Lyme disease surveillance in Canada: Annual edition 2022
Download in PDF format
(406 KB, 14 pages)
Organization: Public Health Agency of Canada
Published: April 2024
Cat.: HP37-46E-PDF
ISBN: 2817-450X
Pub.: 230465
On this page
- 2022 surveillance highlights
- Introduction
- Methods
- Results
- Discussion
- Public health conclusions
- Acknowledgements
- References
2022 surveillance highlights
- A total of 2,525 human cases of Lyme disease were reported to the Public Health Agency of Canada between January 1, 2022 and December 31, 2022, of which, 2,093 (82.9%) were confirmed cases and 432 (17.1%) probable cases.
- Incidence was highest in adults aged 60–79 years (34.9% of cases) and children aged 5–14 years (11.9% of cases) with 54.1% of total cases reported in males.
- 31.8% of cases reported an illness onset in July.
- 94.7% of cases were reported in Ontario, Québec, and Nova Scotia.
- 2.9% of reported cases were likely infected during travel outside of Canada.
- The national incidence rate of Lyme disease has been rising since 2009, underscoring the need for continued prevention and awareness efforts.
Introduction
Vector-borne diseases are infectious diseases caused by bacteria, viruses and parasites that are transmitted to humans from insects. Lyme disease is the most commonly reported vector-borne disease in Canada. Lyme disease is a bacterial infection caused by Borrelia burgdorferi and transmitted to humans through the bite of an infected tick; the blacklegged tick, Ixodes scapularis, in Manitoba, central and eastern Canada and the western blacklegged tick, Ixodes pacificus, in British Columbia. In Alberta, Saskatchewan, and the three northern Territories, no known endemic areas of blacklegged tick populations have been identified to dateFootnote 1Footnote 2. The ticks become infected after feeding on infected small mammals and birds.
Lyme disease can cause a range of clinical manifestations in humans. In the early stage of disease, flu-like symptoms, including joint pain, and erythema migrans rash are common. If untreated, individuals may experience cardiac, neurologic, and musculoskeletal manifestations such as arthritis.
Over the past decade, there has been an increase in the number of locally acquired Lyme disease cases. This occurred in part due to changes in climate, which has contributed to increases in the abundance and geographic range of blacklegged tick populations in central and eastern Canada.
Surveillance for ticks and human Lyme disease cases are conducted using a "One Health" approach. This helps provide information such as the burden of Lyme disease in Canada, trend in infection rates, and changes in tick populations. Applying this knowledge to public health actions including programs and policies can then help minimize the burden of Lyme disease and other emerging tick-borne diseases thereby protecting the health of Canadians.
This report focuses on the human component of the Lyme disease surveillance program, by providing an overview of surveillance data on cases reported between January 1, 2022 and December 31, 2022.
Methods
Since becoming nationally notifiable in 2009, human cases of Lyme disease in Canada have been reported voluntarily to the Public Health Agency of Canada (PHAC) by provincial/territorial health ministries/agencies through the Canadian Notifiable Disease Surveillance System (CNDSS). Information collected through CNDSS include age, sex, and case classification (confirmed and probable cases). In 2011, in collaboration with provincial and territorial partners, PHAC developed and implemented the Lyme Disease Enhanced Surveillance (LDES) system whereby participating jurisdictions (eight provinces in 2022) report information in addition to what is collected by the CNDSS, including information on geographic location of infection acquisition, clinical features and laboratory resultsFootnote 3.
Data obtained from provincial/territorial notifiable disease systems represent a snapshot at the time of data extraction. As a result, potential future changes may cause the data to differ from previous/subsequent reports, data displayed by provincial health authorities and from CNDSS. Lyme disease cases reported to PHAC are classified using the national Lyme disease 2016 case definitionFootnote 3.
Results
Change in incidence over time
In 2022, 2,525 cases of Lyme disease including locally acquired and travel-related cases were reported in Canada. Of these, 2,093 (82.9%) were confirmed and 432 (17.1%) were probable cases.
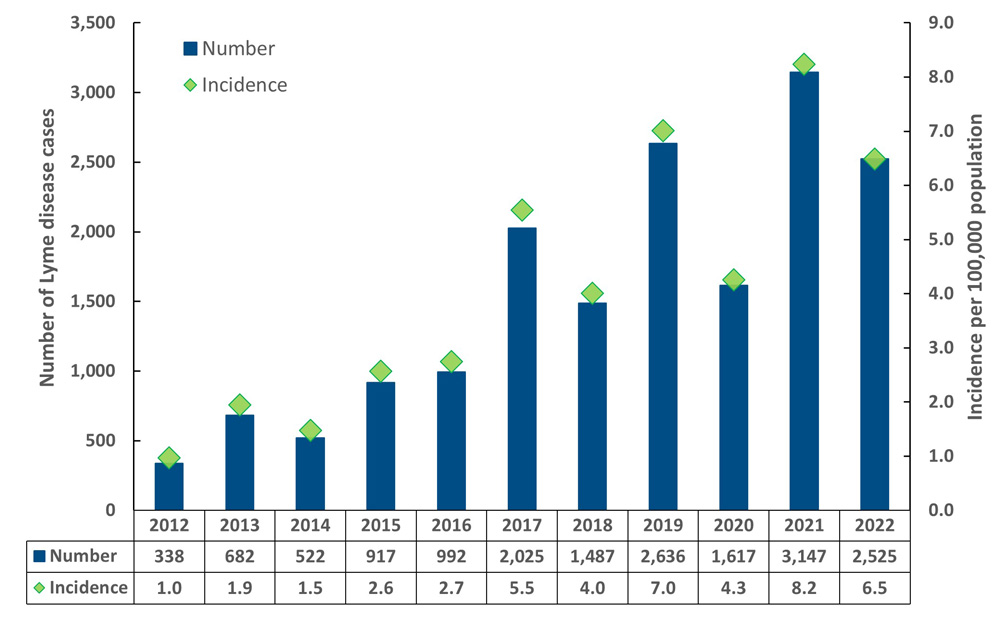
Text description
| Year | Number of cases | Incidence per 100 000 population |
|---|---|---|
| 2012 | 338 | 1.0 |
| 2013 | 682 | 1.9 |
| 2014 | 522 | 1.5 |
| 2015 | 917 | 2.6 |
| 2016 | 992 | 2.7 |
| 2017 | 2,025 | 5.5 |
| 2018 | 1,487 | 4.0 |
| 2019 | 2,636 | 7.0 |
| 2020 | 1,617 | 4.3 |
| 2021 | 3,147 | 8.2 |
| 2022 | 2,525 | 6.5 |
Geographic distribution
Most cases (94.7%) were reported from Ontario (n=1,478), Québec (n=586) and Nova Scotia (n=326) with the highest incidence per 100,000 population being reported in Nova Scotia (32.0 per 100,000 population) (Figure 2). This was nearly 5-fold greater than the national incidence (6.5 per 100,000 population). No cases were reported in the Yukon Territory, Northwest Territories, Nunavut, or Newfoundland and Labrador.
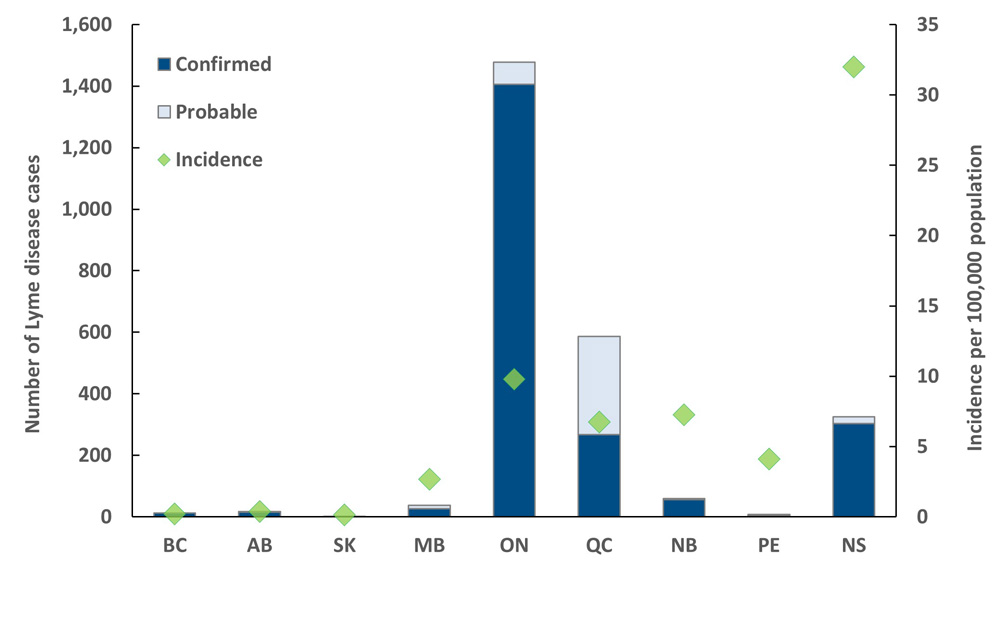
Text description
| Province / territory | Cases – confirmed | Cases – probable | Total | Incidence per 100 000 population |
|---|---|---|---|---|
| British Columbia | 12 | 0 | 12 | 0.23 |
| Alberta | 16 | 1 | 17 | 0.37 |
| Saskatchewan | 2 | 0 | 2 | 0.17 |
| Manitoba | 27 | 11 | 38 | 2.7 |
| Ontario | 1,406 | 72 | 1,478 | 9.78 |
| Quebec | 267 | 319 | 586 | 6.74 |
| New Brunswick | 57 | 2 | 59 | 7.27 |
| Prince Edward Island | 3 | 4 | 7 | 4.1 |
| Nova Scotia | 303 | 23 | 326 | 31.97 |
| Newfoundland and Labrador | 0 | 0 | 0 | 0 |
| Yukon | 0 | 0 | 0 | 0 |
| Northwest Territories | 0 | 0 | 0 | 0 |
| Nunavut | 0 | 0 | 0 | 0 |
Note: In Nova Scotia, due to competing public health priorities in the COVID-19 pandemic, Lyme disease case data were not consistently entered into Panorama, not validated, and therefore under-represent the true burden of diseaseFootnote 4.
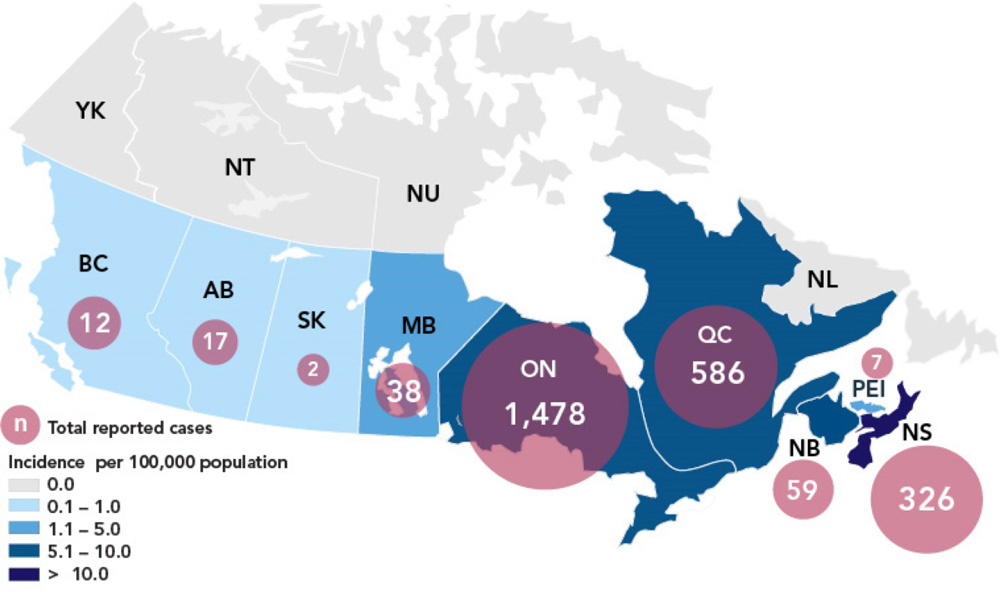
Text description
| Province / territory | Total reported cases | Incidence per 100 000 population |
|---|---|---|
| British Columbia | 12 | 0.23 |
| Alberta | 17 | 0.37 |
| Saskatchewan | 2 | 0.17 |
| Manitoba | 38 | 2.7 |
| Ontario | 1,478 | 9.78 |
| Quebec | 586 | 6.74 |
| New Brunswick | 59 | 7.27 |
| Nova Scotia | 326 | 31.97 |
| Prince Edward Island | 7 | 4.1 |
| Newfoundland and Labrador | 0 | 0 |
| Yukon | 0 | 0 |
| Northwest Territories | 0 | 0 |
| Nunavut | 0 | 0 |
Note: In Nova Scotia, due to competing public health priorities in the COVID-19 pandemic, Lyme disease case data were not consistently entered into Panorama, not validated, and therefore under-represent the true burden of diseaseFootnote 4.
Travel-related cases
Lyme disease is commonly acquired in areas of Canada where blacklegged tick populations are established (i.e., risk areas) or through travel to countries where the disease is endemic. In 2022, information about travel history was available for 2,054 Lyme disease cases (81.3%). Of these, 59 Lyme disease cases (2.9%) were likely infected during travel outside of Canada.
Demographic characteristics
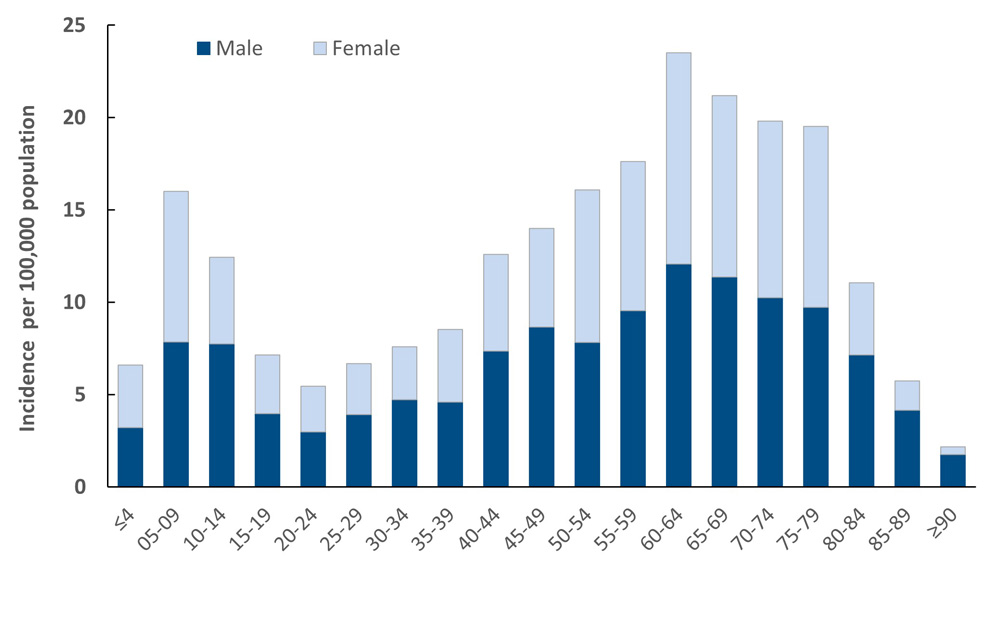
In 2022, information on age and sex was available for 2,513 cases (99.5%). The average and median age of reported Lyme disease cases was 47 and 53 years old, respectively. The incidence per 100,000 population for all reported Lyme disease cases exhibited a bimodal pattern with peaks in children aged 5–14 years (11.9% of cases) and adults aged 60–79 years (34.9% of cases) (Figure 4). Incidence in males was higher than females in the majority of age groups, and overall, 54.1% of cases were male (n=1,359).
Text description
| Age | Incidence per 100 000 – Male | Incidence per 100 000 – Female |
|---|---|---|
| ≤4 | 3.21 | 3.38 |
| 05-09 | 7.85 | 8.15 |
| 10-14 | 7.74 | 4.7 |
| 15-19 | 3.97 | 3.17 |
| 20-24 | 2.97 | 2.49 |
| 25-29 | 3.92 | 2.77 |
| 30-34 | 4.73 | 2.86 |
| 35-39 | 4.6 | 3.93 |
| 40-44 | 7.35 | 5.25 |
| 45-49 | 8.65 | 5.35 |
| 50-54 | 7.82 | 8.27 |
| 55-59 | 9.55 | 8.07 |
| 60-64 | 12.08 | 11.42 |
| 65-69 | 11.36 | 9.83 |
| 70-74 | 10.25 | 9.57 |
| 75-79 | 9.73 | 9.8 |
| 80-84 | 7.16 | 3.9 |
| 85-89 | 4.15 | 1.6 |
| ≥90 | 1.76 | 0.42 |
Seasonality
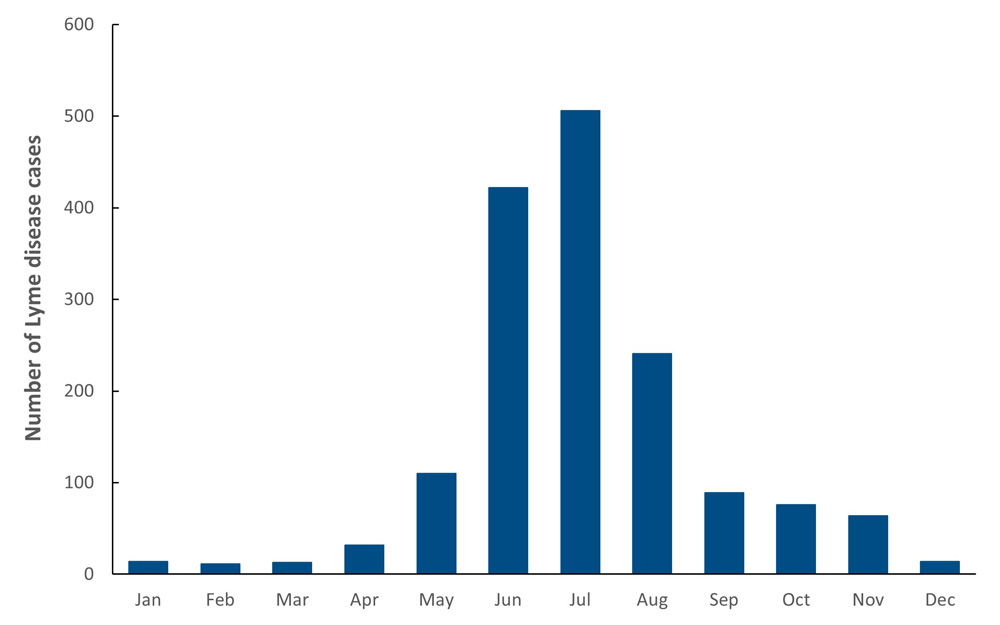
In 2022, 1,592 locally acquired cases included a date of illness onset. Lyme disease cases occurred in every month of the year; however, 94.7% occurred between May and November. More than 73.4% of the cases had a reported illness onset during the months of June (26.5%), July (31.8%), and August (15.1%) (Figure 5).
Text description
| Month | Number of cases |
|---|---|
| January | 14 |
| February | 11 |
| March | 13 |
| April | 32 |
| May | 110 |
| June | 422 |
| July | 506 |
| August | 241 |
| September | 89 |
| October | 76 |
| November | 64 |
| December | 14 |
Discussion
In 2022, nine provinces reported 2,525 cases of Lyme disease to PHAC, representing a year-over-year decrease of reported cases of 19.8% compared to the previous year. Similar fluctuations have occurred in previous years in 2014, 2018, and 2020, likely due to multiple factors such as the strain put on the healthcare system by the COVID-19 pandemic, public health prevention efforts and inter-annual variations in weather affecting tick activityFootnote 5Footnote 6Footnote 7.
Overall, the incidence continues to remain high due to factors such as greater human exposure to risk areas and to risk of infection. Climate change may increase the risk of human exposure by contributing to the expansion of habitat suitable for blacklegged ticks in eastern CanadaFootnote 8Footnote 9, landscape changes, greater activity and range of ticks and their hostsFootnote 10, as well as by leading to an increase in outdoor human activity due to the longer and warmer seasons. Other factors include more frequent detection and reporting due to enhanced surveillance and greater awareness among clinicians and the public.
Factors that may explain the variation in the proportion of cases classified as confirmed or probable between provinces may include the difference in surveillance effort and investigation procedures for reported cases. These efforts can vary according to the evolution of the endemicity of the disease in the respective jurisdiction.
Children aged 5−14 years and adults aged 60-79 years were the age groups with higher risk of acquiring Lyme disease, and, for most age groups, incidence was higher in males. These age groups are likely at greater risk of Lyme disease infection due to behavioural differences that increase their exposure to ticks. For example, there may be greater tendency to engage in outdoor activities such as gardening and playing near leaf litter or greater awareness of risk and precautions during such activities in some age groups over others.
These observed age and sex variations in risk are similar to findings from previous years in Canada and in the USAFootnote 3Footnote 5Footnote 6Footnote 11Footnote 12Footnote 13. It remains important to target these at-risk groups to enhance awareness and promote the adoption of preventative measures and reduce their risk of Lyme disease.
Illness onset was reported in every month of the year, with the majority of cases reported to have occurred between May and November. As observed in previous years in Canada and in the USA, more illness onset was reported in summer months, peaking in June and JulyFootnote 3Footnote 11Footnote 13. This corresponds to the season in which ticks, and, specifically, nymphal ticks that are harder to spot, are most actively seeking hosts and when Canadians are more likely to participate in outdoor activitiesFootnote 14. As a result, Canadians should be aware of the risk of tick bites during such activities as gardening, camping, hiking and outdoor excursions.
As in previous years, a large proportion of reported cases acquired infection in locations in southern and southeastern Ontario, southern Québec and in Nova Scotia, where the main vector of Lyme disease, the blacklegged tick is established. In British Columbia, Lyme disease incidence remained low and stable, in part due to lower prevalence of the pathogen among western blacklegged ticksFootnote 15.
Outside of Canada, there continues to be a risk of Lyme disease infection for travellers visiting endemic regions in the USA and Europe. The number of cases identified as likely acquired during foreign travel is larger than recent years. The decrease in recent years was likely due to travel restrictions associated with the COVID-19 pandemic that influenced travel patterns and reduced the risk of foreign travel-related disease acquisition.
Public health conclusions
Lyme disease continues to be the most frequently reported vector-borne disease in Canada. Although there was a dip in the number of reported cases in 2022, this has occurred in the past, and the overall trend continues to rise. It is estimated that the number of reported Lyme disease cases will continue to increase in the futureFootnote 16. This trend will be influenced by several factors including the local abundance of infected tick populations, including in urban areas, and the continued range expansion of tick populations in Canada associated with anticipated warmer temperatures.
The key findings of this report highlight the importance of sustained human and vector surveillance, as well as preventative strategies, especially enhancing public awareness regarding ways to prevent tick bites, to minimize the burden of Lyme disease in Canada.
Acknowledgements
The Public Health Agency of Canada acknowledges the provincial and territorial partners for their participation in the Canadian Notifiable Disease Surveillance System (CNDSS) and Lyme Disease Enhanced Surveillance (LDES) system.
References
- Footnote a
-
The denominators used to calculate the incidences were obtained from Statistics Canada, population estimates on July 1st.
- Footnote b
-
Cases reported in Alberta, Saskatchewan, and Prince Edward Island with known exposure were travel-related only.
- Footnote 1
-
Guillot C, Badcock J, Clow K, Cram J, Dergousoff S, Dibernardo A, et al. Sentinel surveillance of Lyme disease risk in Canada, 2019: Results from the first year of the Canadian Lyme Sentinel Network (CaLSeN). Can. Commun. Dis. Rep. 2020;46(10):354.
- Footnote 2
-
Chilton NB, Curry PS, Lindsay LR, Rochon K, Lysyk TJ, Dergousoff SJ. Passive and active surveillance for Ixodes scapularis (Acari: Ixodidae) in Saskatchewan, Canada. J. Med. Entomol. 2019; 57(1):156.
- Footnote 3
-
Gasmi S, Koffi JK, Nelder MP, Russell C, Graham-Derham S, Lachance L, et al. Surveillance for Lyme disease in Canada, 2009–2019. Can. Commun. Dis. Rep. 2022; 48(5):219.
- Footnote 4
-
Government of Nova Scotia. Notifiable Diseases in Nova Scotia 2022 Surveillance Report. https://novascotia.ca/dhw/populationhealth/documents/Annual-Notifiable-Disease-Surveillance-Report-2022.pdf. p.19. [Accessed 2024 Jan 10].
- Footnote 5
-
Public Health Agency of Canada. Lyme disease surveillance report: Annual report 2018; 2023. https://www.canada.ca/en/public-health/services/publications/diseases-conditions/surveillance-lyme-disease-annual-edition-2018.html [Accessed 2023 Oct 30].
- Footnote 6
-
Public Health Agency of Canada. Lyme disease surveillance report: Annual report 2020; 2023. https://www.canada.ca/en/public-health/services/publications/diseases-conditions/lyme-disease-surveillance-canada-annual-edition-2020.html [Accessed 2023 Oct 30].
- Footnote 7
-
McCormick DW, Kugeler KJ, Marx GE, Jayanthi P, Dietz S, Mead P, et al. Effects of COVID-19 pandemic on reported Lyme disease, United States, 2020. Emerg. Infect. Dis. 2021; 27(10):2715.
- Footnote 8
-
Robinson EL, Jardine CM, Koffi JK, Russell C, Lindsay LR, Dibernardo A, et al. Range Expansion of Ixodes scapularis and Borrelia burgdorferi in Ontario, Canada, from 2017 to 2019. Vector-Borne Zoonotic Dis. 2022;22(7):361.
- Footnote 9
-
Bouchard C, Leonard E, Koffi JK, Pelcat Y, Peregrine A, Chilton N, et al. The increasing risk of Lyme disease in Canada. Can. Vet. J. 2015;56(7):693.
- Footnote 10
-
Simon JA, Marrotte RR, Desrosiers N, Fiset J, Gaitan J, Gonzalez A, et al. Climate change and habitat fragmentation drive the occurrence of Borrelia burgdorferi, the agent of Lyme disease, at the northeastern limit of its distribution. Evol. Appl. 2014;7(7):750.
- Footnote 11
-
Public Health Agency of Canada. Lyme disease surveillance report: Annual report 2021; 2023. https://www.canada.ca/en/public-health/services/publications/diseases-conditions/lyme-disease-surveillance-canada-annual-edition-2021.html [Accessed 2023 Dec 18].
- Footnote 12
-
Ogden NH, Koffi JK, Lindsay LR, Fleming S, Mombourquette DC, Sanford C, et al. Vector-borne diseases in Canada: Surveillance for Lyme disease in Canada, 2009 to 2012. Can. Commun. Dis. Rep. 2015; 41(6):132.
- Footnote 13
-
Schwartz AM, Hinckley AF, Mead PS, Hook SA, Kugeler KJ. Surveillance for Lyme Disease-United States, 2008-2015. Morb. Mortal. Wkly Rep. 2017; 66(22):1.
- Footnote 14
-
Kurtenbach K, Hanincová K, Tsao JI, Margos G, Fish D, Ogden NH. Fundamental processes in the evolutionary ecology of Lyme borreliosis. Nat. Rev. Microbiol. 2006; 4(9):660.
- Footnote 15
-
Morshed MG, Lee M-K, Man S, Fernando K, Wong Q, Hojgaard A, et al. Surveillance for Borrelia burgdorferi in Ixodes ticks and small rodents in British Columbia. Vector Borne Zoonotic Dis. 2015;15(11):701.
- Footnote 16
-
Bouchard C, Dibernardo A, Koffi JK, Wood H, Leighton PA, Lindsay LR. Increased risk of tick-borne diseases with climate change. Can. Commun. Dis. Rep. 2019;45(4):81.