The state of virtual care in Canada as of wave three of the COVID-19 pandemic: An early diagnostic and policy recommendations

Download the alternative format
(PDF format, 3,411 Kb, 88 pages)
- Organization: Health Canada
- Date published: June 29, 2021
- Will Falk BSc., MPPM
- June 29, 2021
Health Canada is the federal department responsible for helping the people of Canada maintain and improve their health. Health Canada is committed to improving the lives of all of Canada's people and to making this country's population among the healthiest in the world as measured by longevity, lifestyle and effective use of the public health care system.
Table of Contents
- Foreword
- Introduction
- Section 1: What happened? Four different perspectives
- Section 2: Provincial/territorial, private sector, and international review
- Section 3: Virtual care policy for Canadians: Six pillars framework
- Section 4: Recommendations, implementation issues and governance
- Table 1: Summary of recommendations
- Acronyms
- Glossary
- Acknowledgements
- Endnotes
- References
Foreword
Jo Voisin and Sandra Cascadden Co-Chairs
FPT Virtual Care Table By e-mail
June 29th, 2021
Dear Jo and Sandra, Attached please find my report to the Federal Provincial Territorial Virtual Care Table: The State of Virtual Care in Canada as of Wave Three of the COVID-19 Pandemic. Congratulations on the excellent discussion amongst the more than 80 participants at the FPT virtual care summit last week. I was so pleased to see them taking on the tough issues for Canadians
This report is an early diagnostique with policy recommendations. It is written at a time in our history when many changes to the health system are still in progress. As such, I ask that you accept it as a work in progress and I appreciated having the ideas improved upon by the FPT Virtual Care Table and others at the summit as well as by individual policy makers who take and improve the recommendations in their jurisdictions.
The report is longer than I had planned. This is in part because of the four different perspectives that emerged as clinicians and administrators struggle with the huge move to virtual care during the pandemic. I have tried to centre the report around the broad agreement that while change was forced upon us by the pandemic it was, in many cases, long overdue.
The Policy recommendations under the six pillars fall into several broad categories that I summarize as follows:
- Care is Care. Virtual care is no longer an adjunct therapy; it is a core part of our publicly- funded health delivery system.
- Key health information components—diagnostic test results, prescriptions, consults, and referrals— should always be created in a usable digital format. When requested by or on behalf of a patient, hospital and physician records, should be provided on demand in a usable digital format as of April 1, 2023.
- Payment policies should not favour one modality of care over another, except when warranted for clinical reasons. Physical, video, phone, and messaging modalities (and other future modalities) should be available to providers and patients at their choice.
- Governments must switch their mindset from paying for particular technologies to paying for desired outcomes and services (allowing providers and patients to make technology choices within a standards framework).
- Licensure needs to be modernized. A national licensure framework agreement should be the goal. Several immediate changes must be made to ensure continuity of care and availability of the best culturally appropriate care.
- A new approach to clinical change management and medical education is needed to ensure that we keep the best of what we have learned and gather new data to further improve practice standards.
- Equity of access must be a priority. The phone has been a critical modality of care during the current crisis and should not be blocked. Digital literacy is clearly higher for the telephone. Technology infrastructure in many parts of the country continue to demand improvement to improve equitable access. This needs to be supported by expanded IT support and digital literacy
- User experience needs to be a priority for system development and adoption. This is true for both patients and clinicians. Good technology solutions have higher usage levels, good net promoter scores, and well-reported and widely comparable experience and outcome measures.
There is one more recommendation which came directly from reviewers and their comments over the past several weeks who noted how important the culture change of the past fifteen months has been. I will add this as Recommendation Zero.
Recommendation 0: Keep the culture change of the past fifteen months for as long as we can.
The "we can get it done" attitude that arose around the use of virtual care in the pandemic has been remarkable. Problems that had blocked progress for years evaporated. The public and private sectors collaborated and found new solutions. Stuff got done. There's a quote attributed to Harvard management guru Peter Drucker that I love: "Culture eats strategy for breakfast." The essence is that all the planning in the world doesn't make up for a "can-do" culture.
I recognize that some reversion to established behaviour patterns will happen. Both organized medicine and government are inherently conservative and slow to change. We should continue to ask questions and challenge the pre-2020 status quo. Let's keep the needs of patients and providers central to our technology choices and keep the best part of our new culture. Such a modern culture focused on user experience can be part of a revitalized commitment to Canada's public health care system.
My thanks to the two of you, to the over 100 people who gave their time for interviewees, to the members of the Expert Working Group and others who provided comments on earlier drafts, and to the team at Health Canada for their support during this project. During the course of this work, I have been supported by staff and clinicians at the Centre for Digital Health Evaluation; the project team of Michael Cheung, Leah Kelley, Karen Palmer, and Denise Zarn have made working on this project a lot of fun and they have each contributed majorly to its success. The errors and omissions are mine.
Sincerely,
Will Falk
East Garafraxa, ON

Figure 1 - Text Description
Six policy pillars, resting on three policy foundations.
- Six policy pillars
- Patient and Community Centered Approaches
- Equity in Access
- Provider Remuneration/ Incentive Structures
- Appropriateness, Safety, and Quality of care
- Provider Change Management
- Licensure
- Policy Foundations
- Privacy and Security
- Data Standards and Integration
- Technology (Procurement, Standards, and Operation)
Introduction
This “diagnostique” offers a summary of the state of virtual care in Canada as of May 2021. It relies on more than 100 key informant interviews, grey literature from the past 12 months, and the few relevant peer-reviewed scientific publications. We rely on the best available information at this time to summarize the impact of the COVID-19 pandemic on virtual care across the country. Organized in four sections, we assess policy options within the Six Pillar Framework, and make recommendations to the provinces, territories, and federal government.
Section 1. What happened?: Four different perspectives presents four competing narratives on what happened with virtual care since February of 2020. Competing, because interviews demonstrated to us that our collective interpretation of what has taken place is still being debated. Clinicians, patients, and policy makers are struggling with the huge changes and forced modernization of our health care systems.
Section 2. Provincial/territorial, private sector, and international reviews recapitulates some of the key findings from our preliminary report (March 1, 2021) with a brief re-evaluation of jurisdictional and private sector responses to the changed environment. The full preliminary report slide deck (with updates) is available in the Appendices.
Section 3. Six policy pillars: options and recommendations discusses the six policy pillars and makes policy recommendations for each pillar. These recommendations range from higher level principles to practical, foundational items needed to advance implementation of virtual care.
Section 4. Recommendations, implementation issues and governance reiterates the recommendations and addresses several governance issues to attempt to set the framework for an agreed national implementation plan.
Section 1. What happened?: Four different perspectives

Figure 2 - Text Description
Four competing perspectives on what happened to virtual care in 2020:
- Emergency Life Raft
- Low Rules Environment
- A Stress Test of our Existing (Pilot) Systems
- A Shift to Consumer-Oriented Health Care
In March 2020, the COVID-19 pandemic upended Canada’s health care systems. The direct impact of the pandemic has been widely analyzed and will continue to evolve. This diagnostique covers the abrupt switch to virtual care that arose due to the high costs of physical contact (CoPC) between health care providers and patients. CoPC weights the benefits of care against the “cost of contact” from any physical interaction with the health care system.Footnote 1 The shift was dramatic and sharp. In just one month, virtual care went from 2-3% of ambulatory care visits to more than two-thirds.
This major shift in clinical practice can be viewed in several ways, with different observations and conclusions drawn depending on one’s viewpoint. This section describes four competing perspectives that emerged from over 80 key informant interviews—with patients, clinicians, system administrators, and policy makers—conducted between February and April of 2021. Each of these narratives has some truth to it and the intent of this section is to present them in a productive and engaging way that describes what has happened in the past 14 months to our health care system.
Perspective one: Emergency life raft
Many observers started Wave 1 with the perspective that virtual care was a temporary expedient. They viewed virtual care as an emergency measure necessary due to high CoPC. They presumed virtual care would stop as it had during earlier pandemics. Indeed, some provinces reinstituted the same billing codes used during earlier epidemics almost 20 years prior. These codes cover video, phone, and even some secure messaging. Virtual care usage was very high during Wave 1. Usage during the first quarter of 2020/21 across all ambulatory visits in Ontario was 77%.Footnote 2 In many provinces, we also saw a huge expansion of primary care call lines (e.g., 811, telehealth) and the rise of virtual Emergency Departments. The private sector also stepped in and offered expanded, and in some cases free, services (e.g., Dialogue).
But was this all temporary? Through the summer of 2020 we saw virtual care levels start dropping in Canada and elsewhere. The assumption was that levels would continue to decline back down to something more “normal”, as in closer to pre-pandemic. Even in the summer/pre Wave 2 fall, when virtual use plateaued around 40% at many centres (according to interviews and Infoway dataFootnote 3), this was still far above pre-pandemic levels despite more in-person care options. When Wave 2 hit, the rate of virtual care climbed back up. Anecdotally, it appears that sometime in late 2020, primary and specialty practices started making more permanent changes to their practice patterns.
For some visits, phone calls absolutely make sense for both the patient and the provider: they save the patient money and time, and the provider can see more patients in a day. All that was needed by the system was to enable this through appropriate reimbursement. IT and logistical systems failed, sometimes spectacularly (more on this later). New, better IT systems were introduced by several major vendors. Several provinces opened up codes to allow use of commercial video products such as Zoom and Teams. Volumes started growing and normalizing on the existing services that worked well. Wave 3 has hit at the time of this writing and it is becoming clear that more and more practices are now making adjustments to permanently include virtual care in their workflow.
Early academic reports are showing that many people like virtual care. Even when they have the choice of in-person care, some appear to prefer virtual.Footnote 4,Footnote 5 Providers are mixed as to exactly how to monitor and assure quality of care and appropriateness,Footnote 6,Footnote 7 but seem to mostly embrace virtual care. 81% of eVisits through Kaiser Permanente Northern California required no follow up care.Footnote 8 This speaks to the frequency of virtual care as a one-and-done modality, though it may also reflect self-selection by those who choose these modalities. We anticipate much more evaluation of these questions. Governments have also been watching the polling data provided by InfowayFootnote 5 and others. While some officials still may be looking at how to “roll back the fee codes”, this is becoming increasingly unlikely to be supported by Canadians.
Candidly, I was in this rollback camp a year ago. I said last summer to a Queen’s University MBA panel that I expected virtual care to stabilize somewhere around 20-40%. Like many others, I no longer believe this. Virtual care is no longer an adjunct therapy; it is now a core part of health care delivery.
Recommendation 1 Care is care. Virtual care should remain a publicly-funded service that can be used by clinicians when they, in consultation with their patients, judge it appropriate.
Recommendation 2: All care modalities need to be continually evaluated against the Quadruple Aim to ensure they are enhancing patient experience, improving population health, reducing cost, and improving the work life of health care providers (Bodenheimer and Sinsky, 2014) .Footnote 9
Perspective two: Low rules environment
This perspective views virtual care during COVID-19 as a great experiment in changing the rules. Rules that had existed, mis-applied standards, arbitrary payment, and historical practices were all subject to a fresh re-examination. A zero-based analysis interrogates every function within an organization for its needs and costs. We should now include high CoPC in such an analysis as an important variable for both providers and patients. For example, key informants spoke about privacy and security “practices” that were not supported by legislation or regulation. Rather, they had arisen through years of overly conservative interpretation, misidentification of whose rights are being protected, and even misunderstanding of laws and regulations. They also pointed to the risk averse approach of many health system actors to virtual care, resulting in a default to physical care services even when virtual care was known to be a good (sometimes better) option that promotes one or more aspects of the Quadruple Aim.
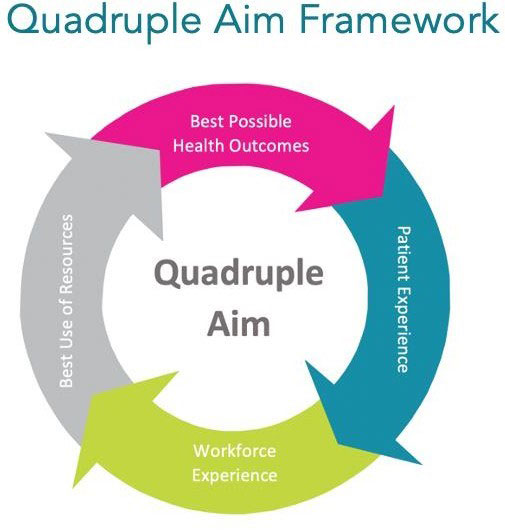
Figure 3 - Text Description
Quadruple Aim is an internationally recognized framework for an effective health system consisting of four parts:
- Best Possible Health Outcomes
- Patient Experience
- Workforce Experience
- Best Use of Resources
* Image from Women’s College Hospital: https://www.womenscollegehospital.ca/about-wch/accountability/performance-report-card/.
There is more than a hint from the people who hold this viewpoint that many of the rules were either: a) completely unnecessary; b) used by software vendors to protect market positions and to lock in their client base; c) used by service providers to protect outmoded and inefficient guild- based production models; d) used by government officials managing costs in a “penny-wise pound-foolish” fashion; and/or e) used by government agencies to further their own survival (i.e., budget allocation) in a model of regulation-controlled competition. There is some truth in these explanations. In some cases, that truth has been made painfully apparent during the pandemic.
Experimentation with new modalities of care was forced in a manner that Christensen et al. refer to as “disruptive innovation”.Footnote 10 A new “measure of performance” was introduced into our health care system which resulted in a switch to a new “basis for competition”. Specifically, the risk of physical presence made it necessary to change how we deliver clinical care. This happened in the past year with the higher CoPC in many specialties and for most primary care.Footnote 1 As the pandemic progressed, more and more producers “retooled” to better serve their patients. This process was greatly hastened in some (but not all) specialties by very dramatic declines in providers’ incomes. Those who experimented with practical solutions that involved virtual care did better for the health of their patients and the health of their practices.
As we “return to normal” the question from a low-rules perspective is how much do we add back the old rules and the old reimbursement system?
Recommendation 3: A practical review of privacy and security interpretations and administrative rules should be undertaken in the context of the learnings from the past year. This should be a fresh evaluation specifically designed to reduce overly risk averse and impractical interpretations.
Perspective three: A stress test of our existing (pilot) systems
This perspective is a bit more critical of past decisions. It takes the perspective that for twenty years, and with the best of intentions, we have built telemedicine as an adjunct system. Several core beliefs informed our system architecture for virtual care and digital health systems. These included: a) a technical architecture borrowed from the banking industry in the 2000s; b) centralization of specifications and networks; c) virtual care being defined as video; d) reliance on the fax machine as a reserve technology; and e) the need to prove technology through pilots before deploying at scale rather than allowing choice among several systems. We have spent billions building digital technology to enable virtual health care systems. We usually did it through a central planning bureaucracy at the regional and provincial level.
The pandemic acted as a huge stress test of all the IT systems we had built. Some have performed well and have thus grown substantially to meet demand. They are now deployed at scale and probably offer valuable lessons going forward. There were many systems that did not scale well during the pandemic. Sometimes, they were set up inside of buildings at fixed locations which became less accessible and less safe due to CoPC during lockdowns (e.g., classic telemedicine). In other cases, they were just old or outdated technology, like fax machines or legacy software systems. The fax machine suffered from both, experiencing catastrophic failure for all or part of the pandemic. For example, our key informants estimate that 15% of faxes were failing on one major platform during a month in the middle of the pandemic. Some provinces had to resort to calling long-term care (LTC) homes for infection and death reports because the information systems seized up and were too slow to be useful.
It should surprise no one that some systems failed. Many of our information systems were the original systems funded over a decade ago by the PTs with help from Infoway. Often, they have only seen modest usage levels and have struggled to get appropriate upgrades to the technology. Upgrading systems is always difficult and requires a disciplined and organized approach. This has been complicated in the case of virtual care because of the huge advances in available technology while usage remained below 3%. When we jumped to virtual care representing the majority of visits, many of our IT systems failed to scale.
The intention here is not to embarrass agencies or vendors but each PT should assess how their own critical systems functioned over the past year.
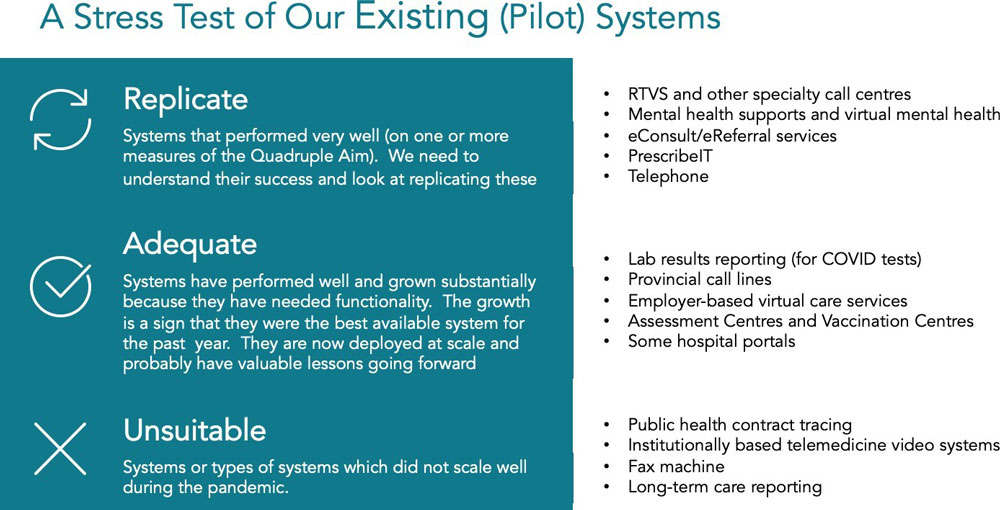
Figure 4 - Text Description
Assess existing systems after the COVID stress test. IT systems fall into three categories - those that should be replicated, those that are adequate, and those that are unsuitable.
- Replicate: Systems that performed very well (on one or more measures of the Quadruple Aim). We need to understand their success and look at replicating these.
- RTVS and other specialty call centres
- Mental health supports and virtual mental health
- eConsult/eReferral services
- PrescribeIT
- Telephone
- Adequate: Systems have performed well and grown substantially because they have needed functionality. The growth is a sign that they were the best available system for the past year. They are now deployed at scale and probably have valuable lessons going forward.
- Lab results reporting (for COVID tests)
- Provincial call lines
- Employer-based virtual care services
- Assessment Centres and Vaccination Centres
- Some hospital portals
- Unsuitable: Systems or types of systems which did not scale well during the pandemic.
- Public health contract tracing
- Institutionally based telemedicine video systems
- Fax machine
- Long-term care reporting
In many cases these reviews have already been started and in some cases are near completion (e.g., Ontario and Nova Scotia). A distillation of learnings for each jurisdiction might include a letter grade for each major system based on existing publicly available measures.
This “stock taking” of IT system performance also presents an opportunity to create a baseline for Patient Reported Experience Measures (PREMS) and other usability and usage statistics for virtual care for the future. Infoway has already begun this process. Usage and usability need to be widely and transparently reported as virtual care becomes a routine part of services.
Our crisis response was appropriate. We freed clinicians to choose the best available tools and actively encouraged the use of more modern technology. They flocked to non-industry tools and to newly available private offerings. There was no structured change management. Centralized specification and slow purchasing were not possible. Decisions were fast-tracked and common sense was used as we abandoned some unscalable systems and started using others. Some physicians returned to their role as active buyers of technology and moved quickly to pick better systems for their practices. Many found this experience liberating and commented with some version of: “We have made more progress in the last ten months than the prior ten years”.
We need to hold on to this practical can-do attitude as we move forward. Too often, our large procurement processes have taken the clinician and patient out of the decision-making process and have not produced timely decisions. Those who hold this perspective believe that the pandemic forced usability, and patient/clinician experience into purchase and usage decisions.
In this regard the biggest surprise was the dominance of the humble telephone. Government-built video care systems (i.e., telemedicine) in many provinces did not perform well. Telemedicine systems were located in a few fixed clinics and hospitals, so providers and patients were required to travel to buildings equipped with the technology for consultations. High CoPC made these buildings hard to reach and the user experience (UX) was not as good. Many key informants pointed out that the telephone provided strong basic access for Canadians. This experience was reflected in the NHS, Australia, and many other nations.
“The default model, which involved, on average, $100 out-of-pocket costs to patients to attend physically, the CoPC, and office logistics on the clinician side never really made the most sense for some tasks. And frankly, video was also too cumbersome and didn’t make sense for those tasks which is why people weren’t using it despite a reimbursement model. This, to me, is proof positive that the barriers to some aspects of virtual came down to ONE thing…and one thing only…appropriate reimbursement for the phone.”
- Specialist Physician
Recommendation 4: Each PT should urgently conduct an objective inventory of IT systems and their pandemic performance. Develop replacements where appropriate. Each PT will have a development plan across existing and planned information systems.
Recommendation 5: There should be transparent reporting on usage levels and on user experience (UX) for all existing virtual care systems (probably for all digital systems). Patient and provider feedback should be readily available and transparent to all users.
Recommendation 6: PREMS for UX should incorporate non-health software measures (e.g., Net Promoter Score, Apps Store ratings) that are standard across all industries to allow comparability and to avoid the creation of health care-only services that are substandard.
Recommendation 7: Keep the telephone as a permissible modality under the virtual billing codes. The value of video over phone has been overinflated. Phone was foundational for equity and access.
Perspective four: A shift to consumer-oriented health care
Some observers see the pandemic as having unleashed consumer forces in health care. More modern virtual care technology has been a big winner in the pandemic. Those who view themselves as health care “consumers” or “clients” have demanded it. They switched, en masse, to good tech where it is available in the publicly-funded system and to privately-funded technology where it wasn’t.
Capital markets looked at the failure of government-sponsored virtual care technology and stepped up with billions of dollars of capital investments (Figure 5). Maple, Dialogue, Well, Babylon, Teladoc, PointClickCare, AlayaCare, ThinkReseach, and MindBeacon have now joined Loblaw and TELUS as major providers of virtual care services. We also have non-health care entrants at the table from multinationals like Zoom, Microsoft, and Amazon.

Figure 5 - Text Description
Virtual care companies’ market capitalization is approximately $10B, and is claimed by large, established companies and smaller growth companies. Some large companies include Well, Telus, PCC, Dialogue, Weston, and AlayaCare. Other companies include Maple, Teladoc Health, PointClickCare, Telus Health, Dialogue, MindBeacon, Orion Health, Well Health Technologies Corp, Babylon by Telus Health, and ThinkResearch.
Our governments moved very nimbly when they recognized this new reality, creating fee codes to let physicians bill provincial health insurance plans for virtual care while using these platforms. Their shared clients can now access better tech through public payment methods in many provinces. Existing, unusable, technology was abandoned quickly in the face of COVID- 19 and many jurisdictions (not all) allowed new entrants. Several governments just bought Zoom or Teams licenses for every clinician, to support them in caring for their own patients.
These new players are not the small start-ups that for the last two decades policy makers have been funding and encouraging to step up and innovate. In a very short period, our young digital health industry has matured to full blown adulthood. To use a folksy analogy, policy makers are both surprised and pleased with the child they have nurtured suddenly moving from being a teenager to having become a mature industry in a matter of months. As any parent of a 20-year- old knows, the process going forward will continue to have some tension!
Digital health in Canada is now a fully mature industry. This year alone we have seen eight companies go public on the TSX, VSE and even US exchanges. The largest of the Canadian players have market capitalizations that are larger than all but four of the provinces’ total budget spends. The total capitalization of the digital health market in Canada is now somewhere between $15 and $20 billion; this is approximately twice as much as all the money Infoway and the PTs have invested since 2001.
In some ways, this is a huge policy success. We should be justifiably proud of the mature industry that we have actively nurtured through smart policies and investments. Canadian governments, in a non-partisan way, decided to invest in health technology and today we have a huge native industry that is ready to take on the world. These are, in the politician’s words, “good clean knowledge economy jobs”. This market dynamic will, however, need to be managed and regulated going forward. The days of publicly subsidizing new system builds are largely over. The role of government has changed to one of managing competition among the myriad of virtual care platforms and providers. This becomes especially challenging given that the technology for many of these organizations is part and parcel with care delivery. The consequences of this new care model have yet to be fully understood.
There are more extreme versions of this perspective among the interviewees who would argue that policy makers need to get out of the way altogether and let the market decide. Or only step in when market failure is clear. We do not agree with this. Going forward, public policy needs to set the rules for competition in this immature market. Already evident are “rent-seeking behaviours” (excess charges for interfaces) and “walled gardens” that work well on their own but prevent access to information to those outside the walls. Appropriate market regulation can continue to not only support growth in this new industry but also ensure a strong public health care system that is true to the values of our country. At the same time, governments and health systems must honestly acknowledge that the technologies they built in-house were often inferior and unworkable.
Recommendation 8: Governments need to move from capability creation and subsidization to the management of a mature and competitive digital health industry. This recommendation is expanded in Section 4. Implementation Planning.
Figure 2: Four competing perspective on what happened to virtual care in 2020
Each of these four perspectives has some very good arguments to support it. Clinicians and policy makers across Canada are grappling with how to make sense of a very fast-paced year. New data have forced a re-evaluation of our worldview that is profound and deep. The one common element is echoed in the first recommendation: virtual care is no longer an adjunct therapy or an add-on to our workflow. Care is care: whether virtual or physical.
Note that although there is a section dedicated to equity and access, we must be clear that equity is a cross-cutting consideration integrated into every aspect of this report. Equity is central to health care policy in Canada. It is essential that every decision in virtual care policy be made in light of equity considerations. There must be ongoing monitoring to identify any unintended negative consequences on equity that may occur as a result of policy decisions for virtual care.
Recommendation 9: Develop feedback and monitoring processes to ensure policy decisions for virtual care promote equity and to identify any unintended inequitable consequences of virtual care development across Canada.
Section 2: Provincial/territorial, private sector, and international reviews
Interim reports were prepared as part of this diagnostique and presented to the FPT Expert Working Group and to PTs for validation and comment in March and April of 2021. These three interim analyses are summarized in the sections below.
Provincial/territorial reviews
COVID-19 forced rapid virtual care policy changes across provinces and territories. These changes came first and foremost in the form of billing codes. Prior to COVID-19, only British Columbia (BC) and Ontario (ON) allowed providers to bill for real-time video visits outside of designated telehealth sites. In the crisis of last year, governments responded nimbly and with a great deal of common sense.
During the course of interviews it became clear that real and exciting virtual care innovation is happening across the PTs. We have summarized some of that innovation in this section. We have also incorporated much of this innovation into the recommendations articulated throughout this report. We recognize that some PTs will be well ahead on some recommendations. To understand progress on each recommendation across the PTs, we have asked them to identify (before the June 2021 summit) which recommendations are underway in their PT, using Table 2 in Section 4.
Between March 13–March 27, 2020, all provinces and territories added temporary virtual care billing codes or temporary permissions to use in-person billing codes for virtual care.Footnote i There was a great deal of variety in the approaches taken. BC and ON expanded their codes (which already allowed for video visits) to allow for phone visits (voice only).Footnote ii Saskatchewan (SK) tied the video visit billing codes to use of a specific platform (Pexip) but is reviewing whether to make this permanent. Importantly, provinces typically did not differentiate the fee code between a video visit and a phone visit. All provinces, except Prince Edward Island (PEI), excluded asynchronous messaging (e.g., email, text) from the permissible modalities under which the virtual codes could be billed. ON allowed for some providers to bill for secure messaging, but only those who were part of the Ontario Telemedicine Network (OTN) Enhanced Access to Primary Care pilot program implemented in 2017.
Some provinces restricted their fee codes so that those who provided virtual-only walk-in clinics, rather than virtual walk-in visits as part of a “Bricks and Clicks” offering (i.e., both virtual and physical services), could not bill the system. Provinces with billing codes that could be used by providers working with these corporate platforms saw rapid proliferation in the number of companies offering these services (Figure 6 below). SK and New Brunswick (NB) introduced special billing codes for virtual walk-in visits, but at a lower rate than with patients’ regular providers (SK: $24.5 vs $35 and NB: $29 vs $47.50).

Figure 6 - Text Description
A depiction of Virtual Care Companies Whose Physicians Bill the Public System across Canada:
- British Columbia: CloudMD, Maple, Tia Health, Babylon by Telus Health, Viva Care, Walk in Virtual Clinics, Access Virtual
- Alberta: Maple, Babylon by Telus Health, Tia Health
- Saskatchewan: Babylon by Telus Health, Lumeca
- Manitoba: MobileMD, Tia Health, Sabe Wellness
- Ontario: Maple, Tia Health, CloudMD, Babylon by Telus Health, Tulip Health, Pulse On Call, Appletree Medical Group, Get Well Clinic, MyDoctor Now, The Doctor’s Office
None yet identified:
- Newfound and Labrador (Virtual appointments with NPs through 811)
- Nova Scotia
- Nunavut
- Quebec
- NWT
- Yukon
Many provinces saw increased demand and reliance on nurse helplines (e.g., Telehealth, 811 and 211 services) and mental health call lines. Anecdotal reports cite increases in call volumes between 600-700% in some provinces. Several provinces report hiring additional staff to increase capacity. In Nova Scotia (NS) and PEI, 811 became a central resource for coordinating COVID-19 testing and answering questions.
Some provinces purchased communication technologies through various non-industry-specific companies to improve access to existing services, while others purchased bundled virtual care platforms. For example, BC, NB, NS, Northwest Territories (NWT), and PEI all provided Zoom licenses to physicians. Nunavut (NT) and Manitoba (MB) used Microsoft Teams. Alberta entered into an agreement with TELUS to compensate physicians through an alternative relationship plan when they provide virtual services via the Babylon app. PEI and Alberta procured Maple to provide virtual care to their beneficiaries. This decision about whether to purchase à la carte communication technologies that can be used by existing clinicians versus a fully integrated platform is a tricky one – with benefits and disadvantages on both sides. With enough resources, it does not necessarily have to be one or the other. These two solutions can co-exist.
We have seen some creative uses of the virtual care platform in several provinces, where it has been used to augment monitoring of patients. Some creative steps were taken in billing. For example, MB included billing codes for virtual management of chronic disease patients. BC and SK invested in the TELUS Health Home Monitoring platform, which uses technology to remotely monitor patients’ health and then shares the information electronically with their health care teams. In SK, this service allows for home monitoring of certain post-surgical patients and recovering COVID patients. In BC, this was used to monitor COVID patients.
These innovations did not come in the early months from a desire to be innovative, but rather in response to the “Emergency Life Raft” approach to the pandemic. As the pandemic progressed, health care systems developed innovative approaches, at first to avoid admitting COVID patients when possible to limit use of hospital resources. As the pandemic continued, there was increasing concern that chronic disease patients were falling through the cracks. However, in- person care was still restricted, leading to expansion of these programs into non-COVID monitoring. This provided an opportunity to build on these emergency systems and make them permanent fixtures of a patient-centred health system (see section 3.2.4 on remote patient monitoring).
An area of particular focus for all provinces has been virtual mental health services. This was partly driven by expanded demand for support, reported widely by interviews. Many provincial governments directly invested in expansion of virtual mental health support services. These ranged from online forums (e.g., in AB, Togetherall), to self-directed CBT (e.g., in MB, AbilitiCBT), to resource centres (e.g., in NB, Newfoundland and Labrador (NL), and PEI, Bridge the gApp), to therapist-guided mental health services (e.g., in ON, MindBeacon). These investments have been mirrored by employer-based private supplemental insurance or as part of Employee Assistance Programs (EAPs), and through individually-purchased insurance plans.
BC and ON have worked on providing faster access virtually to certain specialty care. BC implemented the Real-Time Virtual Support (RTVS) program for residents and health care providers in rural, remote, and Indigenous communities. This program provides rural and remote primary care providers with 24/7 Zoom access to consultations with specialists in maternity, pediatric, emergency, and intensive care. The program is expanding to include rapid (not immediate) access to other specialists, such as dermatologists and rheumatologists. In ON, several hospitals have opened up Virtual Emergency Departments (EDs), allowing patients to call into virtual EDs and schedule time to talk with a provider, typically the same or next day. This was developed to address the concern that patients were not accessing the physical ED due to the high CoPC environment. Some of these programs existed prior to the pandemic and expanded greatly as need met opportunity.
There has been particularly impressive innovation in some Indigenous communities in virtual care. This is in part because they were already using virtual services and had relevant experience so could scale. Similarly, the territories and northern regions of some of the provinces were able to build on existing systems.
As described above, there have been dozens of innovations and many successes during the pandemic but ensuring equity in access has been a constant challenge across many communities. Virtual care allows some groups to gain access, but others are subject to poor IT infrastructure and other systemic disadvantages.
Review of private sector solutions for virtual care
The pandemic was a coming-of-age event for the digital health industry in general, and for virtual care in particular. There are currently over 40 private-sector digital solutions for virtual care in use in Canada, covering both physical and mental health, and expanding into labs and pharmacies. The combined market capitalization of the Canadian digital and virtual care industry is estimated to be approximately $15-20 billion. The industry has grown rapidly as these companies mature and innovate. In some respects this is a major policy success by the federal and provincial governments who invested in expanding this sector.
Of note, TELUS Health, the Weston Group, and WELL Health have made significant investments in virtual care through acquisitions and investment in virtual care technology solutions. TELUS Health acquired InputHealth Akira, EQ Care, and the Canadian operation of Babylon Health, adding them to its suite of digital health products. The Weston Group acquired QHR Technologies, the parent company of virtual care provider Medeo, and purchased a minority share of Maple. WELL Health made significant acquisitions, including Tia Health, Insig, and Adracare, with the goal of building a virtual ecosystem on its existing Virtual Clinic + platform. WELL is now also the largest integrator of services for Oscar EMRs; in essence creating a third major EMR vendor in Canada.
As growth in demand for virtual care services increased, revenues for these companies also increased significantly. In 2020, ten digital health companies were listed as publicly-traded companies. In December 2020, both MindBeacon (a virtual mental health provider) and Think Research (a company that developed a virtual care solution listed as an Ontario Telemedicine Network Vendor of Record) became publicly-traded. Dialogue Technologies, a virtual care provider used by large insurance companies such as Canada Life Assurance Company and Sun Life Financial, followed by going public in March 2021. This month, CloudDx listed on the Vancouver exchange, and Maple, a direct-to-consumer virtual care solution popular in ON, BC, NB, and PEI, announced in March 2021 that they are preparing to go public.

Figure 7 - Text Description
Virtual Care Acquisitions, Investments, & IPOs. Since late 2019, there has been significant activity within the Canadian virtual care industry as a few large, well- capitalized firms dominated the market, making moves to acquire and invest in many virtual care solutions
Pre 2020:
- Telus Health: Adracare, Akira, RH, Babylon*
- George Weston Limited: Medeo
2020:
- WELL Health: MedBASE, Indivica, DoctorCare, Insig, Tia Health, Li Ka Shing Investment
- Telus Health: eCare
- George Weston Limited, Maple*
- IPOs: Mind Beacon, Think Research
2021:
- Telus Health: Babylon
- IPOs: Dialogue, Cloud DX, Maple **
* Minority Share/ Partnership
** Expected
The models under which each of these platforms operate also varies across the virtual care landscape. In Figure 8, we have identified four main operating models for virtual care technology solutions: virtual walk-in, bricks and clicks, Electronic Medical Record (EMR) launch, and technology connecting patients to a designated clinician.
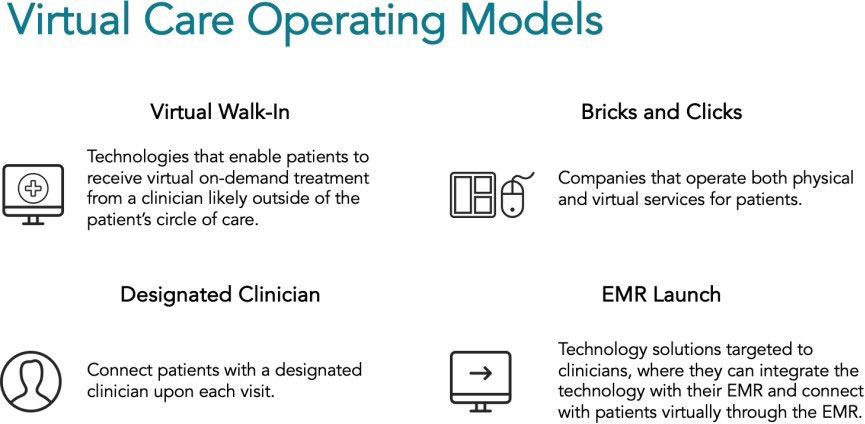
Figure 8 - Text Description
Privately-owned virtual care companies are adopting varied operating models. Four main operating models for virtual care technology solutions are identified: virtual walk-in, bricks and clicks, Electronic Medical Record (EMR) launch, and technology connecting patients to a designated clinician
- Virtual Walk-In: technologies that enable patients to receive virtual on-demand treatment from a clinician likely outside of the patient’s circle of care.
- Bricks and Clicks: companies that operate both physical and virtual services for patients.
- Designated Clinician: connect patients with a designated clinician upon each visit.
- EMR Launch: Technology solutions targeted to clinicians, where they can integrate the technology with their EMR and connect with patients virtually through the EMR.
Among the virtual care solutions currently available, there are few with pure unbundled technology that can be purchased and used as a separate piece of virtual care software. This may represent a gap in the current offering of virtual care solutions. It may also be that EMR launch solutions will dominate going forward, especially when offered in software as a service model. Virtual walk-in services have historically proven difficult to add into our public health care system and are subject to significant public protest by physicians and others. This is particularly interesting given that 811, telehealth, and nurse call lines are not subject to the same opposition. Designated clinician is currently mainly happening in mental health.
There has also been a dramatic shift in payers during the pandemic. As provinces relaxed reimbursement rules and created options for providers to bill provincial insurance plans, many platforms began to offer virtual care services funded by provincial and territorial health plans. Where there were coverage gaps, some patients chose to pay out-of-pocket to access (currently) uninsured solutions. In some provinces, provincial health systems purchased access to these bundled virtual care services from private companies, such as Babylon and Maple.
Employers stepped in during the pandemic and greatly expanded their coverage of virtual care providers through employee benefit plans. Several of these offerings were even provided for free during mid-2020 by virtual care providers seeking to expand market share. These offerings have now matured and have pricing models that are attractive enough for more employers to include them in employee benefits plans. Dialogue is one of the principal companies in this space and recently went public at a market capitalization of over a billion dollars -- making it the first virtual health “unicorn” in Canada. It almost certainly won’t be the last and WELL might dispute that it is the first.
Supplemental insurance companies also represented a major payer group. Dialogue partnered with major insurance providers including SSQ, IA Financial Group, Canada Life Assurance Company, and Sun Life Financial. When the COVID-19 pandemic hit Canada, Sun Life released its Lumino Health Virtual Care platform using the Dialogue Technologies solution, charging $3.49 per member per month. Other virtual care providers such as Akira, EQ Care, and Teladoc also partnered with major insurance providers in Canada. Millions of Canadians are now covered by such employer-based plans.
Some summary observations of this coming-of-age event:
- The Physician EMR market is dominated by three very large players: TELUS, George Weston Group, and WELL.
- Each of these players controls a sizable portion of the physician desktop business and has added virtual care to their EMRs.
- Each has acquired physician practices and is building “Bricks and Clicks” services as well as providing desktops (EMRs) to many other clinicians.
- Employer-based virtual care is available to many Canadians. Estimates for single products are over five million covered employees and their families.
- Mental health platforms are much more widely available because of the pandemic through both provincial reimbursement and employer coverage.
- Stand-alone virtual walk-in is increasingly being brought into the public sector. The private pay, direct-to-consumer market is a niche market in uncovered services, such as secure messaging and Nurse Practitioner video calls. It has grown temporarily.
- Many large practices are looking to build or partner to create their own bricks and clicks delivery systems. Some of these will come forward as “virtual first” offerings.
- Another half a dozen substantial but smaller players are trying to come into this market. These companies have market capitalizations between $100M and $1B. Several of these are now publicly-traded.
- Canada’s two leading vendors for older adult care are global champions. PointClickCare (PCC) in the long-term care and retirement home market and AlayaCare in the home care market have both redefined their sectors.
International experience
International experience with virtual care is broadly confirmatory of the Canadian experience during the pandemic:
- All countries for which we have data or reports from consultancies saw the same large and rapid expansion of virtual care due to high CoPC.
- This expansion varies by specialty. Mental health, endocrinology and several others have moved quickly to virtual while other specialties have struggled or gone back and forth.
- Incorporating virtual and physical care into one workflow is a key challenge everywhere, driven in part by reimbursement and regulation.
- Phone is the dominant modality. In the NHS England phone usage for virtual is even higher than in Canada. US payers have pushed for video and there is more video in the US as a result.
- Where secure messaging is allowed and compensated it is used for about one quarter of total volumes. Some of the best data on this are from Kaiser Permanente Northern California, shown below in Pillar 3.
- Equity, access, and infrastructure are tensions in virtual care globally, just as they are in in-person health care.
The next few years will see major reviews on how different health care systems have adapted during the pandemic and there will be important lessons in each of the six policy pillars.
Section 3: Virtual care policy for Canadians: Six pillars framework
This section is organized using the Six Pillars Framework developed by the Federal-Provincial- Territorial (FPT) Virtual Care Table in its deliberations during 2020/21. We have found this framework to be useful in organizing options and recommendations:
Figure 1- Six policy pillars, in which the recommendations in this diagnostique are grounded
One of the advantages of this framework is that it allows us to stay at the policy level when considering virtual care and not to get dragged into the details of the three policy foundations that underpin the pillars, namely:
- Privacy and Security
- Data Standards and Integration
- Technology
We offer some policy recommendations on these foundational elements but stay out of detailed arguments about data standards and specific technology choices. For example, we use the phrase “usable digital format” to describe data standards rather than getting into the details of FIHR, Blue Button, and other approaches. We stay away from any specific legislative or regulatory recommendations on privacy and security. We note, however, that many interviewees pointed out that existing rules has been conservatively interpreted prior to the pandemic. This changed with high CoPC. There will be a lot of work on these foundations by others in the coming years. We address some of the related policy issues in the framework of the Six Pillars but attempt to stay out of the details.
Pillar 1: Patient and community-centered approaches
Many patients love virtual care. As one provider said,
“Patients don’t want to come into the office. They are very resistant to that if it isn’t clinically necessary.”
- Rural Family Physician
Virtual care provides an opportunity to design a health system that is actually patient-centred. Our current system focuses itself on the needs of the provider, forcing patients to hop from building to building, bringing their records with them in the form of CDs, printed documents, or not at all. It is disconnected, inconvenient, time-consuming, and costly to patients. Virtual care has the potential to bring care to the patient, to improve care transitions, and to make engagement with the health system safer and more convenient for patients.
Designing virtual care for patients
Being patient-centred means that we put our clients at the centre of our system design discussions. One way to do this is to create archetypes or personas that represent the patients we serve and their needs. We have created six such personas. To ground this policy discussion, we invite you to consider each of them and their specific virtual care needs. Our experience, and a theme in our interviews, is that one size solutions fit no one. We must consider specific needs as we test new models and think about how to develop policy that better serves all Canadians.
- Aarya – medically complex older adult
- Aarya is an 84-year-old woman of South Asian descent who lives independently in a downtown retirement home on a fixed income. She has nine regular medications and seven specialists. English is her second language, and she relies on her daughter who supports much of her medical care.
- Casey – student attending university out-of-province
- Casey is an Albertan in first year university at Western University. They maintain their Alberta health coverage and driver’s license while completing their studies out-of-province. Casey has a sexual health problem that can be solved through antibiotic treatment but has had a previous negative reaction to an antibiotic. Casey accesses care either through an in-person or virtual walk-in clinic.
- Stevie – stressed adult with limited time to seek care
- Stevie is a 43-year old in downtown Montreal who has worked long days their entire career. They are 30 pounds overweight, diagnosed with high blood pressure, diabetes, and anxiety. The thought of leaving their busy job to see their doctor adds even more stress. Last week, Stevie’s partner recommended that they seek therapy for anxiety.
- Robin – rural farmer with poor IT connectivity
- Robin, a 54-year-old farmer, lives 300 kilometres north of Toronto in a rural region with poor technological infrastructure and lower than average per-capita income. On the farm, internet access is unreliable, and Robin goes hours at a time without internet. Rogers is the only available phone provider, so they are on a pre-paid voice-only phone plan with Rogers for which data is prohibitively expensive.
- Norman - Cree (Eeyou Istchee) hunter living in remote First Nation community
- Norman is a member of the Cree Nation on James Bay. He is a hunter who lives off the land for part of the year and receives some income support to do so. In the past Norman has been diligent about attending his follow-up appointments with the medical clinic that helps him manage his diabetes and high blood pressure when he is in town. But often these appointments conflict with his seasonal activities on the land. Sometimes he's out of reach by the time a call is made to schedule a follow-up, and as a result his medical care is interrupted for months at a time. Other times, he sacrifices precious time at his camp to make the day- long trek back to town for an appointment.
- Chris – youth with Crohn’s disease
- Chris is a healthy, active, kid living outside of a major city. Diagnosed with IBD about seven years ago. They and their parents have lived with the IBD schedule for years after stabilizing on a biologic treatment. Every six weeks Chris receives an infusion, originally at the downtown children’s centre and now locally. Every 3-4 months he goes for blood work and meetings with the nurse and doctor. One of his parents takes five hours off work for every visit and drives them downtown, an hour each way and $20 for parking. Chris’ dad says, “I do it because I am salaried and can do my work while taking care of my child. For my wife the income loss would be hard.”
There is no “average” patient with “typical” virtual care needs. These patient examples are distributed throughout the report (in Boxes 1-6) with added details about how their care changed during the pandemic. We need to “segment” these markets and develop a “consumer” approach for each of the different personas. We might see some overlap between their needs but we would never assume that there is one record or one service that would cover six such different people with such varying needs.
Let’s review the “virtual care” needs for each of these six persona in summary:
- Aarya: Circle of care support product which includes all providers and gives control of access rights to daughter and primary care provider; remote monitoring technology.
- Casey: Online pharmacy portal, access to lab results online, and virtual visits in-province for on-demand care or (preferably) out-of-province for access to health records.
- Stevie: e-referrals, e-Prescribing, and virtual visits via phone, video, or asynchronous modalities with family physician, as well as virtual mental health therapy from an app- supported service.
- Robin: Secure messaging and phone are the only modalities that will currently work for Robin, who would benefit from other virtual care tools including video visits and online access to their record. Local infrastructure at a pharmacy or library or next gen satellite technology will change this.
- Norman: Ability to access care while maintaining his culture and lifestyle. A mix of modalities that recognize infrastructure limits and seasonal barriers
- Chris: They and their family are an example of a specialty where both consumers and providers win from the shift to virtual care. Chris’ family gets the same high quality care and gains more than one hundred hours of time back and reduces costs. The health system gains capacity and does a better job of communicating and medical education.
Different people have very different virtual care needs. To be patient-centred means, in part, to consider the individual needs of the patient/consumer/client. In Canada, our notions of fairness in the public provision of health care services means that equal access is not always equitable.
Being fair and patient-centred means that at different times in our lives, we need different levels of service. More pithily: one size fits no one.
Means, medians, modes and modalities
In their work on health care spending, Wodchis et al. demonstrated that “one size fits no one”.Footnote 11 In 2009-2011, the top 1% of Ontario’s users consumed 33% of public health care resources, spending at least $44,906 per person. Just 5% of the population accounted for 65% of all costs, with a starting threshold of $7,960 per person. Yet, 50% of the population had median annual costs of just $333 or less, accounting for only 2% of all allocated expenditures.Footnote 12 We cannot treat the person who costs the system $5000 in the same way as we treat the person who costs the system $50. The personas above make clear that these same patterns are likely to hold true in virtual care. The need for a full “circle of care” product, with distributed access to formal and informal caregivers, is likely a major concern for only a small portion of the population. Others will value continuity of recordkeeping to monitor an occasional flare up of a longstanding condition. The question of which modality is the most patient-centred has no clear answer. Some clients prefer secure messaging, but for others that is unworkable or undesirable. Some prefer video to phone in a high CoPC environment because they want the visual cues for communication and diagnosis, but for others the phone is satisfactory. And sometimes people need, or want, in-person care. And always will.
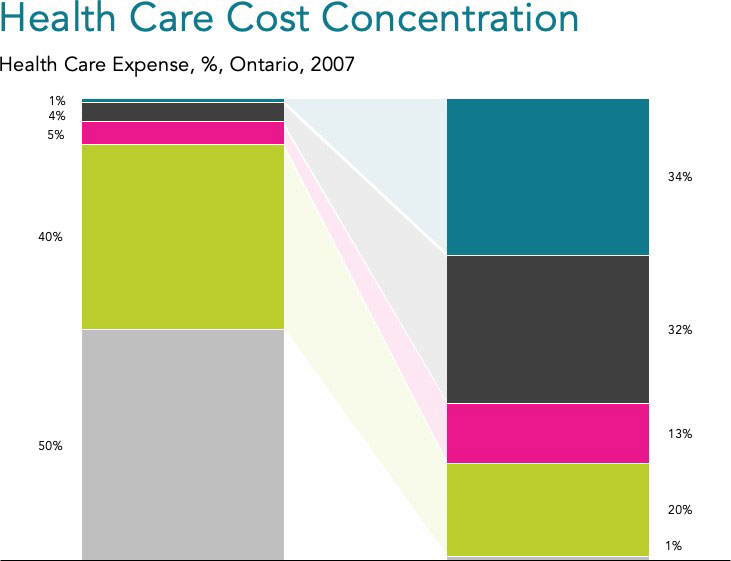
Figure 9 - Text Description
A graph showing that the concentration of healthcare spending is unevenly weighted a small portion of the population in Ontario from 2007. The top 1% of Ontario’s users used 34% of health care costs in Ontario. 4% of the top users used 32%, and the top 5% used 13% of the health care costs. 40% of the top users used 20%. The bottom 50% of the population used 1% of the health care expenses.
Determining which specific modalities are appropriate for which specific types of patient, consumer, or condition will be challenging. The clinical modality decision in April 2021 may be wrong in the near future. Technology is changing in some surprising ways. During interviews we stumbled upon a subset of physicians (in several provinces) who now use communications applications that allow them to switch between phone and video and secure messaging (e.g., WhatsApp and FaceTime). Last month, Zoom announced a telephone service, so we can reasonably predict that phone and video are not going to be separate modalities for much longer. This will solve some problems but will make reimbursement even trickier.
Determining which specific modalities are appropriate for which specific types of patient, consumer, or condition will be challenging. The clinical modality decision in April 2021 may be wrong in the near future. Technology is changing in some surprising ways. During interviews we stumbled upon a subset of physicians (in several provinces) who now use communications applications that allow them to switch between phone and video and secure messaging (e.g., WhatsApp and FaceTime). Last month, Zoom announced a telephone service, so we can reasonably predict that phone and video are not going to be separate modalities for much longer. This will solve some problems but will make reimbursement even trickier.
Rural Robin
Robin, a 54-year-old-farmer, lives 300 kilometres north of Toronto in a rural region with poor technological infrastructure and lower than average per-capita income. On the farm, internet access is unreliable, and Robin goes hours at a time without internet. Rogers is the only available phone provider, so they are on a pre-paid voice-only phone plan with Rogers for which date is prohibitively expensive.
Last month, Robin suffered a serious wound as they were operating heavy machinery. They asked their daughter to drive them to the closest hospital, two-hours away. After a physician treated Robin’s wound, they recommended that Robin monitor the wound with their GP and provided an online link to view the electronic records. However, when Robin tried accessing the record at the farm, bandwith was insufficient. Robin’s physician was another 45-minute drive away and referred Robin to a dermatologist in Toronto. The GP recommended that next time Robin set up a video visit, which was impossible due to the unreliable internet access.
There are many benefits of virtual care for Robin, cut with existing infrastructure and cost constraints. They are unable to access virtual care.
Future-proofing our virtual care decisions becomes even more difficult if we look out five years. Let’s consider three examples using our personas. In April, Microsoft spent $20Bn on Nuance speech technology. Imagine Aarya’s world if she could use speech recognition in Hindi. What would Robin’s care experience be if Elon Musk’s Low Earth Orbiting Satellites (LEOS) were in place and Robin could switch seamlessly from voice to video and back during the same visit? For Casey and all their college roommates, what they really want is to be using virtual reality for discussions with their family physician whom they have known since they were two.
Future-proofing patient-centred modalities is going to be tricky and we need to accept that the future is going to keep changing. We need to empower clinicians and patients to make these decisions and not set an overly high bar for the adoption of new approaches. A foundation for this is a universal data right for all patients.
Recommendation 10: Different patients will require different modalities and mixes of services for our system to be patient-centred and to support continuity of care. We need to be humble and flexible in our systems’ rules, regulations, and policies to allow innovation to continue apace.
Recommendation 11: Every person has the right to receive their health care data in a usable digital format by April 1, 2023. This should include a simple-to-administer ability to delegate control to a family member and to share information among a circle of care.
Improving both public health and patient-centred care through robust health information systems
Canada’s current health data infrastructure is still weak, threatening our communicable disease surveillance and response systems. The experience of the past year has confirmed that it is a matter of public safety that we do a better job on disease surveillance and infection control monitoring in our public health systems. A more robust data infrastructure will also improve our ability to provide excellent and well-organized virtual care to Canadians. We describe these five related recommendations next.
1. Lab Requisitions and Results
We must know who is at risk of COVID-19 infection and who is immune. Patients’ results have been digitally available for decades in Canada, but through imperfect mechanisms and often not accessible to the patient. Consumers now expect their test results to be available online for at least one important test: COVID-19. All tests should now be made digital.
Recommendation 12: All requisitions/results for standard lab tests should be sent/received in a usable digital format by April 1, 2023. No payment should be made for requisitions or results sent/received by paper.
2. E-Prescriptions
During the pandemic, PrescribeIT saw phenomenal growth, as shown in Figure 10.

Figure 10 - Text Description
Infoway’s PrescribeIT enables prescribers to electronically transmit a prescription directly from an electronic medical record to the pharmacy management system of a patient’s pharmacy of choice. PrescribeIT has seen significant growth and interest over the last 12 months. National highlights include:
- 165% increase in prescriber enrollment
- 163% in LIVE prescribers
- Over 62,000 enrolled
- 300% increase in transaction volume
- 44% increase in pharmacy enrollment
- 118% increase in LIVE pharmacies
- 48% of pharmacies enrolled
- 300% increase in Transaction Volume
There are a few competing commercial services to help keep this service competitive. This base of service allows us to make the following recommendation.
Recommendation 13: All prescriptions should be sent/received digitally by April 1, 2023. Because of the crisis in opioid usage in Canada, all opioid prescriptions should be sent/received digitally by April 1, 2022.
The added recommendation on opioid prescribing is long overdue and given the available services could occur immediately.
3. Home Care, Retirement Home and Long-Term Care records
Home Care: Canada now has a serious national champion in AlayaCare that allows caregivers to collect patient-reported outcome and experience measures – PROMS and PREMS. This software is built primarily as a logistics and scheduling platform and has a light health record that is focused on activities of daily living. This is of great interest to someone like Aarya’s daughter as she seeks to keep track of her parent’s health status. It is of occasional interest to others in her circle of care. AlayaCare has an automated PROM that assesses overall health status as well as several PREMs and reported experience measures for care providers, including personal support workers or health care aides.
Long-term care (LTC) is paradoxical in Canada from a digital perspective: we are both very sophisticated and woefully lacking in good virtual care and digital infrastructure in our LTC homes. Canada has the number one long-term care software system on the planet based in Mississauga. PointClickCare (PCC) employs 1300 people in North America and is worth about $5 Bn US. PCC is a huge Canadian success story and a national asset. Yet, there has been little discussion about using PCC as a reporting tool to assess quality of LTC homes and to track pandemic progress and vaccination. By current estimates, PCC already has more than 70% of the LTC market. They should be invited, among others, to co-design a standard reporting infrastructure. Note: this will require an aggressive translation program as PCC does not currently have an available French language version.
Recommendation 14: Pan-Canadian health care organizations should work with the two major Canadian eldercare software companies to redesign institutional and home care reporting systems.
4. Hospital sector
The large US IT vendors are struggling to provide similar functionality in ambulatory care under the weight of their monolithic inpatient IT systems. These systems are bound to US Medicare’s “Meaningful Use” standards. This drives their product development because they are the specific features of an electronic medical record (EMR) that providers must use to qualify for incentive payments. Some jurisdictions and/or their regions are doing well with their vendors to provide these services. Others are struggling. Frankly, the user experience for both patients and physicians is not uniform and often not good. Addressing this deficit will continue to be a problem for the next generation. But the US has introduced reporting standards that we, too, should insist upon in Canada for virtual care to be successful.
Recommendation 15: All hospitals should provide a discharge or encounter summary upon request in a usable, machine readable and searchable, digital format as of April 1, 2023. An appropriate small fee should be paid by government on behalf of requesting consumers.
5. Physician EMRs
Primary care is an excellent place to collate patients’ records and to provide a communications hub for patients about their health care. They have increasingly evolved from being databases and billing systems to multimodal communications systems. Figure 11 shows a visualization of this change:
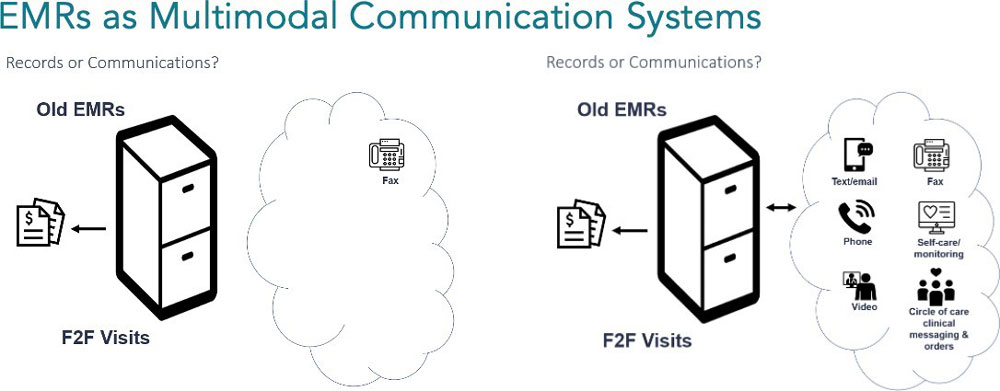
Figure 11 - Text Description
A graphic depicting how EMRs are evolving from databases and billing systems (e.g. fax machines) to multimodal communication systems (e.g. text/emails, phone, video, fax, self-care/monitoring, and circle of care clinical messaging & others).
Input Health (now owned by TELUS Health) and other innovative software developers have changed the game. Rather than building billing systems first, they started with communications and collection of validated information from patients. This patient-first, virtual care-first approach is being widely replicated in employer-based and on-demand virtual care. Some public health care systems are now also collecting automated data, as are the Ontario Virtual Care Clinic (OVCC) and 811/telehealth lines.
The next generation of primary care EMRs will start with the patient, build a history, and validate a set of symptoms. They will enable a virtual-first visit pattern. This will often start with some “Do-it-yourself” (DIY) assessment online and the sharing of resources by secure messaging. Virtual-first care will often proceed then with a simple phone call (or secure message if that is appropriately remunerated) that can be supplemented by pictures or switched to video during the same connection. Currently, there is a separation between phone and video, but we expect this to disappear in the next few years. Multimodal calls are already occurring regularly during the pandemic by some capitated primary care physicians. The barrier between portal, phone, messaging, and video is transitional only. Omnichannel systems will be the norm shortly. They already are for employer-based care systems that have exploded during the pandemic.
Before the pandemic we spoke about “building virtual into the workflow”. Today, virtual is the primary workflow for many practices and the need is to build a patient-centred multimodal experience. The EMR will not be the only system of innovation for patients.
Interviewed clinicians pointed to the need for better systems for patients in Wodchis’ et al.’s top ten percent of health system users. Some call this a “circle of care” product, others say “patient relationship management”, and some even hope that their own EMR may someday evolve into such a system. This information service may well be different for people whose health status indicates that they will be in a high user group for a number of years, so there are likely several types of products/ services needed depending on diagnosis and prognosis. A portal for pregnant patients is different than a circle of care product for an elderly cancer patient, and both are different again from platforms to support patients struggling with mental health and addictions. All need to be linked back to the system of record which will be usually held at the hospital or doctor’s office. Stevie and Aarya need information systems that are quite different even though they may both link back to the same base information stores in hospitals and physicians’ offices.
Occasional patients—most of us who rarely seek care— need a comprehensive data store to go back to as a “source of truth” (e.g., College Casey) but their active needs are usually more for communications technology or for a disease specific intervention (e.g., Stevie’s CBT platform, well-baby support).
Recommendation 16: All Primary Care EMRs should provide a summary upon request in a usable, machine readable and searchable, digital format as of April 1, 2023. An appropriate small fee will be paid by government on behalf of requesting consumers.
Some will say that these five recommendations are difficult or expensive. That view is penny wise and pound foolish. What is difficult and expensive is trying to manage health care during a pandemic without a strong digital backbone. We are ready to push full conversion of these and other foundational services and should do so immediately. There may be some remediation support needed to help transition gracefully and to ease genuinely sub-scale situations.
Recommendation 17: A temporary paper record remediation service should be made available to service providers (at their expense) to allow them to meet patient information requests during FY 2022 to 2026 to ease transition to a fully digital world.
The question of portals for patients
If we were starting with a blank sheet of paper, we would probably use the PCP’s EMR as the basis for all patient information needs and queries. But we are not doing so. Current consumer access to information in Canada has relied on 20th century portal technology first developed in other countries. At last count, there were more than 90 portals in Ontario alone. Many hospitals have implemented these patient portals with mixed success during the pandemic. Separate personal records also exist in many of the health care segments listed above, including lab systems and pharmacies. LTC and home care provide patient summaries to family members. We have provincial immunization systems with portal like “yellow cards” that will be more important after the last year.
Broader enrollment and use of such personal health record services should be encouraged to create an information rich system. These payments will also serve to reward players who have already started addressing this need and to encourage others to do so. The “push” recommendations above will create costs; our policy in this area should create a “pull”. A small payment of about 25 cents per active user each month ($3 per year) should be paid to each provider who has an active consumer portal. Active management of these systems will be needed in coming years. Major systems exist in pharmacy, labs, and hospitals. They exist and should be more common in primary care. Having such systems in place is a key part of bringing virtual care into the workflow of all system providers.
Ambulatory Aarya
Aarya is an 84-year-old South Asian woman who lives independently in a downtown retirement home on a fixed income. She has nine regular medications and seven specialists. English is her second language, and she relies on her daughter who supports much of her medical care.
- Cardiologist calls to review blood pressure (which is taken by the LPN)
- Endocrinologist calls and emails with daughter to discuss routine bloodwork
- Regular macular degeneration appointments have been suspended and sight is deteriorating
- Daily dermatology treatments have continued at the home by a PPE clad RPN
Virtual visits for Aarya cannot be done over video because of her poor eyesight. Secure messaging (email) is with her daughter, and breaks privacy rules. Written communication in English relies heavily on the daughter’s support. Three-way calls with the provider and the daughter on the line have been essential for ensuring information is received by both Aarya and her daughter. E-labs and e-prescriptions would help Aarya’s daughter keep track of all relevant medical updates. The daughter needs a circle of care record.
Recommendation 18: A small monthly fee (25 cents) should be paid each month to providers as an information fee for providing a personal health record service (aka portal) that is being actively used by consumers. This fee should have a sunset period of five years as it becomes a normal part of the workflow of the health service providers (declining by 5 cents per month each year).
Recommendation 19: All government supported PHR services and portals must publicly report monthly active users, Net Promoter Score and such other PREMS as may be directed by the Pan-Canadian Health Organizations in order to receive payment.
There would be no need for a central government portal if there existed a working standards architecture and an Application Programming Interface (API) system that allows applications to talk to each other. APIs are ubiquitous in our everyday lives. Each time we pay for something with PayPal in an eCommerce store, we are using an API. When we use travel booking sites, it’s an API that aggregates thousands of flights and destinations to showcase the cheapest option.
During COVID, with a proper API in place, the various vaccine scheduling systems would be able to “talk” to each, more efficiently booking second doses, and directing people to the most appropriate vaccination site. Without an API, siloed information can still be shared by uploading information to a portal, but this is a clunky solution. APIs are a far more elegant way to do this. In a world in which foundational data elements were only created digitally, aggregating them into custom views would be the basis for competition among IT communication system providers. Said another way: in a virtual world it only makes sense that health care providers, labs, and others will continue to improve these products well beyond the traditional “portal”.
Patients want one place to log in that can connect them to their information on the care they received in different clinics and hospitals, summarized in plain language. That starting point will be different for different patients given their different needs.
Recommendation 20: Canadian health information services and communications providers must publish and support usable application programming interfaces (APIs). Infoway should set tough standards for basic APIs.
With such foundational elements in place, building community-wide systems will become much more manageable, including disease surveillance and population health management. Currently, policy makers and innovators are “pushing on a string”. They are unable to push closed systems to open up. Large US and Canadian vendors exhibit rent-seeking behaviours, manipulating public policy barriers to entry and standards as a strategy for increasing revenues. This bad behaviour is widely known by Chief Information Officers and competing vendors. There are reports of Canadian vendors charging as much as $8 per month per doctor for access to their EMRs. This allows the health record company to use its dominant market position to extract rents on top of the software’s original cost and maintenance fees. Hospital EMRs ask hundreds of thousands of dollars for interfaces to their systems. This is entirely predictable. Large US vendors who publicly report show more than half of revenues (billions of dollars) coming not from software but from “services and integration”. The public sector is paying twice for its software. Once to install it and then again and again to use it. This needs to be stopped by bundling open access architecture into these systems through the recommendations above. In this way, we enable community-centred innovation that improves population health while also improving user experience for patients and their clinicians.
Recommendation 21: Where vendors charge fees, they should be published transparently and be subject to commercial review. Vendors should not be allowed to use dominant position in one sector to force use of their system in another health sector.
We have known for some time that this was an issue. What the pandemic brought home was that, in addition to obstruction and price gouging, the lack of good connectivity is a safety issue as well. Other more formal reports and inquests are likely to show this in much more detail. We need to recognize it early and act now to correct it.
Pillar 2: Equity in Access
Access and Equity
At the start of the pandemic, a dramatic loss of in-person access to care providers was soon followed by an unprecedented suspension of formal and informal rules, and then by the introduction of fee codes and tariffs for virtual care. Opening up reimbursement and regulations allowed us to address the access crisis of the pandemic in some interesting ways that changed equity and access. Viewed through an equity lens, there were losses and gains as a result.
Virtual care was sometimes a huge equalizer. In some cases, rural populations were on the same playing field as urban populations, often for the first time.
“Virtual care was transformative – communities with no access to supports, no physician presence – [prior to COVID], at best they could call community hundreds of kilometres away and talk to someone who is distracted and busy.”
- Policy Person, First Nations, Rural & Remote Health Care
Key informants who provide care to Indigenous populations spoke of the culturally safe aspects of virtual care. Phone and video visits provide a welcome alternative to showing up at unfamiliar, culturally intimidating, edifices to access care. Virtual visits empower people to end a call if they feel uncomfortable or disrespected, which is easier for some than simply walking out of the office. They also spoke about including traditional healers and gifted elders in palliative care and the ability to be culturally specific rather than pan-Indigenous.
At the same time, and often in the same interview, people spoke about the dangers of hollowing out care systems by using urban-based virtual care for rural communities or by enabling providers to stay out of Indigenous communities that very much needed a physical presence.
These access issues are tough and multi-faceted. They were difficult in a physical-only world and they will be in a mixed modality world as well.
Virtual care has huge potential as a cost and time saver for patients. Infoway data recently showed that patients estimate they save on average $105 per visit using virtual care over in- person, due to not taking time off work, not having to pay for child care, and other reasons.Footnote 5 This is a huge non-pandemic CoPC that was largely ignored in non-rural settings prior to the pandemic. In some ways it is correct to view this as a user fee on the system; a systemic barrier that falls very heavily on those in hourly wage positions, families with children or elder care needs, and those who face transportation barriers. Again, these access issues were all familiar to us in the pre-pandemic physical care world.
There are early data on access from a recent study by the Centre for Digital Health Evaluation (unpublished) showing that virtual care does not have the negative impact by income and age that many expected. These are, of course, only broad averages and likely hide problems within.
Figure 12 shows that in one study, neighbourhood income quintile had little effect on Canadians’ ability to access virtual care. This effect has widely been assumed and is not supported by the early data.
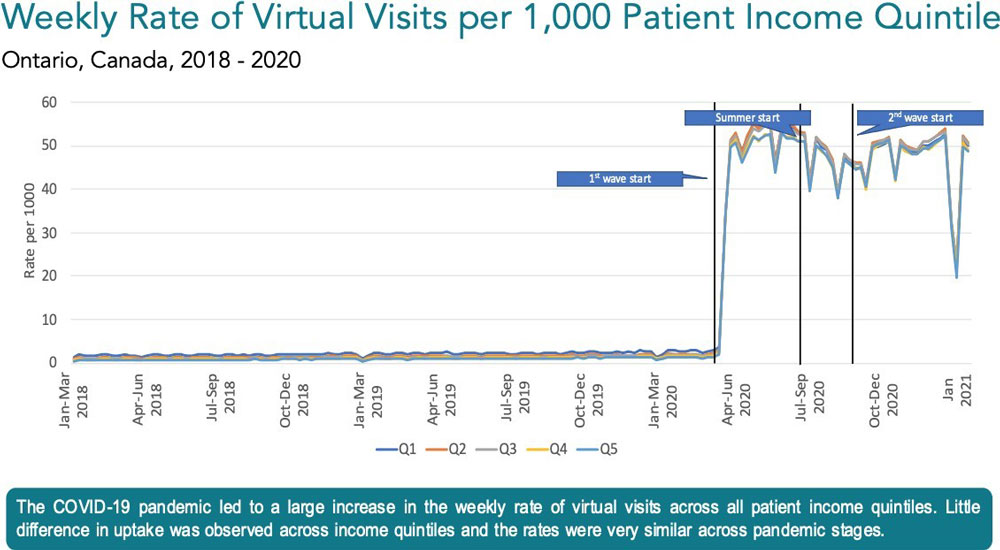
Figure 12 - Text Description
A line graph depicting the weekly rate of virtual visits per 1000 patient income quintile from January 2018 to January 2021 in Ontario, which shows that the COVID-19 pandemic led to a large increase in the weekly rate of virtual visits across all patient income quintiles. Little difference in uptake was observed across income quintiles and the rates were very similar across pandemic stages.
It is reasonable to assume that phone support was a large reason for this fairly equitable distribution because of its low barrier to access.
Similarly, the highest using age group for virtual care is older adults. This is what we would expect given the usage patterns of the age groups, but it is good to see that older adults are using virtual care.
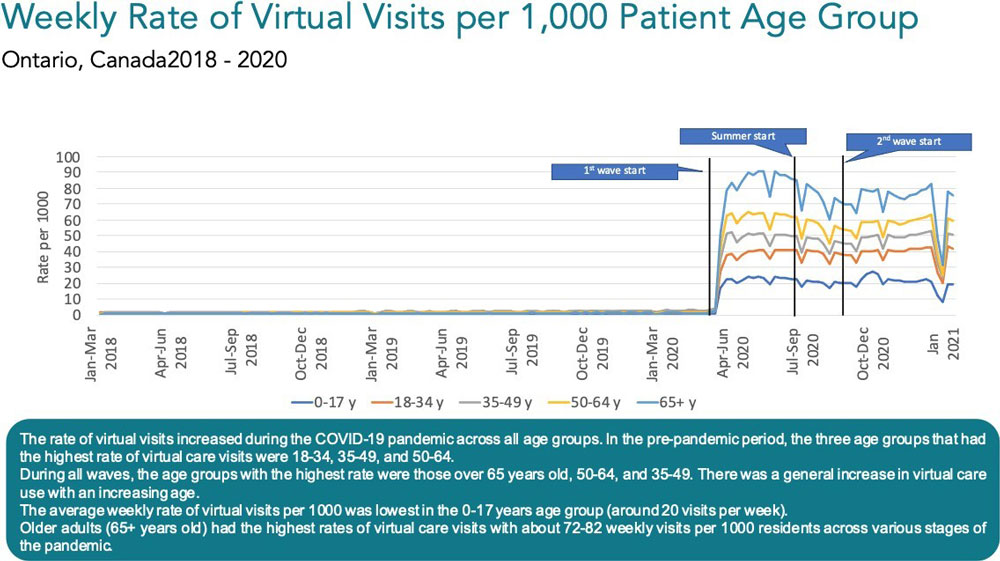
Figure 13 - Text Description
A line graph depicting the weekly rate of virtual visits per 1000 patient age group from January 2018 to January 2021 in Ontario, which shows that the COVID-19 pandemic led to a large increase in the weekly rate of virtual visits across all patient age groups. In the pre-pandemic period, the three age groups that had the highest rate of virtual care visits were 18-34, 35-49, and 50-64.
During all waves, the age groups with the highest rate were those over 65 years old, 50-64, and 35-49. There was a general increase in virtual care use with an increasing age.
The average weekly rate of virtual visits per 1000 was lowest in the 0-17 years age group (around 20 visits per week).
Older adults (65+ years old) had the highest rate of virtual care visits with about 72-82 weekly visits per 1000 residents across various stages of the pandemic.
We need to be careful about generalizing from these data. Again, our persona of Aarya brings this home to us. She cannot use virtual care on her own. She needed other systems and people to support her during the pandemic. While Robin may be able to get their phone calls answered, how do we know that is sufficient and appropriate for their care needs? On the other hand, Casey is fluent in all modalities but has to pay up front and be reimbursed later under current inter- provincial practices.
Again, we need to be truly patient-centred. To do this, providers need to be able to assess their patients’ communication needs and preferences, and thoughtfully suggest the communication architecture that will suit those needs. Digital literacy needs to be considered in system design to ensure that all patients can access care. Even the worst designed physical system has the one advantage that the bad design is visible to all. There is a concern that virtual-only or virtual-first access may hide problems. Those who have challenges may be already in a vulnerable population or have lower health status.
Norman of the Cree Nation (Eeyou Istchee)
Norman is a member of the Cree Nation on James Bay. He is a hunter who lives off the land for part of the year and receives some income support. In the past Norman has been diligent about attending follow-up appointments with the medical clinic that helps him manage his diabetes and high blood pressure when he is in town. But often these appointments conflict with his seasonal activities on the land. Sometimes he’s out of reach by the time a call is made to schedule a follow-up, and as a result his medical care is interrupted for months at a time. Other times, je sacrifices precious time at his camp to make the day-long trek back to town for an appointment.
He is a strong and healthy man in his 60s and is a residential school survivor who struggled with mental health and addictions issues in his 30s and 40s. Time on the land has helped him heal from past trauma. He and his doctor also notice how much easier it is to control his diabetes and hypertension when he’s out on the land. Norman is proud of his heritage and thoughtful about his medical needs. He values advice from both Native healers and Western medicine. At the same time, he lives off the land for long periods of time and is understandably reluctant to “come into town”.
Norman has a good smartphone as his principal communications device but when he is hunting in northern Quebec there are often serious connectivity issues. He knows where hot spots are and can manage his trip schedule to be near hotspots if he needs to be. He’s very happy to be able to skidoo from his camp down to the highway for a chat with his doctor, rather than drive 10 hours into town for a 20-minute diabetes follow-up.
When he is in town, he gets the needed bloodwork and tests done. But his scheduled visits with his supporting clinicians can now be done by phone. As a result, his no-show rate has dropped from about one in three to almost zero. His care and monitoring can be done on a schedule that suits a hunter and respects his lifestyle. When he is in town for longer periods, he will restart his in-person visits. He enjoys the interactions when they work for him and respect his schedule and his culture.
There have also been clear negatives for access. The pandemic shut down physical care for a period of months. This report is not seeking to elaborate that point. Nor to over emphasize obvious negative aspects of losing the ability to do a physical exam and look one’s patient in the eyes. There are many aspects of patient care that are not appropriate for virtual care. This will always be the case and we need to not push too far or inappropriately. More on this in a later pillar.
Infrastructure
“Those that have inequitable access today will have inequitable access virtually. Bandwidth will still be inequitable. Remote First Nations have problems today and will have problems virtually.”
- Consultant
There is a major caveat to this broader comment about equity and access. One of the foremost issues affecting equitable access to virtual care is the inequitable distribution of internet infrastructure and digital literacy across the country. Whereas a video or phone visit with a specialist is a non-issue in Toronto (high-speed internet, no long- distance phone bills), this is not the case once you live a couple hours outside of Toronto in Shelburne or Grand Valley, and certainly not the case when you are in Nunavut or rural Newfoundland. This problem is not unique to virtual care and is not unique to health care.
One key informant estimated that 35% of Indigenous communities do not have access to basic connectivity – they’re using point-to-point satellite or dial-up. These systems are not capable of running virtual care. Virtual care using phone, sharing of health information by fax, and broadcasting of health education by radio are essential under the current infrastructure. Of the other 65%, few have fiber optic.
Unreliable internet persists across the land.
“Internet needs to be part of the infrastructure of health care – it is as important as the bricks and mortar.”
- First Nations Health Administrator
Virtual care will not solve the geographically-generated inequities in access to care until internet infrastructure is improved in areas where it is lacking. This digital divide is a problem that some people interviewed think will be solved within five years by low-earth orbit satellites (LEOS). Integrating with on-the-ground internet networks, the hope is that LEOS will ensure that people living in rural and remote communities have access to affordable, high-quality, broadband. If this comes to fruition, some Canadians have only a short-term access problem to solve. Until then, phone and low bandwidth secure messaging seem well-suited to help bridge this gap, even though they don’t enable higher bandwidth video care and patient monitoring. In the interim, we can look to solutions like the Real-Time Virtual Support network in BC, fixed-location telehealth sites, and continuing to allow reimbursement for phone visits to bridge the gap and allow at least some access to virtual care in these areas.
Rural Robin will someday be able to access reliable high speed broad band. Until that day, their care providers, in collaboration with them, need to consider what the appropriate mix of phone, messaging, and physical visits are. Insisting on video is currently unworkable for Robin.
The telephone (19th century technology) has been a cornerstone for equitable access. This appears to have played out in most OECD nations. In response to WHO’s declaration of a pandemic, provincial and territorial governments and medical associations moved rapidly to adapt physician fee schedules to allow patient visits by phone. Phone is broadly recognized now as a necessary option to mitigate the digital divide. Those living in rural areas without internet access or with poor quality infrastructure are inherently disadvantaged by virtual care being defined as video visits only (which it often was pre-pandemic). Phone is the great equalizer. It enables equitable access for people having difficulty finding a private space for a video visit, for those who do not have the technology required for video (e.g., smart phone, web cam, internet access), and for those who have difficulty using computers and video software.
“Keep phone for equity issues alone – scrapping temporary visit codes [for phone visits] will make physicians mad and patients no-shows. Paying phone at extreme discount to video is the same.”
- Specialist Physician
Another cornerstone of equitable access and distribution of health information in rural Indigenous communities has been radio. The First Nations Health Managers Association (FNHMA) has been broadcasting weekly updates to 150 First Nations radio stations across Canada to provide COVID and vaccine updates to communities. The beauty of radio is that it is nearly ubiquitous.
Recommendation 22: Partner with individual communities to co-develop care delivery and infrastructure to suit their needs and wants. Collaborate with Indigenous health partners and organizations to ensure holistic approaches to meeting health needs in a culturally safe and appropriate way, including considerations of language and specific needs of individual communities.
In some parts of Canada, we cannot scrap the fax machine – not yet. One interviewee spoke of the essential educational needs of many Indigenous communities to empower them to manage their tech infrastructure. She spoke of computers being shipped to communities with no one there to help set them up or train people to use them. As infrastructure to support virtual care develops, we need to train people in these communities to use that infrastructure. Digital literacy needs to be considered alongside infrastructure investments. Right now, people rely on fax as a (somewhat) reliable way to send health information to remote communities.
We note that this is not “just a health care issue”. The infrastructure needs in these communities are profound and difficult. Internet connectivity and good information technology and IT support are needed for education, social services, to support the economy, and for basic human rights.
But even that may not be a broad enough lens to view this equity issue through. Many Indigenous communities need basic infrastructure and transportation supports as well. Several experienced leaders mentioned the hope for low earth orbit satellite systems and next generation information infrastructure generally. These topics are getting attention and need more. On the health system side, we have a responsibility to make sure new technologies are usable by local communities and bands.
Recommendation 23: Provide federal funding in partnership with FNHMA to develop a credentialed band and community-based IT support group to work with communities to develop tech literacy.
Access in Primary Care
Walk-in clinics have existed in Canada for decades. Regularly decried as providing an inferior product, they have stubbornly resisted this criticism and have continued to provide large amounts of primary care in many provinces. With the opening of the virtual codes, the physical walk-in “problem” became virtual.
Soon after the pandemic was declared, the payment barrier was removed and the use of virtual walk-ins, of all types, exploded. In the case of COVID-related care they were often promoted by government as the first point of contact. Several provinces have reported call volume increases of 500-700%. Virtual walk-in clinics exist in many forms. 811, Maple, Dialogue, Virtual ED, Doctor of the Day, and the Ontario Virtual Care Clinic are all variants of this same model. A clinician takes a more or less automated history from a patient virtually and then does their best to meet the patients’ needs. They generally have no access to the patient’s historical chart, and it is usually left to the patient to reconnect the records back to their medical home, if they have one.
Amongst health care policy makers, there is an almost universal concern about continuity of care. The quality of care cannot be as good when the physician has no access to the patient record and the record does not go back to the patient’s primary care provider. While true, we need to see the obvious: Data showing the jump in users and the ubiquitously positive patient experience across virtual services means that patients want rapid access to care, whether by virtual means or in-person. Our public system needs to figure out how to provide quicker access to care or the demand for a second tier available to those who can pay will increase.
The Canadian health care system needs to put a value on patients’ time and user experiences. There were always costs of physical contact. Patients had to take time off work, hire a babysitter, pay for gas and parking, risk driving on treacherous roads over long distances, and wait in the waiting room. Waiting rooms and elevators lost 75% of their capacity. Public transit and babysitting became unsafe. The CoPC affected the providers as well. PPE costs and very real infection risks meant that CoPC forced ambulatory care to go virtual. This is why there has been a rapid expansion in both public and private services of this type.
As policy makers, we need to sort through the trade-offs in primary care between “Continuity of Care” and “Ease of Access.” We propose to do that in a systematic way using three charts that represent the pre-pandemic and current situation in primary care. This analysis is illustrative based on our judgment and interviews. It ignores jurisdictional variations and is simplified.
Crohn’s Chris
Chris is a healthy active kid living outside of a major city. Diagnosed with IBD about seven years ago. They and their parents have lived with the IBD schedule for years after stabilizing on a biologic treatment. Every six weeks an infusion; originally at the downtown children’s centre and now locally. Every 3-4 months for blood work and meetings with the nurse and doctor. One of his parents takes five hours of work for every visit and drives them downtown; an hour each way and $20 for parking. Chris’ dad says “I do it because I am salaried and can do my work while taking care of my child for my wife the income loss would be hard.”
Since COVID, all bloodwork is now timed with the infusion and is done locally. Some lower priority tests were eliminated from the routine blood work to make this possible. They were probably always low value and unneeded but that had never been questioned.
Both parents now feel better connected – especially mom. The IBD specialty nurse is available by email and phone. Every three to four months they meet with a doctor by video. Chris can be at school and either or both parents can join the video call at work. Both the nurse and the doctor are on the videoconference. On a recent video call, the subspecialty Fellow joined from halfway around the world after their flight was delayed due to COVID thus supporting medical education. When needed other members of the circle of care can be included. “No more pick up. No more 5 hours every six weeks. Sometimes I kind of miss it in a weird way but then I give my head a shake and think about the lost school time and what it must mean for most parents in hourly jobs and tenuous employment situations.”
Their doctor recently told Chris and the family that the clinic is “never going back”.
In Figure 14 we show the eight types of current primary care services on the axes of continuity of care (y-axis) vs ease of access (x-axis):
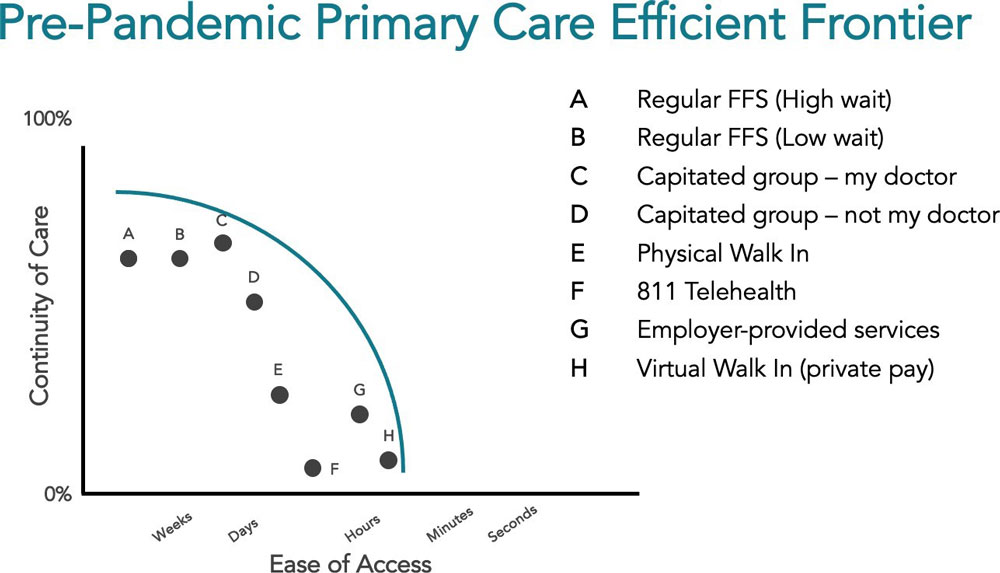
Figure 14 - Text Description
| Pre-Pandemic Primary Care Efficient Frontier | ||
|---|---|---|
| Types of Primary Care (in order of low to high ease of access) | Ease of Access | Ranking of Continuity of Care (0-100%) from highest to lowest |
| Regular FFS (high wait) | Weeks | 2 |
| Regular FFS (Low wait) | Weeks | 2 |
| Capitated group – my doctor | Weeks-Days | 1 |
| Capitated group – not my doctor | Days | 3 |
| Physical Walk In | Days | 4 |
| 811 Telehealth | Days-Hours | 7 |
| Employer-provided services | Hours | 5 |
| Virtual Walk In (private pay) | Hours | 6 |
The mapping of these services is shown against a Pareto Efficient Frontier. An Efficient Frontier is a representation of where trade-offs must be made between the two variables. To the left on the x-axis and below the frontier curve, gains can still be made. What this illustrates is that physical visits pre-pandemic had higher continuity of care but lower ease of access. 811 and other virtual services had high ease of access but worse continuity. This graph makes clear the role that in-person walk-ins played because they provided same day service.
Figure 15 shows what it looks like mid-pandemic: With the opening of virtual fee codes, the three existing virtual services experienced huge growth (i.e., F, G, H), and in some cases they improved on one or both axes. New services also proliferated (i.e., I, J, K).

Figure 15 - Text Description
| Mid Pandemic Primary Care Efficient Frontiers | ||
|---|---|---|
| Types of Primary Care available during the pandemic | Ease of Access | Ranking of Continuity of Care (0-100%) from highest to lowest |
| Regular FFS (high wait) | Weeks | 3 |
| Regular FFS (Low wait) | Weeks | 3 |
| Capitated group – my doctor | Weeks-Days | 2 |
| Capitated group – not my doctor | Days | 4 |
| Physical Walk In | Days | 6 |
| 811 Telehealth | Days-Hours | 10 |
| Employer-provided services | Hours-MinutesTable 2 Footnote 2 |
5Table 2 Footnote 2 |
| Virtual Walk In (private pay) | Hours-MinutesTable 2 Footnote 2 | 9 |
| Large Group Digital Front DoorTable 2 Footnote 1 | Days-Hours | 1 |
| 24-hour on-demand virtual careTable 2 Footnote 1 | Days-Hours | 8 |
| Provincial/regional front door servicesTable 2 Footnote 1 | Minutes | 7 |
First, you will note that there are three new services available. A digital front door (I) provided by a modern capitated practice (i.e., set fee per patient per year, regardless of treatment provided), a provincial/regional virtual clinic or doctor-of-the-day service (K), and 24-hour private pay virtual care (J). Two of the existing services “moved” aggressively because of new investment to improve access (virtual walk-in) or to increase continuity and improve access (employer-funded). 811 grew initially because of convenience and lack of options, and physical walk-in and high wait FFS both appear less and less attractive.
The speed of access through these new and expanding services is remarkable. Many boast a response time of minutes to talk to a doctor online, by secure messaging (private pay), phone, or video. The patient chooses the modality, and most are choosing secure messaging. Dialogue, Lumino and others offer employers a service to match patients to providers in minutes. They have multidisciplinary team-based care and use history collection to identify the appropriate member of the clinical team. One third of the visits during the past year were for mental health services.
One of these services has published their fee level of $3.49 per member per month; anecdotally, others appear to be similar. Each member typically averages 1.3-1.5 family members, meaning that these services average under $2 per month with a response time of less than an hour. These services undoubtedly represent a paradigm shift in access to care – interacting with a doctor in minutes, from the comfort of home. Travel time is eliminated, as are hours in a waiting room for a 5-15 minute visit. It is no wonder that in a high CoPC environment, employers who were concerned about their employees’ welfare flocked to these services.
COVID-19 has pushed out the access frontier through the proliferation of virtual-only clinical services, digital triage tools, and virtual billing codes. Some in-person services have been left behind in terms of access, including high-wait FFS and in-person only walk-in clinics. Their wait times are unacceptably long, but integration of virtual services could significantly reduce wait times and improve access in these settings too. Smaller practices may not have adequate staffing to enable the triaging necessary to increase efficiency and may prove to be subscale. We may need to link these practices to a regional front door service. We could also do front door services on a cultural on linguistic basis, as is already occurring in some Indigenous communities.
Currently, there are legitimate concerns about continuity of care and equity of access. These services rarely connect back to the primary care provider in the patient’s home practice, and they run the risk of operating on limited information because they have no access to the patient’s existing record. Both of these risks have existed for some time in the system around both physical walk-in clinics and ED visits. The same information connectivity issues also exist for 811/Telehealth primary care and for the new provincial variants of publicly provided virtual walk-ins (e.g., OVCC, Doctor of the Day). Walk-in clinics exist in part because of access failures in other parts of the system. Care needs to be taken to address these access failures and not just masking the symptom.
What could this look like post pandemic? Figure 16 shows our representation of the next generation primary care:
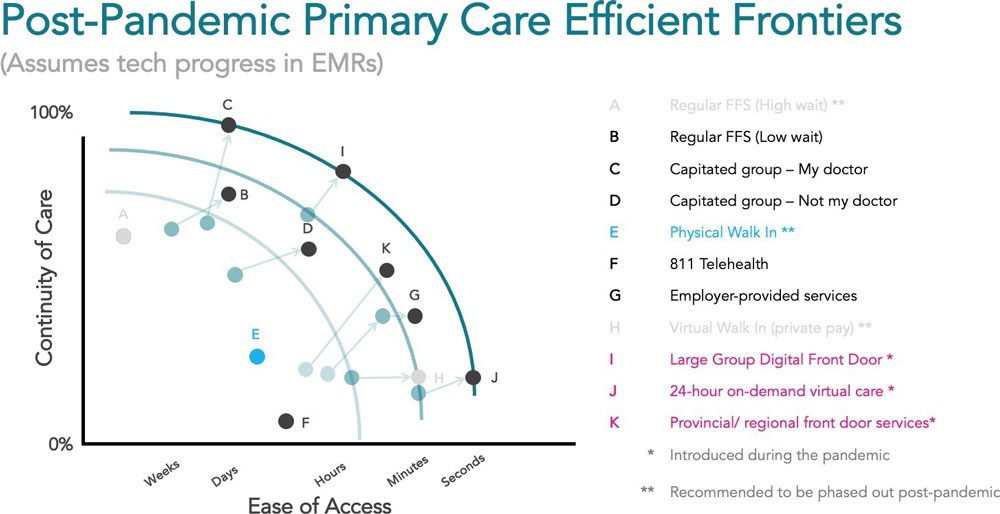
Figure 16 - Text Description
| Post-pandemic Primary Care Efficient Frontiers (assumes tech progress in EMRs) | ||
|---|---|---|
| Types of Primary Care available during the pandemic | Ease of Access | Ranking of Continuity of Care (0-100%) from highest to lowest |
| Regular FFS (high wait) | Recommended to be phased out post-pandemic | Recommended to be phased out post-pandemic |
| Regular FFS (Low wait) | DaysTable 3 Footnote 2 | 3Table 3 Footnote 2 |
| Capitated group – my doctor | Weeks-DaysTable 3 Footnote 2 | 1Table 3 Footnote 2 |
| Capitated group – not my doctor | HoursTable 3 Footnote 2 | 4Table 3 Footnote 2 |
| Physical Walk In | Recommended to be phased out post-pandemic | Recommended to be phased out post-pandemic |
| 811 Telehealth | Days-Hours | 8 |
| Employer-provided services | MinutesTable 3 Footnote 2 | 6 |
| Virtual Walk In (private pay) | Recommended to be phased out post-pandemic | Recommended to be phased out post-pandemic |
| Large Group Digital Front DoorTable 3 Footnote 1 | HoursTable 3 Footnote 2 | 2Table 3 Footnote 2 |
| 24-hour on-demand virtual careTable 3 Footnote 1 | SecondsTable 3 Footnote 2 | 7Table 3 Footnote 2 |
| Provincial/regional front door servicesTable 3 Footnote 1 | MinutesTable 3 Footnote 2 | 5Table 3 Footnote 2 |
811 should evolve into regional/provincial front doors that are connected back to existing primary care practices. Large groups should have their own digital front door and provide both good access and excellent continuity. All virtual care options, irrespective of modality, should be covered under PT fee schedules and not left as a separate private pay tier that undermines equitable access. Employer-based plans should be kept because of their immediacy and the role they play in supporting services such as mental health care, but they should link back to the primary care system for continuity (if desired by the patient). We discuss some of the payment mechanisms to make this happen in a later pillar. The shared goal should be to reduce standalone walk-ins that do not share information, while connecting walk-in clinics back to the system by better sharing of information.
Doing this as a two-step process is much less desirable than simply offering virtual-first primary care. Many large groups are currently looking at how best to do this. Because more than 50% of their visits are currently virtual (during the pandemic), this is much easier to imagine now than it was a year ago. But there are major challenges that need to be worked through.
Recommendation 24: All virtual care modalities should be covered under all fee schedules.
There is a corollary to this recommendation: any service left out of the fee schedule in a province will be privatized. Leave out provider types (such as nurses or Nurse Practitioners) or modalities (such as secure messaging) and there will be a private pay service. It would be a major shame if the Canadian health care system allowed a two tier, multi-payer, option in which the higher private pay tier was characterized by access to more modern service levels or technologies. The lesson of the pandemic is that care is care. Choice of modality should be left to clinicians and patients.
Recommendation 25: All patients who desire it should have same-day access to a virtual front door that connects them to the rest of the health care system. There are at least three ways that this should happen in 2021: provincial/regional front door, (large) group practice front door, employer-based assistance program.
There is a tough balance to be maintained here between creating good front door services that are tightly linked with larger primary care practices and providing large regional/provincial front door services that look more like revamped 811/Telehealth lines. Smart, larger primary care practices will want to control their virtual first front door. Yet, government will need to provide a safety net for smaller practices to ensure basic standards. This will not be easy. But it is certainly better than simply creating one front door that will inevitably become bureaucratic and clunky over time.
Some clinicians will object to same day as unnecessarily fast for quality care. While this argument could have been credibly made before COVID, it no longer can be. Infection control and public health tracing alone require same day turnaround.
I have included employer-based services in spite of the fact that they are paid outside of the public system for three reasons: 1) One-third of their services are for mental health and it would be foolish to shut off mental health services at this time; 2) They are broadly interdisciplinary and only a very small part of their services appear to be physician services; and 3) They already cover at least 4 million Canadians and so are in fact broadly available through employment. This is a bargain that Canada has long since made and accepted for other employer-covered services. Others will disagree with this opinion; I am not a legal expert. But that is my take. I respect the fact that some PTs will not agree with this.
Access in Specialty Care
Specialty care was also a mixed virtual care story during the pandemic. Initially, there were dramatic drops in visit volumes in every specialty. Globally, reports showed 40-70% of specialty care being cancelled.Footnote 2 Most specialties tried to force conversion of visits to virtual care. In many specialties there are still backlogs equal to a half a year of procedures or more.Footnote 13,Footnote 14
In some specialties, forced conversion to virtual worked well. Even very well. Returning to our earlier analysis of the four perspectives, it allowed specialists to operate in a low rules environment for a period of time, testing ideas that might work to care for patients they could not safely see in-person. It was a large but uncontrolled clinical trial of these new techniques. The evidence is still anecdotal, but interviews showed that several specialties completely embraced virtual care while others couldn’t make it work. The grey literature has been building in recent reports about eating disorders (healthydebate), cancer care (UHN Foundation), CHF medication titration (Medly), endocrinology (anecdotal from interviews), pediatric Crohn’s disease and other IBD treatment (anecdotal from interviews), well-baby care (Infoway), and post-surgical follow-up (Semple, JMIRFootnote 15). Clearly, there is a lot of academic work to be done to assess the large number of natural experiments that we are living through. Infoway has already taken excellent first steps to report on usage levels. Quality and appropriateness studies are underway at several centres. From interviews, it is clear that many specialty services have already decided to “not go back” and are communicating the same to their patients.
The biggest gain has been virtual mental health care, including through some free or low-cost programs in most PTs. In Canada and in other countries, mental health care switched to virtual (phone and video). The Mental Health Commission of Canada reported on the benefits of e- mental health care, such as patient empowerment, rapid access, and equal effectiveness to in- person care as far back as 2014.Footnote 16 Patients and providers report that they value the experience, some over in-person.Footnote 4,Footnote 17 Virtual mental health care has also helped to ease decades of shortages of providers by putting in place virtual care supports and technology tools that allow an expansion of panel size (the number of patients per clinician).
This same sort of expansion of panel size is reported by Medly for cardiac patients (at UHN). Specialty capacity expansion will be a priority for the next few years. Wherever gains can be made by leveraging new modalities, they should be encouraged. The good news is that there will be public money to spend if it increases capacity and helps solve the backlog of care.
The customer feedback on virtual care experiences has been widely positive. Infoway now produces a tracking service that interviews thousands of Canadians and provides fascinating ongoing, longitudinal data on patient and provider attitudes. The response has been overwhelmingly positive from both groups.Footnote 5
Several of our interviews with academic clinicians reported unpublished data showing that, in some specialties, care did not move back to in-person during the summer/fall between Waves 1 and 2. Prominent among these were mental health and endocrinology. We expect much more work to be done in this area and to be published in the next year. Obviously, what is appropriate post-pandemic may be different but the patients and providers we spoke with universally expect that some major portion of care will continue to be delivered virtually post-pandemic.
1. Specialist communications
There are at least four inter-related problems that need to be addressed in specialty care as we redesign for a 50%+ virtual care world:
a) Provider-to-provider communication among physicians: e-consults, messages, and advice
Remove barriers to this and make it the expected norm through secure email and/or a provincial messaging service. In many places, it is already happening regularly through everyday technology such as Microsoft Teams and WhatsApp. There should be a community norm established to enable this. Whether it is a “free” good paid as part of basic practice expectations in the “office visit” code (like record keeping) or an additional billable service is an ongoing debate. But it should exist and usually does. In Pillar 3 on remuneration, we recommend block funding of secure messaging to acknowledge these communications.
b) Provider-to-provider communication that may move or involve patients: e-consults and referrals
This should always be a paid service but need not be a major formal messaging system. E-referral and e-consult services are an excellent improvement and they had huge growth during the pandemic:
“Ironically, access to specialties was better because specialists were doing virtual. There were e-consults - all the specialists were taking them. They used to ask for the referrals for better reimbursement.”
- Consultant
E-consults are a fancy way of saying structured larger messages between peers that don’t “move the patient.” They require enough time and effort to write and respond to that providers need to be compensated. E-referrals are e-consults that result in the movement of a patient to the care of a new clinicians. But e-referrals run the risk of keeping us stuck in our historic “pen pal” or “snail mail” model of care. The formal communication can get in the way of collaboration. So, while we are excited about the rise of e-referrals and e-consults, we caution that it is only an intermediate point.
With virtual care as the norm, a quick discussion about the case while the patient waits or even a three-way call involving the primary care clinician, the specialist, and the patient are now feasible. In some parts of the country, e-consults are the “new normal”. This is a huge gain that some of our visionary telemedicine leaders have seen coming for a while. Once the consult or referral is no longer tied to a “letter” or “message” we are in a new space, a world in which problem identification and problem solving may regularly be closed in minutes instead of months (snail mail/fax) or days (e-referral or e- consult).
We should be aiming to “close the loop” by immediately involving the needed specialty where appropriate. This is possible with modern technology and is already being done in some provinces (e.g., RTVS in BC). Some of the patients interviewed clearly valued this option:
“Allows team calls, with 3-4 people on the same call sometimes – that’s been very helpful rather than trying to coordinate different people, different opinions, different times.”
- Patient
Stressed Stevie
Stevie is a 43-year-old in downtown Montreal who has worked long days their entire career. They are 30 pounds overweight, diagnosed with high blood pressure, diabetes, and anxiety. The thought of leaving their busy job to see their doctor adds even more stress. Last week, Stevie’s partner recommended that they seek therapy for anxiety.
Stevie phoned their family doctor for a refill of blood pressure medications. Rather than taking a long lunch break, Stevie was able to have their physician send the prescription electronically to the pharmacy on the ground floor of Stevie’s office. While on the phone, the physician also suggested that they send an electronic referral for Stevie to visit an endocrinologist and reminded them that they could view their most recent lab test through the online portal.
When Stevie got home, they logged onto their computer and found a specialized psychologist with availability. They schedule weekly video sessions, saving them a long commute each week.
c) Specialist-to-patient communication pre-and post-acute care
With the acute care usually being in-person, virtual services pre- and post- surgery or major procedures should be a default option based on clinical and access factors. Bundled fees can encourage this. No patient should be made to travel for follow-ups that can be safely done virtually. A number of services are showing that virtual follow-up is actually superior to physical in-person follow-up (breast reconstruction, meds titration for congestive heart failure (CHF), eating disorder follow-ups). Where appropriate, these communications should include other caregivers (both formal and informal).
d) Specialist-to-patient communication for chronic conditions and ongoing follow-up
Mental health and endocrinology are the two specialties in this category that are very enthusiastic about chronic condition management. CHF and chronic obstructive pulmonary disease (COPD) are both highly favourable, with some caveats. GI, respirology, and neurology are mixed. Oncology and others who have immunocompromised patients are very keen in a high CoPC environment, but may return to more physical care for operations reasons. Ongoing work will be needed on a specialty-by-specialty basis to develop these new standards of care.
Recommendation 26: All referrals and provider-to-provider consults must be made electronically by April 1, 2023. This may include conference calls.
2. Remote patient monitoring
Pilot projects of remote patient monitoring (RPM) have been underway for years across the country. RPM has scaled very slowly and has consistently served only a small proportion of the population, with numbers reaching 14,819 patients enrolled in RPM programs in 2019.Footnote 18 Like so many other digital innovations, COVID-19 resulted in a significant jump in RPM patients.
However, this jump has been overwhelmingly monitoring of COVID-19 patients.
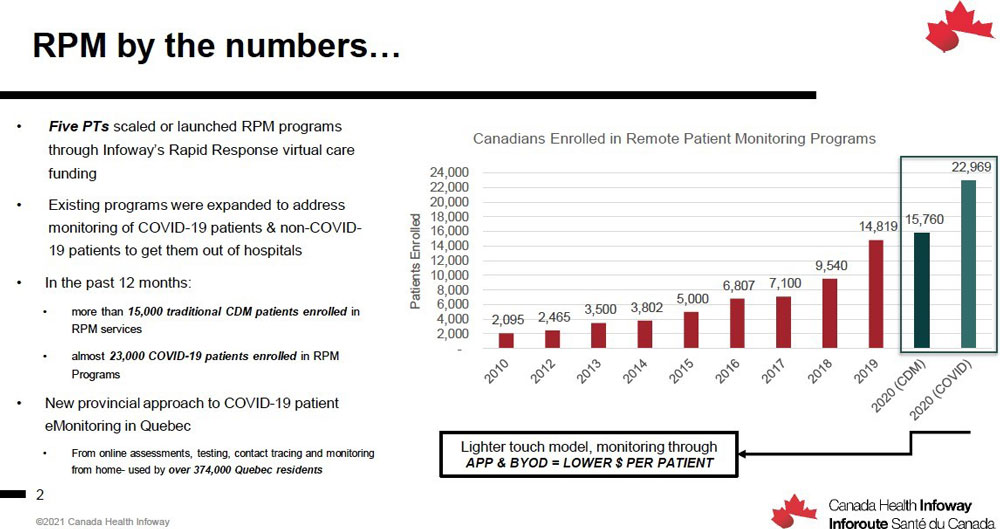
Figure 17 - Text Description
Remote Patient Monitoring by the numbers…
Infoway data on patients enrolled in remote monitoring programs across Canada
- Five provinces scaled or launched RPM programs through Infoway’s Rapid Response virtual care funding
- Existing programs were expanded to address monitoring of COVID-19 patients & non-COVID-19 patients to get them out of hospitals.
- In the past 12 months:
- More than 15,000 traditional CDM patients enrolled in RPM services
- About 23,000 COVID-19 patients enrolled in RPM Programs
- New provincial approach to COVID-19 patient eMonitoring in Quebec
- From online assessments, testing, contact tracing, and monitoring from home – used by over 374, 000 Quebec residents
| Year | Canadians Enrolled in Remote Patient Monitoring Programs |
|---|---|
| 2010 | 2,095 |
| 2012 | 2,465 |
| 2013 | 3,500 |
| 2014 | 3,802 |
| 2015 | 5,000 |
| 2016 | 6,807 |
| 2017 | 7,100 |
| 2018 | 9,540 |
| 2019 | 14,819 |
| 2020 (CDM) | 15,760 |
| 2020 (COVID) | 22,969 |
Scale has been the consistent problem with RPM. People have struggled to figure out how to translate RPM pilots into permanent programs. The challenge is primarily in resourcing.
Currently, there is little dedicated funding for RPM programs, so clinical programs are funded through temporary grants. It is not economically viable to rely on hospitals to staff people to monitor patients when, if those patients come in person to the hospital, the hospital would be paid. The hospital both loses a revenue source and incurs an additional staffing expense. Virtual visits have changed the viability of this model, since a physician can be paid to have a virtual consult with a patient. However, this does not solve the issue of continuous monitoring. Most effective RPM programs require one or several dedicated nurses to monitor the data from patients and to address and triage issues. Funding for this staffing measure is necessary to promote scale of RPM programs. This can also be remunerated through bundled funding approaches.
Like other virtual care initiatives, patients and providers should be able to choose the best monitoring system to suit their needs. Programs should be, where possible, software-based and allow the patient to bring their own monitoring hardware. This is hard to do because the physical plant of most hospital ambulatory care centres is viewed as a free good. Even associated staffing may be subsidized. In such a model, new programs have to amortize new investments but older programs are fully depreciated and have no capital costs and hence a large economic advantage. This capital advantage of physical care needs to be recognized and dealt with in a fair way to create sustainable programs. In the current environment with much physical infrastructure unusable due to high CoPC, we should be able to redress this imbalance.
Finally, funded programs should necessarily incorporate measures of PREMs, PROMs, and net promoter scores (NPS) to ensure the programs are effective and valuable to patients.
Recommendation 27: Scale up implementation of patient monitoring programs. Provide permanent funding envelopes in a system neutral way that allows competing hardware/software/services bundles to compete with physical visit monitoring in a fair way.
3. Clearing specialist backlogs
There is one important role that virtual care can and should play post-pandemic – helping to clear the backlog of procedural and surgical cases. Provincial/regional specialty virtual care centres could be established to assess and triage referrals. This would be an alternative to waiting for the pre-pandemic system to clear the backlog. This is highly desirable because many cases that are referred for surgical consults do not end up being surgical cases. They are diverted for further tests, for drug treatment, for physiotherapy, or are just monitored. Yet some surgeons are not inclined to see new referrals if their OR slate is full for the next nine months. This is understandable. But the health system needs to assess and clear this backlog.
Such a model would be similar to the RTVS model in BC or the Accelerated Specialist Access Program (ASAP) proposed in Ontario by Ed Brown several years ago. A virtual care centre would be opened with 6-10 specialties represented who would take case notes from primary care and use peer-to-peer communications and three-way meetings with the patient to assess, triage, and, if possible, recommend treatment options and further follow-up. Such a model would have the added bonus of creating the start of a central wait list for these services that could be used to aggressively purchase services from public hospitals during off hours to clear the backlog.
We have only begun to scratch the surface of virtual specialty care. Home monitoring tools and smart garments are both coming into mass production this decade. Holter-like underwear is feasible to monitor hearts. The ability of home care to address higher acuities has been greatly increased and this trend will likely continue. The home monitoring world has been slow to realize its promise but it is clear that we are getting much nearer to being able to realize it.
Recommendation 28: Create a temporary specialist access centre to promote rapid virtual access to specialty care. To reduce wait times, this incremental capacity will triage first by virtual to determine which specialist visits require in-person care.
Pillar 3: Remuneration
The fee schedule or tariffs were mentioned by the vast majority of people interviewed as being one of the key issues to be solved moving forward. Most felt that one key lesson of the pandemic was that we could always have done virtual care, but payment models prevented it. Many worried that there would be an attempt to close down codes again after the pandemic.
This worry seems misplaced. Virtual care codes cannot easily be closed for three practical reasons. First, patients really like the convenience and are not willing to give it up. Second, providers rely on the income it provides. Third, closing down some codes will create a second tier of virtual services in the private pay system. These three taken together seem fairly definitive. Any government that tries to close virtual care codes will face serious opposition from citizens, physicians, and fans of Canada’s health care system. There may be a few companies who would prefer that the codes close again (and a private tier be opened) but they are unlikely to have significant influence over policy once their financial interests are made transparent.
Payment for services
Resetting the fee schedule may be a simpler negotiation than past adversarial discussions between governments and medical associations. It must be a principles-based working agreement. The good news is that there is lot of fiscal room given lower earnings by physicians during the pandemic and the need to add back missed procedures from the past year. Taken together, the following three basic realities would, if recognized, allow for a better discussion.
First, there is money to spend. Both sides should spend it together in furtherance of better care. Develop a deal agreement that has shared benefits and penalties on the spending of those funds.
Secondly, there is a shared goal to modernize the health care system. Both sides of the negotiation must design the new system using agreed-upon principles. The following principles might be a starting point:
- Create a modality-neutral fee schedule: to the extent possible, the fee schedule should not drive choice of modality.
- Use capitation or salary where possible to leave the choice of modality to the provider and patient.
- Use bundled funding for major procedures where one service is at least 75% of the bundle. Include all pre-and post-surgical/procedural visits in the bundle regardless of modality. Allow patient and physician to set the cadence and modality of follow-up care, including asynchronous follow-up and remote patient monitoring.
- Pay for asynchronous care in a fair way and make it a normal, foundational service. Evidence is emerging to show that asynchronous is of equal clinical quality to in-person care for many health care conditions.Footnote 19
- Build from PT experience in Manitoba, Nova Scotia and elsewhere. Also consider international experience from Denmark and Kaiser Permanente (Northern CA.)
- Pay for basic provider-to-provider communications in fair ways that enhance system capacity.
- Allow for incorporation of accessible virtual front door services in a way that enhances continuity of care and avoids punishing capitated providers for out-of-network usage.
- Don’t micromanage an evolving innovation. Let innovative virtual care thrive to improve the quality of health services.
Thirdly, all medically necessary care should be in the fee schedule. Do not differentiate medically necessary care by modality. Care is care regardless of modality. Do not leave any bits and bites of modalities for private pay services.
There are many ways to pay physicians. Some ways are better than others, but there are no really good ways. It is not a science that lends itself to best practice thinking because any system of payment is subject to intentional or passive gaming. And even saints change their behaviours in response to incentives, sometimes without even realizing it. We have recommended the use of salary, capitation, and bundles that allow choice of visit modality to be decided by the physician in consultation with the patient and their family. This allows for innovation among existing modalities and allows next generation tech (e.g., Apple Watch, Hexoskin monitoring underwear, Virtual Reality, and others) to enter naturally into care processes as they mature and the physician judges them to be ready.
There is an ongoing concern that virtual care will reduce friction in the care system and be used in ways that overbill. We don’t see any data (yet) to support this concern. In one (as yet unpublished) Ontario data set reported by an interviewee, there were no wild increases in income by physician or specialty observed during the pandemic when we had high levels of virtual care. This indicates that physicians are not using virtual to overbill the system. However, there may be outliers, so we need mechanisms to monitor billing patterns and practices, deter physicians who misuse virtual codes, and, where appropriate, seek recovery of inappropriately paid monies.
Detect, deter, recover. Do not design the system around those (few) who will abuse it. Rather, conduct auditing to catch abuse. One model could be BC’s Billing Integrity Program.Footnote 20 We advise against fee-for-service (FFS) as a way of paying physicians because it necessarily drives use of certain modalities. We have seen this prior to the pandemic, when less than a few percent of providers were using phone and video. Payment constrained choices, but not in the interests of either physicians or patients. Terrible decisions were regularly made by good people because otherwise there was simply no payment. When payment models changed dramatically in March of 2020, behaviour followed quickly and necessarily. In many areas it will not willingly change back. But FFS remains a terribly imperfect way of paying physicians.
Any set of fee codes will have a hidden preference for one or the other of the modalities. Over the past two months we have had these conversations dozens of times:
“If we don’t provide incentive to the most efficient channel, then we end up pushing the supply and demand to less efficient channels, costing system more anyway. This is a simple equation – flatten. Leave incentive alone. Have virtual be the same as physical.”
- Consultant“My personal opinion is that FFS won’t work. Especially as we add asynchronous.”
- Health Policy Person“Phone is definitely our primary virtual care usage. One of our challenges is that our billing codes are the same for phone and video. That implicitly incents phone. Or it doesn’t incent video use. It costs more to set up a video call.”
- Family Physician“Be agnostic. Let’s talk about synchronous and asynchronous – shouldn’t matter. Realize majority of value creation is asynchronous in other industries. Why should health care be any different?”
- Consultant“We need to modernize our fee schedule. We need a table where this can be discussed collaboratively. Rewrite the whole collective agreement but virtual is a big part.”
- Clinician involved in past fee negotiations
So, we repeat: Don’t use FFS if possible. Capitate or salary primary care and bundle specialty care in a way that allows the provider (and patient) to choose their modalities for the non- physical parts of the care. But if FFS must be used, we recommend a ratio among the modalities as follows: $1 Messaging: $3 Phone: $5 Video; $5 in-person. We arrived at this ratio through discussions with well-informed interviewees. It is a starting point for discussion. There will be unintended consequences from any FFS ratio. Mitigation through rules and some common sense will be needed. This will be an ongoing process but here are some guidelines to start with.
Additional FFS Rules (if FFS is necessary):
- Phone can be only used for minor and intermediate assessment.
- Video can only be used if over half the visit is video.
- Intermediate for phone and video is only for visits over ten minutes (tracked and audited through EMRs).
- If an in-person follow-up is required after a phone or video visit, the charge for the initial virtual visit becomes a 50% code for triage.
- For example, a phone plus in-person would be the ratio of $6.50 (on our 1:3:5:5 scale) and a video plus in-person would be $7.50.
- An appropriateness guard rail might be considered if providers are billing both modalities at questionable levels. If systemic problems arise, the 50% number might have to be moved up or down so that it is not unduly influencing care decisions.
- A portion of visit fees should be paid as an information component and should not be paid to walk-in visits unless the visit record appears back in the patient’s chart through an API within a week.
- For illustrative purposes: A $32 visit with a virtual walk-in would become a $25 visit if the loop is not closed. The added $7 would be paid only if the record is forwarded.
Several clinicians interviewed strongly object to video being paid more than phone. They believe that this will create a strong incentive to use video unnecessarily and further hobble the system. These clinicians feel that there has been a false narrative favouring video and that we should stop overpaying for video. We have left in a higher video code as a recommendation but we are concerned by the potential for misuse. We acknowledge that video is becoming easier by the month, so this should be carefully monitored and evaluated. As phone and video reach parity in time and effort, this ratio may need to be changed.
Being principles-based should allow negotiators to come together at this time and design a system that will be consciously adapted in perpetuity. With near-term technology changes likely, this will be an evolving problem and will need good will on both sides to reach agreements that are in the best of interests of patients while also supporting providers and the health systems.
Recommendation 29: Enter into principles-based negotiations with an understanding that system modernization will be a shared responsibility over several years. Several possible principles have been offered.
Recommendation 30: Capitation, salary, and bundling of services are preferable as they allow modality choice and switching.
Recommendation 31: Where FFS must be used it should be paid in a ratio of 1:3:5:5 for messaging:phone:video:physical. Triage virtual phone/video visits at 50% (but not messaging).
Recommendation 32: Walk-ins fees should be split with an information portion equal to about 25% to encourage continuity of care. This should apply to physical and virtual walk-ins.
Recommendation 33: A formal system of communications codes should be established for peer-to-peer communications. They should include a block funding for basic messaging, e-consult, e-referral, and conference call codes that appropriately reward collaborating providers in a patient-friendly system.
Payment for virtual care tools
There must be clear responsibility as to who is paying for tools to support virtual care. The appropriateness of the provider choosing and funding their desired technology versus a hospital procuring a technology versus a region or province paying. There are advantages to each of the three but also serious issues. Getting good provider feedback on virtual care tools in the future will be as important to providers as choosing their office space was in the past. Really important. This is not something that most will want to leave to a provincial or regional panel to decide.
Yet, as a practical manner, we need tools that allow collaboration and interoperate well. PTs/regions/hospitals have access to capital funds to pay for those tools.
The costs for phone and internet connectivity are already built into physicians’ practice expenses. Building tools into EMRs is one sensible option. Most physician EMRs have, or will soon have, some form of multimodal communications technology embedded in the record system. These systems are viewed as a cost of practice for physicians.
Some PTs chose to pay for separate video platforms such as Zoom for Healthcare, Microsoft Teams, Google Meet or other during the pandemic. Providing software as a service (SaaS) platforms makes some sense as they will continue to develop and are often linked to email and basic office suites. Obviously, there is an infrastructure dependency here that will make this less suitable in some communities. We expect Amazon and Apple to both have offerings of this type in the near future.
There are also free alternatives, like WhatsApp and FaceTime, about which Privacy Officers will give opinions. But these are reported to be entirely serviceable from a clinical point of view.
Some PTs are looking at designing video platforms with a virtual waiting room and are investing significantly in these systems. With the evolution in modalities discussed above, we do not recommend large infrastructure investments in basic video platforms.
Only continued change is certain. As this technology improves, providers and patients will easily be able to switch to better and preferable alternatives if we keep switching costs low. Some technologies have greater technical requirements, such as remote monitoring platforms, wound care tools, AI-enabled triage, and decision support tools. These technologies are rapidly developing and will be more expensive and have higher associated safety concerns. At the same time, the price for these technologies is dropping dramatically as Moore’s Law has an impact as in every other industry: speed and capability increase every couple of years, and costs drop. We can imagine the consumer electronic revolution in medical care and particularly remote monitoring further crashing prices. Keeping switching costs low needs to be a priority. This means favouring software over hardware models.
These tools should be supported but not procured centrally, as the procurement process inhibits innovation and risks providers being forced to use established solutions. Providers should be empowered to use digital tools as they evolve that demonstrate clinical value and safety to improve the care they provide.
Recommendation 34: Do not make large infrastructure investments in basic video platforms. Keep technology switching costs low and avoid vendor lock-in.
Recommendation 35: Develop a funding model for providers and hospitals to purchase and administer new digital technologies that work for them and their patients. This probably means a Technical Code or “T-code” that provides a small but appropriate amount of funding to pay for infrastructure expenses.
Pillar 4: Quality, appropriateness, and safety
Quality, appropriateness, and safety are paramount considerations as we transition to including virtual care as a permanent element of Canada’s health care system. This is going to be a tough set of discussions, and one that doesn’t have simple answers. Here are some of the perspectives we heard in interviews:
“When the patient calls you are giving advice not physically examining. Sometimes I enjoy the novelty. Sometimes I really worry.”
- Family Physician“Some people feel like they don’t get the same level or quality of care, while others feel as though they are – it’s a tough line to draw”
- Fee negotiator“Virtual care is great for safety of not going in person during this time and other times (e.g., flu season). for people who are not as mobile, it is much easier to have virtual care. You don’t have to worry about transportation, or spending whole day between transportation and the waiting room.”
- Patient“There is no baseline for the physical system for us to compare the virtual system to. Do office visits every six months work? I have no idea. It is just the community standard?
- Specialist physician“We have to re-think health care – how is that changing, then apply the technology to it. How do we escalate this conversation about guidelines on appropriateness”
- Health Policy Person“There is a lack of clarity around who is responsible for setting these standards. It is a bit of a hodge podge and there is a dearth of existing guidance for virtual care.”
- Specialist physician
As a non-clinician wading into this area, I have been amazed by the ability of clinicians to judge for themselves when they can and cannot do certain clinical things virtually. I confess that I am a bit in awe of how difficult this must have been and the stress that many clinicians have had to take on to fly to these high levels of virtual care without the safety net of clear medical society guidance.
During the pandemic we relied on existing standards and allowed clinicians to use their judgment given their scope of practice. This was a reasonable solution given the high CoPC and the urgency of the situations. There are de facto standards of care being set in the field every day.
These are built on top of community norms for physical care. Many of these norms have been passed down from generation to generation without examination. The question for policy makers is how we incorporate those norms and standards into a more formal set of standards of practice for virtual care.
Setting standards across specialties
We need a formal method to reset the baseline for our standards of practice. This should involve a specialty-by-specialty review of what services are appropriate to provide by secure messaging, phone, video, physically, and through monitoring technologies. Virtual care appears to fit differently into each specialty service. The Canadian Medical Association (CMA) and Royal College of Physicians and Surgeons (RCPS) both have legitimate roles to play in governing this, as do individual specialty associations. Given the CMA’s past role of looking at Virtual Care, the simplest thing may be for them to act as a convenor and for the RCPS to bless and formalize outputs. These specific details need to be agreed on.
There are a few questions that probably need to be specifically examined and reported on for each specialty and sub-specialty:
- When is physical contact necessary to make or confirm a diagnosis?
- Can that physical examination be reasonably done by another person either licensed or unlicensed?
- Can a remote measurement substitute for the physical contact?
- When is visual contact necessary to make or confirm a diagnosis?
- To what extent is a physical contact important to establish a relationship with the patient and/or to understand other factors such as social determinants?
Other questions may be vitally important for certain specialties and much less important for some others. Virtual care may often be the better way of maintaining a closer clinical relationship by allowing a known provider to continue to care for a particular patient. An example of a standards-based approach is the OTN Virtual Visits Solution Requirements, developed in November 2020 to support providers in choosing virtual tools that meet various technical, privacy, and interoperability requirements.Footnote 21
Recommendation 36: Specialty-by-specialty review to determine which services are appropriate to conduct virtually should be undertaken by the Canadian Medical Association in concert with the Royal College and other specialty associations. This review should be explicitly separated from reimbursement review and remuneration discussion.
There is a related question of what we will do with genuinely bad actors. We hesitate to raise some of these examples without any evidence that they in fact exist, or at least not in any way that has yet seen the light of day. Each of the four fictitious but plausible examples was given during interviews:
- A LTC medical director who switches to virtual-only for reasons of convenience when the home they supervise is hit by an outbreak, refusing to see patients in-person even when that would be more appropriate.
- A PCP who pumps fee-generating utilization by doing multiple text messages, phone, and/or emails interactions in the same episode of care, billing for each one, or uses video instead of phone for higher reimbursement.
- A clinician unwilling to visit a First Nation community due to fear of infection, instead insisting on virtual care even though in-person would be safer for some patients.
- The hollowing out of a small town’s general internal medicine and general surgery patient volumes through virtual visits to urban specialists.
Are these real concerns? Maybe. It is undoubtedly true that with new care options, there will be new ways for bad actors to act badly. These should be dealt with in the same way that they were in the pre-pandemic physical care world. As noted above, our overwhelming experience from interviews and data have been that clinicians acted faithfully in the best interests of their patients and to the best of their abilities.
One interesting aspect of virtual care is that it creates an audit log by virtue of the electronic communications involved. If well designed, this creates transparency. Transparency and even patient simulation will be needed for medical education. It could also be used for real time practice review and mediation. It will send shivers down spines when I say it but: “Calls may be monitored for quality and training purposes.” Obviously, that one is going to take some real thought by medical schools, training programs, privacy commissioners, and licensing bodies. But there are also real opportunities to build in feedback and better coaching of “phone-side manner”. We return to this issue in Pillar 5 on change management.
Quality by modality
Phone dominated among modalities, consistently reported as representing upwards of 90% of virtual care across the board. Opinions on appropriateness and quality by modality vary by person. Interviewees raised concerns about whether some care is appropriate to conduct by video but not by phone. There is often a presumption that care by phone is a lower fidelity service than care by video. This presumption needs to be tested. It may well be that we have been overcomplicating virtual care for a decade.
“I am shocked at how much we can do by phone. In part because we know our people and we have a solid EMR. We always share our patients among our group (of 7).”
- Rural Family Physician
Stable international systems that have long history with virtual care were providing over 50% of care by phone and secure messaging pre-pandemic (e.g., Kaiser Permanente Northern California). However, they also use video at a rate higher than Canadian systems during the pandemic. Our expectation is that video will rise as we sort through technology issues. We also believe that secure messaging is highly useful and often the easiest accessible high-quality care for some issues. Its use should also rise in Canada.
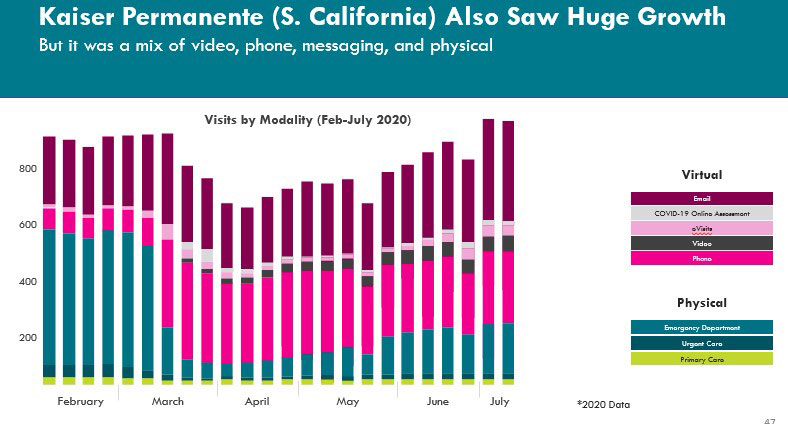
Figure 18 - Text Description
A bar graph that shows number of visits by modality at Kaiser Permanente between February 2020 and July 2020. Kaiser Permanente (South California) saw huge growth in virtual care use (e.g. email, COVID-19 online assessment, eVisits, video, and phone) and a decrease in in-person care (e.g. emergency department, urgent care, and primary care).
Omnichannel is a word used in other industries for multi-modality communication and interactions with customers. A retail service is omnichannel if consumers can access the service through phone, website, app, email/SMS, and in-person. We all know from our daily lives that often these customer experiences are mostly terrible and too rarely excellent. But none of us want to go back to the time when banks only saw us between 10 and 3, and we only booked airplane tickets at something called a travel agency.
Our interviews with physicians turned up the surprising finding that many doctors are already improvising omnichannel during the pandemic. Some specific examples:
- Physicians who said they were using FaceTime and WhatsApp are starting the “call” as voice only, but switching to in-App video when needed, and then back to voice.
- Clinicians spoke of telephone calls in which they asked that a photo of an area of the body be taken and sent by email.
- Physicians discussed good and bad practice in being able to switch between phone and video. Apparently, many of the integrated video apps require very heavy administrative and tech support.
- Patient expectations are different for video interactions vs phone vs physical interactions. They are much higher:
“If you’re an endocrinologist and you’re checking in with someone’s bloods, get them on the phone, know it’s secure. Takes a couple minutes, say hello and goodbye, you’re done. Same thing on video takes at least 10 minutes”
- Specialist Physician - Email and secure messaging are being widely used in some capitated practices and anywhere that a compensation workaround can be found.
- Many clinicians and some provinces report that texting and peer-to-peer services are being used regularly without any associated payment.
We are living in a transition age and so we need to be humbler in a time of very fast-paced technological change: we don’t know it all. In addition to the technologies widely in use, voice recognition, consumer wearables (including underwear) and possibly virtual reality are three more modalities that will likely be in widespread use in health care in the next five years. There may well be others. We need to trust providers and patients to determine which channel among the omnichannel to use in which circumstance. Care is care regardless of how it is delivered. We need to have faith that providers will make ethical choices in consultation with their patients and based on their understanding of their patients’ best interests.
Recommendation 37: Take care to not reintroduce unneeded regulation into the patient-provider relationship around choice of visit modality.
Quality by vendor
Quality and appropriateness also raise questions about the specific technology that is being used. Is it appropriate to allow providers to choose the technology that best fits their practice, or do we risk quality issues with too much leeway to provider choice?
“I love email but worry that my inbox is cluttered with other stuff and I could miss something. I forget to copy and paste; what if I get hit by a bus; you can’t analyze it properly because data don’t come in the right format (e.g., xls vs photo of a piece of paper)”
- Family Physician
The freedom of email may not be well-suited for clinical messaging with patients. Or it may be just fine. Providers need a high-quality way of making sure that their secure communications are acted upon and, where important, recorded. Yet we also need to not overcomplicate front desk functions around scheduling and quick updates. This is going to be an ongoing discussion for some time. We will repeat a couple of principles here: It should be driven by physician- and patient-centred approaches and not by reimbursement policies. Again, this means a determination of whether messaging can continue to be safely used for a particular service that is separate from the question of whether it is a paid service.
Solid, secure, clinical email addresses that are separate but also well-run are very useful. We recommend this be a condition of licensure, as discussed in Section 3.6. It is not at all clear that services developed in-house are a good idea. Providers report that they are clunky. They appear to be expensive. There are artificial barriers being placed on the ease with which email inboxes can be combined on a single device. Many knowledge workers have two email accounts – one personal, one professional – either as a condition of their employment or to protect their own privacy. Some carry two devices as a result. Secure clinical email/messaging separate from administrative email is an important component of a safe high-quality system. Getting this moving while also keeping future switching costs low is important. Do not lock into your email plan on a multi-year contract.
Recommendation 38: Secure clinical email for patient and provider-to-provider communications should be available for purchase for all providers. Policy makers should consciously future-proof these messaging systems by keeping switching costs low in the future.
Reporting patient measures on experience and outcomes
PREMs and PROMs need to be developed. There are other commentators and whole national agencies working on these problems and they will put forward solutions.
Well-designed software can collect outcome measures as part of the patient process. Experience measures already exist in the software world. They are robust and validated and should be incorporated into health care’s PREMs. These include NPS, user ratings on App stores, raw usage numbers, dropped call numbers, call satisfaction numbers, among others. Using software measures allows other companies to enter health care more easily. Zoom’s relatively high customer satisfaction rating was important to its selection at the start of the pandemic. If they had to create a new industry-specific experience measure, this would have blocked entry to the market. This is partly what happened with “meaningful use” in the US for Hospital systems.
Epic, Cerner, and friends were able to create barriers to entry around key specifications that even tech giants such as Microsoft and Google were unable to easily compete against. Good open competition means that we design PREMs so that great multi-industry software players can play well in health care and not be excluded.
Outcome measures (PROMs) should be a normal part of well-designed software processes and should actively enable the clinician in evaluating the patient, setting the plan and monitoring its success.
Recommendation 39: Understand current customer outcome and experience measures being collected by major Canadian software vendors who compete in the health care space and incorporate them into our national PROMs and PREMs programs.
Pillar 5: Change management
A new approach to Change management is needed
For nearly 60 years, since Everett Rogers first published Diffusion of Innovations,Footnote 22 change management practitioners have used Roger’s five consecutive waves of adopters to inform and guide the implementation process. It is a familiar storyline, of early adoption of pilot projects followed by scaling of the “innovation”. Also familiar is getting stuck in the early phases.
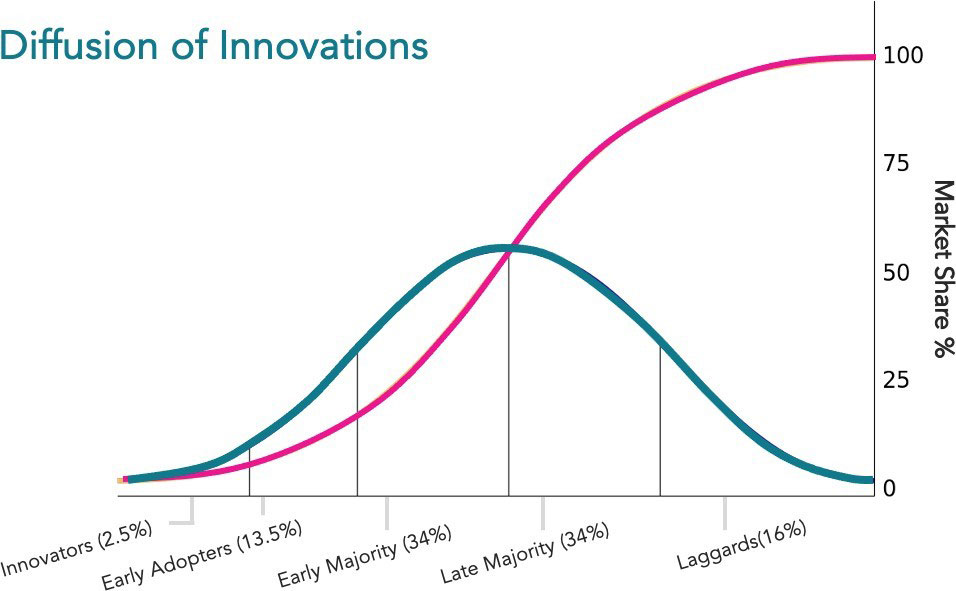
Figure 19 - Text Description
A visualization of Everett Rogers’ Diffusion of Innovations. Points along the x-axis include innovators (2.5%), early adopters (13.5%), early majority (34%), late majority (34%), and laggards (16). Points along the y-axis include 0%, 25%, 50%, 75%, 100% market share. With successive groups of consumers adopting the new technology (shown in blue), its market share (yellow) will eventually reach the saturation level.
That did not happen this time. Before the pandemic, innovators represented nearly all the uptake and had stalled at just a few percent for several years. Virtual care was bumping along, and we spoke about it as an adjunct therapy. Once the pandemic hit in early March 2020, we collapsed the last four categories, early adopters through to late majority, in three months. Today, ninety percent of providers have adopted virtual care in some form.
The old change management paradigm is not useful in the case of virtual care. As we look at health care in Canada, this shift will impact us all in some predictable and unpredictable ways. Change management will not be needed to encourage uptake. Instead, we may need to support mechanisms that speed the dissemination of leading practices.
For example, we should share process learnings and remuneration schema that support conversion from one modality to another in the same visit, shifting from phone to video and back again. To a much greater extent providers will manage their own change. We need policy and funding to play a supporting role. They will choose tools that work for them and their patients.
Some specific considerations include:
- Create an environment that keeps switching costs low, avoiding mega projects based on a particular technology.
- Make it easy for providers to use digital tools by providing recommendations on which tools meet safety and quality standards.
- Respond nimbly to the unintended consequences (positive and negative) that will arise as we move to the new normal.
- Enable provider choice of tech. What works best for a provider depends on a multitude of factors, such as the type of practice, type of care they deliver, where they’re situated, the patient population they serve.
- Work with enthusiasts to develop excellent models of care and spread them widely.
- Support the laggards for a period of time. They will eventually either adopt or be forced out of the market as the majority integrates virtual care permanently.
- Set up evaluation and measurement systems now to evaluate new models of care against the Quadruple Aim.
One difficult question is what baseline we use for evaluation? As several interviews pointed out, there is no great wealth of data to support practice standards as they existed in 2019. Why did a given specialty care patient get a 6-month in-person follow-up exam as opposed to 3-months or 9-months? Realistically, six months was usually plus or minus 60 days anyway. Given the lack of data, how do we compare that to our now-customary practice of 6-month phone call, or a nurse video visit, or a monthly secure messaging check-in? As we have discussed in the personas and half a dozen other examples throughout this report, there are now two baselines for many clinical pathways.
Evaluating practice standards will require a “double baseline” review process. Investigators will need to look at practice patterns and standards pre-COVID vs during the current pandemic, and determine where there are enough data to judge where further study is needed. In examples discussed above, like management of IBD and management and medication titration of CHF, there has been a clear shift towards much more virtual care and nursing involvement in that virtual care. Clinicians and patients may be unwilling to have a physical-visit-only control arm that represents 2019 practice. A double baseline approach is a first step towards resolving this question as we set up the specialty-by- specialty reviews that will be needed over the next several years to manage change in practice patterns.
It is fair to say there is a huge amount of work in this space, so coordination, alignment, and support are needed to marshal efforts across the country.
Recommendation 40: Assign Healthcare Excellence Canada the lead role to scale and spread virtual care innovation in clinical practice across Canada. This should be done in partnership with Canada Health Infoway who will provide guidance/support on securing/implementing the tools.
Recommendation 41: Assign the Centre for Digital Health Evaluation as lead in coordinating the evaluation of spread and scale of virtual care.
Medical Education and Virtual Care
Medical education using virtual care has been a major challenge during the pandemic and also represents a huge change management opportunity. The challenge comes from needing to extend learning opportunities to ambulatory care settings where virtual care makes up a large proportion of care delivered. The opportunity is that these learners are all young technology natives who are generally very comfortable with interacting through a variety of modalities and systems.
Key informants mentioned several ideas about how to use virtual care technologies. These included:
- Learners start the phone or video interactions, with supervising clinicians either joining midstream and/or coming in at the end of the history collection and diagnosis process.
- Learners drafting responses to secure messages for review prior to sending.
- The role of patient simulation in learning and the ease with which virtual interactions can be simulated.
Digital natives moving from service to service throughout their residency are also likely to be an important source of ideas to inform best practice. We have seen this in the past with EMR usage, where digitally savvy learners actually coach attending physicians. We may well see a similar phenomenon in virtual care.
Moving forward, the learnings from the 2020/21 academic year will inform the redesign of medical education and the education of other professionals. This could be an area for major innovation and the introduction of big new ideas. What is the role of virtual reality in medical education and in providing an excellent clinical experience? Will we re-enter a world in which the large operating theatre is (virtually) open to students? Could we extend that to more aspects of learning with a virtual theatre experience, observing the best clinicians as they practice their craft? How does patient rounding in white lab coats work online?
Recommendation 42: A detailed review of health professions education in the time of virtual care should be undertaken by suitable academic groups.
Pillar 6: Licensure
In-person delivery of care has historically made cross-jurisdictional licensure less of a challenge. With traditional in-person care, there is an imposed practical limit on the ability of providers to be paid for serving patients who live in other provinces. For providers where this limit on physical presence doesn’t exist (e.g., radiology), there have always been anecdotes of Canadian physicians in exotic locations providing services to Canadians and being reimbursed by the provincial plan. Similarly, professional groups who do not have strong provincial licensing bodies (e.g., speech pathologists) regularly provide services across provincial borders. But it has been a minor issue, and so long as these providers are licensed and providing quality service, no one worried much.
Virtual care makes it possible to provide services across Canada, irrespective of physical location. Easily. There are huge advantages to this. It could solve labour shortages. It could allow off-hour coverage. It could allow better coverage for English, French, Indigenous, and global languages. It could foster competition and cause prices to drop (if competition were allowed). It could create a global industry that would be an engine for economic development.
Alas, all of these ideas run into some predictably Canadian roadblocks: (over)-regulation, provincial jurisdiction over health care services, and squeamishness about health care as an economic driver. As one key informant put it: this becomes a constitutional debate. Virtual care is today an integral part of health care. A national approach to licensure (using the Canadian securities industry models and the Australian model as examples the CMA has investigated) is the comprehensive solution to support virtual care. Anything else will be a patchwork and may lead to a fractured regulatory system. Given this, my overall recommendation for this section is that collaborative work continue apace toward pursuing a national approach.
Recommendation 43: Collaborative work should continue apace toward a national approach to licensure.
However, there is an urgent need to move forward on some items in the short term, where licensure must be improved for the sake of the country and its residents. The following recommendations are divided into process and specific use cases.
Virtual requirements of licensure
Licensure should be redefined by all Colleges and licensing bodies to recognize the importance of virtual care as an integral part of caring for patients and communities. Patients who prefer virtual care want rules that require providers to do virtual care. Right now, if a provider does not want to do it, patients are powerless to change that, and switching providers can be difficult in some parts of Canada.
While providers cannot be forced to provide virtual services as well as physical services, standards of practice should be changed to reflect the fact that at least in times of medium-to- high CoPC, no provider can safely provide care in Canada without providing virtual care. As a practical matter every provider should henceforth be registered with a secure email address as a condition of licensure. This would enable secure communication with patients. As discussed above, the health care system must modernize, and licensing can enable this. Fax communications should cease. Similarly, all service providers should be henceforth required to provide and/or accept electronic prescriptions and electronic (standard) lab requisitions. All requests for referrals or consults must be made electronically.
Virtual care is today an integral part of health care, and these recommendations should be implemented immediately. Phase in period through March 31, 2023 should be allowed.
Recommendation 44: All providers must register a secure email as a condition of licensure; fax machine will no longer be considered a secure form of communication.
Licensure should be used as a tool to enforce these recommendations:
Recommendation 12: All requisitions/results for standard lab tests should be sent/received in a usable digital format by April 1, 2023. No payment should be made for requisitions or results sent/received by paper.
Recommendation 13: All prescriptions should be sent/received digitally by April 1, 2022.
Recommendation 17: A temporary paper remediation service should be made available to service providers (at their expense) to allow them to meet patient information requests during FY 2022- 2026 to ease transition to a fully digital world.
Recommendation 26: All referrals and e-consults must be made electronically by April 1, 2023.
Licensure and Continuity of Care
There are certain use cases for cross-jurisdictional, virtual care licensure that must be resolved to promote high quality continuity of care. Reciprocal billing and remuneration should be adjusted as necessary to enable these types of cross-jurisdictional care.
1. Pre- and post-specialty care follow-up
To achieve our goal of continuity of care, we should allow proper follow-up virtual care by the treating provider for patients who return to their home province, after having had procedures delivered in another PT. It is common in parts of Canada for patients to travel across provincial borders to receive certain specialty or surgical care. Post-treatment or post-surgical follow-up across borders should be permissible under licensure.
Consider this specific example from our key informant interviews. A surgeon in Manitoba must be allowed to bill for appropriate virtual follow-up post-surgery for Northwest Ontario patients. Preferably this should be paid as part of a bundled surgical code. Otherwise, post-procedure follow-up care, provided by treating physicians to patients who return to their home jurisdiction, should be specifically included in the fee schedule. Currently, that patient would be referred for virtual follow-up care to a new specialist in Toronto who has little information on their procedure. Licensure also restricts Saskatchewan patients from following up virtually with their treating specialist or surgeon in Alberta. Instead, patients must physically travel across the Alberta border before they can make a virtual follow-up call. This is absurd.
Recommendation 45: Patients who receive specialty care across provincial/territorial borders should have the right to virtual follow-up care with the same provider and access to their health records, across PT borders. Licensure should allow this. Privacy rules should allow for cross-boundary sharing of health information at the request of patients and their providers.
2. Cross-provincial university students
Similarly, students who attend school outside of their home province continue to be residents of their home province for the purpose of health care, remaining enrolled in their home province’s health plan. Think about College Casey. The Reciprocal Billing Agreement notwithstanding, in practice this often limits their ability to receive covered services from a full-service family practice in the province where they go to school, given that they may first have to pay out-of- pocket and then seek reimbursement from their home province. Also, they may not be able to find an appropriate provider accepting new patients. Often their health care needs are very occasional. Thus, they may be limited to a student clinic or paying for a walk-in clinic visit unless home for holidays. Students should be able to have virtual visits with their own family physician in their home province, who has access to their full record of care, to support continuity and quality of care.
College Casey
Casey is an Albertan in first year university at Western University. They maintain their Alberta health coverage and driver’s license while completing their studies out-of-province. Casey has a sexual health problem that can be solved through antibiotic treatment but has had a previous negative reaction to an antibiotic. Casey accesses care either through an in-person or virtual walk-in clinic.
During COVID, Casey contacted a virtual walk-in clinic, who sent them for a physical encounter to test for STIs. Casey received lab tests through the online portal, and the walk-in doctor reached out to discuss a treatment plan. However, the provider at the virtual walk-in clinic is hesitant to prescribe treatment without knowing which antibiotic they reacted to previously.
Because of licensing issues, Casey cannot have a virtual visit with their primary care provider back in Alberta who has been their provider since they were an infant. Instead, the walk-in physician in Ontario must request the information from their family doctor, delaying Casey’s treatment. The record from the walk-in visits will not link back to Casey’s health record in Alberta.
Recommendation 46: Out-of-province students should have the right to virtual visits with their own physicians in their home PT. Licensure should allow this.
This same right to continuity of virtual care should also be examined for seasonal and migrant workers. It may be that these workers have good access to employer-provided care. We did not investigate this.
3. Accessing French-speaking specialists
Bilingualism is core to Canadian identity, yet people often have to meet with English specialists in provinces outside of Quebec. For example, in New Brunswick, there is a significant French- speaking population but there are few specialist physicians who practice in French. To promote high quality care, respect language rights, and support patient understanding of the care they are receiving, patients should be able to virtually access specialist care in French. This means, for example, allowing francophone patients in New Brunswick to make virtual appointments with specialists in Quebec.
Recommendation 47: Licensure should allow French language speakers virtual access to a French-speaking specialist in another province rather than an in-province English-speaking specialist and vice-versa.
4. Accessing culturally safe care
Too often, Indigenous communities are treated as a monoglot pan-Indigenous community. Interviewees pointed out that there are over 200 Indigenous languages recognized in Canada. Virtual care should mean that Indigenous peoples can receive culturally safe care in their own language much more frequently. This should be a priority for the federal government and for provinces. It can be supported by available technological solutions that allow much wider access to translation services. Virtual care allows for an expansion of culturally safe practices and for the inclusion of gifted elders and healers in care processes.
Recommendation 48: Licensure should allow pan-Canadian practice by clinicians who speak Indigenous languages. Consideration should be given to creating a Centre of Excellence in these services.
These six recommendations are admittedly “half a loaf”. But a half a loaf is better than none. Some key informants suggest that the institutional inertia on licensure is such that normalizing interprovincial virtual health care services is years, if not decades, away. This will be passively resisted by existing interests that cannot be easily addressed. Better to take these four concrete recommendations and implement them now. They are all completely clear cases where all principles that Canada holds dear are reflected in the examples.
Section 4: Recommendations, implementation issues and governance
Governance and Implementation Issues
Canada’s health care system(s) are managed, organized, and delivered by provincial and territorial governments. Implementation of the recommendations in this report would ideally be administered nationally with shared responsibility among PTs, PCHOs, and Health Canada. This will require some discussion and organization at and after the June 2021 Summit. We recognize that this is not a simple set of issues.
We offer one set of observations around the current structure of the digital health industry in Canada and how it needs to be managed to best serve the Canadian health care systems and its patients. Gone are the days of writing cheques to small and growing vendors who employ fewer than 100 people and are trying to develop a stable set of products. Successful policy has created a robust and growing industry that now employs tens of thousands of people across the country.
Many of these companies are now international players. Health care is a growing export industry in the same way that education was two decades ago. These will be good clean knowledge economy jobs.
The role of government changes in this new decade. Health Canada will need to restructure the PCHOs for this new reality. The good news is that these organizations are all well aware of this and are doing work to prepare. There is a solid framework on this topicFootnote 10. A new industry goes through three phases over a period of decades: 1) Subsidize, 2) Stabilize, and 3) Encourage Competition.
Before the pandemic, Canada was generally still in the Stabilize phase. With the incredible level of investment of the past eighteen months, we are now firmly in the Encourage Competition phase. This means a very different role for governments going forward. Figure 20 shows of the model.

Figure 20 - Text Description
The evolution of innovation is a three-step framework describing the role of government innovation according to Christenson and colleagues (2010). The intent of government intervention to influence and regulate industries in the public interest evolves through stages:
- Subsidize: the foundation of industry. To support early-stage industry government makes investments in the coalescing of an industry.
- Stabilize: strengthening the companies involved. Once established, governments intervene in a market to stabilize it through regulation and policy to ensure quality and performance.
- Encourage competition: to reduce prices. Once quality and stability are assured government policy and regulations shift to improve affordability and convenience.
I have been involved with Infoway since 2004, very early in the “Subsidize” phase, when I led the management consulting team on the six-domain strategic plan that year. Infoway and the PTs established the foundation of an industry. Infoway set up domains to fund and created a gated process to bring through early projects and then to scale and spread those projects across the country. Diagnostic Imaging, Labs, Drugs, Registries, and other domains were funded. Hospital and physician systems originally were not. An EHR Solution Blueprint was published and then updated to help guide the sustainable development of interoperable EHRs across Canada.Footnote 23 Health informatics programs were encouraged, and vendors were given signals that a large subsidization was underway. Money flowed. In later tranches, Infoway expanded to wait times (although that money was repurposed), public health, and telehealth. The provinces were ahead of Infoway in some parts of the country in funding physician systems and hospital systems.
In the Stabilization phase, Infoway and the provinces spoke about spread and scale. New funding was made available for physician systems and then for telehealth. The X-prizes were awarded for innovation and surprising upstarts were brought into the fold and into the architecture.
Meaningful use in the US Stabilized the hospital EHR market and collapsed it to a few dominant players. McKesson, Siemens and GE all left the Canadian market. The remaining vendors were Cerner, Meditech, Epic, and Allscripts, plus a few specialty players in Quebec and eastern Ontario. In the physician desktop market, the telephone company and the drug store acted as consolidators: more than 18 small EMRs were collapsed into what are now three major competitors. In other market segments, national players emerged such as PointClickCare and AlayaCare. In the case of drug prescribing, a new stable entrant was created by government: PrescribeIT. There arose around this stable foundation another dozen companies with scope and scale who now serve the industry.
Moving forward, the job to be done by government is a different one. Christensen clearly shows why past approaches will not work in this decade in digital health in Canada. Using these past approaches of cheque-writing and central planning will hurt rather than help progress in my opinion. Buying the wrong technology actually hampers adoption of better technology by the clinicians and patients who use it. Great care needs to be taken to not allow agencies of government to offer competing products in situations where there are good commercial products available. Infoway and the other PCHOs need to manage competition among Canadian and global digital health care players who are providing services to health systems, employers, clinicians, and directly to Canadians. The Competition Bureau’s mandate is to ensure Canadian businesses and consumers prosper in a competitive and innovative marketplace. Infoway may need to develop a much closer working relationship with the Bureau. CIHI, HEC, and CADTH each will play important roles in managing this large and competitive industry for the benefit of Canadians.
When we talk about standards in this context, we need to be realistic about evaluation and credentialing programs at the provincial and territorial level. Global vendors may not show up to be evaluated or be willing to play by our provincial rules. There will be trade issues that need to be considered and interprovincial commerce issues. There is also the issue of job creation and ongoing industry support.
” …we should be approaching virtual care with as little regulation as possible (save for regulation on the actual medical practice). The problem with regulation is that government adopts an approach where they amass large amounts of unnecessary requirements on the technology application and then inserts itself into the business of UX design - which in effect stifles innovation and time to market - there are many examples of this…”
– Software executive
Infoway’s currently voluntary RFQ process is a solid start towards getting a simple common set of requirements. Vendor interviews suggested that what most of these companies want is a clear set of rules that govern commerce in this important sector.
It may well be that the current collection of Pan-Canadian Health Care Organizations is not fit for purpose to manage this new role. Health Canada will recognize that similar recommendations came forward from Naylor’s and other reports that looked at Canada’s competitiveness in health care (e.g., NaylorFootnote 24, Forest and MartinFootnote 25, Thompson (unpublished)).
Absent constitutional reform, the best working solution is a solid arrangement under the CDoM and the FPT VC Table that creates a national system and supports national PCHOs to manage competition and standards across the country.
Recommendation 49: Health Canada must review the mandates of the Pan- Canadian Health Care Organizations to ensure that they provide clear national governance of virtual care and the digital health industry. With support of PT governments, an agreed structure for managing national standards needs to be developed.
Note on Standards
A well-run health system and public health safety and surveillance demand that this issue be dealt with now. That is why we recommend a secure email for all, usable digital format for lab tests and prescriptions, patient right to data, hospital and physician reports on request, and other basics.
This report has for the most part respected the boundary around the foundational elements: Privacy and Security, Data Standards and Integration, and Technology (procurement, standards, and operations). At several points we comment on these from a policy point of view, but we have stayed away from detailed execution issues. On standards in particular, we have used the phrase “usable digital format” and the phrase “readable and searchable” to describe the idea that a standards-based approach to these issues is absolutely needed. It is. But we are respectful of the fact that it is a difficult set of issues. We are reminded of the old joke about standards. Standards are like toothbrushes; everyone has one and I don’t want to use yours.
Here are some thoughts to frame the standards discussion:
Escalating standards may be appropriate. PDF record copies and decent secure messaging would be an improvement in 2023. Let’s build on paper-based QR codes and other existing technologies to get to a standards-based future quickly.
US standards will certainly be an important safe harbour to consider for hospital standards given that all of our major Hospital EMRs are US-based: Blue Button has survived the longest and is driven by US ONC: https://www.healthit.gov/topic/health-it-initiatives/blue-button.
A more modern standard is SMART on FHIR, an accessible patient record via CURES ACT: https://www.nature.com/articles/s41746-020-00358-4..
Central identity is important and already a problem for governments. There is little consensus nationally and, while helpful, it doesn’t solve all problems. For example, the walled garden issue about still not being able to retrieve the data forces the need for open APIs so patients have access. As we know, forced API access can be manipulated by vendors to provide lackluster data sharing via performance down-tuning, changing data formats, rate-limiting, and security obstruction. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7762678/.
Probably the key question to start with is: “What do patients want?” Patients seem well- positioned to manage information flows within their circle of care. Again, this probably breaks out by persona. Here are three:
- Tech savvy patients? They want to be able to combine their personal apps like diet tracking, vitals, and wearables with their health care records. They want to understand what western medicine recommends against their personal biases and mixed methods.
- Medically conscious patients? They want to be in control of all relevant data. They want to find a way to make specialists and doctors read their collected information when assisting with their care.
- High-utilization dependent patients and their caregivers? They want more information about services to support managing care. They want to feel like their loved ones are protected while feeling supported with the direct care of the patient. They don't want to waste time without getting access to support or finding a treatment that can affect quality of life.
Our policy recommendations have sought to answer these needs by recommending the creation of a data-rich environment in which data elements can be combined and that shift decision making back to the patient (or caregiver). We're still early in the journey to a meaningful patient managed data set. This means that there are few well-used existing common standards that could be used to consolidate data well enough to give value to patients equally. This means we have to start with something that provides value as is: patient-oriented discharge summaries, longitudinal data exports of patient record via PDFs, e-prescriptions and lab tests.
We can also connect the future using older technologies. With faxes, e-mails, SMS or even PDFs, make a standard to print off a QR code or web URL that points digitally savvy consumers to a public token for that patient. This allows for low-tech readability, while creating a creative callback to more enabled portals to retrieve the data via scan-based APIs.
Hence, the shorthand of “usable digital format.”
Recommendations summary
In Table 1, we summarize our recommendations, with preliminary guidance around who is responsible, what the timeframe should be, and other comments regarding implementation. We suggest that this be considered by governments individually before the June 2021 Summit and then discussed at that time. Prior to the Summit, we request that governments tabulate which recommendations are already underway or are planned to be implemented.
Several of the recommendations could be addressed though bold national statements by the Federal Government. Doing so might help or hinder the progress of those recommendations given the nature of Canadian federal/provincial relationships. Better might be for the FPT VC Table to bring forward a set of recommendations to the Conference of Deputy Ministers of Health that they know are already well-supported by a majority of the PTs and by the Federal Government. Such a ground-up national consensus might still be used by federal politicians for announceables and governmental commitments, if so desired.
“That decision is above my pay grade.”
– Donald Rumsfeld (former US Secretary of Defense)
| Recommendation | Timeframe | Responsibility | Comments |
|---|---|---|---|
| 1. Care is care. Virtual care should remain a publicly-funded service that can be used by clinicians when they, in consultation with their patients, judge it appropriate. | Already happening | All | As of Wave 3, virtual care has now been normalized as an essential element of care delivery across the nation. |
| 2. All care modalities need to be continually evaluated against the Quadruple Aim to ensure they are enhancing patient experience, improving population health, reducing cost, and improving the work life of health care providers (Bodenheimer and Sinsky, 2014).Footnote 9 | Ongoing | National | - |
| 3. A practical review of privacy and security interpretations and administrative rules should be undertaken in the context of the learnings from the past year. This should be a fresh evaluation specifically designed to reduce overly risk adverse and impractical interpretations. | ASAP | PCHO | - |
| 4. Each PT should urgently conduct an objective inventory of IT systems and their pandemic performance. Develop replacements where appropriate. Each PT will have a development plan across existing and planned information systems. | ASAP | PTs | - |
| 5. There should be transparent reporting on usage levels and on user experience (UX) for all existing virtual care systems (probably for all digital systems). Patient and provider feedback should be readily available and transparent to all users. | Ongoing; Formal system in place within 2 years | PTs; CIHI and Infoway | - |
| 6. PREMS for UX should incorporate non-health software measures (e.g., Net Promoter Score, Apps Store ratings) that are standard across all industries to allow comparability and to avoid the creation of healthcare only services that are substandard. | Ongoing | All | - |
| 7. Keep the telephone as a permissible modality under the virtual billing codes. The value of video over phone has been overinflated. Phone was foundational for equity and access. | Already happening | PTs | - |
| 8. Governments need to move from capability creation and subsidization to the management of a mature and competitive digital health industry. | 6 months | All | - |
| 9. Develop feedback and monitoring processes to ensure policy decisions for virtual care promote equity and to identify any unintended inequitable consequences of virtual care development across Canada. | Ongoing | All Health Systems | This is now a broad equity concern for each of the health systems |
| 10. Different patients will require different modalities and mixes of services for our system to be patient-centred and to support continuity of care. We need to be humble and flexible in our systems' rules, regulations, and policies to allow innovation to continue apace. | Ongoing; check in annually | Fee negotiations at PTs | - |
| 11. Every person has the right to receive their health care data in a usable digital format by April 1, 2023. This should include a simple-to-administer ability to delegate control to a family member and to share information among a circle of care. | 2 years | PTs; Infoway to monitor | - |
| 12. All requisitions/results for standard lab tests should be sent/received in a usable digital format by April 1, 2023. No payment should be made for requisitions or results sent/received by paper. | 2 years | PTs; Infoway | - |
| 13. All prescriptions should be sent/received digitally by April 1, 2023. Because of the crisis in opioid usage in Canada, all opioid prescriptions should be sent/received digitally by April 1, 2022. | 2 years; ASAP | PTs; Infoway | - |
| 14. Pan-Canadian health care organizations should work with the two major Canadian eldercare software companies to redesign institutional and home care reporting systems.Table 1 Footnote * | ASAP | PCHO | - |
| 15. All hospitals shall provide a discharge or encounter summary upon request in a usable, machine readable and searchable, digital format as of April 1, 2023. An appropriate small fee will be paid on behalf of requesting consumers. | 2 years | PTs; Infoway | - |
| 16. All Primary Care EMRs shall provide a summary upon request in a usable, machine readable and searchable, digital format as of April 1, 2023. A price of $XX will be paid by the government on behalf of requesting consumers. | 2 years | PTs; Infoway | - |
| 17. A temporary paper record remediation service should be made available to service providers (and at their expense) to allow them to meet patient information requests during FY 2022 to 2026 to ease transition to a fully digital world. | 2 years | PTs | Should there be a national service? |
| 18. A small monthly fee (25 cents) should be paid each month to providers as an information fee for providing a personal health record service (aka portal) that is being actively used by consumers. This fee should have a sunset period of five years as it becomes a normal part of the workflow of the health service providers (declining by 5 cents per month each year). | 2 years | Subject for discussion. Could be a good way for PCHOs to pay for information transparency | - |
| 19. All government supported PHR services and portals must publicly report monthly active users, Net Promoter Score and such other PREMS as may be directed by the Pan-Canadian Health Organizations in order to receive payment. | 1 year | PTs; CIHI | - |
| 20. Canadian health information services and communications providers must publish and support usable application programming interfaces. Infoway should set tough standards for basic APIs. | ASAP | Infoway | - |
| 21. Where vendors charge fees, they should be published transparently and be subject to commercial review. Vendors should not be allowed to use dominant position in one sector to force use of their system in another health sector. | ASAP | Infoway | - |
| 22. Partner with individual communities to co-develop care delivery and infrastructure to suit their needs and wants. Collaborate with Indigenous health partners and organizations to ensure holistic approaches to meeting health needs in a culturally safe and appropriate way, including considerations of language and specific needs of individual communities. | ASAP | PTs; GoC | - |
| 23. Provide federal funding in partnership with FNHMA to develop a credentialed band and community-based IT support group to work with communities to develop tech literacy | Ongoing | GoC; Indigenous Bands and Communities | - |
| 24. All virtual care options, irrespective of modality, should be covered under all fee schedules. | ASAP | PTs | Subject for annual updates and discussion |
| 25. All patients who desire it should have same-day access to a virtual front door that connects them to the rest of the health care system. There are at least three ways that this should happen in 2021: provincial/regional front door, (large) group practice front door, employer-based assistance program. | 1 year | PTs | - |
| 26. All referrals and consults must be made electronically by April 1, 2023. | 2 years | PTs; Infoway | - |
| 27. Scale up implementation of patient monitoring programs. Provide permanent funding envelopes in a system neutral way that allows competing hardware/software/services bundles to compete with physical visit monitoring in a fair way. | 2 years | PTs; Infoway | - |
| 28. Create a temporary specialist access centre to promote rapid virtual access to specialty care. To reduce wait times, this incremental capacity will triage first by virtual to determine which specialist visits require in- person care. | ASAP | PTs | - |
| 29. Enter into principles-based negotiations with an understanding that system modernization will be a shared responsibility over several years. Several possible principles have been offered. | ASAP | PTs | - |
| 30. Capitation, salary, and bundling of services are preferable as they allow modality choice and switching. | 2 years | PTs | - |
| 31. Where FFS must be used it should be paid in a ratio of 1:3:5:5 for messaging:phone:video:physical. Triage virtual phone/video visits at 50% (but not messaging). | 1 year | PTs | This is only advice. The situation on the ground and past negotiation history will require local variation |
| 32. Walk-ins fees should be split with an information portion equal to about 25% to encourage continuity of care. This should apply to physical and virtual walk-ins. | 1 year | PTs | - |
| 33. A formal system of communications codes should be established for peer-to-peer communications. They should include a block funding for basic messaging, e-consult, e-referral, and conference call codes that appropriately reward collaborating providers in a patient-friendly system. | 1 year | PTs | - |
| 34. Do not make large infrastructure investments in basic video platforms. Keep technology switching costs low and avoid vendor lock-in. | ASAP | All | - |
| 35. Develop a new funding model for providers and hospitals to purchase and administer new digital technologies that work for them and their patients. This probably means a Technical Code or "T-code" that provides a small but appropriate amount of funding to pay for infrastructure expenses. | ASAP | PTs | - |
| 36. Specialty-by-specialty review to determine which services are appropriate to conduct virtually should be undertaken by the Canadian Medical Association in concert with Healthcare Excellence Canada, the Royal College and other specialty associations. This review should be explicitly separated from reimbursement review and remuneration discussion | ASAP | CMA; HEC; RCPS | - |
| 37. Take care to not reintroduce unneeded regulation into the patient-provider relationship around choice of visit modality. | ASAP | PTs | - |
| 38. Secure clinical email for patient and peer-to-peer communications should be available for purchase for all providers. Policy makers should consciously future proof these messaging systems by keeping switching costs low in the future. | 6 months | PTs, PCHOs | - |
| 39. Understand current customer outcome and experience measures being collected by major Canadian software vendors who compete in the health care space and incorporate them into our national PROMs and PREMs programs. | 1 year | - | - |
| 40. Assign Healthcare Excellence Canada the lead role to scale and spread virtual care innovation in clinical practice across Canada. This to be done in partnership with Canada Health Infoway who will provide guidance/support on securing/implementing the tools. | 1 year | HEC CHI | This could be modeled on the excellent LTC+ program |
| 41. Assign the Centre for Digital Health Evaluation the lead role to evaluate spread and scale of virtual care. | 6 months | CDHE | - |
| 42. A detailed review of medical education in the time of virtual care should be undertaken by a suitable academic group. | Ongoing and 2 years | Specialty organizations, CASN, AFMC and AFPC CMA, RCPS(C) | - |
| 43. Collaborative work continue towards a national approach to licensure. | Ongoing | CMA FPTs | - |
| 44. All providers must register a secure email as a condition of licensure; fax machine will no longer be considered a secure form of communication. | 1 year | Unclear | - |
| 45. Patients who receive specialty care across provincial borders should have the right to virtual follow-up care with the same provider, across PT borders. Licensure should allow this. | 1 year | Each PT | - |
| 46. Out-of-province students should have the right to virtual visits with their own physicians in their home PT. Licensure should allow this. Privacy rules should allow for cross-boundary sharing of health information at the request of patients and their providers. | 1 year | Each PT | - |
| 47. Licensure should allow French language speakers virtual access to a French-speaking specialist in another province rather than an in-province English-speaking specialist and vice-versa. | 1 year | PTs | - |
| 48. Licensure should allow pan- Canadian practice by Indigenous speaking clinicians in all parts of the country. Consideration should be given to a centre of excellence in these services. | 1 year | GoC | - |
| 49. Health Canada needs to review the mandates of the Pan- Canadian Health Care Organizations to ensure that they provide clear national governance of virtual care and the digital health industry. With support of PT governments an agreed structure for managing national standards needs to be developed. | 6 months | GoC | This has been discussed for years. One small but important part of a larger issue |
Acronyms
- API
- Application Programming Interface
- CDHE
- Centre for Digital Health Evaluation
- CIHI
- Canadian Institute for Health Information
- CoPC
- Costs of Physical Contact
- EMR
- Electronic Medical Record
- FFS
- Fee-for-Service
- LOES
- Low Earth Orbiting Satellite
- LPN
- Licensed Practical Nurse
- NP
- Nurse Practitioner
- NPS
- Net Promoter Score
- OTN
- Ontario Telemedicine Network
- OVCC
- Ontario Virtual Care Clinic
- PCP
- Primary Care Provider
- PREMs
- Patient-Reported Experience Measures
- PROMs
- Patient-Reported Outcome Measures
- RTVS
- Real-Time Virtual Services
- UX
- User Experience
Glossary Footnote iii
- Asynchronous Messaging: encompasses virtual care modalities of secure messaging (i.e., through a patient portal), email, or text messaging.
- Alternative Payment Models (APMs): are alternatives to fee-for-service remuneration (i.e., capitation) for physicians that are often intended to promote value-based care.
- Circle of Care: The patient, their relevant caregivers and family members (at the direction of the patient).
- Clinical appropriateness: refers to whether the health care services provided are suitable according to the symptoms presented by a patient.
- Costs of Physical Contact (CoPC): Costs to patients of providing care in-person including financial and convenience costs (e.g., child care, parking, time off work, travel) and health risk (e.g., viral exposure in waiting rooms).
- Health Care Provider (HCP) or Provider: refers to any person or institution (e.g., physicians, nurse practitioners, social workers, occupational therapists, pharmacists, hospitals, laboratories) that provide health care services to patients.
- Modality: refers to the method by which care is delivered, such as in-person, phone, video, asynchronous messaging, and remote monitoring. We note that past technologies (e.g., radio, TV, PSA, road signs) have been used during the pandemic. Future technologies will be added to this list and need to be contemplated when writing regulations or tariffs (e.g., virtual reality, voice, supervised DIY).
- Ontario Health Teams (OHT): supports patients across the continuum of care through a team of health care providers and organizations in a certain geographic catchment area, including hospitals, physicians, and home and community care providers. Specifically, the goal of each OHT is for patients to receive all care from one team of Health Care Providers to help patients navigate the system and transition easily between different providers and health services all within an OHT.
- Primary Care Provider (PCP): refers to a sub-group of Health Care Providers or Providers who provide primary care services (e.g., family physician, nurse practitioner, registered nurse, social worker, dietician, pharmacist).
- Quadruple Aim: Framework of four dimensions for health care evaluation: enhancing patient experience, improving population health, reducing cost, and improving the work life of health care providers
- Virtual Care: refers to any interaction between patients and/or members of their circle of care, occurring remotely, using any forms of communication or information technologies, with the aim of facilitating or maximizing the quality and effectiveness of patient care.
- Virtual visits: refer to synchronous modalities of providing virtual care, specifically phone and video conferencing, for which the equivalent would be an in-person appointment.
Acknowledgements
In preparing this diagnostique I have been supported by a superb team from the Centre for Digital Health Evaluation. Michael Cheung, Leah Kelley, Karen Palmer, and Denise Zarn have dedicated their time and thought leadership to this project. They are individually and together great colleagues.
Several people have read early drafts and many more have participated in interviews. All told more than 100 people have contributed their ideas and their comments. My thanks to each and all of them. I want to particularly recognize Drs. Payal Agarwal, Sacha Bhatia, Onil Bhattacharyya, and Trevor Jamieson for their support and feedback.
Virtual care has evolved quickly in the past fourteen months and will continue to do so. Taking a point in time snapshot of such an evolution may mean I got some stuff wrong. I hope that what I present may be of value to you in your deliberations as we work together to improve health care in Canada.
Author Affiliation(s) and conflicts declaration: Woman’s College Hospital Institute for Health Sustainability and Virtual Care Innovation Fellow, University of Toronto Rotman School of Management Adjunct Faculty and Executive in Residence, CD Howe Institute Senior Fellow.
Investor/advisor/director to several digital health start-ups mentioned in the report or relevant to the area including Alayacare, ThinkResearch, Verto Health, and FirstHx. The author has occasionally advised or done speeches at more than a dozen different health care enterprises, associations, agencies of government, companies in the past several years both directly and occasionally through Satov Consultants. He is also a retired partner (and pensioner) of PwC Canada. A complete list of conflicts of interest was filed with Health Canada before the start of this work and has been updated during the project.