For immunization providers: Interim national vaccine storage, handling and transportation guidelines for ultra-low temperature and frozen temperature COVID-19 vaccines
Posted April 14, 2021
On this page
- About this document
- List of acronyms used
- Part 1: Ultra-low temperature vaccine(s)
- Part 2: Frozen temperature vaccine(s)
- Part 3: General guidelines
- List of references and resources for additional information
- Acknowledgments
- Contact us
About this document
The objective of the Interim National Vaccine Storage, Handling and Transportation Guidelines for Ultra-Low Temperature and Frozen Temperature COVID-19 Vaccines – 2021 is to supplement and update the guidance for storage, handling and transportation of ultra-low temperature and frozen temperature COVID-19 vaccines for immunization providers in Canada.
Vaccines must be stored in specific temperature conditions and handled with extreme care in order to maximize their shelf life, and to ensure their potency and efficacy. Specific guidelines for vaccine storage and handling procedures may vary among public health offices and immunization programs, therefore this document is meant to supplement existing jurisdictional policies and manufacturer instructions rather than to replace them. This document does not replace the National Vaccine Storage and Handling Guidelines for Immunization Providers – 2015 and as such, the 2015 guidelines takes precedence over this policy document in the event that clarity is needed on any related subject. Individuals and companies that hold an establishment license from Health Canada who access information from these guidelines are still expected to meet all applicable requirements of the Food and Drugs Act and Food and Drug Regulations (FDR) as this document does not replace the requirements under the FDR as outlined in the Good Manufacturing Practices Guide for Drug Products (GUI-0001) .
Key assumptions informing these guidelines
The information provided in these guidelines are based on the following assumptions:
- The recommendations for storage, handling and transportation of the Health Canada authorized ultra-low temperature and frozen temperature COVID-19 vaccines is informed by stability, temperature and other studies carried out by the manufacturers at the time the version of the guidelines was issued.
- These guidelines will be updated periodically as additional evidence, experience and knowledge of vaccine storage, handling and transportation practices for the authorized ultra-low temperature and frozen temperature COVID-19 vaccines become available.
List of acronyms used
- CCE
- Cold Chain Equipment
- CSA
- Canadian Standards Association
- E2E
- End-to-End
- EOC
- Emergency Operations Center
- EPS
- Expanded Polystyrene
- FPTs
- Federal, Provinces and Territories
- IR
- Infrared
- IQ
- Installation Qualification
- ISCFootnote 1
- Intelligent Supply Chain
- LMIS
- Logistics Management Information System
- LSPs
- Logistics Service Providers (note: in some jurisdictions, referred to as 3LP for Third Party Logistics Provider)
- NOC
- National Operations Center
- OQ
- Operational Qualification
- PCM
- Phase Change Material
- PHAC
- Public Health Agency of Canada
- POD
- Points of Distribution
- PPE
- Personal protective equipment
- PQ
- Performance Qualification
- P/Ts or PTs
- Provinces and Territories
- UCC
- Ultra-Cold Chain
- ULT
- Ultra-Low Temperature
- VDS
- Vaccine delivery site
- WICs
- Walk-In Cold Rooms
- WIFs
- Walk-In Freezer Rooms
Part 1: Ultra-low temperature vaccine(s)
The information provided below are general guidelines for the management of ultra-low temperature COVID-19 vaccines. Detailed instructions for storage, handling and transportation processes of authorized ultra-low temperature COVID-19 vaccine products in Canada (PDF) can be found on the manufacturer’s website and supersedes any information captured below.
Storage of ultra-low temperature COVID-19 vaccine(s)
Storing conditions
The storage conditions of the product have been specified by the manufacturer, including minimum and maximum temperature conditions for the safe storage of the product based on clinical and stability studies data provided by the manufacturer.
Storage equipment
Ultra-low temperature COVID-19 vaccines must be stored in appropriate cold chain equipment (CCE) that can maintain its ultra-low temperature. The manufacturer will indicate whether its vaccine(s) can be stored in the active CCEFootnote 2 and/or passive CCEFootnote 3 described below.
Ultra-low temperature (ULT) freezers
Technology features: ULT freezers are active CCE that produce ultra-low temperatures to store vaccines requiring ultra-cold chain, with temperature requirement ranging from -80°C to -60°C. ULT freezers must be maintained at the temperature requirement of the particular vaccine provided by the manufacturer. Vials are stable at -80ºC to -60ºC until the expiration date on the vial and tray (6 months after manufacture). In addition to storing vaccines, ULT freezers can be used to freeze ultra-cold freezer packs (also known as phase change materials) to -80°C.
Power requirements: A reliable power supply is needed for optimal functionality of ULT freezers. If the building where the ULT freezer is kept provides less than the rated voltage, power voltage boosters may be required, depending on the type of ULT freezer. A back-up source of power supply is recommended, particularly if the building where the freezer will be stored is in an area with frequent power outages. A locking plug or a metal cage to prevent the freezer from being accidently unplugged from the electrical outlet/wall socket. All ULT freezers cause additional heat load and must be installed in an air-conditioned room to ensure working ambient temperature of <30°C.
Temperature monitoring: All ULT freezers should have data loggers to automate cold chain tracking. Data loggers for ULT freezers should have a data recording period of not less than 30 days at a data rate of not less than one data point per half hour. The data loggers should also have not less than 30 days of battery life and must have an integrated USB port for uploading data. It is also important that the computer requirements for uploading USB data is met.

Copyright: Fisher Scientific; PHC Corporation of North America; Sensitech
Figure 1 - Text description
Left to right: An ultra-low temperature standing freezer, an ultra-low temperature chest freezer, a data logger shown at multiple angles, and a data logger connected with USB port.
Thermal shippers
In the absence of ULT freezers, a thermal shipper/container can be used as passive CCE to store the vaccine temporarily at the clinic or vaccine delivery site. Thermal shippers require dry ice and maintain a temperature range of -90°C to -60°C. Thermal shippers have a capacity range of 3.4 to 6.2 liters and come with a vial rack system and a temperature data logger. In the event that thermal shipper does not contain a temperature data logger, arrangement should be made for the provision of data loggers to ensure proper monitoring of the cold chain. The duration and conditions for the use of thermal shippers as temporary storage for ultra-low temperature vaccines are available and can be obtained from the manufacturer.
Active refrigerated devices
The manufacturer of ultra-low temperature COVID-19 vaccines will provide guidance on scenarios where their product can be stored in refrigerators as well as the specific duration and temperature of storage. In the event that refrigerators will be required, it is important to know the specific features of the device that can affect the storage of vaccines. For this reason, guidance has been provided on the refrigerators that are acceptable for vaccine storage and those that are not on pages 26-30 of the National Vaccine Storage and Handling Guidelines for Immunization Providers – 2015. Some refrigerators come as a fridge/freezer combination to enable the storage of different vaccines at their appropriate temperatures. The fridge compartment should maintain temperatures between 2°C and 8°C for vaccine storage, and it is advisable for fridges to be set at the temperature mid-range of about 5°C to provide the best safety margin for temperature fluctuations. A digital data logger should also be placed in each refrigerated device for continuous monitoring of the cold chain’s temperature. Refer to pages 24-35 of the National Vaccine Storage and Handling Guidelines for Immunization Providers – 2015 for more information on refrigerators.
Handling of ultra-low temperature COVID-19 vaccine(s)
Personal protection measures for handling dry ice
It is important that appropriate protection is provided to personnel at vaccine delivery sites who will be handling dry ice. Jurisdictional occupational health and safety requirements, MSDSFootnote 4 and federal laws on workplace safety should be referred to for information on potential hazards and how to work safely with dry ice. In the absence of an existing jurisdictional guidance, the requirements for safe handling of dry ice for individual protection are provided below:
Eye/face protection: Safety eyewear complying with current CSA standard Z94.3 should be used when a risk assessment indicates this is necessary to avoid exposure to liquid splashes, mists, gases or dusts. If contact is possible, safety glasses with side-shields or face shields should be worn, unless the assessment indicates a higher degree of protection is required.
Hand protection: Chemical-resistant, impervious and insulated gloves complying with jurisdictional standards should be worn at all times when handling dry ice. Gloves can be leather or nitrile, with fabric liner and cuffs. Ice scoops can also be used together with gloves to further prevent unintentional direct contact of dry ice with bare hands.
Body protection: Personal protective equipment (PPE) for the body such as aprons, or other similar PPE that meet jurisdictional standards, should be selected based on the task being performed and the risks involved before handling dry ice and related product, when a risk assessment indicates this is necessary. Apron, or other similar PPE, can be leather or canvas-type fabric.
Hygiene measures: Hands, forearms and face must be washed after handling dry ice, before eating, smoking, using the lavatory, and at the end of the working period.
Health and safety considerations: Dry ice must be handled in a well-ventilated area with ease of access to first aid kits.

Copyright: Fisher Scientific
Figure 2 - Text description
Left to right: A face shield with an apron and gloves, tongs, and a scoop for dry ice handling.
Disposal of used multi-dose vaccine vials/vial trays
Vials should be discarded in biomedical waste containers and in compliance with jurisdictional protocols. Vaccine vials should not be disposed of in sharps containers as vials are not considered a sharp and also because, sharps containers are not meant to store/have liquids. Therefore, vials containing vaccines should not be put in sharps containers or else they can leak if they are broken in the sharps container. Unlike the biomedical waste pails which are leak proof the sharps containers are not. Store empty COVID-19 vaccine vials in white and/or blue biomedical waste containers until they are ready for disposal. Incinerate the white and/or blue pharmaceutical waste containers. Do not autoclave and dispose of them in landfills since this poses a security risk for counterfeiting operations. Discard vial trays and all packaging associated with the vaccine so they cannot be reused and to prevent counterfeit efforts and any other potential criminal activities. Refer to jurisdictional and manufacturer instructions for more guidance on the disposal of ultra-low temperature COVID-19 vaccine.
Transporting ultra-low temperature COVID-19 vaccine(s)
Ultra-low temperature COVID-19 vaccine(s) can be transported either ultra-frozen or thawed at refrigerator temperature for transport. Vaccine may be removed from a ULT freezer in a frozen state to thaw while in transport – however, the vaccine is considered to be “thawed” for the purpose of transportation guidelines and allowed storage time limits. When in the thawed state, the vaccine is susceptible to interfacial stresses and as such, it is important that it is handled with care and protected as much as possible from shocks, drops, vibration, etc. Portable vaccine refrigerator and freezer units that have built-in temperature regulation are considered the best options for vaccine transport. Expedited transportation service with an insulated container containing dry ice (for ultra-cold transport) / gel packs (for 2°C to 8°C transport) is required to ensure the vaccine is kept at the right temperature. Temperature tracking logs/devices should be put in place for full trays and separate vials during transfer activities, pack-out, repacking and redistribution. Detailed instructions for transportation of ultra-low temperature COVID-19 vaccine(s) in frozen or refrigerated state, including timing, is available and can be obtained from the manufacturer. Also refer to jurisdictional guidance, if available.
Part 2: Frozen temperature vaccine(s)
The information provided below are general guidelines for the management of frozen temperature COVID-19 vaccines. Detailed instructions for storage, handling and transportation processes of authorized frozen temperature COVID-19 vaccine products in Canada can be found on the manufacturer’s website and supersedes any information captured below.
Storage of frozen temperature COVID-19 vaccine(s)
Storing conditions
The storage conditions of the product have been specified by the manufacturer, including minimum and maximum temperature conditions for the safe storage of the product based on clinical and stability studies data provided by the manufacturer.
Storage equipment
Frozen temperature COVID-19 vaccines must be stored in appropriate cold chain equipment (CCE) that can ensure maintenance of the vaccine cold chain. Frozen temperature COVID-19 vaccines can be stored in active and passive CCE; these types of equipment and when they should be used are described below.
Stand-up freezers
Stand-up freezers are active CCE that can be used to store frozen temperature COVID-19 vaccines. They must be maintained at a temperature of –15°C or colder, depending on the temperature requirement of the particular frozen vaccine provided by the manufacturer. Many stand-up freezers come with a chart logger that contains spare charts and ink. A digital data logger must also be placed in each freezer for continuous monitoring of the cold chain’s temperature. The temperature in newly installed or newly repaired freezer unit may take 2 to 5 days to stabilize within the recommended range of –15°C or colder. Therefore, 2 to 5 days of twice daily freezer temperature recordings must be carried out before using the unit to store vaccines or as stipulated in jurisdictional guidance or recommended by the manufacturer. Freezer validation (installation qualification – IQFootnote 5, operational qualification – OQFootnote 6 and performance qualification – PQFootnote 7) is required when/where the freezer location is subject to good manufacturer practices regulations. Refer to pages 31-35 of the National Vaccine Storage and Handling Guidelines for Immunization Providers – 2015 for more information on freezers.

Copyright: ThermoFisher Scientific
Figure 3 - Text description
Left to right: A stand-up freezer, closed and open.
Qualified transport containers
The frozen temperature COVID-19 vaccine can be transported in its frozen state using conditioned insulated containers that are qualified to maintain the vaccine at -18°C or colder for at least the duration of the intended transportation specified by the manufacturer(s) of the container. Molded expanded polystyrene (EPS) foam shippers, or hard plastic vacuum insulated shippers are qualified to hold the vaccine in the appropriate condition during transportation. The transport containers must be secured (strapped/braced) when being transported to prevent unnecessary movement. The container must be labeled prominently with “Fragile: Handle with Care, Do Not Drop” cautionary statements. A frozen digital data logger and an infrared thermometer (IR) should be placed in each qualified transport container for monitoring the temperature of the cold chain.
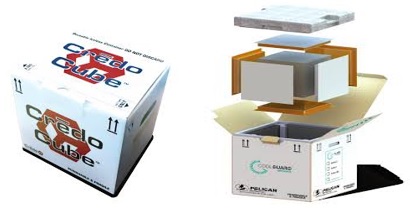
Copyright: Pelican Biothermal
Figure 4 - Text description
Left to right: A qualified transport container for frozen state transportation, put together and in pieces.
Active refrigerated devices
Frozen temperature COVID-19 vaccine while thawing, or after being thawed to refrigerator temperature, can be stored in a refrigerator qualified to maintain the vaccine at 2°C to 8°C for up to 30 days. It is advisable for refrigerators to be set at the temperature mid-range of about 5°C to provide the best safety margin for temperature fluctuations. Different refrigerators will have specific features that can affect the storage of vaccines. Refer to page 27 of the National Vaccine Storage and Handling Guidelines for Immunization Providers – 2015 for a list of refrigerators that are appropriate for use and pages 24-30 of the same document for more information about refrigerators.
Walk-in cold and freezer rooms
Walk-In Cold Rooms (WIC) and Walk-In Freezer Rooms (WIF) are refrigerated enclosures accessible via at least one door and large enough for a person to walk into, housed within existing buildings. Frozen temperature COVID-19 vaccines can be stored in WICs when thawed and during thawing and in WIFs in its frozen state per the temperature specifications of the vaccine manufacturer. WICs and WIFs are an important storage point in the temperature-controlled supply chain and usually used at the central depots at federal or provincial/territorial levels. The specifications listed in the table below are standard requirements for WICs and WIFFootnote 8:
| Specification | Requirement |
|---|---|
| Thermostat | Thermostat must be calibrated to ITS-90 (International Temperature Scale) and should be accurate to +/- 0.5°C |
| Hold-over time | The stated hold-over time (Temperature must remain above +2°C for cold climate zones, below +10°C for hot and temperate zones for WIC, and must not rise above -10°C for WIF) for at least 8 hours for both WIC and WIF |
| Lighting | Lighting must be internal ceiling mounted tungsten filament light fitting or LED with external switch and pilot light (fluorescent lighting must not be used) |
| Gas | CFC Free refrigerant gas must be used |
| Compressors | All compressors to be fitted with hour meter to record the running duration for each unit |
Types of WICs and WIFs: There are two distinct WICs and WIFs models:
1. Plug-in model
A plug-in product has the controls, the compressor, the condenser and the evaporator as a complete unit, assembled and ready for installation. Each WIC/WIF is supplied with two complete plug-in refrigeration units to provide 100 per cent stand-by cooling. These are hung on the prefabricated panel walls of the WIC/WIF, or mounted on the ceiling panels.
2. Split-unit model
Unlike the Plug-in refrigeration units, the split unit refrigeration model consists of two main parts: the condensing component for installation outside the room where the WIC/WIF is installed, and the evaporator component installed inside the room. At the site of installation, these parts are linked with solid leak proof connection tubing between the evaporator and the condensing unit.
Power requirements for WICs and WIFs: The electric power supply should be maintained at least 8 hours per day for WIC/WIF to operate properly and maintain the appropriate temperature to safeguard the vaccines. Therefore, it is recommended that all central vaccine depots accommodating WICs and WIFs should be fitted with a standby generator with automatic start up, regardless of the reliability of the mains power supply. WICs and WIFs have electronic components and control systems which are susceptible to power fluctuations. Intermittent national grid power supply, as well as stand-by generators during start-up on heavy load pick-up and shut down, result in transients that contribute to system failure. This creates high surges that are detrimental to sensitive components and accessories, leading to their failure and consequently that of the WICs/WIFs. It is therefore recommended to equip WIC and WIF rooms with voltage stabilizers which only allow power to the system when pre-set conditions are met.
Temperature monitoring of WICs and WIFs: A temperature data logger with integral alarm and auto dialer is a standard requirement for WICs and WIFs. The data logger should have: a temperature sensor for specific locations within thecold/freezer room; a door-open sensor for detecting whether door is open or closed; a power failure sensor; computer to store, display and print temperature and event reports; alarm sounder triggered whenever sensor records a temperature or event excursion outside programmed alarm settings; and an auto dialer which dials pre-programmed telephone numbers or sends E mails, SMS messages in case of alarm.
Another important temperature monitoring component that should be installed in the central depots accommodating WICs and WIFs is an alarm. Alarms should be mains operated and audible with battery back-up and automatic recharge, triggered in the event of mains failure or when cold/freezer room temperatures are outside set parameters.
Prefabrication of WIC and WIF rooms: Depending on the configuration of the WIC/WIF, the door position (on the long or short wall) should be in the middle, leaving a space of 2.5 – 3 meters in front of the door wall for easy access to the room, such as handling and possible repacking of stored goods. When planning the room lay-out, please note that the side and back of the room should be installed with a minimum distance of 100 mm from the existing building wall. As a prerequisite, installation of the WIC/WIF should be done on a levelled concrete floor. As rooms are made of prefabricated insulation panels, the levelling/base evenness requirements are maximum +/- 5 mm per 5 m. The door entrance to the installation area should be at least 900 mm wide to allow access for the prefabricated panels and other components.
Handling frozen temperature COVID-19 vaccine(s)
Frozen temperature COVID-19 vaccine does not require any particular safe handling requirements other than the requirements outlined in the National Vaccine Storage and Handling Guidelines for Immunization Providers – 2015. However, if the manufacturer or local jurisdiction provides specific guidance for safe handling of frozen temperature COVID-19 vaccine, the advice contained in that document will take precedence over the National Vaccine Storage and Handling Guidelines for Immunization Providers – 2015.
Transporting frozen temperature COVID-19 vaccine(s)
Frozen temperature COVID-19 vaccine should be transported in its frozen state, which is the preference of the manufacturer, however, there are certain circumstances were frozen state transportation is not feasible. In those situations, care must be taken to appropriately transport the product in the liquid state.
Frozen state transport
Arrangements must be made by FPTs for transportation solutions to transport the vaccine(s) in its frozen state. Caution must be used to ensure that the passive CCE is within the desirable temperature range before transferring vaccine to the unit for transport – packs taken from a ULT may need to warm up to the proper temperature first. Otherwise, frozen vaccine may be exposed to temperatures that are too cold for their acceptable range. The monitoring of cold chain temperature must be carried out during transit and as such, it is important that data logging for temperature excursions be maintained. Specific instructions on the storage conditions and duration of transportation of the vaccine in this state is available and can be provided by the manufacturer. Also refer to jurisdictional guidance, if available.
Liquid state transport
In the event that frozen state transport resources are not feasible, ability to transport the thawed vaccine at 2°C to 8°C may be required. Vaccine may be removed from a freezer in a frozen state to thaw while in transport – however, the vaccine is considered to be “thawed” for the purpose of transportation guidelines and allowed storage time limits. When in the thawed state, the vaccine is susceptible to interfacial stresses and as such, it is important that it is handled with care and protected as much as possible from shocks, drops, vibration, etc. The vaccine should be transported in a qualified transport containerFootnote 9 that is secured (strapped/braced) to prevent unnecessary movement. Care must be taken to ensure that the thawed vaccine does not re-freeze in transit or on arrival at its destination. Specifically, the thawed vaccine must not come into contact with any frozen packs added to maintain temperature, and the transport container must be labeled prominently with cautionary statements pertaining to prevention of re-freezing. Portable fridge units and qualified passive long-range vaccine carriers are other options for transporting the thawed vaccine at 2°C to 8°C. Specific instructions on the storage conditions and duration of transportation of the vaccine in the thawed state is available and can be provided by the manufacturer. Also refer to jurisdictional guidance, if available.
Part 3: General guidelines
The guidelines that will be provided in this part is not specific to any vaccine and is applicable only in the absence of manufacturer and local jurisdictional advice.
Managing temperature excursions during storage
Heat or cold exposure can cause damage to COVID-19 vaccines in storage. It is important that, when they occur, the appropriate actions take place to preserve the integrity of the vaccines. When temperature excursions occur, the user at the vaccine delivery or storage site should follow the actions outlined on page 83 of the National Vaccine Storage and Handling Guidelines for Immunization Providers – 2015.
If the excursion occurred during initial delivery of vaccines to the FPTs, the user must follow jurisdictional processes to make sure the excursion is reported immediately to the national operations center (NOC) and contact the manufacturer or their designated third party agent for recommendations on the actions to be taken. Once the manufacturer has provided recommendations about the excursion, the user will carry out the advised actions needed to address the excursion including how to store the vaccines involved in the excursion incident that have been determined to be usable by the manufacturer. Local public health authorities and other designated sites must ensure proper documentation of all wastage in their respective information management system. Upon resolution of the excursion incident, the jurisdiction will report the outcome to the NOC using the format below.
Subject: FPT Delivery Temp Excursion Report
A. Date of Incident
B. VDS Location
C. Number of Doses in Question
D. Manufacturer Recommendations
E. Wastage (if any)
F. Impact on FPT
However, if the excursion did not occur during initial delivery of vaccines to the FPTs, the user will follow jurisdictional protocols on the actions to be taken until the situation is resolved. The vaccine delivery or storage site must also dispose of any unusable/wasted vaccine, based on jurisdictional guidance. Local public health authority must ensure proper documentation of all wastage in their respective information management system. Upon resolution of the excursion incident, the jurisdiction will report any wastage to the NOC using the format below.
Subject: FPT Temp Excursion Wastage Report
A. Date of Incident
B. VDS Location
C. Situation Surrounding Incident
D. Wastage
E. Impact on FPT
Jurisdictional procedure should be followed to contact the NOC through the following channels:
- email (PHAC.vaccine.NOC-CON.vaccin.ASPC@canada.ca)
- 24 hours line (1-613-952-0865)
- liaison (1-613-295-5491)
Refer to pages 82-83 of the National Vaccine Storage and Handling Guidelines for Immunization Providers – 2015 for more guidance on managing temperature excursions.
Reporting vaccine wastage
Vaccine wastage is the sum of vaccines discarded, lost, damaged or destroyed. Accurately determining the wastage rate is essential to support the management of vaccine inventory, orders and deliveries and provides better understanding of the pace of administration and consumption. Accurate wastage reporting will enable PHAC and the NOC to target specific assistance to aid vaccine storage and administration at FPTs storage and vaccine delivery sites.
Two types of vaccine wastage should be reported:
- Closed Vial Wastage (wc): This wastage is primarily due to ineffective temperature control, temperature monitoring and stock management during storage and transportation. It may result from expiry, excess heat exposure, freezing, breakage, and missing inventory or discard following outreach sessions.
- Open Vial Wastage (wo): This wastage is attributable to immunization providers’ practices and discarding of unused doses of multi-dose vials.
Users must report all wastage to their local public health authorities based on their outlined jurisdictional documentation process. FPTs will then report all COVID-19 vaccine wastage (in exact numbers) to the NOC, by vaccine manufacturer, inventory, cumulative wastage numbers and their causes in the format below:
| FPT: | ||||
| Date: | ||||
| Inventory (doses) | Closed vial wastage (doses) | Causes of closed vial wastage (percentage) | Open vial wastage (doses) | Causes of open vial wastage (percentage) |
| Vaccine A | ||||
| Vaccine B | ||||
| Sample vaccine | 1,500 | Freezing (75%); missing inventory (5%); heating (20%) | 300 | Discarding of unused multi-dose vial (100%) |
| Total | ||||
Managing vaccine storage equipment breakdown
In order to ensure that COVID-19 vaccines maintain their efficacy, it is important to address cold chain breaks when they occur. If vaccine storage equipment stops working, first protect the vaccines and then check the cause of the problem. Guidance outlined by the jurisdiction/local public health office or immunization program for protecting the vaccines and addressing the equipment problem must be followed when cold chain breaks occur. It is advised that local public health units have a storage equipment breakdown plan in place so as to ensure that vaccine that might still be viable can either be safely moved to a suitable alternate storage location (e.g. fridge) or administered to as many individuals as possible to minimize wastage, if feasible (and only once confirmed with manufacturer that unacceptable temperature excursion has not occurred). Guidance has been provided on page 81 of the National Vaccine Storage and Handling Guidelines for Immunization Providers – 2015 to support the response to cold chain breaks in the event that jurisdictional guidance is not available.
Maintenance of vaccine storage equipment
In order to protect the vaccine cold chain, regular maintenance is important as it helps to ensure optimal functionality of cold chain equipment. This ensures that vaccines will continue to be stored at the required temperatures, and also helps to extend the useful life of the CCE. Two main types of maintenance are required as described below:
Routine maintenance
Routine maintenance of CCE must be carried out at different frequencies; daily, monthly and quarterly by the end-user(s) at all levels of the cold chain. This is usually a do-it-yourself type of maintenance involving the use of simple instructional guides to complete outlined maintenance activities as scheduled. Routine maintenance also enables the identification of issues such as equipment breakdown or malfunctions that may require an expert-led repair response. Please see detailed the guidance on routine maintenance of CCE on pages 36-38 of the National Vaccine Storage and Handling Guidelines for Immunization Providers – 2015.
Planned preventive and corrective maintenance
Planned preventive maintenance of CCE involves the engagement of CCE technical expert(s) to conduct checks on CCE at specified intervals (quarterly or biannually). Corrective actions would be taken to repair any broken or malfunctioning cold chain equipment identified during these maintenance checks. Planned preventive and corrective maintenance can either be insourced or outsourced, and the decision for adopting either or both options is dependent on provincial/local preference and decision-making.
Information management system for COVID-19 vaccine
A hallmark of effective supply chains is the end-to-end (E2E) visibility of supply data, its triangulation with demand information and its use in making decisions and taking effective action. A new information management system known as VaccineConnect will be deployed to support the COVID-19 vaccine rollout in Canada. VaccineConnect encompasses three key sets of functional capabilities, including the Intelligent Supply Chain (ISC) module, which will support the NOC in terms of executing all the functions associated with managing and distributing the Government of Canada procured vaccines. This comprises transportation and distribution, warehousing and handling, inventory control, logistics information management, security, reporting, and integration with other systems.
To ensure full visibility on the tracking and aggregation of essential information, the ISC module’s capabilities will coalesce data at each stage of the distribution, including vaccine ordering, processing and approval of orders, order fulfillment, distribution of order, and end user reporting. ISC capabilities will:
- Provide the ability for provinces/territories to place orders for vaccine and the ability for PHAC to send approved orders to manufacturers and LSPs;
- Track vaccines from manufacture to points of delivery through aggregating information from multiple LSPs and their tracking systems;
- Provide supply chain management of short shelf-life vaccine products, including cold chain status, and end-to-end traceability and visibility of the demand, inventory, and distribution of the vaccines;
- Integrate or capture information inputs from the LSPs and other entities involved in vaccines supply chain from manufacturer to the points of distribution/vaccine delivery sites (VDSs); and
- Provide reporting and representative visual capabilities for pertinent aspects of the distribution system.
Developing and managing VaccineConnect is a federal responsibility to be handled by PHAC. FPTs will be responsible for integrating or inputting information into the VaccineConnect platform which will be interoperable with existing jurisdictional information management systems. FPTs can utilize the data on the VaccineConnect to make evidence-based decisions, consistent with the level of authorized access to the platform that they possess. In the event that a jurisdiction requires some functionalities of the VaccineConnect ISC module added to their information management system to aid vaccine rollout operations, PHAC should be notified by the FPT of the request. The request notification will formally initiate the definition of needs for the specific functionalities requested and the timelines for delivery to the FPTs.
Accessing COVID-19 vaccines labelling information
Some COVID-19 vaccines will come with QR codes and barcodes on the secondary and tertiary packaging containers. The QR codes are intended to provide rapid access to important vaccine information for clinics, health care workers and information management systems. The QR code contains information on real-time shelf life, heat stability and information on the vaccines’ profiles. To obtain the labelling information for the authorized frozen temperature COVID-19 vaccine, scanning the QR code located on the vial or carton will direct the user to a website that contains the information. For the only authorized ultra-low temperature COVID-19 vaccine in Canada, the Canadian-specific labelling information can be accessed by scanning the QR code on the carton label. The vial and/or carton labels include the statements “For use under Emergency Use Authorization.” The US FDA specific information (e.g., Rx only, NDC) should be disregarded as this is not relevant to the Canadian authorization.
List of references and resources for additional information
The documents below provided the materials used to develop these guidelines. They can also be accessed to provide further guidance on COVID-19 vaccines and specifically, on their storage, handling and transportation.
- Health Canada (2020) – Planning guidance for administration of COVID-19 vaccine
- Health Canada (2020) – Planning guidance for immunization clinics for COVID-19 vaccines
- PHAC (2015) – National Vaccine Storage and Handling Guidelines for Immunization Providers
- Health Canada (2020) – Coronavirus disease (COVID-19): Guidance documents
- NACI (2020) – Recommendations on the use of COVID-19 vaccines
- NACI (2020) – Guidance on the prioritization of initial doses of COVID-19 vaccine(s)
- Health Canada (2020) – Product Monograph- Pfizer-BioNTech Comirnaty COVID-19 Vaccine
- Health Canada (2020) – Pfizer-BioNTech Comirnaty COVID-19 vaccine: What you should know
- Health Canada (2020) – Authorization of Pfizer-BioNTech Comirnaty COVID-19 Vaccine with English-only Carton and Vial Labels
- Health Canada (2020) – Product Monograph- Moderna Spikevax COVID-19 Vaccine
- Health Canada (2020) – Moderna Spikevax COVID-19 vaccine: What you should know
- PHAC (2020) – COVID-19 Vaccine Comprehensive Distribution Plan (Draft V2)
- PHAC (2021) – COVID-19 Vaccination Information Resources: Tool Kit for Health Care Providers
- Health Canada (2018) – Good Manufacturing Practices Guide for Drug Products (GUI-0001)
- Health Canada (2020) – Guidelines for environmental control of drugs during storage and transportation (GUI-0069)
- Health Canada (2020) – Storage and handling of immunizing agents: Canadian Immunization Guide
- Health Canada (2020) – Repackaging, Storage and Transport Requirements for Vaccines
- Pfizer-BioNTech Comirnaty – Vaccination Storage & Dry Ice Safety Handling
- WHO (2013) – Effective Vaccine Management (EVM) Model Standard Operating Procedures: Consolidated version, with user guide
- WHO (2016) – Global Ebola Vaccine Implementation Team (GEVIT): Practical guidance on the use of Ebola vaccine in an outbreak response
- WHO (2019) – Revising global indicative wastage rates: a WHO initiative for better planning and forecasting of vaccine supply needs
- WHO/UNICEF (2020) – Guidance on developing a national deployment and vaccination plan for COVID-19 vaccines
- WHO (2020) – PQS devices catalogue: Pre-qualified equipment for the Expanded Programme on Immunization (EPI)
Acknowledgments
The Public Health Agency of Canada would like to acknowledge the work of the Vaccine Logistics Task Group, the Vaccine Supply Working Group (VSWG) of the Canadian Immunization Committee (CIC), Health Canada and staff of the Public Health Agency of Canada in developing these guidelines.
Contact us
For questions or clarification, please contact heather.deehan@canada.ca.
Footnotes
- Footnote 1
-
Please note that ISC is also commonly used to refer to Indigenous Services Canada in other documents.
- Footnote 2
-
CCE that use mechanical or electric systems, powered by an energy source, and combined with thermostatic control to maintain desired temperatures at optimal functionality.
- Footnote 3
-
CCE that do not produce cold but can maintain temperature for a limited time and are mainly used for keeping vaccines cold during transportation.
- Footnote 4
-
Material Safety Data Sheets – A document that contains information on the potential hazards of a chemical product and how to work safely with it.
- Footnote 5
-
IQ – verifies that the equipment has been properly delivered, installed and configured according to standards set by the manufacturer.
- Footnote 6
-
OQ – determines that equipment performance is consistent with the user requirement specification within the manufacturer-specified operating ranges.
- Footnote 7
-
PQ – verifies and documents that the equipment is working with reproducible results within a specific working range in simulated real-world conditions
- Footnote 8
-
WHO PQS Specifications - E001: Cold rooms, freezer rooms, and related equipment
- Footnote 9
-
Qualified transport containers are conditioned insulated containers that are qualified to maintain the vaccine at the manufacturer-approved temperature throughout the duration of the intended transportation.