Lyme disease surveillance in Canada: Annual edition 2019
Download in PDF format
(942 Kb, 11 pages)
- Organization: Public Health Agency of Canada
- Date published: October 2023
On this page
- 2019 surveillance highlights
- Introduction
- Methods
- Results
- Discussion
- Public health conclusions
- Acknowledgements
- References
2019 surveillance highlights
- A total of 2,634 human cases of Lyme disease were reported to the Public Health Agency of Canada, of which, 1,900 (72%) were confirmed cases and 734 (28%) probable cases.
- Incidence peaked in adults aged 55−79 years (46% of cases) and children aged 5−14 years (11% of cases) with a predominance in males.
- 38% of cases reported an illness onset in July.
- 95% of cases were reported in Ontario, Quebec and Nova Scotia.
- 6% of the reported cases were likely infected during travel outside of Canada.
Introduction
Vector-borne diseases are infectious diseases caused by bacteria, viruses and parasites that are transmitted to humans from animals or insects. Lyme disease is the most commonly reported vector-borne disease in Canada. Lyme disease is a bacterial infection caused by Borrelia burgdorferi and transmitted to humans through the bite of an infectious tick; the blacklegged tick, Ixodes scapularis, in Manitoba, central and eastern Canada and the western blacklegged tick, Ixodes pacificus, in British Columbia. In Alberta and Saskatchewan, no known endemic areas of blacklegged tick populations have been detectedFootnote 1. The ticks become infected after feeding on infected small mammals and birds. Lyme disease can cause a range of clinical manifestations in humans. In the early stage of disease flu-like symptoms including joint pain and erythema migrans rash are common. If untreated, individuals may experience cardiac and neurologic manifestations and arthritis.
Over the past decade, there has been an increase in the number of locally acquired Lyme disease cases in part due to the changes in climate, which has contributed to increases in the abundance and geographic range of blacklegged tick populations in central and eastern Canada. Surveillance for ticks and human Lyme disease cases are conducted using a One Health approach to minimize the burden of Lyme disease and other emerging tick-borne diseases and protect the health of Canadians. This report focuses on the human component of Lyme disease surveillance, by providing an overview of surveillance data on cases reported in 2019.
Methods
Since becoming nationally notifiable in 2009, human cases of Lyme disease in Canada have been reported voluntarily to the Public Health Agency of Canada (PHAC) by provincial/territorial health ministries/agencies through the Canadian Notifiable Disease Surveillance System (CNDSS). Information collected through CNDSS include age, sex and case classification (probable and confirmed case). In 2011, in collaboration with provincial and territorial partners, PHAC developed and implemented the Lyme Disease Enhanced Surveillance (LDES) system whereby participating jurisdictions (eight provinces in 2019) report information in addition to what is collected by the CNDSS, including information on geographic location of infection acquisition, clinical features and laboratory resultsFootnote 2. Data obtained from provincial/territorial notifiable disease systems represent a snapshot at the time of data extraction and may differ from previous/subsequent reports, data displayed by provincial health authorities and from CNDSS. Lyme disease cases reported to PHAC are classified using the national Lyme disease 2016 case definition.
Results
Change in incidence over time
In 2019, 2,634 human cases of Lyme disease including locally acquired and travel related were reported in Canada. Of these, 1,900 (72.2%) were confirmed and 734 (27.8%) were probable cases. With the exception of 2014 and 2018, the annual number of total reported Lyme disease cases increased from 144 in 2009 to 2,634 in 2019 (an incidence of 0.4 and 7.0 per 100 000 population, respectively) (Figure 1).
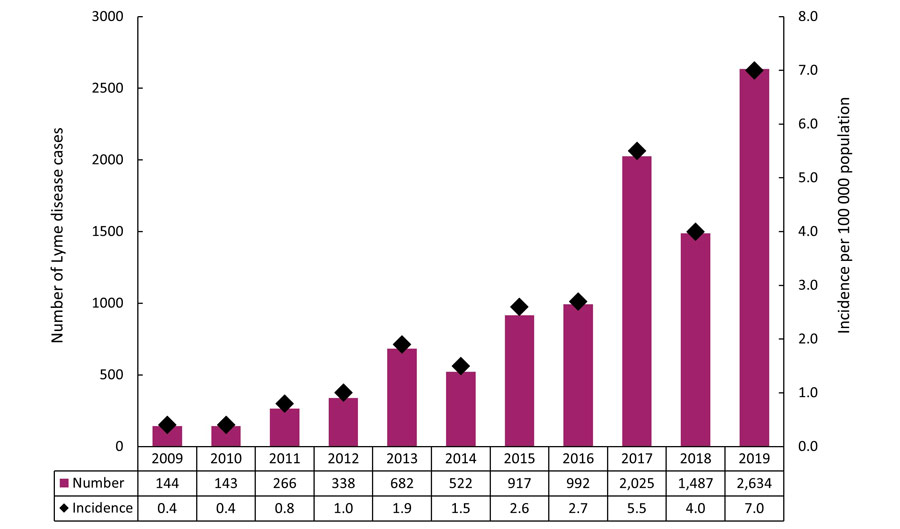
Figure 1 - Text description
| Year | Number of cases | Incidence per 100 000 population |
|---|---|---|
| 2009 | 144 | 0.4 |
| 2010 | 143 | 0.4 |
| 2011 | 266 | 0.8 |
| 2012 | 338 | 1.0 |
| 2013 | 682 | 1.9 |
| 2014 | 522 | 1.5 |
| 2015 | 917 | 2.6 |
| 2016 | 992 | 2.7 |
| 2017 | 2,025 | 5.5 |
| 2018 | 1,487 | 4.0 |
| 2019 | 2,634 | 7.0 |
Geographic distribution
The majority of all cases (94.8%) were reported from Ontario (n=1,168), Nova Scotia (n=830) and Quebec (n=500) (Figure 2). The province with the highest incidence was Nova Scotia (85.6 per 100 000 population) which is 12 folds greater than the national incidence (7.0 per 100 000 population). In 2019, Ontario, Quebec and Nova Scotia reported an increase in Lyme diseases cases by more than 60% compared to 2018.
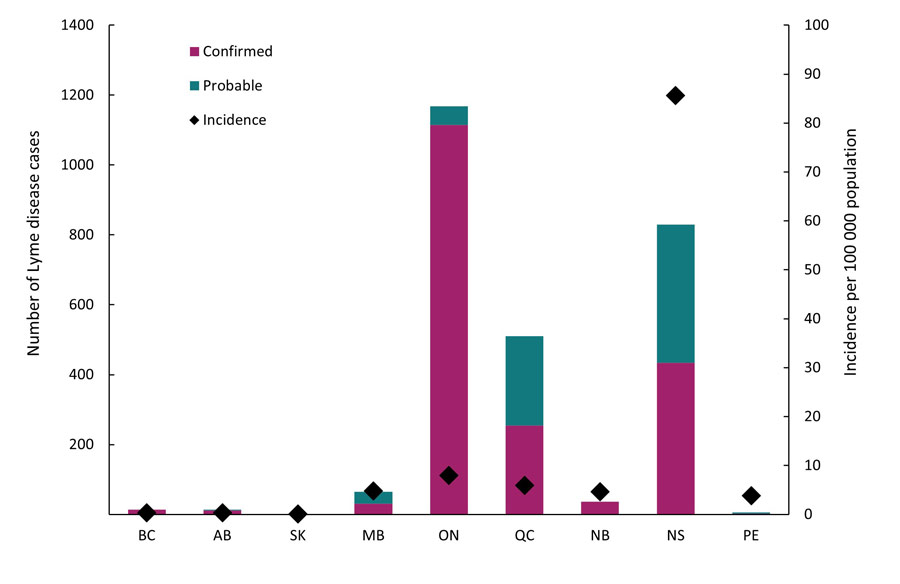
Figure 2 - Text description
Abbreviations: BC, British Columbia; AB, Alberta; SK, Saskatchewan; MB, Manitoba; ON, Ontario; QC, Quebec; NB, New Brunswick; NS, Nova Scotia; PE, Prince Edward Island; NL, Newfoundland & Labrador; YT, Yukon; NT, Northwest Territories; NU, Nunavut
Notes: Probable cases are not reported in British Columbia and Saskatchewan. Cases reported by Alberta, Prince Edward Island and Saskatchewan were travel-related only. No cases have been reported by Yukon, Northwest Territories, Nunavut and Newfoundland & Labrador for 2019.
| Province/Territory | Case classification | Total | Incidence per 100 000 population | |
|---|---|---|---|---|
| Confirmed | Probable | |||
| British Columbia | 14 | 0 | 14 | 0.3 |
| Alberta | 12 | 2 | 14 | 0.3 |
| Saskatchewan | 1 | 0 | 1 | 0.1 |
| Manitoba | 31 | 34 | 65 | 4.8 |
| Ontario | 1,115 | 53 | 1,168 | 8 |
| Quebec | 255 | 255 | 500 | 5.9 |
| New Brunswick | 36 | 0 | 36 | 4.6 |
| Nova Scotia | 434 | 396 | 830 | 85.6 |
| Prince Edward Island | 2 | 4 | 6 | 3.8 |
| Newfoundland & Labrador | 0 | 0 | 0 | 0 |
| Yukon | 0 | 0 | 0 | 0 |
| Northwest Territories | 0 | 0 | 0 | 0 |
| Nunavut | 0 | 0 | 0 | 0 |
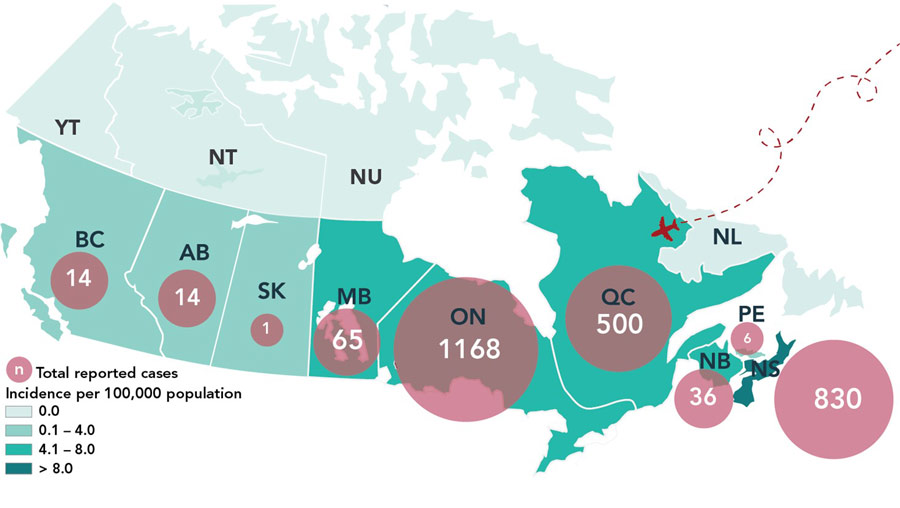
Figure 3 - Text description
In 2019, the majority of locally reported cases are concentrated in locations in southern Manitoba, southern and southeastern Ontario, southern Quebec and in Nova Scotia.
| Province | Total Reported Cases | Incidence per 100 000 population |
|---|---|---|
| British Columbia | 14 | 0.3 |
| Alberta | 14 | 0.3 |
| Saskatchewan | 1 | 0.1 |
| Manitoba | 65 | 4.8 |
| Ontario | 1,168 | 8 |
| Quebec | 500 | 5.9 |
| New Brunswick | 36 | 4.6 |
| Nova Scotia | 830 | 85.6 |
| Prince Edward Island | 6 | 3.8 |
Travel-related cases
Lyme disease is commonly acquired in areas of Canada where blacklegged tick populations are established (i.e., at-risk areas) or through travel to countries where the disease is endemic. In 2019, information about travel-history was available for 2,192 Lyme disease cases. Of these, 139 Lyme disease cases (6.4%) were likely infected during travel outside of Canada to the USA (n=89) and Europe (n=50).
Demographic characteristics
In 2019, information on age and sex was available for 2,633 cases. The average age of reported Lyme disease cases was 48 years old. The incidence per 100 000 population for all reported Lyme disease cases exhibited a bimodal pattern with two peaks of high incidence among children aged 5−14 years and adults aged 55−79 years (Figure 4), representing 11.2% and 45.9% of all cases, respectively. Except for the 0−4 and ≥ 90 age groups, incidence in males was higher than females, and overall 57.3% of cases were male (n=1,510).
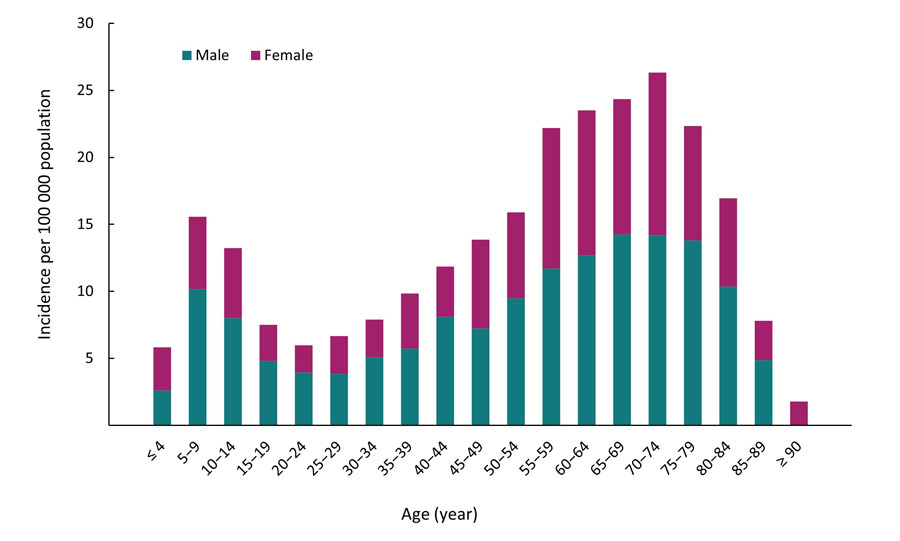
Figure 4 - Text description
| Age (year) | Incidence per 100 000 | |
|---|---|---|
| Male | Female | |
| ≤ 4 | 2.6 | 3.2 |
| 5−9 | 10.2 | 5.4 |
| 10−14 | 8.0 | 5.2 |
| 15−19 | 4.8 | 2.7 |
| 20−24 | 3.9 | 2.0 |
| 25−29 | 3.8 | 2.8 |
| 30−34 | 5.1 | 2.8 |
| 35−39 | 5.7 | 4.1 |
| 40−44 | 8.1 | 3.8 |
| 45−49 | 7.2 | 6.6 |
| 50−54 | 9.5 | 6.4 |
| 55−59 | 11.7 | 10.5 |
| 60−64 | 12.7 | 10.8 |
| 65−69 | 14.3 | 10.1 |
| 70−74 | 14.2 | 12.1 |
| 75−79 | 13.8 | 8.5 |
| 80−84 | 10.3 | 6.6 |
| 85−89 | 4.9 | 2.9 |
| ≥ 90 | 0.0 | 1.8 |
Seasonality
In 2019, Lyme disease cases were reported in every month; however, 96.7% of the cases occurred from May through November. More than 75.4 % of the cases had symptom onset during the summer months of June (15.2%), July (37.9%) and August (22.3%) (Figure 5).
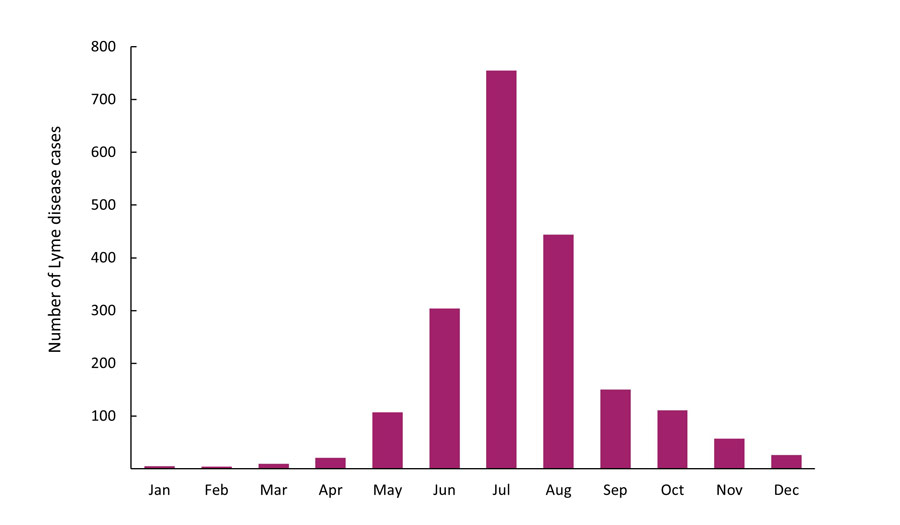
Figure 5 - Text description
| Month | 2019 |
|---|---|
| January | 5 |
| February | 4 |
| March | 10 |
| April | 21 |
| May | 107 |
| June | 304 |
| July | 755 |
| August | 444 |
| September | 150 |
| October | 111 |
| November | 57 |
| December | 26 |
Discussion
In 2019, nine provinces reported 2,634 cases of Lyme disease to PHAC, representing an increase of 77.2% compared to the previous year. This increase has resulted in the highest total number of Lyme diseases cases reported in Canada since 2009. The rise in the number of reported cases in 2019 reflects an increase in human exposure and infection, as well as an increase in detection and reporting through enhanced clinician and public awareness. Overall, the long-term risk of human infection is increasing in Canada partly due to changes in climate, which is contributing to the range expansion of blacklegged ticks in eastern CanadaFootnote 3 and additional factors that may increase the risk of human exposure including the uptake of outdoor activity, landscape changes and the abundance, activity and range of ticks and hostsFootnote 4,Footnote 5. In addition, it is common for underreporting to occur in surveillance systems, as cases may be undetected or not reportedFootnote 6.
In 2019, children aged 5−14 years and adults aged 55−79 years were the age groups with higher risk of acquiring Lyme disease, and for nearly all age groups incidence was higher in males. These observed age and sex variations in risk are similar to findings from previous years in CanadaFootnote 7,Footnote 8 highlighting the importance of targeting these at-risk groups to promote the adoption of preventative measures to reduce the risk of Lyme disease.
Reported illness onset occurred throughout the year, with a majority of cases reported between May and November. The peak month of illness onset was in July, similar to observations for previous years in Canada and the United StatesFootnote 9.The reported illness onset was higher in summer months which corresponds to the season in which ticks are most actively seeking hosts and Canadians are more likely to participate in outdoor activitiesFootnote 10.
A large proportion of reported cases acquired infection in locations in southern Manitoba, southern and southeastern Ontario, southern Quebec and in Nova Scotia, where the main vector of Lyme disease, the blacklegged tick is established. For western provinces, only a small number of locally-acquired cases were reported in British Columbia. The incidence of Lyme disease in British Columbia remains stable compared to 2018, in part due to a smaller number of western blacklegged ticks being infected with the pathogen compared to blacklegged ticks established in central and eastern CanadaFootnote 11.
The majority of the 139 travel-related cases acquired infection in the USA and Europe based on available information on travel history. It is important that Canadians travelling to endemic areas in the USA and Europe to be aware of the risk of infection when participating in outdoor activities and use personal protective measures to prevent tick bites and Lyme disease.
Public health conclusions
Lyme disease continues to be the most frequently reported vector-borne disease in Canada. The number of cases increased in 2019. Overall, there has been an upward trend of reported Lyme diseases in Canada since 2009. It is estimated that the number of reported Lyme disease cases will continue to increase in the future. This trend will be influenced by several factors including the local abundance of infected tick populations, and the continued range expansion of tick populations in Canada.
The key findings of this report highlight the importance of sustained human and vector surveillance and preventative strategies, especially enhancing public awareness, in order to minimize the burden of Lyme disease in Canada.
Acknowledgements
The Public Health Agency of Canada acknowledges the provincial and territorial partners for their participation in the Canadian Notifiable Disease Surveillance System (CNDSS) and Lyme Disease Enhanced Surveillance (LDES) system.