Introduction: The Chief Public Health Officer's Report on the State of Public Health in Canada 2013
Introduction
- Goals of the report
- What the report covers
- Infectious diseases in Canada
- About infectious diseases
- Why infectious diseases are important
- Infectious disease and determinants of health
- Infectious disease and preparedness
The Public Health Agency of Canada was established in September 2004 to strengthen Canada's capacity to protect and promote the health of Canadians.Footnote 1-Footnote 3 In 2006, the Public Health Agency of Canada Act confirmed the Agency as a legal entity and the appointment of a Chief Public Health Officer (CPHO) (see the textbox "The role of Canada's Chief Public Health Officer").Footnote 1 The legislation requires that the CPHO report on the state of public health in Canada annually.Footnote 1
Goals of the report
The CPHO's reports are intended to highlight specific public health issues that the CPHO has determined warrant further discussion and action in Canada.
This report presents the various factors that contribute to good health and what Canadians can do, both individually and collectively, to advance public health in Canada. As much as this report is a mechanism to increase awareness, it is also meant to inspire action, build upon existing health programs and initiatives and develop new solutions to promote, improve and maintain optimal health and well-being for all Canadians.
The role of Canada's Chief Public Health OfficerFootnote 3
The Chief Public Health Officer:
- is the deputy head responsible for the Public Health Agency of Canada, reporting to the Minister of Health;
- is the federal government's lead public health professional, providing advice to the Minister of Health and the Government of Canada on health issues;
- manages the Public Health Agency's day-to-day activities;
- works with other governments, jurisdictions, agencies, organizations and countries on public health matters;
- speaks to Canadians, health professionals, stakeholders, and the public about issues affecting the population's health;
- is required by law to report annually to the Government of Canada on the state of public health in Canada; and
- can report on any public health issue as needed.
In a public health emergency, such as an infectious disease outbreak or natural disaster, the Chief Public Health Officer:
- briefs and advises Canada's Minister of Health and others as appropriate;
- works with counterparts in other departments, jurisdictions and countries, as well as with experts and elected officials, to communicate with Canadians about how to protect themselves and their families;
- delivers public health information to Canadians via media appearances, public statements, updates to the Public Health Agency website, and columns and public advertisements in daily and community newspapers;
- provides direction to Public Health Agency staff, including medical professionals, scientists and epidemiologists, as they plan and respond to the emergency;
- leads daily national teleconferences, as appropriate, with federal government scientists and experts to share information and plan outbreak responses; and
- coordinates with jurisdictions through regular teleconferences with Canada's provincial and territorial Chief Medical Officers of Health and others.
What the report covers
This report, the CPHO's sixth on the state of public health in Canada, focuses on how infectious diseases influence public health and the health status of Canadians. The aim is to shed light on Canada's successes and ongoing challenges in the prevention, control and management of infectious diseases.
This report cannot comprehensively cover all areas of infectious disease in Canada. Instead, its goal is to explore a few related topics, all relevant to infectious disease and public health, that the CPHO has determined warrant further attention and that have a clear call to action. Each topic is independent in its own right, and the issues have been presented in such way that they can be read on their own. Ideally, coverage of these topics will generate greater awareness and foster discussion, engagement and continued commitment among all levels of government, healthcare professionals, educators, researchers and individual Canadians.
The following is a brief summary of the topics covered.
Immunization and Vaccine-preventable Diseases–Staying Protected examines:
- The important role of immunization in preventing infectious diseases in Canada
- How to increase and maintain immunization coverage
- How to continue to educate Canadians about the benefits of vaccines and increase public confidence
- Strategies to improve immunization programs across Canada
Healthcare-associated Infections–Due Diligence discusses:
- How infections are transmitted in healthcare settings
- Some of the more common infections and their effects
- How to reduce the risk of infection and transmission
Antimicrobial Resistance–A Shared Responsibility examines:
- A brief history of antimicrobials and antimicrobial resistance
- What factors have helped increase the rate at which antimicrobial resistance is spreading
- Common ways to transmit antimicrobial-resistant organisms as well as treatment options
- How to manage and minimize the impact of antimicrobial resistance on the population
Tuberculosis–Past and Presentdiscusses:
- Tuberculosis in Canada and internationally, and more specifically, in vulnerable populations
- Common prevention and treatment practices as well as considerations of drug resistance and co-infection
Food-borne and Water-borne Infections–Invisible Threats examines:
- Common causes of food-borne and water-borne infections in Canada
- How food-borne and water-borne infections are transmitted
- Strategies to manage and minimize food and water contamination
Sexually Transmitted Infections–A Continued Public Health Concern explores:
- Common sexually transmitted infections (STIs) in Canada
- The short- and long-term health outcomes of STIs including those with associated chronic conditions
- Strategies and approaches to reduce the transmission of infection and manage disease over the lifecourse
Conclusion–Continuing Efforts underlines:
- The need to remain vigilant in the face of new and existing infectious disease threats
- The common themes among the six sections in the report
- That prevention and control of infectious diseases is a shared responsibility among industry, government, healthcare and individuals
- That a long-term infectious disease strategy must address the social determinants of health
Appendices A–C examine:
- The demographics of the Canadian population, including life expectancy and patterns of ill health, disability and mortality
- Determinants that influence health–income, employment, education and health behaviours
- Definitions and data sources
Infectious diseases in Canada
Canada has made great advances in preventing and controlling infectious diseases as a result of widespread improvements in hygiene and sanitation measures, implementing water treatment systems, enhancing food safety, researching and developing new drugs and immunizing against vaccine-preventable diseases.Footnote 4-Footnote 6 Despite the progress made, infectious diseases are still a major health issue and public health concern. Many Canadians will become ill with at least one infection each year. Most of these infections are minor and go unreported, but some can be serious. Most are preventable.Footnote 7-Footnote 11 Continued commitment to reduce the incidence and prevalence of infectious disease is necessary to keep Canadians healthy and prevent illness and premature death.
About infectious diseases
Figure 1 Epidemiologic triad of disease causationFootnote 12, Footnote 13
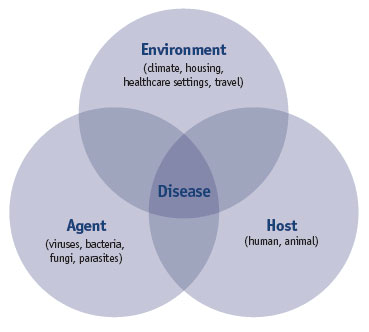
Text Equivalent - Figure 1
The epidemiologic triad consists of an external agent (viruses, bacteria, fungi, parasites), a susceptible host (human, animal), and an environment (climate, housing, healthcare settings, travel).
Infectious diseases arise from the complex interactions between the agent, the environment, and the host (see Figure 1). Agent refers to an infectious micro-organism: a virus, bacterium, fungus or parasite. When infectious micro-organisms break through natural defences and make their way into the host (human or animal), they can multiply and cause illness. In some cases, only one system or organ is affected in the body; in others, the infection affects the entire host.Footnote 14, Footnote 15
Infectious micro-organisms can spread through air or water or food; by direct physical contact or indirect contact with a contaminated object or surface; and via insect or animal or another person.Footnote 12, Footnote 16, Footnote 17 The length of time that a micro-organism stays infectious and the distance it can travel depends on the type of organism and the environment in which it exists.Footnote 17
Many factors in the environment can contribute to the growth and spread of infectious diseases including: global travel, urbanization and immigration; housing; healthcare practices and public health infrastructure; food production and preparation; the use and misuse of antibiotics and microbial adaptation; and human behaviour. The range of diversity plus the ability of micro-organisms to evolve and adapt to changing populations, environments, practices and technologies create ongoing threats to health and continually challenge our efforts to prevent and control infectious diseases.Footnote 14, Footnote 18
Why infectious diseases are important
Infectious diseases are a public health issue. There are areas for concern (e.g. antibiotic-resistant bacteria, healthcare-associated infections, food- and water-borne illnesses and potential disease outbreaks and pandemics) that require attention and action.Footnote 18 Addressing them now, before the risks and impacts advance any further, is essential. Improving Canada's ability to prevent known infectious diseases and to recognize and control rare or newly emerging threats is necessary to reduce the burden of disease and improve and maintain the health of Canadians.Footnote 19, Footnote 20
This issue extends beyond the borders of Canada; infectious diseases are a global concern. A fast-changing, globalized world has provided increased opportunities for emergence and re-emergence of infectious diseases. That being said, it has also brought about significant developments in the prevention and control of infectious diseases.Footnote 18, Footnote 19 Canada has a better understanding of how infections emerge, persist, develop resistance and cause disease. It is important to continually reconsider prevention and control strategies and take advantage of new ways to tackle infectious diseases and improve and maintain the health of Canadians.Footnote 19-Footnote 21
Addressing infectious diseases also involves managing diseases and their impacts after the point of infection. There are particular challenges associated with certain infectious diseases over the long term, when they take on chronic characteristics as an individual ages.Footnote 22 For example, some diseases start as infectious but can become a chronic disease later in life (e.g. human papillomavirus [HPV] and hepatitis B and C). These diseases can have long term health impacts that make individuals more vulnerable to other diseases and conditions such as influenza, cancer and mental health conditions.Footnote 22 Our evolving understanding of the links between infectious and chronic diseases will inform future prevention and treatment efforts.
Infectious disease and determinants of health
Addressing the prevention, control and management of disease also requires broadening our approach to health interventions to consider what influences health both inside and outside the healthcare system. It involves identifying factors that can put Canadians at increased risk of health complications and infections. Social and economic factors, the physical environment and individual behaviour all play a role. These factors interact to influence collective and individual health and well-being (see the textbox "Determinants of health").Footnote 23, Footnote 24
Determinants of healthFootnote 23
- income and social status
- social support networks (e.g. family, peers)
- education and literacy
- employment and working conditions
- social environments (e.g. community, workplace)
- physical environments (e.g. housing, community infrastructure)
- personal health practices and coping skills
- healthy child development (including/during pregnancy)
- biology and genetic endowment (e.g. sex)
- health services
- gender
- culture
Determinants of health contribute to an individual's overall state of health, which in turn, can influence an individual's risk of infection and disease. Determinants of health also play a role in an individual's resistance to infection, the progression of disease and the treatment and management of illness after the point of diagnosis.Footnote 25-Footnote 28 Tuberculosis (TB) is a good example of the relationship between infectious disease and the determinants of health.Footnote 29-Footnote 31 Living in a low income household, living in crowded inadequately ventilated housing or being homeless, being malnourished or affected by other socio-economic conditions are some, but not all, of the known risk factors for developing a TB infection.Footnote 31-Footnote 33 Thus, preventing and managing infectious diseases such as TB firstly, involves addressing what puts Canadians at risk, and secondly, requires building upon and improving economic and social supports.Footnote 25-Footnote 27, Footnote 29-Footnote 31
By strengthening and investing in the determinants of health, there is more opportunity to positively influence the overall health status of Canadians. Individuals with access to adequate health and social services have better health outcomes and a reduced likelihood of developing illness and/or disease.Footnote 24-Footnote 28 Making progress will require identifying and reducing risks and vulnerabilities, as well as expanding efforts to ensure adequate supports and resources are available to meet basic needs.Footnote 23-Footnote 28 Simply put, addressing the determinants of health should be part of any long-term infectious disease strategy.Footnote 24, Footnote 25, Footnote 27, Footnote 28
Infectious disease and preparedness
Diseases can spread globally and affect populations worldwide. Taking steps to make sure Canadians are less vulnerable to the impact of infectious diseases is an ongoing challenge. Canada has made great strides in safeguarding the population and responding to emerging and ongoing health threats.Footnote 19, Footnote 34 Recent experiences with SARS and H1N1 have provided valuable guidance; these events have also emphasized the vulnerability that remains.Footnote 19-Footnote 21 The best approach is to plan and be prepared to respond. Canada cannot become complacent. Planning for all types of threats, combined with other fundamental measures such as surveillance, infrastructure, and capacity, will put Canada in the best position to respond to any emergency.Footnote 20, Footnote 34
References
Page details
- Date modified: