Substance-related poisoning hospitalizations among people who are pregnant in Canada
Table of contents
- Background
- Definitions included in this report
- Key findings
- Summary
- Acknowledgements
- Disclaimer
- Suggested citation
- Technical notes
- Appendix A
- Appendix B
- References
Background
Canada is currently experiencing an overdose crisis. Alongside ongoing surveillance, the Public Health Agency of Canada (PHAC) releases targeted analytical reports on specific topics concerning substance-related harms to address gaps identified by stakeholders.
A recent Canadian report indicated that the prevalence of self-reported opioid use during pregnancy was 1.4%, while 3.1% of individuals reported using cannabis during pregnancy Footnote 1. Substance use during pregnancy presents significant risks to both the pregnant individual and the baby. Individuals who use substances during pregnancy face a higher risk of obstetric complications such as pre-term birth, low birth weight and stillbirth Footnote 2 Footnote 3 Footnote 4. Infants who are exposed to substances before birth may experience a greater likelihood of developing neonatal abstinence syndrome, birth defects and neurodevelopmental issues Footnote 2 Footnote 3 Footnote 5 Footnote 6. The stigma associated with substance use, particularly during pregnancy, may prevent pregnant individuals from seeking appropriate support and treatment Footnote 6. This may further deepen existing social and health inequalities Footnote 6. Despite the importance of maternal and infant health, there are few data on substance-related poisonings among pregnant individuals in Canada.
The objective of this analysis is to examine trends in substance-related poisoning hospitalizations among pregnant individuals in Canada (excluding Quebec) from 2009 to 2022, including hospitalization characteristics and outcomes.
The results of this analysis can be used to inform prevention strategies, treatment and recovery systems, and harm reduction interventions in Canada.
Definitions included in this report
Poisoning hospitalization
A substance poisoning harm (or "overdose") resulting from accidental, intentional, or undetermined manner of substance use. Multiple substances may be involved, either intentionally consumed together or accidentally ingested due to the presence of undisclosed substances. Poisonings may be due to:
- alcohol
- cannabis
- opioids
- stimulants
- hallucinogens
- psychotropic drugs
- other depressants
People who are pregnant
People who have an embryo, fetus or offspring developing in their body.
For more information on these definitions, please refer to the Technical notes section.
Key findings
Trends by year
From January 2009 to December 2022, there were 419 substance-related poisoning hospitalizations in Canada (excluding Quebec) among people who were pregnant (Figure 1). The highest number of such hospitalizations occurred in 2021, totaling 62 hospitalizations. This represents a 63% increase compared to the 38 hospitalizations among pregnant individuals for substance-related poisonings in 2020.
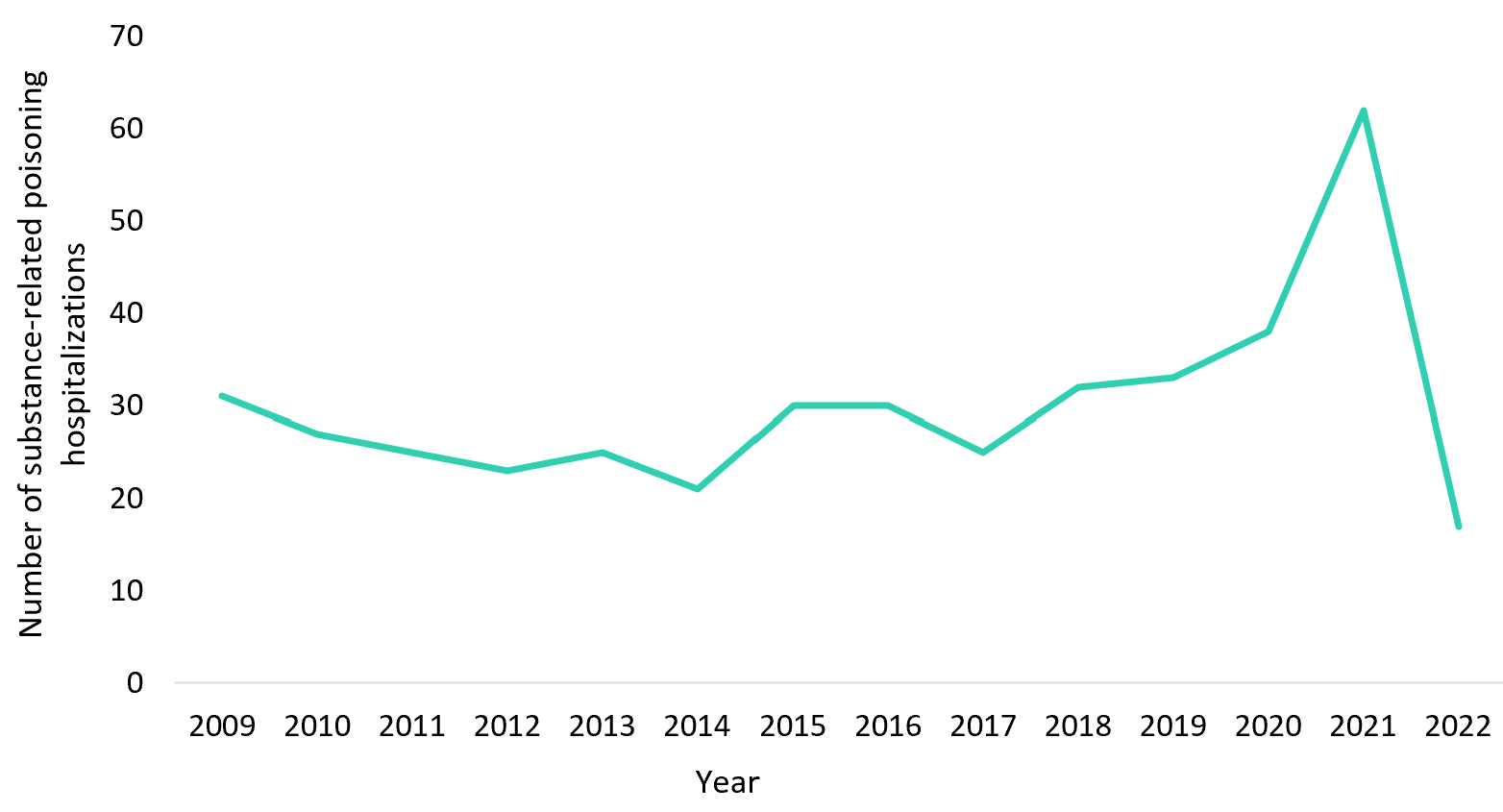
Figure 1 - Text description
| Calendar year | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | 2021 | 2022 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number of substance-related poisoning hospitalizations | 31 | 27 | 25 | 23 | 25 | 21 | 30 | 30 | 25 | 32 | 33 | 38 | 62 | 17 |
| Notes: Excludes data from Quebec. | ||||||||||||||
| Data sources: Discharge Abstract Database (DAD), 2009 to 2022, Canadian Institute for Health Information (CIHI). | ||||||||||||||
Note: Trends should be interpreted with caution since small numbers are reported and could make yearly fluctuations appear more pronounced.
Intention
Intention refers to the documented reason for the poisoning, which may rely on self-reporting, and is classified as accidental, intentional self-harm and undetermined. Between 2009 and 2022, almost half (47%) of substance-related poisoning hospitalizations among pregnant individuals were recorded as accidental. Poisonings that were recorded as intentional self-harm accounted for 38% of all poisonings, and 15% as an undetermined intention. Of note, despite yearly fluctuations during this time period, in the past 5 years (2018-2022) roughly 25% of substance-related poisoning hospitalizations were recorded as intentional self-harm.
The proportion of substance-related poisoning hospitalizations among pregnant individuals which were accidental varied from 2009 to 2022 (Figure 2). There appears to be a trend suggesting that the proportion of accidental poisonings among pregnant individuals may be increasing, with the highest percentages recorded in 2021 at 69%.
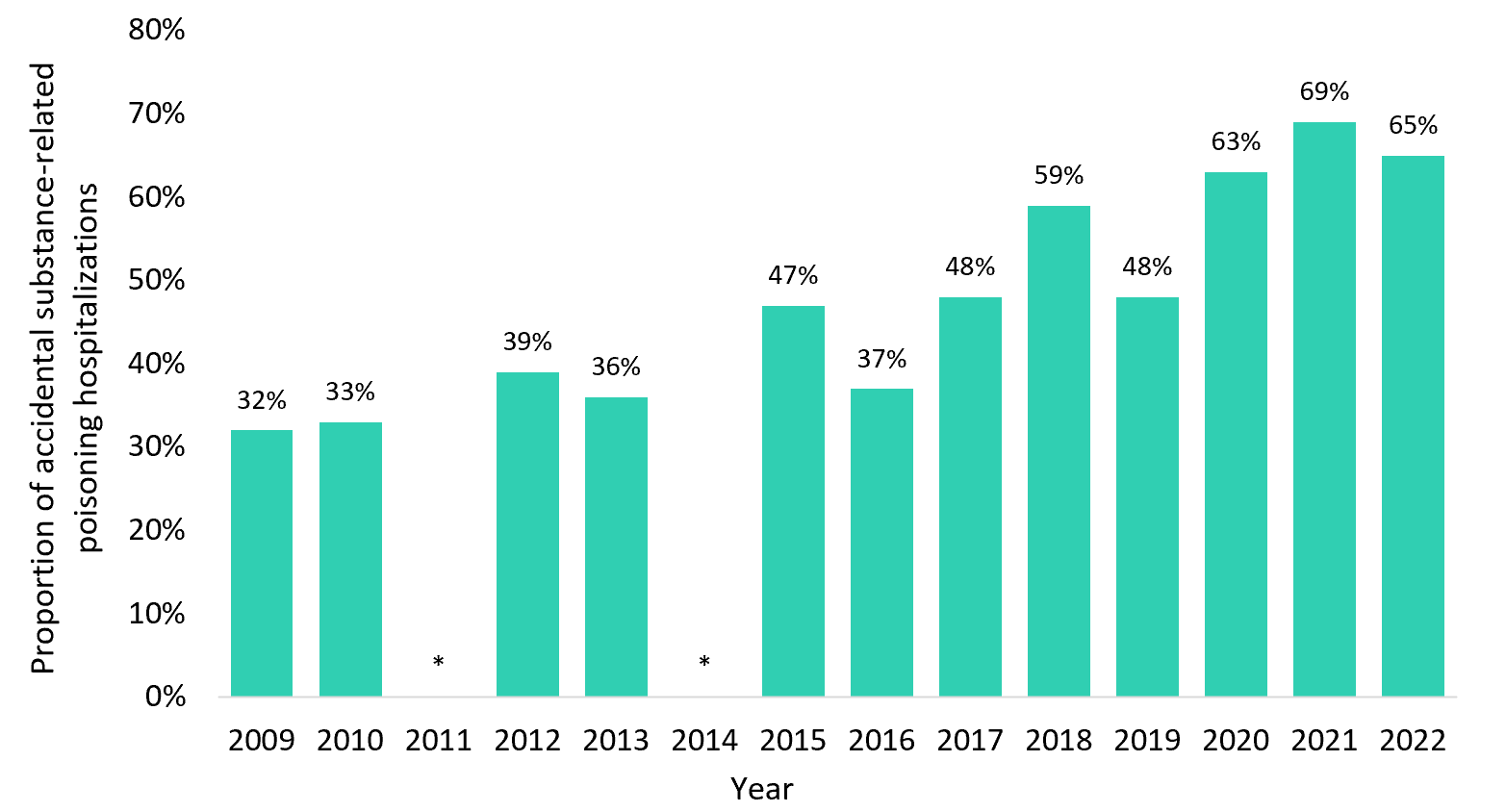
Figure 2 - Text description
| Calendar year | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | 2021 | 2022 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % (N) | % (N) | % (N) | % (N) | % (N) | % (N) | % (N) | % (N) | % (N) | % (N) | % (N) | % (N) | % (N) | % (N) | |
| Proportion of poisoning hospitalizations which were accidental | 32% (10) | 33% (9) | * | 39% (9) | 36% (9) | * | 47% (14) | 37% (11) | 48% (12) | 59% (19) | 48% (16) | 63% (24) | 69% (43) | 65% (11) |
| Notes: Excludes data from Quebec. *Counts less than five have been suppressed as per CIHI privacy guidelines. |
||||||||||||||
| Data sources: Discharge Abstract Database (DAD), 2009 to 2022, Canadian Institute for Health Information (CIHI). | ||||||||||||||
Note: Trends should be interpreted with caution since small numbers are reported and could make yearly fluctuations appear more pronounced.
Poisonings involving opioids
Between 2009 and 2022, there was considerable variability in the proportion of substance-related poisoning hospitalizations involving opioids among pregnant individuals (Figure 3). Notably, there was a peak in 2021 (89%) and the proportion remained high in 2022 (71%). This suggests a recent rise in opioid involvement in substance-related poisoning hospitalizations.
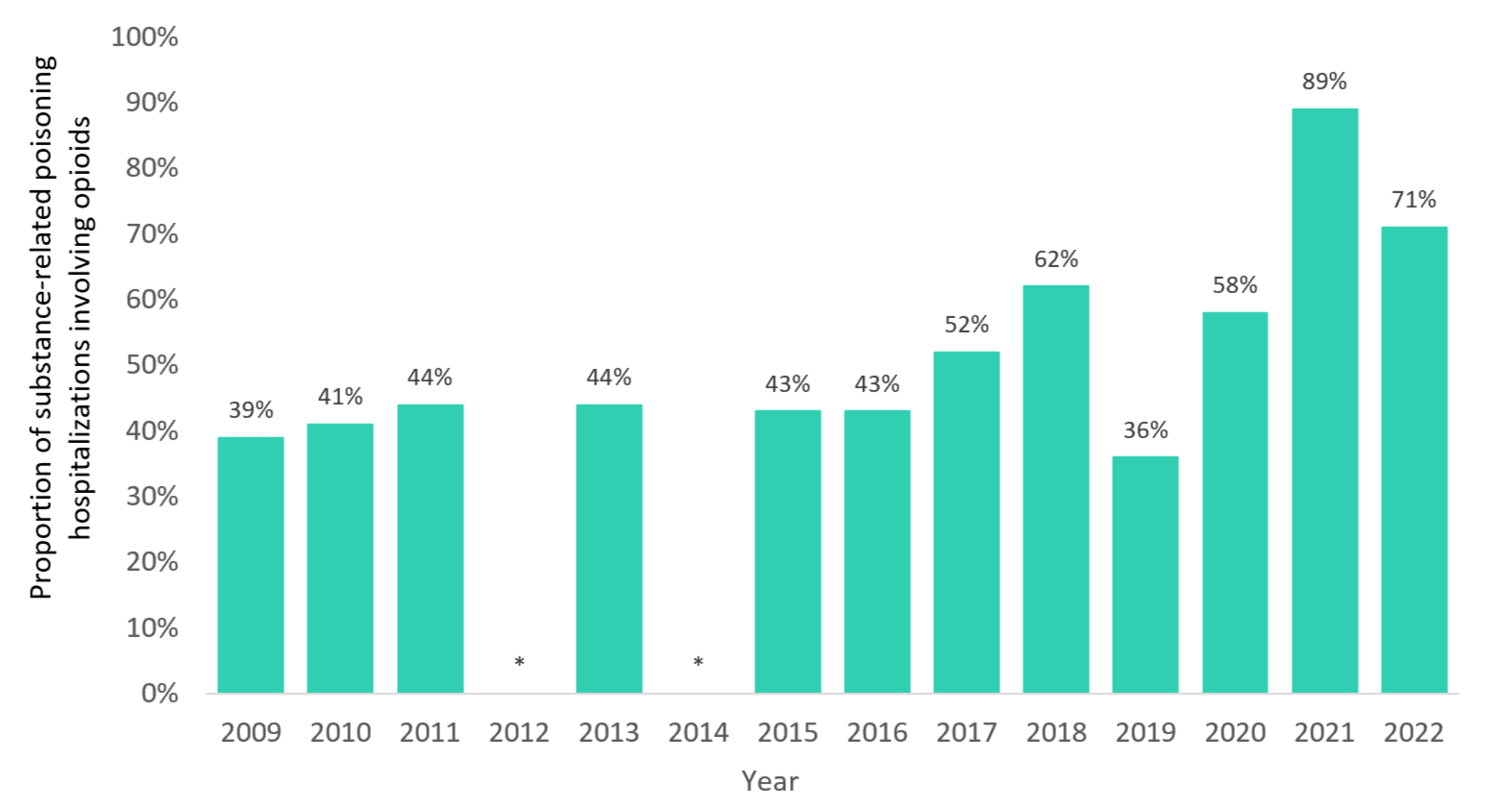
Figure 3 - Text description
| Calendar year | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | 2021 | 2022 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % (N) | % (N) | % (N) | % (N) | % (N) | % (N) | % (N) | % (N) | % (N) | % (N) | % (N) | % (N) | % (N) | % (N) | |
| Proportion of substance-related poisoning hospitalizations involving opioids | 39% (12) | 41% (11) | 44% (11) | * | 44% (11) | * | 43% (13) | 43% (13) | 52% (13) | 62% (20) | 36% (12) | 58% (22) | 89% (55) | 71% (12) |
| Notes: Excludes data from Quebec. *Counts less than five have been suppressed as per CIHI privacy guidelines. |
||||||||||||||
| Data sources: Discharge Abstract Database (DAD), 2009 to 2022, Canadian Institute for Health Information (CIHI). | ||||||||||||||
Note: Trends should be interpreted with caution since small numbers are reported and could make yearly fluctuations appear more pronounced.
Hospitalization characteristics and outcomes
Age
In Canada (excluding Quebec) between 2009 and 2022, the highest proportion of hospitalizations for substance-related poisonings among pregnant individuals was observed among people 26 to 30 years old (30%) (Figure 4). Pregnant individuals 21 to 25 years old accounted for 20% of substance-related poisoning hospitalizations. Hospitalizations among those who were 0 to 20 years old (14%) and 36 years and older (14%) were less common. The median age of pregnant individuals hospitalized for a substance-related poisoning hospitalization was 28 years old.

Figure 4 - Text description
| Age categories | 0 to 20 years | 21 to 25 years | 26 to 30 years | 31 to 35 years | 36 years and older |
|---|---|---|---|---|---|
| % (N) | % (N) | % (N) | % (N) | % (N) | |
| Proportion of substance-related poisoning hospitalizations | 14% (58) | 20% (84) | 30% (126) | 22% (91) | 14% (60) |
| Notes: Excludes data from Quebec. | |||||
| Data sources: Discharge Abstract Database (DAD), 2009 to 2022, Canadian Institute for Health Information (CIHI). | |||||
Length of stay
The total length of stay in hospital includes the number of days a patient spends in acute inpatient care (receiving treatment for a disease or severe episode of illness) and alternate level of care (occupying a bed without intensive services) Footnote 7 Footnote 8. Between 2009 and 2022, the average total length of stay for pregnant individuals hospitalized for a substance-related poisoning in Canada (excluding Quebec) was 5.5 days (median = 2 days). In comparison, the average length of stay among the total population hospitalized for a substance-related poisoning was 6.3 days (median 2 = days) during the same time period.
Special Care Unit (Intensive Care)
The Special Care Unit (SCU) is an organized system providing specialized medical care to critically-ill patients. This care includes life support and monitoring, which may involve mechanical ventilation Footnote 9. Among hospitalizations between 2009 and 2022 for substance-related poisonings among pregnant individuals, 31% were admitted to an SCU. In comparison, 34% of substance-related poisoning hospitalizations among the total population were admitted to an SCU during the same time period.
Discharge Disposition
Discharge disposition describes the status of the patient when they leave the hospital or where they are discharged to. Among pregnant individuals hospitalized for substance-related poisonings between 2019 and 2022, 56% were discharged home. A smaller proportion (13%) of hospitalizations resulted in the patient being transferred to other departments or facilities, for instance to emergency department, ambulatory or inpatient care, group/supportive living or a correctional facility, 28% resulted in a patient-initiated discharge, and less than five patients died in hospital.
Summary
Canada is currently facing a nationwide overdose crisis and requires a better understanding of substance-related harms, including those impacting the health of parents and babies. This knowledge can help inform effective clinical and public health actions.
There were 419 substance-related poisoning hospitalizations among pregnant individuals between 2009 to 2022 in Canada (excluding Quebec), with the greatest number of hospitalizations observed in 2021. This trend is consistent with PHAC's surveillance data on opioid-related poisoning hospitalizations in the total population that reports a slight increase in 2021 and a decrease in 2022 Footnote 10. The trend described in this report should be interpreted with caution since small numbers are reported and could make yearly fluctuations appear more pronounced.
In recent years, there has been a large proportion of substance-related poisoning hospitalizations among pregnant people that were classified as accidental. Opioids may have driven some of the increase in these hospitalizations, as shown by the increase in the proportion of poisonings involving opioids in recent years. Additionally, most substance-related poisoning hospitalizations affected pregnant individuals 26 to 30 years old.
These findings highlight the importance of implementing substance-use stigma reduction approaches (for instance, approaches that are non-judgemental and respectful), harm reduction services and promoting equity-oriented care to support the pregnant population Footnote 11Footnote 12 Footnote 13 Footnote 14. Further research is needed to understand the long-term effects of substance-related poisonings during pregnancy and to strengthen support systems for pregnant individuals who use drugsFootnote 15.
The Government of Canada remains committed to collaborating with partners to explore opportunities for improving data collection and analysis. This ongoing effort aims to inform prevention strategies, treatment and recovery systems and harm reduction interventions that may help to reduce substance-related harms across Canada.
Acknowledgements
We would like to acknowledge the Canadian Institute for Health Information (CIHI) for collecting and providing the data used in this report. We recognize that the data in this report may represent stories of pain, grief and trauma. This report cannot adequately reflect the burden borne by Canadians. We acknowledge all those impacted by substance use, and those who work to save lives and reduce substance related harms on individuals and communities.
Disclaimer
Parts of this material are based on data and information compiled and provided by the CIHI. However, the analyses, conclusions, opinions and statements expressed herein are those of the authors, and not necessarily those of CIHI.
Suggested citation
Substance-related poisonings hospitalizations among people who are pregnant in Canada. Ottawa: Public Health Agency of Canada; December 2023. https://www.canada.ca/en/health-canada/services/opioids/data-surveillance-research/substance-related-poisonings-hospitalizations-people-pregnant-canada.html
Technical notes
Methodology
Data from the Canadian Institute for Health Information's Discharge Abstract Database (DAD) for the period of January 2009 to December 2022 were analyzed for this descriptive report. Closed year data from the DAD were used to report trends of substance-related poisoning hospitalizations between 2009 and 2022.
This analysis was limited to acute inpatient hospital discharges, which are nationally representative across Canada, except for Quebec. This analysis presents the number of acute inpatient hospital discharges for people who are pregnant with a substance-related poisoning. It does not account for transfers, which may have occurred between acute inpatient care facilities.
The International Classification of Diseases and Related Health Problems, Tenth Revision, Canada (ICD-10-CA) is used in the DAD to capture diagnoses from the patient's hospitalization. It is the national standard for reporting morbidity statistics. More information on the DAD and ICD-10-CA coding can be found on CIHI's website.
Identifying hospitalizations for substance poisonings
The methodology for identifying hospitalizations for substance poisonings was adapted from CIHI's Opioid-related Harms in Canada report and Hospital Stays for Harm Caused by Substance Use Indicator.
A complete listing of all ICD-10-CA diagnosis codes used to identify substance-related poisonings presented in this report can be found in Appendix A. Poisonings from the following substances of interest were included in the scope of this analysis:
- opioids
- stimulants
- cannabis
- hallucinogens
- alcohol
- other depressants
- psychotropic drugs
Information on these substance-related poisonings is extracted from patient charts by trained coders, which may be based on toxicological analysis or patient self-report.
Analyses were restricted to the following significant diagnosis types:
- Most responsible diagnosis ("M")
- Pre-admit comorbidity ("1")
- Post-admit comorbidity ("2")
- Service transfer diagnosis ("W", "X", and "Y")
These significant diagnosis types capture hospitalizations in which the poisoning was considered influential to the time spent and treatment received by the patient in hospital. Secondary diagnoses that do not meet the criteria for significance (diagnosis type 3) were excluded. A diagnosis prefix of "Q", indicating unconfirmed diagnoses or query diagnoses recorded by the physician, were excluded from these analyses as the scope of the analysis was concerned with confirmed cases of substance poisonings only. Records indicating the patient was admitted to the facility as a cadaveric donor were also excluded, along with stillbirths.
Identifying hospitalizations for pregnancy
Pregnancy status upon admission was identified using ICD-10-CA codes using the following codes:
- Z321: Pregnancy confirmed
- Z33: Pregnant state, incidental
- Z34: Encounter for supervision of normal pregnancy
- Z35: Supervision of high-risk pregnancy
- Z36: Encounter for antenatal screening of mother
- Z37: Outcome of delivery
- O: Obstetric codes
- Where the 6th digit of the ICD-10-CA code was not "4: postpartum condition or complication"
When examining recorded pregnancy during the patient's substance-related poisoning hospitalization, the following diagnosis types were included:
- Most responsible diagnosis ("M")
- Pre-admit comorbidity ("1")
- Post-admit comorbidity ("2")
- Secondary diagnosis ("3")
- Service transfer diagnosis ("W", "X", "Y")
- Query or unconfirmed diagnosis ("Q")
Of note, diagnosis types of "3" and diagnosis prefix of "Q" were included as the scope of this analysis was concerned with capturing all possible pregnant individuals.
Identifying intention of poisoning
When a patient experiences a poisoning, coders are directed to assign an external cause ICD-10-CA code to indicate the intention or reason for the poisoning. Each poisoning of interest for this analysis was further examined by the documented intention for the poisoning. They were then classified in the following three groups in line with the Intentional Statistical Classification of Diseases and Related Health Problems, Tenth Revision, Canada:
Accidental
A substance-related poisoning hospitalization that is considered to be non-intentional in nature and is identified by an associated external cause ICD-10-CA code of X41, X42 or X45.
Intentional self-harm
A substance-related poisoning hospitalization that occurred as a result of purposely self-inflicted harm and is identified by an associated external cause ICD-10-CA code of X61, X62 or X65.
Undetermined
A substance-related poisoning hospitalization which has been documented to be of undetermined or unknown intention and is identified by an associated external cause ICD-10-CA code of Y11, Y12 or Y15.
In line with CIHI coding standards, a diagnosis type of "9" was used to identify intention using external cause codes. External cause codes are mandatory to assign with codes within the range S00-T98, "Injury, poisoning, and certain other consequences of external causes". External cause codes for intention with a diagnosis prefix of "Q", indicating unconfirmed diagnoses or query diagnoses, were included when identifying intention as the scope of this analysis was concerned with capturing suspected diagnoses for intention.
A list of all poisoning types of interest for this analysis and their associated intention codes can be found in Appendix B.
Identifying discharge disposition
Discharge disposition refers to both the location where the patient was discharged to and the patient's status at the time of discharge. This analysis included hospitalizations that occurred from 2019 to 2022. Category definitions varied from 2009 to 2018 and were therefore excluded from this analysis. A total of four discharge categories were investigated.
- Transferred: Identified by a field value of 10, 20, 30, 40, or 90
- Discharged home: Identified by a field value of 04 or 05
- Patient-initiated discharge: Identified by a field value of 61, 62, 65, 66, or 67
- Died in hospital: Identified by a field value of 72, 73, or 74
Identifying substance poisoning hospitalizations among the total population
Hospitalization characteristics such as Special Care Unit admission and length of stay were compared among pregnant people and the total population. When identifying hospitalizations for a substance-related poisoning among the total population, hospitalizations with a length of stay for more than 365 days were excluded.
Limitations
- The trends described in this report should be interpreted with caution since small numbers are reported and could make yearly fluctuations appear more pronounced.
- This report focuses exclusively on hospitalization data and does not include emergency department or Emergency Medical Services (EMS) data where substance-related poisonings may be treated. Therefore, this analysis does not capture the full scope of the issue surrounding substance-related poisonings among pregnant individuals in Canada.
- Determining intention can rely on self-reported information which patients may not be willing to disclose due to various reasons, or are unable to disclose due to disability or death.
- Poisonings are classified as accidental unless there is clear documentation of intentional self-harm or undetermined intention. This may reflect an overrepresentation of accidental poisonings.
- This analysis focuses on the number of hospitalizations for substance-related poisonings rather than the number of individuals with substance-related poisonings and therefore does not represent the overall prevalence of substance-related poisonings among pregnant individuals.
- This report does not include data from Quebec.
- Data released by provinces and territories may differ from the data provided in this report due to the availability of updated data, differences in the type of data reported, the use of alternate case definitions, differences in time periods presented, differences in population estimates used for calculations, and other factors.
- It was not possible to determine which poisonings, if applicable, were a result of pharmaceutical substances, non-pharmaceutical substances, or a combination of both. It was also not possible to determine whether poisonings involving multiple substances were a result of intended use of multiple substances at the same time or close in time, or if a substance unknowingly contained other substances.
- The DAD captures patients discharged from hospital. Patients who were still hospitalized during the analysis year are not captured in this report.
Data suppression
Values representing less than five hospitalizations are suppressed according to CIHI's privacy guidelines.
Appendix A
List of ICD-10-CA codes used to identify substance-related poisoning hospitalizations
| Poisoning from substance | ICD-10-CA code and descriptions |
|---|---|
| Alcohol | T51 Toxic effect of alcohol |
| Cannabis | T40.7 Poisoning by cannabis (derivatives) |
| Other central nervous system (CNS) depressants | T42.3 Poisoning by barbiturates T42.4 Poisoning by benzodiazepines T42.6 Poisoning by other antiepileptic and sedative - hypnotic drugs T42.7 Poisoning by other antiepileptic and sedative - hypnotic drugs, unspecified |
| Central nervous system (CNS) stimulants | T40.5 Poisoning by cocaine T43.6 Poisoning by psychostimulants with abuse potential (excludes cocaine) Note: this category includes poisonings from methamphetamine |
| Hallucinogens | T40.8 Poisoning by lysergide (LSD) T40.9 Poisoning by other and unspecified psychodysleptics (hallucinogens) |
| Opioids | T40.0 Poisoning by opium T40.1 Poisoning by heroin T40.2 Poisoning by other opioids T40.20 Poisoning by codeine and derivatives T40.21 Poisoning by morphine T40.22 Poisoning by hydromorphone T40.23 Poisoning by oxycodone T40.28 Poisoning by other opioids not elsewhere classified T40.3 Poisoning by methadone T40.4 Poisoning by other synthetic narcotics T40.40 Poisoning by fentanyl and derivatives T40.41 Poisoning by tramadol T40.48 Poisoning by other synthetic narcotics not elsewhere classified T40.6 Poisoning by other and unspecified narcotics |
| Other/unspecified psychotropic drug | T43.8 Poisoning by other psychotropic drugs, not elsewhere classified T43.9 Poisoning by psychotropic drug, unspecified |
Appendix B
Associated ICD-10-CA codes used to identify intention for poisonings
| ICD-10-CA poisoning codes | Associated ICD-10-CA intention codes (external cause codes) |
|---|---|
| Other central nervous system depressants (T42.3, T42.4, T42.6, T42.7) Poisoning by psychostimulants with abuse potential (T43.6) Other/unspecified psychotropic drugs (T43.8, T43.9) |
Accidental: X41 Intentional: X61 Undetermined: Y11 |
| Opioids (T40.0, T40.1, T40.2, T40.3, T40.4, T40.6) Cocaine (T40.5) Cannabis (T40.7) Hallucinogens (T40.8, T40.9) |
Accidental: X42 Intentional: X62 Undetermined: Y12 |
| Alcohol (T51) | Accidental: X45 Intentional: X65 Undetermined: Y15 |
References:
- Footnote 1
-
Grywacheski V, Ali J, Baker MM, Gheorghe M, Wong SL, Orpana HM. Opioid and cannabis use during pregnancy and breastfeeding in relation to sociodemographics and mental health status: a descriptive study. Journal of Obstetrics and Gynaecology Canada. 2021 Mar 1;43(3):329-36. https://doi.org/10.1016/j.jogc.2020.09.017
- Footnote 2
-
Camden A, Ray JG, To T, Gomes T, Bai L, Guttmann A. Identification of prenatal opioid exposure within health administrative databases. Pediatrics. 2021 Jan 1;147(1). https://doi.org/10.1542/peds.2020-018507
- Footnote 3
-
Miller C, Grynspan D, Gaudet L, Ferretti E, Lawrence S, Moretti F, Lafreniere A, McGee A, Lattuca S, Black A. Maternal and neonatal characteristics of a Canadian urban cohort receiving treatment for opioid use disorder during pregnancy. Journal of developmental origins of health and disease. 2019 Feb;10(1):132-7.
- Footnote 4
-
Corsi DJ, Hsu H, Fell DB, Wen SW, Walker M. Association of maternal opioid use in pregnancy with adverse perinatal outcomes in Ontario, Canada, from 2012 to 2018. JAMA Network Open. 2020 Jul 1;3(7):e208256-. https://doi.org/10.1001/jamanetworkopen.2020.8256
- Footnote 5
-
Neonatal abstinence syndrome in Canada: a descriptive analysis of hospitalization data [Internet]. Ottawa, ON: Public Health Agency of Canada; 2021 [cited 2023Sep20]. Available from: www.canada.ca/en/health-canada/services/opioids/data-surveillance-research/neonatal-abstinence-syndrome-descriptive-analysis-hospitalization.html
- Footnote 6
-
Gopman S. Prenatal and postpartum care of women with substance use disorders. Obstetrics and Gynecology Clinics. 2014 Jun 1;41(2):213-28. https://doi.org/10.1016/j.ogc.2014.02.004
- Footnote 7
-
Guidelines to Support ALC Designation [Internet]. Ottawa, ON: Canadian Institute for Health Information [cited 2023Sep6]. Available from: https://www.cihi.ca/en/guidelines-to-support-alc-designation#:~:text=Alternate%20level%20of%20care%20(ALC,patients%20in%20acute%20inpatient%20care
- Footnote 8
-
Acute Care [Internet]. Ottawa, ON: Canadian Institute for Health Information [cited 2023Sep6]. Available from: https://www.cihi.ca/en/acute-care
- Footnote 9
-
Marshall JC, Bosco L, Adhikari NK, Connolly B, Diaz JV, Dorman T, Fowler RA, Meyfroidt G, Nakagawa S, Pelosi P, Vincent JL. What is an intensive care unit? A report of the task force of the World Federation of Societies of Intensive and Critical Care Medicine. Journal of critical care. 2017 Feb 1;37:270-6. https://doi.org/10.1016/j.jcrc.2016.07.015
- Footnote 10
-
Federal, provincial, and territorial Special Advisory Committee on the Epidemic of Opioid Overdoses. Opioid- and Stimulant-related Harms in Canada [Internet]. Ottawa, ON: Public Health Agency of Canada 2023 [cited 2023Sep26]. Available from: https://health-infobase.canada.ca/substance-related-harms/opioids-stimulants/
- Footnote 11
-
Principles of perinatal care for substance using women and their newborns [Internet]. British Columbia: Reproductive Care Program [cited 2023Nov8]. Available from: http://www.perinatalservicesbc.ca/Documents/Guidelines-Standards/Maternal/PrinciplesofCareSubstanceUse.pdf
- Footnote 12
-
Barnett ER, Knight E, Herman RJ, Amarakaran K, Jankowski MK. Difficult binds: A systematic review of facilitators and barriers to treatment among mothers with substance use disorders. Journal of Substance Abuse Treatment. 2021 Jul 1;126:108341. https://doi.org/10.1016/j.jsat.2021.108341
- Footnote 13
-
Rutman D, Hubberstey C, Poole N, Schmidt RA, Van Bibber M. Multi-service prevention programs for pregnant and parenting women with substance use and multiple vulnerabilities: Program structure and clients' perspectives on wraparound programming. BMC Pregnancy and Childbirth. 2020 Dec;20:1-4. https://doi.org/10.1186/s12884-020-03109-1
- Footnote 14
-
Pregnancy and substance use: A harm reduction toolkit [Internet]. National Harm Reduction Coalition [cited 2023Nov8]. Available from: https://harmreduction.org/issues/pregnancy-and-substance-use-a-harm-reduction-toolkit/
- Footnote 15
-
Licit and Illicit Drug Use during Pregnancy: Maternal Neonatal and Early Childhood Consequences [Internet]. Ottawa, ON: Canadian Centre on Substance Use and Addiction [cited 2023Sep6]. Available from: https://www.ccsa.ca/sites/default/files/2019-05/CCSA-Drug-Use-during-Pregnancy-Summary-2013-en.pdf