Framework on Palliative Care in Canada

Download the alternative format
(PDF format, 2.9 MB, 62 pages)
Organization: Health Canada
Date published: 2018-12-04
Contents
- Acknowledgements
- Remarks from Minister Ginette Petitpas Taylor, P.C., M.P.
- Executive Summary
- PART I - Background
- PART II - The Framework on Palliative Care in Canada
- PART III - Implementation and Next Steps
- Bibliography
- Appendices
Acknowledgements
Developing the Framework on Palliative Care in Canada would have been impossible without the participation and direction-setting provided by key organizations, groups and individuals, including provinces and territories (P/Ts) and other federal government departments. The End-of-Life Care Unit at Health Canada would like to acknowledge the contribution made by many stakeholders, including people living with a life-limiting illness and members of their families, health care providers, caregivers, researchers, as well as other individuals living in Canada. Their input and the deeply personal stories they shared with us online, in paper format and face-to-face, helped shape the Framework. Contributors and stakeholders shared a diversity of opinions and brought insight into hidden issues. For these perspectives, we are very grateful. The following document is a reflection of those insights and opinions.
Finally, this Framework would not have been possible without the close collaboration between the contributors and the End-of-Life Care Unit. The Framework on Palliative Care in Canada is the result of shared values and perspectives. Appendix A contains a list of the main groups and individuals that contributed to the development of this document.
Remarks from Minister Ginette Petitpas Taylor, P.C., M.P.
Many Canadians find it difficult to discuss death, dying and end-of-life care with their loved ones and health care providers. We tend to avoid these conversations out of fear and pain. Yet, these topics are important to the well-being of dying people and their families. Encouraging Canadians to have honest and informed conversations about death and end-of-life planning can alleviate stress, anxiety and help to ensure that Canadians have the death that they wish.
Over time, our experience of death and dying has evolved alongside changing causes of death, care and supports, and cultural and social customs. The provision of palliative care has also evolved as a practice that seeks to relieve suffering and improve the quality of living and dying for Canadians and their families. However, we know we have more to do to improve person-centred care and equitable access, so that every Canadian has the best possible quality of life right up to the end of their lives.
Over the course of the summer of 2018, officials from Health Canada heard many stories of dedication and commitment about people living with life-limiting illness, caregivers, volunteers, and health care providers. There were, however, also stories pointing to significant gaps in awareness and understanding of, and access to, palliative care across Canada.
The message from these conversations was clear: the wishes and needs of Canadians nearing the end of life must be at the centre of our approaches to care. It is critical that their cultural values and personal preferences be voiced, understood and respected when discussing care plans and treatment options. This message inspired and influenced the Framework on Palliative Care in Canada.
Together we can accomplish much by exemplifying compassion, learning from each other, and working collaboratively. It will take a concerted effort from all of us to continue to advance palliative care for Canadians. I invite all those who have a role to play to join in implementing the findings of this Framework.
The Honourable Ginette Petitpas Taylor, P.C., M.P.
Minister of HealthExecutive Summary
In late 2017, the Act providing for the development of a framework on palliative care in Canada was passed by Parliament with all-party support. During the spring and summer of 2018, Health Canada consulted with provincial and territorial governments, other federal departments, and national stakeholders, as well as people living with life-limiting illness, caregivers and Canadians. The findings from that consultation, as well as the requirements outlined in the Act, provided the foundation for the Framework on Palliative Care in Canada.
In Part I, the Framework provides an overview of palliative care, setting out the World Health Organization's definition in the Canadian context. The Framework describes how palliative care is provided in Canada, and the roles and responsibilities of the numerous individuals and organizations involved. It lays out the purpose of the Framework as providing a structure and an impetus for collective action to address gaps in access and quality of palliative care across Canada. It also provides a brief description of the consultative process.
Part II, the heart of the Framework, sets out the collective vision for palliative care in Canada: that all Canadians with life-limiting illness live well until the end of life. Key to this vision is a set of Guiding Principles, developed in collaboration with participants of the consultative process. These principles reflect the Canadian context and are considered fundamental to the provision of high-quality palliative care in Canada.
In recognition of the dynamic state of palliative care in Canada, and its multiple players, this section provides a Blueprint to help shape planning, decision making, and organizational change within the current context. It identifies existing efforts and best practices, and sets out goals and a range of priorities for short, medium and long term action to improve each of the four priority areas:
- Palliative care education and training for health care providers and caregivers;
- Measures to support palliative care providers;
- Research and the collection of data on palliative care; and
- Measures to facilitate equitable access to palliative care across Canada, with a closer look at underserviced populations.
In this section, the Framework also lays out how we might recognize success as collective progress is made.
In conclusion, Part III outlines implementation and next steps, proposing a single focal-point to advance the state of palliative care. It concludes with the recognition that advancement of the Framework will require the collective action of parties at all levels, as well as the flexibility to evolve and respond to new ideas and emerging needs over time.
PART I - Background
What Is Palliative Care?
Death and Dying in Canada
- Of the over 270,000 Canadians who die each year, 90% die of chronic illness, such as cancer, heart disease, organ failure, dementia or frailty.
- By 2026, the number of deaths is projected to increase to 330,000, and to 425,000 by 2036.
- Despite Canadians' wishes to die at home, 60% die in hospitals.
Statistics Canada
The term "palliative care" emerged in Canada in the mid-1970's, initially as a medical specialty serving primarily cancer patients in hospitals. However, since then, the scope of palliative care has expanded to include all people living with life-limiting illness. With an aging population, demand for palliative care, delivered by a range of providers, has grown. Palliative care is an approach that aims to reduce suffering and improve the quality of life for people who are living with life-limiting illness through the provision of:
- Pain and symptom management;
- Psychological, social, emotional, spiritual, and practical support; and
- Support for caregivers during the illness and after the death of the person they are caring for.
Palliative care should be person- and familyFootnote 1-centred. This refers to an approach to care that places the person receiving care, and their family, at the centre of decision making. It places their values and wishes at the forefront of treatment considerations. In person- and family-centred care, the voices of people living with life-limiting illness and their families are solicited and respected.
Palliative care can be provided in conjunction with other treatment plans, and is offered in a range of settings by a variety of health care providers, including but not limited to: doctors, nurses, nurse practitioners, pharmacists, social workers, occupational therapists, speech therapists, and spiritual counsellors.
For the purposes of this Framework, Health Canada has adopted the World Health Organization (WHO) definition of palliative care.Footnote 2 Recognizing that the WHO definition is meant for a global audience, the Government of Canada, in consultation with a wide range of stakeholders, developed a set of Guiding Principles. These principles are defined in Part II of the Framework, and allow for the definition of palliative care to be adapted to the Canadian context.
World Health Organization Definition of Palliative CareFootnote 3
Palliative care is an approach that improves the quality of life of persons and their families facing the problem associated with life-limiting illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual. Palliative care:
- Provides relief from pain and other distressing symptoms;
- Affirms life and regards dying as a normal process;
- Intends neither to hasten or postpone death;
- Integrates the psychological and spiritual aspects of care;
- Offers a support system to help persons live as actively as possible until death;
- Offers a support system to help the family cope during the person's illness and in their own bereavement;
- Uses a team approach to address the needs of persons and their families, including bereavement counselling, if indicated;
- Will enhance quality of life, and may also positively influence the course of illness;
- Is applicable early in the course of illness, in conjunction with other therapies that are intended to prolong life, such as chemotherapy or radiation therapy, and includes those investigations needed to better understand and manage distressing clinical complications.
Palliative Care in Canada
Drivers of Change
While the provision of palliative care has improved over the years, a number of reportsFootnote 4 have identified ongoing gaps in access and quality of palliative care across Canada. For example, a 2018 report by the Canadian Institute for Health Information (CIHI) noted that:
- While 75% of Canadians would prefer to die at home, only about 15% have access to palliative home care services.
- Recipients of home palliative care services are 2.5 times more likely to die at home, and are less likely to receive care in an emergency department, or intensive care unit.
- Adults aged 45-74 are more likely to receive palliative care than other age groups.
- While about 89% of people with life-limiting illness, such as a progressive neurological illness, organ failure, or frailty could benefit from palliative care, people with end-stage cancer are three times more likely to receive it.
Other societal changes and pressures driving the need for a Framework include:
Changing demographics and the increasing impact/pressure on caregivers: With the trend towards smaller family sizes and family members living further apart, the onus of caregiving rests on fewer family members, paid staff, and community. While family and friends provide the majority of care for those who are aging or ill, providing such care can create physical, emotional, and financial pressures. One in three caregivers reports distress and burnout.Footnote 5
Changing expectations for person-centred care: A growing number of Canadians expect to have a more active role in decision making about their care, including treatment choices and care settings.
Gaps in professional training: Few health care providers in Canada specialize in or practice primarily in palliative care. Canadian doctors and nurses report varying levels of training for and comfort in providing palliative careFootnote 6. In order to build broader capacity, there are increasing expectations on all health care providers to know how to deliver basic palliative care services. This translates into increased pressure on curriculum development, and education and training methods targeting those whose primary practice is not palliative care.
Increased public discussion about end-of-life care and decisions: On June 17, 2016, the Government of Canada passed legislation to allow for medical assistance in dying to be provided to eligible CanadiansFootnote 7. Public discussion around this issue included significant focus on the importance of Canadians having access to a range of care options at the end of life, including palliative care. The Medical Assistance in Dying (MAID) legislation outlines a commitment to work with provinces, territories (P/Ts) and civil society to facilitate access to palliative and end-of-life care. Further, it commits Parliament to examining the state of palliative care in Canada five years after the coming into force of the MAID law.
To address these changes, governments at all levels, health care providers, stakeholders, caregivers, and communities must work together. The following section describes who is responsible for palliative care in Canada.
Benefits of Palliative Care
Patients with chronic progressive diseases, such as cancer, congestive heart failure, chronic obstructive pulmonary disease, and HIV/AIDS, can develop severe physical, psychosocial, and spiritual symptoms before death. There is strong evidence that palliative care is beneficial in reducing much of this suffering in patients, as well as psychosocial and spiritual or existential distress in families.
Journal of Palliative Medicine Special Report
Who is Responsible for Palliative Care?
There are many parties involved in the development, planning and delivery of palliative care in Canada. These parties range from the funders of services by governments and foundations, the planners and coordinators of services in provincial, territorial or sometimes regional and local health departments; researchers and data collection officers who consider all of the complex issues related to palliative care and how to capture information in order to make informed policy and program decisions. On a more personal level, health care providers, either specialist or non-specialist, provide a variety of treatments and pain and symptom management; while counsellors, volunteers and community members provide respite care, spiritual, grief and bereavement supports, among many others. At the centre of all of these parties, are the people receiving care, their families and caregivers. They too have a role and responsibility in the provision of palliative care in Canada.
With so many responsible parties, and individual P/Ts working from their own palliative care strategies or policies, there are differences across the country in how people receive palliative care.
Through consultations with federal departments, P/Ts, and stakeholder organizations, we were able to see what palliative care programs are currently being provided across Canada. (See Appendix B: Overview of Palliative Care in Canada for more information.)
Government of Canada
Over the years, the federal government has taken action to improve access and quality of palliative careFootnote 8. The following federal initiatives supported the action P/Ts and non-governmental organizations are undertaking to improve palliative care in Canada:
Policy Development
- Recommendations from Special Senate Committees examining end-of-life care (1995 and 2000);
- Appointment of Senator Sharon CarstairsFootnote 9 as Minister with Special Responsibility for Palliative and End-of-Life Care (2001-03);
- Canadian Strategy on Palliative and End-of-Life Care (2002-07): coordinated by Health Canada, five working groups included experts from across the country;
- Employment Insurance Compassionate Care Benefits and the Caregiver Benefit, which enable Canadians to take leave from work to be with a family member who is seriously ill (updated 2017);
- Appointment of a Minister of Seniors, who shares responsibility with the Minister of Health for ensuring government investments in home and palliative care have their intended impacts (2018); and
- Revision of Palliative Care Guidelines and increased palliative care competencies for health care providers in correctional institutions by Correctional Services Canada (2018).
Funding Support
- Development of a framework to integrate a palliative approach to care across settings and providers (the Canadian Hospice Palliative Care Association's (CHPCA's)"The Way Forward initiative"), and a consensus process for determining Canadians' palliative care priorities (Palliative Care Matters);Footnote 10
- Support for development of resources and processes for training health care providers in palliative care (Pallium Canada);
- Support for Pan-Canadian organizations such as the Canadian Institute for Health Information (CIHI), Canadian Foundation for Healthcare Improvement (CFHI), and Canadian Partnership Against Cancer (CPAC), which are working to identify gaps and opportunities for improving access to palliative care in a range of settings, and measurement of outcomes.
Research
- 2004-2009: research funding of $16.5 million through the Canadian Institutes of Health Research (CIHR) to expand the volume and types of palliative care research.
- 2012-2017: research funding by CIHR of $494 million to support research on aging - some of which directly impacts palliative care, e.g. $14.8 million on research related to palliative care in cancer. As well other investments indirectly support palliative care, e.g., the Team Grant in Late Life Issues - a four year grant of $2.8 million to build research capacity and provide high-quality evidence to inform health and social care professionals and policy makers.
Provincial and Territorial Governments
As described in the map that follows, most P/T governments have strategies or policies that address improvements to palliative care. Actions to improve palliative care can draw from and build on best practices from across the country to help identify opportunities and address gaps. More detailed descriptions of provincial and territorial palliative care programs are found in Appendix B, and best practices can be found in Appendix C.
Map of Provincial and Territorial Palliative Care Programs and Policies
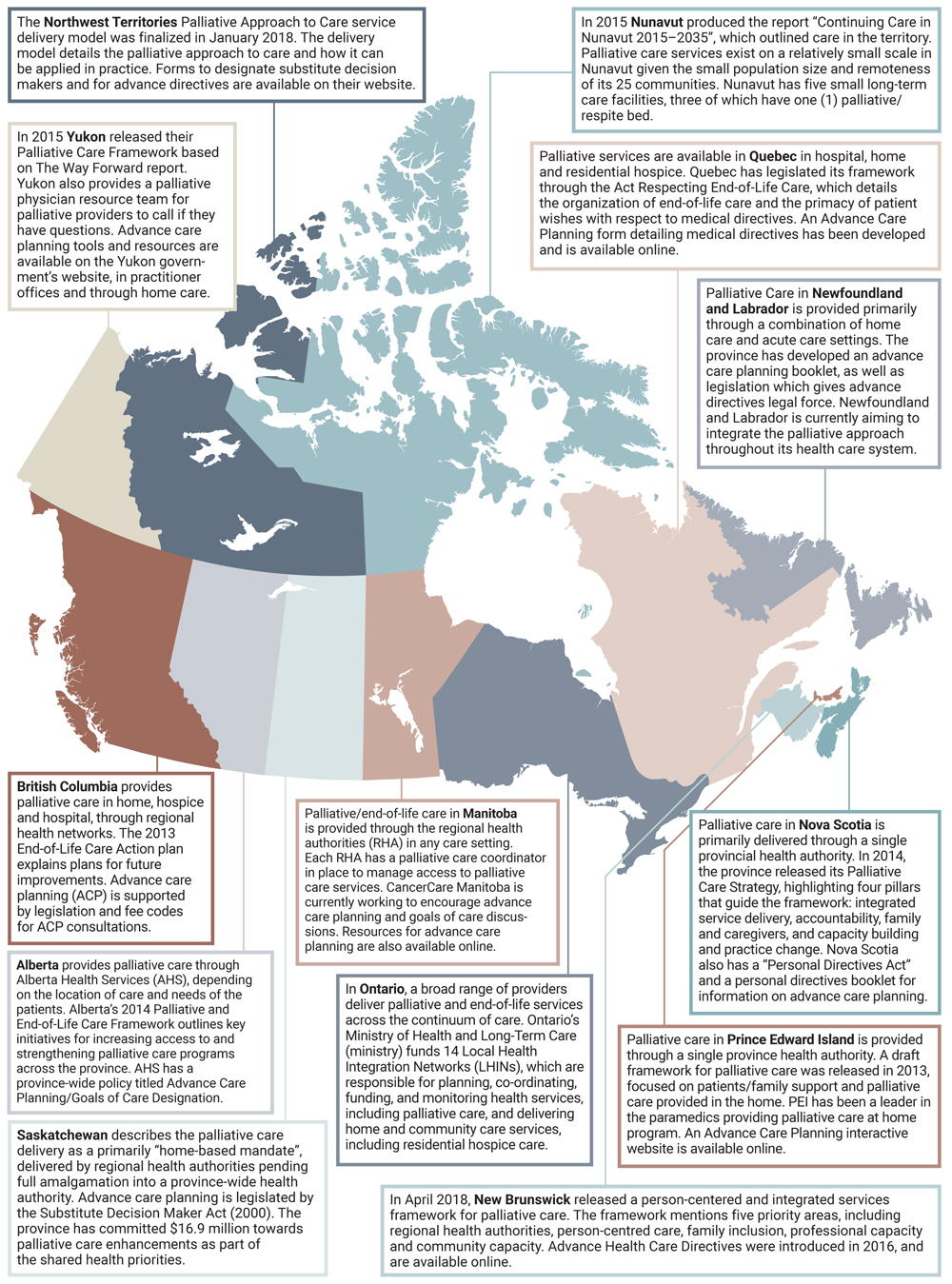
Text Description
The image is a map of Canada, with each province and territory highlighted in a different colour. Below the map are brief descriptions of palliative care in each province and territory. These are the descriptions:
The Northwest Territories Palliative Approach to Care service delivery model was finalized in January 2018. The delivery model details the palliative approach to care and how it can be applied in practice. Forms to designate substitute decision makers and for advance directives are available on their website.
In 2015 Yukon released their Palliative Care Framework based on The Way Forward report. Yukon also provides a palliative physician resource team for palliative providers to call if they have questions. Advance care planning tools and resources are available on the Yukon government's website, in practitioner offices and through home care.
In 2015 Nunavut produced the report "Continuing Care in Nunavut 2015-2035", which outlined care in the territory. Palliative care services exist on a relatively small scale in Nunavut given the small population size and remoteness of its 25 communities. Nunavut has five small long-term care facilities, three of which have one (1) palliative/respite bed.
British Columbia provides palliative care in home, hospice and hospital, through regional health networks. The 2013 End-of-Life Care Action plan explains plans for future improvements. Advance care planning (ACP) is supported by legislation and fee codes for ACP consultations.
Alberta provides palliative care through Alberta Health Services (AHS), depending on the location of care and needs of the patients. Alberta's 2014 Palliative and End-of-Life Framework outlines key initiatives for increasing access to and strengthening palliative care programs across the province. AHS has a province-wide policy titled Advance Care Planning / Goals of Care Designation.
Saskatchewan describes the palliative care delivery as a primarily "home-based mandate", delivered by regional health authorities pending full amalgamation into a province-wide health authority. Advance care planning is legislated by the Substitute Decision Maker Act (2000). The province has committed $16.9 million towards palliative care enhancements as part of the Shared Health Priorities.
Palliative/end-of-life care in Manitoba is provided through the regional health authorities (RHA) in any care setting. Each RHA has a palliative care coordinator in place to manage access to palliative care services. CancerCare Manitoba is currently working to encourage advance care planning and goals of care discussions. Resources for advance care planning are also available online.
In Ontario, a broad range of providers deliver palliative and end-of-life services across the continuum of care. Ontario's Ministry of Health and Long-Term Care funds 14 Local Health Integration Networks (LHINs), which are responsible for planning, co-ordinating, funding, and monitoring health services, including palliative care, and delivering home and community care services, including residential hospice care.
Palliative services are available in Quebec in hospital, home and residential hospice. Quebec has legislated its framework through the Act Respecting End-of-Life Care, which details the organization of end-of-life care and the primacy of patient wishes with respect to medical directives. An Advance Care Planning form detailing medical directives has been developed and is available online.
In April 2018, New Brunswick released a person-centered and integrated services framework for palliative care. The framework mentions five priority areas, including regional health authorities, person-centred care, family inclusion, professional capacity and community capacity. Advance Health Care Directives were introduced in 2016, and are available online.
Palliative care in Prince Edward Island is provided through a single province health authority. A draft framework for palliative care was released in 2013, focused on patients/family support and palliative care provided in the home. PEI has been a leader in the paramedics providing palliative care at home program. An Advance Care Planning interactive website is available online.
Palliative care in Nova Scotia is primarily delivered through a single provincial health authority. In 2014, the province released its Palliative Care Strategy, highlighting four pillars that guide the framework: integrated service delivery, accountability, family and caregivers, and capacity building and practice change. Nova Scotia also has a "Personal Directives Act" and a personal directives booklet for information on advance care planning.
Palliative Care in Newfoundland and Labrador is provided primarily through a combination of home care and acute care settings. The province has developed an advance care planning booklet, as well as legislation which gives advance directives legal force. Newfoundland and Labrador is currently aiming to integrate the palliative approach throughout its health care system.
Palliative Care Stakeholders
Individuals, families and caregivers are the core stakeholders in any discussion about palliative care. However, Canada also has a number of strong national and regional organizationsFootnote 11 with mandates and missions to improve access to palliative care. Many of these organizations are leaders in the field both within Canada and internationally. (See Appendix D for an Overview.) Some of the best practices from these organizations are highlighted throughout the Framework and many more are listed in Appendix C.
Through funding supports listed above, stakeholders improve access to palliative care through various means such as: promoting Compassionate CommunitiesFootnote 12 (CHPCA, Pallium Canada), developing resources and training health care providers in palliative care competencies (Canadian Society of Palliative Care Physicians (CSPCP), Pallium Canada), promoting advance care planningFootnote 13 (CHPCA), developing digital platforms to share knowledge and resources (Canadian Virtual Hospice (CVH), Carers Canada), supporting and promoting independent studies on palliative care (CIHR, Canadian Frailty Network (CFN)), convening experts and advocating on behalf of those living with life-limiting illness, their families and caregivers (Palliative Care Matters, Quality End-of-Life Care Coalition of Canada (QELCCC), CPAC). Many of these organizations have worked closely with all levels of government to provide input and guidance on palliative care programs and activities, as well as on the Framework consultations and development.
Roles and Responsibilities of Key Players
Individuals, Families, and Caregivers
- Promote their own well-being and care for their people (i.e., members of their family and friends)
- Express their perspectives/needs/preferences to guide their own care plans
- Actively participate in their community and broader society through community involvement (i.e., Compassionate Communities) Footnote 14
- Act as change agents in their community and champions of the vision, principles, and outcomes set out in the Framework
Non-Profit and Voluntary Sector
- Effectively represent people living with life-limiting illness and their families
- Act as a bridge between government and the public
- Provide a venue for collaboration and the sharing of knowledge and awareness
- Assist local communities in developing policies and programs appropriate to their needs
- Play a role in convening groups around shared interests and building system capacity
- Champion the vision, principles, and outcomes of the Framework
Health Care Systems/Organizations
- Act as point of first contact for those requiring palliative care
- Prioritize end-of-life care and treatment plans based on the needs and preferences of people and their families
- Tailor care plans so that people and caregivers can access care when and where they need it
- Connect persons and families dealing with a life-limiting illness to community resources
- Where relevant, develop and advance clinical policy, establish best practices and create standards and measurement metrics
- Where applicable, facilitate service delivery and supports (either directly or indirectly)
Compassionate Communities/Organizations
- Listen to the needs of those that they serve and advocate for those with life-limiting illness
- Champion the vision, principles and outcomes of the Framework
Governments
- Local
- Encourage local-level nurturing and spread of Compassionate Communities and Compassionate Organizations
- Champion the vision, principles and outcomes of the Framework
- Provincial/Territorial
- Provide direct or indirect health care services and supports, identify and respond to opportunities and challenges as needed
- Convene groups and facilitate ongoing dialogue
- Encourage and support communities in addressing local needs
- Set standards and legislate to achieve goals
- Where applicable, provide funding and oversight to health system service delivery organizations to deliver palliative care
- Where applicable, fund and administer specific benefit programs (palliative care drug access programs, etc.)
- Support the generation and sharing of information and knowledge
- Provide resources and supports to enhance capacity to deliver palliative care
- Foster the development of a jurisdiction-wide culture that promotes the vision, principles and outcomes of the Framework
- Federal
- Provide fiscal transfers to P/Ts through the Canada Health Transfer
- Administer additional transfer of $6 billion to P/Ts for targeted investments into home, community and palliative care over 10 years (2017 - 2027)
- Support and deliver programs and services (Employment Insurance Compassionate Care Benefit, and the Caregiver Benefit, etc.)
- Provide health care services to mandated populations such as First Nations, Inuit and Métis, veterans, and federal inmates
- Provide support for pan-Canadian organizations with mandates to address improvements to service delivery in targeted areas (Canadian Partnership Against Cancer (CPAC), Canada Health Infoway, etc.) and partners (Canadian Institutes of Health Research (CIHR), Canadian Agency for Drugs and Technology in Health (CADTH), etc.)
- Develop and implement policies and set standards to achieve goals, within federal role
- Provide cohesion for data collection to improve evidence and policy/program decisions
- Support research through the CIHR, knowledge translation through the CFHI, data and information collection through the CIHI
The Framework can be used by organizations with an interest in palliative care as they develop their policies and programs for the future.
What is the Purpose of the Framework?
According to the Economist Intelligence Unit's 2015 Quality of Death Index,Footnote 15 Canada has slipped from 9th to 11th out of 80 countries based on the availability, affordability and quality of palliative care. While the provision of palliative care has improved since its inception in the 1970's, a number of reports have identified ongoing gaps in access and quality of palliative care across Canada. There is considerable variation and disparity in palliative care services provided across Canada due to the fact that there are 14 different systems in place for providing care (13 P/T jurisdictions, as well as the Federal Government which has responsibility for mandated populations).
Recognizing the dynamic state of palliative care in Canada, the purpose of the Framework is to provide a tool for all parties with a responsibility for palliative care, to help shape decision making, organizational change, and planning within the current context. With the development of a common Framework, the Government of Canada aims to support policy and program decision making to ensure that Canadians are able to access high quality palliative care.
A Word about Policy Frameworks…
Policy frameworks are multipurpose tools. They can guide decision making, set future direction, identify important connections, and support the alignment of policies and practices, both inside and outside an organization. In short, policy frameworks are blueprints for something one wants to build, or roadmaps for where one wants to go.
An Act providing for the development of a framework on palliative care in Canada
In December 2017, Parliament passed into law An Act providing for the development of a framework on palliative care in Canada.Footnote 16 (See Appendix E)
The Act required the Minister of Health to conduct consultations with P/Ts and palliative care providers, to inform the development of a framework. The Government of Canada recognized the complexity of palliative care, and so, in keeping with a person-centred approach, the consultation process was expanded to include people living with life-limiting illness, families and caregivers, underserviced populations, non-governmental organizations, health care providers, and researchers to help shape the Framework.
How the Framework was Developed
In May 2018, the Health Canada launched a broad, multi-pronged consultation process, designed to reach Canadians, health care providers, caregivers, people living with life-limiting illness, and subject matter experts. The process used multiple platforms and networks in order to reach out across the country:
- An on-line discussion platform with moderated discussions covered palliative care definition, person- and family-centred care, advance care planning, access issues for those with unique barriers, caregiver supports, grief and bereavement, and community engagement.
- A Federal/Provincial/Territorial Reference Group shared information on existing and planned palliative care policies and programs across the country.
- An Interdepartmental Working Group of federal departments and agencies with a specific interest in palliative care including the departments of Citizenship, Immigration and Refugees, Correctional Services Canada, Indigenous Services Canada, Employment and Social Development Canada, the Public Health Agency of Canada, and Veterans Affairs, shared information on programs and services.
- Twenty-four bilateral discussions and focus groups were held with key stakeholders representing specific populations that face challenges accessing palliative care (such as perinatal, infants, children, adolescents and young adults, homeless, members of the lesbian, gay, bisexual, transgender, queer, two-spirit, (LGBTQ2) community, etc.); other government departments (particularly those with service delivery mandates); Health Portfolio partners like CIHR; and pan-Canadian organizations, such as CFHI and CPAC.
- Two roundtables with people living with life-limiting illness, and families of children who had received palliative care, were held in September 2018.
- A face-to-face meeting of stakeholders including: people living with life-limiting illness, caregivers, palliative care providers and experts, and representatives from several P/Ts was held to discuss consultation results, and provide input on elements of the Framework in September 2018.
These consultations were vital to shaping the Framework on Palliative Care in Canada.
Canada's Indigenous Peoples
Representatives of Canada's Indigenous peoples have been clear about the importance of culturally-appropriate palliative care for their communities. Health Canada and National Indigenous Organizations have started and will continue a discussion about Indigenous-led engagement toward the development of a distinctions-based framework on palliative care for Indigenous peoples, reflecting the specific and unique priorities of First Nations, Inuit and the Métis Nation.
PART II - The Framework on Palliative Care in Canada
The Framework reflects a collective vision for palliative care aiming to ensure Canadians have the best possible quality of life, right up to the end of life.
Vision
All Canadians are touched by end-of-life care issues, either for themselves, or for someone they know. Our vision is for all Canadians with life-limiting illness to experience the highest attainable quality of life until the end of life.
The Framework has three main objectives:
- To clarify what we are trying to achieve, how to get there, and the various roles and responsibilities of those involved;
- To align activities within and between the different levels of government, to harmonize work between governments and other stakeholders, and to ensure there is policy alignment and consistency; and
- To influence and guide the work of governments, health care providers and non-profit organizations to improve palliative care for Canadians, as well as provide overall direction to collective planning and decision making.
The Framework is laid out in the following sections:
- Guiding Principles
- Goals and Priorities related to:
- Palliative care training and education for health care providers and other caregivers
- Measures to support palliative care providers and caregivers
- Research and the collection of data on palliative care
- Measures to facilitate equitable access to palliative care across Canada
- What Success Looks Like
- Framework Blueprint
A good death is an important part of a good life.
Amy Albright
University of Alabama
Psychological Benefits Society
Guiding Principles
In the spirit of bringing greater clarity and consistency to conversations about palliative care in Canada, the Framework sets out ten Guiding Principles. These principles were developed in consultation with people living with life-limiting illness, caregivers, P/Ts, and other stakeholders, and are considered to be fundamental to the provision of high-quality palliative care in Canada. They should be considered and reflected in program and policy design and delivery.
Palliative care is person- and family-centred care
Palliative care is respectful of, and responsive to, the needs, preferences and values of the person receiving care, their family, and other caregivers. It is facilitated by good communication. Individuals and families have personal preferences and varying levels of comfort in discussing, and planning for the dying process and death itself.
Death, dying, grief and bereavement are a part of life
A cultural shift in how we talk about death and dying is required to facilitate acceptance and understanding of what palliative care is and how it can positively impact people's lives. The integration of palliative care at the early stages of life-limiting illness facilitates this culture shift by supporting meaningful discussions among those affected, their families and caregivers regarding care that is consistent with their values and preferences.
Caregivers are both providers and recipients of care
Given their unique role in supporting individuals, family and other caregivers are respected by the health care team for their knowledge of the care preferences and needs of the person with a life-limiting illness. Palliative care encompasses the health and well-being of caregivers, and includes grief and bereavement support.
Palliative care is integrated and holistic
Palliative care is integrated with other forms of care (such as chronic illness management) throughout the care trajectory, and across providers. Services are provided in a range of settings (such as homes, long-term and residential care, hospices, hospitals, homeless shelters, community centres, and prisons). It is holistic, addressing a person's and their family's full range of needs - physical, psychosocial, spiritual, and practical - at all stages of a chronic progressive illness. It requires standardized or shared data systems in order to coordinate care during transitions from one setting or provider, to another.
Access to palliative care is equitable
Canadians with a life-limiting illness have equitable access to palliative care, regardless of the setting of care or personal characteristics, including, but not limited to their:
- Illness(es)
- Age
- Canadian Indigenous peoples status
- Religion or spirituality
- Language
- Legal status with respect to citizenship or incarceration
- Sex, sexual orientation or gender identity
- Marital or family status
- Race, culture, ethnicity, or country of origin
- Economic or housing status
- Geographic location
- Level of physical, mental and cognitive ability
A palliative approach to care requires adaptability, flexibility and humility on the part of the health care provider and the health system, in order to reach a shared understanding of the needs of each individual.
Palliative care recognizes and values the diversity of Canada and its peoples
Canada is a diverse country. Our population consists of myriad ethnic backgrounds, languages, cultures and lifestyles. While diversity is a natural characteristic of every society, being inclusive is a choice. Just as we Canadians pride ourselves on embracing our diversity and on being inclusive, palliative care recognizes Canada's diversity and encourages the adoption of inclusiveness, paying special attention to ensure that underserviced populations are taken into consideration as we aspire to universal access to palliative care.
Palliative care services are valued, understood, and adequately resourced
Palliative care helps identify and respond to people's physical, psychosocial, emotional and spiritual needs early, particularly when coupled with advance care planning. It can also avoid costly, ineffective measures that do not contribute to improving an individual's quality of life. The appropriate use of technology, community-engagement models, and public education are integral to delivering palliative care.
Palliative care is high quality and evidence-based
Program and policy decisions on palliative care are informed by evidence and relevant data. As such, research and data collection must be adequately supported to establish and validate an evidence base necessary for policy decisions and program planning.
Palliative care improves quality of life
Palliative care reduces suffering and improves quality of life for people with life-limiting illness and their families. Palliative care is appropriate for persons of all ages, with any life-limiting illness, and at any point in the illness trajectory. It includes support for family and other caregivers, including in their grief and bereavement. A palliative approach to care may be offered by a broad range of care providers and volunteers, in any setting.
Palliative care is a shared responsibility
The delivery of palliative care in Canada is the shared responsibility of all Canadians. This Framework encourages everyone, in their respective capacity, to work together to achieve the goals set out in this Framework on Palliative Care in Canada.
Goals and Priorities
The following goals and priorities were created in consultation with people living with life-limiting illness, their families, caregivers, P/Ts, other federal departments, and stakeholders. They are designed to guide short term (1 - 2 years), medium term (2 - 5 years) and long term (5 - 10 years) action to reach a shared vision on palliative care.
Given the complex, cross-sectoral nature of palliative care, no one party can be responsible for all of these priorities. They belong to all those involved with palliative care, including persons living with life-limiting illness, caregivers, all levels of government, communities, not-for-profit organizations, health care providers, the voluntary sector, and all Canadians.
Different organizations/institutions may choose to implement one or several of the priorities that follow, and will do so according to their own priority setting exercises. The timeframe over which these priorities span is dependent on who/which organization is implementing them.
The four priority areas for action in the Framework are as follows:
- Palliative care training and education for health care providers and other caregivers;
- Measures to support palliative care providers and caregivers;
- Research and the collection of data on palliative care; and
- Measures to facilitate equitable access to palliative care across Canada
Palliative care training and education for health care providers and other caregivers
A robust and skilled health workforce is essential to future sustainable palliative care delivery. There are many opportunities to improve ways in which health care providers, caregivers, and volunteers are trained, with some promising practices that can be expanded to meet this need. The following priorities refer to training and education programs for both health care professionals and informal care providers (caregivers, volunteers).
- Short term goal: training and education needs are identified for health care providers as well as other caregivers
- Medium term goal: palliative care providers have access to training, education and tools to meet the goals of individuals and their caregivers
- Long term goals: all providers have increased capacity to deliver quality care, and caregivers have appropriate supports to perform their roles
Priorities:
- Position individuals and their families and caregivers as central to palliative care training; ensure their cultural diversity is respected in the development of new tools and resources, including consideration of age-specific needs
- Work with Indigenous peoples to develop and disseminate mandatory cultural competency guidelines
- Work with organizations serving underserviced populations to develop and disseminate competency training for the provision of appropriate care for those populations
- Promote existing or establish new national standardized/accredited education for all health disciplines
- Develop national core competencies for palliative care specialists, and all other health care providers, including unregulated providers, such as personal support workers, etc., with a goal of equipping future health care providers with the competencies and skill base to provide palliative care services appropriate to the needs of the population being served
- Support the development of mandatory palliative care courses as part of undergraduate health provider curricula
- Explore best practice models that integrate palliative care training and education for interdisciplinary teams and others (support staff, volunteers, caregivers, etc.), including communication skills, and advocacy training as core competencies
- Ensure all training and education considers the continuum of care across all settings
- Invest in tool and resource development to ensure training programs are accessible and sustainable
- Develop an awareness campaign targeted to all health disciplines to improve awareness and understanding of the benefits of early integration of palliative care into treatment plans
Best Practices in Palliative Care Training and Education for Health Care Providers and Caregivers
Learning Essential Approaches to Palliative Care (LEAP)
Pallium Canada's LEAP courses, clinical decision and support tools, and toolkits provide learners with the essential, basic competencies of the palliative care approach.
Nursing Curriculum Resources Canadian Association of Schools of Nursing - Palliative and end-of life care teaching and learning resources for nurse educators.
Nova Scotia Palliative Care Competency Framework
Shared and discipline-specific competencies for health professionals and volunteers who care for people with life-limiting conditions and their families in all settings of care.
Just knowing about options is often the biggest barrier to receiving help… Awareness of bereavement supports is (also) really important. - Family Caregiver
Measures to support palliative care providers and caregivers
While many innovative supports exist across Canada, there is often a lack of awareness about them, and how to tap into them. Raising public awareness of these resources and the benefits of palliative care more generally would benefit palliative care providers, as well as their patients, clients, and other elements of the health care system. Improved understanding of existing programs helps to identify gaps and spur innovation to address them.
- Short term goal: supports required for palliative care providers and caregivers are identified, taking into account the range of wishes and needs of people with life-limiting illness
- Medium term goals: caregivers and providers are aware of and can access supports to meet the goals of the individual and their caregivers; there is an increased awareness of palliative care, and uptake of advance care planning and advance directives
- Long term goal: Canadians and caregivers understand and plan for palliative care and develop advance care plans
Priorities:
- Include caregiver assessment to understand the unique needs and capacity of each caregiver
- Explore effective models of consistent processes that ensure family members are involved in care planning and relevant care decisions
- Promote the use of technology to enhance communication between specialized palliative care providers and community-based care providers, including caregivers
- Examine how equitable access to bereavement supports and services can be established
- Build greater care capacity in communities (e.g. by fostering the Compassionate Communities movement) to alleviate pressure on health care systems and caregivers
- Ensure supports and services are culturally appropriate and available in both official languages
- Develop local public awareness campaigns in order to inform caregivers of the supports and services available to them
Best Practices in Measures to Support Palliative Care Providers and Caregivers
Canadian Virtual Hospice
Website providing information, an interactive "Ask a Professional" feature, and videos on "Living My Culture", "Indigenous Voices" and caregiving tasks.
MyGrief.ca and KidsGrief.ca
Free online grief and bereavement resources. Developed by a team of national and international grief experts together with people who have experienced significant loss.
Caregiver Compass
Tips and tools to help caregivers manage their responsibilities, including communication and decision making, navigating the health care system, financial and legal matters.
Research and the collection of data on palliative care
Sustained research and data collection is vital for long-term and continuous improvement in palliative care. Evidence is needed to address knowledge gaps, overcome current challenges and drive innovation towards effective practices. Ultimately, improved data collection and research will enhance the quality of life for all Canadians living with life-limiting illness and their families and caregivers, by providing much-needed data and evidence to drive improvements and support new models and approaches to care.
When the state of publicly funded palliative care in Canada is understood, health system planners can identify service gaps and develop strategies for improving care.
Access to Palliative Care in Canada
CIHI, 2018
- Short term goal: existing research and data collection gaps are identified
- Medium term goals: research is undertaken, applied, and promoted; and data collection activities are planned and reported to align with policy goals
- Long term goal: research, data collection, and best practices are implemented to inform and support policy decisions and government directions about palliative care
Research Priorities:
- Develop the evidence base for non-medical aspects of palliative care to promote comprehensive palliative care services, including psychosocial and spiritual supports
- Promote new and existing research networks and other collaborative processes, valuing quantitative and qualitative research
- Develop economic models and methodologies for further integrating palliative care into home and long-term care settings
- Promote models of care where primary health care professionals (e.g. family physicians or nurse practitioners) provide the majority of ongoing care and support, consulting with palliative care specialists only as needed
- Leverage existing work (i.e. Pan-Canadian Framework for Palliative and End-of-Life Care Research and its three main focus areas: Transforming Models of Caring; Patient and Family Centredness; and Ensuring Equity)
- Disseminate new evidence
- Ensure best practices are implemented across health care systems
- Build on current expertise and explore mechanisms to continue developing capacity in all aspects of palliative care research through a multidisciplinary approach that generates new knowledge, addresses gaps and improves care practices.
Data Priorities:
- Develop and promote the use of standardized person- and family-reported outcomes and experience measures, as well as screening and assessment tools across all settings
- Develop precise indicators related to palliative care, including distinctions-based approaches
- Work with national/international survey developers to add palliative care questions, including information on community care and Compassionate Communities (Census, Canadian Community Health Survey, General Social Survey, etc.)
- Use existing big data sources for more than one purpose and link databases to improve efficiencies in data collection and analysis
- Improve data collection on the uptake and consistency of advance care plans, focusing on where, how and by whom they are most used.
Best Practices in Measures to Improve Research and the Collection of Data on Palliative Care
Canadian Institute for Health Information
CIHI's 2018 report, Access to Palliative Care in Canada provides the baseline for what we know about palliative care service provision, across settings, in the last year of life.
Pan-Canadian Framework for Palliative and End-of-Life Care Research (Canadian Cancer Research Alliance, 2017)
This framework aims to build capacity to address unmet needs and broaden the scope of palliative care research for the future.
Improving End-of-Life Care and Advance Care Planning
The Canadian Frailty Network is supporting a program of research on end-of-life care planning and decision making, to improve the care of older adults living with frailty, their families and caregivers.
Measures to facilitate equitable access to palliative care across Canada
A consistent challenge to accessing quality palliative care stems from the lack of specialized palliative care providers in Canada. However, not all people receiving palliative care require highly specialized care. In fact the majority of them can have high quality palliative care provided by their caregivers, family doctors, nurses, nurse practitioners, social workers, personal support workers, volunteers, and members of the community.
The following figure is a conceptual model of level of need of care for a person living with life-limiting illness, aligned against health care provider involvement. The base of the triangle represents the majority of individuals receiving palliative care, who require minimal specialist care, and whose symptoms can be managed effectively in home and community settings by their primary health care teams, caregivers and through community supports. This majority can benefit from a "palliative approach to care", which integrates core elements of palliative care into the care provided by non-specialists. As the complexity of needs increases, the health care providers become more specialized, but the number of people requiring this level of care is lower. This minority of people at the top of the triangle require the skills of palliative care specialists, often provided in the hospital or hospice setting.
Person's Needs vs. Relative Workforce Involvement

Figure developed by Palliative Care Australia, for the Palliative Care Service Development Guidelines, January 2018. It was kindly shared with Health Canada for the Framework on Palliative Care in Canada.
Text Description
A diagram shows six sets of figures side by side.
On the far left is a vertical arrow pointing upward, divided from bottom to top, in three equal thirds.
To the right of the arrow, is a triangle pointing upward, divided from bottom to top, in equal thirds.
To the right of the triangle is a set of three horizontal arrows pointing to the right, each starting from the middle of each of the thirds of the triangle.
To the right of the three arrows is a set of three rings of different sizes. The largest circle is at the bottom, the middle circle is in the center and the smallest circle is at the top.
Above the triangle is a rectangle and above the circles is another rectangle.
Sixth, at the base of the diagram are two miniature circles, red and one blue. The red circle indicates the predominant use of palliative care specialists. The blue circle indicates the predominant use of other health professionals.
To the far left, the arrow is labeled on the right with the words: "Increasing Complexity of Palliative Care Needs". The arrow is divided into three colours, red to the upper third, royal blue to the central third and dark blue to the lower third.
The triangle, to the right of the arrow, is divided into three colours, pale blue in the upper third, royal blue in the central third and dark blue in the lower third. The three arrows, to the right of the triangle, are pale blue with writing in them. The top arrow is labeled "Complex and Persistent". The center arrow is labeled "Intermediate and variable". The bottom arrow is labeled "Straightforward and predictable".
Each of the three circles to the right of the arrows are divided into two colours, red to the upper portion, royal blue to the lower portion. They differ in colouring with the upper circle being mostly red, the middle being almost equally red and blue, and the bottom circle being mostly blue - representing the intensity of specialist care compared to other health professionals.
Finally the rectangle above the triangle is black. It says "Person’s needs" and the rectangle above the circles is labeled "Relative workforce involvement".
The figure demonstrates that simple and predictable care requires about 25% of specialized palliative care providers and 75% of other health professionals. Intermediate and variable care requires an equal distribution of specialized palliative care providers and other health professionals. Complex and persistent care requires 75% of specialized palliative care providers and 25% of other health professionals.
This modelFootnote 17 requires non-specialist health care providers to have basic palliative care competencies and the ability to access specialists for advice, consultation, and referral when necessary. This aligns with the models of care already provided in Canada where primary care providers and specialists work together in areas such as cardiac or cancer care.
Shoring up these skills among non-specialist care providers would allow for more Canadians to have access to palliative care at the primary care level. This approach also allows for more active involvement of community, family and caregivers. Combining this model with movements such as Compassionate Communities, would be a significant step in providing full coverage and access to supports to improve quality of life through to the end of life. Furthermore, it provides for a more effective use of health resources, and allows the person living with a life-limiting illness to remain in the setting of their choice for as long as possible (e.g., home or community care).
Access issues are complex and occur in all settings, whether in dense urban settings or rural and remote regions of Canada. Many Canadians have difficulty accessing high quality palliative care due to system capacity issues, lack of understanding of the benefits of palliative care among health care professionals and the public, geography and demographic diversity (e.g., age, gender, culture, etc.).
- Short term goal: best practices and barriers to consistent access to palliative care are identified
- Medium term goals: mechanisms to facilitate consistent access are advanced and barriers are addressed; and action aligned with the Framework is taken at multiple levels (e.g., governments, stakeholders, caregivers, and communities) to improve palliative care and achieve the goals of individuals with life-limiting illness
- Long term goals: all individuals with life-limiting illness and their caregivers benefit from a palliative approach to care with all players cooperating to help achieve the goals of individuals throughout the continuum of care.
Priorities:
- Explore models of "patient (and caregiver) navigators" to promote the adoption of a single point of contact for individuals, their families, and caregivers when accessing the health care system - this is particularly important for those with cognitive impairments (e.g., Alzheimer's) as their illness gradually impacts their ability to navigate the health care system independently
- Promote access to telephone and electronic consultations (available 24/7) with interdisciplinary palliative care teams for individuals, families and caregivers to reduce hospital visits and support personal preferences to remain at home as long as possible
- Map national and local palliative care services and supports to highlight what is available but not well known, and where gaps exist
- Undertake awareness campaigns to promote existing services identified above, and more generally, the benefits of early integration of palliative care to improve quality of life for those suffering life-limiting illness and their families and caregivers
- Introduce discussions about death and dying in non-medical settings (such as schools, workplaces, etc.) to increase comfort in the subject and integrate the concept into daily life
- Increase the number of clinical and non-clinical service providers who are skilled in assisting individuals and their families and caregivers to have culturally sensitive discussions on end-of-life care including the development of advance care plans
- Define palliative care integration strategies within health care systems and regional health authorities, to implement across care settings and in the community, always through a culturally sensitive, age-appropriate lens
- Develop partnerships and linkages between health care providers, volunteers and community organizations to build inter-professional teams that deliver distinctions-basedFootnote 18 palliative care
- Recognize and ensure the continued inclusion of lay and spiritual counsellor positions in inter-professional health care teams to increase access to non-medical aspects of palliative care
- Invest in community-based initiatives to scale up and spread innovative models designed to improve access to palliative care services where and when they are needed, particularly for underserviced populationsFootnote 19
- Promote uptake of Compassionate Communities across Canada
- Develop services related to anticipatory grief and adjustment to losses before death to complement existing bereavement services.
All of the priorities identified above will have a positive impact on underserviced populationsFootnote 20; however, the following are more specific to their unique needs:
- Focus concerted efforts on increasing and improving remote consultation capacity
- Scale up and spread successfully proven models designed to increase community capacity in rural and remote areas, (e.g., Kelley Model for Developing Palliative Care Capacity, see Appendix C)
- Explore community-based approaches to specific illness or frailty, e.g., dementia friendly communities, Age-Friendly Communities, and Ontario's Schlegel Villages as holistic health care villages
- Increase support for non-medical care models, such as recreational therapy proven to improve communication in non-verbal children to express values and desires, ultimately improving quality of life
- Develop palliative care policies, programs, and services that are inclusive and considerate of all ages, sex and gender, and cultural diversity.
Best Practices in Measures to facilitate equitable access to palliative care
Palliative Education and Care for the Homeless (PEACH)
PEACH aims to meet the needs of homeless and vulnerably-housed patients with life-limiting illness via a "trailblazing" mobile unit, providing attentive care on the streets, in shelters, and with community-based services.
British Columbia Centre for Palliative Care (BCCPC) Micro-Grants
Every year, the BCCPC gives small grants to 25 hospice societies and other non-profit organizations from across B.C., to help improve access to compassionate palliative care closer to home and empower people to have a voice in their own care through advance care planning.
Paramedics Providing Palliative Care at Home Program
Health authorities, cancer agencies and emergency medical services in Nova Scotia and Prince Edward Island collaborated with the CPAC and Pallium Canada to train all paramedics to support palliative patients at home. An interim analysis has revealed that paramedics are able to keep patients with palliative goals of care at home 55% of the time, when previously, nearly all would have been transferred to hospital. A similar program was implemented in Alberta.
With the adoption of the actions laid out in the priority areas, and concerted effort at all levels, we will see improvements in access to palliative care across Canada. The following table outlines some of the shifts in policy and programming we can bring about through this work:
What Success Looks Like - Shifts in Palliative Care Policies and Programming
| Less of… | More of…. |
|---|---|
| Palliative care treatment plans are focused primarily on controlling physical symptoms such as pain. | Palliative care is holistic, addressing the physical, psychosocial, spiritual, and practical concerns of the person and their family. An inter-professional team is mobilized, where possible, to support the full range of concerns, as needed. |
| Palliative care treatment plans are decided by the health care provider(s). | Palliative care is developed in partnership with the person living with life-limiting illness and their family, and respects their values, culture and preferences. |
| Palliative care is offered almost exclusively in last weeks of life. | Palliative care at appropriate levels is offered as early as diagnosis of a life-limiting illness. |
| Palliative care is discussed only after all other medical interventions are exhausted. | Palliative care is provided in conjunction with other medical interventions. Treatment plans are designed to improve quality of life through to the end of life. |
| Palliative care is only provided by specialists. | All health care providers (regulated or not) have foundational skills to provide a palliative approach to care, supported by specialists as needed. |
| Palliative care is delivered predominantly in hospitals. | Palliative care is available in the home setting or other setting of choice. |
| Access to palliative care is uneven across the country both by location and population. | Innovations and technology are used to ensure that palliative care supports and services are available to those who need them, regardless of where they live or their personal characteristics. |
| Caregivers are on the periphery of the health professional team, but may not be a part of the decision making or care planning. | Caregivers are central to the treatment planning process, respected and consulted as knowledgeable members of the care team, and provided with appropriate training and respite care. |
| There are no national standards for data collection or use, and few person-centred outcome or experience measures. There is insufficient support for research specific to palliative care. | Data are standardized or linkable across care settings and providers, and include measures of the outcomes and experiences of persons with life-limiting illness and their families. There are ongoing and sufficient financial and infrastructure resources to support data systems and research which provide the evidence base for improvements in palliative care. |
Following is a Blueprint - a summary of the Vision, Definition, Guiding Principles, and Short, Medium and Long Term Goals identified through the consultation on palliative care. This Blueprint is a tool that can be used to find common understanding and focus for policy makers and planners in the Canadian palliative care context.
Framework on Palliative Care in Canada - Blueprint
Guiding Principles
- Palliative Care is Person- and Family-Centred
- Death, Dying, Grief and Bereavement are Part of Life
- Caregivers are Both Providers and Recipients of Care
- Palliative Care is Integrated and Holistic
- Access to Palliative Care is Equitable
- Palliative Care Recognizes and Values the Diversity of Canada and its Peoples
- Palliative Care Services are Valued, Understood, and Adequately Resourced
- Palliative Care is High Quality and Evidence-Based
- Palliative Care Improves Quality of Life
- Palliative Care is a Shared Responsibility
Vision: All Canadians with life-limiting illness live well until the end of life
- Long Term Goals 5-10 Years
- Canadians and caregivers understand and plan for palliative care, and develop Advance Care Plans
- All providers have increased capacity to deliver quality care, and caregivers have appropriate supports to perform their roles
- All Canadians and caregivers have consistent access to an integrated palliative approach to care
- Research, data collection and best practices support and inform policy decisions and government directions about palliative care
- Governments, stakeholders, caregivers and communities cooperate to help achieve the goals of Canadians during the entire period of care
- Medium Term Goals 2-5 Years
- There is an increased awareness of palliative care, and greater understanding and uptake of advance care planning and advance care directives
- Palliative care providers have access to training, education, and tools to meet the goals of individuals and their caregivers
- Caregivers and providers are aware of and can access supports to meet the goals of the individual and their caregivers
- Mechanisms to facilitate consistent access are advanced, and barriers are addressed
- Research is undertaken, applied, and promoted, and data collection activities are planned and reported to align with policy goals
- Action aligned with the Framework is taken at multiple levels (governments, stakeholders, caregivers, and communities) to improve palliative care and achieve the goals of individuals with life-limiting illness
- Short Term Goals
- The range of wishes and needs of people with life-limiting illness are identified
- Training and education needs are identified for health care providers and caregivers
- Supports required for palliative care providers and caregivers are identified
- Best practices and barriers to consistent access to palliative care are identified
- Existing research and data collection gaps are identified
- A common framework is developed to guide action and improve access to palliative care in Canada
Palliative Care Definition: An approach to care that improves the quality of life of people of all ages who are facing problems associated with life-limiting illness, and their families. It prevents and relieves suffering through the early identification, correct assessment and treatment of pain and other problems, whether physical, psychosocial or spiritual.
PART III - Implementation and Next Steps
The goals and priorities laid out in this Framework were identified through consultation with people living with life limiting illness, caregivers, stakeholders and P/Ts; they include possible actions for all parties.
Moving forward, the federal government will collaborate with interested parties to develop a plan to implement those elements of the Framework that fall under federal responsibility. Although the timeframe of the Framework development process did not allow for a thorough engagement process with Indigenous peoples around palliative care, ongoing work will include discussions between Health Canada and National Indigenous Organizations about Indigenous-led engagement processes toward the development of a distinctions-based palliative care framework for Indigenous Peoples. This framework would respect the specific unique priorities of First Nations, Inuit and the Métis Nation. The implementation plan will also include the creation of an Office of Palliative Care, which is laid out in more detail below.
The Office of Palliative Care
The Framework on Palliative Care in Canada Act requires the Minister of Health to evaluate the advisability of re-establishing Health Canada's Secretariat for Palliative and End-of-Life Care. From 2001 to 2003, the Government of Canada appointed a Minister with Special Responsibility for Palliative Care (the Honourable Sharon Carstairs). A Strategy on Palliative and End-of-Life Care was implemented from 2002 to 2007. In order to support this Minister and coordinate efforts on the Strategy, Health Canada established a time-limited Secretariat. While the Secretariat ended in 2007, federal initiatives on palliative care continued.
Given the inter-jurisdictional, cross-sectoral nature of the issues identified in the development of the Framework, a single focal point is needed to help connect and facilitate activities at various levels seeking to improve access to palliative care in Canada. As such, Health Canada will establish the Office of Palliative Care (OPC) to provide high level coordination of activities going forward. The OPC will be resourced internally through existing funds within Health Canada.
In order to support the implementation of the Framework, the new OPC could:
- Coordinate implementation of the Framework;
- Connect governments and stakeholders and palliative care activities across Canada;
- Serve as a knowledge centre from which best practices can be compiled and shared;
- Align activities and messaging to support public awareness raising across Canada; and
- Work with stakeholders to facilitate consistency of standards in palliative care.
Health Canada will continue to work with jurisdictions and key stakeholders to more clearly define the OPC's roles and responsibilities, and will consider existing models and networks for format and function to leverage resources and avoid duplication. Creation of the OPC will coincide with the development of the Framework implementation plan.
Conclusion
This Framework outlines the vision, goals and priorities expressed by consultation participants to improve palliative care in Canada. The priorities are complex and require the collaboration of all interested parties, including persons with life-limiting illness and caregivers, academia, health care delivery organizations, health professional groups, community organizations, and all levels of government - we all have a role to play.
Throughout Health Canada's consultations, participants not only shared their lived-experiences and wisdom, but also their innovative ideas and leadership. The resulting Framework is a tool that any level of government or health care or academic organization can use for decision making, to guide organizational change, to inform health care training and education, and for workforce planning. The Framework can be used by people living with a life-limiting illness and their families to facilitate end-of-life discussions with their primary care teams, to learn about best practices, and to explore what supports exist where they live.
Health care systems are not static - they evolve to respond to pressures and meet the needs of citizens. This Framework will also continue to evolve over time and will be revisited by those who contributed to it, in order to ensure it reflects the current state of palliative care in Canada; roles will continue to be clarified and definitions will evolve with increased data collection and research. This is a living document - designed to be a starting place for continuous open dialogue as we address challenges and culture shifts together.
Bibliography
- Aged Care Guide. (n.d.). Care Plan. Accessed from: https://www.agedcareguide.com.au/terms/care-plan
- Australian Commission on Safety and Quality in Health Care. (2017).National Safety and Quality Health Service Standards. 2nd ed. Sydney: ACSQHC.(https://www.safetyandquality.gov.au/search/quality+health+service+standards)
- Canadian Hospice Palliative Care Association. (March 2002). A Model to Guide Hospice Palliative Care: Based on National Principles and Norms of Practice. Ottawa, ON. Accessed from: (http://www.chpca.net/media/7422/a-model-to-guide-hospice-palliative-care-2002-urlupdate-august2005.pdf)
- Canadian Medical Association (2014-2015). Palliative Care - Canadian Medical Association's National Call to Action: Examples of innovative care delivery models, training opportunities and physician leaders in palliative care. Accessed from: https://www.cma.ca/Assets/assets-library/document/en/advocacy/palliative-care-report-online-e.pdf
- Canadian Society of Palliative Care Physicians. (2017). Palliative Care Lexicon. Accessed from: http://www.cspcp.ca/wp-content/uploads/2014/10/Palliative-Care-Lexicon-Nov-2016.pdf http://www.chpca.net/media/7763/LTAHPC_Lexicon_of_Commonly_Used_Terms.pdf
- Farlex Partner Medical Dictionary. (2012). End-of-Life. Accessed from: https://medical-dictionary.thefreedictionary.com/end-of-life
- Farlex Partner Medical Dictionary. (2012). Provider. Accessed from: https://medical-dictionary.thefreedictionary.com/provider
- International Association for the Study of Pain. (2018). Pain. Accessed from: http://www.iasp-pain.org/terminology?navItemNumber=576#Pain
- Journal of Palliative Medicine Special Report: PAL-LIFE White Paper for Global Palliative Care Advocacy is published by the « Journal of Palliative Medicine » (September 2018), in English and Spanish: (https://www.liebertpub.com/doi/10.1089/jpm.2018.0248)
- Palliative Care Australia. (2005). Standards for Providing Quality Palliative Care for all Australians. PCA, World Health Organization Definition of Palliative Care. Accessed from: (http://www.who.int/cancer/palliative/definition/en/)
- Palliative Care Australia. (2008). Palliative and End-of-Life Care - Glossary of Terms, Ed 1, PCA, Canberra: (http://files.mccn.edu/courses/nurs/nurs490r/MaurerBaack/PowerpointFiles/Mod.%206%20End%20of%20Life%20Care/Palliative%20and%20end%20of%20life%20care%20glossary%20of%20terms.pdf)
- Palliative Care Australia. (2018). National Palliative Care Standards. 5th Edition. Australia. Accessed from: http://palliativecare.org.au/wp-content/uploads/dlm_uploads/2018/02/PalliativeCare-National-Standards-2018_web-3.pdf
- Palliative Care Australia. (2018). What is Palliative Care? Accessed from: http://palliativecare.org.au/what-is-palliative-care
- Quality Compliance Systems. (2011). The Care Planning Cycle. Accessed from https://www.qcs.co.uk/care-planningcycle/
- Webster's New World College Dictionary. (2010). Canadian, 4th Edition. Houghton Mifflin Harcourt. Accessed from: https://www.collinsdictionary.com/dictionary/english/canadian
- Witt Sherman, Deborah, and Bookbinder, Marilyn. (2019) Palliative Care: Responsive to the Need for Health Care Reform in the United States. In Palliative Care Nursing: Quality Care to the End of Life, (5th Ed.), by Marianne Matzo and Deborah Witt Sherman (eds.), New York, NY: Springer Publishing Company.( https://books.google.ca/books?id=eGRgDwAAQBAJ&pg=PA285&dq=Palliative+Care+Nursing:+Quality+Care+to+the+End+of+Life,+(5th+Ed.),+by+Marianne+Matzo+and+Deborah+Witt+Sherman+(eds.),+New+York,+NY:+Springer+Publishing+Company.&hl=en&sa=X&ved=0ahUKEwiy64K-yNneAhUJWq0KHdt2ByEQ6AEIKDAA#v=onepage&q=Palliative%20Care%20Nursing%3A%20Quality%20Care%20to%20the%20End%20of%20Life%2C%20(5th%20Ed.)%2C%20by%20Marianne%20Matzo%20and%20Deborah%20Witt%20Sherman%20(eds.)%2C%20New%20York%2C%20NY%3A%20Springer%20Publishing%20Company.&f=false)
- World Health Organization (WHO). (n.d.). Palliative Care Definition (cancer). Accessed from: http://www.who.int/cancer/palliative/definition/en/
Appendices
Appendix A: Key Framework Contributors
Other Levels of Government
- Newfoundland and Labrador
Annette Bridgeman - Nova Scotia
Denise MacDonald Billard - New Brunswick
Roberte Vaultier - Prince Edward Island
Corrine Rowswell & Mireille Lecours - Québec
Marie-Josée Dufour - Ontario
Joshua Lovell - Manitoba
Brooke Ballance - Saskatchewan
Linda Restau - Alberta
Jamie Tycholiz - British Columbia
Alix Adams - Nunavut
Linnea Ingebrigtson - Northwest Territories
Victorine Lafferty - Yukon
Katharina McArthur
National Indigenous Organizations
- Assembly of First Nations
- Inuit Tapiriit Kanatami and the National Inuit Committee on Health
- Métis National Council
Other Federal Government Departments
- Correctional Service Canada
Judith Laroche - Employment and Social Development Canada
Wesley Grant - Indigenous Services Canada
Shubie Chetty - Veterans Affairs Canada
Donna Davis
Pre-Consultation Working Group Members
- BC Centre for Palliative Care
Doris Barwich & Carolyn Taylor - Canadian Hospice Palliative Care Association
Sharon Baxter - Canadian Medical Association
Cécile Bensimon - Canadian Partnership Against Cancer
Cynthia Morton, Esther Green & Deb Dudgeon - Canadian Society of Palliative Care Physicians
David Henderson, Leonie Herx & Kim Taylor - Canadian Virtual Hospice
Shelly Cory & Harvey Max Chochinov - Palliative Care Matters
Carleen Brenneis & Konrad Fassbender - Pallium Canada
Jeff Moat & José Pereira
End-of-Life Care Unit
Helen McElroy, Sharon Harper, Venetia Lawless, Julie Lachance, Craig Macnaughton, Kathie Paddock, Beck Dysart, and Carl Jacob
Appendix B: Overview of Palliative Care in Canada
There is no national palliative care program or strategy in Canada, but rather many parties with distinctive responsibilities related to palliative care. Through our consultations, we were able to create the following snapshot of the current palliative care policies and programs that exist to serve Canadians - these are stand-alone from the Framework on Palliative Care in Canada.
Federal Government and Palliative Care
The federal government is responsible for:
- Setting and administering national standards for the health care system through the Canada Health Act;
- Providing funding support for provincial and territorial health care services;
- Supporting the delivery for health care services to specific groups, including:
- First Nations people living on reserves;
- Inuit;
- Serving members of the Canadian Forces;
- Eligible veterans;
- Inmates in federal penitentiaries; and
- Some groups of refugee claimants.
- Providing other health-related functions, such as:
- Health care data and research.
Various departments, agencies and organizations have some degree of responsibility over supports, programs or services related to palliative care. These include the following:
Canadian Institutes of Health Research (CIHR)
CIHR is the major federal agency responsible for funding health and medical research in Canada. CIHR was created in 2000 as an independent agency and is accountable to Parliament through the Minister of Health. CIHR is part of the Health Portfolio. Composed of 13 Institutes CIHR provides leadership and support to health researchers and trainees across Canada to create new scientific knowledge and to enable its translation into improved health, more effective health services and products, and a strengthened Canadian health care system.
Canada Revenue Agency (CRA)
The CRA administers the Canada Caregiver Credit to support a spouse or common-law partner, or a dependant with a physical or mental impairment. The Canada Caregiver Credit was created in 2017 by combining three previous credits: the Caregiver Credit, the Family Caregiver Credit, and the Credit for Infirm Dependants age 18 or older.
Correctional Services Canada (CSC)
CSC is responsible for the health and well-being of inmates in 43 correctional institutions across five regions. Fifty-seven health centres provide pharmacy, hospital and mental health services to inmates. CSC has Palliative Care Guidelines (currently being updated) to address the need for more timely response to the palliative needs of inmates, and to reflect the new realities of inmate patients' rights to access medical assistance in dying. Correctional facilities are not always set up to provide all of the types of palliative care supports required. Therefore, the Office of the Correctional Investigator recommends that CSC works with the Parole Board to ensure that palliative or terminally ill inmates seek Section 121 "parole by exception" to allow them to spend as much time in the community among family and friends as early as possible, provided they do not pose a risk to society. CSC has recently implemented information-sharing systems to facilitate this process. Challenges with this new approach include limited capacity within community hospices, where they exist.
CSC is also looking at ways to increase palliative care competencies for employees providing health care services to inmate patients.
Employment and Social Development Canada (ESDC)
The Employment Insurance (EI) Compassionate Care Benefits provides up to 26 weeks of income support and job security to eligible individuals caring for a family member with a serious medical condition and a significant risk of death. Benefits can be shared between family members, either at the same time or separately.
The EI Family Caregiver Benefit, for adults provides up to 15 weeks of benefits to individuals who are temporarily away from work to provide care or support for a critically ill or injured adult family member, 18 years of age or older. Eligibility includes immediate and extended family members and individuals that the critically ill adult considers to be like family. The EI Family Caregiver benefit for children provides up to 35 weeks of benefits to any EI-eligible family member who is providing care or support to a critically ill child under the age of 18. In order to be eligible for these EI Caregiver benefits, an individual must have accumulated 600 insured hours of work in the 52 weeks before the start of their claim, or since the start of their last claim, whichever is shorter, or earned the minimum self-employment income and opted to pay EI premiums.
Health Canada (HC)
The Canada Health Act ensures that all eligible Canadian residents have reasonable access to medically-necessary hospital and physician services without paying out-of-pocket costs. Responsibility for health care services is shared between provincial and territorial governments and the federal government. Health Canada transfers money to the P/Ts as part of the Canada Health Transfer - to support health care service delivery across Canada.
Most recently, the Government of Canada has taken an active leadership role, engaging with P/Ts in a discussion about strengthening health care. In addition to funds provided under the Canada Health Transfer, Budget 2017 confirmed a historic targeted investment of $11 billion over ten years directly to P/Ts to address specific gaps in our health care system as described in the Common Statement of Principles on Shared Health Priorities (CSoP). Six billion dollars are dedicated to increasing the availability of home and palliative care. At the time of writing this Framework, eight P/Ts have publicly released the details of their CSoP bilateral agreements with the federal government. The agreements are publicly available at: https://www.canada.ca/en/health-canada/corporate/transparency/health-agreements/shared-health-priorities.html
Immigration Refugees and Citizenship Canada (IRCC)
The Interim Federal Health Program (IFHP) provides coverage of certain health-care benefits in Canada through a third-party service provider to resettled refugees, asylum seekers, and certain other groups, until they become eligible for provincial/territorial health-care coverage or leave Canada. Neither IRCC nor its IFHP provide direct health-care services, including direct delivery of palliative care supports and services.
Indigenous Services Canada (ISC)
ISC funds First Nations and Inuit Home and Community Care (FNIHCC) to provide a continuum of basic home and community care services that enable First Nations and Inuit of all ages, to receive the care they need in their homes in their respective communities. Services are currently available in 98 percent of First Nations communities and 100 percent of Inuit communities. However, gaps remain. In Budget 2017, the Government of Canada announced an additional $184.6 million over five years in investments for home and palliative care to enhance the home care program and provide communities with access to palliative care services for clients to be cared for in their community.
Public Health Agency of Canada (PHAC)
In June 2017, the National Strategy for Alzheimer's Disease and Other Dementias Act came into force. The legislation calls on the Minister of Health to develop a national dementia strategy in collaboration with PTs, convene a national conference on dementia, and establish a Ministerial Advisory Board. Starting in June 2019, the Minister must report annually to Parliament on the effectiveness of the strategy. In May 2018, the national dementia conference was held, and the Ministerial Advisory Board (MAB) on Dementia was established. Members of the MAB include people living with dementia, researchers and advocacy groups, health care professionals, and caregivers.
Budget 2018 allocated $20M over 5 years and $4M per year ongoing for community-based projects to improve the wellbeing of people living with dementia (PLWD) and caregivers, who are predominantly women.
PHAC works with P/Ts through the Canadian Chronic Disease Surveillance System (CCDSS) to collect data on Canadians living and newly diagnosed with dementia. Data have been released and help to provide a more complete picture of dementia in Canada.
The Centre for Aging and Brain Health Innovation was established with federal funding of $42M over five years (2015-20). This Centre enables the development of products and services to support brain health and aging, with a focus on dementia.
Veterans Affairs Canada (VAC)
VAC administers three key programs to support the health care needs of eligible veterans: the Health Care Benefit Program, the Veterans Independence Program, and the Long-Term Care Program. These programs may be used together, providing a continuum of care to meet needs. Though VAC does not have a specific palliative care program, benefits, services, and care in relation to eligible veterans with palliative care needs can be funded under the afore mentioned programs. For example, health care benefits consist of treatment benefits (e.g. coverage for medications, special equipment, and nursing services), and supplementary benefits (e.g. health-related travel and costs for a medical escort). The Veterans Independence Program is a home care program aimed at allowing veterans to remain self-sufficient in their homes, funding services such as: health and support services by health professionals (such as nursing care), personal care services to assist veterans with their activities of daily living, and housekeeping services. The Long-Term Care program funds or contributes toward the cost of care for eligible veterans in receipt of care in health care facilities.
Provincial and Territorial Delivery of Palliative Care
P/Ts are responsible for developing health policies and programs based on their unique characteristics, resources, and population needs. In August 2017, federal, provincial and territorial (F/P/T) governments agreed to a Common Statement of Principles on Shared Health Priorities (CSoP), which outlines agreed upon areas of action in the shared health priorities of home and community care, and mental health and addiction, supported by $11 billion in federal funding over 10 years. Of that, $6 billion will help P/Ts to expand access to home and community care, including palliative care. In addition, F/P/T governments agreed to measure progress and report to Canadians. Based on these joint priorities, bilateral funding agreements are now being negotiated, detailing how federal funding for home and community care and mental health and addiction will be implemented, and CIHI is supporting performance measurement.
The following overview highlights some of the new and innovative approaches P/Ts are taking to deliver palliative care programs and services:
British Columbia
Palliative care in British Columbia (BC) is provided by health care providers from a range of disciplines as part of their routine care of people with life-limiting illness. Specialized palliative care is provided by health care professionals with advanced knowledge and skills in palliative care. Professionals providing specialized palliative care are available to provide consultation support, assume care of people with complex palliative care needs, or share care with generalist providers as needed. Home, community, hospital, and hospice care are delivered through five regional health authorities and complemented by provincial services. The BC Centre for Palliative Care is a provincial hub supporting education, innovation, and leading practice in palliative care. Hospice organizations are an important partner in the continuum of palliative care services, with community organizations providing a range of bereavement, respite, and related support services. Some organizations offer residential hospice care. BC continues to focus on early identification of people who can benefit from a palliative approach to care, and improving access to interdisciplinary care across the health service continuum in urban, rural, and remote locations, including First Nations communities. Tools and resources to support advance care planning and goals of care conversations are available, and further initiatives to enhance these important conversations are underway.
Alberta
The 2014 Alberta Palliative and End-of-Life Care (PEOLC) Provincial Framework consists of a number of initiatives. Those implemented to date include:
- A website that provides a centralized access point for persons, families, and health care providers. It includes PEOLC information on programs and services, resources, and supports;
- The Emergency Medical Services PEOLC Assess, Treat, and Refer Program which provides care and treatment at home for palliative emergencies by emergency medical services practitioners;
- The Advance Care Planning and Goals of Care Designation Policy, a which provides a process of deliberation, documentation, and communication for people wanting to indicate their preferences regarding health care decisions at the end of their life;
- The 24/7 Palliative Physician On-Call Program provides specialty support to primary care physicians for PEOLC paediatric and adult persons;
- Alberta Health's Continuing Care Health Service Standards were amended (2016) to include five standards for palliative care;
- Alberta offers a palliative drug coverage program to provide supplementary health benefits not covered by the Alberta Health Care Insurance Plan.
Saskatchewan
The creation of the Saskatchewan Health Authority has brought forth a transformation in the delivery of health care services in Saskatchewan, which includes palliative care. In this province, palliative care refers to interdisciplinary services that provide active, compassionate care to the terminally ill at home, in hospital or in other care facilities. Currently, there are four full-time palliative care physicians in the province; however, many general practitioners throughout the province provide palliative care services, in consultation with the palliative care physicians and experts.
In 2016, a provincial consultation with palliative care experts and other stakeholders led to the implementation of Pallium Canada's Learning Essential Approaches to Palliative Care (LEAP) training in 2017-18, using federal funding targeted to home and community care. In 2018-19, $2.42 million was allocated to continue improvements and increase access to palliative care services throughout the province. Together with federal funding through its bilateral agreement, this work will enhance the health system's capacity to provide palliative care services, such as pain/symptom management, and result in better support to people wishing to die at home, or another facility of their choice, rather than in an acute care facility.
Manitoba
In Manitoba, palliative/end-of-life care is available in any care setting, including the home, a palliative care unit (e.g., a hospital or an acute care setting) or in a hospice, a personal care home or any other health care facility. The Winnipeg Regional Health Authority Palliative Care program provides access to care 24 hours a day, seven days a week, to people registered with the program, as well as consultative services to persons and health care professionals across Manitoba. Each Regional Health Authority (RHA) has a palliative care coordinator in place to manage access to palliative care services in their region. Direct palliative care services in the community are provided through home care in all RHAs.
Hospice beds are available at two hospices (e.g., Grace Hospice and Jocelyn House) for individuals who do not require specialized treatments in an acute care facility. For individuals needing specialized treatments in a health care facility at end of life, there are palliative care beds available within each RHA.
Workbooks and information regarding advance care planning and goals of care are available to people at end of life. The Changing Focus: Living with Advanced Cancer Initiative by CancerCare Manitoba provides a copy of a standardized care plan, written information about palliative care symptom management, and details about local supports and resources for primary care providers and patients, to assist them as they transition into a primarily palliative approach to care.
Manitoba offers the Palliative Care Drug Access Program, which allows people registered with the program to receive their prescribed medications free of charge. A provincial palliative care program specialist position has been in place since 2016 to advance the provincial coordination and delivery of palliative care education for health care providers and volunteers across the province.
Ontario
In Ontario, a broad range of providers deliver palliative and end-of-life services across the continuum of care. Ontario's Ministry of Health and Long-Term Care funds fourteen Local Health Integration Networks (LHINs), which are responsible for planning, co-ordinating, funding, and monitoring health services, including palliative care. In addition, the LHINs are responsible for delivering home and community care services, including residential hospice care. In 2016, the Ministry announced the launch of the Ontario Palliative Care Network, which serves as the government's principal advisor on palliative care. This network is a key partner in strengthening access to community-based palliative care, and has recently helped the Ministry expand residential hospice capacity with over 200 beds across the province. Negotiations for the bilateral agreement with the federal government were still underway at the time of writing.
Quebec
Quebec adopted an Act respecting end-of-life care in 2014. It proposes a global and integrated vision of the care and rights of people at the end of life. The Act contains two components: (1) the rights, as well as the organization and framing of end-of-life care, which includes palliative and end-of-life care; and (2) the knowledge of the primacy of the individual's decision expressed clearly and voluntarily, by the implementation of a regime on anticipated medical directives.
The province has a range of palliative care services delivered in four service delivery points: hospitals, long-term residential centres, hospice and home care with local and regional particularities. These services are rooted in the Health Insurance Regime, and include more specific programmes, for example support for family caregivers, paediatric palliative care, online support groups for health care providers and caregivers, and services for people who are grieving. To add to these services, Quebec has a 2015-2020 Palliative and End-of-life Development Plan containing fifty measures grouped under nine important priorities. They guide the management of services, and help increase palliative care services.
As part of CSoP, Quebec has an asymmetrical agreement with the federal government. Although palliative care is not specifically mentioned, with federal funding Quebec aims to increase the number of people receiving home support services and enhance services to better meet their needs.
New Brunswick
In April 2018, Palliative care in New Brunswick: A person-centred care and integrated services framework was published by the provincial government. Its emphasis is on people and an integrated care system. It contains five priority sectors, namely: people-centred care; including family support networks; professional capacity; community capacity; and leadership.
In New Brunswick, palliative care is offered through Regional Health Authorities, the Extra-Mural Program / Ambulance New Brunswick, and hospices. In 2016, the Act on Advance Health Care Directives was enacted. In its bilateral agreement with the federal government, NB indicated in its palliative care strategic implementation plans that it would be investing $11.5 million over the next five years. The palliative care improvements will concentrate on the provision of health care provider education, the development and implementation of standardized evaluation and surveillance tools; the establishment of hospices through community support; the design of alternative service approaches in rural communities; and the establishment of an integrated palliative care model for medical doctors.
Prince Edward Island
In Prince Edward Island (PEI), palliative care is delivered by the PEI Provincial Health Authority in a variety of settings, including the home. PEI has been a partner with CPAC for many years, and in 2015, it implemented the program titled "Paramedics providing palliative care at home". Advance care planning is available online through Health PEI's Advance Care Planning interactive workbook and frequently asked questions. PEI has committed to investing $12.4 million towards implementing the interRAI data system and enhancing palliative care through initiatives as part of its bilateral agreement with the federal government. These initiatives include: rapid bridging for persons eligible to return or remain home, or in-person palliative care to ensure care needs are met during transition between care environments, and an expansion of the paramedic check-in program.
Nova Scotia
Nova Scotia released its Provincial Palliative Care Strategy in 2014, which has four pillars: integrated service delivery, accountability, family and caregivers, and capacity building and practice change. This was followed up by the 2017 Palliative Competency Framework, which details the palliative competencies expected of health professionals and volunteers in the province. Nova Scotia has also been a partner with the CPAC in developing a system of paramedics providing palliative care in the home. Nova Scotia has the Personal Directives Act as well as a booklet outlining the process of advance care planning. It is expected that Nova Scotia will open its first two residential hospices in 2019. In its bilateral agreement with the federal government, Nova Scotia will train and support more palliative care clinicians, coordinate volunteers, and improve communication and information sharing about palliative care resources.
Newfoundland and Labrador
Palliative care in Newfoundland and Labrador is provided in alignment with a Home First philosophy. This approach provides supports and services to individuals at home, removing barriers to seamless service delivery. The province has an Advance Health Care Directives Act and clinicians are encouraged to engage in advance care planning with their clients. Newfoundland and Labrador, through its bilateral agreement with the federal government, has committed to invest $43.3 million towards home and community care, which includes a specific focus on palliative and end-of-life care. The province is working to enhance palliative and end-of-life care through increasing educational opportunities for staff and exploring the introduction of a hospice model.
Nunavut
In 2015, Nunavut produced the report titled Continuing Care in Nunavut 2015-2035. Palliative care services exist on a relatively small scale in Nunavut, given the population size and remoteness of its 25 communities. Palliative care services provided in the home are limited to communities that have staff who have received palliative care training. Nunavut has five small long-term care facilities, three of which have one palliative/respite bed. Nunavut is expanding its training on palliative care to enable the provision of palliative care in more communities, helping Nunavummiuts to stay in their homes longer.
Northwest Territories
The Northwest Territories has an integrated service delivery model, detailed in its Palliative Approach to Care Service Delivery model and in its 2017 Continuing Care Services Action Plan, which include palliative care actions as a priority in the following areas: a standardized approach to care; physical resources (drugs & equipment); skilled and supported workforce; and culturally safe palliative care. The territory is currently working towards implementing the interRAI system in both home and community care to evaluate and track outcomes. In 2006, the Northwest Territories passed the Personal Directives Act, giving advance care planning the force of law. The Department of Health and Social Services is working with the Health and Social Services Authorities to develop standardized territorial forms and processes to support advance care planning and documenting goals of care. The Northwest Territories has committed to invest $3.6 million towards implementing the interRAI data system and paid family/community caregiving pilot as part of its bilateral agreement with the federal government.
Yukon
Palliative care services in the Yukon are broad and multi-faceted as there are a variety of services provided in homes, hospitals, and continuing care facilities. They are delivered by a variety of communities and organizations including First Nations, Health and Social Services branches, and others. The Yukon Framework, based on The Way ForwardFootnote 21, enumerates four foundational principles: a continuum of integrated services, supporting care providers, best practice service delivery, and evaluation.
The Yukon Palliative Care Program has collaborated with various partners to build capacity among care providers, and support early integration of a palliative approach to care across all care settings, thereby improving access to appropriate services for all Yukoners, whether they live in urban or rural areas. Future enhancements, such as the addition of a community hospice are in the planning stage.
The Resident Assessment Instrument (RAI) for Home Care and RAI-MDS (minimum dataset) (long-term care) are both in use across the territory to track provision of services. Efforts are underway to establish a system to collect "person-reported outcomes"Footnote 22 and promote advance care planning tools in the territory. A fee code is available for physician counselling time associated with any palliative visit, for example, for the writing up of an advance care plan.
Appendix C: Best Practices
The following are some of the many examples of best practices in the delivery of palliative care across Canada. We appreciate that there are many more that we did not hear about, and recognize those innovators - listed below and otherwise - who are making a difference in palliative care for Canadians.
Palliative Care Training and Education Needs of Health Care Providers and Caregivers
- Advance Care Planning in Canada community training (CHPCA/Speak Up) - advance care planning training materials, in relation to health care consent, which may be used for public education. (http://www.advancecareplanning.ca/resource/advance-care-planning-in-relation-to-health-care-consent-training-materials/)
- Comprehensive Advanced Palliative Care Education Program (CAPCE), including Fundamentals of Hospice Palliative Care - for nurses and other advanced care clinicians. The program embeds best practice standards, aligns with the Model to Guide Hospice Palliative Care, and is taught in most regions of Ontario. (http://www.palliativecareswo.ca/apps/learning_initiatives_CAPCE.html)
- E-Learning modules on Advance Care Planning (ACP) - for health care providers in Alberta - modules to help providers understand their role in supporting ACP and how it relates to patient safety and satisfaction. (https://www.albertahealthservices.ca/info/Page9099.aspx)
- End- of- Life Care During the Last Days and Hours Best Practice Guideline, by the Registered Nurses' Association of Ontario - evidence-based recommendations for registered nurses and registered practical nurses on best nursing practices for end-of-life care during the last days and hours of life. (https://rnao.ca/bpg/guidelines/endoflife-care-during-last-days-and-hours)
- Health Standards Organization (HSO) and its affiliate, Accreditation Canada, have been identifying and publishing leading practices in their Leading Practice Library for over 15 years. A Leading Practice is a practice carried out by a health and/or social services organization, that has demonstrated a positive change, is people-centred, safe and efficient. The Leading Practices Library is a knowledge sharing resource of innovative practices that have been identified through a rigorous evaluation process, and shared with the public, policy makers, and organizations who are seeking ways to improve the quality of health services for all. At the time of writing, they had seven Leading Practices on palliative or hospice care in their Library. (https://healthstandards.org/leading-practices/introduction-to-leading-practices/)
- Hospice Palliative Care Nursing Certification (CHPCN) - palliative care nurses are registered nurses with a baccalaureate degree in nursing. CHPCN is available through the Canadian Nurses Association (https://www.cna-aiic.ca/-/media/nurseone/files/en/hospice_palliative_care_blueprint_and_competencies_e.pdf?la=en&hash=EF462BF689939CEA1CE13614E280CEE9448956FB)
- Learning Essential Approaches to Palliative Care (LEAP) - developed by Pallium Canada - LEAP courses provide learners with the essential, basic competencies of the palliative care approach. Modules include: Core, Mini, Long-Term Care, Paramedic, Oncology, Renal, and Facilitator training, with more under development (https://pallium.ca/equip-yourself/courses/)
- Nova Scotia Palliative Care Competency Framework - outlines shared and discipline-specific competencies for health professionals and volunteers who care for people with life-limiting conditions and their families. It also describes competencies for those who specialize or have a practice focused in palliative care. The competencies are written to emphasize the inter-professional nature of palliative care and they apply to all settings of care. (https://library.nshealth.ca/ld.php?content_id=34202519)
- Nursing School Curriculum - Canadian Association of Schools of Nursing - a palliative and end-of-life care (PEOLC) faculty teaching and learning resource (https://www.casn.ca/2014/12/palliative-end-life-care-teaching-learning-resources-2012/)
- Social Work Competencies in Palliative Education (SCOPE) - a set of core social work competencies to guide education for practice with people facing end-of-life issues (http://www.chpca.net/projects-and-advocacy/projects/scope.aspx)
- Serious Illness Conversation Guide - a reference guide for clinicians for successful discussions about serious illness care in outpatient, non-emergent, settings (https://www.talkaboutwhatmatters.org/documents/Providers/PSJH-Serious-Illness-Conversation-Guide.pdf or http://www.bccancer.bc.ca/new-patients-site/Documents/SeriousIllnessConversationGuideCard.pdf)
- Volunteer training through Canadian Hospice Palliative Care Association - includes webinars, National Norms, online training program, and other resources (http://www.chpca.net/volunteers.aspx)
Measures to Support Palliative Care Providers and Caregivers
- AIDS Bereavement and Resiliency Project of Ontario (ABRPO) collaborates with organizations to build workplace, agency and community resiliency in the face of AIDS-related multiple loss and transition. ABRPO assists in assessment and enhancement of individual and agency strategies related to loss and transition. Programs include interventions, education, presentations, workshops, retreats and research initiatives incorporating evidence-based knowledge and bereavement expertise. (https://abrpo.org/about-us/)
- Canadian Virtual Hospice - free online support and personalized information about palliative and end-of-life care to patients, family members, health care providers, researchers and educators. Includes "how-to" videos and other resources, including "Ask a Professional" and "Living My Culture", and a directory of services across Canada (www.virtualhospice.ca)
- Caregiver Compass - is a free and easy to access online resource that provides tips and tools to help caregivers manage their caregiving responsibilities, navigate the health care system, and deal with financial and legal matters. It can also be printed as a booklet. https://www.saintelizabeth.com/getmedia/89a61fed-0db8-487d-a8d7-d50b99cdb930/Caregiver-Compass-Online.pdf.aspx
- Caregivers Alberta has a variety of caregiver support programs, such as e-learning for caregivers in the home. (https://www.caregiversalberta.ca/)
- Death doula/End-of-Life Doula - provides emotional, educational and practical support that empowers the client to make informed decisions regarding their end-of-life care and to support caregivers. (https://endoflifedoulaassociation.org/)
- Government of Canada - Employment Insurance Family Caregiver Benefits are available to help families care for a critically ill child (up to 35 weeks) or adult (up to 15 weeks). If the family member's health gets worse, caregivers could combine the caregiver benefit with the existing Compassionate Care Benefit, which provides a maximum of 26 weeks of support. (https://www.canada.ca/en/employment-social-development/campaigns/ei-improvements/adult-care.html)
- Hospice Wellington (Guelph, Ontario) - full community service program with a variety of community programming, including Bereavement and Grief Support, Integrated Wellness, Volunteer Visiting, Child and Youth Support and Art Therapy, which is free of charge to those in Wellington County who are experiencing grief and bereavement. (www.hospicewellington.org)
- Living Lessons® Program - GlaxoSmithKline Foundation in partnership with the Canadian Hospice Palliative Care Association. The purpose of the Living Lessons® campaign was to educate and inform the public about palliative and end-of-life care. It created and distributed resources for caregivers and patients. Material is archived at: (http://www.eolcaregiver.com/living-lessons.aspx)
- Mount Sinai Hospital - provides bereavement services through its Wellness Centre; guidance for primary care practitioners in palliative care and dementia. (https://www.mountsinai.on.ca/)
- MyGrief.ca and KidsGrief.ca - Free online grief and bereavement resources for Canadians. Developed by a team of national and international grief experts together with people who have experienced significant loss. (www.mygrief.ca; www.kidsgrief.ca)
- Pregnancy and Infant Loss Network (PAIL Network) - Ontario-wide bereavement care and support to families who have suffered perinatal loss. (https://pailnetwork.sunnybrook.ca/)
- Prince Edward Island's Palliative Care Program provides support for in home respite care, emotional and spiritual support, and bereavement services for caregivers. Resources for caregivers can be accessed through the mobile integrated health services. (https://www.princeedwardisland.ca/en/information/health-pei/palliative-care-program)
- Quality End-of-Life Care Coalition of Canada consists of over 30 health care organizations concerned with end-of-life care. Their website has a list of resources to assist those searching for information on end-of-life care. (http://www.qelccc.ca/projects-and-resources/educational-inventory-of-resources.aspx)
- Victoria Hospice (Victoria, BC) - offers a psychosocial and bereavement program including telephone support; in-person counselling; a variety of bereavement support groups, drop-in and journal groups; information and education; and referrals where appropriate. (www.victoriahospice.org/)
Measures to Improve Research and the Collection of Data on Palliative Care
- Alberta's Palliative and End of Life Care Program has an indicator dashboard of palliative care measures to support quality improvement. (https://www.albertahealthservices.ca/info/Page14778.aspx)
- Canadian Cancer Research Alliance (CCRA) – the Pan-Canadian Framework for palliative and end-of-life care research report - identified priorities for research funding, including: transforming models of caring, patient- and family-centredness, and ensuring equity. CCRA's building blocks include creating and sustaining capacity, standardizing data, and exchanging and acting on knowledge. (https://www.ccra-acrc.ca/index.php/publications-en/strategy-related-publications/item/pan-canadian-framework-for-palliative-and-end-of-life-care-research)
- Canadian Frailty Network - is supporting a research program on end-of-life care, advance care planning and decision making.( https://www.cfn-nce.ca)
- Canadian Institute for Health Information's 2018 report entitled Access to Palliative Care in Canada highlights several innovative programs and practices in palliative care, and provides the most comprehensive data on access to palliative care across settings, to date. (https://www.cihi.ca/en/access-data-and-reports/access-to-palliative-care-in-canada)
- Canadian Partnership Against Cancer - working with 9 jurisdictions on measures of patient reported outcomes and experiences, and early integration of palliative care. (https://www.partnershipagainstcancer.ca/)
- Follow-back studies - Using vital statistics to identify people who died, researchers contacted next-of-kin and asked them about their family member's experience with palliative care, for instance, in Nova Scotia: ( https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3750367/)
- InterRAI is a comprehensive assessment system that can link patient data across health care settings. The InterRAI Palliative Care (PC) Assessment System was developed to provide a comprehensive assessment of the strengths, preferences, and needs of adults in both hospice and palliative care. (http://www.interrai.org/)
- Ontario Palliative Care Network has a data repository, and can generate a number of key statistics regarding where people die, how and when they access palliative care (including at home). (https://www.ontariopalliativecarenetwork.ca/en)
- United Kingdom's National Gold Standards Framework Centre in End of Life Care is the national training and coordinating centre and has many resources regarding measurement and definitions. (http://www.goldstandardsframework.org.uk/)
Measures to Facilitate Consistent Access to Palliative Care across Canada
- British Columbia Centre for Palliative Care (BCCPC) - gives micro-grants to 25 hospice societies and other non-profit organizations across British Columbia to help improve access to compassionate palliative care closer to home, and to empower people to have a voice in their care through advance care planning. (https://www.bc-cpc.ca/cpc/seed-grants/)
- Compassionate Communities - a community approach to caregiving, dying, death and grieving. (https://pallium.ca/work-with-us/launch-a-compassionate-community/)
- Diane Morrison Hospice - Located at the Ottawa Mission, providing 24-hour palliative nursing care to homeless and street-involved people facing the final days of their lives. (https://ottawamission.com/hospice/)
- Health Tapestry Program (McMaster University) - volunteers are trained to talk to individuals in home care settings (clients) about the factors that are important to their health and life. During these visits, volunteers use a specialized computer app to gather this information and send it digitally to the client's health care team. With this information, the health care team develops a plan to help address any health issues and goals with the client. This model effectively reduces hospital visits and improves understanding about client preferences and values related to their health care and end-of-life wishes. (http://healthtapestry.ca/)
- Kelley Model for Community Capacity Development - A research-based community capacity development model developed by Dr. Mary Lou Kelley has been used to guide the development of palliative care programs in rural areas, long term care facilities, and First Nations communities. Most recently it has been used in Compassionate Community projects. The four phase model describes required antecedent conditions for community change, catalysts for change and key processes for capacity building in palliative care. (http://www.palliativealliance.ca/applying-the-kelley-model-for-community-capacity-development)
- Ontario Telemedicine Network's (OTN's) TelePalliative project - monitoring of pain, symptoms and caregiver burden and improved access to consultant supports using Skype (iPads) (www.otn.ca)
- Palliative Education and Care for the Homeless (PEACH) - operates as a mobile unit in Toronto, providing attentive care on the streets, in shelters, and with community-based services. (http://www.icha-toronto.ca/programs/peach)
- Paramedics Providing Palliative Care at Home Programs - trained paramedics provide pain and symptom management at home for palliative care patients after-hours. Programs have already been implemented in Nova Scotia, Prince Edward Island, Alberta, and are being considered (in partnership with CFHI and CPAC) in other jurisdictions. For instance: ( https://www.cfhi-fcass.ca/sf-docs/default-source/newsevents/ceo-forum-2017/presentations/ceo-forum2017-nova-scotia-pei-alberta-health-services-paramedics-providing-care-at-home-program-alix-carter-cheryl-cameron.pdf?sfvrsn=798d744_2)
- Rainbow Resource Centre/Visiting Homemakers Association - training and education to improve the accessibility and quality of health care services for the LGBTQ2 community in Ontario. (https://www.rainbowhealthontario.ca/rainbow-health-ontario-training-and-education/)
- Schlegel Villages - provide a village atmosphere for people living with dementia and could be a model for palliative care and assistance in a home-like setting. (http://schlegelvillages.com/)
- Virtual Hospices, Tele-health, Tele-connect (e.g., Canadian Virtual Hospice; Ask a Professional service/skyping with palliative consultants) (http://www.virtualhospice.ca/en_US/Main+Site+Navigation/Home/Support/Support/Ask+a+Professional.aspx)
Appendix D: Overview of National Non-Governmental Palliative Care Organizations
Among the many organizations providing services or resources relevant to the aims of the Framework on Palliative Care in Canada, the following key stakeholders in particular have had a direct role in developing foundational documents and frameworks and leading palliative care initiatives. Many were part of a Pre-Consultation Working Group that helped to plan and facilitate the consultative process; all of them participated in the consultation process.
Accreditation Canada / Health Standards Organization (AC/HSO) In 2004-05, Health Canada partnered with AC to produce hospice palliative care standards, including for volunteers, based on national norms of practice. HSO is currently renewing the standards to include more (non-institutional) settings of care (for instance, homes and residential facilities).
Canadian Cancer Society (CCS) Its 2016 report, Right to Care: Palliative Care for All Canadians highlights the major gaps in care and existing barriers to all Canadians having access to quality palliative care, when they need it. CCS provides research funding to initiatives such as one which found that integrating palliative care earlier improved patients' quality of life.
Canadian Foundation for Health Care Improvement (CFHI) In its Call for Innovations in Palliative and End-of-Life Care launched in February 2017, CFHI identified 26 successfully emerging or demonstrated innovations, including: Paramedics Providing Care at Home Program; embedding a palliative approach in long-term care facilities; a tool for the earlier identification of people who could benefit from palliative care; two online platforms by the Canadian Virtual Hospice; publication of a special issue of the Journal of Palliative Medicine on the Palliative Care Matters initiative; enhancing front-line care support services for cancer patients.
Canadian Frailty Network (CFN) CFN has supported initiatives on: integrating a quality of life assessment and practice support system in palliative home care; improving palliative care in long-term care facilities; assessing the impact of implementing a 24/7 on‐call consultation service in Nunavik; practice support tools to facilitate transitions from acute care to other settings; translating best practice knowledge in palliative care into tools specifically for community-based providers; web-based videoconferencing for rural palliative home care consultations.
Canadian Hospice Palliative Care Association (CHPCA) From 2011 to 2015, the CHPCA led The Way Forward Initiative, in which it developed a framework promoting the integration of a palliative approach to care across care settings. CHPCA leads various annual and ongoing events to raise public information and awareness about palliative care and advance care planning.
Canadian Institute for Health Information (CIHI) CIHI's data analyses regarding palliative care include: its 2018 report on Access to Palliative Care in Canada which, although there are still a number of significant data gaps, is the most comprehensive portrait of access to palliative care services across settings to date two studies of health care utilization at the end of life in the Western (2007) and Atlantic (2011) provinces, respectively; a report on End-of-Life Hospital Care for Cancer Patients (excluding Quebec) (2013); and a partnership with CPAC for its 2017 system performance report titled Palliative and End-of-Life Care (end-of-life care for cancer patients in acute hospitals).
Canadian Medical Association (CMA) The CMA led national roundtables (2014) on advance care planning, palliative care, and physician-assisted dying; published a report: Palliative Care: CMA's National Call to Action - Examples of innovative care delivery models, training opportunities, and physician leaders in palliative care (2015); updated its policies to promote greater uptake of advance care planning (2015) and palliative care (2016); and, in partnership with other organizations in 2015, conducted the National Palliative Medicine Survey, which confirmed significant differences in the availability of palliative care services and the type and training of physicians providing such services.
Canadian Nurses Association (CNA) The CNA advocates that nurses have a fundamental role in a palliative approach to care and their practice within the palliative approach and primary health care framework is based on CNA's Code of Ethics for Registered Nurses.
Canadian Partnership Against Cancer (CPAC) CPAC has supported a number of palliative care initiatives since 2007, including developing online resources; training; best practices in advance care planning and goals of care; patient-reported outcome measures; early integration of palliative care; and building capacity in more care providers, including paramedics. In addition, CPAC maintains the Palliative and End-of-Life Care National Network (PEOLC NN) of approximately 40 representatives of national health care organizations, provincial and territorial governments and cancer agencies, patients and family caregivers. The PEOLC NN has four working groups focusing on Advance Care Planning/Goals of Care, Education and Capacity, Integration, and Measurement.
Canadian Society of Palliative Care Physicians (CSPCP) The CSPCP has contributed to initiatives to establish national palliative care competencies for undergraduate medical students, and to incorporate these competencies into curricula; developed credentials for those who specialize in palliative medicine; hosts the Annual Advanced Learning in Palliative Medicine Conference; partnered on the 2015 National Palliative Medicine survey; published reports in 2016: How to improve palliative care in Canada: A call to action for federal, provincial, territorial, regional and local decision makers; and 2017: Palliative care: A vital service with clear economic, health and social benefits.
Canadian Virtual Hospice (CVH) CVH presents evidence-based information and resources about palliative and end-of-life care in a variety of electronic media, such as text, videos (including practical caregiving skills) and social media, backed by a pan-Canadian virtual interdisciplinary clinical team. Its innovative and award-winning features include educational videos and text on grieving (including modules about children's grief), cultural contexts (including Indigenous and other cultures), and an interactive clinical consultation (Ask a Professional).
Palliative Care Matters (PCM) PCM initiatives have included a public opinion survey, evidence reviews, and a consensus development conference held in November 2016, during which a lay panel of 12 Canadians prepared a statement and 20 recommendations. The Conference Board of Canada produced a report on how the consensus statement and recommendations could be moved into action.
Pallium Canada Pallium is developing and implementing standardized palliative care educational resources, tools and curricula (Learning Essential Approaches in Palliative Care - LEAP) across Canada. Pallium has trained over 575 Pallium LEAP facilitators to deliver courses to over 12,000 health care providers (e.g., physicians, nurses, social workers, pharmacists, care aides, paramedics, and family carers).
Quality End-Of-Life Care Coalition (QELCCC) The QELCCC is a group of 38 member/national organizations representing disease groups, professional organizations, and sectors of care. The QELCCC has contributed to a number of activities and reports advocating for and supporting integration of a palliative approach to care.
Appendix E: Framework on Palliative Care in Canada Act
Framework on Palliative Care in Canada Act
Appendix F: Glossary
As with any health care domain, palliative care has a wide and diverse terminology. This glossary is designed to help the Framework on Palliative Care in Canada readers understand its content, language, and terminology. It is built and adapted using an array of different sources which are listed at the end of this document. Footnote 23
-
Access
-
People living with life-limiting illness, their families and caregivers can face challenges in accessing a number of different types of supports, such as access to:
- Referral to palliative care services through diagnosis by their health care provider;
- Technology and supports to allow them to receive palliative care in the setting of their choice; and
- Financial supports such as the federal Family Caregivers Benefit, the Employment Insurance Compassionate Care Benefits, the Canadian Pension Plan Disability Benefit, or various provincial and territorial drug plans, respite care plans, etc.
-
Advance Care Plan
-
Is a verbal or written summary of a capable adult's wishes or instructions about the kind of care they want or do not want in the event that they cannot speak for themselves. It sets out a person's preferences about health and personal care, and preferred care settings, in accordance with applicable laws.
-
Advance Care Planning
-
Is the process of reflection and communication that a person goes through to let others know their future health and personal care preferences.
-
Bereavement
-
Is the state of having experienced and being in the period of mourning after a loss, such as a death. It may refer to a specific time, such as a timeframe set out in employment bereavement leave benefits, and/or, may refer to rituals in cultures or religions.
-
Canadian
-
For the purposes of this Framework, Canadian refers to a person living in Canada.
-
Caregiver
-
A caregiver is a person who provides personal care, support and assistance to another individual of any age who needs it. They usually have no formal training. While they are expected to follow certain ethical norms, they are not accountable to professional standards of conduct or practice. A person is not considered a caregiver if they are paid for these services, a volunteer for an organization or caring as part of a training or education program (see "Care Providers"). Caregivers are often family members and friends. However, an individual is not a caregiver merely because they are a spouse, de facto partner, parent, child, other relative or guardian of an individual, or live with an individual who requires care.
-
Care Provider - or Health Care Provider
-
Is a person that provides a health care service. This term is broader than health care professional, and may also include individuals providing health care services that are not regulated in Canada (e.g., personal support workers, also known as health care aides and a number of other titles across Canada). While health care providers are usually paid for providing health care services, a comprehensive definition could also include volunteers.
-
Care Plan
-
The written plan that describes the overall approach to address a person's assessed health needs and goals, prioritized as important by the person and family, as well as who will provide the service and when. It is developed by the person's service providers in consultation with them.
-
Chronic Illness
-
An illness that may develop slowly, last a long time, months to years, be incurable, and be progressive and/or life-limiting. Examples of life-limiting chronic illness include arthritis, cardiovascular illness, chronic kidney illness, chronic obstructive pulmonary disease, congestive heart failure, diabetes, dementia, HIV/AIDS, multiple sclerosis, amyotrophic lateral sclerosis and some forms of cancer. The illness and its treatment may cause symptoms such as fatigue, pain and sleep problems; they can also limit people's activities, cause them psychological distress and have a negative effect on their quality of life. A chronic illness can't be cured, but its symptoms can be managed.
-
Community-Based Care
-
Care provided in the community rather than in hospital. It may include home care or care in a long-term care facility or group home.
-
Compassionate Communities
-
The Compassionate Communities movement calls on community members and organizations to actively engage in supporting end-of-life care and bereavement. Compassionate Communities view palliative and end-of-life care as a community responsibility. As such, they strive to create partnerships, connecting people in the community and local services.
-
Distinctions-based
-
The Government of Canada recognizes First Nations, the Métis Nation, and Inuit as the Indigenous peoples of Canada, consisting of distinct, rights-bearing communities with their own histories, including with the Crown. The work of forming renewed relationships based on the recognition of rights, respect, co-operation, and partnership must reflect the unique interests, priorities and circumstances of each People. Health care policy development needs to recognize these distinctions.
-
End-of-Life
-
Referring to a final period (hours, days, weeks, months) in a person's life, in which it is medically obvious that death is imminent or a terminal moribund state cannot be prevented. Palliative care is provided before this stage, through it, and continues on afterwards, supporting family and caregivers with bereavement supports.
-
Family
-
Those who are closest to the person receiving care in knowledge, care and affection. The person defines their "family" and who will be involved in their care and/or present at the bedside. It may include the following:
- The biological family;
- The family of acquisition (related by marriage/contract, or adoption); and
- The family of choice and friends (including pets).
-
Goals of Care
-
Is the general aim or focus of care. Clinical and other goals for a person's care are determined in the context of a shared decision making process. It should include treatment of the illness and/or symptom management. In some cases, it includes limits on the interventions that people want, such as "do not resuscitate" orders. See "Advance Care Plan".
-
Health Care Professionals
-
All members of the Palliative Care and inter-professional team of care providers, including physicians (primary care and specialist), nurse practitioners, nurses, social workers, psychologists, chaplains, pharmacists, and physical or occupational therapists; also known as health care providers or formal caregivers.
-
Home Care
-
Includes an array of services for people of all ages, provided in the home setting, that encompasses health promotion and teaching, curative intervention, end-of-life care, rehabilitation, support and maintenance, social adaptation and integration, and support for family caregivers. It is usually provided by public or private health care providers. (See "Community-Based Care").
-
Hospice
-
A community-based facility aiming to offer integrated palliative care for people living with life-limiting illness and support for their families and friends. The hospice may admit people as in-patients, provide out-patient services, or provide visiting, or other supportive services.
-
Integrated Palliative Approach to Care/Community Integrated Palliative Care
-
Focuses on meeting a person's and family's full range of needs - physical, psychosocial and spiritual - at all stages of a chronic progressive illness. It reinforces the person's autonomy and right to be actively involved in their own care - and strives to give individuals and families a greater sense of control. It sees palliative care not as a discrete service offered to dying persons but rather an approach to care that can enhance their quality of life throughout the course of their illness. It provides palliative care at appropriate times during the person's illness, focusing particularly on open and sensitive communication about the person's prognosis and illness, advance care planning, as well as physical, psychosocial and spiritual support. As the person's illness progresses, it includes regular opportunities to review the person's goals and plan of care and referrals, if required, to expert palliative care services.
-
Interdisciplinary Team
-
Care providers, with different training and skills, who work together to develop a team, and provide care that addresses as many of the person's health and other needs as possible. The professionals in the team may function under one organisational umbrella or may be from a range of organisations brought together as a unique team. As a person's illness changes, the composition of the team may change to reflect the changing clinical and psychosocial needs of the person. An interdisciplinary team typically includes one or more physicians, nurse practitioners, nurses, social workers, psychologists, spiritual advisors, pharmacists, personal support workers, and volunteers. Other disciplines may be part of the team as needed, if resources permit.
-
Life-Limiting Illness
-
Describes illness where it is expected that death will be a direct consequence of the specified illness. The term "person living with a life-limiting illness" also incorporates the concept that people are actively living with such illnesses, often for long periods of time, not imminently dying. Therefore, it affects health and quality of life, and can lead to death in the foreseeable future.
-
Palliative Care vs. a Palliative Approach to Care
-
Consultation participants shared at length their views on these terms, and emphasized the importance of clarity. For the purposes of this Framework, palliative care is a type of care that can be offered along the full time continuum of any life-limiting illness, including bereavement of family, friends and caregivers. It includes services such as pain and symptom management, addresses psychological and spiritual concerns, supports family and caregivers, and enhances quality of life (see Definition section of this Framework for more details). It is provided by primary health care providers, disease specialists, and palliative care specialists.
The palliative approach to care is a philosophy and set of principles that apply to all people living with and dying from a life-limiting illness. The palliative approach integrates the philosophies and principles of palliative care into primary care, long term care and all mainstream health services.
The term "public health approach to palliative care" is the application of public health sciences (epidemiology, health research, and policy analysis) to develop and deliver palliative care services. It has a slightly broader set of guiding principles compared to the palliative approach to care, as described in the BC Centre for Palliative Care white paper on the topic:
http://bc-cpc.ca/cpc/documents/pdf/Table%20of%20Contents.pdfThe Bow-tie model of an approach to palliative care: early integration of palliative care into the treatment plan (P. Hawley, B.C. Cancer)
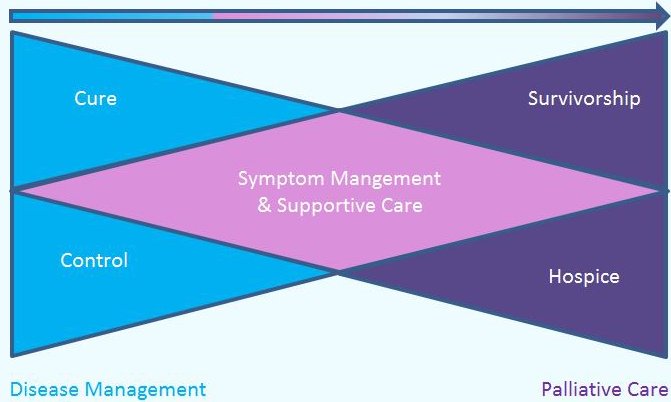
Text description
The diagram shows two interlocking triangles, like a bowtie, a blue triangle on the left and a purple triangle on the right, with the points towards the center of the base of the other triangle, to form a pink diamond shape in the center where the two triangles intersect. There is an arrow above the two triangles pointing to the right. The triangle on the left is labeled "Disease Management". It is divided into three sections, the uppermost and lowermost are labeled "Cure", "Control" respectively, and the center that forms part of the diamond is labeled "Symptom Management and Supportive Care". The triangle on the right side bears the label "Palliative Care" and is divided into three sections; the uppermost and lowermost are labeled "Survivorship", "Hospice", and the center section, "Symptom Management and Supportive Care".
-
Pain and Symptom Management
-
Pain and other symptoms that cause discomfort (e.g., shortness of breath, fatigue, changes in mood or functional ability, psychosocial or spiritual distress) can be caused by underlying illnesses and by the treatments for those illnesses. The integrated palliative approach to care focuses on helping people manage pain and other symptoms as a way to reduce discomfort and improve quality of life.
-
Person-Centred Care/Person- and Family-Centred Care
-
An approach to the planning, delivery and evaluation of health care that is founded in mutually beneficial partnerships among clinicians and people receiving care. Person-centred care is respectful of, and responsive to, the preferences, needs and values of the care recipient. Key dimensions of person-centred care include:
- Respect;
- Emotional support;
- Physical comfort;
- Information and communication;
- Continuity and transition;
- Care coordination;
- Involvement of family and carers; and
- Access to care.
-
Regional Health Programs or Authorities
-
Health planning organizations responsible for setting policies, allocating resources to support care, and approving organizational plans to deliver services.
-
Respite
-
A break, time out, or relief for the informal caregiver. (See "Caregiver")
-
Setting of Care
-
The location where care is provided, such as the person's home, primary care settings (e.g., a doctor's office, nursing station, community clinic), an acute, chronic, or long-term care facility, a hospice or palliative care unit, a jail or prison, or in the case of homeless individuals, the street, etc.
-
Specialist Palliative Care
-
Provided by a specially-trained team of doctors, nurse practitioners, nurses, social workers and other health care professionals who work together with a person's primary care team to provide an extra layer of support for people with serious illness.
It is appropriate at any age and at any stage of a life-limiting illness and can be provided along with curative-intent treatment.
Specialist palliative care providers have recognized qualifications or accreditation in palliative care. They have advanced training, and their main practice is in palliative care. Specialist palliative care providers provide direct care to patients with complex palliative care needs in hospice, hospitals and home care settings; and provide consultation services to support, advise, and educate non-specialist clinicians who provide palliative care.
-
Spirituality
-
An existential construct inclusive of all the ways in which a person makes meaning and organizes their sense of self around a personal set of beliefs, values and relationships. Spirituality is sometimes understood in terms of transcendence or inspiration. Involvement in a community of faith and practice may, or may not, be a part of an individual's spirituality.
-
Underserviced Populations
-
Includes people who have unique needs that may make access to palliative care more difficult than it is for the average Canadian. Included in this definition are: perinatal, infants, children, adolescents and young adults; the elderly; Indigenous Peoples; racial or ethnic minorities; members of the LGBTQ2 community; immigrants and refugees; individuals who have illnesses other than cancer; those who live in rural and remote communities, or are socioeconomically disadvantaged, homeless, or have mental or cognitive impairments. Challenges in access may be due to lack of:
- Understanding about the goals of palliative care or how to access it;
- Knowledge about or access to Canadian health care systems;
- Ability to speak in Canada's two official languages (English or French);
- Services appropriate to age or developmental stage;
- Insurance due to unstable housing or citizenship status;
- Predictable illness patterns; and
- Proximity to services.
Appendix G: References
- Footnote 1
-
For the purposes of this Framework, the definition of family includes not only biological family but also "family of choice": anyone a person chooses to be in their circle of informal caregivers, see Appendix F Glossary.
- Footnote 2
-
Note the WHO is currently updating their definition based on consultations with key stakeholders. Once it is available, Health Canada will review it for applicability and reserves the right to replace the current version with the updated version.
- Footnote 3
-
The WHO also has a palliative care definition specific to paediatric palliative care. http://www.who.int/cancer/palliative/definition/en/
- Footnote 4
-
Palliative Care Matters, 2017. http://www.palliativecarematters.ca/home/
The Way Forward, 2015. http://hpcintegration.ca/resources/the-national-framework.aspx
Right to Care: Palliative Care for all Canadians. Canadian Cancer Society, 2016. http://www.cancer.ca/~/media/cancer.ca/CW/get%20involved/take%20action/Palliative-care-report-2016-EN.pdf?la=en - Footnote 5
-
CIHI, Access to Palliative Care in Canada, 2018. https://www.cihi.ca/en/access-data-and-reports/access-to-palliative-care-in-canada
- Footnote 6
-
Canadian Hospice Palliative Care Association, The Way Forward (2014) surveys of health care professionals. http://hpcintegration.ca/resources/health-care-professional-research.aspx
- Footnote 7
-
Distinguishing palliative care from medical assistance in dying (MAID): MAID is a medical intervention which intentionally ends a person's life at their request, while palliative care intends neither to hasten nor postpone death, and should be available over the continuum of care of a life-limiting illness.
- Footnote 8
-
See Appendix B for more details of federal programming and supports related to palliative care
- Footnote 9
-
Senator Carstairs led the Senate Committees and conducted her own follow-up reports in 2005, 2010, and 2015
- Footnote 10
-
The Way Forward, 2015. http://hpcintegration.ca/resources/the-national-framework.aspx
Palliative Care Matters, 2017. http://www.palliativecarematters.ca/home/ - Footnote 11
-
A detailed description of these organizations is contained in Appendix D.
- Footnote 12
-
See Appendix F Glossary for definition of Compassionate Communities
- Footnote 13
-
Advance care planning is a process to articulate and document care wishes in advance of need - See Appendix F Glossary for more information
- Footnote 14
-
A Compassionate Community is a group of people that provide compassion, care and practical supports to patients who are seriously ill or frail, and their families, throughout the illness and bereavement. See Appendix F Glossary for more information.
- Footnote 15
-
The 2015 Quality of Death Index: Ranking Palliative Care Across the World. The Economist Intelligence Unit (EIU) evaluates 80 countries to measure the quality of palliative care based on 20 indicators across five categories including the palliative and healthcare environment, human resources, the affordability of care, the quality of care and the level of community engagement. To build the Index the EIU used official data and existing research for each country, and also interviewed palliative care experts from around the world.
- Footnote 16
-
In May 2016, Member of Parliament Marilyn Gladu introduced Private Member's Bill C-277, An Act providing for the development of a framework on palliative care in Canada (Framework). It received strong Parliamentarian and stakeholder support. The Bill received Royal Assent and became law on December 12, 2017.
- Footnote 17
-
There are other excellent examples, including the Canadian Society of Palliative Care Physicians model in their November 2016 report: How to improve palliative care in Canada http://www.cspcp.ca/tag/how-to-improve-palliative-care/
- Footnote 18
-
A "Distinctions-based approach" ensures that the unique rights, interests and circumstances of First Nations, Inuit and Métis are acknowledged, affirmed, and implemented. A "distinctions-based approach to care" is one in which the strategies and policies developed to support that care reflect these distinctions. See Appendix F - Glossary for more information.
- Footnote 19
-
During the Consultation, particular focus was paid to access issues for underserviced populations. These populations are identified as any group (geographic, cultural, racial, socio-economic, age, etc.) that faces unique barriers in accessing palliative care. See Appendix F Glossary "Underserviced Populations".
- Footnote 20
-
See Appendix F Glossary for definition.
- Footnote 21
-
In "The Way Forward" initiative, the CHPCA also included a number of background documents, including a synthesis of recommendations from national reports, regarding improving palliative care: http://hpcintegration.ca/resources/discussion-papers/review-of-parliamentary-and-senate-reports.aspx
- Footnote 22
-
"Person-reported outcomes" are measures of the person's health condition that come directly from the person, without interpretation of the person's response by a clinician or anyone else
- Footnote 23
-
Canadian Hospice Palliative Care Association. (2014). Lexicon, The Way Forward Initiative: An Integrated Palliative Approach to Care. Accessed from: http://www.hpcintegration.ca/media/53072/TWF-lexicon-eng-final.pdf