Full report: Mobilizing Public Health Action on Climate Change in Canada
Download in PDF format
(6.40 MB 105 pages)
Organization: Public Health Agency of Canada
Date published: 2022-10-25
Cat.: HP2-10E-PDF
ISBN: 1924-7087
Pub.: 220351
Chief Public Health Officer of Canada's Report on the State of Public Health in Canada 2022
On this page
- Message from the Chief Public Health Officer of Canada
- About this report
- Section 1: Climate change: A threat to health, well-being, and our planet
- Climate change as a global problem
- Health in a changing climate: the Canadian context
- From climate hazards to health impacts: The health risks of climate change in Canada
- Vulnerability and inequitable health risk
- Bringing public health and climate action together to address the threat
- Current public health action in a changing climate
- Section 2: Opportunities to advance climate action in public health
- Implement a range of interventions to address immediate health challenges and prevent future health risks from a changing climate
- Prioritize community expertise and engagement for equitable and effective climate action
- Advance knowledge to understand, predict, and respond to the health impacts of climate change
- Collaborate across sectors for transformative climate-health action and intersectoral co-benefits
- Strengthen public health leadership for climate action and public health building blocks for climate resilience
- Way forward
- Appendix A: Essential public health functions and public health climate action
- Appendix B: An update on COVID-19 in Canada
- Appendix C: Methodology
- Acknowledgements
- References
Message from the Chief Public Health Officer of Canada

Dr. Theresa Tam
Over the past 2 and a half years, we have been challenged by the COVID-19 pandemic. Through our collective response as a society, we have made tremendous progress across Canada, averting many infections and saving many lives. And while we must continue to evolve our management of COVID-19 and its longer-term impacts, we must also turn our attention to other health threats. This includes what is arguably the largest looming threat to the health of our communities and our planet: the climate crisis.
Climate change is making weather patterns more unpredictable and causing more frequent and intense extreme weather events, like heatwaves, hurricanes, flooding, and wildfires. It also threatens the availability and safety of our water and food.
The changing climate is already having a measurable impact on our health, both physically and mentally. For example, it is exacerbating the spread of climate-sensitive infectious diseases and worsening chronic conditions due to heat exposure or poor air quality. And whether it is weeks of breathing wildfire smoke, or suffering through record-setting heatwaves, or being unable to reach traditional grounds to hunt for food, no one is immune to the impact of our changing climate. Not all communities are affected equally, however. Like COVID-19, some face greater risk of exposure, are less able to adapt and more vulnerable to serious health outcomes.
This is a pivotal time for public health systems to draw on the lessons learned from the pandemic, show leadership, and work collaboratively with other sectors. We must continue to bring climate considerations into public health work to prepare for, and respond to, the now inevitable health impacts. This means supporting communities to adapt to the climate risks they will face.
But we also need to put health at the centre of climate action and focus on efforts that will lead to significant and near immediate health and environmental benefits. By advocating for healthy environments like walkable neighbourhoods, cycling, and public transit, we can reduce chronic diseases, premature deaths and hospital admissions, promote positive mental well-being and reduce air pollution. By supporting more tree canopies and building retrofits, we can promote and protect health while mitigating greenhouse gas emissions.
It is clear, climate action is good for our health and public health systems have a critical role to play.
In last year's report, A Vision to Transform Canada's Public Health System, I raised the alarm that, without immediate attention, Canada's public health systems will not be able to respond to overlapping emergencies or carry out essential core functions that keep communities healthy and safe. Even now, as we continue to contend with COVID-19, monkeypox has emerged as a threat globally.
My 2022 Annual Report lays out a roadmap for the broader public health system in Canada to organize and mobilize around climate-health action. It provides concrete direction on how we can use our existing tools and knowledge, while also expanding them to meet new challenges that will come along with a changing climate.
Climate change will truly test our readiness on all fronts. Our actions now will determine the magnitude of future impacts, how quickly they occur, and the extent to which our communities and future generations are able to recover and thrive.
First Nations, Inuit, and Métis Peoples have long recognized the interconnected nature of human, animal, and environmental health. This knowledge has been central to Indigenous identity, resilience, and survival and is essential to a healthy and sustainable future for us all. It is time to embrace Indigenous ways of looking at our place in the natural world. We are not separate from our environment. To be healthy, our air, water, land, and ecosystems must also be healthy.
What lies ahead is no small task. But we know climate action works. We have the tools to understand climate change and figure out how to address this complex and growing challenge to our collective health. By acting together now, we have hope.
Dr. Theresa Tam
Canada's Chief Public Health Officer
About this report
Every year, the Chief Public Health Officer of Canada (CPHO) writes a report on the state of public health in Canada to raise the profile of public health issues, stimulate dialogue, and catalyse action. This year's report focuses on the impacts of climate change in Canada and the role that public health systems can play in taking climate action. It builds on the 2021 CPHO Annual Report by presenting the possibilities of what a strengthened and resilient public health system can do in the face of complex and urgent public health challenges.
The following key concepts are central to the report.
- Adaptation
- The process of modifying our decisions, activities, and ways of thinking to be proactive and better prepared, as well as reactive and better able to respond to a changing climate and its impacts on health.Footnote 1Footnote 2
- Adaptive capacity
- The ability to adjust to or take protective measures against climate hazards and respond to or cope with the health consequences of climate hazards. Existing social inequities mean not all communities or populations have the knowledge, tools, strategies, or financial resources to implement needed climate change and health adaptation actions.Footnote 1Footnote 3Footnote 4
- Co-benefits
- The positive effects that a policy or measure aimed at one objective might have on other objectives. For example, climate mitigation efforts across energy, infrastructure, agriculture, and transportation sectors can improve population health by way of cleaner air, improved housing standards, healthier diets, and increased physical activity.Footnote 1Footnote 5Footnote 6Footnote 7
- Ecological determinants of health
- The elements of nature that are vital for life on Earth, including food sources, fresh water, oxygen, materials to construct shelters and tools, abundant energy, and reasonably stable global climate with temperatures conducive to human and other life forms. Maintaining the integrity, stability, and equitable distribution of these natural systems is an essential condition for health, survival, and prosperity.Footnote 8Footnote 9
- Intersectoral work
- Collaborative approaches used between groups, including government agencies, non-governmental organizations, and relevant stakeholders that have a common goal in addressing a specific issue. In a changing climate, this refers to the actions of many sectors in collaboration, including the health sector, that benefit health and climate change outcomes.Footnote 10Footnote 11Footnote 12
- Maladaptation
- Deliberate adjustments in natural or human systems that increase vulnerability to climatic impacts, resulting in an adaptation that fails in reducing vulnerability and may, instead, increase it.Footnote 13
- Mitigation
- An intervention that aims to reduce the causes of climate change, remove heat-trapping greenhouse gases from the atmosphere, and stabilize their levels.Footnote 1Footnote 2
- One Health
- A collaborative, multi-sectoral, and transdisciplinary approach to achieving optimal health outcomes that recognizes the interconnection between people, animals, plants, and their shared environment.Footnote 14
- Social determinants of health
- Forces and systems that shape the conditions of people's daily lives (e.g., income, education, employment) and influence their health and well-being outcomes. These include economic, social, and political policies and systems, as well as social norms.Footnote 15Footnote 16
- System resilience
- The capacity of social, economic, and environmental systems to cope with a hazardous event, trend, or disturbance. It involves responding in ways that maintain their essential function, identity, and structure, while also maintaining the capacity for adaptation, learning, and transformation.Footnote 1Footnote 5
- Vulnerability
- The predisposition for health to be adversely affected by climate change. This is shaped by the degree of exposure to climate change hazards, the susceptibility to climate change impacts, and the ability to cope with the health impacts of climate change. In public health, the concept of vulnerability can be highly stigmatizing, so it is important to recognize that climate vulnerability is not a label for communities or populations.Footnote 1Footnote 5Footnote 17
Orientation of the report
Section one describes the urgency of climate change. It provides an overview of how climate change is impacting the health and well-being of people living in Canada. Like COVID-19, these impacts are disproportionate and compounding, with some communities affected more than others. These far-reaching population health impacts offer compelling evidence for why public health systems must prioritize and mobilize around this issue.
Section two offers a roadmap for public health action on climate change. It explores opportunities to build on and expand current public health activities, while strengthening public health systems to address this and other complex public health issues.
The way forward outlines cross-cutting priority areas with tangible ideas for system-level actions.
The COVID-19 appendix gives a brief update on the evolution of the COVID-19 pandemic in Canada between August 2021 and August 2022.
This report benefits from the leadership and expertise of many contributors. This includes text boxes provided by partners at the National Collaborating Centres for Public Health that illustrate practical examples of public health action.
What We Heard Report: Perspectives on Climate Change and Public Health in Canada is a companion resource that has informed the development of this report. It is a summary of interviews and focus group discussions with university-based researchers, public health practitioners, non-governmental public health organization leaders, municipal-to-federal government public health system employees, community leaders, and medical practitioners. These experts' voices are woven through the CPHO report.
An additional way in which the report can be actioned is through generating new knowledge or research. Generating Knowledge to Inform Public Health Action on Climate Change provides a list of research opportunities relating to the report to help guide researchers, funders, and others wishing to mobilize research and knowledge.
Land acknowledgement
We respectfully acknowledge that the lands on which we developed this report are the homelands of First Nations, Inuit, and Métis Peoples. Specifically, this report was developed in the following cities:
- In Ottawa, also known as Adawe, on the traditional and unceded territory of the Algonquin People, members of the Anishinabek Nation Self-Government Agreement.
- In Halifax, also knowns as K'jipuktuk, a part of Mi'kma'ki, the ancestral and unceded territory of the Mi'kmaq People. This territory is covered by the "Treaties of Peace and Friendship" which Mi'kmaq and Wolastoqiyik (Maliseet) Peoples first signed with the British Crown in 1725. The treaties did not deal with surrender of lands and resources but in fact recognized Mi'kmaq and Wolastoqiyik (Maliseet) title and established the rules for what was to be an ongoing relationship between nations.
- In Montreal, also known as Tiohti:áke, the traditional and unceded territory of the Kanien'kehà:ka. A place which has long served as a site of meeting and exchange amongst many First Nations including the Kanien'kehá:ka of the Haudenosaunee Confederacy, Huron/Wendat, Abenaki, and Anishinaabeg.
- Lastly, in Toronto, also known as Tkaronto, the traditional territory of many nations including the Mississaugas of the Credit, the Anishnabeg, the Chippewa, the Haudenosaunee, and the Wendat peoples and is now home to many diverse urban First Nations, Inuit, and Métis Peoples. Toronto is within the lands protected by the Dish with One Spoon Wampum Belt Covenant, an agreement between the Haudenosaunee and Anishinaabe and allied nations to peaceably share and care for the resources around the Great Lakes.
We recognize that there is much more work ahead to address the harmful impacts of colonialism and racism that continue to generate inequities between Indigenous and non-Indigenous communities. We remain strongly committed to working collaboratively to advance reconciliation in Canada.
Section 1: Climate change: A threat to health, well-being, and our planet
"When the WHO [World Health Organization] says it's the greatest threat to health in the 21st century, why aren't we taking them at their word? Why aren't we accepting that? If this is the greatest threat to population health in the 21st century, let's start treating it like that."
Our changing climate is a crisis that threatens all aspects of life. The impacts can already be seen in our environment, our economy, and, crucially, our health and well-being.Footnote 5Footnote 18 Climate hazards will continue to emerge over the next 2 decades and beyond, and without significant action, the livability of the planet is at risk.Footnote 19 Climate change influences the core conditions of life, including the air we breathe, the food we eat, the water we drink, and the land we live on.Footnote 5Footnote 18Footnote 20Footnote 21Footnote 22Footnote 23 The rapidly changing climate also multiplies existing population health challenges, including the spread of climate sensitive infectious diseases, and exacerbates health inequities.Footnote 5Footnote 18Footnote 24
Without immediate and effective action, climate change poses catastrophic risks for present and future generations. We must act urgently to reduce these risks, as national and international assessments warn that the window to do so is closing.Footnote 5Footnote 25 Reducing heat-trapping greenhouse gas emissions is critical to limiting climate change. However, even with the most stringent mitigation efforts to reduce them, the planet will continue to warm over the next few decades because of the greenhouse gases already in the atmosphere.Footnote 19 To ensure continued livability of the planet and reduce the harm to our communities, ecosystems, and economies, we must act now and continue to reduce emissions while also working to adapt to the unavoidable current and future impacts.
For public health systems, the urgency of the situation requires assertive and effective action across jurisdictions and sectors to prevent, reduce, and address the health impacts of climate change. It will also require us to detect and monitor health threats and move forward with direct and collaborative action to address them. Through this work, public health can bring its focus on equity, health promotion, and intersectoral partnerships to the collective effort and contribute to climate action in a way that supports and protects health.
Climate change as a global problem
Climate change refers to the long-term shift in the average weather conditions of a region, such as temperature, precipitation, and winds.Footnote 26 It involves changes in average conditions as well as variability, such as extreme weather events.Footnote 27 The unprecedented heatwaves experienced across North America and Europe in the summers of 2021 and 2022, are recent consequences that have affected the day-to-day lives of many people.
These changes are caused by greenhouse gases, a large portion of which are released as a consequence of our heavy reliance on the burning of fossil fuels.Footnote 5Footnote 28Footnote 29 Every year, the combustion of coal, oil, and gas releases billions of tonnes of carbon dioxide into the atmosphere.Footnote 30 Other major greenhouse gases include methane, nitrous oxide, and chloroflurocarbons, released through fossil fuel production, agriculture, landfills, and the use of fertilizers.Footnote 31 Increasing concentrations of these gases in our atmosphere have resulted in unprecedented rises in average temperatures.Footnote 29 This warming has intensified weather systems, causing extreme heatwaves, wildfires, rising sea levels, floods, and droughts. Global temperatures will reach critical levels soon unless significant steps are taken around the world to drastically reduce our emissions.Footnote 32Footnote 33
As with COVID-19, the impacts of climate change are global, including threats to the necessities of life. Over 800 million people are currently undernourished, while climate change is increasing food insecurity through rising temperatures, changing patterns of precipitation, and more frequent extreme weather events.Footnote 5Footnote 34Footnote 35Footnote 36 Modelling suggests that 529,000 deaths worldwide could occur between 2010 and 2050 due to reductions in food availability and changes in consumption patterns related to climate change.Footnote 5Footnote 37 Even under a negative emissions scenario, which refers to activities which remove carbon dioxide from the atmosphere, increased deaths will occur.Footnote 5Footnote 37 These changes will aggravate living conditions broadly and the health of people globally.Footnote 35Footnote 38 Further, it is estimated that by 2050, 200 million people a year could need international humanitarian aid as a result of climate change. This is almost twice the number of people who required assistance in 2018 due to floods, storms, and wildfires.Footnote 5Footnote 39
Climate change threatens the livability of our cities and communities. Almost two-thirds of cities with populations of over 5 million are in areas at risk of sea level rise, while almost 40% of the world's population lives within 100 kilometres of a coast.Footnote 40 Without strong and coordinated action, places like New York, Shanghai, Abu Dhabi, Osaka, and Rio de Janeiro could be underwater within our lifetime, displacing millions of people.Footnote 41
The Intergovernmental Panel on Climate Change (IPCC), a body of the United Nations responsible for advancing knowledge on climate change, regularly assesses the latest science.Footnote 42 Its Sixth Assessment Report, Climate Change 2022: Impacts, Adaptation and Vulnerability assesses the impacts of climate change on ecosystems, biodiversity, and human communities at the global and regional levels.Footnote 43 It projects that under all scenarios, health risks will increase this century, causing injury and loss of life, impacting physical and mental health, damaging infrastructure and ecosystems, disrupting health care and other critical services, and threatening livelihoods.Footnote 44
These impacts will not be equally shared. Those who contribute the most to climate change are the least likely to experience its adverse impacts.Footnote 45 Globally, children will bear 88% of the burden of disease from climate change.Footnote 5Footnote 46 Conditions such as poverty and socioeconomic or political marginalization can put women, children, older adults, and other populations at a disadvantage in coping.Footnote 35Footnote 47Footnote 48 For example, children facing poverty are at increased risk during urban floods and droughts, which can contaminate water and lead to diarrhoeal illness.Footnote 35Footnote 49 People living in low- and medium-income countries, the most vulnerable in high-income countries, and Indigenous communities, are already bearing an inequitable and disproportionate share of climate impacts.Footnote 45
Importantly, the IPCC recognizes colonialism as one driver of climate change vulnerability across the globe.Footnote 19 For that reason, international climate action must acknowledge and respect the rights of Indigenous Peoples. Worldwide, Indigenous Peoples are particularly sensitive to the impacts of climate change because of their close relationships with and dependence on the land, ecosystems, and natural resources.Footnote 50 Through intergenerational and traditional knowledge, Indigenous Peoples were amongst the first to notice changes in our climate and have critical understanding for navigating and adapting to it.Footnote 51 Globally, Indigenous worldviews are gaining prominence, emphasizing the interconnected nature of the land, animals, plants, and people.Footnote 52Footnote 53Footnote 54 Further, the United Nations Declaration on the Rights of Indigenous Peoples (UNDRIP) sets out the right to the "conservation and protection of the environment".Footnote 55Footnote 56Footnote 57Footnote 58 If we are to take strong and sustainable action on climate change at all levels, it must honour Indigenous rights and expertise.
While the situation is urgent, there is still hope. The global response to climate change is increasingly focused on the health impacts. In 2021, over 200 international health journals published editorials about the catastrophic harm to health, and the critical need for action.Footnote 59 At the 26th United Nations Climate Change Conference (COP26), the World Health Organization (WHO) led a parallel conference focused on health, equity, and climate change. Currently, 60 countries have committed to at least one of the initiatives on climate-resilient and low carbon sustainable health systems promoted under the COP26 Health Program.Footnote 60 The upcoming COP27 is expected to convene the global health community and partners to ensure health and equity are at the centre of the conference's climate negotiations.Footnote 61 Findings from a global survey published by the WHO indicate that over 60 countries have either conducted a climate change and health vulnerability assessment or are currently carrying out one. These assessments are crucial to establish an evidence base to understand health risks, evaluate which groups are more vulnerable, identify gaps in current action, and identify effective adaptation measures to support decision-making.Footnote 62
International public health organizations and communities have also been actively working to bring attention to the climate health issue. The International Association of National Public Health Institutes (IANPHI) released a Roadmap for Action on Health and Climate Change at COP26. It highlights existing and potential roles for national public health institutes in climate action and includes commitments for supporting their adaptation and mitigation efforts and policy development.Footnote 45 In 2020, IANPHI created a climate change working group to promote international collaboration between national public health institutes and other stakeholders.Footnote 63
Health in a changing climate: the Canadian context
There is plenty of evidence that climate change is already impacting the health and well-being of people living in Canada.Footnote 5 In June 2021, Western Canada experienced a historic heat dome, which set a Canadian record high temperature of 49.6°C in Lytton, British Columbia and led to 619 heat-related deaths.Footnote 64Footnote 65Footnote 66 A major heatwave in Quebec resulted in 86 deaths in 2018, which was the hottest summer on record in 146 years of meteorological observations in the province.Footnote 5Footnote 67Footnote 68Footnote 69 Further, the area burned by wildfires in Canada has doubled from the 1970s to the 2000s.Footnote 5Footnote 70 In 2021, a record dry spring across the country fueled an early start of wildfire season which ultimately saw 2,500 more active fires recorded than the previous year.Footnote 65 Millions of people in Canada were exposed to wildfire smoke and nearly 50,000 evacuations occurred in British Columbia alone.Footnote 65
In a country with over 243,000 kilometres of coastline populated by about 6.5 million people, rising sea levels pose serious threats to Canada's coastal areas, ecosystems, and communities.Footnote 71 While sea level changes vary significantly by location some regions, such as Atlantic Canada, are expected to exceed the global average.Footnote 5Footnote 72 This poses immediate and long-term risks, including coastal erosion, increased storm surge risk, saltwater intrusion, flooding, and damage to infrastructure, personal property, and transportation.Footnote 65Footnote 71Footnote 72 Additionally, in the North, where temperatures are warming most rapidly, thawing permafrost, changing ice and snow conditions, and shifting wildlife habitat threaten entire ways of life. The range of impacts include culture, infrastructure, livelihoods, food security, and water quality.Footnote 5Footnote 21Footnote 72Footnote 73Footnote 74 Currently, permafrost underlies 40% of Canada's landmass; however, estimates suggest this could decrease by 16% to 20% by 2090.Footnote 75Footnote 76
Offshore, the warming and acidification of oceans create irreversible ecosystem shifts that disrupt wildlife populations and food supplies.Footnote 5 Increasing atmospheric temperatures and humidity can worsen air pollution and create favorable conditions that facilitate the spread of vector-borne diseases, such as Lyme disease.Footnote 5Footnote 77Footnote 78Footnote 79Footnote 80Footnote 81 Figure 1 illustrates a few of the wide-ranging climate change impacts experienced across Canada, each of which influences health and well-being. Through interactive maps, videos, and articles, the Climate Atlas of Canada provides further information on projected climate change impacts and how they affect regions differently.Footnote 82 It is important to note, however, that even though many climate hazards are seen regionally, their impact can have far reaching effects.
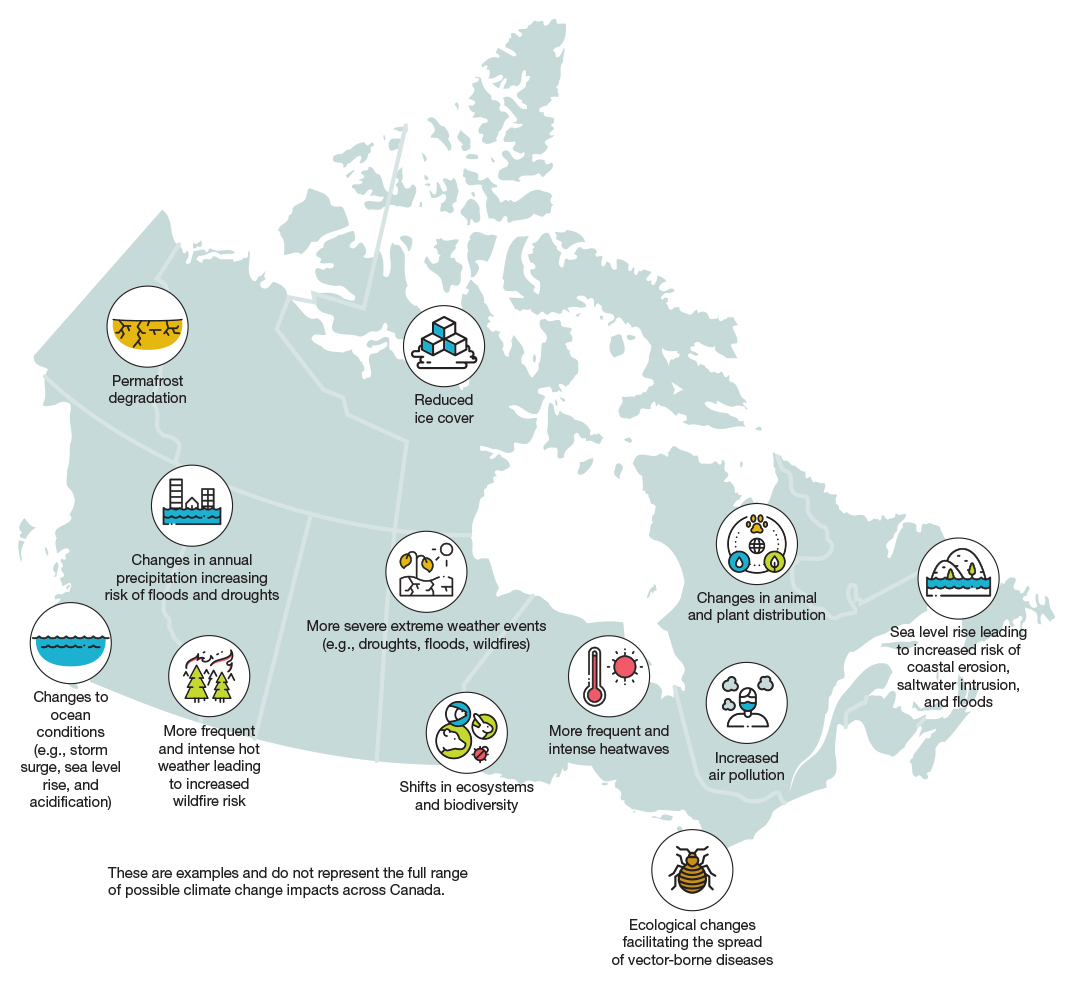
Source: Figure adapted from Council of Canadian Academies. Canada's Top Climate Change Risks (2019).
Figure 1: Text description
The figure provides examples of climate change impacts, overlaid across a map of Canada. These examples do not represent the full range of possible climate change impacts across Canada.
Western Canada (i.e., British Columbia, Alberta): changes to ocean conditions (e.g., storm surge, sea level rise, and acidification), changes in annual precipitation increasing risk of floods and droughts, and more frequent and intense hot weather leading to increased wildfire risk.
The Prairie Provinces (i.e., Alberta, Saskatchewan, Manitoba): more severe extreme weather events (e.g., droughts, floods, wildfires), and shifts in ecosystems and biodiversity.
Central Canada (i.e., Ontario, Quebec): more frequent and intense heatwaves, increased air pollution, and ecological changes facilitating the spread of vector-borne diseases.
Atlantic Canada (i.e., New Brunswick, Nova Scotia, Prince Edward Island, Newfoundland and Labrador): sea level rise leading to increased risk of coastal erosion, saltwater intrusion, and floods.
Northern Canada (i.e., Yukon, Northwest Territories, Nunavut): permafrost degradation, reduced ice cover, and changes in animal and plant distribution.
In 2015, Canada ratified the Paris Agreement, along with 195 other countries.Footnote 32 This legally binding treaty sets long-term goals for member states to limit global warming to well below 2°C compared to pre-industrial levels, with significant efforts to limit global temperature increases to no more than 1.5°C.Footnote 32 To date, average global temperatures have increased 1.1°C.Footnote 84 If global greenhouse gas emissions continue at their current rate, there is a high risk that the world will exceed the 1.5°C target between 2030 and 2052. The current pace of international climate action is too slow. Evidence indicates that global temperatures will exceed the 2°C threshold by the end of this century, unless there are significant and rapid emission reductions across every sector.Footnote 85
Each increment of future warming poses significant risks and increases the probability of compounding impacts to human, animal, and plant health and survival. However, limiting average increases in global temperatures to 1.5°C will reduce the risks of severe climate change outcomes. Exceeding that threshold will lead to numerous preventable illnesses, injuries, and deaths worldwide as a result of disease outbreaks and extreme weather events.Footnote 86 Meanwhile, a 2°C average rise in global temperatures will cause more extreme conditions and dramatic alterations to land, air, and water systems that support survival of all species. The resulting damage will be irreversible in some cases. It is projected that a 2°C increase over pre-industrial levels will regularly expose over one-third of the world's population to health-threatening heatwaves, along with rising sea levels that will increase the risk of flooding for 10 million more people worldwide.Footnote 84Footnote 87
As a whole, Canada is warming at a rate 2 times faster than the global average, while the North is warming 3 to 4 times faster (Figure 2).Footnote 5Footnote 23Footnote 74 Since 1948, average temperatures in this country have increased by 1.7°C, while northern Canada, which encompasses nearly two-thirds of the nation's total landmass, has warmed on average by an alarming 2.3°C.Footnote 23 With a low greenhouse gas emission scenario that is in line with the Paris Agreement, climate models project annual mean temperature will increase in Canada by a further 1.8°C by 2050. In a high heat-trapping greenhouse gas emission scenario, Canada's annual mean temperature will increase by more than 6°C by the end of this century.Footnote 88 The reality is that with even the most stringent greenhouse gas mitigation efforts in place, we are locked into warming patterns for the next few decades because of the greenhouse gases already in the atmosphere.Footnote 89Footnote 90 However, the worsening situation in a high emissions scenario will potentially exceed our ability to respond and protect health.
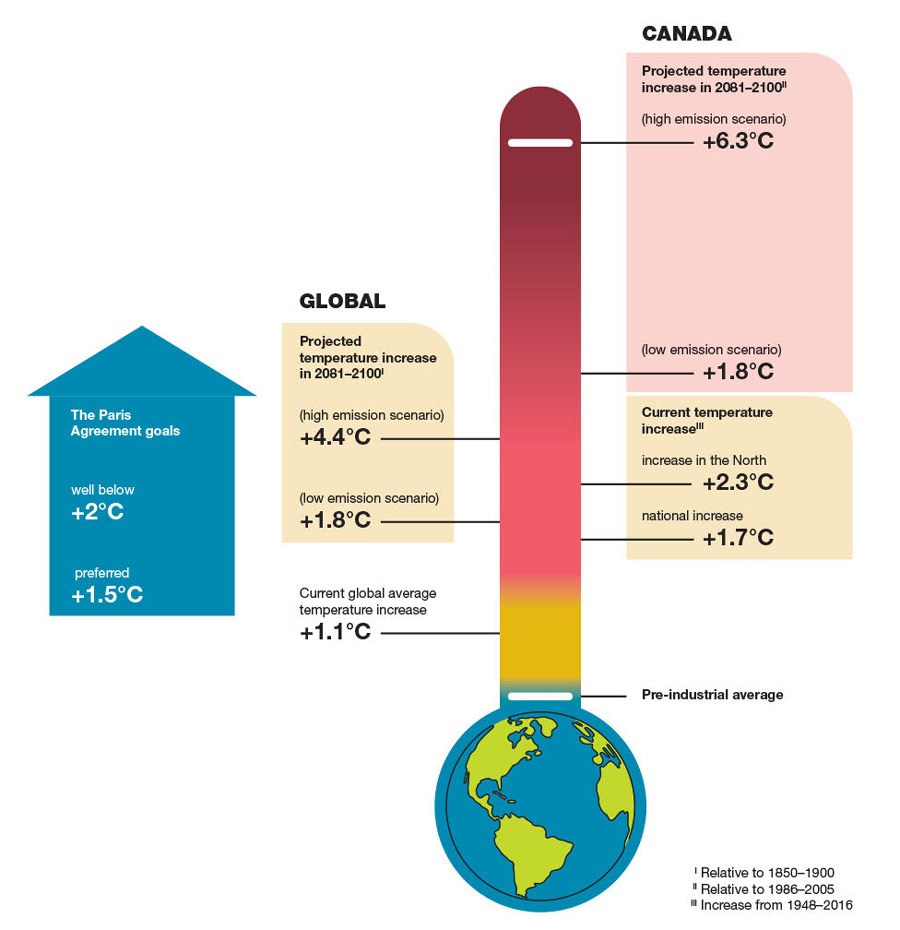
Sources: Government of Canada. Canada's Changing Climate Report (2019). Intergovernmental Panel on Climate Change. Summary for Policymakers. In: Climate Change 2021: The Physical Science Basis. Contribution of Working Group I to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change (PDF) (2021).
Figure 2: Text description
The figure depicts the goals of the Paris Agreement, as well as current and projected temperature increases globally and in Canada by a given year.
The Paris Agreement goals:
- Well below +2 degrees Celsius
- +1.5 degrees Celsius (preferred)
Current global average temperature increase:
- +1.1 degrees Celsius
Global projected temperature increase in 2081-2100 (relative to 1850-1900):
- +4.4 degrees Celsius (high emission scenario)
- +1.8 degrees Celsius (low emission scenario)
Canada's current temperature increase (annual mean temperature increase from 1948-2016):
- +2.3 degrees Celsius in the North
- +1.7 degrees Celsius national increase
Canada's projected temperature increases in 2081-2100 (relative to 1986-2005):
- +6.3 degrees Celsius (high emission scenario)
- +1.8 degrees (low emission scenario)
The health impacts of climate change will become more severe as average annual temperatures increase in the absence of rapidly scaled up adaptations.Footnote 5Footnote 22Footnote 91 These progressive changes also have the potential to limit the effectiveness of available adaptation efforts, making it more difficult to protect the health of the population.Footnote 19 This underscores the importance of international agreements in climate mitigation and adaptation, which can offer significant co-benefits to health. These co-benefits occur when policies aimed at other sectors, such as the environment, also produce positive impacts for health and well-being.Footnote 1 For example, effective mitigation efforts across energy, transportation, building, infrastructure, and agriculture sectors can result in cleaner air, increased levels of physical activity, improved housing standards, healthier diets, lower chronic diseases burden, and lives saved.Footnote 7
From climate hazards to health impacts: The health risks of climate change in Canada
The pathways that connect exposure to climate hazards to health impacts are complex and layered (Figure 3). Vulnerabilities, such as socioeconomic status or geographic location, increase the potential for negative health impacts at individual, community, and population levels.Footnote 5Footnote 43 While some climate hazards, such as severe storms, can result in easily identified negative health outcomes (e.g., injury or death), the health impacts of climate change often do not occur in isolation.Footnote 5Footnote 44 For example, exposure to extreme weather events can cause injury, but may also result in long-term mental health impacts due to displacement, property damage, or loss. Individuals and communities can face multiple and cascading threats at the same time, or compounding impacts over time.Footnote 5Footnote 44 Floods may cause destruction to crucial community infrastructure like power and water supplies, but also lead to food security issues as a result of disruptions or damage to food production processes and systems.Footnote 92 These risks can become more severe if climate threats multiply or repeat. Understanding these pathways, as well as the conditions that create vulnerability, helps identify entry points for public health action and intervention.

Figure 3: Text description
The model describes the impacts of climate change on health. This vertical model works from top to bottom and begins by describing the key drivers of climate change, which influence changes to the Earth's atmosphere and lead to climate impacts. It then describes the pathways from climate hazards to climate sensitive health outcomes.
The key drivers of climate change include a culture of exploitation and belief that nature exists for human use alone, unsustainable economic growth and development, and deforestation and changes in land use.
These drivers influence changes to Earth's atmosphere. Burning of fossil fuels on a mass scale to power homes, vehicles, and agricultural and manufacturing processes leads to the release of greenhouse gases like carbon dioxide and methane that trap heat in the Earth's atmosphere. Destruction of carbon sinks (e.g., trees and plants that trap greenhouse gases and keep them out of the atmosphere) leads to Earth losing some of the ability to absorb carbon dioxide.
Changes to the Earth's atmosphere influence climate impacts, such as increases in local, regional, and global temperatures, ocean acidification, and altered weather patterns.
Climate impacts lead to climate hazards, including:
- Extreme weather events: landslides, wildfires, floods, and storms;
- Heat stress: rise in average temperature, extreme hot days, heat waves, and the heat island effect;
- Air quality: rise in air pollutants;
- Infectious diseases: changes in habitat range of vectors and animals, increasing the risk of vector-borne and zoonotic disease;
- Food quality, safety, and security: crop damage from changes in temperature and precipitation, reduced quality or access to traditional foods, and damage to food distribution infrastructure;
- Water quality, safety, and security: water scarcity, contamination of water sources through flooding, and changes in rainfall patterns; and,
- Slow onset climate events: drought, glacial retreat, desertification, and sea level rise.
While specific climate sensitive health outcomes are listed below certain climate hazards, these outcomes can be influenced by a number of different climate hazards, as well as their interconnections.
These pathways ultimately lead to climate sensitive health outcomes, such as:
- Extreme weather events: injury, death, mental health impacts, and limited access to essential supplies and services;
- Heat stress: heat stroke, dehydration, cardiovascular and respiratory impacts, mental health impacts, and pregnancy complications;
- Air quality: exacerbation of respiratory conditions (e.g., asthma), cardiovascular diseases, and allergies;
- Infectious diseases: Lyme disease, West Nile virus, and Hantavirus;
- Food quality, safety, and security: food-borne illness, undernutrition, food insecurity, and cultural and nutritional loss of food;
- Water quality, safety, and security: water-borne diseases caused by parasites or bacteria, and algal blooms; and,
- Slow onset climate events: effects on physical and mental health, increased food and water insecurity, poverty, forced migration, and conflict.
Compounding factors influence vulnerability and increase the potential for negative health outcomes as a result of exposure to climate hazards. These factors include socioeconomic status and other social determinants of health, health and nutritional status, age, and geographic location.
These are examples and do not represent the full range of possible climate hazards or climate sensitive health outcomes.
Climate-resilient health systems that are able to cope with climate change while continuing to deliver essential public health functions are the foundation of an effective response. Resilient public health systems can anticipate, respond, cope, recover from, and adapt to climate-related shocks and stresses.Footnote 5Footnote 93 This goes hand-in-hand with healthcare systems that are more resilient to adverse weather conditions, supply chain disruptions, and service delivery. As the WHO has identified, climate resilience is necessary for health systems to increase their capacity to protect and promote health in an unstable and changing climate.Footnote 94
Climate hazards, exposure pathways, and health impacts
As our climate continues to change, existing health threats will intensify, and new risks will emerge. While we are still learning about the full scope of the health impacts of climate change, existing research has generated important evidence about climate hazards, exposure pathways, and health risks, such as infectious diseases and mental health impacts. This section will summarize key findings on some of the health impacts of climate change.
Exposure to extreme weather events such as floods, droughts, and tornados, or natural hazards like wildfires and landslides, pose serious health and safety risks. In addition to the potential for injury, illness, and death, these events can also impact health through isolation, disruption of infrastructure by way of power outages, property damage, evacuations, and associated displacement from homes, jobs, and school.Footnote 5Footnote 72 Extreme weather can also restrict access to food and water supplies.Footnote 72 A major snowstorm in St. John's, Newfoundland and Labrador in 2020 caused a state of emergency, forcing businesses, including grocery stores, to close for 4 days. This disruption in the regional food supply chain, coupled with high consumer demand, meant many people were unable to purchase basic food staples.Footnote 5
Extreme weather events can also limit or delay vital access to health, social, and community supports and services. Hospitals affected by flooding may need to close emergency rooms, delay medical procedures, evacuate patients, and reduce operational capacity if staff are unable to travel to work. In northern communities, access to medical services can also be compromised by inaccessible roads due to thawing permafrost, flooding, and wildfires.Footnote 95Footnote 96Footnote 97
Heat stress and heat-related health risks are linked to periods of abnormally high temperatures. Extreme heatwaves are already being felt by millions of people each year across Canada.Footnote 64Footnote 98 Direct health impacts linked to heat exposure are extensive and include heat stroke, dehydration, mental health impacts (e.g., mental health-related hospitalizations, suicidality), pregnancy complications, cardiovascular and respiratory disease, and death.Footnote 5Footnote 91Footnote 99 In Ontario, between 1996 and 2010, each 5°C increase in temperature during the summer was associated with a 2.5% increase in death, with a particular link to cardiovascular disease.Footnote 5 The 2010 and 2018 Quebec heatwaves saw increases in daily mortality, emergency room visits, ambulance trips, and hospitalizations.Footnote 67Footnote 68 Other health implications include loss of biodiversity, transmission of diseases, food insecurity, and drought.Footnote 35Footnote 100 Heatwaves and the associated health impacts are projected to become more severe and intense as annual average temperatures continue to rise across the country.Footnote 5Footnote 101
Extreme heat poses amplified risks to many populations, with disproportionate impacts on older adults, children, infants, people with certain pre-existing physical and mental health conditions, people who live or work outdoors, and those with limited financial or social supports to protect themselves from heat.Footnote 102Footnote 103 Many people experiencing homelessness face increased exposure to extreme weather events.Footnote 5Footnote 104 Prolonged exposure to extreme heat can exacerbate pre-existing health conditions and risk behaviours, including mental health, chronic diseases, and substance use.Footnote 5Footnote 104Footnote 105Footnote 106 Additionally, people without safe and consistent housing can experience challenges connecting to heat warning systems, which also provide information on cooling strategies.Footnote 5Footnote 104 People experiencing homelessness may also find it difficult to access drinking water or to keep food from spoiling during extreme heat events.Footnote 5Footnote 104
In Canada, the reality of climate change means that extreme heat events are becoming more frequent and more intense.Footnote 66 Public health research and coroners' reports have indicated that people and groups of people experiencing material and social deprivation are at highest risk, with a clear link between high indoor temperatures and heat-related injury and death.Footnote 66 Specifically, older adults, those who live with disabilities, mental illness, and chronic diseases, and those who do not have access to air conditioning or protection from surrounding green space, are among those most at risk to extreme heat.Footnote 107 There is ongoing work to understand the consequences of extreme heat and the opportunities for climate-health action to address dangerous indoor temperatures (see text box "Evidenced-based policies and the indoor built environment: limiting indoor temperatures to prevent heat-related injuries and deaths").
Evidenced-based policies and the indoor built environment: limiting indoor temperatures to prevent heat-related injuries and deaths
One key step towards climate change resilience will involve setting a national maximum indoor temperature standard. Once this has been set, building codes, building standards, residential tenancy laws, and purposeful urban design can be used to achieve it. At the same time, strengthening social networks and mitigating the risks of social isolation (e.g., performing health checks during extreme heat events) will also be necessary to reduce the number of heat-related injuries and deaths in coming years.Footnote 108
In Canada, we have mandated minimum indoor temperatures to protect health during cold winters; however, there are no maximum indoor temperatures to protect health during hot weather.Footnote 109Footnote 110 There is evidence that exposure to indoor temperatures above 26°C is associated with increases in emergency calls and death.Footnote 107Footnote 111Footnote 112Footnote 113Footnote 114Footnote 115 An upper limit of 26°C indoors has been proposed as sufficient to protect most occupants from heat-related injury and death, including those more susceptible due to age or health conditions.Footnote 107Footnote 111Footnote 112Footnote 113Footnote 114Footnote 115
Keeping buildings cool in a warming climate
Widespread use of central air conditioning is one way to ensure indoor temperatures do not exceed 26°C. However, this also contributes to greenhouse gas emissions, strains power supplies during extreme heat events, and creates the potential for mass casualties during a power outage.Footnote 116Footnote 117Footnote 118Footnote 119 A multi-faceted approach is required to promote sustainable healthy indoor temperatures. These approaches must be tailored to different types of housing. Public health can work with the planning, energy, and building sectors to develop systems that protect people without destabilizing the electricity grid or fuelling climate change. Strategies may include localized cooling with heat pumps, as well as non-mechanical options, such as different roofing materials and exterior window shadings, both of which help to reduce the building heat.Footnote 118
New buildings: Indoor temperatures must be specified in building codes
The development of a new climate-resilient national building code is underway and should include a maximum indoor temperature standard.Footnote 120 Changes to the code must ensure that building performance considers human health in the context of other objectives, such as energy efficiency and carbon emissions. Doing otherwise can lead to climate maladaptation, such as airtight buildings that become dangerously overheated during hot weather.Footnote 121
Although changes to the building code are a promising adaptation tool, national and provincial amendments will take time. Municipalities and local governments can act faster through the creation of new standards and building by-laws. Metro Vancouver has already changed its Building By-law to require that all new multi-unit residential buildings have mechanical cooling capable of maintaining an indoor temperature of less than 26°C by 2025.Footnote 114
Existing buildings: Evaluation and retrofitting encouraged through voluntary and regulatory means
The average lifespan of publicly-owned residential buildings in Canada ranges from 40-80 years.Footnote 122 Most of the country's 14 million homes were built for past climatic conditions.Footnote 123 Efforts are needed to evaluate and retrofit existing housing to ensure safe indoor temperatures can be maintained in hot weather. In areas where the baseline climate will remain temperate, it may not be necessary to cool the entire home. One or 2 cool rooms can be adequate to keep occupants safe during heat events and is more feasible.
Assessing individual homes at risk of overheating can be accomplished through low-cost technologies, such as internet-connected thermostats. Programs to incentivize these technologies, combined with public health guidance for extreme heat emergency preparedness, could be used by homeowners, tenants, and landlords to identify environments at risk.Footnote 124
Some voluntary action to reduce heat risk in existing buildings can be incentivized through grants and rebate programs, but these may not benefit the populations most at risk. Regulatory action is likely necessary to address residential overheating equitably. Mandating a maximum indoor temperature in residential tenancy by-laws, as is done for minimum acceptable temperatures, and addressing outdated by-laws and regulations that limit installation of cooling devices in multi-unit residential buildings are two such options.Footnote 125
Thank you to contributing authors:
Dr. Angela Eykelbosh, Environmental Health and Knowledge Translation Scientist and Dr. Leah Rosankrantz, Environmental Health and Knowledge Translation Scientist
National Collaborating Centre for Environmental Health
Climate change will increase the level of pollutants and the quantity of pollen in the air. This is expected to exacerbate respiratory diseases, asthma, allergies, and increase the risk of cardiovascular disease and death.Footnote 5 Each year in Canada, 15,300 premature deaths and health impacts valued at $114 billion are linked to current levels of air pollution.Footnote 126 The concentration of air pollutants, such as ground-level ozone and fine particulate matter, is expected to increase as climate change increases temperatures and humidity in many parts of the country.Footnote 127Footnote 128 Ground-level ozone, the air pollutant most commonly linked to smog, aggravates the lungs, exacerbates asthma, and increases hospital admissions and premature deaths.Footnote 126
It is estimated that a third of people in Canada have at least one risk factor which increases their susceptibility to the adverse effects of air pollution exposure.Footnote 129 Yet, some face disproportionate health risks related to air pollution and allergens, including older adults, children, pregnant people, Indigenous Peoples, people with pre-existing respiratory and cardiac conditions, people living in households with low income, people living in high air pollution areas, and people who live, work, or are active outdoors.Footnote 130
As a result of climate-driven increases in the frequency and intensity of wildfires, smoke emissions are exposing millions of people to high levels of toxic air pollutants for days and weeks at a time. It is estimated that between 570 and 2,700 premature deaths occur every year in Canada due to long-term exposure to fine particulate matter from wildfire smoke.Footnote 5 In general, the exposure can cause a range of health complications from eye, nose, and throat irritation, to aggravating cardiovascular and lung disease.Footnote 131 People living in areas prone to wildfires may also face an increased risk of developing lung cancer and brain tumours.Footnote 132 However, wildfire smoke can impact air quality over vast distances, possibly affecting the respiratory health of people who live hundreds or even thousands of kilometres away.Footnote 133 In 2018, wildfire smoke originating in British Columbia and Alberta travelled across Canada to affect air quality in Ontario, Quebec, and the Atlantic provinces, and ultimately reached as far as Ireland.Footnote 134
Increases in temperatures and carbon dioxide concentrations in the atmosphere have shifted the geographic distribution of plants, extending the aeroallergen season in Canada and increasing pollen counts.Footnote 72Footnote 102 Pollens are a major source of allergies, or allergic rhinitis, in North America.Footnote 135
Food quality, safety, and security are essential to health, but are threatened by climate change given the challenges it poses to global and domestic pillars of food systems. Warming temperatures and more frequent high precipitation events can increase occurrences of food-borne pathogens and illness. Droughts and floods can disrupt food supply chains by damaging or diminishing crop yields, reducing the nutritional quality of food, and halting food production processes through associated productivity loss. This can impact food availability, quality, and costs, leading to dietary changes, undernutrition, and food insecurity.Footnote 5Footnote 17Footnote 72Footnote 99Footnote 102Footnote 136
The Prairie provinces are particularly susceptible to these climate change impacts. Alberta, Saskatchewan, and Manitoba account for more than 80% of Canada's agricultural land and the majority of the nation's irrigated agriculture.Footnote 137 High temperatures, combined with droughts, floods, and more variable precipitation can negatively affect crop yields across these regions, impacting domestic food supplies. For example, extreme heat can reduce yields of corn, soybean, canola, and wheat.Footnote 137 As the fifth largest exported of agri-food and other seafood in the world, disruptions in Canada's food productions systems could have global consequences.Footnote 138
Climate change may also increase the frequency of chemical contamination of food sources. Flooding and wildfire smoke can carry pollutants onto agricultural land, spoiling or contaminating crops and livestock. Northern communities are particularly at risk, as glacier and sea ice melt can release contaminants that accumulate in food sources, such as fish and mammals.Footnote 5Footnote 36
Indigenous communities that rely on traditional foods are at increased risk of food insecurity, due to significant impacts on food sources as a result of declines in biodiversity and shifting animal migration and population stability.Footnote 139Footnote 140 In northern regions, the rapidly changing environment is altering key species habitat, while melting sea ice is impeding the safe passage of hunters, reducing food accessibility and availability.Footnote 5Footnote 76Footnote 139 Additionally, climate-related declines in marine fisheries are already impacting coastal Indigenous communities that rely on traditionally harvested seafood as an important source of nutrients that are difficult to replace.Footnote 141 This exacerbates the challenges already posed by colonial disruption of Indigenous food systems and loss of access to traditional lands.
Water quality, safety, and security can also be impacted by climate change, as it increases the risk of microorganisms and toxins, which can lead to water-borne diseases.Footnote 17 Heavy precipitation, rapid snowmelts, or sea level rise can reduce the availability of freshwater and damage supply systems, increasing the risk of contaminants in water used for drinking, cooking, bathing, cleaning, and recreational and ceremonial activities.
Communities that already lack access to safe water may feel the effects of climate change more acutely. About 14% of Canada's population, mostly in rural and remote communities, rely on small drinking water systems that serve less than 300 people.Footnote 142 These systems, particularly those in Indigenous communities, are disproportionately affected by water quality and supply challenges. For example, in 2021, 89% of boil water advisories in Canada were for small drinking water systems serving 500 people or less, and as of May 2022, 29 First Nations communities living on reserves were still affected by long-term drinking water advisories.Footnote 143Footnote 144 To mitigate these threats, public health systems can support water system resilience (see text box "Health protection, climate, and small drinking water systems in Canada").
Health protection, climate, and small drinking water systems in Canada
Climate change could exacerbate the inherent challenges associated with small drinking water systems by affecting source water quality, quantity, and water infrastructure.
Source water will become more variable and difficult to treat consistently to an acceptable standard
Changes to precipitation and flooding patterns will cause periodic increases in bacterial and chemical contamination of source water, as well as increased organic matter, which can negatively affect the treatment process.Footnote 145Footnote 146Footnote 147Footnote 148 Increased occurrence of cyanobacterial blooms will increase potential for cyanotoxins in drinking water.Footnote 149 Wildfires will alter watershed hydrology, changing infiltration and runoff. This will affect surface water quality and groundwater recharge.Footnote 150Footnote 151 Sea level rise will worsen saltwater intrusion in island or coastal groundwater.Footnote 148 Drought will reduce groundwater recharge, increase water demand, and cause pollutants to be more concentrated in surface waters.
Water systems infrastructure will be more at risk of contamination and damage
Changing temperature and baseline water quality will affect microbial growth in pipes and storage tanks. Extreme weather events will cause power outages to pumping stations and treatment plants, knocking out supply and treatment capacity. Damage to distribution pipes and storage systems, such as leaks and line breaks from floods or wildfires could cause pressure loss, impairing water delivery and allowing pollutants to enter systems. Wildfires will cause infrastructure damage, destruction, and melting of plastic pipes in distribution systems, causing chemical contamination.Footnote 152Footnote 153 Thawing permafrost will destabilize ground and damage underground pipes and storage tanks, causing contamination of water or infrastructure.Footnote 154
Addressing climate change impacts on small drinking water systems in Canada
Regional, provincial, and federal agencies can help protect health and build water system resilience by encouraging water safety plans to include climate change associated risks to source water and infrastructure.Footnote 155 Agencies can enable better access to water quality data through increased monitoring, surveillance, and tools for sharing data, alongside trend analysis, modelling, and development of water quality forecasting tools and alert systems.Footnote 156
At the community level, strong intersectoral action and training is needed to ensure sufficient emergency prediction, preparedness, and response, including skills in building operations and maintenance.Footnote 157 Support and resources for water quality testing are also needed to assist response to and recovery from extreme events.
Thank you to contributing authors:
Dr. Juliette O'Keeffe, Environmental Health and Knowledge Translation Scientist
National Collaborating Centre for Environmental Health
Thawing permafrost, droughts, and flooding caused by climate change will exacerbate and compound the existing health challenges stemming from a lack of access to clean fresh water.Footnote 5 Atlantic Canada is expected to experience the largest local sea level rise, which will lead to increased flooding of homes, businesses, community and marine infrastructure, and pose substantial problems for forestry, fisheries, agriculture, and transportation.Footnote 158 The loss of or damage to homes and belongings means a higher risk of physical exposure to the elements, pathogens, and mold growth, as well as reduced indoor air quality, displacement, and mental health issues.Footnote 158
Climate-related health risks amplify the need to respect water rights, which are essential to health equity and justice. Water rights refer to the inherent right to safe drinking water without discrimination for personal and domestic use, as well as social, economic, and cultural purposes.Footnote 159Footnote 160 The United Nations recognize access to safe water and sanitation as a human right, as the lack of access to it has devastating health effects and impedes the realization of other human rights.Footnote 161
Water rights go beyond safe drinking water and include water sources where people fish for food. Prior to colonization, Indigenous practices guided the use of water. Now, inadequate access to safe and sustainable drinking water increases vulnerability to water-borne disease and exposure to chemical contaminants for some First Nations, Inuit, and Métis communities.Footnote 162Footnote 163
Governance gaps make it challenging for Indigenous Peoples to exercise inherent and treaty rights related to water.Footnote 159 Canada's constitutional division of authority over water across different jurisdictions contributes to inconsistent standards for protecting it. Indigenous communities find themselves in a fragmented regulatory system, which increases the challenges related to access to safe drinking water.Footnote 164
The risk of infectious diseases is increasing with a rapidly changing climate. Temperature fluctuations and precipitation changes create expansions and shifts in the geographic range and abundance of climate-sensitive infectious diseases. Moreover, the threat of re-emergence or introduction of zoonotic diseases transmitted between people and animals is exacerbated by climate change, biodiversity and habitat loss, trade, and travel. This elevates the risk of future emerging diseases (see text box "Climate change and the risk for emerging diseases").
Climate change and the risk for emerging diseases
Climate change is affecting life cycles and transmission of viruses and other pathogens because of dramatic changes in weather patterns, water quality, vegetation, population movements, and other environmental factors. Expanded ranges for vectors have contributed to wider dissemination of diseases, such as Lyme disease, and a myriad of mosquito and tick-borne viral pathogens. For example, a 2013 review found a 10 to 50% increase in vector-borne diseases in the northern USA over the median of the preceding 10 years.Footnote 165 The ticks, mice, and mosquitoes that carry pathogens continue to spread into southern Canada.
Climate change's influence on the spread of infectious diseases depends on complex interactions between human behaviour, land utilization, urban planning, vector biology, mitigation strategies, and socioeconomic factors. For example, climate change is leading to certain groups of people, such as displaced or underhoused populations, living in more concentrated situations, such as shelters or community centres, which can facilitate the spread of infectious disease.Footnote 166 Temperature and humidity changes favour viral survival and spread, while shifts in diet may lead to gut microbiome changes that benefit pathogens.Footnote 166 Further, trade and travel can import diseases endemic to other parts of the world.
Climate hazards can also create prime conditions for infectious diseases to spread. For instance, interrupted access to clean water sources and sewage systems damaged by extreme weather events, increase the risk of diarrhoeal and water-borne illnesses.Footnote 167
Thank you to contributing authors:
Dr. Yoav Keynan, Scientific Lead and Margaret Haworth-Brockman, Senior Program Manager
National Collaborating Centre for Infectious Diseases
A changing climate also brings risks of new vector-borne diseases as the potential for vectors to establish themselves in new places in Canada grows.Footnote 168 Climate change has already led to greater ranges for ticks and mosquitos, increasing the risk of human exposure to vectors that can transmit diseases, such as Lyme disease and West Nile virus (see text box "Lyme disease and climate change").Footnote 91
Lyme disease and climate change
Tick-borne diseases are increasingly common in parts of Canada due in part to climate and land use change. Since the 1990s, when ticks first arrived in southern Ontario, the Public Health Agency of Canada has been monitoring the movement of tick populations and exposure patterns in people.Footnote 169 Lyme disease is caused bacteria and spread through the bite of infected blacklegged ticks. It is one of the most rapidly emerging infectious diseases in Canada, the most commonly-reported vector-borne disease in North America, and incidence has increased more than 17-fold between 2009 and 2019.Footnote 170 In addition to Lyme disease, other tick-borne diseases, such as Anaplasmosis, Babesiosis, and Powassan virus, are starting to emerge in Canada and are likely to increase in frequency.
Climate change impacts tick populations through longer, hotter summers and milder winters that promote the ticks' rates of survival, growth, and reproduction.Footnote 171 This means that they can survive and establish populations in areas where they previously could not and increase their numbers where they were already established. Longer summers also mean a prolonged season when ticks are active and people are outdoors, increasing the window of opportunity for the two to physically interact.
Additionally, climate change is expected to expand the range, abundance, and activity of rodent, bird, and deer hosts that carry the disease. These hosts allow the ticks to move through their life cycle and can facilitate tick travel over long distances.Footnote 171
Text partially adapted from the Climate Atlas of Canada.Footnote 169 Learn more about Lyme disease in Canada including prevention measures, symptoms, and risks.
Non-communicable diseases and disability, as well as pre-existing chronic conditions, will also be affected by the changing climate.Footnote 172Footnote 173 Exposure to impacts such as extreme heat, extreme weather events, water-related illnesses, and poor air quality, chronic diseases and disabilities can increase an individual's risk of illness and death.Footnote 5Footnote 174 For instance, older adults with cardiovascular disease, high blood pressure, or diabetes are particularly vulnerable to extreme heat. The risk factors associated with non-communicable diseases and disability are also affected by climate change. Increasingly, there is recognition that infectious diseases can cause chronic illnesses and that infectious diseases are more severe in those affected by chronic illnesses.Footnote 5 To understand and respond to these health concerns in a time of change we need to strengthen the links between public health efforts.
The relationship between mental well-being and climate change is also complex, as it involves compounding and cascading risks. These can include adverse mental, spiritual, and emotional health impacts from exposure to extreme weather events, emergency evacuations, forced displacement, food and water insecurity, and social and economic disruptions.Footnote 175 Slow-onset climate changes such as increasing temperatures, sea level rise, permafrost thaw, and coastal erosion can impact vital landscapes, cultural practices, and heritage sites, leading to increased mental health challenges, particularly for those deeply connected to the land.Footnote 175 The trauma associated with these events, their impacts, and aftermath can exacerbate existing mental health conditions or bring about new ones. This affects individual mental well-being as well as community social well-being, which is considered an aspect of positive mental health.Footnote 17Footnote 99
"We have, I think, really underestimated the mental health impact of the [climate change] information itself because what we're in essence talking about is a distressing diagnosis that impacts all of us, all of the patients we will ever treat, our family and our friends."
Many people in Canada are already experiencing negative mental health impacts due to current and future impacts of climate change. A survey of 2,000 Canadian adults reported that 49% of respondents were increasingly worried about the effects of climate change, while 25% stated that they often think about climate change and feel "really anxious" about it.Footnote 5 Adverse emotional and behavioural responses, such as worry, grief, anxiety, anger, hopelessness, and fear have been linked to anticipated climate change threats.Footnote 5
Children and youth are particularly vulnerable to climate anxiety, as they will bear the heaviest burden in light of escalating climate threats.Footnote 176 Globally, youth have reported significant distress about the impacts on their daily life, including fear about their future and the future of humanity, lack of government response or urgency, and feelings of betrayal and abandonment by adults.Footnote 176 These feelings can be chronic, long-term, and inescapable, increasing the risk of future mental health conditions in the absence of successful mitigation and adaptation efforts.Footnote 176
At the community level, climate change can disrupt social cohesion and community well-being through deterioration of cultural practices, sense of identity, place attachment, sense of belonging, and intergenerational knowledge sharing and transmission.Footnote 21 These outcomes may be immediate or progressive, burdening future generations and emphasizing the structural and systemic nature of vulnerability.Footnote 177 Climate change is becoming an additional mental health stressor for resource-dependent communities, and in northern regions, such as Nunavut, the disruption of land-based activities, loss of comfort, and cultural identity are negatively impacting mental health and well-being.Footnote 178
Those who have a disproportionate risk of adverse mental well-being impacts from the climate crisis include children, youth, and older adults; Indigenous Peoples; those who have certain pre-existing physical and mental health conditions; as well as low socioeconomic groups and populations facing homelessness.Footnote 179 Additionally, certain occupational groups may also experience disproportionate mental health impacts due to climate change, such as those that rely on weather for livelihoods (e.g., farmers), and work in occupations that respond directly to climate-related emergencies (e.g., firefighters, first responders).Footnote 175
The health risks posed by a changing climate are shaped by a combination of climate hazards, exposure, and adaptive capacity. These hazards and health risks are experienced in different ways, in different places, and by different groups of people. Exposure, vulnerability, and adaptive capacity are influenced by the social, economic, and ecological conditions that determine health at the individual, community, and population levels.Footnote 5Footnote 180Footnote 181 These risks change across the life course (Figure 4).Footnote 5Footnote 17Footnote 176Footnote 182
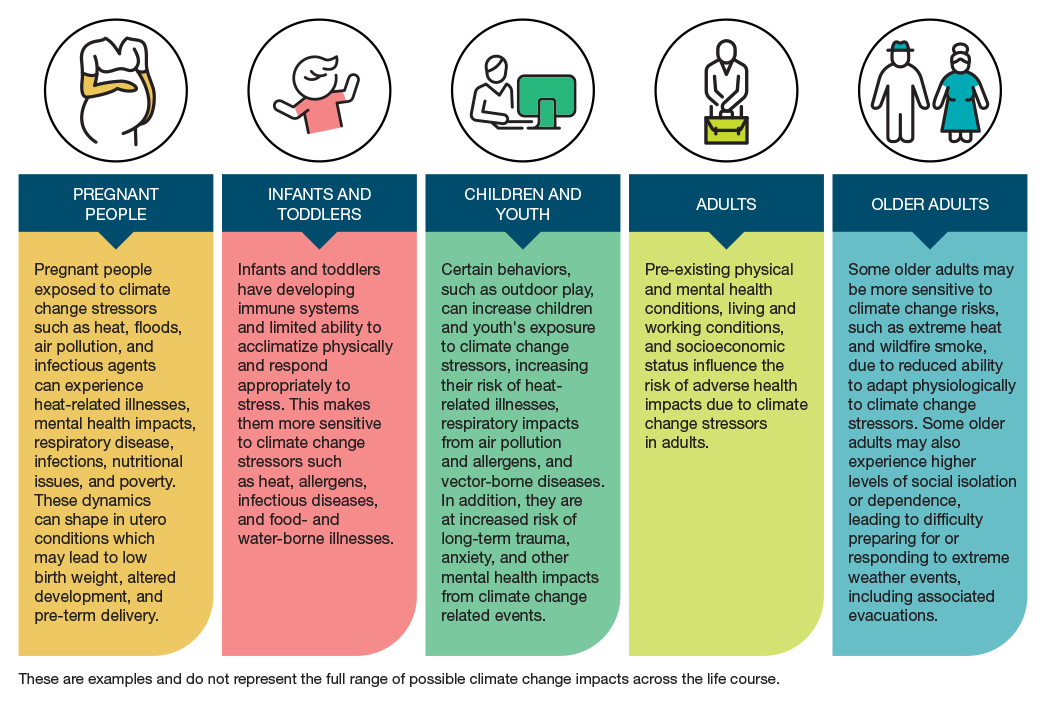
Figure 4: Text description
The figure describes the health impacts of climate change across the life course.
Pregnant people: pregnant people exposed to climate change stressors such as heat, floods, air pollution and infectious agents can experience heat-related illnesses, mental health impacts, respiratory disease, infections, nutritional issues, and poverty. These dynamics can shape in utero conditions, which may lead to low birth weight, altered development, and pre-term delivery.
Infants and toddlers: infants and toddlers have developing immune systems and limited ability to acclimatize physically and respond appropriately to stress. This makes them more sensitive to climate change stressors such as heat, allergens, infectious diseases, and food- and water-borne illnesses.
Children and youth: certain behaviors, such as outdoor play, can increase children and youth's exposure to climate change stressors, increasing their risk of heat-related illnesses, respiratory impacts from air pollution and allergens, and vector-borne diseases. In addition, they are at increased risk of long-term trauma, anxiety, and mental health impacts from climate change related events.
Adults: pre-existing physical and mental health conditions, living and working conditions, and socioeconomic status influence the risk of adverse health impacts due to climate change stressors in adults.
Older adults: some older adults may be more sensitive to climate change risks, such as extreme heat and wildfire smoke, due to reduced ability to adapt physiologically to climate change stressors. Some older adults may also experience higher levels of social isolation or dependence, leading to difficulty preparing for and responding to extreme weather events, including associated evacuations.
These are examples and do not represent the full range of possible climate change impacts across the life course.
Vulnerability and inequitable health risk
"The poorest, the most vulnerable will be hit harder. So, we have a duty to protect the population, and this is through working on inequities. There are many studies that have shown that the less inequities in societies, the more resilient the population is and less hard it will be hit when a crisis comes."
Understanding the concept of climate change vulnerability is important and requires careful consideration and application in the context of public health. In addition to offering information on increased risks to health outcomes, knowledge about climate change vulnerability can help prioritize where resources and adaptation measures are most needed.Footnote 5
In public health, the concept of vulnerability can be highly stigmatizing.Footnote 5 It is important to recognize that climate vulnerability is not a label for communities or populations. Rather, it occurs when long-standing and systemic patterns of inequity drive differential exposure, sensitivity, and adaptive capacity to climate hazards.Footnote 5 Vulnerability is influenced by factors, such as geography, age, sex, sexual orientation, gender identity and expression, experience of colonization, education, ethnicity, race, disability, income, built environments, as well as living and working conditions.Footnote 183 Collectively, these factors are known as the social determinants of health.Footnote 184Footnote 185Footnote 186Footnote 187 An understanding of these must include structural determinants of health, such as colonization and assimilative policies.Footnote 188 These upstream forces influence policies, programs, and systems that benefit some groups of people over others.Footnote 189
For people who experience gender-based marginalization, there is a higher risk of exposure and sensitivity to climate hazards.Footnote 5 Women may experience increased climate-related anxiety and post-traumatic stress disorder, while also taking on disproportionate caregiving roles.Footnote 190 Climate change can exacerbate gender-based violence, with increased risk during or after extreme events. In the wake of the 2013 floods in southern Alberta, gendered mental health impacts were observed, including increased anti-anxiety and sleep-aid prescriptions among women, and an increase in sexual assaults.Footnote 191Footnote 192
Climate vulnerability is dependent on the degree of exposure to climate hazards, sensitivity to possible impacts, and capacity to adapt. These can be strongly influenced by social and structural conditions (Figure 5).Footnote 5 In the case of coastal flooding, not everyone will experience the same risks and impacts. Housing type and location, access to financial resources to repair damage and pay for expenses associated with temporary or permanent displacement, and the stability of one's livelihood are some of the factors that can influence individual physical and mental health impacts of flooding in a community.
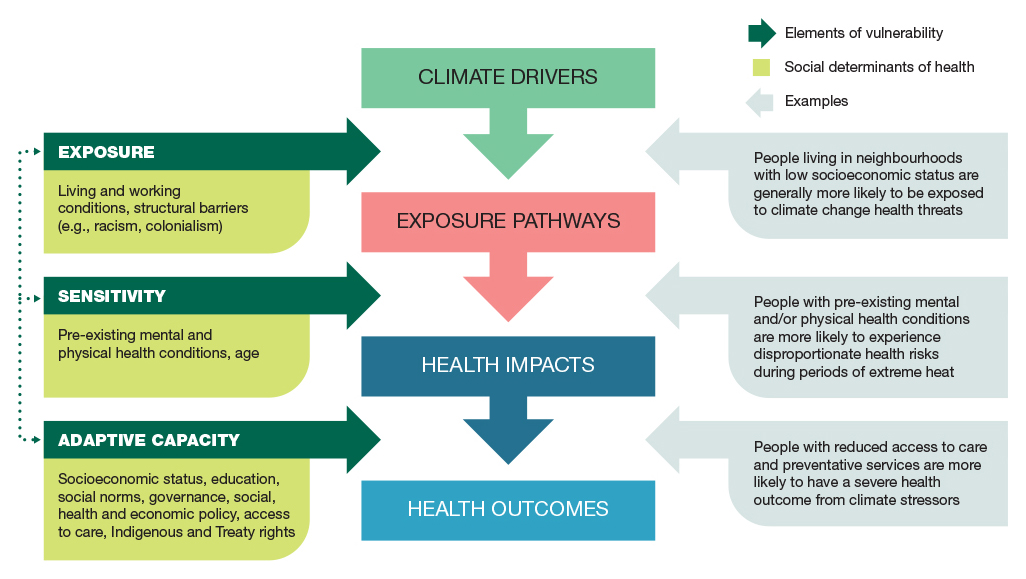
Source: Figure adapted from U.S. Global Change Research Program. The Impacts of Climate Change on Human Health in the United States: A Scientific Assessment (2016).
Figure 5: Text description
The figure depicts a causal chain starting with climate drivers, which influence exposure pathways, which lead to health impacts, and ultimately, health outcomes.
Boxes on the left side provide interconnected examples of social determinants of health associated with each of the elements of vulnerability. These are:
- Exposure (e.g., living and working conditions, structural barriers [e.g., racism, colonialism]);
- Sensitivity (e.g., pre-existing mental and physical health conditions, age); and,
- Adaptive capacity (e.g., socioeconomic status, education, social norms, governance, social, health and economic policy, access to care, Indigenous and Treaty rights).
These elements affect vulnerability at different points in the causal chain from climate drivers to health outcomes (middle boxes). Exposure can influence exposure pathways, sensitivity can influence health impacts, and adaptive capacity can influence health outcomes.
Boxes on the right side provide examples of the implications of the social determinants of health on exposure, sensitivity, and adaptive capacity. The examples are as follows:
- Exposure pathways (exposure): people living in neighborhoods with low socioeconomic status are generally more likely to be exposed to climate change health threats.
- Health impacts (sensitivity): people with pre-existing mental and/or physical health conditions are more likely to experience disproportionate health risks during periods of extreme heat.
- Health outcomes (adaptive capacity): people with reduced access to care and preventative services are more likely to have a severe health outcome from climate stressors.
Social and economic factors also drive differential access to the material and social resources needed to ease and adapt to the impacts to climate change.Footnote 5Footnote 193 For example, the historic and enduring legacy of colonialism underlies and perpetuates the structural disempowerment of Indigenous Peoples and their health, social, and economic inequity.Footnote 194 Generations of First Nations, Inuit, and Métis Peoples have seen land and wildlife destroyed and traditional ways of living degraded by climate change, which has further exacerbated pre-existing health, social, and economic inequities.Footnote 20Footnote 188 This influences the resources available to Indigenous Peoples to respond and adapt to climate risks, such as inadequate community infrastructure, particularly in northern and remote communities.Footnote 20Footnote 91 As noted earlier, climate change disrupts the unique relationship that First Nations, Inuit, and Métis Peoples have to the land, which impacts their physical, emotional, spiritual, psychological, and cultural well-being (see text box "Environment: The ecosystem is our health").Footnote 5Footnote 195
Environment: The ecosystem is our health
Abridged excerpt from Visioning the Future: First Nations, Inuit, and Métis Population and Public Health.Footnote 196
In what became Canada, Indigenous knowledge about relationship, responsibility, and reciprocity is confronted by a differing worldview, starting in the late-15th century. Settlers view environments, inclusive of Indigenous Peoples living within them, as commodities that can be claimed, controlled, and colonized. Colonizers' anthropocentric view of the world drives policies and actions, harming the health of the environment and all beings connected with it. As the 21st century unfolds, the effects of this worldview are becoming increasingly blatant. Humans have exploited the natural infrastructure of Mother Earth, leaving one million species threatened with extinction. This biodiversity loss damages relationships between all beings. What is more, people who depend on these relationships find their livelihoods, food security, health, and quality of life endangered.
Biodiversity loss and climate change are intricately linked, and their common basis must be addressed.Footnote 197 To achieve this, Mother Earth needs to be recognized as foundational to the health of all beings because the ecosystem is our health system. We must shift from anthropocentric worldviews and re-learn that we, as humans, are part of a complex and interdependent web.
As a Hul'qumi'num woman who works as a medical health officer in my home territory, I go to the rivers to bath as Elders have taught me. I ask the water to carry my heaviness away. The land and waters are healers, as recent research has shown.
The urgent need to address our relationship with the environment is exemplified in many ways, including the western North American heatwave that occurred just days into the summer of 2021. Unprecedented high temperatures resulted in increased human deaths, deaths of other species (an estimated one billion deaths for seashore animals on the Salish Sea coastline alone), rapid snowmelts, flooding, exacerbations of drought, and wildfires.Footnote 198Footnote 199 The gravity of this situation necessitates a fundamental shift: we must place the well-being of our environment at the centre of all our decision-making. We need to rapidly re-envision the prevailing anthropocentric worldview of the planet to one where we honour our relationships with all beings in our shared environment.
The recognition, support, and advancement of Indigenous sovereignty is needed to protect the environment. After all, Indigenous sovereignty is sustainability.
Thank you to contributing author:
Dr. Shannon Waters, Medical Health Officer for the Cowichan Valley Region at Island Health – Vancouver Island Health Authority
Inequitable access to resources influences how a community can prepare, react, and adapt to a changing climate. Inequities prevent some communities and populations from proactively implementing climate adaptations.Footnote 200 Even though rural and remote communities generally rely on natural resources and ecosystems, and face greater impacts of climate change, they tend to have fewer resources, systems, and services to respond to its disruptions. Despite this, these communities promote asset-based approaches that support climate resilience and adaptation.Footnote 5Footnote 201
Ecological and social conditions that shape health in a changing climate
Social determinants of health influence the ecological determinants of health.Footnote 8 These are the necessities of life - food sources, fresh water, oxygen, and other natural resources. Canadian communities do not have equal access to these, which is particularly consequential in the context of a changing climate that further threatens their quality, quantity, and availability.
The built environment demonstrates the complex interconnections between the ecological and social determinants of health. The way cities and communities are built can influence conditions for healthy living, greenhouse gas emissions, and the extent to which climate hazards impact health.Footnote 202 Our buildings and homes can affect our vulnerability to climate-related risks (e.g., heating and cooling, ventilation, resistance to extreme weather).Footnote 5 Substandard housing leads to heightened health risks that can be further compounded by extreme weather events, heatwaves, permafrost thaw, storm surges, and severe coastal erosion.Footnote 5Footnote 202Footnote 203Footnote 204 Broader community design features are also important, since walkability, bike paths and lanes, good public transit, and green space can encourage active modes of transportation, and subsequently reduce greenhouse gas emissions.Footnote 202
Social determinants influence the type of built environments we live in. Access to green space has been linked to a variety of health benefits, including improved air quality, fewer urban heat islands, flood mitigation, reduced stress, increased physical activity, greater social connections, and lower risk for premature death.Footnote 206Footnote 207Footnote 208Footnote 209Footnote 210 However, in Canadian urban areas green space is not equally distributed. Less residential 'greenness' was observed for people living with lower income, immigrants (especially recent immigrants), young adults, visible minorities, and tenants.Footnote 211 This means the benefits of green space are unfairly distributed. Without changes to the way natural resources and the environment are valued and governed, these inequalities will grow.Footnote 212
Health and well-being are dependent on and intimately connected to the ecological conditions and the ecosystems in which we exist.Footnote 8Footnote 213 An unsustainable demand for natural resources, land use change (e.g., desertification, deforestation), and increased pollution have fundamentally altered our ecosystems.Footnote 212 The way things are currently managed can lead to multiple deprivations, marginalization, and structural inequalities.Footnote 212 Climate change has altered territories, seasonal practices, and the ability of communities to access land resources, which undermines many articles of UNDRIP, as well as the human rights of Indigenous Peoples by way of climate-driven challenges like food insecurity.Footnote 214Footnote 215
This is evident in the stark reality that despite having the lowest household greenhouse gas emissions per capita, communities in Nunavut are experiencing warming at 3 to 4 times the rate of communities in the rest of Canada, which is causing severe local impacts.Footnote 5Footnote 23Footnote 74Footnote 216 This inequity also holds true in the international context, as most high emitting countries are among the least vulnerable to negative climate change impacts, while those with the lowest emissions are often acutely vulnerable.Footnote 217
Bringing public health and climate action together to address the threat
There are many competing public health challenges but given that climate change threatens the livability of the planet, compounds existing health issues, and widens health inequities, it must be a public health priority. This requires public health action in climate mitigation, adaptation, advancing co-benefits, and preventing maladaptation.
Just as there are limits to what can be done to treat injury or disease once it occurs, there are also limits to how adaptation can reduce the health impacts of climate change. If the annual average global temperature rises even 1.5°C, there will be situations where it will be extremely challenging to protect health.Footnote 19 During heatwaves, some places will be too hot for survival. Though adaptation is important and the focus of many current public health initiatives, the severe and growing climate threat requires a concurrent focus on mitigation. This means addressing pressing threats to health already arising from climate change while working to reduce heat-trapping gas emissions and their effects.Footnote 5Footnote 25Footnote 43Footnote 218Footnote 219Footnote 220Footnote 221
A strong public health response will require a multi-pronged approach that starts with developing dedicated climate-health action, as well as finding entry points for public health in climate efforts across jurisdictions and levels of government.Footnote 43Footnote 222 Health co-benefits offer a way into discussions about the role of public health. For example, modelling in Toronto and Hamilton suggested that in addition to reducing greenhouse gas emissions, shifting to electric cars, electric public transit buses, and more efficient trucks would result in cleaner air, lives saved through improvements to respiratory and cardiovascular health, and billions of dollars in annual social benefits.Footnote 223 Demonstrating and emphasizing the health co-benefits can help individuals, communities, and decision-makers see the direct and tangible advantages of climate action, including immediate results in some cases.Footnote 5Footnote 224Footnote 225 This helps counter the perception that climate efforts require giving up comforts and choices for an abstract long-term environmental benefit.Footnote 224Footnote 225
Public health also has a key role to play in preventing maladaptation. Maladaptation is any deliberate adjustment in natural or human systems that unintentionally increases vulnerability to climatic impacts instead of reducing it.Footnote 13 This occurs when actions increase exposure and risk in ways that are difficult to change and exacerbate existing inequalities.Footnote 19 The intersectoral and equity-oriented nature of public health has relevance to preventing maladaptation by ensuring inclusive decision-making processes that include the perspectives of diverse groups and account for the differential risks they face.Footnote 3Footnote 19 It also has a critical role in preventing health risks or widening health inequities gaps from poorly planned greenhouse gas mitigation measures.Footnote 3
Opportunities for public health systems to contribute to climate action are detailed in Section 2. This includes building on existing strengths in our approaches and systems, and exploring opportunities to support mitigation, adaptation, and co-benefits.
Current public health action in a changing climate
There has been growing international attention to climate change and health. In addition to the WHO's emphasis on health, equity, and climate change at COP26, the Lancet Countdown Report on Health and Climate Change publishes annual international progress on 41 indicators related to climate change and health.Footnote 226 Health impacts are also documented by the IPCC, which informs international discussions and national policies on climate change.Footnote 42 The international health community is also engaged in assessing their countries' commitments to the Paris Agreement (known as Nationally Determined Contributions) to track how health is integrated into climate policy, if at all.Footnote 227
In Canada there is ongoing work to develop and implement a National Adaptation Strategy (NAS).Footnote 228 It sets out a shared vision that includes transformational goals and tangible objectives to drive cohesive and collaborative action to help prepare Canada to adapt to climate change. It outlines a whole-of-society approach that includes roles for federal, provincial, territorial, Indigenous, and local governments, as well as the private sector, communities, and individuals. Health and well-being are prioritized as one of 5 thematic areas, and public health partners have been active in supporting these pillars as part of policy work. Additionally, Health Canada provided multi-year funding for health sector capacity building through HealthADAPT to support the human health and well-being objectives of the Pan-Canadian Framework on Clean Growth and Climate Change.Footnote 229
A knowledge and evidence base on climate and health is also advancing across Canada. The recently released report, Health of Canadians in a Changing Climate: Advancing our Knowledge for Action, provides the latest evidence on health impacts on individuals and health systems, as well as information on effective adaptation measures.Footnote 5 Canadian medical and public health organizations develop an annual Canadian policy submission for the Lancet Countdown on key issues across the country.Footnote 226 Looking ahead, Climate Science 2050: Advancing Science and Knowledge on Climate Change (CS2050), is a national evidence synthesis effort that is underway to better understand the climate change science and knowledge needs that exist in Canada. This will guide and prioritize science investment and research planning for a climate-resilient Canada.Footnote 230 This includes supporting efforts to reduce of emissions to 40 to 45% below 2005 levels by 2030, as well as the ambitious goal of a net-zero Canada by 2050, which is either emitting no greenhouse gases or offsetting the emissions through carbon capture actions.Footnote 230Footnote 231 The plan also puts forward 5 thematic pillars, including one on 'Resilient and Healthy Canadians'.
Strong climate leadership and action among national Indigenous organizations is both long-standing and ongoing. First Nations, Inuit, and Métis Peoples have been at the frontline of climate action to protect their communities and the broader environment. Many Indigenous leaders have called for action to reduce emissions, address the impacts of climate change, and improve the ways in which the natural environment is protected and respected.Footnote 232 All climate action should recognize the leadership and work of Indigenous Peoples, as well as their status as rights holders.
In 2020, the Assembly of First Nations hosted a National Climate Gathering to discuss the climate crisis and explore First Nations perspectives on its impacts, risks, and opportunities.Footnote 233 Their final report emphasized that a healthy environment is the foundation upon which all other aspects of life depend, including health and well-being, language and culture, water, and food security.Footnote 233 Inuit Tapiriit Kanatami's climate change strategy from 2019 recognizes Inuit health as one of the 5 priorities driving climate action for Inuit communities.Footnote 21 Additionally, in 2020, the Métis Nation identified the priorities to advance its climate leadership, such as capacity-building, traditional knowledge, research, and data collection to guide their climate change and health policy.Footnote 232
Federal partners also continue to support Indigenous climate leadership at the local levels. Crown Indigenous Relations and Northern Affairs Canada offers funding for adaptation projects in Yukon, Northwest Territories, Nunavut, Nunavik, Nunatsiavut, Eeyou Istchee Territory and NunatuKavut through Climate Change Preparedness in the North Program.Footnote 234 This program works with Indigenous and northern communities, territorial and regional governments, and others to identify priorities for climate adaptation and action, with projects centred on local knowledges and experiences. Indigenous Services Canada established The Climate Change and Health Adaptation Program (CCHAP) in 2008.Footnote 235 It was also developed in response to concerns from northern First Nation and Inuit communities that were directly impacted by climate change.Footnote 235Footnote 236Footnote 237 In 2016, CCHAP was expanded to include First Nations south of 60° N. It funds communities and organizations working on behalf of or in partnership with Indigenous communities to support efforts to identify, assess, and respond to climate health impacts while respecting Indigenous sovereignty.Footnote 235Footnote 238
Provincial and territorial efforts continue to advance climate action that prioritizes health. In northern Canada, food security has been emphasized in climate change initiatives as a determinant of health.Footnote 239 Climate change and health assessments have identified emergency evacuation plans for each major territorial health-related facility, while community clean air shelter assessments provide safe zones for extreme events, such as wildfires. There are also ongoing efforts across the territories to monitor and plan for the health impacts of extreme events.Footnote 239Footnote 240 In western Canada, an interactive air quality map has increased understanding of air pollution, including wildfire smoke, and provides advice for reducing risk.Footnote 241 Meanwhile in Atlantic Canada, a climate readiness scan has been developed for the continuing care sector, and public health and safety have been incorporated in climate change risk assessments.Footnote 242
Similarly, local public health efforts have galvanized place-based action. Just as the impacts of climate change vary across the country, the work of local public health systems is also not uniform, as it is rooted in local needs and priorities. This includes adapting existing public health initiatives to better focus on climate change.
Examples of provincial, territorial, and local climate-health action are highlighted throughout subsequent sections to illustrate the ongoing leadership of public health systems across jurisdictions in Canada.
Existing public health action, from local to international, offers important contributions to efforts addressing the health impacts of climate change. However, the severity and urgency of the climate crisis demands new and greater attention. Section 2 explores how a deeper range and depth of public health action on climate change can better promote and protect health. It also details how a strengthened public health system is central to addressing this complex public health crisis.
Section 2: Opportunities to advance climate action in public health
To effectively promote and protect health in a rapidly changing climate, public health systems in Canada must both broaden and fine-tune public health functions, tools, and activities. This report includes a roadmap to support ongoing discussions about the role of public health in climate action, as well as the broader conversations about public health system-level transformation sparked during the COVID-19 pandemic (Figure 6).
This roadmap was developed through a literature review and guidance from public health and climate change experts across Canada (see Appendix C: Methodology). It is intended to build on and complement existing guidance, such as the World Health Organization's (WHO) promotion of climate-resilient health systems and direction on climate-health vulnerability and adaptation assessments, as well as the Pan American Health Organization's (PAHO) work on new essential environmental public health functions.Footnote 94Footnote 243Footnote 244Footnote 245Footnote 246 This roadmap shares their focus on understanding and addressing climate-health risks and building resilience. It also offers a unique contribution by focusing on mobilizing public health systems for climate action in the Canadian context against the backdrop of broader public health system transformation (see the 2021 CPHO annual report: A Vision to Transform Canada's Public Health System).
Each of the roadmap's action areas has implications across essential public health functions and system-level building blocks and is illustrated by practice examples from across the country. Many areas have value beyond climate change and can support action to address other complex public health issues.

Figure 6: Text description
The figure provides a roadmap for climate change action across public health systems. The horizontal model flows from left to right, to describe the elements of public health systems in Canada and areas for climate change action.
The model begins by describing the current essential public health functions, which are: (1) health promotion, (2) health surveillance, (3) health protection, (4) population health assessment, (5) disease and injury prevention, and (6) emergency prediction, preparedness and response.
Next, the building blocks of the public health system are provided, which are divided into 2 categories. The first category provides the foundational building blocks: (1) governance, leadership, and engagement, (2) financing, and (3) workforce expertise and human resource capacity. The second category provides the process/tool building blocks: (1) evidence, knowledge, and information; (2) policy and program interventions; and (3) medical and digital health technology.
The essential public health functions and the building blocks of the public health system are needed for public health action in climate change. These action areas are: (1) implement a range of interventions to address immediate health challenges and prevent future health risks from a changing climate; (2) prioritize community expertise and engagement for equitable and effective climate action; (3) advance knowledge to understand, predict, and respond to the health impacts of climate change; (4) collaborate across sectors for transformative climate-health action and intersectoral co-benefits; and, (5) strengthen public health leadership for climate action and public health building blocks for climate resilience.
To address the health impacts of climate change, public health systems will have to work across all essential public health functions.Footnote 243Footnote 247Footnote 248Footnote 249Footnote 250 First developed for Canada in 2003 in the wake of SARS, these functions categorize the "what" of public health action.Footnote 251Footnote 252 They are a useful way to describe the breadth and depth of public health efforts and include health promotion, health surveillance, health protection, population health assessment, disease and injury prevention, and emergency prediction, preparedness, and response.
These functions are interconnected and used together to support a broad range of climate-health action. This work ranges from health promotion initiatives like greening parks and playgrounds, to vector surveillance and control to combat the spread of mosquitos and ticks enabled in part by climate change. The assessment function relating to climate change and health vulnerability and adaptation assessments is particularly important for identifying and preparing for future climate risks to health. Appendix A offers further examples of how public health functions can be applied in this context.
Implement a range of interventions to address immediate health challenges and prevent future health risks from a changing climate
"Public health is doing all this work that is totally related to climate change…the intersections are there. Some health units are doing really well, really engaging in land use planning and transportation planning, where we become a partner in co-developing policies and plans and strategies that fold all of the things that we need to create healthy, sustainable communities into our work."
Public health systems can best support climate action by advocating for interventions and implementing them across the upstream-downstream continuum (Figure 7). Working to simultaneously address immediate challenges and prevent future risks is a familiar model for public health (see 2021 CPHO report).Footnote 253 It also aligns with the dual focus on mitigation and adaptation that climate action requires. There will always be the need to find the right balance between adapting to the downstream impacts while also addressing the conditions that lead to individual and community vulnerabilities and the root causes of climate change. Without this balance -- and particularly in the absence of upstream action -- the downstream climate impacts on disease and injury will continue to grow and burden the health system and broader social-economic systems.
A key focus for upstream public health attention is climate change mitigation. The 2 biggest sources of greenhouse gases in Canada are the oil and gas sector and the transportation sector.Footnote 254 The Intergovernmental Panel on Climate Change (IPCC) has emphasized that cutting greenhouse gas emissions in the energy sector will require a substantial reduction in the use of fossil fuel, greater energy efficiency and conservation, and the use of low-emission energy sources and alternative energy carriers.Footnote 255 In addition to supporting public and active transit, such as walking and biking, mitigation strategies in the transportation sector include electric vehicles powered by low-emissions electricity.Footnote 255 These actions have many potential health co-benefits, and public health can play a role in advancing them through community and policy action, and behavioural science approaches to support people and communities in making climate friendly and healthy choices where they live.Footnote 256Footnote 257Footnote 258 In urban settings, greenhouse gas reduction can be achieved by prioritizing sustainable energy and materials, repurposing or retrofitting buildings, and prioritizing dense development linked by public transit and with local services and jobs. Further, increasing carbon uptake and storage is important, for example through urban forests, which can remove carbon dioxide from the atmosphere through photosynthesis and store carbon in vegetation.Footnote 255
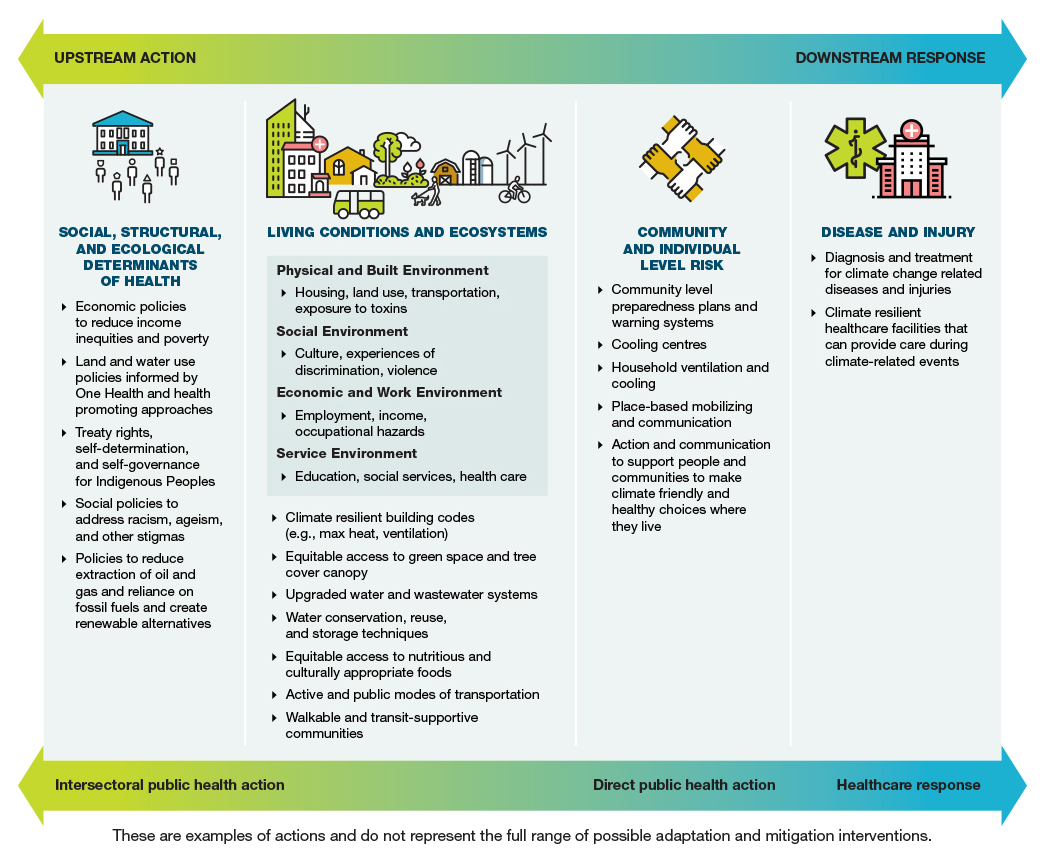
Figure 7: Text description
This figure depicts a continuum of opportunities for climate action across public health systems.
The figure shows upstream action at top left and downstream response at top right. From left to right, the figure also depicts intersectoral public health action, direct public health action, and healthcare response. From left to right the figure describes the following components:
- Social, structural, and ecological determinants of health:
- Economic policies to reduce income inequities and poverty;
- Land and water use policies informed by One Health and health promoting approaches;
- Treaty rights, self-determination, and self-governance for Indigenous Peoples;
- Social policies to address racism, ageism, and other stigmas; and,
- Policies to reduce extraction of oil and gas and reliance on fossil fuels and create renewable alternatives.
- Living conditions and ecosystems:
- Physical and built environment: housing, land use, transportation, and exposure to toxins.
- Social environment: culture, experiences of discrimination, and violence.
- Economic and work environment: employment, income, and occupational hazards.
- Service environment: education, social services, and health care.
- Climate resilient building codes (e.g., max heat, ventilation);
- Equitable access to green space and tree cover canopy;
- Upgraded water and wastewater systems;
- Water conservation, reuse, and storage techniques;
- Equitable access to nutritious and culturally appropriate foods;
- Active and public modes of transportation; and,
- Walkable and transit-supportive communities.
- Community and individual level risk:
- Community level preparedness plans and warning systems;
- Cooling centres;
- Household ventilation and cooling;
- Place-based mobilizing and communication; and,
- Action and communication to support people and communities to make climate friendly and healthy choices where they live.
- Disease and injury:
- Diagnosis and treatment for climate change related diseases and injuries, and
- Climate resilient health care facilities that can provide care during climate-related events.
These are examples of actions and do not represent the full range of possible adaptation and mitigation interventions.
Upstream action on the social and ecological determinants of health can be supported with a health promotion approach. This recognizes that social, economic, ecological, and political conditions intersect to influence where, why, and how risk, vulnerability, and health outcomes occur and cluster.Footnote 259Footnote 260Footnote 261Footnote 262 This requires intersectoral action to build healthy public policy, create supportive and healthy environments, and strengthen community action.Footnote 213 Although challenging, public health can advocate and provide the evidence for focused attention on key societal conditions that impact health, such as income, racism, colonization, ageism, employment, education, built environments, and housing.Footnote 5Footnote 8Footnote 102Footnote 263Footnote 264Footnote 265 International commitments, including the Ottawa Charter for Health Promotion, the Geneva Charter on Well-being, and United Nations Declaration on the Rights of Indigenous Peoples (UNDRIP), underscore the importance of an upstream health promotion approach to public health action on climate change.Footnote 55
Public health initiatives to address downstream impacts must continue alongside upstream action. As detailed in Section 1, climate change poses a number of urgent health threats that require immediate action. Public health systems lead and partner on a number of critical programs to address existing climate impacts and the need for them is likely to grow. Many relate to the role of public health within emergency responses, to protect populations from risks such as extreme weather (e.g., storms, heatwaves), wildfires, or floods.Footnote 266Footnote 267 This includes warning systems, and preparedness plans, as well as public education and risk communication. Downstream impacts are not limited to physical health outcomes. There is growing attention to the need to address the wide range of mental health outcomes impacted by climate change.Footnote 5Footnote 175 Public health responses to this include communication and outreach, community engagement, and mental health literacy and training.Footnote 5Footnote 102
Public health attention across the upstream-downstream continuum is necessary to address the complexity and scale of climate-related health issues. This is consistent with a One Health approach, which takes an integrated and unifying approach to sustainably balance and optimize the health of humans, animals, plants, and ecosystems.Footnote 268Footnote 269Footnote 270 It involves working across sectors, disciplines, and communities to promote and protect health, take action on climate change, contribute to sustainable development, and address our collective need for healthy food, clean water, energy, and air see (Figure 8).Footnote 270 The interconnections between humans, animals, plants, and their shared environments influence, and are influenced by, conditions and interventions at each level along the continuum. A One Health approach calls on public health to think beyond human health, which has particular relevance in the context of climate change.Footnote 265Footnote 271Footnote 272 However, for this approach to fully reflect equity, a guiding principle of public health systems, explicit attention to equity, and justice for human and animal systems is needed.Footnote 253Footnote 273

Figure 8: Text description
The figure describes the components of the One Health approach. Three circles, which represent healthy animals (illustrated by a cow), healthy humans (illustrated by two adults and a child), and healthy ecosystems (illustrated by a deciduous tree) overlap to form the One Health approach.
Prioritize community expertise and engagement for equitable and effective climate action
Climate change has wide-ranging impacts on physical and mental health, as well as on our ecological, social, and economic environments. However, the nature and severity varies a great deal, influenced by determinants of health (e.g., income, employment, living and working conditions) and structural systems of oppression (e.g., colonization, racism, ableism, heteronormativity).Footnote 5Footnote 264 As a result, in order to understand and address the health impacts of climate change, public health systems must prioritize a focus on equity and support the leadership of community.
Embedding equity and justice in public health action on climate change
A focus on equity and the social determinants of health is key to understanding and addressing the differential impacts of climate change.Footnote 19Footnote 264 An equity lens is required across all public health functions. It guides surveillance and population health assessment efforts to identify health inequities and understand their root causes.Footnote 274Footnote 275 It strengthens the case for health promotion and upstream public health action. Focusing on understanding who is most impacted by climate change and why also influences where and how health protection functions are applied. This can include prioritizing action for communities facing disproportionate risk, ensuring public health responses reflect the community and context, and responding to urgent needs while addressing structural issues that lead to greater risk.
To date, an equity lens has not been consistently applied to climate change.Footnote 5Footnote 276Footnote 277 While some social determinants of health have been a focus for research, others require further attention. For example, climate adaptation efforts have had a greater focus on inequities related to income, but less so on the experiences of First Nations, Inuit, and Métis Peoples, racialized, migrant and LGBTQ2S+ populations, and people with disabilities.Footnote 3Footnote 277Footnote 278Footnote 279
Applying an equity lens to knowledge and research can highlight differences in climate-health impacts across populations. It also supports an understanding of how climate change – and our response to it – can create new inequities. This includes the risk of maladaptation, which can exacerbate existing inequities.Footnote 5Footnote 19 For example, if new urban green spaces in low-income neighbourhoods result in gentrification, residents may be displaced.Footnote 5 Maladaptation also occurs when actions favour one group over another, such as a lack of cooling centres in low-income areas, despite the likelihood of higher need.Footnote 5 A commitment to equity can also ensure the potential benefits of climate change activities are distributed fairly.
Peel Region has put equity principles into practice with its urban forest, which was a local priority to support climate mitigation and adaptation.Footnote 280 Working with conservation authorities, local municipalities, public health professionals, foresters, and planners, the region identified neighbourhoods particularly vulnerable to extreme heat and prioritized them for tree planting.Footnote 280Footnote 281 This approach was designed to improve the equitable distribution of tree cover and public greenspace across the region.Footnote 280
Concepts of justice are also important for climate action.Footnote 276 Environmental justice means that no population suffers unjust and disproportionate environmental harm, and that all people are fairly treated and meaningfully involved in environmental laws, regulations, and policies.Footnote 28Footnote 282 Adopting this principle ensures that communities and populations facing vulnerabilities do not face damaged ecosystems or increased health risks because of their vulnerabilities.Footnote 28 It also requires public health to consider equitable access to clean air, water, and food, which are fundamental ecological determinants of health.Footnote 28 Community engagement is key to building equitable processes and outcomes in climate adaptation interventions.Footnote 5 Resources for community capacity building are necessary to support this work.Footnote 19
Environmental justice has particular relevance for First Nations, Inuit, and Métis Peoples, led by Indigenous conceptualizations of justice. It is important for addressing climate change, as well as other wrongs caused by colonization.Footnote 283 Colonialism is directly related to environmental changes that have impacted the ecological systems that support the culture, health, economics, and self-determination of Indigenous Peoples.Footnote 284 It led to industrialization and carbon-intensive economies, driving climate change through deforestation, fossil fuel extraction and burning, and pollution.Footnote 284 This has harmed the environment, displaced Indigenous Peoples, and disrupted customs, skills, and identities connected with local ecosystems, including plants and animals.Footnote 284 In response, an Indigenous environmental justice approach emphasizes the importance of all relations, which requires a concurrent focus on Indigenous knowledge systems, legal orders, governance, and concepts of justice.Footnote 283
A focus on justice also prioritizes youth and recognizes the climate risks past and current generations have created for future generations.Footnote 285Footnote 286Footnote 287 Action for intergenerational justice has been led by youth activists, who have mobilized around the world to address climate change.Footnote 99Footnote 285 They have stressed the importance of recognizing youth as leaders, including early engagement in decision-making, providing platforms for youth to discuss their climate-health concerns, investing in youth-led initiatives, and prioritizing diverse youth voices.Footnote 99Footnote 288 The IPCC has emphasized the critical consequences of climate change for young people and underlined the importance of engagement with youth for effective and equitable climate governance.Footnote 255Footnote 289 This is being recognized through initiatives such as the United Nations Secretary-General's Youth Advisory Group on Climate Change and the Government of Canada's Environment and Climate Change Youth Council.Footnote 290Footnote 291
Collaborating with communities for climate action built on place-based knowledge and leadership
"It's not enough to have epidemiologists, virologists, etc. It's also important to have historians, to have anthropologists, to have Indigenous Elders, to have Black Elders, to have representatives from several communities, to have people who are experts in decolonization, to have a plethora of people so that we can approach and tackle problems with several solutions."
The complex mix of environmental and social conditions that influence health play out differently across communities, giving "place" as a unique local context a central role in how health and health equity are understood and promoted.Footnote 292 Like other public health issues, climate change has global and local implications, requiring responses that are context and community-driven, as well as connected to national and international efforts.Footnote 293Footnote 294
Community members are experts on their local context but are often disconnected from decision-makers with the resources and power to create systemic change.Footnote 8Footnote 283 Community engagement has long been recommended to address this gap and is integral to health promotion.Footnote 213Footnote 263Footnote 295Footnote 296Footnote 297 Inclusive and equitable community engagement in public health action is particularly essential to effectively address complex problems and build the conditions for good health.Footnote 5Footnote 94Footnote 298 Public health can facilitate and advocate for community engagement in climate action.Footnote 243
Community engagement and decision-making are key to procedural justice, which relates to fair participation and a just process.Footnote 276 A crucial role for community partners is involvement in population health assessments as well as in climate change and health vulnerability and adaptation assessments. This form of engagement can help build understanding of local context, identify local threats to health, map community assets and resources, and contribute to monitoring and evaluating interventions.Footnote 5Footnote 94Footnote 229Footnote 277Footnote 299 By looking at hazards, exposures, and vulnerabilities concurrently as part of a process driven by local empowerment and action, public health can better support community climate resilience.Footnote 8Footnote 94Footnote 181Footnote 264Footnote 300
Engagement is also critical to ensure appropriate emergency preparedness and response. The increasing risks posed by natural disasters can threaten the physical and social structures of communities, requiring particular attention from the health system, including public health to protect health and prevent disease and injury (see text box "Supporting community-centred preparedness to address population mobility from the impacts of climate change").
Supporting community-centred preparedness to address population mobility from the impacts of climate change
Many extreme weather events in Canada have forced people to evacuate from their homes and regions, some repeatedly, sometimes never to return.Footnote 301Footnote 302Footnote 303 Evacuees' experiences are traumatic during a disaster and have long-reaching effects when the event itself is over, resulting in increased rates of anxiety, depression, and post-traumatic stress disorders.Footnote 304
The role of public health is to work with communities to prepare for, adapt to, and mitigate the effects of evacuations and other causes of population mobility before, during, and long after evacuations. This needs to include supporting community-centred preparedness that is based on local knowledge and leadership. For example, engaging and collaborating with communities around returning home, rebuilding lives, and ensuring key services, such as mental health and family violence services, are available.Footnote 305Footnote 306Footnote 307
Public health support for community engagement and community-led action in First Nation, Inuit, and Métis communities is particularly important given pre-existing and ongoing health and social inequities as a result of colonization, and emergency preparedness and response efforts that have lacked Indigenous perspectives.Footnote 308Footnote 309Footnote 310Footnote 311Footnote 312Footnote 313
Thank you to contributing authors:
Dr. Yoav Keynan, Scientific Lead and Margaret Haworth-Brockman, Senior Program Manager
National Collaborating Centre for Infectious Diseases
"Decolonizing public health spans the whole gamut. It is the important work of not only reconciliation but resurgence and meaningful allyship (not performative allyship) and LandBack. So, repairing, restoring, and centring Indigenous communities and their right to self-determination, and their leadership on these fronts is essential."
For First Nations, Inuit, and Métis Peoples, public health support for community leadership must go beyond engagement to support self-determination at the pace and in the ways First Nations, Inuit, and Métis partners choose.Footnote 196Footnote 314Footnote 315Footnote 316 As a principle, self-determination is about empowering and enabling communities to build capacity and gain control over the conditions and forces that affect their health and well-being.Footnote 315 It is an essential aspect of decolonizing public health systems, a precondition to reconciliation, and the key to addressing long-standing inequities that influence emerging public health challenges.Footnote 196Footnote 314
Self-determination is deeply relevant to addressing the health impacts of climate change and should be the foundation for climate-health research, assessment, action, and governance. Despite Indigenous leadership in environmental and climate justice movements across the world, many government climate change plans fail to respect the right to self-determination.Footnote 316 Governments and civil society must recognize First Nations, Inuit, and Métis Peoples' expertise and leadership by supporting self-determination in climate action.Footnote 196Footnote 316 Decolonial and anti-racist frameworks must underpin public health action in order to address the unequal distribution of power and access to the ecological and social conditions that determine our health.Footnote 317
Advance knowledge to understand, predict, and respond to the health impacts of climate change
Broader and deeper knowledge is needed in Canada to more fully understand the range of health impacts associated with climate change, their inequitable distribution across populations, and how best to address them.Footnote 5Footnote 318Footnote 319Footnote 320 This can be supported by research on a broader range of climate-health pathways, more attention to diverse climate change experiences, integrated climate-health surveillance, and intervention research and implementation science to understand how to protect and promote health in a changing climate. These priorities will be enhanced by better integrating Indigenous and Western knowledge.Footnote 43
While these areas of inquiry are important for guiding our work, they should not preclude urgent climate-health action. To date, efforts have largely focused on planning and implementation, which has been slow, incremental, and small-scale.Footnote 43 Scaling up of existing actions and implementing new actions are necessary to prevent catastrophic health impacts.Footnote 255Footnote 321
Understanding the full picture of climate impacts on health
While considerable climate-health research has been completed, the myriad of relationships between climate and health require further attention. The field of public health must help address the gaps by researching all health impacts of climate change, advancing research on the pathways between them, and improving intersectional data for public health surveillance to capture climate-health connections. These advances can help identify health co-benefits of various climate actions and inform interventions. Additional details on research and climate-health knowledge gaps can be found in respective chapters of the Health of Canadians in a Changing Climate Report, the CPHO companion document Generating Knowledge to Inform Public Health Action on Climate Change, and Climate Science 2050: Advancing Science and Knowledge on Climate Change.Footnote 230
Current research has focused on a fairly narrow selection of health outcomes related to climate change, particularly infectious diseases as well as respiratory, cardiovascular, and neurological outcomes.Footnote 319Footnote 320Footnote 322 Researchers have emphasized the need for further research on broader health impacts, such as mental, maternal, and child health.Footnote 5Footnote 179Footnote 319Footnote 320Footnote 323 Existing research has also focused more on impacts than on action. Literature reviews have noted a need for more research on mitigation and adaptation interventions.Footnote 91Footnote 319Footnote 320Footnote 324
There is also a need for more research on future impacts, including climate models and simulations that project what is yet to come.Footnote 5Footnote 244Footnote 319Footnote 325 Most climate-health research has focused on past observed impacts. As a result, there is an important knowledge gap about how climate change will differentially impact health under 1.5°C and 2°C warming.Footnote 86 There is also little evidence on how effective, or ineffective, adaptation strategies will be in the future under different levels of warming.Footnote 319Footnote 326
The distribution and clustering of climate-health impacts, as well as the interventions needed to prevent and address them, also requires further attention. The experiences of urban communities have received some consideration, but more regional analyses is required across Canada, particularly in rural and remote areas.Footnote 319Footnote 323 While there is some research in this area that explores the role of age, and sex and/or gender, less has been done on the experiences of racialized populations, gender and sexually diverse populations, Indigenous Peoples, as well as those experiencing homelessness or living with low-income.Footnote 5Footnote 319
Understanding the distribution of climate-health impacts opens further inquiry into the root causes of differential risk.Footnote 5Footnote 276 Public health can help strengthen the knowledge base on the complex direct and indirect pathways between ecological and social determinants of health, climate change, and health outcomes. As described in Section 1, determinants of health influence, and are influenced by, differential exposure, sensitivity, and adaptive capacity to climate change, all of which can impact health outcomes.
A greater understanding of these direct and indirect pathways can inform interventions to protect health and prevent disease and injuries associated with climate change.Footnote 5Footnote 91Footnote 319Footnote 327 This can include intervention research, as well as implementation science research to understand the uptake and implementation of evidence-based practices. Public health research can also support a greater understanding of resilience and protective factors and form partnerships to help promote community resilience and community-based action.Footnote 5Footnote 19Footnote 328
Strengthening climate-health monitoring and surveillance
"We need to be tracking on a health systems-wide level how climate change is impacting people in real time… If you don't have data, then it's really hard to convince people to do anything, convince government to do anything."
Increased surveillance and further monitoring of the health impacts of climate change are needed at the individual, community, and population levels to fill critical knowledge gaps and inform action.Footnote 329 Public health can further increase knowledge of the climate-health impacts through our recognized expertise in data, surveillance, monitoring, and integrated risk assessment. To do so, we need to adapt surveillance tools to better monitor vulnerabilities, risks and exposure to climate hazards, as well as climate-health outcomes.Footnote 5Footnote 324Footnote 330 It also requires the application of broader approaches such as One Health to ensure the full context of human, animal, and environment relationships that shape these outcomes are captured.Footnote 331 One example of bringing One Health into surveillance is underway across Saskatchewan, Alberta, and British Columbia. This collaborative project aims to generate evidence on how ticks and tick-borne disease are impacted by climate change in these 3 western provinces, with a focus on animal and human health.Footnote 332
To inform comprehensive and targeted climate action, surveillance must integrate data on ecosystems, environmental determinants of health, infrastructure, and the capacity of systems to respond to climate risks.Footnote 5Footnote 94Footnote 318 This form of integrated risk monitoring is recommended by the WHO, and the information it could generate would be useful to understand differential risk and develop early warning systems.Footnote 94 For example, heavy rainfall connected to climate change has been found to impact water contamination.Footnote 333Footnote 334 However, the WHO found that more than 60% of countries, including Canada, currently do not include weather and climate information in health surveillance systems for water-borne diseases.Footnote 62
The SUPREME integrated heat health warning system in Quebec is an example of an integrated risk monitoring system.Footnote 335 It was developed in collaboration between the Institut National de Santé Publique du Québec, the Québec Ministry of Public Security, and Environment and Climate Change Canada's Meteorological Service of Canada. It includes indicators related to exposure, neighbourhood vulnerability, and health outcomes, which allows for more targeted heat warnings and interventions to mitigate heat-related risk, particularly for vulnerable populations.
Existing public health surveillance programs can be modified. This requires integration of key data, such as environmental changes, deforestation, and other land use trends, as well as the cumulative nature of the health impacts of climate change.Footnote 62Footnote 330Footnote 336Footnote 337 They can also recognize and account for the given geographic and social context, such as health-related indicators of climate change in Nunavut.Footnote 338 Surveillance systems can be strengthened to better monitor the link between climate change and chronic conditions, such as cardiovascular disease caused by extreme heat, as well as focusing on maternal, children and youth health, mental health, the aging population, and other Canadians in vulnerable situations.Footnote 339
Public health systems can build on lessons from the COVID-19 pandemic to enhance pan-Canadian climate surveillance and reporting of climate-related health effects. For example, COVID-19 has spurred efforts to address longstanding issues that have impacted Canada's ability to collect, share, access, and use health data to inform public health advice and improve the health system through the Pan-Canadian Health Data Strategy.Footnote 340 This is essential to address gaps in existing data across jurisdictions and sectoral silos.Footnote 44Footnote 318Footnote 341 There are other promising initiatives to build on here and internationally.Footnote 318 For example, the Lancet Countdown's indicators cross multiple domains: impacts, exposures, vulnerabilities, adaptation, planning, resilience for health, mitigation actions, health co-benefits, economics, finance, and public and political engagement.Footnote 226
Expanding surveillance also requires a focus on health inequities. Data that can be disaggregated by demographic variables would greatly improve what we know about climate change vulnerabilities.Footnote 5Footnote 190Footnote 243 This also allows for greater understanding of the interconnections between inequities and how they drive risk. A good example is a report completed by the BC Coroners Service, which found that most of the heat-related deaths associated with the 2021 heat dome were among older adults who lived alone and whose health was compromised by multiple chronic diseases.Footnote 66 The data also showed that more of the people who died lived in socially, or materially, deprived neighbourhoods than the general population.Footnote 66 Intersecting inequities can be captured by using multiple equity stratifiers concurrently, such as race, income, gender, and disability status, or through indices.Footnote 342 This would support population health assessment of differential climate-health risks and impacts. The Public Health Agency of Canada recently released a literature review and checklist to support integrating intersectionality theory in quantitative health equity analysis.Footnote 343
Interoperable health data and surveillance are also crucial for capturing the public health impact of climate-driven emergencies. Disaster research links surveillance and emergency preparedness to monitor the health impacts of extreme weather events and natural disasters using hospital, public health, and reportable disease surveillance data.Footnote 344Footnote 345 For example, for 6 weeks after the 2013 floods in southern Alberta, public health surveillance was implemented to detect health outcomes, such as injuries, mental health issues, and infectious diseases.Footnote 192 Data on presenting complaints in emergency departments, prescription drugs, and reportable diseases were used to inform public health responses.Footnote 192
Enhanced climate-health surveillance would help advance climate change and health vulnerability assessments in Canada. In a 2018-2019 survey of 80 health sector officials across Canada, only 35% of respondents reported having undertaken a vulnerability and adaptation assessment for climate change and health.Footnote 5 Health Canada's HealthADAPT program recently provided funding and support to 10 local and regional health authorities to build capacity to understand and address the health impacts of climate change, including completing vulnerability and adaptation assessments.Footnote 5
Fostering Indigenous research leadership and Indigenous knowledges sovereignty
"What we're trying to teach is that traditional knowledge is not just for Indigenous people, it's for everybody. All you have to do, really, is start to respect and understand traditional knowledge of Indigenous peoples and you will see there will be a groundswell of new creative and innovative ways and means in which to address these challenges that we face today in the world."- Siila Watt-Cloutier, excerpt from Indigenous Knowledges and Climate Change, Climate Atlas of Canada.Footnote 51
As discussed in Section 1, First Nations, Inuit, and Métis knowledge systems are critical for identifying, mitigating, and adapting to changing environmental conditions. They make a fundamental contribution to the knowledge base of climate change. Combining the unique contributions of Indigenous and Western knowledge and applying concepts of 'two-eyed seeing' has been found to improve climate-health monitoring and surveillance, better identify and assess climate risks, and enrich climate adaptation policy and practice (see text box "Indigenous knowledges and climate-health action").Footnote 5Footnote 19Footnote 346
Indigenous knowledges and climate-health action
Abridged excerpt from: Climate Change and Indigenous Peoples' Health in Canada.Footnote 347
"Indigenous people have drawn on Indigenous knowledge and science for millennia to understand and respond to climate and environmental changes they faced… We must correct the path we are walking on and return to the special relationships, the teachings, the knowledge and practice that maintains respect, honor, and relationship with the natural world".Footnote 347
Indigenous knowledge systems are comprised of understandings, skills, and philosophies about the ethical, social, political, and governance aspects essential to community survival and resource sustainability. There are different types of Indigenous knowledges such as Traditional Ecological Knowledge, Traditional Knowledge, and Inuit Knowledge or Inuit Qaujimajatuqangit. All are dynamic and living concepts that denote the understanding, interdependence, and relationality between Indigenous Peoples and the lands they call home, including all Creation and beings (animate and inanimate) within that land.Footnote 348
Indigenous knowledges are embedded within Indigenous languages and transmitted to next generations through community knowledge.Footnote 349Footnote 350Footnote 351Footnote 352 This includes observations about the land, plants, insects, forests, waterways, sea, sea ice, soil, weather conditions, and migratory patterns of animals.Footnote 348Footnote 349Footnote 353
Indigenous knowledges have significantly contributed to the survival and resilience of Indigenous Peoples. It is equal to Western scientific information in understanding and adapting to climate change. In fact, Indigenous and Western scientific knowledge systems can accentuate and strengthen each other in understanding and addressing climate change. However, meaningful connections between Indigenous knowledge systems and Western climate change research and policy remains a challenge. Efforts must be made to support the participation of Indigenous scholars and knowledge holders in climate change discussions and action plans to contextualize their unique lived experiences as well as cultural and colonial realities.
Indigenous knowledges and worldviews provide powerful teachings on environmental stewardship to reduce the severity of climate change. Actions can be taken to enhance these knowledges and use them wisely by adopting interventions based on community-driven, participatory, and collaborative approaches. Connecting Western science and Indigenous knowledge systems should be guided by co-production frameworks that address the challenge of inequitable power differentials. A co-production approach promotes community engagement, incorporates community needs and interests, and reflects local context in terms of resources and adaptive capacity. Initiatives to support Indigenous knowledges in climate action must go beyond a focus on integrating Indigenous knowledges into Western science, to instead foster Indigenous research leadership and Indigenous knowledges sovereignty.Footnote 354
Thank you to contributing authors:
Donna Atkinson, Roberta Stout, Regine Halseth, and Margo Greenwood
National Collaborating Centre for Indigenous Health
For example, the Tla'amin Nation in British Columbia are completing a climate-health assessment and adaptation plan to identify and address the risks to community health and wellness.Footnote 355 Funded by the First Nations Health Authority, this initiative works with Tla'amin knowledge keepers, collaborates with the community to draw upon local knowledge, and engages with youth as part of efforts to tour and monitor the land for signs of climate change.Footnote 355 This project is led by Tla'amin Nation staff and supported by a researcher from the University of Saskatchewan.Footnote 355
The Government of Canada is developing an Indigenous Knowledge Policy Framework in the wake of 2019 legislation that requires Indigenous knowledge to be considered in project reviews and regulatory decisions related to the Impact Assessment Act, the Canadian Energy Regulator Act, the Fisheries Act and the Canadian Navigable Waters Act.Footnote 356 This work is driven by a federal commitment to reconciliation with Indigenous Peoples through a renewed, nation-to-nation, government-to-government, and Inuit-Crown relationship based on the recognition of rights, respect, co-operation, and partnership.Footnote 356
Despite these advances, further progress is necessary to connect Indigenous and Western ways of knowing.Footnote 283Footnote 316Footnote 357 For example, the ideas that underpin a One Health approach are similar to the holistic perspectives of Indigenous Peoples regarding the interconnections between human health and the well-being of the land.Footnote 358 Indigenous knowledges preceded the emergence of a One Health perspective, but there has been little attention given to how Indigenous Knowledges should inform a One Health approach.Footnote 358 This includes recognition that Indigenous human health, the well-being of the land, and connection to the land have all been impacted by colonization.Footnote 272 A focus on Indigenous self-determination and the inclusion of Indigenous knowledge systems and leadership can meaningfully strengthen One Health efforts in Canada.Footnote 272Footnote 358
Supporting Indigenous climate leadership requires respecting the governance structures of nations. It means actively supporting the principle of self-determination and self-governance by ensuring space for Indigenous decision-making tables and moving from consultation to true engagement and co-development. This includes policies and protocols that support collaboration and research (e.g., nation-specific principles rooted in ownership, control, access, stewardship, and possession of data and knowledge).
Collaborate across sectors for transformative climate-health action and intersectoral co-benefits
Public health is well-positioned to advocate for, convene, and act on intersectoral public health issues such as climate action.Footnote 94Footnote 300Footnote 359 Climate mitigation and adaptation efforts require coordinated action towards a common goal, across sectors and levels of government. Isolated adaptation and greenhouse gas mitigation efforts will not adequately address the ecological and social conditions that determine health. A lack of coordination could lead to duplicated, fragmented, or maladapted action.Footnote 19Footnote 360Footnote 361 For that reason, the IPCC has identified inclusive governance structures and strong institutional frameworks as key enabling conditions for climate adaptation and mitigation.Footnote 19Footnote 255
Governance for climate action is best supported by alignment and coordination across sectors and policy domains, with high-level coordinating bodies that are not bound by departmental mandates.Footnote 19Footnote 255 This kind of approach is particularly important in Canada, where jurisdictional responsibility for public health and climate change is shared across multiple levels of government, which can make policy coherence a challenge.Footnote 360 This must also include Indigenous self-government, which is an essential component of governance related to climate change in Canada.Footnote 362
Interjurisdictional and intersectoral collaboration is particularly important for upstream initiatives focused on larger and more transformative actions.Footnote 5Footnote 363Footnote 364 Domestic efforts have mostly concentrated on addressing negative impacts of climate change, with less attention to the underlying root causes of risk and vulnerability (i.e., social determinants of health).Footnote 323 The growing threat requires a more comprehensive approach on both.Footnote 323 This highlights the need for public health leadership to drive action.
One way that public health can support intersectoral action is through a focus on co-benefits to help decision-makers better understand the advantages of climate action. There are a number of health co-benefits possible from climate mitigation and adaptation strategies. For instance, investments in cycling, pedestrian, and green infrastructure can decrease greenhouse gas emissions, increase active travel, reduce the burden of cardiac and respiratory disease, and support mental health.Footnote 365 Leadership in Energy and Environmental Design (LEED) green building certification can reduce greenhouse gas emissions, improve air quality, and reduce respiratory-related morbidity and mortality.Footnote 365 However, most research on co-benefits has focused on a small number of health issues, such as air quality and physical activity.Footnote 366Footnote 367Footnote 368
Through research, methods, and tools, public health systems can help identify the diverse health impacts of climate change and facilitate pinpointing health co-benefits of climate action.Footnote 366Footnote 369 Focusing on co-benefits could also help create opportunities for mitigation and adaptation efforts that strengthen determinants of good health and address root causes of differential vulnerability.Footnote 5 There already exist multiple methods and tools to maximize knowledge around co-benefits, such as the Health Impact Assessments tools (see case study "Health Impact Assessment: A promising approach to addressing climate change").
Health Impact Assessment: A promising approach to addressing climate changeFootnote 369
A Health Impact Assessment (HIA) is a structured intersectoral approach to understand the potential effects of a policy, program, or project on the health of a population. Promoted by the World Health Organization, this approach aims to better inform decision-makers about the possible consequences of their decisions on the health and well-being of the population and on inequities.
Health Impact Assessments can be applied to climate change policies and strategies to incorporate a focus on health and lead to better informed choices in the long term.Footnote 370 One U.S.A. study analyzed 12 HIAs that were conducted in 6 states and applied to proposed climate change policies. It concluded that the process can facilitate intersectoral collaboration, help optimize health co-benefits, and raise awareness among decision-makers about the health impacts of potential policies.Footnote 371
Application examples
HIAs were used to assess the health impact of climate change mitigation policies at the local level in Geneva, Switzerland.Footnote 372Footnote 373 In Houston, Texas, it helped estimate the health co-benefits of 3 different land-use scenarios with potential for climate change adaptation and mitigation: a downtown office building renovation, an urban infill, and a university campus sustainability plan.Footnote 374 In Basel, Switzerland, a HIA was employed to analyze the health impacts of 4 transport scenarios tied to local climate change mitigation policies.Footnote 375 Similar work has been carried out in the Netherlands to assess the health co-benefits of greenhouse gas reduction policies in Rotterdam's transportation sector.Footnote 376 These applications of HIAs helped identify which of the proposed climate change mitigation scenarios was most beneficial to health and determine the actions required to optimize the resulting health co-benefits.
Thank you to contributing authors:
National Collaborating Centre for Healthy Public Policy
Climate action can generate additional benefits in other sectors through innovation, agricultural productivity, livelihoods, biodiversity conservation, and a reduction in damages from natural hazards.Footnote 19 These benefits are not only realized far in the future. Some, including improvements in air quality, can be achieved within years.Footnote 90 Many co-benefits in other sectors also have relevance to improving public health. Highlighting co-benefits across sectors could help motivate intersectoral decision-making and action.
Research on climate action co-benefits could lead to better economic valuations of them, which would allow decision-makers to more thoroughly compare the costs and savings of action versus inaction.Footnote 367 Economic savings are often an important incentive for governments, and research has shown that health-related savings could far outweigh the cost of climate mitigation.Footnote 62
As a part of a wider approach, emphasizing health co-benefits can support integrating a public health focus across climate change planning and policy processes in sectors responsible for land use, transportation planning, building standards, urban planning and development, energy planning, agricultural practices, conservation and environmental protection, livelihoods, infrastructure, sanitation, and water (see text box "Quebec's Government Health Prevention Policy and 2022-2025 Inter-Ministerial Action Plan: A lever for action on climate change").Footnote 5Footnote 19Footnote 377
Quebec's Government Health Prevention Policy and 2022-2025 Inter-Ministerial Action Plan: a lever for action on climate changeFootnote 378
In June 2022, the Government of Quebec published the Plan d'action interministériel 2022-2025 de la Politique gouvernementale de prévention en santé (2022-2025 Inter-ministerial Action Plan of the Government Health Prevention Policy). This plan constitutes the second implementation phase of the Politique gouvernementale de prévention en santé and has a budget totaling $120 million. Under the leadership of the Ministry of Health and Social Services, the plan sets up a collaborative partnership with nearly 30 government ministries and agencies and more than 80 non-governmental partners to implement actions to improve population health and reduce health inequalities.Footnote 378 The actions revolve around 4 main areas of focus: developing people's abilities from an early age, building healthy and safe communities, improving living conditions that promote health, and strengthening preventive actions in the health and social services system.
Notably, the action plan, through measure 2.9, supports Quebec regional public health authorities to carry out large-scale intersectoral projects on climate change within regional communities.Footnote 378 This is supported by the Ministry of Health and Social Services, in collaboration with the Ministry of the Environment and the Fight against Climate Change, and in partnership with the 18 regional public health authorities.Footnote 378 A budget of $6 million over 3 years is planned to deploy the measure.Footnote 378
The inter-ministerial action plan is based on a Health in All Policies approach and engages levers under the responsibility of non-health government sectors to take action on the determinants of health and factor in "the inseparable relationship among social, economic and environmental dimensions, in keeping with the principles of sustainable development" (pg. IX).Footnote 378 These actions are intended both to prevent the development of health issues at the population level, as well as relieve pressure on the health system in the coming years.Footnote 378
Thank you to contributing authors:
National Collaborating Centre for Healthy Public Policy
Building public health perspectives into climate change initiatives can not only increase co-benefits, but also reduce maladaptation, which is more likely when singular risks or sectors are the sole focus of action.Footnote 5Footnote 19Footnote 264Footnote 327Footnote 379 Integrating public health can support policy coherence, consistency, effectiveness, and managing trade-offs.Footnote 294 Ensuring that climate action addresses context and promotes equity also helps reduce maladaptation by ensuring that adaptation or mitigation efforts are appropriately tailored for relevant communities.Footnote 5 The IPCC has said that the risk of maladaptation can be reduced with planning that is multi-sectoral, multi-actor and inclusive.Footnote 19
Cities have been at the forefront of intersectoral climate action and are powerful sources of climate resilience and resourceful action.Footnote 380Footnote 381 The emerging movement of sustainable and smart cities promotes scaling up of local innovation to support environments and infrastructure for climate-health action.Footnote 382Footnote 383Footnote 384 Examples of city and municipal intersectoral collaborations with explicit public health involvement are emerging across Canada (see text box "Local intersectoral initiatives across Canada").
To expand and effectively normalize these collaborations, however, requires resources, time, commitment, and staff with expertise and dedicated time.Footnote 385 This work can be resourced through dedicated public health system funds for intersectoral initiatives that support local public health units to directly work with other sectors on climate-health action.
Local intersectoral initiatives across Canada
Intersectoral action is key to addressing complex and challenging public health issues such as climate change. There are local and municipal organizations and public health units leading this work across Canada. Two examples are provided to illustrate the potential associated with these approaches.
On the west coast, at Island Health on Vancouver Island, environmental health officers have moved beyond regulatory roles to focus on healthy built environments with municipal planners, community organizations, and other stakeholders.Footnote 386 This includes work on issues related to air quality, climate change, active transportation, and social cohesion.Footnote 386
In Ontario, Ottawa Public Health co-located 2 staff members in the municipal Planning, Real Estate and Economic Development Department for 3 years. This was intended to inform the city's new official plan and ensure it would create healthy, inclusive, and resilient communities. As a result, the plan includes a focus on building environmental, climate, and health resiliency through walkable 15-minute neighbourhoods, which is an approach that concurrently supports public health, health equity, and climate mitigation and adaptation.Footnote 387
Strengthen public health leadership for climate action and public health building blocks for climate resilience
In addition to partnering across sectors, there are a number of key areas where public health can demonstrate system-level leadership while advocating for climate action. Public health systems can prioritize dedicated resources to expertly inform and coordinate action on health impacts, lead by example by shifting to low carbon health systems, and strengthen the foundation of public health systems to act on complex issues.
Public health advocacy for change
"Public health is very much the catalyst to bring groups together and to break down the silos. We definitely have an advocacy role to make folks aware. But then we also have a role to build the system and get ahead of this, and get upstream, structural challenges, thinking about things like how do we change our city design?"
Actions stemming from this roadmap will require public health to push for transformation, moving beyond a focus on risk management.Footnote 388Footnote 389 This includes taking a strong leadership role in targeting social, economic, and environmental determinants and injustices.Footnote 181Footnote 390 Successful leadership involves building coalitions and influence through direct policy relationships and indirect public mobilization.Footnote 388 This means supporting those working in public health so they can effectively navigate different political climates and highly politicized health issues, including understanding and working with political cycles, policy windows, and policy decision-making, as well as tailoring content to audiences.Footnote 366Footnote 388Footnote 391
These skills are particularly necessary for climate action because of the challenging political and policy environment.Footnote 336Footnote 377Footnote 392 Competing interests have driven misinformation and disinformation that question the severity of climate change and the urgency of climate action.Footnote 336Footnote 366Footnote 388 A small but loud countermovement promotes climate skepticism while advocating strongly against perceived constraints on finances and freedom.Footnote 388Footnote 393 Knowledge sharing is not always enough to change beliefs driven by these types of political or economic ideologies.Footnote 336
To advance climate action, public health will need to be a trusted voice in our communities. Public health officials often have a unique role as representatives of the government that also have scientific credentials. Recent research suggests that people living in Canada view scientists as trusted sources of climate information.Footnote 394 Public health organizations, agencies, and units must maintain their positions as scientifically credible organizations to support public trust.
Dedicated climate-health action
Climate action requires intersectoral coordination and collaboration. However, it also requires dedicated and expert leadership to guide efforts from research to advocacy to implementation. While the climate-health connection is drawing greater attention in Canada, including across a variety of government initiatives, these efforts are dispersed rather than coordinated.
Mainstreaming involves integrating climate consideration and action across sectors, including public health. This approach is important, but it may not be enough to achieve the action necessary to address climate change. Research from Europe and analysis from the IPCC suggests there are limits to how this kind of mainstreaming can be used to integrate climate adaptation into other sectors' priorities and activities.Footnote 385Footnote 395 Integrating climate adaptation efforts can result in an unequal distribution across sectors, diluted implementation responsibilities, disconnected planning and investment, and insufficient coordination across overlapping or competing policy priorities.Footnote 395 At a local level, climate action may be best supported through a combination of dedicated climate approaches, as well as mainstreaming, to ensure adequate focus on climate change and to support movement from policy to implementation across sectors.Footnote 385 Dedicated approaches can involve standalone institutional structures, with dedicated resources and accountabilities.Footnote 385Footnote 396 Examples of dedicated climate-health institutions can be found in academic and government settings.
At the London School of Hygiene and Tropical Medicine, the Centre on Climate Change and Planetary Health was created to partner with academia, government, industry, non-governmental organizations, and civil society to better understand planetary health and build solutions together.Footnote 397 Researchers at the Centre recently worked with the U.K. Health Security Agency to identify geographical areas and population sub-groups at greatest risk of excess mortality related to heat or cold exposure in England and Wales using data from the Office of National Statistics.Footnote 398 The results can be used to inform and target public health initiatives.
The European Climate and Health Observatory is a partnership between the European Commission and the European Environment Agency, among others. It works to deepen understanding of the current and future health impacts of climate change in order to inform prevention and preparedness across member states. Observatory activities include developing and sharing of data on the health impacts, risk indicators (integrating data on hazards, exposure, vulnerability and response capacity), risk assessment tools, monitoring and surveillance tools, early warning tools, predictions, as well as support for policy development.Footnote 399Footnote 400
Building low carbon health systems
In Canada, the health sector accounts for 4.6% of greenhouse gas emissions.Footnote 401 While this is largely due to emissions from hospitals, pharmaceuticals, and physician services, it also includes the emissions associated with public health systems.Footnote 401 It is difficult to determine the specific amount of emissions, but public health associated work and activities likely contribute to the carbon footprint of the sector, including office buildings, laboratories, data centres, supply chains, and transport.
One key way public health systems can limit their greenhouse gas emissions is through supporting and implementing upstream action to prevent the need for downstream clinical healthcare services. Through health promotion and protection, public health can reduce the negative health impacts of climate change and the associated demand for energy and resource intensive healthcare services.Footnote 256Footnote 402Footnote 403Footnote 404
Health systems have a responsibility to model a commitment to climate mitigation, and Canada has signalled this by signing on to the 26th United Nations Climate Change Conference of the Parties COP26 Health Programme commitments, which includes efforts to build climate-resilient and sustainable low carbon health systems.Footnote 405 This involves developing a baseline assessment of the system's greenhouse gas emissions and creating a plan to develop a sustainable low carbon model.Footnote 60
It can involve energy efficiency and conservation, use of renewable energy sources, sustainable procurement, and reducing waste.Footnote 5Footnote 130Footnote 402Footnote 406 Though many initiatives to decrease the carbon footprint focus on healthcare facilities and services, many other recommendations have value for public health systems. This includes improving building designs, reducing energy use, using renewable energy sources, changing purchasing practices, contracting sustainable suppliers, and using low emission vehicles for transportation of supplies, waste, and laboratory samples.Footnote 5Footnote 404Footnote 406Footnote 407 Recommendations from campaigns to reduce unnecessary medical and laboratory tests and healthcare treatments can also apply to public health, such as the guidance from Choosing Wisely Canada, which is organized by the University of Toronto, St. Michael's Hospital, and the Canadian Medical Association.Footnote 408
A facility-level example is Toronto Western Hospital, home to the world's largest raw wastewater energy transfer (WET) system. Construction began in June 2022 and once completed, thermal energy from municipal sewer wastewater will supply up to 90% of the hospital's heating and cooling needs, reducing greenhouse gas emissions by the equivalent of removing 1,800 cars from the road.Footnote 409 A province-level example can be found in Nova Scotia, where the Environmental Goals and Climate Change Reduction Act requires new government buildings and major retrofits to government buildings, including within the health system, to be net-zero energy performance and climate resilient (starting in 2022). It further prioritizes and encourages leased office space in climate-resilient and net-zero performance buildings (starting in 2030).Footnote 410
A strong public health foundation to tackle climate change
A strong foundation is required to ensure that public health systems are resourced and the people who work within them are prepared to act. This was evident throughout the COVID-19 pandemic, which continues to impact the resources and capacity of public health systems across the country.
While the essential public health functions show how public health systems do their work, the associated building blocks represent how systems are organized to support these functions.Footnote 253 Explorations of how public health can take on climate change must also consider what is needed from these building blocks. For a detailed review of them and the steps needed for broader public health transformation, please refer to the 2021 CPHO report. The section below will briefly discuss how the building blocks of public health need to be strengthened in the context of climate action, with a particular focus on the foundational building blocks of financial and human resources, and workforce expertise.
Adequate financing is central to the ability of public health systems to protect and promote health in a changing climate. Alongside other foundational building blocks, sufficient and sustainable financing is essential for addressing pressing public health issues.Footnote 94Footnote 253Footnote 359Footnote 411 This is particularly important for issues such as COVID-19 and climate change because their complexity and scale require public health systems to have the capacity to work across jurisdictions, prioritize addressing the range of determinants of health, collaborate with multiple communities, and convene and support intersectoral action.Footnote 94Footnote 300Footnote 411 However, it became clear during the pandemic that public health systems are already struggling with insufficient resources relative to their expansive mandates.Footnote 253Footnote 359 Climate adaptation programs focused on health have also received only a very small proportion of the funds allocated to adaptation initiatives in Canada, which is insufficient for current and future challenges we will face.Footnote 91Footnote 323 Without broader system-level change and greater support, public health systems will be unable to effectively and sustainably address new challenges arising from climate change.
Public health workforce expertise is central to climate action.
"One of the big things that can be done is changing the way that public health staff are trained, so that they are able to take a more eco-social approach to a variety of issues. And to think in a different way, so that they can do things differently."
A wide range of expertise is required to support climate action, including scientific, assessment, leadership, collaboration, communication, planning, and implementation skills.Footnote 243Footnote 412Footnote 413 Public health can build on existing expertise and skills including those found in the field of environmental health. Environmental health is core to public health practice, working to keep food, water, air, land, and facilities safe. For example, environmental public health professionals can play a key role in building sustainable environments and addressing environmental problems linked to climate change as part of adaptation efforts.Footnote 414Footnote 415Footnote 416
However, a training gap persists in Canada.Footnote 321 Despite recognition of its importance, there is little inclusion of climate change in the curriculum of Canadian graduate programs in public health or in the core competencies for public health.Footnote 9Footnote 417 There are also limited professional development opportunities for current public health professionals related to climate change. As a result, there is a need to train and support public health professionals so they are sufficiently prepared to assess and address the health impacts of climate change in their current work.Footnote 418Footnote 419Footnote 420Footnote 421Footnote 422 Further, as with other public health issues, First Nations, Inuit, and Métis knowledges and leadership are essential to effective climate action.Footnote 196 Culturally safe practice is key for meaningful engagement and this requires education and training on Indigenous knowledges, colonization, truth and reconciliation, and how to take action against anti-Indigenous racism within public health workforces.Footnote 196Footnote 347 However, these topics remain largely absent in current public health education, training, and competencies.Footnote 423Footnote 424
"If you don't have the skill sets and you're trying to do it off the side of your desk, it's really hard to lift it off the ground."
Ensuring sufficient financial and human resources, as well as workforce expertise, will strengthen public health systems and provide the foundation for public health to be a partner in climate action.
This will involve incorporating a climate focus into all other building blocks to drive new and modified approaches to evidence and knowledge generation, policy and programming interventions, medical and digital technology, and governance and engagement.
This roadmap detailed opportunities to strengthen public health systems across Canada and their response to the climate crisis. Protecting and promoting the health of all people living in Canada in the context of a changing climate will necessitate bold and ongoing public health action. The next section offers priority actions as next steps in this essential journey.
Way forward
Urgent public health action is required to prepare for, protect against, and respond to current and future health impacts of climate change. Public health systems can also make valuable contributions to existing climate efforts and show leadership on actions that have wide-reaching impacts. For countries like Canada, that are among the top per capita emitters of greenhouse gases, this is of national and global importance.
Climate action can create significant and almost immediate health benefits, while also protecting the long-term survivability of the planet and its inhabitants. If done well, these efforts will help to promote health, equity, and justice, now and in the future.
The Way Forward describes priority action areas that are entry points for public health systems to achieve the roadmap action items presented in this report. They can guide the preparation of public health systems to take immediate action on climate change, both within these systems as well as working with other key sectors. In this way, the action areas are cross-cutting and support the broader roadmap.
Although not exhaustive, the priorities can support public health professionals to be effective leaders and partners in addressing climate change and its impacts on the health of all people living in Canada, including within the context of the Pan-Canadian Framework on Clean Growth and Climate Change and our first National Adaptation Strategy.
Integrate climate considerations into public health systems
The everyday work of public health offers practical entry points for climate action, such as the deliberate integration of a climate-health lens into current public health functions, tools, and interventions. A climate-health lens also means building on existing approaches, such as One Health, to guide policy and program design and decision-making. These approaches must emphasize the social and ecological conditions that determine physical and mental health and recognize the interconnections between people, animals, and their shared environment. This includes linking with and supporting leadership, knowledges, and practices from First Nations, Inuit, and Métis Peoples' perspectives and experiences.
For public health systems to develop and implement appropriate health adaptation interventions, the right knowledge and evidence is needed. This includes understanding the unique geographical, social, economic, and environmental factors that influence community-level exposure and vulnerabilities. There are existing assessment tools that can guide adaption efforts. These need to be broadly and consistently implemented by public health authorities in collaboration with affected communities.
Actionable priorities to integrate climate considerations into public health systems
- Renew essential public health functions to emphasize socioecological considerations and guide effective public health action on climate change
- Incorporate climate-health considerations into current and future public health practice, policy, and programming
- Conduct equity-informed climate and health vulnerability and adaptation assessments to inform place-based efforts to prepare and respond to the health impacts of climate change
Centre health in climate change action
A focus on health is relatively new within the broader work of climate change mitigation and adaptation. We must continue to bring public health's voice and efforts to existing climate work and emphasize the co-benefits of interventions that span the upstream-downstream continuum from health promotion to emergency response. It will require public health systems to invest in partnerships across sectors and jurisdictions while prioritizing ways of working that put public health at climate action decision-making and planning tables. This focus on health must extend to climate change research, which requires new opportunities to integrate research and knowledge across disciplines that reflects the complex and multi-faceted challenges posed to health by climate change.
Public health has tools and expertise to help advance climate action. This includes approaches to research, community engagement, and program and policy assessment to understand who is most impacted by climate change and how best to protect and promote health, both physical and mental. Public health also has a long history of communicating about risk and protective measures with the public. Such expertise could be used to share information about climate health impacts and the co-benefits of actions that can address both health and climate change.
Actionable priorities to centre health in climate change action
- Identify ways of working together across sectors, jurisdictions, and public health systems to implement climate-health actions
- Draw on public health expertise to implement communication plans for mobilizing key audiences on climate-health action, such as health professionals, communities, the media, the education sector, and key sectors that influence health
- Develop cross-disciplinary research priorities on climate change and health to inform and advance evidence-based action on priority climate-health issues
- Adapt existing equity-informed public health tools (e.g., health and equity impact assessments) to assess the health impacts and potential maladaptive outcomes from climate action
Build climate-resilient public health systems and workforce
Public health systems need dedicated mechanisms to expertly lead climate-health action. This too requires meaningful and enduring collaboration among key partners, including First Nations, Inuit, and Métis communities, and other communities at high risk of displacement or negative health outcomes. Shared governance and accountability structures should also recognize and include youth leadership, as the burden of climate change will disproportionately fall on younger generations.
Dedicated, sustainable, and sufficient funding is required to adequately support climate-health action, keeping pace with the scale of emerging climate risks to health and well-being. For too long this work has been done off the sides of people's desks. These resources need to be prioritized as part of overall government efforts on climate change and to support self-determined actions that drive local community solutions.
For public health professionals to successfully develop, implement, and scale innovative climate-health action alongside partners, they need the right expertise and ongoing resources. Our current workforce is still stretched thin from the intensive COVID-19 response. To do the work that needs to be done, public health systems must build on their foundational expertise in health protection and promotion, including long-standing skills in environmental health, to strengthen its knowledge base and tools to be applied to climate-health connections. Public health systems must continue to build meaningful, healing, and cooperative relationships that put cultural respect and safety first.
Climate leadership also means leading by example and actively working towards carbon-neutral and resilient public health systems that promote health and well-being for all.
Actionable priorities to build climate-resilient public health systems and workforce
- Establish new and sustainable interdisciplinary mechanisms (e.g., hubs or observatories) for dedicated public health attention to climate change that prioritize evidence-to-action and shared governance and accountability structures
- Advocate for appropriate levels of health adaptation funding and public health human resources, with a particular focus on supporting local and Indigenous public health systems to address place-based adaptation priorities
- Strengthen the technical and professional capacity of public health professionals to work on climate-health action, such as updating public health core competencies and designing public health training to include climate change
- Reduce the carbon footprint of public health systems in Canada, including assessing the environmental impact of public health operations
We are now at a pivotal moment in history. As public health systems in Canada, we must build on our strengths and draw on lessons learned from the COVID-19 pandemic to better prepare for and respond to the climate crisis. Already, there is promising work happening across Canada to address the health impacts of climate change. We must leverage this work to strengthen our capacities, advance our knowledge, and maximize our collective efforts across systems, jurisdictions, and sectors. We must also work with communities to make sure the actions we take work for all people, wherever they live.
The time to act is now and we must act boldly - for the benefit of our health, that of our planet, and future generations.
Appendix A: Essential public health functions and public health climate action
First developed for Canada in 2003 in the wake of SARS, the essential public health functions categorize the key activities of public health systems.Footnote 251Footnote 252 While these functions are presented as separate categories, they are interconnected and used together to protect and promote health. The following describes some examples of how public health activities can begin to address climate change according to each function.
Health promotion means working collaboratively with communities and other sectors to understand and improve health through healthy public policy, community-based interventions, public participation, and advocacy or action on determinants of health.
Examples of public health activities related to climate change:
- Advocacy to address the determinants of health that impact climate vulnerability (e.g., affordable housing).
- Policy research for intersectoral action (e.g., health co-benefits of investments in public transit).
- Leadership for healthy built environments (e.g., greening parks and playgrounds, active transport).
- Supporting First Nations, Inuit, and Métis designed and driven projects to build community capacity.
Health surveillance means collecting health data to track diseases, the health status of populations, and determinants of health trends, to promote health, prevent and reduce the impact of disease, as well as monitor health inequities.
Examples of public health activities related to climate change:
- Disease vector surveillance (e.g., mosquito or tick population monitoring).
- Disease incidence (e.g., Lyme disease, West Nile virus).
- Syndromic surveillance (e.g., heat-related illnesses in emergency departments).
- Water safety monitoring (e.g., algal blooms).
- Foodborne diseases (e.g., salmonella, campylobacter).
- Mental health surveillance (e.g., Positive Mental Health Surveillance Indicator Framework).
- Built environment monitoring (e.g., Canadian Bikeway Comfort and Safety Classification System).
Health protection means protecting the population from infectious disease, environmental threats, and unsafe food, water, and air.
Examples of public health activities related to climate change:
- Vector control (e.g., mosquitos, ticks).
- Water testing and advisories (e.g., well water testing after flooding).
- Air quality monitoring and advisories (e.g., Air Quality Health Index).
- Food safety and security (e.g., public awareness campaigns).
- Public education programs about climate risks.
Population health assessment means understanding the health of communities, specific populations, and the determinants of health to create better services and policies, as well as research to identify the most effective interventions.
Examples of public health activities related to climate change:
- Climate change and health vulnerability assessments.
- Population health intervention research to assess adaptation and mitigation interventions, including what works, for whom and in what context.
- Community- and place-based research and assessment that prioritizes other knowledge systems (e.g., Indigenous knowledges).
Disease and injury prevention means promoting safe and healthy lifestyles to prevent illness and injury, and reducing risk of infectious disease outbreaks through investigation and preventive measures.
Examples of public health activities related to climate change:
- Community-based adaptation and mitigation, including emphasis of land-based governance, practices, and activities in Indigenous communities.
- Behavioural science to encourage healthy behaviours that reduce the risk of disease or illness related to climate change (e.g., promoting the use of insect repellent and proper clothing to avoid tick-borne diseases).
- Community-led programming to promote food security and ensure access to nutritious food in a changing climate.
- Mental health programs to help address climate anxiety and stress.
Emergency prediction, preparedness, and response means planning for natural or human-made disasters to minimize serious illness and death, as well as responding to emergencies while minimizing societal disruption.
Examples of public health activities related to climate change:
- Coordination with stakeholders and leadership on health-related emergency preparedness and response.
- Risk assessments on potential public health impacts of natural disasters (e.g., air quality impacts from wildfires).
- Provide public health advice, services, and support to stakeholders (e.g., air quality testing, heat alert and response systems, cooling centres).
- Community outreach and information sharing during natural disasters.
- Identifying and supporting populations that may need additional considerations during an emergency (e.g., older adults).
- Shelter and other supports for populations displaced by natural disasters (e.g., evacuation of remote First Nations communities due to floods and wildfires).
- Community mental health supports for populations impacted by natural disasters and emergency responders.
Appendix B: An update on COVID-19 in Canada
Preamble
This appendix to the 2022 CPHO Annual Report serves as a brief update on key COVID-19 events in Canada to monitor and reflect on the evolution of the pandemic over the past year. It covers the time period between August 2021 and August 2022.
The SARS-CoV-2 virus will continue to circulate and evolve worldwide for the foreseeable future and new variants are expected to emerge and spread. The unpredictable nature of when and how resurgences will occur requires maintaining vigilance and a state of readiness. Canada must plan for the ongoing management of COVID-19 in the fall of 2022 and beyond.
The arrival of Omicron changed the trajectory of the pandemic
Following a Delta-variant driven fourth wave of COVID-19 infections in the fall of 2021, a new variant of concern called Omicron was first detected internationally in November 2021. All previous waves of the pandemic have been marked by distinct characteristics, but the arrival of Omicron resulted in perhaps the most noteworthy and rapid changes in the epidemiology of COVID-19 and the public health response.
Compared to the Delta variant, the initial Omicron variant BA.1 was significantly more transmissible and better able to evade both vaccine and infection-acquired immunity.Footnote 425 Waning immunity and an increase in indoor gatherings over the winter, especially over the holidays, exacerbated its spread.
Despite being associated with less severe illness compared to the Delta variant, Omicron took a substantial toll on healthcare services and the lives of people in Canada, with an increase in hospitalizations and deaths due to the unprecedented rise in the number of infections.Footnote 426 Within only 4 weeks, Omicron became the dominant variant in circulation. By January 2022, it drove daily confirmed case counts to more than 5 times the largest number reported previously. Similarly, the burden of COVID-19-related hospitalizations was twice as high as the largest earlier peak.Footnote 427
Although children and youth are at a relatively lower risk of severe outcomes compared to adults, with the emergence of Omicron, pediatric hospitalization rates exceeded historic trends (see text box "Impacts of COVID-19 in children and youth"). The third week of January 2022 had the highest number of deaths in Canada since the emergence of the virus, with 25% more deaths than would have normally been expected if there had not been a pandemic.Footnote 428 While most excess deaths can be directly attributed to COVID-19, indirect consequences of the pandemic also impacted mortality (Figure 9).
Impacts of COVID-19 in children and youth
Since January 2022, children under 5 years of age have had the highest COVID-19-related hospitalization rates in Canada of any group under 60 years of age.Footnote 429 This is likely a result of the substantial number of cases caused by the highly transmissible Omicron variant and the COVID-19 vaccine ineligibility of younger age groups for much of this period.Footnote 430Footnote 431 In addition to the risk of hospitalization, some can develop a rare but serious condition called multisystem inflammatory syndrome in children (MIS-C), also known as pediatric inflammatory multisystem syndrome (PIMS). It is estimated to affect between 0.5% and 3.1% of all children diagnosed with COVID-19.Footnote 432 Children and youth may also be susceptible to developing post COVID-19 condition (further described below).Footnote 433Footnote 434Footnote 435 This highlights the importance of ensuring all eligible people, including children, are protected with COVID-19 vaccines. However, as of August 14, 2022, less than half of children aged 5 to 11 years had completed their primary series of COVID-19 vaccines.Footnote 436
After the decline of the large initial Omicron wave, the easing of public health measures and spread of the even more transmissible BA.2 Omicron sub-variant resulted in repeated resurgences across the country over the spring and into the summer of 2022.Footnote 427 By June 2022, the COVID-19 Immunity Task Force estimated that 56% of Canadians had been infected by SARS-CoV-2, up from 5% at the start of the fourth wave in August 2021.Footnote 437
In the summer of 2022, the highly transmissible and immune-evasive BA.5 Omicron sub-variant became dominant in Canada, driving an increase in both cases and severe outcomes.Footnote 427 As a result of the unprecedented level of viral transmission, the number of hospitalizations and deaths during the first 7 months of 2022 exceeded those reported in the previous year, despite higher population immunity.Footnote 438 Close monitoring of BA.5, as well as other emerging variants that may evade existing immunity or cause severe illness, will continue to be important.
New ways of monitoring the spread of SARS-CoV-2
In the light of the rapid escalation in cases driven by the Omicron variant, public health and laboratory testing infrastructure was overwhelmed. To alleviate pressure on capacity, many jurisdictions adjusted the eligibility for PCR tests and promoted the use of at-home rapid antigen tests.Footnote 439Footnote 440 This shift to more targeted PCR testing in the winter of 2021-22, focusing on healthcare providers and populations at higher risk of severe outcomes, led to a significant underestimation of the true burden of disease in the population. It also meant that any sociodemographic data collected about reported cases were less representative of the general population. A range of other indicators and innovative solutions used to monitor spread in the community, such as viral genomics and wastewater surveillance, along with hospital and critical care use for COVID-19 patients, became increasingly important.Footnote 441
Evolution in requirements, guidance, and recommendations
The arrival of the Omicron variant altered the course of the pandemic and Canada's approach to COVID-19 management. During the initial Omicron wave, some more restrictive public health measures were re-introduced for short, defined periods to protect acute care capacity.Footnote 442 As Canada reached high levels of COVID-19 vaccination coverage and hospitalization rates declined in February 2022, many of these measures were gradually adjusted. For example, at the federal level the Government of Canada de-escalated international border measures in a phased approach, lifted vaccination requirements for domestic transportation, and developed guidance on assessing personal risk of infection to help people make informed decisions.Footnote 443Footnote 444Footnote 445 With the ongoing goal of minimizing severe COVID-19 illness and death while also minimizing societal disruption, provincial, territorial, and local public health authorities shifted to general guidance and recommendations rather than tailored public health restrictions. As population needs and healthcare capacities varied across the country, there were differences in how jurisdictions responded. They continued to monitor for signals of concern and adapted advice to changing circumstances, including recommending how people can protect themselves and others by assessing risks and adopting layers of protection.Footnote 446
Importance of pharmaceutical interventions: Vaccines and therapeutics
Expansion of COVID-19 vaccination and booster doses
In the fall of 2021, the National Advisory Committee on Immunization (NACI) issued the first recommendations on the use of a booster dose, which can help restore protection against COVID-19. While initially recommended for certain high-risk populations, the recommendation was broadened to all adults in December 2021 in response to evidence around waning immunity and the emergence of Omicron.Footnote 447 Around the same time, Health Canada also approved the first COVID-19 vaccine for use in children aged 5 to 11 years.Footnote 448
With the spread of the more immune-evasive Omicron variant, there was growing evidence that 2 doses of a COVID-19 vaccine offered less protection against infection compared to previous variants. Therefore, booster doses became especially important to increase waning antibody levels in individuals and restore protection against severe health outcomes. Between April 2022 and the end of May 2022, when Omicron variant activity was very high in Canada, unvaccinated people were an estimated 5 times more likely to be hospitalized and 7 times more likely to die, compared to people vaccinated with a booster dose of a COVID-19 vaccine.Footnote 449 This drove home the importance of keeping up to date with COVID-19 vaccinations as the foundation of protection both individually and collectively. As of August 14, 2022, 86% of the population 5 years of age and older had completed their primary series of COVID-19 vaccines and 57% of the population aged 12 years and older had received at least one additional dose.Footnote 436
In anticipation of an expected fall or winter resurgence of COVID-19 activity, in June 2022, NACI issued recommendations for a fall booster dose for those 12 years of age and older, regardless of the number of booster doses previously received. This would help restore protection against serious illness and lessen the potential strain on the health system.Footnote 450 Later in the summer of 2022, NACI issued guidance for booster doses for those aged 5 to 11 years and Health Canada authorized for the first time the use of a COVID-19 vaccine for children aged 6 months to 5 years.Footnote 433Footnote 451 The first bivalent COVID-19 vaccines, based on the spike protein of both the original strain of SARS-CoV-2 as well as the Omicron BA.1 strain, were anticipated to be approved by Health Canada on September 1, 2022.Footnote 426Footnote 452 Since these updated vaccine formulations offer more targeted protection against the Omicron variant and broader protection against known variants of concern, they were expected to be important tools for reducing the impact of future resurgences.
Advances in therapeutics for the management of COVID-19
Canada has approved the use of several monoclonal antibody therapies that prevent the SARS-CoV-2 virus from infecting cells.Footnote 453 However, the arrival of the Omicron variant rendered many of these therapeutics less effective due to mutations in the virus.Footnote 454 In January 2022, Health Canada authorized the use of Paxlovid, the first therapy in pill form that can be used at home to treat mild to moderate COVID-19, including cases caused by the Omicron variant. By preventing viral replication, Paxlovid can be critical in reducing the severity of COVID-19 in adults who are at elevated risk of progressing to serious illness.Footnote 455 Additionally, in April 2022 Health Canada approved the monoclonal antibody drug Evusheld for the prevention of COVID-19 in people who are immunocompromised or for whom COVID-19 vaccination is not recommended.Footnote 456 Treatment is not a substitute for vaccination and keeping up to date with COVID-19 vaccinations is one of the best ways to reduce the risk of severe health outcomes.
Ongoing broader consequences of COVID-19
The previous 2021 CPHO Annual Report highlighted examples that illustrated the wide-reaching consequences of the pandemic outside of the direct impacts of COVID-19 on the health of people in Canada. Figure 9 provides updates on some of the broader consequences that can affect health. This collection of evidence is not exhaustive. Understanding many of the longer-term consequences of COVID-19 on the physical and mental health and well-being of people in Canada will take more time.
Figure 9: Key updates on broader consequences of COVID-19Footnote 428Footnote 457Footnote 458Footnote 459Footnote 460Footnote 461Footnote 462Footnote 463Footnote 464Footnote 465Footnote 466Footnote 467
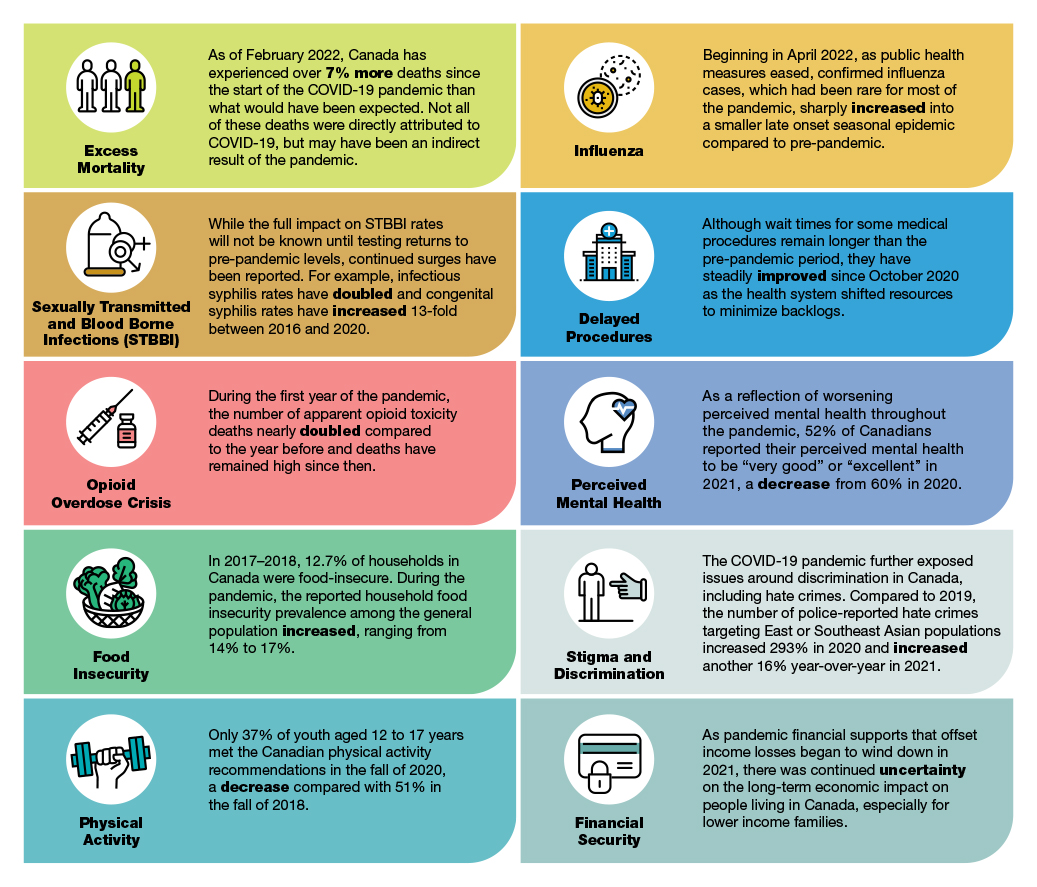
Figure 9: Text description
The figure describes some examples of broader consequences of the COVID-19 pandemic in Canada.
Excess mortality: As of February 2022, Canada has experienced over 7% more deaths since the start of the COVID-19 pandemic than what would have been expected. Not all of these deaths were directly attributed to COVID-19, but may have been an indirect result of the pandemic.
Sexually transmitted and blood borne infections (STBBIs): While the full impact on STBBI rates will not be known until testing returns to pre-pandemic levels, continued surges have been reported. For example, infectious syphilis rates have doubled and congenital syphilis rates have increased 13-fold between 2016 and 2020.
Opioid overdose crisis: During the first year of the pandemic the number of apparent opioid toxicity deaths nearly doubled compared to the year before and deaths have remained high since then.
Food insecurity: In 2017-2018, 12.7% of households in Canada were food-insecure. During the pandemic, the reported household food insecurity prevalence among the general population increased, ranging from 14% to 17%.
Physical activity: Only 37% of youth aged 12 to 17 years met the Canadian physical activity recommendations in the fall of 2020, a decrease compared with 51% in the fall of 2018.
Influenza: Beginning in April 2022, as public health measures eased, confirmed influenza cases, which had been rare for most of the pandemic, sharply increased into a smaller late onset seasonal epidemic compared to pre-pandemic.
Delayed procedures: Although wait times for some medical procedures remain longer than the pre-pandemic period, they have steadily improved since October 2020 as the health system shifted resources to minimize backlogs.
Perceived mental health: As a reflection of worsening perceived mental health throughout the pandemic, 52% of Canadians reported their perceived mental health to be "very good" or "excellent" in 2021, a decrease from 60% in 2020.
Stigma and discrimination: The COVID-19 pandemic further exposed issues around discrimination in Canada, including hate crimes. Compared to 2019, the number of police-reported hate crimes targeting East or Southeast Asian populations increased 293% in 2020 and increased another 16% year-over-year in 2021.
Financial security: As pandemic financial supports that offset income losses began to wind down in 2021, there was continued uncertainty on the long-term economic impact on people living in Canada, especially for lower income families.
Evidence continued to accumulate that the pandemic has further worsened many of the structural and systemic factors that contribute to health inequities. Certain groups, such as Indigenous Peoples, communities that are racialized, women, people living with lower income, and people experiencing homelessness were disproportionately affected by both the direct and indirect consequences of the pandemic, as were people living with disabilities, who use substances, who are incarcerated, and LGTBQ2S+ communities.Footnote 468Footnote 469Footnote 470Footnote 471 For instance, COVID-19 mortality rates were significantly higher for those living in large urban centres, apartments, areas with lower income, and areas with higher levels of ethno-cultural composition.Footnote 469 As called for in previous CPHO reports, addressing structural inequities needs to continually be at the centre of our efforts moving forward.
The impact of post COVID-19 condition on individuals and communities is likely to be substantial
Post COVID-19 condition, also known as long COVID, refers to new or ongoing physical or psychological symptoms that occur 12 weeks or more after an initial infection with SARS-CoV-2.Footnote 472Footnote 473Footnote 474 Individuals experiencing post COVID-19 condition have reported a wide range of different symptoms including fatigue, memory problems, sleep disturbances, shortness of breath, anxiety, and depression.Footnote 472 These may persist long after an initial COVID-19 infection. For example, a study in the United Kingdom estimated that 43% of people with post COVID-19 condition reported having had COVID-19 for the first time at least one year prior.Footnote 475
Based on a review of global evidence, it was estimated that between 30% and 40% of people who were not hospitalized for their initial COVID-19 infection still reported symptoms beyond 12 weeks.Footnote 472 While these studies predated the emergence of Omicron, preliminary evidence suggested that the Omicron variant may be associated with a lower risk of post COVID-19 condition compared to the Delta variant.Footnote 476Footnote 477 Emerging research also suggested that post COVID-19 condition was more likely among females and those who had a more severe initial infection.Footnote 478 In addition, each additional reinfection may increase the risk of developing the condition.Footnote 479 While anyone can develop post COVID-19 condition, vaccination with 2 or more doses of COVID-19 vaccines prior to infection may help reduce the risk.Footnote 472Footnote 480
Available evidence indicated that the medical, social, and economic impacts of post COVID-19 condition are substantial and further stress an already overburdened healthcare system. Affected individuals can experience difficulties accessing care and commonly report negative impacts to their mental health and everyday functioning, including schooling and employment.Footnote 472Footnote 481 This may lead to an economic burden at the population level as post COVID-19 condition affects overall participation in the labour market.Footnote 482 Given the number of COVID-19 cases among healthcare workers, this also has implications for the ability of the healthcare workforce to maintain levels of care.Footnote 483
As of August 2022, there were limited data to fully understand the prevalence and severity of post COVID-19 condition in Canada. However, work is ongoing to develop evidence-based guidelines for the prevention, identification, and management of post COVID-19 condition that are adapted to the Canadian context. For instance, in April 2022, Statistics Canada, Public Health Agency of Canada, and the COVID-19 Immunity Task Force launched a second cycle of the population-based Canadian COVID-19 Antibody and Health Survey to estimate the percentage of adults in Canada who are living with post COVID-19 condition and collect information on symptoms and risk factors.Footnote 484 Although there is no universally agreed upon approach for diagnosis and treatment, many specialized care centres have been established across Canada.Footnote 485
Canada's public health response has helped to minimize COVID-19 harms
Canada's public health response and collective action of people across the country has helped minimize harms since the beginning of the pandemic. At the time of drafting this report in August 2022, Canada had one of the highest 2-dose COVID-19 vaccination rates in the world, but more needed to be done to increase booster uptake.Footnote 486 Vaccination, combined with other public health measures, was estimated to have saved hundreds of thousands of lives in Canada alone.Footnote 449 Without the combination of vaccination and other public health measures, it was estimated that Canada could have experienced 13 times as many total hospitalizations, and 20 times as many total deaths by April 2022.Footnote 487
Although life expectancy in Canada dropped by 7 months in 2020 due to the pandemic, this was a smaller decrease compared to other countries.Footnote 488Footnote 489 For example, life expectancy declined by 1.8 years in the USA in 2020.Footnote 490 Additionally, Canada's COVID-19 death rate for the first 2 years of the pandemic was the second lowest among G10 countries, further illustrating the overall effectiveness of our societal response.Footnote 491
Preparedness and prevention can better equip us to manage COVID-19 moving forward
The emergence of the Omicron variant demonstrated that our health systems must be well-equipped to adapt and respond to the virus moving forward. The reality is that COVID-19 will be with us for the foreseeable future and that progress will not be linear. With waning immunity, the evolution of highly immune-evasive variants, and the easing of public health measures, there may be gaps in our collective protection. Our challenge is to sustain the incredible gains we have made, while not losing sight of the continuing threat of COVID-19 to our health and well-being. We have a shared responsibility, including among individuals and across governments and sectors, to maintain a state of readiness, address long-standing inequities, and move toward a long-term approach to COVID-19 management.
At the individual level, preparedness is best achieved by keeping COVID-19 vaccinations up-to-date and layering personal protective practices like wearing a well-fitted and well-constructed face mask, avoiding crowding, and staying home if experiencing symptoms or testing positive for the virus. At the societal level, ongoing management includes supporting optimal ventilation in public and institutional settings, investing in vaccine technologies that can broaden protection, and strengthening surveillance tools for monitoring the spread and evolution of the virus. Countering misinformation and disinformation while building trust in public health systems are also foundational to the ongoing COVID-19 response.
In addition to preparing for ongoing and future resurgences, healthcare systems continue to face capacity issues. For example, organizations representing nurses and physicians have expressed urgency to address staff shortages and burnout exacerbated by the pandemic.Footnote 492Footnote 493
Public health systems will also need to rise to meet other challenges, such as the needs of an aging population, the return and emergence of other infectious diseases (e.g., influenza and monkeypox), the ongoing opioid overdose crisis, and the health impacts of climate change.
A robust and resilient public health system can protect healthcare systems by reducing the need for medical treatments, and helping people stay healthy and well. We need strong healthcare and public health systems to prepare for and respond to present and future health threats.Footnote 446
Appendix C: Methodology
Process
The 2022 Chief Public Health Officer of Canada (CPHO) Annual Report was drafted based on a review of the best available evidence, including academic research, guidance from expert advisors, and engagement with climate change, public health, and Indigenous experts. Where possible, Canadian research and representative data were prioritized. Existing evidence reviews, such as the Intergovernmental Panel on Climate Change (IPCC) reports and the Health of Canadians in a Changing Climate report, were also prioritized.
The evidence was identified through:
Epidemiological data
- Information published or shared by the Public Health Agency of Canada (PHAC), Statistics Canada, and other federal, provincial, territorial, or municipal government sources
- Rapid review initiatives across Canada such as the COVID-19 Evidence Network to Support Decision-Making (COVID-END), CanCOVID, and the National Collaborating Centre for Methods and Tools evidence platform
- Grey literature and policy reviews of trusted sources, such as health organizations (e.g., World Health Organization, Canadian Institute for Health Information) and government publications (e.g., Public Health Ontario)
- Press briefings by health authorities and media statements where necessary
Research reviews
- An annotated bibliography commissioned by the Office of the CPHO (OCPHO) and led by Dr. Sherilee Harper at the Climate Change & Global Health Research Group at the University of Alberta. The process for this annotated bibliography included a review of literature published between 2013 and 2021 in English or in French, found through:
- A search of 5 electronic databases: MEDLINE via Ovid, CINAHL, Web of Science, Scopus, and Embase via Ovid. The search string consisted of terms related 3 main components: human/population health, climate change, and location
- A hand search of the following journals: Environmental Health Perspectives, The Lancet, Climatic Change, the Canadian Journal of Public Health, and the American Journal of Public Health
- A search of the database associated with Global Adaptation Mapping Initiative (GAMI), with a focus on potentially relevant literature from Canada, the United States, the United Kingdom, and Australia
- Examination of the reference lists of relevant sections of major climate and health publications, such as the IPCC Sixth Assessment Report Working Group II (Chapter 7 Health, Wellbeing, and the Changing Structure of Communities, and Chapter 14 North America), and the 2022 Inter-American Network of Academies of Science (IANAS) report Taking Action Against Climate Change Will Benefit Health and Advance Health Equity in the Americas
- A search of the Canadian government documents by programmable Google search engine to identify relevant government publications
- A gray literature search using a systematic Google search using the search string for the peer-reviewed literature with additional fields to capture a specific organization; the organizations included in the search were the World Health Organization (WHO), Health Canada, and PHAC
- Ongoing and frequent literature searches completed by OCPHO, completed by sub-topic, using online databases such as Medline and Scopus, as well as identifying new and existing research maintained by various academic publishers, such as the British Medical Journal, The Lancet, and Elsevier
- Grey literature review by OCPHO, including an examination of key international efforts to explore the role of public health in climate change, including the WHO's initiatives to build climate-resilient health systems and the Pan American Health Organization's (PAHO) 2022 publication on new essential environmental public health functions.Footnote 243Footnote 494
Public health reports and other grey literature
- Ongoing and frequent literature searches completed by OCPHO to find grey literature and public health reports from trusted sources, such as: public health organizations (e.g., World Health Organization, PAHO), climate researchers (e.g., IPCC) and government publications (e.g., federal, provincial, and municipal governments)
- Collaboration with relevant National Collaborating Centres for Public Health, including the National Collaborating Centre for Indigenous Health, the National Collaborating Centre for Infectious Diseases, the National Collaborating Centre for Healthy Public Policy, and the National Collaborating Centre for Environmental Health, which provided expert content on key topics featured throughout the report
- Identification of applied public health examples in collaboration with CPHO expert advisors
Discussion groups and key informant interviews
- A targeted qualitative research and engagement process, commissioned by OCPHO and led by Dr. Heather Castleden at the University of Victoria, resulting in a What We Heard report entitled Intersectional Perspectives on Climate Change and Public Health in Canada
- The research and report focuses on the current contributions of public health systems concerning climate change adaptation and mitigation, examining the potential roles for the public health system in climate change adaptation and mitigation, and identifying how public health systems need to be strengthened to undertake this work
- The engagement process included:
- Two focus groups completed with Medical Officers of Health recruited through the Urban Public Health Network
- Interviews with 21 key experts from across the country; participants were recruited from the climate/environment sector and the public health related sector, including those from non-governmental organizations, research institutions, and public health organizations; participant selection also focused on intersectional criteria (e.g., Indigenous/distinction-based, racialized communities, youth, LGBTQ2S+, people living with disabilities, minority language communities, migrants) as well as geographical representation (e.g., rural/remote northern, rural/remote other, urban, coastal)
Limitations
Scope and literature search
The 2022 CPHO Annual Report explores the health impacts of climate change and the potential role of public health systems in climate action. Both are vast topics with considerable breadth and depth across a variety of academic and professional disciplines. Since the purpose of the report is to provide an overview of presented topics and concepts, there are necessary restrictions on the level of detail provided in each section. Therefore, the report does not represent an exhaustive evidence review, but rather a summary of select key literature. Only literature published in English and French was reviewed. A detailed assessment of study quality and risk of bias was not conducted in this review.
Language
To the extent possible, we attempted to use standardized, inclusive, and culturally appropriate language when drawing on evidence related to different communities and their experiences of health. However, in some instances we relied on the terminology included in the source documents (e.g., visible minorities), if appropriate alternative language could not be identified.
Acknowledgements
Many people and organizations contributed to the development of this report.
I would like to express my gratitude to the Annual Report advisors who provided invaluable advice, strategic guidance, and expertise:
- Dr. Marcos Espinal, Assistant Director, Pan American Health Organization (PAHO)
- Dr. Sherilee Harper, Canada Research Chair in Climate Change and Health and Associate Professor, University of Alberta
- Dr. Deborah McGregor, Associate Professor and Canada Research Chair in Indigenous Environmental Justice at Osgoode Hall Law School
- Dr. Cory Neudorf, Professor, Department of Community Health and Epidemiology, College of Medicine, University of Saskatchewan and interim Senior Medical Health Officer, Saskatchewan Health Authority
- Kim Perrotta, MHSc, Executive Director, Canadian Health Association for Sustainability and Equity (CHASE)
My deep appreciation to experts from across Canada, including researchers, public health practitioners, non-governmental public health organization leaders, municipal-to-federal government public health system employees, community leaders, and medical practitioners, who participated in interviews and discussion groups. Your insights helped inform my report on the role that public health systems can play in taking action on the health impacts of climate change.
I would like to thank the National Collaborating Centres (NCC) for Public Health for their support. I would also like to acknowledge the staff from the NCC for Indigenous Health, NCC for Healthy Public Policy, NCC for Environmental Health, and NCC for Infectious Diseases for their input and contributions to the report. In addition, I want to extend my thanks to those at PAHO who provided thoughtful feedback.
Thank you to the many colleagues at the Public Health Agency of Canada, Health Canada, Indigenous Services Canada, Crown-Indigenous Relations and Northern Affairs Canada, and Environment and Climate Change Canada who provided insights and guidance throughout the development of the report, and for their critical review of report drafts.
Finally, I am grateful for the work of my office members who came together to support the development of this report. Special thanks to the Reports team for their commitment and dedication in seeing this report from conception to publication: Tammy Bell, Fabienne Boursiquot, Dr. Marie Chia, Dr. Charlene Cook, Dr. Sarah Drohan, Elyse Fortier, Rhonda Fraser, Dr. Kimberly Gray, Dr. David Grote, Holly Lake, Jessica Lepage, Danielle Noble, Kelly Kavanagh Salmond, Kelsey Seal, and Inès Zombré.