Lessons from the HealthADAPT Program (2018-2022): Strengthening Capacity to Prepare for the Health Impacts of Climate Change in Canada
Download in PDF format
(1.1 MB, 16 pages)
Organization: Health Canada
Published: 2025-10-09
Cat. : H129-172/2025E-PDF
ISBN : 978-0-660-78486-1
Pub. : 250186
How to use this report
This report presents a brief overview of the lessons learned from the pilot HealthADAPT program (2018-2022). The report is intended to support health authorities in Canada in addressing climate change impacts by informing their future efforts to understand growing risks and vulnerabilities, develop health adaptation action plans, and foster the networks and partnerships needed for building climate resilience.
Climate change risks to individuals, communities and health systems
Canada's national climate change and health assessment "Health of Canadians in a Changing Climate: Advancing our Knowledge for Action," underscores the importance of taking proactive steps to protect the health of Canadians and the health system in the face of growing risks caused by climate change. Climate change is increasing risks to health and well-being from a number of climate-related hazards, including extreme heat events, wildfires, floods, and ice storms. As well, the expansion of some infectious diseases and impacts on food and water safety and security are endangering health and communities. First Nations, Inuit and Métis peoples face a number of severe impacts and unique challenges associated with climate change and poor determinants of health that exacerbate its effects. Evidence also suggests that there are growing threats to mental health, health equity and health systems, including health facilities from a warming climate. Potential impacts to Canada's healthcare system can include disruptions to power, food and water supplies during extreme weather events, and physical and mental health effects on health professionals, among others (Berry & Schnitter, 2022).
A key finding of the assessment was that there is a health adaptation gap in Canada; many health authorities are not undertaking important actions to prepare individuals and health systems from climate change impacts, for example, undertaking assessments, investing in the education and training of health professional staff, monitoring climate change impacts and examining the vulnerability of health facilities (Berry & Schnitter, 2022). Health authorities in Canada require increased data, guidance and capacity to proactively prepare for a rapidly warming country.
Addressing climate change challenges in Canada requires a coordinated and collaborative effort from all levels of government and other stakeholders and partners, including Indigenous communities, civil society organizations, academia, and the private sector. This effort will need to be based on a deep understanding of the unique challenges and opportunities for climate change and health adaptation and resiliency building facing different regions of the country.
HealthADAPT - building capacity to protect Canadians from climate change
HealthADAPT is a multi-year capacity-building program developed by Health Canada. The pilot program was launched in 2018 and supported 10 health authorities across Canada at local, regional, provincial and territorial scales of the Canadian health sector. Over four years, the HealthADAPT program supported health authorities in building their capacity for addressing climate change and health risks. The objectives of the pilot HealthADAPT program were to:
- Increase understanding of climate change impacts on:
- health systems
- the health of Canadians;
- Identify communities or people who are at higher risk of experiencing negative health effects of climate change;
- Support the development, testing and carrying out of local and regional climate change health adaptation plans with partners;
- Monitor and evaluate the effectiveness of the climate change health adaptation plans (Health Canada, 2022).
The HealthADAPT projects that were part of the pilot program are shown below in Figure 1. Learnings from these projects can provide valuable input and insight on how Canadian health authorities and the healthcare system can better adapt to our changing climate.

Figure 1 - Text Equivalent
A map of Canada showing the locations of the 10 HealthADAPT funded projects:
- New Brunswick Department of Health located in Fredericton, New Brunswick
- Institut national de santé publique du Québec located in Quebec, Quebec
- Centre intégré de Santé et de services sociaux (CISSS) de Chaudière-Appalaches located in Sainte-Marie, Quebec
- Centre intégré de santé et de services sociaux (CISSS) de l'Outaouais located in Gatineau, Quebec
- Northwestern Health Unit located in Kenora, Ontario
- York Region Public Health located in Newmarket, Ontario
- Wellington-Dufferin Guelph Public Health located in Guelph, Ontario/Region of Waterloo Public Health located in Waterloo, Ontario
- First Nations Health Authority located in West Vancouver, British Columbia
- Vancouver Coastal Health located in Vancouver, British Columbia/Fraser Health Authority located in Surrey, British Columbia
- Northwest Territories Department of Health and Social Services located in Yellowknife, Northwest Territories
Climate change & health adaptation planning elements
To document and share lessons learned from the HealthADAPT initiative, throughout 2021, 15 key informant (KI) interviews and surveys were conducted with funding recipients (FRs), other Canadian health authorities who have conducted climate change and health vulnerability and adaptation assessments (CCHVAAs), and experts in the field of climate change and health. KIs comprised of the following groups:
- Representatives from the 10 HealthADAPT funded projects.
- Representatives (2) from non-funded health authorities who have completed CCHVAAs.
- Experts (3) in administering climate change and health programs.
Based on these interviews and surveys, several key elements for building capacity to address climate change risks to health were identified, as shown in Figure 2 below. It is important to recognize that many of these elements overlap. This is representative of the project work, which entailed multiple phases that coincided with one another, rather than following a purely iterative approach.
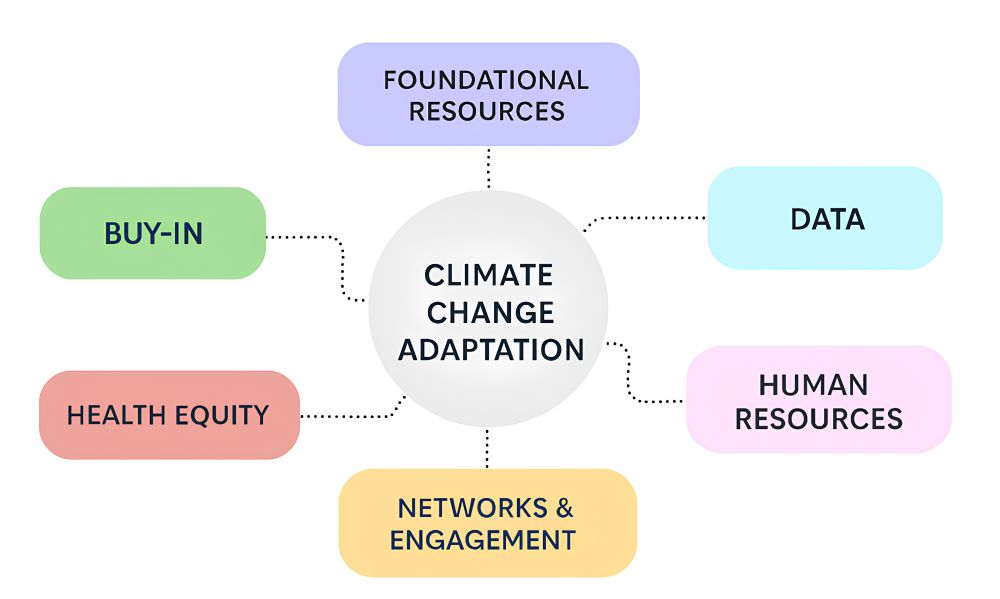
Figure 2 - Text Equivalent
A diagram titled "Climate Change Adaptation" in the center, surrounded by six colored boxes connected with dashed lines. The boxes are labeled: Foundational Resources (purple), Data (blue), Human Resources (pink), Networks & Engagement (yellow), Health Equity (red), and Buy-In (green).
Understanding these key elements, including challenges and enablers associated with them faced by health authorities can help identify effective strategies and approaches for understanding climate change risks to health, for example, through climate change and health assessments, and for developing needed adaptation plans. Each of these elements is described in further detail below.
Buy-in
Buy-in refers to obtaining acceptance and/or willingness from an individual, group, or organization to actively support or participate in a project or activity, such as creation of a new idea, policy, or plan. In the context of climate change and health adaptation, buy-in can be a critical enabler for successful project development and implementation. Securing buy-in can make it easier to obtain dedicated funding, which can contribute to obtaining skilled staff, data, science products and other necessary capacities to prepare for climate change impacts on health.
Challenges:
- Organizational learning: With climate change still being new on the radar for many health organizations, there is a learning curve for health units to integrate climate change into their organizational planning which can affect buy-in. Many health authorities are still new to conducting CCHVAAs and undertaking climate change and health work.
- Limited capacity: Broader issues such as a lack of staff capacity can negatively impact buy-in. This is especially an issue during an emergency or competing priority, such as the COVID-19 pandemic, as it diverts staff from other issues due to surge capacity needs and other requirements.
Enablers:
- Senior management: Buy-in from senior management is especially useful, as these individuals can offer relevant program development insights, and can secure broader internal support, as well as support from external partners and stakeholders.
- Organizational mandate: When an organization has a mandate that includes climate change objectives, health authorities can devote more time to the project, and plan and coordinate project activities, and hire contractors as needed. Notably, it is likewise helpful to be aware of partner mandates that align with those of health authorities to gain stakeholder buy-in within the community as well.
- Internal champions: Champions within the organization can be pivotal in bringing the project forward to decision-makers. Champions can be found at any level within an organization, including subject matter experts or individuals with strong internal connections. These individuals can advocate why climate change and health work is needed to their colleagues and senior management and highlight their benefits to the organization, its employees, stakeholders, and the broader community.
- Understanding impacts: Understanding impacts of climate change on health and how this issue directly affects an organization and the population it serves can motivate buy-in by establishing a "business case" and increasing organizational will to undertake climate adaptation initiatives and programming.
Foundational Resources
A wide range of resources are required to address climate-driven health risks. Within the context of the pilot HealthADAPT program, funding recipients referred to foundational resources, including guidance documents and frameworks, that helped them conduct CCHVAAs and plan adaptation measures. In contrast to data sources, foundational resources refer to reference materials that provide a framework, principles, best practices, or recommendations, acting as sources of guidance on how to approach a specific topic. Foundational resources are highly beneficial for increasing the capacity needed to take protective actions.
Challenges:
- Availability: while health authorities may be aware of some guidance materials on conducting CCHVAAs, some documents and tools may not be readily available or easily accessible. This can be due to a lack of communication channels or platforms to distribute the materials widely to partners that will use them.
- Relevance: while these documents/tools may provide helpful general information, they may not always be relevant to the specific or local context and needs of health authorities. For example, they may have more limited applicability in certain regions (e.g., rural and remote areas) or for specific populations (e.g., Indigenous communities).
- Inclusivity: ensuring that guidance is accessible to practitioners and beginners with varying levels of expertise is a challenge, as it is difficult to develop step-by-step guides and also incorporate the latest knowledge.
Enablers:
- Data: as access to reliable data improves, we can create better guidance documents, frameworks, and tools, and make existing ones more widely applicable.
- Collaboration: collaboration between different health authorities, other civil society health actors, and decision makers in other sectors can help identify and disseminate best practices for reducing exposure to environmental hazards, improving health outcomes, and building community resilience. These strategies can also be used to develop comprehensive foundational resources.
- Funding: adequate funding is necessary for developing guidance documents, frameworks, and tools for climate change adaptation. Investments in research and technical assistance, for example, can support the development of these resources.
Data
Having access to robust quantitative and qualitative data is essential for collecting information for CCHVAAs and towards developing effective adaptation measures that protect those most likely to be impacted by climate change. Climate data-driven research is essential for understanding the potential health impacts of climate change, such as data on extreme weather events, temperature variations, and humidity. Collecting and analyzing health data can also help identify higher risk populations and track changes in climate-related health outcomes over time.
Challenges:
- Availability: certain geographical contexts and environments may not be adequately represented in existing data resources. Findings from the HealthADAPT project demonstrate that important types and sources of data are not available for rural and remote regions. Furthermore, certain population level data is not available or easily accessible, such as data on Indigenous communities. There is also a significant data gap in future projections for vulnerability and data related to mental health impacts from climate change. The lack of this data presents an added barrier to developing CCHVAAs and other adaptation planning.
- Complexity: climate change issues can be quite complex due to the high degree of uncertainty associated with its impacts, and because it is a multi-sectoral issue that requires the cooperation of a range of actors and stakeholders. This complexity can make it more difficult for public health authorities to address climate change impacts on health.
- Limitations in capacity/expertise: data-related barriers can be exacerbated by limitations in capacity and expertise, including limitations in the collection of historical or longer-term data, conducting analysis with diverse types of data, providing adequate reporting, and determining appropriate methods for data collection.
Enablers:
- Prioritization: the prioritization of climate change work at the operational level can help promote knowledge acquisition and tool development, which can enhance data collection and analysis. In addition, the prioritization of certain climate and health variables to track within a local area can help health authorities tailor their work appropriately to their health region.
- Enhancing in-house capacity: in-house capacity for data collection and/or analysis can also be enhanced by providing relevant training or setting up expert committees. However, it is also important to recognize that learning through practical experience is important and enhances internal capacity.
- External support: external support, such as the technical guidance provided by Health Canada's experts during the HealthADAPT program, can help health authorities with their data collection and analysis activities, including by supporting data sharing and data curation.
Human Resources
Human resources refers to the people possessing the skills, and knowledge necessary to accomplish tasks and achieve objectives. Adapting to climate change requires sufficient skilled human resources, as climate change poses complex and multifaceted health challenges that require a wide range of expertise to address.
Challenges:
- Limited funding: some health authorities, particularly those in rural and remote settings, may not have the necessary resources to hire and retain staff with the required expertise in climate change and health, leading to greater staff turnover, which can result in discontinuation of activities. Limited funding may also restrict health authorities' capacity to invest in staff professional development such as education and training.
- Limited awareness: some health authorities may have limited awareness of the importance of addressing the health impacts of climate change. Health authorities generally work on climate issues that impact health (e.g., extreme temperatures), but they may not consider programming/planning for climate change as a whole. More overarching planning is necessary for investing in necessary human resources.
- Competing issues: addressing climate change is often seen as a long-term issue and health authorities may be more preoccupied and focused on addressing immediate health challenges and emergencies. In such situations, this can mean that health authorities are focusing on protection, rather than prevention, leading to less human resource capacity to address certain climate change and health issues due to perceived urgency.
Enablers:
- Multidisciplinary approach: recruiting a multidisciplinary team with various types of expertise, such as climate science, epidemiology, statistical analysis, public health, and stakeholder communications and engagement, can enhance human resource capacity for addressing climate change and health issues.
- Training & education: when staff can access training and educational resources on the impacts of climate change on health they can learn requisite skills such as assessing and managing risks and vulnerabilities and how to develop effective adaptation strategies.
- Collaboration: collaboration with other health authorities, external partners, and stakeholders, including those within other sectors, can fill internal human resource gaps by building capacity through knowledge and expertise sharing.
- Dedicated staff: Having staff who are primarily dedicated to working on climate change within their position can enhance organizational capacity to address climate change issues, as it allows the organization to have staff that work specifically on climate change issues, with specialized knowledge and expertise.
Networks and Engagement
Networking and engagement are essential for effective action on climate change and health, as they enable health authorities to learn from the experiences of others and leverage the expertise and resources of other organizations and stakeholders. When health authorities have access to networks and engagement opportunities, this can lead to increased knowledge and resource sharing, eliminate duplication of efforts, and provide critical support through partnerships.
Challenges:
- Interdisciplinary barriers: because climate change and health is such an interdisciplinary field one type of challenge that may arise is bridging disciplinary gaps and finding common ground for effective networking.
- Limited resources: health authorities may have limited resources available to dedicate to networking and engagement activities, which can make it difficult to build and maintain effective partnerships.
- Time Constraints: health authorities often have demanding work schedules and balancing day-to-day responsibilities with networking efforts can be challenging, reducing opportunities for collaboration and knowledge sharing.
Enablers:
- Communication platforms: having effective platforms for communication make it easier to establish communication channels and share information. Platforms can also have internal mechanisms to support collaboration (e.g., breakout chats during team meetings).
- Dedicated networking spaces: having a dedicated networking space, such as a Community of Practice or a network made up of local stakeholders, where members share a common interest or profession, can enhance knowledge exchange by providing valuable insights on best practices and lessons learned in addressing climate-related health risks.
- External facilitation: external facilitators can help bridge the gap between different organizations and disciplines involved in climate change and health by facilitating dialogues.
Health Equity
In the context of climate change and health adaptation, health equity involves focusing on populations that experience disparities based on social, economic, and/or environmental factors that can heighten the impacts of climate change on health. This includes developing targeted adaptation strategies addressing the needs of at-risk populations and including their perspectives as part of relevant adaptation planning processes.
Challenges:
- Limited resources: climate change and health adaptation planning can be resource-intensive, and resources may be limited, making it challenging to prioritize activities that address health equity concerns.
- Inadequate data: data on the health impacts of climate change applicable to at-risk populations, can be limited. To target interventions more effectively and develop more precise strategies, it becomes imperative to obtain and analyze disaggregated date focusing specifically on at-risk populations.
- Limited trust: establishing trust and credibility between health authorities and communities is crucial for effective engagement. Historical experiences, cultural factors, and previous interactions can limit this level of trust.
- Lack of community engagement: the involvement of communities and community-based organizations in planning and decision making is essential for ensuring that health equity concerns are adequately addressed. However, this can be challenging to undertake and/or broadly implement within projects.
Enablers:
- Community leaders: engaging with community leaders representing at-risk populations is effective in initiating or maintaining partnerships.
- External consultants: in some cases, employing an external consultant who is a member of the at-risk population or has close connections to the community can be beneficial towards integrating health equity considerations in adaptation planning.
- Participatory research: community-based participatory research and engagement helps ensure that health equity considerations inform climate and health adaptation planning and decision-making.
The path forward: strengthening the capacity of health authorities
Based on the lessons learned from the HealthADAPT program, including the identified challenges and enablers for strengthening the capacity of health authorities to prepare for climate change outlined above, the following considerations for supporting actions are presented:
Allocating adequate resources: health authorities can better prepare for climate change when they have adequate resources to undertake this work, particularly:
Expertise: expertise noted by funding recipients to be particularly beneficial include expertise in geospatial data skills, climate change and health knowledge, epidemiology, project management, and communications skills.
Data: reliable data and information on climate change, health impacts, environmental hazards, and at-risk populations is necessary to undertake CCHVAAs and ensure adaptation plans are evidence-based and effective.
Funding: adequate funding is needed to undertake assessments, to develop and implement adaptation plans, and to support research, staffing, monitoring, and evaluation.
Conducting vulnerability assessments: health authorities can prepare better for climate change when they comprehensively assess the potential health impacts of climate change on their population and health systems. Conducting CCHVAAs can help identify at-risk populations, understand health impacts, improve preparedness and response, and support adaptation planning.
Building capacity: along with providing resources, health authorities should also focus on building the capacity of healthcare providers and other relevant professionals and external partners to respond to the health impacts of climate change, including by providing training on climate-related health issues.
Considering higher risk populations: a range of at-risk populations, including children, the elderly, low-income communities, individuals with pre-existing health conditions, outdoor workers, Indigenous Peoples, migrants and refugees, coastal and island communities, urban dwellers, and those experiencing homeless are noticeably more susceptible to the multifaceted health impacts posed by climate change, reflecting the diverse challenges they face in adapting to evolving environmental conditions and extreme weather events. At-risk populations can face compounding vulnerabilities when they possess intersectional risk factors based on their social identities. Climate change assessments and adaptation plans are more effective and robust when they consider the needs of higher risk populations and target adaptation actions accordingly.
Developing adaptation strategies: based on the findings of their CCHVAA, health authorities should develop adaptation strategies that address identified vulnerabilities and risks for their respective health regions. This can include developing early warning systems, supporting community awareness and preparedness, participating in adaptation planning with other community partners, and implementing other interventions to mitigate the impact of climate change on health (including targeted interventions for at-risk populations).
Engaging stakeholders: health authorities can scale-up needed actions more quickly when they engage with a wide range of stakeholders, such as health system planners, community care givers, emergency management officials, clinicians, local government officials, municipal staff, academia, and other relevant organizations, to develop and implement the adaptation plan. Stakeholders' insights on the local health impacts of climate change can help identify effective strategies for adaptation.
Engaging with local communities: health authorities should engage with local communities to understand their concerns, experiences, and perspectives on the health impacts of climate change. This will help inform adaptation strategies so that they align with local needs.
Using a multidisciplinary approach: health authorities may find that a multidisciplinary approach is helpful, particularly one that involves collaborating with experts from different fields, such as environmental science, epidemiology, and others, to ensure that climate change assessments and adaptation planning are comprehensive and consider a broad range of applicable factors.
Communicating findings: Meaningful, inclusive, and effective efforts to reduce climate change impacts rely on the efforts of health authorities to communicate relevant information to stakeholders and the public in a clear and accessible manner. This raises awareness of the health impacts of climate change and promotes informed decision-making and action.
Monitoring and evaluation: A resilient health system is based upon proactive monitoring and evaluation of the effectiveness of adaptation actions over time. Monitoring and evaluation activities benefit from information from regular vulnerability assessments that provide health authorities with additional information to see how the local context is changing and affecting health risks. This will allow for needed adjustment and course corrections as climate change impacts increase and climate surprises affect communities and populations.
Resources
- GCcollab (closed group for Canadian health authorities)
- CCHA 2022
- Health Canada V&A Workbook
- Health Canada Knowledge to Action Guide
- Ontario Climate Change and Health Toolkit
- WHO Framework for Climate Vulnerability Assessments
- Map of Adaptation Actions (includes pilot HealthADAPT program projects)
- HealthADAPT digital case stories
- WHO ClimaHealth Portal
- Global Consortium Pan American Climate Resilient Health Systems Course
References
Berry, P., & Schnitter, R., Health of Canadians in a Changing Climate: Advancing our Knowledge for Action (2022). Retrieved March 15, 2023, from https://changingclimate.ca/site/assets/uploads/sites/5/2022/02/CCHA-REPORT-EN.pdf.
Government of Canada. (2022, November 24). HealthADAPT. Retrieved March 15, 2023, from https://www.canada.ca/en/health-canada/programs/health-adapt.html.