Canada-British Columbia Agreement to Work Together to Improve Health Care for Canadians (2023-24 to 2025-26)
Tables of contents
- Funding agreement
- Annex 1 – Common statement of principles on shared health priorities
- Annex 2 – Shared pan-Canadian interoperability roadmap
- Annex 3 – Headline common indicators
- Annex 4 – Action plan
Funding agreement
(the "Agreement")
Between:
His Majesty the King in Right of Canada (hereinafter referred to as "Canada" or "Government of Canada") as represented by the Minister of Health and the Minister of Mental Health and Addictions and Associate Minister of Health (herein referred to as "the federal Ministers")
- and -
His Majesty the King in Right of the province of British Columbia (hereinafter referred to as "British Columbia" or "Government of British Columbia") as represented by the Minister of Health and the Minister of Mental Health and Addictions (herein referred to as "the provincial Ministers")
Referred to collectively as the "Parties", and individually as a "Party"
Preamble
Whereas, on March 1, 2023, Canada and British Columbia announced an overarching agreement in principle on Working Together to Improve Health Care for Canadians, supported by almost $200 billion over ten years in federal funding, including $46.2 billion in new funding to provinces and territories;
Whereas, Canada has also announced a 5 per cent Canada Health Transfer (CHT) guarantee for the next five years, starting in 2023-24, which will be provided through annual top-up payments as required. This is projected to provide approximately an additional $17 billion over 10 years in new support. The last top-up payment will be rolled into the CHT base at the end of the five years to ensure a permanent funding increase, providing certainty and sustainability to provinces and territories;
Whereas, Working Together to Improve Health Care for Canadians includes a federal commitment of $25 billion in bilateral funding to provinces and territories over ten years focused on four shared health priorities:
- expanding access to family health services, including in rural and remote areas;
- supporting our health workers and reducing backlogs;
- improving access to quality mental health, substance use, and addictions services; and
- modernizing health systems with health data and digital tools.
Whereas, in the area of mental health, substance use, and addictions services, Working Together to Improve Health Care for Canadians also includes a commitment by Canada and British Columbia to continue to work to support collaboration on the Common Statement of Principles on Shared Health Priorities (hereinafter referred to as the "Common Statement", attached hereto as Annex 1), supported by the federal Budget 2017 investment of $5 billion over ten years;
Whereas, British Columbia has the primary responsibility for delivering health care services to its residents and supports diversity, equity, and the needs of underserved and/or disadvantaged populations, including, but not limited to First Nations, Inuit and Métis, official language minority communities, rural and remote communities, children, racialized communities (including Black Canadians), and LGBTIQA2S+;
Whereas, Canada authorized the federal Ministers to enter into agreements with the provinces and territories, for the purpose of identifying activities that provinces and territories will undertake in respect of the four shared health priorities, and for funding in this Agreement associated with the federal investment for mental health, substance use, and addictions services consistent with the Common Statement (and menu of actions outlined in Annex 1);
Whereas, the Lieutenant Governor in Counsel authorized the provincial Ministers under the Ministry of Intergovernmental Relations Act to enter into agreements with the Government of Canada under which Canada undertakes to provide funding toward costs incurred by the Government of British Columbia associated with the federal investment for four shared health priorities, and mental health, substance use and addictions services consistent with the Common Statement; and
Now therefore, this Agreement sets out the terms between Canada and British Columbia as follows:
1.0 Key principles and collaboration
The key principles and commitment to collaboration agreed to in Working Together to Improve Health Care for Canadians are outlined below.
1.1 Canada and British Columbia acknowledge that this Agreement will mutually respect each government's jurisdiction, and be underpinned by key principles, including:
- A shared responsibility to uphold the Canada Health Act that strengthens our public health care system;
- Principles agreed to in the Common Statement (outlined in Annex 1);
- Reconciliation with Indigenous Peoples, recognizing their right to fair and equal access to quality and culturally safe health services free from racism and discrimination anywhere in Canada, including through seamless service delivery across jurisdictions and meaningful engagement and work with Indigenous organizations and governments; and
- Equity of access for under-served groups and individuals, including those in official language minority communities.
1.2 Canada and British Columbia acknowledge the importance of supporting health data infrastructure, data collection and public reporting, and will work together to improve the collection, sharing and use of de-identified health information, respecting federal/provincial/territorial privacy legislation, to improve transparency on results and to help manage public health emergencies, and to ensure Canadians can access their own health information and benefit from it being shared between health workers across health settings. This includes:
- collecting and securely sharing high-quality, comparable information needed to improve services to Canadians, including disaggregated data on key common health indicators with the Canadian Institute for Health Information (CIHI);
- adopting common interoperability standards (both technical exchange and content of data), including the Shared pan-Canadian Interoperability Roadmap (outlined in Annex 2), to improve Canadians' access to their health information in a usable digital format and support the exchange and analysis of health data within and across Canada's health systems in a way that protects Canadians' privacy and ensures the ethical use of data to improve the health and lives of people;
- work to align provincial and territorial policies and legislative frameworks where necessary and appropriate to support secure patient access to health information, and stewardship of health information to support the public good, including improving care quality, patient safety, privacy protection, system governance and oversight, planning and research;
- promoting health information as a public good by working with federal-provincial-territorial Ministers of Health to review and confirm overarching principles, which would affirm Canadians' ability to access their health information and have it follow them across all points of care. The existing draft Health Data Charter, as outlined in the Pan-Canadian Health Data Strategy would serve as the starting point for the discussion of these principles; and
- collecting and sharing available public health data (e.g., vaccination data, testing data) with the Public Health Agency of Canada to support Canada's preparedness and response to public health events, building on commitments made as part of the Safe Restart Agreements.
1.3 Canada and British Columbia acknowledge they will work with other provinces and territories to streamline foreign credential recognition for internationally-educated health professionals, and to advance labour mobility, starting with multi-jurisdictional recognition of health professional licences.
1.4 Canada and British Columbia acknowledge a mutual intent to engage in a two-phased formal review process:
- Phase 1: This review will be done in 2026 by a joint committee of Federal, Provincial, and Territorial health and finance officials to assess results and determine next steps for bilateral agreements related to improvements to home and community care, mental health, substance use, and addiction services associated with the Common Statement and long-term care; and
- Phase 2: A formal five-year review of the healthcare plan outlined on February 7, 2023, recognizing the importance of long-term sustainability for provincial-territorial health systems. This review would consist of an assessment of both the bilateral agreements (herein) and the CHT investments (not included as part of this bilateral agreement). The review will be done by a joint committee of Federal, Provincial, and Territorial health and finance officials, commencing by March 31, 2027, and concluded by December 31, 2027, to consider results achieved thus far in the four shared health priority areas and will include:
- an assessment of progress-to-date on public reporting to Canadians using the common indicators;
- sharing of de-identified health information, and other health data commitments; and
- current and forward-looking Federal, Provincial, and Territorial investments to support this plan.
2.0 Objectives
2.1 Canada and British Columbia agree that, with financial support from Canada, British Columbia will continue to build and enhance health care systems towards achieving some or all of the objectives of:
- timely access to high-quality family health services, including in rural and remote areas;
- a sustainable, efficient and resilient health workforce that provides Canadians timely access to high-quality, effective, and safe health services;
- access to timely, equitable, and quality mental health, substance use, and addictions services to support Canadians' well-being; and
- access to a patient's own electronic health information that is shared between the health professionals they consult to improve safety and quality of care, and which informs Canadians on how the system is working.
2.2 Canada and British Columbia agree that, with Budget 2017 financial support from Canada outlined in 5.2.2, British Columbia will continue to work to improve access to mental health, substance use, and addictions services consistent with the Common Statement (and menu of actions outlined in Annex 1).
3.0 Action plan
3.1 British Columbia set out in their Action Plan (attached as Annex 4) how the federal investment under this Agreement will be used, as well as details on targets and timeframes based on common headline indicators in priority areas where federal funds will be invested, as well as jurisdiction-specific indicators, for each of the initiatives.
3.2 British Columbia will invest federal funding as part of the 2017 commitment for mental health, substance use, and addictions services provided through this Agreement in alignment with the menu of actions listed in the Common Statement.
3.3 British Columbia will invest federal funding in some or all of the four shared health priority areas, without displacing existing planned spending in those areas.
3.4 In developing initiatives under this Agreement, British Columbia agrees to implement measures that also respond to the needs of underserved and/or disadvantaged populations, including, but not limited to First Nations, Inuit and Métis, official language minority communities, rural and remote communities, children, racialized communities (including Black Canadians), and LGBTIQA2S+.
3.5 British Columbia's approach to achieving objectives is set out in their three-year Action Plan (2023-24 to 2025-26), as set out in Annex 4.
4.0 Term of agreement
4.1 This Agreement comes into effect upon the date of the last signature of the Parties and will remain in effect until March 31, 2026 ("the Term"), unless terminated in accordance with section 11 of this Agreement. Funding provided under this Agreement will cover the period April 1, 2023 to March 31, 2026.
4.2 Renewal of Bilateral Agreements
4.2.1 Upon signing renewed bilateral agreements, British Columbia will have access to the remainder of its share of the federal funding, subject to appropriation by Parliament, for:
- 2026-27, the allocation based on the federal commitment in Budget 2017 of $5 billion over ten years for mental health, substance use and addiction services; and
- 2026-27 to 2032-33, the allocation based on the federal commitment in Budget 2023 of $25 billion over ten years to support the Working Together to Improve Health Care for Canadians plan.
5.0 Financial provisions
5.1 The funding provided under this Agreement is in addition to and not in lieu of those that Canada currently provides under the CHT to support delivering health care services within the province.
5.2 Allocation to British Columbia
5.2.1 In this Agreement, "Fiscal Year" means the period commencing on April 1 of any calendar year and terminating on March 31 of the immediately following calendar year.
5.2.2 Canada has designated the following maximum amounts to be transferred in total to all provinces and territories under this initiative based on the allocation method outlined in subsection 5.2.3 for the Term of this Agreement.
Working Together to Improve Health Care for Canadians
- $2.5 billion for the Fiscal Year beginning on April 1, 2023
- $2.5 billion for the Fiscal Year beginning on April 1, 2024
- $2.5 billion for the Fiscal Year beginning on April 1, 2025
Budget 2017 Mental Health, Substance Use, and Addictions Services
- $600 million for the Fiscal Year beginning on April 1, 2023
- $600 million for the Fiscal Year beginning on April 1, 2024
- $600 million for the Fiscal Year beginning on April 1, 2025
5.2.3 Allocation Method
- For the funding associated with Working Together to Improve Health Care for Canadians, annual funding will be allocated to provinces and territories on base ($5,000,000 if population is less than 100,000; $20,000,000 if population is between 100,000 and 500,000; and $50,000,000 if population is greater than 500,000) plus per capita basis. The final total amount to be paid to each jurisdiction will be calculated using the following formula: B + (F - ((N * 5,000,000) + (O * 20,000,000) + (S * 50,000,000)) x (K / L), where:
B is the base amount allocated to each province or territory based on population ($5,000,000 if population is less than 100,000; $20,000,000 if population is between 100,000 and 500,000; and $50,000,000 if population is greater than 500,000), as determined using annual population estimates on July 1st from Statistics Canada;
F is the total annual funding amount available outlined under this program;
N is the number of provinces and territories with a population less than 100,000, as determined using annual population estimates on July 1st from Statistics Canada;
O is the number of provinces and territories with a population between 100,000 and 500,000, as determined using annual population estimates on July 1st from Statistics Canada;
S is the number of provinces and territories with a population greater than 500,000, as determined using annual population estimates on July 1st from Statistics Canada;
K is the total population of British Columbia, as determined using annual population estimates on July 1st from Statistics Canada; and
L is the total population of Canada, as determined using annual population estimates on July 1st from Statistics Canada.
- For funds associated with Budget 2017 Mental Health, Substance Use, and Addictions Services, annual funding will be allocated to provinces and territories on a per capita basis. The per capita funding for each Fiscal Year, is calculated using the following formula: F x K/L, where:
F is the annual total funding amount available under this program;
K is the total population of British Columbia, as determined using the annual population estimates on July 1st from Statistics Canada; and
L is the total population of Canada, as determined using the annual population estimates on July 1st from Statistics Canada.
5.2.4 Subject to annual adjustment based on the formulas described in section 5.2.3, British Columbia estimated share of the amounts will be:
| Fiscal Year | Working Together to Improve Health Care for Canadians Estimated amount to be paid to British Columbia Footnote a (subject to annual adjustment) | Budget 2017 Mental Health, Substance Use, and Addictions Services Estimated amount to be paid to British Columbia Footnote a (subject to annual adjustment) |
|---|---|---|
| 2023-2024 | $325,330,000 | $81,980,000 |
| 2024-2025 | $325,330,000 | $81,980,000 |
| 2025-2026 | $325,330,000 | $ 81,980,000 |
|
||
5.3 Payment
5.3.1 Funding provided by Canada will be paid in semi-annual installments as follows:
- In 2023-2024, the first installment will be paid within approximately 30 business days of execution of this Agreement by the Parties. The second installment will be paid on or about November 15.
- Starting in 2024-2025, the first installment will be paid on or about April 15 of each Fiscal Year and the second installment will be paid on or about November 15 of each Fiscal Year.
- The first installment will be equal to 50% of the notional amount set out in section 5.2.4 as adjusted by section 5.2.3.
- The second installment will be equal to the balance of funding provided by Canada for the Fiscal Year as determined under sections 5.2.3 and 5.2.4.
- Canada will notify British Columbia prior to the first payment of each Fiscal Year, of their notional amount. The notional amount will be based on the Statistics Canada quarterly preliminary population estimates on July 1 of the preceding Fiscal Year. Prior to the second payment, Canada will notify British Columbia of the amount of the second installment as determined under sections 5.2.3 and 5.2.4.
- Canada shall withhold payments if British Columbia has failed to provide reporting in accordance with 7.1.
- Canada shall withhold the second payment in 2023-24 if British Columbia has failed to satisfy all reporting requirements associated with the preceding Canada – British Columbia Home and Community Care and Mental Health and Addictions Services Funding Agreement 2022-23, specifically to:
- continue to participate in a Federal-Provincial-Territorial process to improve reporting on and provide data to CIHI for the 6 common indicators to measure pan-Canadian progress on improving access to mental health, substance use, and addictions services; and
- submit an annual financial statement, with attestation from province's Ministry of Health's Executive Financial Officer, of funding received the preceding Fiscal Year from Canada for mental health and addiction services under the Canada – British Columbia Home and Community Care and Mental Health and Addictions Services Funding Agreement 2022-23 compared against the Expenditure Plan, and noting any variances, between actual expenditures and the Expenditure Plan.
- The sum of both installments constitutes a final payment and is not subject to any further payment once the second installment has been paid.
- Payment of Canada's funding for this Agreement is subject to an annual appropriation by the Parliament of Canada for this purpose.
5.4 Retaining funds
5.4.1 For Fiscal Years 2023-24 through 2024-25, upon request, British Columbia may retain and carry forward to the next Fiscal Year up to 10 percent of funding that is in excess of the amount of the eligible costs actually incurred in a Fiscal Year and use the amount carried forward for expenditures on eligible areas of investment. Any request to retain and carry forward an amount exceeding 10 percent will be subject to discussion and mutual agreement in writing by their designated officials, at the Assistant Deputy Minister level (herein referred to as "Designated Officials"), and is subject to monitoring and reporting to Canada on the management and spending of the funds carried forward on a quarterly basis.
5.4.2 Any amount carried forward from one Fiscal Year to the next under this subsection is supplementary to the maximum amount payable to British Columbia under subsection 5.2.4 of this Agreement in the next Fiscal Year.
5.4.3 Upon request, British Columbia may retain and carry forward up to 10 percent of funding provided in the last Fiscal Year of this Agreement for eligible areas of investment, to be noted in the new agreement and subject to the terms and conditions of that new agreement. The new Action Plan will provide details on how any retained funds carried forward will be expended. Any request by British Columbia to retain and carry forward an amount exceeding 10 percent will be subject to discussion and mutual agreement in writing by their Designated Officials, and is subject to monitoring and reporting to Canada on the management and spending of the funds carried forward on a quarterly basis.
5.5 Repayment of overpayment
5.5.1. In the event payments made exceed the amount to which British Columbia is entitled under this Agreement, the amount of the excess is a debt due to Canada and, unless otherwise agreed to in writing by the Parties, British Columbia shall repay the amount within sixty (60) calendar days of written notice from Canada.
5.6 Use of funds
5.6.1. The Parties agree that funds provided under this Agreement will only be used by British Columbia in accordance with the initiatives outlined in Annex 4.
5.7 Eligible expenditures
5.7.1. Eligible expenditures under this Agreement are the following:
- data development and collection to support reporting;
- information technology and health information infrastructure;
- capital and operating funding;
- salaries and benefits;
- training, professional development; and
- information and communications material related to programs.
6.0 Performance measurement
6.1 British Columbia agrees to designate an official or official(s), for the duration of this Agreement to participate in a CIHI led Federal-Provincial-Territorial indicator process to:
- Refine the eight common headline indicators (outlined in Annex 3);
- Work to identify additional common indicators that are mutually agreed upon, including indicators focused on the health of Indigenous populations with acknowledgement of the role for Indigenous partners in this work;
- Improve reporting on common indicators to measure pan-Canadian progress on improving access to mental health, substance use, and addictions services, associated with the commitment in the Common Statement; and
- Share available disaggregated data with CIHI and work with CIHI to improve availability of disaggregated data for existing and new common indicators to enable reporting on progress for underserved and/or disadvantaged populations including, but not limited to, Indigenous peoples, First Nations, Inuit, Métis, official language minority communities, rural and remote communities, children, racialized communities (including Black Canadians), and LGBTIQA2S+.
7.0 Reporting to Canadians
7.1 Funding conditions and reporting
7.1.1 By no later than October 1, in each fiscal year, with respect of the previous Fiscal Year, British Columbia agrees to:
- Provide data and information annually to CIHI related to the new headline indicators, additional common indicators, and the mental health, substance use, and addictions services indicators identified as part of commitment made in the Common Statement.
- Beginning in Fiscal Year 2024-25, report annually and publicly in an integrated manner to residents of British Columbia on progress made on targets outlined in Annex 4 (Action Plan) for headline indicators in the priority area(s) where federal funds are to be invested, and on jurisdiction-specific indicators for each of the initiatives tailored to their jurisdiction's needs and circumstances.
- Beginning in Fiscal Year 2024-25, provide to Canada an annual financial statement, with attestation from province's Ministry of Health's Executive Financial Officer, of funding received the preceding Fiscal Year from Canada under this Agreement or the Previous Agreement compared against the Action Plan, and noting any variances, between actual expenditures and the Action Plan:
- The revenue section of the statement shall show the amount received from Canada under this Agreement during the Fiscal Year;
- The total amount of funding used for each of the shared health priority areas that are supported by the federal funds;
- If applicable, the amount of any funding carried forward under section 5.4; and
- If applicable, the amount of overpayment that is to be repaid to Canada under section 5.5.
7.1.2 British Columbia will provide quarterly reporting to Canada on the management and spending of the funds retained to the next Fiscal Year.
7.2 Audit
7.2.1 British Columbia will ensure that expenditure information presented in the annual financial statement is, in accordance with British Columbia's standard accounting practices, complete and accurate.
7.3 Evaluation
7.3.1 Responsibility for evaluation of programs rests with British Columbia in accordance with its own evaluation policies and practices.
8.0 Communications
8.1 The Parties agree on the importance of communicating with citizens about the objectives of this Agreement in an open, transparent, effective and proactive manner through appropriate public information activities.
8.2 Each Party will receive the appropriate credit and visibility when investments financed through funds granted under this Agreement are announced to the public.
8.3 In the spirit of transparency and open government, Canada will make this Agreement, including any amendments, publicly available on a Government of Canada website.
8.4 British Columbia will make publicly available, clearly identified on a Government of British Columbia website, this agreement, including any amendments.
8.5 Canada, with prior notice to British Columbia, may incorporate all or any part of the data and information in 7.1, or any part of evaluation and audit reports made public by British Columbia into any report that Canada may prepare for its own purposes, including any reports to the Parliament of Canada or reports that may be made public.
8.6 Canada reserves the right to conduct public communications, announcements, events, outreach and promotional activities about the Common Statement and this Agreement. Canada agrees to give British Columbia 10 days advance notice and advance copies of public communications related to the Common Statement, this Agreement, and results of the investments of this Agreement.
8.7 British Columbia reserves the right to conduct public communications, announcements, events, outreach and promotional activities about the Common Statement and this Agreement. British Columbia agrees to give Canada 10 days advance notice and advance copies of public communications related to the Common Statement, this Agreement, and results of the investments of this Agreement.
8.8 Canada and British Columbia agree to participate in a joint announcement upon signing of this Agreement.
8.9 Canada and British Columbia agree to work together to identify mutually agreeable opportunities for joint announcements relating to programs funded under this Agreement.
9.0 Dispute resolution
9.1 The Parties are committed to working together and avoiding disputes through government-to-government information exchange, advance notice, early consultation, and discussion, clarification, and resolution of issues, as they arise.
9.2 If at any time a Party is of the opinion that the other Party has failed to comply with any of its obligations or undertakings under this Agreement or is in breach of any term or condition of the Agreement, that Party may notify the other Party in writing of the failure or breach. Upon such notice, the Parties will endeavour to resolve the issue in dispute bilaterally through their Designated Officials.
9.3 If a dispute cannot be resolved by Designated Officials, then the dispute will be referred to the Deputy Ministers of Canada and British Columbia responsible for health, and if it cannot be resolved by them, then the federal Minister(s) and the provincial Minister(s) shall endeavour to resolve the dispute.
10.0 Amendments to the agreement
10.1 The main text of this Agreement may be amended at any time by mutual consent of the Parties. Any amendments shall be in writing and signed, in the case of Canada, by the federal Minister(s), and in the case of British Columbia, by the provincial Minister(s).
10.2 Annex 4 may be amended at any time by mutual consent of the Parties. Any amendments to Annex 4 shall be in writing and signed by each Party's Designated Official.
11.0 Termination
11.1 Either Party may terminate this Agreement at any time if the terms are not respected by giving at least 6 months written notice of intention to terminate.
11.2 As of the effective date of termination of this Agreement, Canada shall have no obligation to make any further payments.
11.3 Sections 1.0, and 8.0 of this Agreement survive for the period of the 10-year Working Together to Improve Health Care for Canadians plan.
11.4 Sections 5.4 and 7.0 of this Agreement survive the termination or expiration of this Agreement until reporting obligations are completed.
12.0 Notice
12.1 Any notice, information, or document provided for under this Agreement will be effectively given if delivered or sent by letter, email, postage or other charges prepaid. Any communication that is delivered will be deemed to have been received in delivery; and, except in periods of postal disruption, any communication mailed by post will be deemed to have been received eight calendar days after being mailed.
The address of the Designated Official for Canada shall be:
Assistant Deputy Minister, Strategic Policy Branch
Health Canada
70 Colombine Driveway
Brooke Claxton Building
Ottawa, Ontario
K1A 0K9
Email: jocelyne.voisin@hc-sc.gc.ca
The address of the Designated Official for British Columbia shall be:
Ministry of Health
Associate Deputy Minister, Health Systems Operations
PO Box 9637 STN PROV GOVT
Victoria, BC
V8W 9P1
Email: Jonathan.Dube@gov.bc.ca
13.0 General
13.1 This Agreement, including Annexes, comprises the entire Agreement entered into by the Parties.
13.2 This Agreement shall be governed by and interpreted in accordance with the laws of Canada and British Columbia.
13.3 No member of the House of Commons or of the Senate of Canada or of the Legislature of British Columbia shall be admitted to any share or part of this Agreement, or to any benefit arising therefrom.
13.4 If for any reason a provision of this Agreement, that is not a fundamental term, is found by a court of competent jurisdiction to be or to have become invalid or unenforceable, in whole or in part, it will be severed and deleted from this Agreement, but all the other provisions of this Agreement will continue to be valid and enforceable.
13.5 This Agreement may be executed in counterparts, in which case (i) the counterparts together shall constitute one agreement, and (ii) communication of execution by fax transmission or emailed in PDF shall constitute good delivery. Electronic signature(s) may be accepted as originals so long as the source of the transmission can be reasonably connected to the signatory.
In witness whereof the Parties have executed this Agreement through duly authorized representatives.
Signed on behalf of Canada by the Minister of Health this 7th day of October, 2023.
The Honourable Mark Holland, Minister of Health
Signed on behalf of Canada by the Minister of Mental Health and Addictions and Associate Minister of Health this 7th day of October, 2023.
The Honourable Ya'ara Saks, Minister of Mental Health and Addictions and Associate Minister of Health
Signed on behalf of British Columbia by the Minister of Health this 6th day of October, 2023.
The Honourable Adrian Dix, Minister of Health
Signed on behalf of British Columbia by the Minister of Mental Health and Addictions this 6th day of October, 2023.
The Honourable Jennifer Whiteside, Minister of Mental Health and Addictions
Annex 1 – Common Statement of Principles on Shared Health Priorities
Common Statement of Principles on Shared Health Priorities
Annex 2 – Shared pan-Canadian interoperability roadmap
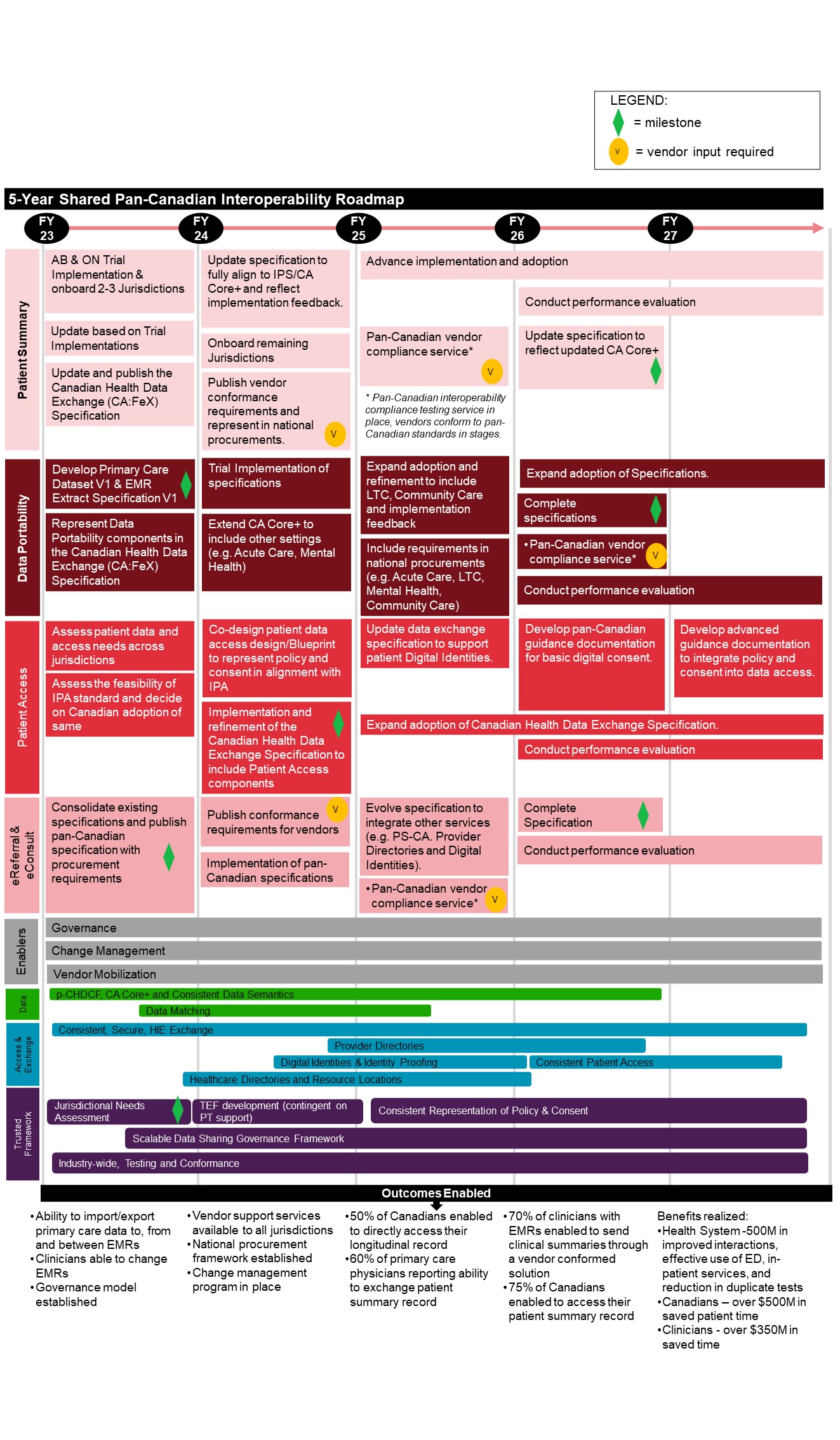
Figure 1 - Text description
The Roadmap outlines 8 categories of activities planned for fiscal years 2023 to 2027, followed by anticipated outcomes enabled. Notes are also included throughout to highlight a "milestone", where "vendor input is required", and/or when an activity is "continued" across multiple fiscal years.
Patient summary
- Fiscal Year 2023
- Alberta & Ontario Trial Implementation & onboard 2-3 Jurisdictions
- Update based on Trial Implementations
- Update and publish the Canadian Health Data Exchange (CA:FeX) Specification
- Fiscal Year 2024
- Update specification to fully align to IPS/CA Core+ and reflect implementation feedback
- Onboard remaining jurisdictions
- Publish vendor conformance requirements and represent in national procurements [vendor input required]
- Fiscal Year 2025
- Advance implementation and adoption
- Pan-Canadian vendor compliance service *(Pan-Canadian interoperability compliance testing service in place, vendors conform to pan-Canadian standards in stages.) [vendor input required]
- Fiscal Year 2026
- Advance implementation and adoption [continued]
- Conduct performance evaluation
- Update specification to reflect updated CA Core+ [milestone]
- Fiscal Year 2027
- Advance implementation and adoption [continued]
- Conduct performance evaluation [continued]
Data portability
- Fiscal Year 2023
- Develop Primary Care Dataset V1 & EMR Extract Specification V1 [milestone]
- Represent Data Portability components in the Canadian Health Data Exchange (CA:FeX) Specification
- Fiscal Year 2024
- Trial Implementation of specifications
- Extend CA Core+ to include other settings (e.g. Acute Care, Mental Health)
- Fiscal Year 2025
- Expand adoption and refinement to include LTC, Community Care and implementation feedback
- Include requirements in national procurements (e.g. Acute Care, LTC, Mental Health, Community Care)
- Fiscal Year 2026
- Expand adoption of Specifications
- Complete specifications [milestone]
- Pan-Canadian vendor compliance service *(Pan-Canadian interoperability compliance testing service in place, vendors conform to pan-Canadian standards in stages.) [vendor input required]
- Conduct performance evaluation
- Fiscal Year 2027
- Expand adoption of Specifications [continued]
- Conduct performance evaluation [continued]
Patient access
- Fiscal Year 2023
- Assess patient data and access needs across jurisdictions
- Assess the feasibility of IPA standard and decide on Canadian adoption of same
- Fiscal Year 2024
- Co-design patient data access design/Blueprint to represent policy and consent in alignment with IPA
- Implementation and refinement of the Canadian Health Data Exchange Specification to include Patient Access components [milestone]
- Fiscal Year 2025
- Update data exchange specification to support patient Digital Identities
- Expand adoption of Canadian Health Data Exchange Specification
- Fiscal Year 2026
- Develop pan-Canadian guidance documentation for basic digital consent
- Expand adoption of Canadian Health Data Exchange Specification [continued]
- Conduct performance evaluation
- Fiscal Year 2027
- Develop advanced guidance documentation to integrate policy and consent into data access
- Expand adoption of Canadian Health Data Exchange Specification [continued]
- Conduct performance evaluation [continued]
eReferral & eConsult
- Fiscal Year 2023
- Consolidate existing specifications and publish pan-Canadian specification with procurement requirements [milestone]
- Fiscal Year 2024
- Publish conformance requirements for vendors [vendor input required]
- Implementation of pan-Canadian specifications
- Fiscal Year 2025
- Evolve specification to integrate other services (e.g. PS-CA. Provider Directories and Digital Identities)
- Pan-Canadian vendor compliance service *(Pan-Canadian interoperability compliance testing service in place, vendors conform to pan-Canadian standards in stages.) [vendor input required]
- Fiscal Year 2026
- Complete Specification [milestone]
- Conduct performance evaluation [continued]
- Fiscal Year 2027
- Conduct performance evaluation [continued]
Enablers
- Fiscal Years 2023 to 2027
- Governance
- Change Management
- Vendor Mobilization
Data
- Fiscal Year 2023
- p-CHDCF, CA Core+ and Consistent Data Semantics
- Data Matching
- Fiscal Year 2024
- p-CHDCF, CA Core+ and Consistent Data Semantics [continued]
- Data Matching [continued]
- Fiscal Year 2025
- p-CHDCF, CA Core+ and Consistent Data Semantics [continued]
- Data Matching [continued]
- Fiscal Year 2026
- p-CHDCF, CA Core+ and Consistent Data Semantics [continued]
- Fiscal Year 2027
- N/A
Access and exchange
- Fiscal Year 2023
- Consistent, Secure, HIE Exchange
- Healthcare Directories and Resource Locations
- Fiscal Year 2024
- Consistent, Secure, HIE Exchange [continued]
- Provider Directories
- Digital Identities & Identity Proofing
- Healthcare Directories and Resource Locations [continued]
- Fiscal Year 2025
- Consistent, Secure, HIE Exchange [continued]
- Provider Directories [continued]
- Digital Identities & Identity Proofing [continued]
- Healthcare Directories and Resource Locations [continued]
- Fiscal Year 2026
- Consistent, Secure, HIE Exchange [continued]
- Provider Directories [continued]
- Digital Identities & Identity Proofing [continued]
- Consistent Patient Access
- Healthcare Directories and Resource Locations [continued]
- Fiscal Year 2027
- Consistent, Secure, HIE Exchange [continued]
- Consistent Patient Access [continued]
Trusted framework
- Fiscal Year 2023
- Jurisdictional Needs Assessment [milestone]
- Scalable Data Sharing Governance Framework
- Industry-wide, Testing and Conformance
- Fiscal Year 2024
- TEF development (contingent on PT support)
- Scalable Data Sharing Governance Framework [continued]
- Industry-wide, Testing and Conformance [continued]
- Fiscal Year 2025
- Consistent Representation of Policy & Consent
- Scalable Data Sharing Governance Framework [continued]
- Industry-wide, Testing and Conformance [continued]
- Fiscal Year 2026
- Consistent Representation of Policy & Consent [continued]
- Scalable Data Sharing Governance Framework [continued]
- Industry-wide, Testing and Conformance [continued]
- Fiscal Year 2027
- Consistent Representation of Policy & Consent [continued]
- Scalable Data Sharing Governance Framework [continued]
- Industry-wide, Testing and Conformance [continued]
Outcomes
- Ability to import/export primary care data to, from and between EMRs
- Clinicians able to change EMRs
- Governance model established
- Vendor support services available to all jurisdictions
- National procurement framework established
- Change management program in place
- 50% of Canadians enabled to directly access their longitudinal record
- 60% of primary care physicians reporting ability to exchange patient summary record
- 70% of clinicians with EMRs enabled to send clinical summaries through a vendor conformed solution
- 75% of Canadians enabled to access their patient summary record
- Benefits realized:
- Health System – $500M in improved interactions, effective use of ED, in-patient services, an reduction in duplicate tests
- Canadians – over $500M in saved patient time
- Clinicians – over $350M in saved time
Annex 3 – Headline common indicators
| Shared health priority area | Indicator |
|---|---|
| Family health services | Percentage of Canadians who report having access to a regular family health team, a family doctor or nurse practitioner, including in rural and remote areas |
| Health workers and backlogs | Size of COVID-19 surgery backlog |
| Net new family physicians, nurses, and nurse practitioners | |
| Mental health and substance use | Median wait times for community mental health and substance use services |
| Percentage of youth aged 12 to 25 with access to integrated youth services (IYS) for mental health and substance use | |
| Percentage of Canadians with a mental disorder who have an unmet mental health care need | |
| Modern health data system | Percentage of Canadians who can access their own comprehensive health record electronically |
| Percentage of family health service providers and other health professionals (e.g., pharmacists, specialists, etc.) who can share patient health information electronically |
Annex 4 – Action plan
Overview/Background
The Government of British Columbia continues to have a strategic vision for an integrated system of care that helps people maintain their mental and physical health, recover from illness and surgery, improve their quality of life, stay independent longer, and avoid unnecessary hospital visits. This health system is person-centered, coordinated, seamless and easy to understand for clients, family members and care providers.
BC is making significant commitments in areas related to all four priority areas outlined in the February 7, 2023 Working Together to Improve Health Care plan: Family Health Services, Health Workers and Backlogs, Mental Health and Substance Use, and Modernizing Health Systems. The recent Budget of 2023 announced almost $6.4 billion in new investments over three years to help strengthen public health care and help people find and stay connected to the care they need. It also included $1 billion in new funding to expand mental health and addictions services Footnote 1.
In September 2020, the Ministry of Health announced its Primary Care Strategy outlining steps to make sure people have faster and better access to the day-to-day healthcare services they need Footnote 2. This includes using team-based care, creating primary care networks, supporting the establishment of patient medical homes as the cornerstone of primary care networks, opening urgent and primary care centres, supporting community health centres to bring health and social services together, and supporting First Nations-led projects.
Supporting and bolstering health workforce across the province is a top priority for the Ministry of Health. BC's Health Human Resources (HHR) Strategy outlines how people are being put first by delivering comprehensive and quality public healthcare services Footnote 3. Through the HHR Strategy, several immediate actions have been taken including increasing the number of doctors trained in medical schools, supporting internationally educated health professionals to work in BC sooner, and expanding the scope of practice for pharmacists. The successful launch of the new physician payment model in February 2023 has attracted new and existing physicians to primary care by moving away from the fee for service model. This is a building block to renew primary care in the province and is the first step among many. In addition, work is underway to implement a new transformative staffing model to better support nurses and patients. In alignment with the HHR Strategy, the model will allow nurses to spend more time with patients and provide better, more person focused services.
BC's Ten-Year Cancer Action Plan was launched in February 2023 to prepare for an increased incidence of cancer and demand for cancer care services due to BC's growing and aging population. The Cancer Plan aims to better prevent and detect cancer, ensure timely access to treatment, and continue to build a modern, evidence-based cancer system that integrates research and care. Efforts to support the recruitment of oncologists and specialized cancer care professionals and build a team-based model of care in the cancer system are priorities to address patient wait times. In addition, BC will build new cancer centres to improve patient access to diagnostics and treatments that rely on complex machines. The Plan builds on investments and efforts since 2017 to strengthen cancer care in BC including launching the new province-wide Lung Cancer Screening Program, the 10-point Youth Vaping Provincial Action Plan, adding Indigenous patient support positions at all cancer centres, and launching pilots for at home HPV testing to improve access and equity in screening for cervical cancer.
Reducing surgical wait times is a priority and BC is committed to ensuring patients receive the life changing surgery they need when they need it. Despite the delays caused by the COVID-19 pandemic, more surgeries have been completed on average compared to pre-pandemic levels and waitlists for patients have predominantly decreased Footnote 4. As of May 2023, health authorities have completed over 99 per cent of surgeries for patients who had their surgery postponed due to COVID-19 and still wanted to pursue surgical treatment Footnote 5.
With respect to mental health services, A Pathway to Hope, a 10-year roadmap for making mental health and addiction care better for people in British Columbia, charts a course to an improved future for health and well-being in BC. The mental health and substance use initiatives outlined below are in alignment with the objectives of this Roadmap. Focus areas of this strategy include improving integration of care and access to services, investing in prevention and early intervention, and improving the mental health and wellbeing of key populations experiencing significant disparity in outcomes. This includes wellness of children, youth, and young adults, supporting Indigenous-led solutions, and improving quality of care. In addition, the Ministry of Mental Health and Addictions is accelerating work to address the illicit drug toxicity crisis through targeted investments, safer supply, and by introducing a new integrated model of care with more addictions withdrawal treatment and recovery services. A Pathway to Hope is a plan to transform BC's mental health and substance use system across the full continuum of care – prevention, harm reduction, safe supply, treatment, and recovery, where people have access to culturally safe and effective care when they need it.
Digital Health and data weave together the health care provider and patient experience across health care settings, enabling seamless transitions of care at every stage of life. BC's Digital Health Strategy envisions a connected, trusted health system, which empowers all users and addresses population health needs Footnote 6. Objectives for this strategy include empowering patients, improving provider experience, establishing a connected health system, and enabling business enterprises. BC's Health Gateway provides British Columbians with secure and convenient access to their health records. Work is actively underway to add more health information to the Gateway and to align various patient portals across the province to ensure a connected patient experience.
BC's commitment to advancing reconciliation with Indigenous people is embedded in its laws through the Declaration on the Rights of Indigenous Peoples Act (DRIPA), which the BC government passed in 2019 to establish the United Nations Declaration on the Rights of Indigenous Peoples as a framework for reconciliation, and it is also reflected in many new investments and initiatives already under way here in BC. In the DRIPA action plan, the Ministry of Health and Ministry of Mental Health and Addictions are partnering on eight commitments to address mental health and wellness, primary care, partnerships, funding, cultural safety and humility, and quality of care for Indigenous people Footnote 7. Underpinning this is the ongoing work across health authorities and with other key partners to implement the recommendations of the In Plain Sight Report to eliminate Indigenous specific racism. The Ministry of Health is committed to reconciliation and the trilateral, bilateral and health authority relationships to improve the health and wellness of Indigenous peoples.Footnote 8
This action plan has been developed in partnership with the Ministry of Health and the Ministry of Mental Health and Addictions. Initiatives outlined in this plan will support the significant work already underway to deliver better health care for everyone in BC.
Initiatives supported by federal funds – Health workers and backlogs
1. Implementation of transformative staffing model to better support nurses and patients
Description of activities – BC has worked with the BC Nurses' Union and the Nurses' Bargaining Association (NBA) to develop a new staffing model that is the first of its kind in Canada and will transform the way people are cared for by nurses as they will spend more dedicated time with patients. The Ministry of Health (the Ministry) is working with the NBA to adopt Nurse-to-Patient Ratios (NPR) as part of team-based care. Federal funds will help advance this work inclusive of hospital-based care, long-term and residential care, and community and non-hospital care. The hospital-based care funding will support 83 acute care sites around the province, representing a combination of tertiary, community, and rural hospitals. Part of this funding will include investments to improve and expand clinical supervision programs for student nurses across the healthcare system. The long-term care and assisted living funding involves increasing clinical supports and clinical supervision and specifically looking at clinical needs of nurses to support increasing clinical demands and complex care needs of seniors. The community and non-hospital care investments will be made in community and non-hospital care, including the development and implementation of the Nurse-to-Patient Ratios (NPR). Actions involved in the implementation of NPRs will include establishment of an Executive Steering Committee, associated working groups, and a robust recruitment and retention strategy necessary to increase staffing levels. The Ministry is also investing in both ongoing and additional one-time funding to support nurses in their career development as well as their well-being and day-to-day operations.
Rationale – Implementation of a standard minimum NPR has been identified as a leading international practice to reduce nursing workloads, increase staff safety, improve nurse retention, and improve access to safe, quality nursing services.
Relation to Broader Initiatives – This initiative is a key part of BC's strategic plan to alleviate health workforce shortages and achieve robust levels of baseline staffing, as outlined in BC's Health Human Resources Strategy – 1.1 Base staffing, demand, and supply pressures. BC's Health Human Resources Strategy is a mandate commitment that responds to long-standing health workforce challenges which have been exacerbated by dual public health crises: the COVID-19 pandemic and the toxic drug supply. The Strategy envisions a health system that puts people first – fostering workforce satisfaction and innovation to ensure health services are accessible to everybody in BC, now and into the future.
2. Create incentive programs to support recruitment and retention of healthcare workers.
Description of activities – In September 2022 the Ministry released a new Health Human Resource Strategy to address healthcare staffing shortages throughout BC. This is a multi-year strategy that highlights four key areas of focus: Retain, Redesign, Recruit, and Train. Actions that have been taken towards this initiative include the addition of medical education and residency seats, expanding roles of pharmacists, and work towards opening BC's second medical school at Simon Fraser University. Part of the Retain area of focus includes an objective to retain staff in high need areas and occupations. The Provincial Health Human Resources Coordination Centre will develop incentive programs to promote retention of priority occupations in high needs communities and service areas, including mental health and substance use. Some objectives in the Recruit area of focus include refreshing enablers and incentives to attract new healthcare workers and removing barriers for internationally educated health care workers. Removing these barriers will help BC meet the increasing demand for nurses across the province while supporting more nurses in building a rewarding healthcare career. Further initiatives in the Strategy focus on expanding training opportunities for nurses, paramedics, first responders, and health responders.
Rationale – Health workforce demand continues to accelerate in BC and across Canada, with staffing shortages becoming particularly acute in rural and remote areas. Staffing shortages and public health emergencies have added pressure onto the health system and workloads for healthcare professionals across all sectors, which has in turn increased levels of stress and burnout.
Relation to Broader Initiatives – Demand for healthcare services and workers has dramatically increased in the last decade in BC, and sufficient base staffing levels are a key element of ensuring safety and wellbeing of both patients and healthcare workers. These incentive programs support BC's larger efforts to develop and maintain a sustainable, skilled health workforce in alignment with Goal 3, Objective 3.1 of the Ministry of Health 2023/24 - 2025/26 Service Plan and Objective 1.1 of BC's Health Human Resources Strategy – Base staffing, demand, and supply pressures.
Addressing the needs of Indigenous peoples and other underserved and disadvantaged populations - BC has demonstrated significant leadership in legislative and policy reforms to address inequities and barriers to inclusion in the workforce and society, including by implementing the Accessible British Columbia Act, the Temporary Foreign Worker Protection Act, and DRIPA. BC's HHR Strategy reflects the BC government's commitment to addressing inequality, including through the implementation of GBA+ and an equity lens across all policy and planning. When developing the Strategy, the Ministry analyzed unique workforce challenges for rural and remote workers, Indigenous workers, immigrants, racialized people, women, workers in entry-level positions, and internationally educated professionals. The HHR strategy acknowledges and embeds the BC government's commitment to ending Indigenous-specific racism by making cultural safety a foundational requirement of the health system and advancing targeted strategies to support Indigenous people as both patients and healthcare providers. Several actions in the HHR strategy are aligned with Indigenous health system priorities as identified in In Plain Sight recommendations. The Ministry has committed to assessing all actions through the lens of cultural safety and anti-racism. This work is complex and requires ongoing and genuine engagement with Indigenous peoples, disruption of existing systems, and investment across enabling sectors, including education and advanced education.
3. Improve outcomes for patients by addressing diagnostic and treatment backlogs and reducing pressure on acute care services.
Description of activities – The pandemic has contributed to large backlogs and long wait times for some care services in BC. One initiative that will contribute to addressing backlogs in radiation therapies is the recently announced 10-year cancer action plan, which will work to increase the capacity of BC Cancer and the broader health care system to deliver timely treatment. Similar initiatives will help to address waitlists and backlogs in other areas of the healthcare system including specialized support services. Improving hospital capacity and flow can be achieved through programs like Hospital at Home by reducing wait times for inpatient services and decreasing pressure on acute inpatient services. Current Hospital at Home prototype programs in BC care for hospital medicine patients including those with heart failure, chronic obstructive pulmonary disease, and serious infections, as well as pre/post surgery patients. These programs are currently able to provide pain management through a number of strategies including those provided by allied health therapy and medication nearly equivalent to inpatient care. At this point patient-controlled analgesia is not something occurring in hospital at home programs. In future, Hospital at Home in BC may be expanded to other areas of care, including mental health and/or substance use care.
Rationale – Long wait times for care services have a significant impact on the wellbeing of patients and families. Wait times associated with services such as cancer care are closely tied to quality of cancer care, as access to treatment within benchmark wait times provides a greater chance of successful results, often with fewer interventions. Clearing the backlog for these services increases the chances of earlier interventions and better outcomes for patients. Several factors have contributed to increased pressure on acute care services in BC's hospitals, including the COVID-19 pandemic, an aging population, and long wait times for specialized support services. The expansion of programs such as Hospital at Home will help reduce pressure on acute inpatient services and improve patient flow.
Relation to Broader Initiatives – The Ministry recently announced the launch of the ten-year Cancer Action Plan to address the increasing burden of cancer with immediate steps to better detect, treat, and prevent cancer. Part of this plan is to increase the capacity of BC Cancer and the broader health care system to deliver timely treatment. Building this capacity involves physicians, and staff recruitment as well as procurement and installation of complex equipment, in alignment with the health workforce goals outlined in BC's Health and Human Resource Strategy and BC's Service Plan. BC's Cancer Care Action Plan – Priority 2.2; BC's Health Human Resources Strategy – 2.3 Attract and Onboard, 2.4 Train: Create Accessible Career Pathways;
Ministry of Health 2023/24 - 2025/26 Service Plan, Goal 2, Objective 2.2
Addressing the needs of Indigenous peoples and other underserved and disadvantaged populations - Minority and disadvantaged populations suffer disproportionately from cancer due to lack of participation in screening programs and lower support to enable expedient navigation of the health care system. For rural and remote populations, extended wait times can lead to lower participation rates in treatment as individuals become less willing to travel for treatment. In offering patients the option to travel out of country to receive radiation treatment, BC Cancer will be providing support for all travel arrangements and will ensure that all costs for travel, accommodation, and per diems are covered up front so that low-income patients do not face additional burdens to accessing care. In conjunction with this initiative, the Ministry has also provided $20M in grant funding to non-profit organizations that deliver a comprehensive suite of travel supports to patients facing challenges with accessing care as a result of travel.
Initiatives supported by federal funds – Mental health and substance use
As committed to in the 2017 Home and Community Care and Mental Health and Addiction Services Agreement, the BC Ministry Mental Health and Addictions and the BC Ministry of Health have been working to improve access to evidence-based mental health and addiction services and supports for Canadians and their families. With remaining funding for mental health and substance use services carried over from the 2017 Agreement, BC remains committed to investing federal funds to support the below initiatives, which are in alignment with the Common Statement of Principles on Shared Health Priorities.
In BC Indigenous people are disproportionately impacted by mental health and substance use. BC is also focused on the UNDRIP and DRIPA commitments. Therefore, much of the information provided will relate to Indigenous peoples. Programs like Foundry and Confident Parents offer virtual and telephone services to support access from all areas of the Province. Foundry specifically works with LGBTIQA2S+ youth and has gender affirming space and programming. Urban Indigenous Friendship Centres provide services to people with accessibility needs and LGBTIQA2S+. All newly funded programs are also analyzed through a GBA+ lens. Evaluation frameworks and disaggregated data are used to support program design with particular attention paid to under-represented populations.
1. Strengthen the capacity of primary care to respond to mental health and addictions, with a focus on prevention/early intervention and children/youth
Description of activities– As an integral component of Primary Care Networks, the province is supporting a range of evidence-based interventions, including virtual care, designed to offer primary care professionals referral tools to help prevent and intervene early with common and debilitating mental disorders. Actions include support for evidence-based virtual care interventions, such as online and telephone Cognitive Behavioral Therapy and positive parenting coaching, which helps parents support children who are dealing with anxiety and provides early access to culturally appropriate supports and services for Indigenous families.
Rationale – With increasing demands on the primary care setting, these initiatives are designed to increase capacity and ensure the availability of effective supports for mild to moderate mental health and substance use problems.
Relation to Broader Initiatives – Federal funding in this area will be used to resource a range of evidence-based interventions designed to offer primary care professionals referral tools to help prevent and intervene early with common and debilitating mental disorders, supporting youth in accordance with the Ministry of Mental Health and Addictions Service Plan. The availability of these interventions will provide increased capacity for mental health and addictions in Primary Care Networks and increased capacity for health authorities to collaborate with First Nations through hiring an additional Liaison. Ministry of Mental Health and Addictions 2023/24 - 2025/26 Service Plan, Goal 2, Objective 2.2
2. Expand access to culturally safer and trauma informed mental health and addictions services for Indigenous communities
Description of activities– Supporting efforts led by the First Nations Health Authority, funding will be used increase the number of individuals and communities with access to culturally safer, trauma-informed, and culturally appropriate healing and treatment services and mental health and substance use care, while building on a longer-term strategy to address the mental health and substance use needs of Indigenous peoples. Program-specific activities will take a holistic approach to individual and family healing.
Rationale – The mental health and substance use needs of Indigenous peoples are disproportionately high due to the ongoing effects of colonization and intergenerational trauma.
Relation to Broader Initiatives – Federal funds will leverage existing provincial investments to expand supports for providing Indigenous Land Based Cultural Treatment and Healing Services to support people with substance use challenges in alignment with Ministry of Mental Health and Addictions 2023/24 - 2025/26 Service Plan, Goal 1, Objectives 1.1 and 1.2.
3. Improve seamlessness across systems of care so that people can ask once and get help fast
Description of activities – Supporting the incremental expansion of access to integrated services centres across BC, especially youth, and building a virtual workforce designed to provide timely mental health and addictions care through virtual clinic access points. The integrated service centres increase timely access for youth and young adults to integrated services by providing youth-friendly services that are easily accessible, either in person or virtually. Additionally, the provincial crisis line network serves as a key access point to the mental health and addictions system for thousands of British Columbians each year.
Rationale – People with mental health or substance use issues in BC, especially young people, experience challenges accessing services quickly.
Relation to Broader Initiatives – BC has invested in integrated service centres, including 15 Foundry centres for youths, to better coordinate services and remove barriers to mental health and wellbeing in alignment with Ministry of Mental Health and Addictions 2023/24 - 2025/26 Service Plan, Goal 2, Objective 2.1
4. Increase access for students to mental health and addictions prevention and early intervention services
Description of activities – Develop and deliver mental health and wellness training to school communities with the aims of reducing stigma and discrimination, improving student connectedness, improving the likelihood of early identification and help seeking, while improving opportunities to dialogue about mental health and wellbeing in school and at home. Action taken on this initiative would include mental health and wellness training in school communities with the aims of reducing stigma and discrimination, improving student connectedness, improving the likelihood of early identification and help seeking, while improving opportunities to dialogue about mental health and wellbeing in school and at home.
Rationale – Schools are a critical setting to improve the mental health and wellbeing of students, and investment here will build capacity for school personnel to recognize and respond to students experiencing mental health and addiction problems.
Relation to Broader Initiatives – Research has demonstrated the importance of early identification and intervention for youth experiencing mental health challenges. Supporting mental health services in schools and youth-oriented mental health programming is key to ensuring that children and youth can access the support services they need in a timely way, in accordance with Ministry of Mental Health and Addictions 2023/24 - 2025/26 Service Plan, Goal 2, Objective 2.2
5. Expand access to evidence-based prevention, early intervention, treatment, and recovery options for vulnerable populations.
Description of activities – Supporting targeted interventions for vulnerable populations to identify and mitigate problems at an early stage (e.g., reduce risk and enhance protective factors), as well as evidence-based treatment options for individuals with severe addictions. Specific initiatives include hospital and community-based services for at-risk pregnant and postpartum women challenged with substance use. Actions will also focus on improving access to treatment and recovery options for adults at higher risk of poor health outcomes and death due to substance use.
Rationale – In BC, some people and groups of people are more vulnerable to mental health problems and/or addictions than others. Health disparities persist among certain vulnerable groups, suggesting the need for further focused attention across the continuum of services.
Relation to Broader Initiatives – This programming will support the expansion of evidence-based treatment options and integrated community-based services as part of the continuum of care for individuals with severe addiction and/or complex health needs, including both the clinical provision of interventions and intensive case management (psychosocial services) as outlined in Ministry of Mental Health and Addictions 2023/24 - 2025/26 Service Plan, Goal 1, Objectives 1.1 and 1.2
Initiatives supported by federal funds – Modernizing health systems
1. Modernizing Health Data Systems to support the full continuum of care and empower patients to engage in their health care.
Description of activities:
- Enhance data assets, data collection, and data management and sharing capacities: One of BC's priorities is expanding the availability and accessibility of data through onboarding new data sets and data contributors and developing a centralized, sector-wide health metadata repository. Enhancing data assets through a series of planned data acquisition and product activities will provide high-quality, secure, comparable data needed to improve services for British Columbians. Modernizing the system will allow analysts, both in academia and the health sector, to perform advanced analytics on large, integrated datasets more efficiently contributing to the knowledge base on health care and support the sharing of data among health users and other partners. Finally, scaling data access services as part of a sector-coordinated data access approach will support safe access to data as well as evaluation and innovation in health policy.
- Empower patients to access and manage their personal health data and care through digital tools: Patients will be empowered with digital tools and access to information to make them more active participants in their health care journey.
- Improve health provider experience through digital tools and access to information: This initiative will reduce administrative burden on providers, and increase their capacity to deliver efficient, trusted, high-quality, consistent care.
- Establish a secure and connected digital health system to support interoperability and enable data sharing and standardization: The connected digital health system initiative enables the seamless and secure sharing and exchange of provincial health data between all users across the care continuum and supports the sharing of data with federal and provincial partners.
Rationale:
Expanding the availability and quality of health authority and Ministry-structured data across the sector will enable a comprehensive understanding of a person's care journey across care providers and organizations. Establishing a more connected health system will support interoperability across regional boundaries and across levels of care, as well as streamlining access to clinical data for both patients and providers. Safe, timely access to data will also be a key building block to building a research-positive health system. A sector-coordinated data access approach will efficiently support safe access to data that will even security and privacy practices, will support efforts to bring innovative ideas to address health challenges, and will support the evaluation and monitoring of policy. An example of where this could be useful is with data related to BC's mental health and substance use patients, services, treatment, and recovery. It is currently collected across multiple systems, organizers, and providers across the province that causes challenges in consistency in data collection, quality, and interoperability between systems. A connected system would allow partners to enhance the current data collection systems in place.
Relation to Broader Initiatives – As outlined in the Ministry of Health 2023/24 - 2025/26 Service Plan, Goal 3, Objective 3.3, this initiative enhances patient experiences by enabling easy access to health information, virtual care, and effective utilization of digital tools. This initiative is also aligned with Objective 3.1, improving the provider experience by digitalizing health human resource processes and structures, reducing administrative burdens, and increasing efficiency. There is a connection to the Pan-Canadian Interoperability Roadmap (PCIR) – Goals 3 and 4 with enabling seamless patient and provider access to longitudinal health records and improving health information interpretation through enhanced data standardization. British Columbia Digital Plan (BCDP) – Missions 1,2, and 3 include empowering patients through enabling citizens to easily interact with the health system, delivering digital services that people can trust and access safely and securely, and supporting reliable service delivery by improving the way technology is built and operated. Other broader initiatives related to this initiative include: Pharmaceutical Management Strategy – Strategic Area of Focus – 7.1; Physician Quality Improvement Initiative – Measurement System; and B.C. Life Sciences and Biomanufacturing Strategy – Pillar 5
Addressing the needs of Indigenous peoples and other underserved and disadvantaged populations: The development of these programs included an Indigenous-specific lens, and the Common Evaluation Model used for digital health initiatives incorporates several equity measures including accessibility, cultural safety, and the inclusion of Indigenous peoples. This initiative focuses on the impacts on marginalized groups like LGBTIQA2S+, people with disabilities, and low-income communities. Enhancing access to data across domains and organizations can also advance health equity by helping to better understand and respond to the health needs of communities that are underserved by the healthcare system.
| Indicator | Baseline | Target and timeframe [at least 3-year target] | |
|---|---|---|---|
| Target | Timeframe | ||
| Family Health Services | |||
| Percentage of Canadians who report having access to a regular family health team including in rural and remote areasFootnote a | N/AFootnote a | ||
| Health workers and backlogs | |||
| Size of COVID-19 surgery backlogFootnote b | -7% (Mar 2020 – Sep 2022) | 0% | Complete |
| Net new family physicians, nurses, and nurse practitionersFootnote c | For 2021: FP: 14 per 10,000 (7,118) NP: 1 per 10,000 (648) RN: 77 per 10,000 (40,343) |
Additional headcount FP: +200 NP: +80 RN: +8,000 based on Nurse Patient Ratio TargetFootnote d |
FP: Annual growth NP: Annual growth RN: Full implementation by 2028 (growth over four years) |
| Mental health and substance use | |||
| Median wait times for community mental health and substance use services | 15 days (2021/22) | 14 days | 2025/26 |
| Percentage of youth aged 12 to 25 with access to integrated youth services for mental health and substance use | 15 IYS active sites 9 YHS sites under development (2023) |
20 IYS active sitesFootnote e | 2025/26 |
| Percentage of Canadians with a mental disorder who have unmet health care needs | 8% (2018) | 7%Footnote f | 2025/26 |
| Modernizing health systems | |||
| Percentage of Canadians who can access their own comprehensive health record electronically | 48% (2022) | 75%Footnote g | 2025/26 |
| Percentage of family health service providers and other health professionals (e.g. pharmacists, specialist, etc.) who can share patient health information electronically | 41% (2021) | 50% | 2025/26 |
|
|||
| Indicator | Baseline | Target and timeframe [at least 3-year target] | |
|---|---|---|---|
| Target | Timeframe | ||
| Family Health ServicesFootnote a | N/AFootnote a | ||
| Health workers and backlogs | |||
| Nurse Patient RatioFootnote b | As of December 2022: RN – 27,764 FTEs LPN – 7,150 FTEs | Increase in nursing capacityFootnote b | 2025/26 |
| Mental health and substance use | |||
| Number of Foundry centres open | 16 | 35Footnote c | 2025/26 |
| % of people on Opioid Agonist Treatment (OAT) who have been retained for 12 months | 49.9% (August 2021) | 2-5% IncreaseFootnote d | Annual Target |
| Percentage of people admitted for mental illness or substance use who are readmitted within 30 days | 15.4% (2021/22) | 13.6%Footnote e | 2025/26 |
| Modernizing health systems | |||
| Number of data holdingsFootnote f in the Health Data Platform | 19 | 34 | 2025/26 |
|
|||
| Initiative | Incremental investments | ||
|---|---|---|---|
| 2023-24 | 2024-25 | 2025-26 | |
| Family health services | N/A | N/A | N/A |
| Health workforce and backlogs | |||
| Implementation of transformative staffing model to better support nurses and patients. | 200 | 250 | 300 |
| Create incentive programs to support recruitment and retention of healthcare workers. | 18 | 0 | 0 |
| Improve outcomes for patients by addressing diagnostic and treatment backlogs and reducing pressure on acute care services. | 78 | 45 | 0 |
| Total (millions) | 296 | 295 | 300 |
| Mental health and substance use | |||
| Strengthen the capacity of primary care to respond to mental health and addictions, with a focus on prevention/early intervention and children/youth. | 23 | 23 | 22 |
| Expand access to culturally safer and trauma informed mental health and addictions services for Indigenous communities. | 14 | 14 | 15 |
| Improve seamlessness across systems of care so that people can ask once and get help fast. | 11 | 11 | 11 |
| Increase access for students to mental health and addictions prevention and early intervention services. | 4 | 4 | 4 |
| Expand access to evidence-based prevention, early intervention, treatment, and recovery options for vulnerable populations. | 30 | 30 | 30 |
| Total (millions) | 82 | 82 | 82 |
| Modernizing health systems | |||
| Modernizing health data systems to support the full continuum of care and empower patients to engage in their health care. | 29.3 | 30.3 | 25.3 |
| Total (millions) | 29.3 | 30.3 | 25.3 |
| Total funding available (millions) | 407.3 | 407.3 | 407.3 |
References:
- Footnote 1
-
https://www.bcbudget.gov.bc.ca/2023/default.htm
- Footnote 2
-
https://www2.gov.bc.ca/assets/gov/health/about-bc-s-health-care-system/heath-care-partners/health-newsletter/context-pcn-december-2019.pdf
- Footnote 3
-
https://news.gov.bc.ca/files/BCHealthHumanResourcesStrategy-Sept2022.pdf
- Footnote 4
-
https://www2.gov.bc.ca/assets/gov/health/conducting-health-research/surgical-renewal-plan.pdf
- Footnote 5
-
https://news.gov.bc.ca/releases/2023HLTH0063-000720
- Footnote 6
-
https://digitalhealthcanada.com/wp-content/uploads/2023/02/BC-Digital-Health-Strategy-Handout-Feb-2023.pdf
- Footnote 7
-
https://www2.gov.bc.ca/assets/gov/government/ministries-organizations/ministries/indigenous-relations-reconciliation/declaration_act_action_plan.pdf
- Footnote 8
-
https://engage.gov.bc.ca/app/uploads/sites/613/2020/11/In-Plain-Sight-Summary-Report.pdf
- Footnote 9
-
BC is committed to working with CIHI to establish the baseline and resolve data quality issues for targets, timelines, and indicators.
- Footnote 10
-
Funding amounts in 2024-2025 and 2025-2026 are estimates and are subject to approvals through BC's annual budget planning process.