Tuberculosis Disease in Canada, 2023 (infographic)
Download in PDF format
(522 KB, 2 pages)
Organization: Public Health Agency of Canada
Date published: 2025-01-31
Cat.: HP40-380/2023E-PDF
ISBN: 978-0-660-75450-5
Pub.: 240811
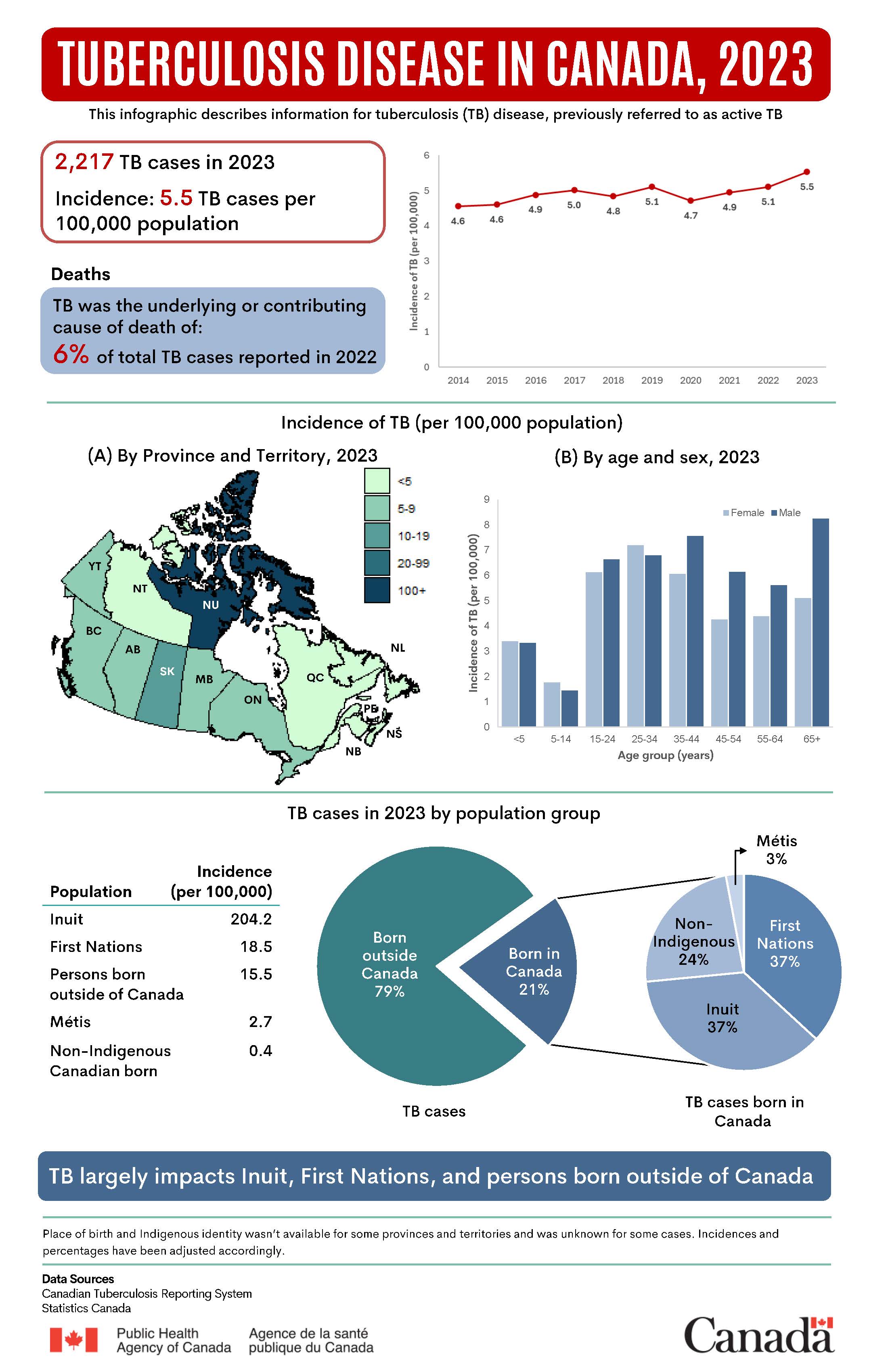
This infographic describes information for tuberculosis (TB) disease, previously referred to as active TB.
In 2023, there were 2,217 cases of TB reported in Canada. This corresponds to a rate of occurrence of new TB cases (incidence) of 5.5 cases per 100,000 population.
| Year | Incidence of TB (per 100,000 population) |
|---|---|
| 2014 | 4.6 |
| 2015 | 4.6 |
| 2016 | 4.9 |
| 2017 | 5.0 |
| 2018 | 4.8 |
| 2019 | 5.1 |
| 2020 | 4.7 |
| 2021 | 4.9 |
| 2022 | 5.1 |
| 2023 | 5.5 |
TB was the underlying or contributing cause of death of 6% of total TB cases reported in 2022.
The incidence of TB per 100,000 in 2023 varied across provinces and territories.
| Province or territory | Range of TB incidence (per 100,000 population) |
|---|---|
| Newfoundland and Labrador | Less than 5.0 |
| Nova Scotia | Less than 5.0 |
| Prince Edward Island | Less than 5.0 |
| New Brunswick | Less than 5.0 |
| Quebec | Less than 5.0 |
| Ontario | 5.0 to 9.9 |
| Manitoba | 5.0 to 9.9 |
| Saskatchewan | 10.0 to 19.9 |
| Alberta | 5.0 to 9.9 |
| British Columbia | 5.0 to 9.9 |
| Yukon | 5.0 to 9.9 |
| Northwest Territories | Less than 5.0 |
| Nunavut | Greater than 100.0 |
The incidence of TB per 100,000 population in 2023 varied by age and sex.
| Age group (years) | Female (per 100,000 population) | Male (per 100,000 population) |
|---|---|---|
| Younger than 5 | 3.4 | 3.3 |
| 5 to 14 | 1.8 | 1.4 |
| 15 to 24 | 6.1 | 6.6 |
| 25 to 34 | 7.2 | 6.8 |
| 35 to 44 | 6.1 | 7.6 |
| 45 to 54 | 4.3 | 6.1 |
| 55 to 64 | 4.4 | 5.6 |
| 65 and older | 5.1 | 8.2 |
In 2023, the incidence of TB per 100,000 population differed by population group:
- Inuit = 204.2
- First Nations = 18.5
- Persons born outside of Canada = 15.5
- Métis = 2.7
- Non-Indigenous Canadian-born = 0.4
By place of birth, 79% of TB cases in 2023 were born outside of Canada and 21% were born in Canada.
Of TB cases born in Canada, 37% were First Nations, 37% were Inuit, 24% were non-Indigenous and 3% were Métis.
TB largely impacts Inuit, First Nations, and persons born outside of Canada.
Place of birth and Indigenous identity wasn't available for some provinces and territories and was unknown for some cases. Incidences and percentages have been adjusted accordingly.
Data sources:
- Canadian Tuberculosis Reporting System
- Statistics Canada
Tuberculosis drug resistance
In 2023, 1,660 (89%) samples tested showed no resistance to first-lineFootnote 1 TB drugs, while 206 (11%) TB samples were resistantFootnote 2 to first-line drugs.
Of the 206 samples that were resistant to first-line drugs:
- 29 (1.6%) were multidrug-resistant
- 164 (8.8%) were mono-resistant
- 11 (0.6%) were poly-resistant
- 2 (0.1%) showed other resistance patterns, that are not one of the previously defined resistance patterns
Of the 29 (1.6%) samples that were multidrug-resistant, 4 (0.2%) were extensively drug-resistant.
Outlined in the following table is data on drug resistance patterns in TB samples from 2014 to 2023:
| Drug resistance pattern | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | 2021 | 2022 | 2023 |
|---|---|---|---|---|---|---|---|---|---|---|
| At least 1 first-line drug | 9.5% | 10.4% | 9.0% | 8.0% | 10.1% | 10.5% | 9.6% | 9.9% | 9.7% | 11.0% |
| Multidrug-resistant TB and/or rifampin-resistant TB | 1.8% | 1.8% | 1.2% | 1.0% | 1.9% | 1.4% | 1.3% | 1.5% | 1.6% | 1.8% |
| Extensively drug-resistant TB | 0.1% | 0.0% | 0.0% | 0.0% | 0.1% | 0.0% | 0.0% | 0.1% | 0.0% | 0.2% |
From 2014 to 2023, resistance to first-line TB drugs was consistently low (8% to 11% of samples). Resistance to rifampin and multidrug-resistant TB was consistently low (1% to 2% of samples). Extensively drug-resistant TB was rare and only reported in 2014, 2018 and 2021 (1 sample in each year). In 2023, 4 samples were reported.
Multidrug-resistant TB and/or rifampin-resistant TB were rare in children younger than 15 years old in the past decade.
In 2023, TB drug resistance was low and consistent with trends observed in the past decade in Canada.
The Public Health Agency of Canada is collaborating with Federal, Provincial, Territorial, and Indigenous partners to develop an approach for TB elimination in Canada.
Together, we can end TB.
Data source:
- Canadian Tuberculosis Laboratory Surveillance System
Footnotes
- Footnote 1
-
First-line TB drugs are part of the initial standard treatment regimen for TB disease. First-line drugs include the following antibiotics:
- rifampin
- isoniazid
- ethambutol
- pyrazinamide
Second-line TB drugs are used when first-line drugs are less effective, usually due to drug resistance. They include:
- fluoroquinolones, such as levofloxacin and moxifloxacin
- injectable drugs, such as kanamycin, amikacin and capreomycin
- bedaquiline
- linezolid
- Footnote 2
-
The definitions of drug resistance are:
- mono-resistance (resistance to only 1 first-line TB drug)
- poly-resistance (resistance to more than 1 first-line TB drug, without resistance to rifampin)
- rifampin-resistant TB (resistance to rifampin)
- multidrug-resistant TB (resistance to isoniazid and rifampin with or without resistance to other first-line TB drugs)
- extensively drug-resistant TB (multidrug-resistant TB with additional resistance to any fluoroquinolone and to at least 1 of the 3 injectable second-line TB drugs, or bedaquiline or linezolid)