A Prescription for Canada: Achieving Pharmacare for All
Final Report of the Advisory Council on the Implementation of National Pharmacare
Download the entire report
(PDF format, 3.11 MB, 184 pages)
Organization: Health Canada
Published: June 2019
Cat.: H22-4/18-2019E-PDF
ISBN: 978-0-660-30974-3
Pub.: 190051
Table of Contents
- Message from the Chair
- Acknowledgements
- Executive summary
- List of recommendations
- Chapter 1: Introduction
- Chapter 2: Drug coverage in Canada today
- Chapter 3: Key challenges facing Canada’s prescription drug system
- Chapter 4: A pharmacare plan for Canada
- Chapter 5: Getting to national pharmacare
- 5.1 Government collaboration
- 5.2 Indigenous engagement
- 5.3 Creating a Canadian drug agency
- 5.4 Developing a national formulary
- 5.5 Implementing a national formulary—starting with essential medicines
- 5.6 National strategy on appropriate prescribing and use of drugs
- 5.7 National strategy for expensive drugs for rare diseases
- Chapter 6: Financing national pharmacare
- Chapter 7: Ensuring the success of national pharmacare
- Chapter 8: What national pharmacare will mean for Canada
- Chapter 9: Conclusion
- Annex 1: Biographies
- Annex 2: Order in Council
- Annex 3: National dialogue participants
- Annex 4: Overview of provincial and territorial drug plans
- Annex 5: Key characteristics of the pharmacare systems in comparator countries
- Annex 6: Drug spending model
- Annex 7: Other pharmacare models considered
- Annex 8: Sex- and gender-based analysis
- References
Message from the Chair

Canadians have considered the idea of universal drug coverage, as a complement to universal health care, for over five decades. For such a long-standing debate there is a surprising level of consensus. After hearing from many thousands of Canadians, we found a strongly held, shared belief that everyone in Canada should have access to prescription drugs based on their need and not their ability to pay, and delivered in a manner that is fair and sustainable. That’s why our council has recommended that Canada implement universal, single-payer, public pharmacare.
If the promise of universal health care is that Canadians are there for each other when we’re sick, by not including prescription drugs we’re placing a limit on that commitment. We may enter the hospital or the doctor’s office with equal access to health care, but we don’t go home with the same prospects for a healthier future, because prescription drug coverage varies greatly from person to person, and from province to province. There are too many people in our country who die prematurely or suffer needlessly in ill health because cost is a barrier to accessing prescription drugs.
This gap—between our values and our reality—is growing because the nature of medicine is changing. When universal health care was first proposed, prescription drugs were important but not as commonly used and much less expensive. Today, drugs are the second-largest cost in Canadian health care, after hospitals and ahead of physician services. We heard from both public and private prescription drug providers that the current system is near the breaking point and in need of significant, even transformational, reform. The common refrain we heard from Canadians: we have to do better.
Even though many Canadians have some form of coverage, Canada relies on a confusing patchwork of over 100 public prescription drug plans and over 100,000 private plans—with a variety of premiums, copayments, deductibles and annual limits. For a family or a single patient with a complex condition, those costs can add up to a significant barrier. Approximately 20 per cent of Canadians have inadequate drug coverage or no coverage at all and must pay out of pocket. A recent study found almost 1 million Canadians had cut their household spending on food and heat to pay for medication. Another found that one in five households reported a family member who, in the past year, had not taken a prescribed medicine due to its cost.
This uneven, inconsistent and tenuous patchwork in no way resembles a “system.” There is no single, uniform method in Canada for a child with asthma to get her inhaler. It depends on her family’s coverage. There is no one consistent way that all cancer patients obtain take-home cancer drugs or medicines for coping with chemotherapy side effects. Some pay more. Some pay less. Some don’t have access to those medicines at all.
Over the past year, we saw provinces and territories taking action, working hard to provide better prescription drug coverage, but we also concluded that the federal government can and should do more, working in partnership with provincial and territorial governments, to ensure all Canadians can access the medicines they need.
There is a cost to universal pharmacare and we understand that governments have fiscal limits. But universal, single-payer, public pharmacare can save billions by lowering the price we pay for prescription medicines and by avoiding the greater costs that accumulate when a manageable condition becomes a serious health crisis or when complications develop because someone could not afford to take medicine as prescribed. It might be the person recently laid off who stops taking medicines for preventing heart attack or stroke. They don’t feel an immediate, daily difference when they take those pills. So, they question the expense when money is tight. They mean to get back on the medicine when they get back on their feet. But time runs out. They end up in an emergency room in crisis. They may now need ongoing home care. Any return to work is delayed or maybe never happens. Barriers to accessing prescribed medication can and do result in additional visits to the doctor’s office, emergency departments and hospital inpatient wards, all costing our society much more than the cost of that preventive medicine. Improving access to prescription medicine improves health outcomes, reduces health care visits, and saves billions in downstream health care costs.
Our current fractured system also weakens Canada’s negotiating position with pharmaceutical companies. We pay some of the highest drug prices in the world. Other countries with universal pharmacare get better deals for the same drugs. Without price reductions, our public and private drug plans will continue to be strained. Pharmaceutical research is producing a new generation of drugs that offer transformational benefits particularly for sufferers of chronic conditions and rare diseases. However, many of these drugs have costs that reach into the tens or even hundreds of thousands of dollars per person, per year. Such developments were not imagined when universal health care was enacted without prescription drug coverage. Canada can meet this challenge, but we need the purchasing power and unified effort of all 37 million Canadians. Already, employer-sponsored plans are having to increase premiums and copayments, and reduce health benefits, because of the growing cost of drugs. More and more drug costs are being passed down to employees. We heard from employers who question how long they can continue to afford to provide drug coverage at all.
Given the changing nature of work and the rising use and cost of drugs, we can’t be certain how many Canadians will have adequate drug coverage in the years ahead. If you believe that the concept of universal health care is part of who we are as Canadians, and I certainly do, then shouldn’t our understanding of that concept change with us—as our country, our economy and the practice of medicine evolve?
In Canada, we know that great national projects can go well beyond building things that we can see with our eyes. Canadians also build programs and initiatives that we can feel in our hearts. Among the generation who launched universal health care fifty years ago were people who had once looked at doctor’s bills and worried how they would pay. They enabled their governments to create a program so that no one in Canada would have that worry again. Today, most of us have never even seen an invoice from a doctor or a bill from a hospital, through the joys of childbirth, the pain of injury or the trials of illness. That’s just the Canada we know—and love.
We, too, can be the kind of generation that builds a national project that changes Canada for the better. Someday in the not-too-distant future, it is within our grasp that every Canadian could walk away from the pharmacy counter with what they need to get better and live better. We can fulfil that original promise of universal care, of being there for one another, and create a future where no Canadian goes without the medicine they need. That will simply, and proudly, be the Canada our children and grandchildren know and love. Ours can be the last generation to look at a prescription and worry how to pay.
Our council has heard the stories of thousands of Canadians and listened to a wide range of perspectives. The time for universal, single-payer, public pharmacare has come. This is our generation’s national project: better access to the medicines we need, improved health outcomes and a fairer and more sustainable prescription medicine system. Let’s complete the unfinished business of universal health care. That can be our promise, and our legacy, to each other and to all future generations.
Dr. Eric Hoskins, OC, MSC, DPhil, MSc, MD, FRCPC
Chair, Advisory Council on the Implementation of National Pharmacare
On behalf of Council members:
Dr. Nadine Caron
Vincent Dumez
Mia Homsy
Camille Orridge
Hon. Diana Whalen
John Wright
Acknowledgements
A report such as this does not come to fruition without a lot of hard work, creative insights and ideas from a diversity of perspectives and personal contributions from countless Canadians.
We would like to thank the Government of Canada, and more particularly the Right Honourable Justin Trudeau, Prime Minister, the Honourable Ginette Petitpas Taylor, Minister of Health and the Honourable Bill Morneau, Minister of Finance, for having placed their trust in all of us as council members. The council was created as an independent advisory body and was given a broad mandate to engage with Canadians and provide its best advice on how to implement national pharmacare. We were given the latitude to do our job with the full support of the government and without any preconceived notions of what national pharmacare should look like and how it should be implemented. For this, we are very grateful.
Throughout its work, the council benefited from extraordinary collaboration and input from provincial and territorial health ministers and senior officials. Health ministers, finance ministers, and in some cases premiers, readily shared their views with the council. Senior officials responsible for the management of public drug plans generously gave their time to engage with the council and the secretariat, and shared information that was critical in helping us understand the opportunities and challenges involved in moving forward with pharmacare.
We are also thankful for the candid conversations the council had with Indigenous leaders and peoples across the country. We recognize the unique and significant challenges facing Indigenous communities in Canada and wanted to ensure that your voices were heard as we developed our thinking on how national pharmacare could improve the accessibility and affordability of drugs for all Canadians.
We would like to thank Canadians, patients, health care providers, stakeholder organizations, industry, business, labour and academics who took the time to participate in discussions and share their views with us. Patients willingly shared their personal experiences and struggles with us so that we could better understand the reality they face every day in navigating a complex system. To the individuals who contributed their personal stories as they appear in the report, we thank you.
Health care providers gave valuable insights on the many challenges they face in ensuring that patients have access to the medication they need. Stakeholders from a range of perspectives—business, labour, pharmaceutical manufacturers and distributors, private insurance—gave us their best advice on what national pharmacare should look like and how it should be implemented. Academics and experts provided insights from their research so that the council’s report would be evidence-based and authoritative. Collectively, your experiences and thoughtful advice helped us understand the issues and contributed greatly to our work.
We are also grateful for the support and expertise provided by Health Canada and Finance Canada whose efforts and hard work benefited us immensely. In particular, we would like to thank the members of the council secretariat for their tireless work in helping us fulfil our mandate. It was your passion, hard work and commitment that fed and sustained our determination.
Thank you to Marcel Saulnier (Executive Director) and Dara McLeod (Deputy Executive Director). Your commitment, enthusiasm and hard work has been both refreshing and absolutely vital to our success. Accommodating the myriad council requests while also running a secretariat cannot have been easy, but you turned it into an art form.
Thank you: Ziana Ahmed, Michelle Bailey, Madeleine Benjamin, Elaine Chong, Mathieu Cornish, Ian Detta, Alexandra Epp, Brennan Graham, Marcus Greenlaw, Shawn Grover, Farhan Hameed, Lindsay Hitchcock, Hilary Jensen, Michelle Kovacevic, Natalie Labonté, Michel LeClerc, Lily Lin, Amanda Meliambro, Kaireen Patton, Daniel Quinn, Omar Rajabali, Karen Reynolds, Daniel Robinson, Margaret Sharp, Lisa Thompson, Dominique Tremblay, Justine Walker and Tom Ward.
The insights and assistance that we received from all those who participated in and supported our work was invaluable. That said, we take full responsibility for the views and advice presented in this report.
Chair’s note: I wish to express my sincere and heartfelt thanks to fellow council members Dr. Nadine Caron, Vincent Dumez, Mia Homsy, Camille Orridge, Hon. Diana Whalen and John Wright. I am privileged and fortunate to have been able to share such an extraordinary year with each of you. Canada has been well-served by your intellect, experience, humility and generosity. Thank you for contributing your time and energy to this important project.
Executive Summary
Where we are today
Canadians spent $34 billion on prescription medicines in 2018. Drugs are the second biggest expenditure in health care, after hospitals. We spend even more on drugs than on doctors. On a per capita basis, only the United States and Switzerland pay more for prescription drugs. Yet for all that spending, there are huge gaps in coverage. One in five Canadians struggle to pay for their prescription medicines. Three million don’t fill their prescriptions because they can’t afford to. One million Canadians cut spending on food and heat to be able to afford their medicine. Many take out loans, even mortgage their homes. Sadly, far too many Canadians die prematurely or endure terrible suffering, illness or poor quality of life because modern medicines are out of reach for them.
This is unacceptable.
Medicines are a critical part of health care. They allow millions of Canadians to prevent and fight disease, manage chronic illness, ease pain and breathe better. Yet the way Canada manages and pays for this vital part of twenty-first century health care is critically flawed.
We are the only country in the world with universal health care that does not provide universal coverage for prescription drugs.
Instead, we rely on a confusing patchwork of more than 100 government-run drug insurance programs and more than 100,000 private drug insurance plans. Despite everyone’s best efforts, the system is fragmented, uneven, unequal and unfair. The result is a non-system where too many people fall through the cracks. Not only does this lead to ill health, it also costs the health system billions of dollars in extra visits to physicians and hospitals when people’s health fails as a result of lack of access to medicines.
Prescription drugs, more than ever before, offer great hope and promise. But their escalating cost is threatening the sustainability of drug programs. It’s time to take another look at how best to ensure that Canadians can have access to the full array of life-saving and life-changing drugs prescribed to them by their health care providers. In short, we can do better.
When Canada created universal health care 53 years ago, we changed this country in a way unimaginable at the time. It is our proudest legacy. Yet the debate at that time over medicare was eerily similar to today’s debate over pharmacare—can we afford it? Is it what’s best for Canada? How will we know that we got it right? Do we have the courage to build it?
Over the past year, we asked Canadians to summon the same courage shown by thoughtful and committed leaders across the political spectrum that led to universal health care five decades ago. We asked for their best advice and their shared wisdom. What we got back surprised us both in its sophistication, and its simplicity. Be bold, Canadians told us. Be brave, they appealed to us. But most of all, they reminded us to heed those uniquely Canadian values: looking out for one another, supporting neighbours and communities through tough times and treating each other with fairness.
They told us if we could harness that intangible thing—what it means to be Canadian—we might just make pharmacare happen.
The result of our national discussion with Canadians is this report. Hopefully, we accomplished what was asked of us.
What we did
In the February 2018 spring budget, the federal government announced the creation of the Advisory Council on the Implementation of National Pharmacare, and by June 2018, the seven-member council was launched.
Over the past twelve months, we studied Canadian and international models of pharmacare. We travelled to every province and territory and sat down with hundreds of Canadians at meetings, roundtables and town halls. We had conversations. We heard both heart wrenching and uplifting, inspiring stories. We heard from patients and practitioners, academics and employers, labour and industry, government officials and members of the public. We met with First Nations, Inuit and Métis peoples. We commissioned papers. We heard from thousands online and received emails and submissions from thousands more. We listened carefully to the full breadth and diversity of voices and perspectives. What we heard, particularly from patients, families and advocates, was enlightening, informative and inspiring.
What we learned
Significant gaps in coverage and access that are unfair and lead to poor outcomes
Canada’s vast number of drug insurance plans offers a false sense of comfort: it’s a common defence of the status quo that most Canadians already have some form of drug coverage, through public or private drug plans. What we discovered, however, is that about 7.5 million citizens—one in five Canadians—either don’t have prescription drug insurance or have inadequate insurance to cover their medication needs. Here’s what else we learned:
- One in five households reported a family member who, in the past year, had not taken a prescribed medicine due to its cost;
- Nearly 3 million Canadians said they were not able to afford one or more of their prescription drugs in the past year;
- People with insurance also struggle to afford their prescriptions because of copayments, coinsurance and deductibles. Of the 3 million people who could not afford their medications, 38 per cent had private insurance coverage and 21 per cent had public coverage but it did not cover enough of their costs;
- Almost 1 million Canadians cut back on food or home heating in order to pay for their medication; and
- Almost 1 million Canadians borrowed money to pay for prescription drugs.
Canadian and international research shows that cost barriers can result in people not taking their medicine properly and poor health outcomes. Failing to take medication that’s been prescribed can have serious health consequences. A recent study looked at what would happen if out of pocket costs were removed from medications for just three diseases—diabetes, cardiovascular disease and chronic respiratory conditions. It concluded there would be 220,000 fewer visits to emergency departments and 90,000 fewer hospitalizations annually—a potential saving of up to $1.2 billion a year.
We also learned that while about 60 per cent of Canadians are enrolled in private drug plans (primarily employer-sponsored benefit plans), these plans cover only 36 per cent of total system-wide spending on prescription drugs. That’s partly because working Canadians are younger and healthier, requiring fewer drugs. But we are also seeing an increasing trend of private plans offloading expensive drugs onto public plans, as well as requiring employees to bear a greater share of the cost through annual and lifetime dollar limits to drug coverage. The nature of work is also changing: more people are working part‑time, and only 27 per cent of part‑time employees have health benefits. Others are self‑employed or contract workers, often in precarious employment, usually with no benefits at all. This situation disproportionately affects women, people with low incomes and young people—all of whom are all more likely to work in part‑time or contract positions—leaving them without drug coverage, simply because of the type of work they do.
Spiralling drug costs that are unsustainable
There are other costs stemming from our patchwork approach to paying for drugs. Having so many public and private plans dilutes bargaining power. The cost of individual drugs is higher here than in other Organisation for Economic Co-operation and Development (OECD) countries and we spend more per person per year on prescription drugs than any other OECD country, with the exception of the United States and Switzerland.
The council heard that governments are struggling with soaring drug costs, particularly the high cost of new drugs coming onto the market. Research by drug companies is resulting in extraordinary treatments—from biologics, made from living cells or organisms, to gene-based therapy. Challenging to develop and often expensive to administer, they can carry staggering price tags. Today’s top selling brand name drugs often cost thousands or even tens of thousands of dollars per year. Drugs for rare diseases are even more expensive: prices can range from $100,000 to upwards of $2 million per patient per year, often for life. A single biologic generated roughly $1 billion in revenue last year in Canada. The number of drugs on the market that cost more than $10,000 per year has more than tripled since 2006. With our current approaches to drug insurance, whether public or private, these costs are not sustainable. We must act.
What we recommend
A national pharmacare plan that works like medicare
The council looked carefully at a range of models in place internationally and in Canada that could serve as a guide for a national pharmacare plan. We observed that countries with high performing health systems include prescription drug coverage as part of their publicly funded universal health care plans. We learned that by joining forces, drug plans could increase their bargaining power with pharmaceutical companies, resulting in lower drug prices. We came to understand that a ‘fill the gaps’ approach was unrealistic since, like our current mixed public/private system, it would do little to lower drug prices or create fairness or uniformity in access across the country. We were told by employers that private drug benefits for their workers were becoming less and less affordable to them. We recognized the important work provinces and territories have done to provide drug coverage and the need to take this further, in a collaborative way, with federal support. And we were reminded of those Canadian values of fairness and looking out for and supporting each other.
We concluded that the best plan for Canada is to organize prescription drug coverage the way universal health care is set up.
That’s why we are recommending the federal government work with provincial and territorial governments and stakeholders to establish universal, single-payer, public pharmacare in Canada.
We propose that the government enact national pharmacare through new legislation embodying the five fundamental principles in the Canada Health Act:
- Universal: all residents of Canada should have equal access to a national pharmacare system;
- Comprehensive: pharmacare should provide a broad range of safe, effective, evidence-based treatments;
- Accessible: access to prescription drugs should be based on medical need, not ability to pay;
- Portable: pharmacare benefits should be portable across provinces and territories when people travel or move; and
- Public: a national pharmacare system should be both publicly funded and administered.
Stepwise implementation of pharmacare developed in partnership with provinces and territories
National pharmacare can’t be implemented overnight. This is a major part of our health care system that affects millions of patients, hundreds of thousands of health care providers and a broad range of dedicated stakeholders. We’re proposing a deliberately stepwise approach that will also enable the introduction of some fundamental and impactful changes immediately.
National pharmacare would start with the creation of a Canadian drug agency (preliminary funding for an agency was announced in the 2019 federal budget). The new agency would be an arms-length organization, with strong patient representation, accountable to Canadians both directly and through the federal, provincial and territorial ministers of health. It would be governed collaboratively by the federal, provincial and territorial governments and would have patient representation on the board.
Among the agency’s first tasks would be to create a national formulary—the list of drugs to be covered by national pharmacare. The agency will be in charge of approving drugs for the formulary, based on both how well they work and whether they offer good value for money. Because it will take time to choose the right drugs and negotiate prices for them, the initial formulary would be a carefully chosen list of essential medicines covering most major conditions and representing about half of all prescriptions. This initial list of drugs would be available through national pharmacare beginning January 1, 2022.
Also by January 1, 2022, a detailed national strategy and distinct pathway for funding and access to expensive drugs for rare diseases would be implemented. The federal government has already committed $500 million per year for this critically important initiative.
Over the subsequent five years, additional prescription drugs would be added to the national formulary as prices and supply arrangements are negotiated with manufacturers. The full, comprehensive national formulary would be in place no later than January 1, 2027.
Other responsibilities for the agency would include providing guidance on the appropriate use of drugs, and monitoring their safety and effectiveness once they are on the market. Concentrating all these operations in one organization would make pharmacare more efficient and speed up access to new drugs, as well as improve consistency in access to prescribed drugs across the country.
As with medicare, it will be up to individual provinces and territories to opt in to national pharmacare by agreeing to the national standards and funding parameters of pharmacare. We recommend the federal government pay for the incremental costs to provinces and territories of expanding coverage and implementing pharmacare in their jurisdictions. The federal government should proceed immediately with ready provincial and territorial partners, understanding that some jurisdictions may take longer than others to join national pharmacare. And building on the council’s dialogue with First Nations, Inuit and Métis governments and representative organizations, discussions should now take place between the federal government and First Nations, Inuit and Métis governments and representative organizations, to determine whether and how they might wish to participate in national pharmacare.

Figure 1: Text description
A timeline beginning in 2019 and extending to 2027 that illustrates the phased approach of pharmacare. There are four arrows representing the different aspects of pharmacare that will evolve over time.
- The first arrow represents the delivery of national pharmacare. Between the end of 2019 and mid-2020, the federal and provincial/territorial governments would negotiate various aspects of pharmacare. Then, from mid-2020 to 2022, legislation would be drafted. Legislation would be introduced in 2022.
- From 2022 onwards, provinces and territories would deliver national pharmacare based on the results of the negotiations and legislation.
- The second arrow shows development of the Canadian drug agency. From 2019 to 2022, there would be a Canadian drug agency transition office. From 2022 onwards, the Canadian drug agency would be fully established.
- The third arrow shows formulary development and growth. From 2020 to 2022, a national formulary would be developed. In 2022, an essential medicines list would be established. From 2022 to 2027, the national formulary would grow. In 2027, a comprehensive national formulary would be completed.
- The final arrow shows a national strategy for expensive drugs for rare diseases, starting in 2022 onwards.
Low copayments that do not pose a barrier to access
There is strong evidence that user fees create barriers to access, whether in the form of copayments or deductibles. Research has shown they prevent people from taking their prescription drugs properly, or even at all. User fees are particularly hard on people with complex or chronic health problems and those with low incomes. Nevertheless, they are a standard feature of almost all drug coverage in Canada and abroad and we are recommending them, within strict limits: drugs on the essential medicines list would carry a copayment of $2, while all other drugs would have $5 copayments. People receiving social assistance, government disability benefits or the federal Guaranteed Income Supplement benefit would all be exempt from copayments, and no person or household would pay more than $100 per year.
A strategy to improve access to expensive drugs for rare diseases
Canadians with rare diseases are both anxious and determined to find treatment that might help their condition, and the pharmaceutical industry is responding by developing a growing number of drugs—most of which are extremely expensive. Over the course of its mandate, the council heard that these drugs can threaten the sustainability of both private and public insurance plans—but at the same time, patients rely on them for life-changing, often life-saving, treatment. With prices often in the tens of thousands and even up to $2 million per patient per year, these drugs are entirely unaffordable for a patient or family to consider paying out of pocket.
No patient should face costs of this magnitude for any drug. That is why the council is recommending the Canadian government develop a formal national strategy for expensive drugs for rare diseases. We are also recommending the Canadian drug agency establish a distinct pathway for the consideration of expensive drugs for rare diseases, and a national expert panel to work with patients and their clinicians to determine which rare disease drugs should be funded for which patients. The national strategy, distinct process and funding for these specialized drugs should be in place in conjunction with the essential medicines list, beginning January 1, 2022.
A responsible implementation plan that requires federal leadership
Although health care delivery falls under provincial and territorial jurisdiction, the federal government has always played a critical role in developing and safeguarding universal health care—most notably with the introduction of medicare in the 1960s and passage of the Canada Health Act in the 1980s.
Over the past year, we saw provinces and territories taking action, working hard to provide better prescription drug coverage, but we also concluded that the federal government can and should do more, working in partnership with provincial and territorial governments, to ensure all Canadians can access the medicines they need.
The implementation and success of national pharmacare will not be possible without strong federal leadership and funding. The provinces and territories deserve credit for advancing prescription drug coverage in their respective jurisdictions. It is due to their hard work that we are not starting from scratch. In fact, provinces and territories have built a strong foundation upon which to build national pharmacare. For that reason, and conscious of divergent federal, provincial and territorial fiscal outlooks, the council is calling on the federal government to pay for the incremental cost of implementing national pharmacare.
We have estimated that it will cost an additional $3.5 billion in 2022 to launch national pharmacare starting with universal coverage for essential medicines. As the national formulary grows to cover a comprehensive list of drugs, we estimate that annual incremental costs will reach $15.3 billion in 2027. The council recognizes the very significant fiscal implications of this investment. But the issue is too important to ignore. Although national pharmacare requires a substantial investment of public funds, it will result in significant savings to Canadian families and lower the total amount being spent on prescription medications.
We propose that the federal government create a new, dedicated fiscal transfer to support national pharmacare, one that will be long-term, predictable, fair and acceptable to provinces and territories—that takes into account demographics and other variables that impact prescription drug consumption. Furthermore, we recommend this transfer and other key parameters of pharmacare be reviewed every five to ten years. Any changes to the key elements of pharmacare, including funding, should require approval by the Parliament of Canada and 70 per cent of participating provinces and territories, representing two-thirds of their combined populations.
Delivering results for Canadians
Saving Canadian families money while expanding access
National pharmacare will save money as lower prices are negotiated for more drugs and as other cost-saving strategies are implemented. As early as 2022, when national pharmacare would cover essential medications, total spending on prescription drugs would be $300 million lower than without pharmacare. By 2027, total spending on prescription drugs would be $5 billion lower than it would be without national pharmacare.
The savings for individual Canadians and their families will be significant and tangible. Since the average Canadian household spends about $450 annually on prescription medicines, the council’s proposed $100 cap on out of pocket spending means Canadian families will save, on average, $350 per year. And with those savings will come the comfort of knowing you and your loved ones will have access to the medicines you need.
When Canadians go to the pharmacy with their prescription and their health card, they will pay no more than $2 or $5, depending on the drug. A straightforward antibiotic will cost $2. For a drug that is hundreds or even thousands of dollars, the copayment will be $5. That’s it. No more complicated forms. No more steep deductibles or limits. No more stress.
Families and individuals will no longer face the postal code lottery, where access to prescribed drugs depends on which province or territory you reside in. And Canadians can rest assured knowing that their drug insurance travels with them, right across Canada.
Perhaps most importantly, Canadians will have access to medicines based on need, not on their ability to pay. The days of patients taking one look at the pharmacist’s invoice, and walking out without a needed medicine, empty-handed, will become a thing of the past. All Canadians will be treated equally, without exception. That is something to be proud of. And it is consistent with the values that underpin our universal health care system—our values as Canadians.
Supporting employees, job creators and the economy
National pharmacare will mean that employees and businesses no longer have to pay for expensive prescription drug coverage. The average business owner who provides drug benefits would save over $750 annually per employee. The average worker with workplace drug benefits would save over $100 per year in plan premiums. In addition, employees who pay hundreds or thousands of dollars per year in copayments, coinsurance or deductibles for themselves and their families would never pay more than $100 per household per year. No more coinsurance. No more annual or lifetime limits.
National pharmacare will provide businesses with much-needed relief from the high and growing cost of prescription drug insurance. Business owners will no longer have to worry about whether they can afford private drug coverage for their hardworking employees. They will have the financial room to offer other health benefits to their workers (for example, mental health and wellness services, physiotherapy, dental and vision care), to pass on the savings to their employees through higher wages, or to invest in their businesses.
National pharmacare should also make it easier for employees to change jobs or move from one employer to another because they will no longer be at risk of “job lock”—unable to change jobs because the drug they need to treat their condition is not insured under the drug plans of other potential employers, or because a potential new employer has no health benefits at all. And pharmacare means workers who choose to retire will not, as is the case for many retirees today, experience a reduction in drug benefits. Part-time and contract workers will, many for the first time, be entitled to prescription drug benefits.
National pharmacare will also level the playing field for small, medium and large businesses by ensuring all workers have comprehensive drug benefits, not just those who work for companies that provide drug insurance as a benefit of employment. For small businesses, many of which cannot afford drug benefits for their employees, pharmacare should make it easier to recruit and retain employees, and maintain a healthy workforce.
Supporting health care providers
National pharmacare means prescribers can finally have confidence their patients will fill their prescriptions. Doctors and other prescribers will no longer have to ask a patient whether she or he has private insurance, and then modify their prescription accordingly. Pharmacists will know their clients are being well-served by our health care system. And as more and more prescription drugs are delivered outside hospital, the inequity of drugs being covered by public insurance in hospital but not out will end. Patients will get the medication they need to get better, to stay healthy, or to manage a chronic condition.
Removing the cost barriers Canadians face when they have prescriptions to fill will make it easier for them to maintain their health or get better, reducing the need for them to visit their doctors or be admitted to hospital. As previously noted, recent research found that removing out of pocket costs for the medications used to treat just three health problems—diabetes, cardiovascular disease and chronic respiratory conditions—would result in up to 220,000 fewer emergency room visits and 90,000 fewer hospital stays annually. This has the potential to save the health care system up to $1.2 billion a year—just for those three diseases.
A stronger, healthier Canada
National pharmacare is not only good for Canadians, it’s good economic policy. It will reduce the economic inefficiencies that come with tens of thousands of private plans, which cost three times more to administer than public plans. It will replace multiple buyers with a single large, powerful purchaser, one that has the clout and authority to negotiate the best, lowest prices for prescription medications for Canadians. The annual savings that will come from strong negotiating power, lower administrative costs and the other efficiencies of pharmacare will save an estimated $5 billion per year by 2027.
The good news is that these savings can be achieved even as coverage is expanded to cover all Canadians. Our plan also means that Canadians with existing coverage will be better off under national pharmacare. Families will save on average $350 per year and businesses $750 per employee. In other words, adopting national pharmacare will lift every Canadian up, and will allow Canada to address longstanding gaps and inequities in access to prescription drugs while spending significantly less than under the status quo.
A call to action
The implementation of national pharmacare in Canada is long overdue. Indeed, the same arguments spoken in favour of pharmacare in the 1960s still apply today. But a lot has also changed since then, making pharmacare even more relevant and more necessary: prescription medicines have a much greater role in improving health and their cost has skyrocketed, putting the whole system at risk of becoming unaffordable. Pharmacare today is not only good health policy, it’s good economic policy: this is a national project whose time has come.
Our proposal for national pharmacare is transformational and life-changing. It will replace a patchwork of thousands of plans that are becoming less and less sustainable, and still leaving millions of Canadians unable to get the medicine they need. National pharmacare will be a drug insurance plan that belongs to all Canadians—one that is sustainable, fair and equitable, where Canadians can have access to prescription medicines based on their need, and not their ability to pay.
We know this is a bold and challenging task. But Canadians have told us—by the thousands—that this is what they want. That this is what we need. And we know we can get it done. Together.
Pharmacare for all: that’s our prescription.
List of recommendations
Principles of national pharmacare
- The council recommends the federal government work with provincial and territorial governments to establish a universal, single-payer, public system of prescription drug coverage in Canada.
- The council proposes the five fundamental principles of medicare, embodied in the Canada Health Act, be applied to national pharmacare
- Universal: all residents of Canada should have equal access to a national pharmacare system;
- Comprehensive: pharmacare should provide a broad range of safe, effective, evidence-based treatments;
- Accessible: access to prescription drugs should be based on medical need, not ability to pay;
- Portable: pharmacare benefits should be portable across provinces and territories when people travel or move; and
- Public: a national pharmacare system should be publicly funded and administered.
Terms of coverage
- The council recommends national pharmacare provide flexibility for provinces and territories to offer coverage beyond the national pharmacare standards.
- The council recommends Canadians be allowed to purchase private insurance to supplement coverage under national pharmacare.
- The council recommends national pharmacare benefits be portable across provinces and territories.
- The council recommends a gender and equity lens be applied throughout the implementation of national pharmacare.
- The council recommends all Canadian residents be eligible for national pharmacare to ensure everyone has access to the drugs they need to maintain their physical and mental health.
- The council recommends national pharmacare provide coverage for a national list of prescription drugs and related products (a national formulary) to ensure all Canadians have equal access to the medicines they need to maintain or improve their health.
- The council recommends out of pocket costs for all products listed on the national formulary not exceed $5 per prescription, with a copayment of $2 for essential medicines and an annual maximum of $100 per household per year to ensure that patients face few barriers to access.
- The council recommends people receiving social assistance, government disability benefits or the federal Guaranteed Income Supplement benefit be exempt from copayments.
Government collaboration
- The council recommends provinces and territories deliver national pharmacare in a manner that meets or exceeds agreed-upon national standards, in exchange for federal funding.
- The council recommends the federal government work collaboratively and in partnership with provincial and territorial governments to begin the implementation of national pharmacare in 2020.
- The council recommends the federal government be prepared to proceed with national pharmacare even if not all jurisdictions are in a position to opt in at the outset.
Indigenous engagement
- The council recommends the federal government work with First Nations, Inuit and Métis governments and representative organizations to develop a framework and process for determining whether and how they will participate in national pharmacare.
- The council recommends ongoing engagement with First Nations, Inuit and Métis partners to consider how the knowledge and perspectives of Indigenous peoples should be incorporated throughout the implementation of national pharmacare.
Creating a Canadian drug agency
- The council recommends federal, provincial and territorial governments collaborate to create a new arms-length Canadian drug agency to oversee national pharmacare. The new agency should have the following functions:
- Assessing the clinical effectiveness of drugs compared to other treatment options;
- Assessing the cost-effectiveness of drugs compared to other treatment options;
- Deciding which drugs and related products (such as devices and supplies) should be on the national formulary;
- Negotiating prices and supply arrangements with manufacturers;
- Providing advice to prescribers, pharmacists and patients on how best to use drugs; and
- Monitoring the safety and effectiveness of drugs in real-world use.
- The council recommends the federal, provincial and territorial governments and the public be represented in the governance of the Canadian drug agency. Patients must be represented on the board and should maintain appropriate links with patient groups.
- The council recommends federal, provincial and territorial governments work together to determine which existing resources and expertise should be brought into the Canadian drug agency from Health Canada, the pan-Canadian Pharmaceutical Alliance, the Canadian Agency for Drugs and Technologies in Health, the Patented Medicine Prices Review Board, the Canadian Institutes of Health Research and others.
- The council recommends the new agency use rigorous, evidence-based methods to evaluate the clinical effectiveness and value for money of prescription drugs to support the development of a national formulary.
- The council recommends the new agency develop and implement a comprehensive evidence-based national formulary to ensure patients have access to the same prescription drugs no matter where they live across the country.
- The council recommends the Canadian drug agency work closely with Health Canada and manufacturers to shorten the time it takes for prescription drugs that present good value for money to be listed on the national formulary.
- The council recommends the Canadian drug agency negotiate prices and supply arrangements with manufacturers to ensure Canada is getting the best deal and the lowest prices.
- The council recommends the new agency monitor the safety and effectiveness of prescription drugs to ensure they continue to benefit patients and deliver value for money.
- The council recommends the new agency implement a national strategy for expensive drugs for rare diseases to provide access to these drugs across Canada.
- The council recommends the new agency report publicly on the performance of national pharmacare to ensure governments and the agency are accountable to Canadians.
- The council recommends the federal government provide ongoing funding for the new agency to ensure it is able to meet its objectives.
Developing a national formulary
- The council recommends the national formulary be evidence-based and comprehensive to offer patients and prescribers effective treatment choices.
- The council recommends the national formulary include prescription drugs that treat both physical and mental health conditions.
- The council recommends the national formulary provide appropriate treatment options for different age, race, ethnicity, sex and gender identity, among other factors, so that it responds to the needs of all Canadians.
- The council recommends the national formulary include prescription drugs that respond to the specific and unique needs of children and youth, and that a strategy be developed to address the availability of approved drugs and formulations for them.
- The council recommends mandatory generic substitution policies to encourage patients and prescribers to choose the most cost-effective therapies and help keep national pharmacare affordable.
- The council recommends formulary management policies, including requiring biosimilar substitution, that support the use of biosimilars and encourage patients and prescribers to choose the most cost-effective therapies to ensure the sustainability of national pharmacare. Prescribers and patients should be better supported with information reinforcing the safety, efficacy and benefits of biosimilars.
- The council recommends the Canadian drug agency work to increase prescriber and public awareness about the equivalency of generics to brand name drugs and the rationale for greater use of generics and biosimilars to keep pharmacare affordable.
Implementing a national formulary—starting with essential medicines
- The council recommends federal, provincial and territorial governments launch national pharmacare by offering universal coverage for a list of essential medicines by January 1, 2022.
- The council recommends governments expand the initial formulary step-by-step toward a fully comprehensive formulary to be in place no later than January 1, 2027.
- The council recommends the Canadian drug agency create a framework to determine the order in which prescription drugs will be evaluated, negotiated and listed on the national formulary as it expands. The framework should prioritize products that are already covered by most public drug plans, respond to national population health priorities and reduce variability in access across the country.
National strategy on appropriate prescribing and use of drugs
- The council recommends the Canadian drug agency create and implement a national strategy on appropriate prescribing to support prescribers and help patients better understand the pharmaceutical treatment choices available to them.
- The council recommends federal, provincial and territorial governments regulate pharmaceutical industry payments to health care providers, institutions and patient groups, beginning with mandatory public disclosure of all such payments.
National strategy for expensive drugs for rare diseases
- The council recommends the federal government work with provincial and territorial governments and patients to immediately develop a national strategy for expensive drugs for rare diseases to support better and more consistent access to these drugs.
- As part of this strategy, the council recommends the Canadian drug agency establish a distinct pathway for the consideration of expensive drugs for rare diseases, and a national expert panel to work with patients and their clinicians to determine which rare disease drugs should be funded for which patients.
- The council recommends the Canadian drug agency work with clinicians and patients to gather structured real-world evidence on the impact of rare disease drugs on patients.
- The council recommends the Canadian drug agency negotiate performance-based funding agreements with manufacturers of rare disease drugs, where the amount paid to the manufacturer depends on how well the drug works.
- The council recommends the Canadian drug agency ensure decisions on expensive drugs for rare diseases are transparent and clearly communicated.
Financing national pharmacare
- The council recommends the federal government provide long-term, adequate and predictable funding to provinces and territories sufficient to cover the incremental costs of national pharmacare.
- The council recommends federal funding for national pharmacare be allocated to provinces and territories in a fair and transparent way, and be responsive to differing levels of need across jurisdictions.
- The council recommends federal funding for national pharmacare be delivered through a new targeted transfer that is separate and distinct from the Canada Health Transfer.
- The council recommends provinces and territories be eligible for federal funding when they accept the principles and the national standards (terms of coverage) for national pharmacare.
- The council recommends intergovernmental financing arrangements for national pharmacare be determined through mutual agreement among federal, provincial and territorial governments.
- The council recommends intergovernmental financing arrangements for national pharmacare be reviewed every five to ten years.
- The council recommends changes to intergovernmental financing arrangements for national pharmacare require the consent of the Parliament of Canada and at least 70 per cent of participating provinces and territories representing two-thirds of their combined population.
- The council recommends the federal contribution to national pharmacare be financed through general revenue in a manner similar to the way medicare is funded.
Legislation
- The council recommends the federal government enshrine the principles and national standards of pharmacare in federal legislation, separate and distinct from the Canada Health Act, to demonstrate its ongoing commitment to partnership on national pharmacare and provide for a dedicated funding arrangement.
- The council recommends the federal legislation outline how governments will work together and share costs, list federal responsibilities and include the steps required for provincial and territorial governments to opt in to national pharmacare.
Transition support
- The council recommends the federal government support provincial and territorial governments to build program capacity to deliver national pharmacare.
- The council recommends federal, provincial and territorial governments engage with private insurers, as well as the employers and employees who benefit from their services, to ensure a smooth transition to national pharmacare.
- The council recommends private insurers be allowed to provide coverage for copayments, as well as for drugs not on the national formulary.
Information technology and drug data
- The council recommends the federal government invest in information technology systems to ensure provincial and territorial governments have sufficient capacity to deliver national pharmacare.
- The council recommends the federal government invest in data collection, including from a gender and equity perspective, to address gaps in data and support ongoing management of national pharmacare. This should include data systems, possibly using blockchain technology, that allow secure sharing of data with the consent and control of patients.
Supporting federal measures
- The council recommends the federal government accelerate efforts to streamline and modernize its assessment of drug safety, quality and efficacy to ensure patients will have faster access to innovative medicines.
- The council recommends the federal government advance efforts to strengthen the Patented Medicines Regulations to lower the prices of patented drugs for all payers.
- The council recommends the federal government continue to work with universities, research hospitals and industry to sustain and grow our world-class health innovation ecosystem and ensure Canada continues to contribute to the development of innovative drugs and related therapies.
Chapter 1: Introduction
1.1 The council’s mandate
Prescription drugs are an essential part of health care. However, unlike hospital and physician services, prescription drugs are not covered by medicare except when they’re used in hospitals. That’s left a crucial part of effective health care inconsistently funded and unevenly available, and means too many patients are at risk of not getting the medication they need. The situation has only gotten worse with the emergence of a growing number of high-cost specialty drugs used to treat chronic, complex conditions such as severe rheumatoid arthritis, multiple sclerosis and cancer. These new treatments, along with a growing number of ultra-specialized and expensive drugs for rare conditions, are threatening to overwhelm both public and private insurance programs.
In its 2018 budget, the federal government announced the creation of the Advisory Council on the Implementation of National Pharmacare (the council). The council’s terms of reference are included in Annex 2. Its task was to advise the government on introducing a national insurance program for prescription drugs—known as pharmacare—which would be affordable for Canadians, their employers and governments. The government asked the council to undertake a dialogue with Canadians and issued a discussion paperEndnote 1 that outlined a range of possible options on how to move forward with national pharmacare and highlighted the key issues the council should address in its work.
The council started its work without any preconceived preference for a particular model and led a national discussion with Canadians—patients and caregivers, health care providers, provincial and territorial governments, Indigenous peoples, experts and academics, the private sector and other stakeholders—to learn what would work best for Canada.
The council deepened its understanding with research into the fiscal, economic and social aspects of Canadian and international experiences with pharmacare. All this work was focused on answering the three main questions about pharmacare in the federal government’s discussion paper: who should be covered under national pharmacare; what drugs should be covered; and who should pay for it.
1.2 National dialogue
To do its work, the council travelled to every province and territory across the country to hear from thousands of Canadians. In each jurisdiction, the council held roundtables attended by patients, their family members, health care providers and academics, as well as representatives from health care organizations, business, labour groups, the pharmaceutical industry, private insurers and employee benefit providers. Through structured discussions, they shared their perspectives on what pharmacare might look like.
Efforts to hear Canadians’ thoughts on national pharmacare did not end there. In Vancouver, Toronto and Halifax, the council held town hall meetings where any member of the public could attend. Small group sessions were also organized with Canadians who had limited or no drug coverage to ensure their voices were heard.
The council believed strongly that we must look at the issue of drug coverage in Canada through the lens of those with lived experience: patients and their families. Dedicated engagement sessions were held with patients and with the patient advocacy groups that serve as a voice for Canadians living with a wide range of health conditions. As well, individual patients and patient group representatives made up at least one quarter of the participants of the council’s roundtable sessions held across the country. Some of the stories patients shared with the council are woven through the report.
To get input from individuals who could not attend in person, an online platform was open from June to September 2018. There were more than 15,000 responses to an online questionnaire, nearly 1,500 comments were posted by Canadians, and the council received more than 150 written submissions.
Council members also met with representatives of national Indigenous organizations, including the Assembly of First Nations, the Inuit Tapiriit Kanatami and the Métis National Council and with other representative organizations, to discuss Indigenous peoples’ experiences in accessing medication and to get their perspective on national pharmacare.
All of the input was extremely valuable to the council’s work. A detailed summary of the council’s discussions with Canadians and stakeholders can be found in its What We Heard Report.Endnote 2
Canada’s federal, provincial and territorial governments all offer various types of drug plans and were key partners in the council’s work. As they travelled across the country, council members heard first-hand from provincial and territorial officials about challenges and opportunities facing public drug plans. As well, a national reference group, comprised of officials responsible for drug plan programs and policy in each jurisdiction was formed to share information and insights with the council. The council also received a briefing from federal officials responsible for the program that provides drug benefits to registered First Nations and recognized Inuit.
As well, the council received briefings from several organizations that play important roles in the drug management system, such as the Canadian Agency for Drugs and Technologies in Health and the Patented Medicine Prices Review Board. Finally, in an effort to better understand approaches to pharmacare in other countries, the council had discussions with representatives from Australia, New Zealand, the Netherlands and the United States.
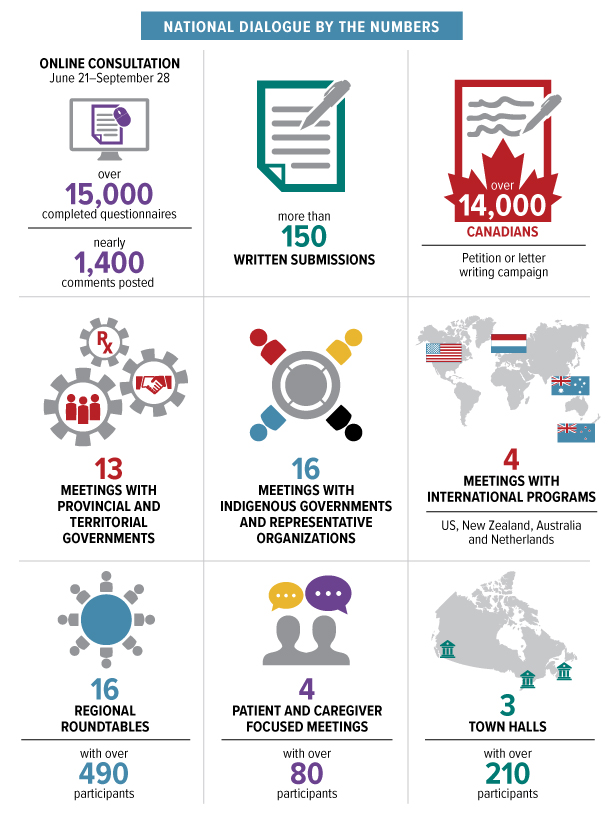
Figure 2: Text description
A graphic showing the various statistics of council engagement activities over the course of its mandate.
- The first shows a computer with the online questionnaire, which was open between June 21 to September 28, with over 15,000 completed questionnaires and nearly 1,400 comments posted.
- The second shows more than 150 written submissions.
- The third shows over 14,000 Canadians contributed to petitions or letter writing campaigns.
- The fourth shows 13 meetings with provincial and territorial governments.
- The fifth shows 16 meetings with indigenous governments and representative organizations.
- The sixth shows a map of the world describing four meetings with international programs in the US, New Zealand, Australia and the Netherlands.
- The seventh shows that there were 16 regional roundtables with over 490 participants across the country.
- The eighth shows four patient and caregiver focused meetings.
- The ninth shows three town halls, one each in Vancouver, Toronto and Halifax.
1.3 Policy research and analysis
The council benefited from a considerable body of work that has been developed over the years on pharmacare and on a range of pharmaceutical issues. In some areas, we felt that additional work was required to provide the council with the most up-to-date information available, or to delve into specific areas where there are gaps in knowledge. We commissioned leading experts to provide us with insights on the following issues:
- International and domestic models of pharmacare;
- Cost-related non-adherence to prescriptions;
- Options for a national formulary;
- Sex- and gender-based analysis of national pharmacare; and
- Impact of improved access to medications on health service utilization and health outcomes.
The council also benefited greatly from cost modelling work done for us by Finance Canada. Our objective was to estimate the costs and savings of national pharmacare as accurately as possible, building on earlier estimates by the Parliamentary Budget Officer.
1.4 What’s in the report
As the council pursued its dialogue with Canadians, it became clear that the issue is not whether Canada needs national pharmacare, it’s how Canada should move forward to create it. This report is therefore not about whether national pharmacare is a good idea, it’s a plan for building it.
It begins with an examination of the state of drug coverage in Canada, outlines its challenges and describes necessary improvements. The report goes on to present what national pharmacare would look like and lays out a detailed plan and timetable, including recommendations to government about how national pharmacare should be implemented. This includes advice on what components of the plan should be introduced and when, who should be responsible, and how it should be financed. The report also discusses the key enablers that will need to be put in place for national pharmacare to succeed and concludes with a summary of what national pharmacare will mean for Canadians.
Chapter 2: Drug coverage in Canada today
2.1 The idea of pharmacare
Prescription medicines allow millions of Canadians to prevent and fight disease, manage chronic illness, ease pain, breathe better—in other words, to live healthier and more productive lives. And yet the way Canada manages and pays for this vital part of 21st century health care is critically flawed. Canada is the only country in the world with universal health care that does not provide universal coverage for prescription drugs. Our fragmented landscape of drug benefit plans leaves too many Canadians unable to afford the drugs they need.
Drug costs have been steadily climbing around the world. In Canada, drug spending (outside of hospitals, where drugs are covered by medicare) has grown from $2.6 billion in 1985 to $33.7 billion in 2018.Endnote 3 The cost of individual drugs is higher here than in other Organisation for Economic Co-operation and Development (OECD) countries and we spend more per person per year on prescription drugs than almost any other OECD country, with the exception of the United States and Switzerland.Endnote 4
There are more than 100 government-run drug insurance programs in Canada—often designed to provide drug coverage for vulnerable groups including seniors and people on social assistance. There are also over 100,000 private drug benefit plans, usually offered as employment benefits but also for sale directly to individuals. Nevertheless, high percentages of Canadians consistently report in surveys that they have either not been able to pay for at least one prescription, or have not taken their medicine as instructed because of its cost.Endnote 5 That’s partly because some Canadians have no drug coverage at all, but also because many people with prescription drug insurance have to pay part of the cost of their prescriptions through deductibles and copayments, or because some plans have annual or lifetime limits on how much an individual can claim.
This situation, in a wealthy country with a commitment to social equity and an established universal health care system, makes no sense and led to the announcement of the Advisory Council on the Implementation of National Pharmacare in February 2018. During the year of its mandate, the council has done a financial, economic and social assessment of Canadian and international models of pharmacare and consulted across the country—with patients, health experts and health care providers, the private sector, labour, academics, provincial and territorial governments and Indigenous peoples. Our conclusion: it’s time for Canada to introduce a national pharmacare system that will ensure all Canadians can get the prescription drugs they need at a cost they can afford. It’s time to end the cost, inefficiency and unfairness inherent in having thousands of different insurance plans—public and private. It’s time to act.
The idea of pharmacare—a publicly funded, universal prescription medicine insurance plan—is not new in Canada. It has been recommended in every major study of Canada’s health care system in the past half-century, from the 1964 Hall Commission report to the Pharmacare Now report tabled by the House of Commons Standing Committee on Health in April 2018. As the box shows, the studies did not all recommend the same model for pharmacare but they all concluded some form of it would result in better health for Canadians and lower costs for families, employers and governments.
A Patient’s Story—Dave
"I’m a type 1 diabetic and a full-time electrician.
If you think being an electrician keeps you busy, try being one who has to watch his diet, exertion level, hydration and sugar levels, all at the same time as wiring a building—safely. There are often long hours, long days and long weeks. Not ideal conditions for a diabetic.
The company I work for does offer group benefits, but their small size means that, although I could join the plan, it wouldn’t cover treatments for my diabetes. I could see their point, but it was a hard pill to swallow (pun intended).
So, I’m paying full cost out of pocket. Like most diabetics who face such resource limits, I find ways to “stretch” things a bit: reusing supplies, skipping doses and testing.
Is it ideal? No way! I worry that if I’m working a long-shift before a paycheque and I’m stretching things, I might get confused or black-out and cause serious damage to myself.
Look, I work hard, I do my bit. I don’t understand why access to medication doesn’t work like our access to doctors or hospitals."
Fifty-five years of endorsements for pharmacare
The Royal Commission on Health Services (1964)
Supreme Court Justice Emmett Hall was appointed to lead the commission in 1961 and his final report laid the groundwork for universal, public health insurance introduced through the Medical Care Act in 1966. Justice Hall said that “in view of the high cost of many of the new life-saving, life-sustaining, and disease-preventing medicines, prescribed drugs should be introduced as a benefit of the public health services program.” The report recommended federal and provincial governments work together to introduce a public drug benefit and called on the federal government to pay for 50 per cent of the program through grants to the provinces. He also recommended the drug benefit be available to all Canadians at a cost of $1 per prescription (equivalent to roughly $8 today).
National Forum on Health (1997)
The forum’s purpose was to advise the federal government on innovative ways to improve the health system and the health of Canadians. It recommended Canada implement a universal public drug benefit program as part of the publicly funded health care system “because pharmaceuticals are medically necessary and public financing is the only reasonable way to promote universal access and to control costs.” The forum recommended that all provinces and territories establish public drug plans to cover drugs that evidence showed offered the best clinical and economic value.
Commission on the Future of Health Care in Canada (2002)
Former Saskatchewan Premier Roy Romanow’s commission was asked to investigate Canadians’ ideas on the future of health care, and make evidence-based recommendations on how to ensure its long-term sustainability. It recommended governments work together to cover prescription drugs under the Canada Health Act, with the first step being a system of universal “catastrophic” drug coverage (which protects people from high drug costs, usually by financing all drug costs that total more than a certain share of household income). The commission also called for the creation of a national agency to negotiate prices, decide what drugs should be covered, monitor prescribing and drug safety and provide objective information about medicine to patients and health care providers.
Standing Senate Committee on Social Affairs, Science and Technology Report on the State of the Health Care System in Canada (2002)
Chaired by Senator Michael Kirby, the committee looked at the federal role in health care, focused mainly on supply, human resources and the need for greater competition. On issues related to prescription drug coverage, it said that no Canadian should suffer undue financial hardship because of the cost of prescription drugs. The committee recommended introducing catastrophic coverage and said the federal government should cover 90 per cent of the cost of the program. It also called for the federal government to work closely with the provinces and territories to establish a single national formulary.
Standing Committee on Health—Pharmacare Now: Prescription Medicine Coverage for All Canadians (2018)
The House of Commons Standing Committee on Health heard from expert witnesses on pharmacare and commissioned a study by the Office of the Parliamentary Budget Officer to examine its potential for cost savings. To ensure all Canadians have affordable access to prescription drugs, the committee recommended establishing a universal, single-payer, public national pharmacare program by expanding the Canada Health Act to include prescription drugs dispensed outside of hospitals as an insured service. The Parliamentary Budget Officer found that approach could reduce total annual prescription expenditures by $4.2 billion.
Each of these studies also said that national pharmacare should be consistent with the principles and values of the public medicare system, regardless of the specific model each study recommended. With that consensus, with the obvious need and the strong support from Canadians, why do we not have a system of national pharmacare? The answer to that goes back to the very beginning of universal, publicly funded health insurance (commonly called medicare) in Canada.
2.2 The evolution of medicare
The idea of universal, public coverage for health care started gaining popularity in Canada after the Great Depression hit in 1929, when progressive organizations and political parties began promoting the idea.Endnote 6 In 1947, Saskatchewan was the first province to introduce universal public hospital insurance (including coverage for drugs administered in hospitals), with British Columbia and Alberta following a few years later. In 1957, the federal government passed the Hospital Insurance and Diagnostic Services Act, which offered to share provincial and territorial costs for hospital and diagnostic services, provided that provincial governments met certain conditions. Within four years, all provinces and territories were providing residents with access to hospital services at no charge.
In 1962, Saskatchewan again led the country by expanding public coverage to include physician services. The move was fiercely resisted by opposition politicians and doctors (who went on strike), foreshadowing the reactions of doctors and some politicians in every province in the years to come as medicare was gradually introduced and expanded.Endnote 7 Despite that powerful opposition, public support for medicare remained strong.
In the summer of 1966, Lester Pearson’s government introduced the Medical Care Act, which offered to share provincial and territorial costs for physician services. According to then Health Minister Allan MacEachen, the government believed “…all Canadians should be able to obtain health services of high quality according to their need for such services and irrespective of their ability to pay. We believe that the only practical and effective way of doing this is through a universal, prepaid, government-sponsored scheme.”Endnote 8 By 1972, all provinces and territories had universal public insurance for physician services.
The establishment of public insurance for hospital and physician services across the country irrevocably cemented the foundational concepts of Canadian health care—universal access, public administration and zero cost at the point of care. In 1984, the Canada Health Act further codified these ideas in its five principles—that health care should be publicly administered, accessible to all, comprehensive, universal and portable.
Neither the Medical Care Act nor the Canada Health Act, however, included coverage of medicines prescribed outside of hospitals. When medicare was introduced in the 1960s, prescription medicines played an important but much more limited role in health care, with a range of fairly inexpensive drugs used to treat common conditions. Government officials decided to focus on the most important and expensive components of health care at the time—hospitals and physician services. Although prescription medicines were intended to be added at a later date, changing economic conditions, shifting priorities, and the ups and downs of federal-provincial-territorial relations sidetracked efforts to bring about national pharmacare.
In the absence of pharmacare, provinces and territories developed their own drug plans. Most were designed for vulnerable groups, such as people on social assistance and seniors. At the same time, employers began offering health benefits (including prescription drugs, vision and dental care), as a way to attract and retain talent in a competitive labour market.
2.3 Public drug plans
The more than 100 drug plans run by federal, provincial and territorial governments are aimed at improving access to prescription medicines primarily for people who might otherwise not be able to afford them. Each plan is different, but often tailored for specific groups such as seniors, children, those with low incomes, or people with serious medical conditions. The federal government provides drug coverage to registered First NationsFootnote i and recognized Inuit populations, federal inmates, members of the Canadian forces, veterans, resettled refugees and refugee claimants.
In addition to those public plans, all provinces have a form of safety net coverage for their residents. The most common form, often called catastrophic coverage, protects people from the financial catastrophes very high prescription drug costs can trigger. British Columbia, Saskatchewan, Manitoba, Ontario, Nova Scotia, Prince Edward Island and Newfoundland and Labrador offer catastrophic coverage, which people become eligible for when their total drug costs exceed a certain percentage of household income (their deductible). Some provinces have more generous deductibles than others.
| Province | Catastrophic Drug Plans: Deductible Levels |
|---|---|
| British Columbia | 0% deductible for incomes below $30,000 2-3% of net family income for incomes above $30,000 |
| Saskatchewan | 3.4% of total adjusted family income |
| Manitoba | 3.17-7.15% of total adjusted family income, depending on income level |
| Ontario | ~4% of net family income |
| Nova Scotia | 1-20% of totaladjusted family income, depending on income level |
| Prince Edward Island | 3-12% of net family income, depending on income level |
| Newfoundland | 5-10% of net family income, depending on income level |
Safety net programs in other provinces are based on premiums. In Alberta and New Brunswick any resident has the option of enrolling in public drug coverage by paying a premium.
Quebec is the only Canadian jurisdiction that has achieved universal drug coverage and it did so by making drug insurance mandatory for all residents. Employers that provide health benefits to their employees are required to provide prescription drug coverage that meets or exceeds the level of coverage provided by province’s public drug plan. Residents who are not eligible for private insurance through their employer or occupation are required to enrol in, and pay premiums for, the provincial drug plan (some vulnerable groups, such as low-income seniors, are exempted from paying premiums).
While the territories do not offer broad-based safety net programs, many residents are covered under the federal Non-Insured Health Benefits Program, which provides drug coverage to over 800,000 registered First Nations and recognized Inuit across Canada. Furthermore, the territorial governments offer a number of targeted public plans for Métis and for non-Indigenous residents, such as drug coverage for seniors and individuals with chronic conditions.
Drug plan design
Drug insurance plans (both public and private) have three main components:
- Eligibility criteria: rules for who is eligible for coverage under the plan (for example, full-time employees of an organization; a specific group of provincial residents, such as seniors);
- A formulary: the list of drugs that are covered (reimbursed) by the drug insurance plan; and
- Cost sharing terms: dictate the share of costs paid by the drug plan sponsor and the share paid out of pocket by plan members (individuals and families). There are several different types of cost sharing:
- Deductible: the dollar amount that an individual or household must pay out of pocket, usually annually, on prescription drugs before the drug plan will begin to pay.
- Copayments and coinsurance: after the deductible limit has been reached, the amount paid out of pocket by an individual each time a prescription is filled, with the remainder of the cost paid by the drug plan. This can either be a percentage amount (for example, a coinsurance of 20 per cent of the prescription cost) or a fixed payment per prescription (for example, a copayment of $5 per prescription).
- Premium: a fixed amount (often paid annually) that an individual or household must pay to enrol in a drug insurance plan. This amount is payable whether or not any claims are made.
- Plan maximum: the maximum amount a drug plan will contribute to an individual’s or household’s prescription drug costs—this can be either an annual maximum or a lifetime maximum.
2.4 Private drug plans
The lack of universal public drug coverage in Canada has created a market for private drug coverage. Private drug plans are generally intended to attract workers and support workplace productivity, not serve as social safety nets. Most private plans have open formularies—that is, the lists of drugs they will pay for includes almost every medication Health Canada approves for use, regardless of whether they are more or less effective, or cost more or less, than other available drugs. This gives physicians and patients access to the broadest possible range of treatments, but also can lead towasteful spending because there is little incentive for patients or providers to choose a lower cost, equally effective therapy. For their part, public formularies emphasize effectiveness and value for money. Having open formularies also limits the buying power of private plans; it’s hard to hold out for a good price when your business is based on offering quick access to all available medicines.
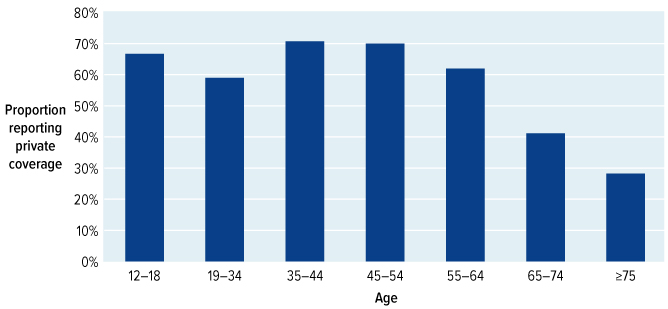
Source: Law, M. (2018). Cost-Related Barriers to Prescription Drug Access in Canada (a report prepared for the Advisory Council on the Implementation of National Pharmacare). Available from Health Canada by request.
Figure 3: Text description
| Age group | Proportion reporting private coverage |
|---|---|
| 12-18 | 66.70% |
| 19-34 | 59.00% |
| 35-44 | 70.70% |
| 45-54 | 70.00% |
| 55-64 | 61.90% |
| 65-74 | 41.10% |
| ≥75 | 28.20% |
Source: Law, M (2018). Cost-related Barriers to Prescription Drug Access in Canada (a report prepared for the Advisory Council on the Implementation of National Pharmacare). Available from Health Canada by request.
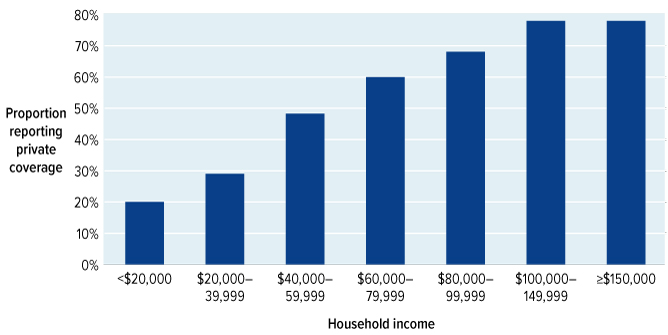
Figure 4: Text description
| Household Income | Proportion reporting private coverage |
|---|---|
| <$20,000 | 20.00% |
| $20,000-39,999 | 29.00% |
| $40,000-59,999 | 48.30% |
| $60,000-79,999 | 60.00% |
| $80,000-99,999 | 68.10% |
| $100,000-149,999 | 78.00% |
| ≥$150,000 | 78.00% |
Source: Law, Michael. Cost-related Barriers to Prescription Drug Access in Canada: A report prepared for the Advisory Council on the Implementation of National Pharmacare. 2018.
Linking drug coverage to employment presents another potential problem—it could limit job choices for people. Unequal access to drug coverage may cause individuals with high drug costs who get workplace health benefits to be afraid to change jobs if there’s a risk they’ll lose their drug coverage. Employment-based drug coverage may even discourage people on social assistance from applying for jobs, because once hired, they may lose their government coverage, but many entry-level and part-time jobs don’t offer drug benefits.
Notably, governments are some of the biggest sponsors of private drug insurance plans. Most public sector workers at the federal, provincial, territorial and municipal levels—including those working in health, education, and social services—have prescription drug coverage as a benefit of employment. This means that as many as 30 per cent of all private plan beneficiaries are public sector employees whose benefits are delivered by private health insurers but paid from general tax revenues. However, as concerned as governments are about runaway prescription drug costs, these plans are more expensive and inefficient than public drug plans.
A Patient’s Story—Kerri MacKay
"I’m a twenty-something freelance writer with two part-time jobs, and no benefits. I take common, but costly, medications for asthma and ADHD. I have not had private insurance since graduating university in 2014 and losing coverage through my dad’s employee plan.
Now I use our public provincial pharmacare program to cover the majority of my medications as it is still affordable. But let me be pointedly clear, the only reason it is “affordable” is that I still live with my parents and have few other expenses.
At the end of each year, I calculate how to deal with health costs for the next year: is it cheaper for me to pay the provincial deductible and medical expenses out of pocket, or should I get a private medical plan? Here’s what I learned. While it SEEMS like I can buy individual insurance, it turns out that few private plans cover “pre-existing conditions.” Even those through freelancers’ and writers’ unions.
With luck and continued work my income will increase, but so will my deductible, to the point where I will be paying the full cost out of pocket.
In our unstable job market, why do we continue to tether drug insurance to stable employment? Where does that leave the creatives and entrepreneurs who just happen to have a chronic illness?"
2.5 The changing drug landscape
How we treat disease is evolving rapidly as pharmaceutical companies push their science further and further in search of new treatments and cures. The landscape of drugs available on the Canadian market is crowded and complex, and pharmaceutical companies continue to introduce new and specialized products at a rapid rate. Developments come so fast, in fact, it’s not always clear when a drug comes on the market just how much it will improve health outcomes, and whether it will be worth the cost. Not all drugs live up to initial expectations and others become outdated quickly as new treatments for the same condition are developed. Newly launched drugs can generate excitement, but some offer little benefit over older, lower cost alternatives.
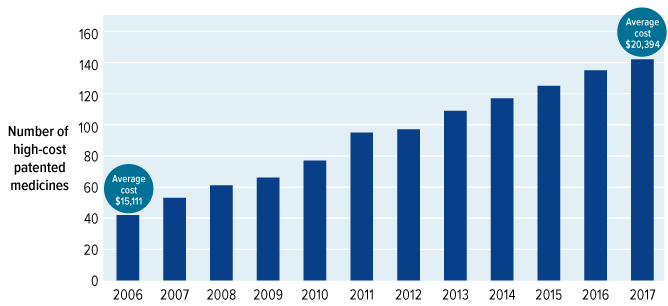
Source: Patented Medicine Prices Review Board. (2018). Annual Report 2017. Ottawa, ON: PMPRB.
Figure 5: Text description
| Year | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Average Rx cost | $15,111 | $15,631 | $15,507 | $15,755 | $16,247 | $17,071 | $17,621 | $18,084 | $18,964 | $20,660 | $20,106 | $20,394 |
Source: PMPRB Annual Report, 2017
It is not just research and development that makes these new specialty drugs so expensive. Many new medications are not just another pill to be dispensed at the pharmacy and taken at home. Often, they are given to patients by injection or infusion and require special storage and handling, and the patients who take them need close monitoring throughout their treatment, all of which adds costs. Many of these new drugs are biologics, which are made from living cells or organisms using biotechnology (many new cancer drugs are biologics, as well as drugs used to treat rheumatoid arthritis, irritable bowel disease and psoriasis, among others). They are harder to develop and manufacture than traditional chemical drugs. Gene-based therapy, which works by introducing genetic material into a person’s DNA to treat or prevent disease, is just coming onto the market and is also very challenging to develop and expensive to give. As well, pharmaceutical companies are developing a growing number of drugs for rare diseases. These products are often the only treatment available for conditions that may be seriously debilitating or life-threatening, but the cost of development, small numbers of patients and few treatment options combine to drive up costs. At the same time, some new (and expensive) specialty drugs are for relatively common conditions, such as migraines, where demand (and therefore spending) could be high.
These new drugs can be life-changing for patients, but they are often staggeringly expensive. For many years, the majority of top-selling patented drugs cost less than $1,000 per patient per year. Today, top-selling brand name drugs often cost thousands or tens of thousands of dollars per year. Drugs for rare diseases are even more expensive: prices can range from $100,000 to upwards of $2 million per patient, per year, often for life. The number of drugs on the market that cost over $10,000 per year has more than tripled since 2006.Endnote 9 It does not take long, in the face of such overwhelming costs, to realize we can no longer continue with a fragmented, expensive, out-dated and poorly thought-out approach to funding such a vital element of health care. A system that depends on every player assuming someone else will find money somehow instead of planning and organizing to ensure needs are met cannot serve the needs of Canadians in the future, or even in the short run.
A Patient’s Story—Grace Alarcon-Isla with Aleiandro Isla
"Just before our son, Aleiandro, turned 16 and after a decade of whirlwind tests and auspicious coincidences, he was finally diagnosed with a rare disease that causes inflamed cartilage throughout his body.
While it was a relief to finally know what was wrong, our world took a very sudden, complex and traumatic turn. A world of looming “medical poverty.”
There’s no cure. He takes 25 medications daily to deal with symptoms. Some covered by my husband’s plan, some through compassionate access, others not covered at all. Just one of these costs $3,000 per month out of pocket. And when you add up the copayments on 25 medications…sigh.
Myself, my son and my other children moved to the city to be closer to appointments and clinics, while my husband had to stay for his job. I had to quit mine as it was impossible to juggle it with all of the appointments and my family.
My faith has been my touchstone throughout this, and I am thankful for it, my family and friends. I can’t help wondering if other Canadians, the federal government and the provinces could take some of the burden from the God I rely on. I know if you were in my position, I would not hesitate."
Chapter 3: Key challenges facing Canada’s prescription drug system
In the absence of national pharmacare, a patchwork of public and private drug plans has evolved in Canada. This fragmented system is not equipped to handle the increasingly complex and expensive medications surging onto the market and is failing Canadians in a number of fundamental ways.
3.1 Fairness
The most profoundly unfair result of not having national pharmacare is that while the majority of Canadians have at least some insurance for prescription medication, many people have none at all. There’s no agreement on just how many people fall into that latter category—the Conference Board of Canada put it at 5.2 per cent of the population, or almost 2 million Canadians,Endnote 10 but in Statistics Canada’s 2016 Canadian Community Health Survey, 19 per cent of Canadians (about 7.5 million people) reported they did not have insurance that covered part or all of the cost of their prescription drugs.Endnote 11 This likely reflects both the uninsured (people who have no coverage) and the underinsured (who have inadequate coverage).
Some of the difference in numbers may be due to catastrophic coverage. If the deductible under a catastrophic plan was 5 per cent of income, someone living on $22,000 per year (which Statistics Canada defines as low income for a single person) would have to pay $1,100 for their prescriptions before insurance would even kick in—and that’s a lot of money for someone already struggling to get by. In that situation, coverage may be more theoretical than real.
One study found that 4.1 million Canadians who are eligible for public insurance don’t enrol, possibly because they know their drug costs won’t be high enough to meet plan deductibles or they don’t know about the plans.Endnote 12 So while only a small proportion of Canadians are actually completely uninsured, a much greater number are underinsured—the two together probably make up 20 per cent of the population—leaving 1 in 5 Canadians struggling to pay for their prescription medications each year.
A substantial proportion of underinsured Canadians have some form of private insurance. But premiums, deductibles, copayments, coinsurance and annual and lifetime limits mean that out of pocket costs can still be high.Endnote 13
Example 1: Family with common conditions
In this hypothetical example, we present Nadia, a 39-year-old single mother with two children. She manages a local small business and earns a net annual income of $45,000.
She and her family have prescriptions for gastric reflux, anxiety, birth control, asthma, attention deficit hyperactivity disorder and the occasional ear infection.
Without drug coverage, these drugs would cost Nadia approximately $1,500 a year.
With public drug coverage, Nadia would have to pay different amounts, depending on where she lived in Canada.
In some provinces, her children are fully covered, so she would only have to pay $300 in drug costs. However, in several jurisdictions, the $1,500 cost of her family’s medications is the same (or lower) than the deductible or premium she would have to pay under the public plan, so she does not benefit from these drug plans.
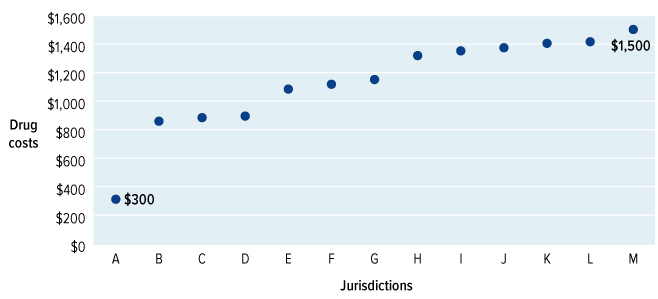
Example 1: Text description
| Jurisdiction | Nadia's drug costs |
|---|---|
| A | $300 |
| B | $800 |
| C | $900 |
| D | $900 |
| E | $1,000 |
| F | $1,100 |
| G | $1,100 |
| H | $1,300 |
| I | $1,300 |
| J | $1,300 |
| K | $1,400 |
| L | $1,400 |
| M | $1,500 |
For those Canadians eligible for government (public) drug benefits, there are differences in coverage within and across provinces. Federal, provincial and territorial drug insurance plans have broadly similar goals—generally, protecting the health of vulnerable people—and a 2017 review by the Patented Medicine Prices Review Board found that for the majority of drug classes, the public drug programs all provided access to equivalent (though not identical) drugs.Endnote 14 But differences in who is covered, how drugs are funded, the amount of out of pocket costs and the rules to be followed are all contrary to the idea that all Canadians should have equal access to health care—based on need, not their ability to pay or where they live.
The effect of the different rules and standards in Canada’s 100-plus public insurance plans means people in one province may not be able to get the same medication as someone who lives in the province next door, or may face a higher copayment or more paperwork before they can. One province may require doctors to get authorization from the plan before prescribing very expensive drugs or for drugs with a high potential for misuse, while other provinces have no such barriers. When some provinces and territories fund a drug and others don’t, access for Canadians with the same condition can be determined by their postal code instead of their medical need.
Example 2: Adult with cancer
David is a 58-year-old man who works as a mechanic and earns a net annual income of $50,000. He was recently diagnosed with advanced lung cancer.
He takes an oral cancer drug that costs almost $100,000 a year without drug coverage.
In some parts of the country, David’s cancer drug would be completely publicly covered, but in other jurisdictions he would pay anywhere from $250 to over $8,000 under the public system.
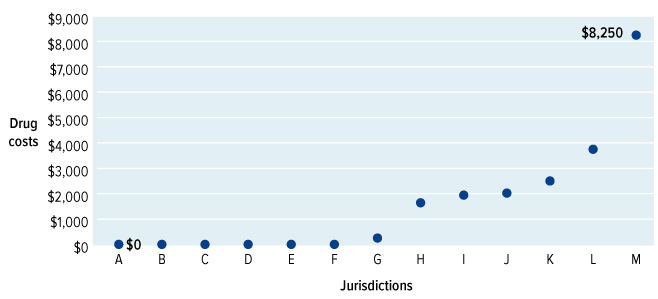
Example 2: Text description
| Jurisdiction | David's drug costs |
|---|---|
| A | $0 |
| B | $0 |
| C | $0 |
| D | $0 |
| E | $0 |
| F | $0 |
| G | $200 |
| H | $1,600 |
| I | $1,900 |
| J | $2,000 |
| K | $2,500 |
| L | $3,700 |
| M | $8,200 |
One of the most common arguments against pharmacare is that most Canadians have private drug insurance. While private plans cover about 60 per cent of Canadians,Endnote 15 they pay out just 36 per cent of Canada’s total spending on prescription drugs each year.Endnote 16 That’s partly because of who these plans serve: those enrolled tend to be healthier, working-age individuals between the ages of 35 and 54 and their families and those with higher household incomes—statistically, groups less likely to need prescription drugs. Also, prescription drug coverage is not evenly distributed among working people—according to the Wellesley Institute, 73 per cent of full-time employees report having medical benefit coverage while only 27 per cent of part-time employees do.Endnote 17 Accessing private drug coverage can also be a challenge for the many Canadians who are self-employed or work temporary jobs, such as contract or casual employment. Overall, it’s estimated between 27 and 45 per cent of all Canadian workers do not have stable, full-time jobs.Endnote 18 That means women, people with low incomes and young people—who are all more likely to work in part-time or contract positions—are often left without drug coverage, simply because of the type of work they do.
The nature of work has changed rapidly over the past two decades. Changing business practices and the emerging gig economy—where more people are working temporary contracts or are self-employed—are reducing opportunities for stable, full-time work. As a consequence, a growing number of Canadians are finding themselves without access to workplace drug benefits. Implementing national pharmacare would help ensure that all Canadians, regardless of what kind of job they have, enjoy fair access to prescription drug coverage now and into the future.
3.2 Cost
Having insurance, as we’ve said, does not mean people have no problems paying for medication. In a national survey, 23 per cent of Canadians told Angus Reid they or someone in their household had not taken their medicines as prescribed in the last year because they were too expensive.Endnote 19 According to the 2016 Canadian Community Health Survey, approximately 8.2 per cent of Canadians with a prescription (about 3 million individuals) said they were not able to afford one or more of their prescription drugs.Endnote 20 The 2016 Commonwealth Fund International Health Policy Survey put the number slightly higher, at 10.2 per cent.Endnote 21 A recent study found almost 1 million Canadians had cut spending on food and heat to pay for medication,Endnote 22 while another found 2.5 per cent of Canadians had borrowed money in the previous year to pay for prescription drugs.Endnote 23 Cost-related non-adherence (not taking a prescription properly because of its cost) is two to five times higher in Canada than in comparable countries with universal pharmacare.Endnote 24
Of those who told the 2016 Canadian Community Health Survey they could not afford one or more of their prescriptions, about 38 per cent had private insurance coverage and 21 per cent had public coverage.Endnote 25 The reason they can’t always pay, despite having insurance, is because most drug plans require members to pay a portion of the cost of each prescription (called a copayment or coinsurance). About 66 per cent of people with private insurance pay some level of coinsurance, typically 20 per cent of each prescription’s cost.Endnote 26 Canadian and international research shows that kind of direct charge makes people less likely to take prescribed drugs.Endnote 27 And the costs that people with private plans pay—between copays and deductibles—is increasing, from 10 per cent of their drug costs in 2005 to 15 per cent in 2017.Endnote 28 As well, the overall share of private health insurance premiums paid by employees has risen rapidly from 26 per cent in 2010 to 40 per cent in 2016.Endnote 29
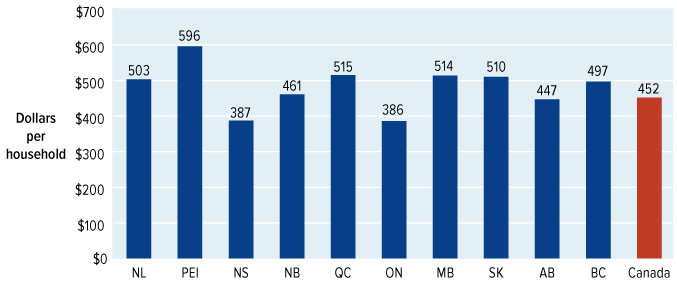
Source: Statistics Canada. (2017). Canadian Survey of Household Spending, Table 11-10-0222-01. CANSIM Database.
Figure 6: Text description
| Province/Territory | Dollars per household ($) |
|---|---|
| NL | 503 |
| PEI | 596 |
| NS | 387 |
| NB | 461 |
| QC | 515 |
| ON | 386 |
| MB | 514 |
| SK | 510 |
| AB | 447 |
| BC | 497 |
| Canada | 452 |
Source: Statistics Canada, Canadian Survey of Household Spending, 2017.
Another cost patients face is caused by some private and public plans not starting coverage until patients have paid a certain amount of their drug costs themselves, which is called a deductible. While deductibles are not common among private plans and, where they exist, are typically under $100 per family,Endnote 30 people on public plans may have to pay deductibles of hundreds or even thousands of dollars themselves before coverage begins.
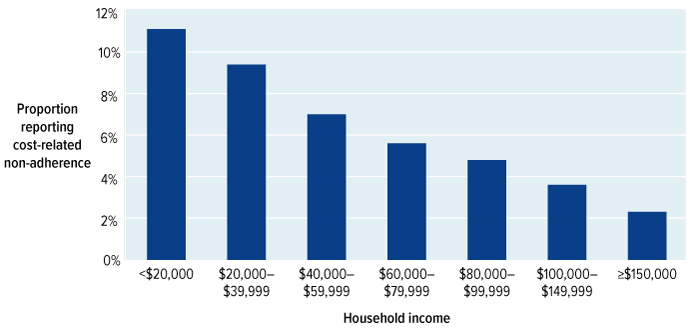
Source: Law, M. (2018). Cost-Related Barriers to Prescription Drug Access in Canada: A report prepared for the Advisory Council on the Implementation of National Pharmacare. Available from Health Canada by request.
Figure 7: Text description
| Household Income | CRNA (%) |
|---|---|
| <$20,000 | 11.1 |
| $20K-$39,999 | 9.4 |
| $40K-$59,999 | 7.0 |
| $60K-$79,999 | 5.6 |
| $80K-$99,999 | 4.8 |
| $100K-$149,999 | 3.6 |
| >$150K | 2.3 |
Source: Law, M. Cost-related Barriers to Prescription Drug Access in Canada: A report prepared for the Advisory Council on the Implementation of National Pharmacare. 2018.
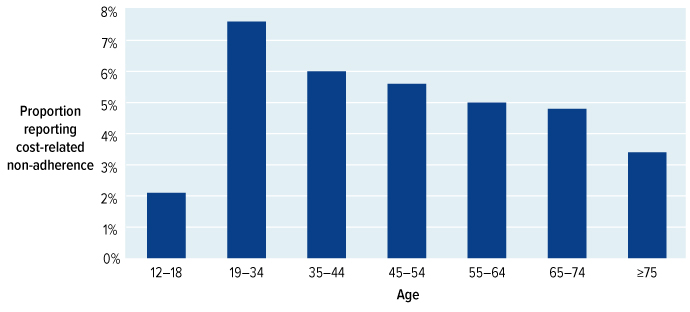
Source: Law, M. (2018). Cost-Related Barriers to Prescription Drug Access in Canada: A report prepared for the Advisory Council on the Implementation of National Pharmacare. Available from Health Canada by request.
Figure 8: Text description
| Age | CRNA (%) |
|---|---|
| 12-18 | 2.1 |
| 19-34 | 7.6 |
| 35-44 | 6.0 |
| 45-54 | 5.6 |
| 55-64 | 5.0 |
| 65-74 | 4.8 |
| ≥ 75 | 3.4 |
Source: Law, M. Cost-related Barriers to Prescription Drug Access in Canada: A report prepared for the Advisory Council on the Implementation of National Pharmacare. 2018
When people don’t take prescription drugs the way they are supposed to, their health can suffer. Several studies of the impact of out of pocket charges on Canadian seniors and people on social assistance found that more of them were admitted to hospitals and nursing homes after copayments were introduced; death rates increased as well.Endnote 31 According to the 2016 Canadian Community Health Survey, 43 per cent of Canadians who skipped prescriptions because they couldn’t afford them said their health worsened.Endnote 32
Copayments are also linked to patients needing more health care than they would have if they hadn’t had to pay them, which increases demand and cost for the health system.Endnote 33, Endnote 34 A 2018 study found approximately one-quarter of Canadians who said drug costs were an issue for them visited a physician, emergency room or hospital more than they would have otherwise.Endnote 35Researchers recently looked at the impact that removing out of pocket costs for medications would have on just three diseases—diabetes, cardiovascular disease and chronic respiratory conditions. They found that, for those three conditions alone, removing cost barriers would result in as many as 220,000 fewer emergency room visits and 90,000 fewer hospitalizations annually, representing potential savings to the health care system of up to $1.2 billion a year.Endnote 36
The cost of not being able to afford a prescription can also include lost wages for people who aren’t well enough to work.Endnote 37 Severe health problems caused by missed medication may eventually force people to stop working altogether.
A Patient’s Story—Ben Tripp-Wamboldt with Michelle Tripp
"I’m 19 and was diagnosed with type 1 diabetes at the age of one.
Diabetes management has always been a team effort between my Mom and me. Now that I’ve finished high school, I’m coming to terms with accepting and managing my condition on my own.
My diabetes has always been hard on my family and I felt guilty growing up. I know better, but I often reuse my syringes, skip tests or hold off on an injection a little longer to make my insulin last.
I’ve ended up in hospital a few times in the last year trying to stretch it a bit too far. To add insult to injury, I just found out that I have inherited sleep apnea. I’ve no idea where the money will come from for that equipment.
We’re in a good place with coverage for now, though the plan only covers 80 per cent and not the sleep apnea gear. With needles, test strips and insulin, it still really adds up.
Mom works two jobs now, it’s a lot of very early mornings that I wish she didn’t have to do. I’d like to take over paying for my medications to help out my Mom, especially because once I turn 21, I’ll be too old for her plan. I’m not sure how I will afford them.
My condition will never go away. With the economy the way it is, I feel the likelihood of me finding a good job with benefits is pretty low. With a pre-existing condition that will deny me private coverage, how will I cope?"
3.3 Sustainability
There have been steep increases in spending on prescription drugs used outside hospital in recent years. Today’s drugs have transformed both how and where patients are cared for. Situations that used to require a hospital stay—whether that’s managing pain, fighting infection, combatting cancer or curing disease—can be treated in the community. However, an increasing number of the drugs developed for use outside hospital are expensive specialty drugs that are steadily driving up the price of treatment. Since 2008, the average annual cost of specialty drugs has increased nearly 13 per cent per year.Endnote 38 The average cost of all drugs has increased by 7.3 per cent per year since 1987.Endnote 39 Prescription medication can greatly enhance people’s lives and can reduce hospital stays and other demands on the health care system, but it comes with a hefty price tag.
High-cost specialty drugs are not the only reason spending has increased: growing rates of chronic disease—such as diabetes and chronic obstructive pulmonary disease (COPD)—have contributed too. Greater demand and the rapidly rising number of high-cost drugs on the market have combined to take our spending on prescription drugs from its 1985 level of $2.6 billion (in today’s dollars) or 0.5 per cent of gross domestic product (GDP) to $34 billion or 1.6 per cent of GDP in 2018.Endnote 40 That averages to $909 per person. To cover those costs, public drug plans paid out $14.4 billion, private drug plans $12.3 billion and individuals and families spent $7.0 billion.Endnote 41 Furthermore, those costs are projected to grow by about 6.5 per cent each year over the next decade (see Annex 6). It’s no wonder that almost everyone we talked to (from both the public and private sectors) said they foresee a point in the near future where drug plans will be and sustainable.
Many employers are already concerned about how much they are spending on their employees’ prescription drugs and are looking for ways to reduce their costs. Some employers try to manage rising drug costs by trimming wages and other employee benefits, or by encouraging employees to shop at less expensive pharmacies. Others are introducing “health spending accounts,” where employees have a fixed amount of credits to put toward a range of health benefits, including drugs. An increasingly prevalent way to contain costs is to cap the amount of prescription drug benefits a plan member and their family can receive, either annually or over a lifetime. From 2013 to 2017, the number of private plan members with an annual or lifetime maximum on their drug coverage grew by around 40 per cent so that today more than a quarter of private plan members have capped coverage. Annual maximums typically range from $2,500 to $5,000; lifetime limits go from around $100,000 to $750,000.Endnote 42 Employees who reach their plan maximum pay for additional costs out of their own pocket or may move on to a public drug program if they are eligible. This trend to capping benefits is expected to accelerate as drug costs continue to climb.
Example 3: Couple with expensive biologic drug
Pierre and Laila are a working couple in their forties. Pierre drives for a local moving company and Laila works at a community centre. They earn a combined net annual income of $65,000.
Laila is taking several prescription drugs for ulcerative colitis, one of which is a high-cost biologic drug.
Without insurance, these drugs would cost the couple approximately $25,000 a year. With public drug coverage, they would have to pay different amounts, depending on where they lived in Canada, anywhere from $0 to over $10,000.
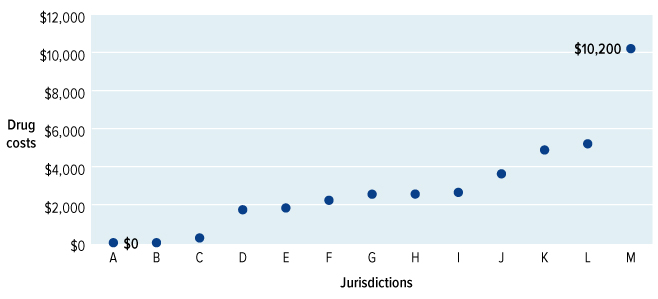
Example 3: Text description
| Jurisdiction | Laila's drug costs |
|---|---|
| A | $0 |
| B | $0 |
| C | $200 |
| D | $1,700 |
| E | $1,800 |
| F | $2,200 |
| G | $2,500 |
| H | $2,500 |
| I | $2,600 |
| J | $3,600 |
| K | $4,800 |
| L | $5,200 |
| M | $10,200 |
A Patient’s Story—Anonymous
"I have a rare form of leukemia. Prognosis and survival are determined by sorting through a slew of predictive factors; how you respond to treatment is as varied as there are patients. Luckily there are some very good treatment options available. They are life-changing, but staggeringly expensive.
Initially, this wasn’t a problem as my husband’s work benefits covered the drug. However, eventually, the president of the company was informed by the insurance provider that “someone” on the company plan was taking a very expensive drug. The carrier decided to boost the premiums for the coming year. He was displeased.
Unaware that I was the patient, the president grumbled to my spouse about ferreting out who this person was, not knowing he was speaking to the very partner.
We’re still not clear about how he found out it was me, but once he did, he made it his mission to get rid of my husband.
Thankfully, my husband is working again, but we worry that it may happen again. His new company's carrier increased premiums due to rising costs of "some patients’ drugs"—at least not just me this time. Senior management at this company does display empathy to employees and their families. We hope the sentiment lasts!
How is it in a country like Canada that employers seem to have the unfettered right to fire someone due to an illness in the family?"
There are other reasons private drug plans are looking less sustainable. Unlike public plans, which tend to fund only proven, cost-effective drugs, private plans have traditionally paid for nearly every drug approved by Health Canada, regardless of effectiveness or the value for money it offers. Private plans are concerned that expensive new drugs, including biologics and drugs for cancer, will drive costs to levels companies will not be able to afford.Endnote 43 To counter the impact of rising drug costs, some private insurers are starting to limit the selection of drugs they will pay for, or raising premiums. According to the Canadian Life and Health Insurance Association, premiums for extended health benefits grew at an annual rate of 3.9 per cent from 2012 to 2016.Endnote 44
Provincial and territorial governments are also struggling to cope with rising drug costs. These cost pressures have the potential to undermine the ability of provincial and territorial governments to provide services within and beyond health care, such as education and infrastructure. In a recent report, the Parliamentary Budget Officer found health care costs may threaten provincial and territorial government finances over the long term.Endnote 45 Rising drug costs are forcing provinces and territories to make difficult decisions about who is eligible for their programs and which drugs they will cover.
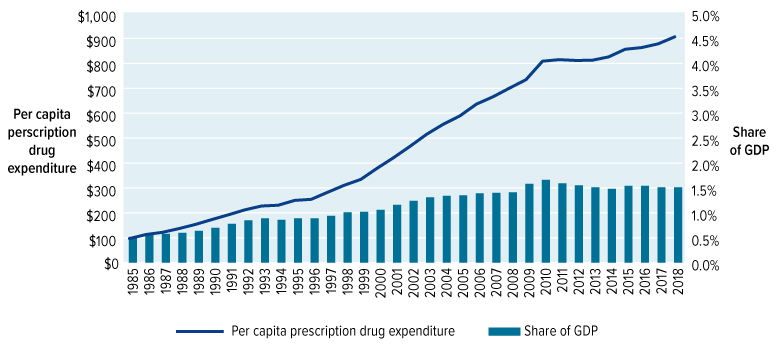
Source: Canadian Institute for Health Information. (2018). National Health Expenditures Database, 1975 to 2018, Table G.14.1. Ottawa, ON: CIHI.
Figure 9: Text description
| Year | 1985 | 1986 | 1987 | 1988 | 1989 | 1990 | 1991 | 1992 | 1993 | 1994 | 1995 | 1996 | 1997 | 1998 | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Share of GDP | 0.52% | 0.58% | 0.58% | 0.60% | 0.64% | 0.70% | 0.78% | 0.85% | 0.89% | 0.86% | 0.89% | 0.89% | 0.94% | 1.01% | 1.02% | 1.06% | 1.16% | 1.24% | 1.31% | 1.34% | 1.35% | 1.39% | 1.40% | 1.41% | 1.58% | 1.66% | 1.59% | 1.55% | 1.51% | 1.48% | 1.54% | 1.54% | 1.51% | 1.51% |
| Per capita prescription drug expenditure |
99.31 | 115.63 | 124.51 | 139.46 | 156.25 | 175.89 | 195.01 | 214.94 | 230.12 | 233.11 | 252.54 | 256.82 | 285.28 | 313.39 | 336.81 | 382.04 | 424.66 | 470.49 | 518.48 | 558.39 | 591.78 | 638.94 | 668.20 | 703.10 | 736.98 | 811.19 | 817.30 | 814.18 | 814.80 | 828.46 | 859.06 | 865.77 | 880.85 | 908.88 |
Source: Canadian Institute for Health Information, National Health Expenditure Database, 2018
3.4 Value for money
All countries struggle with the rising cost of drugs, but in 2017 Canada paid the third highest prices for brand name drugs and the seventh highest prices for generic drugs among the 34 countries of the OECD.
There are a number of reasons we pay more than other countries; one of the most important is buying power. Countries with universal public pharmacare can negotiate price deals with pharmaceutical companies on behalf of their entire population—if a manufacturer doesn’t offer a reasonable price on its new product, it risks being shut out of the market. In Canada, having thousands of different public and private insurance plans dilutes our negotiating power with global pharmaceutical firms. In an effort to counteract that, the provinces and territories established the pan-Canadian Pharmaceutical Alliance (pCPA) in 2010 to negotiate jointly on drug pricing and supply arrangements (such as maximum expenditure agreements) on behalf of participating public drug plans (the federal government joined in 2016). This collaboration is proving successful—as of April 2018, the pCPA had negotiated $1.98 billion in annual cost savingsEndnote 46—but the savings would be far greater if prices were negotiated for all Canadian prescriptions, not just those currently covered by public drug plans.
Other OECD countries also operate more efficiently when it comes to approving new drugs and managing coverage for them. Many have single national agencies or several closely-related organizations to manage medication approval and coverage. In Canada, however, the process that takes a drug from the research lab to the medicine chest is complex, decentralized, costly and slow, as shown in Figure 10.
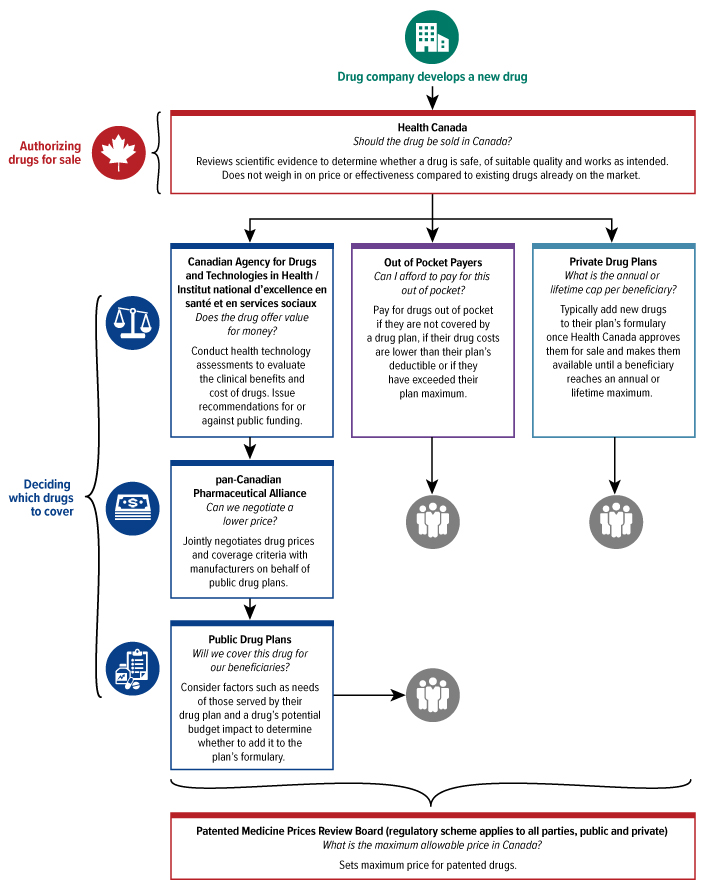
Figure 10: Text description
A tree diagram showing the steps for determining which drugs would be covered under a drug plan
- First, the drug company develops a new drug.
- Next, Health Canada authorizes the drugs for sale. The box reads: Should the drug be sold in Canada? Reviews scientific evidence to determine whether a drug is safe, of suitable quality and works as intended. Does not weigh in on price or effectiveness compared to existing drugs already on the market.
- There are three boxes after this that show how programs decide which drugs to cover. The first box shows the Canadian Agency for Drugs and Technology (CADTH) and l’Institut national d’excellence en santé et en services sociaux (INESS): does the drug offer value for money? Conduct health technology assessments to evaluate the clinical benefits and cost of drugs. Issue recommendations for or against public funding
- Immediately below the box about CADTH and INESS is a box about the pan-Canadian Pharmaceutical Alliance: Can we negotiate a lower price? Jointly negotiates drug prices and coverage criteria with manufacturers on behalf of public drug plans.
- Immediately below the pCPA is Public Drug Plans: will we cover this drug for our beneficiaries? Consider factors such as needs of those served by their drug plan and the drug's potential budget impact to determine whether to add it to the plan's formulary. This box then leads directly to patients.
- Beside the box about CADTH and INESS shows Out of Pocket Payers: Can I afford to pay for this out of pocket? Pay for drugs out of pocket if they are not covered by a drug plan, if their drug costs are lower than their plan's deductible or if they have exceeded their plan maximum. This box leads directly to patients.
- Beside the box about Out of Pocket Payers shows Private Drug Plans: What is the annual or lifetime cap per beneficiary? Typically add new drugs to their plan's formulary once Health Canada approves them for sale and makes them available until a beneficiary reaches an annual or lifetime maximum. This box leads directly to patients.
- Under all these stages is a box with the Patented Medicine Prices Review Board (Regulatory scheme applies to all parties, public and private): What is the maximum allowable price in Canada? Sets maximum price for patented drugs.
Another factor that reduces the value Canadians get for the money they spend on prescriptions is the inefficiency of a mixed system. Administration costs are generally three times higher in the private sector than the public sector, and that gap has widened over time. In 1975, administration accounted for 2.9 per cent of total public sector health expenditure and 2.5 per cent of total private sector expenditure. Since then, the public sector share gradually declined to 1.8 per cent in 2011, while the private sector share rose to 6.4 per cent.Endnote 47 Between these higher administrative costs and the amount kept as profits, private insurance adds considerable costs to an already expensive sector. It’s worth noting, however, the council heard that the profit margin on private prescription drug insurance is not large, particularly when viewed as a proportion of overall private health insurance plan profits.
The fractured approach to prescription drug coverage drives up costs in another way: it gets in the way of gathering data needed to deliver good care and plan for an efficient health system. Each of the federal, provincial and territorial public drug plans have their own ways of gathering information about their plan’s members and drug claims, as do private plans, but most of their systems don’t connect. That means prescribing data in this country is both fragmented and incomplete, making it nearly impossible to track prescription drug use to judge if it’s effective or appropriate, or to track spending or identify gaps in care.
3.5 The case for national pharmacare
The evidence is clear. Our current approach to funding and delivering prescription drugs is failing Canadians. It is unfair because it leaves 1 in 5 Canadians behind and exposed to unaffordable drug costs and poorer health outcomes. It is one of the costliest systems in the world in per capita terms and is increasingly unsustainable in the face of a surge of new high-cost drugs coming on the market. It does not deliver value for money for taxpayers, patients, employees and employers that fund the system.
The bottom line is that Canada needs a new plan: a plan that is fair, affordable, sustainable and delivers better value for money for Canadians.
International models of pharmacare
Before the council could recommend the best approach for Canada, it was essential we study how pharmacare works around the world. In Canada, as Chapter 2 described, the provinces and territories all offer drug insurance programs aimed at certain residents (see Annex 4), often including some variation of catastrophic coverage, alongside a separate private drug insurance system. No other country approaches pharmacare in this way. Instead, most countries with universal health care systems include prescription drugs in their insured services (along with hospital treatment, physician care and often a range of other health services).
The council’s research showed universal pharmacare in other countries (see Annex 5) generally follows one of two approaches:
- Single-payer public insurance, largely paid for by government, with varying degrees of patient cost sharing; or
- Statutory multi-payer insurance, where residents are required by law to buy insurance that meets national standards.
Universal public insurance, paid by government
Australia, New Zealand and the United Kingdom all fund universal public insurance to cover the cost of prescription drugs for their citizens, without deductibles and with limited or no copayments for eligible prescription drugs. Residents of these countries can also purchase complementary private insurance for things not covered by their universal public health insurance.
These systems are all financed through general tax revenues. Through their progressive taxation systems, the cost of care is shared among all members of society according to their means—the wealthy help to pay for services for the poor, and the healthy help to pay for the care of those who are ill.
This model was recommended for Canada by the 1964 Hall Commission, the 1997 National Forum on Health and the 2018 report of the House of Commons Standing Committee on Health.
Statutory multi-payer insurance
In France, Germany and the Netherlands, the law requires residents to buy health insurance, including drug coverage, from insurers that are primarily not-for-profit; it must meet standards set by the government. While it’s funded differently, the experience for patients is similar to single-payer systems with a single formulary, uniform drug coverage and similar out of pocket costs.
In France and Germany, individuals are required to make modest copayments for their prescriptions. In the Netherlands, individuals must pay an annual deductible of approximately $600 CAD for all their health care costs (including prescription drug costs), but do not pay any copayments for prescriptions at the pharmacy. Residents of these countries can also purchase complementary private insurance for things not covered by their statutory health insurance.
Chapter 4: A pharmacare plan for Canada
4.1 Principles of national pharmacare
During our consultations with Canadians, the council heard more than once from people who felt this country couldn’t afford national pharmacare. But it became increasingly clear to us that, in fact, we can’t afford to go on without it. We are already spending tens of billions of dollars on medicines. Canadians pay for prescription drugs through their taxes, through their premiums, through their wages and then they pay some more, when they reach into their pockets to cover their copayments and deductibles. This scattered approach to paying the bill is ill-conceived and inefficient. Ill‑conceived because, unlike services provided by medicare, benefits aren’t allocated on the basis of need. Inefficient because dozens of public and thousands of private plans have become a costly administrative nightmare, with little purchasing power to negotiate the best drug prices.
There is also the issue of fairness. More than ever before, people’s diseases are cured and their chronic conditions treated by medication—but many of those life-changing and life-saving drugs are extremely expensive. While most people are eligible for at least some coverage for drug costs, far too many Canadians suffer financially trying to pay for medication, or risk their health by not taking prescriptions they need, or not taking them properly to try to save money.
A Patient’s Story—Susan F.
"I have chronic illnesses I deal with daily.
A recent job loss coupled with my health status means I’m now on federal disability with a—very—limited income. My husband makes too much money (barely) to qualify for provincial support. No matter which way you cut it, even with two “incomes,” we are in a predicament. The price of everything goes up, support stays the same.
Access to provincial services is a Gordian knot of bureaucracy and interlocked agencies. Provincial pharmacare is a real mess. It takes so much energy to deal with and I must accumulate $1,300 in drug payments BEFORE I get support.
Money I simply don’t have.
I have no choice but to cut medications. This means my heart and thyroid are at risk. I stopped my arthritis meds and no longer have access to cannabis oil for pain. The result is I can barely move, I’ve gained weight, and have worsening circulation.
I wait inordinate amounts of time at the pharmacy and the doctor’s office, in pain, filled with anxiety, and trying to figure out what I can afford each month and which condition requires the most attention.
I’ve worked hard my whole life, but this is no retirement. I know others have it worse. But it’s no way to live."
We know that national pharmacare will result in savings. A single purchaser of prescribed medicines, acting on behalf of all Canadians, will have the necessary leverage to negotiate lower prices for the drugs we need. Billions of dollars of annual savings are expected once pharmacare has been implemented. Families, individuals and employers will save money through pharmacare.
Prescription medicines hold so much promise today. They have become integral to our health care, and vital to improved health outcomes. Fifty years ago, medicines prescribed in hospital were important enough to warrant inclusion in medicare. Today, as more and more medicines are administered in the community and at home, it just makes sense that prescribed medicines—wherever they are taken—should be accessible and affordable to Canadians.
In light of the above, it is difficult—if not impossible—to defend treating prescription drugs differently than other health care essentials. It is not enough to say this is the way it will be, because this is the way it has been. Adding another patch to the current patchwork of public and private drug insurance plans will not address the issue of fairness, access or affordability, nor will it address the need for future sustainability. It is time for Canada to join other advanced countries and implement a model of pharmacare that will improve health outcomes, manage costs and ensure Canadians can count on getting the medication they need, regardless of where they live, what their income is and whether they happen to have a job with benefits.
We are therefore recommending a national pharmacare plan that approaches prescription drug coverage the same way we approach physician and hospital care—through a universal, single-payer, public system that ensures access based on need, not ability to pay—one in which all residents of Canada can get the medication they need to maintain their physical and mental health.
Recommendation
- The council recommends the federal government work with provincial and territorial governments to establish a universal, single-payer, public system of prescription drug coverage in Canada.
If we are to recommend that prescription medicines be treated in the same manner as the other essential elements of health care—hospital and physician services—then it follows that the fundamental principles of national pharmacare should be consistent with the principles of medicare, as expressed in the Canada Health Act.
Principles for national pharmacare
The council proposes the five fundamental principles of medicare, embodied in the Canada Health Act, be applied to national pharmacare:
- Universal: all residents of Canada should have equal access to a national pharmacare system;
- Comprehensive: pharmacare should provide a broad range of safe, effective, evidence-based treatments,;
- Accessible: access to prescription drugs should be based on medical need, not ability to pay;
- Portable: pharmacare benefits should be portable across provinces and territories when people travel or move; and
- Public: a national pharmacare system should be publicly funded and administered.
4.2 Terms of coverage
Any drug plan begins by establishing who is covered, what drugs are covered and how much a patient will pay (through deductibles, copayments and premiums). As things are in Canada, each of these factors varies between public and private coverage and among the different provincial and territorial plans. National pharmacare will change that: consistent and high national standards will apply to all Canadians, and public drug plans will expand or adapt their programs to meet the national standards.
Under the plan we are proposing, provinces and territories would continue their existing coverage and related spending while the federal government funds the expansion of coverage required to meet the national pharmacare standards. In doing so, the federal government would need to acknowledge the actions already taken by provinces and territories so that jurisdictions that are further ahead are not disadvantaged. The provinces and territories would still be able to offer coverage beyond the national standards—for example, by providing coverage to seniors with no copayments—but would have to pay for such additional benefits themselves.
National pharmacare should offer comprehensive and affordable coverage so that no one will need supplementary private drug insurance. Nonetheless, individuals should be able to purchase private insurance to cover any out of pocket costs associated with pharmacare (such as copayments) and for drugs not listed on the national formulary.
When national pharmacare is fully operational, all Canadian residents with a valid Canadian health insurance card will be eligible to receive any medication listed on the national formulary.
As with medicare, Canadians would have continuous prescription drug coverage, even if they move or travel from one province or territory to another. From a patient’s perspective, national pharmacare would be seamlessly integrated with the existing health care system. Canadians should have confidence that when they leave the hospital, move, change jobs or stop working they will have uninterrupted access to the medicines they need to maintain their health.
Recommendations
- The council recommends national pharmacare provide flexibility for provinces and territories to offer coverage beyond the national pharmacare standards.
- The council recommends Canadians be allowed to purchase private insurance to supplement coverage under national pharmacare.
- The council recommends national pharmacare benefits be portable across provinces and territories.
Throughout its deliberations, the council was highly aware of, and sensitive to, the need for pharmacare to support the diversity of Canada’s population. A person’s risk of developing certain diseases and illnesses, and how well they respond to medication, is influenced by sex, race and age, among other factors.Endnote 48 Socio-economic status, isolation, discrimination, environmental factors, how Canadians self-identify and a myriad of other characteristics and behaviours can have a significant influence on health and illness and response to treatment. Each of these factors can also affect how people access health services, and how they experience government programs. The council believes a universal public drug insurance plan with a comprehensive formulary and minimal copayments is the best model for reducing inequities. As this model is put into place, and decisions are made, it will be important to always consider the potential gender and equity impacts—and to collect data that is specific enough to show trends and effects on minority populations.
Recommendation
- The council recommends a gender and equity lens be applied throughout the implementation of national pharmacare.
4.2.1 Who will national pharmacare cover?
The council believes all residents of Canada should be eligible for national pharmacare, just as they are for medicare. Treating drugs in a similar way to hospital and physician services would keep the new service in line with the values and principles that went into creating medicare in Canada. It would also make it easier to integrate pharmacare with provincial and territorial health insurance systems. This would reduce the likelihood that patients will have to struggle with complicated systems to get their benefits and enhance continuity of care and patient safety during transitions in and out of hospital.
Recommendation
- The council recommends all Canadian residents be eligible for national pharmacare to ensure everyone has access to the drugs they need to maintain their physical and mental health.
Almost everyone the council heard from felt that national pharmacare should be available to all Canadians and that coverage should be the same for everyone, regardless of their employment status, age, ability to pay or where they live. Calls to fill the gap, by focusing on the estimated 5 per cent of Canadians who have no coverage at all, do not recognize the problems faced by the 20 per cent of Canadians who may have some coverage, but who still struggle to find the money for deductibles and copayments.
Because of our patchwork of public plans and the huge number of private plans with all their variations, making drugs affordable for everyone was never going to be a straightforward matter of figuring out who doesn’t have coverage and making sure they get it. As we have shown, many millions of Canadians are struggling with gaps in drug coverage, in addition to those who have no coverage at all. It would be extremely challenging to find all the gaps that need filling, and such an approach would not reduce drug prices or address the differences in drug coverage that exist within and between provinces and territories today, or that might develop in the future. Medicare doesn’t just fill the gaps and neither should pharmacare.
4.2.2 What drugs will pharmacare pay for?
National pharmacare will offer patients and prescribers a wide range of medication—but the council believes the formulary—the list of drugs eligible for funding—must be based on the best evidence available, with preference given to drugs that both maximize health benefits and offer good value.
The formulary will include drugs for common conditions, as well as those for more complex, serious illnesses. It should also include a limited number of medical devices and supplies associated with taking prescription drugs, such as aerochambers for inhaled medication. The council heard from many Canadians how access to prescription drugs should also include access to the devices and supplies needed to administer the drug, as well as monitor its effect (such as syringes and blood sugar test strips).
Like all aspects of pharmacare, the formulary should be introduced step by step. The council recommends beginning coverage with a carefully chosen list of priority essential medicines, covering the vast majority of conditions, which would be added to over time. Details on developing and expanding the list are in Chapter 5 of this report.
Recommendation
- The council recommends national pharmacare provide coverage for a national list of prescription drugs and related products (a national formulary) to ensure all Canadians have equal access to the medicines they need to maintain or improve their health.
Special provisions will be needed for expensive drugs for rare diseases, where extremely high prices and often insufficient evidence of effectiveness, safety and value for money means many are unlikely to meet the regular standards for formulary listing. For these expensive drugs for rare diseases, the council is recommending a distinct national process for considering, providing and monitoring these drugs. We give more details in Chapter 5.
4.2.3 What costs will patients pay?
The question of whether national pharmacare should require patients to bear some of the costs of prescription drugs is not an easy one to answer. Most public and private drug insurance in Canada requires patients to pay a share of costs, although the approach to charging them and the amounts vary considerably. Cost sharing, while common, is criticized by health policy experts because it can prevent people from taking the medicine they need to stay healthy. Research shows even small charges to patients when they pick up prescriptions can be a barrier to getting needed medication, which can hurt their health and often costs the health system more down the road. User fees are typically regressive, which means they impose a greater financial burden on lower-income households. User fees can be particularly hard on patients with chronic conditions, because they have to pay them year after year (sometimes called taxing the sick). Both Canadian and international research is quite clear that direct charges to patients can result in them not taking the medication they need.Endnote 49 It is both intuitive and scientifically proven that cost barriers should not be imposed at the point of care, in the time of need. The same rationale for not charging user fees to see your doctor, or visit an emergency room, applies to prescribed medicines.
Furthermore, there is little evidence that ‘free’ prescription medicines lead to overuse, abuse or wastage. In fact, a Scottish study found that as copayments were gradually reduced, use of prescription medication went up. This increase slowed considerably over the course of four years, suggesting that the initial uptick in use was because some people had not been getting the drugs they needed, rather than a surge in wasteful consumption.Endnote 50
Impact of patient cost sharing in Canada
Several studies have examined what happened when Quebec’s health-insurance program, the Régie de l'assurance maladie du Québec, shifted drug benefits from free or $2 per prescription to a 25 per cent coinsurance charge (capped at $200, $500 or $750 per year, depending on income). One study found the change decreased the number of drugs used per day by 9 per cent in the elderly and 14 per cent among people on social assistance.Endnote 51
A study of a Nova Scotia policy that modified seniors’ coverage from no copayment to $3 per prescription (up to an annual maximum of $150) found that among those who were unlikely to reach their annual maximum, the use of drugs for peptic ulcers and reflux disease dropped by 5 per cent and the number of users of one type of diabetes drug also decreased by 5 per cent.Endnote52
In addition to creating a financial barrier, collecting user fees will add to the cost of running pharmacare. Nevertheless, cost sharing by patients is a common feature of both public and private drug insurance plans, in Canada and internationally. Sharing cost would help to finance pharmacare and drug plan officials told the council they believe it does encourage the proper use of drugs.
The council believes that deductibles (where a patient pays 100 per cent of the cost of drugs until a set dollar threshold is reached) are likely to deter people from filling their prescriptions, and can be particularly hard on patients with chronic conditions. For those reasons, we do not support their use. Instead, we support minimal copayments, provided they include measures to limit financial hardship, such as an annual cap on how much any given household must pay out of pocket. Setting this cap at $100 per year would protect households with above-average prescription drug needs and is significantly less than the current average household out of pocket expenditure of $450.Endnote 53 We also recommend that people on very low incomes, such as people receiving social assistance, government disability benefits, or the federal Guaranteed Income Supplement should be exempt from all copayments. To help keep the system affordable over the long term, the council supports using methods that encourage patients and prescribers to choose the most cost-effective therapy (for example, charging lower copayments for a select list of tried and true essential medicines or generic versions of a drug).
Patient Story—Anonymous
"I live in small-town rural Canada, 35 kilometers from the nearest hospital. Specialist care is 600 kilometers away. Three years ago, after getting increasingly sick and a year’s worth of ER visits, I was finally diagnosed.
The accompanying vomiting caused by my condition was so intense that I had a heart attack. Upon release, I was prescribed nine medications costing about $6,000 per year. I only make about $17,000 a year, so the drugs were one-third of my income.
I like working and want to continue to do so, but I don’t have a private drug plan, so can’t afford these medications.
I applied for the public pharmacare program, but my deductible is $1,700, which is still 10 per cent of my income, before I can get benefits.
I can’t afford to eat properly, I keep the house temperature at 10°C, forcing me to wear long johns and sweaters. I’m only able to get my meds because my drugstore is willing to give me my drugs on credit.
Despite the public plan coverage, I’ve had to give up something to afford my prescriptions. I no longer have house insurance, as I need my vehicle to get to work.
It’s pretty clear to me that the system is broken and unfair. I live very modestly. I don’t think I should lose my autonomy and necessities to get assistance with a condition over which I have no say."
Recommendations
- The council recommends out of pocket costs for all products listed on the national formulary not exceed $5 per prescription, with a copayment of $2 for essential medicines, and an annual maximum of $100 per household per year to ensure that patients face few barriers to access.
- The council recommends people receiving social assistance, government disability benefits or the federal Guaranteed Income Supplement benefit be exempt from copayments.
4.3 The way forward
The council strongly believes in its vision for national pharmacare, but understands such transformative change can’t happen overnight. It will take time, significant federal investment and close collaboration among all health system partners to turn Canada’s patchwork of prescription drug insurance plans into a national public pharmacare program. In the next chapters, we will share our recommended implementation strategy and describe the key foundational elements that need to be put in place to ensure success.
Chapter 5: Getting to national pharmacare
There have been repeated calls for national pharmacare over the past half-century as one commission or study or group after another has recognized the critical role prescription drugs play in improving health outcomes for Canadians. But as our name clearly shows, the Advisory Council on the Implementation of National Pharmacare was not created merely to endorse a good idea. It was our mandate to study domestic and international models of prescription drug insurance and then recommend a way to implement a model of pharmacare that will work in Canada, for Canadians.
Because the transformation required is so enormous, it soon became clear to us that implementing national pharmacare would require a careful step-by-step approach, over time, in an achievable, logical order. It will take time, for example, for different governments to expand public drug coverage to all their residents; time to develop a national formulary and negotiate prices; time to work out funding and legislative details. But pharmacare will not have to wait until everything is ready to go. As we have it planned, some changes for the better will begin to be seen almost immediately, and will continue to evolve to be fully operational; others will have to be sequenced and some will begin further down the line. The time frame, however, is limited: we are calling for comprehensive national pharmacare to be fully implemented within eight years.
5.1 Government collaboration
Although pharmacare will be delivered by the provinces and territories, the council strongly believes it should be a uniform experience across the country without the variations and unfairness that result from today’s mixed bag of insurance plans. All Canadian residents, regardless of where they live, their employment status or their income, should receive a consistent standard of coverage.
Because the provinces and territories, and not the federal government, have jurisdiction over health care delivery, achieving national pharmacare will require close collaboration and extensive negotiation to get the program up and running and to ensure it operates smoothly. It’s the council’s view that a shared approach to governance, with collective decisions on pharmacare issues, is the best way to achieve a fair, nationally consistent patient experience. This collaborative approach is at the heart of the council’s recommendation to establish a Canadian drug agency to manage pharmacare.
The federal government and the provincial and territorial governments should begin discussions towards establishing the Canadian drug agency as soon as possible, beginning with confirming the principles and national standards (outlined in the previous chapter) that will underpin national pharmacare and guide the agency’s work. Because federal funding will be central to these negotiations, we have advice on financing arrangements later in this report.
As with medicare, it will be up to individual provinces and territories to opt in to pharmacare by applying the national standards in their jurisdictions. We recognize that jurisdictions’ readiness will vary, so it may take some time before all provinces and territories are prepared to opt in. This should not deter the federal government and jurisdictions that are ready to move forward on national pharmacare. In a country as large and diverse as ours, universal drug coverage on common terms and conditions will only be achieved through a combination of leadership, patience and collaboration.
Recommendations
- The council recommends provinces and territories deliver national pharmacare in a manner that meets or exceeds agreed-upon national standards, in exchange for federal funding.
- The council recommends the federal government work collaboratively and in partnership with provincial and territorial governments to begin the implementation of national pharmacare in 2020.
- The council recommends the federal government be prepared to proceed with national pharmacare even if not all jurisdictions are in a position to opt in at the outset.
5.2 Indigenous engagement
The overall health of First Nations, Inuit and Métis peoples has improved over the last few decades, but the council is aware that the health status of Indigenous peoples remains well below the Canadian average.Endnote 54 Furthermore, Indigenous people are more likely than the average Canadian to report cost-related reasons for not taking prescribed medication.Endnote 55 These differences are rooted in a range of historical, political, cultural, geographical and jurisdictional factors.
The council was given the responsibility of engaging with Indigenous leaders and communities on national pharmacare, and we met separately with First Nations, Inuit and Métis governments and representative organizations. While the council did not have a mandate to make recommendations on the Non-Insured Health Benefits Program, our discussions highlighted some of the key challenges Indigenous peoples experience in accessing medication, including administrative, geographic and systemic barriers. People noted the burden of paperwork and complex processes, and an interest in having a range of treatment options available. In rural and remote communities, we heard about long travels to get to prescribers and pharmacies. Not infrequently, the conversation turned to the lack of adequate food and housing, the effects of systemic racism, cultural trauma and poverty.
Throughout our discussions, we heard a desire to understand how pharmacare could help improve access to medication for Indigenous peoples and an interest in continuing a dialogue on national pharmacare. People may have different views about how existing federal drug benefits for registered First Nations and recognized Inuit should be handled going forward, for example. These discussions impressed on us the need for a national pharmacare plan to recognize the distinct issues different First Nations, Inuit and Métis communities face—there is no one-size-fits-all answer. We recognize that despite our best efforts, in the time we had we only began to scratch the surface of many interconnected challenges, and that many of the people we engaged with could only speak for themselves, not on behalf of others in their community. This is a conversation that must continue.
The council recommends the federal government work with First Nations, Inuit and Métis governments and representative organizations, to develop a framework and process for determining whether and how they might wish to participate in national pharmacare. While the council is not proposing changes to non-insured health benefits, we are aware that only registered First Nations and recognized Inuit qualify for that program. The potential impacts of national pharmacare on First Nations, Inuit and Métis should be addressed in partnership with them.
The council notes that the United Nations Declaration on the Rights of Indigenous Peoples sets out that “Indigenous peoples have the right to be actively involved in developing and determining health, housing and other economic and social programmes affecting them and, as far as possible, to administer such programmes through their own institutions.”Endnote 56 In respect of this, Indigenous peoples of Canada must themselves choose the nature of their participation in national pharmacare.
Recommendations
- The council recommends the federal government work with First Nations, Inuit and Métis governments and representative organizations to develop a framework and process for determining whether and how they will participate in national pharmacare.
- The council recommends ongoing engagement with First Nations, Inuit and Métis partners to consider how the knowledge and perspectives of Indigenous peoples should be incorporated throughout the implementation of national pharmacare.
5.3 Creating a Canadian drug agency
As we mentioned in Chapter 3, other OECD countries run drug insurance systems that are more efficient than ours in several ways, including having single national agencies or several closely-related organizations to manage many aspects of their drug insurance systems. The council believes national pharmacare will work better and deliver greater value if it’s run by a single national agency governed by a board of directors accountable to Canadians, both directly and through federal, provincial and territorial ministers of health.
This board should be made up of representatives from the federal government and every provincial or territorial government participating in national pharmacare. Governments may wish to nominate individuals with a range of relevant skills, such as financial, health and legal expertise, who need not necessarily be government officials. In addition, the board should contain voting members representing patients and the public at large. Patient representatives of the board should maintain appropriate links with patient groups with guidance from the agency once it is established. Appropriate Indigenous representation should be broached as part of the engagement with First Nations, Inuit and Métis governments and representative organizations. An independent chair with experience in public sector governance should be appointed as soon as possible to get the agency up and running.
Governments in Canada have made great strides over the past 15 years developing tools and capacity to evaluate how well drugs work and advise on whether public funds should be used to pay for them. At one time, each government undertook its own assessment independently, which was very inefficient and resulted in different coverage decisions across provinces and territories. Today, the Canadian Agency for Drugs and Technologies in Health (CADTH) evaluates the clinical benefits and value for money of drugs on behalf of governments. Quebec has created its own agency (the Institut national d’excellence en santé et en services sociaux, or INESSS) to evaluate drugs and advise the government on which drugs should be included in the public plan.
Institut national d’excellence en santé et en services sociaux (INESSS)
Created in 2011, INESSS’ mission is to promote clinical excellence and the efficient use of resources in the field of health and social services in Quebec. It assesses the clinical benefit and cost of drugs to recommend whether they should be listed on the province’s public drug plan formulary. In making its recommendations, INESSS reviews the scientific evidence for the drug and considers both expert opinions and the experience of health professionals, patients and their caregivers. Based on its recommendation, Quebec’s minister of Health and Social Services makes the final decision on whether to include the product on the provincial formulary.
Similarly, provincial and territorial governments have made significant progress in the last several years by working together to negotiate better drug prices and supply arrangements with the aim of improving consistency of decision-making. Before this, larger provinces would each negotiate with drug manufacturers to get discounts on drug prices. Smaller jurisdictions had less clout and capacity to do this and ended up paying much higher prices for drugs. By banding together through the pan-Canadian Pharmaceutical Alliance (pCPA), provinces and territories use their collective buying power to negotiate lower prices for all public plans. The federal government joined the pCPA in 2016 and also benefits from lower negotiated prices for drugs covered under federal prescription drug plans.
In Budget 2019, the federal government made a commitment to establish the Canadian Drug Agency to assess prescription drugs and negotiate prices on behalf of Canadians. To lay the groundwork for this vision, Budget 2019 announced funding for a Canadian Drug Agency Transition Office beginning in 2019‑20. The council recommends the new agency be an arms-length body accountable to Canadians both directly and through the federal, provincial and territorial ministers of health.
As successful as the pCPA has been in negotiating $1.98 billion in annual cost savings, the council heard it lacks dedicated resources and that collective decisions to negotiate prices and list new drugs sometimes break down because of different policies and fiscal capacity across jurisdictions. At the same time, we were told its success is due in large part to provincial and territorial governments each having a seat at the table, and that should be an essential feature of its evolution in the future.
Beyond CADTH and the pCPA, the federal government also has resources and expertise in Health Canada, the Patented Medicine Prices Review Board (PMPRB) and the Canadian Institutes of Health Research (CIHR) that should be considered in building a new drug agency. The goal should be to ensure the Canadian drug agency has all the expertise and resources it needs to oversee pharmacare on behalf of all Canadians and their governments. Central to this role is managing the national formulary. To ensure Canadians have access to safe, effective treatment options and can benefit from consolidated bargaining power, the agency will perform a number of key functions including:
- Assessing the clinical effectiveness of drugs compared to other treatment options;
- Assessing the cost-effectiveness of drugs compared to other treatment options;
- Deciding which drugs and related products (such as devices and supplies) should be on the national formulary;
- Negotiating prices and supply arrangements with manufacturers;
- Providing advice to prescribers, pharmacists and patients on how best to use drugs; and
- Monitoring the safety and effectiveness of drugs in real-world use.
Knowing how well a drug works relative to other options on the market will put the agency in a good bargaining position to negotiate with drug manufacturers. Other countries with universal drug coverage use their consolidated market power to negotiate lower prices for both patented and generic drugs—if a manufacturer doesn’t offer an acceptable price on a new drug, it risks being shut out of the country’s market entirely. In its role negotiating pricing and supply arrangements for the drugs covered under national pharmacare, the Canadian drug agency will benefit from similar strong bargaining power and will be better able to control rising drug costs. There are many innovative price-control strategies the drug agency could use, including pay-for-performance agreements. Some countries, including New Zealand, and many Canadian hospitals make extensive use of tendering to get good prices for drugs. We believe the Canadian drug agency should study different approaches and make judicious decisions about which negotiating approaches make sense in the Canadian context.
It will be important for the agency to maintain very high clinical and ethical standards in assessing evidence of the clinical benefit and value for money of drugs. Making patients an integral part of the agency’s work—such as helping to determine what good or better looks like for someone with a particular illness or disease—will help ensure the agency focuses on drugs that will benefit Canadians most.
It is equally critical that the agency be designed and run in a manner that is responsive and accountable to Canadians and their governments. One of the ways to accomplish this is to ensure citizens have a strong, meaningful and ongoing role in decision-making by the agency. Another is by being transparent in governance and decision-making.
By working closely with Health Canada and with manufacturers bringing new drugs to market, the agency can also minimize delays between the time a drug is approved for sale in Canada, and when it is added to the national formulary. For example, if a drug looks promising, the agency could start assessing its value for money while Health Canada is assessing its safety, efficacy and quality, which could speed up and improve access for Canadians. Indeed, as collaborative work with the provinces and territories begins, it will be important to ask the question whether some, or all, of the functions Health Canada currently does could be better and more effectively managed at arms-length by the Canadian drug agency.
To date, there has been a lot of attention paid to the safety and effectiveness of new drugs entering the market, but determining how they work under real-world conditions is equally important. That is why the council recommends the agency also collect and weigh so-called “real-world” evidence, to help inform its formulary decisions. In this way, drugs that stand the test of time will remain on the formulary, while those that turn out to cause more problems than they solve can be removed. Such real-world monitoring will also prove valuable in detecting and responding to prescription drugs found to be associated with adverse events and side effects, important work that is harder to do under a patchwork system.
With all this information, the agency will be well placed to help clinicians and patients make good choices about the drugs that will work best for them. To that end, developing a national strategy for appropriate prescribing will be another key role for the agency, as described in Section 5.6.
The Canadian drug agency would also be responsible for monitoring and reporting on national pharmacare’s success in improving Canadians’ access to medication and their health outcomes. To do this, the agency would work with federal, provincial and territorial officials to develop a set of indicators for measuring national pharmacare’s performance, then work with jurisdictions to gather the necessary data to measure the results. As noted in Chapter 7, data about the use of drugs in Canada is fragmented and incomplete. The launch of national pharmacare is an opportunity to change that.
Recommendations
- The council recommends federal, provincial and territorial governments collaborate to create a new arms-length Canadian drug agency to oversee national pharmacare. The new agency should have the following functions:
- Assessing the clinical effectiveness of drugs compared to other treatment options;
- Assessing the cost-effectiveness of drugs compared to other treatment options;
- Deciding which drugs and related products (such as devices and supplies) should be on the national formulary;
- Negotiating prices and supply arrangements with manufacturers;
- Providing advice to prescribers, pharmacists and patients on how best to use drugs; and
- Monitoring the safety and effectiveness of drugs in real-world use.
- The council recommends the federal, provincial and territorial governments and the public be represented in the governance of the Canadian drug agency. Patients must be represented on the board and should maintain appropriate links with patient groups.
- The council recommends federal, provincial and territorial governments work together to determine which existing resources and expertise should be brought into the Canadian drug agency from Health Canada, pCPA, CADTH, PMPRB, CIHR, and others.
- The council recommends the new agency use rigorous evidence-based methods to evaluate the clinical effectiveness and value for money of prescription drugs to support the development of a national formulary.
- The council recommends the new agency develop and implement a comprehensive evidence-based national formulary to ensure patients have access to the same prescription drugs no matter where they live across the country.
- The council recommends the Canadian drug agency work closely with Health Canada and manufacturers to shorten the time it takes for prescription drugs that present good value for money to be listed on the national formulary.
- The council recommends the Canadian drug agency negotiate prices and supply arrangements with manufacturers to ensure Canada is getting the best deal and the lowest prices.
- The council recommends the new agency monitor the safety and effectiveness of prescription drugs to ensure they continue to benefit patients and deliver value for money.
- The council recommends the new agency implement a national strategy for expensive drugs for rare diseases to provide access to these drugs across Canada.
- The council recommends the new agency report publicly on the performance of national pharmacare to ensure governments and the agency are accountable to Canadians.
- The council recommends the federal government provide ongoing funding for the new agency to ensure it is able to meet its objectives.
5.4 Developing a national formulary
A national formulary—a comprehensive, evidence-based list of prescription drugs covered by pharmacare—will ensure people across the country have access to the drugs they need to maintain their physical and mental health. Once fully implemented, a national formulary will provide an appropriate range of treatment choice across the full continuum of care—from common conditions largely seen in primary care to medically complex conditions treated by specialists and taking both physical and mental health into consideration. Though it will focus on prescription drugs taken in the community, the national formulary should also be harmonized with the formularies of Canada’s hospitals and cancer agencies to support smooth transitions for patients treated by them. The national formulary should also include safe and appropriate options to meet the needs of Canada’s diverse population, including children, seniors, Indigenous peoples, other racial and ethnic minorities and the lesbian, gay, bisexual, transgender, queer, intersex and two-spirit community. The national formulary should focus on drugs shown to be both effective and good value.
Children’s medications
Children and youth represent more than a quarter of the Canadian population, however many drugs available in Canada have not been specifically approved for use by infants, children or youth. This is not necessarily because they aren’t safe or effective, but because research to show they are has not been done, or companies haven’t sought Health Canada approval for pediatric use of their drug. As a result, appropriate approvals, dosing information and child-friendly formulations of many drugs don’t exist in Canada, making it challenging for clinicians to prescribe for children and youth, and for public plans to cover the drugs they need.
Having commercial child-friendly formulations available for Canadian pediatric patients is vital. In many cases, commercialized pediatric formulations are available in the United States and in Europe, but the complexity of Canada’s drug coverage system discourages companies from marketing them here. Under national pharmacare, the creation of the Canadian drug agency and the development of the national formulary will mean a clear and consistent listing and reimbursement process for drugs country wide. That’s expected to encourage drug manufacturers to bring more pediatric formulations to Canada and support optimal treatment of Canadian children and youth.
When commercialized pediatric formulations are not available in Canada, adult medications need to be modified in pharmacies (perhaps by suspending a crushed tablet in a liquid) to create the doses children and youth need. This practice is known as compounding and, while necessary, can introduce significant variability in treatment and increase the risk of dosing errors. A national formulary will be a single, validated, comprehensive and accessible source of information for prescribers and pharmacists and support standardized and safe pediatric medication dosing and pharmacy-based compounding.
To support the safe, effective and consistent treatment of children across the country, the council believes the national formulary must be developed in close collaboration with pediatric clinical experts to ensure the drugs selected and the clinical guidance developed for them accurately reflect the scope of pediatric prescribing and align with best practice. Those same experts can assist the Canadian drug agency in strategic and policy efforts to improve access to pediatric drugs through national pharmacare.
Developing and maintaining the national formulary will be one of the key responsibilities of the Canadian drug agency. We believe the process should start with the agency appointing a group of experts including health care providers, patients and drug plan administrators, among others. This group will determine, based on evidence, which drugs should be included on the national formulary and the conditions for their use (such as whether a drug should be covered only for certain indications, or for certain patients). Because it will operate at arm's length, the Canadian drug agency will be well-positioned to choose drugs based on evidence, not lobbying efforts or political pressure.
Recommendations
- The council recommends the national formulary be evidence-based and comprehensive to offer patients and prescribers effective treatment choices.
- The council recommends the national formulary include prescription drugs that treat both physical and mental health conditions.
- The council recommends the national formulary provide appropriate treatment options for different age, race, ethnicity, sex and gender identity, among other factors, so that it responds to the needs of all Canadians.
- The council recommends the national formulary include prescription drugs that respond to the specific and unique needs of children and youth, and that a strategy be developed to address the availability of approved drugs and formulations for them.
The drug agency would begin building the formulary by establishing principles to guide the evaluation and selection of drugs (see text box: Proposed Principles for Including Drugs on the National Formulary). Decisions on what to include on the formulary will be transparent, and publicly communicated in plain language
Proposed principles for including drugs on the national formulary
The council believes decisions about whether to include a drug on the national formulary should consider:
- The clinical benefit it offers patients;
- Its value for money;
- Its alignment with patient and societal values, including diversity and equity considerations; and
- Its broader impact on health care and health outcomes.
The above principles are based on those considered by formulary review committees across Canada, including those at CADTH and INESSS.
A vast array of drugs is available for sale in Canada today, with dozens of new products being launched every year. Sifting through these products to develop a comprehensive, evidence-based national formulary of medications that maximize health benefits and deliver good value will be a major undertaking. As a foundational step, the drug agency will identify the overall mix of drugs that Canadians would have access to once national pharmacare is fully implemented. Based on this formulary framework, the agency will then proceed to assess groups of drugs (such as all drugs for diabetes) to determine the different drug types and number of choices that should be included on the formulary and then negotiate pricing and supply arrangements for them. It currently takes up to six months to determine whether a new drug offers value for money relative to other treatment options, and this is typically followed by several months of negotiations with the manufacturer to achieve a satisfactory price.
It will be important to develop a prioritization framework to determine the order in which drugs will be evaluated, negotiated and added to the national formulary until it reaches maturity. This prioritization framework should consider: therapeutic areas where there is a high degree of consistency across public drug plans (these are the tried-and-true drugs that are widely accepted as effective choices); therapeutic areas where there is greater variability (such as cancer drugs); as well as national health priorities (such as mental health).
The council supports managing the national formulary to encourage the use of less expensive but equally effective generic drugs by putting generic substitution policies in place. Under these policies, long used by public drug plans and many private plans, pharmacists automatically fill prescriptions with generic, rather than brand name, drugs. Generic drugs are equivalent to brand name drugs in safety, quality, dosage form, strength, intended use and performance but cost less. Canadians who prefer brand names to generics will be able to make that choice but would pay the difference in price. Brand cards provided by drug manufacturers can reimburse patients for the difference in price between generic and brand name prescription drugs, but they undermine the use of generics and their use should be reconsidered.
Biosimilars are biologic drugs proven to have the same clinical effect as more expensive brand name biologic drugs already authorized for sale. Canada’s use of biosimilars has been very low relative to other countries due to a combination of factors, including limited awareness of the clinical and scientific evidence supporting the use of biosimilars, and aggressive marketing techniques used by brand name biologic companies to retain their market share.
Biosimilars made up less than 7 per cent of Canada’s biologic market in 2017, while the OECD average was more than 30 per cent.Endnote 57 Seven of the top 10 prescription drugs in Canada, by sales, are biologics and in 2017, one of them had Canadian sales of almost $1 billion.Endnote 58 The potential for saving money by using more biosimilars is profound. The council recommends that national pharmacare put policies in place to encourage biosimilar use, including biosimilar substitution. Prescribers and patients should be better supported with information reinforcing the safety, efficacy and benefits of biosimilars. National pharmacare also provides an excellent opportunity to collect Canadian data on the effectiveness of biosimilars to inform future decision-making.
Another option to help balance choice and value for money could be reference-based reimbursement. In a given category of drugs that treat the same condition (such as hypertension), and medical evidence shows are equally safe and effective, a drug plan would limit reimbursement to a “reference standard,” typically either the lowest priced drug or the average price of the drugs in a category. In this situation, individuals who opt for more expensive drugs must cover the price difference out of pocket. If an individual cannot take a fully-reimbursed drug for a medical reason (such as side effects), full coverage for a more expensive drug can be provided with special authorization.
Recommendations
- The council recommends mandatory generic substitution policies to encourage patients and prescribers to choose the most cost-effective therapies and help keep national pharmacare affordable.
- The council recommends formulary management policies, including requiring biosimilar substitution, that support the use of biosimilars and encourage patients and prescribers to choose the most cost-effective therapies to ensure the sustainability of national pharmacare. Prescribers and patients should be better supported with information reinforcing the safety, efficacy and benefits of biosimilars.
- The council recommends the Canadian drug agency work to increase prescriber and public awareness about the equivalency of generics to brand name drugs and the rationale for greater use of generics and biosimilars to keep pharmacare affordable.
5.5 Implementing a national formulary—starting with essential medicines
Given the transformation necessary for national pharmacare, and the time required to build a national formulary, it is practical to consider a phased approach to implementing pharmacare. This phased approach could take different paths, however the council recommends beginning with a carefully chosen list of essential medicines available to all Canadians, as the first step towards a fully comprehensive list of drugs available to all Canadians. This will enable a meaningful and early start to national pharmacare to become a reality faster, since evaluating and negotiating prices for the complete formulary will take some time. The list of essential medicines—the most commonly prescribed clinically important drugs—would likely account for about half of all prescriptions dispensed in Canada.Endnote 59
There are two lists we think the Canadian drug agency should use as a starting point for creating the initial essential medicines list: the World Health Organization’s Model List of Essential Medicines (which has approximately 450 drugs) and the CLEAN Meds list (with 136 drugs) developed by clinician and researchers at St. Michael’s Hospital in Toronto. The drugs selected for the initial formulary should also be aligned with the national formulary’s guiding principles.
The council recognizes that patients and their care teams would like to have access to a full range of treatments through a comprehensive national formulary right away. However, if the Canadian drug agency added everything covered by public and private plans to the formulary immediately, without taking the time to exercise the bargaining power the huge national pharmacare market will give us, one of the key advantages of moving to a national drug insurance system would be lost. It would mean missing out on our best opportunity to get better prices and keep national pharmacare affordable.
A Patient’s Story-Alexandra Fox
"In 2009, part way through my undergrad, I went through my first depression.
I was able to access help and was prescribed an anti-depressant for a year. The drug was new and not covered by my insurance, but I was willing to do anything to get out of where I was mentally. Importantly, for me, I did not have an official diagnosis. You know, stigma, label and all.
In 2014, I went through a much worse depression. This time it came with extreme anxiety and mono! Bedridden for a year-and-a-half, I spent $900 per month on two daily medications and weekly therapy.
My partner at the time was a graduate student with amazing benefits. This spurred me to apply for an MA at the same university, as I would have access to the same union benefits. The only real downside was that I had to get an “official diagnosis” to access the programs which meant I now had a “pre-existing” condition.
In 2017, I moved closer to home to pursue a career in health care based on my own experience. For now, I have some extended health coverage as a graduate student in an occupational health program.
My real hope is that by the time I graduate we would have finally plugged the 50 year-old hole in Canadian health care and put the term “pre-existing condition” in a museum, where it belongs.”
Once the initial essential medicines list is in place, to ensure remaining patient needs are addressed as quickly as possible, and to ensure a fair approach to expanding the formulary, the Canadian drug agency would use the prioritization framework (described earlier) to determine the sequence for adding drugs to the formulary. Starting from the essential medicines list, the national formulary would be expanded step-by-step until the comprehensive formulary has been achieved. As noted, assessing a broad range of drugs for clinical and cost-effectiveness and negotiating good prices and coverage conditions with manufacturers will take time. Given that we have waited for national pharmacare for over 50 years, it makes sense to take a little longer to get it right. We believe the essential medicines list can be ready for January 1, 2022, and a comprehensive national formulary should be in place no later than January 1, 2027.
Once the comprehensive formulary is established, new drugs would be considered for it as they become available, according to the principles and priorities applied at the outset. The council also recommends that formulary drugs be periodically re-evaluated to ensure they remain the best choice for benefits to patients and value for money. A reassessment might find no reason to change a drug’s status on the formulary, but it might also lead to the conclusion that conditions for its use should be changed, its price should be renegotiated or that it should be removed from the formulary entirely because other, better choices are available.
Recommendations
- The council recommends federal, provincial and territorial governments launch national pharmacare by offering universal coverage for a list of essential medicines by January 1, 2022.
- The council recommends governments expand the initial formulary step-by-step toward a fully comprehensive formulary to be in place no later than January 1, 2027.
- The council recommends the Canadian drug agency create a framework to determine the order in which prescription drugs will be evaluated, negotiated and listed on the national formulary as it expands. The framework should prioritize products that are already covered by most public drug plans, respond to national population health priorities and reduce variability in access across the country.
5.6 National strategy on appropriate prescribing and use of drugs
Canada’s health care providers decide which drugs their patients should be taking and how much they need. The vast array of drug products on the Canadian market, however, can make it challenging for them to choose the best medicine every time, especially as their patients develop multiple chronic conditions. A recent report found that nearly 2 million Canadian seniors regularly take at least one medication that’s wrong for them, which can lead to falls, memory problems, hospitalizations and even death.Endnote 60 Physicians and patients also tend to be drawn to the newest drugs, even when they may offer little benefit over older, lower-cost alternatives.
During our consultations, we heard about initiatives to support better prescribing and use of drugs in Canada. Several provinces and territories, for example, send trained health professionals to meet with physicians to share evidence on the best drug choices for different conditions. The Canadian Agency for Drugs and Technologies in Health also has resources and tools to support better prescribing and use of drugs. Another example is Choosing Wisely Canada, a health education campaign that aims to reduce unnecessary tests and treatments in health care and to assist physicians and patients in making informed and effective choices to ensure high-quality care.
While these initiatives are a step in the right direction, their reach is often limited and not aligned across jurisdictions, which contributes to inconsistent prescribing across the country. Other countries have seen positive results from coordinated efforts to improve prescribing. Australia, for example, has a National Strategy for Quality Use of Medicines that has helped it improve health outcomes and save money.
Sweden’s Wise List
Building on the World Health Organization’s essential medicine concept, Sweden launched its Wise List in 2001, to promote rational use of drugs—including greater use of generic drugs. Focused chiefly on primary care for common diseases such as heart disease, the Wise List recommends first-, second- and third-line drugs and also provides Wise Advice—clinical practice guidelines in “areas where preventive measures and medicine treatment can be improved.” The Wise List includes 200 drugs to treat common diseases and another 100 for specialized care.
Research shows the Wise List has contributed to more consistent prescribing practices across Sweden and substantial cost savings for the Swedish health system through the increased use of generics.Endnote 61
The Canadian drug agency should develop a strategy on better prescribing and use of medication. This strategy would complement the development of the evidence-based national formulary and could include initiatives to support:
- Better prescribing by health care professionals through prescribing guidelines, assessment, feedback and tools; and
- More appropriate use of drugs by prescribers and patients through targeted education and public awareness campaigns.
This strategy would be developed and coordinated at the national level and could then be adapted to support the unique circumstances in different communities across Canada.
It will also be important to better regulate pharmaceutical industry funding of health care providers, institutions and patient groups, whether through cash or in-kind payments, gifts or funding of educational activities. These payments have been proven to influence prescriber and consumer behaviour. While the pharmaceutical industry remains critical to a thriving research step would be to follow the lead of the United States and Europe in requiring pharmaceutical companies to publicly disclose all such payments to health-related entities, health care practitioners and patients.
Recommendations
- The council recommends the Canadian drug agency create and implement a national strategy on appropriate prescribing to support prescribers and help patients better understand the pharmaceutical treatment choices available to them.
- The council recommends federal, provincial and territorial governments regulate pharmaceutical industry payments to health care providers, institutions and patient groups, beginning with mandatory public disclosure of all such payments.
5.7 National strategy for expensive drugs for rare diseases
People who suffer from rare diseases are often desperate for treatment that might help their condition, and the pharmaceutical industry is responding by developing a growing number of drugs—most of which are extremely expensive. Over the course of its mandate, the council repeatedly heard that these drugs threaten the continued operation of both private and public insurance plans—but at the same time, patients across the country are relying on them for life-changing, and life-saving, treatment. However, with prices of up to $2 million per patient per year, these drugs are entirely unaffordable for a patient or family to consider paying for out of pocket. No patient should face costs of this magnitude for any drug.
Because these drugs are developed for diseases that affect small numbers of people, it is difficult to conduct a standard clinical trial, where a drug is tested on a significant number of people (some of whom are given the drug, while others get placebos or other medications) until there is proof it works and is safe. As a result, the health benefits, long-term safety and cost-effectiveness of many rare disease drugs are uncertain when they’re put on the market. Also, given their high prices, few meet the standards for listing and coverage through a regular drug plan formulary. However, delays in getting these medications to patients can increase suffering and affect health outcomes as Canadians with rare conditions can have few treatment options and can decline rapidly without access to effective medication.
Budget 2019 announced federal funding of up to $500 million per year starting in 2022-23 to support a national strategy on high-cost drugs for rare diseases. The council recommends these funds be used to support more nationally consistent access to expensive drugs for rare diseases and to contribute to the knowledge base about these highly specialized drugs.
Currently, to have the cost of these drugs covered publicly, a patient’s prescriber will request special funding authorization from the provincial public drug plan. Each province reviews its own requests and this can lead to inconsistent funding decisions for people with rare diseases across the country, and delays in access for patients, who may find their chance of treatment is dictated by their postal code,
To address these challenges, the federal government should work with provincial and territorial governments to develop a distinct national process for providing fair, consistent, timely and evidence-based access to expensive drugs for rare diseases.
To provide the flexibility needed to ensure that innovative, life-changing drugs for rare diseases can be made available despite possible uncertainty about their clinical impact, the Canadian drug agency should create a distinct pathway for them. Rare disease drugs would continue to be carefully considered and evaluated, but the distinct pathway would be designed to support timely and appropriate patient access to these specialized drugs. The pathway will require strong collaboration between partners—manufacturers, governments, the Canadian drug agency, prescribers and patients—and a willingness to try a drug that shows promise and whose potential outweighs its risk. Such an approach requires careful and constant real-life follow up and innovative funding mechanisms. It is critically important the pathway and its associated strategies encourage innovation and act as a catalyst to those seeking to develop breakthrough medicines that may prove life-changing for this unique segment of Canada’s population.
A national expert panel (with strong patient representation) would play an important role in implementing the strategy. The panel would work with patients and their care teams, as well as with drug plan administrators, pharmacists and researchers, reviewing individual cases to determine whether a particular drug should be funded for a particular individual. The panel would also draw on specialized expertise to support their deliberations, such as consulting experts in Indigenous health or international rare disease specialists.
This process would involve identifying meaningful indicators for determining whether a drug is helping a patient. Once an initial decision has been made to fund a patient’s treatment, the panel would use ongoing input from the patient’s care team to assess whether treatment goals are being met and treatment and funding should continue.
The assessment indicators could serve as the basis for performance-based funding agreements for these expensive drugs. These are negotiated agreements between governments and drug manufacturers, where governments only pay if the drugs achieve defined goals. The council believes these agreements can be effective to ensure patients have early access to treatment and that real-world evidence is generated to address gaps, while sharing the financial risk involved between governments and drug developers.
The real-world evidence developed by monitoring the indicators would support evidence-based decisions for Canadian patients and allow Canada to contribute to the international knowledge base about these highly specialized drugs for rare diseases.
A Patient’s Story-Jordan Morgan
"Five years ago, a passing comment to my child’s doctor led to my sarcoma diagnosis. After a whirlwind of diagnostic testing, treatment, recurrence and more treatment, my oncologist suggested a new biologic to reduce the tumour enough for more surgery.
As neither private insurance nor public programs were covering it, I faced a dilemma: prepare for the worst or pay $130,000 to get more time with my young family.
But my community surprised me. A friend set up a humbling GoFundMe campaign. Then my luck changed. The drug company started a special access program. I no longer needed to worry about paying.
When I tried to return the money raised through the GoFundMe campaign everyone refused. They all said to put it aside—just in case. Then, just in case happened. After a year, my tumours started to grow again.
I’m thankful for each extra day with my family, friends and community. I get excellent health care—except for access to new medications—I am constantly in bureaucratic limbo and information blackholes. No timelines, all I do is wait.
Yet, the cancers don’t wait. They continue to grow and degrade my health little by little.
No-one battling disease should also have to battle the system. And they certainly shouldn’t have to worry about paying for life-saving medication."
On April 19, 2019, Jordan succumbed to his cancer, asking only that people honour his memory through small acts of kindness.
The distinct process and funding for these specialized drugs should be in place in conjunction with the coverage for the priority list of essential medicines, beginning January 1, 2022.
Recommendations
- The council recommends the federal government work with provincial and territorial governments and patients to immediately develop a national strategy for expensive drugs for rare diseases to support more consistent access to these drugs.
- As part of this strategy, the council recommends the Canadian drug agency establish a distinct pathway for the consideration of expensive drugs for rare diseases, and a national expert panel to work with patients and their clinicians to determine which rare disease drugs should be funded for which patients.
- The council recommends the Canadian drug agency work with clinicians and patients to gather structured real-world evidence on the impact of rare disease drugs on patients.
- The council recommends the Canadian drug agency negotiate performance-based funding agreements with manufacturers of rare disease drugs, where the amount paid to the manufacturer depends on how well the drug works.
- The council recommends the Canadian drug agency ensure decisions on expensive drugs for rare diseases are transparent and clearly communicated.
Chapter 6: Financing national pharmacare
Over the course of the council’s engagement with Canadians, the question of how to fund national pharmacare—how much it would cost, how much it would save and how we should pay for it—generated extensive discussion and debate. In this chapter, we provide the results of our analysis based on careful modelling of current and future drug costs, and set out our recommendations on how our plan should be funded.
6.1 Assessing the cost of national pharmacare
It is important for the country as a whole, as well as for governments, businesses and households to have a clear understanding of the financial implications of the council’s recommendations for national pharmacare.
We expect that the implementation of national pharmacare will affect system wide spending for prescription drugs in Canada in several important ways. For example, moving to a single-payer model with concentrated bargaining power will help reduce drug prices. Public administration of pharmacare will reduce administrative costs. Implementing generic substitution and increasing the use of biosimilars will save money on treatments. On the other hand, removing financial barriers to access—a key objective of national pharmacare—will likely increase system wide drug accessibility and therefore spending. How quickly these different effects will occur will have important implications for the evolution of drug costs under national pharmacare.
6.1.1 The council’s drug spending model
To help the council better understand national pharmacare's fiscal implications and its likely impact on spending for prescriptions, we had a drug spending model developed that builds on the methodologies of the Parliamentary Budget Officer (2017) and Dr. Steve Morgan et al. (2015). The model’s projection component simulates our recommended step-by-step implementation of pharmacare, allowing us to see over time how each element of pharmacare will affect both savings and expenditures. This, in turn, provides us with an estimate of the total cost of pharmacare from inception to full implementation.
To ensure the robustness of both the model and the assumptions used to run it, consultations were held with federal, provincial and territorial officials, as well as with experts, academics and stakeholders. Further details on the model can be found in Annex 6.
The drug spending model was used to simulate prescription drug spending for a wide variety of potential designs for national pharmacare, including simulating different eligibility criteria, lists of drugs and cost sharing provisions (such as copayments and deductibles). For each potential version of national pharmacare, the model estimates drug expenditures covered by:
- National pharmacare;
- Other public plans (spending under existing public plans that will not be covered by national pharmacare, but which is assumed will continue to be covered by those plans);
- Private insurance plans; and
- Out of pocket spending.
The model does not generate estimates of potential transition or administrative costs associated with national pharmacare, secondary savings (such as reducing spending on hospital and emergency room visits because more people will take their prescriptions correctly or other broader economic impacts.
The drug spending model is based on data from IQVIA Solutions Canada, which shows Canadians spent a total of approximately $30 billion on prescription drugs in 2017 (although, after subtracting the estimated confidential rebates manufacturers often give governments, the total was probably about $28 billion.) Of this total, public plans covered about $13.5 billion (likely about $11.5 billion after confidential rebates), private plans covered about $11.5 billion, and out of pocket spending was about $5 billion.Footnote ii
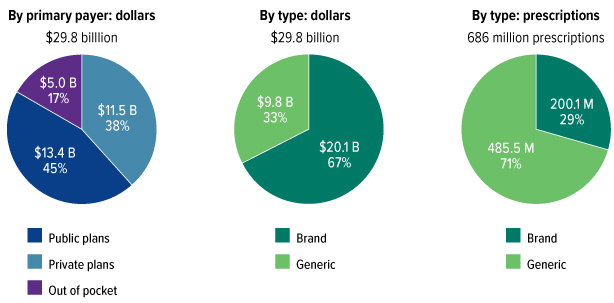
Source: IQVIA Solutions Canada. Note: Totals may not add due to rounding, and do not reflect confidential rebates.
*12-month period ending in May 2018.
Figure 11: Text description
| By primary payer (dollars) | Dollars (billion) |
|---|---|
| Private insurance | 11.5 |
| Public Plans | 13.4 |
| Out of pocket | 5 |
| Total | 29.8 |
| By type (dollars) | Dollars (billion) |
| Brand | 20.1 |
| Generic | 9.8 |
| Total | 29.8 |
| By type (prescriptions) | (million) |
| Brand | 200.1 |
| Generic | 485.5 |
| Total | 686 |
Source: IQVIA Solutions Canada
Note: Totals may not add due to rounding, and do not reflect confidential rebates.
*12 month period ending in May 2018.
It is important to note that up to about 30 per cent of private plan beneficiaries are public sector employees (and their dependents) working in entities such as federal, provincial, territorial and municipal governments, universities, school boards and hospitals.Endnote 62That means up to $3.5 billion of private spending on prescription drugs is, in fact, paid for by governments in the form of employee benefits. When the total spend on prescribed drugs is expressed by source of payment, approximately $17 billion is paid for by governments (likely about $15 billion after confidential rebates), $8 billion privately and $5 billion out of pocket.
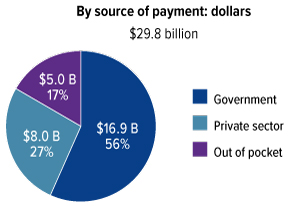
Source: Council’s calculations using data from IQVIA Solutions Canada. Note: Totals may not add due to rounding, and do not reflect confidential rebates.
*12 month period ending in May 2018.
Figure 12: Text description
| By source of payment (dollars) | Dollars (billions) |
|---|---|
| Government | 16.9 |
| Private | 8 |
| Out of pocket | 5 |
| Total | 30 |
Source: Council’s calculations using data from IQVIA Solutions Canada
Note: Totals may not add due to rounding, and do not reflect confidential rebates.
*12 month period ending in May 2018.
There are many assumptions embedded in the council’s drug spending model about a whole range of factors that impact on prescription drug costs. However, the council made sure that under any scenario, no one would be worse off in terms of the benefits they currently receive through public and private plans.
Also, while the model assumes that national pharmacare would result in lower negotiated prices for drugs, we did not factor in any changes in the pharmacy markups and dispensing fees. There exist significant differences in pharmacy fees across the country, which can make up as much as 30 per cent of the total cost of a drug in some places. This can be a complex issue, resulting from different trade-offs made during negotiations by provincial or territorial governments and pharmacists at different points in time. While the cost modelling done for the council did not factor in any changes to these fees under national pharmacare, our hope is that the Canadian drug agency will examine these differences in pharmacy fees and balance efficiencies with proper recognition of the vital services pharmacists provide Canadians.
6.1.2 How drug spending will evolve with national pharmacare
As shown in Figure 13, the drug spending model projects that in the absence of national pharmacare, overall prescription drug spending in Canada will rise from $28 billion in 2017 (net of confidential rebates) to about $52 billion per year by 2027, split between existing public plans ($23 billion), private plans ($20 billion) and out of pocket spending ($9 billion). This amounts to an average annual increase in spending of about 6.5 per cent each year from 2017 to 2027. Figure 13 also indicates an upper and lower bound for the projection to take into account uncertainty around how some of the assumptions would play out in real life.
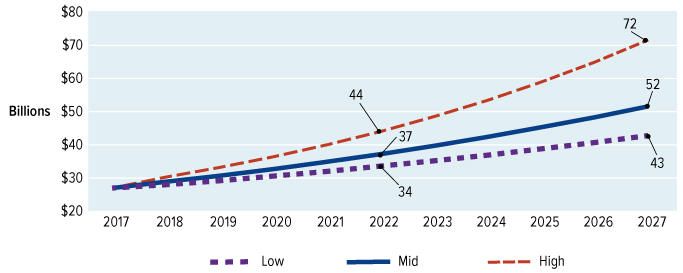
Source: Council’s calculations using data from IQVIA Solutions Canada, CIHI, PMPRB and Health Canada.
Figure 13: Text description
A line graph showing three projection scenarios (low, mid, high) for drug spending in Canada from 2017 to 2027.
- In the low scenario, spending is projected to reach $34B in 2022 and $43B in 2027.
- In the mid scenario, spending is projected to reach $37B in 2022 and $52B in 2027.
- In the high scenario, spending is projected to reach $44B in 2022 and $72B in 2027.
Source: Council’s calculations using data from IQVIA, CIHI, PMPRB and Health Canada.
As we said in Chapter 5, we propose that national pharmacare begin January 1, 2022, with a formulary initially covering a list of essential medicines (together with a distinct process and dedicated funding for expensive drugs for rare diseases) and then expand over the next five years to a comprehensive formulary available no later than January 1, 2027. Patients would pay $2 copayments for essential medicines and $5 for all other prescription drugs with an annual out of pocket cap of $100 per household. For modelling purposes, the essential medicines list was assumed to consist of the drugs on the CLEAN Meds list (developed for Canada by clinicians and researchers at St. Michael’s Hospital in Toronto) and the comprehensive formulary was simulated by expanding coverage over time to the drugs on the Régie de l’assurance maladie du Québec formulary, the largest public plan formulary in the country in terms of its share of system wide drug spending (and used by the Parliamentary Budget Officer in his modelling).
Based on these parameters, it’s estimated total public spending in 2022 to cover essential medicines under national pharmacare would increase by $4.1 billion. However, national pharmacare should also save money for governments through reduced claims for individual tax credits for medical expenses, from increased taxable compensation (to the extent employers reinvest savings from pharmacare into employee salary increases) and from reduced government spending on private drug coverage for public sector employees. Taking these “ancillary savings” into account, the net incremental public cost to cover essential medicines in 2022 would be about $3.5 billion.
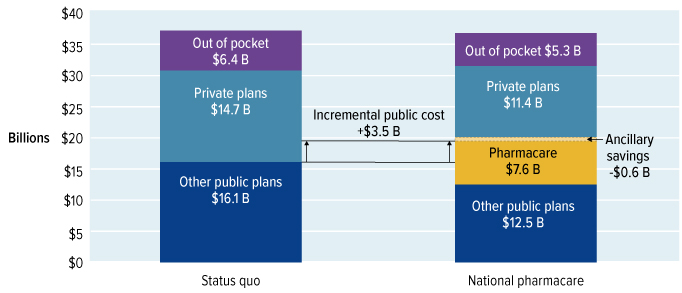
Figure 14: Text description
| Status Quo | National Pharmacare | |
|---|---|---|
| Out of pocket | 6.4 | 5.3 |
| Private plans | 14.7 | 11.4 |
| Other public plans | 16.1 | 12.5 |
| Pharmacare | 0 | 7.6 |
| Incremental public cost | 0 | 3.5 |
| Ancillary Savings | 0 | -0.6 |
Source: Council’s calculations using data from IQVIA, CIHI, PMPRB and Health Canada.
At the same time, spending by private plans would decrease by about $3.3 billion (to $11.4 billion) and out of pocket spending would decrease by about $1.1 billion (to $5.3 billion). The model assumes that because affordability will no longer be an issue for many people, 10 million more prescriptions will be filled. (The initial impact of pharmacare will be slightly dampened because the plan will at first be limited to the list of essential medicines and many of the cost-saving measures, such as negotiating lower drug prices, will take time to realize.)
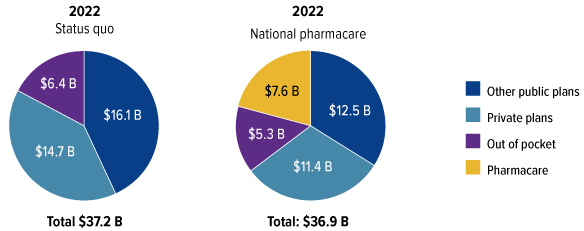
Source: Council’s calculations using data from IQVIA Solutions Canada, CIHI, PMPRB and Health Canada.
Figure 15: Text description
| 2022 Status Quo (billions) |
2022 National Pharmacare (billions) |
|
|---|---|---|
| Out of pocket | 6.4 | 5.3 |
| Private plans | 14.7 | 11.4 |
| Other public plans | 16.1 | 12.5 |
| Pharmacare | 0 | 7.6 |
| Total | 37.2 | 36.9 |
Source: Council’s calculations using data from IQVIA Solutions Canada, CIHI, PMPRB and Health Canada.
Over time, as the formulary is expanded, national pharmacare is expected to increasingly influence prescription drug spending. There will be greater system savings as lower prices are negotiated and extended to a broader list of drugs. By 2027, total spending on national pharmacare is projected to be about $38.5 billion (again, with confidential rebates and copayments deducted) and government spending would be about $15.3 billion higher than it otherwise would have been. This figure takes into account an estimated $2.8 billion in ancillary savings, as described above.
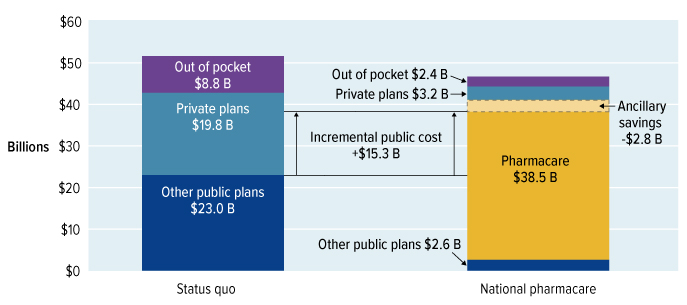
Source: Council’s calculations using data from IQVIA Solutions Canada, CIHI, PMPRB and Health Canada.
Figure 16: Text description
| Status Quo | National Pharmacare | |
|---|---|---|
| Out of pocket | 8.8 | 2.4 |
| Private plans | 19.8 | 3.2 |
| Other public plans | 23 | 2.6 |
| Pharmacare | 0 | 38.5 |
| Incremental Public Cost | 0 | +15.3 |
| Ancillary Savings | 0 | -2.8 |
Source: Council’s calculations using data from IQVIA, CIHI, PMPRB and Health Canada.
With the formulary accounting for an estimated 86 per cent of total drug spending, pharmacare is expected to significantly reduce private-sector spending on prescription drugs. Even assuming individuals and private plans continue to pay for drugs that are not on the national formulary, their spending would decrease significantly from projections based on maintaining the status quo—to about $3.2 billion for private plans, while out of pocket spending would decrease to about $2.4 billion.

Source: Council’s calculations using data from IQVIA Solutions Canada, CIHI, PMPRB and Health Canada.
Figure 17: Text description
| 2027 Status Quo (billions) |
2027 National Pharmacare (billions) |
|
|---|---|---|
| Out of pocket | 8.8 | 2.4 |
| Private plans | 19.8 | 3.2 |
| Other public plans | 23 | 2.6 |
| Pharmacare | 0 | 38.5 |
| Total | 51.6 | 46.8 |
Source: Council’s calculations using data from IQVIA, CIHI, PMPRB and Health Canada.
| 2022 | 2027 | |||
|---|---|---|---|---|
| Status quo | With pharmacare | Status quo | With pharmacare | |
| Total Rx spending | 37.2 | 36.9 | 51.6 | 46.8 |
| National pharmacare | 7.6 | 38.5 | ||
| Other public plans | 16.1 | 12.5 | 23.0 | 2.6 |
| Private plans | 14.7 | 11.4 | 19.8 | 3.2 |
| Out of pocket | 6.4 | 5.3 | 8.8 | 2.4 |
| Net incremental public spending (with ancillary savings) |
N/A | 3.5 | N/A | 15.3 |
Source: Council’s calculations using data from IQVIA, CIHI, PMPRB and Health Canada.
6.1.3 Savings in system wide spending under national pharmacare
As national pharmacare is implemented, significant efficiencies are expected to be realized through negotiation of lower drug prices, increased generic substitution and use of biosimilars, and other shifts in prescribing toward lower-cost therapies. In 2022, when national pharmacare would begin, these savings would likely be modest, at around $0.3 billion relative to the status quo. This reflects the fact that most of the drugs included in the essential medicines list are generics, and most of the efficiencies associated with national pharmacare have not yet been realized. By 2027, at which point national pharmacare would cover a comprehensive formulary of drugs, we project savings in system wide spending of almost $5 billion annually relative to the status quo. In other words, Canada would spend $5 billion less on prescription drugs in 2027 while at the same time improving access and providing universal public coverage for all Canadians.

Source: Council’s calculations using data from IQVIA Solutions Canada, CIHI, PMPRB and Health Canada.
Figure 18: Text description
A line graph showing estimated projections for drug spending in Canada from 2017 to 2027.
- 2027, under the status quo, total spending would reach $52B.
- By 2027, under national pharmacare, total spending would reach $47B.
- There would be $5B in system savings under national pharmacare.
6.1.4 How the council’s projection of pharmacare costs compares with other estimates
In 2017, at the request of the Standing Committee on Health, the Parliamentary Budget Officer (PBO) published cost estimates for national pharmacare. The PBO estimated that if national pharmacare had been fully implemented in 2015-16, it would have required incremental public spending of $7.3 billion ($6.3 billion net of copayment revenues and ancillary savings). Overall, this would amount to a 50-55 per cent increase in public spending on prescription drugs.
The council projects that the incremental public costs of national pharmacare, once fully implemented in 2027 (12 years later than the base year of the PBO), would be $15.3 billion net of copayment revenues and ancillary savings. Overall, this amounts to an increase in public plan spending of about 65 per cent.
It is difficult, however, to directly compare the results of the council’s drug spending model with those of the PBO. While the council’s model builds on the methodology used by the PBO, it is not identical and uses assumptions about the key drivers of prescription drug spending to project future drug costs. As a result, it includes the impacts of factors such as inflation, population growth and aging, and the arrival of new, more expensive drugs. Finally, the council’s estimates reflect the assumption that provincial public plans would continue to cover drugs they are currently covering but that will not be covered by national pharmacare.
It is worth noting that both estimates arrive at similar conclusions in respect of the potential for overall system savings under national pharmacare. The council’s estimates suggest that overall spending on prescription drugs could be reduced by $5 billion (approximately 10 per cent) in 2027. The PBO’s estimates suggest a $4 billion reduction in overall system spending (approximately 15 per cent).
6.2 Financing national pharmacare
The council is confident our approach to national pharmacare is the most sustainable way to provide Canadians with comprehensive and universal coverage for the prescription medicines they need to ease pain, manage chronic disease, and improve and maintain their health. Having recommended, described and costed this model, the next question is how it should be financed.
Key to this question is the fact that implementation of national pharmacare will require a strong and respectful partnership between federal, provincial and territorial governments, as well as with Canada’s Indigenous peoples. This partnership will need to acknowledge and build on the actions already taken by jurisdictions to provide drug coverage, and drive progress towards a common experience for all Canadians who need prescription drugs.
6.2.1 Federal-provincial-territorial fiscal arrangements
One of the first tasks will be to negotiate intergovernmental financing arrangements for national pharmacare. This won’t be the first time that Canada has created a new social program, so there’s a lot of experience to build on. During the 1950s, 60s and 70s, the federal government cost-shared hospital and physician services with provinces and territories. The federal government paid for half of every dollar provinces and territories spent on eligible expenditures in these two areas. In the late 1970s, once these programs became more established, governments agreed to change this arrangement from cost-sharing to a new general transfer for hospital care, physician services and post-secondary education, based on population size.
In the 1980s and 1990s, when government finances became tighter, the federal government made a series of changes to the structure and amount of the transfer in an attempt to control rising costs. These changes were controversial because they did not flow from negotiations and agreement between the federal and provincial and territorial governments.
In the early 2000s, the federal government reinvested in health care through a series of agreements negotiated with the provinces, culminating in the 2004 Health Accord, which established a dedicated health transfer with legislated increases. Beginning in 2017, new bilateral agreements, which included targeted investments in home care and mental health, were signed between the federal government and provinces and territories.
During the council’s consultations, provincial and territorial officials were clear that financing arrangements for national pharmacare would need to be different than what is now in place for medicare. In particular, provinces and territories signalled the need to ensure the federal government provides long-term, adequate, secure and flexible funding to support the objectives of the program, and that the federal government couldn’t make changes to the arrangement without the agreement of provinces and territories.
To ensure success, we think financial arrangements for national pharmacare should draw from the best practices and lessons from the past. First, federal contributions should reflect the full incremental cost of moving from where we are today to where we need to be at different stages of implementation. Our plan assumes provincial and territorial governments will continue to spend the same amount on drug coverage, but recognizes that expanding coverage to all residents and to a national standard will significantly increase their costs. The federal government must be prepared to make the necessary contributions to cover any added costs the provinces and territories incur, while acknowledging actions already taken.
Second, federal funding to provincial and territorial governments must be fair and responsive to their different needs. Spending on drugs will vary by province and territory depending on a number of factors: population size, social determinants of health, demographics (for example, seniors tend to take more prescription drugs than the rest of the population), geography (which may affect mark-ups, transport costs and dispensing fees) and other factors. While financing arrangements may not be able to perfectly adjust for all these factors, it is important to treat all jurisdictions fairly. Provinces and territories that have already made substantial investments in prescription drug coverage should not be penalized for their contributions.
Third, the arrangement must be governed by an ethos of shared decision-making. One party should not be able to make unilateral changes to the arrangement. This will be important at the outset when the arrangement is negotiated, as well as over time as adjustments and course corrections need to be made. Governments could draw inspiration from the shared governance arrangements surrounding the Canada Pension Plan (CPP). Major changes to the legislation governing the CPP require the formal consent of the Parliament of Canada and seven out of 10 provinces, representing two-thirds of the population of the 10 provinces. As the territories will also be active partners in pharmacare, the council suggests a variation on this approach, in which no changes could be made to the financing arrangements without the consent of the Parliament of Canada and at least 70 per cent of participating jurisdictions, representing two-thirds of their combined population.
Finally, the terms and conditions attached to federal funding of pharmacare should be consistent with its broad goals. For a province or territory to opt in and become eligible for federal funding, it must accept the principles for national pharmacare (that it be universal, comprehensive, accessible, portable and publicly funded and administered) and the terms of coverage outlined in Chapter 4.
6.2.2 Revenue generation
Another important issue to be addressed is how to raise the revenue needed to support national pharmacare. As noted above, the council’s costing model projects that the initial list of essential medicines will cost an additional $3.5 billion annually, starting in 2022. This will grow as drugs are added to the national formulary, reaching $15.3 billion by 2027. This would be a major new line item for the federal budget, and needs to be factored into the government’s fiscal planning.
While the costs above are undeniably significant, they must be weighed against the equally significant savings to Canadians. By 2027:
- National pharmacare will reduce annual system wide spending on prescription drugs by $5 billion;
- Businesses and employees will see their prescription drug costs reduced by $16.6 billion annually;
- Families will see their out of pocket drug costs reduced by $6.4 billion;
- The average business will save $750 per employee per year; and
- The average family will save $350 per year.
The council heard many views about financing pharmacare during its consultations. Some participants said if national pharmacare were to eliminate the need for private drug insurance funded by employers and employees, the government should seek to capture and redirect all or part of that stream of funding. Others questioned why employers and employees should be singled out and made to shoulder a large part of the cost for something as essential as health care. Some talked about generating the additional revenue by increasing specific taxes, such as the GST, while others pointed out that type of tax increase would be felt disproportionately by working class and lower-income Canadians who already feel the pinch of grocery bills and gas prices. Some suggested creating a new tax or premium that everyone would pay, something that makes it easy for everyone to know where their tax dollars are going; others felt this might face too much opposition. A large majority of participants suggested the federal government should use general taxation to pay for pharmacare in much the same manner medicare is funded.
We believe the fairest way to fund pharmacare would be consistent with other aspects of health care—through general government revenue. In a sense, this is a combination of various different revenue streams, all of which have their respective pros and cons. It doesn’t single anyone out, or create a new tax. It’s the same system that provides us with many of the benefits of living in this country. Canada’s tax system is designed to ensure each Canadian contributes according to their means, which is why this approach is used to finance medicare.
As the focus of our work was to make recommendations on the design and implementation of national pharmacare, we did not feel it was our place to go more deeply into the issue of how to raise the revenue needed to fund the federal contribution to the program. We consulted widely and can report with certainty there is no easy answer to how to pay for national pharmacare. At the same time, it is clear to us we can no longer afford not to implement pharmacare, which is clearly the surest way to get better value for money out of the significant amounts we spend on prescription medicines. Like medicare, the council believes pharmacare must find its place among the things we agree as a country are worthwhile investments—for Canadians and for our shared prosperity. Ultimately, the precise details of funding national pharmacare must be decided by elected governments, who must weigh current and future funding pressures and decide among trade-offs across the breadth of government activity to meet the needs of all Canadians.
Recommendations
- The council recommends the federal government provide long-term, adequate and predictable funding to provinces and territories sufficient to cover the incremental costs of national pharmacare.
- The council recommends federal funding for national pharmacare be allocated to provinces and territories in a fair and transparent way, and be responsive to differing levels of need across jurisdictions.
- The council recommends federal funding for national pharmacare be delivered through a new targeted transfer that is separate and distinct from the Canada Health Transfer.
- The council recommends provinces and territories be eligible for federal funding when they accept the principles and the national standards (terms of coverage) for national pharmacare.
- The council recommends intergovernmental financing arrangements for national pharmacare be determined through mutual agreement among federal, provincial and territorial governments.
- The council recommends intergovernmental financing arrangements for national pharmacare be reviewed every five to ten years.
- The council recommends changes to intergovernmental financing arrangements for national pharmacare require the consent of the Parliament of Canada and at least 70 per cent of participating provinces and territories representing two-thirds of their combined population.
- The council recommends the federal contribution to national pharmacare be financed through general revenue in a manner similar to the way medicare is funded.
Chapter 7: Ensuring the success of national pharmacare
In the previous two chapters, we outlined the council’s vision for what national pharmacare should look like and how it should be financed. In this chapter, we discuss critical enablers that governments must consider to ensure the successful implementation of national pharmacare.
7.1 Legislation
The council believes legislation would reassure provinces and territories that the federal government has an enduring commitment to national pharmacare, which the premiers told us was vital.Endnotenote 63 Federal legislation would formalize the negotiated standards to which the federal government, provinces and territories would be held, as well as the governance and financing arrangements agreed to by all. It would also spell out the steps required for provinces and territories to join national pharmacare. The federal government should aim to have this legislation in place by the time the essential medicines list is implemented on January 1, 2022.
The 2018 report by the House of Commons Standing Committee on Health recommended legislative amendments to the Canada Health Act to make prescription drugs dispensed outside of hospitals an insured service.Endnote 64 However, the council believes new legislation is both required and preferable for national pharmacare. Inserting pharmacare into the Canada Health Act could limit it, because the Act does not permit user charges such as the copayments we recommend. At the same time, amending the Canada Health Act to allow those copayments could undermine the Act’s commitment to first-dollar coverage for hospital and medical care. Therefore, we prefer stand-alone legislation, which would draw its inspiration from the values and principles of the Canada Health Act, but tailor them to the requirements of a modern national pharmacare plan.
Creating a new piece of legislation would also support a distinct approach to funding. The Canada Health Act is linked to the Canada Health Transfer, which provides equal per capita funding to provinces and territories for health care. However, national pharmacare is a new program that will likely require a different funding approach than the health transfer. Separate financing for pharmacare would also allow governments to better track drug spending and to assess its success.
We are also concerned that amending the Canada Health Act (which has not seen any substantive amendments since its passage in 1984) might lead to pressure to make other changes. Those issues may be worthy of debate, but would delay implementation of pharmacare.
Recommendations
- The council recommends the federal government enshrine the principles and national standards of pharmacare in federal legislation, separate and distinct from the Canada Health Act, to demonstrate its ongoing commitment to partnership on national pharmacare and provide for a dedicated funding arrangement.
- The council recommends the federal legislation outline how governments will work together and share costs, list federal responsibilities, and include the steps required for provincial and territorial governments to opt in to national pharmacare.
Timeline for Pharmacare Implementation
7.2.1 Provinces and territories
The financing arrangements for national pharmacare will be determined through multilateral negotiations among all the parties. However, for national pharmacare to be successful, the federal government will need to ensure provinces and territories are equipped to make the transition to the new program. That support should be negotiated bilaterally between the federal government and each province or territory to deal with each jurisdiction’s unique needs.
The council recommends that provinces and territories be eligible for time-limited transition funding for information technology upgrades and other resources to support the change. Each jurisdiction would develop its own transition plan, outlining a timeline for opting in and aligning their coverage with the national pharmacare standards.
As noted, national pharmacare will be implemented over time, beginning with universal coverage for a smaller list of commonly used essential medicines and expanding to provide coverage for a comprehensive formulary by January 1, 2027. This will give federal, provincial and territorial governments the time they need to work with their partners and stakeholders to smooth the transition to pharmacare. Many Canadians told the council they are relatively satisfied with their private drug insurance coverage, and understandably don’t want to be made worse off under any new pharmacare program. Therefore, it’s critical pharmacare be introduced in a predictable, measured way, coordinated with private insurers to ensure Canadians don’t lose any of their coverage as a result of national pharmacare.
Recommendation
- The council recommends the federal government support provincial and territorial governments to build program capacity to deliver national pharmacare.
7.2.2 Private insurance
When public insurance for hospital and physician services was introduced in the 1950s and 1960s, private insurers (who had offered coverage for those services) adjusted to the new reality and shifted their focus to coverage for services not covered by medicare, such as drugs. The council believes that by working with governments, Canada’s private insurers can successfully adapt their business model over the years it takes pharmacare to roll out, and ensure a seamless transition to the new system.
We heard from employers eager to expand employee health benefits to other areas (such as wellness and more generous vision, dental and paramedical coverage) and that governments should be open to allowing insurers to provide coverage for copayments, as well as prescription drugs not on the national formulary. Our plan supports the private sector taking on these opportunities, and rather than a drastic switch to a fully public plan, we recommend stepwise implementation of a system that still allows private plans to supplement public drug coverage, as many countries do. The almost eight-year transition to full pharmacare allows lots of time for the private sector, working with governments, to adapt their business models to the new reality.
Recommendations
- The council recommends federal, provincial and territorial governments engage with private insurers, as well as the employers and employees who benefit from their services, to ensure a smooth transition to national pharmacare.
- The council recommends private insurers be allowed to provide coverage for copayments, as well as for drugs not on the national formulary.
7.2.3 Pharmacists and the pharmaceutical industry
Other health care providers, including clinicians and pharmacists, will need to adjust their practices and systems and will have to be involved in planning the change from the beginning. Our cost estimates do not assume any significant changes to current dispensing fees or pharmacy mark-up structures, because the intent is to give governments and pharmacists time to identify what appropriate compensation should be under national pharmacare. Pharmacists have extensive frontline experience with Canada’s complex system of thousands of different drug plans, and will be invaluable in finding practical ways to transition to a simpler system.
Governments will also need to engage with manufacturers, distributors and others in the pharmaceutical supply chain to ensure smooth transitions to the new model. The Canadian drug agency will play a vital role in coordinating the supply chain with related stakeholders, such as Health Canada, to ensure timely and consistent supply of medicines on the national formulary.
7.2.4 Patient and public partnerships
Creating a true partnership between patients and the health care system is increasingly viewed as a critical success factor to achieve the triple aim of health systems: better care and better health outcomes at an affordable cost. This needs to happen at all levels, from the policy decision-making table through to the front lines of health care delivery.
The council has observed that the relationship between patients and policy decision-makers has been particularly challenging in the pharmaceutical sector. All too often, patients and patient groups feel they are on the outside looking in. When they don’t find the support they need from governments and the health care system, patients are left to fend for themselves, often finding support from charities or from the pharmaceutical industry, and sometimes serving as unsuspecting players in marketing strategies to advance commercial interests. This is profoundly unfair and unsupportable in a country that takes prides in the concept of universal public health care.
The council has gone to great lengths to engage patients and to listen to the diversity of patient voices and perspectives. We have also ensured that our recommendations about the governance and implementation of pharmacare help to strengthen partnerships between health care systems and patients. This will be critical to the successful implementation of our plan.
7.3 Information technology and drug data
Creating and operating a system of national pharmacare to serve 37 million Canadians, in multiple jurisdictions with tens of thousands of prescribers and pharmacies, can only be accomplished with first-rate information technology (IT). During our consultations, the council learned the transition to national pharmacare will require considerable investment in IT.
7.3.1 Upgrading drug plan IT systems
Each federal, provincial and territorial public drug plan uses a different IT system with its own infrastructure and standards for data to manage information about plan members and drug claims. It’s the same story with private plans. Many of these systems are aging and cannot connect with one another, making sharing data within provinces and territories challenging and worse than that across the country. Several of the provinces and territories told the council their systems are good enough for their needs now but it’s unlikely they could be expanded to handle pharmacare for all their residents.
Over the last few years, Canada Health Infoway (a non-profit organization funded by the federal government, which helps develop digital solutions to health care problems) has been working with a number of provinces and territories to implement a national electronic prescribing service which can transmit prescriptions electronically to pharmacies. This can reduce the number of lost prescriptions, medication-related errors and abuse of prescribed medications. But it will also be a useful source of data on quality, safety and effectiveness of prescribing practices.
Clearly, more work must be done to strengthen and modernize federal, provincial and territorial IT systems to manage the huge shifts in data flow a national pharmacare system will create. Each province and territory, however, will be starting toward that goal from a very different point. Larger provinces generally have more robust technology; some smaller jurisdictions still rely on paper-based systems to process drug claims. The council recommends the federal government provide adequate financial support for provinces and territories to modernize their drug insurance IT systems including automating paper-based systems and adding capacity for a significant expansion of claims and beneficiaries.
Recommendation
- The council recommends the federal government invest in information technology systems to ensure provincial and territorial governments have sufficient capacity to deliver national pharmacare.
7.3.2 Investing in drug data
The council is keenly aware that data on prescription drugs in Canada is fragmented and incomplete. We at times found it tremendously difficult to get information we needed on how Canadians use prescription drugs, to learn about the impact of prescription drugs on the health of Canadians, or to find out who spends what on prescription medicine.
Data about the use of drugs in Canada—from information on prescribing, dispensing and processing of drug claims, to whether a patient’s health improved or she or he had bad side effects—is not systematically gathered and reported. The launch of national pharmacare is a once-in-a-generation opportunity to develop complete records of drug data for all patients. These records would provide patients and their care teams in different settings—even if they become ill on the other side of the country—with essential information for safe and effective prescribing. At the same time, a central repository of essential data would (while following strict privacy standards) be invaluable for measuring drug effectiveness and monitoring benefits, side effects and costs. To evaluate drug efficacy, safety and toxicity across diverse populations in order to make better policy decisions, it will be important to ensure drug data can be linked to data on factors such as age, sex, gender and race.
Drug data has many important and beneficial uses as described above. It will be important to ensure privacy concerns remain paramount and that the patient has ownership and control over their personal health information. It may well be that blockchain technology can offer a powerful and secure solution to do this. IT providers, database managers, researchers and policy makers have an opportunity to establish powerful consent and control parameters that would allow for sharing of prescription drug data, while respecting the rights of patients.
In Canada and around the world, there are gaps in what we know about the safety and effectiveness of drugs as they are used in the real world (as opposed to what was found during clinical trials). The Canadian Institutes of Health Research collects evidence about how drugs affect patients, but national pharmacare could greatly enhance our ability to use data to learn about the impact of drugs on Canadians’ health.
Recommendation
- The council recommends the federal government invest in data collection, including from a gender and equity perspective, to address gaps in data and support ongoing management of national pharmacare. This should include data systems, possibly using blockchain technology, that allow secure sharing of data with the consent and control of patients.
7.4 Supporting federal measures
The federal government has not waited for the introduction of national pharmacare to try to improve the supply and management of prescription drugs in this country. In particular, there are two initiatives underway—streamlining drug approvals and modernizing regulations on the pricing of prescription drugs—which must be completed for national pharmacare to be successful. Equally important is continued federal support for innovation and research in health care, including for prescribed medicines.
7.4.1 Streamlining drug reviews
Before any drug can be sold in this country it must be approved by Health Canada, which reviews scientific evidence provided by manufacturers to determine if a new medicine’s benefits outweigh its risks. This review can take about a year, and new treatments are increasingly becoming more difficult to assess than drugs in the past. That’s brought pressure from patients and health care providers alike, who want faster access to the latest treatments.
Health Canada has responded by looking for ways to speed up reviews and approvals, including by using reviews and decisions by trusted regulators in other countries to speed up Canada’s process, and by sending more drugs for priority review, to get products (including drugs for rare diseases) on the market faster.Endnote 65 Health Canada is also building better links to other parts of the health care system to align the work. For instance, Health Canada and CADTH can now conduct their respective reviews almost simultaneously. This type of streamlining and collaboration will continue to be important as national pharmacare is put into place, so that Canadians can have timely access to pharmaceutical innovations.
Recommendation
- The council recommends the federal government accelerate efforts to streamline and modernize its assessment of drug safety, quality and efficacy to ensure patients will have faster access to innovative medicines.
7.4.2 Regulating patented drug prices
The federal government has proposed changes to the Patented Medicines Regulations that will enable the Patented Medicine Prices Review Board (PMPRB) to better manage drug prices. These changes will enable the PMPRB to:
- Benchmark prices against countries that are like Canada economically and have similar consumer price protections;
- See what prices public and private insurers in Canada are actually paying (after rebates), not just the prices pharmaceutical companies publish; and
- Consider whether the price of a new drug reflects its value to patients and the size of its potential market.
While the consolidated bargaining power that Canada will achieve under national pharmacare is expected to help us negotiate lower drug prices, in cases where a new drug is the only treatment available for a particular condition (as is the case for the majority of rare disease drugs), even a single payer’s negotiating power is limited. In these situations, the PMPRB will be able to assess whether the price of a new medication is in line with the health benefits it offers patients, as well as its overall affordability, and set a maximum price that reflects these considerations. The council recommends the federal government implement these reforms to make pharmacare more sustainable.
Recommendation
- The council recommends the federal government advance efforts to strengthen the Patented Medicine Regulations to lower the prices of patented drugs for all payers.
Maintaining choice under national pharmacare
As we met with Canadians, the council heard concerns that measures to contain costs under national pharmacare might discourage drug companies from bringing new drugs to Canada. However, countries such as Sweden, Norway and the United Kingdom all pay lower drug prices than Canada, yet more new drugs are launched in those countries each year than here.
While Canadians represent only 0.5 per cent of the world’s population, we account for 2 per cent of global drug sales.Endnote 66 Even with reduced drug prices, Canada will remain an important market for drug manufacturers, especially given that overall consumption of drugs in this country is expected to rise under national pharmacare, when people who were previously unable to afford their prescriptions can get the drugs they need.
7.4.3 Supporting innovation and research
Much progress has been achieved in developing medicines to cure otherwise fatal or debilitating illness and disease. This would not have been possible without a strong commitment to research and innovation. Canada has made significant contributions to the discovery of drug therapies, including the discovery of insulin, vaccines, anticoagulants, genes linked to early onset Alzheimer’s, and stem-cell therapies to treat cancer. Public investment in basic science and clinical research has played an important role in these discoveries, supported by a growing number of world-class teaching hospitals and research institutes. Private investment in drug-related research and development also plays a vital role in maintaining a vibrant drug innovation ecosystem.
Looking to the future, innovation in drugs and related therapies is poised to deliver even greater benefits for patients. New biologics currently in the drug pipeline show promise to improve treatment options for a range of illnesses and diseases including cancers, diabetes and multiple sclerosis. Through precision medicine and genomics, clinicians will be able to target drugs to the unique genetic characteristics of individuals and significantly improve health outcomes. Research is also expanding treatment options for cancer through CAR T-cell therapy, a form of immunotherapy that uses specially altered T-cells in the body’s immune system to treat cancer. National pharmacare will provide a robust platform to assess and adopt these new innovations in a coordinated and responsible way for the benefit of all Canadians.
The federal government plays a critical role in creating the conditions that support research and innovation in the health sector. Ongoing investments in health research, research infrastructure and post-secondary education help attract talent to this sector and grow research capacity. New partnerships between the public and private sectors, such as those that are emerging from the government’s innovation strategy, can further strengthen capacity in the life sciences sector. New trade deals and efforts to streamline regulation will also help to create a climate that supports investment in drug-related research and innovation. The council supports these measures and urges the government to continue investing in these areas.
Recommendation
- The council recommends the federal government continue to work with universities, research hospitals and industry to sustain and grow our world-class health innovation ecosystem and ensure Canada continues to contribute to the development of innovative drug and related therapies.
Chapter 8: What national pharmacare will mean for Canada
The implementation of national pharmacare in Canada is long overdue. Indeed, the same arguments spoken in favour of pharmacare in the 1960s still apply today. But a lot has also changed since then, making pharmacare even more relevant and more necessary: prescription medicines have a much greater role in improving health, and their cost has skyrocketed, putting the whole system at risk of becoming unaffordable. Pharmacare today is not only good health policy; it is good economic policy: this is a national project whose time has come.
For the first time in more than 50 years, Canada would be introducing a new pillar to its universal health care system. This is nation building, strengthening the social contract that bonds us, and reinforcing our sense of what it means to be Canadian. And although it will be a challenging transformation—all great national projects are—it will give Canadians and future generations a public prescription drug plan that is effective, fair and sustainable; one that shares the cherished Canadian values that are embedded in universal health care.
8.1 For patients and their families
The benefits of pharmacare for Canadians would be substantial and immediate. The innumerable differences across thousands of prescription drug plans will be a thing of the past. When Canadians go to the pharmacy with their prescription and their health card, they will pay no more than $2 or $5, depending on the drug. A straightforward antibiotic will cost $2. For a drug that is tens of thousands of dollars, the copayment will be $5. That’s it. No more complicated forms. No more steep deductibles. No more stress. Simple. Efficient. Equal.
The maximum households will pay for prescription drugs in a year is $100. And since the average Canadian household spends about $450 on prescription medicines now, that means Canadian families will save, on average, $350 per year. And with those savings will come the comfort of knowing you and your loved ones will have access to the medicine you need.
Families and individuals will no longer face the postal code lottery, where your access to prescribed drugs depends on which province or territory you reside in. And Canadians can rest assured knowing that their drug insurance travels with them, right across Canada.
Perhaps most importantly, Canadians will have access to the medicines prescribed to them based on need, not on their ability to pay. And cost-related non-adherence, where patients can’t afford the drugs they need to stay or get well, will become a thing of the past. All Canadians will be treated equally, without exception. That is something to be proud of. And it is consistent with the values conveyed by our universal health care system; our values as Canadians.
A Patient’s Story—Darren Porter
"I’m a sustainable independent fisherman. I work hard to provide for my family, doing my part to feed the population and fighting to save an unparalleled fragile natural ecosystem.
Taking care of myself? Not such a priority.
I’m happy that my kids are taken care of by my ex-wife’s coverage through work. But as an independent businessman in a tough resource-based industry, there simply aren’t any group insurance options available that I know of.
Sure, I could try to get a private individual plan from one of the insurance companies, but I’m constantly re-investing everything back into my business just to survive. From what I can tell, insurance for someone my age and in my industry is financially out of reach. That’s not even taking into consideration my health. And the public program available from the province is a joke, my income—limited as it is and fraught with uncertainty—is too much to be eligible.
I guess for me it comes down to what I don’t know, won’t hurt me. I’m a pragmatist—though some may call me foolhardy. But what’s the point of going to see the doctor when there’s not enough left for whatever I may be prescribed."
8.2 For employees and businesses
National pharmacare will mean that employees and businesses no longer have to pay for expensive prescription drug coverage. The average business owner who provides drug coverage would save over $750 annually per employee. The average worker with workplace drug coverage would save over $100 per year in plan premiums. In addition, employees who pay hundreds of dollars per year in copayments and deductibles for themselves and their families would never pay more than $100 per household.
Employers may choose to maintain some level of drug coverage—as has been the case in other countries with pharmacare, employee plans will likely cover the modest copayments ($2 or $5 per prescription) of pharmacare, as well as drugs that are not listed on the national formulary. And with a large portion of drug insurance costs off the table, employers could choose to enhance other health benefits that are increasingly in demand, including mental health services, physiotherapy, dental and vision care. This would help address important health needs in the working population and relieve some of the burden on public health care systems.

Figure 19: Text description
A series of three graphics that illustrate the savings that would be achieved from national pharmacare.
- The first graphic shows household savings, at $350 per year.
- The second graphic shows business/employers' savings at $750 per year (per employee).
- The final graphic shows employees' savings of $100 per year.
National pharmacare should also make it easier for employees to change jobs or move from one employer to another because they will no longer be at risk of “job lock”—unable to change jobs because the drug they need to treat their condition is not insured under the drug plans of other potential employers, or because a potential new employer has no health benefits at all. Employees will also no longer face the risk of losing their job if they or a member of their family have a condition that can only be treated with a high-cost drug that might bankrupt their company’s drug plan. And pharmacare means workers who choose to retire will not, unlike today, experience a reduction in drug benefits. Part-time and contract workers will, many for the first time, be entitled to prescription drug benefits.
National pharmacare will provide businesses with much-needed relief from the high and growing cost of prescription drug insurance. Business owners will no longer have to worry about whether they can afford private drug coverage for their hardworking employees. They will have the financial room to offer other health benefits to their workers, to pass on the savings to their employees through higher wages, or to invest in their businesses.
Furthermore, national pharmacare will create a more predictable environment for business by shifting the risk of having to pay for high-cost drugs from private to public plans. In our discussions with business owners, many were clear addressing high-cost drugs was a key concern for their companies.
National pharmacare will also level the playing field for small, medium and large businesses by ensuring all workers have comprehensive drug benefits, not just those who work for companies that provide drug insurance as a benefit of employment. For small businesses, many of which cannot afford drug benefits for their employees, pharmacare should make it easier to recruit and retain employees, and maintain a healthy workforce.
8.3 For the health care system and health care providers
National pharmacare means prescribers can finally have confidence their patients will fill their prescriptions. Doctors and other prescribers no longer have to ask a patient whether she or he has private insurance, and then modify their prescription accordingly. Pharmacists, who are all too familiar with patients leaving pharmacies without their needed medicine once they see the bill, will know their clients are being well-served by our health care system. And as more and more prescription drugs are delivered outside hospital, the inequity of drugs being covered by public insurance in hospital but not out will end. Patients will get the medication they need to get better, to stay healthy or to manage a chronic condition.
Removing the cost barriers Canadians face when they have prescriptions to fill will make it easier for them to maintain their health, reducing the need for them to visit their doctors or be admitted to hospital. As previously noted, recent research found that removing out of pocket costs for the medications used to treat just three health problems—diabetes, cardiovascular disease and chronic respiratory conditions—would result in up to 220,000 fewer emergency room visits and 90,000 fewer hospital stays annually. This has the potential to save the health care system up to $1.2 billion a year—just for those three diseases.
8.4 For citizens and taxpayers
National pharmacare is not only good for Canadians, it’s good economic policy. It will reduce the inefficiencies of the tens of thousands of private plans, which cost three times more to run than public plans. It will replace multiple buyers with a single purchaser, one that has the clout and authority to negotiate the best, lowest prices for prescription medications. The annual savings that will come from strong negotiating power and other efficiencies of pharmacare will save an estimated $5 billion per year by 2027. At the same time, decisions on which drugs to fund will be made by an arms-length agency, based on scientific evidence and value for money—protected from political influence.
In this report, we have described the vision and the promise of national pharmacare, which is more necessary today than ever. We, all of us—Canada—can achieve it together.
Chapter 9: Conclusion
Our proposal for national pharmacare is transformational and life-changing. It will replace a patchwork of thousands of plans that are nearing their financial breaking point (and yet leaving millions of Canadians unable to get the medicine they need) with one that is sustainable, fair and equitable, where all Canadians have access to prescription medicines based on need, and not their ability to pay.
Let’s just take a moment to reflect again on what that phrase “based on need, not ability to pay,” really means: this is our chance to build a healthier society and correct a historic mistake, the decision to leave pharmacare out of medicare.
A half-century ago, not insuring medication seemed a manageable compromise; governments of the day were finally providing Canadians universal access to medical and hospital care. Paying for medicine was not a problem on the same scale, and could be tackled later.
But, because no one foresaw the medical breakthroughs that would lead to today’s enormously expensive drugs, and no one predicted work would evolve in ways that kept private insurance out of reach for millions of people, that compromise has brought inequality and unfairness. Our research turned up different estimates of how many Canadians are uninsured or underinsured: some studies put the number of uninsured at 5 per cent of Canadians—that’s almost 2 million people. Other surveys tell us closer to 20 per cent of Canadians (representing 7.5 million people) are either uninsured or underinsured, and don’t have the drug coverage they need.
It can be too easy to tolerate those abstract numbers. We tell ourselves that if 5 per cent don’t have coverage, that’s not so bad, 95 per cent do. And there may be 7.5 million people without coverage for some or all of their drugs, but we convince ourselves most of them can probably manage. The fact is, those numbers represent untold stress and suffering. We heard from thousands of Canadians over our year of work, and they’ve shared some powerful, and heartbreaking, stories in this report.
There was Grace and her son Aleiandro, whose rare disease has brought their family face to face with “medical poverty.” Aleiandro takes 25 medications a day, just one of which is costing the family $3,000 a month. There was Jordan, who had to find $130,000 for a cancer drug to have any hope of more time with a young family. And there was the person with leukemia, too frightened to give a name, whose spouse was fired after his company’s insurance premiums went up because the medication was so expensive.
One of the most contentious points in the U.S. health insurance debate is coverage for pre-existing conditions—how many Canadians are aware it’s an issue here, too? We told you about Kerri, a freelance writer, who needs expensive drugs for asthma and attention deficit hyperactivity disorder. Private plans won’t cover her because those are pre-existing conditions. “In our unstable job market, why do we continue to tether drug insurance to stable employment?” Kerri asked. And there was Alexandra, who got her expensive anti-depressant as part of graduate student benefits—but knew her formal diagnosis of depression could affect her ability to get private insurance for the rest of her life. “My real hope is that by the time I graduate we would have finally plugged the 50-year old hole in Canadian health care and put the term ‘pre-existing condition’ in a museum, where it belongs,” she said.
We heard from too many people like Dave, who try to make medications (such as asthma drugs, or insulin) last longer by stretching the time between doses—a tactic that often leads to a crisis, a visit to emergency and even long-term harm that cannot be repaired. That’s also what happens to the many people we heard from who can’t pay for all the medications they need.
Imagine how many more stories there must be like this. How many people there are who want to work, want to enjoy their lives and their families, want to contribute to this country, who are limited, day in and day out by health problems they can’t afford to treat. And think about how many more people are only one job loss, one failed marriage, one change in benefits or one diagnosis away from finding themselves in a similar situation.
We’ve given you the data on how the lack of pharmacare affects health care costs. We have presented the financial arguments, from how national pharmacare would let us negotiate better drug prices to how it would reduce emergency visits and hospitalizations for people who couldn’t afford their medicine. We showed how employers, free from soaring premiums, could pay employees better or reinvest in their businesses. That’s all critically important. But at the heart of every decision about pharmacare are people, residents of this great country, who deserve to be treated fairly and to have equal access to the best care we can give.
It's time to close the gap between our values and our reality. It’s time for universal single-payer, public pharmacare.
Annex 1: Biographies
Please refer to Advisory Council on the Implementation of National Pharmacare-Biographies
Annex 2: Annex 2: Order in Council
Please refer to Advisory Council on the Implementation of National Pharmacare-Terms of Reference
Annex 3: National dialogue participants
The Advisory Council on the Implementation of National Pharmacare is deeply grateful to everyone who gave of their time, advice and insights on how to create national pharmacare in Canada. It would have been impossible to propose such an important innovation to Canadian life without their contribution. In total, more than 16,000 individuals and organizations participated through an online questionnaire, discussion forums and formal written submissions. We also received over 14,000 letters via email and post.
It was a privilege to meet so many concerned Canadians face to face, as we travelled to every province and territory where we discussed pharmacare issues with a broad range of patients and health care providers, experts and stakeholders.
We also explored the implications and challenges of a shift to a national pharmacare system in our discussions with provincial and territorial governments and Indigenous governments and representative organizations, including the Assembly of First Nations, Inuit Tapiriit Kanatami and the Métis National Council.
The following is a list of organizations that either met with us or made a submission to us. For privacy reasons, the list does not include the names of any individuals we heard from.
Participants
AbbVie Corporation
Accompass
Acho Dene Koe First Nation
Action Canada for Sexual Health and Rights
Actuariat-conseil Inc
Alberta Blue Cross
Alberta College of Pharmacy
Alberta Dental Association and College
Alberta Federation of Labour
Alberta Federation of Union Retirees
Alberta First Nations Health Co-Management Subcommittee
Alberta Health Services
Alberta Medical Association
Alberta Pharmacists’ Association
Alberta School Employee Benefit Plan
Alberta Union of Provincial Employees
Alberta, Ministry of Health
Alliance for Healthier Communities
ALS Society of Canada
Alzheimer Society of Prince Edward Island
Amgen
Anishinaabeg of Kabapikotawangag Resource Council
Apotex
ArcelorMittal Dofasco G.P.
Archway Insurance
Armco Capital
Arthritis Society
Arthur J. Gallagher & Co.
Assembly of First Nations Chiefs Committee on Health
Association des pharmaciens des établissements de santé du Québec
Association of Family Health Teams of Ontario
Association of Iroquois and Allied Indians
Association of Local Public Health Agencies
Association of Registered Nurses of British Columbia
Association of Registered Nurses of Manitoba
Association of Registered Nurses of Newfoundland and Labrador
Association of Yukon Communities
Association québécoise des pharmaciens propriétaires
Asthma Canada
AstraZeneca Canada Inc.
Atlantic First Nations Health Partnership
Auto Sector Retiree Health Care Trust
Avenue Solutions
Bayshore Specialty Rx
Bell Canada
Benecaid
Benefits by Design
Best Medicines Coalition
Better Pharmacare Coalition
Bigstone Health Commission
Biogen
BioScript Solutions
Biosimilars Canada
BIOTECanada
Bison Transport
Blood Ties
BluePeak Advisors
Boehringer Ingelheim Limited
Bowman’s Pharmasave
BoyneClarke LLP
Bristol-Myers Squibb Canada Co.
British Columbia Cancer Agency
British Columbia Child and Youth Advocacy Coalition
British Columbia Dental Association
British Columbia Federation of Labour
British Columbia Government and Service Employees’ Union
British Columbia Health Coalition
British Columbia Schizophrenia Society
British Columbia, Ministry of Health
Business Council of Canada
Calgary Co-operative Association Limited
Canada Health Infoway
Canadian Agency for Drugs and Technologies in Health
Canadian Arthritis Patient Alliance
Canadian Association for Pharmacy Distribution Management
Canadian Association for Retired Persons
Canadian Association of Community Health Centers
Canadian Association of Pharmacy Students and Interns
Canadian Association of Social Workers
Canadian Blood Services
Canadian Breast Cancer Network
Canadian Cancer Society
Canadian Cancer Survivor Network
Canadian Chamber of Commerce
Canadian Chiropractic Association
Canadian Council for Rehabilitation and Work
Canadian Council of the Blind
Canadian Dental Association
Canadian Diabetes Association
Canadian Doctors for Medicare
Canadian Epilepsy Alliance
Canadian Fabry Association
Canadian Federation of Independent Business
Canadian Federation of Medical Students
Canadian Federation of Nurses Unions
Canadian Foundation for Healthcare Improvement
Canadian Generic Pharmaceutical Association
Canadian Health Policy Institute
Canadian Hemophilia Society
Canadian Imperial Bank of Commerce
Canadian Institute for Health Information
Canadian Institute of Actuaries
Canadian Labour Congress
Canadian Life and Health Insurance Association
Canadian Lung Association
Canadian Medical Association
Canadian Mental Health Association
Canadian Mental Health Association - National Council of People with Lived Experience
Canadian National Pensioners Association
Canadian Nurses Association
Canadian Organization for Rare Disorders
Canadian Paediatric Society
Canadian Patient Safety Institute
Canadian Pharmacists Association
Canadian PKU and Allied Disorders
Canadian Positive People Network
Canadian Public Health Association
Canadian Skin Patient Alliance
Canadian Society of Hospital Pharmacists
Canadian Spondylitis Association
Canadian Treatment Action Council
Canadian Union of Public Employees
Canadians for Equitable Access to Depression Medication
Cancer Care Ontario
CanCertainty
Cardiac Health Foundation
Cardiac Transplant Clinic
Cargill Limited
Carleton University, School of Public Policy and Administration
Catalyst Health Solutions
Centre for Drug Research and Development
Centre for Sexuality
Centre Universitaire de Santé McGill
CGI Inc.
Chiefs of Ontario Health Coordination Unit
Children’s Hospital of Eastern Ontario
Choices for Youth
City of Calgary
City of Red Deer
Clearwater Seafoods Limited Partnership
Coalition for Safe and Effective Pain Management
Coalition solidarité santé
College and Association of Registered Nurses of Alberta
College of Pharmacists of British Columbia
College of Pharmacists of Manitoba
College of Registered Nurses of Prince Edward Island
Communist Party of Canada
Confédération des syndicats nationaux
Conference Board of Canada
Congress of Union Retirees
Connex Health
Conseil du patronat du Québec
Consumer Health Products Canada
Co-operators Life Insurance Company
Core Benefits
Costco Wholesale Canada
Council of Canadians with Disabilities
Council of Senior Citizens of BC
Covenant Health
CPHR Canada
Cystic Fibrosis Canada
D2L Corporation
Dalhousie University
Danish Life Sciences
De dwa da dehs nye>s Aboriginal Health Centre
Dehcho First Nations
Dental Association of Prince Edward Island
Desjardins Financial Security
Diabetes Canada
Dilico Anishnabek Family Care
Doctors Nova Scotia
East Community Health Engagement Committee
Eastern Health
Eli Lilly Canada Inc.
Ellis Health Policy Inc.
Empire Life
Excella Lifestyles
Express Scripts Canada
Families USA
Fancy Pokket Corporation
Federally Regulated Employers – Transportation and Communications
Fédération des chambres de commerce du Québec
Fédération des médecins spécialistes du Québec
Fédération des travailleurs et travailleuses du Québec
Federation of Sovereign Indigenous Nations
Fellows of the Canadian Institute of Actuaries
Finning Canada
First Nations Health Authority
Food Allergy Canada
Fort William Family Health Team Inc.
Friends of Medicare
Giant Tiger Stores Limited
Gibbons Guardian Pharmacy
Gilead Sciences Canada, Inc.
GlaxoSmithKline
Global Public Affairs
Green Shield Canada
Grey Bruce Health Services
Group Medical Services
Gwich'in Tribal Council
H3 Consulting
Halifax Port Authority
Harbourview Family Health Team
Health Advocate
Health Canada
Health Charities Coalition of Canada
Health Consulting Canada
Health Quality Council of Alberta
Health Sciences Association of British Columbia
HealthcareCAN
HealthPRO Procurement Services Inc.
Heart and Stroke Foundation of Canada
Hoffmann-La Roche Limited
Horizon Government Affairs
Horizon Health Network
Horizon Health Patient Experience Advisory Council
HRO Core Inc.
Humania
IAVGO Community Legal Clinic
Independent Voices for Safe and Effective Drugs
Indigenous Primary Health Care Council
Indigenous Services Canada
Inland Technologies
Innovative Medicines Canada
Institut national d'excellence en santé et services sociaux
Institut universitaire de gériatrie de Montréal
Institute for Research on Public Policy
Institute of Health Economics
Inuit Tapiriit Kanatami
Inuvialuit Regional Corporation
Isaac Foundation
Janssen
Johnson & Johnson
Kidney Cancer Canada
Kitchener Downtown Community Health Centre
Kwanlin Dun First Nation
Lakehead Nurse Practitioner-Led Clinic
L'Association francophone des aînés du Nouveau-Brunswick
Le Regroupement provincial des comités des usagers
LGBT Youth Project
Life Sciences Ontario
Little Salmon Carmacks First Nation
Loblaws Companies Limited
Lovell Drugs Limited
Lundbeck Canada Inc.
Magna International Inc.
Manitoba Association of Community Health
Manitoba Blue Cross
Manitoba Chamber of Commerce
Manitoba Health Coalition
Manitoba Metis Federation
Manitoba Nurses Union
Manitoba, Department of Health, Seniors, and Active Living
Manulife Canada
Markham Stouffville Hospital
McKenna, Long & Aldridge
McKesson Canada
McMaster University
Medavie Blue Cross
MEDEC - Canada's Medical Technology Companies
Medical Society of Prince Edward Island
Medical Students Association
Medicine Chest Pharmacy
Memorial University
Mercer Canada
Merck Canada Inc.
Métis National Council
Middlesex-London Health Unit
Mid-Main Community Health Centre
Mi'kmaq Confederacy of PEI
Ministry of Health, Welfare and Sport, the Netherlands
Mississauga Board of Trade
Morneau Shepell
Mount Carmel Clinic
MS Society of Canada
Municipality of Pictou
Munro’s Sorrento Prescriptions
Muscular Dystrophy Canada
Myeloma Canada
National Association of Federal Retirees
National Association of Pharmacy Regulatory Authorities
National Council for Behavioral Health
National Council on Aging
National Pensioners Federation
National Union of Public and General Employees
Native Women’s Association of Canada
Neighbourhood Pharmacy Association of Canada
New Brunswick Association of Nursing Homes
New Brunswick Association of Social Workers
New Brunswick College of Family Physicians
New Brunswick College of Pharmacists
New Brunswick Dental Society
New Brunswick Federation of Labour
New Brunswick Health Council
New Brunswick Lung Association
New Brunswick Medical Society
New Brunswick Nurses Union
New Brunswick Pharmacists’ Association
New Brunswick Senior Citizens Association
New Brunswick Women’s Council
New Brunswick, Department of Health
Newfoundland and Labrador 50+ Federation Inc.
Newfoundland and Labrador Board of Pharmacy
Newfoundland and Labrador Dental Association
Newfoundland and Labrador Federation of Labour
Newfoundland and Labrador Medical Association
Newfoundland and Labrador, Department of Health and Community Services
Nishnawbe Aski Nation
North End Community Health Centre
North Shore MicMac District Council
North Slave Métis Alliance
North York General Hospital
Northern Territories Federation of Labour
Northwest Pharmacy
Northwest Territories Health and Social Services Authority
Northwest Territories, Bureau of Statistics
Northwest Territories, Department of Finance
Northwest Territories, Department of Health and Social Services
Northwest Territory Métis Nation
NorWest Community Health Centre
Nova Scotia Cancer Care, Nova Scotia Health Authority
Nova Scotia College of Pharmacy
Nova Scotia Dental Association
Nova Scotia Federation of Labour
Nova Scotia Health Authority
Nova Scotia Health Coalition
Nova Scotia Nurses Association
Nova Scotia, Department of Health and Wellness
Novartis Pharmaceuticals Canada Inc.
Novo Nordisk Canada Inc.
Nunatsiavut Government, Department of Health and Social Development
Nunavut Status of Women Council
Nunavut Tunngavik Incorporated
Nunavut, Department of Finance
Nunavut, Department of Health
Nunavut, Department of Health – Patient Relations
Nurse Practitioner Association of Manitoba
Nurse Practitioner Association of Nova Scotia
Nurse Practitioners’ Association of Ontario
Nurses Association of New Brunswick
OMG Benefits Consulting
Ontario Chamber of Commerce
Ontario College of Pharmacists
Ontario Dental Association
Ontario Federation of Labour
Ontario Health Coalition
Ontario Medical Association
Ontario Minister’s Patient and Family Advisory Council
Ontario Nurses Association
Ontario Pharmacists Association
Ontario, Ministry of Health and Long-Term Care
Ordre des Pharmaciens du Québec
Organigram
Ostomy Society
Pacific Blue Cross
Paediatric Chairs of Canada
pan-Canadian Pharmaceutical Alliance
Patented Medicine Prices Review Board
Patient Advisors Network
PCL Constructors Inc.
PEERS Alliance
PHARMAC - The Pharmaceutical Management Agency of New Zealand
Pharmaceutical Benefits Scheme and Advisory Committee, Australia
Pharmacists Manitoba
Pharmacists’ Association of Newfoundland and Labrador
Pharmacy Association of Nova Scotia
Pharmacy Association of Saskatchewan
Pharmascience
Positive Living Society of Canada
Prince Edward Island Association for Newcomers to Canada
Prince Edward Island College of Pharmacists
Prince Edward Island Federation of Labour
Prince Edward Island Health Coalition
Prince Edward Island Lung Association
Prince Edward Island Nurses Union
Prince Edward Island Pharmacists Association
Prince Edward Island, Advisory Council on the Status of Women
Prince Edward Island, Department of Health and Wellness
Public Service Alliance of Canada
Pulmonary Hypertension Association
Qikiqtani General Hospital
Quebec First Nations
Quebec, Ministry of Health and Social Services
Queen Elizabeth II Health Sciences Centre
Queen’s University
REACH Community Health Centre
Regina Community Clinic
Registered Nurses Association of the Northwest Territories and Nunavut
Registered Nurses’ Association of Ontario
Registered Nurses’ Union Newfoundland & Labrador
Rethink Cancer
Roche Canada
Roy Lounsbury Holdings Limited
Royal Bank of Canada
Royal College of Physicians and Surgeons of Canada
Saint John Human Development Council
Santé Mercer Canada
Saskatchewan Association of Nurse Practitioners
Saskatchewan Cancer Agency
Saskatchewan Chamber of Commerce
Saskatchewan College of Pharmacy Professionals
Saskatchewan Federation of Labour
Saskatchewan Health Authority
Saskatchewan Registered Nurses Association
Saskatchewan Union of Nurses
Saskatchewan, Ministry of Health
Save Your Skin Foundation
SBW Wealth Management & Employee Benefits
Scotiabank
Selkirk First Nation
Senior Liberal Club of Nepean
Seniors Resource Centre of Newfoundland & Labrador
Seniors’ Action Yukon
Seniors’ Advisory Council of Nova Scotia
Servier Canada Inc.
Shire Pharma Canada ULC
Shoppers Drug Mart
Simon Fraser University
Sinai Health System
Sioux Lookout First Nations Health Authority
Sobeys National Pharmacy Group
Sobi Canada Inc.
Somerset West Community Health Centre
South-East Local Health Integration Network
South Riverdale Community Health Centre
Southwestern Public Health
SSQ Groupe financier
St. John’s Board of Trade
St. John’s Women’s Centre
St. Michael’s Hospital
Stanton Territorial Hospital
Stewart McKelvey
Stoney Nakoda Tsuut’ina Tribal Council
Sun Life Financial
Suncor Energy Inc.
Surrey Board of Trade
Telus Health
Teslin Tlingit Council
TEVA Canada
The Gathering Place
The Goodman Pediatric Formulations Centre of the CHU Sainte-Justine
The Great-West Life Assurance Company
The Hospital for Sick Children
The Pharmacare Working Group
The Tudor Group
Third Party Administrators’ Association of Canada
Thorpe Benefits
Thunder Bay Chamber of Commerce
Thunder Bay Dental Association
Thunder Bay Regional Health Sciences Centre
Tłįchǫ Government
Toronto Public Health
Treaty 8 First Nations of Alberta
TRG Benefits & Pensions Inc.
Tribal Chiefs Ventures
Tr'ondëk Hwëch'in
Unifor
Union des consommateurs
uniPHARM Wholesale Drugs Limited
Unison Benefits
United Church of Canada
United Food & Commercial Workers
United Nurses of Alberta
Université de Montréal
University of British Columbia
University of Calgary, Department of Economics
University of Calgary, Health Technology Assessment Unit
University of Manitoba, Ongomiizwin Indigenous Institute of Health and Healing
University of Ottawa, Institute of Fiscal Studies and Democracy
University of Regina, Graduate School of Public Policy
University of Regina, Saskatchewan Population Health and Evaluation Research Unit
University of Saskatchewan, College of Medicine
University of Saskatchewan, College of Pharmacy and Nutrition
University of Saskatchewan, Geriatric Medicine
University of Toronto, Dalla Lana School of Public Health
University of Toronto, Institute of Health Policy, Management and Evaluation
University of Toronto, Leslie Dan Faculty of Pharmacy
University of Waterloo
University Women’s Club of Montreal
Vitalité Health Network
Waypoint Centre for Mental Health Care
Wellesley Institute
West Community Health Engagement Committee
Willis Towers Watson
Windigo First Nations Council
Winnipeg Chamber of Commerce
Winnipeg Regional Health Authority
Yellowknife Regional Wellness Council
York University
Yukon Anti-Poverty Coalition
Yukon Hospital Corporation
Yukon Pharmacists Association
Yukon Status of Women Council
Yukon, Health and Social Services
Annex 4: Overview of provincial and territorial drug plans
| Province / Territory | Number of plans | General benefit | Targeted benefits for income assistance recipients | Targeted benefits for older persons | Targeted benefits for children/youth |
|---|---|---|---|---|---|
| British Columbia | 11 | Universal, income-based catastrophic drug coverage. | Comprehensive drug coverage, without patient charges. | Reduced income-based deductibles and coinsurance for persons born before 1940. | No age-tested general benefit for children or youth. |
| Alberta | 10 | Voluntary, premium-based plan. | Comprehensive drug coverage, without patient charges. | Age-tested comprehensive drug benefit. | Age-tested and income-tested drug benefit for children in low-income families. |
| Saskatchewan | 10 | Universal, income-based catastrophic drug coverage. | Reduced deductibles and copayments. | Age-tested and income-tested cap on copayment for prescriptions. | Age-tested cap on copayment for prescriptions. |
| Manitoba | 6 | Universal, income-based catastrophic drug coverage. | Comprehensive drug coverage, without patient charges. | No age-tested benefit for older adults. | No age-tested general benefit for children or youth. |
| Ontario | 6 | Universal, income-based catastrophic drug coverage. | Comprehensive drug coverage, with some patient charges. | Age-tested comprehensive drug benefit. | Age-tested and insurance-tested comprehensive drug coverage, without patient chargesFootnote ** |
| Quebec | 2 | Mandatory, premium-based private or public drug coverage. | Income-tested first-dollar public drug coverage. | Age-tested option to purchase premium-based public drug coverage even if private coverage available. | Age-tested and insurance-tested first-dollar public drug coverage. |
| New Brunswick | 16 | Voluntary, premium-based plan. | Comprehensive drug coverage, with some patient charges. | Age-tested and income-tested drug benefit for low-income seniors. | No age-tested general benefit for children or youth. |
| Nova Scotia | 9 | Universal, income-based catastrophic drug coverage. | Comprehensive drug coverage, with some patient charges. | Voluntary, premium-based public drug plan. | Age-tested and income-tested drug benefit for children in low-income families. |
| Prince Edward Island | 28 | Universal, income-based catastrophic drug coverage. | Comprehensive drug coverage, without patient charges. | Age-tested comprehensive drug benefit. | Age-tested and income-tested drug benefit for low-income families with children. |
| Newfoundland and Labrador | 5 | Income-tested and income-based catastrophic drug coverage. | Comprehensive drug coverage, without patient charges. | Age-tested and income-tested drug benefit for low-income seniors. | No age-tested general benefit for children or youth. |
| Yukon | 4 | Universal drug benefit for residents who have one or more qualifying diseases. | No targeted benefit for income assistance recipients. | Age-tested, first-dollar comprehensive drug benefit. | Age-tested and income-tested drug benefit for low-income families with children. |
| Northwest Territories | 3 | Universal drug benefit for residents with one or more qualifying diseases. | No targeted benefit for income assistance recipients. | Age-tested, first-dollar comprehensive drug benefit. | No age-tested general benefit for children or youth. |
| Nunavut | 3 | Universal drug benefit for residents with one or more qualifying diseases. | No targeted benefit for income assistance recipients. | Age-tested, first-dollar comprehensive drug benefit. | No age-tested general benefit for children or youth. |
|
|||||
Annex 5: Key characteristics of the pharmacare systems in comparator countries
| Country | System type | Eligibility | Role of private insurance | Deductible | Copayment / coinsurance |
|---|---|---|---|---|---|
| Australia | Universal, comprehensive public coverage. | Universal: all ages and incomes. | Public plan is payer of first resort. About half of adults have voluntary, complementary private insurance. | None. | Copayment equal to the lesser of $37.00 (AU$39.50) or the full cost of the drug, per item on the prescription. Once a household has paid $1,425 (AU$1,521.80) in copayments during a calendar year, their copayments for the balance of that year are reduced to $6.00 (AU$6.40). |
| France | Universal, comprehensive statutory insurance coverage. | Universal: all ages and incomes. | Statutory plan is payer of first resort. More than 90% of residents have voluntary, complementary private insurance. | None. | Ranges from 0% to 85% of prescription costs depending on the medicine's clinical benefit. |
| Germany | Universal, comprehensive statutory insurance coverage. | Universal: all ages and incomes; residents earning over $90,000 may opt to purchase substitutive private health insurance. | Statutory plan is payer of first resort. A small proportion of the population has voluntary, complementary private insurance. | None. | Ranges between $7.60 (€5) and $15.20 (€10) per prescription. Total patient contributions for prescriptions and other insured health care services are limited to 2% of gross income (or 1% for patients with severe chronic conditions). |
| Netherlands | Universal, comprehensive statutory insurance coverage. | Universal: all ages and incomes. | Statutory plan is payer of first resort. More than 80% of residents have voluntary, complementary private insurance. | Annual deductible of $584 (€385) toward all health care costs. | After the deductible is reached, cost sharing for prescription drugs is limited to fees that may be charged in relation to reference-based reimbursement and preference product schemes. |
| New Zealand | Universal, comprehensive public coverage. | Universal: all ages and incomes. | Public plan is payer of first resort. About 30% of the population has voluntary, complementary private insurance. | None. | $4.30 (NZ$5.00) per item on a prescription. Copayments can be eliminated for families that have paid for more than 20 prescription items in a given year. |
| United Kingdom | Universal, comprehensive public coverage. | Universal: all ages and incomes. | Public plan is payer of first resort. About 10% of the population has voluntary, complementary private insurance. | None. | No copayments in Scotland, Wales, or Northern Ireland. In England, patients pay $15.00 (£8.80) per item; or prepayment of $50.00 (£29.10) for 3 months or $176.00 (£104) for 12 months. |
|
|||||
Annex 6: Drug spending model
This annex provides an overview of the drug spending model (the “DSM”), as well as a description of the data and methodology used to generate the drug spending and drug usage estimates presented in this report.
There is an inherent uncertainty surrounding any cost modelling exercise of this nature and scope. The DSM is also subject to a number of limitations. Some reflect limitations imposed by the data or a lack of information on key issues such as confidential rebates. Other limitations reflect the scope of the DSM, which cannot directly address potentially important issues such as administrative costs, transition costs, economic impacts, revenue-raising options, and the full impacts of national pharmacare on decisions in relation to existing private plans (including insurers and plan sponsors such as employers). Its results, however, can help to inform these types of analyses.
To ensure that the cost estimates included in this report are as accurate as possible, federal, provincial and territorial officials, as well as experts and stakeholders, have been consulted on the data, the methodology and the assumptions underlying the DSM.Footnote iii That said, the Advisory Council on the Implementation of National Pharmacare takes sole responsibility for the analysis and conclusions reached in terms of the potential costs of national pharmacare.
1 Model overview
The DSM builds on methodologies set out in previous studies on the potential cost of national pharmacare (e.g., Parliamentary Budget Officer Footnote iv, Morgan et al.Footnote v). The DSM, however, incorporates a projection component that allows estimation of the potential impacts of national pharmacare on prescription drug spending over time, including the potential to drive improvements in the cost-efficiency of prescribing (e.g., through the increased use of generic and biosimilar drugs), and broaden the application of—and potentially increase the value of—confidential rebates on brand name drugs. As with previous studies on the potential cost of national pharmacare, the DSM also accounts for increased drug usage from the improvement in prescription adherence among individuals who were previously uninsured or underinsured.Footnote vi
The inclusion of a projection component allows the DSM to reflect assumptions about the relative timing of different impacts under national pharmacare. For example, it will likely take time to realize cost savings from the broader application of confidential rebates (discounts negotiated with manufacturers, kept secret to protect their list price), whereas increased usage is likely to manifest more quickly. This projection component provides a more detailed picture of how the impacts of national pharmacare may affect overall drug spending over time. It also allows the model to take into account key drivers of prescription drug expenditures (e.g., population growth, new drug entries) and thereby generate projections of future drug spending—both with and without the implementation of national pharmacare.
2 Prescription drug data
The DSM is based primarily on data acquired from IQVIA Solutions Canada Inc. on prescription drugs dispensed in community pharmacies in Canada.Footnote vii The data was extracted from the Geographic Prescription Monitor and Compuscript databases in June 2018 and covers the period from June 2015 to May 2018. This data is supplemented by information provided by the Canadian Institute of Health Information (CIHI) (e.g., a mapping of the relative cost of treatment for different drugs), Health Canada (e.g., the Drug Product Database), and the Patented Medicine Prices Review Board (e.g., Patent Register Database).
The IQVIA data is stratified according to five categories: drug type, geographyFootnote viii, age cohort, gender and primary payer (Figure 20). “Primary payer” is divided into three categories: public plans, private insurance and out of pocket.Footnote ix
Source: IQVIA Solutions Canada. Note: Totals may not add due to rounding, and do not reflect confidential rebates. *12-month period ending in May 2018.
Figure 20: Text description
This graphic shows the various stratifications used in the drug spending model.
- Drugs: ATC 5, DIN
- Gender: Male/female
- Age: 0-18, 19-44, 45-64, 65+
- Province
- Primary Payer: Public, private insurance, cash
The IQVIA data used in the DSM indicates that, in the 12-month period ending in May 2018 (referred to hereafter as 2017 for simplicity), $29.8 billion was spent on prescription drugs at pharmacies in Canada, of which 45 per cent ($13.4 billion) was delivered primarily by public plans; 38 per cent ($11.5 billion) was delivered primarily by private insurance; and 17 per cent ($5.0 billion) was paid for primarily out of pocket (Figure 21).Footnote x
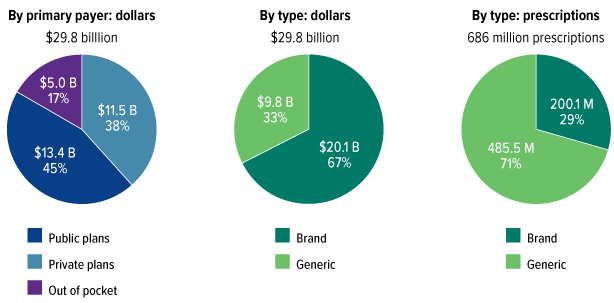
Figure 21: Text description
| By primary payer (dollars) | Dollars (billion) |
|---|---|
| Private insurance | 11.5 |
| Public Plans | 13.4 |
| Out-of-pocket | 5 |
| Total | 29.9 |
| By type (dollars) | Dollars (billion) |
| Brand | 20.1 |
| Generic | 9.8 |
| Total | 29.9 |
| By type (prescriptions) | # Rx (million) |
| Brand | 200.1 |
| Generic | 485.5 |
| Total | 686 |
Source: IQVIA Solutions Canada
|
|
Source: IQVIA Solutions Canada. Note: Totals may not add due to rounding, and do not reflect confidential rebates. *12-month period ending in May 2018.
IQVIA data indicates that while brand name drugs represented 67 per cent of prescription drug spending, they represented only 29 per cent of total prescriptions. Generic drugs represented 33 per cent of spending but 71 per cent of all prescriptions. This makes Canada one of the largest generic drug users among OECD countries in terms of share of total units of drugs consumed, though the United States is well ahead with a generic share closer to 90 per cent.Footnote xi,Footnote xii
On a by-province basis, the IQVIA data illustrates a wide range in prescription drug spending across Canada, ranging from $591 per capita in British Columbia to $1,028 per capita in Quebec (Table 3). The degree of public coverage also varies widely, ranging from 26 per cent of overall spending in Prince Edward Island ($29 million out of $110 million) to about 50 per cent in Saskatchewan ($395 million out of $772 million), Ontario ($5.6 billion out of $11.8 billion) and Quebec ($4.2 billion out of $8.6 billion).
| Provinces | $ Millions ($ Per Capita) | Share of Total | |||||
|---|---|---|---|---|---|---|---|
| Public Plans | Private Insurance | Out of pocket | Total | Public | Private Insurance | Out of pocket | |
| BC | 1,062 (221) | 1,036 (216) | 741 (154) | 2,839 (591) | 37% | 36% | 26% |
| AB | 1,122 (259) | 1,273 (294) | 463 (107) | 2,858 (661) | 39% | 45% | 16% |
| SK | 395 (341) | 214 (184) | 164 (142) | 772 (667) | 51% | 28% | 21% |
| MB | 321 (241) | 275 (207) | 217 (163) | 813 (611) | 39% | 34% | 27% |
| ON | 5,641 (400) | 4,709 (334) | 1,438 (102) | 11,788 (836) | 48% | 40% | 12% |
| QC | 4,163 (497) | 2,853 (341) | 1,595 (190) | 8,611 (1,028) | 48% | 33% | 19% |
| NB | 232 (306) | 386 (509) | 113 (150) | 731 (965) | 32% | 53% | 15% |
| NS | 273 (288) | 447 (471) | 116 (122) | 837 (881) | 33% | 53% | 14% |
| PE | 29 (194) | 59 (393) | 22 (145) | 110 (731) | 26% | 54% | 20% |
| NL | 142 (269) | 258 (490) | 90 (171) | 491 (930) | 29% | 53% | 18% |
| Total | 13,380 (367) | 11,510 (316) | 4,959 (136) | 29,849 (818) | 45% | 38% | 17% |
Source: IQVIA Solutions Canada. Note: Totals may not add due to rounding, and do not reflect confidential rebates.
|
|||||||
3. Methodology
The DSM generates estimates of brand name and generic prescription drug spending, prescription volumes and patient cost sharing under national pharmacare over the projection period, broken down by province and by primary payer. The estimates generated by the model reflect:
- National pharmacare design parameters (e.g., eligibility criteria, formulary and cost sharing terms);
- Assumptions about the impact of national pharmacare on a variety of factors (e.g., confidential rebates, cost-related non-adherence and generic substitution); and
- General assumptions about the drivers of prescription drug spending (e.g., demographic changes).
Given the significant uncertainty surrounding some of these assumptions, DSM results are generated for both low- and high-cost scenarios for national pharmacare that reflect different but plausible sets of assumptions (discussed in more detail below). As discussed below in section 4.1, low- and high-cost scenarios are also generated for the status quo projection (i.e., in the absence of national pharmacare). However, for simplicity, a single mid-range status quo projection is used as the baseline against which to compare scenarios generated by the DSM for national pharmacare. Unless otherwise noted, all references to assumptions used for the status quo scenario reflect this mid-range status quo projection.
3.1 National pharmacare design parameters
The DSM can project prescription drug spending for a wide variety of national pharmacare design parameters, defined by: who is covered (i.e., eligibility criteria); what is covered (i.e., formulary); and the terms of cost sharing with beneficiaries (e.g., copayments, deductibles). Policy decisions in respect of these parameters are the key ways to influence the total cost of national pharmacare and its impacts on access.
Eligibility criteria
Eligibility for coverage under national pharmacare could be universal (i.e., coverage for everyone) or targeted (i.e., focusing on a particular segment of the population). Eligibility or the specific terms of coverage may also vary with income (e.g., providing more coverage for lower-income Canadians).
To simulate eligibility criteria, the DSM requires inputs on the proportion of spending by each population cohort (determined by age, sex and province) that would be covered by a given option for national pharmacare. For example, universal first dollar coverage would be modelled by setting the proportion to 100 per cent for all population cohorts. Age or sex targeted coverage would be modelled by choosing different percentages for different age-sex cohorts. For example, universal seniors’ coverage would be modelled by setting coverage to 100 per cent for the 65-plus age cohort.
Income tested coverage requires additional analysis on income distribution and drug consumption distribution for each age-sex-province combination. In this case, the proportion of spending covered in each age-sex-province cohort would be some percentage between 0 and 100 per cent, depending on parameters of the income tested option.
- Cost estimates presented in Chapter 6 and in this annex are based on universal public coverage for all drugs listed on the essential medicines list (i.e., when pharmacare is initially introduced in 2022) and Quebec’s comprehensive RAMQ formulary (i.e., when pharmacare is fully implemented in 2027).
Formulary
A formulary is a list of drugs that are approved for reimbursement by a drug plan. Based on their clinical benefits, safety and cost-effectiveness, drugs may be listed on a formulary either on an open access or conditional basis. Drugs listed on a conditional basis typically require patients to meet certain criteria (e.g., be of a certain age, disease status or have tried another drug) before the drugs are covered.
The DSM is able to simulate formularies specified using either ATC 5Footnote xiii classification or the DIN.Footnote xiv For the purposes of simulating national pharmacare, the DSM makes the simplifying assumption that all on formulary drugs are covered on an open access basis. The DSM addresses the impact of conditional access indirectly by measuring the relative efficiency of the drug mix covered by different payers. For example, the DSM uses generic substitution rates in existing public plans—which make greater use of cost saving strategies such as conditional access or reference drug pricingFootnote xv—as targets for generic substitution rates that could be achieved system wide under national pharmacare.
Cost estimates presented in Chapter 6 and in this annex are based on either an essential medicines list or Quebec’s comprehensive public plan RAMQ formulary. The Quebec RAMQ formulary was used for consistency with the 2017 Parliamentary Budget Officer pharmacare costing report, and due to the fact that the drugs on the RAMQ formulary represent the largest share of system wide spending of any provincial public plan formulary in Canada.
- Essential medicines: The essential medicines list is based on the Canadian CLEAN Meds list developed by researchers at St. Michael’s hospital in Toronto. As of April 8, 2019, it included 136 primary care medicines (i.e., identified at the ATC 5 level) considered as being the most important for meeting the health needs of Canadians. In 2017, these drugs represented about 27 per cent of system wide drug spending and 42 per cent of overall prescriptions.
- Comprehensive formulary: Coverage of a comprehensive formulary is simulated based on Quebec’s RAMQ public plan formulary. As of September 2018, the RAMQ formulary listed approximately 900 drugs (i.e., identified at the ATC 5 level). In 2017, these drugs represented about 86 per cent of system wide drug spending and 87 per cent of overall prescriptions.
Cost sharing terms
A deductible is an amount that an individual or family must pay out of pocket within a certain period of time (e.g., annually) before the drug plan will begin to pay. The DSM has the ability to simulate deductibles based on either fixed amounts (e.g., $X per person or family) or as a percentage of family income.
A copayment is an amount paid out of pocket by an individual each time a prescription is filled, with the remainder of the cost paid by the drug plan. The DSM has the ability to simulate copayments based on either fixed amounts (e.g., $X per prescription) or as a percentage of prescription costs. Different copayments may be specified for brand name and generic drugs. In addition, it is possible to specify populations exempt from copayments or subject to lower copayments (e.g., social assistance recipients and Guaranteed Income Supplement beneficiaries), within the constraints of the demographic and economic stratification of the available data sets.Footnote xvi
- Cost estimates presented in Chapter 6 and in this annex are based on copayments of $2 for drugs listed on the essential medicines list and $5 for all other covered drugs. Copayment exemptions are provided for Guaranteed Income Supplement recipients, persons on social assistance and persons receiving government disability benefits. In addition, the copayments are limited to a maximum of $100 per family per year.
3.2 Simulating the impacts of national pharmacare
To simulate the impacts of implementing national pharmacare on prescription drug usage and spending, it is necessary to develop assumptions about a variety of factors for which there is often very little available information or reasonable differences of opinion among experts and stakeholders. The following section sets out the key response parameters that influence the impacts of implementing national pharmacare. These are the parameters that are assumed to differ between the status quo scenario and under national pharmacare.
Demand response
A key objective of national pharmacare is to improve Canadians’ access to prescription drugs, which should have the effect of reducing cost-related non-adherence—when individuals forego their prescriptions because they can’t afford them.
Estimates suggest that about 5 per cent to 10 per cent of Canadians report cost-related non-adherence, although it is much higher among low-income Canadians and those without any insurance whatsoever.Footnote xvii To the extent that national pharmacare lowers the out of pocket cost of drugs and improves access, it may be expected to reduce cost-related non-adherence, resulting in an increase in overall drug consumption in Canada.
The DSM simulates a demand response based on the overall change in out of pocket spending (i.e., taking into account copayments and/or deductibles under national pharmacare), the price-elasticity of demand (i.e., the extent to which individuals change their consumption of prescription drugs in response to changes in the costs they face) and the degree of cost-related non-adherence observed in the market. Research and stakeholder consultations suggest that, on average, a 1 per cent reduction in out of pocket drug costs leads to an increase in total drug consumption of between 0.1 per cent and 0.2 per cent.
- The DSM assumes that total drug usage increases by between 0.1 per cent (low-cost scenario) and 0.2 per cent (high-cost scenario) for each 1 per cent decline in overall out of pocket spending. The increase is capped between 5 per cent (low-cost scenario) and 10 per cent (high-cost scenario), reflecting estimates of cost-related non-adherence.
- In terms of timing, the DSM assumes that the improvements in cost-related non-adherence occur in the first year that pharmacare is implemented, reflecting the likelihood that individuals would immediately begin filling prescriptions in response to improved access.
Confidential rebates
Another key objective of national pharmacare is to address high prescription drug costs. Confidential rebates are one potential avenue through which national pharmacare could reduce system wide spending on prescription drugs. This could be achieved by an expansion of confidential rebates—which are currently limited primarily to public plans—to cover a greater swath of system wide spending, and/or potentially increasing the magnitude of these rebates.
Currently, the pan-Canadian Pharmaceutical Alliance negotiates with drug manufacturers on behalf of public plans to obtain confidential rebates on prescription drugs. In exchange, public plans agree to list the drugs on their formularies. Under national pharmacare, existing public plan rebates could potentially be extended over time to “newly covered” brand name drugs (i.e., spending on drugs that was previously covered by private plans or paid out of pocket). In addition, to the extent that national pharmacare involves greater coordination between drug plans and/or an expansion of public plans, it could result in enhanced negotiating power for public plans, such that future confidential rebates could exceed those currently achieved by public plans. The creation of a new Canadian drug agency would help in this respect.
Due to the confidential nature of rebates there is, by definition, relatively little public information on either the drugs for which rebates have been negotiated or the magnitude of the rebates. Based on publicly available information as well as consultations, it is estimated that public plans in Canada currently obtain confidential rebates amounting to between 15 and 25 per cent of total public plan spending on existing brand name drugs, and that these rebates could be higher for new drugs coming to the market.
In addition, it is uncertain whether existing confidential rebates would remain in place under national pharmacare or whether they would have to be renegotiated and how long this would take. It is also possible that the magnitude of rebates would change as a national pharmacare plan would impact the negotiating dynamic with manufacturers.
- Under the status quo scenario, the DSM assumes a 20 per cent overall rebate on current public plan spending on brand name drugs. A 25 per cent overall rebate is assumed for public plan spending on new brand name drugs projected to enter the market over the projection horizon.
- Under the low-cost national pharmacare scenario, the DSM assumes that, within 5 years of implementation, all spending under national pharmacare for current brand name drugs (including spending previously paid for privately) will be subject to the currently assumed 20 per cent public plan rebate. National pharmacare spending on new brand name drugs is assumed to be subject to a 40 per cent overall rebate.
- Under the high-cost national pharmacare scenario, the DSM assumes that no rebates apply to national pharmacare spending on existing brand name drugs that were previously paid for privately. Spending on brand name drugs previously covered by public plans retains the 20 per cent rebate. National pharmacare spending on new brand name drugs is assumed to retain the 25 per cent overall rebate.
- Under both national pharmacare scenarios, the DSM assumes that other public plans (i.e., outside of pharmacare) retain the 20 per cent rebate on spending on existing brand name drugs and the 25 per cent rebate on spending on new brand name drugs. The DSM assumes no confidential rebates for privately covered spending.Footnote xviii
List prices
Examination of prescription drug data reveals that the same prescription drug may sell for different prices in different provinces. Under national pharmacare, however, negotiations could take place to ensure consistent national pricing of all drugs covered by national pharmacare.
- Under the status quo scenario, the DSM assumes no convergence in list prices.
- Under national pharmacare (both scenarios), wholesale drug prices (i.e., before dispensing fees and pharmacy mark-ups) are set to the national average prices. The current provincial dispensing fees and pharmacy mark-ups structures are assumed to remain unchanged under national pharmacare.Footnote xix
Prescription patterns
In addition to potential impacts on prices, the implementation of national pharmacare could enable the adoption of measures to encourage more cost-effective prescription patterns. The DSM takes into account three potential areas for improvements in the cost-efficiency of prescription patterns.
Generic substitution
The DSM defines generic substitution as the use of a chemically identical generic drug in place of a brand name drug. The DSM measures generic substitution by grouping drugs by ATC 5 and strength (i.e., the same molecule at the same dose). Within each generic substitution group, the generic substitution rate is measured as generic units divided by total units (i.e., brand and generic).
IQVIA data indicates that generic substitution is significantly more prevalent in public plans, suggesting that broader public coverage through national pharmacare can be expected to further shift the overall mix of drugs consumed in Canada towards generic drugs (Table 4). That said, the data also indicates that generic substitution rates are improving for all primary payers, suggesting that even in the status quo scenario, overall generic substitution may be expected to increase over time.
| Plans | 2015 | 2016 | 2017 | Average Annual Growth |
|---|---|---|---|---|
| Public plans | 87.4% | 88.9% | 89.1% | 0.8% |
| Private plans | 75.2% | 77.3% | 78.5% | 1.6% |
| Out of pocket | 76.3% | 77.6% | 78.4% | 1.1% |
Source: Council’s calculations, based on IQVIA data.
|
||||
As patents expire, lower priced generic drugs will also likely be introduced and substituted for the brand name drug that currently benefits from patent protection. Based on data from the Patent Register Database and analysis from the Patented Medicine Prices Review Board (PMPRB), the DSM estimates patent expiry dates for brand name drugs and the potential for generic substitution.
To simulate potential savings through generic substitution, the DSM compares measured generic substitution to a target rate (e.g., based on existing public plan generic substitution rates). Over time, prescription patterns are assumed to converge to the target.Footnote xx In addition, the target rates may be assumed to increase over time, reflecting continued potential for improvements in generic substitution rates. The speed of convergence depends on assumptions about trend improvements in generic substitution and potential improvements that may occur under national pharmacare.
- Under the status quo scenario, the DSM assumes that generic substitution rates for all primary payers converge over time to current median public plan generic substitution rates, which are assumed to remain constant. The time to convergence is assumed to be approximately seven years. Generic substitute prices are assumed equal to the minimum price generic alternative.
- Under national pharmacare, the DSM assumes that generic substitution converges to the most efficient public plan (low-cost scenario) or the median public plan (high-cost scenario) over four years. The target generic substitution rates also increase each year by 0.5 per cent (low-cost scenario) or 0.25 per cent (high-cost scenario). Generic substitute prices are assumed to be equal to the minimum price generic alternative.
- For drugs coming off patent, the DSM assumes, under all scenarios, that the cost of newly introduced generic substitutes gradually decreases from 75 per cent of the brand name cost to 25 per cent of the brand name cost over 10 years.Footnote xxi
Increased use of biosimilars
A biosimilar is a biologic drug demonstrated to be similar to a brand name biologic drug already authorized for sale in Canada (the “reference biologic”). Biosimilars are usually available at a discount relative to their reference biologics.Footnote xxii Biosimilar uptake is currently low in Canada compared to peer countries. That said, based on IQVIA data, about $3 billion of current spending on biologics will be coming off patent over the next decade, which can be expected to open the door to greater use of biosimilars and the associated savings.
Similar to the analysis on generic substitution, the DSM includes data on future patent expiry dates for biologic drugs in order to estimate potential savings in respect of biologics currently protected by patents.
- Under the status quo scenario, the DSM assumes that biologics gradually lose 40 per cent of their market share to biosimilars over 10 years (i.e., over time, the share of biosimilars will reach 40 per cent). The biosimilar discount relative to biologics coming off patent is assumed to be 20 per cent. For biologics already on the market, the lowest priced biosimilar is selected.
- Under the national pharmacare low-cost scenario, the DSM assumes that biologics covered by pharmacare gradually lose 60 per cent of their market share to biosimilars over 10 years (i.e., over time, the share of biosimilars will reach 60 per cent). The biosimilar discount for biologics coming off patent is assumed to be 30 per cent. For biologics already on the market, the lowest priced biosimilar is selected.
- Under the national pharmacare high-cost scenario, the DSM uses the same assumptions as the status quo scenario.
Therapeutic efficiency
In addition to generic substitution and increased used of biosimilars, the implementation of national pharmacare could potentially have an impact on the overall mix of drugs consumed in Canada, shifting that mix towards lower cost, therapeutically similar—but not chemically similar—alternatives. In the context of the DSM, the selection of these alternative treatments when available is referred to as therapeutic efficiency.
To measure further potential savings through improved therapeutic efficiency, the DSM groups prescription drugs into broader chemical subgroups (i.e., at the ATC 4 level, which delineates chemical subgroups of medicines). Within each group, therapeutic efficiency of a drug is measured by comparing its average annual cost of treatment (defined at the ATC 5 level) to that of the group as a whole. For each drug, based on the relative average annual cost of treatment, a “therapeutically efficient” amount of spending is then estimated. The overall therapeutic efficiency of a payer (i.e., public plans, private insurance and out of pocket) is then calculated as total spending divided by total “therapeutically efficient” spending.
To estimate potential improvements in therapeutic efficiency, the DSM allows the selection of a therapeutic efficiency target based on the measured therapeutic efficiency of existing public plans. As with generic substitution, potential savings are estimated by comparing the therapeutic efficiency of a plan to the target rate and assuming that it converges to this target over time.
- Under the status quo projection, the DSM assumes that there are no improvements in therapeutic efficiency over the projection period.
- Under the national pharmacare low-cost scenario, the DSM assumes that the therapeutic efficiency of public plans, including national pharmacare, converges to median public plan efficiency over seven years.
- Under the national pharmacare high-cost scenario, the DSM uses the same assumption as the status quo scenario.
Other cost-saving measures
In addition to simulating actual shifts in prescription patterns, the measures discussed above can be used to indirectly simulate other cost-saving measures. For example, adoption of reference-based pricing policies under which national pharmacare would reimburse only the cost of the lowest cost generic alternative could be simulated by assuming 100 per cent generic substitution and setting list prices equal to the lowest observed prices.
3.3 Drivers of prescription drug spending
Prescription drugs are a leading cost driver in the health care system. Canada spends more on drugs than on any other components of health care with the exception of hospitals. Prescription drug costs are forecast to grow faster than the two other largest spending categories in the health care system (hospitals and physicians) in 2018.
According to the Canadian Institute for Health Information (CIHI), total public and private expenditures on prescription drugs have grown by 6.5 per cent annually since 2000, to reach $33.7 billion in 2018. As Table 5 indicates, growth slowed somewhat after 2010, but has shown signs of accelerating in recent years.
| Plans | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | Period Average |
|---|---|---|---|---|---|---|---|---|---|---|
| Public plans | 2.1 | 2.1 | 0.0 | 0.5 | 4.0 | 5.0 | 2.4 | 1.7 | 5.0 | 2.5 |
| Private insurance | 3.3 | 2.4 | 3.3 | 2.6 | 3.0 | 6.8 | 2.7 | 3.7 | 4.6 | 3.6 |
| Out of pocketFootnote * | Footnote * | 0.2 | -1.4 | 0.6 | 0.3 | 0.1 | 0.1 | 4.5 | 1.8 | 0.8 |
| Total spending | Footnote * | 1.8 | 0.8 | 1.2 | 2.8 | 4.6 | 2.0 | 3.0 | 4.2 | 3.5 |
Source: Canadian Institute for Health Information. (2018). National Health Expenditures Database, 1975 to 2018, Table G.14.1. Ottawa, ON: CIHI.
|
||||||||||
Generating estimates of future prescription drug spending and prescription patterns requires making assumptions about how prescription drug prices, prescribing practices, and drug usage for both existing drugs and new drugs coming to the market will evolve over time, both under the status quo and different options for national pharmacare.
The DSM assumptions for the drivers of prescription drug spending reflect broad trends; although they could be influenced by other policy initiatives, it is presumed that these trends would not be directly influenced by the implementation of national pharmacare. Their values are set based on observed prescription drug spending and demographic trends.
The DSM requires making assumptions about four broad trend variables: inflation, demographics, volume growth, and new drug entries.
Impact of pCPA deal on generic drug prices
On January 29th, 2018 (and following a similar deal in Québec), the pCPA announced that it had negotiated generic price reductions for 69 of the most commonly used generic drugs in Canada in exchange for suspending open tender processes for five years. Under this deal, prices of these generic drugs were set to fall by between 25 per cent and 40 per cent as of April 2018.
The IQVIA prescription drug spending data used in the DSM ends on May 2018, shortly after the deal came into effect. As a result, it was necessary to adjust the prices in the data set for the 69 drugs subject to the deal.
Inflation
Over time, the prices of goods and services tend to increase to reflect, among other things, changes in production costs. Prescription drugs are no exception. The DSM can use separate inflation assumptions for the wholesale costs of brand name and generic drugs and pharmacy dispensing fees.
With respect to brand name drugs, the PMPRB patented drug price index indicates that the price of these drugs has been virtually flat since 2012. This is consistent with PMPRB regulation, which prohibits annual price increases for patented drugs to be significantly above increases in the consumer price index.Footnote xxiii
While no similar price index exists for generic drugs, the fact that many of the generics on the market can only be sold at a fixed percentage of their equivalent brand name drug price suggests that the price of generics will tend to move in line with the prices of brand name drugs.
For inflation, the DSM makes the following assumptions for both the status quo and national pharmacare scenarios:
- The DSM assumes no increase in wholesale prices for existing brand name and generic drugs over the projection period (see assumption for new drug entries below).Footnote xxiv Impacts of the 2018 pCPA deal on generic drug prices (see above box) are applied to generic drug prices.
- The DSM assumes that pharmacy dispensing fees (which are specific to each province) grow by 2 per cent each year (i.e., in line with general price inflation).
- The DSM assumes no change to mark-up rates over the projection period.
Demographics
Changing demographics—especially the age structure of the population—will, over time, impact the volume of prescriptions dispensed and the distribution of drug spending among primary payers.
Demographic projections used in the DSM to project future consumption of existing drugs are based on the medium growth scenario produced by Statistics Canada, which projects the structure of the population by age, sex, and province/territory from one year to the next by adding births and net migrants and subtracting deaths.Footnote xxv
In the DSM, demographic assumptions are applied by province and age-sex cohort. Population growth and the change in the age-sex structures of the Canadian population are expected to increase total prescription drug spending by an average of 1.4 per cent per year between 2017 and 2027.
- The DSM assumes that drug use within each cohort in each province will grow in line with the population of that cohort in that province, as projected in Statistics Canada’s medium-growth scenario.
Volume growth
Beyond demographic factors, the number of prescriptions that will be dispensed in any given year is affected by many other variables, including changes in the health status of the population (e.g., increases in the number of health problems that necessitate the use of prescription drugs), changes in prescription practices (e.g., changes in prescription size) and consumer habits (e.g., increasing health consciousness) and increases in the use of prescription drugs instead of other forms of therapy (e.g., surgery).
Although impact on volume is somewhat volatile from one year to the next, the PMPRB estimates that, from 2013 to 2017, volume growth not attributable to demographics has averaged between 0.6 per cent in private plans and 1.3 per cent in public plans.
- The DSM assumes an average annual increase in volume above the impact of demographic factors of 1 per cent per year (i.e., the approximate average of the volume growth not attributable to demographics observed in private plans (0.6 per cent) and public plans (1.3 per cent) from 2013 to 2017).
New drug entries
New drugs and therapies entering the market influence both the price and volume of prescription drugs. According to the PMPRBFootnote xxvi, new and generally higher-cost medicines (e.g., biologics, oncology medicines and hepatitis C treatments) introduced between 2013 and 2017 represented more than 25 per cent of total patented drug sales in 2017. Over that same period, it is estimated that the use of new drugs has, on average, increased annual spending of public and private plans by approximately 4.5 per cent. During the same period, it is estimated that the use of new drugs contributed between 3 and 6 per cent to spending growth for provincial public plans for which information was available. It is, however, important to note that significant uncertainty surrounds new drug entries and their likely impact on costs.
- Based on recent data, the DSM assumes that new drugs add 4.5 per cent per year to overall projected prescription drug spending over the projection period.
3.4 Ancillary public savings
National pharmacare would displace a certain amount of private and out of pocket spending. This could potentially decrease the cost to government of providing employee benefits to government employees and/or increase tax revenues (collectively referred to as “ancillary savings”). Ancillary savings would decrease the net incremental cost of national pharmacare to federal, provincial and territorial governments.
Ancillary savings associated with a decline in private plan spending
A decline in private plan spending could result in ancillary savings through either:
- Decreased spending on employee drug benefits for federal, provincial and territorial government employees;Footnote xxvii and/or
- Increased tax revenue that could follow automatically from a decline in tax exempt, employer-paid premiums for private health benefits.
The magnitude of ancillary savings for these two mechanisms depends on how employers use the savings associated with decreased costs of providing drug benefits. Broadly speaking, there are three possibilities for how employers could use savings:
- Savings may be reallocated to other non-taxable benefits for their employees, resulting in no new tax revenues and no decline in government employee benefits;
- Savings may be reallocated to wages or other taxable compensation, resulting automatically in increased tax revenues on this compensationFootnote xxviii but little to no savings on government employee compensation; and
- Employers may retain the savings, resulting in ancillary savings through reductions in spending on government employee benefits.
It is likely that there would be a mix of outcomes as employers and employees would negotiate an option that best meets their needs. Consultations suggest that it is likely that employee compensation would increase for many employees, either in the form of additional benefits or increased wages and salaries.
Ancillary savings associated with a decline in out of pocket spending
The Medical Expense Tax Credit (METC) provides tax relief for qualifying, out of pocket, above-average medical expenses, including prescription drugs and premiums paid for hospital and medical insurance. The Refundable Medical Expense Supplement (RMES) is a refundable tax credit available to individuals whose earnings from employment or self-employment meet or exceed a minimum threshold.
A decline in out of pocket drug expenses due to national pharmacare would be expected to reduce amounts claimed under METC and RMES. This would be expected to result in higher tax revenues for federal, provincial and territorial governments, regardless of how employers respond to national pharmacare (as discussed above).
Estimated total ancillary savings
A range of total ancillary savings to governments can be estimated based on the scenario that would generate the lowest ancillary savings—namely, where all employers enhance non-taxable benefits—and the scenario that would generate the highest ancillary savings to governments—namely, where all employers increase taxable compensation.
All figures for estimated total ancillary savings included below and in Chapter 6 are based on the mid-point of this range of potential total ancillary savings to federal and provincial governments.Footnote xxix
4 Results
4.1 Status quo projection
A status quo projection that assumes no change to the current regime of drug coverage provides a baseline against which to compare scenarios generated by the DSM for national pharmacare. That said, it is important to note that significant uncertainty surrounds status quo projections over the medium to longer term.
This uncertainty is relatively small for certain cost drivers such as the increase in the size of the population and changes in its age-sex structure. However, it is much higher for many others, with the impact of new drugs on total prescription drug spending being the most uncertain cost driver. To assess the uncertainty around future prescription drug spending, different but plausible assumptions can be used to generate low- and high-cost projections of the status quo. Table 6 describes the range of assumptions used for a number of key variables to generate low- and high-cost projections for the status quo.
| Status quo—low | Status quo—mid | Status quo—high | |
|---|---|---|---|
| Inflation (drug prices) |
0% | 0% | 2% |
| Inflation (pharmacy fees) |
2% | 2% | 2% |
| Demographics | Average overall growth due to demographics projected at 1.4% per year | ||
| Volume growth | 0.6% | 1.0% | 1.3% |
| New drug entries | 3.0% | 4.5% | 6.0% |
| Confidential rebates (Existing public plans) | 25% | 20% | 15% |
As an illustration of the impact of the uncertainty around status quo projections, Figure 22 shows the result of using the range of assumptions presented in Table 6 (above). The $2.3 billion difference in spending between the low- and high-cost status quo scenarios for 2018 increases to $28.8 billion by 2027, with total net prescription drug spendingFootnote xxxranging between $42.8 and $71.6 billion, reflecting the different average annual growth rates of 4.3 per cent and 9.8 per cent over the projection period.
In 2018, the use of different assumptions for confidential rebates (15 versus 25 per cent) and the assumed impact of new drugs entering the market on drug spending (3 versus 6 per cent per year) each explain about a third of the difference in prescription drug spending. However, by 2027, about two-thirds of the gap between the two scenarios is explained by different assumptions on the impact of new drugs and only very little by different assumptions for confidential rebates.
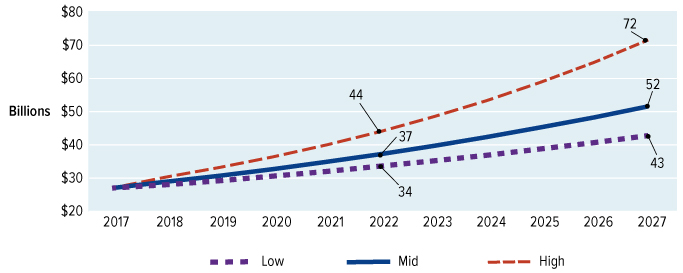
Figure 22: Text description
A line graph showing three projection scenarios (low, mid, high) for drug spending in Canada from 2017 to 2027
- In the low scenario, spending is projected to reach $33.6B in 2022 and $42.8B in 2027.
- In the mid (status quo) scenario, spending is projected to reach $37.2B in 2022 and $51.6B in 2027.
- In the high scenario, spending is projected to reach $44B in 2022 and $71.6B in 2027.
Source: Council’s calculations of data from IQVIA Solutions Canada, CIHI, PMPRB and Health Canada.
A consistent result in the status quo projections is that, all else being equal, public plans are expected to take on an increasing share of overall spending over the projection period. Results from the DSM suggest that, over the 10 years from 2017 to 2027, the share of existing public plans will rise from 45 per cent to 49 per cent of overall system spending on prescription drugs. This can be attributed to the impact of demographic factors on existing public plans, which are heavily weighted towards covering seniors. Based on Statistics Canada’s medium-growth scenario, the population of seniors is expected to grow at an average annual rate of 3.4 per cent from 2017 to 2027, compared to 0.9 per cent for the population overall. By contrast, those relying on private insurance or paying primarily out of pocket tend to belong to younger population cohorts, which are not expected to grow as quickly.
For clarity of presentation, this report presents scenarios for national pharmacare with reference to a status quo projection that lies between the low- and high-cost projections described above. This allows for an assessment of the potential impacts of national pharmacare by changing only cost drivers likely to be affected by the introduction of national pharmacare, while holding those that are unlikely to be affected constant. Under this status quo projection, total prescription drug spending (net of confidential rebates) is projected to increase by 6.3 per cent per year to reach $51.6 billion in 2027. Not including confidential rebates, total prescription drug spending is projected to increase by 6.7 per cent per year to reach $55.8 billion in 2027.
4.2 Assessing the cost of national pharmacare
While only presented with reference to a single status quo projection, the national pharmacare projection is in turn presented as a range, based on relatively more or less optimistic or pessimistic assumptions about the impact of national pharmacare on factors such as confidential rebates, prescription patterns and demand response. Given the importance of these factors, it can be expected that the implementation of national pharmacare will, over time, have an important impact on total prescription drug spending in Canada.
As Table 7 indicates, the DSM projects that total public spending in 2022 to cover essential medicines under national pharmacare would be about $7.6 billion (net of confidential rebates and copayments). To cover that amount, government spending would have to rise by about $4.1 billion relative to what it would otherwise have been under the status quo.Footnote xxxiOver time, as the formulary grows from the essential medicines list to the much more comprehensive RAMQ formulary, total public spending to cover prescription drugs covered by national pharmacare is projected to increase to about $38.5 billion (net of confidential rebates and copayments) and government spending would have to rise by about $18.1 billion relative to the status quo.
As discussed in section 3.4, this net incremental public spending would be partially offset by ancillary public savings. Based on the declines in private plan and out of pocket spending generated by the DSM, the midpoint of the range of potential ancillary public savings would be an estimated $0.6 billion in 2022, reducing the net incremental public cost in that year from $4.1 billion to $3.5 billion. In 2027, the midpoint of the range of potential ancillary public savings would be an estimated $2.8 billion, reducing the net incremental public cost from $18.1 billion to $15.3 billion.
While initially limited, the reductions in private plan and out of pocket prescription drug spending would become more significant by 2027. Even when assuming that individuals and private plans continue to spend on drugs that are not on the national formulary, the DSM projects that, relative to status quo projections, spending by private plans in 2027 would decrease by about $16.6 billion (from $19.8 billion to $3.2 billion) and out of pocket spending would decrease by about $6.4 billion (from $8.8 billion to $2.4 billion).
In terms of changes to overall prescription drug spending, the initial impact of pharmacare is projected to be relatively small as it would be limited to an essential medicines list. In 2022, total prescription drug spending is projected to decline from about $37.2 billion under the status quo to about $36.9 billion under national pharmacare, representing a $300 million reduction. However, as more and more of the cost saving measures, such as negotiating lower drug prices and extending them to more drugs, are implemented, national pharmacare will increasingly influence total prescription drug spending. In 2027, total prescription drug spending under national pharmacare is projected to be lower by about $4.8 billion relative to the status quo, declining from about $51.6 billion to about $46.8 billion.
Despite these projected reductions in system wide spending,s as access is improved, the total number of prescriptions is projected to increase by 10 million relative to the status quo scenario when national pharmacare is introduced 2022, and by 21 million by 2027.
Detailed provincial results are presented in Tables 8 and 9.
| ($ billions) | 2022 | 2027 | |||
|---|---|---|---|---|---|
| Status quo |
National pharmacare |
Status quo |
National pharmacare |
||
| Total prescription drug spending (net of confidential rebates) | |||||
| Total prescription drug spending | 37.2 | 36.9 (±0.3) |
51.6 | 46.8 (±2.5) |
|
| National pharmacare | Gross of copayments | N/A | 8.0 (±0.3) |
N/A | 40.0 (±2.5) |
| Net of copayments | N/A | 7.6 (±0.3) |
N/A | 38.5 (±2.5) |
|
| Other public plansFootnote * | Gross of copayments | 16.1 | 12.4 | 23.0 | 1.9 |
| Net of copaymentsFootnote ** | N/A | 12.5 | N/A | 2.6 | |
| Private plansFootnote * | Gross of copayments | 14.7 | 11.3 | 19.8 | 2.8 |
| Net of copaymentsFootnote ** | N/A | 11.4 | N/A | 3.2 | |
| Out of pocketFootnote * | Gross of copayments | 6.4 | 5.2 | 8.8 | 2.1 |
| Net of copaymentsFootnote ** | N/A | 5.3 | N/A | 2.4 | |
| Incremental public spending | |||||
| Gross incremental public spendingFootnote *** | N/A | 4.3 (±0.3) |
N/A | 18.8 (±2.5) |
|
| less national pharmacare copayments | N/A | 0.4 |
N/A | 1.4 |
|
| plus national pharmacare copayments on prescriptions previously covered by other public plansFootnote ** | N/A | 0.2 |
N/A | 0.7 |
|
| Net incremental public spending | N/A | 4.1 (±0.3) |
N/A | 18.1 (±2.5) |
|
| less ancillary public savings | N/A | 0.6 (±0.4) |
N/A | 2.8 (±2.0) |
|
| Net incremental public spending, after ancillary public savings | N/A | 3.5 (±0.7) |
N/A | 15.3 (±4.5) |
|
| Other impact | |||||
| Change in total prescription drug spending | N/A | -0.3 (±0.3) |
N/A | -4.8 (±2.5) |
|
| Change in private plan spending (net of copayments) | N/A | -3.2 | N/A | -16.6 | |
| Change in out of pocket spending (net of copayments) | N/A | -1.2 | N/A | -6.4 | |
| Total prescriptions (millions) | 806 | 816 | 941 | 962 | |
Source: Council's calculations of data from IQVIA Solutions Canada, CIHI, PMPRB and Health Canada. Note: Totals may not add due to rounding.
|
|||||
| ($ millions) | BC | AB | SK | MB | ON | QC | NB | NS | PE | NL | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|
| National Pharmacare | |||||||||||
| National Pharmacare | 881 (±32) |
820 (±29) |
242 (±9) |
252 (±10) |
2,692 (±98) |
2,558 (±91) |
198 (±7) |
227 (±8) |
37 (±1) |
142 (±5) |
8,050 (±290) |
| less Total Pharmacare Copayments | 34 (±0) |
29 (±0) |
9 (±0) |
11 (±0) |
124 (±1) |
174 (±2) |
7 (±0) |
7 (±0) |
1 (±0) |
5 (±0) |
402 (±3) |
| Total Cost of Pharmacare | 846 (±32) |
791 (±29) |
233 (±9) |
242 (±10) |
2,568 (±97) |
2,384 (±89) |
191 (±7) |
220 (±8) |
35 (±1) |
137 (±5) |
7,647 (±287) |
| Other Public Plans under Pharmacare | |||||||||||
| plus Other Public Plans | 926 | 1,053 | 349 | 298 | 5,387 | 3,763 | 202 | 239 | 25 | 118 | 12,360 |
| plus Other Public Plans share of Pharmacare CopaymentsFootnote * | 11 | 12 | 3 | 3 | 62 | 89 | 2 | 3 | 0 | 2 | 188 |
| Total Public Plan Spending under Pharmacare | 1,783 (±32) |
1,857 (±29) |
585 (±9) |
543 (±10) |
8,017 (±97) |
6,236 (±89) |
396 (±7) |
462 (±8) |
60 (±1) |
257 (±5) |
20,195 (±287) |
| less Status Quo Public Spending | 1,242 | 1,415 | 463 | 379 | 6,755 | 5,040 | 269 | 322 | 35 | 163 | 16,082 |
| Net Incremental Public SpendingFootnote ** | 542 (±32) |
441 (±29) |
122 (±9) |
164 (±10) |
1,262 (±97) |
1,196 (±89) |
127 (±7) |
140 (±8) |
25 (±1) |
94 (±5) |
4,113 (±287) |
| Private Plans under Pharmacare | |||||||||||
| Private Plans under Pharmacare | 1,001 | 1,319 | 196 | 254 | 4,675 | 2,746 | 380 | 432 | 59 | 245 | 11,307 |
| plus Private Plan share of Pharmacare Copayments | 12 | 12 | 3 | 4 | 40 | 45 | 3 | 3 | 1 | 2 | 125 |
| Total Private Plan spending under Pharmacare | 1,014 | 1,331 | 198 | 258 | 4,715 | 2,792 | 383 | 435 | 59 | 247 | 11,432 |
| less Status Quo Private Plan Spending | 1,344 | 1,716 | 271 | 359 | 5,853 | 3,662 | 496 | 563 | 79 | 328 | 14,671 |
| Change in Private Plan Spending | -331 | -385 | -72 | -100 | -1,138 | -871 | -113 | -128 | -20 | -81 | -3,239 |
| Out of pocket Spending under Pharmacare | |||||||||||
| Out of pocket spending under Pharmacare | 751 | 540 | 157 | 213 | 1,561 | 1,624 | 123 | 123 | 21 | 94 | 5,206 |
| plus Out of pocket share of Pharmacare Copayments | 11 | 5 | 3 | 4 | 21 | 39 | 1 | 1 | 0 | 1 | 87 |
| Total Out of pocket spending under Pharmacare | 763 | 545 | 159 | 217 | 1,582 | 1,663 | 124 | 124 | 21 | 95 | 5,293 |
| less Status Quo Out of pocket Spending | 987 | 642 | 212 | 288 | 1,837 | 2,046 | 146 | 147 | 28 | 115 | 6,449 |
| Change in Out of pocket Spending | -224 | -97 | -52 | -71 | -255 | -383 | -22 | -23 | -7 | -20 | -1,156 |
Source: Council’s calculations of data from IQVIA Solutions Canada, CIHI, PMPRB and Health Canada.
|
|||||||||||
| ($ millions) | BC | AB | SK | MB | ON | QC | NB | NS | PE | NL | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|
| National Pharmacare | |||||||||||
| National Pharmacare | 3,840 (±248) |
4,014 (±250) |
1,048 (±64) |
1,120 (±75) |
15,079 (±945) |
12,127 (±723) |
934 (±60) |
1,054 (±67) |
153 (±10) |
606 (±38) |
39,976 (±2,480) |
| less Total Pharmacare Copayments | 115 (±1) |
100 (±1) |
32 (±0) |
35 (±0) |
459 (±2) |
626 (±5) |
25 (±0) |
26 (±0) |
5 (±0) |
18 (±0) |
1,441 (±11) |
| Total Cost of Pharmacare | 3,725 (±247) |
3,914 (±249) |
1,016 (±64) |
1,085 (±74) |
14,620 (±943) |
11,502 (±719) |
909 (±60) |
1,028 (±67) |
149 (±10) |
588 (±38) |
38,535 (±2,469) |
| Other Public Plans under Pharmacare | |||||||||||
| plus Other Public Plans | 127 | 199 | 53 | 47 | 924 | 464 | 28 | 34 | 4 | 21 | 1,901 |
| plus Other Public Plans share of Pharmacare CopaymentsFootnote * | 40 | 44 | 12 | 9 | 242 | 328 | 9 | 11 | 1 | 7 | 703 |
| Total Public Plan Spending under Pharmacare | 3,893 (±247) |
4,157 (±249) |
1,081 (±64) |
1,142 (±74) |
15,785 (±943) |
12,293 (±719) |
947 (±60) |
1,073 (±67) |
154 (±10) |
616 (±38) |
41,139 (±2,469) |
| less Status Quo Public Spending | 1,738 | 2,117 | 652 | 535 | 9,745 | 7,171 | 368 | 448 | 50 | 217 | 23,041 |
| Net Incremental Public SpendingFootnote ** | 2,154 (±247) |
2,040 (±249) |
429 (±64) |
606 (±74) |
6,040 (±943) |
5,122 (±719) |
579 (±60) |
625 (±67) |
104 (±10) |
399 (±38) |
18,097 (±2,469) |
| Private Plans under Pharmacare | |||||||||||
| Private Plans under Pharmacare | 264 | 376 | 46 | 56 | 1,272 | 573 | 68 | 81 | 12 | 49 | 2,797 |
| plus Private Plan share of Pharmacare Copayments | 37 | 36 | 10 | 13 | 129 | 149 | 10 | 10 | 2 | 7 | 403 |
| Total Private Plan spending under Pharmacare | 301 | 413 | 56 | 69 | 1,401 | 721 | 78 | 92 | 14 | 56 | 3,200 |
| less Status Quo Private Plan Spending | 1,871 | 2,419 | 366 | 497 | 7,769 | 4,924 | 658 | 735 | 110 | 432 | 19,781 |
| Change in Private Plan Spending | -1,571 | -2,006 | -310 | -428 | -6,368 | -4,203 | -580 | -643 | -96 | -376 | -16,582 |
| Out of pocket Spending under Pharmacare | |||||||||||
| Out of pocket spending under Pharmacare | 280 | 273 | 57 | 68 | 690 | 645 | 44 | 45 | 7 | 33 | 2,142 |
| plus Out of pocket share of Pharmacare Copayments | 32 | 14 | 8 | 11 | 62 | 120 | 5 | 3 | 1 | 3 | 260 |
| Total Out of pocket spending under Pharmacare | 312 | 287 | 65 | 79 | 752 | 765 | 49 | 48 | 9 | 36 | 2,402 |
| less Status Quo Out of pocket Spending | 1,378 | 919 | 289 | 404 | 2,459 | 2,796 | 195 | 193 | 38 | 151 | 8,822 |
| Change in Out of pocket Spending | -1,066 | -631 | -223 | -325 | -1,707 | -2,031 | -146 | -145 | -30 | -115 | -6,420 |
Source: Council’s calculations of data from IQVIA Solutions Canada, CIHI, PMPRB and Health Canada. Note: Totals may not add due to rounding.
|
|||||||||||
Annex 7: Other pharmacare models considered
Introduction
While the council agreed on a universal single-payer, public model for national pharmacare as the preferred model for Canada, we also explored different approaches for arriving at that end point. In particular, we considered whether existing models in Canada’s current mixed system of public and private drug insurance could be scaled up across the country as an interim step en route to a single-payer model. The two approaches we focused our deliberations on were:
- Standardizing public catastrophic drug coverage across Canada; and
- Regulating the existing private insurance sector nationwide in a mandatory multi-payer insurance model, similar to the system in place in Quebec.
This annex provides additional information and considerations about these two models.
Catastrophic drug coverage model
Catastrophic coverage protects people from very high prescription drug expenses. When an individual’s drug costs exceed a certain share of their income, these types of drug plans absorb all or a portion of the costs over a certain threshold (called a deductible). Individuals are typically required to pay the full cost of their prescription drugs up to their deductible, unless they have private insurance. After this, the drug plan pays for all or a portion of their prescription drug costs. Because eligibility for these programs is tied to income, individuals must generally register for these programs and provide consent for the government to receive their income tax information from the Canada Revenue Agency.
While catastrophic coverage is the most common model of public drug coverage found in Canada, it is not used in any of the international high-performing health systems that Canada would consider as peer countries. While most provinces offer this form of drug coverage to their residents, jurisdictions apply different rules concerning the deductibles, coinsurance or copayments and contribution limits. For example, some provinces calculate deductibles based on total income, while others use taxable income. Some adjust for household size (e.g., number of children). Some use a progressive deductible structure to further target public support to where the need is greatest (i.e., higher income earners pay greater deductibles as a percentage of income, and lower income earners have either no or lower deductibles).
The council considered how national pharmacare could harmonize public coverage under a catastrophic coverage model by establishing a common deductible threshold based on a percentage of income that no public plan could exceed. This national threshold could then be lowered over time in pursuit of the goal of achieving a universal, single-payer, public system.
Approaches to catastrophic drug coverage
There are different ways to design a catastrophic program. Deductibles can be calculated either as a percentage of income (e.g., 4 per cent) or as a fixed dollar amount (e.g., $5,000). The income-based approach is progressive, meaning it accounts for differences in ability to pay and targets public funding to where the need is greatest—those with high drug costs relative to income. For example, with a deductible level set at 4 per cent of family income, a family earning $30,000 would have to pay a deductible of $1,200 before public coverage kicks in, while a family earning $50,000 would have to pay a deductible of $2,000.
Alternatively, a national threshold could be established as a fixed dollar amount (e.g., $5,000 or $10,000 per household). While this approach is simpler to understand and doesn’t require income-testing, it is not as equitable. For example, under this approach, a family earning $30,000 annually would pay the same deductible as another family earning over $100,000.
A key challenge for designing a catastrophic drug plan is determining the right threshold for the deductible. Thresholds can be the same for everyone (as in the example above of 4 per cent) or they can vary by income, so that higher income families face a higher threshold (e.g., 10 per cent) than lower income families (e.g., 1 per cent). A higher threshold is less expensive for governments, but provides less protection for families. Provinces have made a wide variety of choices on this front; current thresholds vary from less than 1 to 20 per cent. Although there is no perfect solution, academics generally agree that thresholds above 2 to 3 per cent are likely to present significant cost barriers, particularly for lower income families.
Another design choice is whether costs covered by private insurance should count toward the deductible. Some programs exclude such third-party payments, so that public funds are more targeted to those without any drug coverage. Other programs include payments made on a patient’s behalf (e.g., by private insurance). This can provide significant relief to families with private insurance but perpetuates the current inequities between those with and without private insurance.
Many catastrophic drug plans have exemptions, so that certain individuals do not have to pay the deductible in part or in full. These exemptions can be based on demographics like age, on income levels or based on other criteria. Most provincial drug plans have exemptions for low-income residents who receive social assistance payments. Some provinces exempt families earning less than a defined income threshold, for example $30,000. Deductibles can also be applied differentially to individuals and families in order to account for the added costs of caring for dependants. For example, exemptions could be provided for individuals earning an annual income below $20,000 and for families with a household income of $40,000 or less. This means families would not begin paying deductibles until they make more than $40,000 annually, compared to $20,000 for individuals.
While income-based exemptions are commonly used in the provision of social benefits in Canada, they also run the risk of creating significant discontinuities between eligible and non-eligible income brackets—sometimes referred to as “income cliffs.” Income cliffs can create perverse incentives by penalizing individuals for improving their financial prospects, such as by obtaining a new job or going off social assistance, because doing so will mean they must begin paying a deductible before receiving the coverage they rely on.
Exemptions could also be provided for specific drugs instead of income levels. A ‘hybrid’ approach to catastrophic drug coverage could remove deductibles for all drugs included on an essential medicines list and apply income-tested deductibles for all other drugs included in the national formulary.
Statutory multi-payer model
The council also considered whether implementation of a statutory multi-payer insurance approach for prescription drugs—where residents are required by law to buy third-party insurance that meets national standards—could work across Canada. A number of OECD countries, including France, Germany and the Netherlands, use this approach to provide universal health insurance (including drug coverage) to their residents. These systems are typically financed through payroll taxes and employee contributions (premiums) which are collected centrally and then re-distributed to not-for-profit third-party insurers via an annual subsidy based on the number and health status of their plan members.
Here in Canada, Quebec is the only jurisdiction that offers universal drug coverage to its residents and it does so using a statutory insurance model. Starting in 1997, the province made it mandatory for all residents to have drug coverage either through a private plan (usually sponsored by their employer or professional association) or through the government-run public plan. Employers that provide health benefits to their employees are required to provide drug coverage that meets or exceeds the level of coverage provided by the province’s public drug plan and employees who are eligible for the plan are required to enrol in it. Private plans must cover at minimum all the drugs included on the public plan formulary.
Residents who do not have access to an employment-related plan are required to enrol in the provincial public drug plan. The public plan charges an annual premium of up to $616 for each adult in a household, regardless of whether the individual purchases prescription drugs. Premiums are calculated based on net family income and are paid through tax returns. Certain populations, such as low-income seniors and social assistance recipients, are not required to pay premiums.
Premiums charged to members of private drug plans are not income-based and are not subject to the $616 maximum. Most Quebecers are also required to pay a share of their drug costs at the pharmacy. The public plan involves a monthly deductible of $19.90 per person plus coinsurance of 34.9 per cent of the total cost of eligible prescriptions, up to a monthly maximum of $90.58 per person ($1,087/year). These monthly maximums apply to private plans as well.
Quebec’s public and private insurance systems operate in parallel, each with separate and distinct sources of funding. Unlike the European systems mentioned above, funding is not collected centrally by government and re-distributed. In 2017, plan member premiums and cost sharing covered 45 per cent of the public plan’s total costs, with the remaining 55 per cent financed through general taxation. Private drug plans receive no government funding and are financed entirely through employer and employee contributions.
Conclusion
The council deliberated the merits of these two models as stepping stones toward the creation of a universal, single-payer, public pharmacare plan. In the final analysis, the council felt that any advantages presented by these models—either because they already exist in some form in Canada or because they might initially entail a lower level of public investment—were outweighed by the longer-term efficiency and sustainability of a single-payer model.Annex 8: Sex- and gender-based analysis
Over the course of its mandate, the council considered the influence that sex and gender, as well as other identity factors such as age, race and income status, can have on a person’s access to health care and their ability to effectively maintain and improve their health.
To support its work, the council engaged Dr. Cara Tannenbaum, Scientific Director of the Institute of Gender and Health of the Canadian Institutes of Health Research, to perform a sex- and gender-based analysis plus (SGBA+) to examine how sex, gender and other intersecting identity factors could impact the implementation of national pharmacare. The resulting report provided eight evidence-based SGBA+ considerations related to key elements of national pharmacare, including eligibility, patient cost sharing, formulary options and financing.Footnote xxxii
SGBA+
Considerations for national pharmacare
National formulary
The national formulary must provide efficacious, safe and appropriate drug options for:
- Females, males, and persons of diverse gender;
- Individuals across the lifespan, including seniors and pediatric populations; and
- Diverse racialized groups.
Data use and reporting
- Information about drug efficacy, safety and toxicity by sex, age and race for the national formulary must be transparently reported on a publicly-accessible website.
- Selection of drugs for the national formulary and regular review through post-marketing surveillance must be undertaken by committees that include SGBA+ expertise.
Coverage
- A single-payer universal pharmacare program is the most equitable option. If a public/private multi-payer program is implemented, it must include ongoing analysis in real-time to identify and mitigate inequities.
Costs to patients/individuals
- To the extent that data is available, all financial analyses to develop recommendations about how to fund national pharmacare must apply an SGBA+ lens.
- Exemptions should be considered for certain subgroups of at-risk people.
The council took these SGBA+ considerations into account when developing its plan for a universal, single-payer, public pharmacare system. Under the council’s plan, all residents of Canada with a valid health card would be eligible for coverage under national pharmacare. By covering everyone equally and consistently across Canada, the council believes a universal, single-payer, public pharmacare plan would best address the needs of diverse types of people and reduce existing inequities in Canada’s current patchwork of public and private drug coverage.
The council also heard countless stories of how patient cost sharing requirements, such as deductibles and copayments, can be unaffordable and prevent individuals from taking the appropriate medication. Overall, 3 million Canadians report not being able to afford their prescription drugs.Footnote xxxiii Demographic groups reporting higher rates of cost-related non-adherence include women, low-income Canadians and those without insurance.Footnote xxxiv
A 2015 Angus Reid Survey found that 23 per cent of Canadians reported that, in the previous year, they or someone else in their household did not take their prescription medications as prescribed, if at all, because of their cost. Another survey conducted by the Commonwealth Fund in 2016 found that 10.2 per cent of Canadian respondents aged 18 and older did not, in the previous year, fill their prescriptions or skipped doses of medications due to cost.
Estimates suggest that about 40 per cent of people who report cost barriers to accessing their medications also report not having access to public or private prescription drug coverage. Currently, approximately 60 per cent of Canadians (with roughly equal percentages of women and men) are enrolled in a private drug insurance plan. Approximately 5 to 7 million Canadians do not have access to either private prescription drug coverage or comprehensive public coverage. Roughly 50 per cent of these Canadians live in households with annual incomes of $40,000 or less.Footnote xxxv
The council’s national pharmacare plan would address the issueof cost-related non-adherence by limiting copayments and annual out of pocket payments to ensure that all individuals can have access to the medicines they need at a cost they can afford. Moreover, the council has recommended that people with very low incomes, such as people receiving social assistance, government disability benefits or the federal Guaranteed Income Supplement, be exempt from copayments and this measure should help reduce barriers for Canadians.
As well, the council supports financing pharmacare through Canada’s general revenues, as it would ensure a fair and equitable distribution of costs. This would ensure that those who are most able to pay contribute their fair share, while protecting those least able to pay. It would also ensure that those whose needs are higher are not unfairly disadvantaged by their health status.
Drug needs differ based on many different demographic characteristics, including sex, gender identity, sexual orientation, age, race and many others. For example, the types of prescription contraceptive agents that are included in (or excluded from) the national formulary will have important implications for women. In addition, people of different age groups will need different types, and doses, of therapies, and the extent to which these are included in (or excluded from) the national formulary will have important implications for children, adults and seniors. The intersection of all of these characteristics is also important—for example, senior women may have very different drug needs than young boys.
Drug Access Barriers for Transgender People
Transgender people can have unique prescription needs. Currently, prescribing hormone replacement therapy to transgender individuals with the goal of changing their appearance is not an approved or recognized use of these drugs. This can create barriers to access and make it difficult for an individual to live in their felt gender, which can in turn lead to mental health issues and the need for more intensive health care services.
Scientific evidence has shown that a person’s risk of developing certain diseases, and how well they respond to medication is influenced by sex, race and age Genetic differences can impact the way drugs are metabolized and can lead to certain treatments being ineffective or unsafe for particular groups. Historically, clinical trials tended to be conducted on men only, putting other identity groups at risk as findings derived from such trials were then generalized.Footnote xxxvi
The council’s plan would respond to this by ensuring national pharmacare covers a comprehensive, evidence-based formulary, with safe and appropriate options to meet the needs of Canada’s diverse population, including children, seniors, persons with disabilities, Indigenous peoples, other racial and ethnic minorities and the lesbian, gay, bisexual, transgender, queer, intersex and two-spirit community. Once it is fully implemented, the national formulary will provide an appropriate range of treatment choice across the full spectrum of care—from common conditions largely seen in primary care to medically complex conditions seen in specialist care settings, taking both physical and mental health into consideration. Covering the full spectrum of care, including complex conditions, would benefit many Canadians, and specifically children. According to the Canadian Organization for Rare Disorders, approximately 1 in 12 Canadians are affected by a rare disease, of which two-thirds are children.Footnote xxxvii
In addition to the national formulary, a number of the other measures the council is recommending as part of the implementation of national pharmacare will address the needs of diverse groups of people, including a national strategy on appropriate prescribing and use of drugs and improved data collection.
A recent report found that nearly 2 million Canadian seniors regularly take at least one inappropriate medication, which can lead to harms such as falls, memory problems, hospitalizations and even death. To reduce this risk, the council proposes a national strategy on appropriate prescribing to promote more responsible use of prescription drugs. The strategy would complement the development of the evidence-based national formulary and support appropriate prescribing through measures that would be designed to reflect the unique needs of diverse groups of people. For example, the national formulary could be complemented by the development of age- or gender-specific prescribing guidance for health care professionals.
The implementation of national pharmacare also presents an opportunity to enhance data collection and reporting to improve health care decision-making and reduce health inequities. The development of complete drug data records—from information on prescribing, dispensing and processing of drug claims, to whether patients’ health improved or they had bad side effects—would provide patients and their care teams with essential information for safe and effective prescribing. It will be important to ensure drug data can be linked to data on age, sex, gender and race in order to make better policy decisions that support Canada’s diversity.