The Chief Public Health Officer’s Report on the State of Public Health in Canada 2018: Preventing Problematic Substance Use in Youth
Download the alternative format
(PDF format, 3.9 MB / KB, 61 pages)
Organization: Public Health Agency of Canada
Published: 2018-10-23
A Message from Canada's Chief Public Health Officer
I am pleased to present my annual report, which is a snapshot of the health of Canadians and a spotlight on the prevention of problematic substance use among youth.
This year I am introducing a new dashboard of health indicators to provide an overall picture of the health status of Canadians. In reviewing the dashboard, it is evident that Canada continues to be a healthy nation. We are generally living long lives and rank among the top or middle third for most indicators when compared to other high income countries.
I do remain concerned, however, about the influence of persistent health inequalities and the impact of social and economic factors as barriers to living well and to the elimination of key infectious diseases.
Major chronic diseases, including cancer, cardiovascular diseases, neurological disorders, chronic respiratory diseases, and diabetes continue to be the leading causes of all deaths in Canada. It is important that as we age, we live in good health. Many chronic diseases can be prevented or delayed by approaches that get to the root causes of risks such as tobacco smoking, physical inactivity, unhealthy eating, and harmful use of alcohol. At the same time, mental health impacts every aspect of our lives, including relationships, education, work, and community involvement. Although the majority of Canadians report positive mental health, a third of us will be affected by a mental illness during our lifetime.
There are also worrying trends in relation to some infectious diseases. We are seeing a rise in sexually transmitted infections, while antimicrobial resistance (AMR) remains a global threat to our ability to cure infections. Lastly, as I highlighted in my previous report, tuberculosis is having a serious and ongoing impact on some First Nations and Inuit communities. Many cases of infectious diseases can be prevented or eliminated by reducing risks of exposure and ensuring access to screening and treatment – provided that partners also tackle underlying social factors by improving living conditions and confronting stigma.
To address key public health issues, I set out my vision and areas of focus for achieving optimal health for all Canadians earlier this year. I will champion the reduction of health disparities in key populations in collaboration with many partners and sectors. I will focus efforts in the areas of tuberculosis, AMR, built environments, sexually transmitted and blood-borne infections, children and youth, and the prevention of problematic substance use.
This brings me to this year's focus on preventing problematic substance use. The growing number of opioid-related overdoses and the over 8000 deaths since 2016 are tragic and unacceptable. The national life expectancy of Canadians may actually be decreasing for the first time in decades, because of the opioid overdose crisis. At the same time, because of its social acceptance, we have lost sight of the fact that continued high rates of problematic alcohol consumption are leading to a wide-range of harms. In fact, 25% of youth in grades 7 to 12 use alcohol excessively. I am also aware that the change in legal status of cannabis means we need to make sure that youth understand that legal does not mean safe.
We have to think about how to reverse these trends for future generations. That is why this report centres on youth and explores the reasons for harmful substance use, as well as effective approaches to prevent problematic use.
There is a complex interplay of factors that may lead youth to use substances. We know that the marketing, advertising, and availability of a substance can increase substance use in youth. We also know that youth are more likely to use substances as a coping mechanism when they have experienced abuse and other forms of trauma. But we also know that there are protective factors that can help build youth resilience, such as stable environments and positive family and caregiver relationships.
The interconnected nature of these factors means there is a critical need to collaborate across many sectors to develop comprehensive prevention solutions. The next generation of interventions can connect sectors such as housing, social services, education, public health and primary health care, at multiple levels to implement coordinated policies, public and professional education and programs. We can also work together with the media and private sector to promote new social norms around lower risk use of substances.
Our efforts need to value the experiences and voices of youth and those who use substances. The media, health care, and social service organizations can help to eliminate stigma and discrimination by adopting equitable and compassionate policies, practices and language.
There will never be just one answer to this ever-shifting issue of problematic substance use. This is a key moment in Canada to examine how we address substance use across all areas of potential action: prevention, harm reduction, treatment and recovery. My aim with this report is to draw attention to the central role of prevention. As important initiatives like the Canadian Drugs and Substances Strategy advance, this report can help to inform these collective efforts to prevent substance use from becoming problematic.
I hope my report will stimulate discussion and lead to renewed action to achieve this goal.
Contents
- About this Report
- Chapter 1: Describing the Health of Canadians
- Chapter 2: Understanding Youth and Problematic Substance Use
- Chapter 3: Interventions for Preventing Problematic Substance Use in Youth
- Chapter 4: The Way Forward – The Path to Preventing Problematic Substance Use in Youth
- References
- Appendix 1: Glossary
- Appendix 2: CPHO Health Status Dashboard
- Appendix 3: Guidelines for Low-Risk Alcohol Drinking and Lower-Risk Cannabis Use
- Acknowledgements
About this Report
This year's report from the Chief Public Health Officer of Canada first provides a snapshot on the health status of Canadians, then shines a light on problematic substance use among youth with a focus on primary prevention. This means tackling risk factors, strengthening protective factors, delaying initiation to the use of substances, and preventing their harmful use.
The report includes the following sections:
Chapter 1: Describing the Health of Canadians provides a snapshot of the overall health of Canadians by discussing select health indicators, such as life expectancy and positive mental health. This section concludes by examining substance use and harm patterns of alcohol, cannabis and opioid use in the general population.
Chapter 2: Understanding Youth and Problematic Substance Use examines the issues around youth and substance use in Canada. It first describes the nature of youth substance use and the potential associated harms. It then explores why youth are drawn to using substances and describes the drivers that put youth at risk or that can protect them from harm.
Chapter 3: Interventions for Preventing Problematic Substance Use in Youth speaks to the need for all relevant health, education and social sectors to coordinate a range of individual, community and society-wide interventions in order to prevent problematic substance use in youth. This chapter also examines population and individual level evidence-based practices and policies that can address the drivers of problematic substance use.
Chapter 4: The Way Forward – The Path to Preventing Problematic Substance Use in Youth calls upon all relevant sectors to implement an integrated suite of interventions that enhances protective factors and reduces risk factors such as stigma and trauma.
Chapter 1: Describing the Health of Canadians
Introduction
The highlights below provide a snapshot of the overall health of Canadians, by drawing on several indicators from the new Chief Public Health Officer's Health Status Dashboard (see Appendix 2).
What is a health indicator?
Health indicators are quantifiable measures that researchers and decision makers use as ways to understand the health of a population.Reference 1
In Brief:
- Overall, Canadians enjoy good health and live long lives. Current inequalities prevent certain populations from achieving their full health potential, such as those Canadians living with low income and those with low education.
- Positive mental health is just as important as good physical health. It has a protective effect that can help to prevent disease and reduce risks such as problematic substance use.
- The opioid overdose crisis in Canada is alarming. It may be shortening our national life expectancy, for the first time in decades.
- Problematic alcohol use accounts for the greatest health and social costs, based on the accumulative harms of hospitalizations, death and lost productivity. More people are hospitalized from alcohol use than from heart attacks.
What are health inequalities?
While Canadians enjoy good health overall, there are barriers preventing some from reaching their full health potential. These barriers, often called inequalities, are influenced by a complex web of individual, socio-economic, environmental, and political factors that include our income, jobs and working conditions, education, housing, the neighbourhoods we live in and the experiences that shape our early childhood. These factors, collectively known as the social determinants of health, shape our lives and influence the odds of achieving and maintaining good health over our lifetime. First Nations, Inuit and Métis peoples in Canada experience additional unique social determinants of health, including the historical impacts of colonization, the legacy of residential schools, land, language and culture.
Life Expectancy
Defined as the number of years the average person can expect to live (usually from birth), life expectancy is considered one of the most general indicators for the overall health of a country.
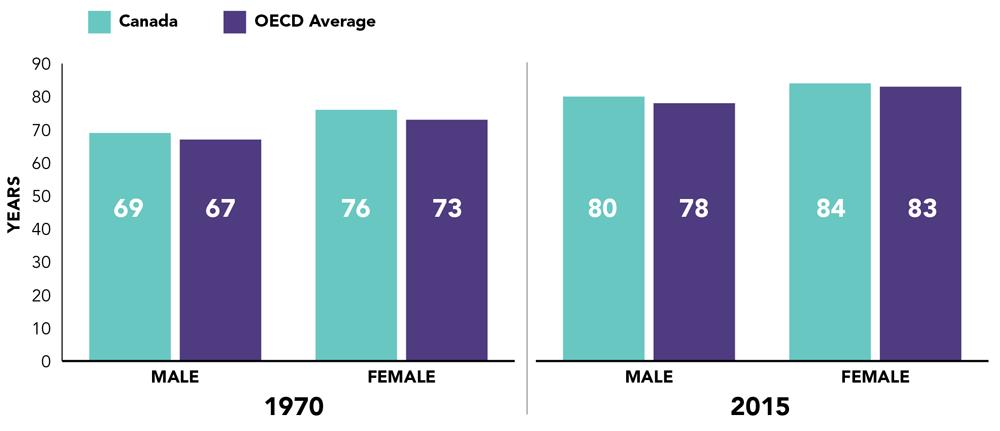
On the whole, life expectancy has been steadily increasing in Canada over many years and it is comparable to other high income countries (see Figure 1).Reference 22 Reference 23 Reference 24 Alarmingly, this is expected to change. For the first time in recent decades, life expectancy in British Columbia is decreasing, due to harms associated with opioid overdoses.Reference 9 While data are not available at the national level, the Public Health Agency of Canada (PHAC) is analyzing the impact of the opioid overdose crisis on overall life expectancy.
Figure 1: Canada's Life expectancy compared to the Organisation for Economic Cooperation and Development'sFigure 1 Footnote * average, 1970 and 2015 (or nearest data year)Reference 23
- Figure 1 Footnote *
-
The Organization for Economic Cooperation and Development (OECD) is a group of countries who develop and discuss economic and social policy.
Source: Health at a Glance 2017
Text Description
| Year | Sex | Canada | OECD Average |
|---|---|---|---|
| 1970 | Male | 69 | 67 |
| 1970 | Female | 76 | 73 |
| 2015 | Male | 80 | 78 |
| 2015 | Female | 84 | 83 |
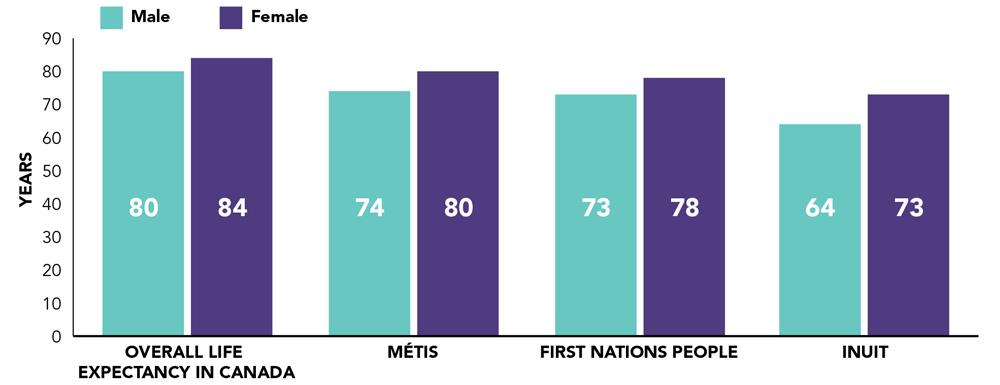
Life expectancy is not equal among all segments of Canadian society. Certain populations such as First Nations, Métis, Inuit, Canadians living with low income and those with low education experience a shorter life expectancy than the national average.Reference 25 As shown in Figure 2, there are gaps in life expectancy for First Nations, Inuit and Métis Peoples compared to overall life expectancy. Inuit have the largest gap, up to 16 years shorter than the overall Canadian life expectancy (64 years for males and 73 years for females).Reference 22 Reference 26 The unique cultural and historical context of Indigenous Peoples contributes to this trend. The lasting legacy of colonization and intergenerational trauma have led to systemic health inequities between Indigenous peoples and non-Indigenous populations.
Figure 2: Overall and Indigenous Peoples life expectancyFigure 2 Footnote * in Canada, 2017Reference 22 Reference 26
- Figure 2 Footnote *
-
The life expectancies for Métis, First Nations people, and Inuit are projections for 2017. Overall life expectancy figures are based on data from 2013-2015.
Sources: Life expectancy and other elements of the life table, Indigenous statistics at a glance
Text Description
| Identity | Male | Female |
|---|---|---|
| Overall life expectancy in Canada | 80 | 84 |
| Métis | 74 | 80 |
| First Nations people | 73 | 78 |
| Inuit | 64 | 73 |
Life expectancy is about 3 years lower for those in the poorest neighbourhoods, compared to the Canadian average.Reference 25 Furthermore, it is almost 2 years higher for those in the most educated neighbourhoods, compared to the average life expectancy.Reference 25
The good news is that the inequality gap in Canada appears to be smaller than that of most other high income countries. For instance, Canada has a smaller gap in life expectancy between the highest and lowest educated groups when compared to most Organization for Economic Cooperation and Development (OECD) countries.Reference 23 This smaller gap in no way justifies inaction. Through dedicated multi-sector actions, the public health community can support more Canadians to be healthier with improved social and economic conditions.
Disease Burden
In 2016, there was a total of 273,000 deaths in Canada. Chronic diseases accounted for 89% of these deaths; 6% were attributed to injuries (specifically self-harm, falls and road injuries); and over 5% were due to infectious, maternal, neonatal and nutritional diseases.Reference 27 As Canada's population continues to live longer, chronic diseases have become more common. The onset of chronic disease, and associated impacts, can be delayed by avoiding specific risk factors.
Chronic Diseases
In 2016, about 244,000 (89%) out of the 273,000 deaths in Canada were due to chronic diseases.Reference 27 Those accounting for the most deaths were cancers (31%), cardiovascular diseases (30%), neurological disorders (10%), chronic respiratory diseases (6%), and diabetes (3%).Reference 27
Although many Canadians are broadly considered to be healthy, many are living with a preventable chronic disease or risk factor. Indeed, more than 20% of Canadians over the age of 20 are experiencing a chronic disease such as cardiovascular disease, cancer, chronic respiratory disease, or diabetes.Reference 24 The risk of developing many chronic diseases increases with age. About 80% of Canadian adults are living with at least one modifiable risk factor for chronic diseases, including tobacco use, physical inactivity, unhealthy eating, and heavy drinking (see Figure 3).Reference 24
Figure 3: Top 4 Chronic Diseases and Risk FactorsReference 24 Reference 25 Reference 28 Reference 29
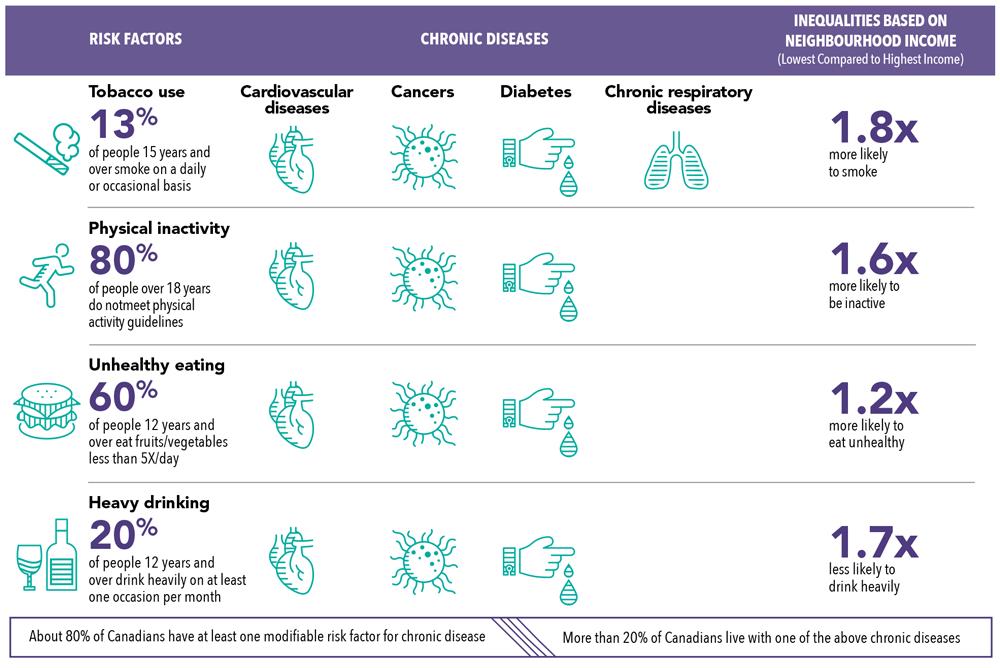
Text Description
About 80% of Canadians have at least one modifiable risk factor for chronic diseases, such as cardiovascular diseases, cancers, diabetes, chronic respiratory diseases. More than 20% of Canadians live with one of these chronic diseases.
The risk factors include tobacco use (13% of people 15 years and over smoke on a daily or occasional basis), physical inactivity (80% of people over 18 years do not meet physical activity guidelines), unhealthy eating (60% of people 12 years and over eat fruits/vegetables less than 5 times per day), and heavy drinking (20% of people 12 years and over drink heavily on at least one occasion per month).
There are inequalities based on neighbourhood income. Individuals from the lowest compared to highest neighbourhood income are 1.8 times more likely to smoke, 1.6 times more likely to be inactive, 1.2 times more likely to eat unhealthy, and 1.7 times less likely to drink heavily.
About 80% of Canadians have at least one modifiable risk factor for chronic disease. More than 20% of Canadians live with one of the above chronic diseases.
Delaying the onset of chronic disease and preventing risk factors are not only individual choices. These diseases are strongly influenced by factors in social, economic and physical environments. For example:
- Those living in walkable and safe neighbourhoods are more likely to be physically active. Almost 20% of Canadians report a crime rate that discourages them from walking at night in their neighbourhoods.Reference 30 Reference 31
- Access to healthy and affordable food is essential for healthy eating. This poses a particular challenge for people living in northern Canadian regions where food products are more expensive and, in some cases, traditional food is less available.Reference 32 Reference 33 Reference 34 Reference 35 Over 2 million Canadians cannot access, or afford, enough safe and nutritious food throughout the year for a healthy life.Reference 36
- Almost 30% of adults from the lowest income neighbourhoods report smoking, compared to about 15% of those from the highest income neighbourhoods.Reference 25 The annual lung cancer incidence rate is higher for those living in the lowest income neighbourhoods versus the highest income neighbourhoods (90 per 100,000 and 54 per 100,000, respectively).Reference 25
An opportunity to reduce health inequities
Applying a social-determinants-of-health lens is particularly powerful for understanding the disproportionate health burden shared by Indigenous Peoples in Canada. Throughout history, First Nations, Métis and Inuit have had to overcome such catastrophic life events as colonialism, racism, the loss of traditional and political institutions, and attempts at cultural assimilation. Problematic substance use, suicide and family violence are examples of lasting intergenerational impacts of residential school placement and resulting trauma that have influenced the health of Indigenous Peoples across the country.
For progress to be made, all partners in health must collectively recognize, support, and foster the strength and resilience of First Nations, Métis and Inuit Peoples in Canada. Long-term commitment to implementing the recommendations of the Truth and Reconciliation Commission will contribute to improving health outcomes, and help individuals, families and communities to reach their full potential.
The Truth and Reconciliation Report provides a way forward to addressing the longstanding racism and discrimination perpetrated against Indigenous Peoples of Canada. The report contains 94 calls to action, which include recommendations on health, language and culture, justice, youth programming, and professional training and development.Reference 13 Reference 17
Infectious and Other Diseases
In 2016, some 13,000 (5%) out of the 273,000 deaths in Canada were due to infectious, maternal, neonatal, and nutritional diseases – a relatively small burden compared to that of chronic diseases.Reference 27 Three percent of all deaths were caused by lower respiratory infections, such as pneumonia and influenza (between them, the leading cause of death for infectious diseases).Reference 27 Pneumonia and influenza are major contributors to deaths and hospitalizations in senior populations, especially in those over the age of 80 years.Reference 37 Reference 38 Influenza vaccinations in the elderly may lower the risk of this infection.Reference 39 Reference 40 Reference 41
About 0.2% of all deaths are the result of tuberculosis and HIV/AIDS.Reference 27 In 2016, there were over 1,700 people diagnosed with active tuberculosis disease and over 2,300 people diagnosed with HIV.Reference 2 While not a particularly large burden for the entire country, certain populations are affected disproportionately by infectious diseases. For example, the rate of active tuberculosis cases among Inuit is close to 300 times higher than the rate in the Canadian-born non-Indigenous population (see Figure 4).Reference 42 Reference 43
Figure 4: Rate ratio of active tuberculosis disease relative to the Canadian-born non-Indigenous population rate of 0.6 per 100,000, 2016Reference 42 Reference 43
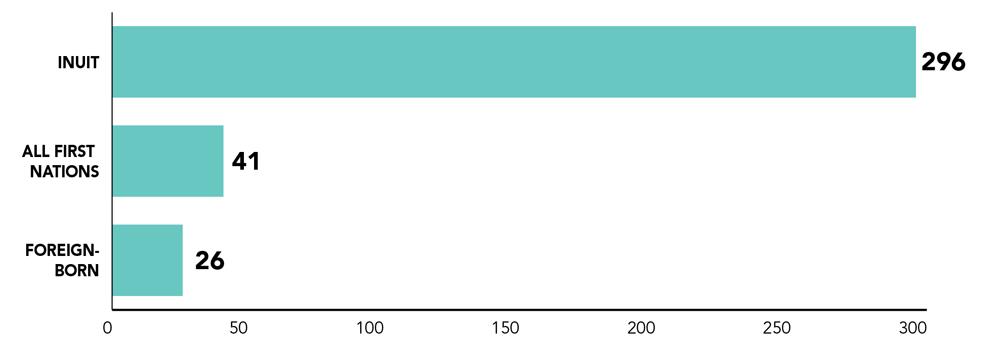
Source: Tuberculosis in Canada, 2016
Text Description
| Population Group | Rate Ratio |
|---|---|
| Foreign-born | 26 |
| All First Nations | 41 |
| Inuit | 296 |
Historically, infectious diseases were far more common across all populations in Canada before large vaccination efforts, improvements in sanitation and built environments, and advancements in screening and in treatments such as antimicrobials.Reference 44 Reference 45 Despite this progress over the past century, complacency is not an option.Reference 46 The trends of antimicrobial resistant (AMR) infections, incomplete vaccination coverage, and emerging infectious diseases related to climate change, all underscore the need to remain vigilant.
Though rates of most AMR infections are stable or declining, the rates are increasing for some, such as Neisseria gonorrhea.Reference 47 Common healthcare-associated infections like methicillin-resistant Staphylococcus aureus (MRSA) and Clostridium difficile can be reduced with the appropriate use of antimicrobials and sterilization practices.Reference 47 The challenge with the majority of AMR infections is that they require more complex treatments.Reference 47
Overall, coverage rates for many common vaccinations in infants and children are below national goals; this may give rise in the future to outbreaks of vaccine preventable diseases, such as measles, invasive pneumococcal disease or pertussis.Reference 48 Reference 49
The number of people with Lyme disease has been steadily increasing over the past decades.Reference 50 Many factors are at play, notably the influence of climate change in expanding the natural habitat of ticks that may carry the disease.Reference 50
Many cases of infectious diseases can be prevented by reducing risks of exposure and ensuring access to screening and treatment – provided that partners in health also tackle underlying social factors by improving living conditions, and confronting stigma.Reference 43 Reference 51 For example, tuberculosis is often described as a social disease with a medical aspect.Reference 43 Unlike chronic diseases, infectious diseases like HIV or TB can be eliminated through prevention and control. It was a combination of collaborative public health efforts, such as vaccination coverage, active surveillance strategies, public awareness and, to a varying level of effectiveness, quarantine interventions, that led to the eradication of polio in Canada two decades ago.Reference 52
The rise of sexually transmitted blood-borne infections (STBBIs)
Some STBBIs have been increasing in Canada over the past two decades, most notably chlamydia, gonorrhea, and syphilis.Reference 2 Many actions can be taken in order to prevent infectious diseases, including greater sexual health education, promotion of safe sexual practices, increased uptake of vaccinations, and the regular use of sterile drug equipment.Reference 12
Mental Health and Substance Use
In addition to good physical health, positive mental health is an essential component contributing to the overall health and well-being of Canadians.Reference 53 Reference 54
Positive mental health is “the capacity of each and all of us to feel, think and act in ways that enhance our ability to enjoy life and deal with the challenges we face”.Reference 55 The majority of Canadians report having positive mental health. About 70% describe their mental health as “very good” or “excellent”.Reference 29 Mental well-being has a protective effect that can help reduce risk factors and prevent diseases. Reference 30 High levels of social support and low stress, for example, have been found to decrease the risk of premature death and poor health.Reference 56 Reference 57 Reference 58
Other definitions of positive mental health
The First Nations Mental Wellness Continuum Framework explains that mental wellness is supported by culture, language, Elders, families, and creation and is necessary for healthy individual, community, and family life.Reference 3
Inuit Tapiriit Kanatami defines mental wellness as the physical, emotional, mental and spiritual wellness, as well as strong cultural identity.Reference 11
The Métis Life Promotion Framework promotes a holistic approach for achieving a balance among various factors of wellness.Reference 16
Over 30% of Canadians will be affected by a mental illness during their lifetime.Reference 59 Commonly reported mental illnesses include mood and anxiety disorders and substance use disorders.Reference 59 Reference 60 About 20% of Canadians report a substance use disorder in their lifetime.Reference 59 Alcohol is the cause of most frequently reported substance use disorders.Reference 59
Substance Use and Potential Harms
Currently, substance use issues are capturing the attention of public health experts, decision-makers, communities and families across Canada. The current opioid overdose crisis and the new reality of cannabis legalization are underpinning a drive to re-examine the range of substance use behaviours and their implications for public health.Reference 61 Given the acute extent of the opioid crisis, some stakeholders, including people with lived and living experiences, have asked that the decriminalizing of additional psychoactive substances in Canada be considered (decriminalization refers to the removal of criminal penalties for the possession of substances for personal use). In addition, Canadians are unfortunately not paying enough attention to the harms of alcohol.
Opioid-related deaths are reducing the life expectancy of British Columbians
Recent data from BC show that life expectancy dropped by 0.12 year from 2014 to 2016 due to deaths involving substances, with over 90% of these related to opioids. Reference 9 This dip in life expectancy was more pronounced in men and in poorer neighbourhoods.Reference 9
Most Canadians use psychoactive substances in moderation without experiencing serious consequences. Problematic use occurs when these substances are consumed in a manner, situation, amount, or frequency that causes physical or mental harm to the person using them or to those around them. This definition can incorporate behaviours beyond a substance use disorder, such as taking substances while pregnant, interfering in major social or personal duties, and/or using substances while engaging in activities that increase the risk, such as driving.Reference 62 This section summarizes the use, harms, and costs associated with alcohol, cannabis, and opioids.
What is stigma?
Stigma refers to the negative attitudes (prejudice), beliefs (stereotypes) or behaviours (discrimination) that devalue another person.Reference 4 Reference 10 There are many levels of stigma and discrimination, ranging from the personal to the societal. Negative judgements based on one's sexual orientation, race/ethnicity, or disability status, can interplay to create multiple layers of stigma. This can lead to additional social and health challenges for some.
At the personal level, stigma can be internalized, which may reduce a person's confidence and hope for the future.Reference 4 Reference 10 It can make people believe they are less worthy of respect, which can, in turn, impact their relationships, ability to get a job, find housing, and may make them less likely to seek help.Reference 10 Communities can also stigmatize people by poorly treating those perceived as different.Reference 18 From a societal perspective, institutional stigma can restrict a person's opportunities, such as access to training and employment, through restrictive policies, guidelines, or workplace culture.Reference 19
Those who live with mental health challenges or use substances often experience stigmatization. Reference 18 Reference 20 Reference 21 Also, those who experience discrimination may go on to adopt harmful use of substances as a coping strategy.Reference 18
Alcohol
Alcohol is a legal, socially acceptable, mind-altering substance that enjoys enormous popularity. However, its problematic use can lead to significant health and social harms.Reference 63 In 2016, the use of alcohol was the leading cause of premature death and disability worldwide, among people aged 15-49 years. Twelve percent of deaths for men in this age group was attributed to alcohol use.Reference 64 Although Canada’s Low-Risk Alcohol Drinking Guidelines for short and long-term risks (see Appendix 3) were introduced in 2011, about 12% and 15% of Canadians exceed these guidelines for short and long-term risks, respectively.Reference 28
Use
Alcohol is the most commonly used psychoactive substance in Canada. Almost 80% of Canadians 15 years and older report drinking alcohol during the past year (see Table 1a).Reference 28 One indicator of problematic alcohol use is heavy drinking (men having 5 or more drinks or women having 4 or more drinks on one occasion at least once a month in the past year), which has been reported by about 20% of Canadians 12 years and over.Reference 29 Rates of heavy drinking have steadily increased from 14% in 1996 to 20% in 2013, and have remained stable since.Reference 29 Reference 65
Certain populations drink more heavily than others. For example, the proportion of males aged 12 years and over who are heavy drinkers is higher than that of females in the same age group (24% versus 15%, respectively).Reference 29 Furthermore, about 30% of bisexual and almost 25% of lesbian women report heavy drinking compared to nearly 15% of heterosexual women.Reference 25 Heavy drinking is reported by about 30% of First Nations living off-reserve, Métis, and Inuit adults, compared to about 20% for non-Indigenous adults.Reference 25 According to the national First Nations Regional Health Survey, about 35% of First Nations adults (18 years and over) on-reserve report heavy drinking.Reference 66
Harms
In 2015, over 3,000 Canadians died of conditions attributed to alcohol.Reference 67 The alcohol-attributed death rate for women increased by 26% from 2001 to 2017, compared with a roughly 5% increase over the same period for men.Reference 67 In 2016/2017, about 80,000 hospitalizations in Canada were due to conditions entirely caused by alcohol.Reference 67 This is higher than the number of hospitalizations for acute myocardial infarctions (heart attacks).Reference 67 Alcohol is the most common substance used by Canadians who visited publicly-funded substance use treatment centres.Reference 68
In 2017, there were over 65,000 incidents of alcohol-impaired driving.Reference 69 While close to 40% of deaths from motor vehicle crashes are alcohol-relatedReference 70, the rate of alcohol-impaired driving incidents has declined by 26% over the last 10 years.Reference 69
In addition to the direct harms of poisoning, diseases and injuries, problematic use of alcohol is strongly associated with family conflict, intimate partner violence, child abuse and neglect, and violent crimes, including sexual assaultReference 71.
Lastly, drinking alcohol during pregnancy can also lead to serious harms to both mother and fetus. It is estimated that about 10% of women in general population of Canada consume alcohol during pregnancyReference 71. Fetal Alcohol Spectrum Disorder (FASD) is one of the most disabling potential outcomes of prenatal alcohol exposure. A recent study provided the first population-based estimate of the prevalence of FASD among elementary school children in Canada, which ranges between 2% and 3%Reference 220. Some special sub-populations may be at an increased risk for FASD, compared to the general population, such as children in care, correctional, special education, specialized clinical, and Indigenous populationsReference 221.
The alcohol harm paradox
Canadians with the lowest incomes report less heavy drinking but are more than twice as likely to be hospitalized for conditions attributed to alcohol, compared to Canadians with the highest incomes.Reference 8 Possible reasons for this may be higher stress levels, limited social supports, fewer resources to cope, poorer diet, and higher levels of physical inactivity among low versus high income Canadians.Reference 15
Cannabis
The Government of Canada introduced the Cannabis Act in October 2018 to legalize, strictly regulate, and restrict access to cannabis for non-medical purposes to better protect the health and safety of Canadians, in particular Canadian youth, and to remove profits from criminals and organized crime. This new policy for Canada takes a public health approach by aiming to reduce health risks from cannabis, and in particular, harms to vulnerable populations such as youth under the age of 18 years. The Act also has several additional public safety objectives which are beyond the scope of this report. Restrictions set out in the Cannabis Act for the legal production, distribution, retail sale and possession of cannabis aim to better protect youth by restricting their access to cannabis while making available a quality-controlled supply to adults. Also the legal framework provides public education and awareness of health risks to ensure Canadians have the information they need to make informed decisions about cannabis use. The Lower-Risk Cannabis Use Guidelines for Canada provide evidence-based recommendations to enable people to reduce associated health risks (see Appendix 3).
Use
Among Canadians, cannabis is the most commonly used substance after alcohol, with 12% of individuals 15 years and older reporting using it in the past year (see Table 1b).Reference 28 Reference 73 This rate has more than doubled since 1985, when it was about 6%.Reference 28 Reference 74 Use is more common among males (15%) compared to females (10%).Reference 28 Three percent of Canadians report daily or almost daily cannabis use in the past 3 months (defined as problematic).Reference 28
Although national level data by socioeconomic status are limited, some studies indicate that cannabis use is higher among urban versus rural Canadians.Reference 75 Use is also more common among certain Indigenous populations. According to the First Nations Regional Health Survey, 30% of First Nations on-reserve adults (18 years and over) used cannabis in the past year and 12% used it daily or almost daily.Reference 66
| Alcohol | Percent | Population size |
|---|---|---|
| Past year use | 77% | 22.7 M |
| Heavy drinking (12 years +)Reference 29 | 20% | 6.0 M |
| Cannabis | Percent | Population size |
|---|---|---|
| Past year use | 12% | 3.6 M |
| Daily or almost daily use (past 3 months) | 3% | 840,000 |
Harms
Although there is more to learn about long-term effects, the public health burden of cannabis use is currently less than that of alcohol and other substances like tobacco and opioids. The main contributors to cannabis-related health burden in Canada are motor vehicle crashes and substance use disorders.Reference 76 Close to 10% of adults who have ever used cannabis will develop a substance use disorder. This statistic increases for those who started using cannabis at an early age, and those who use cannabis frequently.Reference 77 Reference 78There is an increased risk of developing some types of testicular cancers for cannabis users. This risk increases for those who use cannabis frequently and for those who use it for more than 10 years.Reference 79 Although relatively uncommon, excessive and early initiation of cannabis use can increase the risk of developing schizophrenia and other types of psychoses, particularly if there is a family history involved.Reference 77 Additionally, for those who use cannabis frequently, there is a higher risk of developing a mood and anxiety disorder, as well as attempting suicide.Reference 80
In Canada, there are presently no explicit measures of cannabis use and harms during pregnancy and breastfeeding, although surveys exploring this association are underway. According to a recent systematic review on prenatal exposure to cannabis, pregnant women who use cannabis are more likely to have anemia during pregnancy and infants are more likely to be placed in the neonatal intensive care unit.Reference 81 Evidence also shows that inattention and impulsivity at 10 years of age are linked to prenatal exposure. Other poor outcomes include deficits in problem-solving skills, errors of omission and academic underachievement (particularly in reading and spelling), showing that prenatal cannabis exposure affects the ability to maintain attention.Reference 82 Reference 83
Opioids
Canada is experiencing a growing epidemic of opioid-related deaths and harms. Nearly 4,000 Canadians lost their lives to opioid overdoses in 2017 alone.Reference 84 This is equivalent to 11 Canadians dying each day. Nationally, the majority of these deaths to date have occurred among men, and individuals between the ages of 20 and 59; however, national data can sometimes mask local or regional trends.Reference 84 The opioid crisis is rapidly evolving across Canada. While historically the greatest burden of opioid deaths has been observed in Western Canada, particularly in BC and Alberta (AB), other parts of the country are also experiencing recent increases (see Figure 5).Reference 84 Reference 85
The causes of this crisis are complex and include the interplay of the excessive availability of prescription opioids and increased availability of non-prescription (illegal) opioids. First, increased prescribing of opioids is one of the drivers of opioid overdose deaths.Reference 85 Between 1980 and 2015, opioid consumption increased by a factor of 40 in Canada, from 21 to 853 morphine equivalents per person in the population.Reference 86 In 2016, over 20 million prescriptions for opioids were dispensed in Canada – the equivalent to nearly one prescription for every adult over the age of 18 years. This makes Canada the second-largest consumer of prescription opioids in the world, after the United States.Reference 85 Trends also show an increase in the prescription of more potent opioids in recent years. While the proportion of weaker opioid prescriptions (e.g., codeine) decreased between 2012 and 2016, the proportion of stronger opioid prescriptions (e.g., oxycodone, hydromorphone, and morphine) increased from 52% to 57% over the same period.Reference 87 Although relatively modest on the surface, this shift is concerning given the increased risk of harmful outcomes associated with strong opioids.Reference 87
Secondly, sharp rises in opioid-related deaths in the last few years, in parts of Canada, are believed to be mainly driven by the availability of illegal fentanyl, as rates in the legal medical dispensing of fentanyl have remained relatively stable across the country.Reference 85 Reference 87 Reference 88 Fentanyl-related overdose deaths were first reported in BC and AB in 2011.Reference 85 Since then, there has been a sharp increase in both the number and percent of fentanyl-related deaths detected in the West, with more recent rises in jurisdictions like Ontario. Reference 84 Reference 88 In 2012, 4% and 11% of opioid overdose deaths in BC and AB were fentanyl-related; by 2017, this figure climbed to 84% and 79%, respectively.Reference 84 Reference 88 Close to 70% of opioid-related deaths in Ontario (2017) involved fentanyl, compared to 24% in 2012.Reference 84 Reference 88 Additionally, highly toxic synthetic opioids are becoming more pervasive. Carfentanil – 100 times more toxic than fentanyl – has now been detected in overdose deaths in several provinces.Reference 85 More research is needed to understand the sources of illegal fentanyl products in different parts of Canada as these sources are not well understood.
Another factor likely influencing the current epidemic is the lack of awareness among Canadians of the risks associated with both illegal and prescription opioids. A 2017 survey on opioid awareness revealed that about 70% of Canadians were “very aware” that substances obtained illegally or on the street have the potential to contain fentanyl. However, almost 15% were “not at all aware” of the that risk.Reference 89 In addition, only 28% of Canadians said that they would recognize the signs of an overdose, while only about 10% said they would know how to both obtain and administer naloxone, a medication that blocks or reverses the effects of an opioid overdose.Reference 89
Figure 5: Number and rate (per 100,000 population) of apparent opioids-related deaths by province or territory, Canada, 2017Reference 84

Source: Apparent opioid-related deaths in Canada (June 2018)
Text Description
| Province or territory | Number of deaths in 2017 | Rate per 100,000 population |
|---|---|---|
| British ColumbiaFigure 5 Footnote a | 1470 | 30.5 |
| Alberta | 759 | 17.7 |
| SaskatchewanFigure 5 Footnote b | 46 | 4.0 |
| Manitoba | 122 | 9.1 |
| Ontario | 1263 | 8.9 |
| QuebecFigure 5 Footnote c | 181 | 2.2 |
| New Brunswick | 37 | 4.9 |
| Nova Scotia | 65 | 6.8 |
| Prince Edward IslandFigure 5 Footnote b | 3 | 2.0 |
| Newfoundland and LabradorFigure 5 Footnote b | 33 | 6.2 |
| YukonFigure 5 Footnote b | 7 | 18.2 |
| Northwest Territories | 1 | 2.2 |
| Nunavut | Suppressed | Suppressed |
|
||
Use
Data on the impacts of opioids on affected populations are emerging. For example, there are limited data on non-medical use of opioids and limited data as to which populations are most affected, including information on socioeconomic and common risk factors. A national study on opioid- and drug-related overdose deaths, led by the PHAC, is expected to contribute to our understanding of the drivers, causes, and determinants of the epidemic of opioid overdose deaths across Canada, and pinpoint where we need to focus additional research.Reference 6
In 2015, 0.3% of Canadians self-reported using prescribed opioid pain relievers for reasons other than for the prescribed therapeutic purposes.Reference 28 A more recent online survey from Health Canada in 2017 found that nearly 33% of Canadians who reported using opioids in the past year did not always have a prescription.Reference 85
Harms
A common thread across the country is that combined use of multiple substances has been involved in a majority of opioid overdose deaths. National data show that more than 70% of these deaths also involved one or more types of non-opioid substances such as alcohol, benzodiazepines, cocaine or methamphetamines.Reference 84 Confirmed deaths in AB (2017) indicated that 80% of fentanyl overdose deaths involved other substances as well.Reference 84
The opioid overdose crisis has touched all parts of the country and all sectors of society; nevertheless, available data highlight a disproportionate burden on certain populations. Emerging evidence from several provinces indicates that individuals living in poverty, First Nations people, and those who experience unstable housing are disproportionally affected by opioid overdose deaths.Reference 9 Reference 90 Reference 91 Reference 92 Data from Ontario indicate that emergency room visits, hospitalizations, and deaths due to opioid overdoses increase with decreasing neighbourhood income.Reference 91 Data from BC show that First Nations people are 5 times more likely to experience an opioid overdose event and 3 times more likely to die from an overdose than non-First Nations people.Reference 90 While overdoses and overdose-related deaths occur more frequently among men in the general population, First Nations men and women in BC experience similar rates of opioid overdose events.Reference 90
Individuals who experience unstable housing are also at increased risk of opioid-related harms. In BC, data collected in emergency room visits found that approximately 30% of those presenting for a known or suspected illegal substance overdose also reported unstable housing.Reference 93
More research and surveillance is needed to better understand the populations most impacted by the opioid crisis and its drivers.
The Costs of Substance Use in Canada
Compared to other substances, alcohol use was responsible for the highest overall costs in Canada in 2014, at $14.6 billion for healthcare, lost productivity, criminal justice costs and other factors (see Figure 6). This was followed by costs related to tobacco use, estimated to be $12.0 billion a year.Reference 94 Opioid use incurred the third highest costs at $3.5 billion dollars.Reference 94 As harms associated with opioid use have increased dramatically since 2015, the associated costs are also expected to rise substantially. Finally, cannabis use incurred the fourth highest costs at $2.8 billion, with over half associated with the criminal justice system. The cost segment related to criminal justice is expected to decrease following the full implementation of cannabis legalization policy.Reference 94
Figure 6: Overall costs (in billions) by substance and cost type, 2014Reference 94
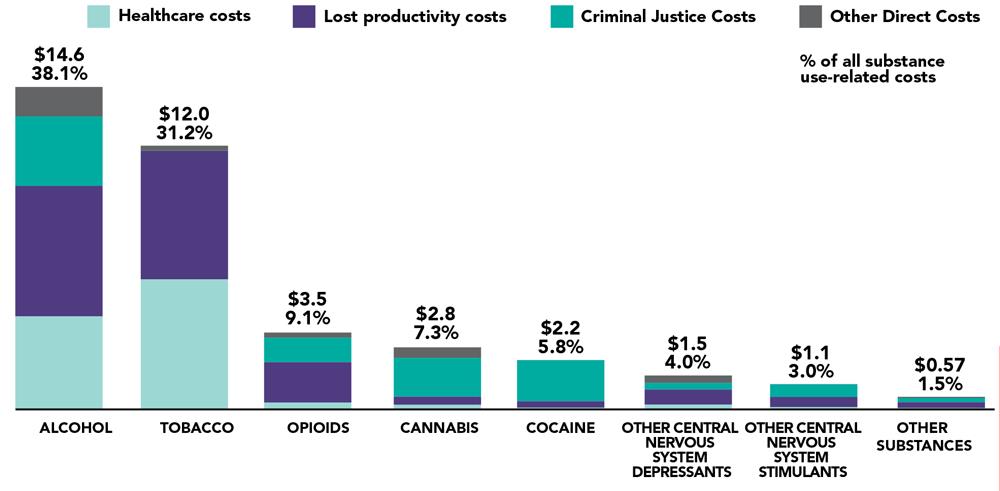
Source: Costs of Substance Use in Canada
Text Description
| Substance | Healthcare costs | Lost productivity costs | Criminal justice costs | Other direct costs | Total | % of all substance use-related costs |
|---|---|---|---|---|---|---|
| Alcohol | 4.2 | 5.9 | 3.2 | 1.3 | 14.6 | 38.1% |
| Tobacco | 5.9 | 5.8 | 0.0 | 0.2 | 12.0 | 31.2% |
| Opioids | 0.3 | 1.8 | 1.1 | 0.2 | 3.5 | 9.1% |
| Cannabis | 0.2 | 0.4 | 1.8 | 0.5 | 2.8 | 7.3% |
| Cocaine | 0.1 | 0.3 | 1.9 | 0.0 | 2.2 | 5.8% |
| Other Central Nervous System Depressants | 0.2 | 0.7 | 0.3 | 0.3 | 1.5 | 4.0% |
| Other Central Nervous System Stimulants | 0.1 | 0.5 | 0.6 | 0.0 | 1.1 | 3.0% |
| Other Substances | 0.07 | 0.26 | 0.19 | 0.05 | 0.57 | 1.5% |
Given the burden of tobacco use on society, it is evident that tobacco control efforts should be continued.Reference 94 Reference 95 While the rest of this report does not include an in-depth focus on tobacco, it refers to tobacco use and intervention efforts as examples of ways to successfully address a complex public health issue.
Chapter 2: Understanding Youth and Problematic Substance Use
Introduction
Adolescence and young adulthood are key life stages when lifelong behaviours often become established. Ongoing physical and social changes occur as the young brain grows, puberty ensues and future adult roles are developed. At the same time, young people are coping with new social relationships and an emerging independence that may present opportunities for risk taking.Reference 96 This evolution takes place within family, community and broader peer, social, and cultural contexts that can support or challenge positive youth development. During this time, many youth experiment with substance use, but some go on to do so in ways that are harmful to themselves and others. Understanding the circumstances that can lead youth to use substances in a problematic way is a crucial step in selecting supportive and effective prevention interventions.
Youth are not a single homogenous group and can vary according to gender, race, sexual identity, ability, cultural background, economic reality and personal identity. Current health and social services may not always meet the needs of those across the spectrum of diverse backgrounds.Reference 5
In Brief:
- Close to 25% of youth in grades 7 to 12 engage in high risk drinking behaviour.
- Opioid-related hospitalizations have been rapidly increasing in the past 5 years among young adults aged 15-24 years.
- The majority of youth who use substances indicate that they do so to feel good and to be sociable.
- A much smaller group say that substances can relieve stress and help them cope with negative situations. This group is more likely to experience negative health and social consequences.
- There is no single cause of problematic substance use among youth. It involves a complex interplay of factors such as the marketing of psychoactive substances, their availability, family and peer relationships, experiences of abuse and trauma, and social factors such as stable housing and family income that can lead one towards – or protect one from – the problematic use of substances.
Youth Substance Use and Potential Harms
The earlier in life that one starts using substances and the more heavy or frequent their use, the higher the risk for problematic substance use and harms later in life.Reference 97 Focusing efforts early on can therefore help to reduce potential risky behaviours and long-term negative health effects.Reference 98
Alcohol
Use
Underage drinking is common in Canada. More than 40% of students in grades 7 to 12 reported consuming an alcoholic beverage in the past 12 months (see Table 2).Reference 99 On average, students tried drinking alcohol for the first time at 13 years of age.Reference 99 Almost 25% of students exhibited high risk drinking behaviour (5 or more drinks on a single occasion). Reference 99 Data available on heavy drinking among adolescents show that national rates increase with income. At the same time, certain sub-populations report varying rates of heavy drinking – for example, Indigenous youth living off-reserve report more frequent heavy drinking than non-Indigenous youth.Reference 25 Thirty-three percent of Métis youth (12-19 years) report heavy drinking in the past month in BCReference 100, while 10% of First Nations youth (12-17 years) living on-reserve report heavy drinking.Reference 66
| Alcohol | Percent or years | Population size |
|---|---|---|
| Past year use | 44% | 859,000 |
| High risk drinking behaviour (i.e. 5 or more drinks on a single occasion) in the past year | 24% | 487,000 |
| Average age of initiation | 13 years | N/A |
Harms
Excessive and risky drinking can impact youth in many ways. Some direct harms associated with alcohol over-consumption include injury, memory loss, sexual coercion and assaults, suicide and other forms of self-harm, alcohol toxicity and motor vehicle crashes. Long-term harms include substance use disorders, learning and memory issues, problems with school performance, increased risk of school dropout, and increased risk for certain chronic diseases. Reference 71 Reference 101 Reference 102 Reference 103 Among youth 10-19 years, girls experience much higher rates of alcohol-related hospitalization than boys, although the reasons for this are not well understood.Reference 8 Given social norms in Canadian society, there appears to be a general lack of perception, among youth, of harms due to alcohol.
Cannabis
Use
Almost 20% of students in grades 7 to 12 reported using cannabis in the past year (2016/2017) (see Table 3).Reference 99 On average, students first used cannabis at 14 years of age.Reference 99 The large majority of the students (80%) who used cannabis reported smoking itReference 99, which can cause respiratory harms.Reference 77 Other methods for consuming cannabis include edibles, vaping, and dabbing – vaporizing concentrated cannabis by placing it on an extremely hot metal object and inhaling the vapours produced.Reference 99 Some youth are more likely to use cannabis than others. For example, according to the First Nations Regional Health Survey, almost 30% of First Nations on-reserve youth (12-17 years) used cannabis in the past year and some 66% of Inuit youth (15-19 years) from a study in Nunavik reported using cannabis in the past year.Reference 66 Reference 104 Furthermore, about 40% of Métis youth (12-19 years) report having tried cannabis in the past year.Reference 100
| Cannabis | Percent or years | Population size |
|---|---|---|
| Past year use | 17% | 340,000 |
| Average age of initiation | 14 years | N/A |
| Smoke cannabis (among students who had reported ever using cannabis) | 80% | 340,000 |
| Perceive that smoking cannabis on a regular basis puts people at “great risk” of harm | 54% | 1.1M |
Canadian youth are more likely to use cannabis than adults. While rates of past year cannabis use among adolescents (about 20% of 15-19 years) and young adults (about 30% of 20-24 years) have remained unchanged between 2013 and 2015, they are still higher than the 10% rate in adults over the age of 25 years.Reference 28 Sustained weekly or more frequent cannabis use in teenagers can increase the risk for substance use disorder or mental health problems later in life.Reference 105 In 2015, about 5.1 % of youth 15-24 years reported using cannabis daily or almost daily in the past 3 months, 4.6 % used it weekly and 3.5% used it monthly.Reference 106
Harms and Risk Perception
The younger a person starts using cannabis, the greater the likelihood of them developing health problems.Reference 77 Reference 97 Initiating cannabis use at a young age – primarily before the age of 16 – and frequent use of cannabis can increase the risk for substance use disorder and psychosis. Reference 77 Reference 97 While more research is needed in this area, daily cannabis use over many years that begins in adolescence has been associated with impairments of memory, attention, and learning.Reference 107 Reference 108
In the context of legalization, the perception of risks associated with cannabis is important to monitor over time, especially among youth. When students in grades 7 to 12 were asked if they thought smoking cannabis once in a while could be harmful, about 20% responded that this could put people at “great risk” of harming themselves, and about the same percentage said that it posed “no risk”.Reference 99 When the same group was asked if they thought that smoking cannabis regularly could be harmful, only just over 50% responded that this could put people at “great risk”, while close to 10% said it posed “no risk” of harms.Reference 99
Opioids
Use
Three percent of students in grades 7 to 12 report using prescribed opioids (this includes opioids prescribed to the survey respondent or taken from a family member or friend) for non-medical reasons (e.g., to get high) in the past year (2016/2017), including 1% and 0.5% who reported using oxycodone and fentanyl to get high, respectively (see Table 4).Reference 99 Some youth are particularly vulnerable to problematic opioid use. In one recent study of young adults (16–25 years) who had used opioids in the last 3 months, LGBT youth were nearly twice as likely to use opioids intensively (i.e., longest duration and most consistent harmful use of opioids).Reference 109
| Prescription Opioids | Percent | Population Size |
|---|---|---|
| Use of pain relievers to get high in the past year | 3% | 61,000 |
| Use of oxycodone to get high in the past year | 1% | 24,000 |
| Use of fentanyl to get high in the past year | 0.5% | 10,000 |
Harms
Between 2010-2015 in Ontario, the most substantial increase in opioid-related deaths occurred among those aged 15-24 years.Reference 110 About 10% of all deaths among young adults aged 15-24 years in Ontario were opioid-related, a rate that has nearly doubled in the last 5 years. Reference 110 While these mortality trends may be unique to Ontario, pan-Canadian hospitalization data mirror these findings, showing that the age group of 15-24 years experienced the fastest-growing rates of hospitalizations related to opioid overdoses between 2007-2008 and 2015-2016.Reference 111 During the same period, over 50% of opioid overdoses among youth that led to hospitalization were intentional, or overdoses that occurred as a result of self-inflicted harm. Reference 112 The reasons for this are not well understood – in order to inform prevention efforts, public health officials need better evidence on the reasons why youth use opioids, as well as on the source of the opioids they obtain.
Reasons Why Youth Use Substances
Youth report a range of reasons to explain why they use substances. The most common reasons in relation to cannabis and alcohol are “having fun” and “being social”.Reference 113 Reference 114 A smaller group report using substances to deal with stress or emotional pain. This group is at greater risk of problematic substance use.Reference 115
Because it is fun and social
Youth most often report that “having fun” and celebrating are the main reasons for drinking alcohol.Reference 113 Reference 114 Students said that they drank alcohol mainly because they enjoy the taste and it is a part of being sociable with their friends.Reference 116 These reasons are similar for why youth report using cannabis, which is “to experiment” and “to be social”. For cannabis specifically, youth also report using it “to be more creative and original”.Reference 117
To deal with stress or emotional pain
A smaller number of young people use alcohol and cannabis to cope with stress. Students who reported poor mental health were more likely to also report using substances as a coping strategy or because they felt down or sad.Reference 115 Youth report using cannabis to cope because they feel depressed, want to reduce stress and anxiety, or want to escape reality or a negative situation.Reference 117 Reference 118 Another study showed that youth who used alcohol as a coping strategy were more likely to report difficulties from their alcohol use, such as fights, arguments with their friends or family members, or having problems with school.Reference 114 Similarly, youth who use cannabis as a coping strategy are also more likely to report problems such memory loss, lower productivity and difficulty sleeping.Reference 119 Lastly, some youth also use cannabis for relief of physical pain.Reference 115 Reference 118
Finally, although reasons for opioid use among youth are not yet fully understood, some have reported using these “to get high” or to self-medicate.Reference 99 Public health officials need more comprehensive surveillance data on the reasons why youth use opioids in order to better inform prevention efforts.Youth Risk and Protective Factors
A range of interacting risk and protective factors in a young person’s life either place them at greater risk of problematic substance use, or protect them from this risk. Reference 5 Reference 120 These factors are neither independent of each other nor are they simply a reflection of an individual’s personal characteristics. Instead, they are dynamic and span across the social contexts in which youth grow up. Reference 5 Reference 120
Figure 7 shows examples of risk and protective factors for problematic substance use in youth. The individual is nested within the influences of society at large as well as within their own family and community context. These factors are shaped through the life course, from the prenatal environment to adulthood. Some risk factors may be more powerful than others at certain stages of development, such as peer pressure during the teenage years. Equally, some protective factors, such as a strong parent-child bond, can have a greater impact on reducing risks during the early years and build resilience. This, in turn, can influence many health and socioeconomic outcomes in childhood and later life.Reference 120 An important goal of prevention is to shift the balance in favour of protective factors over risk factors (see Table 5).
Figure 7: Examples of risk and protective factors associated with problematic substance use in youth

Text Description
This figure depicts a model of various levels of risk and protective factors at the individual, interpersonal, community, and societal/structural levels.
- The individual level includes such factors as resilience, mental health status, and genetics.
- The interpersonal level includes such factors as early childhood development, physical and sexual abuse and other types of violence, and family member with problematic substance use.
- The community level includes such factors as school connectedness and environment, social and community connectedness, availability of and access to health and social services, and availability of and access to substances.
- The societal/structural level includes such factors as marketing practices and social norms, colonization and intergenerational trauma, stigma and discrimination, and income and housing policies.
At the broader societal level in Canada, inequalities related to the determinants of health – in particular, poverty and access to safe and affordable housing – are linked to increased risk of problematic substance use among youth.
At the same time, certain youth populations also face their own unique determinants. The historical and ongoing effects of colonization for First Nations, Inuit and Métis communities reflect intergenerational trauma in the lives of many Indigenous youth and the consequences these legacies have on the eradication of culture, traditional values, and the loss of traditional family stability.Reference 13 These risk factors for Indigenous communities are countered by such protective factors as cultural continuity, which has been associated with reduced suicide rates among First Nations youth in BC.Reference 121 Reference 122 Research shows that connection to land, cultural ceremonies, and healing traditions can reduce the risk of problematic substance use among Indigenous youth by linking them to the knowledge and skills that help them attain meaningful connections around family, spirituality, and identity.Reference 123
Risk and protective factors for harmful use of substances are not distributed equally among all youth. Other specific groups who are at higher risk than their peers include homeless or street-involved youth; youth in custody; youth living with co-occurring mental health problems; youth with a history of trauma; as well as gay, lesbian, bisexual, transgender and questioning youth.Reference 5 Common risk factors among these populations include a history of trauma; exposure to sexual and physical abuse or other types of violence; experiences of stigma and discrimination (including racism, heterosexism, and transphobia); and resulting mental health issues.Reference 5
Some risk factors speak to individual and interpersonal differences – for example, youth who have a family history of substance use and/or a mental illness are also at greater risk of using substances in a harmful manner.
There is growing evidence that protective factors in the lives of even the most vulnerable young person can buffer risk and boost resilience. Connectedness to school, positive relationships with caring adults inside and outside the family, supportive peers, as well as school and community safety, can all enhance an individual’s ability to cope with everyday responsibilities and reduce the likelihood of difficulties that lead to problematic substance use.Reference 120
| Risk and Protective Factors | Association with Problematic Substance Use |
|---|---|
Marketing practices and social norms |
Research shows that exposure to alcohol and tobacco marketing increases the probability of using these substances.Reference 124 Reference 125 Marketing can shape social norms by portraying substances in a positive light and targeting concepts such as social approval, autonomy, self-image and adventure seeking. Reference 124 Popular media also perpetuate the use of both legal and illegal substances.Reference 126 Reference 127 A 2010 scientific review identified that increased non-advertisement media exposure (i.e., television, music and film) was significantly associated with smoking initiation, use of illegal substances and alcohol consumption among children and adolescents.Reference 128 |
Colonization and intergenerational trauma |
The historical and ongoing effects of colonization and the residential school system in Canada continue to impact First Nations, Inuit and Métis communities, across several generations. The latest First Nations Regional Health Survey found higher rates of problematic substance use (i.e., heavy drinking) among First Nations youth who had at least one parent who attended a residential school, when compared to non-First Nations youth.Reference 90 |
Stigma and discrimination |
Experiencing stigma or discrimination based on race/ethnicity, Indigenous identity, mental health status, disability, and/or LGBTQ2 status can heighten the risk of harmful use of substances for certain groups of youth. Reference 5 Reference 129 The resulting intersecting layers of stigma and discrimination can, in turn, perpetuate a cycle of problematic substance use. Reference 129 In addition to public stigma that perpetuates negative language and stereotypes that may lead to social exclusion, restricted opportunities, and diminished self-efficacy among people who use substances, institutional stigma can lead to significant barriers in accessing health care, housing, and employment.Reference 4 Reference 19 As people who use substances internalize public and institutional stigma, they may experience loss of confidence, as well as feelings of embarrassment and shame, discouraging them from seeking help for their disorder.Reference 18 |
Income and housing policies |
Poverty among families with children is associated with substance use later in life, although the pathway may not always be direct. For example, children from low-income families are more likely to go to school hungry. This, in turn, affects their ability to learn and to perform in school – which is associated with increased harmful use of substances.Reference 130 Reference 131 Children from low-income families are also less likely to experience such long-term protective factors as daily reading, parental time, involvement in school based activities, and time and/or money for recreational activities. Reference 130 Reference 131 Reference 132 Reference 133 Reference 134 Living in low-income and disadvantaged neighbourhoods is also linked to higher levels of exposure to illegal substances, substance use and poisonings.Reference 135 Reference 136 Access to safe, stable housing is another important predictor, as those lacking it will often turn to substances as a coping strategy.Reference 137 Youth facing housing insecurity are at a greater risk of engaging in harmful use of substances.Reference 131 Indeed, homeless or street-involved youth experience elevated health and social challenges, and homelessness is a strong determinant of substance use initiation among youth (even after adjustment for various socio-demographic factors).Reference 138 Certain populations also experience higher rates of housing need than others. First Nations people living off reserve, Métis, and Inuit experience housing below standards – homes considered unsuitable, inadequate or unaffordable – at a greater rate than the non-Indigenous population. In Canada, in 2011, about 50% of First Nations people living off reserve and Inuit, and 40% of Métis lived in housing below standards.Reference 25 |
| Risk and Protective Factors | Association with Problematic Substance Use |
|---|---|
School connectedness and environment |
School connectedness refers to the extent to which students perceive that they are accepted, respected, included, and supported by others in the educational environment.Reference 139 Reference 140 Reference 141 These connections protect youth from many health risks, including early initiation of smoking and alcohol use. Reference 139 Reference 140 This is closely related to the concept of positive school environment, which has a demonstrated protective effect against problematic substance use and is associated with lower rates of alcohol and cannabis use among adolescents.Reference 142 Over 60% of Canadian students in grades 6 to 10 reported feeling a sense of belonging at school.Reference 143 |
Social and community connectedness |
The caring and respect engendered by positive social relationships, and the resulting sense of satisfaction and well-being, serve as a buffer against many health issues. The more that youth engage with their communities, the less likely they are to participate in risky behaviours with their peers. Instead, they have greater opportunities to develop independence, confidence and good decision-making, while broadening their social networks to include more peers who model and encourage positive behaviours.Reference 144 Structured community activities can also expose youth to positive mentors and serve as a source of emotional support.Reference 144 Community involvement also increases youths’ sense of competence as they succeed in non-academic pursuits, which may positively influence subsequent attitudes, goals, and other means of contributing to society. Reference 144 Neighbourhood disorganization is associated with problematic substance use.Reference 145 Risk factors associated with disorganized neighbourhoods (e.g., increased crime, limited access to safe outdoor areas, vandalism, and publicly visible substance use) may create an environment that limits protective factors (e.g., access to safe recreational and social spaces, and school- or community-based organizations that offer the opportunity to build caring relationships with adults outside the home). Reference 146 In 2013/2014, about 60% of grades 6 to 10 students reported that they can trust people where they live.Reference 143 Ninety percent of 15–17 year olds reported that their neighbourhood is a place where neighbours help each other.Reference 143 Moreover, about 6% of 15–17 year olds reported that social disorder in their neighbourhood is “a very big problem” or “a fairly big problem”.Reference 143 |
Availability of and access to health and social services |
Youth living with poor mental health are more likely to engage in harmful use of substances than those who are not – early intervention following the first episode of a serious mental illness can lead to positive health outcomes later in life.Reference 146 Fewer than 25% of Canadian children with a mental health disorder receive specialized treatment services.Reference 147 Mental health and other health care practitioners can play a key role in identifying youth who may need support and those who already experience substance use issues by screening, providing brief interventions and, if needed, referring them to substance use treatment programs and ongoing monitoring and follow-up.Reference 146 Several screening tools are available to practitioners.Reference 148 |
Availability of and access to substances |
Substance use increases among youth who have high availability and easy access to them. Substances can become more available through the community (e.g., density of retail locations and low cost), family (e.g., readily found in the home and/or a low level of parental monitoring), peers, and the health care system (e.g., physician prescribing practices). Close to 70% of Canadian students in grades 7 to 12 report that it is fairly easy or very easy to access alcohol, followed by cannabis (39%) and prescription pain relievers (25%).Reference 99 |
| Risk and Protective Factors | Association with Problematic Substance Use |
|---|---|
Early childhood development |
Negative experiences in a child’s life can lead to future poor health (e.g., obesity, cardiovascular disease, and diabetes), poorer educational attainment, economic dependency, and greater risk of problematic substance use and depression.Reference 149 Reference 150 The Early Development Instrument measures school readiness – a demonstrated predictor for substance use later on in life. In Canada, more than 25% of childrenReference 151 are vulnerable in at least one of the 5 areas of development prior to entering grade 1: physical health and well-being, social competence, language and thinking skills, communication skills and general knowledge, and understanding and managing emotions. |
Physical and sexual abuse and other types of violence |
The connection between physical abuse, sexual abuse, and other types of violence with substance use later on in life has been well-established.Reference 152 Reference 153 Abuse can disrupt early development by impeding a child’s ability to cope and by contributing to cognitive impairment. Over time, harmful use of substances may result as a coping mechanism.Reference 153 A nationally representative Canadian survey from 2012 found that those who self-reported physical abuse, sexual abuse, or exposure to intimate partner violence before the age of 16 years were about 3.5 times more likely to report problematic substance use compared to those who did not (even after adjustment for various socio-demographic variables, such as age, sex, education, and income).Reference 152 The severity of child abuse also plays a role in substance use risk. Canadians who have been exposed to all 3 forms of violence (referenced above) are almost 11 times more likely to report a substance use disorder than those not exposed to any abuse. Reference 152 A third of Canadians over the age of 15 (33%) report experiencing at least one of these 3 types of child abuse before the age of 15 years.Reference 154 |
Family member with problematic substance use |
Substance use in the family increases the likelihood that youth have direct exposure and access to substances. Harmful use disrupts routines and social support, contributing to stressful family environments. Reference 155 Reference 156 Negative parental or sibling modeling of behaviors and attitudes regarding substance use is a risk factor for youth.Reference 156 For instance, maternal smoking, alcohol use, and illegal substance use have been linked to cannabis and other substance use disorders in young adults.Reference 157 Moreover, children who experience both maltreatment and dysfunction in a family setting have the highest risk for mental health issues in adulthood.Reference 153 In 2012, nearly 30% of Canadian students (15–17 years) reported having a family member who had problems with their emotions, mental health or use of substances and over 25% said that they were affected “a lot” or “some” by this situation.Reference 143 |
| Risk and Protective Factors | Association with Problematic Substance Use |
|---|---|
Resilience |
Resilience is commonly recognized as a protective factor against problematic substance use among youth. While lacking a universal definition, it is often described as the ability to transform stressful events and/or adversity into opportunities for learning. Reference 158 Reference 159 Resilience includes a dynamic interplay of individual resources (e.g., problem solving skills, confidence, coping skills), relational resources (e.g., relationships with primary caregivers, parents, mentors, teachers) and contextual resources (e.g., community and culture) that help young people cope with challenging situations. Reference 159 Reference 160 There are various ways to measure resilience and no single national indicator is currently used. However, national level data from 2012 (based on proxy measures) show that only 45% of 12-17 year olds reported a high level of perceived control over life changes, while over 40% reported having the skills necessary to cope with everyday responsibilities.Reference 143 |
Mental health status |
Elements of positive mental health, such as living in a stable and nurturing home, attachment to family and school, and living in a safe, supportive neighbourhood have long been shown to protect against problematic substance use among youth.Reference 161 On the other hand, poor mental health and mental illness are well-established risk factors for influencing the harmful use of substances.Reference 77 Youth living with mental illness may use substances as a way to manage or cope.Reference 5 Reference 162 Moreover, youth who use substances frequently and/or at an early age are at greater risk of developing substance use disorders. The co-occurrence of problematic substance use and mental illness and disorders (particularly anxiety and depression) can generate a cycle of poor outcomes, including a high relapse rate if the disorders are not treated at the same time as the mental illness. Reference 161 |
Genetics |
Interactions between genes and the environment may in part explain protective factors (e.g., parental attachment) or risk factors (e.g., childhood trauma, unstable housing, or poverty) that influence substance use early in life.Reference 163 Reference 164 Reference 165 Reference 166 No single gene predisposes one to substance use. Rather a multitude of genes interact with each other and their environments, making individuals more or less susceptible to substance use disorders.Reference 163 Reference 164 Evidence indicates that such disorders can run in families.Reference 157 Reference 167 Their potential to be inherited varies among substances. More addictive ones (such as opiates) are more likely to be passed down through families.Reference 163 |
Chapter 3: Interventions for Preventing Problematic Substance Use in Youth
Introduction
Preventing or reducing problematic substance use among youth in Canada can only be achieved through a range of coordinated actions that serve to promote wellness, reduce risks and harms, strengthen protective factors, and improve access to quality mental health and support services. Any measures implemented must be culturally safe for all youth and not stigmatize those who use substances. This section outlines the principles and components of a comprehensive and equitable approach to prevention. Intervening early to counteract the risk factors of problematic use offers the best chance of having a positive influence on a young person's development and reducing long-term harms to them and to society as a whole.Reference 5
In Brief:
- Actions guided by core principles – trauma-informed, equitable and safe for diverse populations, and youth and community driven – will ensure that policies and programs recognize the diverse needs of youth.
- A range of actions to promote wellness, reduce risks and harms, and improve access to quality mental health and support services are required.
- A comprehensive approach includes policies and programs that:
- Create equitable social and economic conditions
- Promote positive social norms, communicate risks and reduce access to and the availability of substances
- Build the skills and resilience of youth and their families
- Promote early intervention for youth who need support.
Principles to Inform Prevention Interventions
Actions guided by core principles – trauma-informed, equitable and safe for diverse populations, and youth- and community-driven – will ensure that public health policies, systems, programs, and services meet the needs of diverse groups of youth and that existing inequities are not perpetuated or intensified.
Trauma-informed
Many youth who go on to engage in harmful use of substances have previously experienced trauma. A trauma-informed lens incorporates an understanding of experiences of trauma into all aspects of an intervention.Reference 168 This is particularly important for programs and services working directly with youth, to ensure that those accessing the services feel safe and are able to benefit from the intervention. Trauma-informed services and systems avoid re-traumatizing individuals and support choice and control on the part of participating youth.Reference 168 Programs are designed to be inclusive, transparent, collaborative, and empowering.Reference 169 Reference 170
Equitable and safe for diverse populations
Prevention interventions should be equity-driven and culturally safe. This means designing interventions to meet the needs of diverse groups of youth, including those from socially and economically marginalized communities. It also means facilitating access to services and programs by eliminating stigmatizing practices and institutional barriers, such as racism and discrimination, which prevent marginalized youth from seeking help.Reference 18 Being equity-driven also means acknowledging that sex and gender shapes the experience of problematic substance use and that interventions should be designed and evaluated accordingly.Reference 171 Reference 172 Reference 173 This also offers opportunities to engage in gender-transformative programming, which aims to change negative gender stereotypes and norms and redress imbalances of power.Reference 174
Cultural safety is a fundamental principle for all public health practices, particularly in relation to those that support First Nations, Inuit, and Métis populations. It means ensuring that all interactions with, and initiatives for, Indigenous Peoples are based on humility, respect, cultural understanding, and equity.Reference 175 To implement this principle, institutions and organizations can institute policies and training on cultural safety for health professionals, schools, and social service organizations.
Youth and community driven
Community engagement – where community members serve as both a driver and an active participant in a process – is an essential component of equitable and responsive policies and initiatives. Communities may be defined geographically or socio-culturally (e.g., municipalities, Indigenous populations). A community may also be made up of people who share common experiences and vulnerabilities, such as LGBTQ2 youth or youth who use substances.
Community engagement can provide direction on how to design interventions that are appropriate for different populations and stimulate local action to address social inclusion and build community supports. Young people, and specifically those who use substances, can be engaged as collaborators on issues affecting their communities – effectively making them local peer leaders with an opportunity to influence program development and prevention campaigns.Reference 176 Reference 177 This would help ensure that initiatives are non-judgemental and that youth feel comfortable accessing them. Supporting First Nations, Inuit, and Métis communities to shape prevention efforts can strengthen cultural relevancy and facilitate community ownership.
A Public Health Approach to Prevention
A comprehensive public health approach to prevention considers two fundamental questions:
- Which broad interventions can have the most benefit to the greatest number of people?
- What kinds of interventions are needed to reduce health inequities?
The public health pyramid provides direction on where to implement different types of interventions (see Figure 8).Reference 178 Population-level efforts in the bottom half of the pyramid can potentially benefit more youth because they are aimed at reducing overall substance use, either at the societal level, community-level, or in smaller populations, such as schools. At the same time, because they are designed for broad populations, these initiatives can avoid stigmatizing individual groups of youth. More individual-focussed interventions found in the top half of the pyramid are important for meeting the needs of socially marginalized youth with diverse needs.
The public health community has learned from previous efforts that a comprehensive approach needs to address the population-level in order to achieve sufficiently broad results, while also prioritizing specific, more focussed individual-level interventions. For example, population-level policies have markedly decreased the overall number of youth who smoke. At the same time, rates of smoking have remained higher among certain populations, such as those of lower socioeconomic status and LGBTQ2 youth.Reference 179 Reference 180 To help reduce these disparities, the current renewal of the Federal Tobacco Control Strategy specifically targets higher rates of tobacco use in vulnerable populations.Reference 95
Figure 8: Public health interventions for the prevention of problematic substance use in youth
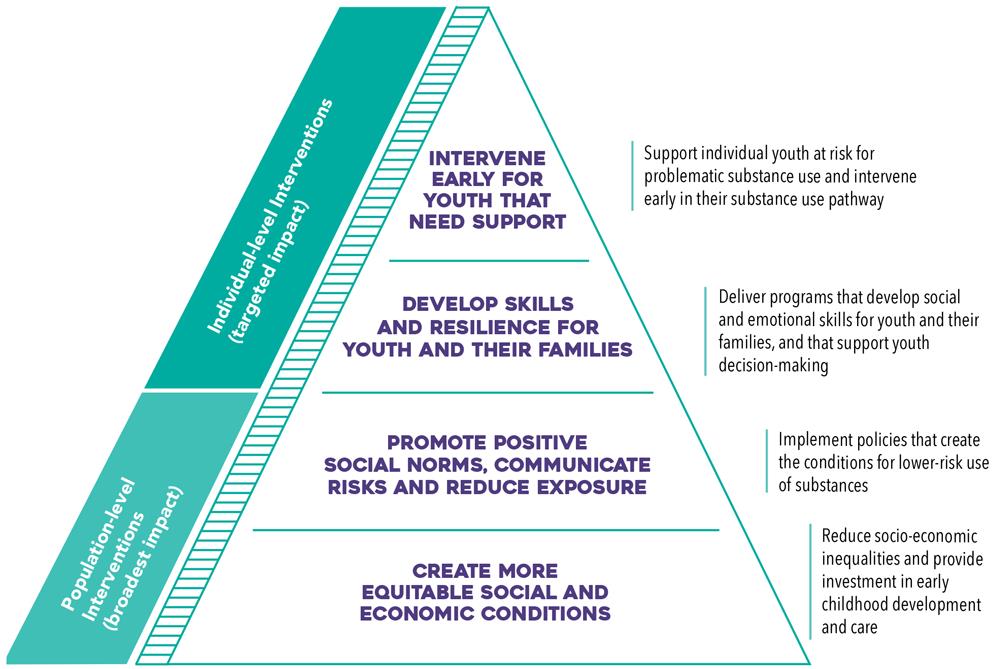
Text Description
This figure depicts a pyramid representing public health interventions for the prevention of problematic substance use in youth. There are 4 levels to the pyramid.
The interventions at the bottom half of the pyramid, also called population-level interventions, are those that have the broadest impact. They: (1) create more equitable social and economic conditions (i.e., reduce socio-economic inequalities and provide investment in early childhood development and care); and (2) promote positive social norms, communicate risks and reduce exposure (i.e., implement policies that create the conditions for lower-risk use of substances).
The interventions at the top half of the pyramid, also called individual-level interventions with a targeted impact. They: (3) develop skills and resilience for youth and their families (i.e., deliver programs that develop social and emotional skills for youth and their families, and that support youth decision-making); and (4) intervene early for youth that need support (i.e., support individual youth at risk for problematic substance use and intervene early in their substance use pathway).
Create more equitable social and economic conditions
Broad interventions that improve socio-economic conditions and early childhood development will improve overall community and individual health and resilience in a manner that reduces the risk of problematic substance use in the future. These types of interventions target the “causes of the causes” of societal health problems.Reference 181 While measuring outcomes directly related to problematic substance use can be challenging, interventions at this level promise to deliver the widest-reaching effects by easing every day economic and social stressors on families and youth. Fundamentally, this requires action to reduce childhood poverty and meet the core housing needs of families. Early childhood represents the greatest opportunity to positively influence health and well-being in the future.Reference 182 Reference 183 Quality early learning and child care from 0-6 years should be available to all children to ensure they benefit from the best possible start in life.
National initiatives are currently underway that aim to strengthen support to families and enhance early childhood development. Four of these initiatives and their potential impact on the prevention of problematic substance use are highlighted in Table 6, below. Moving forward, health and social sectors could consider measuring the health impact of these initiatives.
| Policy Initiative | Potential Impact on Problematic Substance Use |
|---|---|
Canada's Poverty Reduction Strategy Reference 184 |
This strategy aims to reduce poverty by 50% by 2030, while aligning with existing provincial and municipal poverty reduction strategies. It includes a plan to measure and publicly report on progress. Programs like the Canada Child Benefit and the Canada Workers Benefit help to ease poverty and support families living on low income by potentially:
|
Housing FirstReference 217 |
Housing First is an evidence-based approach to reducing homelessness that prioritizes people experiencing it. It is built on harm reduction principles where individuals are not expected to undergo treatment for substance use to access permanent housing. Analysis shows that the program has a positive impact on housing stability and maintenance. It has also been linked to lower alcohol consumption and reduced costs associated with chronic alcohol use in health and social justice settings. Reference 218 Reference 219 |
National Housing StrategyReference 185 |
This strategy is a 10-year plan that includes targets to reduce homelessness and increase access to affordable and sustainable housing. These efforts could potentially reduce family stressors and parental substance use. When coupled with investment in connected, inclusive, community infrastructure, the result could be reduced exposure to substances for youth. |
Indigenous Early Learning and Child Care FrameworkReference 186 |
This framework is being developed to set out an action plan for facilitating access to culturally appropriate, high-quality, fully inclusive, flexible and affordable early learning and child care for First Nations, Inuit, and Métis families. Successful implementation would contribute to life-long developmental benefits to children. |
Promote positive social norms, communicate risks and reduce exposure
Alcohol, cannabis, and some opioids are regulated psychoactive substances that can be legally accessed. Marketing and advertising practices influence social norms (e.g., what is considered to be socially acceptable), and patterns of problematic substance use by increasing exposure to these substances and promoting their use. For prescription opioids, aggressive marketing can influence health professionals and contribute to over-prescription.Reference 187
A range of policy actions can be applied to reduce the availability of these substances, shift social norms, and increase awareness of risks related to substances. For example, regulatory policies can restrict access to substances and limit marketing practices that may promote problematic substance use. Public education campaigns can communicate the health consequences of using substances and deliver harm reduction messaging. Lower-risk guidelines can be introduced to promote new social norms. The history of tobacco control demonstrates that social norms and perceptions of psychoactive substances can change in response to the application of multiple policy measures such as public education, health warnings, and other regulatory policies.Reference 98
Policy measures targeting the prevention of problematic substance use are tailored to specific substances and can be implemented by local, provincial or federal governments. These types of population-level policy interventions are evaluated based on their reach and impact; that is, the number of people who are exposed to, and potentially influenced by, the policy.Reference 98 As such, even though policies may not benefit everyone, they can have a large population effect if many people are exposed to the intervention. To maximize their effectiveness, policy interventions can be coordinated across government levels and correspond with related community- and school-based efforts.
Policy in action: changing the culture of alcohol at the local level
Municipalities across Canada are working to change the culture of alcohol in their communities. Provinces have developed guides that provide a range of policy options and international examples for municipalities to consider.Reference 7 These include evidence-based actions relating to regulating availability, restricting marketing and advertising, modifying the drinking context, developing education strategies, and ensuring enforcement. Comprehensive municipal alcohol policies have proven effective in reducing underage access to alcohol, injuries and hospital visits, and impaired driving.Reference 14
Table 7, below, describes a series of available policy tools for the prevention of problematic substance use in youth, including potential actions for future consideration. In particular, two alcohol-related policy measures appear to show the greatest potential for reducing the harmful use of alcohol.Reference 98
- Policies that ensure higher pricing and taxation: Youth and lower income individuals are ‘price sensitive’ and generally reduce consumption of alcohol in response to higher prices. Price thresholds are also an important consideration for cannabis and other controlled substances. Higher prices can help to lower use, but prices that are too high could shift consumers to seek lower-cost product in the illegal market.
- Policies that reduce availability: Applying restrictions on the retail availability of alcohol can have a significant effect on the substance use behaviour of young people.
Given the current environment of cannabis legalization, coupled with the opioid overdose crisis, further research is needed as to which specific policies will be effective for the prevention of problematic use of cannabis and opioids in youth. That being said, evidence from the tobacco field suggests that policies placing mandatory, comprehensive restrictions on marketing and advertising would help to reduce the problematic use of cannabis and alcohol in young people.Reference 98 Voluntary restrictions do not appear to be as effective. Forthcoming Canadian regulations will soon restrict the marketing and advertising of opioids to health care practitioners, which may help to reduce over-prescribing.Reference 188 Furthermore, recently-released guidelines focus on the problematic use of prescriptions by providing clear direction on appropriate prescribing practices for opioids (including when not to prescribe).Reference 189
Lastly, decriminalization policies are generally considered harm reduction strategies rather than primary prevention. They prioritize a public health approach with harm reduction as a key component instead of law enforcement strategies. In countries that have seen positive results from decriminalizing the simple possession of psychoactive substances, the policy is always a part of a suite of measures that include primary prevention, social support, treatment and harm reduction measures tailored to the country’s context. In the end, a major societal shift such as decriminalization requires societal engagement and discourse, founded on the available evidence and an understanding of the necessity to eliminate stigma and discrimination of the people who use substances.
| Policy Aim | Policy Measure | Current Policy Approach in Canada | Considerations for Future Action in Canada |
|---|---|---|---|
Promote positive social norms and communicate risks |
Restrictions on promotion, including advertising |
Partial restrictions and voluntary standards for alcohol industry Cannabis Act includes comprehensive restrictions Intention to restrict marketing and advertising for opioids to health care practitioners |
Examine comprehensive restrictions on alcohol marketing and advertising Monitor compliance with promotional restrictions and access the need for new or additional measures |
Public education campaigns |
Awareness campaigns in mass media and social media to raise awareness of risks and encourage harm reduction measures (alcohol, cannabis, and opioids) Education and awareness activities targeting parents, youth, youth influencers, and other priority populations (e.g., Indigenous peoples) to communicate the health and safety risks of cannabis use |
Ensure awareness campaigns are Monitor and adapt cannabis public education and awareness activities based on emerging evidence (e.g., prevalence of use, knowledge, attitudes and beliefs) |
|
Guidelines instructing lower-risk use |
Low-risk alcohol use guidelines Lower-risk cannabis use guidelines Guidelines that promote best practices in opioid prescribing |
Promote existing guidelines through health associations and social sectors |
|
School health policies |
Combination of positive youth development and education, depending on province |
Enhance health and education sector opportunities for strengthening youth resilience |
|
Health product warnings |
Mandatory health warning messages, standardized cannabis symbol and labelling of THC and CBD amounts on cannabis products Opioid warning sticker and patient information handout for all prescription opioids |
Monitor and assess compliance with federal labelling regulations for cannabis and assess the need for new or additional measures |
|
Reduce access to and availability of psychoactive substances |
Substance content control |
Federal legislative and regulatory measures for cannabis to limit and control access, inform consumers, protect against accidental consumption, and reduce the appeal of cannabis to youth. Intention to restrict the alcohol concentration of highly-sweetened alcoholic beverages |
Evidence- and risk-based regulations to control the legal sale of additional cannabis products (e.g., edibles and concentrates) by October 2019 |
Legal age of use |
Enforcing legal age for cannabis possession, sale and distribution within each jurisdiction Legal age enforcement for alcohol consumption |
Monitor adequacy of cannabis enforcement measures and share best practices across jurisdictions |
|
Private versus public sales |
Minimum federal legislative conditions for cannabis retailers regardless of P/T retail model, including federal legislative restrictions at points-of-sale Spectrum of approaches in Canada for selling of alcohol, including government monopoly and private sales |
Evaluate retail approaches for cannabis in relation to youth use |
|
Control of supply |
Federal oversight of the cannabis supply chain, including: licensing of cannabis producers, strict product safety and quality control requirements, and mandatory reporting on the movement of cannabis through the supply chain Prescription monitoring systems for opioids to promote appropriate prescribing |
Ongoing calibration of compliance and enforcement measures for cannabis based on assessment of risk |
|
Minimum pricing and taxation |
Federal excise taxes for cannabis products, and recovery of regulatory costs from licensed producers Higher alcohol beverage prices and taxes |
Assess the impact of Canada’s cannabis taxation and cost recovery framework |
Develop skills and resilience for youth and their families
Programs that aim to develop social and emotional skills within youth and their families, improve parent-child relationships, and address social norms around substance use can help to reduce the harmful use of substances among youth. Although interventions at this level are designed to support individuals or sub-groups, they can have a population-level influence if universally and effectively applied.Reference 178 Yet, many programs lack the rigorous evaluation of effectiveness required for them to be widely adopted or expanded. The importance of these programs lie in the opportunities they present to directly engage with youth in their community context and intervene early with those who need additional support. To provide a supportive environment for these programs, communities can ensure a range of initiatives and activities are available for youth and families to connect and engage with each other.Reference 190
This section summarizes key components and approaches that have shown to be effective or promising within prevention programs for schools, social and health services, or activities such as sports programs. Programs that combine a range of components, are strengths-based, and are interactive show the most promise of consistent protective effects for reducing problematic substance use.
Family-focussed
Prevention interventions that help develop the skills and resources of caregivers can lead to improvements in childhood development in the earliest years.Reference 183 Parent-involved programs – when combined with other skills-building programs for youth – effectively strengthen family relationships and communication, build family resilience, and reduce alcohol and substance use in pre-teens and early adolescence.Reference 191 Programs that offer additional social supports for parents early on can potentially improve parent-child relationships (e.g., attachment), reduce child abuse, and reduce any subsequent harmful use of substances by youth.Reference 192 Programs have also been developed to help diverse families support their LGBTQ2 children to achieve well-being and lessen the risk of harmful behaviours, although the evidence is still emerging concerning their effectiveness for reducing problematic substance use.Reference 193
Building skills and enhancing resilience
Programs that teach resistance skills and correct misinformation about psychoactive substances show more promise when combined with elements that aim to build resilience and cognitive skills, such as self-management, decision-making, and social skills.Reference 194 Reference 195 Reference 196 In general, purely knowledge-based programs do not lead to significant changes in youth behaviour.Reference 194 Providing youth with tools and information to reduce harms from substance use (particularly alcohol) and to make informed choices, may also be effective.Reference 197 Reference 198 For Indigenous Peoples, resilience-based program components would be grounded in cultural values, such as culturally distinctive concepts of the person, and the importance of collective history and Indigenous languages and traditions.Reference 199
Interactive and youth-led
Interactions between teachers and students (and among students as peers) that stress communication and balanced discussions about substance use can improve prevention programming.Reference 200 Reference 201 Engaging with youth on program design can help to ensure that education programs are responsive to their needs.Reference 202 In general, fear- and abstinence-based programs delivered by police officers in schools are mostly ineffective and do not resonate with youth.Reference 203
Developmentally appropriate
Research indicates that prevention interventions are most effective when delivered prior to initial substance use or at the very early stages.Reference 204 As such, prevention programming can be implemented at all grade levels, particularly at ages that represent key transition points when youth generally begin to use substances.Reference 205 School-based programs may be most effective if implemented during the middle-school years, when experimentation with substance use is most likely to occur.Reference 200
Intervene early for youth that need support
Interventions based on one-to-one interactions with youth can be implemented in a variety of settings such as clinical environments, schools, child services settings, and community settings. These initiatives can be supported by a strong network of youth-focussed and non-stigmatizing mental health and support services. They are generally designed to help individual youth, although they can also be delivered universally.Reference 206
Screening, Brief Intervention and Referral (SBIR) for adolescents and young adults is the most evaluated individual-level program. The aim of SBIR is to encourage and motivate behaviour change over a short time period (1 to 5 sessions). The brevity and low cost may allow this intervention to be applied on a relatively large scale.Reference 206 SBIR has shown some effect on reducing problematic substance use in youth, particularly for alcohol, and may also be effective in preventing other substance use.Reference 206 Reference 207 The intervention generally consists of initiating a conversation with young people in order to identify early substance use and then take the necessary steps to prevent problems from developing. The screening component assesses substance use behaviours; this information is then used to identify the most appropriate type of intervention, either a brief conversation that attempts to motivate behaviour change, or referral to a more intensive treatment program. The most effective SBIR interventions promote behaviour change by building trust and using empathic and motivational interviewing styles.Reference 208Taking a comprehensive approach
Comprehensive multi-level and multi-sector initiatives could have greater and longer lasting effects than stand-alone interventions.Reference 209 The following two case studies reflect a broad approach to the prevention of substance use, going beyond individual-level interventions aimed at youth to tackle a range of interconnected community and social determinants of health.
The Iceland Youth Initiative (IYI)
“We learned through the studies that we need to create circumstances in which kids can lead healthy lives, and they do not need to use substances, because life is fun, and they have plenty to do—and they are supported by parents who will spend time with them.” Professor Inga Dóra SigfúsdóttirReference 210
The IYI has been heralded as a public health success for reducing harmful use of substances among youth. The initiative tackles wide-scale use of substances by youth through interventions that are implemented at community and societal levels.Reference 211 The program’s impact has been dramatic, particularly on early initiation of alcohol use. The percentage of adolescents (grade 10) who had never used alcohol rose from 20.8% in 1995 to 65.5% in 2015. Similarly, there was a decline over the same period in the proportion of adolescents who had consumed alcohol 40 times or more, from 13.7% to 2.8%.Reference 212
The intervention focuses on reducing known risk factors for substance use, while strengthening a broad range of parental, school and community protective factors. The developers reasoned that if they provided easily accessible, inexpensive alternatives, they could reduce substance use. At the societal level, funding was increased for organized sports, music, art, dance and other clubs, with youth from low-income families receiving financial support to take part in these activities. National policies were implemented for minimum age restrictions on buying tobacco (18 years) and alcohol (20 years), and tobacco and alcohol advertising were banned. A policy was also implemented that prohibited adolescents (13-16 years) from being outside after 10 p.m. in winter and midnight in summer.Reference 212
The initiative’s interpersonal and community streams emphasized the importance of family and parental relationships. Community buy-in was fostered through the building of alliances between schools, parent groups, local authorities and recreational workers, leading to an organized network of mutual support for youth.Reference 212
These interventions are informed by the Youth in Iceland Survey, a population-based survey for 9th and 10th graders to measure their substance use. The information collected helps to inform action at the community level. Survey results are made available to community workers and decision-makers within two months, which allows for quick local reaction. Reference 212
The First Nations Wellness Continuum Framework
The First Nations Wellness Continuum Framework (the Framework) was launched in 2015 to address mental health and substance use in First Nations communities of Canada using a comprehensive and culturally grounded approach.Reference 213 It is the result of extensive collaboration between First Nations communities, Indigenous leaders, and federal departments to identify a way forward in addressing mental wellness that considers the unique needs, values, beliefs and customs of First Nations communities. At the heart of this endeavour are community-led actions and a shared vision amongst First Nations communities and partners who have a responsibility to address mental wellness that focuses on families and communities.
The Framework is a complex model rooted in culture that emphasizes strengths, resilience, and the Indigenous social determinants of health. It is made up of layers of elements that are critical to supporting First Nations mental wellness across the life course, including youth. A key component is the recognition that First Nations culture, knowledge and wisdom must be the foundation to health and wellness. The Framework is based on a systems approach that provides a frame through which all services, supports, and partners can work together to respond to the full range of risks and harms associated with mental wellness in an evidence-based, culturally competent manner.Reference 213
Since its launch, the partners have developed an implementation plan to put the Framework into practice and identify priorities for the short, medium and long term. To move forward, the partners work collaboratively to implement these priorities and continue to engage provincial and territorial governments to advance the work of the Framework. An evaluation plan is being developed to support ongoing improvement of the implementation process. Although still in the early stages, the Framework promises to be a best practice for a systems-oriented public health approach that addresses key social determinants of health across the life course and societal levels. If successful, it could have a substantial long-term impact on reducing problematic substance use and creating the conditions for optimal mental wellness in First Nations youth.Reference 213
“We know that community solutions are the key to our success and we know that First Nations cultures must be central and foundational to addressing substance use issues and promoting wellness for individuals, families, and communities… <Achieving> the envisioned continuum of mental wellness will require sustained leadership, commitment and collaboration by all parties.” Assembly of First Nations Ontario Regional Chief Stan BeardyReference 213
Canadian Drugs and Substances Strategy (CDSS)
The two case studies described above and our knowledge of what is required for a comprehensive approach can inform future action.
In 2016, the Government of Canada introduced the CDSS as the new public approach to strengthening action on illegal and legal problematic substance use.Reference 214 It is a framework to address harmful use of substances through key pillars of prevention, harm reduction, treatment and enforcement. A consultation process was launched in the fall of 2018 to seek stakeholder input into what is needed for a comprehensive and collaborative approach that reflects the latest evidence and best practices.Reference 215
Chapter 4: The Way Forward – The Path to Preventing Problematic Substance Use in Youth
Problematic substance use among youth is driven by a dynamic interplay of factors such as the marketing of psychoactive substances and their availability to youth, family and peer relationships, experiences of abuse and trauma, stable housing, and family income.
Because of this complex reality, our collective response needs to be equally as broad and comprehensive. This report explores a range of prevention interventions which can inform cross-sector and youth-led discussions about how to move forward with innovative and integrated solutions.
I am calling upon all levels of government as well as nongovernmental, private, and philanthropic organizations across sectors – including public health, primary health care, social services, justice, and education – to undertake a coordinated approach to preventing problematic substance use among youth.
Key Action Areas
Implement an integrated suite of solutions
As a complex issue, the prevention of problematic substance use among youth requires a suite of interventions made up of effective policies, programs, and public and professional education.
Our previous public health approaches to tobacco can provide us with direction for addressing other psychoactive substances. Our experience tells us that – in combination with other interventions such as public education – comprehensive restrictions on the marketing, access, and availability of a substance can markedly reduce use and harms at a societal level. The current public health approach to cannabis under the new Cannabis Act aims to restrict youth access, regulate adult access, enhance public awareness of the health risks, and reduce the burden on the criminal justice system. We have an opportunity to evaluate this public health approach to cannabis.
At the same time, this report highlights the high levels of problematic alcohol consumption in Canada and the extent of its harms and costs. Now is the time for a comprehensive re-examination on how best to address problematic alcohol use and the necessary suite of evidence-informed public health measures needed to improve health outcomes.
We can also apply fresh approaches to designing multi-sectoral initiatives. For example, public health education campaigns could be developed in collaboration with social scientists and youth (including those who use or have used substances) to ensure that public messages speak to youth in their context and reflect current attitudes, behaviours, and beliefs.
Collaborate to drive novel approaches
No single entity is capable of implementing a complete suite of solutions. We will need to collaborate across sectors and with youth and people who use substances to pool our knowledge, identify critical gaps in prevention, and collectively develop new ideas.
To move forward with this integrated approach, we must accelerate established and budding collaborations between public health and social and economic sectors such as education, housing, and income support. For example, public health and education leaders could enhance collaborative efforts to bolster healthy school communities and expand or adapt promising school-based approaches for the prevention of problematic substance use. These types of partnerships could support the ongoing building of safe and supportive schools and communities that strengthen youth resilience.
Strengthen multi-disciplinary evidence for decision-making
Data and research form the evidence foundation for an effective suite of solutions. Many sectors have pieces of key information required for a more complete picture. We can do things differently by applying a systems perspective to coordinate networks across disciplines and sectors and gather data that can help us better understand the interplay of biological and social drivers. This will require social and health sciences to collaboratively develop research questions and ways of determining the effectiveness of interventions. Together with robust and linked surveillance systems that capture behaviours and harms, a systems approach can allow us to address the inherent complexity of problematic substance use and effectively respond as new patterns emerge.
We also need to understand the effectiveness of the actions we take to prevent problematic substance use, through rigorous evaluation of existing policies, public education campaigns, and tailored programs. This includes measuring the impact of initiatives on reducing health inequities and whether they meet the needs of different populations of youth. Lastly, we can better apply interventions and practices that we already know to be effective. These interventions could be shared amongst stakeholders and across networks so they can be adapted to new contexts and/or expanded to reach more youth.
Address trauma and eliminate stigma
Everyone has a story to tell. It is critical to recognize that, when not addressed, trauma can lead young people to turn to substances to cope with painful realities. Stigmatizing youth who use substances by thinking of them as addicts or failures is not productive and can further traumatize. We can help reduce the negative effects of stigma by changing the way we talk about substance use. Sectors such as health, justice, social services and the media can use neutral language that puts “people first” (e.g., people who use substances) and is respectful of them. Working closely with young people who have lived and living experience of using substances can help make sure that how we communicate and offer support is appropriate and compassionate.
Young people need community, healthcare, and school environments that are safe and empowering places for them to address past trauma and explore their strengths in culture and identity. To achieve this, we need to apply a trauma-informed lens to policies, practice, and program delivery. This involves institutions incorporating an understanding of the effects of trauma in all organizational aspects, and placing priority on the emotional safety and autonomy of young people. By taking on principles of cultural safety and addressing institutional barriers, we can make sure that programs and services are free of discrimination for the range of young people who access them. For example, reducing institutional barriers – such as not requiring youth to be substance free in order to access housing services – could encourage more of them to access much needed support.
Making prevention a priority
The pervasive harms of problematic substance use require us to do things differently. We must advance action across the entire continuum of prevention, harm reduction, treatment and recovery. Within the context of prevention, we will only succeed by acknowledging and acting on risks, while at the same time strengthening protective factors so that youth are engaged, resilient, and empowered.
I trust that this report provides enough knowledge to help to amplify current prevention efforts aimed at addressing problematic substance use before it begins. We must act now, together, to give us the best chance at ensuring the future well-being of our young people.
References
- Footnote 1
-
Public Health Agency of Canada. What is an Indicator Framework? 2017; Available from: https://infobase.phac-aspc.gc.ca/datalab/indicator-framework-blog-en.html
- Footnote 2
-
Public Health Agency of Canada, Reported cases from 1924 to 2016 in Canada - Notifiable diseases on-line. 2018.
- Footnote 3
-
Thunderbird Partnership Foundation. First Nations Mental Wellness Continuum Framework. 2015; Available from: http://thunderbirdpf.org/first-nations-mental-wellness-continuum-framework/
- Footnote 4
-
City of Toronto. Stigma, Discrimination & Substance Use: Experiences of people who use alcohol and other drugs in Toronto 2010; Available from: https://www.toronto.ca/wp-content/uploads/2018/01/93e2-stigmadiscrim_rep_2010_aoda.pdf
- Footnote 5
-
Canadian Centre on Substance Use and Addiction. Substance Abuse in Canada: Youth in Focus 2007; Available from: http://www.ccsa.ca/Resource%20Library/ccsa-011521-2007-e.pdf.
- Footnote 6
-
Special Advisory Committee on the Epidemic of Opioid Overdoses, Highlights from phase one of the national study on opioid- and drug-related overdose deaths: insights from coroners and medical examiners. 2018.
- Footnote 7
-
Canadian Centre on Substance Use and Addiction. Developing and Implementing Municipal Alcohol Policies. 2018; Available from: http://www.ccdus.ca/Eng/topics/alcohol/Developing-and-Implementing-Municipal-Alcohol-Policies/Pages/default.aspx
- Footnote 8
-
Canadian Institute for Health Information, Alcohol harm in Canada. Examining Hospitalizations Entirely Caused by Alcohol and Strategies to Reduce Alcohol Harm. 2017, Canadian Institute for Health Information.
- Footnote 9
-
Ye, X., Sutherland, J., Henry, B., Tyndall, M., & Kendall, P.R.W. , Impact of drug overdose-related deaths on life expectancy at birth British Columbia. Health Promotion and Chronic Disease Prevention in Canada, 2018. 38(6).
- Footnote 10
-
Centre for Addiction and Mental Health. Stigma- Understanding the impact of prejudice and discrimination. 2018.
- Footnote 11
-
Inuit Tapiriit Kanatami. Social Determinants of Inuit Health in Canada. 2014; Available from: https://www.itk.ca/wp-content/uploads/2016/07/ITK_Social_Determinants_Report.pdf.
- Footnote 12
-
Public Health Agency of Canada, Reducing the health impact of sexually transmitted and blood-borne infections in Canada by 2030: A pan-Canadian STBBI framework for action, Public Health Agency of Canada, Editor. 2018: Ottawa.
- Footnote 13
-
Truth and Reconciliation Commission of Canada. Honouring the truth, reconciling for the future. Summary of the final report of the Truth and Reconciliation Commission of Canada. 2015; Available from: http://www.trc.ca/websites/trcinstitution/File/2015/Honouring_the_Truth_Reconciling_for_the_Future_July_23_2015.pdf
- Footnote 14
-
Ontario Agency for Health Protection and Promotion (Public Health Ontario), Municipal Alcohol Policies and Public Health: A Primer. 2016, Public Health Ontario: Toronto.
- Footnote 15
-
Bellis, M.A., et al., The alcohol harm paradox: using a national survey to explore how alcohol may disproportionately impact health in deprived individuals. BMC Public Health, 2016. 16(1): p. 111.
- Footnote 16
-
Martens, P., et al., Profile of Metis health status and healthcare utilization in Manitoba: a population-based study. Winnipeg, MB: Manitoba Centre for Health Policy, 2010.
- Footnote 17
-
Truth and Reconciliation Commission of Canada. Truth and Reconciliation Commission of Canada: Calls to Action. 2015; Available from: http://www.trc.ca/websites/trcinstitution/File/2015/Findings/Calls_to_Action_English2.pdf
- Footnote 18
-
National Academies of Sciences, E. and Medicine, Ending discrimination against people with mental and substance use disorders: The evidence for stigma change. 2016: National Academies Press.
- Footnote 19
-
Van Boekel, L.C., et al., Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: systematic review. Drug & Alcohol Dependence, 2013. 131(1): p. 23-35.
- Footnote 20
-
Hatzenbuehler, M.L., J.C. Phelan, and B.G. Link, Stigma as a Fundamental Cause of Population Health Inequalities. American Journal of Public Health, 2013. 103(5): p. 813-821.
- Footnote 21
-
Room, R., Stigma, social inequality and alcohol and drug use. Drug and Alcohol Review, 2005. 24(2): p. 143-155.
- Footnote 22
-
Statistics Canada. Life expectancy and other elements of the life table, Canada, provinces and territories, (Table 13-10-0114-01). 2018; Table 053-0003 ]. Available from: https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1310011401
- Footnote 23
-
Organization for Economic Co-operation and Development. Health at a Glance 2017. 2017; Available from: https://www.oecd-ilibrary.org/content/publication/health_glance-2017-en
- Footnote 24
-
Public Health Agency of Canada. How Healthy are Canadians? 2017; Available from: https://www.canada.ca/en/public-health/services/publications/healthy-living/how-healthy-canadians.html
- Footnote 25
-
Public Health Agency of Canada. Health Inequalities Data Tool. 2018; Available from: https://infobase.phac-aspc.gc.ca/health-inequalities/data-tool/
- Footnote 26
-
Statistics Canada. Gap in life expectancy projected to decrease between Aboriginal people and the total Canadian population. 2015; Available from: https://www150.statcan.gc.ca/n1/pub/89-645-x/2010001/life-expectancy-esperance-vie-eng.htm
- Footnote 27
-
Institute for Health Metrics and Evaluation (IHME). Global Burden of Disease Data Visualization. 2017; Available from: http://ghdx.healthdata.org/gbd-results-tool
- Footnote 28
-
Statistics Canada. Canadian Tobacco Alcohol and Drugs (CTADS): 2015 summary. 2017; Available from: https://www.canada.ca/en/health-canada/services/canadian-tobacco-alcohol-drugs-survey/2015-summary.html
- Footnote 29
-
Statistics Canada. Canadian health characteristics, annual estimates (Table: 13-10-0096-01). 2018; Available from: https://www150.statcan.gc.ca/t1/tbl1/en/cv.action?pid=1310009601
- Footnote 30
-
Public Health Agency of Canada. The Chief Public Health Officer’s Report on the State of Public Health in Canada 2017 – Designing Healthy Living. 2017; Available from: https://www.canada.ca/en/public-health/services/publications/chief-public-health-officer-reports-state-public-health-canada/2017-designing-healthy-living.html
- Footnote 31
-
Public Health Agency of Canada. Fast Facts about Canada’s Neighbourhoods and physical activities. Available from: http://www.phac-aspc.gc.ca/hp-ps/hl-mvs/assets/pdf/fast-facts-faits-rapidesV2-eng.pdf
- Footnote 32
-
Centre for Indigenous Peoples’ Nutrition and Environment, Inuvialuit settlement region Inuit Health Survey 2007–2008. 2010.
- Footnote 33
-
Centre for Indigenous Peoples’ Nutrition and Environment, Nunatsiavut Inuit Health Survey 2007–2008. 2010.
- Footnote 34
-
Centre for Indigenous Peoples’ Nutrition and Environment, Nunavut Inuit Health Survey 2007–2008. 2010.
- Footnote 35
-
Institut national de santé publique du Québec, Nunavik Inuit Health Survey 2004. 2008.
- Footnote 36
-
Statistics Canada. Household food insecurity in Canada statistics and graphics (2011 to 2012). 2017; Available from: https://www.canada.ca/en/health-canada/services/nutrition-science-research/food-security/household-food-security-statistics-2011-2012.html
- Footnote 37
-
Public Health Agency of Canada. Life and breath: Respiratory disease in Canada. 2007; Available from: https://www.canada.ca/en/public-health/services/reports-publications/2007/life-breath-respiratory-disease-canada-2007.html
- Footnote 38
-
Statistics Canada. Deaths and Causes of death. 2018; Available from: https://www150.statcan.gc.ca/n1/daily-quotidien/180223/dq180223c-eng.htm
- Footnote 39
-
Demicheli, V., et al., Vaccines for preventing influenza in the elderly. The Cochrane Library, 2018.
- Footnote 40
-
Darvishian, M., et al., Effectiveness of seasonal influenza vaccination in community-dwelling elderly people: an individual participant data meta-analysis of test-negative design case-control studies. The Lancet Respiratory Medicine, 2017. 5(3): p. 200-211.
- Footnote 41
-
National Advisory Committee on Immunization (NACI). Canadian Immunization Guide Chapter on Influenza and Statement on Seasonal Influenza Vaccine for 2017–2018 2017; Available from: https://www.canada.ca/en/public-health/services/publications/healthy-living/canadian-immunization-guide-statement-seasonal-influenza-vaccine-2017-2018.html
- Footnote 42
-
Vachon J., G.V., Siu W.,, Tuberculosis in Canada, 2016. Can Commun Dis Rep, 2018. 44(3/4):75-81.
- Footnote 43
-
Public Health Agency of Canada. The time is now - Chief Public Health Officer spotlight on eliminating tuberculosis in Canada. 2018; Available from: https://www.canada.ca/en/public-health/corporate/publications/chief-public-health-officer-reports-state-public-health-canada/eliminating-tuberculosis.html
- Footnote 44
-
Canadian Public Health Association. This is Public Health: A Canadian History. 2009; Available from: https://cpha.ca/sites/default/files/assets/history/book/history-book-print_all_e.pdf.
- Footnote 45
-
Canadian Public Health Association. Immunization timeline. n.d.; Available from: https://www.cpha.ca/immunization-timeline
- Footnote 46
-
Public Health Agency of Canada. The Chief Public Health Officer's Report on the State of Public Health in Canada 2013 – Infectious disease – The never-ending threat. 2013; Available from: https://www.canada.ca/en/public-health/corporate/publications/chief-public-health-officer-reports-state-public-health-canada/chief-public-health-officer-report-on-state-public-health-canada-2013-infectious-disease-never-ending-threat.html
- Footnote 47
-
Public Health Agency of Canada. Canadian Antimicrobial Resistance Surveillance System Report 2016. 2016; Available from: https://www.canada.ca/en/public-health/services/publications/drugs-health-products/canadian-antimicrobial-resistance-surveillance-system-report-2016.html
- Footnote 48
-
Public Health Agency of Canada. Vaccination Coverage Goals and Vaccine Preventable Disease Reduction Targets by 2025. 2018; Available from: https://www.canada.ca/en/public-health/services/immunization-vaccine-priorities/national-immunization-strategy/vaccination-coverage-goals-vaccine-preventable-diseases-reduction-targets-2025.html
- Footnote 49
-
Public Health Agency of Canada. Vaccine Preventable Disease: Surveillance Report to December 31, 2015. 2017; Available from: https://www.canada.ca/en/public-health/services/publications/healthy-living/vaccine-preventable-disease-surveillance-report-december-31-2015.html
- Footnote 50
-
Public Health Agency of Canada. Lyme Disease in Canada - A Federal Framework. 2017; Available from: https://www.canada.ca/en/public-health/services/publications/diseases-conditions/lyme-disease-canada-federal-framework.html
- Footnote 51
-
Craig, G., et al., Tuberculosis stigma as a social determinant of health: a systematic mapping review of research in low incidence countries. International Journal of Infectious Diseases, 2017. 56: p. 90-100.
- Footnote 52
-
Public Health Agency of Canada. Poliomyelitis (Polio). 2017; Available from: https://www.canada.ca/en/public-health/services/immunization/vaccine-preventable-diseases/poliomyelitis-polio.html
- Footnote 53
-
Canadian Insititute for Health Information. Improving the Health of Canadians: Exploring Positive Mental Health. 2009; Canadian Insititute for Health Information. Ottawa.
- Footnote 54
-
Public Health Agency of Canada. Positive Mental Health Surveillance Indicator Framework. 2016; [Available from: http://www.phac-aspc.gc.ca/publicat/hpcdp-pspmc/36-8/assets/pdf/ar-04-eng.pdf
- Footnote 55
-
Public Health Agency of Canada. Mental Health Promotion. 2014; Available from: https://www.canada.ca/en/public-health/services/health-promotion/mental-health/mental-health-promotion.html
- Footnote 56
-
Ozbay, F., et al., Social support and resilience to stress: from neurobiology to clinical practice. Psychiatry (Edgmont), 2007. 4(5): p. 35.
- Footnote 57
-
Reblin, M. and B.N. Uchino, Social and emotional support and its implication for health. Current opinion in psychiatry, 2008. 21(2): p. 201.
- Footnote 58
-
Uchino, B.N., Social support and health: a review of physiological processes potentially underlying links to disease outcomes. Journal of behavioral medicine, 2006. 29(4): p. 377-387.
- Footnote 59
-
Statistics Canada. Table 1: Rates of selected mental or substance use disorders, lifetime and 12 month, Canada, household population 15 and older, 2012. 2015; Available from: https://www150.statcan.gc.ca/n1/pub/82-624-x/2013001/article/tbl/tbl1-eng.htm
- Footnote 60
-
Public health Agency of Canada, Mood and Anxiety Disorders in Canada. Health Promotion and Chronic Disease Prevention in Canada: Research, Policy and Practice, 2016. 36(12).
- Footnote 61
-
Canadian Public Health Association. Decriminalization of Personal Use of Psychoactive Substances. 2017; Available from: https://www.cpha.ca/decriminalization-personal-use-psychoactive-substances
- Footnote 62
-
U.S. Department of Health & Human Services. Facing addiction in America: The Surgeon General's report on alcohol, drugs, and health. November 2016; Available from: https://addiction.surgeongeneral.gov/sites/default/files/surgeon-generals-report.pdf.
- Footnote 63
-
Canadian Centre for Substance Use and Addiction. Reducing Alcohol-Related Harm in Canada: Toward a Culture of Moderation. 2007; Available from: http://www.ccsa.ca/Resource%20Library/ccsa-023876-2007.pdf
- Footnote 64
-
GBD 2016 Alcohol Collaborators, Alcohol use and burden for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. The Lancet, 2018.
- Footnote 65
-
Bulloch, A.G.M., et al., Trends in binge drinking in Canada from 1996 to 2013: a repeated cross-sectional analysis. CMAJ Open, 2016. 4(4): p. E599-E604.
- Footnote 66
-
First Nations Information Governance Centre. National Report of the First Nations Regional Health Survey: Phase 3. 2018 [cited 1; Available from: http://fnigc.ca/sites/default/files/docs/fnigc_rhs_phase_3_national_report_vol_1_en_final_web.pdf
- Footnote 67
-
Canadian Institute for Health Information. Alcohol harm on the rise for Canadian women. 2018; Available from: https://www.cihi.ca/en/alcohol-harm-on-the-rise-for-canadian-women
- Footnote 68
-
Canadian Centre for Substance Use and Addiction. National Treatment Indicators Report. 2016; Available from: http://www.ccsa.ca/Resource%20Library/CCSA-National-Treatment-Indicators-Report-2016-en.pdf
- Footnote 69
-
Statistics Canada. Police-reported crime for selected offences, Canada 2018 3302]; Available from: https://www150.statcan.gc.ca/n1/daily-quotidien/180723/t001b-eng.htm.
- Footnote 70
-
Transport Canada. Road Safety in Canada. 2011; Available from: https://www.tc.gc.ca/media/documents/roadsafety/tp15145e.pdf
- Footnote 71
-
Public Health Agency of Canada. Chief Public Health Officer’s Report on the State of Public Health in Canada, 2015: Alcohol Consumption in Canada. 2015; Available from: https://www.canada.ca/en/public-health/services/publications/chief-public-health-officer-reports-state-public-health-canada/2015-alcohol-consumption-canada.html
- Footnote 72
-
Popova, S., et al., Prevalence of alcohol consumption during pregnancy and Fetal Alcohol Spectrum Disorders among the general and Aboriginal populations in Canada and the United States. Eur J Med Genet, 2017. 60(1): p. 32-48.
- Footnote 73
-
Canadian Centre on Substance Use and Addiction. Cannabis. 2017; Available from: http://www.ccdus.ca/Resource%20Library/CCSA-Canadian-Drug-Summary-Cannabis-2018-en.pdf
- Footnote 74
-
Rotermann, M. and R. Macdonald, Analysis of trends in the prevalence of cannabis use in Canada, 1985 to 2015. Health Rep, 2018. 29(2): p. 10-20.
- Footnote 75
-
Rotermann, M., Langlois, K. Prevalence and correlates of marijuana use in Canada, 2012. 2015; Available from: https://www150.statcan.gc.ca/n1/pub/82-003-x/2015004/article/14158-eng.htm
- Footnote 76
-
Fischer, B., et al., Crude estimates of cannabis-attributable mortality and morbidity in Canada–implications for public health focused intervention priorities. Journal of Public Health, 2015. 38(1): p. 183-188.
-
National Academies of Sciences, E. and Medicine, The Health Effects of Cannabis and Cannabinoids: The Current State of Evidence and Recommendations for Research. 2017, Washington, DC: The National Academies Press. 486.
- Footnote 78
-
Volkow, N.D., et al., Adverse health effects of marijuana use. New England Journal of Medicine, 2014. 370(23): p. 2219-2227.
- Footnote 79
-
Gurney, J., et al., Cannabis exposure and risk of testicular cancer: a systematic review and meta-analysis. BMC cancer, 2015. 15(1): p. 897.
- Footnote 80
-
Memedovich, K., et al., The adverse health effects and harms related to marijuana use: an overview review. CMAJ open, 2018. 6(3): p. E339-E346.
- Footnote 81
-
Gunn, J., et al., Prenatal exposure to cannabis and maternal and child health outcomes: a systematic review and meta-analysis. BMJ open, 2016. 6(4): p. e009986.
- Footnote 82
-
Viteri, O.A., et al., Fetal anomalies and long-term effects associated with substance abuse in pregnancy: a literature review. American journal of perinatology, 2015. 32(05): p. 405-416.
- Footnote 83
-
Williams, J.H. and L. Ross, Consequences of prenatal toxin exposure for mental health in children and adolescents. European child & adolescent psychiatry, 2007. 16(4): p. 243-253.
- Footnote 84
-
Public Health Agency of Canada. Apparent opioid-related deaths. 2018; Available from: https://www.canada.ca/en/health-canada/services/substance-abuse/prescription-drug-abuse/opioids/apparent-opioid-related-deaths.html
- Footnote 85
-
Belzak, L.H., J., Evidence synthesis - The opioid crisis in Canada: a national perspective. 2018, Health Promotion and Chronic Disease Prevention in Canada: Public Health Agency of Canada p. 224-233.
- Footnote 86
-
Pain & Policy Studies Group - University of Wisconsin. Canada: opioid consumption in morphine equivalence (ME), mg per person. n.d.; Available from: http://www.painpolicy.wisc.edu/country/profile/canada
- Footnote 87
-
Canadian Institute for Health Information. Pan-Canadian Trends in the Prescribing of Opioids, 2012 to 2016. 2017; Available from: https://secure.cihi.ca/free_products/pan-canadian-trends-opioid-prescribing-2017-en-web.pdf
- Footnote 88
-
Fischer, B., L. Vojtila, and J. Rehm, The ‘fentanyl epidemic’in Canada–Some cautionary observations focusing on opioid-related mortality. Preventive medicine, 2018. 107: p. 109-113.
- Footnote 89
-
Statistics Canada. Results of the Survey on Opioid Awareness, November 2017. 2018; Available from: https://www150.statcan.gc.ca/n1/daily-quotidien/180109/dq180109a-eng.htm?CMP=mstatcan
- Footnote 90
-
First Nations Health Authority. Overdose Data and First Nations in BC. 2018; Available from: http://www.fnha.ca/newsContent/Documents/FNHA_OverdoseDataAndFirstNationsInBC_PreliminaryFindings_FinalWeb.pdf
- Footnote 91
-
Public Health Ontario. Poster: Opioid-related harms and socioeconomic inequalities in Ontario: A population health assessment. 2018; Available from: http://www.tophc.ca/wp-content/uploads/2018/04/Poster-78-%E2%80%93-Opioid-Related-Harms-and-Socioeconomic-Inequalities-in-Ontario-A-population-health-assessment.pdf
- Footnote 92
-
Meges D, Zevin B, Cookson E, Bascelli L, Denning P, Little J, Doe-Simkins M, Wheeler E, Watlov Phillips S, Bhalla P, Nance M, Cobb G, Tankanow J, Williamson J, Post P (Ed.). Adapting Your Practice: Recommendations for the Care of Homeless Patients with Opioid Use Disorders. 102 pages. Nashville: Health Care for the Homeless Clinicians' Network, National Health Care for the Homeless Council, Inc., 2014.
- Footnote 93
-
BC Centre for Disease Control. The BC Public Health Opioid Overdose Emergency: March 2017 Update. 2017; Available from: http://www.bccdc.ca/resource-gallery/Documents/Educational%20Materials/Epid/Other/Public%20Surveillance%20Report_2017_03_17.pdf
- Footnote 94
-
Canadian Centre on Substance Use and Addiction. Canadian Substance Use Costs and Harms: 2007-2014. 2018; Available from: http://www.ccdus.ca/Resource%20Library/CSUCH-Canadian-Substance-Use-Costs-Harms-Report-2018-en.pdf
- Footnote 95
-
Health Canada. Seizing the opportunity: the future of tobacco control in Canada. 2018; Available from: https://www.canada.ca/en/health-canada/programs/future-tobacco-control/future-tobacco-control.html
- Footnote 96
-
Patton, G.C., et al., Our future: a Lancet commission on adolescent health and wellbeing. Lancet, 2016. 387(10036): p. 2423-78.
- Footnote 97
-
Fischer, B., et al., Lower-Risk Cannabis Use Guidelines: A Comprehensive Update of Evidence and Recommendations. Am J Public Health, 2017. 107(8): p. e1-e12.
- Footnote 98
-
Hammond D., G.S., Policy Approaches for Problematic Substance Use: Evidence Review (Unpublished). 2018.
- Footnote 99
-
Health Canada. Summary of results for the Canadian Student Tobacco, Alcohol and Drugs Survey 2016-17. 2018; Available from: https://www.canada.ca/en/health-canada/services/canadian-student-tobacco-alcohol-drugs-survey/2016-2017-summary.html
- Footnote 100
-
Tourand, J., Smith, A., Poon, C., Stewart, D. & McCreary Centre Society. Ta Saantii: A profile of Métis youth health in BC. 2016; Available from: http://www.mcs.bc.ca/pdf/ta_saantii.pdf.
- Footnote 101
-
Klingemann, H.W.H.O., Alcohol and its social consequences - the forgotten dimension. 2001: Copenhagen : WHO Regional Office for Europe.
- Footnote 102
-
Testa, M. and J.A. Livingston, Alcohol Consumption and Women's Vulnerability to Sexual Victimization: Can Reducing Women's Drinking Prevent Rape? Substance use & misuse, 2009. 44(9-10): p. 1349-1376.
- Footnote 103
-
Lindgren, K.P., et al., College students' perceptions about alcohol and consensual sexual behavior: alcohol leads to sex. J Drug Educ, 2009. 39(1): p. 1-21.
- Footnote 104
-
Brunelle, N., et al., Patterns of psychoactive substance use among youths in Nunavik. Indittera, 2010. 2: p. 1-12.
- Footnote 105
-
Patton, G.C., et al., Cannabis use and mental health in young people: cohort study. BMJ : British Medical Journal, 2002. 325(7374): p. 1195-1198.
- Footnote 106
-
CTADS – Custom Analysis
- Footnote 107
-
Canadian Centre on Substance Use and Addiction. The effects of cannabis use during adolescence. 2015; Available from: http://www.ccsa.ca/Resource%20Library/CCSA-Effects-of-Cannabis-Use-during-Adolescence-Report-2015-en.pdf
- Footnote 108
-
Porath-Waller, A.J. Clearing the smoke on cannabis: Chronic use and cognitive functioning and mental health. 2016; Available from: http://www.ccsa.ca/Resource%20Library/CCSA-Chronic-Cannabis-Use-Effects-Report-2016-en.pdf
- Footnote 109
-
Schrager, S.M., et al., Correlates and Consequences of Opioid Misuse among High-Risk Young Adults. Journal of Addiction, 2014. 2014: p. 8.
- Footnote 110
-
Gomes, T., et al., Measuring the Burden of Opioid-related Mortality in Ontario, Canada. Journal of Addiction Medicine, 2018. Publish Ahead of Print.
- Footnote 111
-
Canadian Institute for Health Information. Opioid-related harms in Canada (Chartbook). 2017; Available from: https://www.cihi.ca/sites/default/files/document/opioid-harms-chart-book-en.pdf
- Footnote 112
-
Canadian Institute for Health Information & Canadian Centre on Substance Use and Addiction. Hospitalizations and Emergency Department Visits Due to Opioid Poisoning in Canada. 2016; Available from: https://secure.cihi.ca/free_products/Opioid%20Poisoning%20Report%20%20EN.pdf.
- Footnote 113
-
Kuntsche, E., et al., Replication and validation of the Drinking Motive Questionnaire Revised (DMQ-R, Cooper, 1994) among adolescents in Switzerland. Eur Addict Res, 2006. 12(3): p. 161-8.
- Footnote 114
-
Kuntsche, E., S.H. Stewart, and M.L. Cooper, How stable is the motive-alcohol use link? A cross-national validation of the Drinking Motives Questionnaire Revised among adolescents from Switzerland, Canada, and the United States. J Stud Alcohol Drugs, 2008. 69(3): p. 388-96.
- Footnote 115
-
Smith, A., Stewart, D., Poon, C., Peled, M., Saewyc, E., & McCreary Centre Society, From Hastings Street to Haida Gwaii: Provincial results of the 2013 BC Adolescent Health Survey 2014, McCreary Centre Society: Vancouver, British Columbia
- Footnote 116
-
Kairouz, S., et al., For all these reasons, I do...drink: a multilevel analysis of contextual reasons for drinking among Canadian undergraduates. J Stud Alcohol, 2002. 63(5): p. 600-8.
- Footnote 117
-
Zvolensky, M.J., et al., Marijuana Use Motives: A Confirmatory Test and Evaluation among Young Adult Marijuana Users. Addictive Behaviors, 2007. 32(12): p. 3122-3130.
- Footnote 118
-
McKiernan, A., & Fleming, K. , Canadian Youth Perceptions on cannabis. 2017, Canadian Centre on Substance Abuse: Ottawa
- Footnote 119
-
Vilhena-Churchill, N. and A.L. Goldstein, Child maltreatment and marijuana problems in young adults: Examining the role of motives and emotion dysregulation. Child Abuse & Neglect, 2014. 38(5): p. 962-972.
- Footnote 120
-
Public Health England. Health matters: giving every child the best start in life. 2016; Available from: https://www.gov.uk/government/publications/health-matters-giving-every-child-the-best-start-in-life/health-matters-giving-every-child-the-best-start-in-life
- Footnote 121
-
Chandler, M.J. and C. Lalonde, Cultural Continuity as a Hedge against Suicide in Canada's First Nations. Transcultural Psychiatry, 1998. 35(2): p. 191-219.
- Footnote 122
-
Chandler, M., J and C. Lalonde, Cultural Continuity as a Protective Factor Against Suicide in First Nations Youth. Vol. 10. 2008.
- Footnote 123
-
McCormick, R., Indigenous traditions in the treatment of substance abuse. Canadian Journal of Counselling, 2000. 34(1): p. 25-32.
- Footnote 124
-
Lovato, C., A. Watts, and L.F. Stead, Impact of tobacco advertising and promotion on increasing adolescent smoking behaviours. Cochrane Database Syst Rev, 2011(10): p. Cd003439.
- Footnote 125
-
Anderson, P., et al., Impact of alcohol advertising and media exposure on adolescent alcohol use: a systematic review of longitudinal studies. Alcohol and Alcoholism, 2009. 44(3): p. 229-243.
- Footnote 126
-
Moreno, M.A., et al., A content analysis of displayed alcohol references on a social networking web site. J Adolesc Health, 2010. 47(2): p. 168-75.
- Footnote 127
-
Stern, S. and L. Morr, Portrayals of teen smoking, drinking, and drug use in recent popular movies. J Health Commun, 2013. 18(2): p. 179-91.
- Footnote 128
-
Nunez-Smith, M., et al., Media exposure and tobacco, illicit drugs, and alcohol use among children and adolescents: a systematic review. Subst Abus, 2010. 31(3): p. 174-92.
- Footnote 129
-
Matthews, S., R. Dwyer, and A. Snoek, Stigma and Self-Stigma in Addiction. Journal of Bioethical Inquiry, 2017. 14(2): p. 275-286.
- Footnote 130
-
Patrick, M.E., et al., Socioeconomic status and substance use among young adults: a comparison across constructs and drugs. Journal of Studies on Alcohol and Drugs, 2012. 73(5): p. 772-782.
- Footnote 131
-
Canadian Centre on Substance Use and Addiction, Systems Approach Workbook: Socioeconomic determinants of health. 2014, Canadian Centre on Substance Abuse: Ottawa.
- Footnote 132
-
Galea, S. and D. Vlahov, Social determinants and the health of drug users: socioeconomic status, homelessness, and incarceration. Public health reports, 2002. 117(Suppl 1): p. S135.
- Footnote 133
-
Statistics Canada. Readiness to Learn at School Among Five-Year-Old Children in Canada. 2006; Available from: https://www150.statcan.gc.ca/n1/pub/89-599-m/89-599-m2006004-eng.htm
- Footnote 134
-
Raphael, D., Social determinants of health: Canadian perspectives. 2009: Canadian Scholars’ Press.
- Footnote 135
-
Xiang, Y., et al., ED visits for drug-related poisoning in the United States, 2007. Am J Emerg Med, 2012. 30(2): p. 293-301.
- Footnote 136
-
Spiller, H., et al., Epidemiological trends in abuse and misuse of prescription opioids. J Addict Dis, 2009. 28(2): p. 130-6.
- Footnote 137
-
Fischer, B., et al., Determinants of overdose incidents among illicit opioid users in 5 Canadian cities. CMAJ : Canadian Medical Association Journal, 2004. 171(3): p. 235-239.
- Footnote 138
-
Feng, C., et al., Homelessness independently predicts injection drug use initiation among street-involved youth in a Canadian setting. J Adolesc Health, 2013. 52(4): p. 499-501.
- Footnote 139
-
Hawkins, J.D., R.F. Catalano, and J.Y. Miller, Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood: implications for substance abuse prevention. Psychological Bulletin, 1992. 112(1): p. 64.
- Footnote 140
-
Resnick, M.D., et al., Protecting adolescents from harm: findings from the National Longitudinal Study on Adolescent Health. JAMA, 1997. 278(10): p. 823-832.
- Footnote 141
-
Morrison, W. and P. Kirby, Schools as a setting for promoting positive mental health: Better practices and perspectives. 2011: Joint Consortium for School Health.
- Footnote 142
-
Freeman, J.G., King, M., & Pickett, W. . Health Behaviour in School-aged Children (HBSC) in Canada: Focus on Relationships. [Report] 2015; Available from: http://healthycanadians.gc.ca/publications/science-research-sciences-recherches/health-behaviour-children-canada-2015-comportements-sante-jeunes/index-eng.php
- Footnote 143
-
Public Health Agency of Canada. Positive mental health surveillance indicator framework quick stats, youth (12 to 17 years of age). 2017; Available from: http://www.phac-aspc.gc.ca/publicat/hpcdp-pspmc/37-4/assets/pdf/ar-04-eng.pdf
- Footnote 144
-
Kaufmann, D.R., Wyman, P. A., Forbes-Jones, E. L., & Barry, J., Prosocial involvement and antisocial peer affiliations as predictors of behavior problems in urban adolescents: Main effects and moderating effects. Journal of Community Psychology, 2007. 35(4): p. 417-434.
- Footnote 145
-
Winstanley, E.L., et al., The association of self-reported neighborhood disorganization and social capital with adolescent alcohol and drug use, dependence, and access to treatment. Drug Alcohol Depend, 2008. 92(1-3): p. 173-82.
- Footnote 146
-
National Institute on Drug Abuse. Preventing Drug Use among Children and Adolescents (In Brief). 2003; Available from: https://www.drugabuse.gov/publications/preventing-drug-abuse-among-children-adolescents/acknowledgments
- Footnote 147
-
Waddell, C., et al., A public health strategy to improve the mental health of Canadian children. The Canadian Journal of Psychiatry, 2005. 50(4): p. 226-233.
- Footnote 148
-
Leslie, K., Youth substance use and abuse: challenges and strategies for identification and intervention. CMAJ : Canadian Medical Association Journal, 2008. 178(2): p. 145-148.
- Footnote 149
-
Janus, M., Brinkman, S., Duku, E., Hertzman, C., Santos, R., Sayers, M., et al., The Early Development Instrument: Population-based measure for communities. A handbook on development, properties, and use. 2007, Offord Centre for Child Studies. (n.d.). : Hamilton.
- Footnote 150
-
Chan, M., Linking child survival and child development for health, equity, and sustainable development. The Lancet, 2013. 381(9877): p. 1514-1515.
- Footnote 151
-
Canadian Insititute for Health Information. Children Vulnerable in Areas of Early Development: A Determinant of Child Health. 2014; Available from: https://secure.cihi.ca/free_products/Children_Vulnerable_in_Areas_of_Early_Development_EN.pdf
- Footnote 152
-
Afifi, T.O., et al., Child abuse and mental disorders in Canada. Cmaj, 2014. 186(9): p. E324-32.
- Footnote 153
-
SAMHSA’s Center for the Application of Prevention Technologies. The Role of Adverse Childhood Experiences in Substance Abuse and Related Behavioral Health Problems. Available from: https://www.samhsa.gov/capt/sites/default/files/resources/aces-behavioral-health-problems.pdf.
- Footnote 154
-
Statistics Canada. Family violence in Canada: A statistical profile, 2015. 2017; Available from: https://www150.statcan.gc.ca/n1/pub/85-002-x/2017001/article/14698-eng.htm
- Footnote 155
-
Lander, L., J. Howsare, and M. Byrne, The Impact of Substance Use Disorders on Families and Children: From Theory to Practice. Social work in public health, 2013. 28(0): p. 194-205.
- Footnote 156
-
Griffin, K.W. and G.J. Botvin, Evidence-Based Interventions for Preventing Substance Use Disorders in Adolescents. Child and Adolescent Psychiatric Clinics of North America, 2010. 19(3): p. 505-526.
- Footnote 157
-
Stone, A.L., et al., Review of risk and protective factors of substance use and problem use in emerging adulthood. Addict Behav, 2012. 37(7): p. 747-75.
- Footnote 158
-
Hodder, R.K., et al., Systematic review of universal school-based ‘resilience’interventions targeting adolescent tobacco, alcohol or illicit substance use: a meta-analysis. Preventive Medicine, 2017. 100: p. 248-268.
- Footnote 159
-
Liebenberg, L., Joubert, N., & Foucault, M.L. Understanding core resilience elements and indicators: A comprehensive review of the literature. 2017; Available from: http://lindaliebenberg.com/wp-content/uploads/2017/11/PHAC-Resilience-Report-Final-Version-November-2017.pdf.
- Footnote 160
-
Bonell, C., et al., What is positive youth development and how might it reduce substance use and violence? A systematic review and synthesis of theoretical literature. BMC Public Health, 2015. 16(1): p. 135.
- Footnote 161
-
Canadian Centre on Substance Use and Addiction. Substance abuse in Canada: Concurrent disorders. 2009; Available from: www.ccsa.ca/Resource%20Library/ccsa-011811-2010.pdf
- Footnote 162
-
Schuckit, M.A., Comorbidity between substance use disorders and psychiatric conditions. Addiction, 2006. 101 Suppl 1: p. 76-88.
- Footnote 163
-
Goldman, D., G. Oroszi, and F. Ducci, The genetics of addictions: uncovering the genes. Nat Rev Genet, 2005. 6(7): p. 521-32.
- Footnote 164
-
Meyers, J.L. and D.M. Dick, Genetic and Environmental Risk Factors for Adolescent-Onset Substance Use Disorders. Child and adolescent psychiatric clinics of North America, 2010. 19(3): p. 465-477.
- Footnote 165
-
Bierut, L.J., Genetic vulnerability and susceptibility to substance dependence. Neuron, 2011. 69(4): p. 618-627.
- Footnote 166
-
Kreek, M.J., et al., Genetic influences on impulsivity, risk taking, stress responsivity and vulnerability to drug abuse and addiction. Nature Neuroscience, 2005. 8(11): p. 1450.
- Footnote 167
-
Merikangas, K.R. and S. Avenevoli, Implications of genetic epidemiology for the prevention of substance use disorders. Addictive Behaviors, 2000. 25(6): p. 807-820.
- Footnote 168
-
Schmidt, R., Poole, N., Greaves, L., and Hemsing, N, New Terrain Tools to Integrate Trauma and Gender Informed Responses into Substance Use Practice and Policy. 2018, Centre of Excellence for Women’s Health: Vancouver.
- Footnote 169
-
Bowen, E.A. and N.S. Murshid, Trauma-Informed Social Policy: A Conceptual Framework for Policy Analysis and Advocacy. Am J Public Health, 2016. 106(2): p. 223-9.
- Footnote 170
-
BC Centre of Excellence for Women’s Health, Healing Families, Helping Systems: A Trauma-Informed Practice Guide for Working with Children, Youth and Families. 2016.
- Footnote 171
-
Grella, C.E., et al., Gender similarities and differences in the treatment, relapse, and recovery cycle. Evaluation review, 2008. 32(1): p. 113-137.
- Footnote 172
-
Blake, S.M., et al., A review of substance abuse prevention interventions for young adolescent girls. The Journal of Early Adolescence, 2001. 21(3): p. 294-324.
- Footnote 173
-
Clow, B., et al. Rising to the challenge: Sex-and gender-based analysis for health planning, policy and research in Canada. Halifax, NS: Atlantic Centre of Excellence for Women’s Health 2009; Available from: http://bccewh.bc.ca/wp-content/uploads/2012/05/2009_Rising_to_the_challenge.pdf
- Footnote 174
-
Bialystok, L., Nancy, P., Greaves, L. & Thomas, G., Recalculating Risk: An Opportunity for Gender-Transformative Alcohol Education for Girls and Women, in Making It Better: Gender-Transformative Health Promotion. 2014: Canadian Scholar’s Press/Women’s Press.
- Footnote 175
-
Reading, J., C. Loppie, and J. O’Neil, Indigenous health systems governance: From the Royal Commission on Aboriginal Peoples (RCAP) to Truth and Reconciliation Commission (TRC). International Journal of Health Governance, 2016. 21(4): p. 222-228.
- Footnote 176
-
Canadian AIDS Society. Peerology: A guide by and for people who use drugs on how to get involved. 2015; Available from: http://librarypdf.catie.ca/PDF/ATI-20000s/26521E.pdf
- Footnote 177
-
Canadian Centre on Substance Use and Addiction. Ethical Youth Engagement for Substance Use Prevention Campaigns. 2013; Available from: http://www.ccsa.ca/Resource%20Library/CCSA-2013-Ethical-Youth-Engagement-en.pdf
- Footnote 178
-
Frieden, T.R., A Framework for Public Health Action: The Health Impact Pyramid. American Journal of Public Health, 2010. 100(4): p. 590-595.
- Footnote 179
-
Watson, R.J., et al., Sexual minority youth continue to smoke cigarettes earlier and more often than heterosexuals: Findings from population-based data. Drug and Alcohol Dependence, 2018. 184: p. 64-70.
- Footnote 180
-
Brown, T., S. Platt, and A. Amos, Equity impact of interventions and policies to reduce smoking in youth: systematic review. Tob Control, 2014. 23(e2): p. e98-105.
- Footnote 181
-
Marmot, M., Social determinants of health inequalities. The Lancet, 2005. 365(9464): p. 1099-1104.
- Footnote 182
-
McCain, M.N., J.F. Mustard, and S. Shanker. Early years study 2: Putting science into action. 2007; Available from: http://earlylearning.ubc.ca/media/publications/early_years_study_2.pdf.
- Footnote 183
-
National Institute on Drug Abuse. Principles of Substance Abuse Prevention for Early Childhood: A Research-Based Guide. 2016; Available from: https://www.drugabuse.gov/publications/principles-substance-abuse-prevention-early-childhood/table-contents
- Footnote 184
-
Employment and Social Development Canada. Poverty Reduction Strategy. 2018; Available from: https://www.canada.ca/en/employment-social-development/campaigns/poverty-reduction.html
- Footnote 185
-
Canada Mortgage and Housing Corporation. National Housing Strategy. n.d.; Available from: https://www.cmhc-schl.gc.ca/en/nhs
- Footnote 186
-
Employment and Social Development Canada. Indigenous Early Learning and Child Care. 2017; Available from: https://www.canada.ca/en/employment-social-development/programs/indigenous-early-learning.html
- Footnote 187
-
Van Zee, A., The Promotion and Marketing of OxyContin: Commercial Triumph, Public Health Tragedy. American Journal of Public Health, 2009. 99(2): p. 221-227.
- Footnote 188
-
Health Canada. Notice of Intent to Restrict the Marketing and Advertising of Opioids. 2018; Available from: https://www.canada.ca/en/health-canada/services/drugs-health-products/drug-products/announcements/restrict-advertising-opioids.html
- Footnote 189
-
National Pain Centre. Canadian Guideline for Opioids for Chronic Non-Cancer Pain. 2017; Available from: http://nationalpaincentre.mcmaster.ca/documents/Opioid%20GL%20for%20CMAJ_01may2017.pdf.
- Footnote 190
-
Canadian Centre for Substance Use and Addiction. Competencies for the youth substance use prevention workforce: Prevention workforce competencies report. 2015; Available from: http://www.ccsa.ca/Resource%20Library/CCSA-Prevention-Workforce-Competencies-Report-2015-en.pdf.
- Footnote 191
-
etrie, J., F. Bunn, and G. Byrne, Parenting programmes for preventing tobacco, alcohol or drugs misuse in children <18: a systematic review. Health Education Research, 2007. 22(2): p. 177-191.
- Footnote 192
-
Miller, T.R., Projected Outcomes of Nurse-Family Partnership Home Visitation During 1996-2013, USA. Prev Sci, 2015. 16(6): p. 765-77.
- Footnote 193
-
Ryan, C., Generating a revolution in prevention, wellness & care for LGBT children & youth. Temple Political & Civil Rights Law Review, 2014. 23(2): p. 331-344.
- Footnote 194
-
Faggiano, F., et al., Universal school-based prevention for illicit drug use. Cochrane Database Syst Rev, 2014(12): p. Cd003020.
- Footnote 195
-
Slater, M.D., et al., Combining in-school and community-based media efforts: reducing marijuana and alcohol uptake among younger adolescents. Health Educ Res, 2006. 21(1): p. 157-67.
- Footnote 196
-
Foxcroft, D.R. and A. Tsertsvadze, Universal school-based prevention programs for alcohol misuse in young people. Cochrane Database of Systematic Reviews, 2011(5).
- Footnote 197
-
McBride, N., et al., Harm minimization in school drug education: final results of the School Health and Alcohol Harm Reduction Project (SHAHRP). Addiction, 2004. 99(3): p. 278-91.
- Footnote 198
-
McBride N, F.F., Muleners L, Midford R, School health and alcohol harm reduction project: details of intervention development and research procedures. 2006, National Drug Research Institute: Curtin University of Technology, Perth.
- Footnote 199
-
Kirmayer, L.J., et al., Rethinking resilience from Indigenous perspectives. Can J Psychiatry, 2011. 56(2): p. 84-91.
- Footnote 200
-
Soole, D.W., L. Mazerolle, and S. Rombouts, School-Based Drug Prevention Programs: A Review of What Works. Australian & New Zealand Journal of Criminology, 2008. 41(2): p. 259-286.
- Footnote 201
-
Moffat, B.M., R.J. Haines-Saah, and J.L. Johnson, From didactic to dialogue: Assessing the use of an innovative classroom resource to support decision-making about cannabis use. Drugs: Education, Prevention and Policy, 2017. 24(1): p. 85-95.
- Footnote 202
-
Canadian Centre on Substance Use and Addiction. Building on our strengths. Canadian standards for school-based youth substance abuse prevention. 2010; Available from: http://www.ccsa.ca/Resource%20Library/ccsa-011815-2010.pdf
- Footnote 203
-
Singh, R.D., Jimerson, S.R., Renshaw, T. et al., A Summary and Synthesis of Contemporary Empirical Evidence Regarding the Effects of the Drug Abuse Resistance Education Program (D.A.R.E.). Contemporary School Psychology, 2011. 15(1): p. 93-102.
- Footnote 204
-
McBride, N., A systematic review of school drug education. Health Educ Res, 2003. 18(6): p. 729-42.
- Footnote 205
-
Onrust, S.A., et al., School-based programmes to reduce and prevent substance use in different age groups: What works for whom? Systematic review and meta-regression analysis. Clin Psychol Rev, 2016. 44: p. 45-59.
- Footnote 206
-
Tanner-Smith, E.E. and M.W. Lipsey, Brief alcohol interventions for adolescents and young adults: a systematic review and meta-analysis. J Subst Abuse Treat, 2015. 51: p. 1-18.
- Footnote 207
-
Tanner-Smith, E.E., et al., Can Brief Alcohol Interventions for Youth Also Address Concurrent Illicit Drug Use? Results from a Meta-analysis. Journal of Youth and Adolescence, 2015. 44(5): p. 1011-1023.
- Footnote 208
-
Tevyaw, T.O.a.M., P.M., Motivational enhancement and other brief interventions for adolescent substance abuse: Foundations, applications and evaluations. Addiction Science & Clinical Practice, 2004. 99: p. 63-75.
- Footnote 209
-
Canadian Centre on Substance Use and Addiction. Standards for Preventing Problematic Substance Use. 2014; Available from: http://www.ccdus.ca/Eng/topics/Children-and-Youth/Drug-Prevention-Standards/Pages/default.aspx
- Footnote 210
-
Young, E. How Iceland Got Teens to Say No to Drugs. 2017; Available from: https://www.theatlantic.com/health/archive/2017/01/teens-drugs-iceland/513668/.
- Footnote 211
-
Sigfusdottir, I., et al., Trends in prevalence of substance use among Icelandic adolescents, 1995–2006. Vol. 3. 2008. 12.
- Footnote 212
-
Arnarsson, A., G.K. Kristofersson, and T. Bjarnason, Adolescent alcohol and cannabis use in Iceland 1995-2015. 2018. 37 Suppl 1: p. S49-s57.
- Footnote 213
-
Assembly of First Nations. First Nations Mental Wellness Continuum Framework Launched. 2015; Available from: http://www.afn.ca/2015/01/28/first-nations-mental-wellness-continuum-framework-launched/
- Footnote 214
-
Government of Canada. The New Canadian Drugs and Substances Strategy. 2016; Available from: https://www.canada.ca/en/health-canada/news/2016/12/new-canadian-drugs-substances-strategy.html
- Footnote 215
-
Health Canada. Strengthening Canada’s Approach to Substance Use Issues. 2018; Available from: https://www.canada.ca/en/health-canada/services/substance-use/canadian-drugs-substances-strategy/strengthening-canada-approach-substance-use-issue.html
- Footnote 216
-
Canadian Centre on Substance Abuse. (2013). "Canada’s Low-Risk Alcohol Drinking Guidelines [brochure]." from http://www.ccsa.ca/Resource%20Library/2012-Guidelines-For-Healthcare-Providers-to-Promote-Low-Risk-Drinking-Among-Patients-en.pdf
- Footnote 217
-
Employment and Social Development Canada. (2017). Housing First. Available from https://www.canada.ca/en/employment-social-development/programs/communities/homelessness/housing-first.html
- Footnote 218
-
Collins, S. E., D. K. Malone and M. E. Larimer (2012). "Motivation to change and treatment attendance as predictors of alcohol-use outcomes among project-based Housing First residents." Addictive Behaviors 37(8): 931-939.
- Footnote 219
-
Larimer, M. E., D. K. Malone, M. D. Garner, D. C. Atkins, B. Burlingham, H. S. Lonczak, K. Tanzer, J. Ginzler, S. L. Clifasefi, W. G. Hobson and G. A. Marlatt (2009). "Health care and public service use and costs before and after provision of housing for chronically homeless persons with severe alcohol problems." JAMA 301(13): 1349-1357.
- Footnote 220
-
Popova, S., Lange, S., Chudley, A.E., Reynolds, J.N., & Rehm, J. in collaboration with May, P.A. and Riley, E.P. (2018). World Health Organization International Study on the Prevalence of Fetal Alcohol Spectrum Disorder (FASD): Canadian Component. Toronto, ON: Centre for Addiction and Mental Health. Available from https://www.camh.ca/-/media/files/pdfs---reports-and-books---research/who-fasd-report-english-april2018-pdf.pdf?la=en&hash=347373E4C8C362E1F746C28BB063C7DA9E2987AE
- Footnote 221
-
Popova, S., Lange, S., Shield, K., Burd, L., & Rehm J. (under review). Prevalence of Fetal Alcohol Spectrum Disorder among special sub-populations: A systematic review and meta-analysis. Addiction.
Appendix 1: Glossary
- Cannabis
- A generic term used to denote the several psychoactive preparations of the plant from the genus Cannabis. It contains hundreds of chemical substances and more than 100 cannabinoids, many of which are biologically active. Among these, two cannabinoids have received the most scientific interest: delta-9-tetrahydrocannabinol (THC) and cannabidiol (CBD). THC has therapeutic effects and is the compound mainly responsible for the characteristic psychomimetic effects of cannabis, while CBD has therapeutic but no obvious psychomimetic effects, though it is psychoactive.
- Early Development Instrument
- A widely used measure of children’s readiness to learn. It is a kindergarten teacher-completed checklist that was developed to assess a child’s school readiness in five developmental areas: physical health and well-being, social competence, emotional maturity, language and cognitive development, and communication skills and general knowledge. EDI scores are calculated as the percentage of children who fall below the 10% cut-off of the comparison population (e.g., province or Canada) on at least 1 of the 5 areas of development.
- Fetal Alcohol Spectrum Disorder
- An umbrella diagnostic term describing the range of effects that can occur in an individual who was prenatally exposed to alcohol. These effects may include physical, cognitive, memory, behavioural and learning difficulties with lifelong implications.
- Harm reduction
- Policies, programs, and practices that aim to reduce the adverse health, social and economic consequences of the use of legal and illegal psychoactive drugs, without necessarily requiring people who use these substances from abstaining or stopping. A harm reduction approach respects the rights of individuals to use substances, increases awareness of lower-risk use, and addresses risk and protective factors relating to harms.
- Health inequities
- Differences in health status or in the distribution of health determinants between different population groups. These differences can be due to unmodifiable health determinants such as biological factors and/or chance, or modifiable health determinants such as income, education, employment and/or social supports.
- Health inequities
- A subset of health inequalities that arise from the persistence of modifiable health determinants in certain population groups.
- Heavy drinking
- Classified as an excessive amount of standard drinks of alcohol (i.e., 12 ounces of beer or cider, 5 ounces of wine, or 1.5 ounce of distilled alcohol), at least five for males and four for females, in one occasion at least once a month in the past year.
- Indigenous peoples
- A collective name for the original peoples of North America and their descendants. There are three distinct populations of Indigenous peoples in Canada: First Nations, Inuit, and Métis.
- LGBTQ2
- An evolving acronym for Lesbian, Gay, Bisexual, Transgender, Queer, Two-Spirit and additional identities.
- Opioids
- A family of powerful drugs (such as codeine, oxycodone, morphine, hydromorphone and fentanyl) that are usually prescribed to relieve pain; they can create a feeling of euphoria which makes them prone to abuse. If taken in large quantities or with other depressants (such as alcohol), opioids can lead to respiratory depression and death. In addition to be prescribed medications, they can also be produced or obtained illegally.
- Positive youth development
- A strengths-based approach that focuses on resilience and building protective factors in a young person’s environment. It promotes positive outcomes for young people by providing opportunities, fostering positive relationships, and facilitating the support needed for them to overcome adversity.
- Problematic substance use
- The use of a psychoactive substance in a manner, situation, amount, or frequency that can cause harm to the person using the substance or those around them.
- Protective factors
- Factors that decrease the likelihood of an individual developing problematic substance use or health problems associated with substance use.
- Psychoactive substances
- These are substances, that when taken into one's system, affect mental processes. For the purposes of this report, the term "substances" refers to psychoactive substances. Substances discussed in this report include alcohol, cannabis, and opioids.
- Resilience
- The capacity to bounce back from adversity. Resilient individuals, families and communities are more able to cope with difficulties and adversities than those with less resilience.
- Risk factors
- Factors that increase the likelihood of individuals beginning to use substances problematically and/or developing health problems associated with use.
- Social determinants of health
- The conditions in which people are born, grow, work, live, and age. These relate to an individual's place in society, such as income, education or employment. Experiences of discrimination and/or historical trauma are also important social determinants of health for certain groups such as Indigenous peoples.
- Social norms
- Customary rules of behaviour that are considered acceptable in groups and societies.
- Substance use
- This occurs across a continuum, ranging from experimentation to high-intensity chronic use.
- Substance use disorder
- Occurs when the recurrent use of a substance causes clinically and functionally significant impairment, such as health problems, disability, and failure to meet major responsibilities at work, school, or home. According to the Diagnostic and Statistical Manual of Mental Health Disorders-Fifth Edition (DSM-V), a diagnosis of substance use disorder is based on evidence of impaired control, social impairment, risky use, and pharmacological criteria.
- Trauma
- Describes the effects of experiences that overwhelm a person’s capacity to cope. These experiences may be early life events of abuse, neglect, and witnessing violence, or later life events such as sexual assault, partner violence, natural disaster, war, accidents, sudden unexpected loss, and forced disconnection from home or culture.
- Trauma-informed approach
- Trauma-informed approaches (TIAs) involve integrating an understanding of past and current experiences of trauma into various aspects of organizational systems, policies, programs, and practices to respond effectively and compassionately to those who have experienced trauma. TIAs operate at multiple levels, including the practitioner level, organizational level, as well as through wider collaboration across systems and sectors. The goal of TIAs is to minimize harm and avoid re-traumatizing individuals while supporting safety, choice, and control.
- Youth (adolescents and young adults)
- Aligned with the World Health Organization definition, adolescence in this report is characterized as the period from 10-19 years, and young adulthood, the period from 20-24 years. “Youth” is used to refer to either of these terms throughout the report.
Appendix 2: CPHO Health Status Dashboard
| Topic | Indicator | Most Current Data year | Data Source | Trend over time (up to 15 years) | International benchmark |
|---|---|---|---|---|---|
Life expectancy at birth |
82 years |
2013-2015 |
Vital Statistics |
Better |
Same (1) |
84 years |
2013-2015 |
Vital Statistics |
Better |
Same (1) |
|
80 years |
2013-2015 |
Vital Statistics |
Better |
Same (1) |
|
Health Adjusted Life Expectancy (HALE) at birth |
71 years |
2010-2012 |
Vital Statistics, Birth and Death Databases and population estimates; Canadian Community Health Survey; National Population Health Survey, Health institutions component; Residential Care Facilities Survey; Canadian Health Measures Survey; Census of population |
Better |
BetterAppendix 2 Table A Footnote * |
69 years |
2010-2012 |
Better |
|||
Perceived health |
61% |
2017 |
Canadian Community Health Survey (CCHS) |
Same |
BetterAppendix 2 Table A Footnote ** |
Perceived mental health |
70% |
2017 |
Canadian Community Health Survey (CCHS) |
Worse |
N/A |
|
|||||
| Category | Topic | Indicator | Indicator result | Most Current Data year | Data Source | Trend over time (up to 15 years) | International benchmark |
|---|---|---|---|---|---|---|---|
Social Factors |
Community belonging |
69% |
69 |
2017 |
Canadian Community Health Survey (CCHS) |
Better |
N/A |
Poverty (Canada's Official Poverty Line) |
11% |
11 |
2016 |
Canadian Income Survey (CIS) |
Better |
N/A |
|
Childhood poverty (Canada's Official Poverty Line) |
11% |
11 |
2016 |
Canadian Income Survey (CIS) |
Better |
N/A |
|
Education |
14% |
14 |
2017 |
Labour Force Survey |
Better |
Better |
|
Core housing need |
12% |
13 |
2016 |
Census |
Same |
N/A |
|
Food insecurity |
8% |
8 |
2011-2012 |
Canadian Community Health Survey (CCHS) |
Same |
N/A |
|
Problematic substance use |
Smoking |
13% |
13 |
2015 |
Canadian Tobacco, Alcohol and Drugs Survey (CTADS) |
Better |
Better |
Cannabis |
3% |
3 |
2015 |
Canadian Tobacco, Alcohol and Drugs Survey (CTADS) |
N/A |
WorseAppendix 2 Footnote * |
|
Alcohol |
20% |
20 |
2017 |
Canadian Community Health Survey (CCHS) |
Same |
||
Opioids |
11 per 100,000 |
11 |
2017 |
Opioid surveillance |
N/A |
||
16 per 100,000 |
16 |
2017 |
Hospital Morbidity Database (HMDB) |
Worse |
N/A |
||
Childhood risk and behavioural factors |
Bullying |
22% |
22 |
2014 |
Health Behaviour in School-aged Children |
Same |
Same |
Physical activity |
7% |
7 |
2015 |
Canadian Health Measures Survey (CHMS) |
Same |
N/A |
|
Sedentary behaviour |
29% |
29 |
2014-2015 |
Canadian Health |
N/A |
N/A |
|
Overweight and obesity |
17% |
17 |
2015 |
Canadian Health Measures Survey (CHMS) |
Same |
SameAppendix 2 Footnote **** |
|
14% |
14 |
2015 |
Same |
||||
Child abuse |
33% |
33 |
2014 |
General Social Survey |
N/A |
N/A |
|
Early childhood protective factors |
Early development index |
26% |
26 |
Various data years pooled |
Offord Centre for Child Studies, McMaster University |
N/A |
N/A |
Immunization |
89% |
89 |
2015 |
Childhood National Immunization Coverage Survey |
Same |
Worse |
|
77% |
77 |
2015 |
Same |
Worse |
|||
91% |
91 |
2015 |
Same |
N/A |
|||
75% |
75 |
2015 |
Same |
N/A |
|||
Maternal and Infant Health Factors |
Low birthweight |
6% |
6 |
2016 |
Vital Statistics |
Worse |
Same |
Breastfeeding |
32% |
32 |
2017 |
Canadian Community Health Survey (CCHS) |
Better |
Same |
|
|
|||||||
| Category | Topic | Indicator | Most Current Data year | Data Source | Trend over time (up to 15 years) | International benchmark |
|---|---|---|---|---|---|---|
|
Chronic diseases and injuries |
Cancer |
564 per 100,000 |
2015 |
Canadian Chronic Disease Indicators (CCDI) |
N/A |
Same |
66 per 100,000 |
2017 |
Canadian Cancer Registry (CCR) |
N/A |
N/A |
||
Cardiovascular Disease |
592 per 100,000 |
2015 |
Canadian Chronic Disease Indicators (CCDI) |
Better |
BetterAppendix 2 Table C Footnote * |
|
Diabetes |
595 per 100,000 |
2015 |
Canadian Chronic Disease Indicators (CCDI) |
Better |
SameAppendix 2 Table C Footnote ** |
|
Mood disorders |
9% |
2017 |
Canadian Community Health Survey (CCHS) |
Worse |
N/A |
|
Dementia (including Alzheimer's disease) |
1373 per 100,000 |
2015 |
Canadian Chronic Disease Indicators (CCDI) |
Better |
SameAppendix 2 Table C Footnote ** |
|
Suicide |
11 per 100,000 |
2016 |
Vital Statistics |
Same |
Same |
|
Unintentional injuries |
601 per 100,000 |
2016 |
Discharge Abstract Database (DAD), Hospital Morbidity Database (HMDB) |
Better |
N/A |
|
Communicable diseases |
Tuberculosis |
5 per 100,000 |
2016 |
Notifiable Disease on-line tool |
Same |
Better |
Hepatitis C |
31 per 100,000 |
2016 |
Better |
Better |
||
HIV |
6 per 100,000 |
2016 |
Same |
N/A |
||
|
||||||
International Comparisons
- Organization for Economic Development Canada. (2017). Health at a Glance 2017. Available from: http://www.oecd.org/health/health-systems/health-at-a-glance-19991312.htm
- World Health Organization. (2018). World Health Statistics. Available from: http://www.who.int/gho/publications/world_health_statistics/en/
- Organization for Economic Development Canada. (2017). Education at a Glance 2017. Available from: http://www.oecd.org/education/education-at-a-glance-19991487.htm
- World Health Organization. (2016). Cannabis use lifetime. Available from: https://gateway.euro.who.int/en/indicators/hbsc_27-cannabis-use-lifetime/
- Organization for Economic Development Canada. (2017). PISA 2015 Results. Available from: https://www.oecd-ilibrary.org/education/pisa-2015-results-volume-iii/students-exposure-to-bullying-results-based-on-students-self-reports-and-index-of-exposure-to-bullying_9789264273856-graph38-en
- Organization for Economic Development Canada. (2017). OECD Family Database. Available from: http://www.oecd.org/els/family/database.htm
- World Health Organization. (2017). Global Tuberculosis Report. Available from: http://www.who.int/tb/publications/global_report/gtbr2017_annex4.pdf?ua=1
- Mohd Hanafiah K, Groeger J, Flaxman AD, Wiersma ST. Global epidemiology of Hepatitis C virus infection: New estimates of age-specific antibody to HCV seroprevalence. Hepatology. 2013; 57(4):1333-42.
Appendix 3: Guidelines for Low-Risk Alcohol Drinking and Lower-Risk Cannabis Use
Low-Risk Alcohol Drinking Guidelines
The Low-Risk Alcohol Drinking Guidelines (LRADGs) recommend to:Reference 216
- Reduce long-term health risks (e.g., liver disease and some cancers)
- Women should have no more than 10 drinks a week, with no more than 2 drinks a day most days
- Men should have no more than 15 drinks a week, with no more than 3 drinks a day most days
- Reduce short-term risks of injury or acute illness
- Women should not have more than 3 drinks on any single occasion
- Men should not have more than 4 drinks on any single occasion
- Abstain from using in situations that are considered hazardous
- When driving a vehicle or using machinery and tools
- When taking medicine or other drugs that interact with alcohol
- When doing any kind of dangerous physical activity or making important decisions
- When living with mental or physical health problems, or alcohol dependence
- When pregnant or planning to be pregnant, or before breastfeeding
- When responsible for the safety of others
Lower-Risk Cannabis Use Guidelines
The Lower-Risk Cannabis Use Guidelines (LRCUGs) recommend to:Reference 97
- Abstain from use, as it is the most effective way to avoid health risks
- Delay starting cannabis use until later in life
- Identify and choose lower-risk cannabis products
- Do not use synthetic cannabinoids
- Avoid smoking burnt cannabis
- Avoid harmful inhaling practices such as breath-holding and deep-inhalation
- Avoid frequent or intensive cannabis use (e.g., daily or near-daily)
- Abstain from using in situations that are considered hazardous:
- When driving a vehicle or using machinery
- If you are at risk for mental health problems
- If you are pregnant
- Avoid combining these risks
Acknowledgements
Many individuals and organizations have contributed to the development of The Chief Public Health Officer's Report on the State of Public Health in Canada, 2018: Preventing Problematic Substance Use in Youth.
I would like to express my appreciation to the consultants who provided invaluable expert advice:
- Dr. Cory Neudorf, Chief Medical Health Officer, Saskatoon Health Region, University of Saskatchewan
- Dr. David Mowat, Canadian Partnership Against Cancer
- Dr. Elizabeth Saewyc, University of British Columbia
- Dr. Jeff Reading, University of Victoria
- Dr. John Frank, University of Edinburgh
- Dr. Margo Greenwood, University of Northern British Columbia, National Collaborating Centre for Aboriginal Health
- Dr. Michael Routledge, Medical Officer of Health, Manitoba
- Dr. Perry Kendall, University of British Columbia
I would like to extend a special thank you to problematic substance use experts for sharing their expertise in reviewing many drafts:
- Dr. Benedikt Fischer, Centre for Addiction and Mental Health
- Dr. David Hammond, University of Waterloo
- Dr. Jean-Sébastien Fallu, Université de Montréal
- Dr. Rebecca Saah, University of Calgary
In addition, I would also like to recognize contributions made by partners and stakeholders who were consulted on the report, including Marlene Laroque and Nelson Alisappi from the Assembly of First Nations, Eduardo Vides from the Métis National Council and staff from Inuit Tapiriit Kanatami, as well as the National Youth Council from the Boys and Girls Club of Canada.
I would also like to sincerely thank the many staff within Health Canada, Public Health Agency of Canada, Canadian Mortgage and Housing Corporation, and Employment and Social Development Canada for review of and input into the report.
I appreciate the excellence and dedication of my support staff and CPHO Reports Unit in researching, consulting on and developing this report: Bonnie Hostrawser, Anne-Marie Robert, Debjani Mitra, Kimberly Gray, Larry Shaver, Fatimah Elbarrani, Aimée Campeau, and Rhonda Fraser.