CompassRx, 8th Edition
Annual Public Drug Plan Expenditure Report, 2020/21

ISSN 2369-0518
Cat. No. H79-6E-PDF
January 2023
PDF - 908 KB
Table of Contents
- Executive Summary
- Key Findings
- Introduction
- Methods
- Limitations
- Analyses
- 1. Trends in Prescription Drug Expenditures, 2015/16 to 2020/21
- 2. The Drivers of Drug Costs, 2019/20 to 2020/21
- 3. The Drivers of Dispensing Costs, 2019/20 to 2020/21
- References
- Appendix A: Drug Reviews and Approvals
- Appendix B: Distribution of Patients on Biosimilar Initiative Medicines by Jurisdiction, 2020/21
- Appendix C: Biosimilar Switching Initiatives by Canadian Public Payers
- Appendix D: Top 50 Patented Medicines by Drug Cost, NPDUIS Public Drug Plans, 2020/21 ($million)
- Appendix E: Top 50 Multi-Source Generic Drugs by Drug Cost, NPDUIS Public Drug Plans, 2020/21 ($million)
- Appendix F: Top 50 Single-Source Non-Patented Medicines by Drug Cost, NPDUIS Public Drug Plans, 2020/21 ($thousand)
- Appendix G: Top 50 Manufacturers by Drug Cost, NPDUIS Public Drug Plans, 2020/21 ($million)
About CompassRx
CompassRx is an annual Patented Medicine Prices Review Board (PMPRB) publication that explores trends in prescription drug expenditures in Canadian public drug plans. It focuses on the pressures that contribute to the annual change in drug and dispensing costs, including the switch in use between lower- and higher-priced drugs and changes in the beneficiary population, drug prices, and the volume of drugs used, as well as other key factors.
About the PMPRB
The Patented Medicine Prices Review Board (PMPRB) is an independent quasi-judicial body established by Parliament in 1987. The PMPRB has a dual regulatory and reporting mandate: to ensure that prices at which patentees sell their patented medicines in Canada are not excessive; and to report on pharmaceutical trends of all medicines and on research and development spending by patentees.
The NPDUIS Initiative
The National Prescription Drug Utilization Information System (NPDUIS) is a research initiative established by federal, provincial, and territorial Ministers of Health in September 2001. It is a partnership between the PMPRB and the Canadian Institute for Health Information (CIHI).
Pursuant to section 90 of the Patent Act, the PMPRB has the mandate to conduct analysis that provides decision makers with critical information and intelligence on price, utilization, and cost trends so that Canada’s healthcare system has more comprehensive and accurate information on how medicines are being used and on sources of cost pressures.
The specific research priorities and methodologies for NPDUIS are established with the guidance of the NPDUIS Advisory Committee and reflect the priorities of the participating jurisdictions, as identified in the NPDUIS Research Agenda. The Advisory Committee is composed of representatives from public drug plans in British Columbia, Alberta, Saskatchewan, Manitoba, Ontario, New Brunswick, Nova Scotia, Prince Edward Island, Newfoundland and Labrador, Yukon, the Non-Insured Health Benefits (NIHB) Program, and Health Canada. It also includes observers from CIHI, the Canadian Agency for Drugs and Technologies in Health (CADTH), the Ministère de la Santé et des Services sociaux du Québec (MSSS), and the pan-Canadian Pharmaceutical Alliance (pCPA) Office.
Acknowledgements
This report was prepared by the Patented Medicine Prices Review Board (PMPRB) as part of the National Prescription Drug Utilization Information System (NPDUIS) initiative.
The PMPRB wishes to acknowledge the members of the NPDUIS Advisory Committee for their expert oversight and guidance in the preparation of this report. Please note that the statements and findings for this report do not necessarily reflect those of the members or their organizations.
Appreciation goes to Yvonne Zhang for leading this project, and to Tanya Potashnik, Kevin Pothier and Jared Berger for their oversight in the development of the report. The PMPRB also wishes to acknowledge the contribution of the analytical staff Lokanadha Cheruvu and Jun Yu, and editorial staff Shirin Paynter and Ronja Francoeur.
Disclaimer
NPDUIS operates independently of the regulatory activities of the Board of the PMPRB. The research priorities, data, statements, and opinions expressed or reflected in NPDUIS reports do not represent the position of the PMPRB with respect to any regulatory matter. NPDUIS reports do not contain information that is confidential or privileged under sections 87 and 88 of the Patent Act, and the mention of a medicine in an NPDUIS report is not and should not be understood as an admission or denial that the medicine is subject to filings under sections 80, 81, or 82 of the Patent Act or that its price is or is not excessive under section 85 of the Patent Act.
Although based in part on data provided by the Canadian Institute for Health Information (CIHI), the statements, findings, conclusions, views, and opinions expressed in this report are exclusively those of the PMPRB and are not attributable to CIHI.
Contact Information
Patented Medicine Prices Review Board
Standard Life Centre
Box L40
333 Laurier Avenue West Suite 1400
Ottawa, ON K1P 1C1
Tel.: 1-877-861-2350
TTY 613-288-9654
Email: PMPRB.Information-Renseignements.CEPMB@pmprb-cepmb.gc.ca
Web: https://www.canada.ca/en/patented-medicine-prices-review.html
Suggested Citation
Patented Medicine Prices Review Board. (2023). CompassRx, 8th edition: Annual Public Drug Plan Expenditure Report, 2020/21. Ottawa: PMPRB.
Executive Summary
Prescription drug expenditures for the NPDUIS public drug plans increased sizably by 4.2% in 2020/21, a faster pace than the 1.3% annual change to the Consumer Price Index (CPI) in Health and Personal CareReference I, with varying rates of change in its two main components: drug costs (which saw an increase of 5.3%) and dispensing costs (which saw a decrease of 0.2%). The overall growth in prescription drug expenditures continued to be primarily driven by notable increases in the use of higher-cost drugs.
The PMPRB’s CompassRx report monitors and analyzes the cost pressures driving changes in prescription drug expenditures in Canadian public drug plans. This eighth edition of CompassRx provides insight into the factors driving growth in drug and dispensing costs in 2020/21, as well as a retrospective review of recent trends in public drug plan costs and utilization.
The main data source for this report is the National Prescription Drug Utilization Information System (NPDUIS) Database at the Canadian Institute for Health Information (CIHI), which includes data for the following jurisdictions: British Columbia, Alberta, Saskatchewan, Manitoba, Ontario, New Brunswick, Nova Scotia, Prince Edward Island, Newfoundland and Labrador, Yukon, and the Non-Insured Health Benefits Program.
The findings from this report will inform policy discussions and aid decision makers in anticipating and responding to evolving cost pressures.
Key Findings
The key findings cover the three areas of analysis in CompassRx (see Analyses): the trends in prescription drug expenditures; the drivers of drug costs; and the drivers of dispensing costs.
Prescription drug expenditures
Prescription drug expenditures for the NPDUIS public drug plans grew by 4.2% in 2020/21, following a 3.7% increase in 2019/20.
- Between 2015/16 and 2020/21, the total prescription drug expenditures for Canada’s public drug plans rose by $2.5 billion, for a compound annual growth rate of 5.6%.
- Drug costs, which represent 82% of prescription drug expenditures, grew by 5.3% from 2019/20 to 2020/21, while dispensing costs, which account for the remaining 18% of expenditures, had no growth (-0.2%).
- The NPDUIS public drug plans paid an average of 87% of the total $12.3 billion in prescription costs for 289 million prescriptions dispensed to almost 6 million active beneficiaries in 2020/21.
- The overall NPDUIS public plan beneficiary population declined by 5.8% from 2019/20 to 2020/21. Approximately 366 thousand fewer Canadians filled a prescription for reimbursement to public drug plans, with the onset of the COVID-19 pandemic.
Drug costs
Drug cost growth for the NPDUIS public plans in 2020/21 was primarily driven by a greater use of higher-cost drugs combined with a sizable increase in the volume of drugs used per patient.
- Increase in drug costs was moderated, in part, by the decreasing use of direct acting antivirals (DAAs) for hepatitis C; savings from generic and biosimilar substitution; and a decrease in the number of active beneficiaries.
- The increased use of higher-cost drugs continued to be the most pronounced driver in 2020/21, pushing costs upward by 6.3%, while declining use of DAAs for hepatitis C had a pull effect of 2.1%.
- Nealy 60% of the total drug costs in 2020/21 were attributable to just 7% of public drug plan beneficiaries. High-cost drugs, which were used by 2.5% of beneficiaries, accounted for more than one third of costs.
- Due to COVID-19, a notable decrease in the number of active beneficiaries exerted a 2.3% downward demographic effect, though this was more than offset by a 4.6% upward volume effect.
- In 2020/21, the price change effect was negligible at less than 0.1%, while the substitution effect gained strength, pulling drug costs down by 1.4%.

Figure description
This column graph describes the key factors or effects that impacted the rates of change in drug costs across all NPDUIS public drug plans for each year from 2015/16 to 2020/21. Each column is broken out to give the positive or negative contribution of each effect: drug-mix; volume; demographic; price change; and substitution. The drug-mix effect for direct-acting antiviral (DAA) drugs for the treatment of hepatitis C is shown separately, as is the effect of the Ontario Health Insurance Plan Plus (OHIP+ ) initiative. The OHIP+ effect is not captured for 2020/21. Separate rows above and below the bar graph show the total positive push effect, negative pull effect, and net change for each year.
| 2015/16 | 2016/17 | 2017/18 | 2018/19 | 2019/20 | 2020/21 | |
|---|---|---|---|---|---|---|
|
OHIP+ |
- |
- |
1.5% |
4.7% |
-3.0% |
- |
|
Drug-mix, direct-acting antiviral (DAA) drugs |
8.0% |
-2.3% |
2.4% |
0.6% |
-1.6% |
-2.1% |
|
Drug mix, other drugs |
4.1% |
4.4% |
4.7% |
6.1% |
5.8% |
6.3% |
|
Volume |
1.2% |
1.0% |
1.0% |
-0.3% |
1.3% |
4.6% |
|
Demographic |
3.0% |
1.8% |
1.4% |
1.0% |
3.0% |
-2.3% |
|
Price change |
-1.8% |
-1.0% |
-1.1% |
-4.0% |
-0.5% |
<0.1% |
|
Substitution |
-2.3% |
-1.8% |
-1.3% |
-2.2% |
-0.6% |
-1.4% |
|
Total push effect |
16.2% |
7.2% |
11.0% |
12.4% |
10.2% |
11.0% |
|
Total pull effect |
-4.1% |
-5.1% |
-2.3% |
-6.5% |
-5.7% |
-5.8% |
|
Net change |
12.0% |
2.0% |
8.3% |
5.8% |
4.3% |
5.3% |
A table to the right of the graph provides additional information for each effect in 2020/21.
Drug-mix, other drugs |
The increased use of higher-cost drugs other than DAA drugs had the greatest push effect, with an overall impact of 6.3%. The number of high-cost medicines increased from 95 in 2015/16 to 135 in 2020/21. Biologic drugs captured an increasing share of total drug costs for the NPDUIS public plans, exceeding 30%. Antineoplastic and immunomodulating agents accounted for 29.5% of drug costs, the largest share held by a single therapeutic class. The 10 highest-cost drugs for 2020/21 all had average treatment costs exceeding $200,000. |
Volume |
The increased use of drugs contributed 4.3% to the growth in drug costs despite fewer active beneficiaries. |
Demographic |
In relation to the COVID-19 pandemic, a decrease in the number active beneficiaries exerted 2.0% downward demographic effect. |
Price change |
The influence of the price change effect has diminished to less than 0.1% in 2020/21. |
Substitution |
Shifts from brand-name to generic drugs or biosimilars pulled overall drug costs down by 1.4%. Biosimilars contributed more to the substitution effect than generic medicines. |
Drug-mix, |
The use of direct-acting antiviral (DAA) drugs for hepatitis C continued to decline in 2020/21, lowering total drug costs by 2.1%. |
Note: This analysis is based on publicly available pricing information. It does not reflect confidential drug price discounts negotiated by the pan-Canadian Pharmaceutical Alliance on behalf of the public plans.
Values for 2016/17 onward reflect a revised methodology; previous results have not been updated, as there would have been no notable change in the relative contribution of each effect. Data for Yukon is also included from 2016/17 onward. Data from the NIHB Program is not included in 2020/21.
Values may not add to totals due to rounding and the cross effect.
Data source: National Prescription Drug Utilization Information System Database, Canadian Institute for Health Information.
Dispensing costs
Dispensing costs in the NPDUIS public plans were virtually unchanged in 2020/21 relative to the previous year, owing primarily to temporary changes to dispensing frequency in many provinces during the COVID-19 pandemic and policy changes in Ontario.
- The overall change in dispensing costs was -0.2% (or -$4.9 million) in 2020/21, the first negative growth of dispensing costs in the past 6 years, though results varied among individual plans.
- The zero-dollar dispensing fee model introduced to the long-term care (LTC) program in Ontario had a significant impact on the decrease in dispensing costs, pulling costs down by 4.1% ($94 million) nationally, and by 7.0% in Ontario.
- A decrease in the number of active beneficiaries reduced costs by 1.3% in 2020/21 due to the onset of the COVID-19 pandemic, though this was more than offset by a 3.1% increase in the quantity of drugs dispensed to patients.
- Changes in prescription size following the temporary changes to policies on dispensing frequency during the COVID-19 pandemic pushed costs upward by a sizable 3.4% in 2020/21.
Introduction
Canadian public drug plan expenditures represent a significant portion of the overall healthcare budget. The Canadian Institute for Health Information (CIHI) reported that the total cost of prescription drugs in Canada was $34.3 billion in 2019, with the largest component financed by the public drug plans (43.6%) and the remainder paid by private plans (36.9%) or out of pocket by households and individuals (19.9%).Reference 1
This edition of the report focuses on the 2020/21 fiscal year, with a retrospective look at recent trends. The results of this study will aid stakeholders in anticipating and responding to the evolving cost pressures that affect Canada’s public drug plans. The analysis focuses on the public drug plans.
The analysis focuses on the public drug plans participating in the National Prescription Drug Utilization Information System (NPDUIS) initiative, which includes all provincial public plans (with the exception of Quebec), Yukon, and the Non-Insured Health Benefits (NIHB) Program. These plans account for approximately one third of the total annual spending on prescription drugs in Canada.
Each public drug plan reimburses eligible beneficiaries according to its own specific plan design and implements policies related to the reimbursement of drug prices and dispensing fees. Summaries of the plan designs and policies are available on the PMPRB website.
Health Canada, the PMPRB, and the Canadian Agency for Drugs and Technologies in Health (CADTH) are responsible for drug approvals, price reviews, and health technology assessments, respectively. Details of the 2020/21 approvals and reviews are provided in Appendix A of this report.
Methods
The main data source for this report is the National Prescription Drug Utilization Information System (NPDUIS) Database, developed by the Canadian Institute for Health Information (CIHI). This database houses pan-Canadian information on public drug programs, including claimslevel data collected from the plans that participate in the NPDUIS initiative. Data is reported on a fiscal year basis.
Results are presented for the following public drug plans: British Columbia, Alberta, Saskatchewan, Manitoba, Ontario, New Brunswick, Nova Scotia, Prince Edward Island, Newfoundland and Labrador, Yukon, and the Non- Insured Health Benefits (NIHB) Program.
The analysis focuses exclusively on data for beneficiaries that met their deductible and received public reimbursement. Results reported for Saskatchewan and Manitoba include the accepted prescription drug expenditures for individuals who are eligible for coverage but have not submitted an application and, therefore, do not have a defined deductible.
Long-term care (LTC) sub-plans may not have a typical dispensing frequency due to the more specialized needs of their patients. The LTC sub-plan prescriptions were only separated out from the dispensing costs analysis in Ontario due to a notable influence from their size.
For this edition, the data from the NIHB Program was not available. Therefore, it is not included in the results for 2020/21. It is worth noting that the impact of NIHB data on the overall growth trends among NPDUIS public drug plans would be insignificant (approximately 0.1%).
The analysis of drug and dispensing cost drivers follows the methodological approach detailed in the PMPRB’s The Drivers of Prescription Drug Expenditures: A Methodological Report.Reference 2 Drug costs include any associated markups. Analyses of the average prescription size, as well as pricing, are limited to oral solids to avoid data reporting inconsistencies that may exist in the days’ supply and unit reporting of other formulations. Anatomical Therapeutic Chemical (ATC) levels reported here are based on CIHI NPDUIS data and reflect the ATC classification system maintained by the World Health Organization Collaborating Centre for Drug Statistics Methodology. Vaccines and pharmacy services are not represented in this report.
The methodological approach used in CompassRx is reviewed on an annual basis and updated as needed to respond to changes in the pharmaceutical landscape and data access. Thus, the scope of the report and the data analyzed may vary slightly from year to year. New changes to the methodology are detailed in Methods and Limitations sections of each edition.
A glossary of terms for NPDUIS studies is available on the PMPRB website.
Limitations
Drug expenditure and utilization levels vary widely among the jurisdictions and cross comparisons of the results are limited by differences in the plan designs and policies of the individual public drug plans, as well as the demographic and disease profiles of the beneficiary populations.
For example, public drug plans in British Columbia, Saskatchewan, and Manitoba provide universal incomebased coverage, while other provincial public drug plans offer specific programs for seniors, income assistance recipients, and other select patient groups. The NIHB provides universal care to its entire population. As Yukon is a small jurisdiction, any plan design changes will result in more significant fluctuations in their rates of growth.
The NPDUIS Database includes available sub-plan data specific to particular jurisdictions, such as Alberta, Nova Scotia, and Prince Edward Island. This further limits the comparability of results across plans. A comprehensive summary of the sub-plans available in the database, along with their eligibility criteria, is available on the PMPRB website.
Drug claims for beneficiaries in Ontario who also have coverage through the NIHB are primarily reimbursed by the Ontario Drug Benefit program, with any remaining drug costs covered by the NIHB. Therefore, claims reported for the NIHB include those coordinated with the Ontario Drug Benefit program.
Totals for the NPDUIS public drug plans are heavily skewed toward Ontario due to its population size. As such, the introduction and subsequent revision of the OHIP+ program for Ontario residents aged 24 years or younger had a notable influence on the overall trends for 2018/19 and 2019/20, but little impact after 2019/20 as Ontario OHIP+ program spending became stable. CompassRx will not report the effect separately after this edition. For historical data, please consult previous editions.
High-cost medicines are defined as having an annual treatment cost greater than $10,000. If medicines reach this threshold in any given year, they are included in the count for all other years. Thus, the number and composition of high-cost medicines in any given year may vary depending on the time of analysis.
The number of oncology medicines and other high-cost medicines covered by public plans may be underestimated, as some are reimbursed through specialized programs, such as cancer care, that are not captured in the data.
The reported drug costs are the amounts accepted toward reimbursement by the public plans, which may not reflect the amounts paid by the plan/program and do not reflect off-invoice price rebates or price reductions resulting from confidential product listing agreements.
The prescription drug expenditure data for the public drug plans reported in this study represents only one segment of the Canadian pharmaceutical market, and hence, the findings should not be extrapolated to the overall marketplace.
This edition of the CompassRx reports on data up to and including the 2020/21 fiscal year. Any plan changes or other developments that have taken place since then will be captured in future editions.
Analyses
The components that make up prescription drug expenditures can be expressed from two perspectives: cost-sharing and pharmaceutical.
From a cost-sharing perspective, the expenditures reported in this study represent the total amount accepted for reimbursement by the NPDUIS public drug plans. These amounts reflect both the plan-paid and beneficiary-paid portions of the prescription costs, such as co-payments and deductibles.
From a pharmaceutical pricing perspective, the cost of a prescription drug plan in this section is measured by the total of two components: the cost of the prescription drugs (including associated markups) and the cost for dispensing the prescription drugs, represented here by this formula:
Prescription Drug Expenditures = Drug Costs + Dispensing Costs
The following sections detail each component of this formula by analyzing data trends and adding greater context in the form of Brief Insights.
1. Trends in prescription drug expenditures, 2015/16 to 2020/21
Prescription drug expenditures for public plans increased by 4.2% in 2020/21.
High-cost patented medicines (other than DAAs for hepatitis C) continued to be the most significant contributor to the growth in public plan drug costs, offset in part by a continued decline in the use of new hepatitis C drugs as well as cost savings from generic and biosimilar substitution.
Brief Insights: Drug Plan Designs
The expenditure and utilization levels reported in this study depend on the specific plan design and policies of each jurisdiction, as well as the demographic and disease profiles of the beneficiary population. This affects the comparability of results across plans.
Changes in plan designs or policies can have a significant effect on trends in any given year. For instance, early in 2020, the implementation of a new capitation funding model in Ontario’s long-term care (LTC) program, as well as temporary changes to policies associated with dispensing frequency introduced in many provinces to reduce supply-chain demand and prevent stockpiling due to the onset of the COVID-19 pandemic, directly shaped the growth of dispensing costs, and had notable impacts on expenditures for the 2020/21 fiscal year.
Supplementary reference documents providing information on individual public drug plan designs, policies governing markups and dispensing fees, and a glossary of terms are available on the PMPRB website.
Prescription Drug Expenditures
Prescription Drug Expenditures = Drug Costs (82%) + Dispensing Costs (18%)
Between 2015/16 and 2020/21, annual prescription drug expenditures for the public drug plans grew at a compound annual growth rate of 5.6%, rising from $10.5 billion to $12.3 billion, with $0.5 billion of this growth seen over the last year (Figure 1.1).
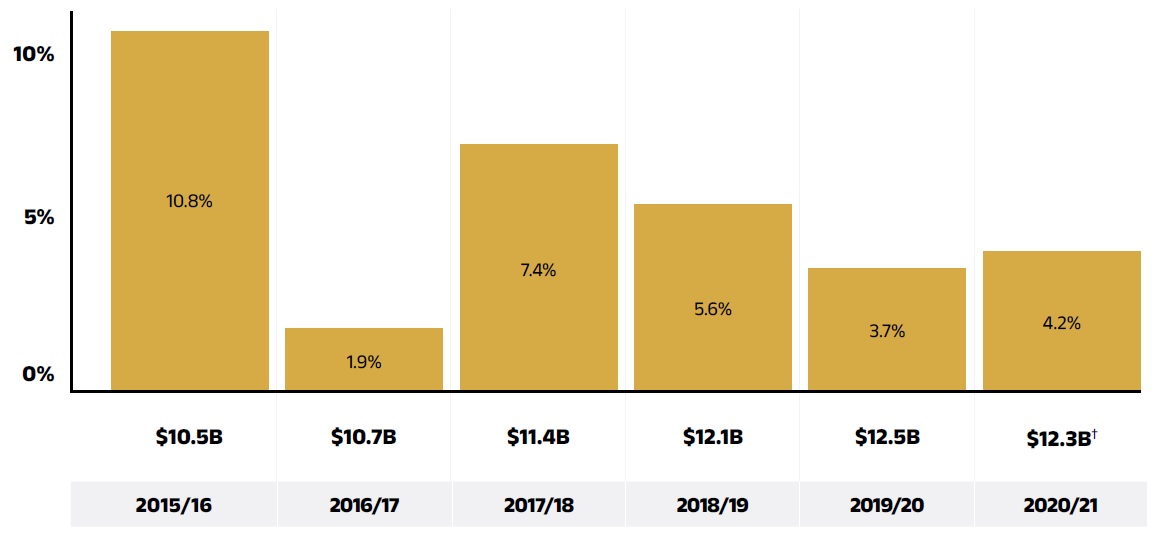
Figure description
This column graph shows the trend in the annual rates of change for prescription drug expenditures from 2015/16 to 2020/21. Price tags below each bar show the annual prescription drug cost in billions of dollars.
| 2015/16 | 2016/17 | 2017/18 | 2018/19 | 2019/20 | 2020/21 | |
|---|---|---|---|---|---|---|
Rate of change |
10.8% |
1.9% |
7.4% |
5.6% |
3.7% |
4.2% |
Prescription drug expenditure (billions of dollars) |
$10.5 |
$10.7 |
$11.4 |
$12.1 |
$12.5 |
$12.3† |
Note: This analysis only includes data for beneficiaries that met their deductible and received public reimbursement.
* British Columbia, Alberta, Saskatchewan, Manitoba, Ontario, New Brunswick, Nova Scotia, Prince Edward Island, Newfoundland and Labrador, Yukon, and the Non-Insured Health Benefits Program.
† The 2020/21 total prescription drug expenditures, the 2019/20 to 2020/21 rate of change and the CAGR were calculated without data from the NIHB program. The impact of NIHB data on the rate of change would be insignificant (approximately 0.1%).
Data source: National Prescription Drug Utilization Information System Database, Canadian Institute for Health Information.
The overall growth in expenditures in 2020/21 consists of a 5.3% growth in drug costs (with associated markups) and a slight (0.2%) decrease in dispensing costs. Due to the disparity in their rates of growth, the drug cost component continued to capture a significantly greater share of overall expenditures (82%), while the dispensing costs share dropped to a new low (18%) (Figure 1.2).
These amounts reflect both the plan-paid portions of prescription costs and beneficiary-paid portions, such as co-payments and deductibles.
Beneficiary Share of Prescription Drug Expenditures
Prescription Drug Expenditures = Plan-paid (87%) + Beneficiary-paid (13%)
In 2020/21, public plans paid an average of 87% (Figure 1.2) of the total expenditures for prescription drugs that were eligible for reimbursement, with the remainder paid by the beneficiaries either out of pocket or through a thirdparty private insurer. The beneficiary-paid share varied across jurisdictions, ranging from 9% to 34%.
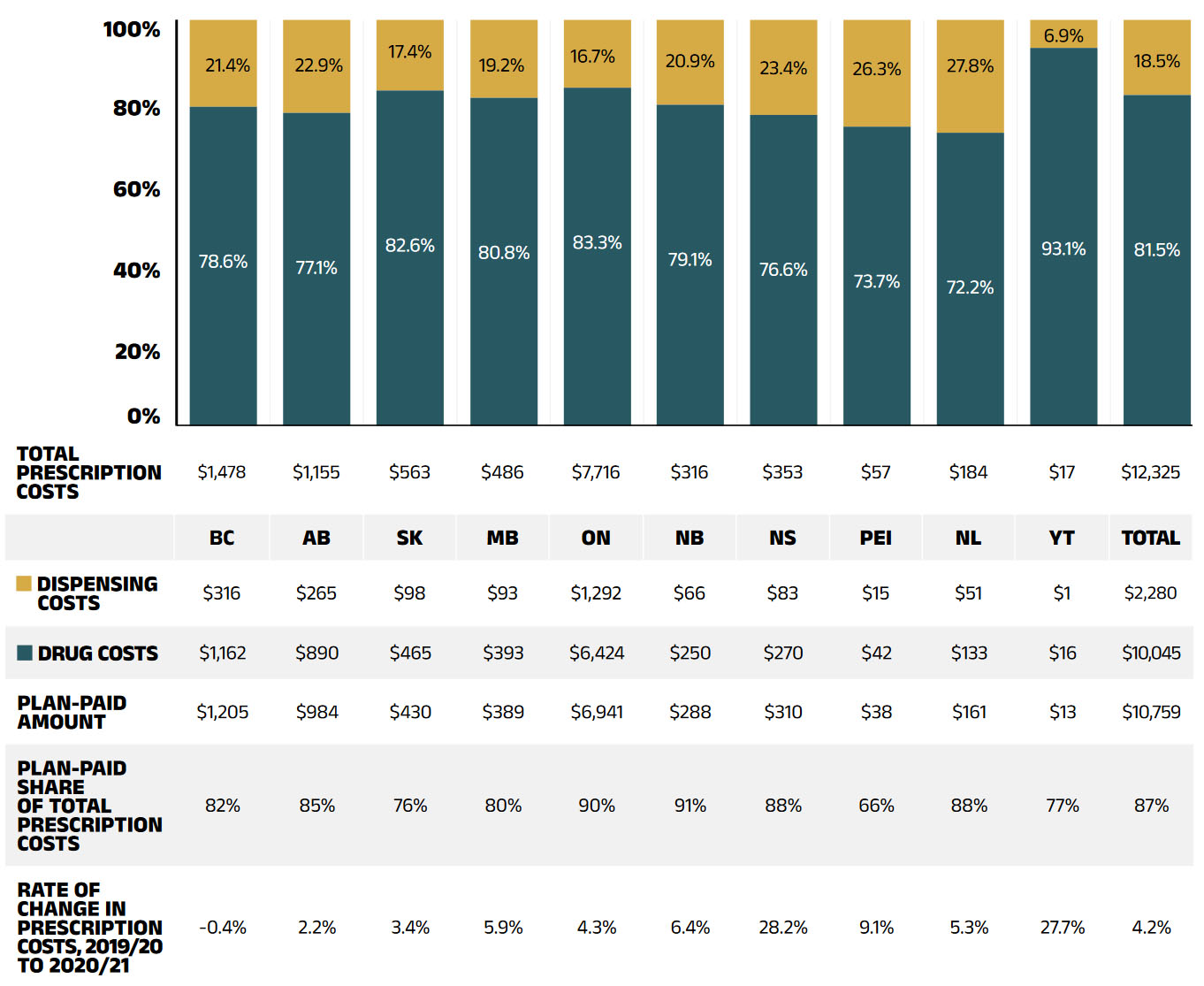
Figure description
This stacked column graph shows the total prescription drug expenditure in 2020/21 for each NPDUIS public drug plan broken out by percent shares of drug costs and dispensing costs, along with the total costs across all plans. A table below provides absolute values for the drug and dispensing costs in millions of dollars, as well as the plan-paid shares of the total prescription costs and the rate of change since 2019/20.
| British Columbia | Alberta | Saskatchewan | Manitoba | Ontario | New Brunswick | Nova Scotia | Prince Edward Island | Newfoundland and Labrador | Yukon | Total | |
|---|---|---|---|---|---|---|---|---|---|---|---|
Total prescription cost (millions of dollars |
$1,478 |
$1,155 |
$563 |
$486 |
$7,716 |
$316 |
$353 |
$57 |
$184 |
$17 |
$12,325 |
Dispensing cost share |
21.4% |
22.9% |
17.4% |
19.2% |
16.7% |
20.9% |
23.4% |
26.3% |
217.8% |
6.9% |
18.5% |
Drug cost share |
78.6% |
77.1% |
82.6% |
80.8% |
83.3% |
79.1% |
76.6% |
73.7% |
72.2% |
93.1% |
81.5% |
Dispensing costs (millions of dollars) |
$316 |
$265 |
$98 |
$93 |
$1,292 |
$66 |
$83 |
$15 |
$51 |
$1 |
$2,280 |
Drug costs (millions of dollars) |
$1,162 |
$890 |
$465 |
$393 |
$6,424 |
$250 |
$270 |
$42 |
$133 |
$16 |
$10,045 |
Plan-paid amount (millions of dollars) |
$1,205 |
$984 |
$430 |
$389 |
$6,941 |
$288 |
$310 |
$38 |
$161 |
$13 |
$10,759 |
Plan-paid share of total prescription cost |
82% |
85% |
76% |
80% |
90% |
91% |
88% |
66% |
88% |
77% |
87% |
Rate of change in prescription costs, 2018/19 to 2019/20 |
-0.4% |
2.2% |
3.4% |
5.9% |
4.3% |
6.4% |
28.2% |
9.1% |
5.3% |
27.7% |
4.2% |
Note: This analysis only includes data for beneficiaries that met their deductible and received public reimbursement. Markup amounts are captured in the drug costs. Values may not add to totals due to rounding.
Data source: National Prescription Drug Utilization Information System Database, Canadian Institute for Health Information.
The annual growth in prescription expenditures is a function of increases in the number of active beneficiaries and their drug costs. In relation to the COVID-19 pandemic, the overall NPDUIS public plan beneficiary population declined by 5.8%. In 2020/21, close to 6 million active beneficiaries filled 289 million prescriptions that were accepted towards a deductible or paid for (in full or in part) by the NPDUIS public drug plans.
After 2019/20, the redesign of Ontario OHIP+ program was completed and became stable. It had little impact to the NPDUIS public drug plans. However, with the onset of the COVID-19 pandemic, approximately 366 thousand fewer Canadians filled a prescription for reimbursement to public drug plans. As this decline primarily impacted non-senior population, seniors made up a more dominant proportion (64%) of the total active beneficiaries, though this share varied greatly across jurisdictions because of differences in plan design, eligibility, and the demographics of the beneficiary population (Figure 1.3).
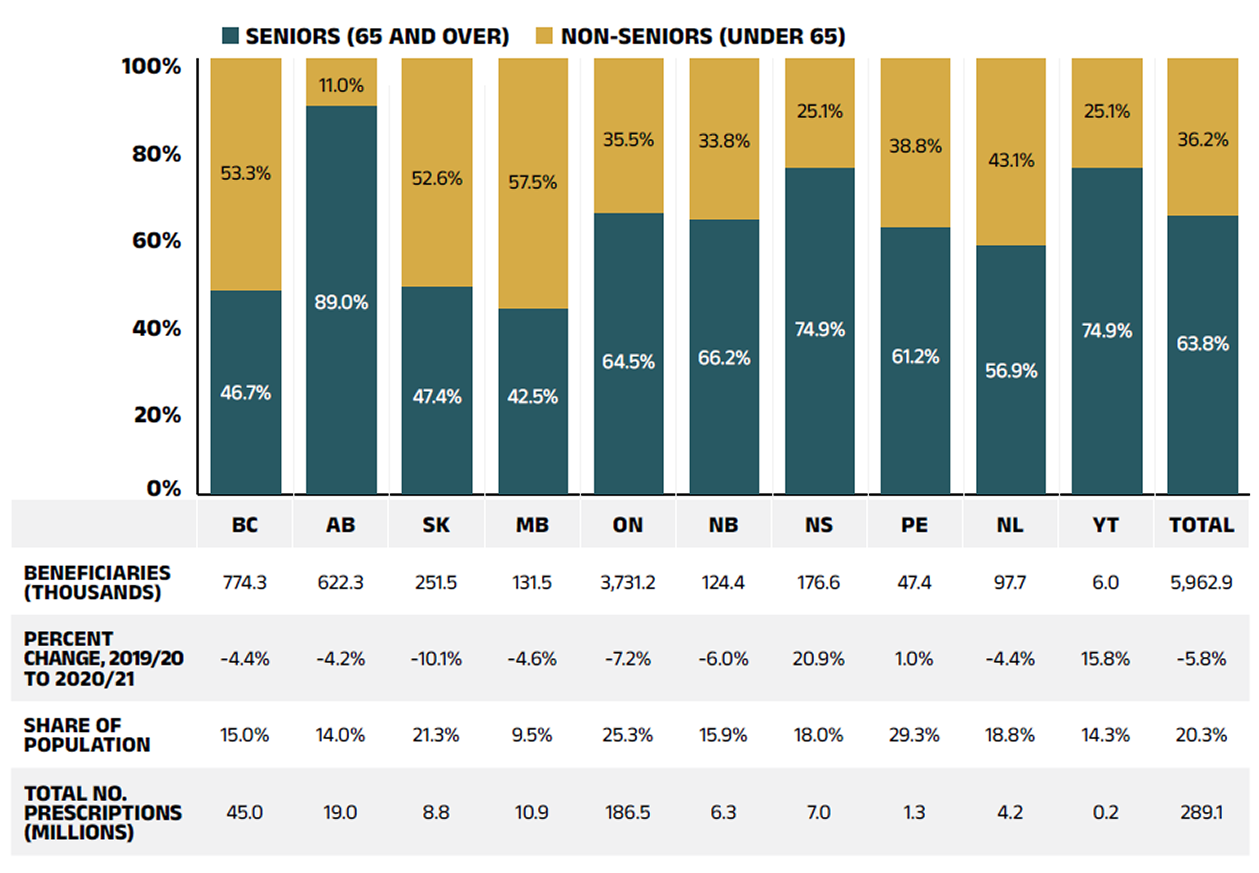
Figure description
This stacked column graph shows the percent share of utilization in senior and non-senior populations for each of the NPDUIS public drug plans in 2020/21, along with the totals across all plans. A table below gives the number of active beneficiaries in thousands, the change in beneficiary population from 2019/20 to 2020/21, the number of active beneficiaries as share of the population, and the total number of prescriptions, in millions.
| British Columbia | Alberta | Saskatchewan | Manitoba | Ontario | New Brunswick | Nova Scotia | Prince Edward Island | Newfoundland and Labrador | Yukon | Total | |
|---|---|---|---|---|---|---|---|---|---|---|---|
Seniors |
46.7% |
89.0% |
47.4% |
42.5% |
64.5% |
63.0% |
74.9% |
61.2% |
56.9% |
74.9% |
63.7% |
Non-seniors |
53.3% |
11.0% |
52.6% |
57.5% |
35.5% |
37.0% |
25.1% |
38.8% |
43.1% |
25.1% |
36.3% |
Beneficiaries (thousands) |
774.3 |
622.3 |
251.5 |
131.5 |
3,731.2 |
124.4 |
176.6 |
47.4 |
97.7 |
6.0 |
5,962.9 |
Percent change in the beneficiary population from 2019/20 to 2020/21 |
-4.4% |
-4.2% |
-10.1% |
-4.6% |
-7.2% |
-6.0% |
20.9% |
1.0% |
-4.4% |
15.8% |
-5.8% |
Beneficiary share of population |
15.0% |
14.0% |
21.3% |
9.5% |
25.3% |
15.9% |
18.0% |
29.3% |
18.8% |
14.3% |
20.3% |
Total number of prescriptions (millions) |
45.0 |
19.0 |
8.8 |
10.9 |
186.5 |
6.3 |
7.0 |
1.3 |
4.2 |
0.2 |
289.1 |
Note This analysis only includes data for beneficiaries that met their deductible and received public reimbursement. Not all the sub-plan data for the jurisdictions is reported to NPDUIS, which may impact the distribution of senior and non-senior shares.
Data source: National Prescription Drug Utilization Information System Database, Canadian Institute for Health Information; Statistics Canada, CANSIM Table 051-0005.
Drug Costs of Prescription Drug Expenditures
Prescription Drug Expenditures = Drug Costs (82%) + Dispensing Costs (18%)
Drug costs, including average reported markups of about 5%Reference II, represent the largest component of prescription drug expenditures and have the greatest influence on overall trends. Following an increase of 4.3% in 2019/20, drug costs rose by another sizable rate of 5.3% in 2020/21. The average rate of change over the last three years was 5.2% across the public plans.
Figure 1.4 reports the annual rate of change in drug costs for each NPDUIS drug plan from 2018/19 to 2020/21. Many plans experienced positive rates of change in 2020/21, ranging from 0.9% in Alberta to 29.3% in Yukon. Drug costs in British Columbia declined the second year by 1.1%.

Figure description
This column graph illustrates the trend in annual rates of change in drug costs from 2018/19 to 2020/21 for each of the NPDUIS drug plans. Total annual results for all plans are included. The compound annual growth rates for the period are given in a table below.
| British Columbia | Alberta | Saskatchewan | Manitoba | Ontario | New Brunswick | Nova Scotia | Prince Edward Island | Newfoundland and Labrador | Yukon | Total | |
|---|---|---|---|---|---|---|---|---|---|---|---|
2018/19 |
5.4% |
3.5% |
6.9% |
1.3% |
7.5% |
1.7% |
2.7% |
3.9% |
0.5% |
13.4% |
5.8% |
2019/20 |
-1.4% |
9.2% |
6.2% |
4.1% |
4.1% |
9.9% |
8.4% |
8.9% |
4.8% |
-24.9% |
4.3% |
2020/21 |
-1,1% |
0.5% |
4.3% |
6.0% |
6.4% |
8.2% |
25.3% |
9.3% |
6.9% |
29.3% |
5.3% |
Compound annual growth rate |
0.9% |
4.3% |
5.8% |
3.7% |
6.0% |
6.5% |
11.7% |
7.3% |
4.0% |
3.3% |
5.2% |
Note: This analysis only includes data for beneficiaries that met their deductible and received public reimbursement.
* Compound annual growth rate.
† The 2019/20 to 2020/21 rate of change and the 3-year CAGR were calculated without data from the NIHB program. The impact of NIHB data on the rate of change would be insignificant (approximately 0.1%).
‡ In Nova Scotia, Community Services Pharmacare Benefits (Plan F) data was not previously submitted to the CIHI NPDUIS database but has been submitted since 2020/21. This addition resulted in a large, one-time increase in the beneficiary population and their drug use in 2020/21.
Data source: National Prescription Drug Utilization Information System Database, Canadian Institute for Health Information.
Figure 1.5 breaks down the annual rate of change in drug costs from 2019/20 to 2020/21 by market segment (bar chart) and gives the corresponding market share in 2020/21 for each (pie chart). These results provide a snapshot of how the distribution of sales across market segments has shifted over the last year. As the market status of a medicine is dynamic, the medicines contributing to any one segment may differ from year to year.
Patented medicines represent the largest segment of the market, capturing 56.4% of public plan drug costs in 2020/21. Costs for direct-acting antivirals (DAAs) for hepatitis C decreased by 6.8% in 2020/21, reflecting a decline in the use of these medicines (see Spotlight on DAA drugs for hepatitis C in Section 2, under “Drug-mix effect”). Despite this pull, the patented market segment still increased moderately by 2.1%, driven mainly by the use of high-cost medicines—those with an average annual cost per beneficiary greater than $10,000, other than DAAs—which grew by a considerable 14.3%.
Unlike the substantial growth in the previous year, the single-source non-patented market decreased by 7.4% in 2020/21, reflecting diminishing costs of this segment without significant patent status changes over the course of 2020/21.
Costs for multi-source non-patented medicines, which include generics and their reference brand-name drugs as well as biosimilars and their originator biologics, increased by 11.0% in 2020/21, now accounting for 30.2% of drug costs. This segment can be broken down into two distinct sub-segments: multi-source generic medicines made up 17.2% ($1,730 million) of drug costs in 2020/21 and grew by 4.7%, while the remaining medicines, consisting mainly of off-patent biologics and biosimilars, experienced a faster growth at a rate of 20.6% to reach 13.0% ($1,304 million) of drug costs. Multi-source non-patented biologics are an important group of medicines to monitor in future years as biosimilars gain traction in the public plans.

Figure description
This graph consists of two parts: a horizontal bar chart on the left breaks down the annual rate of change in drug costs between 2019/20 and 2020/21 by market segment and a pie chart on the right displays the market share of the total drug cost for each segment. Both represent the combined totals for NPDUIS public drug plans.
The bar chart is divided into three parts. The first gives the annual rate of change for all drugs; the second displays the growth rates for the three main market segments; and the third focuses on the patented medicine segment. Results indicate whether they include or exclude the direct-acting antiviral (DAA) drugs for the treatment of hepatitis C. High-cost drugs have an annual cost greater than $10,000 and include both biologics and non-biologics. Total drug costs for each segment in 2020/21 are also given.
Annual rates of change
| Rate of change in drug costs from 2019/20 to 2020/21 | Total drug costs in 2020/21, in millions of dollars | |
|---|---|---|
All drugs |
5.3% |
$10,045 |
All drugs excluding DAA drugs |
7.4% |
$9,753 |
By market segment |
||
Patented |
2.1% |
$5,666 |
Patented excluding DAA drugs |
5.7% |
$5,378 |
Multi-source non-patented |
11.0% |
$3,034 |
Single-source non-patented |
-7.4% |
$867 |
Patented medicines |
||
High-cost drugs excluding DAA drugs |
14.3% |
$3,114 |
DAA drugs |
-6.8% |
$288 |
Biologics |
12.7% |
$1,977 |
Non-biologics excluding DAA drugs |
7.3% |
$3,402 |
Share of drug cost
| Market segment | Share of drug cost |
|---|---|
Patented† |
56.4% |
Multi-source non-patented: generic |
17.2% |
Multi-source non-patented: non-generic |
13.0% |
Single-source non-patented |
8.6% |
Other§ |
4.7% |
Note: This analysis only includes data for beneficiaries that met their deductible and received public reimbursement. DAA drugs are direct-acting antivirals used in the treatment of hepatitis C. A glossary of terms with information on each of the market segments is available on the PMPRB website.
* British Columbia, Alberta, Saskatchewan, Manitoba, Ontario, New Brunswick, Nova Scotia, Prince Edward Island, Newfoundland and Labrador, and Yukon.
† The patented medicines market segment includes all medicines that had patent protection in the period of study, whether or not the patent expired during that period. As such, the rate of growth does not reflect the loss of patent exclusivity for medicines over the course of the fiscal year.
‡ High-cost drugs have an average annual treatment cost greater than $10,000 and include both biologics and non-biologics.
§ This market segment includes devices, compounded drugs, and other products that are reimbursed by public drug plans but do not have a Health Canada assigned Drug Identification Number (DIN).
Data source: National Prescription Drug Utilization Information System Database, Canadian Institute for Health Information.
Dispensing Costs of Prescription Drug Expenditures
Prescription Drug Expenditures = Drug Costs (82%) + Dispensing Costs (18%)
Dispensing costs make up an important part of prescription drug expenditures. Owing largely to temporary dispensing frequency practices during the COVID-19 pandemic and policy changes to the long-term care (LTC) program in Ontario, the overall dispensing costs in the NPDUIS public plans had no growth. Dispensing costs declined slightly by 0.2% in 2020/21, for a compound annual growth rate of 2.0% over the last three years. Figure 1.6 reports the annual rate of change in dispensing costs for each NPDUIS drug plan from 2018/19 to 2020/21. Jurisdictional variations may be due to changes in dispensing fee policies and plan designs, as well as changes in the number of prescriptions and their size, among other factors.
Brief Insights: Dispensing Fees and Policies
On January 1, 2020, the Ontario government introduced a new long-term care (LTC) capitation funding model. It included a shift in the payment model for professional pharmacy services (dispensing fees and professional pharmacy services) for LTC homes from fee-for-service to a fixed per-patient amount. As such, ODB-eligible prescription claims submitted for residents of LTC homes reflect a zero-dollar dispensing fee. This change is reflected in the full course of fiscal year 2020/21.
Beginning March/April 2020, most NPDUIS public drug plans introduced temporary changes to policies on dispensing frequency during the COVID-19 pandemic. These changes are also reflected in Section 3, “The Drivers of Dispensing Costs”.
A summary of dispensing fee policies for each of the public drug plans is available on the PMPRB website.
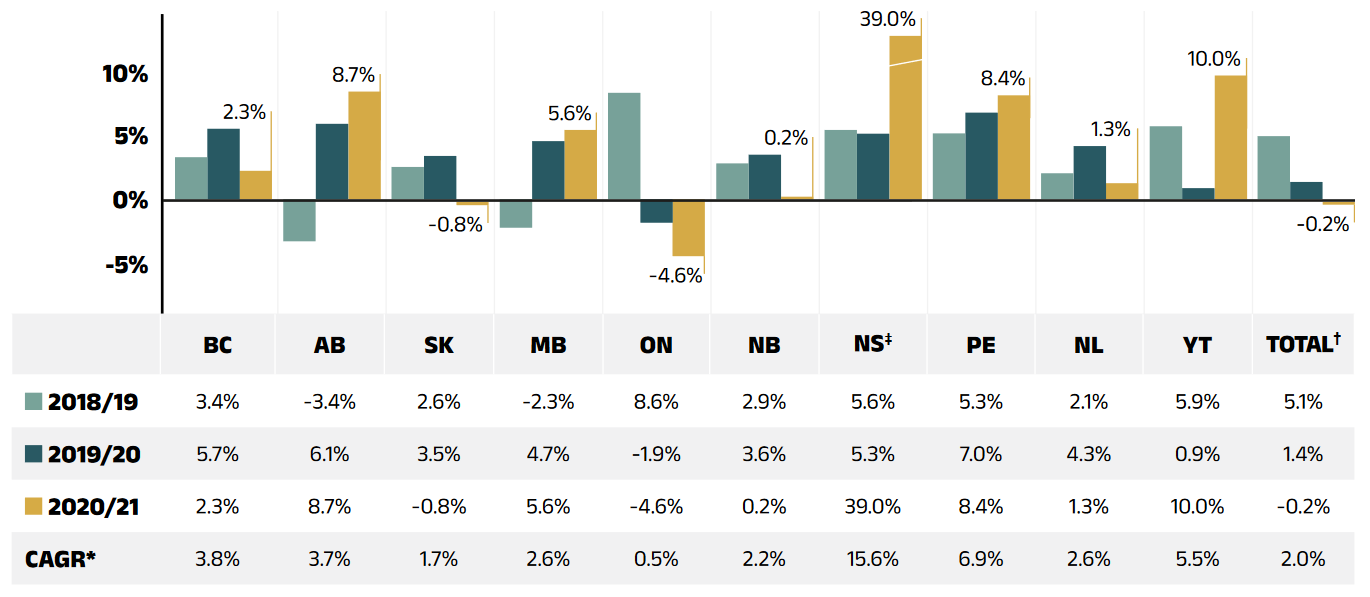
Figure description
This column graph illustrates the trend in annual rates of change for dispensing costs from 2018/19 to 2020/21 for each of the NPDUIS public drug plans. Total annual results for all plans are included. Compound annual growth rates for the period are given in a table below.
| British Columbia | Alberta | Saskatchewan | Manitoba | Ontario | New Brunswick | Nova Scotia | Prince Edward Island | Newfoundland and Labrador | Yukon | Total | |
|---|---|---|---|---|---|---|---|---|---|---|---|
2018/19 |
3.4% |
-3.4% |
2.6% |
-2.3% |
8.6% |
2.9% |
5.6% |
5.3% |
2.1% |
5.9% |
5.1% |
2019/20 |
5.7% |
6.1% |
3.5% |
4.7% |
-1.9% |
3.6% |
5.3% |
7.0% |
4.3% |
0.9% |
1.4% |
2020/21 |
2.3% |
8.7% |
-0.8% |
5.6% |
-4.6% |
0.2% |
39.0% |
8.4% |
1.3% |
10.0% |
-0.2% |
Compound annual growth rate |
3.8% |
3.7% |
1.7% |
2.6% |
0.5% |
2.2% |
15.6 % |
6.9% |
2.6% |
5.5% |
2.0% |
Note: This analysis only includes data for beneficiaries that met their deductible and received public reimbursement.
* Compound annual growth rate.
† The 2019/20 to 2020/21 rate of change and the 3-year CAGR were calculated without data from the NIHB program. The impact of NIHB data on the rate of change would be insignificant (approximately 0.1%).
‡ In Nova Scotia, Community Services Pharmacare Benefits (Plan F) data was not previously submitted to the CIHI NPDUIS database but has been submitted since 2020/21. This addition resulted in a large, one-time increase in the beneficiary population and their drug use in 2020/21.
Data source: National Prescription Drug Utilization Information System Database, Canadian Institute for Health Information.
Unlike drug costs, dispensing costs have grown at a slow to negative rate over the last three years. Their share of overall prescription drug expenditures has continued to decline, from 20.2% in 2018/19 to 18.5% in 2020/21
Figure 1.7 depicts the trend in the dispensing cost share of total prescription expenditures for each NPDUIS drug plan from 2018/19 to 2020/21.
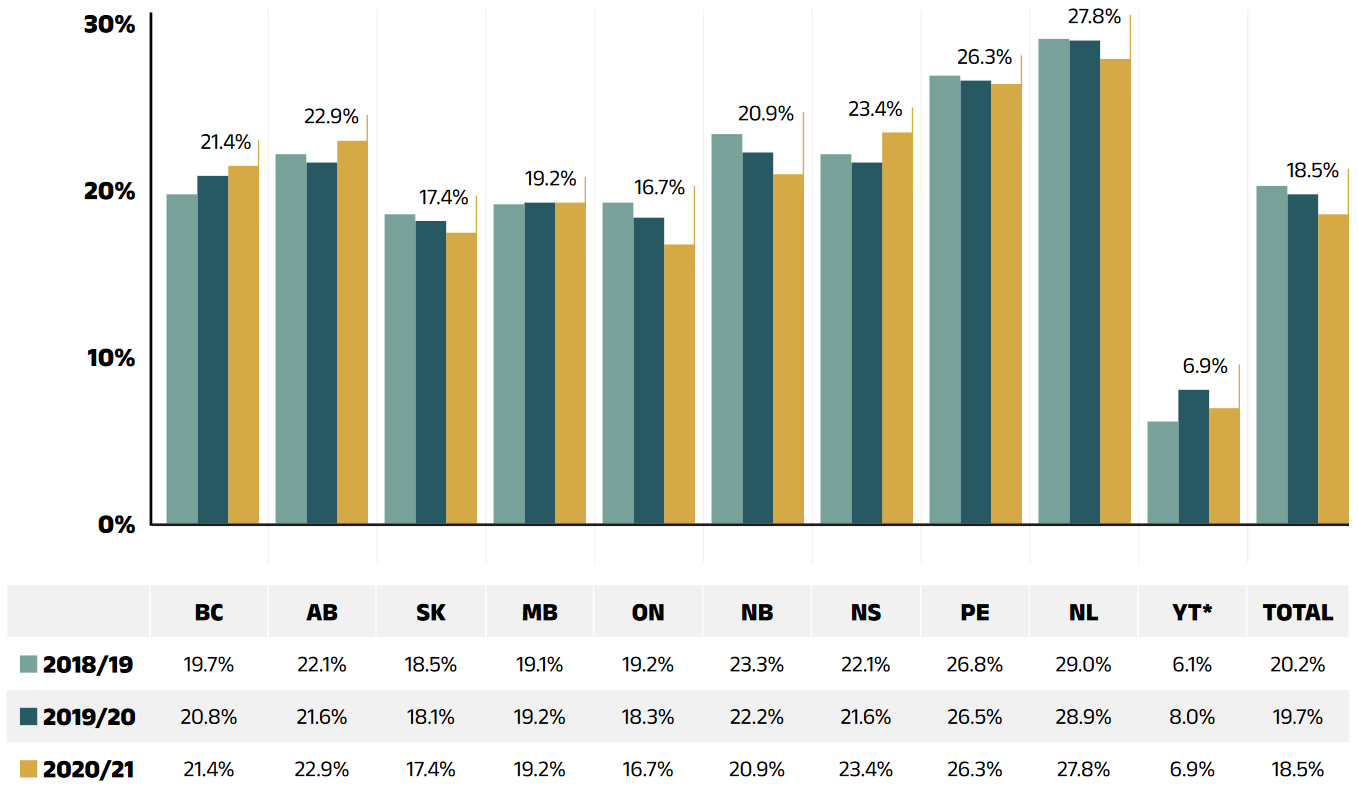
Figure description
This column graph shows the trend in annual dispensing costs as a share of the total prescription expenditures from 2018/19 to 2020/21 for each of the NPDUIS public drug plans. Total annual results for all plans are included.
| British Columbia | Alberta | Saskatchewan | Manitoba | Ontario | New Brunswick | Nova Scotia | Prince Edward Island | Newfoundland and Labrador | Yukon* | Total | |
|---|---|---|---|---|---|---|---|---|---|---|---|
2018/19 |
19.7% |
22.1% |
18.5% |
19.1% |
19.2% |
23.3% |
22.1% |
26.8% |
29.0% |
6.1% |
20.2% |
2019/20 |
20.8% |
21.6% |
18.1% |
19.2% |
18.3% |
22.2% |
21.6% |
26.5% |
28.9% |
8.0% |
19.7% |
2020/21 |
21.4% |
22.9% |
17.4% |
19.2% |
16.7% |
20.9% |
23.4% |
26.3% |
27.8% |
6.9% |
18.5% |
Note: This analysis only includes data for beneficiaries that met their deductible and received public reimbursement.
* Yukon allows for markups of up to 30%; as such, dispensing costs account for a smaller share of their total expenditures.
Data source: National Prescription Drug Utilization Information System Database, Canadian Institute for Health Information.
2. The Drivers of Drug Costs, 2019/20 to 2020/21
Drug cost increases in the NPDUIS public plans in 2020/21 were primarily driven by a sustained increase in the use of higher-cost medicines. This is despite the decreasing use of DAA drugs. As generic prices have stabilized, the effect from substitution became stronger than the price effect; however, these combined forces no longer offset the increasing cost pressures from the drug-mix effect. In 2020/21, there was a notable decrease in the number of active beneficiaries due to COVID-19. This exerted a downward demographic effect, which was more than offset by a sizable increase in the number of claims per patient (captured in the volume effect), pushing spending upwards and resulting in an overall increase of 5.3%.
In this section, a comprehensive cost driver analysis is used to determine how much public plan drug costs would have changed between 2019/20 and 2020/21 if only one factor (e.g., the price of drugs) was considered while all the others remained the same.Reference III
Changes in drug costs are driven by a number of push and pull effects. The net effect of these opposing forces yields the overall rate of change.
Price change effect: Changes in the prices of both brand-name and generic drugs, determined at the molecule, strength, and form level.
Substitution effect: Shifts from brand-name to generic drugs, as well as shifts to biosimilar use.
Demographic effect: Changes in the number of active beneficiaries, as well as shifts in the distribution of age or gender.
Volume effect: Changes in the number of prescriptions dispensed to patients, the average number of units of a drug dispensed per prescription, and/or shifts in the use of various strengths or forms of a medicine.
Drug-mix effect: Shifts in use between lower- and higher-cost drugs, including those entering, exiting, or remaining in the market during the time period analyzed.
In addition to the standard annual effects, Ontario’s OHIP+ program was previously treated as a separate factor in the cost driver analysis, encompassing all effects associated with the program (e.g., volume and demographic changes). As such, the OHIP+ effect reflected the overall impact from the plan design changes. After 2019/20, OHIP+ program spending stabilized and had little impact; therefore, it is no longer reported as a separate factor of cost drivers in this edition of CompassRx. For historical data, please consult previous editions.
Figure 2.1 provides insight into the pressures driving the rates of change in drug costs from 2015/16 to 2020/21.
Typically, changes in the patient population and the volume of drugs prescribed result in a slight to moderate increase of drug costs. Over the past few years, this increase has been between 1% and 3% for the demographic effect, and remained stable at 1% for the volume effect. In 2020/21, however, these forces were impacted by the COVID-19 pandemic. Despite the 2.3% downward pull of the demographic effect from a notable pandemic-led decrease in the number of active beneficiaries, there is a sizable increase in the number of claims per patient captured in the volume that pushed overall spending upward by 4.6% over the same period. These effects are expected to gradually return to pre-pandemic levels in future years.
The most pronounced upward push on costs can be attributed to the use of higher-cost medicines (other than DAAs for hepatitis C), which consistently accounted for 4% to 5% of annual growth between 2015/16 and 2017/18, and jumped to an average of 6.1% over the past three years. In contrast, the use of DAAs continued to decrease in 2020/21, pulling drug costs down by 2.1%. The combined effects of DAAs and other higher-cost drugs still added a sizable 4.3% upward pressure on drug costs in NPDUIS public plans.
Counterbalancing these upward cost pressures, generic and biosimilar substitution and price reductions generally exert a downward pull on costs. The magnitude of these effects can vary from year to year depending on the timing of generic and biosimilar market entries and the implementation of policies lowering generic prices. In 2020/21, the influence of the price change effect diminished to less than 0.1%. The substitution effect became stronger, pulling drug costs down by 1.4%. Over the past two years, the combined rate of these two effects has stabilized to slightly below -1%.
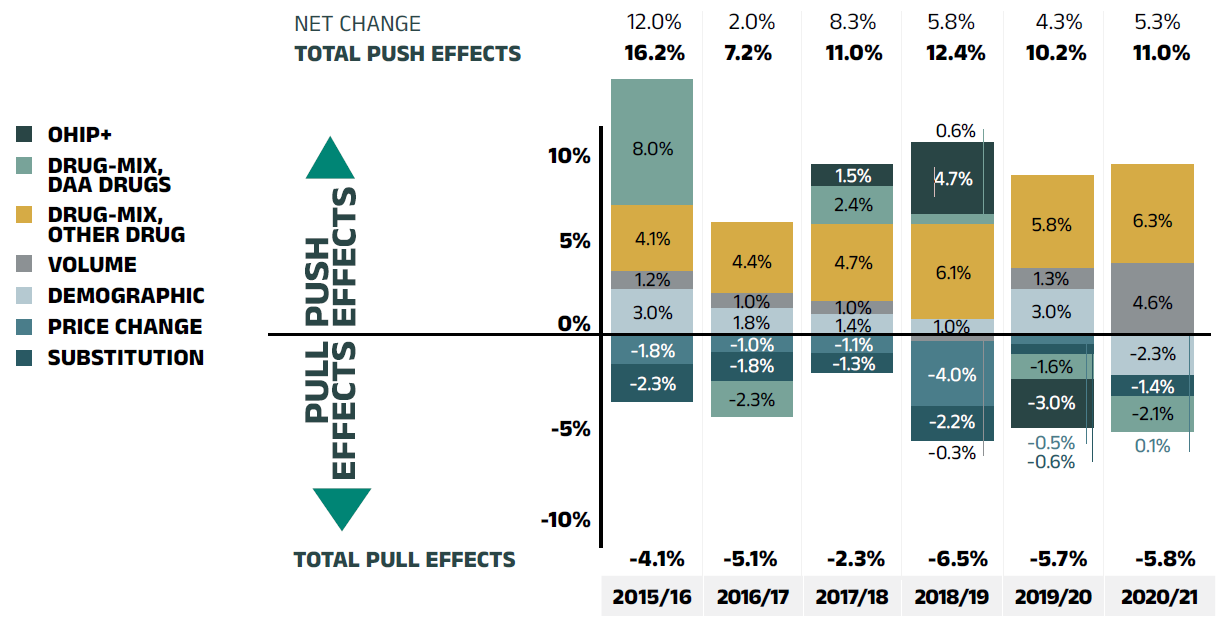
Figure description
This column graph describes the key factors or effects that impacted the rates of change in drug costs across all NPDUIS public drug plans for each year from 2015/16 to 2020/21. Each column is broken out to give the positive or negative contribution of each effect: drug-mix; volume; demographic; price change; and substitution. The drug-mix effect of direct-acting antiviral (DAA) drugs for hepatitis C is shown separately, as are the effects of the Ontario Health Insurance Plan Plus (OHIP+) initiative. The OHIP+ effect is not captured for 2020/21. The total positive push effect, negative pull effect, and net change are given for each year.
| 2015/16 | 2016/17 | 2017/18 | 2018/19 | 2019/20 | 2020/21 | |
|---|---|---|---|---|---|---|
OHIP+ |
– |
– |
1.5% |
4.7% |
-3.0% |
– |
Drug-mix, direct-acting antiviral (DAA) drugs |
8.0% |
-2.3% |
2.4% |
0.6% |
-1.6% |
-2.1% |
Drug mix, other drugs |
4.1% |
4.4% |
4.7% |
6.1% |
5.8% |
6.3% |
Volume |
1.2% |
1.0% |
1.0% |
-0.3% |
1.3% |
4.3% |
Demographic |
3.0% |
1.8% |
1.4% |
1.0% |
3.0% |
-2.0% |
Price change |
-1.8% |
-1.0% |
-1.1% |
-4.0% |
-0.5% |
<0.1% |
Substitution |
-2.3% |
-1.8% |
-1.3% |
-2.2% |
-0.6% |
-1.4% |
Total push effect |
16.2% |
7.2% |
11.0% |
12.4% |
10.2% |
11.0% |
Total pull effect |
-4.1% |
-5.1% |
-2.3% |
-6.5% |
-5.7% |
-5.8% |
Net change |
12.0% |
2.0% |
8.3% |
5.8% |
4.3% |
5.3% |
Note: Historic values are reported for 2015/16.
This analysis is based on publicly available pricing information. It does not reflect confidential price discounts negotiated by the pCPA on behalf of the public plans.
Values may not add to totals due to rounding and the cross effect. Results for Yukon were included from 2016/17 onward.
* British Columbia, Alberta, Saskatchewan, Manitoba, Ontario, New Brunswick, Nova Scotia, Prince Edward Island, Newfoundland and Labrador, Yukon, and the Non-Insured Health Benefits (NIHB) Program. Results for 2020/21 do not include the NIHB program.
Data source: National Prescription Drug Utilization Information System Database, Canadian Institute for Health Information.
The overall 5.3% increase in drug costs in 2020/21 represents an absolute growth of $505 million, with varying rates of growth among the public drug plans ranging from approximately -1% to 9%. Nova Scotia and Yukon were the exceptions with 25.3% and 29.3% increases, respectively (Figure 2.2). These variations were mainly due to differences in the magnitude of the opposing factors. Other jurisdictions with higher overall growth rates included Prince Edward Island (9.3%), New Brunswick (8.2%), and Newfoundland and Labrador (6.9%).
The increased use of higher-cost drugs other than DAAs had the greatest push effect, with an overall impact of 6.3% ($605 million) ranging from 0.6% to 10.5% across jurisdictions. The use of DAA drugs for hepatitis C continued to decrease and drove costs down by 2.1% ($197 million). Differences in the drug-mix effect across public drug plans may be related to plan designs, formulary listing decisions, or the disease profiles of the population, among other determinants. The overall declining impact of DAA drugs also varied, with the largest downward pull in British Columbia (-5.1%), followed by Yukon (-4.1%) and Manitoba (-2.4%). The use of DAAs in Nova Scotia and Newfoundland and Labrador pushed costs upward very slightly (0.4% and 0.1%, respectively).
In recent years, as a result of growth of the overall population of a jurisdiction, an increase in the number of Canadians eligible for senior coverage (65+), and/or plan design changes that expanded coverage to new populations or patient groups, the demographic effect boosted drug costs in the NPDUIS public plans by a fairly consistent 1% to 3%. However, with the onset of the COVID-19 pandemic, in 2020/21, fewer active beneficiaries submitted claims for reimbursement to public plans in many provinces, exerting an overall downward demographic effect of 2.3% ($223 million). This downward pull effect was observed in many provinces, with the largest impact in New Brunswick (-5.6%), British Columbia (-4.4%), Alberta (-3.9%) and Newfoundland and Labrador (-2.7%).
Despite fewer active beneficiaries in many public plans, a sizable increase in the number of prescriptions dispensed per patient (captured by the volume effect) pushed overall drug costs upward by 4.6% or $443 million in 2020/21. This effect was an important driver and more than offset the downward demographic effect in Alberta (7.9%), British Columbia (6.3%), Newfoundland and Labrador (5.3%) and New Brunswick (4.8%).
The price change effect (<0.1% or $4 million) had the smallest contribution and was relatively uniform across jurisdictions. The cost savings effects of generic and biosimilar substitution (-1.4% or -$129 million) was stronger than the price change effect but varied across public plans. The substitution effect was more pronounced in Alberta (-3.8%) and British Columbia (-3.4%), as a result of the introduction of biosimilar switching initiatives. The key effects for 2020/21—price change, substitution, and drug-mix—are explored in more detail in the following section.
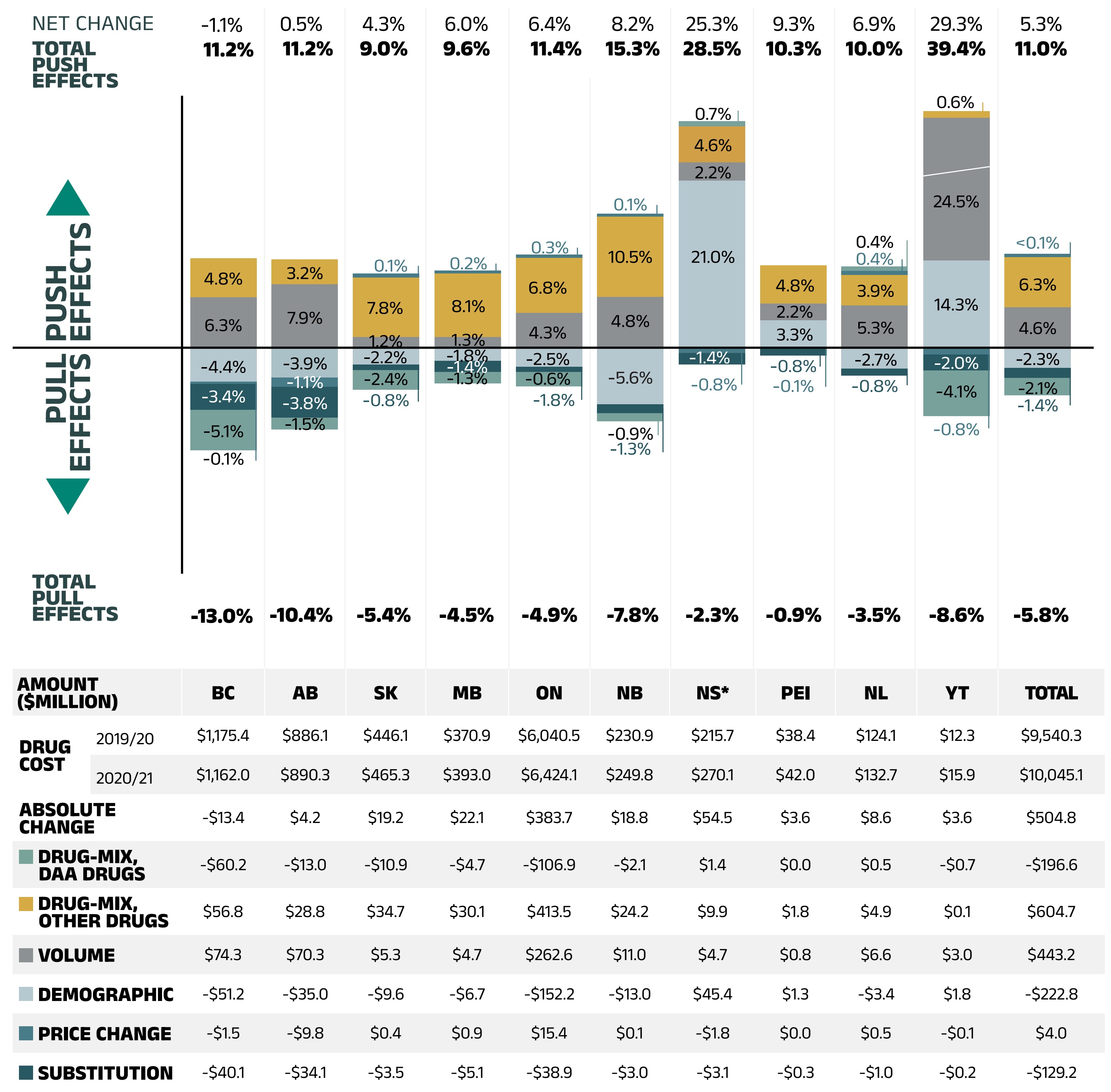
Figure description
This column graph and table describe the key factors or effects that impacted the rates of change in drug costs for each of the NPDUIS public drug plans from 2019/20 to 2020/21. Each column is broken out to give the positive or negative contribution of each effect: drug-mix; volume; demographic; price change; and substitution. The drug-mix effect of direct-acting antiviral (DAA) drugs for hepatitis C is shown separately. The total positive push effect, negative pull effect and net change are given for each year. Total results for all plans are also included.
| British Columbia | Alberta | Saskatchewan | Manitoba | Ontario | New Brunswick | Nova Scotia | Prince Edward Island | Newfoundland and Labrador | Yukon | Total | |
|---|---|---|---|---|---|---|---|---|---|---|---|
Demographic |
-4.4% |
-3.9% |
-2.2% |
-1.8% |
-2.5% |
10.0% |
21.0% |
3.3% |
-2.7% |
11.0% |
-2.0% |
Volume |
6.3% |
7.9% |
1.2% |
1.3% |
4.3% |
-9.4% |
2.2% |
2.2% |
5.3% |
18.0% |
4.3% |
Drug Mix, Other Drugs |
4.8% |
3.2% |
7.8% |
8.1% |
6.8% |
10.5% |
4.6% |
4.8% |
3.9% |
0.6% |
6.3% |
Price Change |
-0.1% |
-1.1% |
0.1% |
0.2% |
0.3% |
0.1% |
-0.8% |
-0.1% |
0.4% |
-0.8% |
0.0% |
Substitution |
-3.4% |
-3.8% |
-0.8% |
-1.4% |
-0.6% |
-1.3% |
-1.4% |
-0.8% |
-0.8% |
-2.0% |
-1.4% |
Drug Mix, DAA Drugs |
-5.1% |
-1.5% |
-2.4% |
-1.3% |
-1.8% |
-0.9% |
0.7% |
0.0% |
0.4% |
-5.7% |
-2.1% |
Total push effect |
11.2% |
11.2% |
9.0% |
9.6% |
11.4% |
15.3% |
28.5% |
10.3% |
10.0% |
39.4% |
11.0% |
Total pull effect |
-13.0% |
-10.4% |
-5.4% |
-4.5% |
-4.9% |
-7.8% |
-2.3% |
-0.9% |
-3.5% |
-8.6% |
-5.8% |
Net change |
-1.1% |
0.5% |
4.3% |
6.0% |
6.4% |
8.2% |
25.3% |
9.3% |
6.9% |
29.3% |
5.3% |
An accompanying table gives the corresponding changes in millions of dollars, as well as the total drugs costs in 2019/20 and 2020/21 and the absolute change for each plan.
| British Columbia | Alberta | Saskatchewan | Manitoba | Ontario | New Brunswick | Nova Scotia | Prince Edward Island | Newfoundland and Labrador | Yukon | Total | |
|---|---|---|---|---|---|---|---|---|---|---|---|
Drug cost 2019/20 |
$1,175.40 |
$886.10 |
$446.10 |
$370.90 |
$6,040.50 |
$230.90 |
$215.70 |
$38.40 |
$124.10 |
$12.30 |
$9,540.30 |
Drug cost 2020/21 |
$1,162.00 |
$890.30 |
$465.30 |
$393.00 |
$6,424.10 |
$249.80 |
$270.10 |
$42.00 |
$132.70 |
$15.90 |
$10,045.10 |
Absolute change |
-$13.40 |
$4.20 |
$19.20 |
$22.10 |
$383.70 |
$18.80 |
$54.50 |
$3.60 |
$8.60 |
$3.60 |
$504.80 |
Drug-mix, direct-acting antiviral (DAA) drugs |
-$60.20 |
-$13.00 |
-$10.90 |
-$4.70 |
-$106.90 |
-$2.10 |
$1.40 |
$0.00 |
$0.50 |
-$0.70 |
-$196.60 |
Drug-mix, other drugs |
$56.80 |
$28.80 |
$34.70 |
$30.10 |
$413.50 |
$24.20 |
$9.90 |
$1.80 |
$4.90 |
$0.10 |
$604.70 |
Volume |
$74.30 |
$70.30 |
$5.30 |
$4.70 |
$262.60 |
$11.00 |
$4.70 |
$0.80 |
$6.60 |
$3.00 |
$443.2 |
Demographic |
-$51.20 |
-$35.00 |
-$9.60 |
-$6.70 |
-$152.20 |
-$13.0 |
$45.40 |
$1.30 |
-$3.40 |
$1.80 |
-$222.8 |
Price change |
-$1.50 |
-$9.80 |
$0.40 |
$0.90 |
$15.40 |
$0.10 |
-$1.80 |
$0.00 |
$0.50 |
-$0.10 |
$4.00 |
Substitution |
-$40.10 |
-$34.10 |
-$3.50 |
-$5.10 |
-$38.90 |
-$3.00 |
-$3.10 |
-$0.30 |
-$1.00 |
-$0.20 |
-$129.20 |
Note: This analysis is based on publicly available pricing information. It does not reflect confidential drug price discounts negotiated by the pCPA on behalf of the public plans. Values may not add to totals due to rounding and the cross effect.
* In Nova Scotia, Community Services Pharmacare Benefits (Plan F) data was not previously submitted to the CIHI NPDUIS database but has been submitted since 2020/21. This addition resulted in a large, one-time increase in the beneficiary population and their drug use. As such, the overall impact was captured in the demographic and volume effects in 2020/21.
Data source: National Prescription Drug Utilization Information System Database, Canadian Institute for Health Information.
Price Change Effect
This effect captures changes in the prices of both brandname and generic medicines. Following the significant one-time drop in generic prices resulting from the implementation of the pan-Canadian Generic Price Initiative in April 2018, its influence has diminished. In 2020/21, changes in drug prices played a very minor role in the growth of drug costs, accounting for less than 0.1% ($4 million).
An analysis by market segment suggests that the reduction in the average unit costs reimbursed in the multi-source non-patented category saw little change. The average unit costs of patented medicines remained stable, while the costs of single-source non-patented medicines increased at a steady pace.
Figure 2.3 reports long-term trends in average unit costs from 2009/10 to 2020/21 by market segment for (a) patented medicines; (b) multi-source generic medicines; and (c) single-source non-patented medicines, along with their corresponding 2020/21 market shares. The results are presented as an index, with the base year (2009/10) set to one and subsequent years reported relative to this value. The findings are a cost-weighted average of changes in the reimbursed unit costs for individual medicines. The analysis was restricted to oral solid formulations to ensure unit consistency.
From 2009/10 to 2020/21, the prices of patented medicines were stable, increasing by a modest average of 7%, while prices of single-source non-patented medicines increased by an average of 31%. Despite the significant rise in prices, the impact of this segment was limited due to its small size: single-source non-patented medicines make up just 8.6% of the market, while patented medicines represent a 56.4% share. The multi-source generics market shows a similar trend across all NPDUIS public drug plans that is tied to the various waves of generic price reforms. Average unit costs rapidly declined by nearly 40% in the first few years after the initial wave of reforms, and then decreased more gradually from 2014/15 to 2016/17 as generic prices stabilized. Following the most recent pricing initiatives, prices declined by an average of 3% in 2017/18 before a more notable 11% drop in 2018/19. Since then, they have remained steady without any further decrease from 2019/20 to 2020/21. As a result, the average multi-source generic unit cost across all jurisdictions in 2020/21 was less than half of the 2009/10 average.
Brief Insights: pCPA Initiatives
Through the pan-Canadian Pharmaceutical Alliance (pCPA), the provinces, territories, and federal government have been working collectively to achieve greater value for generic and brand-name medicines for Canada’s publicly funded drug programs.
Generic medicines:
Between April 1, 2015, and April 1, 2016, the prices of 18 commonly used generic medicines were reduced to 18% of their brand-name reference products. In addition, a one-year bridging period was initiated on April 1, 2017, which further reduced the prices of six of the molecules to 15% of the brand reference price.
As of April 1, 2018, a five-year joint agreement between the pCPA and the Canadian Generic Pharmaceutical Association (CGPA) reduced the prices of 67 of the most prescribed generic medicines in Canada by 25% to 40%, resulting in overall discounts of up to 90% off the price of their brand-name equivalents.
Effective April 1, 2022, the Historical Products Policy developed by pCPA and CGPA addresses concerns regarding assessments for generic products whose brand reference product has been cancelled post market.
Brand-name medicines:
As of July 31, 2022, 454 joint negotiations or product listing agreements (PLAs) for brand-name drugs had been completed by the pCPA, with another 38 negotiations underway. The impact of the confidential drug prices negotiated is not reflected in this analysis.
For more details, see the overview of generic pricing policies and pCPA initiatives available on the PMPRB website.
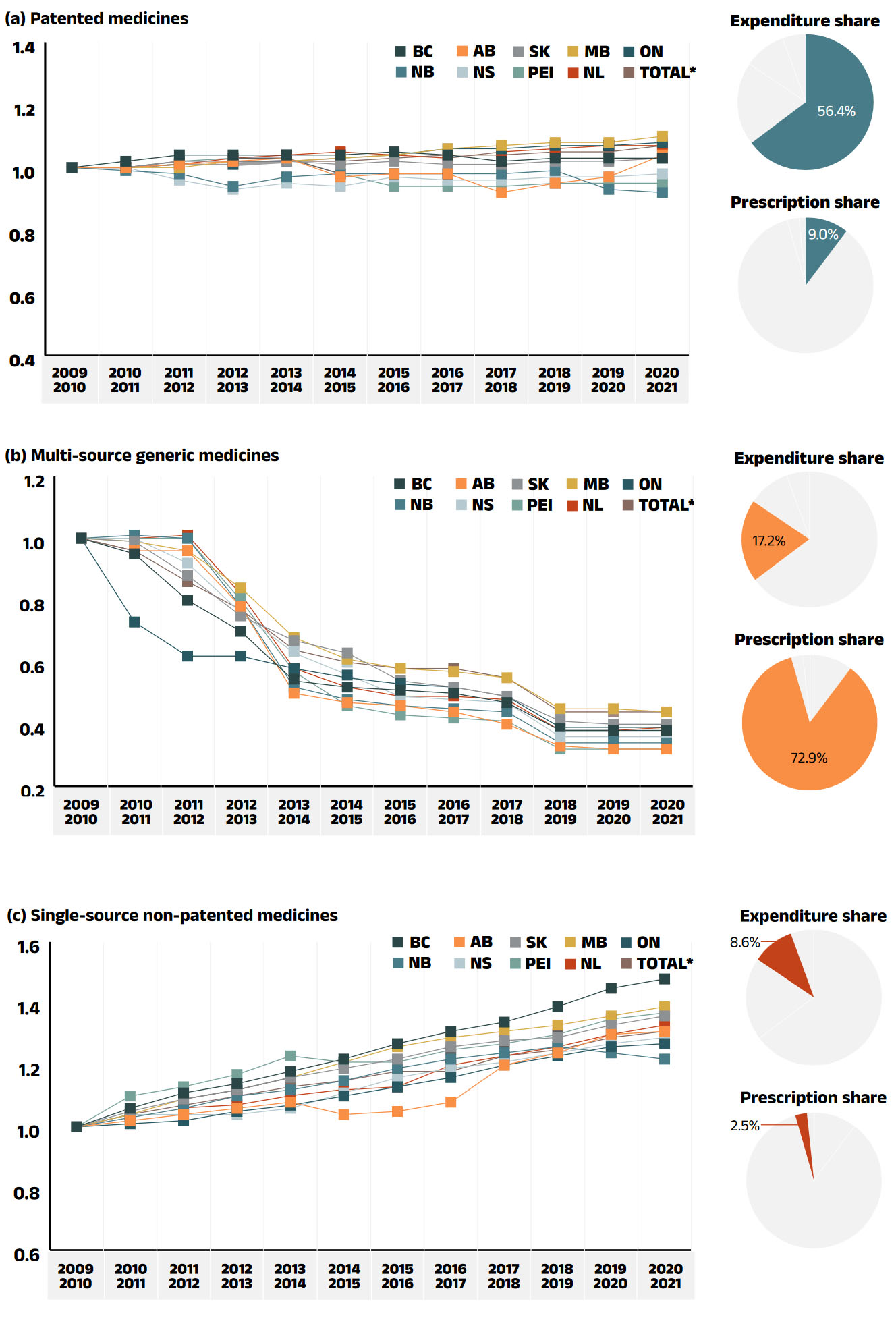
Figure description
This figure has three sections, each with a line graph depicting the average unit cost index from 2009/10 to 2020/21 for (a) patented medicines, (b) multi-source generic medicines, and (c) single-source non-patented medicines. Results are given for each NPDUIS drug plan, as well as the total for all plans. Expenditure and prescription shares for 2020/21 are shown in pie charts beside each graph.
(a) Patented medicines
Expenditure share: 56.4%
Prescription share: 9.0%
| 2009/10 | 2010/11 | 2011/12 | 2012/13 | 2013/14 | 2014/15 | 2015/16 | 2016/17 | 2017/18 | 2018/19 | 2019/20 | 2020/21 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
British Columbia |
1.00 |
1.02 |
1.04 |
1.04 |
1.04 |
1.04 |
1.05 |
1.04 |
1.02 |
1.03 |
1.03 |
1.03 |
Alberta |
1.00 |
1.00 |
1.01 |
1.02 |
1.03 |
0.97 |
0.98 |
0.98 |
0.92 |
0.95 |
0.97 |
1.04 |
Saskatchewan |
1.00 |
1.00 |
1.02 |
1.02 |
1.02 |
1.01 |
1.02 |
1.01 |
1.01 |
1.02 |
1.02 |
1.03 |
Manitoba |
1.00 |
1.00 |
1.00 |
1.02 |
1.02 |
1.03 |
1.04 |
1.06 |
1.07 |
1.08 |
1.08 |
1.10 |
Ontario |
1.00 |
1.00 |
1.01 |
1.01 |
1.02 |
1.03 |
1.04 |
1.06 |
1.06 |
1.07 |
1.07 |
1.08 |
New Brunswick |
1.00 |
0.99 |
0.98 |
0.94 |
0.97 |
0.98 |
0.98 |
0.98 |
0.98 |
0.99 |
0.93 |
0.92 |
Nova Scotia |
1.00 |
1.00 |
0.96 |
0.93 |
0.95 |
0.94 |
0.97 |
0.96 |
0.96 |
0.97 |
0.97 |
0.98 |
Prince Edward Island |
1.00 |
1.00 |
1.02 |
1.03 |
1.03 |
0.98 |
0.94 |
0.94 |
0.94 |
0.95 |
0.95 |
0.95 |
Newfoundland and Labrador |
1.00 |
1.00 |
1.01 |
1.03 |
1.04 |
1.05 |
1.04 |
1.03 |
1.05 |
1.06 |
1.07 |
1.07 |
Total* |
1.00 |
1.00 |
1.01 |
1.01 |
1.02 |
1.02 |
1.03 |
1.04 |
1.04 |
1.05 |
1.05 |
1.07 |
(b) Multi-source generic medicines
Expenditure share: 17.2%
Prescription share: 72.9%
| 2009/10 | 2010/11 | 2011/12 | 2012/13 | 2013/14 | 2014/15 | 2015/16 | 2016/17 | 2017/18 | 2018/19 | 2019/20 | 2020/21 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
British Columbia |
1.00 |
0.95 |
0.80 |
0.70 |
0.54 |
0.52 |
0.51 |
0.50 |
0.47 |
0.38 |
0.38 |
0.38 |
Alberta |
1.00 |
0.96 |
0.96 |
0.78 |
0.50 |
0.47 |
0.46 |
0.44 |
0.40 |
0.33 |
0.32 |
0.32 |
Saskatchewan |
1.00 |
0.99 |
0.88 |
0.75 |
0.67 |
0.63 |
0.54 |
0.52 |
0.49 |
0.41 |
0.40 |
0.40 |
Manitoba |
1.00 |
0.99 |
0.96 |
0.84 |
0.68 |
0.61 |
0.58 |
0.57 |
0.55 |
0.45 |
0.45 |
0.44 |
Ontario |
1.00 |
0.73 |
0.62 |
0.62 |
0.58 |
0.55 |
0.53 |
0.52 |
0.49 |
0.39 |
0.39 |
0.39 |
New Brunswick |
1.00 |
1.01 |
1.00 |
0.78 |
0.52 |
0.48 |
0.46 |
0.45 |
0.44 |
0.34 |
0.34 |
0.34 |
Nova Scotia |
1.00 |
1.00 |
0.92 |
0.76 |
0.63 |
0.56 |
0.49 |
0.48 |
0.47 |
0.36 |
0.36 |
0.36 |
Prince Edward Island |
1.00 |
1.00 |
1.00 |
0.80 |
0.57 |
0.46 |
0.43 |
0.42 |
0.41 |
0.32 |
0.32 |
0.32 |
Newfoundland and Labrador |
1.00 |
1.00 |
1.01 |
0.82 |
0.58 |
0.52 |
0.49 |
0.49 |
0.48 |
0.38 |
0.38 |
0.39 |
Total* |
1.00 |
0.96 |
0.86 |
0.77 |
0.64 |
0.60 |
0.58 |
0.58 |
0.55 |
0.44 |
0.44 |
0.44 |
(c) Single-source non-patented medicines
Expenditure share: 8.6%
Prescription share: 2.5%
| 2009/10 | 2010/11 | 2011/12 | 2012/13 | 2013/14 | 2014/15 | 2015/16 | 2016/17 | 2017/18 | 2018/19 | 2019/20 | 2020/21 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
British Columbia |
1.00 |
1.06 |
1.11 |
1.14 |
1.18 |
1.22 |
1.27 |
1.31 |
1.34 |
1.39 |
1.45 |
1.48 |
Alberta |
1.00 |
1.02 |
1.04 |
1.06 |
1.08 |
1.04 |
1.05 |
1.08 |
1.20 |
1.24 |
1.30 |
1.31 |
Saskatchewan |
1.00 |
1.05 |
1.09 |
1.12 |
1.16 |
1.19 |
1.22 |
1.26 |
1.28 |
1.29 |
1.33 |
1.36 |
Manitoba |
1.00 |
1.04 |
1.09 |
1.12 |
1.16 |
1.21 |
1.26 |
1.29 |
1.31 |
1.33 |
1.36 |
1.39 |
Ontario |
1.00 |
1.01 |
1.02 |
1.05 |
1.07 |
1.10 |
1.13 |
1.16 |
1.20 |
1.23 |
1.26 |
1.27 |
New Brunswick |
1.00 |
1.03 |
1.06 |
1.10 |
1.12 |
1.15 |
1.19 |
1.22 |
1.24 |
1.26 |
1.24 |
1.22 |
Nova Scotia |
1.00 |
1.04 |
1.04 |
1.04 |
1.06 |
1.11 |
1.16 |
1.19 |
1.21 |
1.24 |
1.27 |
1.29 |
Prince Edward Island |
1.00 |
1.10 |
1.13 |
1.17 |
1.23 |
1.21 |
1.21 |
1.25 |
1.27 |
1.30 |
1.35 |
1.37 |
Newfoundland and Labrador |
1.00 |
1.04 |
1.06 |
1.07 |
1.10 |
1.12 |
1.13 |
1.20 |
1.23 |
1.26 |
1.30 |
1.33 |
Total* |
1.00 |
1.04 |
1.07 |
1.10 |
1.13 |
1.15 |
1.18 |
1.18 |
1.23 |
1.25 |
1.29 |
1.31 |
Note: This analysis only includes data for beneficiaries that met their deductible and received public reimbursement.
Yukon is not reported due to data limitations. National results for 2020/21 do not include the Non-Insured Health Benefits (NIHB) program.
The findings are a cost-weighted average of changes in the reimbursed unit costs for individual medicines. The analysis was limited to data for oral solid formulations. The remaining share of prescriptions and expenditures includes devices, compounded drugs, and other products that are reimbursed by public drug plans but do not have a Health Canada assigned Drug Identification Number (DIN).
* Total results for the drugs plans captured in this figure.
Data source: National Prescription Drug Utilization Information System Database, Canadian Institute for Health Information.
Substitution Effect
Shifts from brand-name to generic or biosimilar medicines pulled overall drug costs down by 1.4% in 2020/21, translating to savings of $129 million for the NPDUIS public plans. The top three generic contributors to the substitution effect, which included an adrenergic inhalant (fluticasone/salmeterol), and an immunomodulator (fingolimod) and a drug used in addictive disorders (buprenorphine/naloxone), offered merely -0.3% in savings. Biosimilars contributed more to the substitution effect than generic medicines in 2020/21: three immunosuppressants and one insulin were responsible for half of the savings from substitution: Inflectra/Renflexis (-0.5%), Brenzys/Erelzi (-0.1%), Basaglar (-0.04%) and Truxima/Riximyo/Ruxience (-0.03%).
The share of prescriptions for multi-source non-patented medicines in public plans increased to 87.4% in 2020/21, a significant rise over 83.0% in 2015/16, while their corresponding share of total drug costs changed little over the same time period, from 29.9% to 30.2%. This six-year trend reflects the implementation of generic pricing policies, as well as the genericization of a number of commonly used medicines that lost patent protection in recent years. Multi-source generics alone accounted for 72.9% of prescriptions and 17.2% (as shown in Figure 1.5) of drug costs on 2020/21.
Patented medicines accounted for a decreasing share of prescriptions in 2020/21, dropping from 11.5% to 9.0% since 2015/16. Their share of total public plan drug costs also fell slightly to 56.4% as a result of changes to the patent status of a few top-selling medicines. Despite the loss of patent for a few significant medicines, this segment has held steady around 60% as a result of the increased use of high-cost drugs such as biologics and oral oncology medicines and the introduction of new high-use drugs such as antidiabetics.
Figure 2.4 reports the 2015/16 to 2020/21 trends in market shares by market segment: patented, multi-source non-patented, and single-source non-patented medicines.
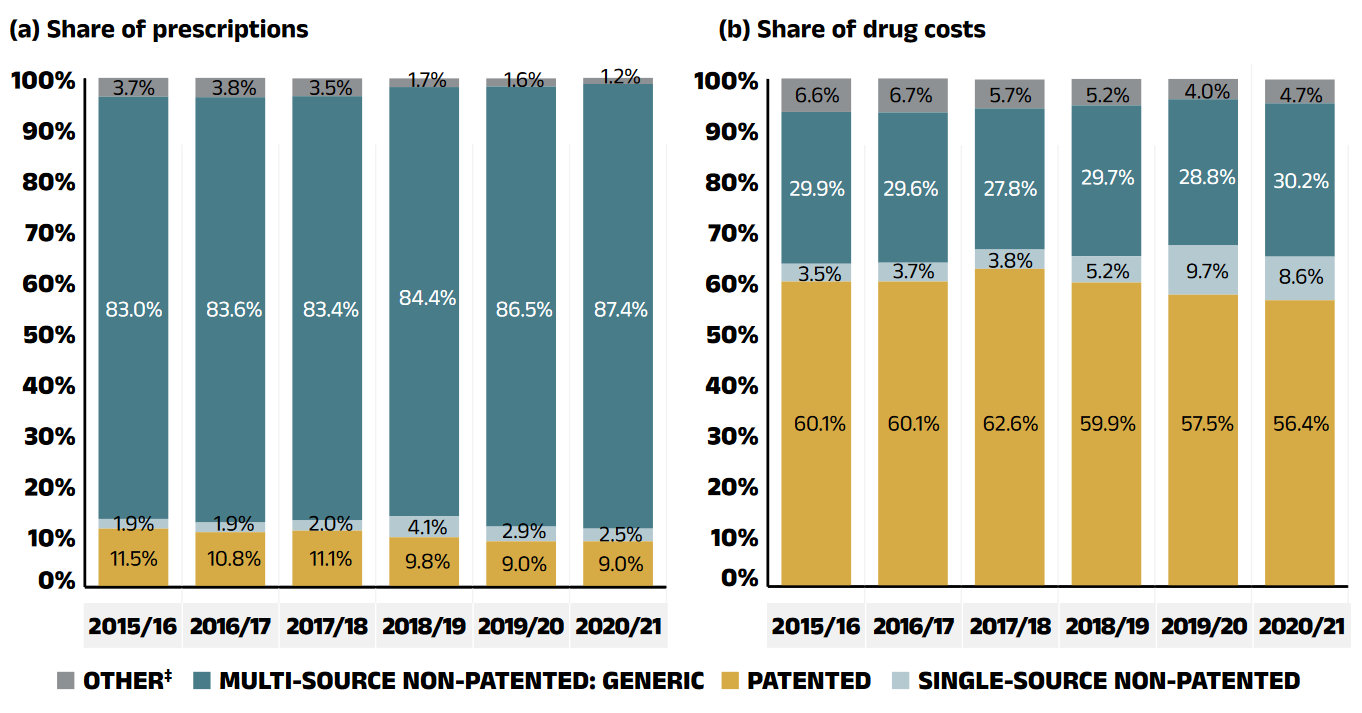
Figure description
This figure shows two complementary stacked column graphs. Graph (a) shows the share of prescriptions by market segment from 2015/16 to 2020/21 for all NPDUIS public drug plans. Graph (b) shows the share of drug costs by market segment for the same period.
(a) Share of prescriptions
| Market segment | 2015/16 | 2016/17 | 2017/18 | 2018/19 | 2019/20 | 2020/21 |
|---|---|---|---|---|---|---|
Patented |
11.5% |
10.8% |
11.1% |
9.8% |
9.0% |
9.0% |
Single-source non-patented |
1.9% |
1.9% |
2.0% |
4.1% |
2.9% |
2.5% |
Multi-source generic |
83.0% |
83.6% |
83.4% |
84.4% |
86.5% |
87.4% |
Other‡ |
3.7% |
3.8% |
3.5% |
1.7% |
1.6% |
1.2% |
(b) Share of drug costs
| Market segment | 2015/16 | 2016/17 | 2017/18 | 2018/19 | 2019/20 | 2020/21 |
|---|---|---|---|---|---|---|
Patented |
60.1% |
60.1% |
62.6% |
59.9% |
57.5% |
56.4% |
Single-source non-patented |
3.5% |
3.7% |
3.8% |
5.2% |
9.7% |
8.6% |
Multi-source generic |
29.9% |
29.6% |
27.8% |
29.7% |
28.8% |
30.2% |
Other‡ |
6.6% |
6.7% |
5.7% |
5.2% |
4.0% |
4.7% |
Note: This analysis only includes data for beneficiaries that met their deductible and received public reimbursement.
* British Columbia, Alberta, Saskatchewan, Manitoba, Ontario, New Brunswick, Nova Scotia, Prince Edward Island, Newfoundland and Labrador, Yukon, and the Non-Insured Health Benefits (NIHB) Program. Results for 2020/21 do not include the NIHB program.
‡ This market segment includes devices, compounded drugs, and other products that are reimbursed by public drug plans but do not have a Health Canada assigned Drug Identification Number (DIN).
Data source: National Prescription Drug Utilization Information System Database, Canadian Institute for Health Information.
Brief Insights: Biosimilars
In April 2016, the pCPA issued the First Principles for Subsequent Entry Biologics to guide negotiations and inform expectations for biologics and biosimilars. This was followed by the creation of the Biologics Policy Directions in September 2018 to further guide and define the process by which biologic and biosimilar products are negotiated and considered for reimbursement by Canada’s public drug plans.
Additionally, the pCPA recently partnered with Cancer Care Ontario on a joint oncology biosimilars initiative, the pan-Canadian Oncology Biosimilars Initiative (pCOBI), that recognizes the unique considerations in the implementation of oncology biosimilars. As of June 2019, biosimilars are no longer subjected to CADTH review and are instead filed directly with the jurisdictions and the pCPA. The pCPA subsequently engaged the Canadian Agency for Drugs and Technologies in Health (CADTH) to conduct an extensive stakeholder consultation and engagement exercise on the implementation and expanded use of biosimilars in Canada. A final summary report from the consultation was released in February 2020.
Many Canadian payers, including public plans in British Columbia, Alberta, Manitoba, Ontario, Quebec, and New Brunswick, have recently undertaken or announced initiatives to prompt switching to available biosimilars and to encourage biosimilar uptake. For more information, see Appendix C: Biosimilar Switching Initiatives by Canadian Public Payers.
A biosimilar drug, or biosimilar, is a biologic drug that is very similar to but less expensive than its originator biologic drug. Although biosimilars are not identical to their originator biologics, there are no expected differences in efficacy and safety between a biosimilar and the originator biologic drug.Reference IV The biosimilars market is a relatively complex space. Compared to traditional generic drug markets, the savings from biosimilars have been limited by slower initial uptake.
Table 2.1 provides an overview of the biosimilars recently approved in Canada. Inflectra, which was approved in Canada in 2014 and marketed publicly in 2016, was one of the first biosimilars available on the Canadian market and has one of the highest list price discounts. Inflectra and Renflexis, approved in 2017, are both indicated for most of the same autoimmune inflammatory diseases as their originator infliximab product Remicade, but despite having list prices set at approximately half that of Remicade, their initial market uptake was slow in the previous years. Over the last year, public drug plans in British Columbia and Alberta have undertaken initiatives to encourage switching from biologics to biosimilars with an aim of increasing biosimilar uptake, contributed to the increase in uptake for the biosimilars targeted by these initiatives. By 2020/21, Inflectra and Renflexis had achieved sizable uptake, capturing 42% of prescriptions.
Brenzys and Erelzi, biosimilars of another anti-TNF-α drug etanercept (Enbrel), were approved for market in Canada in 2016 and 2017, respectively. At approximately two thirds of the list price of their originator biologic, similarly targeted by the biosimilar switching initiatives, they had captured 51.4% of the prescription share of the etanercept market by 2020/21.
Truxima, Riximyo and Ruxience were the recent market entry of biosimilars approved in 2019 and 2020, for the monoclonal antibody medicine rituximab (Rituxan), as a result from the introductions of biosimilar switching initiatives, have captured 26.8% of the prescription share of the rituximab market since the first year being available in the NPDUIS public plans.
To explore the impact of biosimilar entry in a key therapeutic market, Figure 2.5 assesses the distribution of patients receiving anti-TNF-α drugs in the public plans before and after the introduction of biosimilars. Although this market has grown considerably over the last several years, patients on originator biologics without available biosimilars continued to make up the majority (55%) of anti-TNF-α beneficiaries in 2020/21. Although the number of beneficiaries in this class has increased, the introduction of new biosimilars and ongoing initiatives to improve biosimilar uptake have stabilized spending on these medicines.
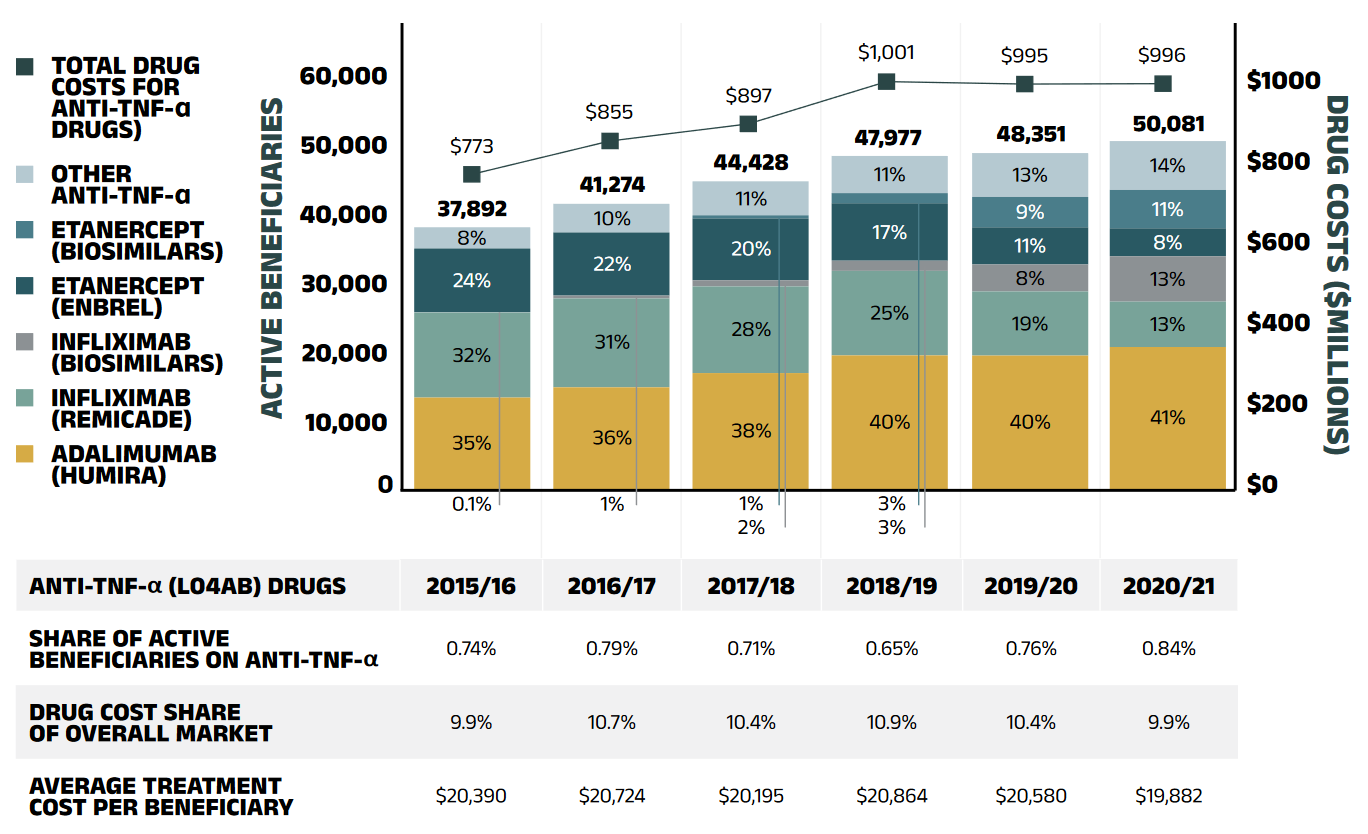
Figure description
A bar graph gives the number of active beneficiaries using anti-TNF-α drugs in the NPDUIS public plans by drug in each year from 2015/16 to 2020/21. Results are given by number of beneficiaries as well as by share of total anti-TNF-α beneficiaries. The total annual drug costs for the class are given in a line above the bars, in millions of dollars.
| Adalimumab (Humira) | Infliximab (Remicade) | Infliximab (biosimilars) | Etanercept (Enbrel) | Etanercept (biosimilars) | Other anti-TNF-α drugs | Total anti-TNF-α beneficiaries | Drug costs, in millions of dollars | |
|---|---|---|---|---|---|---|---|---|
2015/16 |
13,449 (35%) |
12,247 (32%) |
23 (<1%) |
8,998 (24%) |
– |
3,176 (8%) |
37,892 (100%) |
$773 |
2016/17 |
14,867 (36%) |
12,728 (31%) |
314 (1%) |
9,264 (22%) |
– |
4,101 (10%) |
41,274 (100%) |
$855 |
2017/18 |
16,885 (38%) |
12,473 (28%) |
931 (2%) |
8,919 (20%) |
500 (1%) |
4,720 (11%) |
44,428 (100%) |
$897 |
2018/19 |
19,010 (40%) |
12,229 (25%) |
1,615 (3%) |
8,142 (17%) |
1,505 (3%) |
5,476 (11%) |
47,977 (100%) |
$1,001 |
2019/20 |
19,467 (40%) |
8,953 (19%) |
4,080 (8%) |
5,474 (11%) |
4,156 (9%) |
6,221(13%) |
48,351 (100%) |
$995 |
2020/21 |
20,465 (41%) |
6,563 (13%) |
6,542 (13%) |
4,150 (8%) |
5,514 (11%) |
6,847 (14%) |
50,081 |
$996 |
A table below the graph gives the share of total NPDUIS plan active beneficiaries held by anti-TNF-α patients in each year, as well as the anti-TNF-α share of overall drug costs and the average anti-TNF-α treatment cost per beneficiary.
| 2015/16 | 2016/17 | 2017/18 | 2018/19 | 2019/20 | 2020/21 | |
|---|---|---|---|---|---|---|
Anti-TNF-α share of active beneficiaries |
0.74% |
0.79% |
0.71% |
0.65% |
0.76% |
0.84% |
Anti-TNF-α share of overall drug costs |
9.9% |
10.7% |
10.4% |
10.9% |
10.4% |
9.9% |
Average anti-TNF-α treatment cost per beneficiary |
$20,390 |
$20,724 |
$20,195 |
$20,864 |
$20,580 |
$19,882 |
Note: Other anti-TNF-α drugs included golimumab (Simponi) and certolizumab pegol (Cimzia). Results do not distinguish between indications.
* British Columbia, Alberta, Saskatchewan, Manitoba, Ontario, New Brunswick, Nova Scotia, Prince Edward Island, Newfoundland and Labrador, and Yukon.
Data source: National Prescription Drug Utilization Information System Database, Canadian Institute for Health Information.
It has been observed that biosimilars used to treat an acute indication often have a significantly higher rate of uptake than those used for chronic indications. Grastofil, Nivestym and the recently approved Lapelga, Fulphila and Ziextenzo, biosimilars of the white blood cell stimulator filgrastim (Neupogen) and pegfilgrastim (Neulasta), respectively, have the highest uptake in the public plans, at 93.8% and almost 100% in 2020/21, despite the latter having been available in NPDUIS plans for only one year (Table 2.1). Their discount from the originator biologic list price ranged from 25% to 43%.
Biosimilars used in the management of diabetes, including Basaglar, a biosimilar of insulin glargine (Lantus), and Admelog, a biosimilar of insulin lispro (Humalog), have been relatively slow in their market uptake, acquiring 28.3% and 0.1% share of prescriptions of their respective markets, and the latter having been available in NPDUIS plans for only half a year. Their 25% discount from the originator biologic list price places them at the bottom of the biosimilars in terms of price discounts.
Table 2.1 Biosimilars recently approved in Canada, NPDUIS public drug plans*, 2020/21
| Originator biologic | Biosimilar | |||||
|---|---|---|---|---|---|---|
| Medicinal ingredient (trade name) | Drug cost, $million (% share) | Trade name | Market approval | First reimbursement | Price discount† from originator biologic | Share of prescriptions for medicinal ingredient |
Remicade (infliximab) |
$268.5 (2.7%) |
Inflectra |
15-Jan-14 |
Q1-2016 |
46.8% |
42% |
Renflexis |
01-Dec-17 |
Q3-2018 |
50.1% |
|||
Enbrel (etanercept) |
$85.4 (0.8%) |
Brenzys |
31-Aug-16 |
Q3-2017 |
33.7% |
51.4% |
Erelzi |
06-Apr-17 |
Q4-2017 |
37.2% |
|||
Rituximab (rituxan) |
$28.5 (0.3%) |
Truxima |
04-Apr-19 |
Q1-2020 |
30.0% |
26.8% |
Riximyo |
28-Apr-20 |
Q3-2020 |
37.0% |
|||
Ruxience |
04-May-20 |
Q3-2020 |
35.0% |
|||
Lantus |
$79.5 (0.8%) |
Basaglar |
01-Sep-15 |
Q3-2017 |
25.0% |
28.3% |
Insulin lispro |
$41.2 (0.4%) |
Admelog |
16-Nov-17 |
Q4-2020 |
25.0% |
0.1% |
Neupogen (filgrastim) |
$3.1 (<0.1%) |
Grastofil |
07-Dec-15 |
Q4-2016 |
25.0% |
93.8% |
Nivestym |
16-Apr-20 |
Q3-2020 |
25.0% |
|||
Neulasta (pegfilgrastim) |
N/A |
Lapelga |
05-Apr-18 |
Q2-2019 |
25.0% ‡ |
100.0% |
Fulphila |
24-Dec-18 |
Q1-2020 |
36.1% |
|||
Ziextenzo |
21-Apr-20 |
Q3-2020 |
43.1% |
|||
Note: This analysis is based on publicly available pricing information. It does not reflect confidential price discounts negotiated by the pCPA on behalf of the public plans.
* British Columbia, Alberta, Saskatchewan, Manitoba, Ontario, New Brunswick, Nova Scotia, Prince Edward Island, Newfoundland and Labrador, and Yukon.
† Based on Ontario Drug Benefit formulary listing price at the time of the biosimilar entry. This price may change over time; for example, the list price for Brenzys was recently lowered to match Erelzi. The price discounts do not reflect confidential rebates from negotiation.
‡ Based on the value reported in CADTH’s Biosimilar Summary Dossier , which sourced prices from Alberta’s Health Formulary as Alberta was the only CADTH-participating jurisdiction with publicly available pricing for Neulasta at the time of the biosimilar entry. The price discounts do not reflect confidential rebates from negotiation.
Data source: National Prescription Drug Utilization Information System Database, Canadian Institute for Health Information.
Recently, Canadian payers, including public drug plans in British Columbia, Alberta, Manitoba, and New Brunswick, have undertaken or proposed a number of initiatives to increase biosimilar uptake. For more information on the market distribution of biosimilars and their originator biologics in each jurisdiction, see Appendix B. Future editions of CompassRx will continue to follow the impact of these initiatives.
Drug-Mix Effect
Shifts in use between lower - and higher-cost drugs pushed overall cost levels for the NPDUIS drug plans up by 6.3% ($605 million) in 2020/21. The separately reported DAA drugs for the treatment of hepatitis C, which have had significant impacts on public plan drug costs trends over the last few years, cost $197 million less in 2020/21 than they did in 2019/20, pulling overall costs downward by -2.1%.
Spotlight on DAA drugs for hepatitis C
Direct-acting antiviral (DAA) drugs for hepatitis C have had a significant but variable impact on public plan drug costs over the last few years. Pricing agreements for most of these medicines were reached between 2014 and 2016 through the pan-Canadian Pharmaceutical Alliance (pCPA) and were expanded in 2017 with a multistakeholder agreement that included several new drugs along with those that were already being reimbursed.
The number of active beneficiaries using DAA drugs spiked in 2015/16 and declined sharply the following year. With the subsequent entry of newer DAAs and expanded treatment criteria, the beneficiary group increased by nearly 60% to reach 11,920 in 2017/18 and continued to rise through 2018/19, bringing the total number of active beneficiaries to 13,019.
As these medicines are curative treatments and have now been on the market for several years, it was not unexpected to observe that the national reported hepatitis C rate had declined by 10% (from 33.9 to 30.4 cases per 100,000 population) from 2018 to 2019.Reference V Although DAAs continued to hold a sizable share (5.4%) of drug costs in NPDUIS public drug plans in 2019/20, the number of active beneficiaries using DAA drugs fell to 10,887 and continued to decline in the subsequent year. In 2020/21, the share of drug costs and the number of active beneficiaries for DAA drugs dropped by nearly 50% to 2.9% of drug costs and 6,248 active beneficiaries in NPDUIS public plans, representing a $197 million reduction in overall costs for the fiscal year.
Given their diminishing impact on the growth in spending for public plans, this will be the last edition of CompassRx to include a separate DAA effect. For historical data, please consult previous editions.
Figure 2.6 reports the 10 medicines that made the greatest contribution to the drug-mix effect in 2020/21, together accounting for an upward push of 3.4% on overall drug costs. Four medicines made their first appearance on this list in 2020/21: Tagrisso, Ocrevus, Skyrizi, and Fasenra. These medicines received market authorization from Health Canada only two to five years prior.
Two antidiabetics, semaglutide (Ozempic) and empagliflozin (Jardiance), topped the list of high-impact drugs with a 1.3% contribution to the growth in drug costs, while another antidiabetic, insulin degludec (Tresiba) also remained on the top 10 contributors list. Five of the other top contributors were high-cost drugs with average annual treatment costs ranging from $10,988 to $69,717, including one oral oncology product, two immunosuppressants, one antiviral, and a new biologic treatment for obstructive airway diseases. The two remaining medicines were either high-use drugs or had relatively low annual treatment costs.
Four medicines that made the top 10 contributors list in the 2019/20 report were left out in 2020/21. Imbruvica, Ibrance, and Entyvio continued to have a sizable impact on the drug-mix effect and remained among the top 20 contributors in 2020/21, while Eylea’s costs remained stable without any appreciable uptake.
The share of total drug costs for each of the top contributors is reported table accompanying Figure 2.6. Note that this value differs from the contribution to the drug-mix effect, which measures the growth (increase or decrease in costs over time) rather than the costs themselves.
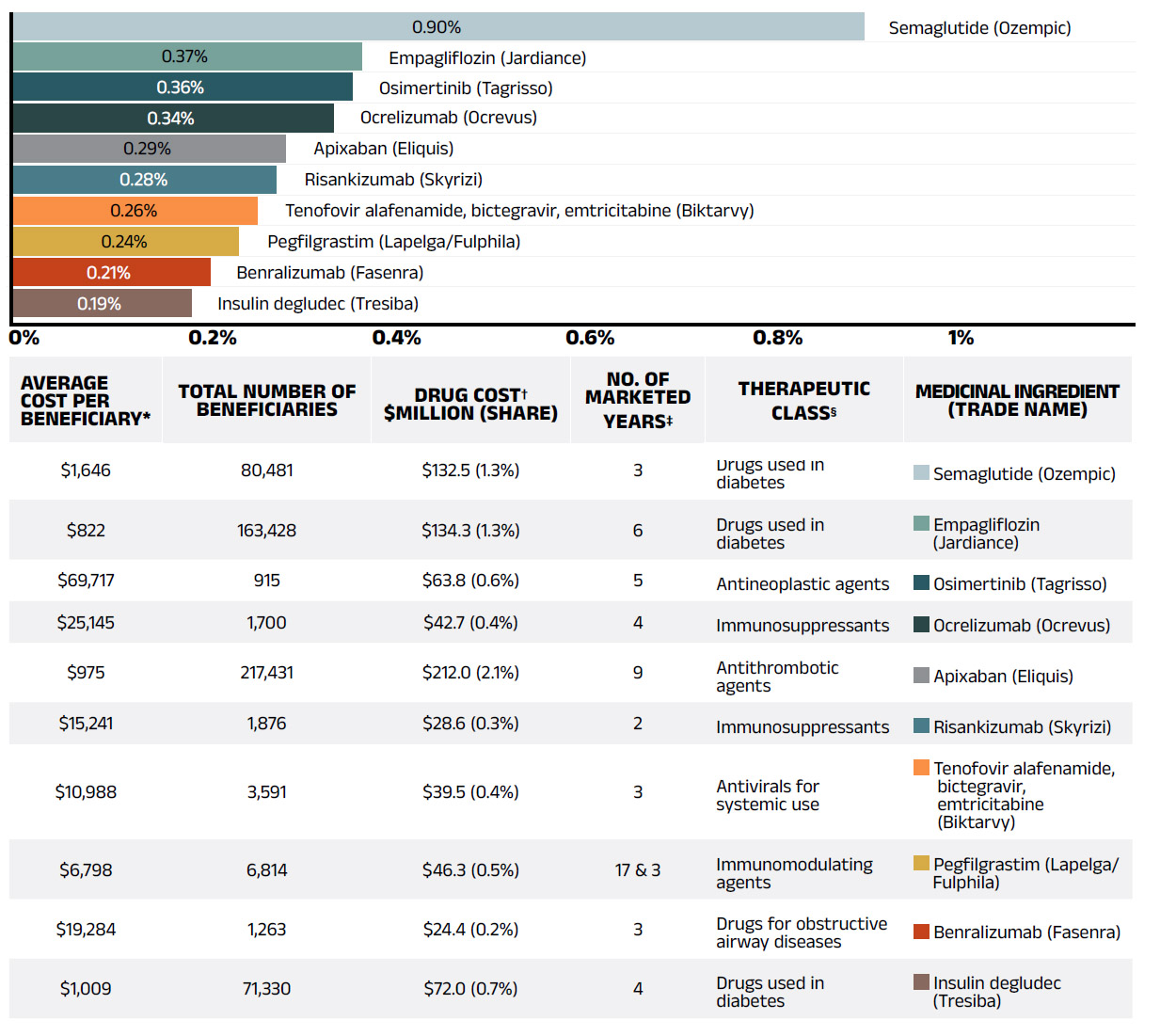
Figure description
A horizontal bar graph depicts the top 10 drugs that contributed to the drug-mix effect in the NPDUIS public drug plans in 2020/21. An accompanying table gives the average cost per beneficiary; total number of beneficiaries; drug cost in millions of dollars; share of the total drug cost; number of years the drug has been marketed in Canada; therapeutic class; and trade name and medicinal ingredient for each drug.
| Average cost per beneficiary* | Total number of beneficiaries | Drug cost†, in millions of dollars (share) | Number of marketed years‡ | Therapeutic class§ | Medicinal ingredient (trade name) | Contribution to the drug-mix effect |
|---|---|---|---|---|---|---|
$1,646 |
80,481 |
$132.5 (1.3%) |
3 |
Drugs used in diabetes |
Semaglutide (Ozempic) |
0.90% |
$822 |
163,428 |
$134.3 (1.3%) |
6 |
Drugs used in diabetes |
Empagliflozin (Jardiance) |
0.37% |
$69,717 |
915 |
$63.8 (0.6%) |
5 |
Antineoplastic agents |
Osimertinib (Tagrisso) |
0.36% |
$25,145 |
1,700 |
$42.7 (0.4%) |
4 |
Immunosuppressants |
Ocrelizumab (Ocrevus) |
0.34% |
$975 |
217,431 |
$212 (2.1%) |
9 |
Antithrombotic agents |
Apixaban (Eliquis) |
0.29% |
$15,241 |
1,876 |
$28.6 (0.3%) |
2 |
Immunosuppressants |
Risankizumab (Skyrizi) |
0.28% |
$10,988 |
3,591 |
$39.5 (0.4%) |
3 |
Antivirals for systemic use |
Tenofovir alafenamide, bictegravir, emtricitabine (Biktarvy) |
0.26% |
$6,798 |
6,814 |
$46.3 (0.5%) |
17 & 3 |
Immunomodulating agents |
Pegfilgrastim (Lapelga/Fulphila) |
0.24% |
$19,284 |
1,263 |
$24.4 (0.2%) |
3 |
Drugs for obstructive airway diseases |
Benralizumab (Fasenra) |
0.21% |
$1,009 |
71,330 |
$72 (0.7%) |
4 |
Drugs used in diabetes |
Insulin degludec (Tresiba) |
0.19% |
Note: This analysis only includes data for beneficiaries that met their deductible and received public reimbursement.
* British Columbia, Alberta, Saskatchewan, Manitoba, Ontario, New Brunswick, Nova Scotia, Prince Edward Island, Newfoundland and Labrador, and Yukon.
† All of the top contributors to the push effect are associated with product listing agreements (PLAs) from pCPA negotiations for one or multiple indications; however, reported drug costs do not reflect price reductions resulting from confidential PLAs.
‡ The number of years since the drug was authorized for market by Health Canada, as of 2020/21.
§ The therapeutic class is based on ATC level 2. Jurisdictions that have special programs for ophthalmological drugs are not captured in the results.
Data source: National Prescription Drug Utilization Information System Database, Canadian Institute for Health Information.
A growing number of high-cost drugs have been reimbursed by NPDUIS public plans in recent years, often targeting relatively small patient populations. The number of medicines with an average annual cost per beneficiary exceeding $10,000 increased significantly from 95 in 2015/16 to 135 in 2020/21. These drugs, which accounted for 27.3% of the overall NPDUIS drug costs in 2015/16, made up 34.7% of costs in 2020/21, while representing only a very small percentage of active beneficiaries (2.5%).
Although there has been a sustained growth in the drug cost share of all high-cost drugs in recent years, the steepest increase has been among those in the highest cost band ($50,000+), other than DAAs. Figure 2.7 reports on trends in the market for high-cost drugs from 2015/16 to 2020/21 by average annual drug cost per active beneficiary determined at the medicinal ingredient level: $10,000–$20,000; $20,000–$50,000; and $50,000 or more.
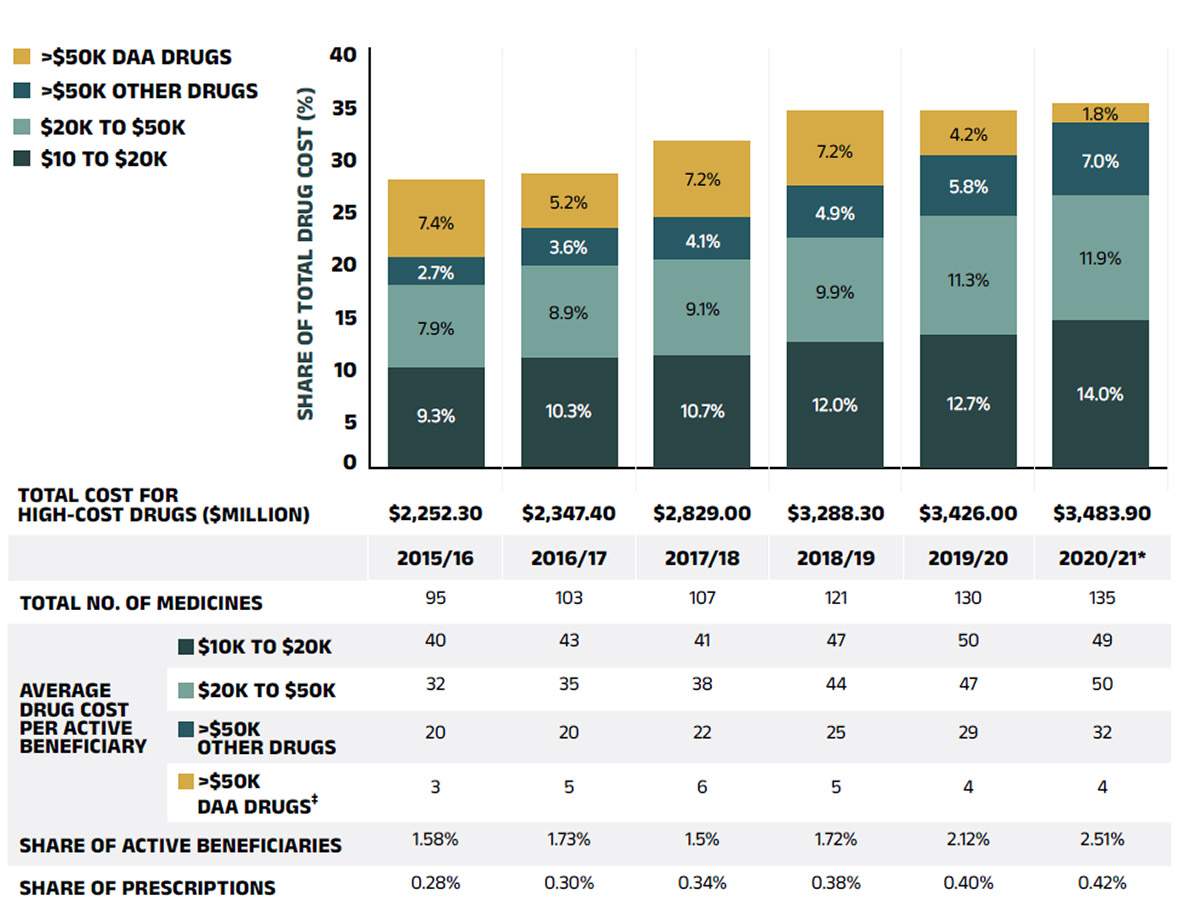
Figure description
This stacked column graph and accompanying table give the trends in high-cost drugs from 2015/16 to 2020/21. A graph reports the share of drug costs for high-cost drugs broken out by average cost per active beneficiary: $10,000‒20,000; $20,000–$50,000; and greater than $50,000. The share of new direct-acting antiviral drugs for hepatitis C is reported separately. The table gives the total number of high-cost medicines, the number of medicines in each cost band, the share of beneficiaries using these drugs, and the share of prescriptions that they represent.
| 2015/16 | 2016/17 | 2017/18 | 2018/19 | 2019/20 | 2020/21* | |
|---|---|---|---|---|---|---|
Total number of medicines |
95 |
103 |
107 |
121 |
130 |
135 |
Total drug cost for all high-cost drugs, in millions of dollars |
$2,252.3 |
$2,347.4 |
$2,829.0 |
$3,288.3 |
$3,426.0 |
$3,483.9 |
Average cost per active beneficiary of $10,000‒20,000: share of total drug cost |
9.3% |
10.3% |
10.7% |
12.0% |
12.7% |
14.0% |
Average cost per active beneficiary of $10,000‒20,000: number of medicines |
40 |
43 |
41 |
47 |
50 |
49 |
Average cost per active beneficiary of $20,000–$50,000: share of total drug cost |
7.9% |
8.9% |
9.1% |
9.9% |
11.3% |
11.9% |
Average cost per active beneficiary of $20,000–$50,000: number of medicines |
32 |
35 |
38 |
44 |
47 |
50 |
Average cost per active beneficiary of greater than $50,000: share of total drug cost for other drugs |
2.7% |
3.6% |
4.1% |
4.9% |
5.8% |
7.0% |
Average cost per active beneficiary of greater than $50,000: number of medicines for other drugs |
20 |
20 |
22 |
25 |
29 |
32 |
Average cost per active beneficiary of greater than $50,000: share of total drug cost for direct-acting antiviral drugs |
7.4% |
5.2% |
7.2% |
7.2% |
4.2% |
1.8% |
Average cost per active beneficiary of greater than $50,000: number of medicines for direct-acting antiviral drugs |
3 |
5 |
6 |
5 |
4 |
4 |
High-cost drugs – share of total drug cost |
27.3% |
27.9% |
31.0% |
34.1% |
34.0% |
34.7% |
High-cost drugs – share of active beneficiaries |
1.58% |
1.73% |
1.75% |
1.72% |
2.12% |
2.51% |
High-cost drugs – share of total prescriptions |
0.28% |
0.30% |
0.34% |
0.38% |
0.40% |
0.42% |
Note: This analysis only includes data for beneficiaries that met their deductible and received public reimbursement. These results may be underestimated, as some high-cost drugs are reimbursed through special public drug plan programs that are not captured in the NPDUIS data. The methodology for this analysis was revised for the 2018/19 report, and as such, historical results may not match those reported in previous editions.
* Average annual drug costs per active beneficiary exceeding $10,000.
† British Columbia, Alberta, Saskatchewan, Manitoba, Ontario, New Brunswick, Nova Scotia, Prince Edward Island, Newfoundland and Labrador, Yukon, and the Non-Insured Health Benefits (NIHB) Program. Results for 2020/21 do not include the NIHB program.
‡ Direct-acting antiviral (DAA) drugs used in the treatment of hepatitis C.
Data source: National Prescription Drug Utilization Information System Database, Canadian Institute for Health Information.
Figure 2.8 provides a more detailed breakdown of the share of high-cost drugs by jurisdiction in 2020/21. Highcost drugs account for a greater share of costs in incomeand premium-based programs; for example, they make up approximately half of the total drug costs for public plans in British Columbia (44.4%) and Manitoba (57.4%).
These types of programs require beneficiaries to be responsible for a portion of prescription costs, either as a percentage of income or a premium. As such, plan spending is more heavily skewed toward beneficiaries with higher overall costs, and therefore high-cost drugs.
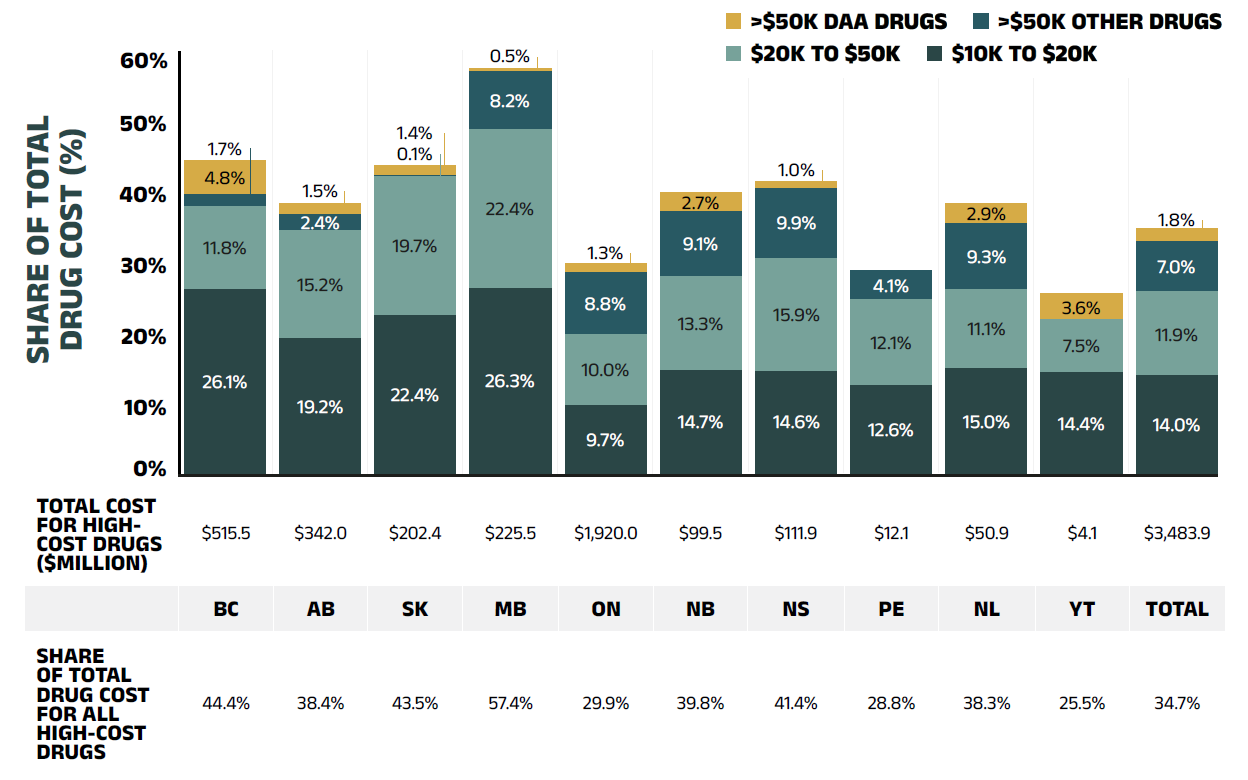
Figure description
This stacked column graph and accompanying table give the share of high-cost drugs for the total drug cost of each NPDUIS public drug plan in 2020/21. The share of high-cost drugs is broken out by average cost per active beneficiary: $10,000‒20,000; $20,000–$50,000; and greater than $50,000. The share of new direct-acting antiviral drugs for hepatitis C is reported separately. Price tags below the bars give the total costs for all high-cost drugs, and the table lists the total share for all high-costs drugs for each jurisdiction.
| British Columbia | Alberta | Saskatchewan | Manitoba | Ontario | New Brunswick | Nova Scotia | Prince Edward Island | Newfoundland and Labrador | Yukon | Total | |
|---|---|---|---|---|---|---|---|---|---|---|---|
Total drug cost for all high-cost drugs, in millions of dollars |
$515.5 |
$342.0 |
$202.4 |
$225.5 |
$1,920.0 |
$99.5 |
$111.9 |
$12.1 |
$50.9 |
$4.1 |
$3,483.9 |
Average cost per beneficiary of $10,000‒20,000: share of total drug cost |
26.1% |
19.2% |
22.4% |
26.3% |
9.7% |
14.7% |
14.6% |
12.6% |
15.0% |
14.4% |
14.0% |
Average cost per beneficiary of $20,000–$50,000: share of total drug cost |
11.8% |
15.2% |
19.7% |
22.4% |
10.0% |
13.3% |
15.9% |
12.1% |
11.1% |
7.5% |
11.9% |
Average cost per beneficiary of greater than $50,000: share of total drug cost for other drugs |
1.7% |
2.4% |
0.1% |
8.2% |
8.8% |
9.1% |
9.9% |
4.1% |
9.3% |
0.0% |
7.0% |
Average cost per beneficiary of greater than $50,000: share of total drug cost for direct-acting antiviral drugs |
4.8% |
1.5% |
1.4% |
0.5% |
1.3% |
2.7% |
1.9% |
0.0% |
2.9% |
3.6% |
1.8% |
High-cost drugs share of total drug cost |
44.4% |
38.4% |
43.5% |
57.4% |
29.9% |
39.8% |
41.4% |
28.8% |
38.3% |
25.5% |
34.7% |
Note: This analysis only includes data for beneficiaries that met their deductible and received public reimbursement. These results may be underestimated, as some high-cost drugs are reimbursed through special public drug plan programs that are not captured in the NPDUIS data.
* Average annual drug costs per active beneficiary exceeding $10,000.
† Direct-acting antiviral (DAA) drugs used in the treatment of hepatitis C.
Data source: National Prescription Drug Utilization Information System Database, Canadian Institute for Health Information.
NPDUIS public plans paid the majority (i.e., over 91% as shown in Figure 2.9) of prescription costs for a relatively small number of high-cost beneficiaries in 2020/21. These beneficiaries were responsible for close to 60% of total drug costs. As shown in Figure 1.2, NPDUIS public plans paid an average of 87% of total prescription costs in 2020/21, while the remaining 13% was paid by the beneficiaries either out of pocket or through a private insurer. To understand the extent the plan-paid and beneficiary-paid portions of prescription costs are associated with the beneficiary’s total annual drug costs, Figure 2.9 provides a breakdown of the plan-paid share of NPDUIS drug plan expenditures by average beneficiary annual drug cost level in 2020/21.
The figure shows that plans paid a larger portion of prescription costs for higher-cost beneficiaries. In 2019/20, the 5% of beneficiaries that had annual drug costs over $5,000 accounted for nearly 60% of overall drug costs for the public plans. For beneficiaries in the highest cost band—those with annual costs over $50,000—the plan-paid share of costs ranged from 97% to close to 100%.
Beneficiaries are grouped into five cost tiers: less than $5,000; $5,000–$10,000; $10,000–$20,000; $20,000– $50,000; and $50,000 or more.
There were considerable jurisdictional differences in planpaid shares due to variations in plan design, eligibility, and other factors.
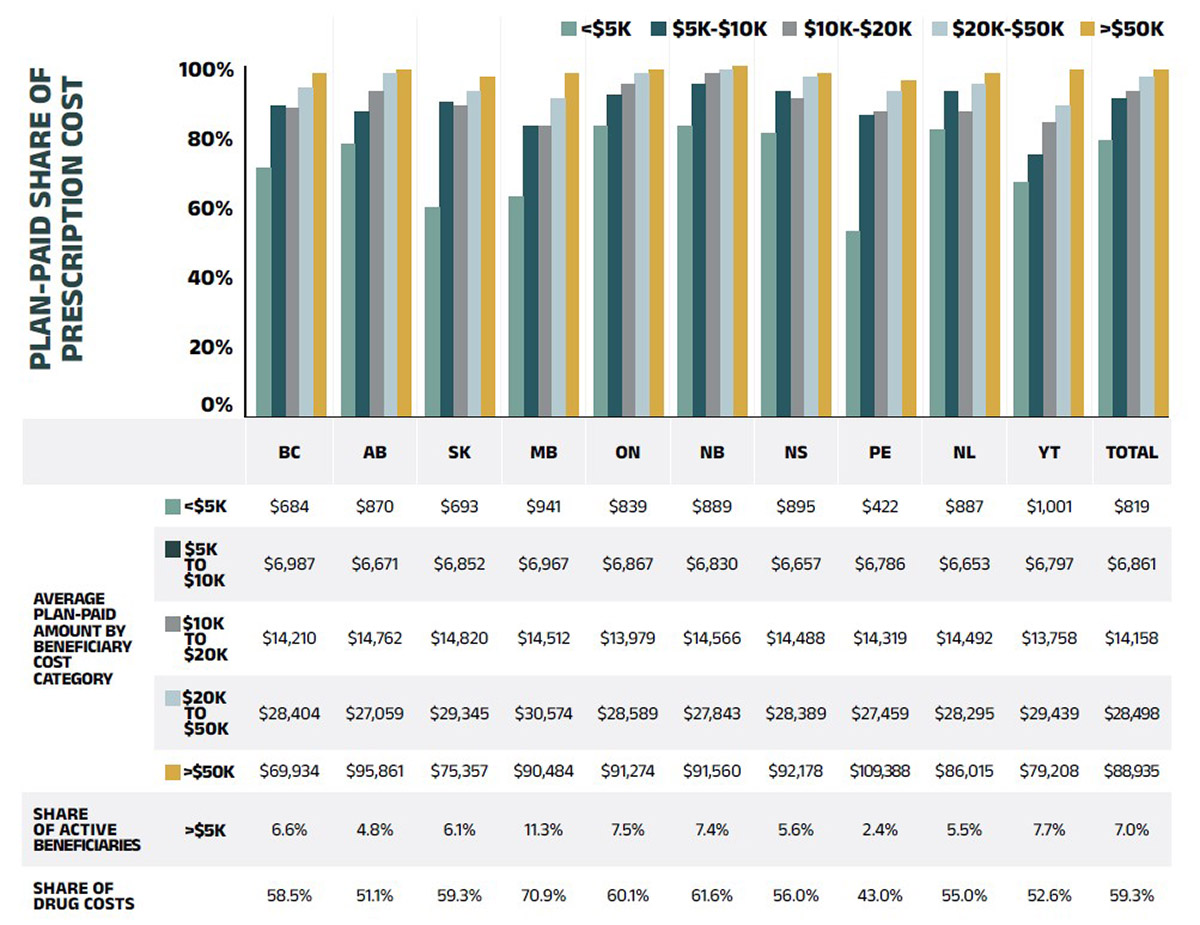
Figure description
This column graph gives the percentage of prescription costs paid by the public drug plans in 2019/20 by beneficiary drug cost. Beneficiaries are grouped by average annual drug costs: less that $5,000; $5,000–$10,000; $10,000–$20,000; $20,000–$50,000; and greater than $50,000.
| Average beneficiary annual drug cost | British Columbia | Alberta | Saskatchewan | Manitoba | Ontario | New Brunswick | Nova Scotia | Prince Edward Island | Newfoundland and Labrador | Yukon | Total | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
Plan-paid share of prescription cost |
Less than $5,000 |
71% |
78% |
60% |
63% |
83% |
83% |
81% |
53% |
82% |
67% |
79% |
$5,000–$10,000 |
89% |
87% |
90% |
83% |
92% |
95% |
93% |
86% |
93% |
75% |
91% |
|
$10,000–$20,000 |
88% |
93% |
89% |
83% |
95% |
98% |
91% |
87% |
87% |
84% |
93% |
|
$20,000–$50,000 |
94% |
98% |
93% |
91% |
98% |
99% |
97% |
93% |
95% |
89% |
97% |
|
Greater than $50,000 |
98% |
99% |
97% |
98% |
99% |
100% |
98% |
96% |
98% |
99% |
99% |
A table below the graph gives the plan-paid amounts in absolute values, as well as the total share of active beneficiaries with annual drug costs over $5,000 and their share of drug costs in each jurisdiction.
| Average beneficiary annual drug cost | British Columbia | Alberta | Saskatchewan | Manitoba | Ontario | New Brunswick | Nova Scotia | Prince Edward Island | Newfoundland and Labrador | Yukon | Total | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
Average plan-paid amount |
Less than $5,000 |
$684 |
$870 |
$693 |
$941 |
$839 |
$889 |
$895 |
$422 |
$887 |
$1,001 |
$819 |
$5,000–$10,000 |
$6,987 |
$6,671 |
$6,852 |
$6,967 |
$6,867 |
$6,830 |
$6,657 |
$6,786 |
$6,653 |
$6,797 |
$6,861 |
|
$10,000–$20,000 |
$14,210 |
$14,762 |
$14,820 |
$14,512 |
$13,979 |
$14,566 |
$14,488 |
$14,319 |
$14,492 |
$13,758 |
$14,158 |
|
$20,000–$50,000 |
$28,404 |
$27,059 |
$29,345 |
$30,574 |
$28,589 |
$27,843 |
$28,389 |
$27,459 |
$28,295 |
$29,439 |
$28,498 |
|
Greater than $50,000 |
$69,934 |
$95,861 |
$75,357 |
$90,484 |
$91,274 |
$91,560 |
$92,178 |
$109,388 |
$86,015 |
$79,208 |
$88,935 |
|
Share of active beneficiaries |
Greater than $5,000 |
6.6% |
4.8% |
6.1% |
11.3% |
7.5% |
7.4% |
5.6% |
2.4% |
5.5% |
7.7% |
7.0% |
Share of drug costs |
|
58.5% |
51.1% |
59.3% |
70.9% |
60.1% |
61.6% |
56.0% |
43.0% |
55.0% |
52.6% |
59.3% |
* Beneficiaries were categorized based on the amount that a drug program paid per year.
Data source: National Prescription Drug Utilization Information System Database, Canadian Institute for Health Information.
Table 2.2 reports the 10 highest-cost drugs reimbursed by the NPDUIS public plans in 2020/21 ranked by their average annual drug cost per active beneficiary. All 10 drugs were indicated to treat rare diseases and had treatment costs exceeding $200,000.
Note that although Table 2.2 presents the overall results for all NPDUIS public drug plans, there are significant variations at the individual plan level.
Table 2.2 Top 10 drugs with the highest average annual drug cost per active beneficiary, NPDUIS public drug plans*, 2020/21
| Medicinal ingredient (trade name) |
Therapeutic class, ATC level 2 | Average drug cost per beneficiary† | No. of marketed years‡ |
|---|---|---|---|
Alglucosidase alfa (Myozyme) |
Other alimentary tract and metabolism products |
$578,128 |
15 |
Asfotase alfa (Strensiq) |
Other alimentary tract and metabolism products |
$543,611 |
6 |
Eculizumab (Soliris) |
Immunosuppressants |
$474,173 |
12 |
Cerliponase alfa (Brineura) |
Other alimentary tract and metabolism products |
$438,690 |
2 |
Nusinersen (Spinraza) |
Other drugs for disorders of the musculo-skeletal system |
$365,871 |
4 |
Elosulfase alfa (Vimizim) |
Other alimentary tract and metabolism products |
$299,413 |
7 |
Velaglucerase alfa (Vpriv) |
Other alimentary tract and metabolism productss |
$291,415 |
11 |
Teduglutide (Revestive) |
Other alimentary tract and metabolism products |
$253,420 |
6 |
Ivacaftor (Kalydeco) |
Other respiratory system products |
$235,150 |
8 |
Migalastat (Galafold) |
Other alimentary tract and metabolism products |
$223,505 |
4 |
Note: This analysis only includes data for beneficiaries that met their deductible and received public reimbursement. This list of drugs does not include high-cost drugs reimbursed through special programs, which are not captured in the NPDUIS data.
* British Columbia, Alberta, Saskatchewan, Manitoba, Ontario, New Brunswick, Nova Scotia, Prince Edward Island, Newfoundland and Labrador, and Yukon.
† Represents the total drug cost divided by the total number of beneficiaries and, thus, may include beneficiaries with incomplete treatment costs.
‡ The number of years since the drug was authorized for market by Health Canada, as of 2020/21.
Data source: National Prescription Drug Utilization Information System Database, Canadian Institute for Health Information.
Over the past few years, biologic medicines have captured an increasing share of the total drug costs for the NPDUIS public plans. In 2020/21, the biologics market share grew by 7.8% to reach 30.3% ($3.0 billion) of total drug costs. The top four biologic medicines— adalimumab (Humira), infliximab (Remicade and biosimilars), aflibercept (Eylea), and ranibizumab (Lucentis)—were responsible for 13.0% of total NPDUIS drug costs.
Figure 2.10 reports on trends in the biologic share of total drug costs for the NPDUIS public drug plans, along with the growth in drug costs for this market segment and the current list of top 10 biologic medicines.
Saskatchewan and Alberta had the highest levels of biologics-related costs relative to total drug costs in 2020/21 (41.7% and 39.0%, respectively), while Nova Scotia and New Brunswick had the highest rates of growth (19.4% and 14.2%, respectively). Variations among plans may be driven by differing plan designs, eligibility for reimbursement, the disease profiles of the population, and the size of the plan, among other considerations.
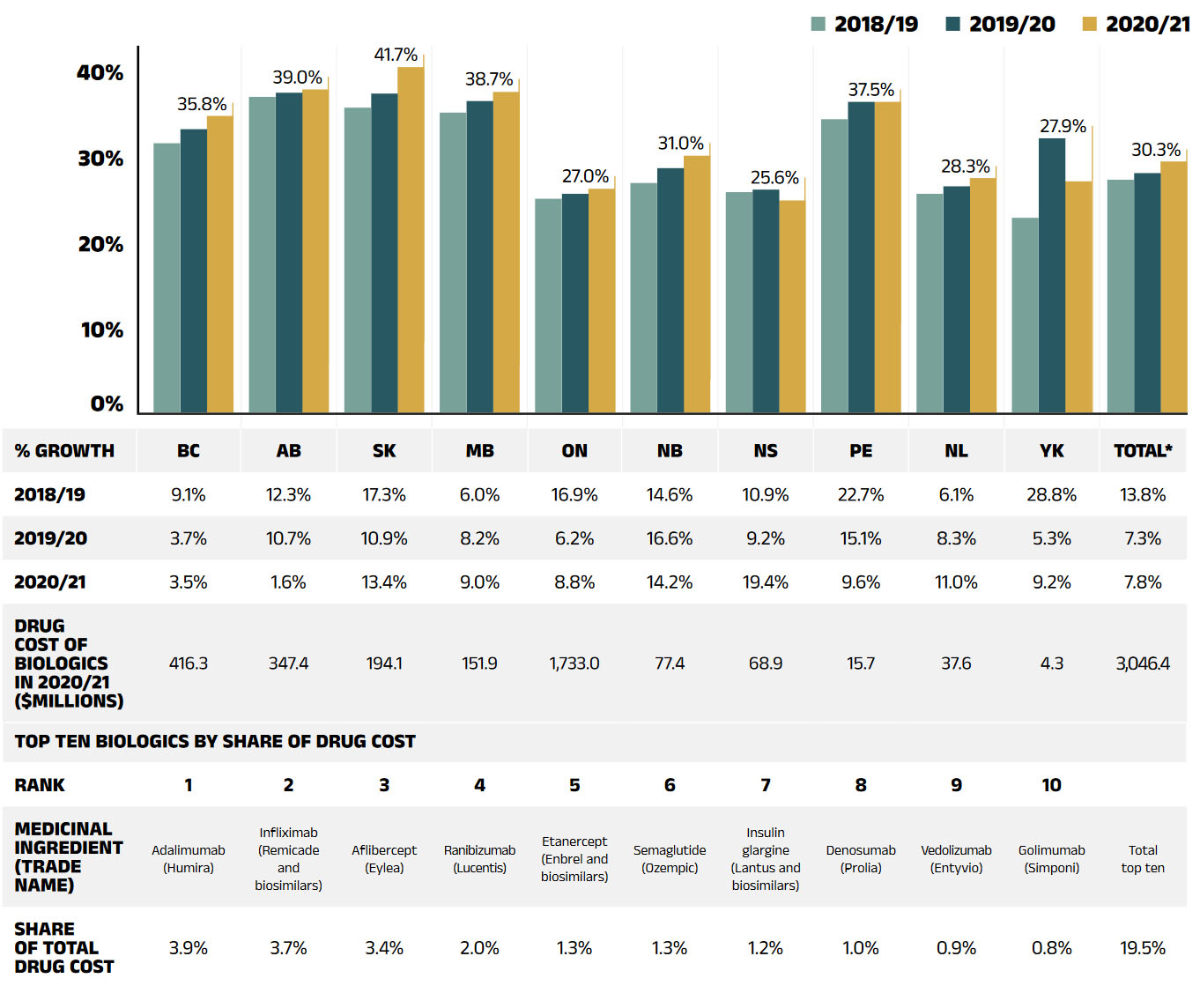
Figure description
This column graph gives the biologic drug share of the total drug costs for the NPDUIS public drug plans from 2018/19 to 2020/21. There are three tables below the bar graph: the first shows the percent year-over-year growth in biologic drug costs over three years for each NPDUIS plan; the second gives the total cost of biologics in millions of dollars for 2020/21by plan; and the third lists the top ten biologics by share of drug cost for all plans in 2020/21.
| British Columbia | Alberta | Saskatchewan | Manitoba | Ontario | New Brunswick | Nova Scotia | Prince Edward Island | Newfoundland and Labrador | Yukon | Total | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Biologic share of total drug costs by year | |||||||||||
2018/19 |
32.5% |
38.1% |
36.8% |
36.2% |
25.8% |
27.7% |
26.6% |
35.4% |
26.4% |
23.5% |
28.1% |
2019/20 |
34.2% |
38.6% |
38.5% |
37.6% |
26.4% |
29.5% |
26.9% |
37.5% |
27.3% |
33.1% |
28.9% |
2020/21 |
35.8% |
39.0% |
41.7% |
38.7% |
27.0% |
31.0% |
25.6% |
37.5% |
28.3% |
27.9% |
30.3% |
| Percent growth year over year | |||||||||||
2018/19 |
9.1% |
12.3% |
17.3% |
6.0% |
16.9% |
14.6% |
10.9% |
22.7% |
6.1% |
28.8% |
13.8% |
2019/20 |
3.7% |
10.7% |
10.9% |
8.2% |
6.2% |
16.6% |
9.2% |
15.1% |
8.3% |
5.3% |
7.3% |
2020/21 |
3.5% |
1.6% |
13.4% |
9.0% |
8.8% |
14.2% |
19.4% |
9.6% |
11.0% |
9.2% |
7.8% |
Drug cost of biologics in 2019/20, in millions of dollars |
416.3 |
347.4 |
194.1 |
151.9 |
1,733.00 |
77.4 |
68.9 |
15.7 |
37.6 |
4.3 |
3,046.40 |
Top 10 biologics by share of drug cost
| Rank | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | Total top 10 |
|---|---|---|---|---|---|---|---|---|---|---|---|
Trade name |
Adalimumab (Humira) |
Infliximab (Remicade and biosimilars) |
Aflibercept (Eylea) |
Ranibizumab (Lucentis) |
Etanercept (Enbrel and biosimilars) |
Semaglutide (Ozempic) |
Insulin glargine (Lantus and biosimilars) |
Denosumab (Prolia) |
Vedolizumab (Entyvio) |
Golimumab (Simponi) |
|
Share of total drug cost |
3.9% |
3.7% |
3.4% |
2.0% |
1.3% |
1.3% |
1.2% |
1.0% |
0.9% |
0.8% |
19.5% |
Note: This analysis only includes data for beneficiaries that met their deductible and received public reimbursement.
Data source: National Prescription Drug Utilization Information System Database, Canadian Institute for Health Information.
An analysis by therapeutic area suggests that over two thirds of the total drug costs in 2020/21 were concentrated in just five classes. Antineoplastic and immunomodulating agents topped the list of therapeutic classes, the same as in 2015/16; however, they represented a significantly higher share of the total costs (having increased from 19.1% in 2015/16 to 29.5% in 2020/21). This reflects a further shift towards oral oncology medicines and a higher use of immunomodulating drugs. Alimentary tract and metabolism medicines held the second highest share of costs (14.4%), due in part to new antidiabetics.
Nervous system medicines, which include relatively lowcost drugs used by a large number of active beneficiaries, represented a lower share of costs (10.8%) in 2020/21, primarily due to significant increases in other therapeutic areas. The cost share of anti-infectives for systemic use was largely shaped by the introduction and use of DAA drugs for the treatment of hepatitis C from 2015/16 to 2020/21.
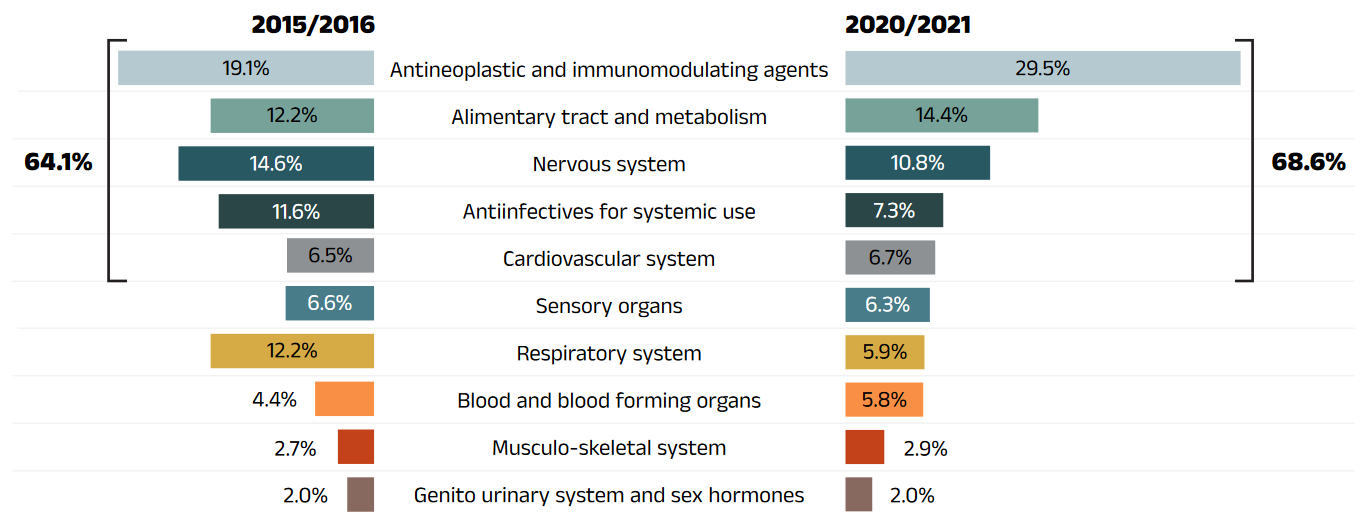
Figure description
This butterfly-shaped figure is composed of two bar graphs depicting the share of total drug costs in the NPDUIS public drug plans for each of the top 10 therapeutic classes in level 1 of the Anatomical Therapeutic Chemical Classification System. The shares for 2015/16 are shown on the left and shares for 2020/21 on the right. The top five classes in 2019/20 accounted for 64.1% of costs in 2015/16 and 68.6% of costs in 2020/21.
| Top 10 therapeutic classes | 2015/16 | 2020/21 |
|---|---|---|
Antineoplastic and immunomodulating agents |
19.3% |
27.1% |
Alimentary tract and metabolism |
12.7% |
13.5% |
Nervous system |
16.3% |
11.0% |
Antiinfectives for systemic use |
5.1% |
8.8% |
Cardiovascular system |
13.5% |
7.4% |
Sensory organs |
6.9% |
6.8% |
Respiratory system |
7.1% |
6.3% |
Blood and blood forming organs |
4.4% |
5.4% |
Musculo-skeletal system |
3.4% |
2.9% |
Genito urinary system and sex hormones |
2.4% |
2.1% |
Note: This analysis only includes data for beneficiaries that met their deductible and received public reimbursement.
* Anatomical Therapeutic Chemical (ATC) classification system maintained by the World Health Organization.
† British Columbia, Alberta, Saskatchewan, Manitoba, Ontario, New Brunswick, Nova Scotia, Prince Edward Island, Newfoundland and Labrador, Yukon, and the Non-Insured Health Benefits (NIHB) Program. Results for 2020/21 do not include the NIHB program.
Data source: National Prescription Drug Utilization Information System Database, Canadian Institute for Health Information.
3. The Drivers of Dispensing Costs, 2019/20 to 2020/21
The marginally negative rate of change in dispensing costs in 2020/21 was decidedly lower than the growth in drug costs, continuing the trend of slower growth observed over the last few years. Upward cost pressures from smaller prescription sizes and an increase in the volume of units dispensed over 2020/21 were more than offset by a drop in the number of active beneficiaries, a decreased overall average dispensing fee and a significant downward pull from the zero-dollar dispensing fee model introduced in Ontario’s long-term care (LTC) program.
Like drug costs, changes in dispensing costs are driven by a number of push and pull effects. The net effect of these opposing forces yields the overall rate of change.
Demographic effect: Changes in the number of active beneficiaries, as well as shifts in the age or gender distribution.
Drug volume effect: Changes in the number of units dispensed to patients.
Fee effect: Changes in the average dispensing fee per prescription.
Prescription size effect: Changes in the number of units dispensed per prescription.
In this section, a comprehensive cost driver analysis is used to determine how much public plan dispensing costs would have changed between 2018/19 and 2020/21 if only one factor (e.g., the average dispensing fee) was considered while all the others remained the same.Reference VI
In addition to the standard annual effects, Ontario’s OHIP+ program was previously treated as a separate factor in the cost driver analysis, encompassing all effects associated with the OHIP+ program (e.g., volume and demographic changes). As such, the OHIP+ effect reflected the overall impact from plan design changes. After 2019/20, OHIP+ program spending stabilized and had little impact; therefore, it is no longer reported as a separate factor of cost drivers in this edition of CompassRx . For historical data, please consult previous editions.
Long-term care (LTC) prescriptions in Ontario had been excluded from the dispensing costs analysis from 2017/18 to 2018/19, as their dispensing patterns may differ from those of the general beneficiary population. LTC prescriptions typically contribute less than 0.1% to growth and are therefore not presented in the cost drivers figure; however, as the effect is greater over 2019/20 and 2020/21, they have been included as a separate factor.
Dispensing costs in the NPDUIS public plans decreased slightly by 0.2% or $4.9 million in 2020/21, keeping at a total of $2.3 billion, the first negative growth of dispensing costs in the past 6 years.
Figure 3.1 provides insight into the pressures driving changes in dispensing costs from 2015/16 to 2020/21. The demographic effect, which has typically followed a predictable upward trend, instead contributed a downward pull of 1.3% on dispensing costs in 2020/21, resulting from a decrease in the number of active beneficiaries with the onset of the COVID-19 pandemic.
In contrast, the prescription size effect increased from 1.4% in 2019/20 to a more significant push of 3.4% in 2020/21, following the temporary changes to policies on dispensing frequency during the COVID-19 pandemic introduced in many provinces. The volume effect continued to exert a sizable upward push of 3.1%, reflecting an increased quantity of drugs dispensed to patients, while changes in the average dispensing fee per prescription decreased dispensing costs by 0.8% in 2020/21.
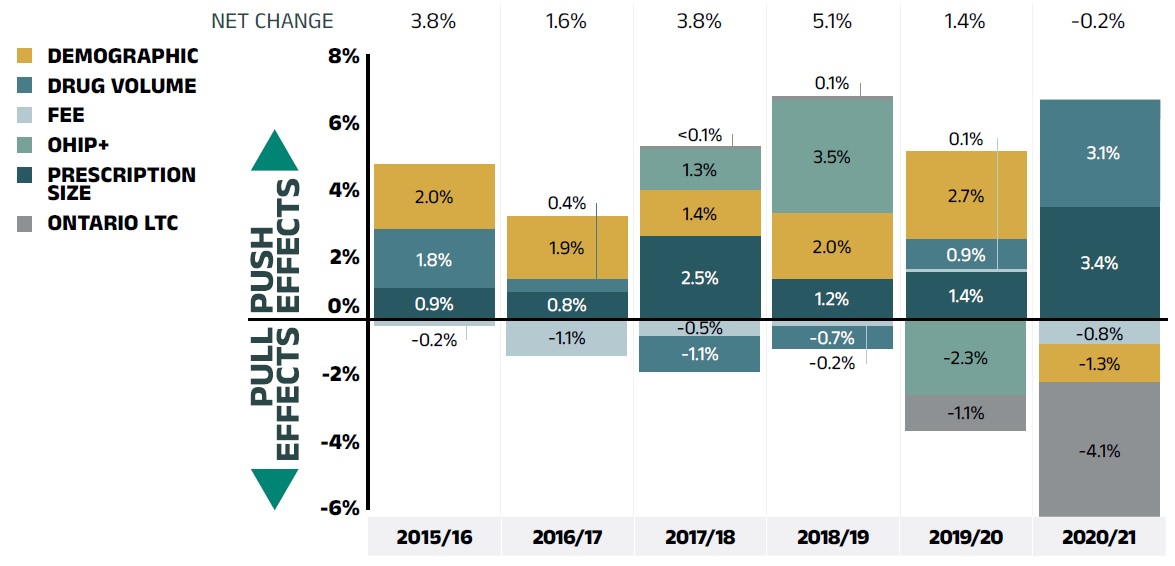
Figure description
This column graph describes the key factors or effects that impacted the rates of change in dispensing costs across all NPDUIS public drug plans for each year from 2015/16 to 2020/21. Each column is broken out to give the positive or negative contribution of each effect: demographic; volume; fee; and prescription size. Starting in 2017/18, the effects of the recent Ontario Health Insurance Plan Plus (OHIP+) program are shown separately. Ontario long-term care is presented separately started in 2019/20 and was calculated to be less than 0.1% in the two previous years. The OHIP+ effect is not captured for 2020/21. The net change is given for each year.
| 2015/16 | 2016/17 | 2017/18 | 2018/19 | 2019/20 | 2020/21 | |
|---|---|---|---|---|---|---|
Demographic |
2.0% |
1.9% |
1.4% |
2.0% |
2.7% |
-0.8% |
Volume |
1.8% |
0.4% |
-1.1% |
-0.7% |
0.9% |
2.6% |
Fee |
-0.2% |
-1.1% |
-0.5% |
-0.2% |
0.1% |
-0.8% |
Prescription size |
0.9% |
0.8% |
2.5% |
1.2% |
1.4% |
3.4% |
OHIP+ |
– |
– |
1.3% |
3.5% |
-2.3% |
- |
Ontario LTC |
– |
– |
0.0% |
0.1% |
-1.1% |
-4.1% |
Net change |
3.8% |
1.6% |
3.8% |
5.1% |
1.4% |
-0.2% |
Note: Values may not add to totals due to rounding and the cross effect.
* British Columbia, Alberta, Saskatchewan, Manitoba, Ontario, New Brunswick, Nova Scotia, Prince Edward Island, Newfoundland and Labrador, Yukon, and the Non-Insured Health Benefits (NIHB) Program. Results for 2020/21 do not include the NIHB program.
† Long-term care (LTC) prescriptions in Ontario had been excluded from the dispensing costs analysis for 2017/18 and 2018/19, as their dispensing patterns may differ from those of the general beneficiary population. In 2017/18 and 2018/19, the LTC sub-program contributed less than 0.1% to the growth in dispensing costs across all NPDUIS public plans.
Data source: National Prescription Drug Utilization Information System Database, Canadian Institute for Health Information.
The overall rate of change in dispensing costs varied widely among individual plans, from a high of 10.0% in Yukon, to a low of -4.6% in Ontario (Figure 3.2). A notable exception was the 39% increase in Nova Scotia. This was due to the addition of a Community Services Pharmacare Benefits program, resulting in a large, one-time increase in the beneficiary population and the volume of drugs used, which translated into a large push on dispensing costs from the demographic and volume effects. In Ontario, the reduction in dispensing costs resulted mainly from the zero-dollar dispensing fee model introduced in long-term care (LTC), without which dispensing costs would have increased moderately by 2.4%.
Long-term care (LTC) prescriptions were separated out from Ontario results in this cost driver analysis, as they may not have a typical dispensing frequency. For example, there may be a significantly higher number of prescriptions per patient than in the general beneficiary population due to the more specialized needs of these patients. LTC patients account for a small portion of all beneficiaries and typically contribute less than 0.1% to the growth in Ontario dispensing costs. However, a new LTC capitation funding model was introduced on January 1, 2020, eliminating dispensing fees for residents of LTC homes. The LTC program is reflected in the last quarter of fiscal year 2019/20 and the full course of fiscal year 2020/21. The program pulled Ontario dispensing costs down markedly by 7.0% (or $94 million), which is significant given Ontario’s relative size, contributing -4.1% to the growth of dispensing costs to the total NPDUIS public plans in 2020/21.
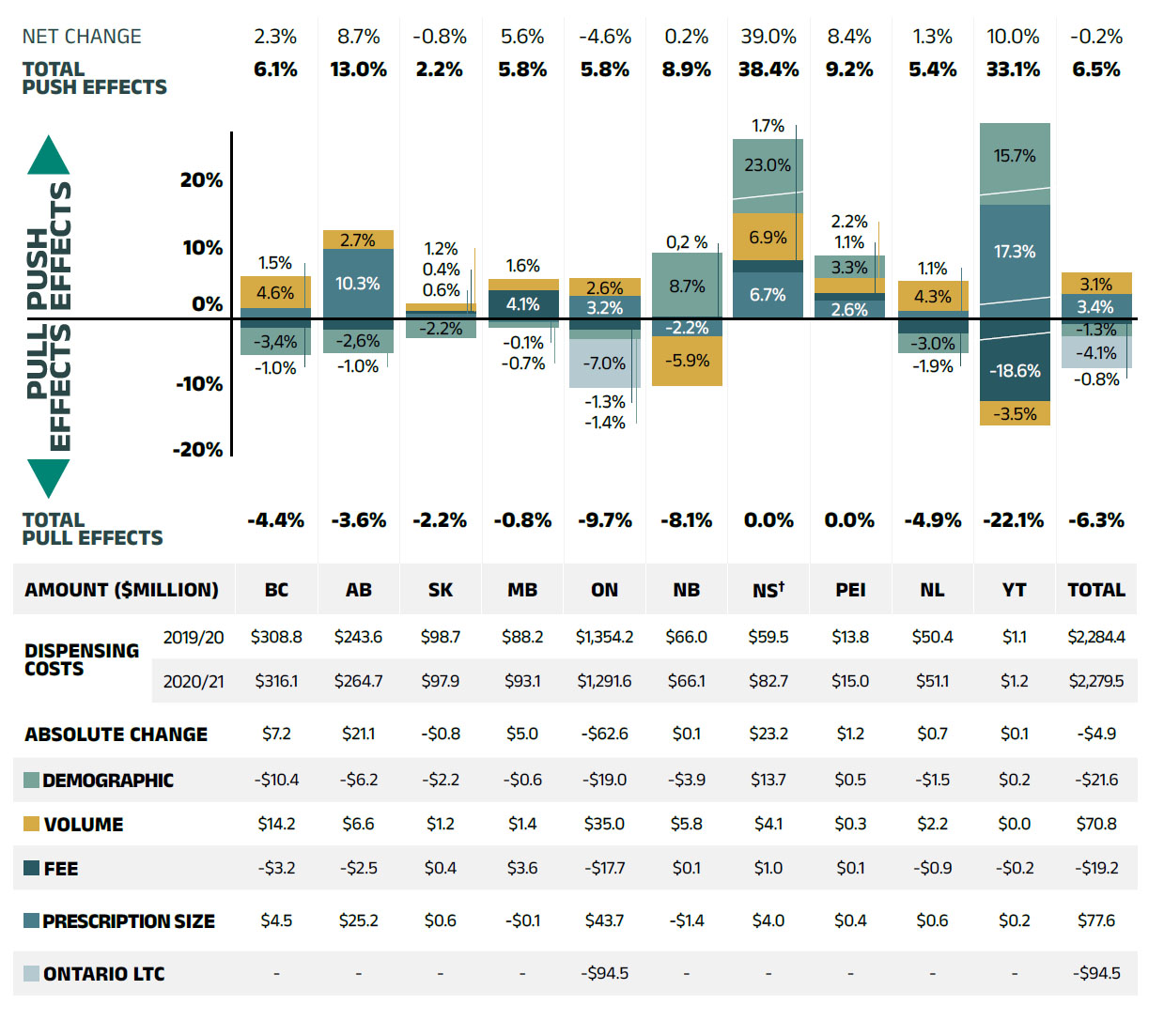
Figure description
This column graph and table describe the key factors or effects that impacted the rates of change in dispensing costs for each of the NPDUIS public drug plans from 2019/20 to 2020/21. Each column is broken out to give the positive or negative contribution of each effect: demographic; volume; fee; and prescription size. The effects of the recent Ontario Health Insurance Plan Plus (OHIP+) program as well as Ontario long-term care are shown separately. The OHIP+ effect is not captured for 2020/21. The total positive push effect, negative pull effect, and net change are given for each year.
| British Columbia | Alberta | Saskatchewan | Manitoba | Ontario | New Brunswick | Nova Scotia | Prince Edward Island | Newfoundland and Labrador | Yukon | Total | |
|---|---|---|---|---|---|---|---|---|---|---|---|
Demographic |
-3.4% |
-2.6% |
-2.2% |
-0.7% |
-1.4% |
10.1% |
23.0% |
3.3% |
-3.0% |
15.7% |
-0.8% |
Volume |
4.6% |
2.7% |
1.2% |
1.6% |
2.6% |
-7.1% |
6.9% |
2.2% |
4.3% |
-3.5% |
2.6% |
Fee |
-1.0% |
-1.0% |
0.4% |
4.1% |
-1.3% |
0.2% |
1.7% |
1.1% |
-1.9% |
-11.5% |
-0.8% |
Prescription size |
1.5% |
10.3% |
0.6% |
-0.1% |
3.2% |
-2.2% |
6.7% |
2.6% |
1.1% |
17.3% |
3.4% |
Ontario LTC |
– |
– |
– |
– |
-7.0% |
– |
– |
– |
– |
– |
-4.1% |
Total push effect |
6.1% |
13.0% |
2.2% |
5.8% |
5.8% |
8.9% |
38.4% |
9.2% |
5.4% |
33.1% |
6.5% |
Total pull effect |
-4.4% |
-3.6% |
-2.2% |
-0.8% |
-9.7% |
-8.1% |
0.0% |
0.0% |
-4.9% |
-22.1% |
-6.3% |
Net change |
2.3% |
8.7% |
-0.8% |
5.6% |
-4.6% |
0.2% |
39.0% |
8.4% |
1.3% |
10.0% |
-0.2% |
An accompanying table gives the corresponding changes in millions of dollars, as well as the total dispensing costs in 2019/20 and 2020/21 and the absolute change for each plan.
| British Columbia | Alberta | Saskatchewan | Manitoba | Ontario | New Brunswick | Nova Scotia | Prince Edward Island | Newfoundland and Labrador | Yukon | Non-Insured Health Benefits | Total | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
Dispensing cost 2019/20 |
$308.8 |
$243.6 |
$98.7 |
$88.2 |
$1,354.2 |
$66.0 |
$59.5 |
$13.8 |
$50.4 |
$1.1 |
$2,284.4 |
$308.8 |
Dispensing cost 2020/21 |
$316.1 |
$264.7 |
$97.9 |
$93.1 |
$1,291.6 |
$66.1 |
$82.7 |
$15.0 |
$51.1 |
$1.2 |
$2,279.5 |
$316.1 |
Absolute change |
$7.2 |
$21.1 |
-$0.8 |
$5.0 |
-$62.6 |
$0.1 |
$23.2 |
$1.2 |
$0.7 |
$0.1 |
-$4.9 |
$7.2 |
Demographic |
-$10.4 |
-$6.2 |
-$2.2 |
-$0.6 |
-$19.0 |
-$3.9 |
$13.7 |
$0.5 |
-$1.5 |
$0.2 |
-$21.6 |
-$10.4 |
Volume |
$14.2 |
$6.6 |
$1.2 |
$1.4 |
$35.0 |
$5.8 |
$4.1 |
$0.3 |
$2.2 |
$0.0 |
$70.8 |
$14.2 |
Fee |
-$3.2 |
-$2.5 |
$0.4 |
$3.6 |
-$17.7 |
$0.1 |
$1.0 |
$0.1 |
-$0.9 |
-$0.2 |
-$19.2 |
-$3.2 |
Prescription size |
$4.5 |
$25.2 |
$0.6 |
-$0.1 |
$43.7 |
-$1.4 |
$4.0 |
$0.4 |
$0.6 |
$0.2 |
$77.6 |
$4.5 |
Ontario long-term care |
– |
– |
– |
– |
-$94.5 |
– |
– |
– |
– |
– |
– |
-$94.5 |
Note: Values may not add to totals due to rounding and the cross effect.
† In Nova Scotia, Community Services Pharmacare Benefits (Plan F) data was not previously submitted to the CIHI NPDUIS database but has been submitted since 2020/21. This addition resulted in a large, one-time increase in the beneficiary population and their drug use. As such the overall impact was captured in the demographic and volume effects in 2020/21.
Data source: National Prescription Drug Utilization Information System Database, Canadian Institute for Health Information.
The contribution of the fee effect, which reflects changes in the average dispensing fee per prescription, is directly related to the reimbursement policies of each public drug plan.
In 2020/21, the rates of change in the average dispensing fee per prescription varied across NPDUIS drug plans. Most plans showed moderate changes ranging from -1.9% to 4.1%, except for Yukon. Over the past five years, Nova Scotia and Prince Edward Island have had a relatively high growth in fees, with compound annual growth rates of 1.2% and 1.1%, respectively.
Table 3.1 reports the average dispensing fee per prescription from 2015/16 to 2020/21, along with the rate of growth between 2019/20 and 2020/21 and the compound annual growth rate for the entire period. The results are an average across all prescriptions and include a range of dispensing fees. An overview of the dispensing fee policies of the NPDUIS public drug plans is available on the PMPRB website.
Table 3.1 Average dispensing fee per prescription, NPDUIS public drug plans, 2015/16 to 2020/21
| Jurisdiction | 2015/16 | 2016/17 | 2017/18 | 2018/19 | 2019/20 | 2020/21 | Growth rate, 2019/20 to 2020/21 | CAGR*, 2015/16 to 2020/21 |
|---|---|---|---|---|---|---|---|---|
British Columbia |
$7.30 |
$7.26 |
$7.18 |
$7.13 |
$7.10 |
$7.03 |
-1.0% |
-0.8% |
Alberta |
$14.29 |
$14.33 |
$14.45 |
$14.18 |
$14.11 |
$13.96 |
-1.0% |
-0.5% |
Saskatchewan |
$10.91 |
$10.97 |
$10.92 |
$10.92 |
$11.04 |
$11.09 |
0.4% |
0.3% |
Manitoba |
$9.35 |
$9.48 |
$8.82 |
$8.19 |
$8.24 |
$8.58 |
4.1% |
-1.7% |
Ontario† |
$7.72 |
$7.59 |
$7.55 |
$7.58 |
$7.58 |
$7.48 |
-1.3% |
-0.6% |
New Brunswick |
$10.54 |
$10.54 |
$10.48 |
$10.43 |
$10.48 |
$10.50 |
0.2% |
-0.1% |
Nova Scotia |
$11.19 |
$11.25 |
$11.32 |
$11.48 |
$11.67 |
$11.87 |
1.7% |
1.2% |
Prince Edward Island |
$10.93 |
$11.03 |
$11.23 |
$11.38 |
$11.42 |
$11.54 |
1.1% |
1.1% |
Newfoundland and Labrador |
$12.34 |
$12.39 |
$12.38 |
$12.41 |
$12.37 |
$12.14 |
-1.9% |
-0.3% |
Yukon |
$5.76 |
$5.80 |
$5.81 |
$5.76 |
$7.16 |
$5.83 |
-18.6% |
0.2% |
NIHB |
$8.76 |
$8.92 |
$8.97 |
$9.02 |
$9.17 |
- |
- |
- |
Note: This analysis only includes data for beneficiaries that met their deductible and received public reimbursement.
* Compound annual growth rate.
† Ontario long-term care (LTC) sub-plan prescriptions were excluded from all years of this analysis as their dispensing patterns may differ from those of the general beneficiary population.
The addition of Ontario’s OHIP+ program, implemented in the last quarter of 2017/18, was also excluded from this analysis to allow for comparison with historical results.
Data source: National Prescription Drug Utilization Information System Database, Canadian Institute for Health Information.
Various plans have specific policies in place related to dispensing frequency policy and compensation. The average dispensing fee per prescription is also related to prescription size: plans with lower average dispensing fees generally reimburse prescriptions with shorter days’ supply and vice versa. Manitoba, British Columbia, and Ontario, which had some of the lowest dispensing fees in 2020/21, generally reimbursed prescriptions with relatively small average sizes. Decreases in the average days’ supply per prescription can exert an upward pressure on dispensing costs, as a greater number of prescriptions are required to dispense the same volume of drugs.
The results for the average days’ supply per prescription suggest that prescription size was either stable or declined in public drug plans from 2019/20 to 2020/21. Nova Scotia and Alberta had the largest proportional decreases in average prescription size, at -10.3% and -14.2%, respectively.
Figure 3.3 depicts the trend in average days’ supply per prescription from 2015/16 to 2020/21. The results represent the average across all prescriptions for oral solid formulations and encompass brand-name and generic medicines for both acute and maintenance therapies.
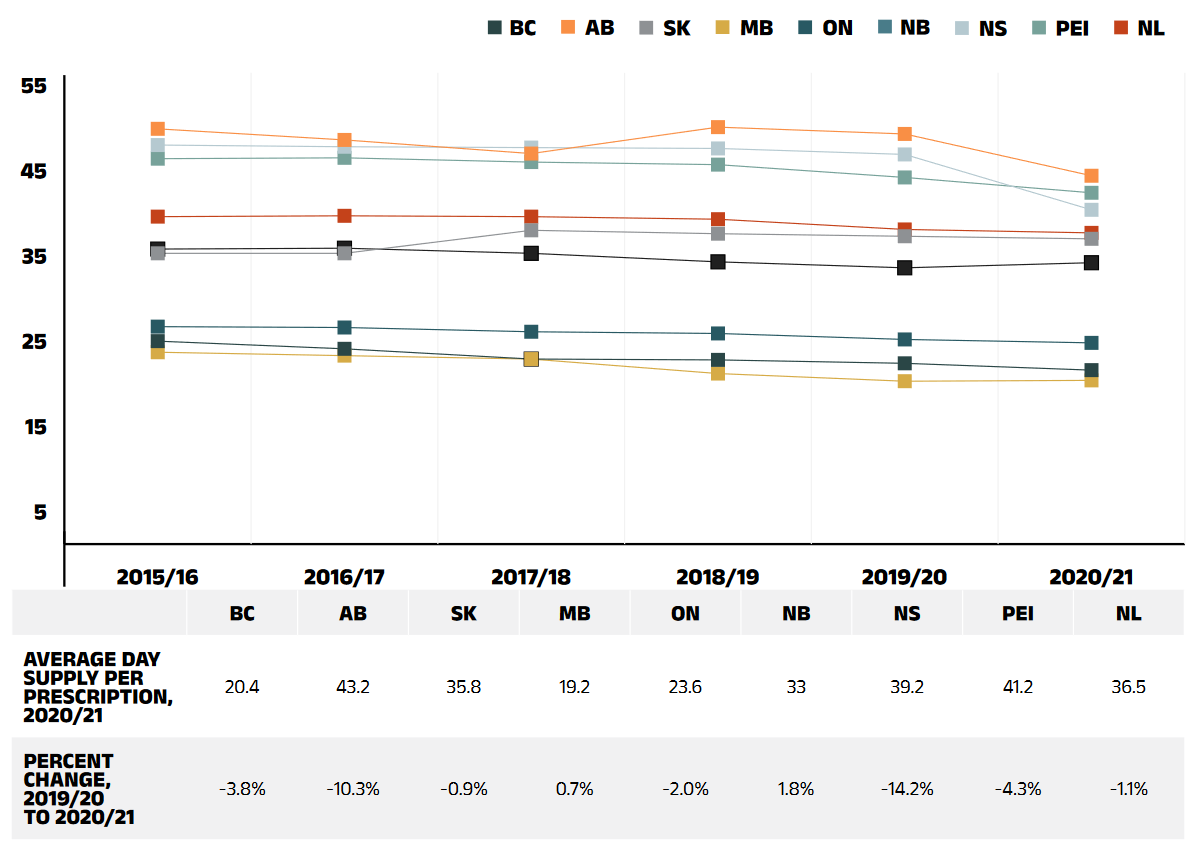
Figure description
This line graph shows the trend in average days’ supply per prescription 2015/16 to 2020/21to 2020/21 for each NPDUIS public drug plan. A table below the graph shows the average days’ supply per prescription for 2020/21 and the percent change from 2019/20 to 2020/21.
| 2015/16 | 2016/17 | 2017/18 | 2018/19 | 2019/20 | 2020/21 | Percent change, 2019/20 to 2020/21 | |
|---|---|---|---|---|---|---|---|
British Columbia |
23.8 |
22.9 |
21.7 |
21.6 |
21.2 |
20.4 |
-3.8% |
Alberta |
48.7 |
47.4 |
45.8 |
48.9 |
48.1 |
43.2 |
-10.3% |
Saskatchewan |
34.1 |
34.1 |
36.8 |
36.4 |
36.1 |
35.8 |
-0.9% |
Manitoba |
22.5 |
22.1 |
21.7 |
20.0 |
19.1 |
19.2 |
0.7% |
Ontario |
25.5 |
25.4 |
24.9 |
24.7 |
24.0 |
23.6 |
-2.0% |
New Brunswick |
34.6 |
34.7 |
34.1 |
33.1 |
32.4 |
33.0 |
1.8% |
Nova Scotia |
46.8 |
46.6 |
46.5 |
46.4 |
45.7 |
39.2 |
-14.2% |
Prince Edward Island |
45.2 |
45.3 |
44.8 |
44.5 |
43.0 |
41.2 |
-4.3% |
Newfoundland and Labrador |
38.4 |
38.5 |
38.4 |
38.1 |
36.9 |
36.5 |
-1.1% |
Note: This analysis only includes data for beneficiaries that met their deductible and received public reimbursement.
The analysis was limited to data for oral solid formulations. Yukon is not reported due to data limitations.
Data source: National Prescription Drug Utilization Information System Database, Canadian Institute for Health Information.
Although the average days’ supply and dispensing fee per prescription are useful measures for comparison, the roster of medicines covered by each plan also factors into the average dispensing cost. Comparing the dispensing costs for the same suite of medicines can provide greater insight into the differences between plans.
Figure 3.4 compares the dispensing costs across jurisdictions for the generic medicines reduced to 10% (previously 18%) of their brand-name reference price through the 2018 pCPA–CGPA agreement. Dispensing costs for one million tablets of each medicine are given for two fiscal years: 2015/16 and 2020/21. These medicines collectively accounted for 19.7% and 21.9% of the total NPDUIS public drug plan dispensing costs in 2015/16 and 2020/21, respectively.
Dispensing costs for the select medicines was stable or increased between 2015/16 and 2020/21 in most provinces, although the size of the changes varied considerably. The highest rates of increase were observed in Manitoba and British Columbia, while only Saskatchewan experienced a modest decrease. In four NPDUIS public plans—British Columbia, Saskatchewan, Manitoba, and Newfoundland and Labrador—dispensing costs for one million tablets exceeded $200,000 in 2020/21.
While the same drugs were studied across all plans, the disease profile of the beneficiary populations and the type of therapy for which the drugs were prescribed (acute or maintenance) influenced the average days’ supply and, hence, the overall dispensing costs for each jurisdiction.
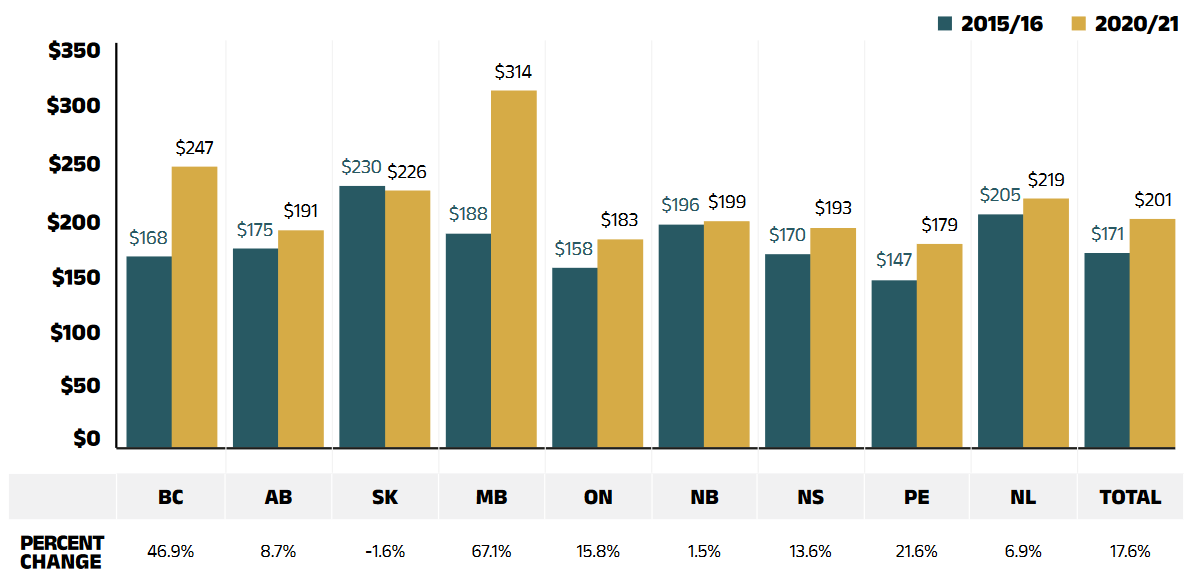
Figure description
This bar graph shows the dispensing cost in thousands of dollars for one million tablets of the generic medicines reduced to 10% of their brand reference price through recent pan-Canadian Pharmaceutical Alliance policy initiative. The dispensing costs are given for 2015/16 and 2020/21 for each NPDUIS public drug plan, as well as total results for all plans. A table below the graph gives the percent change over the period.
| British Columbia | Alberta | Saskatchewan | Manitoba | Ontario | New Brunswick | Nova Scotia | Prince Edward Island | Newfoundland and Labrador | Total† | |
|---|---|---|---|---|---|---|---|---|---|---|
2015/16 |
$168 |
$175 |
$230 |
$188 |
$158 |
$196 |
$170 |
$147 |
$205 |
$171 |
2020/21 |
$247 |
$191 |
$226 |
$314 |
$183 |
$199 |
$193 |
$179 |
$219 |
$201 |
Percent change |
46.9% |
8.7% |
-1.6% |
67.1% |
15.8% |
1.5% |
13.6% |
21.6% |
6.9% |
17.6% |
Note: Long-term care homes were excluded from this analysis, as they may not have a typical dispensing frequency due to the more specialized needs of their patients. The following sub-plans were not included in the analysis: BC: Permanent Residents of Licensed Residential Care Facilities; MB: Personal Home Care/Nursing Homes; NB: Individuals in Licensed Residential Facilities, Nursing Home Residents; ON: Long Term Care, Home Care and Homes for Special Care. Yukon is not reported due to data limitations.
* Subject to the pCPA–CGPA agreement that reduced the prices of these medicines to 10% of their brand-name reference price: atorvastatin, ramipril, venlafaxine, amlodipine, omeprazole, rabeprazole, rosuvastatin, pantoprazole, citalopram, simvastatin, clopidogrel, gabapentin, metformin, olanzapine, olanzapine ODT, donepezil, ezetimibe, quetiapine, ranitidine, and zopiclone.
† Total results for the drug plans captured in this figure.
Data source: National Prescription Drug Utilization Information System Database, Canadian Institute for Health Information.
Appendix A: Drug Reviews and Approvals
In Canada, Health Canada, the Patented Medicine Prices Review Board (PMPRB), and the Canadian Agency for Drugs and Technologies in Health (CADTH) are responsible for drug approvals, price reviews, and health technology assessments, respectively. This appendix provides an overview of recent trends in drug reviews and approvals.Reference VII
Health Canada
Health Canada grants the authority to market a drug in Canada by issuing a Notice of Compliance (NOC) once it has met the regulatory requirements for safety, efficacy, and quality. In 2020, Health Canada issued NOCs for 40 new active substances: 11 biologics and 29 small molecule pharmaceuticals.
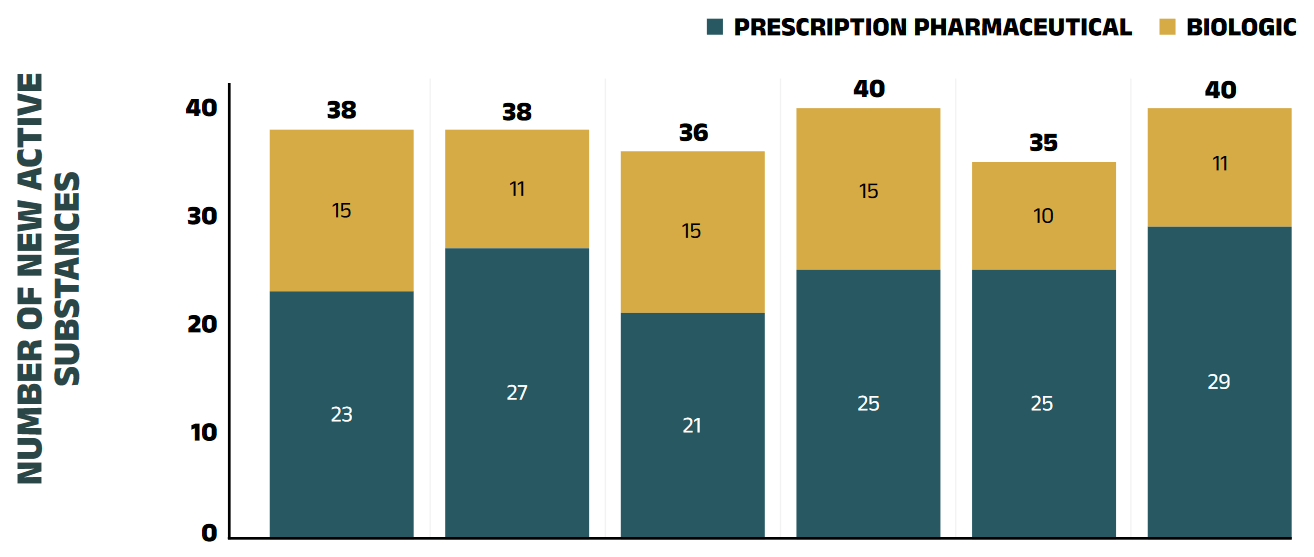
Figure description
This stacked column graph shows the number of new active substances approved by Health Canada from 2015 to 2020. The number of prescription pharmaceuticals and biologics are given for each year.
| Prescription pharmaceutical | Biologic | Total | |
|---|---|---|---|
2015 |
23 |
15 |
38 |
2016 |
27 |
11 |
38 |
2017 |
21 |
15 |
36 |
2018 |
25 |
15 |
40 |
2019 |
25 |
10 |
35 |
2020 |
29 |
11 |
40 |
Note: “Prescription pharmaceutical” and “biologic” are terms used to define product types when submitting a Notice of Compliance (NOC ) to Health Canada.
Data source: Notice of Compliance Database, Health Canada.
Patented Medicine Prices Review Board
The PMPRB reviews the factory-gate prices of patented medicines sold in Canada and ensures that they are not excessive. As part of the current price review process, the PMPRB’s Human Drug Advisory Panel (HDAP) evaluates each new medicine and assigns a recommended level of therapeutic improvement.
The PMPRB completed scientific reviews for 175 of the 227 medicines approved by Heath Canada between 2015 and 2020. Over this six-year period, only 7% were classified in the Substantial Improvement or Breakthrough categories. Three quarters of the medicines reviewed demonstrated Slight or No Improvement over existing therapies, while 18% were classified in the Moderate Improvement category (Figure A2).
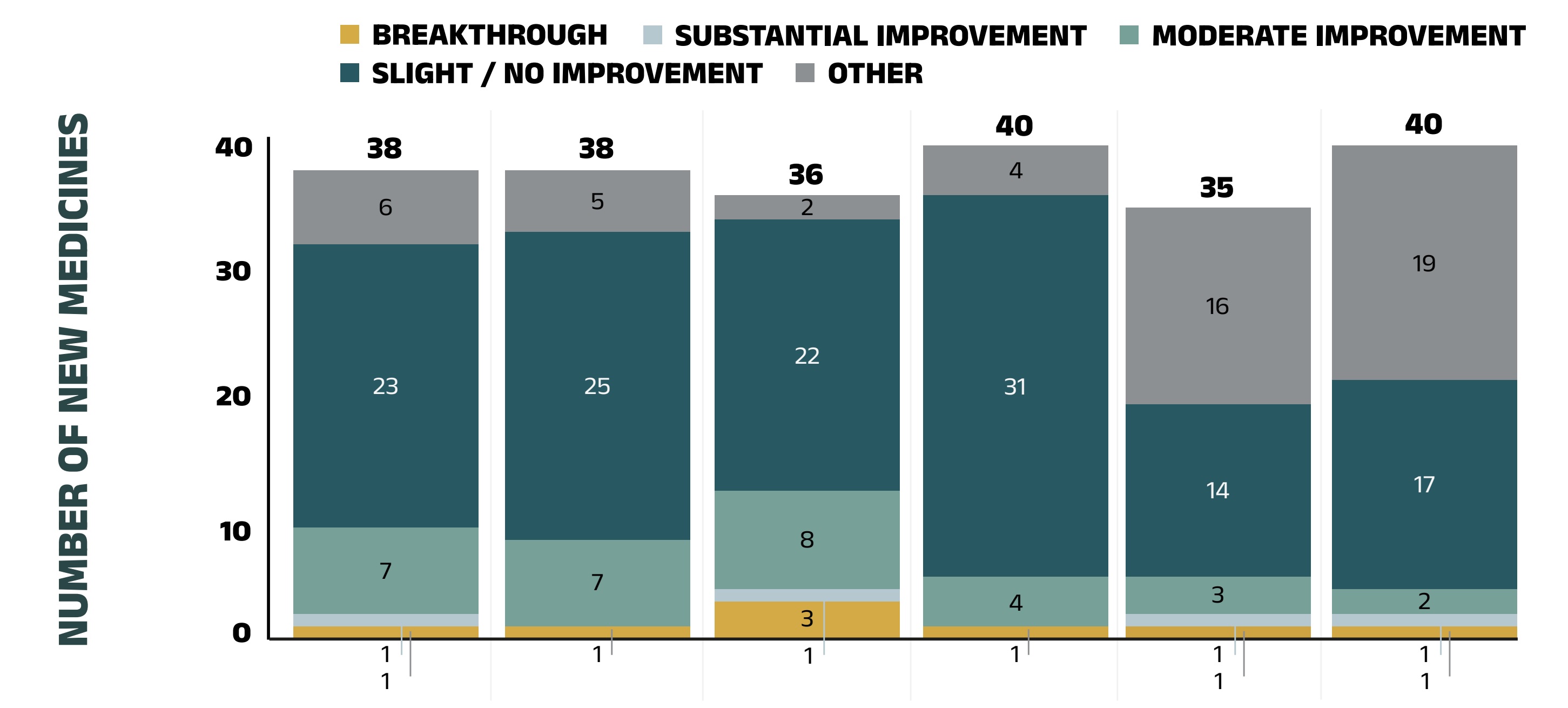
Figure description
This stacked column graph gives the distribution of new medicines reviewed by the Patented Medicine Prices Review Board from 2015 to 2020 by their assessed level of therapeutic improvement.
| Breakthrough | Substantial Improvement | Moderate Improvement | Slight or No Improvement | Other† | Total | |
|---|---|---|---|---|---|---|
2015 |
1 |
1 |
7 |
23 |
6 |
38 |
2016 |
1 |
0 |
7 |
25 |
5 |
38 |
2017 |
3 |
1 |
8 |
22 |
2 |
36 |
2018 |
1 |
0 |
4 |
31 |
4 |
40 |
2019 |
1 |
1 |
3 |
14 |
16 |
35 |
2020 |
1 |
1 |
2 |
17 |
19 |
40 |
* The year of reporting reflects the year in which the Notice of Compliance was issued (Figure A1) rather than the year that the PMPRB conducted its price review.
† New medicines not reported to the PMPRB as of the 2020 Annual Report.
Data source: Notice of Compliance Database, Health Canada; Patented Medicine Prices Review Board (PMPRB).
Canadian Agency for Drugs and Technologies in Health
CADTH’s Reimbursement Reviews consolidated its previous multiple-pathway product review processes (e.g., the pan-Canadian Oncology Drug Review and the Common Drug Review programs) into one pathway as of October 2020 CADTH provides reimbursement recommendations and advice to Canada’s publicly funded drug plans (except for Quebec) based on an evaluation of the clinical, economic, and patient evidence of drugs marketed in Canada. The jurisdictions take these recommendations under advisement when making formulary listing decisions and in price negotiations.
Figure A3 summarizes the CADTH recommendations for fiscal years 2015/16 to 2020/21.Reference VIII The total number of Reimbursement Review recommendations, including both former the Common Drug Review and the pan- Canadian Oncology Drug Review programs, has varied from year to year, with a high of 72 in 2016/17. In 2020/21, 58 recommendations were issued: 48 medicines were recommended as “reimburse with clinical criteria and/or conditions” and 2 as “reimburse”, while 8 received a “do not reimburse” recommendation.
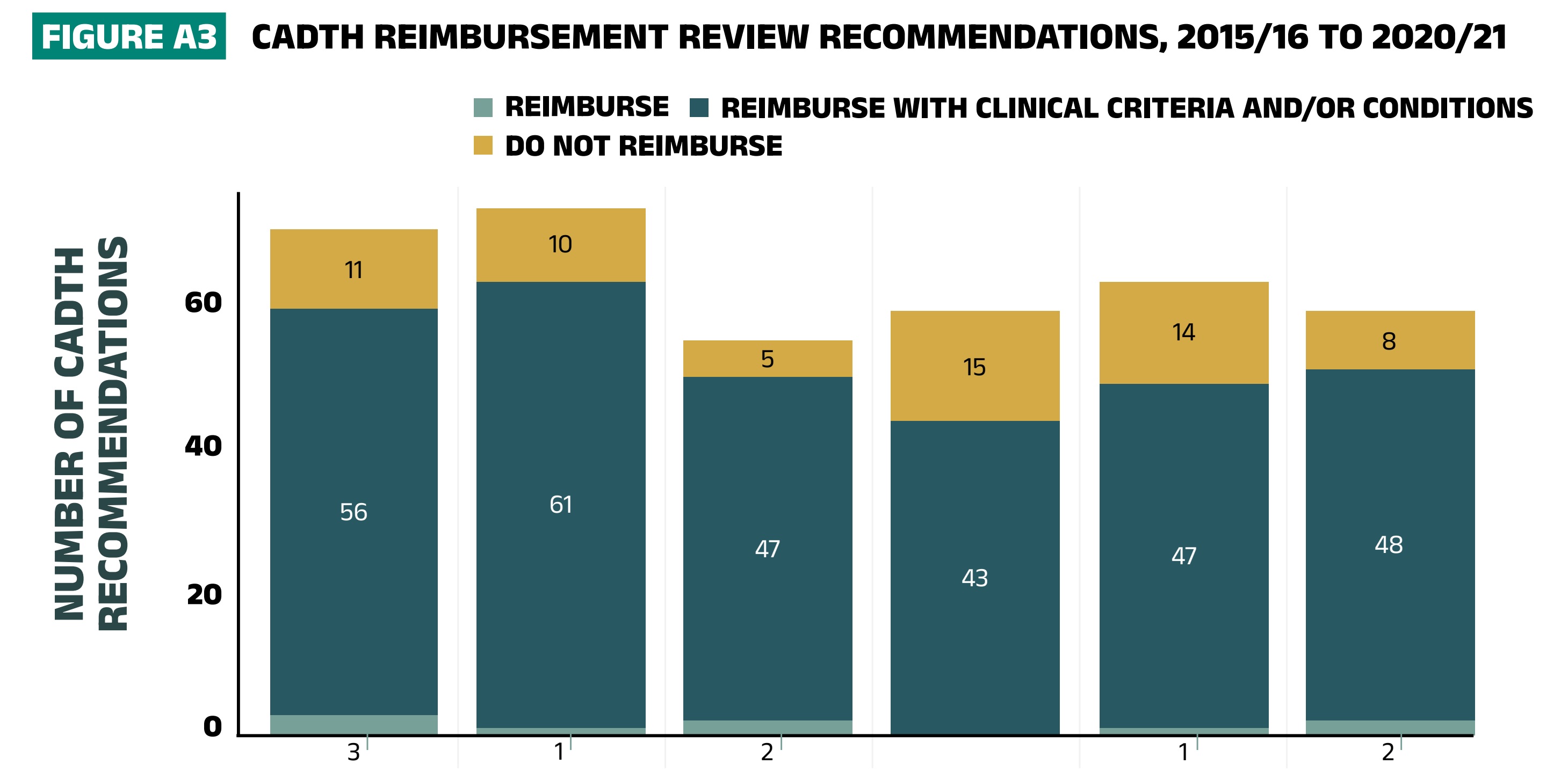
Figure description
The column graph shows the total number of Common Drug Review reimbursement recommendations from 2015/16 to 2020/21broken out by category of recommendation.
| Reimburse | Reimburse with clinical criteria and/or conditions | Do not reimburse | Total | |
|---|---|---|---|---|
2015/16 |
3 |
56 |
11 |
70 |
2016/17 |
1 |
61 |
10 |
72 |
2017/18 |
2 |
47 |
5 |
54 |
2018/19 |
– |
43 |
15 |
58 |
2019/20 |
1 |
47 |
14 |
62 |
2020/21 |
2 |
48 |
8 |
58 |
Note: Drugs may have multiple recommendations if they are reviewed for more than one indication. CADTH currently uses three possible recommendation categories to guide the reimbursement decisions of participating jurisdictions. For this analysis, “Reimburse with clinical criteria and/or conditions” includes recommendations completed prior to May 2016 for “List with clinical criteria and/or conditions,” “List in a similar manner to other drugs in class,” and “Do not list at submitted price”. “Reimburse” is equivalent to the previous “List” category, and likewise, “Do not reimburse” corresponds to “Do not list”.
Data source: CADTH Common Drug Review Reports.
Appendix B: Distribution of Patients on Biosimilar Initiative Medicines by Jurisdiction, 2020/21
Recently, numerous Canadian public payers have announced or undertaken initiatives to increase biosimilar uptake (see Appendix C). In 2019, British Columbia became the first Canadian province to initiate a switch to biosimilar medicines for patients covered under the PharmaCare program. By the end of fiscal year 2020/21, British Columbia had launched three phases of its non-medical switching policy. Since January 2021, Alberta has also implemented a switching policy. These initiatives require originator biologic patients on Remicade (infliximab), Enbrel (etanercept), Lantus (insulin glargine, 100 IU/ml) and Rituxan (rituximab) for select indications to switch to a biosimilar.
To monitor the uptake of biosimilars and explore the impact of switching policies in the public drug plans, Figures B1 and B2 present the distribution of public plan patients on anti-TNF-α drugs, insulin glargine and rituximab by NPDUIS jurisdiction. Future editions of this report will continue to monitor the impact of these initiatives as they take effect.
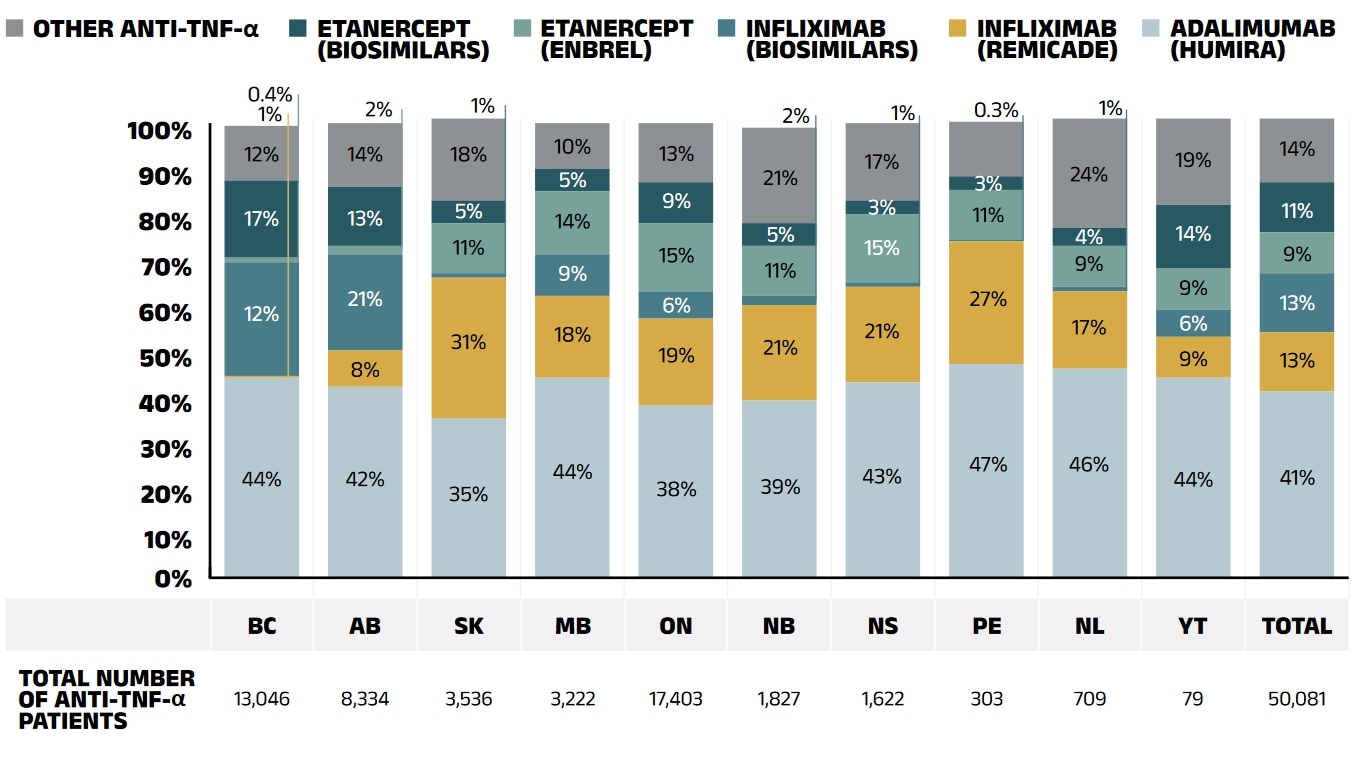
Figure description
A stacked bar graph breaks down the distribution of patients on an anti-tumor necrosis factor (TNF)-alpha drug for each of the NPDUIS public plans in 2020/21. The distribution is also given for the total across all plans. A table below the graph shows the total number of patients for this class of medicines.
| British Columbia | Alberta | Saskatchewan | Manitoba | Ontario | New Brunswick | Nova Scotia | Prince Edward Island | Newfoundland and Labrador | Yukon | Total | |
|---|---|---|---|---|---|---|---|---|---|---|---|
Humira |
44% |
42% |
35% |
44% |
38% |
39% |
43% |
47% |
46% |
44% |
41% |
Remicade (infliximab) |
0.4% |
8% |
31% |
18% |
19% |
21% |
21% |
27% |
17% |
9% |
13% |
Infliximab (biosimilars) |
25% |
21% |
1% |
9% |
6% |
2% |
1% |
0.3% |
1% |
6% |
13% |
Enbrel (etanercept) |
1% |
2% |
11% |
14% |
15% |
11% |
15% |
11% |
9% |
9% |
9% |
Etanercept (biosimilars) |
17% |
13% |
5% |
5% |
9% |
5% |
3% |
3% |
4% |
14% |
11% |
Other anti-TNF-α drugs |
12% |
14% |
18% |
10% |
13% |
21% |
17% |
12% |
24% |
19% |
14% |
Total number of patients |
13,046 |
8,334 |
3,536 |
3,222 |
17,403 |
1,827 |
1,622 |
303 |
709 |
79 |
50,081 |
Note: Other anti-TNF-α drugs included golimumab (Simponi) and certolizumab pegol (Cimzia).
Results do not distinguish between indications.
Totals may not add to 100% due to rounding.
Data source: National Prescription Drug Utilization Information System Database, Canadian Institute for Health Information.
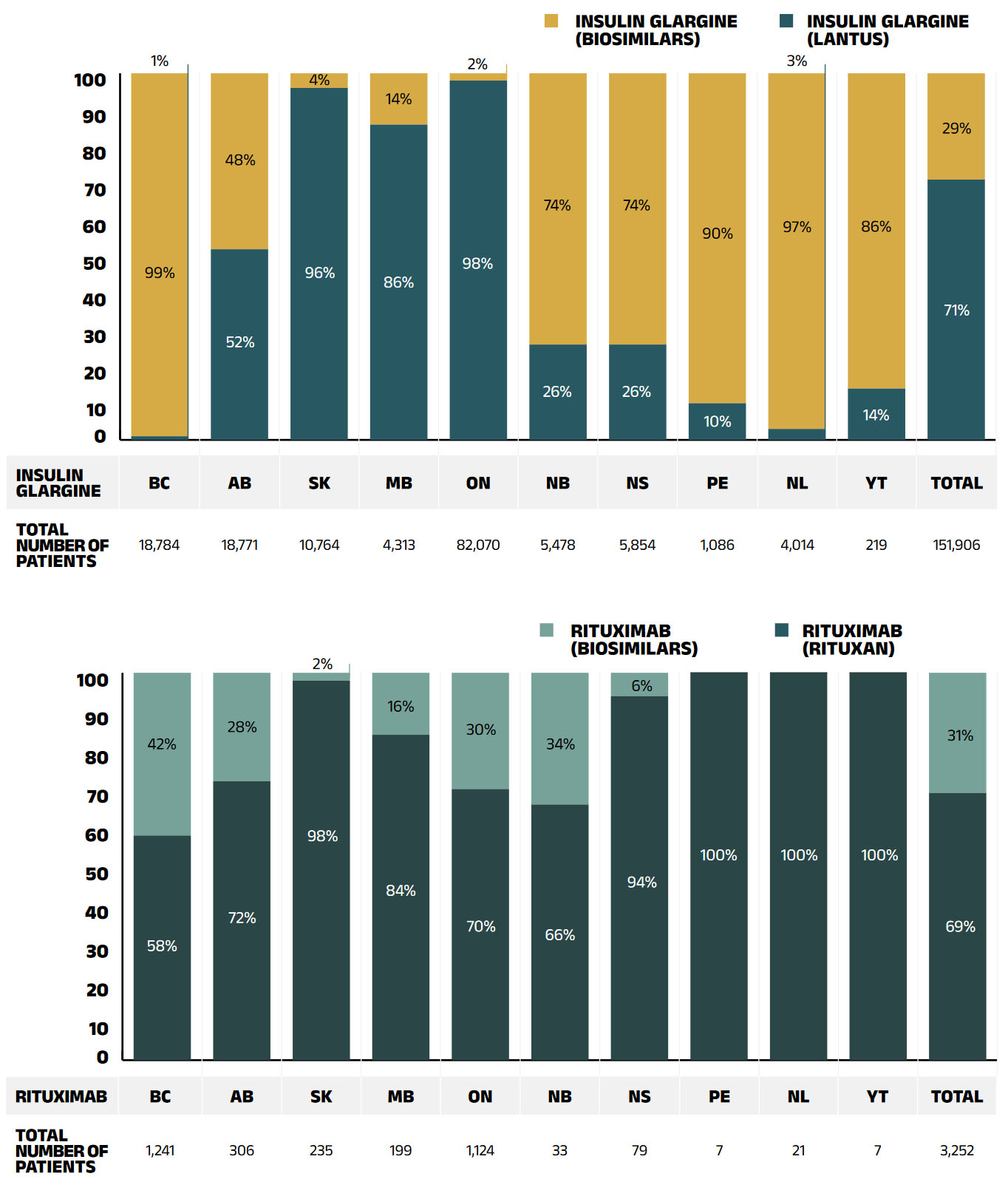
Figure description
A stacked bar graph breaks down the distribution of patients on insulin glargine by originator biologic (Lantus) and biosimilars for each of the NPDUIS public plans in 2020/21. The distribution is also given for the total across all plans. A table below the graph shows the total number of public plan patients using insulin glargine.
| British Columbia | Alberta | Saskatchewan | Manitoba | Ontario | New Brunswick | Nova Scotia | Prince Edward Island | Newfoundland and Labrador | Yukon | Total | |
|---|---|---|---|---|---|---|---|---|---|---|---|
Lantus |
1% |
52% |
96% |
86% |
98% |
33% |
32% |
13% |
5% |
17% |
82% |
Insulin glargine biosimilars |
99% |
48% |
4% |
14% |
2% |
74% |
74% |
90% |
97% |
86% |
29% |
Total number of patients |
18,784 |
18,771 |
10,764 |
4,313 |
82,070 |
5,478 |
5,854 |
1,086 |
4,014 |
219 |
151,906 |
Note: Totals may not add to 100% due to rounding.
* For comparison purposes, this analysis only considers patients using the 100 IU/ml strength of insulin glargine; those using 300 IU/ml or a multi-strength 100 IU/ml + 300 IU/ml were excluded.
† Results do not distinguish between indications.
Data source: National Prescription Drug Utilization Information System Database, Canadian Institute for Health Information.
Appendix C: Biosimilar Switching initiatives By canadian public payers
Given the high cost of biologics in Canada, biosimilars offer the potential for important savings. Recently, Canadian public payers have announced or undertaken a number of initiatives to increase biosimilar uptake, which are outlined in the table below.
| Initiative | |
|---|---|
British Columbia |
In 2019, British Columbia became the first Canadian province to initiate a switch to biosimilar medicines for patients covered under the PharmaCare program. Under the Phase 1 & 2 policy initiatives, patients using Enbrel, Remicade, and Lantus for specific indications are required to switch to the biosimilar. The switching policy expanded to Phase 3 & 4 in 2020 and 2021 to include Rituxan and Humira. |
Alberta |
Effective Jan. 2021, Alberta announced that all patients taking Enbrel, Remicade, Lantus, Neupogen, Neulasta, Rituxan, and Copaxone for indications ranging from rheumatoid arthritis to diabetes and multiple sclerosis are required to switch to the biosimilar. This policy has since been expanded to include Humira, Lovenox, and Hamlog |
New Brunswick |
Effective Apr. 2021, New Brunswick only reimburses biosimilar versions of approved indications of Humira, Enbrel, Remicade, Lantus, Humalog, Rituxan, Copaxone, and Lovenox. |
Quebec |
Effective Apr. 2021, the Quebec government announced a non-medical switching policy to require patients covered by the Quebec public drug plan who are treated with biologics drugs to switch to biosimilar versions where available and on an ongoing basis. |
|
MB, ON, NS, PEI, NL, YT, NIHB |
Planning to implement biosimilar switching strategies. |
Appendix D: Top 50 Patented Medicines by Drug Cost, NPDUIS Public Drug Plans, 2020/21 ($million)
| Rank | Medicinal ingredient (trade name) | Manufacturer | Total | BC | AB | SK | MB | ON | NB | NS | PE | NL | YT |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
1 |
Adalimumab (Humira) |
AbbVie Corporation |
$388.02 |
$115.00 |
$57.32 |
$30.02 |
$33.46 |
$120.00 |
$9.38 |
$13.49 |
$2.52 |
$5.97 |
$0.86 |
2 |
Aflibercept (Eylea) |
Bayer Inc. |
$344.15 |
- |
$8.23 |
$5.53 |
- |
$319.34 |
$8.63 |
- |
$1.44 |
$0.43 |
$0.55 |
3 |
Lenalidomide (Revlimid) |
Celgene Inc. |
$233.94 |
- |
- |
- |
$13.89 |
$193.97 |
$8.11 |
$10.56 |
$1.21 |
$5.97 |
$0.22 |
4 |
Apixaban (Eliquis) |
Bristol-Myers Squibb Canada |
$212.05 |
$22.04 |
$24.73 |
$8.61 |
$4.39 |
$146.88 |
$2.53 |
$2.10 |
$0.34 |
$0.29 |
$0.15 |
5 |
Sofosbuvir/velpatasvir (Epclusa) |
Gilead Sciences Canada Inc. |
$155.86 |
$50.69 |
$12.94 |
$6.15 |
$1.80 |
$76.42 |
$2.50 |
$1.18 |
- |
$3.87 |
$0.31 |
6 |
Ibrutinib (Imbruvica) |
Janssen Inc. |
$137.67 |
- |
- |
- |
$6.33 |
$118.01 |
$3.28 |
$5.68 |
$0.30 |
$3.82 |
$0.25 |
7 |
Rivaroxaban (Xarelto) |
Bayer Inc. |
$137.57 |
$13.77 |
$17.27 |
$7.19 |
$3.80 |
$88.23 |
$3.26 |
$2.77 |
$0.44 |
$0.84 |
$0.01 |
8 |
Empagliflozin (Jardiance) |
Boehringer Ingelheim |
$134.32 |
$10.31 |
$12.91 |
$3.58 |
$1.85 |
$102.33 |
$1.58 |
$1.39 |
$0.21 |
$0.12 |
$0.03 |
9 |
Semaglutide (Ozempic) |
Novo Nordisk Canada Inc. |
$132.92 |
$0.62 |
$16.18 |
$0.74 |
$0.16 |
$113.17 |
$0.66 |
$0.50 |
$0.74 |
$0.10 |
$0.05 |
10 |
Sitagliptin/metformin hydrochloride (Janumet) |
Merck Canada Inc. |
$113.46 |
<$0.01 |
$7.64 |
$1.11 |
$0.13 |
$103.21 |
$1.10 |
$0.25 |
$0.01 |
$0.01 |
- |
11 |
Sitagliptin (Januvia) |
Merck Canada Inc. |
$109.80 |
$0.01 |
$9.34 |
$2.59 |
$1.58 |
$92.47 |
$2.84 |
$0.84 |
$0.04 |
$0.08 |
$0.01 |
12 |
Glecaprevir/pibrentasvir (Maviret) |
AbbVie Corporation |
$105.95 |
$28.13 |
$5.42 |
$6.76 |
$4.20 |
$56.41 |
$1.03 |
$2.62 |
- |
$1.28 |
$0.10 |
13 |
Denosumab (Prolia) |
Amgen Canada Inc. |
$96.33 |
$1.49 |
$3.34 |
$1.51 |
$0.36 |
$89.10 |
$0.18 |
$0.26 |
$0.04 |
$0.03 |
$0.02 |
14 |
Vedolizumab (Entyvio) |
Takeda Canada Inc. |
$90.11 |
$36.66 |
$12.40 |
$13.83 |
$7.23 |
$14.19 |
$2.44 |
$2.40 |
$0.23 |
$0.71 |
$0.03 |
15 |
Paliperidone (Invega Sustenna) |
Janssen Inc. |
$88.92 |
$19.36 |
$1.33 |
$4.65 |
$2.53 |
$54.44 |
$3.51 |
$2.28 |
$0.19 |
$0.61 |
$0.04 |
16 |
Formoterol fumarate dihydrate/dudesonide (Symbicort) |
AstraZeneca Canada Inc. |
$86.32 |
$8.13 |
$11.78 |
$2.93 |
$2.37 |
$56.25 |
$1.33 |
$2.60 |
$0.19 |
$0.66 |
$0.09 |
17 |
Etanercept (Enbrel) |
Immunex Corporation |
$80.74 |
$2.02 |
$8.32 |
$6.96 |
$9.66 |
$45.21 |
$2.85 |
$4.01 |
$0.54 |
$1.02 |
$0.16 |
18 |
Insulin glargine (Lantus) |
Sanofi-Aventis Canada Inc. |
$79.54 |
$0.27 |
$8.62 |
$8.36 |
$2.93 |
$56.31 |
$1.23 |
$1.56 |
$0.08 |
$0.13 |
$0.04 |
19 |
Golimumab (Simponi) |
Janssen Inc. |
$76.23 |
$15.01 |
$13.61 |
$8.72 |
$5.08 |
$23.60 |
$4.45 |
$2.98 |
$0.47 |
$2.15 |
$0.16 |
20 |
Palbociclib (Ibrance) |
Pfizer Canada ULC |
$72.85 |
- |
- |
- |
$3.30 |
$61.72 |
$2.71 |
$3.06 |
$0.28 |
$1.78 |
- |
21 |
Ustekinumab (Stelara) |
Janssen Inc. |
$70.27 |
$8.68 |
$12.59 |
$15.21 |
$4.01 |
$22.76 |
$3.12 |
$2.64 |
$0.32 |
$0.93 |
$0.03 |
22 |
Tofacitinib (Xeljanz) |
Pfizer Canada ULC |
$69.09 |
$12.71 |
$6.05 |
$3.15 |
$3.32 |
$39.48 |
$0.93 |
$2.49 |
$0.20 |
$0.63 |
$0.12 |
23 |
Osimertinib (Tagrisso) |
AstraZeneca Canada Inc. |
$63.79 |
- |
- |
- |
$2.83 |
$57.34 |
$1.25 |
$1.33 |
$0.50 |
$0.51 |
$0.03 |
24 |
Linagliptin (Trajenta) |
Boehringer Ingelheim |
$59.45 |
$7.29 |
$3.86 |
$1.06 |
$0.67 |
$45.77 |
$0.72 |
$0.05 |
$0.02 |
$0.01 |
- |
25 |
Sacubitril/valsartan (Entresto) |
Novartis Pharmaceuticals Canada Inc. |
$56.15 |
$6.68 |
$4.76 |
$1.53 |
$0.68 |
$39.56 |
$1.35 |
$1.33 |
$0.06 |
$0.17 |
$0.03 |
26 |
Vilanterol/fluticasone furoate (Breo Ellipta) |
GlaxoSmithKline Inc. |
$52.18 |
$5.43 |
$5.80 |
$1.94 |
$1.84 |
$34.13 |
$1.18 |
$1.03 |
$0.25 |
$0.52 |
$0.05 |
27 |
Abiraterone acetate (Zytiga) |
Janssen Inc. |
$50.84 |
- |
- |
- |
$2.18 |
$44.21 |
$1.41 |
$2.41 |
$0.20 |
$0.36 |
$0.07 |
28 |
Aripiprazole (Abilify Maintena) |
Otsuka Pharmaceutical Co., Ltd |
$49.84 |
$14.55 |
$0.68 |
$2.62 |
$0.73 |
$28.25 |
$1.38 |
$1.28 |
$0.07 |
$0.27 |
$0.02 |
29 |
Dimethyl fumarate (Tecfidera) |
Biogen Canada Inc. |
$49.75 |
$10.13 |
$9.87 |
$6.33 |
$3.50 |
$14.25 |
$2.22 |
$1.81 |
$0.15 |
$1.35 |
$0.14 |
30 |
Canagliflozin (Invokana) |
Janssen Inc. |
$49.47 |
<$0.01 |
$4.85 |
$1.29 |
$0.68 |
$42.26 |
$0.34 |
$0.02 |
<$0.01 |
$0.02 |
<$0.01 |
31 |
Abacavir/lamivudine/dolutegravir (Triumeq) |
ViiV Healthcare ULC |
$49.24 |
- |
- |
$1.69 |
$3.11 |
$42.74 |
$1.28 |
- |
- |
$0.25 |
$0.16 |
32 |
Nintedanib (Ofev) |
Boehringer Ingelheim |
$49.17 |
$6.52 |
$6.88 |
$1.46 |
$2.69 |
$27.43 |
$1.09 |
$1.85 |
$0.72 |
$0.55 |
- |
33 |
Sitagliptin/metformin hydrochloride (Janumet XR) |
Merck Canada Inc. |
$48.34 |
- |
$2.69 |
$0.27 |
$0.12 |
$44.91 |
$0.31 |
$0.04 |
<$0.01 |
<$0.01 |
- |
34 |
Eculizumab (Soliris) |
Alexion Pharma GmbH |
$48.11 |
- |
$6.42 |
- |
$1.57 |
$39.15 |
$0.46 |
- |
$0.51 |
- |
- |
35 |
Omalizumab (Xolair) |
Novartis Pharmaceuticals Canada Inc. |
$46.20 |
$2.18 |
$8.52 |
$2.43 |
$1.89 |
$29.18 |
$0.49 |
$1.15 |
- |
$0.34 |
$0.02 |
36 |
Pirfenidone (Esbriet) |
Hoffmann-La Roche Ltd |
$45.01 |
$3.65 |
$7.47 |
$1.45 |
$2.67 |
$25.98 |
$1.09 |
$1.49 |
$0.28 |
$0.91 |
$0.01 |
37 |
Ocrelizumab (Ocrevus) |
Hoffmann-La Roche Ltd |
$43.13 |
$0.59 |
$13.37 |
$7.87 |
$6.14 |
$11.91 |
$1.26 |
$1.10 |
- |
$0.54 |
$0.36 |
38 |
Ruxolitinib (Jakavi) |
Novartis Pharmaceuticals Canada Inc. |
$42.61 |
- |
- |
- |
$2.53 |
$36.20 |
$1.84 |
$1.44 |
- |
$0.58 |
$0.02 |
39 |
Abatacept (Orencia) |
Bristol-Myers Squibb Canada |
$41.64 |
$13.04 |
$6.81 |
$2.72 |
$1.54 |
$14.53 |
$0.67 |
$1.58 |
$0.31 |
$0.40 |
$0.04 |
40 |
Tenofovir alafenamide/bictegravir/emtricitabine (Biktarvy) |
Gilead Sciences Canada Inc. |
$40.11 |
- |
- |
$3.90 |
$1.64 |
$32.81 |
$1.50 |
- |
- |
$0.24 |
$0.03 |
41 |
Secukinumab (Cosentyx) |
Novartis Pharmaceuticals Canada Inc. |
$38.96 |
$16.88 |
$5.40 |
$3.58 |
$5.44 |
$3.91 |
$0.81 |
$1.04 |
$0.04 |
$1.70 |
$0.15 |
42 |
Enzalutamide (Xtandi) |
Astellas Pharma Canada Inc. |
$38.34 |
- |
- |
- |
$3.43 |
$30.05 |
$1.44 |
$1.87 |
$0.39 |
$1.12 |
$0.05 |
43 |
Tocilizumab (Actemra) |
Hoffmann-La Roche Ltd |
$37.80 |
$7.49 |
$6.42 |
$2.89 |
$2.28 |
$16.99 |
$0.40 |
$0.84 |
$0.05 |
$0.36 |
$0.08 |
44 |
Octreotide (Sandostatin LAR) |
Novartis Pharmaceuticals Canada Inc. |
$37.32 |
$0.05 |
$6.48 |
$0.52 |
$2.98 |
$25.24 |
$0.84 |
$0.77 |
- |
$0.44 |
- |
45 |
Mirabegron (Myrbetriq) |
Astellas Pharma Canada Inc. |
$36.87 |
$0.01 |
$3.53 |
$0.83 |
$1.00 |
$29.97 |
$0.65 |
$0.68 |
$0.05 |
$0.13 |
$0.02 |
46 |
Lisdexamfetamine dimesylate (Vyvanse) |
Takeda Canada Inc. |
$36.18 |
$2.42 |
$2.33 |
$2.44 |
$1.97 |
$25.64 |
$0.51 |
$0.59 |
$0.08 |
$0.15 |
$0.04 |
47 |
Emtricitabine/elvitegravir/cobicistat (Genvoya) |
Gilead Sciences Canada Inc. |
$35.18 |
- |
- |
$2.63 |
$2.00 |
$29.19 |
$0.87 |
- |
- |
$0.34 |
$0.15 |
48 |
Tiotropium (Spiriva) |
Boehringer Ingelheim |
$35.07 |
$1.92 |
$5.05 |
$1.41 |
$0.68 |
$23.36 |
$1.01 |
$1.09 |
$0.12 |
$0.31 |
$0.11 |
49 |
Onabotulinumtoxina (Botox) |
Allergan Inc. |
$34.60 |
$5.12 |
$7.16 |
$1.13 |
$0.93 |
$18.83 |
$0.30 |
$1.08 |
- |
- |
$0.05 |
50 |
Tiotropium (Spiriva Respimat) |
Boehringer Ingelheim |
$33.78 |
$3.46 |
$4.65 |
$1.21 |
$0.70 |
$22.15 |
$0.50 |
$0.83 |
$0.10 |
$0.14 |
$0.04 |
Total |
$4,265.23 |
$452.29 |
$373.05 |
$190.78 |
$170.79 |
$2,829.44 |
$94.82 |
$92.36 |
$13.68 |
$43.14 |
$4.87 |
||
Share of all patented medicines |
75% |
75% |
76% |
79% |
73% |
75% |
77% |
75% |
78% |
75% |
73% |
||
Data source: National Prescription Drug Utilization Information System Database, Canadian Institute for Health Information.
Appendix E: Top 50 Multi-Source Generic Medicines by Drug Cost, NPDUIS Public Drug Plans, 2020/21 ($million)
| Rank | Medicinal ingredient | Total | BC | AB | SK | MB | ON | NB | NS | PE | NL | YT |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
1 |
Atorvastatin |
$61.99 |
$7.24 |
$7.47 |
$2.15 |
$1.41 |
$39.08 |
$1.34 |
$1.88 |
$0.40 |
$0.88 |
$0.13 |
2 |
Rosuvastatin |
$54.86 |
$4.37 |
$6.49 |
$2.14 |
$0.73 |
$36.10 |
$1.41 |
$2.05 |
$0.43 |
$1.11 |
$0.04 |
3 |
Pantoprazole |
$54.77 |
$3.71 |
$8.65 |
$2.34 |
$0.75 |
$34.41 |
$2.74 |
$1.12 |
$0.48 |
$0.52 |
$0.05 |
4 |
Amlodipine |
$43.92 |
$5.06 |
$5.30 |
$1.67 |
$0.99 |
$27.79 |
$0.91 |
$1.37 |
$0.34 |
$0.43 |
$0.07 |
5 |
Duloxetine |
$35.78 |
$0.77 |
$4.14 |
$1.72 |
$1.01 |
$27.43 |
$0.34 |
$0.28 |
$0.02 |
$0.01 |
$0.05 |
6 |
Pregabalin |
$34.77 |
$0.10 |
$1.81 |
$1.67 |
$0.57 |
$28.93 |
$0.75 |
$0.71 |
$0.04 |
$0.14 |
$0.04 |
7 |
Candesartan |
$26.52 |
$2.58 |
$2.86 |
$1.27 |
$0.30 |
$17.58 |
$0.46 |
$0.79 |
$0.14 |
$0.49 |
$0.05 |
8 |
Buprenorphine, combinations |
$24.14 |
$6.97 |
$0.81 |
$0.59 |
$0.66 |
$11.44 |
$0.72 |
$1.19 |
$0.34 |
$1.42 |
$0.01 |
9 |
Escitalopram |
$24.01 |
$4.53 |
$2.12 |
$0.52 |
$0.30 |
$15.66 |
$0.24 |
$0.39 |
$0.06 |
$0.16 |
$0.02 |
10 |
Perindopril |
$23.59 |
$0.48 |
$1.46 |
$0.72 |
$0.17 |
$19.39 |
$0.52 |
$0.51 |
$0.06 |
$0.26 |
$0.01 |
11 |
Sertraline |
$22.92 |
$3.77 |
$1.47 |
$1.28 |
$0.94 |
$12.45 |
$0.87 |
$1.21 |
$0.23 |
$0.68 |
$0.02 |
12 |
Gabapentin |
$22.44 |
$5.25 |
$2.88 |
$1.06 |
$1.21 |
$10.11 |
$0.91 |
$0.73 |
$0.16 |
$0.09 |
$0.03 |
13 |
Perindopril and diuretics |
$21.04 |
- |
$2.88 |
$1.57 |
$0.42 |
$13.64 |
$1.05 |
$0.91 |
$0.10 |
$0.47 |
$0.01 |
14 |
Aripiprazole |
$19.20 |
$2.93 |
$0.36 |
$0.30 |
$0.85 |
$14.19 |
$0.29 |
$0.22 |
$0.02 |
$0.03 |
$0.01 |
15 |
Ramipril |
$18.50 |
$4.26 |
$1.93 |
$0.80 |
$0.49 |
$9.52 |
$0.40 |
$0.46 |
$0.17 |
$0.39 |
$0.08 |
16 |
Nabilone |
$18.37 |
$2.48 |
$0.89 |
$0.02 |
$0.89 |
$12.29 |
$0.75 |
$0.82 |
<$0.01 |
$0.23 |
<$0.01 |
17 |
Tamsulosin |
$17.77 |
$1.93 |
$3.41 |
$0.91 |
$0.38 |
$9.61 |
$0.49 |
$0.49 |
$0.15 |
$0.37 |
$0.04 |
18 |
Quetiapine |
$17.57 |
$3.46 |
$0.75 |
$1.20 |
$0.65 |
$9.74 |
$0.67 |
$0.68 |
$0.05 |
$0.36 |
$0.01 |
19 |
Lansoprazole |
$17.08 |
$0.32 |
$1.09 |
$0.14 |
$0.10 |
$15.23 |
$0.13 |
$0.05 |
<$0.01 |
$0.01 |
$0.01 |
20 |
Salmeterol and fluticasone |
$17.06 |
$1.43 |
$0.75 |
$0.45 |
$0.55 |
$12.80 |
$0.38 |
$0.44 |
$0.05 |
$0.17 |
$0.03 |
21 |
Hydromorphone |
$16.57 |
$4.18 |
$1.13 |
$1.03 |
$0.52 |
$8.40 |
$0.41 |
$0.61 |
$0.13 |
$0.14 |
$0.02 |
22 |
Levodopa and decarboxylase inhibitor |
$16.47 |
$1.67 |
$1.98 |
$0.66 |
$0.39 |
$10.70 |
$0.28 |
$0.44 |
$0.09 |
$0.23 |
$0.02 |
23 |
Olanzapine |
$16.33 |
$2.72 |
$0.56 |
$0.64 |
$0.82 |
$9.71 |
$0.85 |
$0.69 |
$0.11 |
$0.24 |
$0.01 |
24 |
Metoprolol |
$16.15 |
$2.26 |
$2.39 |
$1.25 |
$0.81 |
$6.72 |
$0.59 |
$1.11 |
$0.20 |
$0.79 |
$0.03 |
25 |
Clozapine |
$15.71 |
$9.17 |
$0.53 |
$1.93 |
$2.73 |
- |
$0.70 |
- |
$0.04 |
$0.59 |
$0.02 |
26 |
Rabeprazole |
$15.34 |
$1.53 |
$0.43 |
$1.05 |
$0.44 |
$9.27 |
$0.19 |
$1.54 |
$0.06 |
$0.81 |
$0.01 |
27 |
Metformin |
$15.34 |
$2.18 |
$1.90 |
$0.96 |
$0.49 |
$8.20 |
$0.41 |
$0.65 |
$0.16 |
$0.34 |
$0.04 |
28 |
Clopidogrel |
$15.18 |
$1.55 |
$1.40 |
$0.59 |
$0.39 |
$9.76 |
$0.43 |
$0.58 |
$0.10 |
$0.37 |
$0.02 |
29 |
Diltiazem |
$15.17 |
$2.18 |
$1.39 |
$0.60 |
$0.42 |
$9.09 |
$0.65 |
$0.53 |
$0.13 |
$0.16 |
$0.02 |
30 |
Venlafaxine |
$14.97 |
$2.83 |
$1.33 |
$0.86 |
$0.63 |
$7.37 |
$0.63 |
$0.69 |
$0.12 |
$0.49 |
$0.02 |
31 |
Valproic acid |
$14.63 |
$2.96 |
$0.46 |
$0.74 |
$0.60 |
$8.40 |
$0.50 |
$0.44 |
$0.11 |
$0.41 |
$0.01 |
32 |
Oxycodone and paracetamol |
$14.20 |
$0.60 |
$0.66 |
- |
$0.48 |
$11.26 |
$0.47 |
$0.28 |
$0.09 |
$0.35 |
$0.01 |
33 |
Fluoxetine |
$13.67 |
$3.08 |
$1.01 |
$1.05 |
$0.71 |
$6.49 |
$0.37 |
$0.49 |
$0.10 |
$0.36 |
$0.02 |
34 |
Salbutamol |
$13.56 |
$2.13 |
$0.53 |
$0.60 |
$0.50 |
$7.79 |
$0.61 |
$0.78 |
$0.14 |
$0.45 |
$0.03 |
35 |
Mycophenolic acid |
$12.50 |
$0.56 |
- |
$1.02 |
$0.58 |
$9.95 |
$0.19 |
$0.13 |
<$0.01 |
$0.01 |
$0.07 |
36 |
Risperidone |
$12.30 |
$2.35 |
$0.40 |
$0.84 |
$0.73 |
$6.38 |
$0.63 |
$0.49 |
$0.11 |
$0.35 |
$0.01 |
37 |
Epinephrine |
$12.25 |
$1.16 |
$0.69 |
$0.88 |
$0.27 |
$8.80 |
$0.19 |
$0.19 |
$0.01 |
$0.05 |
<$0.01 |
38 |
Methotrexate |
$11.92 |
$2.12 |
$2.01 |
$0.62 |
$0.42 |
$5.66 |
$0.36 |
$0.43 |
$0.08 |
$0.19 |
$0.03 |
39 |
Irbesartan |
$11.74 |
$0.35 |
$2.22 |
$0.49 |
$0.43 |
$7.50 |
$0.16 |
$0.41 |
$0.09 |
$0.09 |
$0.01 |
40 |
Risedronic acid |
$11.59 |
$0.19 |
$1.51 |
$0.27 |
$0.08 |
$8.84 |
$0.21 |
$0.37 |
$0.04 |
$0.09 |
<$0.01 |
41 |
Omeprazole |
$11.36 |
$0.23 |
$0.99 |
$0.41 |
$1.16 |
$6.04 |
$0.69 |
$1.10 |
$0.17 |
$0.50 |
$0.07 |
42 |
Levetiracetam |
$11.06 |
$1.70 |
$1.10 |
$0.64 |
$0.51 |
$6.11 |
$0.26 |
$0.41 |
$0.08 |
$0.22 |
$0.02 |
43 |
Ondansetron |
$10.70 |
$1.31 |
$2.64 |
$0.09 |
$1.46 |
$4.71 |
$0.18 |
$0.27 |
$0.01 |
$0.02 |
<$0.01 |
44 |
Mirtazapine |
$10.64 |
$1.44 |
$0.58 |
$0.42 |
$0.67 |
$6.42 |
$0.27 |
$0.41 |
$0.05 |
$0.38 |
<$0.01 |
45 |
Gliclazide |
$10.55 |
$0.63 |
$1.07 |
$0.52 |
$0.56 |
$6.09 |
$0.33 |
$0.73 |
$0.16 |
$0.44 |
$0.02 |
46 |
Methadone |
$10.37 |
$0.16 |
$0.07 |
- |
$0.30 |
$9.07 |
$0.06 |
<$0.01 |
- |
$0.70 |
- |
47 |
Timolol, combinations |
$10.34 |
$1.75 |
$2.01 |
$0.66 |
$0.36 |
$4.41 |
$0.35 |
$0.44 |
$0.08 |
$0.24 |
$0.03 |
48 |
Ezetimibe |
$10.26 |
$0.05 |
$0.66 |
$0.34 |
$0.10 |
$8.40 |
$0.25 |
$0.28 |
$0.01 |
$0.16 |
<$0.01 |
49 |
Tenofovir disoproxil |
$10.11 |
$2.26 |
$1.02 |
$0.20 |
$0.24 |
$6.33 |
$0.02 |
$0.02 |
- |
- |
$0.01 |
50 |
Fentanyl |
$9.84 |
$1.57 |
$0.86 |
$0.96 |
$0.62 |
$5.28 |
$0.20 |
$0.26 |
$0.02 |
$0.05 |
$0.02 |
Total |
$967.11 |
$118.53 |
$91.07 |
$42.81 |
$31.78 |
$600.54 |
$26.84 |
$31.07 |
$5.72 |
$17.45 |
$1.26 |
|
Share of all multi-source generic medicines |
58% |
59% |
56% |
56% |
51% |
60% |
56% |
54% |
54% |
52% |
53% |
|
Data source: National Prescription Drug Utilization Information System Database, Canadian Institute for Health Information.
Appendix F: Top 50 Single-Source Non-Patented Medicines by Drug Cost, NPDUIS Public Drug Plans, 2020/21 ($thousand)
| Rank | Medicinal Ingredient (trade name) | Manufacturer | Total | BC | AB | SK | MB | ON | NB | NS | PE | NL | YT |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
1 |
Ranibizumab (Lucentis) |
Novartis Pharmaceuticals Canada Inc. |
$205,046 |
- |
$5,783 |
$1,179 |
- |
$185,357 |
$9,418 |
- |
$584 |
$2,726 |
- |
2 |
Insulin degludec (Tresiba) |
Novo Nordisk Canada Inc. |
$72,846 |
- |
$9,936 |
$3,595 |
$1,826 |
$46,455 |
$2,881 |
$4,577 |
$1,814 |
$1,754 |
$9 |
3 |
Insulin aspart (Novorapid) |
Novo Nordisk Canada Inc. |
$36,962 |
$2,958 |
$3,472 |
$834 |
$1,257 |
$22,857 |
$932 |
$1,974 |
$547 |
$2,095 |
$37 |
4 |
Teriflunomide (Aubagio) |
Sanofi Genzyme, a division of Sanofi-Aventis Canada Inc. |
$34,465 |
$7,336 |
$2,848 |
$2,861 |
$1,382 |
$15,000 |
$1,856 |
$2,118 |
$304 |
$694 |
$65 |
5 |
Mepolizumab (Nucala) |
GlaxoSmithKline Inc. |
$29,947 |
$4,875 |
$5,301 |
$1,269 |
$169 |
$16,292 |
$1,118 |
$797 |
- |
$126 |
- |
6 |
Goserelin (Zoladex LA) |
TerSera Therapeutics, LLC |
$25,558 |
- |
$3 |
$8 |
$23 |
$22,575 |
$712 |
$1,563 |
$245 |
$346 |
$84 |
7 |
Dalteparin sodium (Fragmin) |
Pfizer Canada ULC |
$24,106 |
$4,857 |
$911 |
$390 |
$1,588 |
$14,234 |
$504 |
$1,493 |
$18 |
$1 |
$110 |
8 |
Insulin detemir (Levemir Penfill) |
Novo Nordisk Canada Inc. |
$17,981 |
$2,364 |
$2,687 |
$625 |
$132 |
$11,221 |
$171 |
$633 |
$24 |
$105 |
$20 |
9 |
Darbepoetin alfa (Aranesp HSA-free) |
Amgen Canada Inc. |
$16,448 |
- |
$8,317 |
$614 |
$36 |
$5,126 |
$1,264 |
$29 |
- |
$1,047 |
$14 |
10 |
Insulin lispro/insulin lispro protamine suspension (Humalog Mix) |
Eli Lilly Canada Inc. |
$13,746 |
$829 |
$587 |
$2 |
$505 |
$11,576 |
$118 |
- |
$88 |
$33 |
$7 |
11 |
Tinzaparin sodium (Innohep) |
Leo Pharma Inc. |
$12,832 |
$378 |
$6,453 |
$1,669 |
$9 |
$4,319 |
- |
$5 |
- |
- |
- |
12 |
Fusidic acid (Fucidin) |
Leo Pharma Inc. |
$10,123 |
$968 |
$473 |
$240 |
$199 |
$7,739 |
$121 |
$224 |
$25 |
$131 |
$1 |
13 |
Treprostinil (Remodulin) |
United Therapeutics Corporation |
$8,894 |
$1,914 |
- |
$59 |
$516 |
$5,356 |
$1,050 |
- |
- |
- |
- |
14 |
Levonorgestrel (Mirena) |
Bayer Inc. |
$8,103 |
$1,738 |
$222 |
$488 |
$297 |
$4,919 |
$144 |
$150 |
$11 |
$134 |
- |
15 |
Enoxaparin sodium (Lovenox with preservative) |
Sanofi-Aventis Canada Inc. |
$7,983 |
$605 |
$614 |
$393 |
$17 |
$5,974 |
$159 |
$72 |
$20 |
$123 |
$7 |
16 |
Dornase alfa (Pulmozyme) |
Hoffmann-La Roche Ltd |
$6,760 |
$2,376 |
- |
$852 |
$341 |
$2,562 |
$297 |
- |
- |
$295 |
$37 |
17 |
Tacrolimus (Protopic) |
Leo Pharma Inc. |
$6,268 |
$132 |
$111 |
$80 |
$85 |
$5,816 |
$20 |
$19 |
$3 |
$2 |
- |
18 |
Conjugated estrogens (Premarin Vaginal) |
Pfizer Canada ULC |
$6,078 |
$973 |
$986 |
$387 |
$132 |
$3,087 |
$161 |
$151 |
$46 |
$141 |
$14 |
19 |
Insulin aspart/insulin aspart protamine (Novomix) |
Novo Nordisk Canada Inc. |
$5,959 |
$205 |
- |
- |
- |
$5,753 |
- |
- |
- |
- |
$1 |
20 |
Elosulfase alfa (Vimizim) |
BioMarin International Ltd |
$4,491 |
- |
- |
- |
- |
$4,491 |
- |
- |
- |
- |
- |
21 |
Terbinafine hydrochloride (Lamisil) |
Novartis Pharmaceuticals Canada Inc. |
$4,273 |
- |
$325 |
$110 |
$5 |
$3,644 |
$51 |
$76 |
- |
$57 |
$4 |
22 |
Pentosan polysulfate sodium (Elmiron) |
Janssen Inc. |
$3,639 |
$1,545 |
$344 |
$118 |
$174 |
$413 |
$283 |
$626 |
$24 |
$112 |
- |
23 |
Glycerol phenylbutyrate (Ravicti) |
Horizon Therapeutics Ireland DAC |
$3,587 |
$86 |
$334 |
$358 |
- |
$2,621 |
$140 |
$48 |
- |
- |
- |
24 |
Aprepitant (Emend Tri-Pack) |
Merck Canada Inc. |
$3,512 |
$541 |
$451 |
- |
$323 |
$2,057 |
$74 |
$37 |
$14 |
- |
$14 |
25 |
Flupentixol decanoate (Fluanxol Depot) |
Lundbeck Canada Inc. |
$3,224 |
$499 |
$79 |
$215 |
$132 |
$2,029 |
$61 |
$153 |
$1 |
$54 |
$1 |
26 |
Deferiprone (Ferriprox) |
Chiesi Canada Corp. |
$3,077 |
$779 |
$196 |
- |
- |
$1,860 |
$91 |
$151 |
- |
- |
- |
27 |
Pentoxifylline (Pentoxifylline SR) |
AA Pharma Inc. |
$3,053 |
$363 |
$321 |
$98 |
$40 |
$2,057 |
$36 |
$34 |
$14 |
$87 |
$3 |
28 |
Degarelix (Firmagon) |
Ferring Inc. |
$2,984 |
- |
- |
- |
- |
$2,686 |
$93 |
$144 |
$5 |
$46 |
$11 |
29 |
Atovaquone (Mepron) |
GlaxoSmithKline Inc. |
$2,905 |
$46 |
$823 |
$44 |
$77 |
$1,874 |
$9 |
- |
- |
$17 |
$15 |
30 |
Alemtuzumab (Lemtrada) |
Sanofi Genzyme, a division of Sanofi-Aventis Canada Inc. |
$2,880 |
$2,025 |
$388 |
$157 |
- |
$193 |
- |
- |
$71 |
- |
$46 |
31 |
Idursulfase (Elaprase) |
Takeda Canada Inc. |
$2,703 |
- |
- |
- |
- |
$2,703 |
- |
- |
- |
- |
- |
32 |
Pimecrolimus (Elidel) |
Bausch Health, Canada Inc. |
$2,586 |
$13 |
- |
$35 |
$8 |
$2,530 |
- |
- |
- |
- |
- |
33 |
Vitamin A/vitamin B12/vitamin D (Multi) |
Sandoz Canada Inc. |
$2,525 |
- |
- |
- |
- |
$2,525 |
- |
- |
- |
- |
- |
34 |
Methylprednisolone (Solu-Medrol) |
Pfizer Canada ULC |
$2,285 |
$184 |
$126 |
$77 |
$8 |
$1,639 |
$41 |
$83 |
$70 |
$53 |
$3 |
35 |
Alfacalcidol (One Alpha) |
Leo Pharma Inc. |
$2,183 |
$659 |
$73 |
$162 |
$7 |
$1,105 |
$56 |
$94 |
$0 |
$27 |
$1 |
36 |
Zuclopenthixol decanoate (Clopixol Depot) |
Lundbeck Canada Inc. |
$2,167 |
$710 |
$51 |
$252 |
$50 |
$886 |
$77 |
$76 |
$0 |
$64 |
$0 |
37 |
Dexamethasone/tobramycin (Tobradex) |
Novartis Pharmaceuticals Canada Inc. |
$2,144 |
$271 |
$280 |
$155 |
$17 |
$1,253 |
$43 |
$69 |
$4 |
$50 |
$2 |
38 |
Medroxyprogesterone acetate (Depo-Provera) |
Pfizer Canada ULC |
$2,044 |
$303 |
$25 |
$222 |
$112 |
$1,112 |
$82 |
$75 |
$12 |
$101 |
- |
39 |
Megestrol acetate (Megestrol) |
AA Pharma Inc. |
$1,874 |
$148 |
$23 |
$8 |
$287 |
$1,107 |
$157 |
$109 |
$10 |
$25 |
- |
40 |
Amantadine hydrochloride (pdp-Amantadine Hydrochloride) |
Pendopharm,a division of Pharmascience Inc. |
$1,870 |
$283 |
$177 |
$272 |
$54 |
$930 |
$44 |
$60 |
$14 |
$32 |
$4 |
41 |
Diphenoxylate hydrochloride/atropine sulfate (Lomotil) |
Pfizer Canada ULC |
$1,784 |
$123 |
$315 |
$87 |
$20 |
$1,087 |
$41 |
$48 |
$1 |
$61 |
$0 |
42 |
Beclomethasone dipropionate (Qvar) |
Bausch Health, Canada Inc. |
$1,657 |
$206 |
$238 |
$279 |
$61 |
$775 |
$40 |
$49 |
$3 |
$5 |
$2 |
43 |
Fluorouracil (Efudex) |
Bausch Health, Canada Inc. |
$1,561 |
$132 |
$216 |
$48 |
$17 |
$1,059 |
$30 |
$38 |
$13 |
$6 |
$2 |
44 |
Icatibant (Firazyr) |
Takeda Canada Inc. |
$1,519 |
$226 |
$89 |
$77 |
$438 |
$649 |
- |
- |
- |
$41 |
- |
45 |
Thyroid (Thyroid) |
Erfa Canada 2012 Inc. |
$1,393 |
$380 |
$828 |
$119 |
$10 |
- |
$21 |
$34 |
$0 |
$1 |
- |
46 |
Macrogol/sodium sulfate (PegLyte pdr sol) |
Pendopharm,a division of Pharmascience Inc. |
$1,392 |
- |
- |
$6 |
$3 |
$1,383 |
- |
- |
- |
$0 |
- |
47 |
Chlorthalidone (Chlorthalidone) |
AA Pharma Inc. |
$1,330 |
$202 |
$119 |
$54 |
$15 |
$878 |
$15 |
$22 |
$4 |
$17 |
$5 |
48 |
Calcipotriol (Dovonex) |
Leo Pharma Inc. |
$1,276 |
$231 |
$122 |
$36 |
$97 |
$591 |
$38 |
$68 |
$11 |
$73 |
$7 |
49 |
Thyrotropin alfa (Thyrogen) |
Sanofi Genzyme, a division of Sanofi-Aventis Canada Inc. |
$1,270 |
- |
$355 |
- |
- |
$864 |
- |
$51 |
- |
- |
- |
50 |
Salmeterol (Serevent Diskus) |
GlaxoSmithKline Inc. |
$1,235 |
$184 |
$187 |
$62 |
$60 |
$663 |
$29 |
$25 |
$6 |
$7 |
$11 |
Total |
$624,530 |
$42,647 |
$55,184 |
$18,596 |
$10,529 |
$443,882 |
$22,479 |
$15,979 |
$4,008 |
$10,690 |
$536 |
||
Share of all single-source non-patented medicines |
94% |
85% |
93% |
85% |
81% |
96% |
93% |
90% |
94% |
90% |
93% |
||
Data source: National Prescription Drug Utilization Information System Database, Canadian Institute for Health Information.
Appendix G: Top 50 Manufacturers by Drug Cost, NPDUIS Public Drug Plans, 2020/21 ($million)
| Rank | Company | Total | BC | AB | SK | MB | ON | NB | NS | PE | NL | YT |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
1 |
Janssen Inc. |
$897.16 |
$67.35 |
$74.76 |
$90.16 |
$55.74 |
$534.00 |
$27.54 |
$29.94 |
$4.11 |
$12.44 |
$1.13 |
2 |
AbbVie Corporation |
$572.43 |
$148.95 |
$69.80 |
$38.40 |
$42.76 |
$228.81 |
$12.91 |
$18.23 |
$2.67 |
$8.88 |
$1.02 |
3 |
Novartis Pharmaceuticals Canada Inc. |
$555.41 |
$35.66 |
$39.87 |
$12.63 |
$18.85 |
$411.11 |
$18.60 |
$10.22 |
$0.99 |
$7.17 |
$0.32 |
4 |
Bayer Inc. |
$522.45 |
$17.82 |
$26.95 |
$15.62 |
$6.58 |
$432.74 |
$13.01 |
$3.97 |
$2.08 |
$3.09 |
$0.59 |
5 |
Apotex Inc. |
$434.06 |
$43.10 |
$29.07 |
$13.37 |
$12.29 |
$307.07 |
$11.72 |
$8.89 |
$1.83 |
$6.23 |
$0.49 |
6 |
Boehringer Ingelheim |
$392.35 |
$41.60 |
$40.76 |
$11.70 |
$8.74 |
$271.33 |
$6.56 |
$7.76 |
$1.50 |
$2.15 |
$0.25 |
7 |
Novo Nordisk Canada Inc. |
$298.24 |
$9.81 |
$38.39 |
$6.85 |
$4.50 |
$213.54 |
$5.67 |
$10.46 |
$3.40 |
$5.42 |
$0.22 |
8 |
Merck Canada Inc. |
$295.60 |
$2.37 |
$20.47 |
$4.37 |
$2.78 |
$258.88 |
$4.83 |
$1.67 |
$0.06 |
$0.14 |
$0.02 |
9 |
AstraZeneca Canada Inc. |
$288.10 |
$19.82 |
$30.09 |
$7.28 |
$9.14 |
$209.04 |
$4.19 |
$5.79 |
$0.81 |
$1.75 |
$0.18 |
10 |
Gilead Sciences Canada Inc. |
$266.03 |
$56.18 |
$14.37 |
$14.07 |
$6.31 |
$162.28 |
$5.93 |
$1.40 |
- |
$4.66 |
$0.82 |
11 |
Sandoz Canada Inc. |
$265.84 |
$40.08 |
$27.87 |
$11.99 |
$7.19 |
$159.63 |
$5.53 |
$7.84 |
$1.27 |
$4.03 |
$0.41 |
12 |
Teva Canada Ltd |
$258.16 |
$32.44 |
$22.80 |
$12.93 |
$11.75 |
$152.99 |
$8.57 |
$8.97 |
$1.41 |
$5.85 |
$0.44 |
13 |
Celgene Inc. |
$257.62 |
$0.01 |
- |
- |
$14.81 |
$213.51 |
$8.62 |
$11.74 |
$1.31 |
$7.40 |
$0.22 |
14 |
Bristol-Myers Squibb Canada |
$257.55 |
$35.18 |
$31.66 |
$11.35 |
$6.55 |
$164.30 |
$3.23 |
$3.73 |
$0.65 |
$0.71 |
$0.19 |
15 |
GlaxoSmithKline Inc. |
$254.16 |
$32.43 |
$28.62 |
$11.96 |
$7.83 |
$151.01 |
$8.43 |
$8.00 |
$1.13 |
$4.41 |
$0.33 |
16 |
Pfizer Canada ULC |
$235.87 |
$27.12 |
$12.96 |
$6.57 |
$12.32 |
$156.46 |
$6.23 |
$9.27 |
$0.80 |
$3.83 |
$0.30 |
17 |
Pharmascience Inc. |
$213.45 |
$29.42 |
$18.78 |
$10.64 |
$8.03 |
$127.14 |
$4.76 |
$7.56 |
$1.32 |
$5.64 |
$0.16 |
18 |
Hoffmann-La Roche Ltd |
$184.14 |
$24.74 |
$30.39 |
$16.12 |
$15.60 |
$84.23 |
$4.38 |
$4.88 |
$0.41 |
$2.71 |
$0.69 |
19 |
Sanis Health Inc. |
$179.13 |
$19.89 |
$21.68 |
$8.64 |
$6.43 |
$103.15 |
$6.96 |
$7.22 |
$1.09 |
$3.63 |
$0.44 |
20 |
Takeda Canada Inc. |
$165.60 |
$43.40 |
$19.61 |
$18.54 |
$11.96 |
$63.07 |
$3.31 |
$3.39 |
$1.08 |
$1.15 |
$0.09 |
21 |
Sanofi-Aventis Canada Inc. |
$150.68 |
$3.38 |
$11.95 |
$11.09 |
$3.76 |
$112.45 |
$2.70 |
$3.68 |
$0.51 |
$1.08 |
$0.08 |
22 |
Amgen Canada Inc. |
$148.73 |
$6.86 |
$12.47 |
$2.54 |
$0.52 |
$122.58 |
$1.79 |
$0.62 |
$0.04 |
$1.27 |
$0.03 |
23 |
Allergan Inc. |
$133.47 |
$10.80 |
$12.03 |
$3.28 |
$2.23 |
$99.78 |
$1.36 |
$2.72 |
$0.34 |
$0.84 |
$0.08 |
24 |
Eli Lilly Canada Inc. |
$120.28 |
$32.13 |
$10.70 |
$7.75 |
$7.54 |
$45.82 |
$4.65 |
$5.31 |
$1.26 |
$4.80 |
$0.32 |
25 |
Astellas Pharma Canada Inc. |
$111.90 |
$0.03 |
$3.55 |
$3.09 |
$7.55 |
$90.12 |
$3.22 |
$2.56 |
$0.44 |
$1.25 |
$0.08 |
26 |
Biogen Canada Inc. |
$103.36 |
$16.79 |
$20.38 |
$7.46 |
$9.38 |
$40.42 |
$3.85 |
$2.64 |
$0.29 |
$1.81 |
$0.34 |
27 |
Sivem Pharmaceuticals ULC |
$100.41 |
$17.51 |
$26.31 |
$7.19 |
$8.04 |
$21.24 |
$5.17 |
$9.64 |
$2.41 |
$2.90 |
$0.01 |
28 |
Mylan Pharmaceuticals ULC |
$95.76 |
$13.48 |
$10.68 |
$4.53 |
$5.37 |
$51.64 |
$3.84 |
$3.16 |
$0.71 |
$2.22 |
$0.14 |
29 |
Immunex Corporation |
$85.35 |
$2.34 |
$8.92 |
$7.29 |
$9.91 |
$47.75 |
$2.87 |
$4.48 |
$0.54 |
$1.08 |
$0.17 |
30 |
Celltrion Healthcare Co.,Ltd |
$77.17 |
$36.43 |
$18.83 |
$0.74 |
$5.53 |
$14.97 |
$0.38 |
$0.16 |
$0.01 |
$0.08 |
$0.04 |
31 |
Purdue Pharma |
$68.73 |
$5.46 |
$7.33 |
$4.77 |
$3.28 |
$42.44 |
$2.34 |
$2.45 |
$0.14 |
$0.46 |
$0.06 |
32 |
AA Pharma Inc. |
$67.06 |
$15.29 |
$6.11 |
$4.09 |
$2.65 |
$31.16 |
$2.32 |
$2.94 |
$0.47 |
$1.95 |
$0.09 |
33 |
Auro Pharma Inc. |
$66.30 |
$7.69 |
$5.02 |
$1.80 |
$1.34 |
$47.83 |
$0.65 |
$1.23 |
$0.19 |
$0.47 |
$0.08 |
34 |
ViiV Healthcare ULC |
$65.65 |
- |
- |
$2.64 |
$4.11 |
$56.60 |
$1.73 |
- |
- |
$0.41 |
$0.16 |
35 |
Otsuka Pharmaceutical Co., Ltd |
$59.83 |
$15.52 |
$1.51 |
$2.73 |
$1.00 |
$35.99 |
$1.43 |
$1.29 |
$0.07 |
$0.27 |
$0.02 |
36 |
Sanofi Genzyme, a division of Sanofi-Aventis Canada Inc. |
$55.19 |
$9.36 |
$3.59 |
$3.70 |
$3.39 |
$29.66 |
$1.91 |
$2.40 |
$0.38 |
$0.69 |
$0.11 |
37 |
Alexion Pharma GmbH |
$51.92 |
- |
$8.92 |
- |
$1.57 |
$40.45 |
$0.46 |
- |
$0.51 |
- |
- |
38 |
Bausch Health, Canada Inc. |
$50.05 |
$3.96 |
$5.59 |
$1.53 |
$1.16 |
$34.37 |
$1.33 |
$1.18 |
$0.19 |
$0.71 |
$0.02 |
39 |
Samsung Bioepis Co., Ltd |
$49.60 |
$27.97 |
$6.59 |
$1.47 |
$1.52 |
$10.82 |
$0.61 |
$0.32 |
$0.05 |
$0.17 |
$0.07 |
40 |
Leo Pharma Inc. |
$46.40 |
$3.06 |
$8.49 |
$3.06 |
$0.45 |
$29.89 |
$0.47 |
$0.47 |
$0.05 |
$0.44 |
$0.02 |
41 |
Taro Pharmaceuticals Inc. |
$44.70 |
$4.66 |
$2.72 |
$1.84 |
$1.82 |
$30.02 |
$0.94 |
$1.62 |
$0.27 |
$0.77 |
$0.05 |
42 |
BGP Pharma ULC |
$40.81 |
$6.08 |
$5.45 |
$1.86 |
$1.34 |
$22.36 |
$1.22 |
$1.72 |
$0.27 |
$0.46 |
$0.06 |
43 |
Organon Canada Inc. |
$36.21 |
$3.27 |
$3.87 |
$1.08 |
$0.47 |
$24.90 |
$1.31 |
$0.69 |
$0.13 |
$0.46 |
$0.03 |
44 |
UCB Canada Inc. |
$35.54 |
$8.97 |
$3.36 |
$2.46 |
$0.84 |
$17.14 |
$0.51 |
$1.54 |
$0.18 |
$0.41 |
$0.13 |
45 |
JAMP Pharma Corporation |
$32.89 |
$3.67 |
$3.71 |
$1.29 |
$0.84 |
$21.31 |
$0.83 |
$0.57 |
$0.14 |
$0.50 |
$0.03 |
46 |
Marcan Pharmaceuticals Inc. |
$31.26 |
$3.14 |
$2.93 |
$1.45 |
$0.88 |
$19.85 |
$0.71 |
$1.33 |
$0.14 |
$0.75 |
$0.06 |
47 |
Sun Pharma Canada Inc. |
$29.16 |
$2.95 |
$2.29 |
$0.82 |
$0.37 |
$20.97 |
$0.61 |
$0.63 |
$0.09 |
$0.39 |
$0.04 |
48 |
Mint Pharmaceuticals Inc. |
$29.13 |
$3.77 |
$2.20 |
$1.13 |
$0.61 |
$19.64 |
$0.42 |
$0.80 |
$0.12 |
$0.27 |
$0.18 |
49 |
TerSera Therapeutics, LLC |
$25.56 |
- |
<$0.01 |
$0.01 |
$0.02 |
$22.57 |
$0.71 |
$1.56 |
$0.25 |
$0.35 |
$0.08 |
50 |
Covis Pharma GmbH |
$23.20 |
$1.15 |
$1.09 |
$0.35 |
$0.14 |
$19.42 |
$0.38 |
$0.36 |
$0.18 |
$0.14 |
$0.01 |
|
Total |
$8,829.64 |
$993.11 |
$815.48 |
$416.24 |
$357.78 |
$5,628.49 |
$221.68 |
$228.97 |
$38.31 |
$118.68 |
$10.91 |
Data source: National Prescription Drug Utilization Information System Database, Canadian Institute for Health Information.