Canadian Alcohol and Drugs Survey (CADS): summary of results for 2019
Table of contents
Introduction
Understanding Canadian trends in alcohol and drug use is vital to the effective development, implementation and evaluation of national and provincial strategies, policies and programs.
The Canadian Alcohol and Drugs Survey (CADS) is a biennial general population survey of alcohol and drug use among Canadians aged 15 years and older. CADS is conducted by Health Canada, in partnership with Statistics Canada for data collection. CADS evolved from the Canadian Tobacco, Alcohol and Drugs Survey (CTADS), which was conducted biennially from 2013 to 2017, whereupon Health Canada decided to separate CTADS into two surveys: CADS, focused on alcohol and drug surveillance, and the Canadian Tobacco and Nicotine Survey (CTNS), focused on tobacco use and vaping.
The following summary presents findings based on the first biennial CADS data collection, which commenced in June 2019 and ended in December 2019. The results for 2019 are based on telephone interviews with 10,293 respondents across all 10 provinces, representing a weighted total of 31 million Canadian residents aged 15 years and older (15.3 million males and 15.7 million females). A set of detailed tables and some definitions of terms used in this report are also provided.
All reported increases, decreases, and "differences" in the text below are statistically significant changes at the p≤0.05 level. The words "statistically significant" will not be used to allow for more readable text. "Unchanged" refers to differences that are not statistically significant.
Please note that where data are reported for consuming a substance in the past year, this refers to having consumed the substance in question at least once in the 12 months preceding the date of the survey.
Please note that where numbers of individuals are provided along with prevalence, these numbers are estimates.
Alcohol
Respondents were asked about alcohol use, including questions examining the quantity of alcohol consumed, alcohol-related harms, alcohol use during pregnancy, and alcohol impaired driving.
Prevalence of Alcohol Use
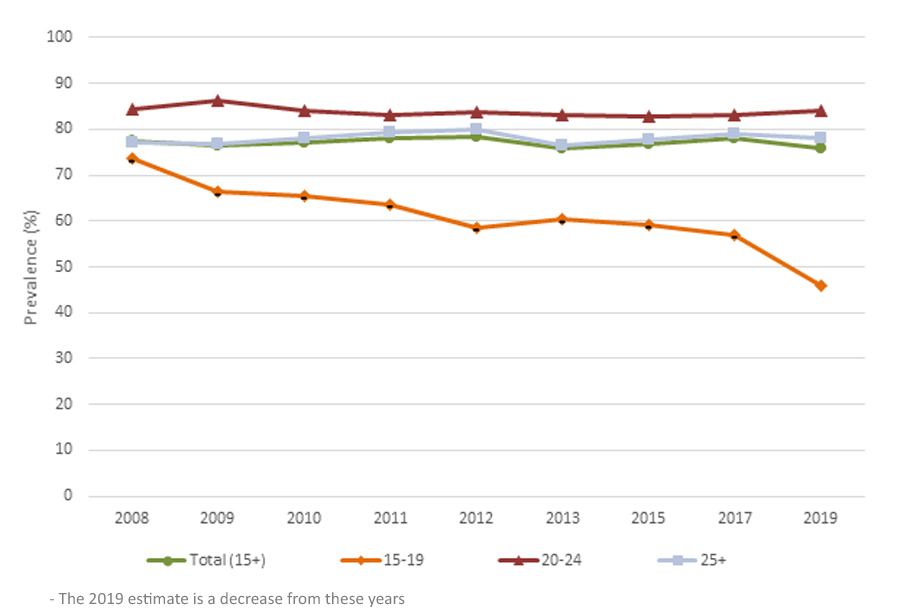
In 2019, three-quarters (76% or 23.7 million) of Canadians reported consuming an alcoholic beverage in the past year, unchanged from 78% (23.3 million) in 2017. Males were more likely than females to report past-year alcohol use (78% or 12 million males and 75% or 11.7 million females), and both were unchanged from 2017 (79% or 11.6 million for males and 77% or 11.6 million for females). The prevalence of past-year alcohol use was higher among young adults aged 20 to 24 (84%) and adults aged 25 years and older (78%) than among youth aged 15 to 19 (46%). The prevalence of past-year alcohol use among youth aged 15 to 19 decreased from 2017 (57%), whereas there was no change among young adults aged 20 to 24 and adults aged 25 years and older. For more details on long-term trends in past year alcohol use, see Table 1.
Table 1: Past-year alcohol use, Canada 2008–2019Footnote *
Provincial prevalence of alcohol use in the past year ranged from 74% in Ontario (or 9 million Ontario residents) to 81% in Quebec (or 5.7 million Quebec residents) (see Table 2 for more details). For all provinces, the prevalence of alcohol use remains unchanged compared to 2017.
Table 2: Past-year alcohol use, by province, 2013–2019Footnote *

Low-Risk Alcohol Use
Canada's Low-Risk Alcohol Drinking Guidelines (LRDG) consists of five guidelines and a series of tips. Guidelines 1 and 2, and acute and chronic effects are explained in the definitions section. People who drink within the low-risk alcohol drinking guidelines consume no more than the recommended quantity of alcohol within the number of days specified, whereas those who exceed the guidelines consume more alcohol than recommended within the stated timeframe. The basis of the LRDG is reported alcohol consumption in the seven days prior to the survey.
Among Canadians who consumed alcohol in the past year, 23% (representing 18% of the population aged 15 years and older or 5.4 million) exceeded guideline 1 for chronic effects and 17% (representing 13% of the population aged 15 years and older or 4 million) exceeded guideline 2 for acute effects. A higher percentage of males than females drank in patterns that exceeded guideline 2 for acute effects, while there was no difference in percentage of male drinkers and female drinkers who reported drinking in patterns that exceeded guideline 1 for chronic effects. The acute-risk guideline was exceeded by 19% (or 2.3 million) of male drinkers and 15% (or 1.8 million) of female drinkers. The chronic-risk guideline was exceeded by 24% (or 2.9 million) of males who drank and 22% (or 2.5 million) of females who drank. For more detail on the prevalence of Canadians exceeding the LRDG for chronic and acute effects since 2008, see Table 3.
Table 3: Exceeding Low Risk Drinking Guidelines, Canada 2008–2019Footnote *
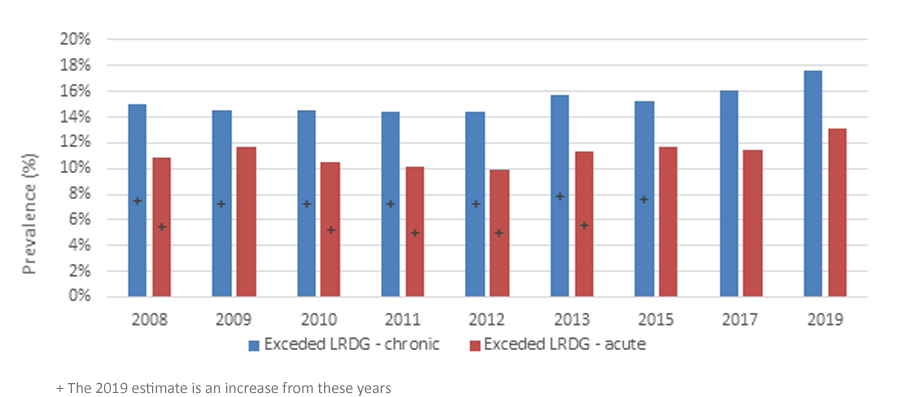
The chronic-risk guideline was exceeded by young adult drinkers aged 20 to 24 at a higher percentage than among adult drinkers aged 25 years and older, while the acute-risk guideline was exceeded by young adult drinkers aged 20 to 24 at a higher percentage than among youth drinkers aged 15 to 19 and adult drinkers aged 25 or older. The guideline for chronic risk was exceeded by 31% (594,000) of young adult drinkers aged 20 to 24 compared to 23% (229,000) of youth drinkers aged 15 to 19 and 22% (4.6 million) of adult drinkers aged 25 years and older. The acute-risk guideline was exceeded by 26% (494,000) of young adult drinkers aged 20 to 24 compared to 13% (127,000) of youth drinkers aged 15 to 19 and 17% (3.4 million) of adult drinkers aged 25 years and older.
The prevalence estimates for risky alcohol consumption are unchanged from 2017, except for exceeding guideline 2 for acute effects among those who consumed alcohol in the past year, where the prevalence increased from 15% (or 3.3 million) in 2017.
Alcohol-related harms
In 2019, for the first time, the survey asked about five harms people may have experienced in the past 12 months due to alcohol consumption. Types of harm include being unable to stop drinking once started, failing to do what was normally expected from you because of drinking, needing a first drink in the morning to get yourself going after a heavy drinking session, being unable to remember what happened the night before because of your drinking, or having a feeling of guilt or remorse after drinking.
Of those who reported past-year alcohol use, 21% (4.8 million) experienced at least one alcohol-related harm in the past year due to alcohol use. There was no difference in the prevalence of reported harm in the past year due to alcohol consumption between male drinkers (21% or 2.5 million) and female drinkers (20 % or 2.3 million). A higher proportion of young adults aged 20 to 24 (40% or 758,000) and youth aged 15 to 19 (38% or 378,000) reported harm due to alcohol use in the past year than adults aged 25 years and older (18% or 3.7 million).
Maternal experience with alcohol consumption
Females aged 15 to 44 years who gave birth in last five years and who ever had a drink of alcohol were asked if they drank alcohol during their last pregnancy. Just under one in five (18% or 210,000) reported drinking alcohol during their last pregnancy. The results are for females aged 25 to 44 years; there were no observations for consuming alcohol during pregnancy among youth females aged 15 to 19 and young females aged 20 to 24.
Alcohol impaired driving
Also new to CADS in 2019, respondents were asked to indicate if they had ever been a passenger in a car driven by someone who consumed two (2) or more alcoholic drinks in the previous two (2) hours or if they had ever driven after consuming two (2) or more drinks in the previous two (2) hours.
Among Canadians who consumed alcohol in the past year, 8% (or 1.8 million) reported being a passenger in a vehicle driven by someone who had consumed alcohol in the past 2 hours, which was higher than among those who did not consume alcohol in the past year (2% or 140,000). There was no difference in the prevalence of this behaviour between males (8% or 859,000) and females (9% or 988,000) who consumed alcohol in the past year.
Among Canadians who reported consuming alcohol in the past year, 6% (1.3 million) reported that they had driven within two hours of drinking two (2) or more drinks. Males were more likely than females to report driving within 2 hours of drinking alcohol (9% or 983,000 vs. 4% or 351,000, respectively). Adults aged 25 years or older were more likely than young adults aged 20 to 24 to report driving within 2 hours of drinking alcohol (7% or 1.3 million vs. 3% or 41,000). The prevalence of driving after drinking among youth aged 15 to 19 was not reportable due to small sample size.
Drug Use
The survey asked about past-year and lifetime use of cannabis, psychoactive pharmaceuticals, and illegal drugs including cocaine or crack, ecstasy, speed or methamphetamines, hallucinogens, heroin, and others.
Cannabis Use
Cannabis was legalized and regulated in 2018, and has remained the most used drug in Canada.
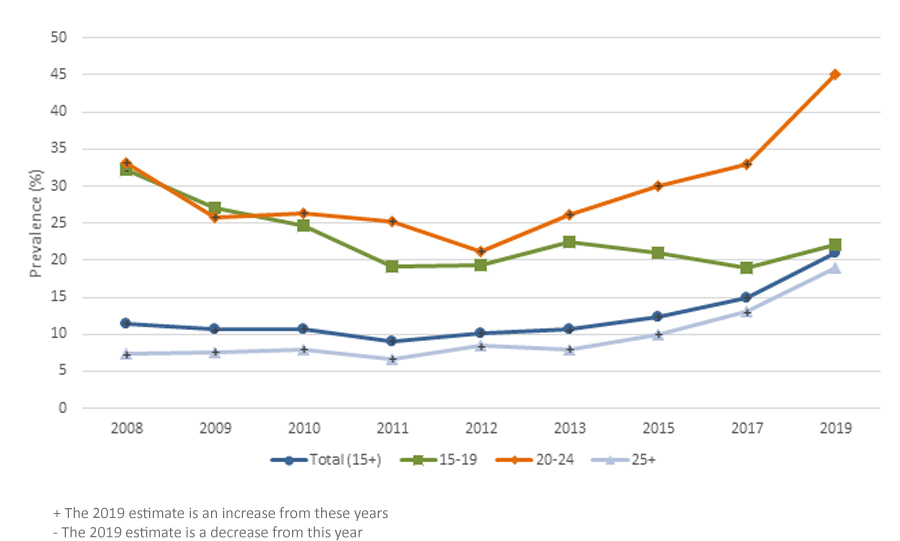
In 2019, the prevalence of past-year cannabis use (for medical or non-medical purposes) was 21% (6.4 million), an increase compared to 2017 (15% or 4.4 million), and compared to 2015 (12% or 3.6 million). In 2019, past-year cannabis use was more prevalent among males (23% or 3.5 million) than females (19% or 2.9 million), which is consistent with previous cycles. The prevalence of past-year cannabis use among males and females increased from 2017 (19% and 11%, respectively). Table 4 presents past-year cannabis use among Canadians since 2008.
Table 4: Past-year cannabis use, Canada 2008–2019Footnote *
Provincial prevalence of past-year cannabis use ranged from 18% (1.2 million) in Quebec to 33% (269,000) in Nova Scotia. Table 5 presents cannabis use by province since 2013.
Table 5: Past-year cannabis use by province, 2013–2019Footnote *

Past-year use of cannabis was more prevalent among young adults aged 20 to 24 (45% or 1 million) than among youth aged 15 to 19 (22% or 468,000) and adults aged 25 years and older (19% or 4.9 million). Past-year use of cannabis among young adults aged 20 to 24 and adults aged 25 years and older increased from 2017 (33% and 13%, respectively), whereas there was no change among youth aged 15 to 19 (19%). The mean age of initiating use of cannabis was 19 years old for both males and females, unchanged from 2017 (18 years for males and 19 years for females).
Among people who have used cannabis in the past year, 36% (or 2.3 million) reported using it for medical purposes, unchanged from 2017 (37% or 1.6 million). Canadians reported using cannabis for medical reasons to treat a variety of conditions. The main medical conditions for which Canadians used cannabis for medical purposes were anxiety (33% or 641,000), arthritis (21% or 416,000), depression (8% or 156,000), and other medical conditions (32% or 623,000). Canadians also reported using cannabis for the following medical conditions: spinal cord injuries, irritable bowel syndrome or other inflammatory bowel disease, post-traumatic stress disorder, and multiple sclerosis (all 2% or under). The survey does not collect information on how people obtained the cannabis for medical purposes.
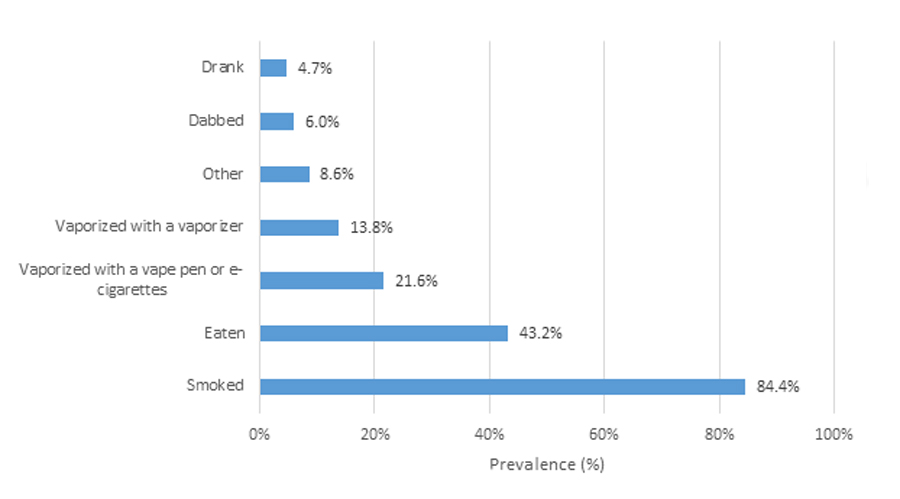
Of the methods used to consume cannabis in the past 12 months, smoking was the most common. Eighty-four percent (84% or 5.2 million) of those who used cannabis in the past year smoked cannabis. Other common methods of consumption among those who used cannabis in the past year include consuming cannabis in edibles (brownies, etc. — 43% or 2.7 million), through a vape pen or e-cigarette (22% or 1.3 million), and vaporizing it with a vaporizer (14% or 852,000). Other methods of consuming cannabis were drinking it, dabbing, and other not specified methods (all under 10%). Those who reported using cannabis may have tried more than one method over the past 12 months. See Table 6 for more details.
Table 6: Methods of cannabis consumption, 2019Footnote *
Canadians reported using a variety of different cannabis products in the past year. Marijuana or herb was the most commonly reported product used (88% or 5.4 million), followed by edibles (42% or 2.6 million), cannabis oil (30% or 1.9 million), hashish or kief (17% or 1.1 million), and cannabis cartridges or disposable vape pens (16% or 965,000). Other cannabis products include solid concentrate, liquid concentrate, liquid (in drinks, such as tea), and other products (all under 10%). See Table 7 for more details.
Table 7: Cannabis products consumed, 2019Footnote *

The majority (84% or 5.2 million) of those who reported using cannabis in the past year reported using cannabis in the past three months, an increase from 2017 (75% or 3.3 million). Of those who had used cannabis in the past three months, many reported consuming cannabis on a daily or almost daily basis (27% or 1.4 million, unchanged from 32% or 1 million in 2017). There was no difference in daily or almost daily use among males and females (28% vs. 26%, respectively), nor was there any difference between young adults aged 20 to 24 and adults aged 25 and older (25% and 29%, respectively). Daily or almost daily use in the past three months was not reportable for youth aged 15 to 19 due to small sample size.
Just over two-thirds (69% or 4.1 million) of those who used cannabis in the past year reported using cannabis in the past 30 days. Of those who had consumed cannabis in the past 30 days, 35% (1 million) reported consuming cannabis on a daily or almost daily basis.
Three quarters (75% or 4.7 million) of Canadians who consumed cannabis in the past year reported using cannabis in combination with other substances. Males were more likely than females to report using cannabis in combination with other substances (80% or 2.7 million vs. 70% or 2 million, respectively). Among those who have consumed cannabis in the past year, alcohol was the most commonly reported substance consumed in combination with cannabis (68% or 4.2 million). Other substances consumed in combination with cannabis include tobacco, e-cigarettes or vaping devices (30% or 1.8 million), prescription sedatives or anti-anxiety medications (7% or 424,000), and illegal hallucinogens (6% or 338,000).
According to the WHO ASSIST screening test, among Canadians who reported using cannabis in the past year, 51% (3.2 million) were at low risk of developing health or other problems due to their cannabis use, while 48% (3.1 million) were at moderate risk. Few Canadians (1% or 72,000) were at high risk of developing health or other problems or developing cannabis dependency due to their cannabis use in the past year. Males were more likely than females to be at high risk (2% for males, but unreportable due to small sample size for females). These results are unchanged from 2017.
Five percent (5% or 1.4 million) of Canadians aged 15 and older reported being a passenger in a vehicle driven by someone who had used cannabis in the past two hours. Among Canadians who had used cannabis in the past year, this increased to 18% (1.1 million). Twenty-four percent (24% or 228,000) of young adults aged 20 to 24 who had used cannabis in the past year reported being passengers in a vehicle driven by someone who had used cannabis in the past two hours, and 16% (725,000) of adults aged 25 and older who had used cannabis in the past year reported the same. An estimate was not reportable for youth aged 15 to 19 due to small sample size. Among Canadians who reported using cannabis in the past year, 9% (513,000) reported driving within two hours of consuming cannabis. Males were more likely than females to report driving within two hours of consuming cannabis (11% or 349,000 vs. 7% or 164,000, respectively). Fourteen percent (14% or 119,000) of young adults aged 20 to 24 who had used cannabis in the past year reported driving within two hours of consuming cannabis and 8% (370,000) of adults aged 25 and older who had used cannabis in the past year reported the same. An estimate was not reportable for youth aged 15 to 19 due to small sample size.
Among females aged 15 to 44 who had ever used cannabis and had given birth in the past five years, 5% (29,000) reported consuming cannabis during their last pregnancy, and 6% (36,000) reported consuming cannabis while breastfeeding their child. There were no observations reported for female youth aged 15 to 19 or young females aged 20 to 24.
Since cannabis was legalized and regulated in 2018, CADS 2019 was the first opportunity to ask respondents if they were more willing to report on their cannabis consumption that before legalization and regulation. About one-quarter (27% or 3.4 million) indicated that they were more willing to report on their cannabis consumption, 41% (5.2 million) were no more or less willing, and 32% (4.2 million) were not more willing to report. It is possible that the increase in the past-year prevalence of cannabis consumption is, in part, related to an increased willingness to report on cannabis consumption since it was legalized and regulated, however this is untested and thus not a direct conclusion from the data.
Finally, among Canadians who reported using cannabis in the past year, 31% (1.9 million) reported using more cannabis since it was legalized and regulated than they used pre-legalization, 26% (1.6 million) reported using less, and 43% (2.6 million) reported using the same amount. Females were more likely than males to report using more cannabis since legalization (36% or 1 million, vs. 27% or 887,000).
Use and Problematic Use of Psychoactive Pharmaceutical Drugs
CADS 2019 includes questions relating to the use and problematic use of three classes of psychoactive pharmaceutical drugs: opioid pain relievers, stimulants (such as medication prescribed for Attention Deficit Hyperactivity Disorder), and tranquillizers and sedatives. While these drugs are prescribed for therapeutic purposes, they have the potential to be used in a problematic manner due to their psychoactive properties.
Among respondents who had reported using psychoactive pharmaceuticals, further questions were asked to determine whether the drugs were used for reasons other than for prescribed therapeutic purposes including use for the experience, for the feeling they caused, to get high, to feel better (improve mood), to feel numb, to cope with stress or problems or for "other" reasons. In the text below, such non-therapeutic use is referred to as problematic use.
The overall prevalence of psychoactive pharmaceutical use among Canadians aged 15 years and older was 23% (7 million), unchanged from 2017 (22% or 6.5 million). The prevalence of past-year psychoactive pharmaceutical use in 2019 was higher among females (27% or 4.1 million) than males (19% or 2.8 million). The prevalence of use was lower among youth aged 15 to 19 (15% or 315,000) than among young adults aged 20 to 24 (27% or 607,000) and adults aged 25 years and older (23% or 6 million). The prevalence of psychoactive pharmaceutical use for males and females was unchanged from 2017 (20% or 2.9 million males and 24% or 3.6 million females). The prevalence of use for each age category was unchanged from 2017: 17% (332,000) of youth aged 15 to 19; 21% (492,000) of young adults aged 20 to 24; and 23% (5.7 million) of adults aged 25 and older. Table 8 presents past-year psychoactive pharmaceutical use among Canadians since 2008.
In 2019, of those who reported having used psychoactive pharmaceuticals in the past year, 7% (493,000) engaged in problematic use of such a drug (i.e. used it for the experience, for the feeling it caused, to get high or for any other reasons than prescribed use). Among all those who used psychoactive pharmaceuticals (therapeutic or non-therapeutic use) in the past year, there was no difference in the prevalence of past-year problematic use between males (9% or 259,000) and females (6% or 234,000). The prevalence of past-year problematic use among those who used psychoactive pharmaceuticals was higher among young adults aged 20 to 24 (20% or 124,000) than among adults aged 25 years and older (6% or 341,000), while the prevalence for youth aged 15 to 19 was not reportable due to small sample size. Two percent (2% or 493,000) of the population aged 15 and older engaged in problematic use of psychoactive pharmaceuticals in the past year, unchanged from 2017 (1% or 336,000). Tables 9 and 10 present problematic use of psychoactive pharmaceuticals since 2008.
Opioid Pain Relievers
Of the three classes of psychoactive pharmaceuticals, overall use of opioid pain relievers (including prescribed or non-prescribed drugs for therapeutic and non-therapeutic purposes) was the most common. Fourteen percent (14% or 4.4 million) of Canadians aged 15 years and older reporting having used such opioid pain relievers in the past year, an increase from 2017 (12% or 3.5 million). The prevalence of past-year opioid pain reliever use was higher among females (16% or 2.5 million) than males (12% or 1.9 million). The prevalence of past-year opioid pain reliever use among males was unchanged from 2017 (11% or 1.6 million), though there was an increase from 2017 (12% or 1.8 million) among females.
One percent of all Canadians aged 15 and older engaged in problematic use of opioid pain relievers in the past year (Table 9). Among the 14% of Canadians who used opioid pain relievers in the past year, 6% (269,000) reported problematic use of them, an increase from 2017 (3% or 100,000) (Table 10). Among all Canadians aged 15 and older, there was no difference in the prevalence of problematic use of opioids between males and females (1% or 127,000 and 1% or 142,000, respectively). The prevalence of problematic use of opioids was not reportable for youth aged 15 to 19 in the overall population due to small sample size.
Stimulants
Stimulants are defined as products that can be obtained from a doctor such as Ritalin, Concerta, Adderall, Dexedrine or others, and that are prescribed by doctors to help people who have attention or concentration problems (such as ADHD).
In 2019, 2% (660,000) of Canadians aged 15 years and older reported having used a stimulant in the past year (including therapeutic and problematic use), unchanged from 2017 (2% or 714,000), and an increase from 2015 (1% or 338,000) (Table 8). There was no difference between males and females (2% or 324,000, and 2% or 337,000, respectively). The prevalence of past-year use of stimulants among youth aged 15 to 19 was 5% (101,000). Past-year use of stimulants was higher among young adults aged 20 to 24 (9% or 206,000) than among adults aged 25 years and older (1% or 354,000).
Of those who reported past-year stimulant use, 37% (244,000 Canadians representing 1% of Canadians aged 15 years and older) reported problematic use of such a drug, an increase from 2017 (19% or 103,000) (Table 10). Among all Canadians aged 15 years and older, there was no difference in the prevalence of problematic use of stimulants between males and females (1% or 151,000 and 1% or 93,000, respectively). The prevalence of problematic use of stimulants was higher among young adults aged 20 to 24 (5% or 108,000) than among youth aged 15 to 19 (1% or 20,000) and adults aged 25 years and older (less than one percent (0.4%) or 117,000). The prevalence of problematic use of stimulants among those who used stimulants in the past year was 33% (117,000) among adults aged 25 and older, while the prevalence was not reportable for youth aged 15 to 19 and young adults aged 20 to 24 as well as for both sexes due to small sample size.
Sedatives
In 2019, 11% (3.3 million) of Canadians aged 15 years and older reported past-year use of sedatives (including both therapeutic and problematic use), unchanged from 2017 (12% or 3.5 million) (Table 8). The prevalence of sedative use by females (14% or 2.2 million) was higher than that of males (7% or 1.1 million) and both were unchanged from 2017 (14% or 2.1 million and 9% or 1.3 million, respectively). Past-year use of sedatives was lower among youth aged 15 to 19 (3% or 72,000) than young adults aged 20 to 24 (12% or 272,000) and adults aged 25 and older (11% or 3 million).
In 2019, of those who reported past-year use of sedatives, 3% (85,000) reported using sedatives to get high, unchanged from 2017 (1% or 49,000) (Table 10). This is less than one percent (0.3%) of the population aged 15 years and older, and unchanged from 2017 (0.2%) (Table 9). Among those who reported past-year use of sedatives, there was no difference in the prevalence of sedative use to get high between males and females (5% or 60,000, and 1% or 25,000 respectively). The prevalence of problematic use of sedatives was not reportable among youth aged 15 to 19 and young adults aged 20 to 24 due to small sample size. Among those who reported past-year use of sedatives, the prevalence of use of sedatives to get high among adults aged 25 and older was 2% (51,000).
Table 8: Past-year psychoactive pharmaceutical use, Canada 2008–2019Footnote *

Table 9: Problematic use of psychoactive pharmaceuticals, all Canadians 2008–2019Footnote *

Table 10: Problematic use of psychoactive pharmaceuticals, among users 2008–2019Footnote *

Illegal Drug Use
Respondents were asked about past-year use of illegal drugs. Similar to CTADS, illegal drugs included cocaine or crack, ecstasy, speed or methamphetamines, hallucinogens, inhalants, heroin, and salvia. For 2019, respondents were also asked about their use of synthetic cannabinoids, mephedrone, BZP/TFMPP, kratom and other drugs.
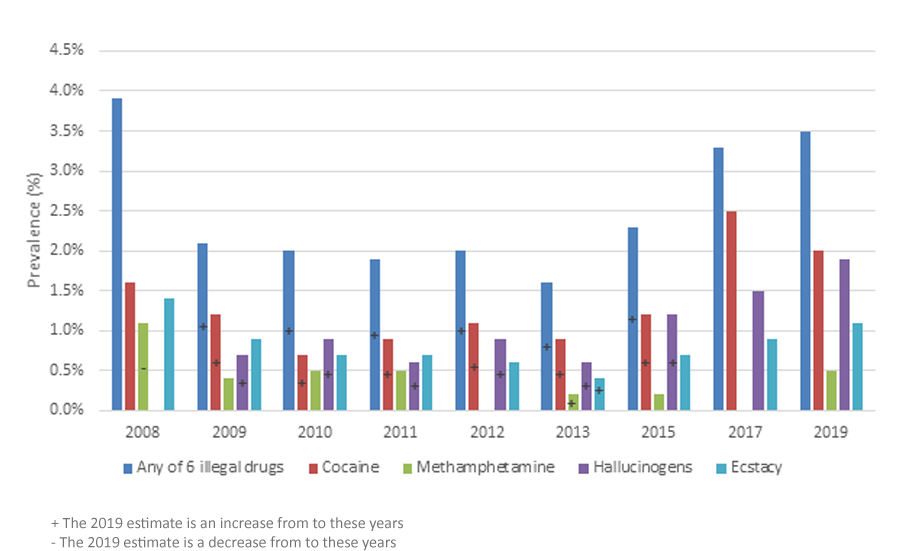
Past-year use of at least one of six illegal drugs (cocaine/crack, speed/methamphetamine, ecstasy, hallucinogens, heroin, salvia) was 3% (1.1 million), unchanged from 3% (987,000) in 2017 and an increase from 2% (678,000) in 2015.
Overall, prevalence of past-year use of these illegal drugs was similar among males (4% or 616,000) and females (3% or 465,000). For males, this is unchanged from 2017 (5% or 719,000), while for females, this is an increase from 2017 (2% or 268,000).
Past-year use of at least one of six illegal drugs was higher among young adults aged 20 to 24 (14% or 310,000) than among youth aged 15 to 19 (3% or 63,000) and adults aged 25 and older (3% or 708,000). There was no change from 2017 for any age group.
Overall, among Canadians past-year illegal drug use remained low. Cocaine/crack remained the most-consumed illegal substance, with 2% (605,000) of respondents having consumed cocaine or crack in the past year, unchanged from 2017 (2% or 730,000). Males (2% or 362,000) and females (2% or 243,000) consumed cocaine or crack in similar amounts, unchanged from 2017 (4% for males and 1% for females). Past-year use of cocaine or crack was higher among young adults aged 20 to 24 (9% or 203,000) than adults aged 25 and older (1% or 390,000), and both were unchanged from 2017. Cocaine/crack use among youth aged 15 to 19 was not reportable due to small sample size.
Hallucinogen use was similar to cocaine/crack use in 2019. Hallucinogens are drugs such as LSD, PCP, and psilocybin (magic mushrooms). Two percent (2% or 587,000) of Canadians consumed hallucinogens in 2019, unchanged from 1% (443,000) in 2017. Males (2% or 352,000) and females (1% or 234,000) consumed hallucinogens in similar amounts. For males this is unchanged from 2017 (2% or 341,000) but for females this is an increase from 2017 (less than one percent (0.7%) or 102,000). Hallucinogen consumption was higher among young adults aged 20 to 24 (6% or 129,000) than youth aged 15 to 19 (2% or 47,000) and adults aged 25 and older (2% or 411,000).
One percent (1% or 353,000) of Canadians reported consuming ecstasy in the past year, unchanged from 2017 (1% or 271,000). Methamphetamine/amphetamine use was reported by 0.5% (142,000) of Canadians, though data were not reportable for 2017 so no comparison can be made. The number of Canadians who reported consuming inhalants (glue or other solvents), synthetic cannabinoids, kratom, and other drugs in the past year was very low, and there were no observations for consumption of salvia, heroin, mephedrone, or BZP/TFMPP in the past year. Table 11 presents past-year illegal drug use among Canadians since 2008.
Table 11: Illegal drug use, Canada 2008–2019Footnote *
Among Canadians who reported ever consuming any illegal drugs, cannabis or psychoactive pharmaceuticals, 1% (199,000) reported ever injecting drugs. Males were more likely than females to have ever injected drugs (1% or 145,000 vs. less than 1% or 54,000, respectively). Data were not reportable for youth aged 15 to 19 or young adults aged 20 to 24 due to small sample size.
Harms Related to Drug Use
Respondents were asked if there ever was a time that they felt their drug use (i.e. cannabis and illegal drugs) had a harmful effect on one of nine factors: physical health; mental health; friendships and social life; financial position; home life or marriage; work, studies, or employment opportunities; legal problems; difficulty learning; or housing problems.
Overall, 5% (1.1 million) of Canadians aged 15 years and older reported experiencing at least one harm in the past year due to their drug use, unchanged from 2017 (4% or 820,000). There was no difference in the prevalence of reported harm as a result of one's own drug use between males (5% or 616,000) and females (4% or 482,000), both unchanged from 2017 (6% or 518,000 and 3% or 302,000, respectively). A higher proportion of young adults aged 20 to 24 (14% or 284,000) reported harm due to their own illegal drug use than youth aged 15 to 19 (6% or 125,000) and adults aged 25 years and older (3% or 689,000). The prevalence of reported harm for each age category (i.e. youth aged 15 to 19, young adults aged 20 to 24, and adults 25 years and older) was unchanged from 2017.
The prevalence of reported harm was higher among individuals who reported the use of cannabis, the use of any illegal drug (i.e., cocaine/crack speed/methamphetamine/crystal meth, hallucinogens including salvia, ecstasy, inhalants, or heroin) or problematic use of psychoactive pharmaceuticals. One in six (17% or 1.0 million) of those who used cannabis in the past year, used illegal drugs in the past year, or who reported problematic use of psychoactive pharmaceuticals in the past year reported having experienced some harm in the past year due to their drug use, unchanged from 2017 (18% or 820,000). Among this population, there was no difference in the prevalence of reported past-year harm between males (17% or 616,000) and females (16% or 478,000) and both were unchanged from 2017 (19% or 518,000 and 18% or 302,000, respectively). Among this population, the prevalence of reported past-year harm was higher among young adults aged 20 to 24 (27% or 284,000) than adults aged 25 and older (14% or 685,000), both unchanged from 2017. Data were not reportable for youth aged 15 to 19 due to small sample size. Table 12 presents harms related to drug use among Canadians since 2008.
Table 12: Harms related to drug use, Canada 2008–2019Footnote *

Naloxone
Among Canadians aged 15 years and older, two percent (2% or 542,000) reported obtaining a naloxone kit in the past year. There was no difference in the prevalence of obtaining a naloxone kit between males and females (2% or 255,000 vs. 2% or 287,000, respectively). Three percent of young adults aged 20 to 24, and 2% of adults aged 25 years and older reported obtaining a naloxone kit. An estimate was not reportable for youth aged 15 to 19 due to small sample size.
Among those who reported past-year opioid pain reliever use, 3% (150,000) reported obtaining a naloxone kit in the past year, and there was no difference between males and females (3% or 47,000 and 4% or 103,000, respectively). Among this population, four percent (4% or 140,000) of adults aged 25 and older reported obtaining a naloxone kit, while the prevalence for youth aged 15 to 19 and young adults aged 20 to 24 was not reportable due to small sample size.
Among those who reported receiving a naloxone kit in the past year, the most commonly reported reason for obtaining a naloxone kit was in case of a need for someone else (69%), followed by other reasons (19%) and in case of a need for oneself (12%).
Treatment
For the first time in 2019, CADS gathered information from Canadians on obtaining professional help for substance use. Professional help is defined as starting a professional treatment or counselling plan, no matter the length or how many sessions were actually attended. It includes any treatment or counselling given by doctors, counsellors, social workers or other health professionals. Among Canadians who reported consuming alcohol, cannabis, psychoactive pharmaceuticals, over-the-counter medications, and/or illegal drugs, 2% (551,000) reported ever receiving professional help for their substance use. Males were more likely than females to have ever received professional help (3% or 395,000 vs. 1% or 155,000, respectively).
Among those who had ever received professional help for substance use, 20% (112,000) received professional help in the past year.
Drug overdose
For the first time, CADS 2019 included questions about respondents' experience with overdose events related to use of pain relievers, stimulants, sedatives, cannabis, cocaine/crack, amphetamines/methamphetamine, ecstasy, hallucinogens, heroin, salvia, inhalants, synthetic cannabinoids, mephredone, kratom, BZP, or other drugs.
Of those who reported ever using any of these drugs, two percent (2% or 327,000) had ever overdosed. There was no difference in the prevalence of lifetime drug overdose between males (2% or 205,000) and females (1% or 123,000). There was also no difference in the prevalence of drug overdose between young adults aged 20 to 24 (4% or 70,000) and adults aged 25 and older (1% or 217,000), while the prevalence among youth aged 15 to 19 was not reportable due to small sample size.
Provincial prevalence of lifetime drug overdose ranged from 1% in Alberta, New Brunswick, and Prince-Edward to 2% in Nova Scotia, Quebec, Ontario, Manitoba and Saskatchewan, while the prevalence was not reportable for Newfoundland and Labrador and British Columbia due to small sample size.
Overdose interventions
The majority (72% or 219,000) of those who reported having ever experienced an overdose reported receiving some kind of assistance the last time they experienced an overdose (i.e. calling for ambulance or being brought to hospital, being placed in a rescue position, performing CPR on you or administering naloxone by someone, or having any other kind of assistance). Calling for an ambulance or being brought to hospital (41% or 134,000) was the most commonly reported intervention. Other interventions include receiving another kind of assistance (27%), being placed in the rescue position (23%), and performing CPR or administrating naloxone by someone else (20%).
Reference information
Health Canada has worked with Statistics Canada on the delivery of CADS 2019. The target population for CADS is all persons 15 years of age and older living in Canada, excluding residents of the Yukon, Northwest Territories and Nunavut, people who live on reserves, and full-time residents of institutions.
A sample of 10,293 respondents was obtained from a household sampling frame of 20,000 Canadians. The sample consists of 591 individuals aged 15 to 24, and 9,702 individuals aged 25 years and older across Canada.
CADS used a self-administered electronic questionnaire survey format, with follow-up telephone interviews for non-responses, and the sample was generated using the Dwelling Universe File (DUF). The overall response rate was 50.9%. For the purposes of this report only univariate and bivariate analyses were conducted, with a t-test used to determine if results are statistically significantly different from one another. The data presented in this report have been weighted to allow the results to be generalized to the Canadian population using the Canadian Census 2011.
For more information about the survey and the results, please write to the Office of Drug Research and Surveillance, Controlled Substances Directorate, Health Canada, Address Locator 0302A, Ottawa, ON, K1A 0K9, or send an e-mail request to odss.bssd@hc-sc.gc.ca.
For information on the public-use microdata file, please contact Statistics Canada's Client Services, Special Surveys Division by e-mail (statcan.infostats-infostats.statcan@canada.ca), or by calling the toll-free telephone number (1-800-263-1136).