this result increased to 91% for the following 2 years, surpassing targets.
Furthermore, SCSs have been established in areas where there are high rates of public drug use to provide important health, social, and treatment services. Health Canada has authorized the operation of various types of SCS to improve reach to different populations, such as stand-alone services, mobile units, and sites co-located in community health centres, inpatient or outpatient hospital settings, homeless shelters, and supportive housing settings.
In addition, in response to the rise in overdose harm and deaths in Canada at the outset of the COVID-19 pandemic, Health Canada issued 63 exemptions or exemption extensions under the CDSA.Footnote 83 These exemptions gave PTs greater flexibility in implementing harm reduction activities in response to urgent local needs, such as establishing an Urgent Public Health Need Site (also known as an overdose prevention site) more quickly and in temporary spaces, including shelters.Footnote 84 Furthermore, Health Canada helped ensure access to prescribed controlled substances during stay-at-home orders through an additional exemption under the CDSA that allowed health practitioners to verbally prescribe controlled substances and authorized pharmacists to prescribe, sell, and provide controlled substances in limited circumstances.Footnote 85
While many interviewees supported the increased uptake of harm reduction programming throughout Canada in the past few years, many suggested opportunities for improvement. Several interviewees, mostly CDSS federal partners, called for more evidence to be gathered for federally funded harm reduction interventions in order to better understand what works best and share best practices nationally. However, Health Canada and CIHR are already in the process of collecting and assessing information on the impact of these programs and services.
Specifically, CIHR's SCS Evaluation (2021-22) End-of-Grant Virtual Workshop took place on October 28, 2022. The 4 regional projects funded through this initiative evaluated several facets of the dual crises (COVID-19 and national overdose crisis), including usage and uptake patterns, barriers to access, flexible formats, holistic and integrated care, advocacy, and resourcing. In the end-of-grant workshop, research findings were shared alongside the perspectives and expertise of knowledge users, providing a comprehensive view of the topic and enhancing the potential impact of the findings.Footnote 86
Meanwhile, several internal and external interviewees criticized the piecemeal or incremental approach of pilot projects and felt they were insufficient to reduce harm. These interviewees wanted current interventions, including decriminalization, safer supply, and safe consumption sites, to go further or be expanded considering the urgency of the current opioid overdose crisis in Canada.
Medium-term outcome 4: Stigma is reduced and people who use drugs are increasingly accessing and are supported with appropriate health and social services.
National surveys have found that people in Canada continue to hold stigmatizing beliefs around substance use and substance use disorders (see Short-term Outcome 5). Research and survey evidence show that stigma in the Canadian health care system continues to affect access to services for people who use substances. This was also described by several interviewees, including members of organizations representing people with lived and living experience of substance use. These representatives called for more training for health care providers, including pharmacists, in addressing stigma in the health care system.
Despite increased awareness, support, and availability of harm reduction services over the past 5 years, there continue to be inequities in access to harm reduction services for people who use substances. For example, program documents and interviews highlighted how rural and remote communities have few or no services available. Meanwhile, although Health Canada has authorized different modes of consumption at SCSs, most sites are only equipped for injection drug delivery, which disproportionately excludes those racialized groups that are more likely to use non-injection methods.
Additionally, there are regional variations in availability of services despite existing need. For instance, in 2021 and 2022, Yukon reported the highest age-adjusted rate of opioid toxicity deaths of any Canadian province or territory and in 2020 and 2021, Manitoba reported age-adjusted rates comparable to those in Ontario. There are currently no safer supply projects active in Manitoba, nor in any of the Territories.Footnote 87
A 2021 PHAC survey of adults who used substances found that many respondents who use harm reduction and STBBI-related health services experienced barriers to access. Over half of respondents (58%) were not always able to access needle and syringe distribution programs or naloxone training (50%), and the majority (83%-84%) were not always able to access drop-in centres for people who use drugs or drug checking services.Footnote 88 Respondents cited the following challenges in receiving services:
- reduced hours of service or closures;
- difficulties in getting an appointment;
- difficulty accessing services due to public health measures; and
- concerns or fears around stigma, discrimination, and violence.Footnote 89
Enforcement
Key takeaways
Federal regulatory approaches have enhanced law enforcement's capacity to intercept and seize illegal substances. However, there were challenges with the increasing illegal importation of precursor chemicals used in illegal drug production and the ability to identify and intercept them. There were also issues with the ability to evaluate the broader impact of enforcement activities on the illegal market, as well as the federal government's capacity to conduct financial investigations to effectively target and seize the proceeds of drug crime. Finally, collaboration between law enforcement and public health has led to a wider recognition of the enabling role law enforcement plays in advancing public health outcomes for substance-related issues, which will continue to be enhanced by efforts to address discrimination.
Short-term outcome 6: Federal regulatory approaches ensure access to controlled substances for medical, research, and industrial purposes while effectively minimizing diversion of controlled drugs and precursor chemicals used to make illegal drugs.
Regulatory actions
In 2017, amendments to the CDSA were made to better equip both health and law enforcement officials to reduce the harms associated with drug and substance use in Canada. These included:
- prohibiting unregistered importation of designated devices that may be used in the illegal manufacture of controlled substances;
- amending the Customs Act to remove the exception that prevented border services officers (BSOs) from opening mail weighing 30 grams or less; and
- amending the CDSA to allow several measures, like allowing temporary scheduling of controlled substances and faster disposition of drugs and substances by law enforcement.Footnote 91
In 2021-22, CBSA seized 96% less fentanyl, in grams, when compared to 2017-18 (see Figure 10). While this appears to be a positive development, evidence shows that higher volumes of precursor chemicals are being seized, pointing to an upward shift in domestic production of illegal controlled substances. Specifically, in the first half of 2021, CBSA seized more than 5,000 kg of precursor chemicals, compared to only 512 kg in 2020. It should be noted that most of these chemicals are sourced from China and trafficked through the marine mode. These chemicals remain difficult to interdict because Canada's substance-by-substance scheduling method cannot keep pace with the advent of new molecular compounds. Interviews and other reporting indicate that these chemicals remain difficult to interdict because CBSA's front line detection capacity and Canada's scheduling method cannot keep pace with the emergence of new molecular compounds.Footnote 92

Figure 10 - Text description
Figure 10 is a line graph showing CBSA fentanyl seizures in grams from 2017-18 to 2021-22:
- 2017-18: 14,605 grams
- 2018-19: 5,166 grams
- 2019-20: 2,951 grams
- 2020-21: 7,399 grams
- 2021-22: 563 grams
Illegal importation of precursor chemicals
Most of the precursor chemicals being used in the illegal production of controlled substances, including fentanyl, are controlled under the CDSA. Health Canada, in collaboration with other federal partners, made additional regulatory changes in 2019 and 2022 to schedule novel precursors, thereby allowing law enforcement and BSOs to take action to halt their illegal importation, distribution, and use. Despite these regulatory changes, there has been an increase in illegal importation of precursors used domestically in the illegal production of controlled substances, as opposed to illegal importation of controlled substances.
While enforcement partners recognized efforts that had been made, concerns were expressed about the high threshold associated with accelerated scheduling and how precursors are being defined for the purpose of scheduling.Footnote 94 Even though Health Canada has accelerated some scheduling for fentanyl precursor analogues and derivatives, organized crime groups have been adaptive and will often find an alternative precursor chemical to use.
As previously noted, it is challenging for the regulatory regime to keep pace with the composition of chemicals that are used by organized crime. Given these challenges, enforcement partners identified a need to strengthen and review precursor regulations to make them nimbler and to make it more challenging for organized crime groups to import chemicals used to produce illegal substances.
Area of risk and need: Toxic illegal drug supply
According to several interviewees, particularly those external to the CDSS, one of the greatest risks for substance use in Canada is the high amount of harm and fatalities caused by a toxic illegal drug supply.
Evidence shows that the illegal drug supply has become even more toxic in recent years, furthering this risk. Interviewees described that more potent forms of synthetic opioids and unpredictable substances are now being mixed into the illegal drug supply, including benzodiazepines, methamphetamines, and other stimulants. This makes it more difficult to reverse overdoses as some of these substances do not respond to Naloxone. Additionally, a few interviewees and other evidence suggests that the toxicity of the illegal drug supply has worsened since the start of the pandemic due in part to disruptions of the supply chain and the growing production of illegal synthetic drugs.Footnote 95
Finally, interviews and documents show that the illegal drug market in Canada is shifting, adding another layer of complexity to supply reduction efforts. With the increase in fentanyl precursor chemicals being imported illegally into Canada, law enforcement suspect that fentanyl is increasingly being produced domestically using these chemicals, and that a surplus supply of finished fentanyl is being illegally exported to foreign markets. CBSA front line officers face challenges in their ability to effectively detect synthetic drugs at the border and to prevent precursor chemicals or synthetic drugs from being exported. A few internal interviewees described how other countries are beginning to see Canada as an exporter of illegal drugs. This concerning trend was also noted at the 2021 Law Enforcement Roundtable on Drugs.Footnote 96
Taking action at the border
As part of the federal government's efforts to address the overdose crisis, additional funding was allocated to CBSA as part of the Opioids Initiative. Key activities included:
- Training 6 additional detector dog teams with the fentanyl scent and deploying them to the highest risk ports of entry.
- Equipping 82 Designated Safe Examination Areas (DSEA) to allow officers to more safely conduct safe examinations of goods suspected of containing highly toxic substances, such as opioids, synthetic opioids, and other illicit drugs.
- Implementing 3 Designated Safe Sampling Areas (DSSAs) located at the highest risk ports for encountering opioids and synthetic opioids like fentanyl and fentanyl analogues. These are regional sites equipped with advanced detection equipment and staffed by chemists who perform real-time analysis and identification of suspected illegal chemicals and contraband drugs. In 2022-23, DSSAs analyzed approximately 8,400 exhibits.
The Pacific Region's DSSA is located at Vancouver Air Cargo. This is a regional hub where goods from other ports of entry in the region can be sampled, analyzed, and identified locally. This approach has demonstrated the most success in stopping precursor chemicals and synthetic drugs at the border. Since its launch in August 2021, the Vancouver Air Cargo DSSA has seen a 5-fold increase in analysis referrals, a 34% increase in the number of seizures, and has identified over 4500 kg of precursor chemicals. All regions with a DSSA have seen the benefits to localized field testing.
While there have been numerous actions taken to stem the flow of illegal drugs, there are still challenges at certain ports of entry as not all have the capability to analyze and identify goods. This means that goods requiring identification must be transferred to laboratory facilities in Ottawa, which in turn creates delays and reduces the feasibility of carrying out a controlled delivery. CBSA continues to explore additional technology and actions to overcome these challenges.
Drug Analysis Service and knowledge sharing
Health Canada provides support to public health and enforcement partners by providing drug sample analysis services to identify, measure and report on controlled drugs and substances under the CDSA, including confirming the identification and purity of substances tested in supervised consumption sites and at festivals. This service is separate from community-operated drug checking services funded through SUAP.
In the first 3 years of the Strategy's implementation, the percentage of samples analyzed within service standards has consistently met and exceeded the target of 95%. However, as a result of the COVID-19 pandemic, only 40% of samples were analyzed within the service standards in 2021-22. As noted in public reports and interviews, there has been a significant increase in demand for analysis with the emergence of new potent substances. This has also increased the level of complexity of the analyses conducted.Footnote 97
The Drug Analysis Service (DAS) also collects data and produces research evidence on drugs and emerging drug trends for members of the federal Health Portfolio and their partners. They issue notifications to clients and to provincial and territorial health authorities on newly identified potent illegal drugs in communities. While this activity is demand driven, the number of drug notifications issued has increased since the implementation of the CDSS (see Figure 11).
![Figure 11: Number of [DAS] notifications issued to clients and provincial and territorial health authorities on newly identified potent illegal drugs in communities](/content/dam/hc-sc/images/corporate/transparency/corporate-management-reporting/evaluation/canadian-drugs-substances-strategy/fig11-en.jpg)
Figure 11 - Text description
Figure 11 is line graph showing the number of Drug Analysis Service (DAS) notifications issued to clients and provincial and territorial health authorities on newly identified potent illegal drugs in communities by fiscal year between 2017-18 and 2021-22:
- 2017-18: 74 notifications
- 2018-19: 40 notifications
- 2019-20: 106 notifications
- 2020-21: 272 notifications
- 2021-22: 179 notifications
Short-term outcome 7: Increase collaboration between law enforcement and public health to recognize and address substance use as individuals interact with the criminal justice system.
Alternatives to criminal penalties for people who use substances
At PS's 2021 Law Enforcement Roundtable on Drugs, law enforcement, governmental agencies, and health care providers recognized the ways in which they work together to reduce overdose harms. Several panelists discussed the different ways they are trying to bridge the gap between law enforcement and health services, such as the development of specialized police units and training.Footnote 98
Some interviewees, mostly internal, shared general views about how law enforcement and criminal justice partners are taking more of a public health approach in their work, noting their unique position to assist individuals who engage in substance use. For example, new guidelines for federal prosecutors have been recently developed to focus efforts on the most serious cases raising public safety concerns, and to consider suitable alternatives to criminal charges for cases of personal possession. Additionally, positive views were shared about the Good Samaritan Drug Overdose Act, which provides an exemption from being charged for possession of controlled substances, and other charges, for people who call 911 for themselves or for someone else having an overdose, as well as the passage of Bill C5Footnote 99, which is expected to help address over-incarceration of marginalized Canadians and promote judicial discretion in sentencing. While these actions are not specifically funded under the CDSS, they support the Enforcement Pillar's objective to advance public health outcomes related to substance use issues. Positive views were also shared about improved access to substance use stigma training for law enforcement officers as well as efforts to exempt personal simple possession of certain illegal drugs from criminal penalties under the CDSA in British Columbia (BC).
Subsection 56(1) exemption in British Columbia (BC)
Panelists at the 2021 Law Enforcement Roundtable on Drugs outlined how decriminalization could help increase collaboration between law enforcement and health care providers to assist people who use substances in getting the support they need and to reduce the stigma associated with drug use.Footnote 100
Though the Subsection 56 (1) exemption related to personal possession in BC was viewed as a step forward, some interviewees noted potential challenges and a need for additional supports, evidence and guidance going forward. Specifically, a few interviewees noted that without a complement of other supports like effective treatment and recovery mechanisms, an exemption alone might not have the intended impact. A few other interviewees indicated a need for rapid impact evaluation of the exemption in BC to be able to inform implementation in other regions. Finally, interviewees noted that additional training and guidance for law enforcement officials, including frontline police, are needed to help connect individuals to appropriate pathways of care.
It should be noted that, as of September 2022, CIHR is funding a team of CRISM researchers over 5 years to undertake an independent and scientific evaluation of the impacts of the subsection 56(1) exemption in BC on people who use drugs, the general population, police services and the criminal justice system, as well as an evaluation of the economic consequences.
Short-term Outcome 8: Increase effectiveness of law enforcement efforts to address organized crime and target the proceeds of drug crime.
Collaboration among law enforcement
Many of the federal enforcement partners indicated positive collaboration and engagement between each other, with provincial and municipal law enforcement, and with international counterparts, in their efforts to address organized crime. For example, some of the interviewees noted the positive impacts of the Canadian Integrated Response to Organized Crime, which is a coordinated national response for disrupting transnational organized crime groups and drug networks, as well through the North American Drug Dialogue, which is the primary mechanism that Canada, Mexico, and the US use to address current and emerging drug threats facing North America, such as through improved information sharing on trends in trafficking of illegal drugs.
High-value seizures of illegal drugs
Enforcement partners have reported many successful investigations and seizures. Between 2017-18 and 2021-22, CBSA seized over 155 million grams of illegal drugs, including over 6.5 million grams of opioids.Footnote 101 Every fiscal year between 2017-18 and 2021-22, CBSA met or exceeded its CDSS performance indicator target for drug seizures through intelligence investigations. Each year, the average dollar value of drugs and precursors that CBSA seized through intelligence-led investigations was 16 to 70 times greater than the average dollar value of drugs seized without an intelligence investigation like a routine check at the border.
As part of the Enforcement pillar, the RCMP has committed to focusing its efforts on investigating the highest threats related to organized crime networks, including those involved in the illegal importation and trafficking of drugs. Performance data showed that the number of drug seizure-related occurrences remained stable over time, with a total of 105,565 occurrences in the last 4 years. In June 2022, the RCMP seized enough precursor chemicals to produce 320 kilograms of fentanyl. As stated by RCMP officials, "the recovery of these precursors represents a significant disruption to the illegal synthetic drug market."Footnote 102
Furthermore, between 2019 and 2022, the RCMP laid 38,293 drug charges for possession, trafficking, production, and import or export of illegal substances. The number of reported drug-related charges significantly decreased (32%) from 2020-21 to 2021-22, which is largely due to a reduction in the number of possession-related (-44.3%) and cannabis-related (-18.8%) drug charges from the previous fiscal year. Although the RCMP provided performance results from 2019 to 2022, the evaluation was unable to assess the number and percentage of RCMP investigations with a transnational nexus due to a change in the methodology in 2021-22. GAC also supported seizures of illegal drugs smuggled via legal maritime containers in selected countries in the Americas and met their target of supporting seizures of over 20 tons in all beneficiary countries over the evaluation period.
With the increasing number of seizures, law enforcement partners have made significant strides in drug-related investigations and seizures. While these activities supported collaborative efforts to address organized crime, interviews and public reporting noted challenges related to the use of technology like encryption by organized crimes groups (OCGs), the technological responses by police to counteract these activities, and police access to data stored or located outside of Canada.Footnote 103 Moreover, interviews and documents have identified a gap in addressing the online sales of illegal drugs. Drug traffickers exploit the anonymity of the surface and dark web to complete sales by mail or courier delivery, especially as offline interdiction efforts push traffickers into other, under-policed areas. Currently, no federal partner has taken the lead in assessing the extent of this threats, nor in coordinating a federal response to this issue.Footnote 104
As shown in Figure 12, necessary spending exceeded budgeted amounts, particularly at PPSC. This variance was attributed to the growing complexities of the public prosecution files due to increasing criminal sophistication and the scale of criminal activities. Additionally, law enforcement agencies across the country have received increased funding for initiatives directly and indirectly linked to drug trafficking which also contributed to a rise in more complex cases.
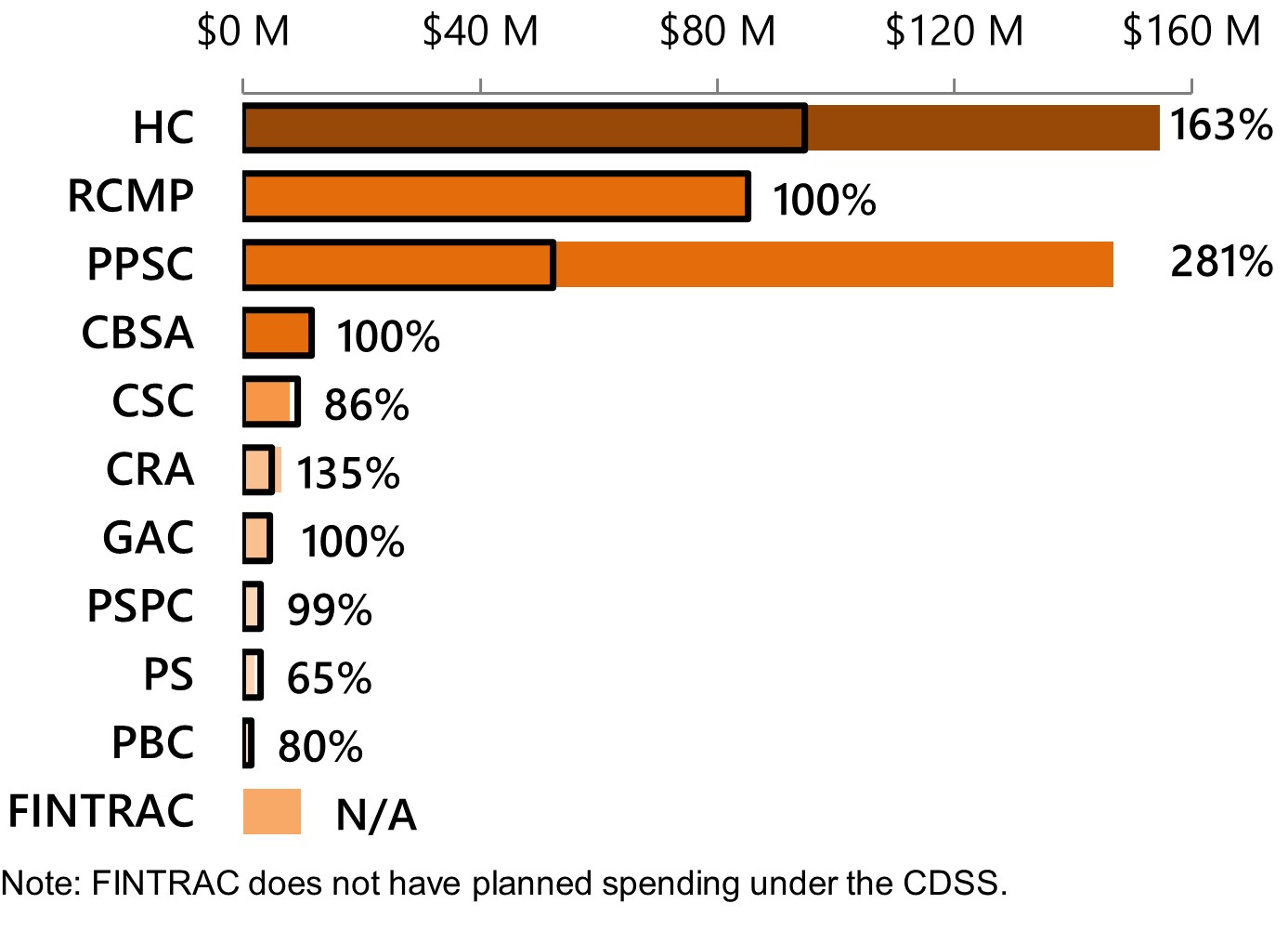
Note: FINTRAC does not have planned spending under the CDSS.
Figure 12 - Text description
Figure 12 is a horizontal bar chart showing the CDSS total actual spending as a percentage of planned spending between 2017-18 and 2021-22 for the Enforcement pillar. Each bar represents a partner under the Enforcement pillar. They are listed as follows from top to bottom:
HC
- Planned: $94,799,995
- Actual: $154,605,110
- Budget spent: 163%
RCMP
- Planned: $85,101,491
- Actual: $85,101,491
- Budget spent: 100%
PPSC
- Planned: $53,755,195
- Actual: $150,459,694
- Budget spent: 281%
CBSA
- Planned: $12,800,000
- Actual: $12,800,000
- Budget spent: 100%
CSC
- Planned: $9,258,483
- Actual: $7,956,095
- Budget spent: 86%
CRA
- Planned: $4,881,541
- Actual: $6,570,260
- Budget spent: 135%
GAC
- Planned: $4,500,000
- Actual: $4,500,000
- Budget spent: 100%
PSPC
- Planned: $3,000,000
- Actual: $2,980,930
- Budget spent: 99%
PS
- Planned: $2,942,660
- Actual: $1,910,096
- Budget spent: 65%
FINTRAC
- Planned: N/A
- Actual: $9,696,076
- Budget spent: Not applicable as they did not have planned spending under the CDSS
Forensic accounting
Enforcement partners rely on forensic accounting advice and expertise from PSPC to support investigations. However, demand for these services goes beyond current resources, as these activities are cost-recovered and require a fee. As indicated by federal partners, there have been several instances where law enforcement agencies did not have the funding for forensic accounting analyses.Footnote 105 In such cases, they would often forego a full forensic accounting analysis, such as a Net Worth Analysis, and opt instead for reduced services (or none at all) to lower the fees or to refer the case to the civil forfeiture process. Budget restrictions have limited the PSPC's ability to provide services to identify and seize assets derived from criminal activity and remove the financial incentives of crime.
Given these challenges, a few federal enforcement partners highlighted the need to direct more resources and capacity towards forensic accounting and money laundering investigations as this would better enable law enforcement to target larger illegal drug operations and organized crime networks, leading to a more significant forfeiture of criminal proceeds.
Medium-term Outcome 5: Decreased diversion of drugs and reduced size and profitability of the illegal drug market.
Compliance and enforcement (C&E)
Health Canada contributes to decreasing the diversion of drugs by monitoring the drug supply chain, including licensed dealers and pharmacies, to ensure that controlled substances and precursor chemicals are handled appropriately and remain within legal distribution channels. For example, in 2018-19, Health Canada helped identify a pharmacy in Hamilton, Ontario that was involved in diverting more than 400,000 doses of pharmaceutical narcotics to the illegal market. The RCMP subsequently laid 15 criminal charges.Footnote 106
C&E of licensed dealers and pharmacies
Authorized activities in the drug supply chain are monitored through reports received from licensed dealers and pharmacies. For licensed dealers, this includes reports of monthly and annual activities, loss or theft, and suspicious transactions. For pharmacists, this includes loss or theft reports. The compliance history of both licensed dealers and pharmacies through inspections and other compliance activities is also monitored. Compliance and enforcement activities are guided by Compliance and Enforcement Policy for Controlled Substances and Precursors (CS-POL-001).Footnote 107
Highlights of their activities included having inspection and compliance rates within target, initiating compliance promotion activities for pharmacies, improving their risk-based approach, as well as positive collaboration with provincial law enforcement. Other highlights included a partnership with the RCMP's National Chemical Precursor Diversion Program to conduct outreach and education to minimize the diversion risk of chemicals and precursor chemicals, as well as support for harm reduction activities like ensuring that the appropriate controls are in place for safer supply pharmacies.
In terms of C&E for pharmacies, a few interviewees noted that Health Canada is limited in their ability to impose corrective measures. As a result, if concerns are raised through C&E activities, Health Canada must refer to their provincial regulatory colleagues for follow up. While this is a limitation, interviewees noted that the Colleges of Pharmacy have been very open and communicative in working with Health Canada in this area and that improvements are forthcoming as a result, though they did not elaborate on what those improvements would be.
In addition to this, RCMP has developed educational material for Canada's chemical industry to raise awareness of the indicators of suspicious chemical transactions that might indicate precursor chemical diversion for illegal drug manufacturing.
Consistent with international initiatives, internal interviewees spoke on how Health Canada's pharmacovigilance activities have standardized and strengthened pre- and post-market safety oversight for marketed opioid products across their lifecycle, including controlled distribution programs to reduce the risk of diversion.
Finally, authorization to perform legitimate activities with controlled substances and precursor chemicals have consistently been processed within a timely manner throughout the evaluation period. Over 90% of authorizations were processed within the service standards, thus consistently exceeding their performance target each year since the indicator was added in 2019-20. However, concerns from law and border enforcement have also been expressed about the framework in place for suspicious precursor chemical transactions. The fact that licensed dealers are under no obligation to report on these transactions was the main challenge noted, as it usually means that very little information is passed along to enforcement agencies.
Overall impacts of the Strategy
Key takeaways
The CDSS has made significant progress in framing substance use as a social and public health issue in Canada, however, the rates of substance use and related harm continue to rise. While there have been some efforts to target youth and other at-risk populations, more work is needed to target the root causes of substance use and implement early prevention efforts for populations at highest risk, or who face barriers to care. Moreover, the CDSS and Opioid Initiative have made significant strides in enhancing the evidence-base around substance use; however, gaps still remain.
Long-term outcome 1: Substance use is addressed as a health and social issue by governments, communities, stakeholders and Canadian society.
Based on evidence across all pillars and themes, substance use is being addressed increasingly as a health and social issue by governments and Canadian society.
At the federal level, the CDSS and the Opioid Initiative serve as 2 key multi-departmental initiatives that promote a public health approach to substance use. External interviewees pointed to the re-introduction of the harm reduction pillar in the CDSS as a key example of the shift away from a law enforcement approach to a public health approach. These initiatives have expanded access to harm reduction services at the community level, launched national public education on opioid use and the negative impacts of substance use stigma, and fostered collaborations between public health and law enforcement. Interviewees have suggested that Canada's public health-oriented drug and substance use policy has made it an international leader in this domain.
Since 2018, Canada has been advancing public health focused issues, including stigma, at the UN Commission on Narcotic Drugs (CND).Footnote 108,Footnote 109 On an international front, Health Canada and the United Nations Office on Drugs and Crime co-hosted an international technical consultation on stigma in January 2020 to discuss how stigma affects people who use drugs and the interventions currently in place. They also continued to promote the use of non-stigmatizing approaches during discussions and negotiations with other countries at the CND March 2020 Session.Footnote 110 In April 2021, Canada continued to advance and promote Canadian drug policy priorities at the international level by tabling a resolution, adopted by the 64th session of the CND entitled "Facilitating access to comprehensive, scientific evidence-based drug demand reduction services and related measures, including for people impacted by social marginalization".Footnote 111,Footnote 112
Among the numerous interviewees that pointed to opportunities to improve the federal government's activities to address substance use as a health and social issue, the most common was based on exploring opportunities for intersectoral collaboration, namely in mental health and housing.
PT governments are starting to enhance access to harm reduction services, a key component of a public health approach to substance use. However, these services are being implemented inconsistently, which some interviewees suggest is due to differences in capacity, funding, priorities, and views on ways to address substances use harms.
There is also evidence that people living in Canada and the law enforcement community view substance use as a health issue, although stigma against people using drugs persists. Public opinion research has shown that over two-thirds of people in Canada agree the opioid overdose crisis is a public health issue and that it is as serious as the COVID-19 pandemic.Footnote 113 Additionally, interviewees highlighted the BC exemption that was granted so that adults in BC can possess small amounts of certain illegal substances for personal use as a clear sign of greater acceptance of substance use as a health issue among the public.
Long-term outcome 2: Rates of substance related harms in Canada are minimized, especially for youth and those most at risk of harm, including preventing, reducing or delaying the use of drugs and other substances.
Rates and harms of substance use continue to rise in Canada. While the number of lives lost to opioid toxicity showed some decline between 2018 and 2019, opioid-related harms increased significantly when the COVID-19 pandemic began in March 2020, and deaths from opioid toxicity reached record levels in 2020 and 2021.Footnote 114 Since then, opioid-related deaths have remained higher than pre-pandemic levels. Harms from substance use in Canada also rose for other substances, including alcohol and stimulants, particularly during the pandemic. Footnote 115
In 2019, among Canadians aged 15 and older, 76% reported consuming alcohol, 14% reported having used opioid pain relievers, and 3% reported having used at least 1 of 6 illegal drugs (cocaine/crack, speed/methamphetamine, ecstasy, hallucinogens, heroin, salvia). Past year alcohol and illegal drug use was unchanged from 2017, whereas use of opioid pain relievers had increased by 2% since 2017.Footnote 116
Past year use of alcohol among post-secondary students aged 17-25 in 2019-20 was higher (84%) than among the general Canadian population (76% in 2019). Furthermore, 23% of post-secondary students reported having used pain relievers in a way other than prescribed, including using a greater quantity, using more frequently, using to get high, and 14% reported having used at least 1 of 6 illegal drugs (cocaine/crack, amphetamines, methamphetamine, ecstasy, hallucinogens, heroin) in the past year.Footnote 117
Among youth (secondary school students in grades 7 to 12) in 2021-22, 39% reported having consumed alcohol in the past year, relatively unchanged from 44% in 2018-19 (see Figure 13). Past year use of psychoactive pharmaceuticals to get high, including, opioid pain relievers, stimulants and sedatives / tranquilizers, by secondary school students was 7% in 2021-22Footnote 118

Source: Health Infobase, Public Health Agency of Canada
Figure 13 - Text description
Figure 13 is vertical side-by-side bar chart showing the past twelve-month use of alcohol among secondary students, grouped by grades and year. The left bar represents use in 2018-19 whereas the right bar shows use in 2021-22. The three bar groupings represent secondary schools grades as follows:
Grades 7-9
- 2018-19: 24.9%
- 2021-22: 22.7%
Grades 10-12
- 2018-19: 63.5%
- 2021-22: 55.7%
Total
- 2018-19: 44.1%
- 2021-22: 39.0%
Interviewees also observed that the pandemic had increased alcohol use-related harms. PHAC's 2021 survey found that 89% of respondents used alcohol, 57% of whom increased their use of alcohol during the pandemic.Footnote 119 Surveillance data showed that hospitalizations due to alcohol use increased by 5% in 2020 compared to 2019. Footnote 120
According to a 2021 survey conducted by PHAC on the impact of COVID-19 on access to STBBI-related health services among adults living in Canada who reported substance use, many increased their use during the pandemic. For example, 13% of respondents reported using opioids, of whom 57% increased their use of opioids. Around half of respondents who used cocaine, crack or stimulants like methamphetamines also reported increased use of those substances. Footnote 121
While there have been some efforts to target youth and other at-risk populations through community-led projects, evidence suggests more work is needed to target the root causes of substance use and early prevention efforts to populations at highest risk or who face barriers to care and to better integrate services across a continuum of care that comprises prevention, harm reduction, treatment, and recovery, and with other social supports, such as housing, food security, mental health. Surveillance data shows that opioid-related deaths disproportionately affect men and adults aged 20 to 59 years old (see Figure 14). Surveillance data also shows that life expectancy at birth in Canada started stalling in 2010, driven in part by the rise of the overdose crisis.Footnote 122

Source: Health Infobase, Public Health Agency of Canada
Figure 14 - Text description
Figure 14 is vertical side-by-side bar chart showing the number of accidental apparent opioid toxicity deaths by sex and age group in Canada from January to June 2022. The dark purple bar represents female use while the light purple bar represents male use. The six bar groupings represent age groups as follows:
0 to 19 years
- Female (left bar): 16
- Male (right bar): 23
20 to 29 years
- Female (left bar): 109
- Male (right bar): 257
30 to 39 years
- Female (left bar): 152
- Male (right bar): 532
40 to 49 years
- Female (left bar): 136
- Male (right bar): 481
50 to 59 years
- Female (left bar): 118
- Male (right bar): 368
60 years or more
- Female (left bar): 44
- Male (right bar): 165
Since the start of the COVID-19 pandemic, Canada has seen unfortunate record levels of hospitalizations and deaths due to opioid overdoses (see Figure 15). At the pre-pandemic height of the opioid overdose crisis in 2018, an average of 12 people in Canada lost their lives to opioid-related overdose each day. In 2021, this increased to an average of 22 people per dayFootnote 124
Experts say the pandemic contributed to the increase in fatalities in several ways, including increased substance use to cope with stress and anxiety in addition to decreased accessibility of health services and supports.Footnote 125 Also, law enforcement and frontline staff in community organizations observed more people using drugs in isolation during the pandemic due to decreased availability of supportive housing and shelter beds, as well as increased use of single rooms for quarantining. As a result, people were consuming substances alone, with no one around to reverse potential overdoses with naloxone or to call for help. Finally, the pandemic may have worsened the toxicity of the illegal drug supply. Disrupted supply chains during this time led to greater contamination of the illegal drug supply with more potent opioids like fentanyl and carfentanil, and with non-opioid sedatives like benzodiazepines.Footnote 126 Contaminated drugs do not respond as well to naloxone, which means overdoses are more difficult to reverse, leading to a higher likelihood of fatalities.Footnote 127

Figure 15 - Text description
Figure 15 shows a line graph of number of opioid overdose deaths in Canada by quarter between 2016 and the first quarter of 2022 overlayed with a timeline of key events since the launch of the CDSS.
Line Graph:
- 2016
- First quarter: 668
- Second quarter: 637
- Third Quarter: 654
- Fourth Quarter: 860
- 2017
- First quarter: 920
- Second quarter: 1021
- Third Quarter: 1055
- Fourth Quarter: 921
- 2018
- First quarter: 998
- Second quarter: 969
- Third Quarter: 1099
- Fourth Quarter: 1103
- 2019
- First quarter: 1042
- Second quarter: 1051
- Third Quarter: 741
- Fourth Quarter: 860
- 2020
- First quarter: 1041
- Second quarter: 1694
- Third Quarter: 1789
- Fourth Quarter: 1874
- 2021
- First quarter: 1914
- Second quarter: 1898
- Third Quarter: 1959
- Fourth Quarter: 2127
- 2022:
- First quarter: 1879
Key events:
- December 2016 – Launch of the CDSS
- The Government of Canada introduces a new national drug strategy that highlights harm reduction-focused policies and a strong evidence base.
- February 2018 – Launch of the OpioidInitiative
- The Government of Canada allocates additional resources through Budget 2018 to addressing the opioids crisis in Canada.
- March 2020 – COVID-19 Pandemic
- The World Health Organization declares COVID-19 a pandemic.
Long-term outcome 3: Canadians and their communities are supported with evidence-based tools, programs, and services to be safer, healthier, and more resilient.
As demonstrated throughout the Pillar sections, the federal government has made significant progress in supporting the development of a wide range of evidence-based tools. Both internal and external interviewees highlighted progress on enhancing the evidence base since the implementation of the CDSS, with some highlighting that it has been a key priority of the Strategy.
Many interviewees noted that evidence and resources supported by the CDSS have been useful, with some specifically highlighting evidence generated by CRISM, like the iOAT Guidelines, and SUAP funded activities.
Still, many identified evidence gaps across all 4 pillars, especially with respect to prevention. For example, some internal interviewees noted gaps in knowing what has been prevented and in measuring the effectiveness of risk minimization efforts. While this ties into overall performance measurement challenges, it also speaks to the need identified by many interviewees, both internal and external, to continuously monitor and evaluate impacts of piloted approaches to see if they are improving health outcomes.
A few internal interviewees spoke about how they have started to evaluate pilot harm reduction services and are working towards building an evidence base on these. For instance, CIHR has funded CRISM to undertake arms length evaluations of SCS and safer supply pilot projects as they are implemented. The goal is to develop evidence and best practices on harm reduction interventions for decision makers and overall knowledge, while taking into consideration the impact of the COVID-19 pandemic and local contexts.
Knowledge mobilization
A few internal interviewees spoke about knowledge mobilization efforts, most of whom highlighted CIHR's "End of Grant" workshops, where researchers meet with policymakers, health care providers and persons with lived and living experience to expand the results of their research. End of Grant Workshop Synthesis reports are published on the CIHR websiteFootnote 128. Still, some interviewees identified a need for more knowledge exchange and mobilization, particularly at the community level and among SUAP-funded projects.
Surveillance data and monitoring
Surveillance data and monitoring have improved since the implementation of the CDSS. As the opioid overdose crisis has persisted, the federal government has invested in enhancing data collection and surveillance of opioid-related deaths and harm. Interviews indicate a collaborative relationship to share information between Health Canada, PHAC, Statistics Canada, and PT coroners and medical examiners. This collaboration goes beyond the CDSS although substance-related toxicity is a key priority for all involved. While stakeholders expressed appreciation for the resulting reports and evidence-based resources, there are still challenges with the evidence base around substance use in Canada, including the following:
- Gaps in disaggregated surveillance data and harms on substance use to understand how sub-populations may be affected inequitably;
- Lack of data to monitor and assess treatment and recovery services nationally, namely the types and availability of services;
- Lack of evaluations of various federally funded projects to identify which interventions to scale up or scale back, although some assessments have begun recently for safer supply projects across Canada; Footnote 129,Footnote 130 and
- Need for more evidence to better understand the pathways and root causes of substance use and how to address them.
Since the implementation of the CDSS, Health Canada has conducted multiple general population surveys, including the Canadian Alcohol and Drugs Survey, the Canadian Student Tobacco Alcohol and Drugs Survey, and the Canadian Postsecondary Education Alcohol and Drug Use Survey (CPADS), which are critical for understanding substance use trends and impacts of interventions over time.
Furthermore, Health Canada conducts targeted surveys and research to fill recognized gaps in general population surveys. Examples of such targeted surveillance include the following:
- Surveys of PWLLE to obtain information on high-risk populations typically unaccounted for in policy and program development;
- Online surveys to document the demand for and use of new psychoactive substances, monthly data collection from supervised consumption sites on site performance, such as number of visits and clients; and
- Service provision, including number of referrals to health and social services, and potential drug toxicity issues, such as drugs being used and overdoses prevented.
Health Canada, in joint effort with federal partners, is leading the development of a Data and Evidence Framework in order to better coordinate and collaborate with partners to develop indicators and collect, analyze, and disseminate timely and meaningful data and information on the use and impacts of drugs and substances in Canada, including understandings of the illegal drug market. This framework will support the government's tracking and monitoring of the overdose crisis and broader substance use trends.
Table 5: Federal data sources for substance use and harms
Opioid- and Stimulant-Related Harms Surveillance
PHAC publishes quarterly data Footnote 131 on the public health impact of opioid- and stimulant-related harms in Canada. The surveillance system includes data on apparent opioid and stimulant toxicity deaths provided by PT Chief Coroners and Chief Medical Examiners, opioid- and stimulant-related poisoning hospitalizations from the Canadian Institute for Health Information (CIHI), and suspected opioid-related overdoses provided by PT Emergency Medical Services.
Canadian Alcohol and Drugs Survey (CADS)
Health Canada conducts the CADS, a biennial general population survey of alcohol and drug use among Canadians aged 15 years and older. Footnote 132
Canadian Student Tobacco, Alcohol and Drugs Survey (CSTADS)
Health Canada conducts the CSTADS, a survey of student tobacco, alcohol and drug use among youth in grades 7 to 12 (secondary I through V in Quebec). Footnote 133
Canadian Postsecondary Education Alcohol and Drug use Survey (CPADS)
Health Canada conducts the CPADS, a survey on the prevalence and patterns of substance use and associated harms among postsecondary (college and university) students aged 17 – 25 across Canada.
Drug Analysis Service (DAS) Reports
The DAS shares annual statistics and trends based on the samples of illegal drugs submitted by Canadian law enforcement agencies to Health Canada for analysis. Footnote 134
Canadian Hospitals Injury Reporting and Prevention Program (CHIRPP)
The CHIRPP is a PHAC injury and poisoning surveillance system that collects and analyzes data on injuries to people who are seen at participating emergency rooms in Canada. Footnote 135
Statistics Canada (StatsCan) Data and Research
StatsCan collects and publishes administrative and population survey data and research related to substance use and harms. Footnote 136
Canadian Institute for Health Information (CIHI) Data
CIHI collects pan-Canadian health system data and reports on various indicators related to substance use. Footnote 137
In addition, Health Canada collaborated with Statistics Canada to conduct wastewater analysis through the Canadian Wastewater Survey to detect and track the presence of drug metabolites in samples collected from municipal wastewater treatment plants in Canada.Footnote 138,Footnote 139
Statistics Canada is also working to develop a disaggregated data action plan to address data gaps in surveillance. The department now publishes health statistics that include data on substance consumption broken down by racialized groups, distinct Indigenous groups, and income. While the data action plan extends beyond the CDSS and the Opioid Initiative, interviews suggest that this plan could have a direct benefit for the Strategy.
The Centre for Surveillance and Applied Research (CSAR) at PHAC has also been working with the provinces and territories to conduct a national chart review study (CRS) to better understand the characteristics of individuals who have died from drug- and alcohol-related acute toxicities between 2016 and 2017, including the substances involved and the circumstances surrounding the death. This first-of-its-kind study in Canada provides an important baseline to assess changes in the overdose crisis over time.
Finally, CSAR produces a simulation model of opioid-related deaths in Canada to help inform policy and program decisions. CSAR activities on opioids and stimulant-related harms also supported the release of 5 joint statements from the co-chairs of the Special Advisory Committee on the Opioid Overdoses Crisis.
Performance measurement
This evaluation faced challenges in analyzing program performance measurement data. Over the period assessed for the evaluation, performance data were not available or could not be assessed for a quarter of the expected results under the CDSS and a third of the expected results under the Opioid Initiative due to poor data quality. For example, in the case of several indicators under both initiatives, the metrics used to report the result did not align with the definition of the indicator or the metric used for the target. CDSS federal partners interviewed mentioned how performance measurement indicators were not useful for assessing or capturing impact of federal efforts. Specifically, partners described how current indicators quantify short-term outputs rather than assessing whether federal efforts are improving health outcomes.
Additionally, evidence suggests some of the performance indicators selected for the CDSS may not be an appropriate measure to represent the breadth or nature of activities delivered under the Strategy. For example, outcomes for the CDSS are difficult to measure and performance data does not always provide an understanding of the effectiveness of certain activities and interventions. Interviews supported this, with many federal partners speaking to gaps in performance-related data, including need for disaggregated data on people affected by federal efforts and some CDSS-related activities lacking indicators in the CDSS performance measurement strategy.
Finally, there did not appear to be a strong shared understanding among partners on the Strategy's expected outcomes and achievements. There was also a lack of clarity in how activities described under the CDSS have contributed to the Strategy's long-term outcomes. For instance, partners often had difficulty describing how their work related to that of other partners and were often unable to comment on the overall progress of the CDSS. Similarly, partners reported on performance measurement indicators that often could not be linked to expected outcomes of the Strategy. However, it should be noted that there are ongoing efforts in place to review and improve performance measurement for the CDSS.
Governance and engagement
Key takeaways
Most funded partners provided mixed views on governance, noting that there was positive collaboration within the governance structure, but also challenges. Areas for improvement included clarifying the program mandate and roles and responsibilities for each partner, increasing engagement and discussion opportunities for other federal partners and stakeholders to ensure all views are included, and providing meeting materials earlier to allow other government departments to meet their internal briefing needs. In terms of external engagement, all feedback about interactions with Health Canada has been positive; however, it was noted that there should be opportunities to engage with a broader range of individuals.
Governance of the CDSS
The CDSS governance structure was created in 2017 with a secretariat to support and coordinate information sharing, work planning, and facilitating connections between departments and committees. All relevant departments, including unfunded partners, were included in the various committees governing the CDSS. Since 2018, progress has been made to make the governance structure more efficient. For example, while the initial structure was led by the Assistant Deputy Minister (ADM) Executive Committee, this committee was put on hold since members were already involved in another complementary committee that has been renamed the Federal Inter-Departmental ADM Working Group on the Opioid Overdose Crisis and the CDSS (see Annex E for a description of the governance structure).
Many interviewees and survey participants indicated that the governance structure works well, and that collaboration and relationships are good between horizontal partners. There were some interviewees who indicated that Health Canada lacks a streamlined governance structure, especially for drug policy, both internally and with CDSS partners. Some suggested implementing a more coordinated structure with enhanced policy leadership to help minimize duplication and increase consistency. There was an indication that some reorganization may be underway within the governance structure to improve coordination. Still, interviewees from both Health Canada and partner departments indicated a need to clarify the CDSS mandate, its affiliated committees and working groups, and the roles and responsibilities of all involved.
In a survey of governance committee members (CDSS Director General Standing Committee and CDSS Working Group), most participants reported that roles and responsibilities of committee members were not clear or only moderately clear. Interviewees from both Health Canada and other departments also reported a lack of awareness about roles, and they were not aware of what the governance structure was. There was confusion over the way committees were connected to the CDSS. This was especially true of the federal/provincial/territorial (FPT) committees and associated working groups. Others noted that they had been part of committees but did not know if they were still meeting or had been dissolved. A review of the governance structure revealed other changes to the intended structure, including several planned working groups not coming to fruition.
Additionally, committee meetings are viewed by partners and stakeholders as mostly transactional opportunities for Health Canada to present information, which is helpful, but does not allow time for deep discussions about priorities or possible alternative approaches. Meanwhile, external interviewees, including PTs and People with Lived and Living Experience (PWLLE), would like more opportunities for discussion and engagement, and including PWLLE in policymaking.
External engagement
The CDSS has made several efforts to engage stakeholders outside of the program including setting up the PWLLE Council; the Canadian Pain Task ForceFootnote 140, the Expert Task Force on Substance UseFootnote 141, and the Expert Advisory Group on Safer Supply Footnote 142, established in 2020. Consultations also took place in 2018 to gather information to contribute to the potential next steps for the CDSS.
Funding recipients have been quick to indicate that the support they receive from Health Canada is excellent and responsive, with several noting their respective contacts' attention to their questions. At the same time, funding recipients report they do not have many learning opportunities and would benefit from more formal opportunities or a platform to allow community organizations to collaborate with each other.
There are also opportunities to engage further with PWLLE. Some interviewees highlighted the need to broaden the voices of PWLLE in engagement efforts to bring in more voices from individuals in recovery. Opportunities for improvement raised by interviewees included more meaningful engagement with PWLLE, which is defined as timely engagement with a purpose, following the concept of "Nothing about us without us". This includes seeking out a broader range of individuals who use substances, such as people currently using substances including those who do not want to stop, people in recovery, and people who previously used substances, while also considering the impact of ongoing engagement on current contacts, including too much consultation. Opportunities to engage further with Indigenous communities was also noted by some interviewees who identified this as lacking.
Interviewees suggested expanding engagement with substance use prevention and treatment subject matter experts, possibly through a stakeholder advisory committee, encouraging more contact and open dialogue across jurisdictions, as well as highlighting successes and best practices to support work at other levels, and more time to ask questions during meetings.
Conclusions and recommendations
Conclusions
Despite notable efforts and progress on delivering key activities that support CDSS and Opioid Initiative objectives, substance related harms and deaths continue to rise. Recognizing that the COVID-19 pandemic had an unprecedented impact on substance use trends during the evaluation period, the CDSS quickly adapted its interventions to address the rise in overdoses, specifically using the Subsection 56 (1) class exemption for patients, practitioners, and pharmacists prescribing and providing controlled substances in Canada in limited circumstances. However, given the urgency of the overdose crisis, prevention activities and collaboration to address the root causes of substance use were limited.
Moreover, much of the Strategy's focus has consequently been on illegal drugs. While the overdose crisis should continue to be a priority, evidence strongly suggests that other substances could be better addressed under the CDSS, and in accordance with their long-term health and socio-economic impacts.
Prevention
The evaluation found that limited prevention activities were undertaken over the last 5 years and that more upstream prevention is needed to have a greater impact on changing substance use behaviours among Canadians. There was also limited evidence on collaboration to better address the root causes of substance use. While there have been national public advertising campaigns, educational engagements and community-led projects funded by the SUAP, there is more work needed in terms of generating and assessing behavioural changes among Canadians to prevent harm related to substance use.
Treatment
Recognizing that PTs are primarily responsible for the delivery of treatment services, federal actions have supported improving access to evidence-based treatment services and systems through initiatives such as the ETF, SUAP, DTCs, as well as ISC's Mental Wellness Program, treatment centre accreditation, and certification incentive funding for substance use workers. However, barriers to access remain, in particular for marginalized groups. Significant progress has also been made on enhancing the evidence base for treatment. Highlights include the development of treatment guidelines for opioid use disorders, guidance documents in response to the COVID-19 pandemic, and studies on treatment effectiveness for OAT.
Harm reduction
Federal actions have also helped to expand the availability of harm reduction services, including SCSs and safer supply projects, though barriers to access remain. Stigmatization of people who use substances continues to be among the most important barriers for people to seek help. The evaluation found that federal campaigns and resources to address stigma have reached Canadians, health care professionals and law enforcement, and that awareness of substance use stigma is generally high. Nonetheless, stigmatizing attitudes persist.
Enforcement
The CDSS and Opioid Initiative have supported ongoing efforts to decrease diversion of drugs through regulatory actions, like the accelerated scheduling of novel precursor chemicals, compliance promotion, and C&E of licensed dealers and pharmacies. Still, challenges persist with the increasing illegal importation of precursor chemicals at the borders and the regulatory regime's capacity to keep pace with the composition of chemicals that are used by organized crime groups. Many of the federal enforcement partners indicated positive collaboration with partners in their efforts to address organized crime, though capacity challenges have limited efforts to conduct forensic accounting investigations to effectively target the proceeds of drug crime. Finally, the evaluation found that law enforcement plays an enabling role in advancing public health outcomes for substance-related issues, and that law enforcement and criminal justice partners are taking more of a public health approach to their work, noting their unique position to assist individuals who engage in harmful substance use. However, additional training and guidance is still needed.
Overall, based on evidence across all pillars and themes, substance use is being addressed increasingly as a health and social issue by governments and Canadian society. In addition to the CDSS and Opioid Initiative, there are several complimentary activities that support CDSS objectives, though are not funded under the Strategy. While most of these have been considered in the broader federal actions on addressing the overdose crisis, the evaluation found that there could be more opportunities to create synergies with CDSS activities to ensure a holistic response to substance use, one with enhanced considerations of social determinants of health, such as housing.
The evaluation also examined the CDSS governance structure and found that despite positive collaboration between horizontal partners, there are still challenges within the structure that limit effective coordination. In terms of external engagement, the establishment of the PWLLE Council was a key success. However, greater representation of people from different places on the spectrum of substance use treatment and recovery is needed, and from more diverse backgrounds, including more meaningful engagement with Indigenous communities and partners.
Lastly, there were limitations with respect to performance measurement and review of the Strategy's impact due to overall performance data issues and evidence gaps across all 4 pillars. While considerable progress has been made on enhancing the evidence base and improving surveillance data and monitoring, continued work in this area and on addressing evidence and data gaps were identified as key priorities going forward.
Recommendations
Recommendation #1
Address the prevalence of alcohol use and harms [Health Canada and PHAC].
Alcohol use was identified as a gap in the Strategy and an area of risk and need that requires prevention efforts, including targeted approaches for specific populations like youth. Alcohol is the second leading cause of death from substance use in Canada after tobacco, incurring higher costs and harm than other substances. This includes health care costs, criminal justice system costs, losses in productivity, and other direct costs. Yet challenges remain to prevent alcohol use-related harm due to the normalization of alcohol and the lack of awareness of its harms. The evaluation found a need to continuously improve on prevention and outreach to minimize the harm associated with alcohol use.
Recommendation #2
Enhance prevention and outreach efforts for higher-risk groups to address the root causes of substance use [Health Canada and PHAC].
Despite public education campaigns, knowledge of drug and substance use risks and harms among people in Canada has remained unchanged over the past 5 years. The minimal changes since 2017 to rates of high-risk behaviours around substance use suggest further prevention efforts are required, including more upstream prevention to have a greater impact on changing substance use behaviours among Canadians. There are opportunities to increase use of policy measures to drive behaviour change as well as improve collaboration between partners to address homelessness and mental illness.
Recommendation #3
Contribute towards addressing evidence gaps to get a more comprehensive national and regional picture of substance use issues and the domestic illegal drug supply, as well as a better understanding of the impact of services and supports [Health Canada and PHAC, in collaboration with all CDSS partners].
While surveillance data and monitoring have improved since the implementation of the CDSS, there are still challenges with the evidence base around substance use and related harm in Canada, including data gaps, especially in disaggregated surveillance data, as well as data to effectively monitor treatment and recovery services and supports on a national scale. As such, the evaluation identified a need to improve on disaggregated surveillance data to get a better understanding of differential impacts on sub-groups of the population. There is also a need for continued evidence-building related to the effectiveness of interventions and policies.
Recommendation #4
Enhance the performance measurement strategy to align better with the CDSS's outcomes, including a review of performance indicators to focus more on the impacts of activities [Health Canada, in collaboration with all CDSS partners].
There were challenges with the quality of the performance data and limited information to effectively measure the Strategy's impact. This included gaps in performance-related data, including a need for disaggregated data on people impacted by federal efforts and some CDSS-related activities lacking indicators in the CDSS performance measurement strategy. Additionally, there did not appear to be a strong shared understanding among partners around the Strategy's expected outcomes and achievements. There was also a lack of clarity in how activities described under the CDSS contributed to the Strategy's long-term outcomes. As such, the evaluation found a need to improve the performance measurement strategy, including a review of its indicators and outcomes for the next iteration of the Strategy.
Recommendation #5
Review the governance structure to clarify roles and responsibilities, and streamline where possible, while still facilitating ongoing information sharing between partners and all levels of government [Health Canada, in collaboration with all CDSS partners].
There were several challenges within the governance structure that had a negative impact on effective coordination, including overlapping roles and potential duplication with other committees. The evaluation found there is a need to clarify the mandate of the CDSS, its affiliated committees and working groups, and the roles and responsibilities for all involved. There was also confusion about how newly formed committees are connected to the CDSS. Additionally, committee meetings are viewed by partners and stakeholders as mostly transactional opportunities for Health Canada to present information, which is helpful, but does not allow time for deep discussions about priorities or possible alternative approaches. Opportunities to improve governance included clarifying the program mandate and roles and responsibilities for each partner, increasing engagement and discussion opportunities for other federal partners and stakeholders to ensure all views are included.
Recommendation #6
Work to better understand the domestic illegal drug supply, including its growing toxicity, and the tools that are needed to support more effective law, border and health responses [RCMP and Public Safety Canada, in collaboration with Health Canada and CBSA].
One of the greatest risks for substance use in Canada is the high number of harm and fatalities caused by a toxic illegal drug supply. Moreover, evidence suggests that the illegal drug market in Canada is shifting, adding another layer of complexity to efforts to address the illegal supply. Specifically, there are challenges with the increasing illegal importation of precursor chemicals used to produce illegal drugs and the regulatory regime's capacity to keep pace with the composition of chemicals that are used by organized criminal groups. Considering these challenges, there is a need to gain a better understanding of the illegal domestic drug supply to better target response efforts.
Management Response and Action Plan
Health Canada welcomes the Evaluation of the Canadian Drugs and Substances Strategy (CDSS) conducted by Health Canada's (HC) Office of Audit and Evaluation (OAE), and is in general agreement with the recommendations put forward in this report. The Management Response and Action Plan (MRAP) sets out Health Canada's approach to address the recommendations.
The Government of Canada recognizes that the overdose crisis is one of the most serious and unprecedented public health crises in Canada's history, with over 36,000 overdose-related deaths from 2016 to 2022. The CDSS guides the federal government's comprehensive response to this complex and wide-scale public health issue and was developed in collaboration with a number of federal departments and agencies before and after its release in 2016. Within the framework of the CDSS, Health Canada coordinated horizontal work to take urgent action to address the overdose crisis and toxic drug supply, including: increasing access to evidence-based substance use treatment and harm reduction services and supports; prevention, awareness, and stigma reduction activities; data collection, research, and surveillance to inform decision-making; and law enforcement actions to address the illegal toxic drug supply underlying the crisis.
The overdose crisis has since been made more complex by the COVID-19 pandemic. Based on the latest available statistics from 2022, nearly 20 people per day are dying of a drug overdose in Canada. This is up from 10 people per day prior to the pandemic. The sharp rise in the number of overdoses and deaths is directly linked to the continued and worsening contamination of the illegal drug supply with synthetic opioids and other substances, including fentanyl and benzodiazepines. A number of additional factors may have contributed to a worsening of the overdose crisis over the course of the pandemic, including increased feelings of isolation, stress and anxiety, and changes in the availability or accessibility of services for people who use drugs.
In addition to delivering the CDSS, Health Canda is also working closely with provinces and territories to change the way our health care system delivers mental health and substance use services to Canadians. It is important for Canadians to have timely access to trauma-informed, culturally sensitive, quality mental health and substance use services that meet their needs, including underserved and equity-deserving individuals. Through Budget 2023, the federal government committed $198.6 billion over 10 years to bolster the health care system. This includes top-ups to the Canada Health Transfer to address immediate health care pressures, and $25 billion over 10 years to support shared health priorities through tailored bilateral agreements, including increased access to mental health and substance use services and integrating mental health and substance use across the health care system.
The driving factors of the crisis are complex, multifaceted and interrelated. The Government recognizes that social determinants of health, such as poverty, discrimination, and trauma, can place individuals at an increased risk of substance use harms and that the approaches to reduce these harms require sustained efforts and supports from diverse systems. Health Canada continues to work closely across federal departments to ensure that federal actions on mental health and addictions, homelessness and housing, poverty, and reconciliation are coordinated and synergistic. We are also committed to engaging collaboratively with provinces and territories, First Nations, Inuit, and Métis communities, and other stakeholders to advance whole-of-society approaches to these issues.
Going forward, Health Canada will continue to work closely with CDSS federal departments and agencies, as well as other key partners including provinces and territories, people with lived and living experience and Indigenous communities, and stakeholders to address this complex public health crisis.
Recommendation 1
Address the prevalence of alcohol use and harms [Health Canada and PHAC].
Management response
Management agrees with the recommendation. Building on past and present activities, Health Canada and PHAC will continue to address the prevalence of alcohol use and related harms, in the broader context of harm reduction and prevention activities related to substance use.
Action Plan
1.1 Health Canada will continue to monitor Canadians' awareness of harms and fund, through the Substance Use and Addictions Program (SUAP), specific initiatives related to knowledge mobilization, guidance and/or innovative programs to address alcohol harms.
1.2 PHAC will pursue activities that address the prevalence of alcohol use and related harms, in the broader context of harm prevention activities related to substance use.
| Deliverables | Expected Completion | Accountability | Resources |
|---|---|---|---|
| 1.1.1 The Public Awareness of Alcohol-related Harms Survey (a biennial general population public opinion survey) will be conducted and the results will be analyzed and publicly released. | December 31, 2023 | Lead: Director General, Controlled Substances Directorate (CSD), Controlled Substances and Cannabis Branch, Health Canada | Existing resources |
| 1.1.2 Through SUAP, HC will fund the development of knowledge mobilization strategies, tools, products and/or activities, developed in collaboration with key populations, to raise awareness about alcohol-related harms and how to reduce them. | June 30, 2025 | Lead: Director General, Controlled Substances Directorate, Controlled Substances and Cannabis Branch, Health Canada Director General, Horizontal Policy, Planning and Program Directorate, Controlled Substances and Cannabis Branch, Health Canada. Support: Director General, Health Programs and Strategic Initiatives, Strategic Policy Branch, Health Canada |
Existing resources |
| 1.1.3 Through SUAP, support the development of guidance and innovative projects to address alcohol harms. | June 30, 2024 (confirmation of project funding) | Lead: Director General, Controlled Substances Directorate, Controlled Substances and Cannabis Branch, Health Canada Director General, Horizontal Policy, Planning and Program Directorate, Controlled Substances and Cannabis Branch, Health Canada. |
Existing resources |
| 1.2.1 Systematic review on the effectiveness of alcohol labelling. | Currently in progress, completion by September 2023 | Executive Director, Centre for Surveillance and Applied Research, Public Health Agency of Canada | Existing CSAR resources, meaning there is no funding via CDSS;100% of 1 EC-05; 30% of 2 EC-06s between now and end of September 2023. |
Recommendation 2
Enhance prevention and outreach efforts for higher-risk groups to address the root causes of substance use [Health Canada and PHAC].
Management response
Management agrees with the recommendation. Additionally, PHAC notes the following:
- There is an opportunity to enhance our prevention efforts with young people who are a higher-risk group.
- Adolescence and young adulthood are key life stages when lifelong behaviours often become established.
- During this time, many youths experiment with substance use: some go on to do so in ways that are harmful to themselves and others. The earlier in life that an individual starts using substances and the heavier or frequent their use, the higher the risk for substance-related harms later in life. Focusing efforts early on can therefore help to reduce potential risky behaviours and long-term negative health effects.
- The research shows that intervening early to counteract the risk factors of substance-related harms, offers the best chance of having a positive influence on a young person's development and reducing long-term harms to them and to society as a whole.
Action Plan
2.1 Health Canada will work with INFC and others on alignment of levers to advance support for complex needs (homelessness, mental health and substance use).
2.2 Health Canada will leverage the Canadian Drugs and Substances Strategy (CDSS) Director General's Steering Committee to identify actions that could be taken to address the underlying inequities driving substance use related harms.
2.3 The Centre for Mental Health and Wellbeing will launch a new community-based Grants and Contributions Program to prevent substance use among young people.
| Deliverables | Expected Completion | Accountability | Resources |
|---|---|---|---|
| 2.1.1 Undertake research and develop policy advice to help explore and identify opportunities to work with other governments to advance pan-Canadian work on complex needs (mental health and substance use). | September 30, 2023 | Lead: Director General, Mental Health and Substance Use Integration Directorate | Existing Resources |
| 2.1.2 Knowledge mobilization and/or synthesis - host an event and/or conduct a review to explore best practices and identify opportunities for collaboration on complex needs. | March 31, 2024 | ||
| 2.2.1 Development of a CDSS Equity Action Plan. | March 31, 2024 | Lead: Director General, Controlled Substances Directorate Support: All CDSS Partners |
New resources provided through Budget 2023/CDSS renewal |
| 2.3.1 Funding agreements signed with recipients under the new Youth Substance Use Prevention Grants and Contributions (Gs&Cs) program focussed on building protective factors with a community collaborative approach based on evidence. | Signing of first round of Youth Prevention Program G&C funding agreements 2024-25 Q1. | Director General, Centre for Mental Health and Wellbeing, Public Health Agency of Canada | $20.2M over 5 years starting in 2023-24 as part of a renewed CDSS |
Recommendation 3
Contribute towards addressing evidence gaps to get a more comprehensive national and regional picture of substance use issues and the domestic illegal drug supply, as well as a better understanding of the impact of services and supports [Health Canada and PHAC, in collaboration with all CDSS partners].
Management response
Management agrees with the recommendation. The Health Portfolio's (HC, PHAC, CIHR) surveillance, applied research and modelling have been a critical component of the federal government's ability to monitor, understand and report on the overdose crisis at a national level. Ongoing work in these areas will continue to contribute toward building the evidence base on substance related harms.
Action Plan
3.1 Conduct targeted surveys, research and data collection to fill recognised data gaps and monitor the impact of harm reduction services. Disaggregated data collection will be supported to enhance substance use surveillance from hard-to-reach, at-risk and priority populations.
3.2 PHAC's Centre for Surveillance and Applied Research will continue undertaking public health surveillance and applied research to contribute to the evidence base on substance related harms.
| Deliverables | Expected Completion | Accountability | Resources |
|---|---|---|---|
| 3.1.1 Develop and publish the infographic of the CDSS Data and Evidence Framework on Canada.ca. Through quarterly meetings, the CDSS Data and Evidence Partners Table (CDSS DEPT) will promote the development and improvement of data and surveillance initiatives on substances and their use to address critical evidence gaps. | March 31, 2024 (Quarterly meetings began in January 2023) | Lead: Director General, Controlled Substances Directorate (CSD), Controlled Substances and Cannabis Branch, Health Canada Support: All CDSS data and evidence partners | Existing resources |
| 3.1.2 Conduct Surveys of People with Lived and Living Experience (PWLLE) and the Online New Psychoactive Substances Survey to obtain information on sub-sections of the population (especially high-risk populations), to monitor substance use related harms and the emergence of new psychoactive substances. | March 31, 2024 | Lead: Director General, Controlled Substances Directorate (CSD), Controlled Substances and Cannabis Branch, Health Canada | Existing resources |
| 3.1.3 Enhance data collection from Supervised Consumption Sites (SCS) offering services in Canada and publish a new dynamic, user-friendly dashboard with SCS statistics to monitor the differential impacts of harm reduction services. | December 31, 2023 | Lead: Director General, Controlled Substances Directorate (CSD), Controlled Substances and Cannabis Branch, Health Canada | Existing resources |
| 3.2.1 Continued quarterly reporting of opioid- and stimulant-related harms and ongoing publication of surveillance and research findings. | Next quarterly data release to take place September 2023 | Executive Director, Centre for Surveillance and Applied Research, Public Health Agency of Canada | $16M over 5 years starting in 2023-24 as part of a renewed CDSS |
Recommendation 4
Enhance the performance measurement strategy to align better with the CDSS's outcomes, including a review of performance indicators to focus more on impacts of activities [Health Canada, in collaboration with all CDSS partners].
Management response
Management agrees with the recommendation. Management previously identified this issue, and work on the response has been ongoing.
Action Plan
4.1 The Canadian Drugs and Substances Strategy Horizontal Initiative (CDSS HI) logic model, and its associated indicators, are being updated to reflect the renewed strategy.
| Deliverables | Expected Completion | Accountability | Resources |
|---|---|---|---|
| 4.1 The renewed Canadian Substances and Drugs Strategy Horizontal Initiative Framework (CDSS HIF) will identify outcomes and key performance indicators that focus more on impacts instead of activities. | September 30, 2023 | Lead: Director General, Controlled Substances Directorate (CSD) Controlled Substances and Cannabis Branch, Health Canada Support: all CDSS Partners |
Existing Resources |
Recommendation 5
Review the governance structure to clarify roles and responsibilities, and streamline where possible, while still facilitating ongoing information sharing across partners and all levels of government [Health Canada, in collaboration with all CDSS partners].
Management response
Management agrees with the recommendation.
Action Plan
5.1 Governance for the CDSS will be reviewed and adjusted as needed to reduce duplication and ensure effective information sharing across partners and stakeholders.
| Deliverables | Expected Completion | Accountability | Resources |
|---|---|---|---|
| 5.1 Refreshed governance structure, meaning committees with appropriate membership are re-established at various levels required to support CDSS implementation. | November 30, 2023 | Lead: Director General, Controlled Substances Directorate (CSD) Controlled Substances and Cannabis Branch, Health Canada Support: All CDSS partners |
Existing |
Recommendation 6
Work to better understand the domestic illegal drug supply, including its growing toxicity, and the tools that are needed to support more effective law, border and health responses [RCMP and Public Safety Canada, in collaboration with Health Canada and CBSA].
Management response
Management agrees with the recommendation. Public Safety management notes planned work will support improved collaboration and information-sharing between the law enforcement and public health communities, improved first response to overdoses by both law enforcement and health actors, gather actionable information on organized crime's drug trafficking patterns and help strengthen a weak evidence base on the illegal drug supply to inform decision-making under a modernized CDSS. This work also supports the Minister of Public Safety's mandate letter to address cross-border drug-trafficking. RCMP management supports the findings of this evaluation report. Additional resources as requested in the CDSS renewal, as well as ongoing operations and maintenance funding, will be required to fully implement these recommendations, and to continue building capacity and capability across the organization in support of policing operations. In addition, activities are dependent on partners having proper systems and resources in place.
Action Plan
6.1 Develop and establish data collection and reporting process and tools to better understand the domestic illegal drug supply.
6.2 Improve the sharing of information, intelligence and best practices related to the domestic illegal drug supply with domestic and international partners.
6.3 Establish an illegal drug fusion center to enhance cooperation and sharing between law enforcement, non-law enforcement, academia and private industry.
6.4 Invest in new mechanisms to better understand the dynamics of the illegal drug supply, its toxicity, and the tools needed to support effective responses, pending Treasury Board approval for programming and dependent upon available resources for research.
6.5 Provide timely drug analysis services as well as timely scientific and analytical support to increase the effectiveness of law enforcement and public health responses.
| Deliverables | Expected Completion | Accountability | Resources |
|---|---|---|---|
| 6.1.1 Complete analysis and creation of an analytical report created as a result of the new data collection process put in place to streamline seizure data for the Health Canada Drug Analysis System. | December 31, 2024 | Lead: Director General, Federal Policing Criminal Operations, Serious and Organized Crime/ Business Intelligence, RCMP |
New Resources must be provided through Budget 2023/CDSS renewal |
| 6.1.2 Complete analysis and creation of an analytical report created as a result of the new data collection process put in place to streamline seizure data for the Records Management System. | December 31, 2024 | Lead: Director General, Federal Policing Strategic Management, RCMP | New Resources must be provided through Budget 2023/CDSS renewal |
| 6.2.1 Reports shared internally and externally with domestic and international partners. | March 31, 2025 | Lead: Director, Federal Policing Criminal Operations, Serious and Organized Crime/ Business Intelligence, RCMP |
New Resources must be provided through Budget 2023/CDSS renewal |
| 6.2.2 Intelligence products shared internally and externally with domestic and international partners | March 31, 2025 | Lead: Director General Federal Policing National Intelligence, RCMP |
New resources must be provided through Budget 2023/CDSS renewal |
| 6.3.1 Fusion Center Integration of current illegal drug resources within Criminal Intelligence Service Canada. | March 31, 2025 | Lead: Director General, Criminal Intelligence Service Canada, RCMP | New resources must be provided through Budget 2023/CDSS renewal |
| 6.3.2 Creation of a working group which seeks alternative measures of disruption to encourage non-law enforcement measures to disrupt organized crime involvement in the illegal drug supply. | March 31, 2025 | Lead: Director General, Criminal Intelligence Service Canada, RCMP | New resources must be provided through Budget 2023/CDSS renewal |
6.4.1 Adapt for Canada and pilot in up to 3 jurisdictions the successful US-based Overdose Detection Mapping Application Program (ODMAP), which provides near real-time information about suspected overdoses to support public health and public safety response and information about illegal drug trafficking patterns. To this end:
|
|
Lead: Director General, Law Enforcement and Border Strategies, Crime Prevention Branch; Senior Assistant Deputy Minister, Crime Prevention Branch; Public Safety Canada |
New resources provided through Budget 2023/CDSS renewal |
| 6.4.2 Commission a research project on priority topics to better understand the dynamics of the illegal drug market and how to improve responses to it. | Deliver first report by September 2024 | Existing resources | |
| 6.5.1 Reduce service standard for the issuance of the sample result to law enforcement agencies from over 60 days to 45 days | April 1, 2023 | Lead: Director, Drug Analysis Service (DAS) and Cannabis Labs | Existing resources and new resources provided through Budget 2023/CDSS renewal |
Annexes
Annex A: Methodology, limitations and mitigation strategies, and evaluation governance
Data sources
The evaluation collected and analyzed multiple lines of evidence from horizontal partners and external sources, as described in this section. These lines of evidence were triangulated to improve the reliability and credibility of evaluation findings and conclusions.
Document and file review
Evaluators reviewed approximately 296 documents and files provided by funded partners. These documents included administrative files, guiding policy documents, records of decisions, briefing materials, summary reports, examples of public education materials, and internal work plans.
Interviews
Interviews were conducted with 92 representatives from the following groups:
Internal:
- Health Canada: 23
- Funded Federal Partners: 22
- Unfunded Partners: 2
External stakeholders and partners:
- PT Government Representatives: 7
- Indigenous Partners: 3
- SUAP Funding Recipients: 6
- Academics and Experts: 8
- Health care Professional Associations: 1
- PWLLE organizations: 4
- PT Chief Medical Officer of Health: 1
Academic and grey literature review
Evaluators conducted a focused review of academic literature and grey literature from reliable to further inform evaluation findings.
Comparative analysis
The comparative analysis included a review of provincial and territorial strategies to address drug and substance use, with a focus on alcohol and opioid use, as well as a review of strategies in comparable countries.
Performance measurement data
Horizontal partners each provided performance measurement data for the period under review. Performance indicators were specified for all funded partners in the Health Canada Departmental Results Report, Supplementary Information Tables, as well as relevant performance information profiles. Evaluators analyzed data for key trends and results against established targets.
Financial analysis
A breakdown of annual planned vs actual expenditures for Horizontal Initiative activities was provided by each funded partner for the period under review. Evaluators analyzed these data for variance and key trends.
Governance survey and questionnaire
A survey link was distributed to members of the Director General Standing Committee and CDSS Working Group. The survey included a series of questions to gather views on the governance structure and process of the CDSS. OAE also distributed a governance questionnaire, via email, to working level staff involved in CDSS governance committees.
Limitations and mitigation strategies
Despite triangulation across various lines of evidence, most evaluations still face constraints that may affect the validity and reliability of findings and conclusions. Table 5 outlines the limitations encountered during the current evaluation, as well as mitigation strategies put in place to ensure evaluation findings were sufficiently robust.
| Limitations | Potential impact | Mitigation strategies |
|---|---|---|
| The COVID-19 pandemic has affected many departments and agencies across the Government of Canada, requiring mobilization of priorities and resources. | A shift in resources and the introduction of transitional provisions had an impact on planned deliverables, as well as availability of certain performance data. | Administrative data and evidence from other sources, such as interviews, were used to fill any gaps and to estimate the impact of COVID-19 on planned deliverables and expected results. |
| Key informant interviews are retrospective in nature, providing only a recent perspective on past events. | This could influence the validity of respondents' assessment of activities or results that may have changed over time. | The other lines of evidence were triangulated with the data received from interviews to substantiate or provide further information. Document review also provided corporate knowledge. |
| The evaluation was conducted concurrently during the Strategy's renewal. | Comprehensive evaluation findings were not available to inform and support the Strategy's renewal. | The evaluation took a phased approached. A summary of literature review and comparative analysis findings was provided earlier. This exercise was intended to support renewal planning for the CDSS in the Fall. Findings were then triangulated with interview and performance data to support overall evaluation findings. While comprehensive findings were not available to support renewal planning, evaluation recommendations can be considered and addressed as part of implementation and other forward planning exercises. |
| The evaluation originally planned to form an advisory panel comprised of PWLLE to include their perspectives in a participatory and meaningful way throughout each phase of the evaluation project. Since the timing of the evaluation coincided with the Strategy's renewal, a process through which the PWLLE council had already been extensively engaged with, and the fact that new members were joining the Council, it was decided that it was not an appropriate time for further engagement. | Some perspectives may not have been captured due to limited engagement, and those shared may not be representative of the stakeholder group. | The evaluation incorporated representatives from a wide variety of internal and external stakeholders, including from organizations that advocate for PWLLE. In-depth interviews were conducted based on the focused interview guides unique to key informants' area of expertise. Triangulation with other lines of evidence was also conducted to substantiate interview findings. |
| Given the high-level and horizontal nature of the evaluation, most internal interviews were conducted with senior management. | Some perspectives may not have been captured, and those shared may not always be representative of those involved at the working level. | As part of the interview scheduling, interviewees were welcomed to invite other team members to participate in a group interview. Furthermore, we developed a survey and questionnaire that was sent out to secondary contacts and members of other working level committees. |
| There were limitations with the performance data analysis as there were inconsistencies, gaps, and overall issues with the quality of the data provided. | Data inconsistencies make it challenging to assess overall impact of activities. | Performance data was triangulated with other lines of evidence to fill in any gaps and provide context on methodological challenges and updates to indicators throughout the evaluation period. |
Evaluation lenses and government priorities
The CDSS and the Opioid Initiative respond to one of the Government of Canada's priorities to address the opioid overdose crisis in Canada, an issue that has been highlighted in each federal budget and economic statement since 2017. In 2021, the federal government introduced the Minister of Mental Health and Addictions and Associate Deputy Minister of Health. The Minister's mandate letter from December 2021 identified a commitment to advance the CDSS as a "comprehensive strategy to address problematic substance use in Canada."Footnote 143 Finally, the Government of Canada is committed to ensuring public policies address systemic inequities and disparities in Canadian society by applying and intersectional lens to its decision-making. To this effect, the evaluation applied several lenses and frameworks to assessing progress and impacts of the CDSS and the Opioid Initiative. These were:
- Sex and Gender-Based Analysis Plus (SGBA +) Lens: The evaluation acknowledged how issues of substance use had differential impacts for different population sub-groups. The evaluation considered areas where the CDSS and the Opioid Initiative are successful or could improve their ability to address the needs of populations disproportionately impacted by substance-related harms.
- Surveillance Lens: The evaluation examined how national surveillance for rates of substance use and related harm supported achievement of CDSS and Opioid Initiative outcomes. The evaluation also examined to what extent supporting surveillance systems were timely and useful, and produced high-quality and appropriately disaggregated data.
- United Nations Sustainable Development Goals (SDGs): The evaluation considered the extent to which the CDSS and Opioid Initiative aligned with and contributed to the achievement of SDG 3 to "ensure healthy lives and promote well-being for all at all ages." Specifically, the evaluation looked at Target 3.5 to "strengthen the prevention and treatment of substance abuse, including narcotic drug abuse and harmful use of alcohol."Footnote 144
- Quality of Life (QoL) Framework for Canada: The evaluation examined the extent to which the CDSS and the Opioid Initiative directly addressed the Health domain in the QoL Framework. Given the intersectional nature of substance use issues, the evaluation also considered indicators under the domains of Prosperity and Good Governance.
- Truth and Reconciliation Commission (TRC) Calls to Action: The evaluation acknowledged that Indigenous populations are disproportionately impacted by the opioid crisis and other substance related harms and by discrimination and unequal access to services. The evaluation considered the TRC Calls to Action around the role of the federal government in addressing health inequities and impacts of the criminal justice system for Indigenous peoples in Canada.
- Official Languages: The evaluation did not specifically examine compliance with and implementation of the Official Languages Act. However, use of official language did not appear to be an issue for CDSS or Opioid Initiative activities.
Evaluation governance
In conducting the evaluation, a single window was identified within each Health Canada branch involved in the CDSS or Opioid Initiative, with whom the Office of Audit and Evaluation (OAE) worked closely throughout the evaluation. The scope for this evaluation was shared with the Performance Measurement, Evaluation and Results Committee (PMERC) as well as with the CDSS Director General Steering Committee in June 2022. The preliminary findings were presented to the PMERC on March 23, 2023, and the final report will be presented to the PMERC in June 2023. Moreover, given the horizontal nature of the Strategy, an interdepartmental evaluation working group (IEWG) was formed to ensure timely communication and information sharing with all federal partners. The IEWG included a member from each partner department's evaluation office, who served as the single window between their respective program areas and the OAE.
Annex B: Financial Information
| Fiscal year | Planned | Actual | Total Variance | % Budget Spent |
|---|---|---|---|---|
| 2017-18 | $118,869,614.00 | $132,973,255.00 | $14,103,641.00 | 112% |
| 2018-19 | $128,293,301.00 | $154,738,829.00 | $26,445,528.00 | 121% |
| 2019-20 | $120,670,904.00 | $145,785,927.00 | $25,115,023.00 | 121% |
| 2020-21 | $126,313,394.00 | $149,602,055.01 | $23,288,661.01 | 118% |
| 2021-22 | $123,094,938.00 | $158,564,271.00 | $35,469,333.00 | 129% |
| Total | $617,242,151.00 | $ 741,664,337.01 | $124,422,186.01 | 120% |
| Average | $123,448,430.20 | $148,332,867.40 | $24,884,437.20 | 120% |
Amounts exclude internal services.
| Fiscal year | Planned | Actual | Total variance | >% budget spent |
|---|---|---|---|---|
| 2018-19 | $20,414,965.00 | $12,803,277.00 | -$7,611,688.00 | 63% |
| 2019-20 | $25,071,101.00 | $25,972,681.00 | $901,580.00 | 104% |
| 2020-21 | $19,305,458.00 | $21,865,516.00 | $2,560,058.00 | 113% |
| 2021-22 | $16,161,446.00 | $17,822,580.00 | $1,661,134.00 | 110% |
| Total | $80,952,970.00 | $78,464,054.00 | -$2,488,916.00 | 97% |
| Average | $20,238,242.50 | $19,616,013.50 | -$622,229.00 | 97% |
Amounts exclude internal services.
| Organization | Planned | Actual | Total variance | % budget spent |
|---|---|---|---|---|
| HC | $269,946,764.00 | $299,504,931.00 | $29,558,167.00 | 111% |
| PPSC | $52,313,295.00 | $146,813,199.00 | $94,499,904.00 | 281% |
| RCMP | $93,889,757.00 | $93,889,757.00 | $- | 100% |
| ISC | $89,733,585.00 | $87,356,181.00 | -$2,377,404.00 | 97% |
| JUS | $26,469,146.00 | $26,961,890.00 | $492,744.00 | 102% |
| PHAC | $30,563,440.00 | $24,408,192.01 | -$6,155,247.99 | 80% |
| CIHR | $16,874,990.00 | $16,557,641.00 | -$317,349.00 | 98% |
| CBSA | $11,500,000.00 | $11,500,000.00 | $- | 100% |
| FINTRAC | $- | $9,696,076.00 | $9,696,076.00 | N/A |
| CSC | $9,258,483.00 | $7,956,095.00 | -$1,302,388.00 | 86% |
| CRA | $4,791,031.00 | $6,450,271.00 | $1,659,240.00 | 135% |
| GAC | $4,500,000.00 | $4,519,078.00 | $19,078.00 | 100% |
| PSPC | $3,000,000.00 | $2,980,930.00 | -$19,070.00 | 99% |
| PS | $2,942,660.00 | $1,910,096.00 | -$1,032,564.00 | 65% |
| PBC | $1,459,000.00 | $1,160,000.00 | -$299,000.00 | 80% |
| Total | $617,242,151.00 | $741,664,337.01 | $124,422,186.01 | 120% |
Amounts exclude internal services.
| Or | Planned | Actual | Total Variance | % Budget Spent |
|---|---|---|---|---|
| CBSA | $17,362,396.00 | $25,117,078.00 | $7,754,682.00 | 145% |
| HC | $44,714,826.00 | $37,105,648.00 | -$7,609,178.00 | 83% |
| PHAC | $12,179,715.00 | $14,025,249.00 | $1,845,534.00 | 115% |
| PS | $2,522,995.00 | $3,025,904.00 | $502,909.00 | 120% |
| StatsCan | $1,684,122.00 | $1,679,091.00 | -$5,031.00 | 100% |
| Total | $78,464,054.00 | $80,952,970.00 | $2,488,916.00 | 103% |
Amounts exclude internal services.
Background on Funding Sources
- The CDSS reports on allocated funding and designated activities that originally began with the National Anti-Drug Strategy (NADS), the previous national drug strategy first launched in 2006. In 2006, the NADS had funding and activities for Prevention, Treatment, and Enforcement.
- In 2014, the NADS expanded to include funding and activities for the Problematic Prescription Drug Use (PPDU) program under the Prevention pillar. NADS and PPDU funding has never been renewed or changed.
- In 2017, the CDSS replaced the NADS and included funding and activities under 2 new pillars: Harm Reduction and Evidence Base.
- In 2018, the Addressing the Opioid Crisis initiative began and received $19,497,063 in funding, including internal services, that was reallocated from the total federal funding for the CDSS to the Opioid Initiative.
- Recent Opioid Initiative funding and activities, including from Budget 2019, the 2020 Fall Economic Statement, Budget 2021, and Budget 2022, are not reported in CDSS financial information in public reporting.
- Historically, several partners have reported significant variances in their actual spending compared to their planned spending, that is, generally spending more than their allocation from NADS.
Annex C: CDSS logic modelFootnote 145

DRAFT (v5)
*Outputs and Activities will be further defined during Phase 2 - Performance Incidator Review
Figure Annex C - Text description
Annex C shows the draft logic model for the CDSS. This logic model is a draft from April 9, 2019. The CDSS is continuing to refine its logic model and performance measurement strategy. However, as a retrospective exercise, the evaluation used this latest available logic model to assess achievement of outcomes. Additionally, Health Canada has moved away from stigmatizing language such as “problematic substance use.” While terminology updates are reflected throughout the evaluation report, this logic model contains original language that is no longer in use.
The title at the top of the diagram appears in a box as follows:
- Canadian Drugs and Substances Strategy (CDSS) Logic Model – Draft April 9, 2019
Description of the Logic Model diagram starting from the bottom:
Target populations and stakeholders
- A large rectangle going across the page horizontally lists the target populations and stakeholders of the CDSS as follows: Canadians; People who use drugs; People engaged in problematic substances use (e.g. dependence); Persons with lived and living experience; first responders; Health professionals and practitioners; law enforcement; Provinces, territories, municipal, Indigenous governments; Regulated parties (e.g. Licensed Dealers, Registered Dealers, etc.); International organizations and partners; and other stakeholders.
Outputs and Activities – (Products/Services & Actions Undertaken)
Four boxes appear across the page representing each CDSS pillar.
- Prevention: Prevention outputs and activities are listed in the first box from the left. This box is connected to short-term outcomes one and two in the row above and lists the following: Public awareness and knowledge (information and tools) activities; actions to address social determinates of problematic drug and substance use; federal policing prevention and public engagement activities.
- Treatment: Treatment outputs and activities are listed in the second box from the left. This box is connected to short-term outcome three in the row above and lists the following: activities to improve provincial/territorial treatment systems and capacity; support for treatment guideline development; funding for federal Drug Treatment Courts and drug treatment programming for youth involved in the justice system.
- Harm Reduction: Harm Reduction outputs and activities are listed in the third box from the left. This box is connected to short-term outcomes four and five in the row above and lists the following: Regulatory activities (e.g. assessment of applications for supervised consumption sites); federal funding for community based projects to reduce blood-borne infections and sexually transmitted diseases; drug analysis services and knowledge sharing.
- Enforcement: Enforcement outputs and activities are listed in the fourth box from the left. This box is connected to short-term outcome six in the row above and lists the following: Regulatory authorization, compliance and enforcement actions; federal drug law enforcement activities (charges/prosecutions, seizures and destruction, border security, financial intelligence/investigations/audits); drug analysis laboratory services.
Short-term Outcome(s) – Change of Awareness Capacity Years 1-2
- First box from left: Increase knowledge to help Canadians make informed choices and reduce risks and harms of drug and substance use [STO1]
- Second box from left: Increase awareness and collaboration to address the root causes of problematic substance use [STO2]
- STO1 and STO2 are connected to medium-term outcome 1 in the row above.
- Third box from left: Federal actions support the expansion of evidence-based treatment services and systems [STO3]
- STO 3 is connected to medium-term outcome 2 in the row above.
- Fourth box from the left: Increase awareness of harm reduction principles and services for a wide variety of drugs and substances [STO4]
- STO 4 is connected to medium-term outcome 3 in the row above.
- Fifth box from the left: Increase awareness of, and begin to reduce the negative impacts of stigma towards people who use drugs problematically [STO5]
- STO 5 is connected to medium-term outcome 3 in the row above.
- Sixth box from the left: Federal regulatory approaches ensure access to controlled substances for medical, research, and industrial purposes while effectively minimizing diversion of controlled drugs and precursor chemicals used to make illegal drugs [STO6]
- STO 6 is connected to short-term outcomes 6 and 7 which appear in boxes above.
- Seventh box from the left and above STO6: Increase collaboration between law
- enforcement and public health to recognize and address problematic substance use as individuals interact with the criminal justice system [STO7]
- STO 7 is connected to medium-term outcome 4.
- Eighth box from the left and above STO 6: Increase effectiveness of law
- enforcement efforts to address organized crime and target the proceeds of drug crime [STO8]
- STO 8 is connected to medium-term outcome 5 in the row above.
Medium-term Outcome(s) Change in Behaviour Years 3-5
- First box from the left: Canadians make better informed choices around substances use and risks to reduce harms [MTO1]
- MTO 1 is connected to long-term outcome 1 in the row above.
- Second box from the left: Treatment and recovery services/systems are easily accessible, comprehensive and appropriately tailored to the needs of individuals [MTO2]
- MTO 2 is connected to long-term outcome 1 in the above and interconnected to MTO 3 on the right.
- Third box from the left: Increased uptake of community-based harms reduction programs and services across Canada [MTO 3]
- MTO 3 is connected to long-term outcome 2 in the row above and interconnected with MTO 4 on the right.
- Fourth box from the left: Stigma is reduced and people who use drugs are increasingly accessing and are supported with appropriate health and social services [MTO 4]
- MTO 4 is connected to long-term outcomes 2 and 3 in the row above.
- Fifth box from the left: Decreased diversion of drugs away from authorized activities and
- reduced size and profitability of the illegal drug market [MTO 5]
- MTO 5 is connected to long-term outcome 3 in the row above.
Long-term Outcome(s) Change of State Year 5+
- First box from the left: Problematic substance use is addressed as a health and social issue by governments, communities, stakeholders and Canadian society [LTO1]
- LTO 1 is interconnected to long-term outcome 2 on the right.
- Second box from the left: Rates of problematic substance use in Canada are minimized, especially for youth and those most at risk of harm, including preventing, reducing and/or delaying the use of drugs and other substances [LTO2]
- LTO 2 is interconnected to long-term outcome 3 on the right.
- Third box from the left: Canadians and their communities are supported with evidence-based tools, programs and services to be safer, healthier and more resilient [LTO3]
Impact(s) Results for Canadians
- At the top of the Logic Model, above the long-term outcomes, a rectangle appears outlining the ultimate outcome. This rectangle extends across the page and outlines in bold: Protect the health and safety of all Canadians by minimizing harms from substance use for individuals, families and communities.
Annex D: Addressing the Opioid Crisis Initiative - intended outcomes by theme
Shared outcome: Reducing harms and deaths related to opioid use
- Supporting additional prevention and treatment interventions [HC]
- Targeted stakeholders use evidence-informed information on opioid use to change policies, programs, and practice
- Targeted stakeholders and Canadians are equipped with the capacity (knowledge, skills and supports) to inform their decisions and actions related to opioid use
- Addressing stigma [HC, PS]
- Increased perception among Canadians of drug use as a public health issue
- Increased sympathy among Canadians for people using opioids
- Increased awareness of the impacts of stigma and support for people who use substances amongst law enforcement community about de-stigmatization of people who use opioids
- Taking Action at Canada's Borders [PS, CBSA]
- Enhanced capability to interdict illegal cross-border movement of drugs, such as opioids, at ports of entry (Public Safety, CBSA)
- Increased knowledge generation and sharing of information on targeted issues related to reducing the illegal supply of opioids in Canada (PS)
- Increased capacity to identify high-risk goods at ports of entry
- Increased ability to risk assess and identify high risk shipments
- Increased communications related to threat assessment information and intelligence provided to personnel and partnering agencies
- Enhanced capability to interdict illegal cross-border movement of drugs, such as opioids, at postal locations
- Enhancing the Evidence Base [PHAC, StatsCan]
- Enhanced quality surveillance data is available
- Enhanced quality surveillance data and research are available
- Increased use and relevance of CCMED among stakeholders
Annex E: CDSS governance structure

Figure Annex E - Text description
Annex E is a diagram depicting the CDSS governance structure and other related committees and working groups. The diagram shows a large square representing the CDSS governance structure. Inside the square are a number of boxes and arrows showing the hierarchal reporting structure of the various governance committees/working groups and how they are connected.
Starting at the bottom of the structure, a large shaded box outlines the various working groups that support the CDSS – most of which have not met in years. At the very bottom shows the Research & Evidence Working Group – which was never implemented – with arrows pointing towards the three other working groups:
- Logic Model – Evaluation & Reporting Working Group
- Supply Reduction Working Group
- Demand & Harm Reduction Working Group
An arrow from the shaded Working Groups box then points upwards to a box representing the Director General's (DG) Steering Committee. A shaded box on the left hand side then depicts groups involved in the CDSS renewal with arrows pointing towards the DG Steering Committee box. These groups include:
- Health Canada's Controlled Substances Directorate Offices
- CDSS Working Group
Another arrow from the DG Steering Committee box then points to a blue box on the right hand side representing the CDSS Secretariat Function – the governance coordinating function for the CDSS. Finally, from the DG Steering Committee box, another arrow points upwards to the ADM Executive Committee which was put on hold after the implementation of the Federal Inter-Departmental ADM's Working Group on the Opioid Overdose Crisis and the CDSS. This latter group is depicted on the right hand side with arrows pointing down toward the DG steering Committee and up toward the Deputy Minister's Task Force on the Opioid Crisis and the CDSS. Note that while the ADM Executive Committee is on hold, the DG Steering Committee reports to Federal Inter-Departmental ADM's Working Group on the Opioid Overdose Crisis and the CDSS, which then reports to the DM Task Force.
Lastly, outside of the CDSS governance structure square shows two shaded boxes representing other committees outside if the formal CDSS governance structure that are related to addressing substance use harms and the overdose crisis.
The shaded box on the bottom of the right side shows the Federal/Provincial/Territorial (FPT) groups which include:
- The FPT ADM Inter-Departmental Working Group on the Opioid Crisis
- FPT ADM Committee on Substance Use and Harms
- The box on the top of right side represents Health Canada's Strategic Policy Branch ADM Committee on Mental health and Substance Use.
Annex F: Endnotes
- Footnote 1
-
Health Canada (2022). Federal Actions on Opioids to Date. Retrieved from
https://www.canada.ca/content/dam/hc-sc/documents/services/opioids/federal-actions/overview/overview.pdf - Footnote 2
-
Health Canada. (2021). Supplementary Information Tables 2020-2021 Departmental Results Report: Health Canada - Canada.ca. Retrieved from
https://www.canada.ca/en/health-canada/corporate/transparency/corporate-management-reporting/departmental-performance-reports/2020-2021-supplementary-information-tables.html#a4.1 - Footnote 3
-
Special Advisory Committee on the Epidemic of Opioid Overdoses. Opioid- and Stimulant-related Harms in Canada. (2022). Ottawa: Public Health Agency of Canada. Retrieved from
https://health-infobase.canada.ca/substance-related-harms/opioids-stimulants/ - Footnote 4
-
Health Canada & Earnscliffe Strategy Group. (2019). Follow-up survey and qualitative research on opioid awareness, knowledge and behaviours for public education: final report / prepared for Health Canada. Retrieved from
https://publications.gc.ca/collections/collection_2019/sc-hc/H21-313-2019-eng.pdf - Footnote 5
-
Health Canada & Earnscliffe Strategy Group. (2022). Follow-up survey and qualitative research on opioid awareness, knowledge and behaviours for public education (2021): final report / prepared for Health Canada. Retrieved from
https://publications.gc.ca/collections/collection_2022/sc-hc/H21-313-2022-eng.pdf - Footnote 6
-
Health Canada & Earnscliffe Strategy Group. (2019). Follow-up survey and qualitative research on opioid awareness, knowledge and behaviours for public education: final report / prepared for Health Canada. Retrieved from
https://publications.gc.ca/collections/collection_2019/sc-hc/H21-313-2019-eng.pdf - Footnote 7
-
Health Canada. (2022). Know More: Opioid public awareness. Retrieved from
https://www.canada.ca/en/health-canada/services/opioids/know-more-public-awareness.html - Footnote 8
-
Public Health Agency of Canada (2021). Preventing substance-related harms among Canadian youth through action within school communities: A policy paper. Retrieved from
https://www.canada.ca/en/public-health/services/publications/healthy-living/policy-paper-preventing-substance-related-harms-canadian-youth-action-school-communities.html - Footnote 9
-
Public Health Agency of Canada (2021). Blueprint for Action: Preventing substance-related harms among youth through a Comprehensive School Health approach. Retrieved from
https://www.canada.ca/en/public-health/services/publications/healthy-living/blueprint-for-action-preventing-substance-related-harms-youth-comprehensive-school-health/guide.html#s0000 - Footnote 10
-
Health Canada. (2022). Supplementary Information Tables 2021-22 Departmental Plan: Health Canada - Canada.ca. Retrieved from https://www.canada.ca/en/health-canada/corporate/transparency/corporate-management-reporting/report-plans-priorities/2021-22-supplementary-information-tables.html#ah3
- Footnote 11
-
Health Canada. (2022). Supplementary Information Tables 2021-2022 Departmental Results Report: Health Canada - Canada.ca. Retrieved from https://www.canada.ca/en/health-canada/corporate/transparency/corporate-management-reporting/departmental-performance-reports/2021-2022-supplementary-information-tables.html#a4.1
- Footnote 12
-
Health Canada. (2021). Supplementary Information Tables 2020-2021 Departmental Results Report: Health Canada - Canada.ca. Retrieved from https://www.canada.ca/en/health-canada/corporate/transparency/corporate-management-reporting/departmental-performance-reports/2020-2021-supplementary-information-tables.html#a4.1
- Footnote 13
-
Palepu A, Gadermann A, Hubley AM, Farrell S, Gogosis E, Aubry T, et al. (2013) Substance Use and Access to Health Care and Addiction Treatment among Homeless and Vulnerably Housed Persons in 3 Canadian Cities. PLoS ONE 8(10): e75133. Retrieved from https://doi.org/10.1371/journal.pone.0075133
- Footnote 14
-
Employment and Social Development Canada (2021). Addiction, Substance Use and Homelessness – An Analysis from the Nationally Coordinated Point-in-Time Counts. Retrieved from
https://www.canada.ca/content/dam/canada/employment-social-development/programs/homelessness/publications-bulletins/report-addiction/HPD-Report-AddictionsReport-20210121-VF.pdf - Footnote 15
-
Torchalla et al. (2011). Substance use and predictors of substance dependence in homeless women. Drug and Alcohol Dependence 118(2-3):173-9. DOI:10.1016/j.drugalcdep.2011.03.016. https://www.researchgate.net/publication/51055964_Substance_use_and_predictors_of_substance_dependence_in_homeless_women
- Footnote 16
-
Infrastructure Canada. (2022). Infrastructure Canada - Reaching Home: Canada's Homelessness Strategy Directives (infc.gc.ca). Retrieved from
https://secure.infc.gc.ca/homelessness-sans-abri/directives-eng.html - Footnote 17
-
Health Canada. (2021). Canadian Pain Task Force Report: March 2021. Retrieved from
https://www.canada.ca/en/health-canada/corporate/about-health-canada/public-engagement/external-advisory-bodies/canadian-pain-task-force/report-2021.html - Footnote 18
-
Nicholas Papadomanolakis-Pakis et al. (2021). Prescription opioid characteristics at initiation for non-cancer pain and risk of treated opioid use disorder: A population-based study", Drug and Alcohol Dependence, Volume 221, Retrieved from
https://www.sciencedirect.com/science/article/pii/S037687162100096X - Footnote 19
-
Rosenblum A, Marsch LA, Joseph H, Portenoy RK. Opioids and the treatment of chronic pain: controversies, current status, and future directions. Exp Clin Psychopharmacol. 2008;16(5):405-416. doi:10.1037/a0013628
- Footnote 20
-
Chang YP, Compton P. Management of chronic pain with chronic opioid therapy in patients with substance use disorders. Addict Sci Clin Pract. 2013 Dec 16;8(1):21. doi: 10.1186/1940-0640-8-2
- Footnote 21
-
Nadeau et al. (2021) Opioids and Chronic Pain: An Analytic Review of the Clinical Evidence. Frontiers in Pain Research. DOI=10.3389/fpain.2021.721357
- Footnote 22
-
Canada Gazette, Part 2, Volume 152, Number 9: Regulations Amending the Food and Drug Regulations (Opioids): SOR/2018-77
- Footnote 23
-
Health Canada. (2018). Submission of targeted risk management plans and follow-up commitments for prescription opioid-containing products - Guidance for industry – Summary. Retrieved from
https://www.canada.ca/en/health-canada/services/drugs-health-products/reports-publications/medeffect-canada/submission-targeted-rm-plans-commitments-prescription-opioid-containing-products-guidance-industry.html - Footnote 24
-
Health Canada. (2018). New regulations to provide better information for patients on the safe use of opioid medications. Retrieved from
https://www.canada.ca/en/health-canada/news/2018/05/new-regulations-to-provide-better-information-for-patients-on-the-safe-use-of-opioid-medications.html - Footnote 25
-
Statistics Canada. (2021). The Daily — Alcohol and drug use in Canada, 2019. Retrieved from:
https://www150.statcan.gc.ca/n1/daily-quotidien/211220/dq211220c-eng.htm - Footnote 26
-
Public Health Agency of Canada, Centre for Communicable Diseases and Infection Control (2021). Survey of the impact of COVID-19 on access to STBBI-related health services including harm reduction services among people who use drugs or alcohol in Canada. Retrieved from https://health-infobase.canada.ca/datalab/covid-19-stbbi-services.html
- Footnote 27
-
Public Health Agency of Canada, Centre for Communicable Diseases and Infection Control (2021). Survey of the impact of COVID-19 on access to STBBI-related health services including harm reduction services among people who use drugs or alcohol in Canada. Retrieved from https://health-infobase.canada.ca/datalab/covid-19-stbbi-services.html
- Footnote 28
-
Health Canada. (2021). Canadian Alcohol and Drugs Survey (CADS): 2019 detailed tables. Retrieved from
https://www.canada.ca/en/health-canada/services/canadian-alcohol-drugs-survey/2019-summary/detailed-tables.html - Footnote 29
-
Health Canada. (2021). Canadian Tobacco, Alcohol and Drugs (CTADS) Survey: 2017 detailed tables. Retrieved from
https://www.canada.ca/en/health-canada/services/canadian-alcohol-drugs-survey/2017-summary/2017-detailed-tables.html#t15 - Footnote 30
-
Health Canada has moved away from stigmatizing language such as "problematic substance use." While terminology updates are reflected throughout the evaluation report, previous documents and survey report summaries contain original language that is no longer in use.
- Footnote 31
-
Health Canada & Earnscliffe Strategy Group. (2022). Follow-up survey and qualitative research on opioid awareness, knowledge and behaviours for public education (2021): final report / prepared for Health Canada. Retrieved from
https://publications.gc.ca/collections/collection_2022/sc-hc/H21-313-2022-eng.pdf. - Footnote 32
-
Marteau, T., Kelly, M., & Hollands, G. (2015). Changing population behavior and reducing health disparities: Exploring the potential of "choice architecture" interventions,. Population Health: Behavioral and Social Science Insights,, (Section 2), 121.
https://doi.org/10.17863/CAM.69953 - Footnote 33
-
Canadian Substance Use Costs and Harms Scientific Working Group. (2020). Canadian Substance Use Costs and Harms 2015–2017. Ottawa: Canadian Centre on Substance Use and Addiction. Retrieved from
https://csuch.ca/publications/CSUCH-Canadian-Substance-Use-Costs-Harms-Report-2020-en.pdf - Footnote 34
-
Canadian Substance Use Costs and Harms Scientific Working Group. (2020). Canadian Substance Use Costs and Harms 2015–2017. Ottawa: Canadian Centre on Substance Use and Addiction. Retrieved from
https://csuch.ca/publications/CSUCH-Canadian-Substance-Use-Costs-Harms-Report-2020-en.pdf - Footnote 35
-
Canadian Substance Use Costs and Harms Scientific Working Group. (2023). Canadian substance use costs and harms 2007–2020. (Prepared by the Canadian Institute for Substance Use Research and the Canadian Centre on Substance Use and Addiction.) Ottawa, Ont.: Canadian Centre on Substance Use and Addiction. Retrieved from
https://csuch.ca/documents/reports/english/Canadian-Substance-Use-Costs-and-Harms-Report-2023-en.pdf - Footnote 36
-
Health Canada. (2019). What we heard: Strengthening Canada's Approach to Substance Use Issues. Government of Canada. Retrieved from
https://www.canada.ca/en/health-canada/services/substance-use/canadian-drugs-substances-strategy/strengthening-canada-approach-substance-use-issue.html. - Footnote 37
-
Ibid.
- Footnote 38
-
Canadian Centre on Substance Use and Addiction. (2022). Low-Risk Drinking Guidelines Project 2022. Retrieved from
https://ccsa.ca/canadas-guidance-alcohol-and-health - Footnote 39
-
Canadian Alcohol Policy Evaluation. (2023). CAPE 3.0: Federal Results. Retrieved from
https://www.uvic.ca/research/centres/cisur/assets/docs/cape/cape3/fed-results-en.pdf - Footnote 40
-
Health Canada. (2021). Emergence Treatment Fund. Retrieved from
https://www.canada.ca/en/health-canada/services/opioids/responding-canada-opioid-crisis/emergency-treatment-fund.html - Footnote 41
-
CIHR. (2022). Finding a new intervention for methamphetamine use disorder while tackling social issues and stigma. Retrieved from
https://cihr-irsc.gc.ca/e/53269.html - Footnote 42
-
CIHR. (2022). Alcohol Policy and Intervention Research. Retrieved from
https://www.canada.ca/en/institutes-health-research/news/2022/04/alcohol-policy-and-intervention-research.html - Footnote 43
-
Justice Canada. (2021). Evaluation of the Drug Treatment Court Funding Program. Retrieved from
https://www.justice.gc.ca/eng/rp-pr/cp-pm/eval/rep-rap/2021/drug-drogue/index.html - Footnote 44
-
Public Prosecution Service of Canada. (2020). Public Prosecution Service of Canada Departmental Results Report 2018-2019. Retrieved from
https://www.ppsc-sppc.gc.ca/eng/pub/drr-rrm/2018_2019/index.html - Footnote 45
-
Health Canada & Earnscliffe Strategy Group. (2022). Follow-up survey and qualitative research on opioid awareness, knowledge and behaviours for public education (2021): final report / prepared for Health Canada. Retrieved from
https://publications.gc.ca/collections/collection_2022/sc-hc/H21-313-2022-eng.pdf - Footnote 46
-
Health Canada. (2022). Safer supply: Prescribed medications as a safer alternative to toxic illegal drugs - Canada.ca. Retrieved from
https://www.canada.ca/en/health-canada/services/opioids/responding-canada-opioid-crisis/safer-supply.html - Footnote 47
-
Papamihali, K., Ng, J. & Buxton. J.A. (July 2020). Harm Reduction Strategies and Services Policy Indicators Report: Review of data to December 2019. Vancouver, BC. BC Centre for Disease Control (BCCDC). Retrieved from
https://towardtheheart.com/assets/uploads/1596137863wb4SEZpOWVX8K6xLRMEK8tRS8rsSIEpMuOCHk4a.pdf - Footnote 48
-
Health Canada. (2023). Naloxone - Canada.ca. Retrieved from
https://www.canada.ca/en/health-canada/services/opioids/naloxone.html - Footnote 49
-
Health Canada (2022). Supervised consumption explained: types of sites and services - Canada.ca. Retrieved from
https://www.canada.ca/en/health-canada/services/substance-use/supervised-consumption-sites/explained.html - Footnote 50
-
Leonieke C. van Boekel, Evelien P.M. Brouwers, Jaap van Weeghel, Henk F.L. Garretsen, Stigma among health professionals towards patients with substance use disorders and its consequences for health care delivery: Systematic review, Drug and Alcohol Dependence, Volume 131, Issues 1–2, 2013, Pages 23-35, ISSN 0376-8716,
https://doi.org/10.1016/j.drugalcdep.2013.02.018. - Footnote 51
-
Kelly JF, Westerhoff CM. Does it matter how we refer to individuals with substance-related conditions? A randomized study of 2 commonly used terms. Int J Drug Policy. 2010 May;21(3):202-7. doi: 10.1016/j.drugpo.2009.10.010. Epub 2009 Dec 14. PMID: 20005692.
- Footnote 52
-
Public Health Agency of Canada. (2020. Addressing stigma: towards a more inclusive health system. Retrieved from
https://www.canada.ca/en/public-health/corporate/publications/chief-public-health-officer-reports-state-public-health-canada/addressing-stigma-toward-more-inclusive-health-system - Footnote 53
-
Health Canada. (2022). Supplementary Information Tables 2021-2022 Departmental Results Report: Health Canada - Canada.ca. Retrieved from
https://www.canada.ca/en/health-canada/corporate/transparency/corporate-management-reporting/departmental-performance-reports/2021-2022-supplementary-information-tables.html#a4.1 - Footnote 54
-
Health Canada. (2021). Supplementary Information Tables 2020-2021 Departmental Results Report: Health Canada - Canada.ca. Retrieved from
https://www.canada.ca/en/health-canada/corporate/transparency/corporate-management-reporting/departmental-performance-reports/2020-2021-supplementary-information-tables.html#a4.1 - Footnote 55
-
Health Canada. (2020). Supplementary Information Tables 2019-2020 Departmental Results Report: Health Canada - Canada.ca. Retrieved from
https://www.canada.ca/en/health-canada/corporate/transparency/corporate-management-reporting/departmental-performance-reports/2019-2020-supplementary-information-tables.html#h.1 - Footnote 56
-
Health Canada. (2019). Health Canada 2018-2019 Departmental Results Report - Canada.ca. Retrieved from
https://www.canada.ca/en/health-canada/corporate/transparency/corporate-management-reporting/departmental-performance-reports/2018-2019-departmental-results-report.html - Footnote 57
-
Health Canada. (2019). Health Canada 2018-2019 Departmental Results Report - Canada.ca. Retrieved from
https://www.canada.ca/en/health-canada/corporate/transparency/corporate-management-reporting/departmental-performance-reports/2018-2019-departmental-results-report.html - Footnote 58
-
Health Canada & Earnscliffe Strategy Group. (2022). Follow-up survey and qualitative research on opioid awareness, knowledge and behaviours for public education (2021): final report / prepared for Health Canada. Retrieved from
https://publications.gc.ca/collections/collection_2022/sc-hc/H21-313-2022-eng.pdf - Footnote 59
-
Health Canada & Earnscliffe Strategy Group. (2019). Follow-up survey and qualitative research on opioid awareness, knowledge and behaviours for public education : final report / prepared for Health Canada. Retrieved from
https://publications.gc.ca/collections/collection_2019/sc-hc/H21-313-2019-eng.pdf - Footnote 60
-
Van Boekel LC, Brouwers EP, Van Weeghel J & Garretsen HF (2013). Stigma among health professionals toward patients with substance use disorders and its consequences for healthcare delivery: Systematic review. Drug and Alcohol Dependence, 2013;131(1):23-35.
- Footnote 61
-
Honouring Our Strengths: A Renewed Framework to Address Substance Use Issues Among First Nations People in Canada, 2011
- Footnote 62
-
Kennedy-Hendricks A, Barry CL, Gollust SE, Chisolm MS, McGinty EE. Social Stigma Toward Persons With Prescription Opioid Use Disorder: Associations With Public Support for Punitive and Public Health-Oriented Policies. Psychiatr Serv. 2017;May 1;68(5):462-469. doi: 10.1176/appi.ps.201600056. Epub 2017 Jan 3.
- Footnote 63
-
UK Drug Policy Commission. Getting Serious about Stigma: the Problem with Stigmatising Drug Users - An Overview. Retrieved from
https://www.ukdpc.org.uk/publication/getting-serious-about-stigma-problem-stigmatising-drug-users-summary. Published in 2010. Accessed September 23, 2019. - Footnote 64
-
Health Canada. (2021). Supplementary Information Tables 2020-2021 Departmental Results Report: Health Canada - Canada.ca. Retrieved from
https://www.canada.ca/en/health-canada/corporate/transparency/corporate-management-reporting/departmental-performance-reports/2020-2021-supplementary-information-tables.html#a4.1 - Footnote 65
-
Public Safety Canada (2018). 2018 Law Enforcement Roundtable on the Opioid Crisis. Retrieved from
https://www.publicsafety.gc.ca/cnt/rsrcs/pblctns/lw-nfrcmnt-rndtbl-pd-crss-2018/index-en.aspx - Footnote 66
-
Public Safety Canada (2022). Fourth Law Enforcement Roundtable on Drugs (publicsafety.gc.ca). Retrieved from
https://www.publicsafety.gc.ca/cnt/rsrcs/pblctns/2022-frth-lw-nfrcmnt-rndtbl-drgs/index-en.aspx - Footnote 67
-
Public Safety Canada (2022). Fifth Law Enforcement Roundtable on Drugs (publicsafety.gc.ca). Retrieved from
https://www.publicsafety.gc.ca/cnt/rsrcs/pblctns/2022-ffth-lw-nfrcmnt-rndtbl-drgs/index-en.aspx - Footnote 68
-
Public Health Agency of Canada (2020). Public Health Agency of Canada 2019-2020 Departmental Results Report - Canada.ca. Retrieved from
https://www.canada.ca/en/public-health/corporate/transparency/corporate-management-reporting/departmental-performance-reports/2019-202020.html - Footnote 69
-
Public Health Agency of Canada. (2020). A Primer to Reduce Substance Use Stigma in the Canadian Health System. Retrieved from
https://www.canada.ca/en/public-health/services/publications/healthy-living/primer-reduce-substance-use-stigma-health-system.html - Footnote 70
-
Public Safety Canada (2019). Departmental Results Report 2018-2019 (publicsafety.gc.ca). Retrieved from Departmental Results Report 2018-2019 (publicsafety.gc.ca)
- Footnote 71
-
Health Canada. (2021). Government of Canada announces $16.5 million to support harm reduction and people who use substances in British Columbia. Retrieved from
https://www.canada.ca/en/health-canada/news/2021/04/government-of-canada-announces-165-million-to-support-harm-reduction-and-people-who-use-substances-in-british-columbia.html - Footnote 72
-
Health Canada. (2022). Health Canada 2021–22 Departmental Results Report - Canada.ca. Retrieved from
https://www.canada.ca/en/health-canada/corporate/transparency/corporate-management-reporting/departmental-performance-reports/2021-2022-departmental-results-report.html - Footnote 73
-
Health Canada. (2021). Health Canada 2020–21 Departmental Results Report - Canada.ca. Retrieved from
https://www.canada.ca/content/dam/hc-sc/documents/corporate/transparency/corporate-management-reporting/departmental-performance-reports/2020-2021/2020-2021-departmental-results-report.pdf - Footnote 74
-
Health Canada (2018). Supplementary Information Tables 2017-18 Departmental Results Report Health Canada - Canada.ca. Retrieved from:
https://www.canada.ca/en/health-canada/corporate/transparency/corporate-management-reporting/departmental-performance-reports/2017-18-supplementary-information-tables/page-8-2017-18-supplementary-information-tables.html#a14 - Footnote 75
-
Health Canada (2022). Interactive map: Canada's response to the opioid crisis. Retrieved from
https://health.canada.ca/en/health-canada/services/drugs-medication/opioids/responding-canada-opioid-crisis/map - Footnote 76
-
Canadian Institutes of Health Research. (2021). What We Heard: End-of-Grant Knowledge Exchange Workshop Report: Evaluation of Interventions to Address the Opioid Crisis. Retrieved from
https://cihr-irsc.gc.ca/e/52687.html#1 - Footnote 78
-
Health Canada and Dale McMurchy Consulting. (2022). Early findings from safer supply pilot projects. Retrieved from
https://www.canada.ca/en/health-canada/services/opioids/responding-canada-opioid-crisis/safer-supply/early-findings-safer-supply-pilot-projects.html - Footnote 79
-
Canadian Institutes of Health Research. Research Net – Recherche Net: Funding Opportunity Details: Operating Grant : Evaluation of Harm Reduction Approaches to Address the Opioid Crisis in the Context of COVID-19 ARCHIVED. Retrieved from
https://www.researchnet-recherchenet.ca/rnr16/vwOpprtntyDtls.do?prog=3380&language=E - Footnote 80
-
Public Health Agency of Canada (2022). 2019–2020 Progress Report: Government of Canada Five-Year Action Plan on Sexually Transmitted and Blood-Borne Infections. Ottawa. Retrieved from
https://www.canada.ca/en/public-health/services/publications/diseases-conditions/2019-2020-progress-report-action-plan-sexually-transmitted-blood-borne-infections.html - Footnote 81
-
Public Health Agency of Canada (2020). Canadian Supervised Consumption Sites Statistics — 2017 to 2019 - Data Blog - Public Health Infobase | Public Health Agency of Canada. Retrieved from
https://health-infobase.canada.ca/datalab/supervised-consumption-sites-blog.html - Footnote 82
-
Federal, provincial, and territorial Special Advisory Committee on the Epidemic of Opioid Overdoses. Opioid- and Stimulant-related Harms in Canada. Ottawa: Public Health Agency of Canada; December 2022. Retrieved from
https://health-infobase.canada.ca/substance-related-harms/opioids-stimulants/ - Footnote 83
-
Health Canada. (2021). Supplementary Information Tables 2020-2021: Health Canada - Canada.ca. Retrieved from
https://www.canada.ca/en/health-canada/corporate/transparency/corporate-management-reporting/departmental-performance-reports/2020-2021-supplementary-information-tables.html#a4.2 - Footnote 84
-
Health Canada. (2021). Health Canada 2020–21 Departmental Results Report - Canada.ca. Retrieved from
https://www.canada.ca/content/dam/hc-sc/documents/corporate/transparency/corporate-management-reporting/departmental-performance-reports/2020-2021/2020-2021-departmental-results-report.pdf - Footnote 85
-
Health Canada. (2021). Supplementary Information Tables 2020-2021: Health Canada - Canada.ca. Retrieved from
https://www.canada.ca/en/health-canada/corporate/transparency/corporate-management-reporting/departmental-performance-reports/2020-21-supplementary-information-tables.html#a4.2 - Footnote 86
-
Canadian Institutes of Health Research. (2023). What We Heard Report: Operating Grant: Evaluation of Harm Reduction Approaches to Address the Opioid Crisis in the Context of COVID-19 – Supervised Consumption Sites Evaluation. Retrieved from
https://cihr-irsc.gc.ca/e/53469.html - Footnote 87
-
Health Canada (2022). Interactive map: Canada's response to the opioid crisis. Retrieved from
https://health.canada.ca/en/health-canada/services/drugs-medication/opioids/responding-canada-opioid-crisis/map.html - Footnote 88
-
Public Health Agency of Canada, Centre for Communicable Diseases and Infection Control (May 2021). Survey of the impact of COVID-19 on access to STBBI-related health services including harm reduction services among people who use drugs or alcohol in Canada. Retrieved from
https://health-infobase.canada.ca/datalab/covid-19-stbbi-services.html - Footnote 89
-
Public Health Agency of Canada, Centre for Communicable Diseases and Infection Control (May 2021). Survey of the impact of COVID-19 on access to STBBI-related health services including harm reduction services among people who use drugs or alcohol in Canada. Retrieved from
https://health-infobase.canada.ca/datalab/covid-19-stbbi-services.html - Footnote 90
-
Public Health Agency of Canada, Centre for Communicable Diseases and Infection Control (February 2021). Survey of the impact of COVID-19 on the ability of healthcare service providers to deliver STBBI prevention, testing and treatment including harm reduction services in Canada. Retrieved from
https://health-infobase.canada.ca/datalab/covid-19-impact-stbbi-services.html - Footnote 91
-
Health Canada. (2017). Royal Assent of Bill C-37 - An Act to amend the Controlled Drugs and Substances Act and to make related amendments to other Acts. Retrieved from
https://www.canada.ca/en/health-canada/news/2017/05/royal_assent_of_billc-37anacttoamendthecontrolleddrugsandsubstan.html - Footnote 92
-
Public Safety Canada. (2021). Fifth Law Enforcement Roundtable on Drugs September & October 2021 Meeting Summary. Retrieved from
https://www.publicsafety.gc.ca/cnt/rsrcs/pblctns/2022-ffth-lw-nfrcmnt-rndtbl-drgs/index-en.aspx - Footnote 93
-
CBSA. (2022). Canada Border Services Agency seizures. Retrieved from
https://www.cbsa-asfc.gc.ca/security-securite/seizure-saisie-eng.html - Footnote 94
-
Pursuant to s. 60.1(1) of the CDSA, "the Minister may, by order, add to Schedule V any item or portion of an item for a period of up to one year, or extend that period by up to another year, if the Minister has reasonable grounds to believe that it (a) poses a significant risk to public health or safety; or (b) may pose a risk to public health or safety and (i) is being imported into Canada with no legitimate purpose, or (ii) is being distributed in Canada with no legitimate purpose.
- Footnote 95
-
CBC. (2022). Why is Canada's illicit drug supply so deadly and what's being done about it? Retrieved from
https://www.cbc.ca/news/canada/canada-illicit-drug-supply-explainer-1.6361623 - Footnote 96
-
Public Safety Canada. (2021). Fifth Law Enforcement Roundtable on Drugs September & October 2021 Meeting Summary. Retrieved from
https://www.publicsafety.gc.ca/cnt/rsrcs/pblctns/2022-ffth-lw-nfrcmnt-rndtbl-drgs/index-en.aspx - Footnote 97
-
Health Canada. (2022). Health Canada Departmental Plan 2022-23 – Supplementary Information Table – CDSS. Retrieved from
https://www.canada.ca/en/health-canada/corporate/transparency/corporate-management-reporting/report-plans-priorities/2022-23-supplementary-information-tables.html#cdss - Footnote 98
-
Public Safety Canada. (2021). Fifth Law Enforcement Roundtable on Drugs September & October 2021 Meeting Summary. Retrieved from
https://www.publicsafety.gc.ca/cnt/rsrcs/pblctns/2022-ffth-lw-nfrcmnt-rndtbl-drgs/index-en.aspx - Footnote 99
-
This enactment amends the Criminal Code and the Controlled Drugs and Substances Act to, among other things, repeal certain mandatory minimum penalties, allow for a greater use of conditional sentences and establish diversion measures for simple drug possession offences.
- Footnote 100
-
Public Safety Canada. (2021). Fifth Law Enforcement Roundtable on Drugs September & October 2021 Meeting Summary. Retrieved from
https://www.publicsafety.gc.ca/cnt/rsrcs/pblctns/2022-ffth-lw-nfrcmnt-rndtbl-drgs/index-en.aspx - Footnote 101
-
Canada Border Services Agency. (2022). Canada Border Services Agency seizures (cbsa-asfc.gc.ca). Retrieved from
https://www.cbsa-asfc.gc.ca/security-securite/seizure-saisie-eng.html - Footnote 102
-
Royal Canadian Mounted Police. (2022). Opioid precursors CLEARed out. Retrieved from
https://bc-cb.rcmp-grc.gc.ca/ViewPage.action?siteNodeId=2087&languageId=1&contentId=75461 - Footnote 103
-
Public Prosecution Service of Canada. (2018). Public Prosecution Service of Canada Departmental Results Report 2017-18. Retrieved from:
https://www.ppsc-sppc.gc.ca/eng/pub/drr-rrm/2017_2018/index.html - Footnote 104
-
Public Safety Canada. (2021). Fifth Law Enforcement Roundtable on Drugs. Retrieved from
https://www.publicsafety.gc.ca/cnt/rsrcs/pblctns/2022-ffth-lw-nfrcmnt-rndtbl-drgs/index-en.aspx - Footnote 105
-
Commission of Inquiry into Money Laundering in British Columbia: Final Report, June 2022, Retrieved from
https://cullencommission.ca/ - Footnote 106
-
Health Canada (2020). Health Canada 2018-2019 Departmental Results Report. Retrieved from
https://www.canada.ca/en/health-canada/corporate/transparency/corporate-management-reporting/departmental-performance-reports/2018-2019-departmental-results-report.html - Footnote 107
-
Health Canada. (2019). Compliance and Enforcement Policy for Controlled Substances and Precursors (CS-POL-001). Retrieved from
https://www.canada.ca/en/health-canada/services/health-concerns/controlled-substances-precursor-chemicals/controlled-substances/compliance-monitoring/compliance-monitoring-controlled-substances/enforcement-policy.html - Footnote 108
-
Health Canada. (2019). Supplementary Information Tables 2018-2019 Departmental Results Report: Health Canada - Canada.ca. Retrieved from
https://www.canada.ca/en/health-canada/corporate/transparency/corporate-management-reporting/departmental-performance-reports/2018-19-supplementary-information-tables.html#a32 - Footnote 109
-
United Nations. (2018). Report on the Sixty-first session of the United Nations Commission on Narcotic Drugs, Resolution 61/11, page 28. Retrieved from
https://www.unodc.org/unodc/en/commissions/CND/session/61_Session_2018/session-61-of-the-commission-on-narcotic-drugs.html - Footnote 110
-
Health Canada. (2020). Health Canada 2019–2020 Departmental Results Report - Canada.ca. Retrieved from
https://www.canada.ca/en/health-canada/corporate/transparency/corporate-management-reporting/departmental-performance-reports/2019-2020-departmental-results-report.html - Footnote 111
-
Health Canada (2023). Health Canada 2021-2022 Department Results Report – Canada.ca. Retrieved from
https://www.canada.ca/en/health-canada/corporate/transparency/corporate-management-reporting/departmental-performance-reports/2021-22-supplementary-information-tables.html#a4.3 - Footnote 112
-
United Nations. (2022). Report on the 64th session of the United Nations Commission on Narcotic Drugs, Resolution 64/5, page 21. Retrieved from:
https://www.unodc.org/unodc/en/commissions/CND/session/64_Session_2021/documentation.html - Footnote 113
-
Health Canada & Earnscliffe Strategy Group. (2022). Follow-up survey and qualitative research on opioid awareness, knowledge and behaviours for public education (2021): final report / prepared for Health Canada. Retrieved from
https://publications.gc.ca/collections/collection_2022/sc-hc/H21-313-2022-eng.pdf - Footnote 114
-
Health Canada. (2022). Health Canada 2021–22 Departmental Results Report - Canada.ca. Retrieved from
https://www.canada.ca/en/health-canada/corporate/transparency/corporate-management-reporting/departmental-performance-reports/2021-2022-departmental-results-report.html - Footnote 115
-
Public Health Agency of Canada, Centre for Communicable Diseases and Infection Control (2021). Survey of the impact of COVID-19 on access to STBBI-related health services including harm reduction services among people who use drugs or alcohol in Canada. Retrieved from
https://health-infobase.canada.ca/datalab/covid-19-stbbi-services.htmlb - Footnote 116
-
Health Canada. (2021). Canadian Alcohol and Drugs Survey (CADS): summary of results for 2019 - Canada.ca. Retrieved from
https://www.canada.ca/en/health-canada/services/canadian-alcohol-drugs-survey/2019-summary.html - Footnote 117
-
Public Health Infobase. (2021). Canadian Postsecondary Education Alcohol and Drug Use Survey, 2019/2020. Retrieved from
https://health-infobase.canada.ca/alcohol/cpads/data-tables.html - Footnote 118
-
Health Canada. (2023). Summary of results for the Canadian Student Tobacco, Alcohol and Drugs Survey 2021-22. Retrieved from
https://www.canada.ca/en/health-canada/services/canadian-student-tobacco-alcohol-drugs-survey/2021-2022-summary.html - Footnote 119
-
Public Health Agency of Canada, Centre for Communicable Diseases and Infection Control (2021). Survey of the impact of COVID-19 on access to STBBI-related health services including harm reduction services among people who use drugs or alcohol in Canada. Retrieved from
https://health-infobase.canada.ca/datalab/covid-19-stbbi-services.html - Footnote 120
-
Health Canada. (2021). Health Canada 2020–21 Departmental Results Report - Canada.ca (page 49). Retrieved from
https://www.canada.ca/content/dam/hc-sc/documents/corporate/transparency/corporate-management-reporting/departmental-performance-reports/2020-2021/2020-2021-departmental-results-report.pdf - Footnote 121
-
Public Health Agency of Canada, Centre for Communicable Diseases and Infection Control (2021). Survey of the impact of COVID-19 on access to STBBI-related health services including harm reduction services among people who use drugs or alcohol in Canada. Retrieved from
https://health-infobase.canada.ca/datalab/covid-19-stbbi-services.html - Footnote 122
-
Chief Public Health Officer of Canada, Health of People in Canada Dashboard. Retrieved from:
https://health-infobase.canada.ca/health-of-people-in-canada-dashboard/life-expectancy.html - Footnote 123
-
Federal, provincial, and territorial Special Advisory Committee on the Epidemic of Opioid Overdoses. Opioid- and Stimulant-related Harms in Canada. Ottawa: Public Health Agency of Canada; December 2022. Retrieved from
https://health-infobase.canada.ca/substance-related-harms/opioids-stimulants/ - Footnote 124
-
Health Canada. (2022). Health Canada 2021–22 Departmental Results Report - Canada.ca. Retrieved from
https://www.canada.ca/en/health-canada/corporate/transparency/corporate-management-reporting/departmental-performance-reports/2021-2022-departmental-results-report.html - Footnote 125
-
Health Canada. (2022). Health Canada 2021–22 Departmental Results Report - Canada.ca. Retrieved from
https://www.canada.ca/en/health-canada/corporate/transparency/corporate-management-reporting/departmental-performance-reports/2021-2022-departmental-results-report.html - Footnote 126
-
Public Safety Canada (2022). Fourth Law Enforcement Roundtable on Drugs (publicsafety.gc.ca). Retrieved from
https://www.publicsafety.gc.ca/cnt/rsrcs/pblctns/2022-frth-lw-nfrcmnt-rndtbl-drgs/index-en.aspx - Footnote 127
-
Health Canada. (2022). Health Canada 2021–22 Departmental Results Report - Canada.ca. Retrieved from
https://www.canada.ca/en/health-canada/corporate/transparency/corporate-management-reporting/departmental-performance-reports/2021-2022-departmental-results-report.html - Footnote 128
-
Canadian Institutes of Health Research. (2023). Research in Substance Use: Publications. Retrieved from
https://cihr-irsc.gc.ca/e/52357.html - Footnote 129
-
Health Canada. (2022). Early findings from safer supply pilot projects. Retrieved from
https://www.canada.ca/en/health-canada/services/opioids/responding-canada-opioid-crisis/safer-supply/early-findings-safer-supply-pilot-projects.html - Footnote 130
-
Canadian Institute for Health Research. (2022). Funding Decision Database: A proposal to evaluate safer supply pilot programs in Canada. Retrieved from
https://webapps.cihr-irsc.gc.ca/decisions/p/project_details.html?applId=441626&lang=en - Footnote 131
-
Health Canada. (2023). Health Infobase: Opioid- and Stimulant-related Harms in Canada Published. Retrieved from:
https://health-infobase.canada.ca/substance-related-harms/opioids-stimulants - Footnote 132
-
Health Canada. (2021). Canadian Alcohol and Drugs Survey. Retrieved from
https://www.canada.ca/en/health-canada/services/canadian-alcohol-drugs-survey.html - Footnote 133
-
Health Canada. (2023). Canadian Student Tobacco, Alcohol and Drugs Survey. Retrieved from
https://www.canada.ca/en/health-canada/services/canadian-student-tobacco-alcohol-drugs-survey.html - Footnote 134
-
Health Canada. (2023). Drug Analysis Service Reports. Retrieved from
https://www.canada.ca/en/health-canada/services/health-concerns/controlled-substances-precursor-chemicals/drug-analysis-service.html#drug - Footnote 135
-
Public Health Agency of Canada. (2022). Canadian Hospitals Injury Reporting and Prevention Program. Retrieved from
https://www.canada.ca/en/public-health/services/injury-prevention/canadian-hospitals-injury-reporting-prevention-program.html - Footnote 136
-
Statistics Canada. (2021). Data and Research on Opioids. Retrieved from
https://www.statcan.gc.ca/search/results/site-search?q=%2522opioids%2522%2520OR%2520%2522substance%2520use%2522%2520OR%2520%2522overdose%2522&fq=stclac:2&sort=score%20desc&rows=25&page=1 - Footnote 137
-
Canadian Institute for Health Information. (2023). Indicator library: Mental Health and substance use. Retrieved from
https://www.cihi.ca/en/access-data-and-reports/indicator-library?keyword=&type_of_care=All&place_of_care=All&population_group=All&health_conditions_outcomes=903&health_care_quality=All&health_system_overview=All&hsp_framework=All&sort_by=title&items_per_page=20 - Footnote 138
-
Statistics Canada. (2022). Wastewater analysis suggests that use of particular opioid pain medications decreased during the COVID-19 pandemic in 2020. Retrieved from
https://www150.statcan.gc.ca/n1/daily-quotidien/220309/dq220309c-eng.htm - Footnote 139
-
Statistics Canada. (2021). Wastewater analysis suggests that consumption of fentanyl, cannabis and methamphetamine increased in the early pandemic period. Retrieved from
https://www150.statcan.gc.ca/n1/daily-quotidien/210726/dq210726a-eng.htm - Footnote 140
-
Health Canada. (2022). Canadian Pain Task Force. Retrieved from
https://www.canada.ca/en/health-canada/corporate/about-health-canada/public-engagement/external-advisory-bodies/canadian-pain-task-force.html - Footnote 141
-
Health Canada. (2023). Expert Task Force on Substance Use. Retrieved from
https://www.canada.ca/en/health-canada/corporate/about-health-canada/public-engagement/external-advisory-bodies/expert-task-force-substance-use.html - Footnote 142
-
Health Canada. (2022). Expert Advisory Group on Safer Supply. Retrieved from
https://www.canada.ca/en/health-canada/corporate/about-health-canada/public-engagement/external-advisory-bodies/expert-advisory-group-safer-supply.html - Footnote 143
-
Office of the Prime Minister of Canada. Minister of Mental Health and Addictions and Associate Minister of Health Mandate Letter. Retrieved from
https://pm.gc.ca/en/mandate-letters/2021/12/16/minister-mental-health-and-addictions-and-associate-minister-health - Footnote 144
-
United Nations Department of Economic and Social Affairs. (n.d.) Goal 3: Ensure health lives and promote well-being for all at all ages. Retrieved from
https://sdgs.un.org/goals/goal3 - Footnote 145
-
This logic model is a draft from April 9, 2019. The CDSS is continuing to refine its logic model and performance measurement strategy. However, as a retrospective exercise, the evaluation used this latest available logic model to assess achievement of outcomes. Additionally, Health Canada has moved away from stigmatizing language such as "problematic substance use." While terminology updates are reflected throughout the evaluation report, this logic model contains original language that is no longer in use.
Page details
- Date modified: