Canada-Ontario Agreement to Work Together to Improve Health Care for Canadians (2023-24 to 2025-26)
Tables of contents
- Funding agreement
- Annex 1 – Common statement of principles on shared health priorities
- Annex 2 – Shared pan-Canadian interoperability roadmap
- Annex 3 – Headline common indicators
- Annex 4 – Action plan
Funding agreement
(the "Agreement")
Between:
His Majesty the King in Right of Canada (hereinafter referred to as "Canada" or "Government of Canada") as represented by the Minister of Health and the Minister of Mental Health and Addictions and Associate Minister of Health (herein referred to as "the federal Ministers")
- and -
His Majesty the King in Right of the Province of Ontario (hereinafter referred to as "Ontario" or "Government of Ontario") as represented by the Minister of Health (herein referred to as "the provincial Minister")
Referred to collectively as the "Parties", and individually as a "Party"
Preamble
Whereas, on February 23, 2023, Canada and Ontario announced an overarching agreement in principle on Working Together to Improve Health Care for Canadians, supported by almost $200 billion over ten years in federal funding, including $46.2 billion in new funding to provinces and territories;
Whereas, Working Together to Improve Health Care for Canadians includes a federal commitment of $25 billion in bilateral funding to provinces and territories over ten years focused on four shared health priorities:
- expanding access to family health services, including in rural and remote areas;
- supporting our health workers and reducing backlogs;
- improving access to quality mental health and substance use services; and
- modernizing health systems with health data and digital tools.
Whereas, in the area of mental health and substance use, Working Together to Improve Health Care for Canadians also includes a commitment by Canada and Ontario to continue to work to support collaboration on the Common Statement of Principles on Shared Health Priorities (hereinafter referred to as the "Common Statement", attached hereto as Annex 1), supported by the federal Budget 2017 investment of $5 billion over ten years;
Whereas, Ontario has the primary responsibility for delivering health care services to its residents and makes ongoing and significant investments in health consistent with its broader responsibilities for delivering health care services to its residents and in supporting diversity, equity, and the needs of underserved and/or disadvantaged populations, including, but not limited to First Nations, Inuit and Métis, official language minority communities, rural and remote communities, children, racialized communities (including Black Canadians), and LGBTIQA2S+;
Whereas, Canada authorized the federal Ministers to enter into agreements with the provinces and territories, for the purpose of identifying activities that provinces and territories will undertake in respect of the four shared health priorities, and for funding in this Agreement associated with the federal investment for mental health, substance use, and addictions services consistent with the Common Statement (and menu of actions outlined in Annex 1);
Whereas, the Ministry of Health and Long-Term Care Act authorized the provincial Minister to enter into agreements with the Government of Canada under which Canada undertakes to provide funding toward costs incurred by the Government of Ontario associated with the federal investment for four shared health priorities, and mental health, substance use and addictions services consistent with the Common Statement; and
Now therefore, this Agreement sets out the terms between Canada and Ontario as follows:
1.0 Key principles and collaboration
The key principles and commitment to collaboration agreed to in Working Together to Improve Health Care for Canadians are outlined below.
1.1 Canada and Ontario acknowledge that this Agreement will mutually respect each government's jurisdiction, and be underpinned by key principles, including:
- A shared responsibility to uphold the Canada Health Act that strengthens our public health care system;
- Principles agreed to in the Common Statement (outlined in Annex 1);
- Reconciliation with Indigenous Peoples, recognizing their right to fair and equal access to quality and culturally safe health services free from racism and discrimination anywhere in Canada, including through seamless service delivery across jurisdictions and meaningful engagement and work with Indigenous organizations and governments; and
- Equity of access for under-served groups and individuals, including those in official language minority communities.
1.2 Canada and Ontario acknowledge the importance of supporting health data infrastructure, data collection and public reporting, and will work together to improve the collection, sharing and use of de-identified health information, respecting federal/provincial/territorial privacy legislation, to improve transparency on results and to help manage public health emergencies, and to ensure Canadians can access their own health information and benefit from it being shared between health workers across health settings. This includes:
- collecting and securely sharing high-quality, comparable information needed to improve services to Canadians, including disaggregated data on key common health indicators with the Canadian Institute for Health Information (CIHI);
- adopting common interoperability standards (both technical exchange and content of data), including the Shared pan-Canadian Interoperability Roadmap (outlined in Annex 2), to improve Canadians' access to their health information in a usable digital format and support the exchange and analysis of health data within and across Canada's health systems in a way that protects Canadians' privacy and ensures the ethical use of data to improve the health and lives of people;
- work to align provincial and territorial policies and legislative frameworks where necessary and appropriate to support secure patient access to health information, and stewardship of health information to support the public good, including improving care quality, patient safety, privacy protection, system governance and oversight, planning and research;
- promoting health information as a public good by working with federal-provincial-territorial Ministers of Health to review and confirm overarching principles, which would affirm Canadians' ability to access their health information and have it follow them across all points of care. The existing Health Data Charter, as outlined in the Pan-Canadian Health Data Strategy would serve as the starting point for the discussion of these principles; and
- collecting and sharing available public health data (e.g., vaccination data, testing data) with the Public Health Agency of Canada to support Canada's preparedness and response to public health events, building on commitments made as part of the Safe Restart Agreements.
1.3 Canada and Ontario acknowledge they will work with other provinces and territories to streamline foreign credential recognition for internationally-educated health professionals, and to advance labour mobility, starting with multi-jurisdictional recognition of health professional licences.
1.4 Canada and Ontario acknowledge a mutual intent to engage in a two-phased formal review process:
- Phase 1: This review will be done in 2026 by a joint committee of Federal, Provincial, and Territorial health and finance officials to assess results and determine next steps for bilateral agreements related to improvements to home and community care, mental health, substance use, and addiction services associated with the Common Statement and long-term care; and
- Phase 2: A formal five-year review of the healthcare plan outlined on February 7, 2023, recognizing the importance of long-term sustainability for provincial-territorial health systems. This review would consist of an assessment of both the bilateral agreements (herein) and the CHT investments (not included as part of this bilateral agreement). The review will be done by a joint committee of Federal, Provincial, and Territorial health, and finance officials, commencing by March 31, 2027, and concluded by December 31, 2027, to consider results achieved thus far in the four shared health priority areas and will include:
- an assessment of progress-to-date on public reporting to Canadians using the common indicators;
- sharing of de-identified health information, and other health data commitments; and
- current and forward-looking Federal, Provincial, and Territorial investments to support this plan.
2.0 Objectives
2.1 Canada and Ontario agree that, with financial support from Canada, Ontario will continue to build and enhance its health care system towards achieving some or all of the objectives of:
- timely access to high-quality family health services, including in rural and remote areas;
- a sustainable, efficient and resilient health workforce that provides Canadians timely access to high-quality, effective, and safe health services;
- access to timely, equitable, and quality mental health and substance use services to support Canadians' well-being; and
- access to a patient's own electronic health information that is shared between the health professionals they consult to improve safety and quality of care, and which informs Canadians on how the system is working.
2.2 Canada and Ontario agree that, with Budget 2017 financial support from Canada outlined in 5.2.2, Ontario will continue to work to improve access to mental health and substance use services consistent with the Common Statement (and menu of actions outlined in Annex 1).
3.0 Action plan
3.1 Ontario set out in their Action Plan (attached as Annex 4) how the federal investment under this Agreement will be used, as well as details on targets and timeframes based on common headline indicators in priority areas where federal funds will be invested, as well as jurisdiction-specific indicators, for each of the initiatives.
3.2 Ontario will invest federal funding as part of the 2017 commitment for mental health, and substance use services provided through this Agreement in alignment with the menu of actions listed in the Common Statement.
3.3 Ontario will invest federal funding in some or all of the four shared health priority areas, without displacing existing planned spending in those areas.
3.4 In developing initiatives under this Agreement, Ontario agrees to implement measures that also respond to the needs of underserved and/or disadvantaged populations, including, but not limited to First Nations, Inuit and Métis, official language minority communities, rural and remote communities, children, racialized communities (including Black Canadians), and LGBTIQA2S+.
3.5 Ontario's approach to achieving objectives is set out in their three-year Action Plan (2023-24 to 2025-26), as set out in Annex 4.
4.0 Term of agreement
4.1 This Agreement comes into effect upon the date of the last signature of the Parties and will remain in effect until March 31, 2026 ("the Term"), unless terminated in accordance with section 11 of this Agreement. Funding provided under this Agreement will cover the period April 1, 2023 to March 31, 2026.
4.2 Renewal of Bilateral Agreements
4.2.1 Upon signing renewed bilateral agreements, Ontario will have access to the remainder of its share of the federal funding, subject to appropriation by Parliament, for:
- 2026-27, the allocation based on the federal commitment in Budget 2017 of $5 billion over ten years for mental health, substance use and addiction services; and
- 2026-27 to 2032-33, the allocation based on the federal commitment in Budget 2023 of $25 billion over ten years to support the Working Together to Improve Health Care for Canadians plan.
5.0 Financial provisions
5.1 The funding provided under this Agreement is in addition to and not in lieu of those that Canada currently provides under the CHT to support delivering health care services within the province.
5.2 Allocation to Ontario
5.2.1 In this Agreement, "Fiscal Year" means the period commencing on April 1 of any calendar year and terminating on March 31 of the immediately following calendar year.
5.2.2 Canada has designated the following maximum amounts to be transferred in total to all provinces and territories under this initiative based on the allocation method outlined in subsection 5.2.3 for the Term of this Agreement.
Working Together to Improve Health Care for Canadians
- $2.5 billion for the Fiscal Year beginning on April 1, 2023
- $2.5 billion for the Fiscal Year beginning on April 1, 2024
- $2.5 billion for the Fiscal Year beginning on April 1, 2025
Budget 2017 Mental Health, Substance Use, and Addictions Services
- $600 million for the Fiscal Year beginning on April 1, 2023
- $600 million for the Fiscal Year beginning on April 1, 2024
- $600 million for the Fiscal Year beginning on April 1, 2025
5.2.3 Allocation Method
- For the funding associated with Working Together to Improve Health Care for Canadians, annual funding will be allocated to provinces and territories on base ($5,000,000 if population is less than 100,000; $20,000,000 if population is between 100,000 and 500,000; and $50,000,000 if population is greater than 500,000) plus per capita basis. The final total amount to be paid to each jurisdiction will be calculated using the following formula: B + (F – ((N * 5,000,000) + (O * 20,000,000) + (S * 50,000,000)) x (K / L), where:
B is the base amount allocated to each province or territory based on population ($5,000,000 if population is less than 100,000; $20,000,000 if population is between 100,000 and 500,000; and $50,000,000 if population is greater than 500,000), as determined using annual population estimates on July 1st from Statistics Canada;
F is the total annual funding amount available outlined under this program;
N is the number of provinces and territories with a population less than 100,000, as determined using annual population estimates on July 1st from Statistics Canada;
O is the number of provinces and territories with a population between 100,000 and 500,000, as determined using annual population estimates on July 1st from Statistics Canada;
S is the number of provinces and territories with a population greater than 500,000, as determined using annual population estimates on July 1st from Statistics Canada;
K is the total population of Ontario, as determined using annual population estimates on July 1st from Statistics Canada; and
L is the total population of Canada, as determined using annual population estimates on July 1st from Statistics Canada.
- For funds associated with Budget 2017 Mental Health, Substance Use, and Addictions Services, annual funding will be allocated to provinces and territories on a per capita basis. The per capita funding for each Fiscal Year, is calculated using the following formula: F x K/L, where:
F is the annual total funding amount available under this program;
K is the total population of Ontario, as determined using the annual population estimates on July 1st from Statistics Canada; and
L is the total population of Canada, as determined using the annual population estimates on July 1st from Statistics Canada.
| Fiscal Year | Working Together to Improve Health Care for CanadiansEstimated amount to be paid to OntarioFootnote * (subject to annual adjustment) | Budget 2017 Mental Health, Substance Use, and Addictions Services Estimated amount to be paid to OntarioFootnote * (subject to annual adjustment) |
|---|---|---|
| 2023-2024 | $832,060,000 | $232,870,000 |
| 2024-2025 | $832,060,000 | $232,870,000 |
| 2025-2026 | $832,060,000 | $232,870,000 |
|
||
5.3 Payment
5.3.1 Funding provided by Canada will be paid in semi-annual installments as follows:
- In 2023-2024, the first installment will be paid within approximately 30 business days of execution of this Agreement by the Parties. The second installment will be paid on or about November 15.
- Starting in 2024-2025, the first installment will be paid on or about April 15 of each Fiscal Year and the second installment will be paid on or about November 15 of each Fiscal Year.
- The first installment will be equal to 50% of the notional amount set out in section 5.2.4 as adjusted by section 5.2.3.
- The second installment will be equal to the balance of funding provided by Canada for the Fiscal Year as determined under sections 5.2.3 and 5.2.4.
- Canada will notify Ontario prior to the first payment of each Fiscal Year, of their notional amount. The notional amount will be based on the Statistics Canada quarterly preliminary population estimates on July 1 of the preceding Fiscal Year. Prior to the second payment, Canada will notify Ontario of the amount of the second installment as determined under sections 5.2.3 and 5.2.4.
- Canada shall withhold payments if Ontario has failed to provide reporting in accordance with 7.1.
- Canada shall withhold the second payment in 2023-24 if Ontario has failed to satisfy all reporting requirements associated with the preceding Canada – Ontario Home and Community Care and Mental Health and Addictions Services Funding Agreement 2022-23, specifically to:
- continue to participate in a Federal-Provincial-Territorial process to improve reporting on and provide data to CIHI for the 6 common indicators to measure pan-Canadian progress on improving access to mental health, substance use, and addictions services; and
- submit an annual financial statement, with attestation from the province's Chief Financial Officer, of funding received the preceding Fiscal Year from Canada for mental health and substance use services under the Canada – Ontario Home and Community Care and Mental Health and Addictions Services Funding Agreement 2022-23 compared against the Expenditure Plan, and noting any variances, between actual expenditures and the Expenditure Plan.
- The sum of both installments constitutes a final payment and is not subject to any further payment once the second installment has been paid.
- Payment of Canada's funding for this Agreement is subject to an annual appropriation by the Parliament of Canada for this purpose.
5.4 Retaining funds
5.4.1 For Fiscal Years 2023-24 through 2024-25, upon request, Ontario may retain and carry forward to the next Fiscal Year up to 10 percent of funding that is in excess of the amount of the eligible costs actually incurred in a Fiscal Year and use the amount carried forward for expenditures on eligible areas of investment. Any request to retain and carry forward an amount exceeding 10 percent will be subject to discussion and mutual agreement in writing by their designated officials, at the Assistant Deputy Minister level (herein referred to as "Designated Officials"), and is subject to monitoring and reporting to Canada on the management and spending of the funds carried forward on a quarterly basis.
5.4.2 Any amount carried forward from one Fiscal Year to the next under this subsection is supplementary to the maximum amount payable to Ontario under subsection 5.2.4 of this Agreement in the next Fiscal Year.
5.4.3 Upon request, Ontario may retain and carry forward up to 10 percent of funding provided in the last Fiscal Year of this Agreement for eligible areas of investment, to be noted in the new agreement and subject to the terms and conditions of that new agreement. The new Action Plan will provide details on how any retained funds carried forward will be expended. Any request by Ontario to retain and carry forward an amount exceeding 10 percent will be subject to discussion and mutual agreement in writing by their Designated Officials, and is subject to monitoring and reporting to Canada on the management and spending of the funds carried forward on a quarterly basis.
5.5 Repayment of overpayment
5.5.1. In the event payments made exceed the amount to which Ontario is entitled under this Agreement, the amount of the excess is a debt due to Canada and, unless otherwise agreed to in writing by the Parties, Ontario shall repay the amount within sixty (60) calendar days of written notice from Canada.
5.6 Use of funds
5.6.1. The Parties agree that funds provided under this Agreement will only be used by Ontario in accordance with the initiatives outlined in Annex 4.
5.7 Eligible expenditures
5.7.1. Eligible expenditures under this Agreement are the following:
- data development and collection to support reporting;
- information technology and health information infrastructure;
- capital and operating funding;
- salaries and benefits;
- training, professional development; and
- information and communications material related to programs.
6.0 Performance measurement
6.1 Ontario agrees to designate an official or official(s), for the duration of this Agreement to participate in a CIHI led Federal-Provincial-Territorial indicator process to:
- Refine the eight common headline indicators (outlined in Annex 3);
- Work to identify additional common indicators that are mutually agreed upon, including indicators focused on the health of Indigenous populations with acknowledgement of the role for Indigenous partners in this work;
- Improve reporting on common indicators to measure pan-Canadian progress on improving access to mental health, substance use, and addictions services, associated with the commitment in the Common Statement; and
- Share available disaggregated data with CIHI and work with CIHI to improve availability of disaggregated data for existing and new common indicators to enable reporting on progress for underserved and/or disadvantaged populations including, but not limited to, Indigenous peoples, First Nations, Inuit, Métis, official language minority communities, rural and remote communities, children, racialized communities (including Black Canadians), and LGBTIQA2S+.
7.0 Reporting to Canadians
7.1 Funding conditions and reporting
7.1.1 By no later than October 1, in each fiscal year, with respect of the previous Fiscal Year, Ontario agrees to:
- Provide data and information annually to CIHI related to the new headline indicators, additional common indicators, and the mental health and substance use services indicators identified as part of commitment made in the Common Statement.
- Beginning in Fiscal Year 2024-25, report annually and publicly in an integrated manner to residents of Ontario on progress made on targets outlined in Annex 4 (Action Plan) for headline indicators in the priority area(s) where federal funds are to be invested, and on jurisdiction-specific indicators for each of the initiatives tailored to their jurisdiction's needs and circumstances.
- Beginning in Fiscal Year 2024-25, provide to Canada an annual financial statement, with attestation from the province's Financial Officer, of funding received the preceding Fiscal Year from Canada under this Agreement or the Previous Agreement compared against the Action Plan, and noting any variances, between actual expenditures and the Action Plan:
- The revenue section of the statement shall show the amount received from Canada under this Agreement during the Fiscal Year;
- The total amount of funding used for each of the shared health priority areas that are supported by the federal funds;
- If applicable, the amount of any funding carried forward under section 5.4; and
- If applicable, the amount of overpayment that is to be repaid to Canada under section 5.5.
7.1.2 Ontario will provide quarterly reporting to Canada on the management and spending of the funds retained to the next Fiscal Year.
7.2 Audit
7.2.1 Ontario will ensure that expenditure information presented in the annual financial statement is, in accordance with Ontario's standard accounting practices, complete and accurate.
7.3 Evaluation
7.3.1 Responsibility for evaluation of programs rests with Ontario in accordance with its own evaluation policies and practices.
8.0 Communications
8.1 The Parties agree on the importance of communicating with citizens about the objectives of this Agreement in an open, transparent, effective and proactive manner through appropriate public information activities.
8.2 Each Party will receive the appropriate credit and visibility when investments financed through funds granted under this Agreement are announced to the public.
8.3 In the spirit of transparency and open government, Canada will make this Agreement, including any amendments, publicly available on a Government of Canada website.
8.4 Ontario will make publicly available, clearly identified, on a Government of Ontario webpage this Agreement, including any amendments to the Agreement.
8.5 Canada, with prior notice to Ontario, may incorporate all or any part of the data and information in 7.1, or any part of evaluation and audit reports made public by Ontario into any report that Canada may prepare for its own purposes, including any reports to the Parliament of Canada or reports that may be made public.
8.6 Canada reserves the right to conduct public communications, announcements, events, outreach and promotional activities about the Common Statement and this Agreement. Canada agrees to give Ontario 10 days advance notice and advance copies of public communications related to the Common Statement, this Agreement, and results of the investments of this Agreement.
8.7 Ontario reserves the right to conduct public communications, announcements, events, outreach and promotional activities about the Common Statement and this Agreement. Ontario agrees to give Canada 10 days advance notice and advance copies of public communications related to the Common Statement this Agreement, and results of the investments of this Agreement.
8.8 Canada and Ontario agree to participate in a joint announcement upon signing of this Agreement.
8.9 Canada and Ontario agree to work together to identify mutually agreeable opportunities for joint announcements relating to programs funded under this Agreement.
9.0 Dispute resolution
9.1 The Parties are committed to working together and avoiding disputes through government-to-government information exchange, advance notice, early consultation, and discussion, clarification, and resolution of issues, as they arise.
9.2 If at any time a Party is of the opinion that the other Party has failed to comply with any of its obligations or undertakings under this Agreement or is in breach of any term or condition of the Agreement, that Party may notify the other Party in writing of the failure or breach. Upon such notice, the Parties will endeavour to resolve the issue in dispute bilaterally through their Designated Officials.
9.3 If a dispute cannot be resolved by Designated Officials, then the dispute will be referred to the Deputy Ministers of Canada and Ontario responsible for health, and if it cannot be resolved by them, then the federal Minister(s) and the provincial Minister(s) responsible for health shall endeavour to resolve the dispute.
10.0 Amendments to the agreement
10.1 The main text of this Agreement may be amended at any time by mutual consent of the Parties. Any amendments shall be in writing and signed, in the case of Canada, by the federal Minister(s), and in the case of Ontario, by the provincial Minister(s).
10.2 Annex 4 may be amended at any time by mutual consent of the Parties. Any amendments to Annex 4 shall be in writing and signed by each Party's Designated Official.
11.0 Termination
11.1 Either Party may terminate this Agreement at any time if the terms are not respected by giving at least 6 months written notice of intention to terminate.
11.2 As of the effective date of termination of this Agreement, Canada shall have no obligation to make any further payments.
11.3 Sections 1.0, and 8.0 of this Agreement survive for the period of the 10-year Working Together to Improve Health Care for Canadians plan.
11.4 Sections 5.4 and 7.0 of this Agreement survive the termination or expiration of this Agreement until reporting obligations are completed.
12.0 Notice
12.1 Any notice, information, or document provided for under this Agreement will be effectively given if delivered or sent by letter, email, postage or other charges prepaid. Any communication that is delivered will be deemed to have been received in delivery; and, except in periods of postal disruption, any communication mailed by post will be deemed to have been received eight calendar days after being mailed.
The address of the Designated Official for Canada shall be:
Assistant Deputy Minister, Strategic Policy Branch
Health Canada
70 Colombine Driveway
Brooke Claxton Building
Ottawa, Ontario
K1A 0K9
Email: jocelyne.voisin@hc-sc.gc.ca
The address of the Designated Official for Ontario shall be:
Assistant Deputy Minister: Strategic Policy, Planning & French Language Services
Ministry of Health
438 University Avenue, 10th Floor
Toronto, Ontario
M7A 1N3
Email: greg.hein@ontario.ca
13.0 General
13.1 This Agreement, including Annexes, comprises the entire Agreement entered into by the Parties.
13.2 This Agreement shall be governed by and interpreted in accordance with the laws of Canada and Ontario.
13.3 No member of the House of Commons or of the Senate of Canada or of the Legislature of Ontario shall be admitted to any share or part of this Agreement, or to any benefit arising therefrom.
13.4 If for any reason a provision of this Agreement, that is not a fundamental term, is found by a court of competent jurisdiction to be or to have become invalid or unenforceable, in whole or in part, it will be severed and deleted from this Agreement, but all the other provisions of this Agreement will continue to be valid and enforceable.
13.5 This Agreement may be executed in counterparts, in which case (i) the Parties have caused this Agreement to be duly signed by the undersigned authorized representatives in separate signature pages in accordance with the following signature process, which together shall constitute one agreement, and (ii) the Parties agree that facsimile signature(s) and signature(s) transmitted by PDF shall be treated as original signature(s). Electronic signature(s) may be accepted as originals so long as the source of the transmission can be reasonably connected to the signatory.
In witness whereof the Parties have executed this Agreement through duly authorized representatives.
SIGNED on behalf of Canada by the Minister of Health
The Honourable Mark Holland, Minister of Health
SIGNED on behalf of Canada by the Minister of Mental Health and Addictions and Associate Minister of Health
The Honourable Ya'ara Saks, Minister of Mental Health and Addictions and Associate Minister of Health
SIGNED on behalf of Ontario by the Minister of Health
The Honourable Sylvia Jones, Deputy Premier and Minister of Health
Annex 1 – Common Statement of Principles on Shared Health Priorities
Common Statement of Principles on Shared Health Priorities
Annex 2 – Shared pan-Canadian interoperability roadmap
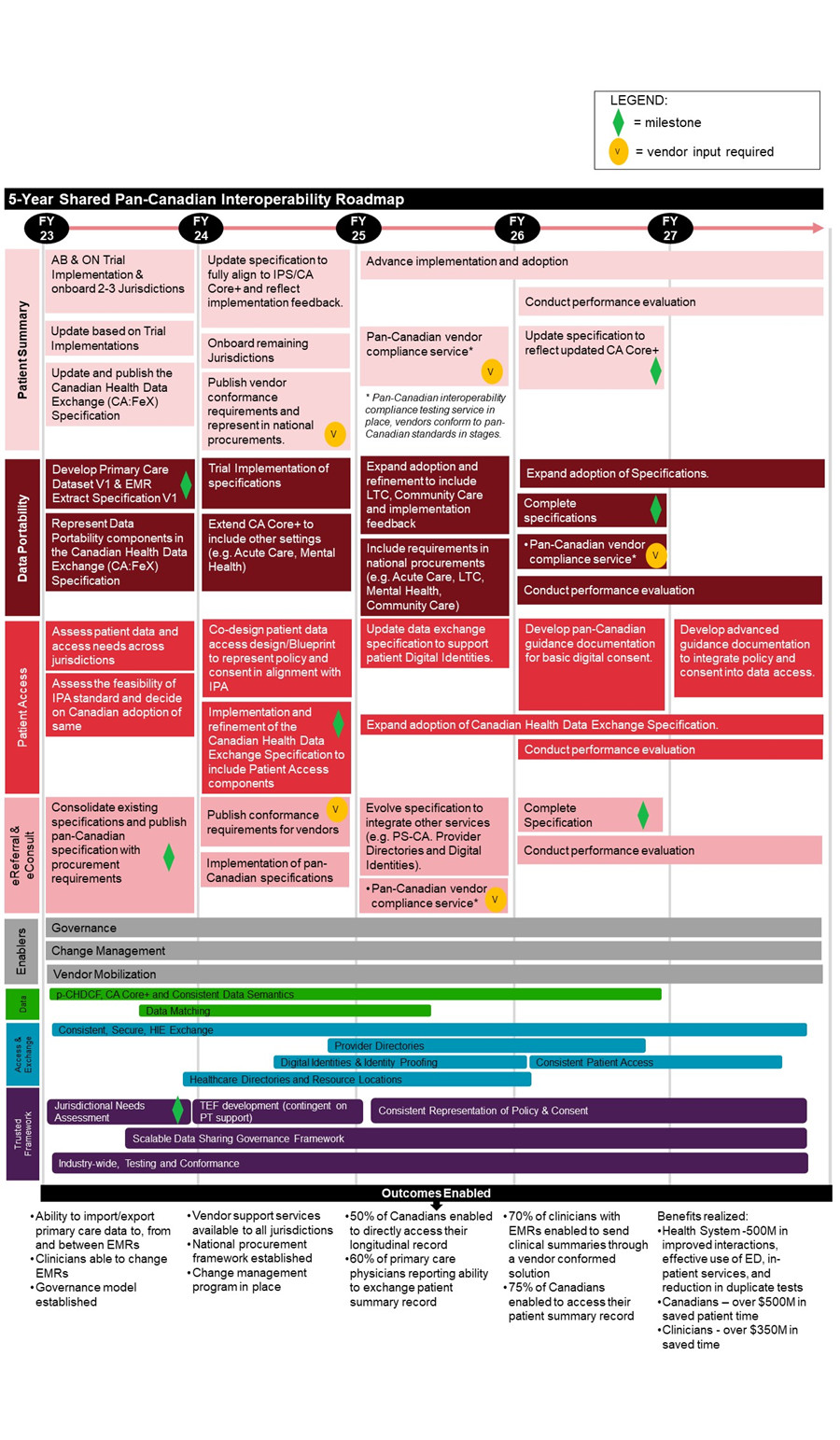
Figure 1 - Text description
The Roadmap outlines 8 categories of activities planned for fiscal years 2023 to 2027, followed by anticipated outcomes enabled. Notes are also included throughout to highlight a "milestone", where "vendor input is required", and/or when an activity is "continued" across multiple fiscal years.
Patient Summary
- Fiscal Year 2023
- Alberta & Ontario Trial Implementation & onboard 2-3 Jurisdictions
- Update based on Trial Implementations
- Update and publish the Canadian Health Data Exchange (CA:FeX) Specification
- Fiscal Year 2024
- Update specification to fully align to IPS/CA Core+ and reflect implementation feedback
- nboard remaining jurisdictions
- Publish vendor conformance requirements and represent in national procurements [vendor input required]
- Fiscal Year 2025
- Advance implementation and adoption
- Pan-Canadian vendor compliance service *(Pan-Canadian interoperability compliance testing service in place, vendors conform to pan-Canadian standards in stages.) [vendor input required]
- Fiscal Year 2026
- Advance implementation and adoption [continued]
- Conduct performance evaluation
- Update specification to reflect updated CA Core+ [milestone]
- Fiscal Year 2027
- Advance implementation and adoption [continued]
- Conduct performance evaluation [continued]
Data Portability
- Fiscal Year 2023
- Develop Primary Care Dataset V1 & EMR Extract Specification V1 [milestone]
- Represent Data Portability components in the Canadian Health Data Exchange (CA:FeX) Specification
- Fiscal Year 2024
- Trial Implementation of specifications
- Extend CA Core+ to include other settings (e.g. Acute Care, Mental Health)
- Fiscal Year 2025
- Expand adoption and refinement to include LTC, Community Care and implementation feedback
- Include requirements in national procurements (e.g. Acute Care, LTC, Mental Health, Community Care)
- Fiscal Year 2026
- Expand adoption of Specifications
- Complete specifications [milestone]
- Pan-Canadian vendor compliance service *(Pan-Canadian interoperability compliance testing service in place, vendors conform to pan-Canadian standards in stages.) [vendor input required]
- Conduct performance evaluation
- Fiscal Year 2027
- Expand adoption of Specifications [continued]
- Conduct performance evaluation [continued]
Patient Access
- Fiscal Year 2023
- Assess patient data and access needs across jurisdictions
- Assess the feasibility of IPA standard and decide on Canadian adoption of same
- Fiscal Year 2024
- Co-design patient data access design/Blueprint to represent policy and consent in alignment with IPA
- Implementation and refinement of the Canadian Health Data Exchange Specification to include Patient Access components [milestone]
- Fiscal Year 2025
- Update data exchange specification to support patient Digital Identities
- Expand adoption of Canadian Health Data Exchange Specification
- Fiscal Year 2026
- Develop pan-Canadian guidance documentation for basic digital consent
- Expand adoption of Canadian Health Data Exchange Specification [continued]
- Conduct performance evaluation
- Fiscal Year 2027
- Develop advanced guidance documentation to integrate policy and consent into data access
- Expand adoption of Canadian Health Data Exchange Specification [continued]
- Conduct performance evaluation [continued]
eReferral & eConsult
- Fiscal Year 2023
- Consolidate existing specifications and publish pan-Canadian specification with procurement requirements [milestone]
- Fiscal Year 2024
- Publish conformance requirements for vendors [vendor input required]
- Implementation of pan-Canadian specifications
- Fiscal Year 2025
- Evolve specification to integrate other services (e.g. PS-CA. Provider Directories and Digital Identities)
- Pan-Canadian vendor compliance service *(Pan-Canadian interoperability compliance testing service in place, vendors conform to pan-Canadian standards in stages.) [vendor input required]
- Fiscal Year 2026
- Complete Specification [milestone]
- Conduct performance evaluation [continued]
- Fiscal Year 2027
- Conduct performance evaluation [continued]
Enablers
- Fiscal Years 2023 to 2027
- Governance
- Change Management
- Vendor Mobilization
Data
- Fiscal Year 2023
- p-CHDCF, CA Core+ and Consistent Data Semantics
- Data Matching
- Fiscal Year 2024
- p-CHDCF, CA Core+ and Consistent Data Semantics [continued]
- Data Matching [continued]
- Fiscal Year 2025
- p-CHDCF, CA Core+ and Consistent Data Semantics [continued]
- Data Matching [continued]
- Fiscal Year 2026
- p-CHDCF, CA Core+ and Consistent Data Semantics [continued]
- Fiscal Year 2027
- N/A
Access & Exchange
- Fiscal Year 2023
- Consistent, Secure, HIE Exchange
- Healthcare Directories and Resource Locations
- Fiscal Year 2024
- Consistent, Secure, HIE Exchange [continued]
- Provider Directories
- Digital Identities & Identity Proofing
- Healthcare Directories and Resource Locations [continued]
- Fiscal Year 2025
- Consistent, Secure, HIE Exchange [continued]
- Provider Directories [continued]
- Digital Identities & Identity Proofing [continued]
- Healthcare Directories and Resource Locations [continued]
- Fiscal Year 2026
- Consistent, Secure, HIE Exchange [continued]
- Provider Directories [continued]
- Digital Identities & Identity Proofing [continued]
- Consistent Patient Access
- Healthcare Directories and Resource Locations [continued]
- Fiscal Year 2027
- Consistent, Secure, HIE Exchange [continued]
- Consistent Patient Access [continued]
Trusted Framework
- Fiscal Year 2023
- Jurisdictional Needs Assessment [milestone]
- Scalable Data Sharing Governance Framework
- Industry-wide, Testing and Conformance
- Fiscal Year 2024
- TEF development (contingent on PT support)
- Scalable Data Sharing Governance Framework [continued]
- Industry-wide, Testing and Conformance [continued]
- Fiscal Year 2025
- Consistent Representation of Policy & Consent
- Scalable Data Sharing Governance Framework [continued]
- Industry-wide, Testing and Conformance [continued]
- Fiscal Year 2026
- Consistent Representation of Policy & Consent [continued]
- Scalable Data Sharing Governance Framework [continued]
- Industry-wide, Testing and Conformance [continued]
- Fiscal Year 2027
- Consistent Representation of Policy & Consent [continued]
- Scalable Data Sharing Governance Framework [continued]
- Industry-wide, Testing and Conformance [continued]
Outcomes
- Ability to import/export primary care data to, from and between EMRs
- Clinicians able to change EMRs
- Governance model established
- Vendor support services available to all jurisdictions
- National procurement framework established
- Change management program in place
- 50% of Canadians enabled to directly access their longitudinal record
- 60% of primary care physicians reporting ability to exchange patient summary record
- 70% of clinicians with EMRs enabled to send clinical summaries through a vendor conformed solution
- 75% of Canadians enabled to access their patient summary record
- Benefits realized:
- Health System – $500M in improved interactions, effective use of ED, in-patient services, an reduction in duplicate tests
- Canadians – over $500M in saved patient time
- Clinicians – over $350M in saved time
Annex 3 – Headline common indicators
| Shared health priority area | Indicator |
|---|---|
| Family health services | Percentage of Canadians who report having access to a regular family health team, a family doctor or nurse practitioner, including in rural and remote areas |
| Health workers and backlogs | Size of COVID-19 surgery backlog |
| Net new family physicians, nurses, and nurse practitioners | |
| Mental health and substance use | Median wait times for community mental health and substance use services |
| Percentage of youth aged 12 to 25 with access to integrated youth services (IYS) for mental health and substance use | |
| Percentage of Canadians with a mental disorder who have an unmet mental health care need | |
| Modern health data system | Percentage of Canadians who can access their own comprehensive health record electronically |
| Percentage of family health service providers and other health professionals (e.g., pharmacists, specialists, etc.) who can share patient health information electronically |
Annex 4 – Action plan
I. Context and Current Status
Introduction
Over 14.5 million people are served by Ontario's health care system, which offers a range of publicly funded health services, including family health, surgical care and mental health and addictions. To ensure that these services are delivered faster, more easily, and closer to home, Ontario introduced Your Health: A Plan for Connected and Convenient Care in February 2023.
Under Your Health, Ontario is making record investments under three pillars:
- The right care in the right place;
- Faster access to care; and,
- Hiring more health care workers
New bilateral funding from the federal government's Working Together to Improve Health Care for Canadians plan will support Ontario to deliver connected and convenient care to residents. Ontario will allocate new federal Shared Health Priorities funding across the four shared health priority areas to further bolster the implementation of Your Health initially, over the next three years. This includes innovative actions that will improve access to family health services, grow the health workforce, reduce backlogs, improve mental health and addictions services, and expand access to digital health services.
Federal funding will complement and build on the significant investments that Ontario is making – and will continue to make – to improve the overall health care experience of Ontarians, including Indigenous peoples and underserved groups and individuals, such as those in official language minority communities.
Ontario is committed to ensuring that under-served communities receive equitable health care access, experience, and outcomes. Ontario is working to include supports by identifying and addressing needs for underserved communities, including Indigenous, Francophone, Black and other racialized communities, refugees and individuals experiencing homelessness.
Indigenous communities
Ontario is making investments to improve Indigenous health and wellness through a continuum of delivered programs and services that are culturally appropriate and Indigenous designed. In addition, for the past six years, Ontario has been engaged in First Nations health transformation with First Nations partners and Indigenous Services Canada to support First Nations partners' visions for a health care system that is culturally responsive, effective, and equitable. Ontario is also working to address anti-Indigenous racism in the health system by investing in regional and local Indigenous cultural safety training and other cultural safety initiatives (e.g., cultural safety and trauma-informed care trainings for health professionals, improved health navigation services).
It is important that trilateral processes and new federal investments are responsive to priority areas identified by First Nations partners and allow for detailed health planning conversations with tangible outcomes that align with jurisdictional roles and responsibilities.
Francophone communities
Ontario is working to address the challenges faced by the increasingly diverse Francophone populations in accessing French Language Health Services. For example, Ontario is working to increase French Language Health Services human resource capacity, improve data collection, and expand French Language communications capacity and engagement. These equity efforts aim to not only enhance access to quality French Language Health Services for Francophones in Ontario, but to also ensure compliance with the French Language Services Act.
Racialized and other under-served communities
Ontario supports improved health care access, experience, and outcomes for under-served communities. For example, the High Priority Communities Strategy provided resources to support barrier-free health services via community ambassadors and partnerships.
II. Shared Health Priorities and description of initiatives
Family health services
Primary care and family health services are funded by the government of Ontario and are provided to Ontarians by family physicians nurse practitioners, interprofessional primary care teams and other allied health care providers. From 2021 to 2022, 89.9% per cent of Ontario's adults were attached to a primary care provider (a family physician or nurse practitioner). Although Ontario leads the country in the number of people who benefit from a long-term, stable relationship with a family doctor or primary care provider, like other Canadian and international jurisdictions, there is an increasing need for Ontarians to be connected to additional interprofessional primary care teams and improve access to comprehensive primary care services.
Ontario is developing and implementing new initiatives that will help connect more people to interprofessional primary care teams without having to visit emergency rooms and experience long wait times, especially in communities with the greatest need. This includes expanding access to team-based models of care to meet patient needs which will be supported through additional federal funding. These teams will help bridge the gap in accessing care offered by several health care providers, including physicians, mental health workers, and social workers.
As captured in the Health Workers and Backlog section of this Action Plan, Ontario is also implementing several initiatives to bolster the supply of health workers, including primary care and family physicians. These initiatives include:
- Programs through Ontario Health, the crown agency that helps communities with recruitment and retention and promotes career opportunities in places that need physicians.
- The Northern Ontario School of Medicine University which trains medical students and residents throughout Northern Ontario
- Distributed medical education programs, which provide clinical education opportunities outside of traditional settings to promote physician practice in rural and northern communities
- The Northern and Rural Recruitment and Retention Initiative, which offers financial incentives for physicians to establish practice in rural and Northern Ontario
In implementing these initiatives, and with the help of new federal funding, the quality of health care delivered across the province will be improved for years to come.
Initiatives to be supported by the federal Shared Health Priorities funding:
Expanding interprofessional primary care teams
Ontario will invest $90M from 2023-2026 ($30M per year) to create more interprofessional primary care teams; expand existing teams in communities with greatest needs; and assist existing teams that have increasing operational costs.
These care teams include members from two or more professions, such as physicians, nurses, including nurse practitioners, social workers, mental health workers, and other health care professionals and will offer care to communities that include vulnerable, marginalized, and patients without a regular source of primary care (a physician or nurse practitioner). With more interprofessional primary care teams, patients will be provided with access to comprehensive and timely care and can avoid visiting emergency rooms and experiencing long-wait times. These teams will also help improve patients' continuity of care and health outcomes, by providing them with access to preventive care and screening procedures.
Ontario will also be investing $12.75M from 2023-2026 ($4.25M per year) towards additional activities that address anti-Indigenous racism in the health system through training, education, and capacity-building and that enhance health teams' skills and capacity to deliver culturally safe care to Indigenous patients.
Health workers and backlogs
Ontario's population is projected to increase by almost 15 per cent over the next 10 years. The population of seniors aged 75 and older is expected to increase by 49.3 per cent, from 1.2 million to 1.8 million over the same period. Ontario is committed to increasing our health care workforce to meet the needs of our growing population and ensure the continued delivery of high-quality care to the people of Ontario.
Your Health: A Plan for Connected and Convenient Care is focused on hiring and training more health care professionals. To achieve the objectives of Your Health Plan, Ontario is working with sector partners to implement a comprehensive, multi-faceted health human resources strategy focused on increasing the size of the workforce through education expansion, increasing pathways for internationally educated providers as well as programs to support the retention of our health workforce and reduce attrition and burnout, leveraging available federal funding. One component of the retention strategy is having access to mental health supports. In 2021-22 and 2022-23, the Government of Ontario invested in existing and expanded mental health and addictions supports for healthcare workers whose mental health has been adversely impacted by COVID-19 and workplace and occupational stress. With new federal funding, -Your Health will be bolstered to address key professions of need across the health system, while tackling short, medium and long-term issues to ensure a robust health workforce for the people of Ontario.
Ontario is also making innovative change to make it easier and faster for health care workers registered in other jurisdictions to begin working and providing care to people in Ontario. With new "As of Right" rules, Ontario is leading jurisdictional efforts to allow health care workers registered in other provinces and territories to immediately start providing care, without having to first register with one of Ontario's health regulatory colleges. This change will help Canadian health care workers overcome excessive red tape that makes it difficult for them to practice in Ontario.
Initiatives to be supported by the federal Shared Health Priorities funding:
Ontario will invest approximately $476M from 2023-2026 to support these additional health human resources initiatives which improve access to care across the health system, including in underserviced areas of the province:
Supporting internationally educated health professionals ($69M per year)
- The Supervised Practice Experience Program to extend the Internationally Educated Nurses Supervised Practice Experience Program, which offers internationally trained nurses the opportunity to undertake a supervised practice experience to demonstrate current nursing knowledge while allowing them to meet their evidence of practice and/or language proficiency requirements to enter practice as a nurse.
- Reimbursing inactive and internationally educated nurses for registration fees and the development of a centralized site for internationally educated health professionals to help streamline access to registration in Ontario.
- Launch of the Physician Practice Ready Assessment Program, which will help internationally educated physicians, with previous medical practice experience, undergo screening and assessment to determine if they can enter practice in Ontario immediately without having to complete re-education programs.
Recruitment ($40M per year)
- Expanding medical school education by adding 260 undergraduate seats and 449 postgraduate positions in the province over the next five years to increase access to family and specialty-physicians and other health care professionals. Of the 449 new postgraduate positions, 60 per cent will be dedicated to family medicine and 40 per cent will be dedicated to specialty programs.
- The Northern Ontario School of Medicine will receive 30 undergraduate seats and 41 post-graduate positions to support northern communities and the Ontario First Nation Residency Program.
- Nursing Enrolment Expansion to help increase Ontario's nursing supply and reduce shortages.
- Supports for upskilling nurses, respiratory therapists and other health care professionals to work in priority clinical areas of need, such as critical care and emergency nursing.
- An additional 150 permanent education seats in the Primary Health Care Nurse Practitioner program starting in 2023-24 to increase the supply of nurse practitioners in primary care settings.
Retention/innovation ($49M per year)
- Models of Care Innovation Fund to support individual hospitals, long-term care homes, home care providers and Ontario Health Teams in finding innovative ways of maximizing the skills and expertise of their current health care workers in order to mitigate HHR shortages, reduce burnout, increase capacity and improve access to care. For example, projects can include allowing health care providers to work to the full scope of their abilities and innovative 9-1-1 models of care.
- Expanding the Ontario Learn and Stay Grant to address unique health care challenges in small, rural, and remote communities, by providing financial support to post-secondary students who enroll in high-priority programs in growing and underserved communities.
Your Health: A Plan for Connected and Convenient Care is focused on providing faster access to care and reducing wait times for surgeries and procedures, which is a challenge that Ontarians have been facing. Ontario leads the country in the number of people who receive hip and knee replacements, but more needs to be done. For this reason, Ontario will be making it easier and faster to get the publicly funded surgeries and procedures leveraging the support of community surgical and diagnostic centres. Legislation introduced in February 2023 will allow existing community diagnostic centres to conduct more MRI and CT scans to increase access to publicly funded diagnostic services faster and closer to home, as is consistent with the Canada Health Act.
- Starting in 2024, this initiative will also expand hip and knee replacement surgeries
- These facilities will work with local public hospitals to ensure health system integration and linkages, including connecting and reporting into Ontario's wait times information system and participation in regional central intakes, where available
Initiatives to be supported by the federal Shared Health Priorities funding:
Ontario will also be investing $1,246.5M from 2023-2026 to increase surgical and diagnostic capacity in communities and hospitals and reduce wait times. Investments will include:
Increasing surgical and diagnostic capacity (communities) ($125M per year)
- Support the continuation of the Surgical Recovery Strategy to return surgical and diagnostic imaging wait times back to pre-pandemic levels.
- Support hospitals to increase surgical volumes and MRI/CT operating hours.
- Support regional innovation and efficiency projects to help increase surgical capacity and address long-waiters.
- Funding growth needs to support the aging population and support system enhancements to adapt programs to meet patient care needs.
Increasing hospital surgical capacity/growth ($290.5M per year)
- Support growth volumes in lung, colorectal, and breast cancer screening programs. This includes increased access to FIT kits in First Nations Communities and the expansion of trailer-based mobile health services in Northern Ontario to reduce barriers associated with preventative cancer screening services.
Mental health and addictions
Every year, more than one million people in Ontario experience a mental health or addictions (MHA) challenge, which can have a serious impact on their quality of life, including the ability to go to school or make a living.
Supporting the mental health and well-being of all Ontarians is a key priority under Your Health, which focuses on improving access to MHA services and builds on successful integrated models of care. This includes 9-1-1 patient care models that enable paramedics to treat patients on scene and refer or discharge them to supports in the community, to help avoid unnecessary emergency department visits. Mental health is also integrated with the broader health and community sectors through Ontario Health Teams, which bring together health care providers across these sectors to better coordinate care and share resources.
In 2020, Ontario released Roadmap to Wellness, a plan to build a world-class MHA system. Supported by a commitment to invest $3.8 billion over ten years, the Roadmap to Wellness is adding capacity to meet demand, filling gaps in the care continuum, and creating a provincial infrastructure for an MHA continuum of care that connects community, primary and acute care to better wrap around the needs of people with MHA issues.
Roadmap to Wellness is a plan to fix these longstanding challenges, based on four pillars:
- Improving quality;
- Expanding existing services;
- Implementing innovative solutions; and,
- Improving access.
Since launching the Roadmap to Wellness, Ontario has invested $525M in new base funding annually to help MHA services expand to increase access to care and reduce wait times.
Previous federal investments and collaboration through the 2017 Common Statement of Principles on Shared Health Priorities have strengthened access to quality MHA in Ontario.
2017 Common Statement of Principles on Shared Health Priorities
With the remaining 4 years of funding for MHA services associated with the 2017 Common Statement of Principles on Shared Health Priorities (CSOP), Ontario is continuing to invest federal funds in the following MHA initiatives:
Child and Youth Community-Based MHA Services
Reduce the barriers that children and youth face in accessing early intervention and prevention MHA supports with investments in:
- Child and youth supports to reduce MHA services, wait times, and wait lists.
- Developmentally appropriate withdrawal management services for youth.
- Resources to children and youth to access services remotely to avoid escalating into crisis through tele-mental health and other virtual services including One Stop Talk.
- Innovative solutions to support mental health and well-being of children and youth through the Step-Up-Step-Down live-in treatment program and the Complex Transition Fund.
- An Eating Disorders Early Intervention Program.
- Funding for post-secondary mental health supports.
- Expanding early identification and assessment tools for students.
- Integrated services for youth through Youth Wellness Hubs.
Community-based core MHA services
Continue to support the expansion of services to fill critical service gaps across the lifespan, with investments in:
- Access to psychotherapy and counseling support programs.
- Addiction services for adults, focusing on opioid, alcohol, and cannabis addictions substance use.
- Access to the early psychosis intervention programs.
- Programs for priority populations, particularly racialized, immigrant, refugee, French- speaking and LGBTQ2S populations.
- Access to specialized eating disorders services.
- Indigenous community MHA services.
Integrated community-based MHA services for people with complex needs
- Continue to provide services that address complex mental health needs, including those struggling with poverty, homelessness, dual diagnosis, and involvement in the criminal justice system and expand the availability and support access to integrated community MHA services, including programs such as:
- The Mobile Crisis Rapid Response and supportive housing units; and,
- Affordable housing and support services to individuals who have MHA and are designated alternate level of care in hospitals.
Initiatives to be supported by the federal Shared Health Priorities funding:
In addition to federal funding received from the 2017 Common Statement of Principles on Shared Health Priorities, Ontario will be investing approximately $596M from 2023-2026 to build on Ontario's investments to address mental health and addictions. These investments will include:
- Funding for community MHA programming ($97M per year) These investments will support a broad range of activities across the care continuum including:
- Depression, Anxiety, and Anxiety-Related Disorder support- Supporting the continued rollout of the Ontario Structured Psychotherapy Program that provides evidence-based psychotherapy; support will include the provision of service in French.
- Data Digital Initiative- Ongoing implementation of the mental health and addictions provincial data standard, investing in data infrastructure, and building an MHA provincial coordinated access system to support increased access to the right care in the right place.
- Indigenous MHA Services and Supports- Funding to support Indigenous care and services in target communities, including during social emergencies.
- Funding for MHA programming and supporting needs across the continuum of care including child and youth mental health, community MHA, supportive housing and mental health and justice ($93.3M per year).
- Indigenous MHA Programming ($8.3M per year), which includes: expansion of the Regional Social Emergency Manager Program which will build social emergency capacity at the regional level, in crisis prevention, mitigation, preparedness, response, and recovery.
- This programming also includes support for the Indian Residential Schools Burials Funding Program that will provide culturally appropriate, trauma- informed MHA and wellness supports throughout an Indigenous-led process to identify, investigate, protect, and commemorate burials at the sites of the 18 former Indian Residential Schools recognized in the federal Indian Residential School Settlement Act.
Modern health data system
As a leader in digital health and data, Ontario has been actively delivering on its commitment to provide better and more connected digital services for Ontario's front-line providers and patients. Ontario introduced its Digital First for Health strategy to streamline and interconnect digital health systems across the province and give patients and providers access to online tools and services. As part of this strategy, Ontario is also providing patients with more virtual care options to access health care services.
Ontario is also working towards expanding patient access to online appointment booking and increasing data access for patients, enabling them to access their secure health record online and make informed choices about their care. Nearly all Ontarians who receive health services now benefit from digital records and other provincial digital health assets containing information that can be accessed by authorized clinicians.
To modernize the patient experience, Ontario will allocate new federal funds for digital tools to build on work to give providers access to patient records stored across multiple health organizations.
Ontario also recognizes the opportunity to increase access to health data to improve population health and drive innovation through the appropriate regulations, policies, and platforms. As part of the provincial COVID-19 response, Ontario launched the Ontario Health Data Platform COVID- 19, which links large health data sets held across various organizations for research and analysis. In addition, in July 2021, Ontario launched the Ontario Health Data Council (OHDC) to advise the Minister of Health on the strategic management of Ontario's health data to foster a person-centered learning health system. OHDC released its report – A Vision for Ontario's Health Data Ecosystem in November 2022 outlining data's ability to improve health care.
Initiatives to be supported by the federal Shared Health Priorities funding:
Ontario will be investing $88M from 2023-2026 ($29M per year) to modernize and expand provincial electronic health records, including medication records over the next few years. This modernization will enable future investment opportunities that can enable health care providers to access more patient health information, such as primary care referrals, drug and pharmacy data, and MHA data, to support integrated patient care.
Through this investment, Ontario health care providers will also be supported in moving onto existing digital alternatives and cutting-edge tools instead of relying on fax machines. By transitioning to faster and easier ways of communication, providers will be able to minimize risks associated with delaying diagnosis; face reduced administrative burdens; and promote safer patient care and more patient privacy.
Indigenous partners such as the Indigenous Primary Care Council are being consulted to ensure that digital initiatives are addressing the needs of Indigenous people.
III. Funding allocation
| Initiative | Incremental Investments ($M) | Total | ||
|---|---|---|---|---|
| 2023-24 | 2024-25Footnote * | 2025-26Footnote * | ||
| Family health services | ||||
| Expanding Interprofessional Teams | $30.000 | $30.000 | $30.000 | $90.000 |
| Indigenous Health | $4.250 | $4.250 | $4.250 | $12.75 |
| Total | $34.250 | $34.250 | 34.250 | $102.750 |
| Health workforce and backlogs | ||||
| Supporting internationally educated health professionals (Supervised practice experience program, Supporting internationally educated health professionals, Physician practice ready assessment program) | $69.300 | $69.300 | $69.300 | $207.900 |
| Recruitment (Medical school expansion, Nursing enrolment expansion, Primary health care nurse practitioner program expansion) | $40.000 | $40.000 | $40.000 | $120.000 |
| Retention/innovation (Models of Care Innovation Fund, Nursing upskilling, Ontario Learn and Stay Grant) | $49.300 | $49.300 | $49.300 | $147.900 |
| Increasing surgical and diagnostic capacity (communities) (Surgical recovery strategy; Increasing surgical volumes and MRI/CT hours; Regional innovation projects; Growth needs for aging populations; System enhancements) | $125.000 | $125.000 | $125.000 | $375.000 |
| Increased hospital surgical capacity/growth (Waitlist improvements for key procedures; cancer screening programs) | $290.510 | $290.510 | $290.510 | $871.530 |
| Total | $574.11 | $574.11 | $574.11 | $1,722.33 |
| Mental health and addictions | ||||
| Community MHA programming | $97.000 | $97.000 | $97.000 | $291.000 |
| MHA programming and supporting needs across the care continuum | $93.310 | $93.310 | $93.310 | $279.930 |
| Indigenous MHA programming (Regional Social Emergency Manager Program, Indian Residential Schools Burials Funding Program) | $8.325 | $8.325 | $8.325 | $24.975 |
| Total | $198.635 | $198.635 | $198.635 | $595.905 |
| Modernizing health systems | ||||
| Modernizing and expanding provincial electronic health records | $29.250 | $29.250 | $29.250 | $87.750 |
| Total | $836.245 | $836.245 | $836.245 | $2,508.735 |
|
||||
| Initiatives | Investments ($M) | ||||
|---|---|---|---|---|---|
| 2023-24 | 2024-25 | 2025-26 | 2026-27 | Total | |
| Child and youth community-based MHA services | $75.045 | $75.045 | $75.045 | $75.045 | $300.180 |
| Community-based core MHA services | $78.925 | $78.925 | $78.925 | $78.925 | $315.700 |
| Integrated community-based MHA services for people with complex needs | $78.624 | $78.624 | $78.624 | $78.624 | $314.496 |
| Totals | $232.594 | $232.594 | $232.594 | $232.594 | $931.76 |
IV. Measuring and reporting on results
Ontario looks forward to measuring the progress that will be made across the four shared health priority areas through this investment of new federal funding and demonstrating this progress to Ontarians through annual reporting. As we continue to roll out Your Health, this will include tracking access to services such as primary care and MHA services, as well as wait times for MRI and CT scans, and how Ontario is expanding our health care workforce to ensure it grows as our population in Ontario grows and ages. This Action Plan includes Ontario specific indicators and targets for these priority areas.
Additionally, Ontario is working with Health Canada, the Canadian Institute for Health Information and other provinces and territories to develop common headline indicators that are reported across all provinces and territories. Work is still underway to finalize these common headline indicators, as such, the indicators included below for Ontario are still draft and in development. Ontario looks forward to continuing working alongside Health Canada, the Canadian Institute for Health Information and other provinces and territories to update and refine these indicators.
Targets and timeframes
Please note, all of the common headline indicators listed below reflect the indicators and baseline figures published by the Canadian Institute for Health Information in its August 2, 2023 report: "Taking the pulse: A snapshot of Canadian health care, 2023' (available on cihi.ca)
| Indicator | Baseline | Target and timeframe 2023-2026Footnote 1 | |
|---|---|---|---|
| Target | Timeframe | ||
| Family health services | |||
| Headline Indicator | |||
| Percentage of Ontarians who report having access to a regular family health team, a family doctor or nurse practitioner, including in rural and remote areas | 90% | 91% | By March 2026 |
| Ontario-specific Indicators | |||
| Number of new and expanded interprofessional primary care teams | 302 | 320 | Funding will be used to maintain the 18 new and expanded teams in 2024-25, 2025-2026 |
| Health workers and backlogs | |||
| Headline Indicator | |||
| Size of COVID-19 surgery backlogFootnote 2 | -15% | 0%Footnote 3 | CompleteFootnote 2 |
| Net new family physicians, nurses, and nurse practitionersFootnote 4 | 2021 Supply: FP: 12 per 10,000 (17,220) NP: 3 per 10,000 (3861) RN: 72 per 10,000 (106,595) | Additional Headcounts: FP: +200 NP: +200 RN: +1,000 | Average Annual Growth Rates |
| Ontario-specific Indicators | |||
| Patients on wait list receiving surgeries within acceptable wait timesFootnote 5 | 131, 000 on March 31, 2023 | 150,000 | March 31, 2026 |
| Number of new nurses and physicians that are internationally educated | 3,055 international nurses and 1,052 international physicians | 3,000 international nurses and 500 international physiciansFootnote 6 | March 2026 |
| Mental health and addictions | |||
| Headline Indicators | |||
| Median wait times for community mental health and substance use services | n/aFootnote 7 | Adult: 103 daysFootnote 8 Child and Youth Mental Health: 62 daysFootnote 9 | Adult: March 2024 Child and Youth Mental Health: March 2024 |
| Percentage of youth aged 12 to 25 with access to integrated youth services (IYS) for mental health and substance useFootnote 10 | 22 active IYS active sitesFootnote 11 (in Total) 8 active IYS sites under development | 27 active IYS sitesFootnote 12 | March 2025 |
| Percentage of Canadians with a mental disorder who have an unmet mental health care need | 7%Footnote 13 | n/aFootnote 14 | March 2025 |
| Ontario-specific Indicators | |||
| New clients enrolled in the Ontario Structured Psychotherapy (OSP) program | 12, 281 as of March 2023 | 17, 100 | March 2026 |
| Modern health data system | |||
| Headline IndicatorsFootnote 15 | |||
| Percentage of Ontarians who can access their own comprehensive health record electronicallyFootnote 16 | 35% | 40% | March 2026 |
| Percentage of family health service providers and other health professionals (e.g., pharmacists, specialists, etc.) who can share patient health information electronicallyFootnote 17 | 44% | 49% | March 2026 |
| Ontario-specific Indicators | |||
| Number of sending clinicians participating in eReferral through the provincial eServices program | 7, 500 as of March 31, 2023 | 11,000 | March 2026 |
References:
- Footnote 1
-
As noted above, Ontario continues to work with the Canadian Institute for Health Information to refine the common headline indicators, targets and timeframes. As such, these indicators and targets are subject to change and will be updated accordingly.
- Footnote 2
-
As noted in the Canadian Institute for Health Information's August 2, 2023 Snapshot Report, this indicator measures the estimated percentage change in number of surgeries done monthly between March 2020 and September 2022, compared with 2019.
- Footnote 3
-
Baseline reporting is from the Canadian Institute for Health Information's August 2, 2023 Snapshot Report and is not a metric that Ontario uses given that it does not measure the impact of COVID-19 on surgical performance. Ontario uses the Wait Times Information System (WTIS) and tracks the percentage of surgical cases completed within benchmark wait times, which is at 79% as of October 1, 2023, up from 73% in 2022.
- Footnote 4
-
The following indicator is a Canadian Institute for Health Information measure of the supply of family physicians, nurses, and nurse practitioners in 2021.
- Footnote 5
-
This data is from Ontario's Wait Times Information System (WTIS). Patients with emergency conditions (Priority 1) are seen immediately and are not included in wait times data. Priority levels 2, 3, and 4 are determined by surgeons, specialists, and other health care providers, based on clinical evidence, to guide treatment decisions and improve patient access and outcomes.
- Footnote 6
-
These are annual new additions to the workforce up until March 2026 (i.e. not net growth).
- Footnote 7
-
Baseline not available due to insufficient CIHI data coverage.
- Footnote 8
-
Adult targets are based on high intensity counselling services delivered through the Ontario Structured Psychotherapy Program (OSP) and excludes Bounceback (which the Canadian Institute for Health Information previously excluded from their counselling wait time definition) and clinician assisted bibliotherapy.
- Footnote 9
-
Child and Youth Mental Health (CYMH) projections align with 2022-23 median wait times for counselling services. Please note that counselling used given this was the previous definition for this indicator.
- Footnote 10
-
As noted in the Canadian Institute for Health Information's August 2, 2023 Snapshot Report, this indicator measures the type and number of IYS sites.
- Footnote 11
-
Please note that these 22 active IYS sites listed include the 8 IYS sites under continued development (i.e. not mutually exclusive).
- Footnote 12
-
Projections based on five IYS sites approved through the paediatric fund being fully up and running by end of next fiscal. Please note that targets will be achieved by March 2025 and sustained thereafter.
- Footnote 13
-
This data, while reported in 2023, is taken from the 2018 Canadian Community Health Survey — Annual Component and there is more recent data in "A Mental Health and Access to Care Survey, 2022" released 2023 which shows 10.7% unmet needs for Canadians.
- Footnote 14
-
Data are taken from Statistics Canada, Canadian Community Health Survey (CCHS), 2024. Baseline value was established using the best data available at the time; however, the indicator methodology and data source have since changed, meaning current results are not comparable to those baselines. Target not set as data became available in 2025.
- Footnote 15
-
The Ontario Ministry of Health prefers to track indicators in numeric values rather than in percentages, due to difficulty in determining an accurate denominator.
- Footnote 16
-
The Ontario Ministry of Health tracks the number and percentage of people registered to access their provincial health records through patient portals (myUHN, myChart, etc).
- Footnote 17
-
The Ontario Ministry of Health tracks the number of front line providers with access to provincially-held integrated health records.