Archived: Rapid risk assessment: Avian influenza A(H5N1) clade 2.3.4.4b
Download in PDF format
(852 KB, 26 pages)
Organization: Public Health Agency of Canada
Date published: 2023-07-27
Assessment completed: June 21, 2023
On this page
- Overall risk statement
- Risk assessment summary
- Future risk in Canada
- Proposed actions for public health authorities and One Health partners
- Disclaimer
- Rapid risk assessment background and methods
- Risk estimate summary
- Limitations
- Knowledge gaps
- Acknowledgements
- Appendix A: Methods
- Appendix B: Occupational and recreational groups with potentially relevant exposures
- References
Overall risk statement
The overall risk to the general population in Canada from avian influenza A(H5N1) clade 2.3.4.4b is low. Those with higher-level exposure to domestic or wild birds or wild mammals are at increased risk of infection.
For the general population in Canada with low level of exposure to birds, human infection with avian influenza A(H5N1) clade 2.3.4.4b acquired from birds (wild birds or commercial or backyard poultry) is very unlikely. For the population with higher level of exposure to birds, infection is unlikely due to the low proportion of birds infected as well as the limited capacity of the virus to infect humans. The uncertainty associated with these estimates varies widely, due to limited information on the infectivity of this clade for humans, limited surveillance and testing in human populations exposed to birds as well as backyard poultry, and gaps in information regarding backyard poultry flocks in Canada.
Infection with avian influenza A(H5N1) clade 2.3.4.4b from mammals is very unlikely for the general population with higher-level exposure to domestic mammals (e.g., dogs and cats) but lower-level exposure to wild mammals. For the population with higher-level exposure to wild mammals (e.g., wild carnivores and scavengers), infection is unlikely due to the low proportion of wild mammals infected and the limited capacity of the virus to infect humans. There is moderate to high uncertainty in these estimates due to limited surveillance and testing of mammalian species and the limited information on the infectivity of this clade for humans.
The impact on the first infected individual(s) in Canada is estimated to be major, considering the severe clinical manifestations seen in some cases globally, as well as the expected burden from control measures, such as isolation and quarantine, on affected individuals and their close contacts. Notably, early detection and prompt treatment in Canada will likely reduce disease severity. Uncertainty in this estimate is high, because of the variability in clinical presentations, ranging from asymptomatic infection to death, among the limited number of reported human detections from other countries to date.
Since there is no evidence that the virus has acquired the capacity for sustained transmission among humans, further human-to-human transmission is not expected. Therefore, the overall impact to the Canadian population would be minor, with low uncertainty.
Risk question
What is the likelihood and impact of at least one human infection with avian influenza A (H5N1) clade 2.3.4.4b due to exposure to either birds or mammals in Canada up to the end of the 2023 fall bird migratory season?
Risk assessment summary
Likelihood or impact |
Description |
Estimate |
Uncertainty |
|---|---|---|---|
Likelihood of infection from birds |
Likelihood of infection for general population with lower/negligible exposure to domestic or wild birds |
Very unlikely |
High |
Likelihood of infection for population with higher exposure to domestic or wild birds |
Unlikely |
Very low to highTable 1 footnote a |
|
Likelihood of infection from |
Likelihood of infection for general population with higher exposure to domestic mammals (e.g., dogs and cats) but negligible/lower exposure wild mammals |
Very unlikely |
Moderate to highTable 1 footnote a |
Likelihood of infection for population with higher exposure to wild mammals (e.g., wild carnivores and scavengers, as well as free-ranging cats and dogs) |
Unlikely |
Moderate to highTable 1 footnote a |
|
Impact on individuals |
Impact on infected individuals, including effects on mental health, disease morbidity/mortality, and general welfare |
Major |
High |
Impact on the population |
Overall impact on the general population given that no further spread beyond initial zoonotic infection is expected |
Minor |
Low |
Future risk in Canada
Continued transmission of avian influenza A(H5N1) clade 2.3.4.4b viruses in wild and domestic bird populations, and repeated spill-over into mammalian species, increases the likelihood of viral reassortment and/or adaptation that could enable sustained transmission in wild and/or domestic mammalian species. This may result in increased opportunities for human exposure to these viruses. Although human infections, including fatalities, have been documented in other countries among individuals with exposure to animals infected with avian influenza A(H5N1) clade 2.3.4.4b viruses and possibly virus-contaminated environments, human-to-human transmission has not been reported to date. There is high uncertainty regarding the likelihood of these viruses acquiring mutations that enable sustained human-to-human transmission. A recent multisectoral Pandemic Risk Scenario Analysis led by the Agency determined that the most likely scenario by March 2024 is sustained transmission in non-human mammals, according to majority expert opinion. Sustained human-to-human transmission leading to a pandemic was considered a scientifically credible but less likely scenario.
If sustained human-to-human transmission does occur, the human health impacts will depend on virus transmissibility (the reproduction number); the speed of transmission (epidemic doubling time); the role of asymptomatic and pre-symptomatic virus shedding in transmission; illness severity; individual, health system and societal vulnerabilities; and the effectiveness and availability of countermeasures. There is high uncertainty regarding all of these factors. The course of a human epidemic, were it to occur, is therefore highly uncertain at present, emphasizing the importance of surveillance and preparedness activities in both human and animal sectors.
Even in the absence of widespread community transmission, clusters of disease in high-risk settings such as healthcare institutions could put strain on medical and public health resources for diagnostics, medical treatment and outbreak management, and result in staff shortages through absenteeism if healthcare staff are affected.
Wider transmission in animal populations could also have indirect impacts on human wellbeing and wider society. Increasing outbreaks in farmed animals could have large-scale economic impacts in the agricultural sector from direct losses due to illness as well as outbreak containment measures and international trade implications. The wellbeing of producers and farm employees could also be affected due to animal welfare impacts, loss of livelihood, and disruption of the agricultural sector. Outbreak containment measures could also affect the wellbeing of personnel involved in outbreak response and clean-up and disposal on farms. Shortages in food animal commodities could affect food security in certain sectors of the population. Widespread virus transmission in wildlife populations could also have food security implications in Indigenous communities that rely on wildlife for food. Wildlife population numbers, particularly for at-risk or endangered species, could be impacted, and there could also be impacts on the wellbeing of personnel involved in response and clean-up of wildlife die-offs. Impacts on human wellbeing could also occur from reduced interaction with natural ecosystems, resulting from fear of exposure to infected animals.
Proposed actions for public health authorities and One Health partners
Recommendations proposed below are based on the knowledge gaps identified during this risk assessment. It is important that the public health response be proportionate to the risk, taking into consideration available public health resources and capacity.
PHAC will continue to engage One Health partners (federal, provincial, territorial and other non-government organizations) domestically and collaborate with international partners to assess public health risks associated with current and future avian influenza A strains. The recommendations proposed below are to guide public health actions in the following areas:
Surveillance and reporting
- Continue efforts to further enhance and integrate surveillance activities for avian influenza across the One Health spectrum to,
- improve understanding of infection and disease burden due to avian influenza A(H5Nx) clade 2.3.4.4b in different animal species, particularly understudied mammalian species;
- monitor changes in virus evolution and species adaptation as well as antiviral resistance;
- understand infection risk in human population groups with higher exposure (e.g., backyard poultry, agriculture workers); and
- rapidly detect and respond to a potential human infection, especially where human-to-human transmission may be occurring.
- Establish enabling mechanisms and structures between animal and human health surveillance systems in Canada for rapid information sharing of case detections, exposure data, genomic analysis including timely clade identification, and other relevant intelligence that can inform the global avian influenza knowledge base.
Communication and coordination
- Continue to foster timely coordinated communication and actively build trust among One Health stakeholders, including counterparts in human, environmental and animal health sectors at local, provincial, regional and federal levels, such that established relationships may be leveraged for harmonized inter-agency pandemic preparedness and outbreak prevention and response activities, including response planning for the first human case(s).
- Continue regular communication with the public on the current avian influenza A(H5N1) clade 2.3.4.4b and share associated guidance related to preventive measuresFootnote 1, specifically, for those at potentially higher risk of exposure and infection, including but not limited to farmers/producers and farm workers; hunters/trappers; and those who work with wildlife, stray and feral animals; etc.). When necessary, correct and counter mis- or disinformation.
Research
- Consider discussing and pursuing potential research activities as identified in the Knowledge gaps (Table 5).
Disclaimer
The qualitative and expert-opinion-based methodology is intended to be used in situations where policy decisions need to be made in the face of high uncertainty. The assessment was primarily informed by the team's collective professional knowledge on such topics as infectious diseases, virology, epidemiology, the health system, industry practices, and human-animal interactions. Where appropriate, some references have been provided, but this is not intended as a literature review. The estimates represent the consensual, but not necessarily unanimous, opinions of the participants, and should not be interpreted as representing the views of all participants and their respective organizations.
Rapid risk assessment background and methods
Event background (current situation as of May 30, 2023)
Birds
The avian influenza A(H5N1) clade 2.3.4.4b virus emerged in 2020, spreading across Europe, Asia, and Africa, in both wild birds and domestic poultry, and replaced the previously circulating avian influenza A(H5N8) clade 2.3.4.4b virus in Europe by spring 2021.
The Canadian Food Inspection Agency (CFIA)'s National Centre for Foreign Animal Diseases (NCFAD) first confirmed the avian influenza A(H5N1) clade 2.3.4.4b virus in Canada in December 2021, in a fancy chicken at a small mixed animal exhibition farm in Newfoundland and Labrador.Footnote 2 Since then, over 7 million birds from commercial and non-commercial flocks in Canada have been culled as a result of virus containment measures or have died from infection with the virus.Footnote 3
Avian influenza A(H5N1) clade 2.3.4.4b viral activity is unprecedented in terms of the number of wild bird species infected, the extensive geographic spread, and duration of the epizootic.Footnote 4 Detection of avian influenza A(H5N1) clade 2.3.4.4b viruses containing the polymerase basic protein 2 (PB2) E627K amino acid substitution, a known marker of mammalian adaptation, has been reported since April 2023 in viruses from some infected poultry farms in Canada (12 in Québec, 1 in Ontario). While this adaptation has been detected in wild birds and birds of prey previously, this is the first time PB2 has been seen in Canadian domestic poultry.Footnote 5,Footnote 6
Non-human mammals
Since October 2020, sporadic avian influenza A(H5N1) and avian influenza A(H5) infections in several wild mammalian species have been reported in Europe and the Americas affecting at least 24 species of carnivores and 4 species of cetaceans. Footnote 7 In March 2023, 10 South American bush dogs in a captive breeding program in England tested positive for avian influenza A(H5N1). All were either dead or euthanized over a 9-day period.Footnote 8 They were tested as part of a routine investigation into an unusual mammal die-off in November 2022 and had minimal clinical signs before death.Footnote 8 There was no clear evidence suggesting mammal-to-mammal transmission and it is very likely all animals were exposed to the same source of infected wild birds.Footnote 8 In Canada, wild mammal species reported to have been infected with avian influenza A(H5N1) clade 2.3.4.4b include, but are not limited to, foxes, skunks, bears, raccoons, seals and dolphins.Footnote 4 Avian influenza A(H5N1) has recently been reported in a domestic dog and in feral cats in Ontario. The dog and one cat have been confirmed infected with avian influenza A(H5N1) clade 2.3.4.4b. Additional results are pending.
In an analysis of tissue samples collected from dead or euthanized mesocarnivores in Canada between April to July in 2022,Footnote 9 histologic lesions associated with avian influenza A(H5N1) clade 2.3.4.4b viruses were found in several red foxes, indicating extensive meningoencephalitis and pneumonia, as well as abundant virus antigen in the brain sections.Footnote 9 Ferret experiments conducted in Canada demonstrated efficient transmission by direct contact of an avian influenza A(H5N1) clade 2.3.4.4 virus (A/Red Tailed Hawk/ON/FAV-0473-4/2022), resulting in lethal outcomes.Footnote 10 These ferrets succumbed to infection within one week and showed detectable infectious virus in the brain, consistent with the neurotropism seen in infected foxes.Footnote 10
Following detection of avian influenza A(H5N1) clade 2.3.4.4b in a free-ranging poultry farm in Rome virological and serological investigations were conducted in pigs with no clinical signs on the same premises. Serological samples were positive for avian influenza A(H5N1) and phylogenetic analysis confirmed the virus detected belonged to clade 2.3.4.4b.Footnote 11 There are limited reports of potential direct mammal-to-mammal transmission with avian influenza A(H5N1) clade 2.3.4.4b virus. In October 2022, an outbreak occurred on a farm of over 52,000 mink in Spain.Footnote 12 Of 15 mink tested, 14 were positive for avian influenza A(H5N1) clade 2.3.4.4b by RT-PCR and the mortality rate on the farm started at 0.8% the first week of October and by the third week reached a peak mortality rate of 4.3%.Footnote 12 Based on epidemiological evidence, onward transmission of the virus from mink-to-mink may have taken place on the affected farm.Footnote 12
Large numbers of marine mammals have been infected with avian influenza A(H5N1) clade 2.3.4.4b viruses during the current global epizootic.Footnote 13 In an outbreak among New England seals in the United States, transmission is likely to have occurred from wild birds to seals via environmental transmission of shed virus.Footnote 14 In January and February 2023, a large sea lion die-off in Peru coincided with an outbreak of avian influenza A(H5N1) clade 2.3.4.4b in seabirds. A report of this event concluded that transmission likely occurred due to close contact with or consumption of infected birds, but direct transmission between sea lions could not be ruled out.Footnote 15
Humans
Since December 2021, detections of avian influenza A(H5N1) clade 2.3.4.4b viruses in humans have been reported from China (n=2)Footnote 16,Footnote 17, the United Kingdom (n=3)Footnote 18,Footnote 19, the United States (n=1)Footnote 20, Spain (n=2)Footnote 21, Viet Nam (n=1; clade not confirmed at time of writing)Footnote 17,Footnote 22, Ecuador (n=1)Footnote 16 and Chile (n=1)Footnote 23. Human-to-human transmission has not been reported. Clinical severity has varied widely; the avian influenza A (H5N1) cases reported in humans from Europe and North America were asymptomatic or mild, while those in Asia and South America were severe or fatal. Almost all cases had known exposure to infected poultry. Exposure information was limited for the Chilean case, although highly pathogenic avian influenza A(H5) was detected in wild birds and sea lions in the area in which the case resided. Footnote 24 This case was notable because the virus identified from the Chilean patient had two mutations in the polymerase basic protein 2 (PB2) that have been shown to contribute to mammalian adaptation in experimental animal models. Footnote 25 In May 2023, avian influenza A(H5N1) clade 2.3.4.4b virus was detected in nasal swab specimens from two asymptomatic poultry farm workers in the UK as part of a voluntary testing program for individuals exposed to infected birds.Footnote 19 Virus detection in one of these two individuals is thought to have resulted from contamination of the nasal passages through inhalation of virus, rather than true infection.Footnote 19
It is possible that human infections are under-detected, due to reliance on passive surveillance and limited testing of individuals exposed to infected animals. Mild and subclinical cases are likely to be detected only as part of special investigations during animal outbreaks or contact tracing for a confirmed human case.
In June 2022, the Public Health Agency of Canada (PHAC) analyzed the risk to humans from avian influenza A(H5N1) in Canada. At that time, the risk of infection with avian influenza A(H5N1) for the general population with limited contact with infected animals was considered to be low. The assessment is being updated due to continued widespread circulation of avian influenza A(H5N1) clade 2.3.4.4b in wild and domestic bird populations, the increasing range of mammalian species in which infection with this virus has been reported, and additional reports of isolated human cases in other countries.
Methods
This assessment was led by CDSB-CIRA, within the Public Health Agency of Canada (PHAC) in May and June 2023, and conducted in collaboration with a multi-sectoral team. The rapid risk assessment (RRA) methodology used by CDSB-CIRA has been adapted from the Joint Risk Assessment Operational Tool (JRA OT) to assess the risk posed by zoonotic disease hazards Footnote 26, developed jointly by the World Health Organization (WHO), the Food and Agriculture Organization of the United Nations (FAO), and the World Organization for Animal Health (WOAH). PHAC has adapted the JRA OT by modifying the likelihood and impact scales and associated definitions to incorporate elements from other RRA frameworks that are relevant to the Canadian context. Footnote 27,Footnote 28
Detailed methodology outlined in Appendix A.
Definitions
This risk assessment focuses on the risk of human infection with avian influenza A(H5N1) clade 2.3.4.4b virus in Canada from zoonotic or environmental exposures (due to animal contamination). Exposure risks related to contact with a human case are not included. If human-to-human transmission were to occur with this virus, a separate risk assessment would be conducted that includes such exposure risks, e.g., those experienced by close contacts of cases and healthcare workers.
Refer to Appendix B for a list of occupational and recreational groups with potentially relevant exposures.
| Higher-level exposure | High intensity (within 2 metres and/or prolonged) contact with animals infected with avian influenza A(H5N1) clade 2.3.4.4b virusTable 2 footnote a (i.e., wild birds, poultry, or mammals), or infected materials from these animals (e.g., feces, blood, secretions, or tissues), or an environment highly contaminated by infected animals.
Note: higher dose contact combined with appropriate use of PPE and hand hygiene could be considered lower or negligible exposure depending on circumstances. |
Lower-level exposure |
Low intensity (greater than 2 meters and/or transient) contact with animals infected with avian influenza A(H5N1) clade 2.3.4.4b virusTable 2 footnote a (i.e., wild birds, poultry, or mammals), or infected materials from these animals (e.g., feces, blood, secretions, or tissues), or an environment not highly contaminated by infected animals (e.g., diluted recreational bodies of water, open-air environment).
|
Negligible exposure |
The following are considered negligible exposures (i.e., not considered plausible exposure pathways):
|
General population exposure |
The exposure experienced by the general (human) population is assumed to be:
|
Key assumptions
- Relatively little is known about the epidemiological or viral characteristics of avian influenza A(H5N1) clade 2.3.4.4b viruses and this assessment assumes some similarities with other highly pathogenic avian influenza (HPAI) viruses.
- This assessment assumes that there will be no significant genetic changes to the currently circulating avian influenza A(H5N1) clade 2.3.4.4b viruses during the assessment period that would influence infectivity, transmissibility, or clinical severity in humans.
- This assessment considers all avian influenza A(H5N1) viruses belonging to clade 2.3.4.4b currently in circulation at the time of this assessment.
- Pathway assumptions:
- Infection routes for humans are primarily through respiratory and/or mucous membrane contact irrespective of animal source and/or human exposure groups (occupational/recreational), but it is assumed that, where applicable, prevention and control guidance will recommend measures to avoid all possible infection routes, which may include handling and consumption of raw or undercooked, contaminated animal products.
- There is limited information regarding the susceptibility to and prevalence of infection in many of the different bird and animal species. To provide more precautionary estimates of the likelihood of infection (i.e., representing the worst-case scenario), the following guidance was used for estimating the likelihood of infection in different animal groups:
- Wild birds: birds known to be susceptible to infection based on current evidence (e.g., Anseriformes and Charadriiformes).
- Domestic mammals: mammals known to be susceptible to infection to some degree based on current evidence (e.g., cats and dogs); note that farmed mammals were not expressly included in this assessment as part of domestic mammals, although farmed mink are known to be susceptible, and a recent study found serological evidence of infection in swine.Footnote 11,Footnote 12
- Wild mammals: mammals known to be susceptible to infection based on the current evidence (e.g., terrestrial and marine mammals).
Detailed risk assessment results
Risk pathway
Risk pathway depicting sources and exposures leading to, and impacts of, a human infection with avian influenza A(H5N1) clade 2.3.4.4b in Canada by the end of the 2023 fall bird migratory season (generally ranging from October to December in Canada). Refer to Appendix A for explanation of the use of the risk pathway to develop risk sub-questions.

Figure 1: Text description
The likelihood of such an infection is dependent on the prevalence of infection in different groups of animals (Questions 1a-1e), combined with the likelihood of exposure to a sufficient amount of virus to potentially cause infection following different types of animal contact (Questions 2a-2b), and then combined with the likelihood that an individual exposed to a sufficient amount of virus actually develops infection (Question 3). The impact estimates presented in Table 4 include consideration of the most likely spread scenario were a human case to occur in Canada (Question 4), together with the magnitude of effects on infected individuals (Question 5) and the overall impact for the Canadian population (Question 6).
Likelihood and impact estimates
Estimates of the likelihood of a human infection with avian influenza A(H5N1) clade 2.3.4.4b in Canada resulting from exposure to infected birds or mammals by the end of the 2023 fall bird migratory season are presented in Table 3, together with associated rationales and uncertainty estimates. The likelihood of such an infection is dependent on the prevalence of infection in different groups of animals (Questions 1a-1e), combined with the likelihood of exposure to a sufficient amount of virus to potentially cause infection following different types of animal contact (Questions 2a-2b), and then combined with the likelihood that an individual exposed to a sufficient amount of virus actually develops infection (Question 3). The likelihood scale used in this assessment is described in Table A2.
The impact estimates presented in Table 4 include consideration of the most likely spread scenario were a human case to occur in Canada (Question 4), together with the magnitude of effects on infected individuals (Question 5) and the overall impact for the Canadian population (Question 6). The magnitude of effects and impact scales used in this assessment are described in Table A3 and Table A4.
| Pathway sub-question | Estimate |
Rationale |
Uncertainty |
|
|---|---|---|---|---|
1a |
What is the likelihood that a random individual animalTable 3 footnote a from a commercial poultry flock in Canada is infected with avian influenza A(H5N1) clade 2.3.4.4b during the assessment period? |
Unlikely |
There continues to be outbreaks of avian influenza A(H5N1) clade 2.3.4.4b in commercial poultry flocks across Canada as biosecurity measures cannot entirely prevent transmission between wild birds and commercial poultry, however, the proportion of flocks infected remains small at <3%: from May to December 2022 (same date range as this assessment but last year), there were 141 commercial infected premises reported, with 4775 commercial poultry producers in Canada (in 2021).Footnote 3,Footnote 30 Geographic variation in infection prevalence is expected, depending on the local avian influenza A(H5N1) clade 2.3.4.4b epidemiology, density of commercial operations and wild bird populations. |
Very low to Low Based on existing surveillance information from poultry farms in Canada. |
1b |
What is the likelihood that a random individual animalTable 3 footnote a from a backyard poultry flock in Canada is infected with avian influenza A(H5N1) clade 2.3.4.4b during the assessment period? |
Unlikely |
Given continuing circulation of avian influenza A(H5N1) clade 2.3.4.4b in wild migratory birds, the lower level of biosecurity for backyard compared with commercial flocks, as well as the high susceptibility of poultry to infection, further sporadic infections in backyard poultry are expected in the assessment period and there is no indication that the rate of new infected premises will change during the next migratory season. During May-December 2022 (same date range as this assessment but last year), there were 66 backyard infected premises reported; although the total number of backyard premises in Canada is unknown, estimates from one province alone are >10 000 backyard flocks, resulting in a proportion of <1%.Footnote 31 |
High Based on limited surveillance in and limited information on the number, size, and geographic distribution of backyard flocks in Canada, and high variability in implementation of biosecurity measures. |
1c |
What is the likelihood that a random individual wild birdTable 3 footnote a in Canada is infected with avian influenza A(H5N1) clade 2.3.4.4b during the assessment period? |
Unlikely |
The avian influenza A(H5N1) clade 2.3.4.4b virus is detected in wild birds on an ongoing basis, with approximately 4% positivity in apparently healthy wild birds (mostly waterfowl) during this time last year: of 9,900 samples tested between May and December, 2022, 386 have resulted in confirmed or suspected avian influenza A(H5N1) clade 2.3.4.4b detections (3.9%), with the majority identified in September. Increases in infection prevalence are observed during spring and fall migration seasons, and there is geographic variation in infection prevalence, depending on the local avian influenza A(H5N1) clade 2.3.4.4b epidemiology.Footnote 4 |
Very low to Low Based on existing surveillance and other evidence demonstrating ongoing transmission in this population despite gaps in knowledge, underestimation of prevalence, and suspected variation in susceptibility between species. |
1d |
What is the likelihood that a random individual domestic mammalTable 3 footnote a in Canada is infected with avian influenza A(H5N1) clade 2.3.4.4b during the assessment period? |
Very unlikely |
Given continuing circulation of avian influenza A(H5N1) clade 2.3.4.4b in wild migratory birds, domestic mammals with direct contact to these birds may become infected; however, the number of detections in domestic mammals to date has been very small, in Canada and elsewhere. Footnote 32,Footnote 33 |
Moderate Based on limited surveillance in domestic mammals in Canada |
1e |
What is the likelihood that a random individual wild mammalTable 3 footnote a in Canada is infected with avian influenza A(H5N1) clade 2.3.4.4b during the assessment period? |
Unlikely |
Reports in wild mammals continue and are increasing, Footnote 34 however, numbers are still limited in Canada, the USA and elsewhere. Footnote 13,Footnote 14,Footnote 35,Footnote 36,Footnote 37,Footnote 38 |
High Based on very limited surveillance in wild mammals in Canada and suspected variation in susceptibility between species. |
2a |
What is the likelihood that a higher-level exposureTable 3 footnote b involves a sufficient amount of virusTable 3 footnote c to potentially cause an infection (for the average person)? |
Highly likely |
Infected birds are known to shed high quantities of virus into the air and surrounding environment. Footnote 39,Footnote 40,Footnote 41 Most human cases reported to date have involved higher-level exposure with infected poultry and/or highly contaminated environments.Footnote 16,Footnote 17,Footnote 18,Footnote 19,Footnote 20,Footnote 21,Footnote 22,Footnote 23, Sero-epidemiological studies of other avian influenza A(H5N1) viruses from numerous settings demonstrate the potential for infection in humans highly exposed to infected birds.Footnote 42 |
Low Based on current knowledge of the route of exposure in confirmed cases to date |
2b |
What is the likelihood that a lower-level exposureTable 3 footnote b involves a sufficient amount of virusTable 3 footnote c to potentially cause an infection (for the average person)? |
Very unlikely |
Globally, there are no known cases associated with this type of exposure.Footnote 16,Footnote 17,Footnote 18,Footnote 19,Footnote 20,Footnote 21,Footnote 22,Footnote 23 Due to the high volume of infections with this virus that have occurred in wild animals and poultry in Canada, there have likely been numerous low dose contacts that have not resulted in exposure to sufficient amount of virus.Footnote 43 |
High Based on lack of information concerning potential infectious dose in lower-level exposure situations, and potential for under-detection of asymptomatic or mild infections following lower-level exposures. |
3 |
What is the likelihood that a person who had exposure to sufficient amount of virusTable 3 footnote c will develop an infection? |
Unlikely |
Although human populations are expected to have very little immunological protection against avian influenza A(H5N1) clade 2.3.4.4b viruses, there have been only a small number of human cases reported to date globally. This is despite frequent high-dose exposures in certain populations, particularly those in contact with poultry. Although data specific to avian influenza A(H5N1) clade 2.3.4.4b are lacking, a recent US study reported 1 PCR detection of highly pathogenic avian influenza A(H5) virus in a respiratory sample, among more than 4000 humans exposed to avian influenza A(H5N1)-infected birds. Footnote 44 Previous meta-analyses of serosurveys have reported seroprevalence of avian influenza A(H5N1) antibodies of 1%-2% among poultry workers and those exposed to infected poultry. Footnote 45,Footnote 46 |
Moderate Based on lack of information on this specific clade, the small number of detections in humans and limited surveillance activities in populations exposed to infected animals |
| no data | What is the likelihood of at least one human infection with avian influenza A(H5N1) clade 2.3.4.4b due to exposure to birds in Canada up to the end of the 2023 fall bird migratory season? |
no data | Infection with avian influenza A(H5N1) clade 2.3.4.4b is very unlikely for the general population that have negligible or lower-level exposure to birds (wild birds, or commercial or backyard poultry), driven by low likelihood of exposure to the virus. There is high uncertainty with this estimate due to the lack of information on potential infectious dose for lower-level exposures. Logic to derive the overall likelihoodTable 3 footnote d = [1a OR 1b OR 1c] AND 2b AND 3:
Infection with avian influenza A(H5N1) clade 2.3.4.4b is higher but still unlikely for populations that have higher-level exposure to birds (wild birds, or commercial or backyard poultry) due to the limited capacity of the virus to infect humans as well as the low level of infection in birds. The uncertainty ranges from very low to high for this estimate due to large number of drivers: lack of information on the infectivity of this clade, the small number of infections in humans, limited surveillance and testing in human populations exposed to birds as well as backyard poultry, the lack of surveillance in backyard poultry and information regarding the number of backyard poultry flocks in Canada. Logic to derive the overall likelihoodTable 3 footnote d = [1a OR 1b OR 1c] AND 2a AND 3:
|
no data |
| no data | What is the likelihood of at least one human infection with avian influenza A(H5N1) clade 2.3.4.4b due to exposure to mammals in Canada up to the end of the 2023 fall bird migratory season? |
no data | Infection with avian influenza A(H5N1) clade 2.3.4.4b is very unlikely for the general population that has higher exposure to domestic mammals (e.g., dogs and cats) but not wild mammals, due to the very low likelihood that domestic mammals are infected. There is a moderate to high level of uncertainty due to limited surveillance in domestic mammals and the lack of information on potential infectious dose for lower-level exposures to wild mammals.
+
Infection with avian influenza A(H5N1) clade 2.3.4.4b is unlikely for the population that has higher-level exposure to wild mammals (e.g., wild carnivores and scavengers) despite their higher likelihood of exposure to the virus, due to the low likelihood of infection in wild mammals and the limited capacity of the virus to infect humans. There is a moderate to high level of uncertainty estimates due to limited surveillance and testing of wild mammals and limited information on the infectivity of this clade for humans.
|
no data |
| Pathway sub-questions | Estimate |
Rationale |
Uncertainty |
|
|---|---|---|---|---|
4 |
In the event that human infection occurs, what would be the most likely spread scenario? |
No further transmission |
The most likely spread scenario is that of zoonotic infection with no further transmission, given that there is no evidence that the virus has acquired the capacity for sustained transmission among humans. |
Low Based on the small number of detections of this virus in humans to date and the absence of evidence for human-to-human transmission of this virus. However, this assessment would change if evidence emerges of virus mutations or adaptations leading to efficient transmission in humans. |
5 |
What would be the impact on an individual infected person (the magnitude of effects, including impact on mental health, disease morbidity/mortality, and/or welfare)? |
Major |
Detection of initial human cases would likely involve infection control measures such as isolation and quarantine, with impacts on the physical and mental health as well as financial wellbeing of affected individuals, their families, and other close contacts. |
High Due to variability in clinical presentation seen in the limited number of human cases so far (ranging from asymptomatic to death), and lack of data on the frequency of asymptomatic and mild infection. |
6 |
What would be the impact on the Canadian population during the assessment period (based on the response to the most likely spread scenario in Question 4)? |
Minor |
Based on most likely spread scenario (Sub-question 4 above), human-to-human transmission is not expected to occur; health impacts will likely be limited to isolated zoonotic cases. Some indirect impacts could occur, such as the potential for public anxiety from media coverage of human cases. |
Low There is a lack of evidence of human-to-human transmission for currently circulating viruses. |
Risk estimate summary
Based on the available data at this point in time, up to the end of the 2023 fall bird migratory season (generally ranging from October to December in Canada):
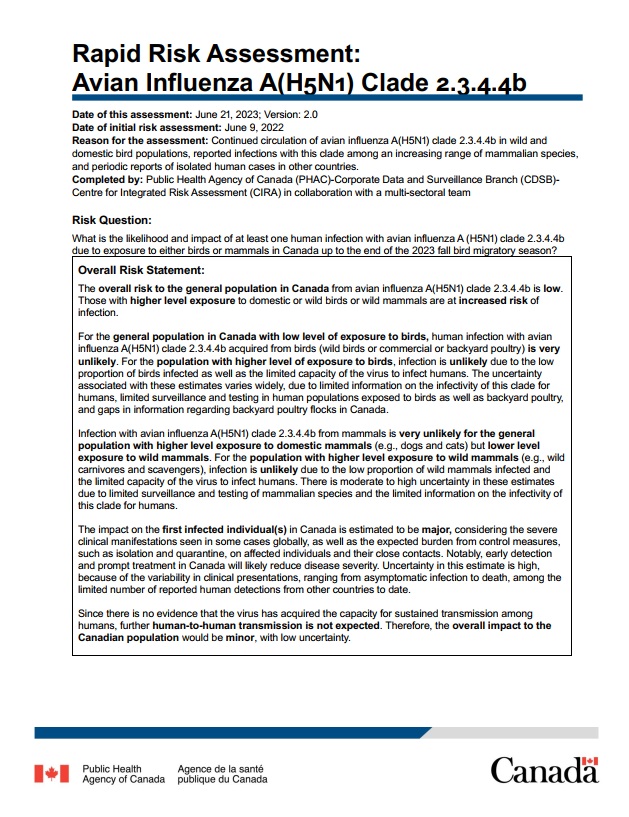
- The overall risk to the general population from lower or negligible exposure to either birds or mammals (number 2 in Figure 2 in darker green area) is low.
- The risk for those with higher exposure to either birds or wild mammals is "increased" compared to the risk experienced by the general population (number 1 in Figure 2 in the lighter green-yellow area)

Figure 2: Text description
Risk matrix depicting the overall level of risk for the general population (indicated with the number 2) and populations with higher exposure to bird and/or mammals (indicated with the number 1). A scale of likelihood is along the vertical axis with very unlikely at the bottom to highly likely at the top. A scale of impact is along the horizontal axis with minimal to the far left and severe on the far right. The risk matrix is a gradient with the lowest overall risk in the bottom left corner (darkest green) and highest overall risk in the top right corner (bright red).
Limitations
This assessment does not explicitly consider the frequency of human interactions with different types of animals; the size of different animal populations; or geographic variations in the distribution of animal populations, infection prevalence in animal species and human-animal contacts.
The qualitative method used for the likelihood estimation leads to an over-inflation of likelihood since the cumulative effect of probabilities less than 100% along the pathway will reduce the likelihood in a way that cannot be captured without quantitative data. This bias is in line with the use of the precautionary principle.
There was substantial variation in initial estimates provided by multi-sectoral experts to pathway sub-questions related to the likelihood of infection in different animal groups. Analysis of rationales provided by experts for their estimates indicated that the question had been interpreted in two different ways by Technical Team members, resulting in a divergence of estimates. The intended interpretation of the questions was subsequently clarified and revised likelihood estimates derived after discussion with Technical Team members and review of relevant evidence.
The wording of questions 2a and 2b (and associated naming of exposure levels) were changed during the review process to improve clarity. In the poll the questions were worded as follows: "What is the likelihood of at least one person getting exposed to sufficient amount of virus to potentially cause an infection for the average person following a higher/lower dose contact".
Knowledge gaps
The key scientific uncertainties and knowledge gaps in this assessment are included below (refer to Table 5).
| Risk pathway sub-section | Unknown or more information needed |
Infection in animals |
|
Exposure |
|
Human susceptibility |
|
Immediate/direct impacts |
|
Interventions |
|
Acknowledgements
Completed by the Public Health Agency of Canada's Centre for Integrated Risk Assessment within the Corporate Data and Surveillance Branch.
The individuals listed, along with their affiliated agencies, are acknowledged for their contributions to this report.
Alberta Health/Alberta Agriculture and Irrigation: Hussein Keshwani
British Columbia Centre for Disease Control: Erin Fraser, Linda Hoang, Agatha Jassem, Samantha Kaweski, Shannon Russell, Inna Sekirov, Danuta Skowronski
British Columbia Ministry of Agriculture: Theresa Burns, Chelsea G. Himsworth
Cadham Provincial Laboratory (Manitoba): Paul Van Caeseele
Canadian Food Inspection Agency: Tamiru Alkie, Yohannes Berhane, Maud Carron, Caroline Dubé, Andrea Ellis, Logan Flockhart, Kathleen Hooper, Charles Nfon, Marc Sabourin, Primal Silva
Canadian Veterinary Medical Association: Mike Petrik
Canadian Wildlife Health Cooperative: Damien Joly
Environment and Climate Change Canada: Michael Brown, Brigitte Collins, Jolene Giacinti, Jack Hughes, Daniel Leclair, Hannah Lewis
Fisheries and Oceans Canada: Ole Nielsen
Indigenous Services Canada: Shawn Donaldson, Amole Khadilkar, Maxime Trubnikov
Institut national de santé publique du Québec: Cassi Bergeron-Caron, Maude Bigras, Hugues Charest, Judith Fafard, Alejandra Irace-Cima
Manitoba Agriculture: Dale Douma
Ministère de l'Agriculture, des Pêcheries et de l'Alimentation du Québec: Isabelle Picard
Ministère de la santé et des services sociaux du Québec: Josée Dubuque, Colette Gaulin, Juliette Martin
New Brunswick Public Health Laboratories: Richard Garceau
Nova Scotia Health Authority: Todd Hatchette, Jason Leblanc
Ontario Ministry of Agriculture, Food and Rural Affairs: Maureen Anderson, Paul Innes
Ontario Ministry of Health: Melissa Helferty
Parks Canada: Todd Shury
Prince Edward Island Chief Public Health Office: Karen Phillips
Public Health Agency of Canada: Rukshanda Ahmad, Sandra Radons Arneson, Nicole Atchessi, Dima Ayache, Christina Bancej, Nathalie Bastien, Philippe Belanger, Anna Bellos, Samuel Bonti-Ankomah, Natalie Bruce, Peter Buck, Sharon Calvin, Taeyo Chestley, Mette Cornelisse, Lesley Doering, Catherine Elliott, Raquel Farias, Aamir Fazil, Manon Fleury, Vanessa Gabriele-Rivet, Eleni Galanis, Corey Green, Heather Hannah, Marianne Heisz, Kirsten Jacobsen, Emmanuelle Jean, Nina Jetha, Danielle Julien, Mira Kelada-Antoun, Darwyn Kobasa, Lisa Landry, Erin Leonard, Tiffany Locke, Aaron MacCosham, Janice Merhej, Rachel Milwid, Rhonda Mogk, Nicholas Ogden, Toju Ogunremi, Nicole Pachal, Renee Parisien, Matthew Peake, Kirsten Querbach, Charlene Ranadheera, Simran Sandhu, Jill Sciberras, Lisa Slywchuk, Ming Su, Clarence Tam, Joe Tanelli, Francois-William Tremblay, Jan Trumble-Waddell, Linda Vrbova, Lisa Waddell, Lindsay Whitmore
Public Health New Brunswick: Jackie Badcock, Renee Bourque, Carole Breau, Shelley Landsburg, Arifur Rahman
Public Health Ontario: Maan Hasso, Emily Karas, Richard Mather, Karam Ramotar
Sunnybrook Health Sciences Centre: Samira Mubareka
Appendix A: Methods
The Centre for Integrated Risk Assessment at PHAC convened a Canadian One Health multi-sectoral team that formed two committees: the Rapid Risk Assessment (RRA) Steering Committee and the RRA Technical Team. The Steering Committee (largely comprised of senior managers and decision makers) defined the hazard, agreed on the purpose and key objectives for the assessment, outlined the scope, drafted the risk question, and reviewed the recommendations. The Technical Team (largely comprised of those with expertise and/or information related to the assessment) characterized the risk by providing qualitative estimates of likelihood, impact and uncertainty in relation to the risk questions being assessed, based on the available evidence and expert opinion. The Canadian One Health multi-sectoral team consisted of federal, provincial and academic experts from human, animal, and ecosystem health sectors, representing a variety of disciplines such as epidemiologists, virologists, wildlife biologists, veterinarians, and physicians.
The risk question being assessed was visualized using a risk pathway (Figure 1), a diagrammatic representation of the key components of the sequence of the hazard from its source to its infection of the host of interest. Each step in the risk pathway is associated with a likelihood or impact sub-question that was then addressed as part of the risk assessment. The risk pathway and sub-questions also included the animal and exposure sub-groups listed in Table 2.
The Technical Team were introduced to the risk pathway and associated questions in a meeting. Subsequently, a poll was used to obtain initial, independently assessed qualitative estimates from Technical Team members on the likelihood or impact associated with each risk pathway sub-question, using standardized qualitative scales (Tables A1-A4 below). The risk pathway, a slide deck explaining exposure groups, definitions for likelihood and impact and an evidence table were provided to assist each expert in making their best-considered estimation of risk. For each estimate, members were also asked to provide a rationale, indicate the level of uncertainty associated with their estimate and give a short explanation of the factors influencing this uncertainty. Lastly, members were given the option to not answer specific questions if they lacked sufficient expertise.
The poll results were used as a basis for discussion; final estimates were based on discussion with the Technical Team and review of the draft report by Technical Team and Steering Committee. A summary of poll responses was presented to Technical Team members in a meeting following the poll, highlighting where estimates and rationales clearly converged, and areas where poll results suggested differing interpretations of the questions or divergent estimates or rationales. Estimates and rationales that aligned with a common understanding of the rapid risk assessment questions were finalized based on subsequent discussions, as well as feedback through draft document review by the Technical Team and final review and feedback by the Steering Committee. In addition, Technical Team members were asked to identify key uncertainties and knowledge gaps that influenced their level of uncertainty in likelihood and impact estimates during the poll and in meetings. These were consolidated into a list of key uncertainties and knowledge gaps related to this risk assessment (Table 5).
Definitions of likelihood (Table A2), impact (Table A3 and Table A4), and uncertainty (Table A1) are provided below. Since the risk pathway describes the sequence of events leading up to the undesired outcome, the likelihood of each event is conditional on the likelihood of preceding steps in the risk pathway, as assessed in the estimation process for each risk pathway sub-question. The likelihood for the overall risk question is therefore determined by the lowest likelihood estimated along the risk pathway. A risk matrix, adapted from WHO (2012), is used to integrate the likelihood and impact estimates into a summary risk estimate to support risk communication. Summary risk estimates are presented in context with the likelihood and impact estimates, given the known limitations of risk matrices.Footnote 47
The findings and conclusions represent the consensual, but not necessarily unanimous, opinions of experts contributing to this risk assessment, and should not be interpreted as representing the views of all participants and their respective organizations. Evidence was gathered by scientific experts using a rapid, non-systematic literature search and includes published articles and pre-print manuscripts, reports on the current outbreak including surveillance reports, and communication from multi-sectoral experts. Where appropriate, some references have been included; where references are not included this evidence was informed by input from the subject matter experts.
| Uncertainty | Criteria |
|---|---|
Very high |
Lack of data or reliable information; results based on crude speculation only |
High |
Limited data or reliable information available; results based on educated guess |
Moderate |
Some gaps in availability or reliability of data and information, or conflicting data; results based on limited consensus |
Low |
Reliable data and information available but may be limited in quantity, or be variable; results based on expert consensus |
Very low |
Reliable data and information are available in sufficient quantity; results strongly anchored in empiric data or concrete information |
| Likelihood estimate | Criteria |
|---|---|
Highly likely |
The situation described in the risk assessment question is highly likely to occur (i.e., is expected to occur in most circumstances) |
Likely |
The situation described in the risk assessment question is likely occur |
Unlikely |
The situation described in the risk assessment question is unlikely to occur |
Very unlikely |
The situation described in the risk assessment question is very unlikely to occur (i.e., is expected to occur only under exceptional circumstances) |
| Estimate | Criteria |
|---|---|
Severe |
Severe impact on mental health and/or disease morbidity/mortality, and/or welfare (e.g., loss of income) |
Major |
Major impact on mental health and/or disease morbidity/mortality, and/or welfare (e.g., loss of income) |
Moderate |
Moderate impact on mental health and/or disease morbidity/mortality, and/or welfare (e.g., loss of income) |
Minor |
Minor impact on mental health and/or disease morbidity/mortality, and/or welfare (e.g., loss of income) |
Minimal |
Minimal or no impact on mental health and/or disease morbidity/mortality, and/or welfare (e.g., loss of income) |
| Estimate | Criteria |
Population impact criteria |
|---|---|---|
Severe |
The situation described in the risk assessment question will have severe negative consequences on the population under assessment |
Potential pandemic in the general population or large numbers of case reports, with significant impact on the well-being of the population
|
Major |
The situation described in the risk assessment question will have major negative consequences on the population under assessment |
Case reports with moderate to significant impact on the well-being of the population
|
Moderate |
The situation described in the risk assessment question will have moderate negative consequences on the population under assessment |
Case reports with low to moderate impact on the well-being of the population
|
Minor |
The situation described in the risk assessment question will have minor negative consequences on the population under assessment |
Rare case reports, mainly in small at-risk groups, with moderate to significant impact on the well-being of the population
|
Minimal |
The situation described in the risk assessment question will have minimal or no negative consequences on the population under assessment |
No or very rare case reports with low to moderate impact on the well-being of the population
|
Appendix B: Occupational and recreational groups with potentially relevant exposures
The population with either occupational or recreational exposure to potentially infected wild birds, poultry, or mammals, their carcasses or highly contaminated environments includes the following:
- Poultry farm worker
- Backyard/small poultry flock owner
- Poultry processing plant worker
- Poultry culler (catching, bagging, transporting, or disposing of dead birds)
- Dealer, breeder, or handler of pet and other birds (e.g., exotics, falconry, racing pigeons)
- Butcher or person working with live or recently killed poultry or other potentially affected animals
- Person working in live animal market
- Veterinarian or other animal health worker
- Wildlife officer or biologist collecting specimens or euthanizing birds or mammals
- Wildlife rehabilitator
- Person performing permitted activities with wildlife (e.g., bird banding, capturing, sampling, removal, restoration, etc.)
- Person involved in hunting and trapping including Indigenous harvester
- Laboratory worker or researcher working with wild birds and/or mammals
- Caretaker of animals (e.g., pets, guardian dogs, hunting dogs) that regularly interact with wild birds or other potentially affected stray, or wild animals
- Person with other significant occupational or recreational exposure to wild birds and other potentially affected animals (e.g., mink farmer, biologist)
Note: If human-to-human transmission starts occurring for this virus, then healthcare workers and other contacts of cases would also need to be included.
References
- Footnote 1
-
Public Health Agency of Canada. Wildlife and avian influenza – Handling guidelines to protect your health. Canada.ca. July 15, 2022. https://www.canada.ca/en/public-health/services/flu-influenza/fact-sheet-guidance-on-precautions-handling-wild-birds.html
- Footnote 2
-
Canadian Network for Public Health Intelligence. Alert. RA-005071. January 19, 2022.
- Footnote 3
-
Canadian Food Inspection Agency. Status of ongoing avian influenza response by province. Government of Canada. Updated 2023. Accessed March 17, 2023. https://inspection.canada.ca/animal-health/terrestrial-animals/diseases/reportable/avian-influenza/hpai-in-canada/status-of-ongoing-avian-influenza-response/eng/1640207916497/1640207916934
- Footnote 4
-
Canadian Food Inspection Agency. Highly pathogenic avian influenza- wild birds. https://cfia-ncr.maps.arcgis.com/apps/dashboards/89c779e98cdf492c899df23e1c38fdbc
- Footnote 5
-
Jonges M, Welkers MR, Jeeninga RE, et al. Emergence of the virulence-associated PB2 E627K substitution in a fatal human case of highly pathogenic avian influenza virus A(H7N7) infection as determined by Illumina ultra-deep sequencing. J Virol. 2014;88(3):1694-1702. doi:10.1128/JVI.02044-13
- Footnote 6
-
Lee CY, An SH, Choi JG, Lee YJ, Kim JH, Kwon HJ. Rank orders of mammalian pathogenicity-related PB2 mutations of avian influenza A viruses. Sci Rep. 2020;10(1):5359. Published 2020 Mar 24. doi:10.1038/s41598-020-62036-5
- Footnote 7
-
European Food Safety Authority. Avian influenza overview December 2022-March 2023. 8 March 2023. https://www.ecdc.europa.eu/sites/default/files/documents/avian-influenza-overview-march-2023.pdf
- Footnote 8
-
Department for Environment Food Rural Affairs. Confirmed findings of influenza of avian origin in captive mammals. GOV.UK. March 15, 2023. https://www.gov.uk/government/publications/bird-flu-avian-influenza-findings-in-captive-mammals/confirmed-findings-of-influenza-of-avian-origin-in-captive-mammals#:~:text=These%20animals%20were%20part%20of,over%20a%209%20day%20period
- Footnote 9
-
Alkie TN, Cox S, Embury-Hyatt C, et al. Characterization of neurotropic HPAI H5N1 viruses with novel genome constellations and mammalian adaptive mutations in free-living mesocarnivores in Canada. Emerg Microbes Infect. 2023;12(1):2186608. doi:10.1080/22221751.2023.2186608
- Footnote 10
-
Kobasa D, Warner B, Alkie T, et al. Transmission of lethal H5N1 clade 2.3.4.4b avian influenza in ferrets. April 21, 2023. https://www.researchsquare.com/article/rs-2842567/v1
- Footnote 11
-
Rosone F, Bonfante F, Sala MG, Maniero S, Cersini A, Ricci I, Garofalo L, Caciolo D, Denisi A, Napolitan A, et al. Seroconversion of a Swine Herd in a Free-Range Rural Multi-Species Farm against HPAI H5N1 2.3.4.4b Clade Virus. Microorganisms. 2023; 11(5):1162. https://doi.org/10.3390/microorganisms11051162
- Footnote 12
-
Agüero M, Monne I, Sánchez A, et al. Highly pathogenic avian influenza A(H5N1) virus infection in farmed minks, Spain, October 2022. Euro Surveill. 2023;28(3):2300001. doi:10.2807/1560-7917.ES.2023.28.3.2300001
- Footnote 13
-
Thorsson E, Zohari S, Roos A, Banihashem F, Bröjer C, Neimanis A. Highly Pathogenic Avian Influenza A(H5N1) Virus in a Harbor Porpoise, Sweden. Emerg Infect Dis. 2023;29(4):852-855. doi:10.3201/eid2904.221426
- Footnote 14
-
Puryear W, Sawatzki K, Hill N, et al. Highly Pathogenic Avian Influenza A(H5N1) Virus Outbreak in New England Seals, United States. Emerging Infectious Diseases. 2023;29(4):786-791. doi:10.3201/eid2904.221538
- Footnote 15
-
Gamarra-Toledo V, Plaza PI, Gutiérrez R, et al. Mass Mortality of Marine Mammals Associated to Highly Pathogenic Influenza Virus (H5N1) in South America. bioRxiv; 2023. DOI: 10.1101/2023.02.08.527769
- Footnote 16
-
World Health Organization. Influenza at the human-animal interface. Summary and risk assessment, from 6 October to 11 November 2022. https://cdn.who.int/media/docs/default-source/influenza/human-animal-interface-risk-assessments/influenza-at-the-human-animal-interface-summary-and-assessment--from-6-october-to-11-november-2022.pdf?sfvrsn=db9a4370_1&download=true
- Footnote 17
-
World Health Organization. Influenza at the human-animal interface. Summary and risk assessment, from 27 January to 3 March 2023. https://cdn.who.int/media/docs/default-source/global-influenza-programme/influenza-at-the-human-animal-interface-summary-and-assessment--from-27-january-to-3-march-2023.pdf?sfvrsn=6065458a_1&download=true
- Footnote 18
-
Oliver I, Roberts J, Brown CS, et al. A case of avian influenza A(H5N1) in England, January 2022. Euro Surveill. 2022;27(5):2200061. doi:10.2807/1560-7917.ES.2022.27.5.2200061
- Footnote 19
-
UK Health Security Agency. Avian flu detected in 2 individuals taking part in testing programme. GOV.UK. May 16, 2023. https://www.gov.uk/government/news/avian-flu-detected-in-2-individuals-taking-part-in-testing-programme
- Footnote 20
-
Centers for Disease Control. U.S. case of human avian influenza A(H5) virus reported. CDC Web site. Updated 2022. https://www.cdc.gov/media/releases/2022/s0428-avian-flu.html
- Footnote 21
-
Aznar E, Casas I, González Praetorius A, et al. Influenza A(H5N1) detection in two asymptomatic poultry farm workers in Spain, September to October 2022: suspected environmental contamination. Euro Surveill. 2023;28(8):2300107. doi:10.2807/1560-7917.ES.2023.28.8.2300107
- Footnote 22
-
World Health Organization. Assessment of risk associated with recent influenza A(H5N1) clade 2.3.4.4b viruses. Published December 21, 2022. https://www.who.int/publications/m/item/assessment-of-risk-associated-with-recent-influenza-a(h5n1)-clade-2.3.4.4b-viruses
- Footnote 23
-
World Health Organization. Influenza at the human-animal interface. Summary and risk assessment, 24 April 2023. https://cdn.who.int/media/docs/default-source/influenza/human-animal-interface-risk-assessments/influenza-at-the-human-animal-interface-summary-and-assessment--from-4-march-to-24-april-2023.pdf?sfvrsn=e667a5dc_1&download=true
- Footnote 24
-
World Health Organization. Human infection caused by Avian Influenza A (H5) – Chile. April 6, 2023. https://www.who.int/emergencies/disease-outbreak-news/item/2023-DON453
- Footnote 25
-
Centers for Disease Control and Prevention. Human Infection with highly pathogenic avian influenza A(H5N1) virus in Chile. Updated April 17, 2023. https://www.cdc.gov/flu/avianflu/spotlights/2022-2023/chile-first-case-h5n1-addendum.htm
- Footnote 26
-
WHO, OIE and FAO. (2020). Joint Risk Assessment Operational Tool (JRA OT): An Operational Tool of the Tripartite Zoonoses Guide – Taking a Multisectoral, One Health Approach: A Tripartite Guide to Addressing Zoonotic Diseases in Countries. Food and Agriculture Organization of the United Nations. https://www.fao.org/documents/card/en/c/cb1520en/
- Footnote 27
-
World Health Organization. (2012). Rapid risk assessment of acute public health events. https://www.who.int/publications/i/item/rapid-risk-assessment-of-acute-public-health-events
- Footnote 28
-
European Centre for Disease Prevention and Control. (2019). Operational tool on rapid risk assessment methodology. https://www.ecdc.europa.eu/en/publications-data/operational-tool-rapid-risk-assessment-methodology-ecdc-2019
- Footnote 29
-
Slusher MJ, Wilcox BR, Lutrell MP, et al. Are passerine birds reservoirs for influenza A viruses?. J Wildl Dis. 2014;50(4):792-809. doi:10.7589/2014-02-043
- Footnote 30
-
Government of Canada. Canada's poultry and egg industry profile. Agriculture and Agri-Food Canada. June 23, 2021. https://agriculture.canada.ca/en/sector/animal-industry/poultry-egg-market-information/industry-profile
- Footnote 31
-
Van Esch HL. Characterization of Alberta Backyard Poultry Flocks and the Submission Level Prevalence of Infectious Laryngotracheitis Within This Sector. Thesis. 2021
- Footnote 32
-
Weese S. H5N1 avian flu in cats. Worms & Germs Blog. April 8, 2023. https://www.wormsandgermsblog.com/2023/04/articles/animals/cats/h5n1-avian-flu-in-cats/
- Footnote 33
-
Canadian Food Inspection Agency. Domestic dog tests positive for avian influenza in Canada. Canada.ca. April 5, 2023. https://www.canada.ca/en/food-inspection-agency/news/2023/04/domestic-dog-tests-positive-for-avian-influenza-in-canada.html
- Footnote 34
-
Chestakova IV, Linden A van der, Martin BB, et al. High number of HPAI H5 virus infections and antibodies in wild carnivores in the Netherlands, 2020-2022. bioRxiv. May 12, 2023. https://www.biorxiv.org/content/10.1101/2023.05.12.540493v1
- Footnote 35
-
Alkie TN, Cox S, Embury-Hyatt C, et al. Characterization of neurotropic HPAI H5N1 viruses with novel genome constellations and mammalian adaptive mutations in free-living mesocarnivores in Canada. Emerg Microbes Infect. 2023;12(1):2186608. doi:10.1080/22221751.2023.2186608
- Footnote 36
-
United States Department of Agriculture. 2022-2023 detections of highly pathogenic avian influenza in mammals. May 26, 2023. https://www.aphis.usda.gov/aphis/ourfocus/animalhealth/animal-disease-information/avian/avian-influenza/hpai-2022/2022-hpai-mammals
- Footnote 37
-
World Organisation for Animal Health. Avian Influenza. WOAH. https://www.woah.org/en/disease/avian-influenza/#ui-id-2
- Footnote 38
-
Food and Agriculture Organization of the United Nations. Global AIV with Zoonotic Potential . AnimalHealth. April 27, 2023. https://www.fao.org/animal-health/situation-updates/global-aiv-with-zoonotic-potential/en
- Footnote 39
-
James J, Warren CJ, De Silva D, et al. The Role of Airborne Particles in the Epidemiology of Clade 2.3.4.4b H5N1 High Pathogenicity Avian Influenza Virus in Commercial Poultry Production Units. Viruses. 2023;15(4):1002. Published 2023 Apr 19. doi:10.3390/v15041002
- Footnote 40
-
Filaire F, Lebre L, Foret-Lucas C, et al. Highly Pathogenic Avian Influenza A(H5N8) Clade 2.3.4.4b Virus in Dust Samples from Poultry Farms, France, 2021. Emerg Infect Dis. 2022;28(7):1446-1450. doi:10.3201/eid2807.212247
- Footnote 41
-
Scoizec A, Niqueux E, Thomas R, Daniel P, Schmitz A, Le Bouquin S. Airborne Detection of H5N8 Highly Pathogenic Avian Influenza Virus Genome in Poultry Farms, France. Front Vet Sci. 2018;5:15. Published 2018 Feb 13. doi:10.3389/fvets.2018.00015
- Footnote 42
-
Van Kerkhove MD. Brief literature review for the WHO global influenza research agenda--highly pathogenic avian influenza H5N1 risk in humans. Influenza Other Respir Viruses. 2013;7 Suppl 2(Suppl 2):26-33. doi:10.1111/irv.12077
- Footnote 43
-
Shi J, Zeng X, Cui P, Yan C, Chen H. Alarming situation of emerging H5 and H7 avian influenza and effective control strategies. Emerg Microbes Infect. 2023;12(1):2155072. doi:10.1080/22221751.2022.2155072
- Footnote 44
-
Kniss K, Sumner KM, Tastad KJ, et al. Risk for Infection in Humans after Exposure to Birds Infected with Highly Pathogenic Avian Influenza A(H5N1) Virus, United States, 2022. Emerg Infect Dis. 2023;29(6):1215-1219. doi:10.3201/eid2906.230103
- Footnote 45
-
Wang TT, Parides MK, Palese P. Seroevidence for H5N1 influenza infections in humans: meta-analysis. Science. 2012;335(6075):1463. doi:10.1126/science.1218888
- Footnote 46
-
Chen X, Wang W, Wang Y, et al. Serological evidence of human infections with highly pathogenic avian influenza A(H5N1) virus: a systematic review and meta-analysis. BMC Med. 2020;18(1):377. Published 2020 Dec 2. doi:10.1186/s12916-020-01836-y
- Footnote 47
-
Cox, L. A. (2008). What's wrong with risk matrices? Risk Analysis, 28(2), 497–512. https://doi.org/10.1111/j.1539-6924.2008.01030.x