Canada-Prince Edward Island Home and Community Care and Mental Health and Addictions Services Funding Agreement
Table of Contents
- Funding Agreement
- Annex I - Common Statement of Principles on Shared Health Priorities
- Annex II - Action Plans
Funding Agreement
BETWEEN:
HER MAJESTY THE QUEEN IN RIGHT OF CANADA (hereinafter referred to as "Canada" or "Government of Canada") as represented by the Minister of Health (herein referred to as "the federal Minister")
- and -
HER MAJESTY THE QUEEN IN RIGHT OF THE PROVINCE OF PRINCE EDWARD ISLAND (hereinafter referred to as "Prince Edward Island" or "Government of Prince Edward Island") as represented by the Minister of Health and Wellness (herein referred to as "the provincial Minister")
REFERRED to collectively as the "Parties"
PREAMBLE
WHEREAS, on January 31, 2016 Canada and Prince Edward Island agreed to targeted federal funding over 10 years, beginning in 2017-18, for investments in home and community care and mental health and addictions, in addition to the existing legislated commitments through the Canada Health Transfer;
WHEREAS, Canada and Prince Edward Island agreed to a Common Statement of Principles on Shared Health Priorities (hereinafter referred to as the Common Statement, attached hereto as Annex 1) on August 21, 2017, which articulated their shared vision to improve access to home and community care as well as mental health and addictions services in Canada;
WHEREAS, Canada authorizes the federal Minister to enter into agreements with the provinces and territories, for the purpose of identifying activities provinces and territories will undertake in home and community care and mental health and addictions services, based on a menu of common areas of action and in keeping with the performance measurement and reporting commitments, consistent with the Common Statement;
WHEREAS Canada and Prince Edward Island agree that data collection and public reporting of outcomes is key to reporting results to Canadians on these health system priorities, and that the performance measurement approach taken will recognize and seek to address differences in access to data and health information infrastructure;
WHEREAS, the Financial Administration Act R.S.P.E.I, c- F-9 authorizes the provincial Minister to enter into agreements with the Government of Canada under which Canada undertakes to provide funding toward costs incurred by the Government of Prince Edward Island for the provision of health services which includes home and community care and mental health and addictions initiatives;
WHEREAS, Prince Edward Island makes ongoing investments in home and community care and mental health and addictions services, consistent with its broader responsibilities for delivering health care services to its residents;
WHEREAS the Government of Canada makes ongoing investments in home and community care and mental health and addictions services for Indigenous communities and other federal populations.
WHEREAS, since March 2020, Canada has been in the midst of the COVID-19 global pandemic, which has disproportionately affected Canadians living in supportive care settings in the community, namely long-term care facilities, assisted living facilities, and seniors' residences where they receive continuing care services (hereinafter referred to as long-term care settings), and which is requiring provinces and territories to put in place stronger measures to reduce the risk of harm to residents of these facilities;
WHEREAS, the Government of Canada announced an investment of $19 billion to help provinces and territories to safely restart their economies and make Canada more resilient to possible future surges in cases of COVID-19, of which $740M is to support provinces and territories through 2020-21 with one-time investments for infection prevention and control, including in long-term care settings;
WHEREAS, on November 30, 2020, the Government of Canada committed to a further investment of $1 billion to support provinces and territories to protect residents in long-term care settings, given the continued serious risk to health of these vulnerable Canadians;
WHEREAS, Canada authorizes the federal Minister to enter into agreements with the provinces and territories, for the purpose of identifying activities provinces and territories will undertake to protect residents in long-term care settings through increased infection prevention and control measures and in keeping with performance measurements and reporting commitments;
AND WHEREAS, the Financial Administration Act R.S.P.E.I, c- F-9 authorizes the provincial Minister to enter into agreements with the Government of Canada under which Canada undertakes to provide Safe Long-term Care Funding toward expenditures incurred by Prince Edward Island for activities to protect residents in long-term care settings through increased infection prevention and control measures;
NOW THEREFORE, Canada and Prince Edward Island agree as follows:
1.0 Objectives
1.1 Building on Prince Edward Island's existing investments and initiatives, Canada and Prince Edward Island commit to work together to improve access to home and community care and strengthen access to mental health and addictions services (listed in the Common Statement, attached as Annex 1).
1.2 Further, Canada and Prince Edward Island commit to work together to improve access to safe care through increased infection prevention and control in long-term care settings.
2.0 Action Plan
2.1 Prince Edward Island will invest federal funding for Home and Community Care and Mental Health and Addictions Services provided through this Agreement in alignment with the selected action(s) from each menu of actions listed under home and community care and mental health and addictions in the Common Statement.
2.2 Prince Edward Island's approach to achieving home and community care and mental health and addictions services objectives is set out in their five-year Action Plan (2017-18 to 2021-22), as set out in Annex 2.
2.3 Prince Edward Island will invest the federal Safe Long-term Care Funding provided under this Agreement on infection prevention and control activities in long-term care settings in each of the following three areas:
- Retention measures for existing staff, including wage top-ups, and/or hiring of additional human resources (e.g. personal support workers, licensed practical nurses, cleaners);
- new infrastructure and renovations to existing infrastructure, such as ventilation of self-isolation rooms and single rooms; and,
- readiness assessments conducted in long-term care settings to prevent COVID infections and spread.
2.4 In addition, Prince Edward Island may also invest the federal Safe Long-term Care Funding through this Agreement on infection prevention and control activities in long-term care settings in one or more of the following areas;
- Strengthened infection prevention and control measures and training for existing staff;
- adequate supply of personal protective equipment for staff and visitors;
- rapid training programs to increase the number of supportive care workers, including training for students and workers from other sectors;
- enhanced screening and regular testing of staff and visitors to quickly detect, prevent or limit spread; and,
- additional inspectors and infection prevention and control specialists to support in-person inspections of all facilities, as well as accreditation costs associated with meeting long-term care standards.
2.5 Prince Edward Island's approach to achieving the objective of the Safe Long-term Care Funding, as set out in section 1.2, in the areas identified above, is set out in Annex 2, as amended.
3.0 Term of Agreement
3.1 The term of this agreement is four years, from April 1, 2018 to March 31, 2022 (the Term).
3.2 Subject to sections 4.4 and 4.5, the Safe Long-term Care Funding provided under this Agreement may be used by Prince Edward Island for expenditures that are incurred from December 1, 2020, to March 31, 2022.
3.3 Renewal of Bilateral Agreement
3.3.1 Prince Edward Island's share of the federal funding for 2022-23 to 2026-27, based on the federal commitment in Budget 2017 of $11 billion over ten years, will be provided upon the renewal of bilateral agreements, subject to appropriation by Parliament, and Prince Edward Island and Canada's agreement on a new five-year action plan.
3.3.2 The renewal will provide Prince Edward Island and Canada the opportunity to review and course correct, if required, and realign new priorities in future bilateral agreements based on progress made to date.
4.0 Financial Provisions
4.1 The contributions made under this Agreement are in addition and not in lieu of those that Canada currently provides to Prince Edward Island under the Canada Health Transfer to support delivering health care services within their jurisdiction.
4.2 Allocation to Prince Edward Island
4.2.1 In this Agreement, "Fiscal Year" means the period commencing on April 1 of any calendar year and terminating on March 31 of the immediately following calendar year.
4.2.2 Canada has designated the following maximum amounts to be transferred in total to all provinces and territories under this initiative on a per capita basis for the Term starting on April 1, 2018 and ending on March 31, 2022.
Home and Community Care
- $600 million for the Fiscal Year beginning on April 1, 2018
- $650 million for the Fiscal Year beginning on April 1, 2019
- $650 million for the Fiscal Year beginning on April 1, 2020
- $900 million for the Fiscal Year beginning on April 1, 2021
Mental Health and Addictions Services
- $250 million for the Fiscal Year beginning on April 1, 2018
- $450 million for the Fiscal Year beginning on April 1, 2019
- $600 million for the Fiscal Year beginning on April 1, 2020
- $600 million for the Fiscal Year beginning on April 1, 2021
Safe Long-term Care
- $1 billion for the Fiscal Year beginning on April 1, 2021
4.2.3 For Home and Community Care and Mental Health and Addictions Services, annual funding will be allocated to provinces and territories on a per capita basis, for each Fiscal Year that an agreement is in place. The per capita funding for each Fiscal Year, are calculated using the following formula: F x K/L, where:
F is the annual total funding amount available under this program (funding amount will change depending on Fiscal Year);
K is the total population of the particular province or territory, as determined using annual population estimates from Statistics Canada; and
L is the total population of Canada, as determined using annual population estimates from Statistics Canada.
For Safe Long-term Care, annual funding will be allocated to provinces and territories with a base amount of $2,000,000 for each province and territory, and the remainder of the fund allocated on a per capita basis, for each Fiscal Year that an agreement is in place. The total amount to be paid to Prince Edward Island will be calculated using the following formula: $2,000,000+ (F- (N x 2,000,000)) x (K/L), where:
F is the total one-time funding amount available under this initiative;
N is the number of jurisdictions (all 13) that will be provided the base funding of $2,000,000;
K is the total population of a particular province or territory, as determined using the annual population estimates from Statistics Canada; and,
L is the total population of Canada, as determined using annual population estimates from Statistics Canada.
4.2.4 For the purposes of the formula in section 4.2.3, the population of Prince Edward Island for each fiscal year and the total population of all provinces and territories for that Fiscal Year are the respective populations as determined on the basis of the quarterly preliminary estimates of the respective populations on July 1 of that Fiscal Year. These estimates are released by Statistics Canada in September of each Fiscal Year.
4.2.5 Subject to annual adjustment based on the formulas described in section 4.2.3, Prince Edward Island's estimated share of the amounts will be:
| Fiscal Year | Home and community care Estimated amount to be paid to Prince Edward IslandTable note* (subject to annual adjustment) |
Mental health and addictions services Estimated amount to be paid to Prince Edward IslandTable note* (subject to annual adjustment) |
|---|---|---|
| 2018-2019 | $2,480,000 | $1,040,000 |
| 2019-2020 | $2,690,000 | $1,860,000 |
| 2020-2021 | $2,690,000 | $2,480,000 |
| 2021-2022 | $3,730,000 | $2,480,000 |
|
||
4.2.6 Subject to annual adjustment based on the formulas described in subsection 4.2.3, Prince Edward Island's estimated share of the amounts will be:
| Fiscal Year | Safe Long-term Care Estimated amount to be paid to Prince Edward IslandFootnote * (subject to annual adjustment) |
|---|---|
| 2021-2022 | $ 6,090,876 |
|
|
4.3 Payment
4.3.1 Canada's contribution for Home and Community Care and Mental Health and Addictions Services will be paid in approximately equal semi-annual installments as follows:
- The first installment will be paid on or about April 15 of each Fiscal Year. The second installment will be paid on or about November 15 of each Fiscal Year.
- The amount of the first installment will be equal to 50% of the notional amount set out in Article 4.2.5 as adjusted by Article 4.2.3.
- The amount of the second installment will be equal to the balance of Canada's contribution to Prince Edward Island for the Fiscal Year as determined under sections 4.2.5 and 4.2.3.
- Canada will notify Prince Edward Island at the beginning of the Fiscal Year of their notional amount. The notional amount will be based on the Statistics Canada quarterly preliminary population estimates on July 1 of the preceding Fiscal Year. Canada will notify Prince Edward Island of the actual amount of the second installment in each Fiscal year as determined under the formula set out in sections 4.2.5 and 4.2.3.
- Canada shall withhold payment of the second installment for the Fiscal Year if Prince Edward Island has failed to provide its annual financial statement for the previous Fiscal Year or to provide data and information related to home and community care and mental health and addictions to CIHI for the previous Fiscal Year in accordance with section 5.1.2
- The sum of both semi-annual installments constitutes a final payment and is not subject to any further adjustment once the second installment of that Fiscal Year has been paid.
- Payment of Canada's funding for each Fiscal Year of this Agreement is subject to an annual appropriation by Parliament of Canada for this purpose.
4.3.2 Canada's contribution for Safe Long-term Care will be paid in approximately equal semi-annual installments as follows:
- The first installment will be paid within 30 days of Canada's acceptance of Prince Edward Island's proposed approach and initiatives for the use of the Safe Long-term Care Funding, as set out in Annex 2.
- The second installment will be paid on or about December 15, 2021, following Prince Edward Island's fulfillment of the obligations identified in subsection 5.1.2, and amendment of Annex 2 in accordance with subsection 5.1.3.
4.3.3 Where Prince Edward Island fails to put in place a cost-recovery agreement as required pursuant to section 4.8, Canada shall deduct from the payment referred to in subsection 4.3.2(b) an amount equivalent to the amount of funding provided by Prince Edward Island to those facilities with whom they do not have the required cost-recovery agreements in place.
4.4. Carry Over
4.4.1. At the request of Prince Edward Island, Prince Edward Island may retain and carry forward to the next Fiscal Year the amount of up to 10 per cent of the contribution paid to Prince Edward Island for a Fiscal Year under subsection 4.2.5 and 4.2.6. that is in excess of the amount of the eligible costs actually incurred by Prince Edward Island in that Fiscal Year, and use the amount carried forward for expenditures on eligible areas of investment incurred in that Fiscal Year. Any request by Prince Edward Island to retain and carry forward an amount exceeding 10 per cent will be subject to discussion and mutual agreement in writing by the Parties via an exchange of letters.
4.4.2. For greater certainty, any amount carried forward from one Fiscal Year to the next under this subsection is supplementary to the maximum amount payable to Prince Edward Island under subsection 4.2.5. and 4.2.6. of this Agreement in the next Fiscal Year.
4.4.3 In the event this bilateral agreement is renewed in accordance with the terms of section 3.2.1, and at the request of Prince Edward Island, Prince Edward Island may retain and carry forward up to 10 percent of funding provided in the last Fiscal Year of this Agreement for eligible areas of investment in the renewed 5-year agreement (2022-23 to 2026-27), subject to the terms and conditions of that renewed agreement. The new Action Plan (2022-23 to 2026-27) will provide details on how any retained funds carried forward will be expended. Any request by Prince Edward Island to retain and carry forward an amount exceeding 10 per cent will be subject to discussion and mutual agreement in writing by the Parties via an exchange of letters.
4.5. Repayment of overpayment
4.5.1. In the event payments made to Prince Edward Island exceed the amount to which Prince Edward Island is entitled under this Agreement, the amount of the excess is a debt due to Canada and, unless otherwise agreed to in writing by the Parties, Prince Edward Island shall repay the amount within sixty (60) calendar days of written notice from Canada.4.6. Use of Funds
4.6.1. Canada and Prince Edward Island agree that funds provided under this Agreement will only be used by Prince Edward Island in accordance with the areas of action outlined in Annex 2.
4.7. Eligible Expenditures
4.7.1 Eligible expenditures for funds provided under this Agreement are the following:- capital and operating funding,
- salaries and benefits;
- training, professional development;
- information and communications material related to programs;
- data development and collection to support reporting; and,
- information technology and infrastructure.
4.7.2 Canada and Prince Edward Island agree that amounts paid to Prince Edward Island under the Safe Long-term Care Fund may be provided by Prince Edward Island to:
- Publicly-owned long-term care settings;
- privately-owned not-for-profit long-term care settings; and,
- subject to section 4.8, privately-owned for-profit long-term care settings.
4.8 Cost Recovery
4.8.1 Where Prince Edward Island provides Safe Long-term Care Funding to privately-owned, for-profit facilities in accordance with this Agreement, Prince Edward Island agrees to put in place cost-recovery agreements with these facilities and report on these agreements through amendments to Annex 2 by no later than December 1, 2021 in accordance with the requirements set out in subsection 5.1.3
4.8.2 Where Prince Edward Island has cost-recovery agreements in place with one or more privately-owned for-profit facilities pursuant to subsection 4.8.1, Prince Edward Island agrees to invest all funds recovered through those agreements in accordance with the terms of this Agreement and the initiatives outlined in Annex 2.
5. Performance Measurement and Reporting to Canadians
5.1 Funding conditions and reporting
5.1.1 As a condition of receiving annual federal funding, Prince Edward Island agrees to participate in a Federal-Provincial-Territorial process, including working with stakeholders and experts, through the Canadian Institute for Health Information (CIHI), to develop common indicators and to share relevant data in order to permit CIHI to produce annual public reports that will measure pan-Canadian progress on home and community care and mental health and addictions services.
- Prince Edward Island will designate an official or official(s), for the duration of this agreement, to work with CIHI and represent the interests of Prince Edward Island related to performance measurement and reporting for home and community care, as well as mental health and addictions services.
5.1.2 As a condition of receiving annual federal funding, by no later than October 1 of each Fiscal Year during the Term of this Agreement, Prince Edward Island agrees to:
- Provide data and information (based on existing and new indicators) related to home and community care and mental health and addictions services to the Canadian Institute for Health Information annually. This will support the Canadian Institute for Health Information to measure progress on the shared commitments outlined in the Common Statement and report to the public.
- Provide to Canada an annual financial statement, with attestation from the province's Chief Financial Officer, of funding received from Canada under this Agreement during the Fiscal Year compared against the action plan, and noting any variances, between actual expenditures and Prince Edward Island's Action Plan (Annex 2):
- The revenue section of the statement shall show the amount received from Canada under this Agreement during the Fiscal Year;
- The total amount of funding used for home and community care and mental health and addictions programs and services;
- If applicable, the amount of any amount carried forward by Prince Edward Island under section 4.4; and
- If applicable, the amount of any surplus funds that is to be repaid to Canada under section 4.5.
- For the Safe Long-term Care Funding, the annual financial statement will also set out, for the previous fiscal year:
- The amount of the federal funding flowing to each facility, and the type of facility (as set out in 4.7.2); and
- The estimated amount of funds to be recovered under cost-recovery agreements, where applicable, and the priority areas where those funds will be reinvested
5.1.3 As a condition of receiving the second payment installment of the Safe Long-term Care Funding, Prince Edward Island agrees to, by no later than December 1, 2021, amend Annex 2 to:
- Provide up-to-date information on performance measures, targets and intended outcomes for the three areas identified in section 2.3, and for any other areas in which Prince Edward Island has used Safe Long-term Care Funding to support infection prevention and control, and interim results for each initiative.
- Provide a breakdown of the facilities receiving funding under this Agreement, and specifically, identifying those privately-owned, for-profit facilities receiving funding pursuant to this Agreement and whether or not cost-recovery agreements are in place with them with respect to this funding;
- Indicate the amount paid to each recipient operating a privately-owned, for-profit facility and describe the incremental impact that will be achieved through these investments;
- Provide information on the estimated amount of funding to be recovered pursuant to the cost-recovery agreements; and,
- Indicate how Prince Edward Island will use recovered funding to increase infection prevention and control pursuant to the terms of this Agreement.
5.1.4 Prince Edward Island also agrees to amend Annex 2, by March 31, 2022, to report, in accordance with the performance measures set out in Annex 2, on the outcomes and results achieved using the Safe Long-term Care Funding.
5.2 Audit
5.2.1 Prince Edward Island will ensure that expenditure information presented in the annual financial statement is, in accordance with Prince Edward Island's standard accounting practices, complete and accurate.
5.3 Evaluation
5.3.1 Responsibility for evaluation of programs rests with Prince Edward Island in accordance with its own evaluation policies and practices.
6 Communications
6.1 Canada and Prince Edward Island agree on the importance of communicating with citizens about the objectives of this Agreement in an open, transparent, effective and proactive manner through appropriate public information activities.
6.2 Each Party will receive the appropriate credit and visibility when investments financed through funds granted under this Agreement are announced to the public.
6.3 In the spirt of transparency and open government, Canada will make this Agreement, including any amendments, publicly available on a Government of Canada website and Prince Edward Island shall make the results under this Agreement related to the Safe Long-term Care Funding, as set out in Annex 2, publicly available on its Government of Prince Edward Island website.
6.4 Canada, with prior notice to Prince Edward Island, may incorporate all or any part or parts of the data and information in 5.1.2 and 5.1.3, or any parts of evaluation and audit reports made public by Prince Edward Island into any report that Canada may prepare for its own purposes, including any reports to the Parliament of Canada or reports that may be made public.
6.5 Canada reserves the right to conduct public communications, announcements, events, outreach and promotional activities about the Common Statement, Safe Long-term Care Funding and bilateral agreements. Canada agrees to give Prince Edward Island 10 days advance notice and advance copies of public communications related to the Common Statement, Safe Long-term Care Funding, bilateral agreements, and results of the investments of this Agreement.
6.6 Prince Edward Island reserves the right to conduct public communications, announcements, events, outreach and promotional activities about the Common Statement, Safe Long-term Care Funding and bilateral agreements. Prince Edward Island agrees to give Canada 10 days advance notice and advance copies of public communications related to the Common Statement, Safe Long-term Care Funding, bilateral agreements, and results of the investments of this Agreement.
7 Dispute Resolution
7.1 Canada and Prince Edward Island are committed to working together and avoiding disputes through government-to-government information exchange, advance notice, early consultation, and discussion, clarification, and resolution of issues, as they arise.
7.2 If at any time either Canada or Prince Edward Island is of the opinion that the other Party has failed to comply with any of its obligations or undertakings under this Agreement or is in breach of any term or condition of the Agreement, Canada or Prince Edward Island, as the case may be, may notify the other party in writing of the failure or breach. Upon such notice, Canada and Prince Edward Island will endeavour to resolve the issue in dispute bilaterally through their designated officials, at the Assistant Deputy Minister level (hereinafter the "Designated Officials").
7.3 If a dispute cannot be resolved by Designated Officials, then the dispute will be referred to the Deputy Ministers of Canada and Prince Edward Island responsible for health, and if it cannot be resolved by them, then the respective Ministers of Canada and Prince Edward Island most responsible for Health shall endeavour to resolve the dispute.
8 Amendments to the Agreement
8.1 The main text of this Agreement (not including attached annexes) may be amended at any time by mutual consent of the Parties. To be valid, any amendments shall be in writing and, signed, in the case of Canada, by Canada's Minister of Health, and in the case of Prince Edward Island, by Prince Edward Island's Minister of Health and Wellness.
8.2 Annex 2 may be amended at any time by mutual consent of the Parties. To be valid, any amendments to Annex 2 shall be in writing and, signed, in the case of Canada, by their Designated Official, and in the case of Prince Edward Island, by their Designated Official.
9 Equality of Treatment
9.1 During the term of this Agreement, if another province or territory, except the province of Quebec, negotiates and enters into a Home and Community Care and Mental Health and Addictions Services Agreement with Canada, or negotiates and enters into an amendment to such an agreement and if, in the reasonable opinion of Prince Edward Island, any provision of that agreement or amended agreement is more favourable to that province or territory than the terms set forth in this Agreement, Canada agrees to amend this Agreement in order to afford similar treatment to Prince Edward Island, if requested by Prince Edward Island. This includes any provision of the bilateral agreement except for the Financial Provisions set out under section 4.0. This amendment shall be retroactive to the date on which the Home and Community Care and Mental Health and Addictions Services Agreement or the amendment to such an agreement with the other province or territory, as the case may be, comes into force.
10 Termination
10.1 Canada may terminate this Agreement at any time if the terms of this Agreement are not respected by Prince Edward Island by giving at least 12 months written notice of its intention to terminate. Prince Edward Island may terminate this Agreement at any time if the terms of this Agreement are not respected by Canada by giving at least 12 months written notice of its intention to terminate.
10.2 As of the effective date of termination of this Agreement under section 10.1, Canada shall have no obligation to make any further payments to Prince Edward Island after the date of effective termination.
11 Notice
11.1 Any notice, information, or document provided for under this Agreement will be effectively given if delivered or sent by letter or email, postage or other charges prepaid. Any notice that is delivered will have been received in delivery; and, except in periods of postal disruption, any notice mailed by post will be deemed to have been received eight calendar days after being mailed.
The address for notice or communication to Canada shall be:
Health Canada
70 Colombine Driveway
Brooke Claxton Building
Ottawa, Ontario
K1A 0K9
Email: marcel.saulnier@canada.ca
The address for notice or communication to Prince Edward Island shall be:
Department of Health and Wellness
P.O. Box 2000
Charlottetown, PE
Canada C1A 7N8
Email: smacneill@gov.pe.ca
12 General
12.1 This Agreement, including Annexes 1 and 2, comprise the entire agreement entered into by the Parties with respect to the subject matter hereof.
12.2 This Agreement is based on the Common Statement of Principles on Shared Health Priorities, Annex 1, finalized on August 21, 2017.
12.3 This Agreement shall be governed by and interpreted in accordance with the laws of Canada and Prince Edward Island.
12.4 No member of the House of Commons or of the Senate of Canada or of the Legislature of Prince Edward Island shall be admitted to any share or part of this Agreement, or to any benefit arising therefrom.
12.5 If for any reason a provision of this Agreement that is not a fundamental term is found by a court of competent jurisdiction to be or to have become invalid or unenforceable, in whole or in part, it will be deemed to be severable and will be deleted from this Agreement, but all the other provisions of this Agreement will continue to be valid and enforceable.
SIGNED on behalf of Canada by the Minister of Health at Charlottetown, Prince Edward Island on this 23rd day of February, 2018.
The Honourable Ginette Petitpas Taylor, Minister of Health
SIGNED on behalf of Prince Edward Island by the Premier of Prince Edward Island at Charlottetown, Prince Edward Island this 23rd day of February 2018.
The Honourable Wade MacLauchlan, Premier of Prince Edward Island
SIGNED on behalf of Prince Edward Island by the Minister of Health and Wellness at Charlottetown, Prince Edward Island on this 23rd day of February, 2018.
The Honourable Robert Mitchell, Minister of Health and Wellness
Annex 1 to the Agreement
Common Statement of Principles on Shared Health Priorities
Annex 2 to the Agreement
Prince Edward Island Home and Community Care and Mental Health and Addiction Services Action Plan
Overview
The PEI health care system is experiencing a surge in demand for both home care services and across the spectrum of services and programs that address mental health and addictions issues. In a climate of limited resources and competing demands, this has created the push for innovative models of service delivery that move away from institutionalized care and that seek to embed upstream programs that serve clients in their homes and communities. In response to these pressures and demands, the Government of Prince Edward Island (PEI) has made significant efforts to expand access to important services in both home and community care, and in mental health and addictions.
Home and Community Care
In the areas of home and community care, the Government of PEI has made progress in addressing challenges in service access and the availability of services and supports. Enhanced investment in home care and community care has increased the availability of resources and supports in recent years, but this growth has not kept pace with rising demand. Despite the excellent work of provincial home care staff (nurses and supporting staff) as well as the paramedics and allied health professionals who supplement those core services, demand for these services continues to grow.
Fortunately, PEI has showcased a very successful service delivery model that offers a template for expanding access to home and community care services in a way that is impactful, sustainable, and cost effective. Through PEI's Paramedics Providing Palliative Care at Home program, trained paramedics will provide palliative care patients with pain and symptom management to clients at home, after-hours, and free of charge. This program is open to all Islanders (adults and children) who are part of the Provincial Integrated Palliative Care Program, which has been nationally recognized by the Canadian Foundation for Healthcare Improvement (CFHI) with a 2017 CFHI Palliative and End of Life Care Innovation Award. It utilizes the expertise and capacity of our paramedic community to enhance access to essential publicly funded services, in consultation and coordination with core staff within the public service.
With the anticipated growth in demand for home care services that will impact health system decisions and priorities in the coming decades, this program offers a model for service enhancement that will have an immediate and tangible impact on available services. In conjunction with an enhanced and standardized intake process, and implementation of an information technology platform that provides all health care providers with appropriate access to client information to streamline service delivery, this integrated model of care will leverage the expertise among the Island's paramedic community and within core home care staff to enhance access to key services.
Priority Areas for Investment in Home and Community Care are:
- Mobile Integrated Health Initiative
- Rapid Bridging - Integrated Palliative Care Program
- Rapid Bridging - Hospital and Emergency Department Patients
- Paramedic Check-In Program
- Home Care IT Infrastructure Initiative
- Implementation of InterRAI Assessment tool
Mental Health and Addictions
Work has been underway since 2012 to develop a long-term vision for mental health and addictions in the Province. This culminated in the 2016 release of Moving Forward Together, a 10-year Mental Health and Addictions Strategy for Prince Edward Island that was jointly issued by the Ministers of the social policy departments (Health, Justice and Public Safety, Family and Human Services, and Education, Early Learning and Culture). This Strategy sets out an ambitious, interdepartmental framework to guide actions that will address gaps in the mental health system, and in the social supports that are intimately tied to that system. The five pillars of the strategy are:
- Invest Early: Focus on Children, Young People and Families
- Access to the Right Service, Treatment and Support
- Mental Health Promotion for People of All Ages
- Foster Recovery and Well-being for People of All Ages
- Innovative and Collaborative Workforce
This work also identified specific challenges and barriers to addressing the mental health needs of Islanders:
- Resources required for transformational change
- Workforce issues (recruitment and retention)
- System integration between government and community
- Lack of capacity to deal with wait lists
- Lack of mental health resources in schools
- Need for assessment and intervention capacity building in primary care, public health, and education
To address the barriers, and advance work under the five pillars, a Mental Health and Addictions Strategy Action Plan was subsequently developed that outlined 44 specific recommendations to significantly expand both the scope and impact of mental health and addictions services in the province. That Action Plan, and the recommendations within it, was the driving factor behind not only the identification of the specific programs that will be advanced through the allocation of targeted federal funds under this plan, but also led to a number of ongoing investments that are working to improve access to mental health and addictions services Island-wide including:
- Additional dedicated frontline positions were hired to support in-patient adolescent mental health clients on Unit 9 at the Queen Elizabeth Hospital.
- Expanding the Strength Program in 2015 to Summerside has virtually eliminated the need to refer youth out of province for treatment. On average, 75 clients are admitted to the program each year.
- Strongest Families is currently serving 369 Island families, reducing waitlists for other mental health services. On average, the service receives 40 new referrals per month. Families completing the program are very satisfied with the outcomes, of which there is a 94% success rate.
- The Behavioural Support Team, which helps children aged 4-12 with moderate to severe behavioural difficulties, currently provides service to 51 children and families.
- The Insight Program provides a stepped care approach for youth who are struggling with significant/persistent primary mood, anxiety and or psychotic disorders. Since it opened in October 2016, there have been 20 participants in the 16-week program.
- 21 mental health and addictions staff members have been trained in the Triple P Parenting approach to provide earlier intervention and parenting support for behavioral issues.
Mental health walk-in clinics are now available in several communities, including: Charlottetown, Summerside, Lennox Island, O'Leary and at Westisle High School (this clinic is for students only). The clinics offer immediate mental health support to help with anxiety, as well as life events causing stress and other mental health issues. Individuals are seen by a therapist and may receive up to one hour of counseling. Individuals may also be referred on to other programs/services for more support.
Despite this significant work that is underway, additional supports in mental health and addictions are still needed. In 2016-17:
- there were 1,274 children under 17 years of age referred to Community Mental Health services, of which 1,102 children were referred directly for clinical therapy services and 172 were direct referrals for psychiatry assessment;
- the most common reasons for hospital admission for children aged 17 and under included: depressive episode, stress reaction/adjustment disorder, and childhood/adolescent disorder; and,
- the most common reasons associated with longest lengths of hospital stay include: obsessive compulsive disorder, poisoning/toxic effect of drug, and childhood/adolescent disorder.
These and other indicators suggest a need to continue to strengthen both acute metal health services, as well as the capacity to provide mental health and addictions supports to children and youth outside of a hospital setting and in their community.
Priority areas for investment in mental health and addictions are:
- Student Well-being Program
- Mobile Mental Health Crisis Program
Federal Funding
In recognition of the growing demands that exist in the areas of mental health and addictions, and in home and community care, on January 31, 2017, "the federal government and the Government of PEI agreed to new targeted federal funding over 10 years for investments in home care and mental health care."Footnote1 This funding was intended to enhance access to essential services in the two targeted areas, and would be steered by the Common Statement of Principles on Shared Health Priorities that was agreed by all Federal-Provincial-Territorial governments on August 21, 2017. Specifically, the Common Statement on Shared Health Priorities outlined the governments' commitment to "work together to improve access to evidence-supported mental health and addiction services and supports for Canadians and their families" and to "work together to improve access to appropriate services and supports in home and community, including palliative and end-of-life care".Footnote2
These objectives would be guided by three key principles:
- Collaboration: FPT Health Ministers agree to work together to achieve the objectives set out in this Statement of Principles;
- Innovation: FPT Health Ministers agree to continue the development and evaluation of innovations which deliver better outcomes for Canadians, and to share successes and lessons learned with a view to further stimulating improvement across health systems; and,
- Accountability: FPT Health Ministers agree to measure progress on the collective and jurisdiction-specific goals under this Statement of Principles, and to report to Canadians.
This Action Plan outlines the initiatives and commitments of the Government of PEI that will utilize the targeted federal funding to advance these objectives, while adhering to the agreed principles. By articulating specific actions in the areas of both home and community care, and in mental health and addictions, this plan will improve access to key services within the health care continuum.
In an effort to advance these important objectives, the Government of Canada has committed to provide 10 years of targeted funds to the Government of PEI in the following estimated amounts (based on 2017 Statistics Canada population estimates, to be updated annually):
| $ millions | 17-18 | 18-19 | 19-20 | 20-21 | 21-22 | 5-yr Total | 22-23 | 23-24 | 24-25 | 25-26 | 26-27 | 10-yr Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Home Care | 0.82 | 2.48 | 2.69 | 2.69 | 3.73 | 12.41 | 2.48 | 2.48 | 2.48 | 2.48 | 2.48 | 24.81 |
| Mental Health | 0.41 | 1.04 | 1.86 | 2.48 | 2.48 | 8.27 | 2.48 | 2.48 | 2.48 | 2.48 | 2.48 | 20.67 |
| Total | 1.23 | 3.52 | 4.56 | 5.18 | 6.21 | 20.68 | 4.96 | 4.96 | 4.96 | 4.96 | 4.96 | 45.48 |
| Note: The values of all allocations noted above are estimates that will be revised each year based on Statistics Canada's population estimates. Equal per capita allocations will be determined based on PEI's share of the Canadian population (approx 0.4%). | ||||||||||||
As a condition of receiving this funding, the Government of PEI has committed to specific initiatives and reporting requirements that acknowledge the need for accountability of these funds.
Part 1 - Home and Community Care
Consistent with a broader regional trend in Atlantic Canada, the population in PEI is older than the Canadian average, with higher rates of most chronic diseases (and higher occurrence of co-morbidities of those diseases). These factors are already impacting health care costs, and these impacts will grow in the coming years. This demand will drive the need for innovative approaches that are not only effective, but which are also cost-effective.
According to the 2016 Census, the percentage of people aged 65 and older was 19.4% in PEI, compared to the national average of 16.9%. While ambitious immigration targets are seeking to redress this imbalance, the large cohort of seniors will put significant pressures on health care resources as they age. These pressures will be felt both within the system via acute and primary care systems, and in the community where demand already taxes the available supports and programs.
Compounding this issue are rates of chronic disease that are both regionally and provincially higher than the national average. Compared to the Canadian average, PEI has significantly higher rates of chronic disease at ages 50 years and older, following the trend of the other Atlantic Provinces. The Canadian Community Health Survey (CCHS) provides comprehensive, current information that shows significant prevalence of many chronic conditions.
| PEI | Canada | |
|---|---|---|
| Arthritis | 21.2% | 16.5% |
| COPD | 5.7% | 4% |
| Diabetes | 8.4% | 6.7% |
| High Blood Pressure | 22% | 17.7% |
As our population ages and chronic disease rates continue to increase, Islanders will need access to more health care services outside the traditional settings such as physicians' offices and hospitals. This will necessitate ongoing investment in innovative models of care that are cost-effective and which provide access to patient-centred services in the setting of their choice.
To date, PEI's investment in home care services has lagged behind other areas of need, such as investment in the acute care system or the institution-based long term care (LTC) system. While approximately 4,500 Islanders received home care services last year (2016), with staff supporting approximately 2,200 clients each month, public funding of home care as a share of provincial health spending is markedly lower in PEI when compared to other Canadian Jurisdictions (2.8% in PEI versus 4% nationally). This lower investment has led to pressures on other parts of the health care system, such as wait lists for LTC beds, which in turn leads to bed shortages in hospitals caused by an inability to discharge patients who could be medically discharged but who cannot move into an LTC bed or receive the necessary home care supports in a timely manner.
As a result, the PEI Government is putting in place new approaches to service delivery that will enhance access to vital health care and support services at home and in the community, and reduce reliance on more expensive hospital infrastructure. Shifting the paradigm of service delivery is needed to ensure sustainability of programs and services while still meeting Islander's expectations. This will be done by pursuing a vision of home care that offers a broad spectrum of home based services which are accessible to all Islanders, which supports their choice to remain at home and age-in-place as long as possible and to live with dignity and independence, and which allows them to return home more quickly from hospital, or delay or even avoid admission to a hospital or long-term care home. The investments made through this Plan will build on the Island's current range of health care and support services to individuals who have acute, chronic, palliative or rehabilitative health care needs. These services currently include:
- Nursing care - including health monitoring, IV therapy, injections, wound care and patient teaching.
- Home support - Assistance with daily activities such as bathing and dressing.
- Palliative care - comfort and support to live fully until the end of life.
- Social work - individual and family counseling for illness, loss or end-of-life issues.
- Dietitian services - nutrition assessment and education.
- Physiotherapy - to maximize independence, function and mobility.
- Occupational therapy - support for daily living, special devices/equipment or modification to home/ workplace.
- Adult protection - for vulnerable adults who need protection from neglect or abuse.
- Long-term care - assessment for nursing home admission.
- Adult day programs - enriching social activities for seniors.
To help achieve this vision, the PEI Government is taking steps to improve access to appropriate services and supports in the community. These actions will not replace the existing publically funded home care program, but will build off of the strengths and successes that program, including the Integrated Home Palliative Care Program.
Priority areas for investment
To assist with improving access to appropriate home and community care, the federal government will provide provincial and territorial governments with $6.0 billion over the next 10 years. For PEI, the provincial share of these funds amounts to approximately $24.8M over the next ten years (2017-2027). In alignment with the principles and objectives noted in the Common Statement of Principles, the Government of PEI will pursue the following programs to enhance access to services in Home and Community Care:
- Mobile Integrated Health Program
- Home Care IT Infrastructure Initiative
- Implementation Plan for InterRAI Assessment tool
| 2017-18Footnote * | 2018-19 | 2019-20 | 2020-21Footnote ** | 2021-22Footnote ** | Total | |
|---|---|---|---|---|---|---|
| Federal Funding ReceivedFootnote ** | $820,000 | $2,481,000 | $2,713,000 | $2,730,000 | $3,687,000 | $12,611,000 |
| Mobile Integrated Health (MIH): | $620,000 | $1,083,000 | $1,341,000 | $1,157,000 | $1,295,000 | $5,496,000 |
| Enhanced Palliative Care (MIH) Co-ordination | - | - | $0 | $66,000 | $170,000 | $236,000 |
| Home Care IT Infrastructure Initiative | $200,000 | $403,000 | $0 | $0 | $0 | $603,000 |
| Implementation of InterRAI | $0 | $0 | $818,000 | $1,165,000 | $1,276,000 | $3,259,000 |
| Total Expenditure | $820,000 | $1,510,000 | $2,159,000 | $4,191,000 | $3,730,000 | $9,594,000 |
| Carry-over to be Spent in the Next YearFootnote *** | $995,000 | $1,549,000 | $1,891,000 | $3,017,000 | -- | |
|
||||||
Please Note: Funding allocations noted in the table above are estimated based on current information. As such, decisions on funding allocations in future years noted in the table may be subject to change. This flexibility reflects an acknowledgement that current planning activities do not allow articulation of a totally fixed five-year spending plan. Despite this, the Government of PEI is fully committed to advancing the principles and objectives outlined in the Common Statement of Principles on Shared Health Priorities. In addition, the current work on a Seniors Health and Wellness Strategy and a report on the continuum of care in PEI will inform future decisions about targeted activities to advance access to home and community care.
Detailed Program Descriptions - Home & Community Care
1. Mobile Integrated Health
- The Mobile Integrated Health (MIH) initiative will be delivered through three inter-related projects that utilize and build on the capacity and expertise within PEI's paramedic community and will be provided free of charge to eligible clients. These three integrated initiatives will be implemented in tandem to leverage potential administrative efficiencies and economies of scale. The three programs identified are:
- Rapid Bridging - Integrated Palliative Care Program;
- Rapid Bridging - Hospital and Emergency Department Patients; and,
- Paramedic Check-In Program.
Within this cluster of services, administrative capacity and other supports will be shared to leverage the maximum investment in new front line service delivery. While some of the federal funding will be used to establish the infrastructure and mechanisms necessary to administer the programs (such as a Clinical Navigation Desk that will work with home care staff to coordinate paramedic care) as well as administration of the program's evaluation framework, the bulk of the funding will be used to support the addition of new service delivery staff resources within the paramedic fleet. This investment will bring these additional front line staff into the home care program, and will represent a substantial increase in available human resource capacity that will be integrated into home care management plans, thereby building on the existing system of supports that are currently in place.
Paramedic services are available and accessible to all areas of the province. The current fleet includes 14 ambulances, 2 Rapid Response Units (non-transport SUVs), and 2 inter-facility ambulance transfer units. As a result of these investments, extra capacity will be added to the Rapid Response Units, including the addition of one additional vehicle and the extension of coverage hours to 7 days per week. The additional fleet resource is equivalent to approximately 5-6 new full-time Advanced Care Paramedic (ACP) positions. In addition, new clinical capacity (Registered Nurse positions) will also be added to the Emergency Communications Center to support the MIH programs.
While the number of new clients served will vary by MIH initiative, it is expected the "Paramedic Check-In Program" will be the most resource demanding program during these first two years. For reference, in the only existing MIH Initiative (Paramedics Providing Palliative Care at Home Program), over 450 palliative clients have accessed the program to date.
This period of time that a patient can participate in an MIH initiative will vary depending on the specific care needs of the patient (and their family) enrolled in an MIH Program. As each specific MIH Program is developed, clinical practice guidelines and clinical pathways will continue to be co-developed by emergency services and the referring service area or agency (i.e. home care, palliative care, emergency departments, long term care, etc.). When a patient is referred to any one (or more) of the MIH Programs, each referral will be individually screened and reviewed for eligibility and in-take (against the developed clinical pathway). If accepted, a specialized care plan will be developed using the approved clinical practice guideline as a template that can be tailored to meet the needs of each patient or family with respect to type and frequency of visits. Each clinical practice guideline will be regularly reviewed/updated between the MIH program (i.e., program coordinator, registered nurse, medical oversight), the referring program/service area (i.e., hospital, emergency department, etc.) and home care/palliative care (i.e., palliative care coordinator, home care in-take coordinator/liaison etc.).
In the Island's two largest First Nations communities, paramedics will work with nurses in the community health centres to ensure that home care services are culturally sensitive. Community leaders were engaged during the planning of on-reserve services, and paramedics will meet with community elders to help ensure successful implementation of the services. These services will also be rolled out with specific strategies for the Island's francophone residents. Program planners will work with the Acadian and Francophone Community Advisory Committee to ensure that the MIH program is fully integrated with ongoing efforts to meet the home care needs of these communities. These efforts include meeting with a range of key stakeholders and informants to review appropriate service delivery models that could be adapted to meet the needs of the Island's Acadian and francophone residents.
This investment aligns with the Common Statement of Principles on Shared Health Priorities by:
- Spreading and scaling evidence-based models of home and community care that are more integrated and connected with primary health care;
- Enhancing access to palliative and end of life care at home or in hospices;
- Increasing support to caregivers; and,
- Enhancing home care infrastructure, such as digital connectivity, remote monitoring technology and facilities for community-based service delivery (in this case through the addition mobile non-transport units).
A brief description of the 3 MIH programs are as follows.
MIH 1 - Rapid Bridging - Integrated Palliative Care Program
- Supports discharge from acute care of patients registered with the Provincial Integrated Palliative Care Program by arranging paramedic follow up at home until home care and palliative care services are available to assume care for these patients.
Project Description and Goals:
At the present time, many palliative patients must remain in hospital to receive necessary medications and treatments (i.e., IV medication administration) until a receiving home care team is able to assess them and implement the necessary services in their home. Due to service demands and other system bottlenecks, there are often delays in a patient being able to move directly into their home to receive palliative care. In addition, some treatments are not currently provided in the homes (i.e., episodic IV therapy or medication administrations). The latter is also true for nursing home and community care environments where many palliative patients may require episodic IV therapies. Taken together, these factors can often lead to significant delays for palliative patients seeking to receive treatment in their home, which in turn impacts bed utilization and other resource allocation considerations within the acute care system.
Given this dynamic, there is an opportunity for interventions, follow up, assessments and support of these patients by having advanced care paramedics assess and, when necessary, administer the necessary medication in the patient's home. This would allow patients to be discharged from acute care and receive necessary follow up and treatment in a timely manner by health care providers working well within their recognized scope of practice. Patients would be able to return to their homes as soon as possible while receiving safe follow-up care by paramedics until home care nursing is able to assume care to these patients.
Working in collaboration with the patient's attending physician, nurse practitioner, or palliative care physician, the advance care paramedics will perform treatments including medication review and administration to those palliative patients under the medical oversight of a palliative or attending physician. The palliative patient will be discharged from the hospital and a paramedic will be contacted to provide treatments and to help with the "rapid bridging" back to home.
Program Objectives:
- Support for post-acute palliative clients;
- Arranging facilitated transports to home from hospital; and,
- Focus on treating and supporting patients in community.
Target Populations:
Palliative care patients registered in the Provincial Integrated Palliative Care Program who are hospitalized but ready to return to their home with the appropriate and necessary supports.
Overall Outcomes
- Decreased average length of stay in hospital for patients registered in the Provincial Integrated Palliative Care Program;
- Decrease re-admission rates for patients registered in the Provincial Integrated Palliative Care Program;
- Develop a template for the "rapid" bridging to home between acute care and home care services utilizing emergency health services (EHS) to inform potential opportunity for future expansion in other areas (i.e., long term care, mental health & addictions etc.);
- Develop a template for the "rapid" bridging to home between acute care and home care services utilizing EHS, to support a potential opportunity for future expansion in other areas (i.e., long term care, mental health & addictions etc.); and,
- Improved patient and family satisfaction.
MIH 2 - Rapid Bridging - Hospital and Emergency Department Patients
- Eligible patients may be discharged from hospital with an individualized care plan, developed in collaboration with care team. Paramedic(s) would provide treatments and assist with rapid bridging back to home in conjunction with acute care and home care services.
Project Description and Goals:
Many patients must remain in hospital to receive necessary medications or treatments that could be managed more effectively in the home. This project will support patients at home until a receiving home care team is able to assess and support them. The patient will be discharged from hospital with an individualized care plan, developed in collaboration with care team. Paramedics will provide treatments and other corollary supports to assist with rapid bridging back to home in conjunction with home care staff.
Similar to the first Rapid Bridging program, this program will provide interventions, follow-up assessments and supports, including administration of medications, for individuals who would otherwise remain in hospital. Suggested types of care to be provided by paramedics could include the following:
- Patient/Family Education;
- New-start medication concerns (i.e., insulin / warfarin supportive training;
- Medication reconciliation (storage, sorting, management, timing, education etc).
- Home safety (e.g. smoke detectors) and risk of fall concerns;
- Vital monitoring and reporting;
- Venipuncture/Point of care testing;
- Medication administration;
- Urinary catheter care;
- Feeding tube care (G-Tube, J-Tube);
- Ostomy care and management;
- Wound care management (site assessment, dressing changes etc); and,
- Identification of barriers and direct referral / navigation to community resources for follow-up.
By facilitating this expanded range of services provided in the home, this program will allow patients to return to home as soon as possible while receiving safe follow-up by paramedics until home care nursing is able to assume care to these patients. In doing so, this program will facilitate the discharge of patients to a more appropriate setting while receiving necessary services to support care in the community.
Program Objectives:
- Support for post-acute clients;
- Arranging facilitated transports to home from hospital; and,
- Focus on treating and supporting patients in community.
Overall Outcomes:
- Decreased average length of stay (LOS) in hospital;
- Decrease re-admission rates;
- Develop a template for the "rapid" bridging to home between acute care and home care services utilizing EHS, to support a potential opportunity for future expansion in other areas (i.e., long term care, mental health & addictions etc.); and,
- Improved patient and family satisfaction.
MIH 3 - Paramedic Check-In Program
- Seniors living at home who are at increased risk for poor health outcomes, falls, disability or hospitalization, may be referred to local paramedics for scheduled home visits during periods of downtime.
The Paramedic Check-In Program will improve the response and support available to frequent users of EHS by referring them for community-based paramedic support, when appropriate. Through the identification of frequent users of the Island's emergency medical services (facilitated by the Medacom Atlantic communications center, and through identification by individual paramedics), high priority clients would be enrolled in the program. These clients would generally be seniors that are living at home, and who are at increased risk for poor health outcomes, falls, disability, hospitalization and death. These target clients would be referred to local paramedics for scheduled home visits during periods of downtime. In turn, theses paramedics would provide home-based services such as assessments for those with chronic conditions or with mobility issues. Provision of these services and supports in the home aligns directly with an established provincial objective of increasing support for frail seniors.
This program would leverage recent investments made in the EHS Dispatch technology (Computer Assisted Dispatch, Emergency Medical Dispatch) to further streamline service delivery and integration. Given that the intent is to leverage idle or "down" time of existing paramedic resources to support this initiative, federal funding requirements for this specific element of MIH would be modest, and would relate to the administrative and coordination capacity within the Medacom Atlantic communications center.
Target Populations
As an initial, priority population, the program would target frequent callers to 911 that are 65 and over. Residents 65 years of age and over make up 58% of the pre-hospital emergency call volume. Approximately 80% of all calls to 911 by residents over the age of 65+ are for non-emergent purposes. Investments in MIH infrastructure/resources (i.e., addition of ambulance fleet, registered nurses, and clinical expertise to the emergency communication center) will significantly improve capacity for navigation and direct referral to more appropriate care areas vs. emergency department visits.
The Medacom Atlantic communications centre currently monitors calls/clients to identify these frequent users of EMS, who are ideal candidates for the early stage of the program. In addition, paramedics may identify high-needs clients that would benefit from this program. While precise numbers of potential clients are not known at this time, comprehensive analytic work is underway to identify the most frequent callers (by address/name/medical record number) in real time. The initial program participants for the Paramedic Check-In Program will be identified using this process.
Overall Outcomes:
- Decrease in 911 calls within target populations;
- Decrease number of non-emergent transports from home to the emergency department; and,
- Upstream health care support for seniors living at home in the community.
Evaluation of the 3 MIH Initiatives
An Evaluation Working Group has been constituted to plan and oversee the evaluation component of the three MIH initiatives and will develop a comprehensive and systematic evaluation framework for the three MIH initiatives, and to establish baseline data to support this evaluation. An initial set of indicators could include, but would not be limited to:
- Hospital length of stay (LOS);
- Hospital re-admission rates;
- Emergency department visits by seniors for non-emergent concerns;
- Admission age and LOS in long-term care (as seniors will have additional supports in the community);
- Patient and family satisfaction with care;
- Frequency of 911 (among Check-in Program target populations); and,
- Number of non-emergent transports from home to emergency department (among Check-in Program target populations).
Aside from indicator data, additional evaluation work is being planned that will include components of the following:
- Formative evaluation: Provides information to makes changes in the program.
- Process evaluation: Understanding of how the program worked and why.
- Summative evaluation: Did the program achieve what it set to?
- Impact/outcome evaluation: Measuring the overall impact/outcomes of the program in relation to the program goals.
It should also be noted that MIH planners have engaged a variety of different stakeholders while determining the activities of the committee, and are seeking to appoint a patient advocate to the committee to ensure that a client-centered approach is incorporated into the finalized evaluation plan.
Mobile Integrated Health - Palliative Care Initiative
Utilizing the re-profiled funding from the Home Care IT Infrastructure Initiative (see explanation below), the Province will establish key supports to improve care under the palliative stream of the Mobile Integrated Health program. These new investments would directly support one of the primary objectives of the Common Statement of Principles on Shared Health Priorities "to improve access to appropriate services and supports in home and community, including palliative and end-of-life care".
From 2010/11 to 2017/18, the Provincial Palliative Care Program has experienced a 90% increase in client demand. This increase in demand has stretched available human resources and impacted the ability of program staff to develop individualized care plans for clients. The available funding would be used to support the establishment of two crucial functions which would enhance planning and integration between the Home Care program and the palliative care delivered through the highly successful MIH program. These additional functions would consist of Care Coordinator positions and a Provincial Clinical Educator Position.
Care Coordinators
While more and more individuals in Prince Edward Island are choosing to die at home, the care coordination hours available through existing Home Care staff have not been able to keep pace due to multiple priorities that compete for the limited pool of staffing resources. The addition of dedicated Palliative Care Coordinators within the Home Care Program would ensure that resources are available to support the creation of an individualized, evidenced-based plan of care for each client. As part of the Home Care team, these Palliative Care Coordinators would work directly in the home with clients and families and also work with local palliative care teams and MIH representatives to ensure optimal coordination of services.
With the steady increase in client numbers and complexities, provision of the required care and coordination is not possible with present resources. This has resulted in unnecessary presentations to the ER and unnecessary admissions to acute care. More importantly, clients have been removed from their preferred location of care, during their acknowledged end of life. Additional care coordination supports within the program would address these issues and allow individuals to spend their final days in the location of their choosing.
Provincial Clinical Educator
Aside from care coordination, a consistent focus on education is also required within the program given the degree of program growth and the increased requirement to meet hospice, palliative and end of life quality standards at all sites where palliative care is provided. At present, there is no clinical educator to support Palliative Care learning needs within this provincial program. Education is currently provided by existing program staff occupying front line positions, and this results in a direct reduction in the hours of care they are able to provide. The establishment of a Provincial Clinical Educator position would eliminate this diversion of front line resources, and would help ensure a planned approach to clinical education in light of continued program growth. This position would also enhance broader public awareness of palliative care and would improve overall understanding and decision-making around end of life through public education.
2. Home Care IT Infrastructure Initiative (funding re-profiled)
In the initial 5 year Action Plan, PEI proposed the implement a Home Care EMR to support the activities of the Home Care unit. A pilot was conducted to assess and test implementation of an EMR solely within the Home Care program area.
After completion of the pilot project, the Department of Health chose to pursue a provincial EMR solution for the entire health system (with assistance from Canada Health Infoway). Because this initiative goes beyond the scope of the targeted funding under this agreement the available funding for this item has been re-profiled to support the Mobile Integrated Health - Palliative Care Initiative described above.
Evaluation and Performance Measurement
During the initial project period, an Evaluation and Assessment Committee has been constituted to plan, oversee, and report on the evaluation of the EMR. Preliminary membership includes involved clinicians and program managers, representatives from the Department of Health and Wellness, Health PEI, the provincial government's IT Shared Services branch, the proponent, and others as needed.
The stated objectives of this Committee will be to ensure evaluation of the EMR with respect to:
- Security - protection of privacy and client information
- Compatibility - interoperability with other elements of PEI's e-health infrastructure
- Utility - demonstrable value to both care providers and health system administrators
This important new investment will allow for a degree of integration and coordination within home and community care that was previously not possible under a hybrid information system that mixed elements of e-health with traditional paper-based systems. By enhancing the level of digital connectivity between all home and community care service providers, both clients and care providers will benefit greatly.
3. Implementation of the Home Care InterRAI Assessment tool
- To standardize client assessment and ensure consistency and evidence-informed decision making, a detailed implementation plan for adoption of the InterRAI Home Care Assessment Tool will be developed and then executed within the province's home care and long term care system.
The Resident Assessment Instrument (RAI) is a suite of over twenty assessment tools which are utilized across the continuum of the health care system. Most jurisdictions (such as Alberta, British Columbia, Manitoba, Newfoundland and Labrador, Nova Scotia, Ontario, Saskatchewan, and Yukon) currently use at least some of the InterRAI tools to assess individuals' need for home support services. In the Northwest Territories, Nunavut and New Brunswick, a continuing care assessment package is used. Québec uses a multi-client assessment tool, and PEI applies the Seniors Assessment Screening Tool, as well as other resources.
In PEI's Caring for Our Seniors Report (2016), it was recommended that the province consider replacing the Seniors Assessment Screening Tool (SAST) with InterRAI tools. Despite the anticipated implementation challenges (including new technology and the need for significant staff training and education), the InterRAI instruments are standardized, reliable, and validated tools which offer several benefits, including helping clinicians identify important health issues among patients, developing appropriate care plans, and monitoring patient progress. InterRAI instruments also provide quality indicators to assess care quality, and case-mix classification algorithms to facilitate appropriate funding of health services.
Given these benefits to clients, clinicians and administrators, this is an opportune time to implement the Home Care InterRAI assessment tool to support improved services for Island seniors. Further to this, a business plan is being developed (with assistance from the Canadian Institute for Health information (CIHI)) that will provide a roadmap for adoption of the full InterRAI suite, including identification of costs, barriers, benefits, potential synergies, etc. Once this business plan is developed, the Department of Health and Wellness, in coordination with Health PEI, will use it to plan and guide the full implementation of InterRAI in the PEI Home Care system.
This initiative will dovetail with the ongoing regional push to harmonize data standards, information management processes, and program parameters within Atlantic health care programs and services. As noted previously, elements of InterRAI are already present in some of the region's health care, home care, and/or long term care systems. Thus, PEI's adoption of this tool within the home care and long term care system will represent an important step towards a regionally harmonized approach to client assessment. This approach would not only aid in ensuring the application of common criteria across multiple programs in multiple jurisdictions, but would also open up the future potential to leverage truly regional data sets to facilitate better population health analysis.
This investment aligns with the Common Statement of Principles on Shared Health Priorities by:
- Enhancing home care infrastructure, such as digital connectivity, remote monitoring technology and facilities for community-based service delivery.
Aside from the inter-jurisdictional potential of InterRAI adoption, there are also intra-jurisdictional benefits that may accrue, insofar as the Department of Health and Wellness' planned adoption of the InterRAI tool may eventually fit into a broader framework of standardized data and assessment processes within the PEI Government. A broader corporate initiative is being explored that could lead to the implementation of a cross-Departmental client assessment platform that can be utilized across different domains. This horizontal initiative would enable greater integration of service delivery and more seamless care of clients within PEI Government departments. Thus the potential (albeit limited) implementation of InterRAI Assessment tools in the home care and long term care system could serve a s a precursor to its adoption in other social policy departments with overlapping clients/interests. Insofar as InterRAI is a candidate for consideration within this broader process, the early adoption of its proven assessment tools related to home care and long term care would establish the health care system as a demonstration platform for the value of this tool.
Target Populations: Current and future clients of the Island's home care system will benefit from the adoption of a standardized assessment tool to better inform decision-making. Given the administrative nature of this initiative, Island clinicians, service providers, and administrative staff could also be considered a secondary "target population" since the implementation of InterRAI will leverage efficiencies in planning and programming activities.
Given the costs associated with transitioning to InterRAI, federal funding will be used to partially offset the costs associated with securing the necessary software licenses, to purchase any additional hardware that is required for implementation, and to support staff during the transition to the new assessment regime through appropriate training and education. It is anticipated that the bulk of these costs will occur in the first 2 years of implementation, with "maintenance" costs (ongoing software licensing and ongoing staff training) occurring annually thereafter.
Overall Outcomes
Implementing InterRAI in the Province will introduce an evidence-based assessment process for seniors and will facilitate the development of individualized care plans as well as ensuring that individuals are more appropriately supported in the community. This assessment tool will also inform the development of evidence-based policy and practices with a lens towards continuous quality improvement for the continuum of care. This will lead to greater consistency between client assessments and decisions about appropriate care pathways, and greater opportunity for harmonization both between departments in PEI with overlapping clients/interests and within different health care systems in the Atlantic region. In addition, the more robust assessment framework will provide significantly better data over the medium- to long-term to better inform program planning and design.
Performance Measurement
Given the nature of this initiative, performance measurement and evaluation of the InterRAI tool would be a longer term undertaking, assessing the tool in practice. This would be initiated during the later years of this Action Plan. Expected outcomes would include the ability to enable better-informed client decisions and planning processes and better quality of care for patients, by having more appropriate care plans and consistency for all clients.
Part 2 - Mental Health & Addictions
PEI is currently experiencing significant demands across the spectrum of mental health and addictions programs and services. Despite rising investments, which saw an increase of approximately $3.5 million in the last year, significant pressures remain in all parts of the system - from early interventions and preventative mental health care to acute specialized psychiatric care.
This lack of resources in this program area is being felt in other parts of the health care system. In the absence of additional services, PEI continues to experience higher than necessary emergency department use and police response to mental health issues. The Queen Elizabeth Hospital emergency department had 296 mental health related visits in the first six months of 2017. The RCMP on PEI responded to over 200 mental health related calls in the same time period. Clearly, these interventions are not in the best interest of clients, and indicate a need for more targeted services and programs.
Similarly, with respect to specific youth impacts, there are a host of indicators that point to the extent of the problem in PEI. As of 2014-15, the following statistics underscore the need for investment:
- Wait time for psycho-educational assessment for youth is approximately 3.25 years
- 225 children in care of Province and over 3000 referrals to child protection
- Average wait time to see psychiatrist for youth (<18 years): 50 days (75 days for adults)
- Average wait time to see mental health provider for youth (<18 years): 25 days for individual triaged as urgent (16 days for adults)
- Per cent of youth clients seen by CMH within current access standards: 23% (57% for adults)
- PEI students (Grades 7-12) have the highest rate of binge drinking in Canada at 32.2%
- PEI students have highest rate of cannabis use in Canada at 24.8%
Following the release of the Mental Health and Addictions Strategy, and the subsequent development of the action plan to guide progress, a significant number of initiatives have already been implemented or are currently being rolled out, that will advance the central themes and objectives of the Strategy. Some highlights of work that has been completed to date include the establishment of:
- Behavioural Support Team
- Strongest Families Program
- INSIGHT Program
- Women's Wellness Centre
- Triple P Parenting Program
- Support and partnership with the Reach Foundation
- Safety and security review for inpatient mental health
Despite the progress of these initiatives however, areas of need still exist, and more needs to be done to further enhance access to crucial mental health and addictions services. Strengthening the direct access to mental health services among children and youth is a key priority that requires additional investment.
This Action Plan identifies two key initiatives that advance ongoing work to address the challenges associated with mental health and addictions in the Province: the Student Well-being Program and the Mobile Mental Health Crisis Program. These two initiatives will directly advance the themes and objectives set out in the Mental Health and Addictions Strategy and will take an integrated approach to providing mental health and addictions services to Islanders. Specifically, the Student Well-being Program will impact the Strategy pillars focused on early investment in children and youth and fostering collaboration among service providers. With a more acute focus, the Mobile Mental Health Crisis Program will provide an innovative new pathway for mental health and addictions services in the province and will emphasize providing the right service at the right time. These key initiatives, taken from the provincial mental health and addictions action plan, represent important new investments in mental health and addictions care in the province.
Priority areas for investment
To assist with improving access to appropriate mental health and addictions services, the federal government will provide provincial and territorial governments with $5.0 billion over the next 10 years. For PEI, the provincial share of these funds amounts to approximately $20.7M over the next ten years (2017-2027). In alignment with the principles and objectives noted in the Common Statement of Principles, and consistent with the priorities identified in the Mental Health and Addictions Strategy, the Government of PEI will invest in the following programs:
- Student Well-being Program
- Mobile Mental Health Crisis Program (MMHCP)
This investment is aligned with the Common Statement of Principles on Shared Health Priorities by:
- Spreading evidence-based models of community mental health care and culturally-appropriate interventions that are integrated with primary health services; and,
- Expanding availability of integrated community-based mental health and addiction services for people with complex health needs.
Specifically, the Student Well-being Program will provide a meaningful expansion of access to community-based (delivered in schools) mental health and addiction services for children and youth, in recognition of the effectiveness of early interventions to treat mild to moderate mental health disorders. Similarly, the Mobile Mental Health Crisis Program represents a significant addition to the suite of integrated mental health and addiction services delivered in the community, and targeting people with complex health needs.
| Funding Breakdown by Initiative | 2017-18Table note* | 2018-19 | 2019-20 | 2020-21 | 2021-22 | Total |
|---|---|---|---|---|---|---|
| Federal Funding Received | $410,000 | $1,040,000 | $1,860,000 | $2,480,000 | $2,480,000 | $8,270,000 |
| Student Well-being Program | $410,000 | $1,033,000 | $1,253,000 | $2,105,000 | $1,933,000 | $6,734,000 |
| Mobile Mental Health Crisis Program | ---- | ---- | $626,000 | $415,000 | $645,000 | $1,686,000 |
| Total Expenditure | $410,000 | $1,033,000 | $1,879,000 | $2,520,000 | $2,578,000 | $8,420,000 |
|
||||||
Detailed Program Descriptions - Mental Health and Addictions
1. Student Well-being Program
- Multi-disciplinary teams will be established and embedded within families of schools across the island to advise, consult with, and provide direct service to children and youth who are struggling with mental, social and physical health issues. Registered nurses with mental health training will provide mental health counseling to students with non-acute mental health needs and serve as navigators within the community mental health system for those students with more acute needs. This integrated approach to student well-being will help address identified gaps in school-based service delivery that may lead to poor health outcomes, learning difficulties, barriers to participation, lack of coping skills, and eventually mental health and addictions concerns.
The Student Well-being Program provides a collaborative approach to working with children and families to provide education, support and guidance for the overall well-being, including mental health and disease prevention. The Program's priority is to promote knowledge, resilience and coping skills so that students and families can make informed decisions affecting mental health and addictions, psycho-social and physical health.
Federal funding will be to support the staffing of registered nurses, with training in mental health, who will focus on upstream efforts to build resiliency within the school population, to promote positive mental health, and to avoid and/or mitigate mental health issues as they emerge. These mental health trained registered nurses will work with other mental health staff resources to provide direct mental health counseling to students with non-acute mental health needs. In addition, these nurses will provide a navigation function within the mental health system for those students with more acute needs by coordinating access to community-based mental health services for students and their families. They will work within an integrated team of allied health professionals, with staff that includes social workers and occupational therapists funded by the Province. Together, these teams will collaborate on care for their child and youth clients.
While new staffing resources will be limited during the early phase of this initiative (4 FTE school health nurses in year 1), the planned complement of 20.5 FTE federally funded school health nurses will be in place by the end of year 3, and will work within the broader school wellness teams that will include mental health therapists, school outreach workers, and counselling consultants, who will all work together to support students and families. This holistic approach to student well-being will seek to prevent mental health issues from materializing in some cases, and where they are present, to prevent them from escalating.
To meet the needs of the Island's francophone student population, bilingual positions will be established to support the French Language Schools in both the eastern and western parts of the province. In addition, plans are in place to fully integrate the Island's First Nations schools and students into the school wellness program. School nurses will work with Indigenous nurses in the Island's First Nations health centres to ensure that services are provided in a culturally sensitive and appropriate way.
This investment is aligned with the Common Statement of Principles on Shared Health Priorities by:
- Expanding access to community-based mental health and addiction services for children and youth (age 10-25), recognizing the effectiveness of early interventions to treat mild to moderate mental health disorders.
Program Principles
Student well-being teams will focus on wellness and timely access to services for children, youth and their families, based on the following principles:
Child-centered: Every aspect of the program has the child, youth and family at the center. Teams strive to build on the strengths of the child and to make accessing and receiving services as easy as possible. Services are tailored to meet the needs of children and youth, ensuring they receive the right service at the right time where they are.
Every door is the right door: Children and youth have additional opportunities to seek support. They can approach a core team member directly during drop-in hours, or speak to a trusted school staff member who will help them access the support they need.
Early Intervention: Every effort will be made to meet the needs of children, youth and families as early as possible and in the least-intrusive manner. Having services available in schools makes accessing services easier and more timely, allows issues to be addressed earlier, and prevents these issues from escalating and impacting their ability to succeed in school and throughout life.
Collaboration: Team members will work together to meet the individual needs of children, youth and their families, by accessing all necessary programs and services as early as possible -while building a culture of wellness in the school community.
Target Populations
This initiative will target school-aged children and youth, a currently under-serviced group where demands are high and where upstream investment can be an effective way of preventing the development more acute conditions. When the initiative is rolled out across the Island's 10 families of schools, this will provide access to non-acute mental health and addictions services to over 20,000 Island students, and will also provide them with a streamlined point of access into the formal mental health and addictions system where warranted. For those families of schools with significant First Nations representation within the student populations, cultural safety and awareness training would be a key component for the involved staff.
Program Goals
The Student Well-being Program has identified clear and defined objectives:
- Increase collaboration for student wellness by:
- Increasing information sharing, networking and communication between government
- Identifying and addressing gaps in services among professionals and programs
- Building capacity of existing services within schools
- Improve access to government and community services by:
- Reducing or eliminating timeline gaps and duplication of services among professionals and programs
- Providing services via a team approach across a family of schools
- Improving student engagement and school success
- Improving community engagement
- Establish a flexible, child youth and family centered program that strengthens capacity in youth and families by:
- Developing an array of programming and services offered at school sites
- Identifying and responding to children, youth and families in need of additional supports and services in a timely manner
Performance Measurement
Evaluation work for the Student Well-being Program is being developed to measure process and impact of the program. The purpose of the evaluation framework is to inform future roll-out of the program and to assess short and long term impact. Phase 1 of the project involves implementation of the model within two families of schools on the Island, with eventual implementation within the remaining eight families of Island schools. In the end, this will provide direct access to services for the more than 20,000 Island students. With this implementation plan in mind, the emerging evaluation plan is being designed to monitor immediate results and help inform subsequent roll-outs. While measures of student interactions and key outcomes from those interactions would be a primary indicator, additional monitoring will be undertaken to assess coordinated interactions with the formal mental health and addictions system. These detailed assessments will primarily take two forms.
First, surveys and focus groups for students participating in the program (and their family members) will be conducted regarding:
- Self-perceived changes for the student in various aspects of social/emotional well-being, physical well-being and mental well-being;
- Level of accessibility to program;
- Level of timeliness to program;
- Level of communication and active participation through pathways for services; and,
- Level of ease of transition through pathways for services (e.g., less re-telling of stories; streamlined referral process).
In addition, analysis of the provincial education, health, social services and justice system data sets will be used to assess the impact of intervention on students with respect to the various aspects of social/emotional well-being, physical well-being and mental well-being. This will include documenting changes in:
- Children/youth at emergency for services that could be dealt with through Student Well-being Program;
- Acute care readmissions;
- Reporting of child neglect/abuse;
- Children/youth placed into care under child protection;
- Children/youth in formal justice system; and,
- Youth referred to community mental health.
The results of these monitoring efforts will be used to inform future planning of programs and services targeting children and youth.
2. Mobile Mental Health Crisis Program
This initiative would establish a 24-7 provincial mobile mental health crisis program composed of highly trained mental health professionals (in most cases, registered nurses and social workers) supported by psychiatry. While planning for this program is still evolving, the broad vision and parameters for the program are outlined below.
Mobile crisis teams are a leading approach to providing mental health services to people in crisis in the community. In a crisis situation, individuals are best served by responsive access to mental health assessment, stabilization and connection to appropriate ongoing care. Other provinces have established some form of mobile mental health crisis team (whether run in collaboration with hospital emergency departments or regional police, or operating as stand-alone teams of clinicians), and have seen reductions in presentation to emergency departments and psychiatric hospital admissions as a result of these mobile mental health crisis. In the absence of this service, PEI will continue to experience higher than necessary emergency department and police response to mental health issues. In the first six months of 2017, the Queen Elizabeth Hospital emergency department had 296 mental health related visits, and the RCMP on PEI responded to over 200 mental health related calls during that same time period. These pressures resulted from a lack of timely access to mental health and addictions services at both the time and place they were needed. In other jurisdictions, the establishment of mobile mental health crisis teams have resulted in significant reductions in presentation to emergency departments and psychiatric hospital admissions.
Under the proposed model, new teams of clinicians will be connected with other first points of contact for individuals in mental health crisis (e.g., police, child and adult protection, etc.) who will also receive training in recognizing mental health issues and responding appropriately. The mobile mental health crisis teams will provide a key support for those first points of contact when the level of acuity out-strips their ability to respond.
These mobile mental health crisis teams will be composed of highly trained mental health professionals (in most cases, registered nurses with mental health training and social workers) embedded in each county of the province and supported by psychiatric resources. Effective teams are connected with other first points of contact for individuals in mental health crisis (e.g., police, child and adult protection, etc.) who also receive extensive training in recognizing mental health issues and responding appropriately. The teams will provide 24-7 rapid response either via telephone or in-person, thereby supporting earlier and more appropriate mental health care.
Federal funding will be used to support additional practitioners who would staff these response units, with any additional administrative, infrastructure and support costs funded by the Province.
Aside from addressing a key gap in the Island's mental health and addictions system, the addition of community-based mobile mental health crisis teams will meet a key goal of the Common Statement of Principles on Shared Health Priorities. Specifically, it will represent spread of evidence-based models of community mental health care.
While the cost associated with the mobile mental health crisis teams will exceed the available federal funds, the targeted funding will be used to offset the cost of hiring the necessary front line staff, with the remaining staffing costs and any necessary administrative costs funded by the Province.
Target Populations
While target populations for this initiative will be diverse, a key mechanism for identification of clients would be the inputs of those aforementioned first responders and first points of contact that encounter individuals in crisis. Thus strong partnerships with police, paramedics, child and adult protection, etc., would facilitate a clear pathway for individuals to receive services. This initiative would also build on the Province's ongoing efforts to ensure cultural safety and awareness training for many mental health and addictions staff, including members of the mobile mental health crisis teams.
Performance Measurement
Given the dynamic nature of this initiative and the current state of planning, a robust performance measurement framework has not yet been articulated. However, given the significance of this undertaking, it is expected that performance and monitoring metrics would be developed to assess the ongoing impact of the program, both in terms of individual outcomes for referred clients, as well as the program's overall impact on pressure points and service utilization within the broader mental health and addictions system.
Overall Performance Measurement and Monitoring of the Action Plan
In addition to the monitoring and evaluation that will be taking place within individual programs and initiatives described under the initiatives above, the Province of PEI is also committed to full participation in the development and reporting of a set of pan-Canadian indicators intended to monitor progress in the two areas of focus. Further to this, provincial representatives are currently engaged in discussions with CIHI and other Provincial-Territorial representatives to collaborate on the development of an appropriate set of indicators. Based on discussions among FPT Deputy Ministers of Health, the preliminary expectation is that this work will identify 3-5 indicators for each priority area, and that a phased approach to reporting will be rolled out over the term of the funding agreement. PEI is fully committed to working with CIHI and the other provinces and territories to establish an appropriate suite of indicators, and to report on them annually thereafter.
Prince Edward Island
Action Plan for Increased Infection Prevention and Control
- Overview
Background
Long Term Care Program description
On Prince Edward Island long term care is defined as the provision of specialized nursing and personal care services to individuals who can no longer live on their own, with family or home care supports. Long term residential care is provided by privately and publicly funded homes. Services provided in both public and private long term care homes include:
- 24-hour care which is provided by resident care workers, licensed practical nurses and registered nurses
- Room and board
- Personal care
- Medical services
Number and types of facilities
Prince Edward Island private and publicly owned long term care homes provide a total of 1,244 beds. The overall distribution of privately owned homes (for profit: 47% and not for profit: 6%) and publicly owned homes (47%) is similar to the national average.
There are nine publicly owned long term care homes and ten private long term care homes (eight of which are dual homes which contain both community care designed beds and long term care beds).
The relatively even distribution of facilities and beds between the private and public sector on Prince Edward Island has resulted in the development of supportive working relationships to ensure that the province's long term care needs are met. These relationships enhance the province's approach to the provision of long term care services as evidenced in the following examples:
Coordinated Pandemic Response
Private and public long term care homes have participated in regular virtual town halls, disseminated information resources, contributed to the development of contingency plans, and shared infection control expertise to embed a consistent response to the pandemic throughout the long term care sector.
Health Human Resource Planning
The Department of Health and Wellness, Health PEI and owners of private long term care homes participate in a monthly Private Nursing Homes Staffing Task Group to share information, strategies, and plan health human resource activities.
Provincial Seniors Health Services Planning
Private long term care home staff, owners and Directors of Nursing contributed to the development of the Provincial Seniors Health Services Plan and continue to be engaged in the implementation of the five year plan. A priority of this plan aims to ensure that quality, safety, and long term care services for residents are comparable across the sector.
Service type
Within a long term care home residents may have a variety of health and support requirements. On Prince Edward Island several categories of specialized support bed types are recognized:
- Designated dementia care. Dementia is not an uncommon diagnosis for individuals awaiting admission to or living in long term care and the number of people diagnosed with dementia is increasing. Quality dementia care requires not only safe and supportive environmental design but also staff expertise. Residents who wander can more safely move within designated dementia care areas which are designed to reduce the risk of unsafe wandering. The most complex designated dementia care beds are currently in publicly funded long term care homes. These specialty care beds require increased staff training and competency as well as safe and secure spaces.
- Complex care. Some residents may have multiple chronic conditions, complex medication routines, be at higher risk of acute health changes, complex psychological and/or behavioural responses requiring high level monitoring and care. Islanders with complex medical needs are growing and include the need for skills and competencies in managing peritoneal dialysis, bariatric care, and advanced respiratory support such as overnight ventilation. Complex care homes require increased physical and human resources most often found in public long term care homes.
- Cultural specialization. Recognizing and supporting diversity in long term care is an important quality indicator. Respecting the diversity, cultural, and linguistic needs of residents can help to ease the transition to long term care, reduce discrimination, isolation, communication barriers while improving overall quality of life. As an example, some long term care homes on Prince Edward Island provide cultural specialization by providing care in French, recognizing special holidays and offering traditional cuisine. Growing difficulty with recruitment of culturally competent staff, such as fully bilingual care workers has created challenges in continuing to offer culturally competent care. Indigenous Cultural Sensitivity training also a part of the strategic plan for the public long term care sector, but the onset of the pandemic caused a delay in the delivery of this training. However, this training will be pursued in the future.
- Young resident care. Some residents in Prince Edward Island long term care homes are under 60 years of age and require residential support to address complex care needs. This unique population has social, rehabilitation and programming needs that may differ significantly from the majority of other residents and be challenging to provide in the absence of allied health providers such as physiotherapists, speech therapists and occupational therapists. Prince Edward Home is currently the long term care home with the largest proportion of young residents. The care of young residents with complex needs in long term care is a unique to Prince Edward Island as other options for residential care are available in other jurisdictions.
- Respite care. Long term care respite beds provide an opportunity for caregivers to schedule a temporary stay in a long term care home for their care receiver in a safe setting designed to meet care needs. As illustrated in Figure 1, these beds are available in several communities across Prince Edward Island. There are 12 respite beds available in Prince Edward Island, all of which are in public long term care homes. Presently there are no respite beds routinely available for Islanders who may be in crisis in the community with the only available option being to present to a local hospital emergency department for admission.
The figure below depicts the distribution of beds by type across long term care homes (private and public).
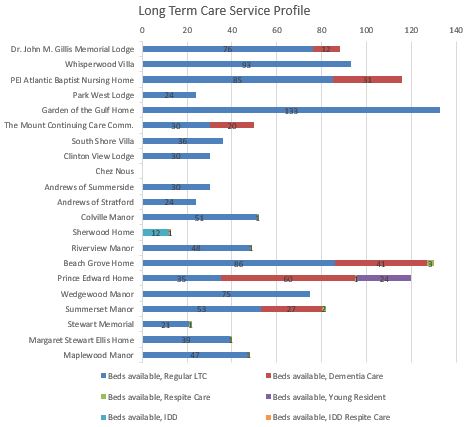
Figure 1 - Text Equivalent
| Long Term Care Facility | Beds available, by type |
|---|---|
| Dr. John M. Gillis Memorial Lodge | 76 regular long term care, 12 dementia care |
| Whisperwood Villa | 93 regular long term care |
| PEI Atlantic Baptist Nursing Home | 85 regular long term care, 31 dementia care |
| Park West Lodge | 25 regular long term care |
| Garden of the Gulf Home | 133 regular long term care |
| The Mount Continuing Care Comm. | 30 regular long term care, 20 dementia care |
| South Shore Villa | 36 regular long term care |
| Clinton View Lodge | 30 regular long term care |
| Chez Nous | - |
| Andrews of Summerside | 30 regular long term care |
| Andrews of Stratford | 24 regular long term care |
| Colville Manor | 51 regular long term care, one respite care |
| Sherwood Home | 12 IDD, one IDD Respite Care |
| Riverview Manor | 48 regular long term care, one respite care |
| Beach Grove Home | 86 regular long term care, 41 dementia care, three respite care |
| Prince Edward Home | 35 regular long term care, 60 dementia care, one respite care, 24 young resident |
| Wedgewood Manor | 75 regular long term care |
| Summerset Manor | 53 regular long term care, 27 dementia care, two respite care |
| Stewart Memorial | 21 regular long term care, one respite care |
| Margaret Stewart Ellis Home | 39 regular long term care, one respite care |
| Maplewood Manor | 47 regular long term care, 1 respite care |
Quality Assessment and Regulation
The Department of Health and Wellness is responsible for inspecting and licensing of private long term care homes pursuant to the Community Care Facilities and Nursing Homes Act. Private long term care homes are required to renew their license each year and must meet requirements as defined by the Community Care Facilities and Nursing Homes Act and Regulations. Private long term care homes are subject to inspections (food service, building, fire, care) to demonstrate adherence to requirements. Inspection results are reviewed with operators and posted publicly on the Department of Health and Wellness web pages. Private long term care licenses are issued by the Community Care and Nursing Homes Board, a corporate body appointed by the Minister of Health and Wellness.
Publicly funded home care homes are not licensed by the Community Care and Nursing Homes Board but participate in an Accreditation Canada assessment and quality improvement processes to meet quality standards. Accreditation status is based on the results of an external review which assesses Prince Edward Island results against national standards of excellence. As a result of the most recent evaluation process Health PEI was awarded Accreditation Status in October 2017. This status remains in effect for four years for all publicly funded long term care homes.
Challenges and issues faced in the delivery of services prior to March 2020
System challenges
- Availability of healthcare providers – both private and publicly funded long term care homes face challenges recruiting and retaining staff (all categories). As an example, of the most recently funded 100 long term care beds, 32 remain unopened due to staffing shortages. Wage differences between the public (higher) and private (lower) long term care sectors increase the challenges of staffing for private operators. Training opportunities, specifically seats, and a finite number of clinical placement opportunities may also limit the number of students entering and completing their professional training. These staffing pressures extend across the continuum of seniors health services to primary care, acute care and other areas such that staffing changes or the attempt to introduce new programs in one area may impact the provision of services in other areas.
- Different access to allied health care providers between private and public long term care homes– access to occupational, recreational, and physical therapists, dietitians and other providers differs between long term care homes. As an example, there is limited or no access to pharmacy services in publicly funded long term care homes while privately funded long term care homes partner with community pharmacies to coordinate services such as medication reviews.
- Limited availability of home care and support services – Long term care homes are part of a continuum of health services and do not exist in isolation. Pressure points, short or long term gaps or barriers to services in other areas of the continuum (ie primary care, acute care, community care, home care, social and community services) may result in premature transition to long term care homes. Gaps in the availability and accessibility of home care and community support services increase the risk of unnecessary time spent in hospital (alternate level of care) and premature admission to long term care. Prince Edward Island's current system of care is skewed toward institutionalizing older adults in the absence of other options that are required to prevent premature admission to long term care homes such as health promotion, restorative care, and home care.
- Data gaps in long term care – A lack of consistent tool used to track infection, safety, and resident health outcomes across care settings results in knowledge gaps in understanding the outcomes for older adults in long term care settings. Prince Edward Island is one of only two jurisdictions that does not use InterRAI for assessment and planning purposes. The difference between private and public long term care homes extends to the clinical information system which allows staff to review residents' health information and guide care. While all public long term care homes have access to the clinical information system only some private long term care homes have this functionality.
Demographic and individual challenges
- Age and Life expectancy – On Prince Edward Island, 20% of Islanders are aged 65 or older. Similar to the Canadian average, Islanders have some of the highest life expectancies in the world with Prince Edward Island male life expectancy at 78 years and females at 83 years. A higher population proportion of older adults requires greater attention and investment in geriatric care. If Prince Edward Island continues on its current path, based on population and demographic projections a 35% increase in the total number of long term care beds will be required by 2025.
- Health status – Overall 35.7% of Islanders report having a chronic condition (arthritis, diabetes, heart disease, COPD, hypertension) however this increases to 65.7%, compared to the national average of 62.7% for those ages 65 and older (CPHO report 2016). The presence of multiple chronic conditions can increase an individual's medical complexity and influence transitions in care.
- Frailty and disability – A report by the Chief Public Health Officer (2014) found that similar to other Canadians 43% of Islanders age 65 years and older were frail and 29% of those 50 to 64 years were frail. These rates of frailty require specialized interventions in long term care.
- Dementia – The prevalence of dementia on Prince Edward Island is increasing over time and as a consequence people with dementia may experience the longest wait times for a long term care bed. This wait for care often occurs in acute care as the individual experiences physical and cognitive losses living in an environment (hospital) not designed to meet their needs. Prince Edward Island has lengthy alternate level of care stay. Approximately 21.5% of patient days on Prince Edward Island were ALC which is higher than the Canadian average of 15.6% (CIHI 2017-2018).
Challenges since spring 2020
In the early days of the pandemic, supply chains for Personal Protective Equipment ("PPE") were chaotic and unreliable. Given the uncertain marketplace at that time, the increased level of competition for a finite pool of PPE, and the anticipated increases in local utilization, it was clear that a coordinated solution would be required to avoid a where small long term care facilities were simply unable to obtain these necessary and essential products.
Rapid and efficient communication of information concerning public health restrictions and vital infection prevention and control measures also proved to be challenging during the very early stages of the pandemic. Whether it was guidance on how to interpret and implement changing public health guidance, or advising on effective and necessary infection prevention and control measures, there were challenges involved with disseminating information effectively and consistently across the public and private long term care sectors.
With respect to Health Human Resources ("HHR") there were a number of pre-existing pressure points that also compounded the challenges of the pandemic response.
A long-standing national shortage of nursing, coupled with recent health program expansion in Prince Edward Island, contributed to staffing shortages for Prince Edward Island's long term care sector. More recently, shortages of staff such as geriatric assistants and resident care workers provided additional pressures in both the public and private long term care sectors. In addition, Resident Care Workers make up a significant portion of long term care facility staff on Prince Edward Island, but as an unregulated professions there is a limited ability to centrally assess and monitor the workforce, thereby ensuring quality of care;
Throughout the pandemic the level of access to residents in long term care by families and caregivers has varied. During the most restrictive public health measures, residents and families were separated and unable to support each other. This significant reduction in caregiver support not only affected residents but also increased the workload of staff who were required to perform additional caregiving duties normally taken on by the network of informal caregivers. This was further compounded by the necessary restrictions that prevented long term care staff from working at multiple sites to avoid/limit COVID spread within and between facilities.
The Response to Date
To help address these and other challenges, the Province put in place a number of significant measures after the onset of the pandemic.
To ensure the necessary and essential supply of PPE, the province established a provincial PPE warehousing system to meet the needs of a range of public and private health sector stakeholders. By integrating this vetting, distribution and warehousing function with both public and private sector stakeholders, we were able to ensure fair and adequate distribution of PPE despite the constrained supply and uncertainties of the marketplace at that time. As part of this effort, facilities provided regular inventory information to ensure optimal distribution of limited PPE supplies. Substantial support for this effort was provided by the Federal Government through the ongoing procurement and provisions of bulk PPE supplies, which was essential given the dynamic and constrained market for PPE during the early phases of the pandemic.
To further support the private long term care sector, a series of regular Town Halls were conducted virtually with facility owner/operators and government staff to ensure currency of information and accessibility of public health officials to resolve any questions of concerns that might arise. These Town Halls were invaluable in disseminating information and ensuring a shared understanding of public health measures.
To help address Health Human Resource constraints and challenges, a number of HHR initiatives were put in place which utilized funding previously provided under the Safe Restart Agreement, including additional funding supports for private facility owner/operators and the creation of a provincial working group with representatives from the private nursing homes association. This working group helped to ensure that HHR issues were identified immediately and addressed quickly. These issues included retention measures, hiring additional HHR where possible, and establishing additional janitorial capacity to meet the demands of increased cleaning regimens. In addition, student roles were expanded and extended within the health care system (including long term care) to help support the increased demand for support.
To further support both Community Care Facilities and Nursing Homes, the province quickly staffed and established an Infection Control and PPE Support Team that visited each facility during the early days of the pandemic. Once on site, they conducted comprehensive readiness assessments that reviewed the plans, practices and HHR capacity in place within each facility, and reviewed the range of measures and supports available to support their efforts. This initial effort was followed up by a second series of site visits to refresh the readiness assessments and review the response planning that was underway.
Finally, a strong degree of collaboration and coordination between long term care facilities and the provincial Public Health Nursing unit ensured that the campaign to deliver vaccines to long term care residents and staff was both rapid and effective. Enabled by strong Federal procurement efforts and ongoing vaccine provision, the provincial campaign was successful in rapidly vaccinating all residents and staff of long term care facilities (both public and private sector) during the first phase of the campaign. This was a key infection prevention and control measure in the provincial COVID response.
- Planned Response
Given the challenges noted above, the pandemic (and the response to it) have highlighted areas within the long term care sector where increased effort and investment are needed. With respect to infection prevention and control measures, the Government of Prince Edward Island is proposing to advance a number of initiatives that will lead to safer and more effective care for residents, not only in the event of possible future outbreaks but also during periods of more routine care where infection prevention and control remain important elements of quality and resident safety.
The total Federal funding envelope for the Safe Long Term Care Fund for Prince Edward Island is approximately $6.1Million. This is intended to support various infection prevention and control measures that address some of the issues noted above. Further to this, the Government of Prince Edward Island commits to the following initiatives that will enhance quality as well as resident and staff safety throughout both the public and private long term care sectors.
Workforce and Readiness Assessment Priorities
-
Education campaign/community of practice regarding hygiene and infection prevention and control measures
This would involve an ongoing effort to ensure a common baseline of training among all long term care staff (public and private) with respect to infection prevention and control measures such as hand hygiene, cleaning, etc. This is a long term initiative that would have the potential to have a high degree of impact in resident health and safety. By establishing a common baseline of training and ongoing professional development, this initiative will ensure system-wide knowledge of infection prevention and control measures and best practices.
A key element of this initiative would be the involvement of staff at various levels within the facilities. This would ensure that all aspects of long term care benefit from professional development opportunities and knowledge exchange.
An education tracking system is an additional component of this initiative that would be implemented to facilitate tracking of current education status for all long term care staff within the system. This would further support the move to standardize learning opportunities across the public and private long term care sectors and to integrate professional development opportunities. Initially the tracking system would be implemented for public long term care staff, with the understanding that the integration of private long term care staff would come later.
Cost estimate: $600,000
-
Establishment of an infection prevention and control program within the private sector (already in place within the public long term care system)
This initiative would involve the creation and implementation of a comprehensive infection prevention and control program within private long term care facilities, where designated infection prevention and control staff would be established within each facility in adherence to a specific staff-to-bed ratio.
Developing an appropriate staffing ratio would be the first step in establishing this program. This ratio would need to recognize the level of need, the challenges associated with recruitment of Registered Nurses, the existing capacity and expertise within the long term care system, and the need to accommodate smaller facilities that may not have enough beds to warrant a single dedicated position focused solely in infection prevention and control.
Once established, these lead staff would coordinate annual training and on-boarding for new staff (including cleaning staff) and would oversee a range of infection prevention and control measures within all long term care facilities across Prince Edward Island. Like the aforementioned education campaign, this would be a long term initiative that would have substantial impact on quality and resident safety over time. By ensuring the implementation of a comprehensive infection prevention and control program at all facilities, these dedicated staff would be a key component in strengthening the Island's long term care system.
This initiative would be coordinated with the education campaign initiative to ensure that the training provided to staff is integrated with the needs identified through the infection prevention and control program.
To ensure this additional support does not displace existing investments made by these for profit facilities, and to demonstrate the facilities' commitment to contributing to enhanced infection prevention and control, facilities will also contribute financial and in kind support to the implementation of this program.
Cost estimate: $500,000
Infrastructure Priority
-
Equipment purchase and replacement program
This initiative would involve the provision of funding to replace aging and outdated (but essential) equipment. Given the age of some facilities, the prioritization of other operational costs such as staffing, and the advancement of technology, there are a range of equipment needs that have evolved within both public and private long term care facilities. These can include items such as touchless sinks to allow for more frequent and more hygienic handwashing, older suction machines that are in need of replacement with those that are more easily cleaned and maintained, or extra slings that would allow for more thorough and regular laundering.
To ensure a fair allocation of funds, the Province will be establishing a funding distribution mechanism that balances the urgent need for new equipment in specific facilities with a general need for equitable access across the sector. The first step in this initiative would involve a provincially-led equipment audit to identify equipment gaps and replacement needs. This audit would involve an assessment of both the public and private long term care systems, and would provide an objective baseline against which specific applications and requests for funding could be assessed. (In the absence of this audit, it isn't possible to identify facility-specific expenditures at this time, but the Government of Prince Edward Island commits to the administration of a fair distribution mechanism and to ensuring that for profit facilities are cost-sharing as appropriate).
Once completed, this time-limited initiative would result in significant improvement in infection prevention and control measures by allowing for improved hygiene across a range of activities that regularly occur within both the public and private long term care sectors.
Cost estimate: $1,000,000
-
Infrastructure development and upgrades
This initiative would include essential infrastructure upgrades such as the installation of new ventilation systems and the conversion of double rooms to single rooms.
With respect to the planned replacement of ventilation units, Government of Prince Edward Island begin by engaging an HVAC consultant (via a tendering process) to conduct a comprehensive assessment of all public and private long term care facilities. This consultant would identify and prioritize the areas of highest need, and would advise on the optimal ventilation solutions for the facilities that were identified as priorities. To ensure that these expenditures are "future-proof", the assessment would include consideration of future air conditioning needs to meet the increased cooling demands anticipated as a result of climate change.
In terms of planned room conversions, three specific items within the public long term care system, have been identified as part of this initiative. First, planned renovations within the Beach Grove facility will convert existing double rooms into a purpose-built dementia unit (to be known as "Meadow") that will consist solely of single rooms. Given the challenges that can be encountered when implementing effective infection prevention and control measures within this client group, the creation of a dedicated dementia unit based on effective infection prevention and control design principles will be important step forward. In addition to the creation of this unit, additional room conversion will take place within the Beach Grove facility, as well as within the Wedgewood facility.
Within the private long term care system, some in-scope work was already completed at the Chez Nous facility during the identified eligibility period under this funding (i.e. since December 1, 2020). This work consisted of the installation of a new ventilation system and conversion of double rooms to single rooms to allow for improved infection prevention and control. This conversion of rooms supports the identified need for isolation rooms that allow for facilities to "care in place" for any COVID-positive residents (rather than transferring them to hospitals), in alignment with the provincial plans for infection prevention and control. To support the distribution of these funds within the private long term care sector, an application process would be put in place to allocate funds to those facilities that wanted to leverage supports for enhanced infection prevention and control infrastructure. As with the mechanism to allocate funding for equipment upgrades, the distribution of these funds would balance the areas of highest priority with the need to ensure fair and equitable access to financial supports, and ensure for-profit facilities are not displacing their own existing investments to improve infection and prevention control.
Cost estimate: $4,000,000
Oversight
As part of the commitments made within this Action Plan, the Province of Prince Edward Island commits to the ongoing oversight of funding allocated to any recipient long term care facilities. This would include the establishment of fair and appropriate distribution mechanisms, and the requirement of detailed and regular financial reporting from both private and public sector recipients.
While detailed and itemized spending information has not been provided as part of this Action Plan, these ongoing accountability and reporting requirements will ensure that all funding allocated under this agreement is spent in accordance with the principles guiding this funding. In short, the Government of Prince Edward Island commits to ensuring that all Safe Long Term Care funding provided under this agreement will be used to enhance infection prevention and control measures within Island's longer term care sectors.
Updates and further detail will be provided at the time of interim reporting (in December 2021).
| Priority areas | Output | Interim results (reported by December 1, 2021Footnote i) | Results (reported by March 31, 2022)1 |
|---|---|---|---|
| Education campaign/community of practice | X number of staff trained Province-wide tracking system for training |
Planning is underway for the education campaign but due to competing pressures related to COVID-19, and the need to be mindful of change management needed in introducing new changes to the sector, the implementation of a new education campaign/community of practice has been delayed to 2022-23. The Government of Prince Edward Island will begin the procurement and installation of the province-wide tracking system for training in the coming months, to standardize a common curriculum of hygiene and infection prevention and control measures. The final results for this initiative, to be provided in 2022/23, will include the details of the tracking system, as well as the number of staff trained across long-term care facilities. |
- |
| Infection prevention and control program within the private sector | Appropriate ratio of staff to facility to support infection prevention and control (number to be confirmed based on audit) | To date, the Government of Prince Edward Island has completed foundational work to create the infection, prevention and control program, including engaging staff, lead registered nurses facility owners/operators and initial program model development. In the coming months, the program model will be finalized, designated infection prevention and control staff will be hired and trained, and the new program model will be fully operationalized. |
- |
| Equipment purchase and replacement program | Replacement of outdated equipment based on needs identified in provincially-led equipment audit | To date, the Government of Prince Edward Island has identified many of the core equipment needs and upgrades that need to be made within facilities to increase infection, prevention and control. Due to capacity constraints related to COVID-19 and high demand for equipment, procuring equipment and implementing the replacement program in long-term care facilities across the province has faced some delays. The procurement and installation of this new equipment will be completed in the coming months. |
- |
| Infrastructure development and upgrades | External assessment of infrastructure needs Infrastructure upgrades in facilities |
To date, the Government of Prince Edward Island has provided infrastructure support for facilities in both the public and private sectors. This includes the installation of a new ventilation system, the conversion of double rooms to single rooms to allow for improved infection prevention and control, and other essential infrastructure improvements. Due to capacity constraints related to COVID-19, including availability of goods and materials as well as labour pool shortages, delays have occurred in procuring equipment and facilitating infrastructure upgrades in some long-term care facilities. In the coming months, The Government of Prince Edward Island will continue the assessment of infrastructure needs across facilities as well as implement a program to allocate funds to facilities. This process will be informed by evidence arising from the patterns of infection and transmission in long-term care homes which was documented by the Chief Public Health Office. |
- |
|
|||