Sustaining the Wellbeing of Military Healthcare Personnel during COVID-19 Pandemic
April 1, 2020 - Defence Stories
Adapted from guidelines by World Health Organization and Centre for the Study of Traumatic Stress.
The novel coronavirus pandemic has plunged healthcare systems worldwide into a stressful and uncertain time that puts considerable demand on medical staff.
Taking care of yourself, and encouraging others to look after themselves, sustains our ability to care for those in need and to maintain essential healthcare services as the situation evolves.
You owe it to yourself, your family, your team, and your patients to take some time to maintain your own health and wellbeing.
Challenges for Healthcare Personnel during the COVID-19 Pandemic
There are multiple sources of stress for healthcare workers and leaders, whether screening or treating those suspected to have COVID-19, or managing the ongoing essential care for our patients with other illness and injury.
- Surge in healthcare demands may cause conflict between personal responsibilities to family and professional demands such as working long hours.
- Ongoing risk of infection and the need to employ strict infection control measures demands constant awareness and vigilance.
- Higher demands in the work setting including long work hours, increased patient numbers and keeping up-to-date with best practices as information about COVID-19 develops.
- Use of Personal Protective Equipment can be uncomfortable, limit mobility and interfere with communication.
- Reduced capacity to use social supports and other stress relieving activities, such as physical exercise, due to intense work schedules, family responsibilities and limited access to the facilities.
- Providing emotional support to distressed patients and their families, as well as medical care, can be very draining.
- Helping those in need can be extremely rewarding, but this pandemic setting is unusually challenging and so healthcare workers may experience feelings such as grief, guilt, frustration, insomnia, and exhaustion.
- Fear that as a frontline healthcare worker one might pass COVID-19 onto their friends and family as a result of their work.
- Feelings of guilt or letting others down if you become sick with the illness or are in self-isolation.
Rest and recovery allow you to be at your best
Recognizing that this pandemic may take an emotional toll, below are some suggested positive coping strategies.
- Meet basic needs. Be sure to eat, consume fluids, be physically active, and sleep regularly. It is easy to “forget” to do these important things as you care for your patients, but becoming physiologically run-down puts you at risk, and may compromise your ability to care for patients.
- Take breaks. Even if all you have is a moment between patients, take a few deep breaths and look out the window or make a quick call home; if you have fifteen or thirty minutes, listen to music, take a walk outside, or connect with a colleague (while respecting physical distancing); when your shift is over, do something unrelated to work that you find comforting, fun or relaxing. Some people may feel guilty about taking time to relax when so many others are suffering; but, recognize that rest and recovery is part of being a good healthcare provider and leader, and making sure you are your best self at work.
- Create a menu of personal self-care activities that you enjoy and provide you much needed recovery time. Many find exercise or hobbies very helpful.
- Moderate use of caffeine, alcohol or recreational drugs. While in the short-term use of these may seem helpful, in the long term reliance on these substances can worsen your mental and physical wellbeing.
- Connect with colleagues while respecting different coping styles. Talk to your colleagues and receive support from one another. The people you work alongside understand what you are facing. Recall that some people like to talk while others prefer to recharge alone with their tablet or take a walk. Recognize and respect these differences in your patients and your colleagues.
- Communicate constructively and work as a team. Communicate with co-workers clearly and in a positive manner. Identify deficiencies or opportunities in work processes in a constructive way. Share your frustrations and work together to find solutions. Problem solving is a professional skill and it can be very satisfying to fix even small problems.
- Contact family and friends virtually. Set aside time to contact your loved ones. They can be a cornerstone of support outside the healthcare system. Schedule regular telephone calls or virtual group chats in addition to text messages.
- Stay informed, but avoid excessive exposure to media coverage of COVID-19. Periodically check the news and recommendations from trusted sites as the Government of Canada COVID-19 webpage and local health authorities, or the DND/CAF COVID-19 webpage. Take breaks from the news as it can be upsetting to hear about the crisis in a constant stream.
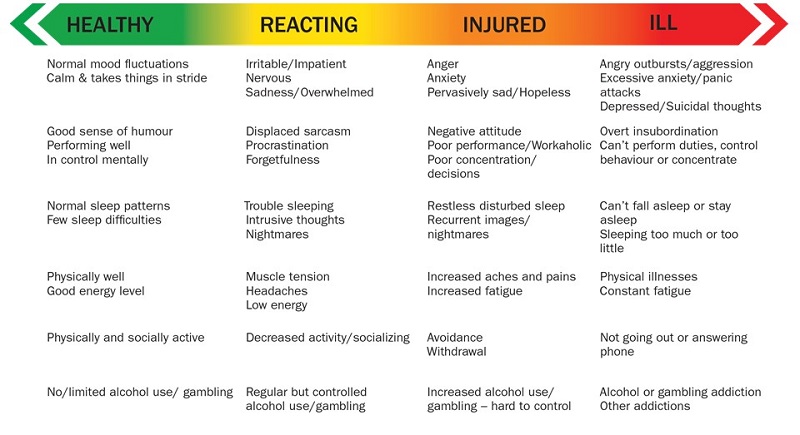
Mental Health Continuum Model - Text version
This diagram describes the range of mental health—healthy, reacting, injured and ill—and lists the behaviours associated with each part of this range.
Healthy behaviours include normal mood fluctuations, calmness and the ability to take things in stride, a good sense of humour, good performance, being in control, normal sleep patterns, few sleep difficulties, being physically well, having a good energy level, being physically and socially active, and limited or no alcohol use or gambling.
Reacting behaviours include being irritable or impatient, being nervous, being sad or overwhelmed, expressing displaced sarcasm, procrastination, forgetfulness, having trouble sleeping, having intrusive thoughts, having nightmares, having muscle tension or headaches, having low energy, decreased activity or socializing, and regular but controlled alcohol use or gambling.
Injured behaviours include anger, anxiety, pervasive sadness or hopelessness, a negative attitude, poor performance or workaholic behaviour, poor concentration or decisions, restless or disturbed sleep, recurrent images or nightmares, increased aches and pains, increased fatigue, avoidance, withdrawal, and increased alcohol use or hard-to-control gambling.
Ill behaviours include angry outbursts or aggression; excessive anxiety or panic attacks; depression or suicidal thoughts; overt insubordination; an inability to perform duties, control behaviour or concentrate; an inability to fall asleep or stay asleep; sleeping too much or too little; physical illnesses; constant fatigue; not going out or not answering phone; and an alcohol or gambling addiction or other addictions.
During times of increased stress, it is common for healthcare personnel, whether providing frontline patient care or in leadership roles, to enter the Reacting (Yellow) Zone of the Mental Health Continuum. This is a normal response, and most people will use their own positive coping strategies to manage the increased demands. It is important to monitor your health and wellbeing. Note any significant changes in behaviour (like those listed in the Injured (orange) or Ill (red) sections of the table) and listen to friends and family members if they express concern for you. Ask for help if you feel you are on the right-hand side of the Continuum, or are concerned about your ability to care for yourself, your family, or patients. Reach out as appropriate to a peer, supervisor or a professional.
- Remind yourself that despite obstacles or frustrations, you are fulfilling a critical role in this very difficult time.
- Recognize your colleagues—either formally or informally—for their contribution.
- Finally, recognize your positive experiences. It is okay to experience pride in your ability to cope and manage the situation, and to take satisfaction in your role of helping others.
If you, or someone you care about, are feeling overwhelmed with emotions like sadness, depression, or anxiety, reach out. Options include:
- CAF Member Assistance Program (CFMAP) or EAP 1-800-268-7708
- LifeSpeak – online health and wellness platform
- CAF Medical Clinic nearest you – psychosocial services and mental health program
- Military Family Resource Centres
- Family Information Line 1-800-866-4546
- Wing or Base Chaplain
- If it is an urgent or life-threatening situation – call 911
- Sexual Misconduct Response Centre
Services are available by calling
1-844-750-1648
24 hours a day / 365 days a year