Canada-Prince Edward Island Aging with Dignity funding agreement (2023-24 to 2027-28)
Table of contents
- Funding agreement
- Annex 1 – Common statement of principles on shared health priorities
- Annex 2 – Shared pan-Canadian interoperability roadmap
- Annex 3 – Indicators: Access to home and community care
- Annex 4 – Action plan
Funding agreement
(the "Agreement")
BETWEEN:
HIS MAJESTY THE KING IN RIGHT OF CANADA (hereinafter referred to as "Canada" or "Government of Canada") as represented by the Minister of Health (herein referred to as "the federal Minister")
- and -
HIS MAJESTY THE KING IN RIGHT OF THE PROVINCE OF PRINCE EDWARD ISLAND (hereinafter referred to as "Prince Edward Island" or "Government of Prince Edward Island") as represented by the Minister of Health and Wellness (herein referred to as "the provincial Minister")
REFERRED to collectively as the "Parties", and individually as a "Party"
PREAMBLE
WHEREAS, on February 23, 2023, Canada and Prince Edward Island announced an overarching agreement in principle on Working Together to Improve Health Care for Canadians, supported by almost $200 billion over ten years in federal funding, including $46.2 billion in new funding to provinces and territories, Canada and Prince Edward Island acknowledged the importance of helping Canadians age closer to home;
WHEREAS, Canada has also announced a 5 per cent Canada Health Transfer (CHT) guarantee for the next five years, starting in 2023-24, which will be provided through annual top-up payments as required. This is projected to provide approximately an additional $17 billion over 10 years in new support. The last top-up payment will be rolled into the CHT base at the end of the five years to ensure a permanent funding increase, providing certainty and sustainability to provinces and territories;
WHEREAS, in the area of home and community care, Working Together to Improve Health Care for Canadians also includes a commitment by Canada and Prince Edward Island to continue to work to support collaboration on the Common Statement of Principles on Shared Health Priorities (hereinafter referred to as the "Common Statement", attached hereto as Annex 1), supported by the federal Budget 2017 investment of $6 billion over ten years;
WHEREAS, this Agreement also provides financial support for long-term care as it relates to the Government of Canada's Budget 2021 investment of $3 billion over 5 years to support provinces and territories in keeping long-term care residents safe and improve their quality of life;
WHEREAS, Prince Edward Island has the primary responsibility for delivering health care services to its residents and supports diversity, equity, and the needs of underserved and/or disadvantaged populations, including, but not limited to First Nations, Inuit and Métis, official language minority communities, rural and remote communities, children, racialized communities (including Black Canadians), and LGBTIQA2S+;
WHEREAS, Canada authorized the federal Minister to enter into agreements with the provinces and territories, for the purpose of identifying activities that provinces and territories will undertake in respect of long-term care, and for funding in this Agreement associated with the federal investment for home and community care consistent with the Common Statement (and menu of actions outlined in Annex 1);
WHEREAS, the Financial Administration Act R.S.P.E.I, c- F-9 authorized the provincial Minister to enter into agreements with the Government of Canada under which Canada undertakes to provide funding toward costs incurred by the Government of Prince Edward Island associated with the federal investment for long-term care, and home and community care consistent with the Common Statement; and
NOW THEREFORE, this Agreement sets out the terms between Canada and Prince Edward Island as follows:
1.0 Key principles and collaboration
The key principles and commitment to collaboration agreed to in Working Together to Improve Health Care for Canadians are outlined below.
1.1 Canada and Prince Edward Island acknowledge that this Agreement will mutually respect each government's jurisdiction, and be underpinned by key principles, including:
- A shared responsibility to uphold the Canada Health Act that strengthens our public health care system;
- Principles agreed to in the Common Statement (outlined in Annex 1);
- Reconciliation with Indigenous Peoples, recognizing their right to fair and equal access to quality and culturally safe health services free from racism and discrimination anywhere in Canada, including through seamless service delivery across jurisdictions and meaningful engagement and work with Indigenous organizations and governments; and
- Equity of access for under-served groups and individuals, including those in official language minority communities.
1.2 Canada and Prince Edward Island acknowledge the importance of supporting health data infrastructure, data collection and public reporting, and will work together to improve the collection, sharing and use of de-identified health information, respecting federal/provincial/territorial privacy legislation, to improve transparency on results and to help manage public health emergencies, and to ensure Canadians can access their own health information and benefit from it being shared between health workers across health settings. This includes:
- collecting and securely sharing high-quality, comparable information needed to improve services to Canadians, including disaggregated data on key common health indicators with the Canadian Institute for Health Information (CIHI);
- adopting common interoperability standards (both technical exchange and content of data), including the Shared pan-Canadian Interoperability Roadmap (outlined in Annex 2), to improve Canadians' access to their health information in a usable digital format and support the exchange and analysis of health data within and across Canada's health systems in a way that protects Canadians' privacy and ensures the ethical use of data to improve the health and lives of people;
- work to align provincial and territorial policies and legislative frameworks where necessary and appropriate to support secure patient access to health information, and stewardship of health information to support the public good, including improving care quality, patient safety, privacy protection, system governance and oversight, planning and research;
- promoting health information as a public good by working with federal-provincial-territorial Ministers of Health to review and confirm overarching principles, which would affirm Canadians' ability to access their health information and have it follow them across all points of care. The existing Health Data Charter, as outlined in the Pan-Canadian Health Data Strategy would serve as the starting point for the discussion of these principles; and
- collecting and sharing available public health data (e.g., vaccination data, testing data) with the Public Health Agency of Canada to support Canada's preparedness and response to public health events, building on commitments made as part of the Safe Restart Agreements.
1.3 Canada and Prince Edward Island acknowledge they will work with other provinces and territories to streamline foreign credential recognition for internationally-educated health professionals, and to advance labour mobility, starting with multi-jurisdictional recognition of health professional licences.
1.4 Canada and Prince Edward Island acknowledge a mutual intent to engage in a two-phased formal review process:
- Phase 1: This review will be done in 2026 by a joint committee of Federal, Provincial, and Territorial health and finance officials to assess results and determine next steps for bilateral agreements related to improvements to home and community care, mental health, substance use, and addiction services associated with the Common Statement and long-term care; and
- Phase 2: A formal five-year review of the healthcare plan outlined on February 7, 2023, recognizing the importance of long-term sustainability for provincial-territorial health systems. This review would consist of an assessment of both the bilateral agreements (herein) and the CHT investments (not included as part of this bilateral agreement). The review will be done by a joint committee of Federal, Provincial, and Territorial health and finance officials, commencing by March 31, 2027, and concluded by December 31, 2027, to consider results achieved thus far in the four shared health priority areas and will include:
- an assessment of progress-to-date on public reporting to Canadians using the common indicators;
- sharing of de-identified health information, and other health data commitments; and
- current and forward-looking Federal, Provincial, and Territorial investments to support this plan.
2.0 Objectives
2.1 Canada and Prince Edward Island agree that, with financial support from Canada, Prince Edward Island will continue to build and enhance health care systems towards achieving some or all of the objectives of:
- Improving access to home and community care services (listed in the Common Statement, attached as Annex 1); and
- Supporting workforce improvements for long-term care and standards, to keep long-term care residents safe and to improve their quality of life.
3.0 Action plan
3.1 Prince Edward Island will set out in their Action Plan (attached as Annex 4) how the federal investment under this Agreement will be used, as well as details on targets and timeframes for each of the initiatives supported under the Agreement.
3.2 Prince Edward Island will invest federal funding as part of the 2017 commitment for home and community care provided through this Agreement in alignment with the menu of actions listed in the Common Statement.
3.3 Prince Edward Island will invest federal funding for long-term care provided through this Agreement to bolster efforts to support workforce improvements and standards by:
- Supporting activities/initiatives to achieve stability in the long-term care workforce, including through hiring and wage top-ups and/or improvements to workplace conditions (e.g., staff to patient ratios, hours of work); and
- Applying long-term care standards, with an emphasis on strengthened enforcement (e.g., enhanced inspection and enforcement capacity, quality and safety improvements to meet standards).
3.4 In developing initiatives under this Agreement, Prince Edward Island agrees to implement measures that also respond to the needs of underserved and/or disadvantaged populations, including, but not limited to First Nations, Inuit and Métis, official language minority communities, rural and remote communities, children, racialized communities (including Black Canadians), and LGBTIQA2S+.
3.5 Prince Edward Island's approach to achieving home and community care and long-term care objectives is set out in their five-year Action Plan, as set out in Annex 4.
4.0 Term of agreement
4.1 This Agreement comes into effect upon the date of the last signature of the Parties and will remain in effect until March 31, 2028, unless terminated in accordance with section 12 of this Agreement. Funding provided under this Agreement will be for five years and will cover the period April 1, 2023 to March 31, 2028 ("the Term").
5.0 Financial provisions
5.1 The funding provided under this Agreement is in addition to and not in lieu of those that Canada currently provides under the CHT to support delivering health care services within the province.
5.2 Allocation to Prince Edward Island
5.2.1 In this Agreement, "Fiscal Year" means the period commencing on April 1 of any calendar year and terminating on March 31 of the immediately following calendar year.
5.2.2 Canada has designated the following maximum amounts to be transferred in total to all provinces and territories under this initiative based on the allocation method outlined in subsection 5.2.3 for the Term of this Agreement.
Budget 2017 home and community care
- $600 million for the Fiscal Year beginning on April 1, 2023
- $600 million for the Fiscal Year beginning on April 1, 2024
- $600 million for the Fiscal Year beginning on April 1, 2025
- $600 million for the Fiscal Year beginning on April 1, 2026
Budget 2021 long-term care
- $600 million for the Fiscal Year beginning on April 1, 2023
- $600 million for the Fiscal Year beginning on April 1, 2024
- $600 million for the Fiscal Year beginning on April 1, 2025
- $600 million for the Fiscal Year beginning on April 1, 2026
- $600 million for the Fiscal Year beginning on April 1, 2027
5.2.3 Allocation Method
- For funds associated with Budget 2017 Home and Community Care committed by the federal government in 2017, annual funding will be allocated to provinces and territories on a per capita basis. The per capita funding for each Fiscal Year is calculated using the following formula: F x K/L, where:
F is the annual total funding amount available under this program;
K is the total population of Prince Edward Island, as determined using the annual population estimates on July 1st from Statistics Canada; and
L is the total population of Canada, as determined using the annual population estimates on July 1st from Statistics Canada.
- For funds associated with Budget 2021 Long-Term Care committed by the federal government in 2021, annual funding will be allocated to provinces and territories with a base amount of $1,200,000 and the remainder of the funding allocated on a per capita basis. The total amount to be paid will be calculated using the following formula: $1,200,000+(F-(N x 1,200,000)) x (K/L), where:
F is the annual total funding amount available under this program;
N is the number of jurisdictions (13) that will be provided the base funding of $1,200,000;
K is the total population of Prince Edward Island, as determined using the annual population estimates on July 1st from Statistics Canada; and
L is the total population of Canada, as determined using the annual population estimates on July 1st from Statistics Canada.
5.2.4 Subject to annual adjustment based on the formulas described in section 5.2.3, Prince Edward Island estimated share of the amounts will be:
| Fiscal Year | Budget 2017 Home and Community Care
Estimated amount to be paid to Prince Edward IslandFootnote * (subject to annual adjustment) |
Budget 2021 Long-Term Care Estimated amount to be paid to Prince Edward IslandFootnote * (subject to annual adjustment) |
|---|---|---|
| 2023-2024 | $2,630,000 | $3,760,000 |
| 2024-2025 | $2,630,000 | $3,760,000 |
| 2025-2026 | $2,630,000 | $3,760,000 |
| 2026-2027 | $2,630,000 | $3,760,000 |
| 2027-2028 | n/a | $3,760,000 |
|
||
5.3 Payment
5.3.1 Funding provided by Canada will be paid in semi-annual installments as follows:
- In 2023-24, the first installment will be paid within approximately 30 business days of execution of this Agreement by the Parties. The second installment will also be paid within approximately 30 business days of execution of this Agreement by the Parties, subject to 5.3.1.g.
- Starting in 2024-25, the first installment will be paid on or about April 15 of each Fiscal Year and the second installment will be paid on or about November 15 of each Fiscal Year.
- The first installment will be equal to 50% of the notional amount set out in section 5.2.4 as adjusted by section 5.2.3.
- The second installment will be equal to the balance of funding provided by Canada for the Fiscal Year as determined under sections 5.2.3 and 5.2.4.
- Canada will notify Prince Edward Island prior to the first payment of each Fiscal Year, of their notional amount. The notional amount will be based on the Statistics Canada quarterly preliminary population estimates on July 1 of the preceding Fiscal Year. Prior to the second payment, Canada will notify Prince Edward Island of the amount of the second installment as determined under sections 5.2.3 and 5.2.4.
- Canada shall withhold payments if Prince Edward Island has failed to provide reporting in accordance with 8.1.
- Canada shall withhold the second payment in 2023-24 if Prince Edward Island has failed to satisfy all reporting requirements associated with the preceding Canada – Prince Edward Island Home and Community Care and Mental Health and Addictions Services Funding Agreement 2022-23, specifically to:
- continue to participate in a Federal-Provincial-Territorial process to improve reporting on and provide data to CIHI for the 6 common indicators (listed in Annex 3) to measure pan-Canadian progress on improving access to home and community care; and
- submit an annual financial statement, with attestation from province's Chief Financial Officer, of funding received the preceding Fiscal Year from Canada for home and community care under the Canada – Prince Edward Island Home and Community Care and Mental Health and Addictions Services Funding Agreement 2022-23 compared against the Expenditure Plan, and noting any variances, between actual expenditures and the Expenditure Plan.
- The sum of both installments constitutes a final payment and is not subject to any further payment once the second installment has been paid.
- Payment of Canada's funding for this Agreement is subject to an annual appropriation by the Parliament of Canada for this purpose.
5.3.2 Where Prince Edward Island will use cost-recovery agreements with one or more privately-owned for-profit facilities as an accountability measure and Prince Edward Island has failed to put in place a cost-recovery agreement by April 1, 2024, Canada shall deduct from the payment referred to in subsection 5.3.1(b) an amount equivalent to the amount of funding noted in Annex 4 to be provided by Prince Edward Island to those facilities with whom they do not have the required cost-recovery agreements in place.
5.4 Retaining funds
5.4.1 For Fiscal Years 2023-24 through 2026-27, upon request, Prince Edward Island may retain and carry forward to the next Fiscal Year up to 10 percent of funding that is in excess of the amount of the eligible costs actually incurred in a Fiscal Year and use the amount carried forward for expenditures on eligible areas of investment. Any request to retain and carry forward an amount exceeding 10 percent will be subject to discussion and mutual agreement in writing by their designated officials, at the Assistant Deputy Minister level (herein referred to as "Designated Officials"), and is subject to monitoring and reporting to Canada on the management and spending of the funds carried forward on a quarterly basis.
5.4.2 For Fiscal Year 2027-28, Prince Edward Island is not entitled to retain any amounts beyond March 31, 2028. Any amounts that remain unexpended at the end of that Fiscal Year are considered debts due to Canada and shall be repaid in accordance with section 5.5.2.
5.4.3 Any amount carried forward from one Fiscal Year to the next under this subsection is supplementary to the maximum amount payable to Prince Edward Island under subsection 5.2.4 of this Agreement in the next Fiscal Year.
5.5 Repayment of overpayment
5.5.1. In the event payments made exceed the amount to which Prince Edward Island is entitled under this Agreement, the amount of the excess is a debt due to Canada and, unless otherwise agreed to in writing by the Parties, Prince Edward Island shall repay the amount within sixty (60) calendar days of written notice from Canada.
5.5.2 Funds not spent within the Term of the Agreement will be considered a debt due to Canada and Prince Edward Island shall repay the amount within sixty (60) calendar days of written notice from Canada.
5.6 Use of funds
5.6.1 The Parties agree that funds provided under this Agreement will only be used by Prince Edward Island in accordance with the initiatives outlined in Annex 4.
5.7 Eligible expenditures
5.7.1 Eligible expenditures under this Agreement are the following:
- data development and collection to support reporting;
- information technology and health information infrastructure;
- capital and operating funding;
- salaries and benefits;
- training, professional development; and
- information and communications material related to programs.
5.7.2 The Parties agree that the long-term care funding may be provided to:
- publicly-owned long-term care settings;
- privately-owned not-for-profit long-term care settings; and
- subject to section 6.0, privately-owned for-profit long-term care settings.
6.0 Accountability mechanisms for long-term care
6.1 Where federal funding is provided to privately-owned, for-profit facilities in accordance with this Agreement, Prince Edward Island agrees to put in place the accountability mechanisms outlined in Annex 4.
6.2 Where Prince Edward Island has cost-recovery agreements in place with one or more privately-owned for-profit facilities pursuant to subsection 6.1, Prince Edward Island agrees to report on these in accordance with the requirements set out in subsection 8.1.1 and invest all funds recovered through those agreements in accordance with the terms of this Agreement and the initiatives outlined in Annex 4.
7.0 Performance measurement
7.1 Prince Edward Island agrees to designate an official or official(s), for the duration of this Agreement to participate in a CIHI led Federal-Provincial-Territorial indicator process to:
- Improve reporting on common indicators to measure pan-Canadian progress on improving access to home and community care, associated with the commitment in the Common Statement;
- Develop new common indicators for long-term care; and
- Share available disaggregated data with CIHI and work with CIHI to improve availability of disaggregated data for existing and new common indicators to enable reporting on progress for underserved and/or disadvantaged populations including, but not limited to, Indigenous peoples, First Nations, Inuit, Métis, official language minority communities, rural and remote communities, children, racialized communities (including Black Canadians), and LGBTIQA2S+.
8.0 Reporting to Canadians
8.1 Funding conditions and reporting
8.1.1 By no later than October 1, in each fiscal year, with respect of the previous Fiscal Year, Prince Edward Island agrees to:
- Provide data and information annually to CIHI related to the home and community care common indicators (listed in Annex 3) identified as part of the commitment made in the Common Statement, and, new common indicators on long-term care.
- Beginning in Fiscal Year 2024-25, report annually and publicly in an integrated manner to residents of Prince Edward Island on progress made on targets outlined in Annex 4 (Action Plan).
- Beginning in Fiscal Year 2024-25, provide to Canada an annual financial statement, with attestation from province's Chief Financial Officer, of funding received the preceding Fiscal Year from Canada under this Agreement or the Previous Agreement compared against the Action Plan, and noting any variances, between actual expenditures and the Action Plan:
- The revenue section of the statement shall show the amount received from Canada under this Agreement during the Fiscal Year;
- The total amount of funding used for home and community care and long-term care;
- If applicable, the amount of any funding carried forward under section 5.4;
- If applicable, the amount of overpayment that is to be repaid to Canada under section 5.5; and
- With respect to the long-term care funding under this Agreement, where cost-recovery is used, the annual financial statement will also set out:
- The amount of the federal funding flowing to private, for-profit facilities; and
- The estimated amount of funds to be recovered under cost-recovery agreements, where applicable, and the priority areas where those funds will be reinvested.
8.1.2 Prince Edward Island will provide quarterly reporting to Canada on the management and spending of the funds retained to the next Fiscal Year.
8.2 Audit
8.2.1 Prince Edward Island will ensure that expenditure information presented in the annual financial statement is, in accordance with Prince Edward Island's standard accounting practices, complete and accurate.
8.3 Evaluation
8.3.1 Responsibility for evaluation of programs rests with Prince Edward Island in accordance with its own evaluation policies and practices
9.0 Communications
9.1 The Parties agree on the importance of communicating with citizens about the objectives of this Agreement in an open, transparent, effective and proactive manner through appropriate public information activities.
9.2 Each Party will receive the appropriate credit and visibility when investments financed through funds granted under this Agreement are announced to the public.
9.3 In the spirit of transparency and open government, Canada will make this Agreement, including any amendments, publicly available on a Government of Canada website.
9.4 Prince Edward Island will make publicly available, clearly identified on a Government of Prince Edward Island website, this Agreement, including any amendments.
9.5 Canada, with prior notice to Prince Edward Island, may incorporate all or any part of the data and information in 8.1, or any part of evaluation and audit reports made public by Prince Edward Island into any report that Canada may prepare for its own purposes, including any reports to the Parliament of Canada or reports that may be made public.
9.6 Canada reserves the right to conduct public communications, announcements, events, outreach and promotional activities about the Common Statement and this Agreement. Canada agrees to give Prince Edward Island 10 days advance notice and advance copies of public communications related to the Common Statement, this Agreement, and results of the investments of this Agreement.
9.7 Prince Edward Island reserves the right to conduct public communications, announcements, events, outreach and promotional activities about the Common Statement and this Agreement. Prince Edward Island agrees to give Canada 10 days advance notice and advance copies of public communications related to the Common Statement, this Agreement, and results of the investments of this Agreement.
9.8 Canada and Prince Edward Island agree to participate in a joint announcement upon signing of this Agreement.
9.9 Canada and Prince Edward Island agree to work together to identify mutually agreeable opportunities for joint announcements relating to programs funded under this Agreement.
10.0 Dispute resolution
10.1 The Parties are committed to working together and avoiding disputes through government-to-government information exchange, advance notice, early consultation, and discussion, clarification, and resolution of issues, as they arise.
10.2 If at any time a Party is of the opinion that the other Party has failed to comply with any of its obligations or undertakings under this Agreement or is in breach of any term or condition of the Agreement, that Party may notify the other Party in writing of the failure or breach. Upon such notice, the Parties will endeavour to resolve the issue in dispute bilaterally through their Designated Officials.
10.3 If a dispute cannot be resolved by Designated Officials, then the dispute will be referred to the Deputy Ministers of Canada and Prince Edward Island responsible for health, and if it cannot be resolved by them, then the federal Minister(s) and the provincial Minister(s) shall endeavour to resolve the dispute.
11.0 Amendments to the agreement
11.1 The main text of this Agreement may be amended at any time by mutual consent of the Parties. Any amendments shall be in writing and signed, in the case of Canada, by the federal Minister(s), and in the case of Prince Edward Island, by the provincial Minister(s).
11.2 Annex 4 may be amended at any time by mutual consent of the Parties. Any amendments to Annex 4 shall be in writing and signed by each Party's Designated Official.
12.0 Termination
12.1 Either Party may terminate this Agreement at any time if the terms are not respected by giving at least 6 months written notice of intention to terminate.
12.2 As of the effective date of termination of this Agreement, Canada shall have no obligation to make any further payments.
12.3 Sections 1.0 and 9.0 of this Agreement survive for the period of the 10-year Working Together to Improve Health Care for Canadians plan.
12.4 Sections 5.4 and 8.0 of this Agreement survive the termination or expiration of this Agreement until reporting obligations are completed.
13.0 Notice
13.1 Any notice, information, or document provided for under this Agreement will be effectively given if delivered or sent by letter, email, postage or other charges prepaid. Any communication that is delivered will be deemed to have been received in delivery; and, except in periods of postal disruption, any communication mailed by post will be deemed to have been received eight calendar days after being mailed.
The address of the Designated Official for Canada shall be:
Assistant Deputy Minister, Strategic Policy Branch
Health Canada
70 Colombine Driveway
Brooke Claxton Building
Ottawa, Ontario
K1A 0K9
Email: jocelyne.voisin@hc-sc.gc.ca
The address of the Designated Official for Prince Edward Island shall be:
Assistant Deputy Minister, Community Health and Policy Branch
Department of Health and Wellness
P.O. Box 2000
Charlottetown, PE
Canada C1A 7N8
Email: MDBRADLEY@gov.pe.ca
14.0 General
14.1 This Agreement, including Annexes, comprises the entire Agreement entered into by the Parties.
14.2 This Agreement shall be governed by and interpreted in accordance with the laws of Canada and Prince Edward Island.
14.3 No member of the House of Commons or of the Senate of Canada or of the Legislature of Prince Edward Island shall be admitted to any share or part of this Agreement, or to any benefit arising therefrom.
14.4 If for any reason a provision of this Agreement, that is not a fundamental term, is found by a court of competent jurisdiction to be or to have become invalid or unenforceable, in whole or in part, it will be severed and deleted from this Agreement, but all the other provisions of this Agreement will continue to be valid and enforceable.
14.5 This Agreement may be executed in counterparts, in which case (i) the Parties have caused this Agreement to be duly signed by the undersigned authorized representatives in separate signature pages in accordance with the following signature process, which together shall constitute one agreement, and (ii) the Parties agree that facsimile signature(s) and signature(s) transmitted by PDF shall be treated as original signature(s). Electronic signature(s) may be accepted as originals so long as the source of the transmission can be reasonably connected to the signatory.
IN WITNESS WHEREOF the Parties have executed this Agreement through duly authorized representatives.
SIGNED on behalf of Canada by the Minister of Health
The Honourable Mark Holland, Minister of Health
IN WITNESS WHEREOF the Parties have executed this Agreement through duly authorized representatives.
SIGNED on behalf of Prince Edward Island by the Minister of Health and Wellness
The Honourable D. Mark V. McLane, Minister of Health and Wellness
Annex 1 – Common Statement of Principles on Shared Health Priorities
Common Statement of Principles on Shared Health Priorities
Annex 2 – Shared pan-Canadian interoperability roadmap
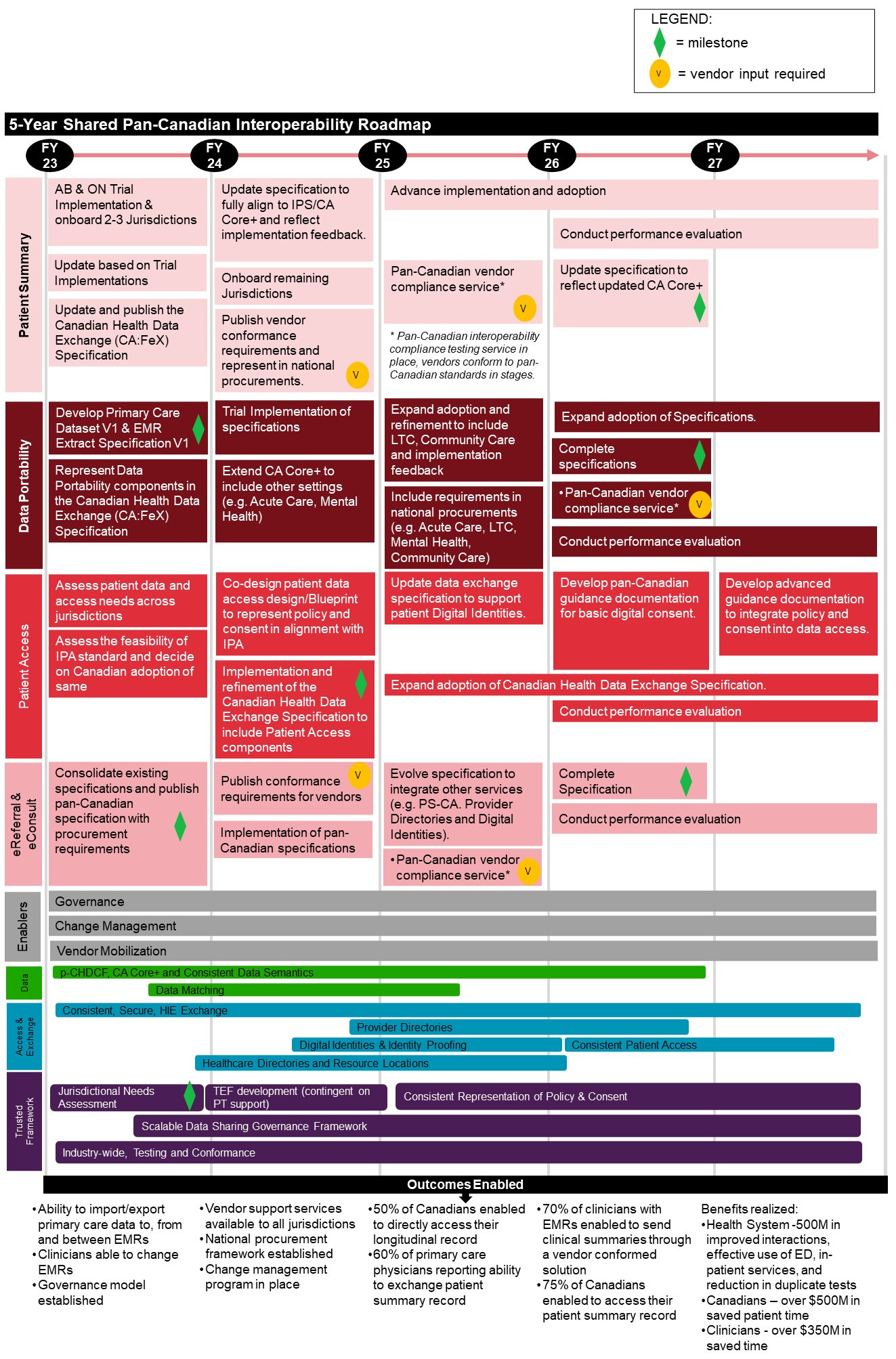
Figure 1 - Text description
5-Year Shared Pan-Canadian Interoperability Roadmap
The Roadmap outlines 8 categories of activities planned for fiscal years 2023 to 2027, followed by anticipated outcomes enabled. Notes are also included throughout to highlight a "milestone", where "vendor input is required", and/or when an activity is "continued" across multiple fiscal years.
Patient Summary
- Fiscal Year 2023
- Alberta & Ontario Trial Implementation & onboard 2-3 Jurisdictions
- Update based on Trial Implementations
- Update and publish the Canadian Health Data Exchange (CA:FeX) Specification
- Fiscal Year 2024
- Update specification to fully align to IPS/CA Core+ and reflect implementation feedback
- Onboard remaining jurisdictions
- Publish vendor conformance requirements and represent in national procurements [vendor input required]
- Fiscal Year 2025
- Advance implementation and adoption
- Pan-Canadian vendor compliance service *(Pan-Canadian interoperability compliance testing service in place, vendors conform to pan-Canadian standards in stages.) [vendor input required]
- Fiscal Year 2026
- Advance implementation and adoption [continued]
- Conduct performance evaluation
- Update specification to reflect updated CA Core+ [milestone]
- Fiscal Year 2027
- Advance implementation and adoption [continued]
- Conduct performance evaluation [continued]
Data Portability
- Fiscal Year 2023
- Develop Primary Care Dataset V1 & EMR Extract Specification V1 [milestone]
- Represent Data Portability components in the Canadian Health Data Exchange (CA:FeX) Specification
- Fiscal Year 2024
- Trial Implementation of specifications
- Extend CA Core+ to include other settings (e.g. Acute Care, Mental Health)
- Fiscal Year 2025
- Expand adoption and refinement to include LTC, Community Care and implementation feedback
- Include requirements in national procurements (e.g. Acute Care, LTC, Mental Health, Community Care)
- Fiscal Year 2026
- Expand adoption of Specifications
- Complete specifications [milestone]
- Pan-Canadian vendor compliance service *(Pan-Canadian interoperability compliance testing service in place, vendors conform to pan-Canadian standards in stages.) [vendor input required]
- Conduct performance evaluation
- Fiscal Year 2027
- Expand adoption of Specifications [continued]
- Conduct performance evaluation [continued]
Patient Access
- Fiscal Year 2023
- Assess patient data and access needs across jurisdictions
- Assess the feasibility of IPA standard and decide on Canadian adoption of same
- Fiscal Year 2024
- Co-design patient data access design/Blueprint to represent policy and consent in alignment with IPA
- Implementation and refinement of the Canadian Health Data Exchange Specification to include Patient Access components [milestone]
- Fiscal Year 2025
- Update data exchange specification to support patient Digital Identities
- Expand adoption of Canadian Health Data Exchange Specification
- Fiscal Year 2026
- Develop pan-Canadian guidance documentation for basic digital consent
- Expand adoption of Canadian Health Data Exchange Specification [continued]
- Conduct performance evaluation
- Fiscal Year 2027
- Develop advanced guidance documentation to integrate policy and consent into data access
- Expand adoption of Canadian Health Data Exchange Specification [continued]
- Conduct performance evaluation [continued]
eReferral & eConsult
- Fiscal Year 2023
- Consolidate existing specifications and publish pan-Canadian specification with procurement requirements [milestone]
- Fiscal Year 2024
- Publish conformance requirements for vendors [vendor input required]
- Implementation of pan-Canadian specifications
- Fiscal Year 2025
- Evolve specification to integrate other services (e.g. PS-CA. Provider Directories and Digital Identities)
- Pan-Canadian vendor compliance service *(Pan-Canadian interoperability compliance testing service in place, vendors conform to pan-Canadian standards in stages.) [vendor input required]
- Fiscal Year 2026
- Complete Specification [milestone]
- Conduct performance evaluation [continued]
- Fiscal Year 2027
- Conduct performance evaluation [continued]
Enablers
- Fiscal Years 2023 to 2027
- Governance
- Change Management
- Vendor Mobilization
Data
- Fiscal Year 2023
- p-CHDCF, CA Core+ and Consistent Data Semantics
- Data Matching
- Fiscal Year 2024
- p-CHDCF, CA Core+ and Consistent Data Semantics [continued]
- Data Matching [continued]
- Fiscal Year 2025
- p-CHDCF, CA Core+ and Consistent Data Semantics [continued]
- Data Matching [continued]
- Fiscal Year 2026
- p-CHDCF, CA Core+ and Consistent Data Semantics [continued]
- Fiscal Year 2027
- N/A
Access & Exchange
- Fiscal Year 2023
- Consistent, Secure, HIE Exchange
- Healthcare Directories and Resource Locations
- Fiscal Year 2024
- Consistent, Secure, HIE Exchange [continued]
- Provider Directories
- Digital Identities & Identity Proofing
- Healthcare Directories and Resource Locations [continued]
- Fiscal Year 2025
- Consistent, Secure, HIE Exchange [continued]
- Provider Directories [continued]
- Digital Identities & Identity Proofing [continued]
- Healthcare Directories and Resource Locations [continued]
- Fiscal Year 2026
- Consistent, Secure, HIE Exchange [continued]
- Provider Directories [continued]
- Digital Identities & Identity Proofing [continued]
- Consistent Patient Access
- Healthcare Directories and Resource Locations [continued]
- Fiscal Year 2027
- Consistent, Secure, HIE Exchange [continued]
- Consistent Patient Access [continued]
Trusted Framework
- Fiscal Year 2023
- Jurisdictional Needs Assessment [milestone]
- Scalable Data Sharing Governance Framework
- Industry-wide, Testing and Conformance
- Fiscal Year 2024
- TEF development (contingent on PT support)
- Scalable Data Sharing Governance Framework [continued]
- Industry-wide, Testing and Conformance [continued]
- Fiscal Year 2025
- Consistent Representation of Policy & Consent
- Scalable Data Sharing Governance Framework [continued]
- Industry-wide, Testing and Conformance [continued]
- Fiscal Year 2026
- Consistent Representation of Policy & Consent [continued]
- Scalable Data Sharing Governance Framework [continued]
- Industry-wide, Testing and Conformance [continued]
- Fiscal Year 2027
- Consistent Representation of Policy & Consent [continued]
- Scalable Data Sharing Governance Framework [continued]
- Industry-wide, Testing and Conformance [continued]
Outcomes
- Ability to import/export primary care data to, from and between EMRs
- Clinicians able to change EMRs
- Governance model established
- Vendor support services available to all jurisdictions
- National procurement framework established
- Change management program in place
- 50% of Canadians enabled to directly access their longitudinal record
- 60% of primary care physicians reporting ability to exchange patient summary record
- 70% of clinicians with EMRs enabled to send clinical summaries through a vendor conformed solution
- 75% of Canadians enabled to access their patient summary record
- Benefits realized:
- Health System – $500M in improved interactions, effective use of ED, in-patient services, an reduction in duplicate tests
- Canadians – over $500M in saved patient time
- Clinicians – over $350M in saved time
Annex 3 – Indicators: Access to home and community care
Indicator
- Death at home or in community (Percentage)
- Home care services helped the recipient stay at home (Percentage)
- Wait times for home care services (Median, in days)
- Caregiver distress (Percentage)
- New long-term care residents who potentially could have been cared for at home (Percentage)
- Hospital stay extended until home care services or supports ready (Median, in days)
Annex 4 – Action plan
Introduction
Home care, community care, and long-term care services are critical to ensuring that Island residents can access the right type of care, in the right place, by the right provider at all stages of life. Island residents are living longer on average, and seniors are a growing share of the provincial population. Prince Edward Island has more seniors than ever before, and the province is shifting to match the changing demographic. Also, Island residents who are under 65 with complex care needs often require specialized support to address their unique care needs.
As of 2022, there were 34,664 Island residents age 65+ comprising 20.3% of the population in PEI (compared to 18.8% nationally). Fifty-four percent (54%) of Island seniors are female, compared to 45.7% male. Life expectancy at birth for females in PEI is 83.7 years, compared to 79.8 for males.
Approximately 3.8% of people age 65+ in PEI live in long-term care, with an average length of stay of 2.9 years. In 2022-23, there were 236 admissions to public long-term care homes in PEI, an increase of 100 new residents. There are approximately 1,244 long-term care beds in PEI, with 38.7 beds per 1,000 population age 65+.
In 2022-23 there were a total of 5,167 clients served by home care, 3,128 of whom were age 75+.
These statistics help inform the initiatives identified in this action plan.
Home and Community Care
Context
PEI has made Home and Community Care a strategic priority for seniors' health services. Inadequate home and community care services are known to negatively impact activities of daily living and are a strong predictor of institutionalization and overall utilization of health care services. In fact, older adults in PEI move to long-term care at a higher rate than many other provinces in part due to limited home supports, and many of those individuals move into long-term care without having received any home care services. As well, about 75% of total home care hours are currently being met by unpaid caregivers with the demand for potential unpaid caregivers expected to grow significantly.
These factors point to a need for improved access to a range of home and community-based supports to better address the health needs of older adults and individuals with complex medical conditions, with the aim of enabling seniors to age at home. Accessing the right care and supports closer to home can help older Islanders to remain home for as long as possible.
Public Home Care services in PEI are provided through the Home Care Program. The Home Care Program provides a range of health care and support services for acute, chronic, palliative, and/or rehabilitative health care needs, including:
- Nursing care: nursing procedures including health monitoring, IV therapy, injections, wound care, and patient teaching,
- Home support: assistance with daily activities such as bathing and dressing,
- Palliative care: comfort and support to live fully until the end-of-life,
- Social work: individual and family counseling for illness, loss, or end-of-life issues,
- Dietitian services: nutrition assessment and education,
- Physiotherapy: support to maximize independence, function, and mobility,
- Occupational Therapy: support for daily living, special devices, equipment, or modification to home or workplace,
- Adult Protection: for vulnerable adults who need protection from neglect or abuse,
- Long-term Care: assessment for long-term care facility admission, and
- Adult Day Programs: enriching social activities for seniors.
- Respiratory Therapy: treatment, rehabilitation and education of patients with heart and lung disorders
- Pharmacy: therapeutic and clinical appropriateness of drug therapy for safety and efficacy.
- Geriatric Program: interdisciplinary team providing specialized care and support to frail seniors and their families.
- Caring for Older Adults in the Community and at Home (COACH) Program: specialized team of health care professionals who support frail seniors to live at home longer and return home from hospital sooner.
Home Care Programming is provided based on assessed need at a point in time. Applications and referrals can be made by the client, family members, care providers, and family doctors through five Home Care Program offices across PEI (in Souris, Montague, Charlottetown, Summerside, and O'Leary) through a standardized and consistent Intake process. In 2024 the current Intake Assessment will be replaced with the InterRAI Contact Assessment.
Community care services are provided by 36 private community care facilities in PEI. These facilities are distributed tip-to-tip from Tignish to Souris so that Islanders can receive care close to family and friends. Community care facilities provide light care, assistance with meals, bathing, medications, laundry, and general basic supports for everyday living.
Seniors Mental Health Resource Teams (SMHRT) are multi-disciplinary teams that provide specialized services to seniors experiencing complex mental health problems, as well as support to their families and/or caregivers. SMHRTs are located in all three counties – Kings, Queens, and Prince – and include psychiatrists, nurse practitioners, registered nurses, licensed practical nurses, and social workers. SMHRTs provide service deliver in-office and to clients living at home or in community care through community outreach.
Achievements
Strides have been made in Home and Community Care since the inception of federal funding associated with the Common Statement of Principles on Shared Health Priorities (2017). Specifically:
- Launching of Mobile Integrated Health (MIH) services: provision of health care using patient-centred mobile resources in the community. These resources are delivered and coordinated by an array of health and social care entities, programs, services, and practitioners who are clinically integrated with emergency service providers. MIH programs include Seniors Check-in, Rapid Bridging, and Paramedics Providing Palliative Care. Paramedics support home-based chronic disease management, facilitate hospital discharge, and a palliative approach to care.
- Implementation of the InterRAI assessment tool for home care clients: ongoing implementation of the InterRAI assessment tool provides a basis for an outcome-based assessment of a patient's response to care or services, for enhanced continuum of care, and better system planning and reporting.
- Established Brackley Stables and the Small Options Home:
- Brackley Stables provides five beds for clients with mental illness and complex needs who require an extended period of support to transition to a community residential setting.
- The Small Options Home provides two long-term beds for clients with mental illness and complex needs who require a more intensive staffing model.
- Clients at both facilities are provided with care plans, life skill, and recreational programming to support connections with services and supports in the community.
Initiatives to be supported by federal funding over the next four years
Federal funding of up to $10.8M over four years will support Home and Community Care initiatives under the Mobile Integrated Health/Home Care-Community Paramedicine and Home and Community Care IT Infrastructure banners.
Mobile Integrated Health / Home Care-Community Paramedicine:
- The Mobile Integrated Health (MIH) initiative was launched in 2017. MIH aims to support individuals to access collaborative resources, without duplicating existing Public Home Care services.
- The following outlines a realignment and strengthening of services being provided by Public Home Care with the Community Paramedics further engrained into services and part of the Integrated team
- Federal funding of up to $5.2M over four years will be used to support two initiatives under this category, including the Hospital at Home team service and Palliative Home Care Coordinator staffing:
- Hospital at Home Team Service:
- The Hospital at Home Team Service enables patients to receive acute care at home, rather than in the hospital. This has been shown to improve patient outcomes and patient satisfaction, and is expected to increase acute care capacity as more patients receive care at home and outside of the hospital setting.
- LPNs, RNs, and Community Paramedics together in collaboration under one service with shared scope, mentoring and expanding to support vulnerable, frail senior population. Interventions include advanced wound care, assessments, central venous access device/care. No home care services will be replaced, the intent is focus and strengthen collaborations, access to services, and best utilizing funds, by building a Hospital at Home Team within the home-based care division.
- Palliative Home Care Coordinator Staffing:
- The province will establish key supports to improve care under the palliative stream of the MIH program. These investments will directly support one of the primary objectives of the Common Statement of Principles on Shared Health Priorities (2017) to improve access to appropriate services and supports in home and community, including palliative and end-of-life care.
- Federal funding for Palliative Home Care Coordinator staffing will enable the hiring of 3.4 FTE staff.
- Hospital at Home Team Service:
- The above initiatives align with the menu of actions outlined in the Common Statement of Principles on Shared Health Priorities (2017), specifically by:
- Providing an evidence-based model of home and community care that is more integrated and connected with primary health care;
- Enhanced access to palliative and end of life care at home; and
- Enhanced home care infrastructure through community-based service delivery.
- The Hospital-at-Home Service and Palliative Home Care Coordinator staffing initiatives are part of Health PEI's larger team of professionals, services, and programs in Home Care. The goal of the Home Care Program is to allow clients to age at home in their own communities, prevent ER visits, mitigate hospitalizations, support discharge from acute care, and to prevent early institutionalizations of older adults into long-term care. These programs also perform InterRAI contact assessment to support client care planning and allow the Home Care Program to submit additional population data to CIHI, with a goal of using those data at a client level for care planning, at a program level for service allocation, and at a system level for program development and resource allocation.
- Public Home Care initiatives and programs address the needs of vulnerable populations in PEI, particularly rural populations, individuals without access to a family physician including many recent immigrants and minority communities, individuals living with disabilities, and low-income individuals and families who may experience transportation challenges. Community Paramedics working in Public Home Care allow paramedics the opportunity to work alongside an integrated team of health professionals, visit clients in their homes, and assess living arrangements as they pertain to the social determinants of health. Home care services allow clients to experience a more seamless transition between various components of the health care continuum.
Home and Community Care IT Infrastructure:
- Improvements to Home and Community Care IT Infrastructure supports the needs of patients, health care providers, and administrators with the home and community care system. Investments in the InterRAI help to standardize client assessment and ensure consistency and evidence-informed decision-making. InterRAI was introduced into home care in 2022, providing health care professionals a standardized approach to assessing individuals' care needs and informing the most appropriate supports for the person.
- Home and Community Care IT Infrastructure initiatives align with the menu of actions outlined in the Common Statement on Shared Health Priorities (2017) as follows:
- Evidence-based model of home and community care that is more integrated and connected with primary health care; and
- Enhances home care infrastructure with a standardized digital assessment technology and modernized community-based service delivery.
- Federal funding of up to $4.0 million over four years will be used to secure and retain staffing to ensure robust support for the InterRAI Home Care Program.
| Home and Community Care Initiatives | 2023-24 | 2024-25 | 2025-26 | 2026-27 | Total |
|---|---|---|---|---|---|
| Total Funding Available | $3.0M | $2.6M | $2.6M | $2.6M | $10.8M |
| Hospital at Home | $1.6M | $1.2M | $1.2M | $1.2M | $5.2M |
| Palliative Home Care Coordinator Staffing | $400,000 | $400,000 | $400,000 | $400,000 | $1.6M |
| Home and Community Care IT Infrastructure | $1.0M | $1.0M | $1.0M | $1.0M | $4.0M |
| Total Planned Expenditure | $3.0M | $2.6M | $2.6M | $2.6M | $10.8M |
|
|||||
Measuring and reporting on results
PEI will continue to work with and provide data to the Canadian Institute for Health Information (CIHI) on the six pan-Canadian indicators for home and community care, to support measuring progress to improve access. Most recently, CIHI and PEI have amended bilateral funding and data sharing agreements to permit the disclosure of InterRAI home care data in the interest of supporting these indicators. The six pan-Canadian indicators for home and community care include:
- Death at Home or in Community;
- Home Care Services Helped the Recipient Stay at Home;
- Wait Times for Home Care Services (note – PEI does not currently submit data for this indicator, but is working to ensure data are available in the future);
- Caregiver Distress;
- New LTC Residents Who Potentially Could Have Been Cared for at Home; and
- Hospital Stay Extended Until Home Care Services or Supports Ready.
PEI will report annually on the following jurisdiction-specific indicators through the Department of Health and Wellness' regular annual reporting process, and through news releases related to specific initiatives and programs.
| Baseline | Target | Time Frame | |
|---|---|---|---|
| Mobile Integrated Health (MIH) / Hospital at Home Service | |||
| Active Hospital at Home caseloadFootnote a | 0 | 1,450 | March 2027 |
| Home and Community Care IT Infrastructure | |||
| Number of InterRAI home care assessments completed (annually) | 1,400 | 1,800 | 2024Footnote b |
| Number of InterRAI contact assessments completed (annually) | 0 | 2,000 | 2024Footnote b |
|
|||
Long-Term Care
Context
Prince Edward Island has both private and publicly owned long-term care (LTC) homes providing a total of 1,244 beds. The overall distribution of privately owned homes (for profit: 47% and not for profit: 6%) and publicly owned homes (47%) is comparable to the national average. There are nine publicly owned LTC homes and ten private LTC homes (eight of which are dual homes that contain both community care designated beds and long-term care beds). Services provided in both public and private LTC homes include:
- 24-hour care provided by resident care workers, licensed practical nurses, registered nurses, physicians, and nurse practitioners;
- Room and board;
- Personal care; and
- Medical services.
Within PEI LTC homes, residents have a variety of health and support requirements necessitating specialty services based on resident needs. These services include:
- Designated dementia care: Quality dementia care requires not only safe and supportive environmental design but also staff expertise. Residents who wander can more safely move within designated dementia care areas designed to reduce the risk of unsafe wandering. Most designated dementia care beds are currently in publicly funded LTC homes.
- Complex care: Some residents may have multiple chronic conditions, complex medication routines, be at higher risk of acute health changes, complex psychological and/or behavioural responses requiring high level monitoring and care. The number of Island residents with complex medical needs is growing and this increases the demand for those with skills and competencies in managing peritoneal dialysis, bariatric care, and advanced respiratory support such as overnight ventilation. Complex care requires increased physical and human resources most often found in public LTC homes.
- Cultural specialization: Recognizing and supporting diversity in long-term care is an important quality indicator. Respecting the diversity, cultural, and linguistic needs of residents can help to ease the transition to long-term care, reduce discrimination, isolation, communication barriers while improving overall quality of life. Some LTC homes in PEI offer cultural specialization by providing care in French, recognizing special culturally meaningful holidays, and offering traditional cuisine. Recruitment of fully bilingual staff has created challenges in offering culturally competent care.
- Young resident care: Some residents in PEI long-term care homes are under 60 years of age and require residential support to address complex care needs. This unique population has social, rehabilitation, and programming needs that may differ significantly from the majority of other residents and may be challenging to provide in the absence of allied health providers such as physiotherapists, speech therapists and occupational therapists. Prince Edward Home is currently the LTC home with the largest proportion of young residents. The care of young residents with complex care needs in LTC is a unique to PEI as other options for residential care are limited when compared to other jurisdictions.
- Respite care: Long-term care respite beds provide an opportunity for caregivers to schedule a temporary stay in a LTC home for their care receiver in a safe setting designed to meet care needs. There are a limited number of respite beds available in PEI, all of which are in public long-term care homes.
Achievements
The province of Prince Edward Island has taken several strategic actions towards better understanding and defining the priority issues which must be addressed to improve LTC services. The following section describes three key reports that have informed PEI's actions to improve LTC.
- The Seniors Health Services Plan: Aging Well 2021: In 2020 the Department of Health and Wellness commissioned work to establish a provincial plan for seniors' health services. In collaboration with Health PEI, the Department of Social Development and Seniors, and older adults, a steering committee of senior staff and leaders examined areas of strength and opportunities for improvement across the continuum of health services offered to older adults. These health services included health promotion, primary and acute care, home care, residential care, long-term care, and end of life supports. This plan was used by the Department of Health and Wellness to establish a strategic direction for seniors' health services. The Seniors Health Services Plan: Aging Well 2021 has been foundational in leveraging new investments and informing plans for federal funding to achieve progress in three priority areas:
- Providing care at home and closer to home
- Ensuring quality and safety across the seniors' health service continuum, and
- Strengthening health human resources dedicated to seniors' health services.
- Internal Long-term Care Review (2021): As a related project arising from the development of the Seniors Health Services Plan and in the wake of increasing evidence that older adults in residential settings were disproportionately impacted by COVID-19 an internal review of long-term care homes was conducted under the direction of an expert Steering Committee for the purpose of informing decision making and future investments. The Internal Long-term Care Review 2021 examined PEI's LTC sector (private and public) to:
- Describe the current context (physical environments, staffing, resident health, and wellness);
- Identify the differences within the private and public LTC sectors; and
- Identify information, monitoring, and reporting gaps.
- This rapid internal review identified several important challenges facing the LTC care sector:
- Long-term care homes had become a default solution for gaps in funding for home care and community-based services. Though the majority of older adults live in their own homes and age in community, much of public discourse portrays long-term care homes as an inevitability for older adults. This skewed transitioning towards institutionalizing older adults, both earlier and longer, in the absence of other options that are required to prevent premature admission to LTC homes.
- Many older adults waiting for a designated dementia care bed on Prince Edward Island were waiting in hospital. Waiting for a long-term care bed in a hospital has adverse consequences for older adults and the overall health system. For older adults, a loss of mobility, risk of exposure to hospital acquired illness, and negative social impacts may arise during an extended alternate level of care (ALC) stay in hospital. High rates of ALC reduces the health system's capacity to admit, accept transfers from the emergency department, delays the transfer of inpatients to appropriate units, and potentially prevents older adults from receiving care in the optimal setting.
- Current information systems did not support the collection and reporting of resident health outcome information in long-term care homes. Planned initiatives which will establish InterRAI as a standard within long-term care homes would support data collection, monitoring of trends and reporting. The use of InterRAI will also facilitate the comparison of Prince Edward Island health data to that of other provinces.
- PEI public and private long-term care homes operated in markedly different ways. These differences included access to primary care, quality assessment, adverse event reporting, infection prevention and control, staff training, access to allied health care providers, and staff compensation. Efforts to align quality and safety measures between public and private LTC homes are underway to ensure that Island residents received comparable care across the sector.
- COVID-19 Long-term Care Review: As noted by the national media, researchers, and advocates the COVID-19 pandemic exposed long-standing quality and safety gaps in long-term care which required action. Understanding the degree to which these nationally profiled quality and safety issues impacted long-term care on PEI provided the impetus for an external review of the measures taken to prevent and contain the spread of COVID-19 in LTC homes. As part of the scope of the review the external panel was directed to comment on the pandemic impact of existing physical infrastructure, staffing, clinical oversight, and the system's readiness to implement new national LTC standards. The COVID-19 Long-term Care Review identified several pre-existing conditions that exacerbated the effects of the pandemic:
- LTC homes were not sufficiently prepared for a pandemic;
- Public and private LTC homes in the province operate differently, resulting in multiple inconsistencies and inequities, e.g., in resource availability, resident and family access to services, gaps in wages and benefits for staff;
- Staffing levels had not kept pace with the increased complexities of today's resident population; and
- Neither LTC homes nor the system had sufficient data with which to manage the system or a major event such as a pandemic.
Several pandemic specific challenges were also noted:
- Resident-centred care quality deteriorated;
- Facility lockdowns intensified resident isolation and had a negative impact on resident health quality of life and that of their family or partners in care;
- Staffing was insufficient to balance the demands of the pandemic with resident care;
- Restrictions on staff mobility between workplaces negatively affected the ability of operators to adequately staff their homes; and
- Elevated levels of stress and burnout had a negative effect on workers and resulted in workers leaving LTC.
The review contained 17 recommendations, cross linked to the new national LTC standards as applicable, in the following four areas designed to improve resident care:
- enhancing resident-centred care;
- strengthening infection prevention and control;
- workforce recovery and development; and
- improving the long-term resiliency of PEI's LTC system (oversight and accountability).
The Government of Prince Edward Island has accepted the findings of the COVID-19 LTC Review and has committed to collaborating with the LTC sector to make progress towards improving resident care.
Initiatives to be supported by incremental federal funding over the next five years
PEI public and private long-term care homes operate in markedly different ways. These differences include access to primary care, quality assessment, adverse event reporting, infection prevention and control, clinical information systems, staff training, access to allied health care providers, and staff compensation. Many of the long-term care initiatives to be supported by incremental federal funding over the next five years are aimed at aligning quality and safety measures between public and private long-term care homes to ensure Island residents receive comparable care across the sector.
Federal funding of up to $19.0M over five years will be used to support four initiatives under long-term care, including expanding allied health care providers in private long-term care, expanding InterRAI into private long-term care, establishing a capital funding program for private long-term care, and establishing a mobile x-ray unit.
Expand Allied Health Care Providers in Private Long-term Care:
- Allied health care providers offer a range of recreation, rehabilitation, and wellness services to improve the lives of residents. The availability of these providers varies between long-term care homes, with physiotherapists, occupational therapists, and recreation therapists representing approximately 4% of staff members in private long-term care homes (as of April/May 2021).
- Some residents in PEI long-term care homes are under 60 years of age and require social, rehabilitation, and programming needs that may differ significantly from most other residents. These needs can be challenging to meet in the absence of allied health providers.
- The COVID-19 LTC Review found that inequities in access to allied health care providers existed between the public and private LTC sectors and recommended that steps be taken to increase access to allied health care providers in private LTC homes.
- This recommendation is consistent with CAN/HSO standard 5.1.1 which seeks to provide team-based care through appropriate staffing levels, mix, and ratio of providers.
- The current average of allied health care providers in publicly funded LTC homes is:
- OT/PT and assistants: 0.05 hours per resident day;
- Recreation and activity providers: 0.21 hours per resident day; and
- Dietitians: 2.1 FTE.
- Federal funding of up to $3.2M over five years for this initiative will enable the hiring of additional allied health providers to provide services to private long-term care homes, with the purpose of improving the recreation, rehabilitation, and wellness of residents, leading to higher quality of life.
Expand InterRAI into Private Long-term Care Sector:
- Current information systems do not support the collection and reporting of resident health outcome information in private long-term care homes. PEI has made significant efforts towards implementing InterRAI in recent years with phase 1 of implementation set to occur in public homes in 2024-25. Implementing InterRAI in private long-term care homes as well will support data collection, monitoring of trends, and reporting across the public and private arms of the long-term care sector. The use of InterRAI will also facilitate the comparison of PEI health data to that of other provinces and territories.
- InterRAI is the international standard for assessing the care needs of our most vulnerable populations. Having this standardized tool available for use within private long-term care will help ensure the best care is provided, to each individual, in the right place, and at the right time.
- Ten private long-term care facilities will be served by providing this service. By using a standardized assessment instrument, all Island residents will be better served, whether they reside in a public or private long-term care home. As InterRAI is the national standard, all health-care providers from coast to coast will be enabled to better understand and provide optimal care. The InterRAI standard levels the playing field and ensures that every individual is assessed through an unbiased lens.
- It is anticipated that the introduction of InterRAI in private long-term care homes (as well as public long-term care homes) will support a more nuanced understanding of risk ratios, the interplay of resident factors (both biological and behavioural), and the risk of falls for long-term care residents through the collection of more complete and comparable data.
- Federal funding of up to $6.0M over five years will support the implementation of InterRAI in private long-term care homes for comparable data standards across the long-term care sector in PEI.
Establish a Capital Funding Program for Private Long-term Care Facilities:
- Many of the long-term care initiatives identified in this plan are intended to help mitigate the demand for long-term care beds while respecting seniors' desire to live at home for as long as possible. However, PEI population projections suggest that additional seniors' long-term care beds will be required to meet the care needs of the increasing number of older adults.
- As well, the impact of the COVID-19 pandemic has shifted the attention to the design of long-term care homes and infection prevention and control procedures. Efforts to enhance infection prevention and control measures have resulted in many challenges for long-term care services, and the pandemic exposed long-standing quality and safety gaps which require action.
- A long-term care home capital development program is intended to govern the provision of funding to eligible private operators to support the development of new long-term care beds or facilities, or the redevelopment of existing long-term care beds or facilities to current design and infection prevention and control standards.
- Private long-term care facilities are struggling to secure funding for new long-term care beds. The DHW is updating its long-term care bed projections. Accurate projections will enable the DHW to better target where new builds and new long-term care beds should be developed.
- PEI currently has 10 private long-term care facilities in locations across the province, focused primarily in Charlottetown (with six facilities). As well, PEI residents are served by 36 community care facilities with a wider distribution across the province, from Tignish and Alberton in western PEI to Souris and Montague in eastern PEI. Tables 3 and 4 provide more detail on private long-term care homes and community care homes in the province. Note that some facilities house both private long-term care and community care.
- Federal funding will support a new capital fund that will permit long-term care facilities to build new beds, and community care facilities to build and/or convert sections of their facilities into long-term care beds. This will enable the provision of long-term care services to residents in more places throughout PEI, permitting them to remain closer to home, family, and friends. Rural areas in PEI feature higher proportions of seniors, a higher proportion of official language minority communities (francophone Acadians), and the Island's two prominent Mi'kmaq communities (Abegweit First Nation and Lennox Island First Nation).
- Capital funding to private facilities under this priority will be accompanied by contract agreements that describe funding parameters, including where and how funds are to be used, eligible and ineligible projects, and reporting and accountability requirements. Agreements will require private facilities to agree to a recovery mechanism whereby facilities that do not use the entire funding, or who use the funding for projects not specifically authorized by the Department of Health and Wellness, will be required to refund excess funds or ineligible funds back to the provincial government.
- Federal funding of up to $6.9M over five years will support capital projects in private long-term care homes to ensure that capacity and infection prevention and control measures are comparable across the long-term care sector in PEI.
| Long-term Care Home | Location | Urban/Rural |
|---|---|---|
| Andrews of Park West | Charlottetown | Urban |
| Andrews of Stratford | Stratford | Urban |
| Andrews of Summerside | Summerside | Urban |
| Clinton View Lodge | Kensington | Rural |
| Dr. John Gillis Memorial Lodge | Belfast | Rural |
| Garden Home | Charlottetown | Urban |
| PEI Atlantic Baptist Home | Charlottetown | Urban |
| South Shore Villa | Crapaud | Rural |
| The Mount Continuing Care Community | Charlottetown | Urban |
| Whisperwood Villa | Charlottetown | Urban |
| Community Care Facility | Location | Urban/Rural |
|---|---|---|
| Andrews of Charlottetown | Charlottetown | Urban |
| Andrews of Park Hill | Summerside | Urban |
| Andrews of Park West | Charlottetown | Urban |
| Andrews of Stratford | Stratford | Urban |
| Andrews of Summerside | Summerside | Urban |
| Bayview Lodge | Souris | Rural |
| Bevan Lodge | Sherwood | Urban |
| Burnside Community Care | Clyde River | Rural |
| Champion Lodge | Charlottetown | Urban |
| Charlotte Residence | Charlottetown | Urban |
| Clinton View Lodge | Kensington | Rural |
| Corrigan Home | Charlottetown | Urban |
| Dr. John Gillis Memorial Lodge | Belfast | Rural |
| Emerson Lodge | Charlottetown | Urban |
| Geneva Villa | Charlottetown | Urban |
| Grafton House | Charlottetown | Urban |
| Kensington Community Care Home | Kensington | Rural |
| La Cooperative Le Chez Nous Ltee. | Wellington | Rural |
| Lady Slipper Villa | O'Leary | Rural |
| Langille House | Charlottetown | Urban |
| MacKinnon Pines Lodge | Montague | Rural |
| Miscouche Villa | Miscouche | Rural |
| Old Rose Lodge | Charlottetown | Urban |
| Perrins Marina Villa | Montague | Rural |
| Rev. W.J. Phillips Residence | Alberton | Rural |
| Rosewood Residence | Hunter River | Rural |
| South Shore Villa | Crapaud | Rural |
| Stamper Residence | Charlottetown | Urban |
| Tenderwood Lodge | Charlottetown | Urban |
| The Mews | Margate | Rural |
| The Mount Continuing Care Community | Charlottetown | Urban |
| Tignish Seniors Home Care Cooperative | Tignish | Rural |
| Valley House | Charlottetown | Urban |
| Villa Marguerite | North Rustico | Rural |
| Whisperwood Villa | Charlottetown | Urban |
| Woodland Home | Souris | Rural |
Establish a Mobile X-Ray Unit for Long-term Care:
- The Mobile X-Ray program will support our commitments to expedite offload delays for ambulances at hospitals by reducing transfers for non-urgent diagnostic imaging and reduce response time of ambulances by ensuring ambulance services are available for other types of transfers and emergency situations.
- This initiative also supports our priority to provide a seamless experience for patients. By providing x-ray services in long-term care facilities, patients can remain in their home to access care and reduce stresses associated with transportation between care settings for services.
- The initial phase of the rollout of this program began in fall, 2023 in Charlottetown and will expand to serve all private and public long-term care facilities across PEI. The opportunity to rollout Mobile X-Ray units to serve community care and home care settings will be explored depending on the success of the program.
- It is anticipated that mobile X-ray units will help to reduce the demand on patient transfers between long-term care and hospital settings for diagnostic imaging and contribute to reduced off-load delays within PEI hospitals.
- Staff will be supported with communication materials created specifically for the program (e.g. posters, scripts to help have conversations about the program, process details, etc.) and DHW and HPEI will work closely with each participating home to ensure the right infrastructure and safety measures in place to support the program.
- Federal funding of up to $2.9M over five years will enable the purchase and operation of mobile x-ray units across the province to provide seamless care to long-term care patients in their place of residence.
| Long-Term Care Initiative | 2023-24 | 2024-25 | 2025-26 | 2026-27 | 2027-28 | Total |
|---|---|---|---|---|---|---|
| Priority Area 1 – Workforce Stability | ||||||
| Initiative 1 – Enhance Health Care Provider Support in LTC | ||||||
| Expand allied health care providers in private long-term care | $300,000 | $500,000 | $800,000 | $800,000 | $800,000 | $3.2M |
| Subtotal | $300,000 | $500,000 | $800,000 | $800,000 | $800,000 | $3.2M |
| Priority Area 2 – Long-Term Care Standards | ||||||
| Initiative 1 - Long-term Care IT Infrastructure | ||||||
| Expand InterRAI into Private Long-term Care Sector | $800,000 | $1.3M | $1.3M | $1.3M | $1.3M | $6.0M |
| Subtotal | $800,000 | $1.3M | $1.3M | $1.3M | $1.3M | $6.0M |
| Initiative 2 – Long-term Care Capital Infrastructure | ||||||
| Establish a Capital Funding Program for Private Long-term Care Facilities | $1.5M | $1.58M | $1.28M | $1.28M | $1.28M | $6.92M |
| Establish a Mobile X-Ray Unit | $1.2M | $420,000 | $420,000 | $420,000 | $420,000 | $2.88M |
| Subtotal | $2.7M | $2.0M | $1.7M | $1.7M | $1.7M | $9.8M |
| TOTAL | $3.8M | $3.8M | $3.8M | $3.8M | $3.8M | $19.0M |
| * Allocations are rounded and notional, based on the 2022 July 1st population estimate published by Statistics Canada. | ||||||
Accountability Measures in Place for Funds Directed to Private For-Profit Facilities
- Funding that is provided directly to private facilities for long-term care initiatives, specifically capital and IT (InterRAI) projects, will be accompanied by contract agreements that describe funding parameters, including where and how funds are to be used, eligible and ineligible projects, and reporting and accountability requirements. Agreements will require private facilities to agree to a recovery mechanism whereby facilities that do not use the entire funding, or who use the funding for projects not specifically authorized by the Department of Health and Wellness, will be required to refund excess funds or ineligible funds back to the provincial government
- If funds must be recovered by the provincial government, those funds will be redistributed among other private LTC facilities for eligible projects under the priority areas for Long-Term Care Aging with Dignity funds. Redistribution of funds to eligible private LTC facilities will be allocated on a per-bed basis, with possible adjustments based on need.
- See tables 3 and 4 for a list of private long-term care and community care facilities in PEI.
Measuring and reporting on results
- PEI commits to working with CIHI to establish common LTC indicators, and will work with CIHI to begin submitting data from InterRAI to CIHI..
- PEI will report annually on the following jurisdiction-specific indicators through the Department of Health and Wellness' regular annual reporting process, and through news releases related to specific initiatives and programs.
| Indicator | Baseline | Targets | Timeframe |
|---|---|---|---|
| Priority Area 1 – Workforce Stability | |||
| Enhance Health Care Provider Support in LTC | |||
| Hours per week per 100 residents of OT/PT support to private LTC facilities | 0 | 11 hrs OT 10 hrs PT |
March 2028 |
| Hours per week per 100 residents of Nutritionist support to private LTC facilities | 0 | 32 hrs | March 2028 |
| Priority Area 2 – Long-Term Care Standards | |||
| Long-term Care IT Infrastructure | |||
| Number of clients assessed with InterRAI prior to entry into private LTC | 0 | All | March 2028 |
| Long-term Care Capital Infrastructure | |||
| Reduction in transfers for diagnostic imaging per year, per mobile x-ray unitFootnote a | 0 | 225 | March 2028 |
|
|||
| 2023-24 | 2024-25 | 2025-26 | 2026-27 | 2027-28 | Total | |
|---|---|---|---|---|---|---|
| Home and Community Care | $3.0M | $2.6M | $2.6M | $2.6M | n/a | $10.8M |
| Long-Term Care | $3.8M | $3.8M | $3.8M | $3.8M | $3.8M | $19.0M |
| TOTAL | $6.8M | $6.4M | $6.4M | $6.4M | $3.8M | $29.4M |
| * Total federal funding available for Home and Community care in 2023-2024 includes the estimated $400,000 carry-forward from the Canada-PEI Home and Community Care and Mental Health and Substance Use 2022-2023 Agreement. | ||||||
Footnotes
- Footnote 1
-
https://www2.gov.bc.ca/assets/gov/government/ministries-organizations/ministries/indigenous-relations-reconciliation/declaration_act_action_plan.pdf
- Footnote 2
-
https://engage.gov.bc.ca/app/uploads/sites/613/2020/11/In-Plain-Sight-Summary-Report.pdf