Full report: A Vision to Transform Canada's Public Health System
Chief Public Health Officer's Report on the State of Public Health in Canada 2021
Download in PDF format
(1.54 MB, 129 pages)
Organization: Public Health Agency of Canada
Date Published: 2021-12-13
Cat.: HP2-10E-PDF
ISBN: 1924-7087
Pub.: 210338
Table of contents
- Message from the Chief Public Health Officer of Canada
- About this report
- Section 1. COVID-19 in Canada and the world
- Section 2. Public health in Canada: Opportunities for transformation
- Section 3. A vision to transform public health in Canada
- The way forward
- Appendix A: Methodology
- Acknowledgements
- References
- Endnotes
Message from the Chief Public Health Officer of Canada
The COVID-19 pandemic represents the biggest public health crisis that our country has confronted in a century. There is no doubt that this has tested our public health systems. And while there have been challenges, there have also been remarkable achievements, such as Indigenous ownership of the pandemic response in their communities and the rollout of the largest mass vaccination program in Canadian history. I am incredibly proud of the over 28 million Canadians 12 years of age and older who have been fully vaccinated so far. With the recent approval of Canada’s first COVID-19 pediatric vaccine formulation for children 5 to 11 years old, we will continue to see our vaccine coverage rates increase across the country.
There is no doubt that the COVID-19 pandemic will continue to be a key public health priority in Canada for the foreseeable future. At the time of publishing this report, Canada is in the midst of a fourth wave fuelled by the highly transmissible Delta variant and a new variant of concern, Omicron, has recently been identified by the World Health Organization. It is still too early to know how this new variant will impact our pandemic response in Canada but its emergence reminds us that we need to remain vigilant and adapt our response as needed moving forward. At the same time, there are other pressing public health issues that also require urgent action. These include the worsening opioid overdose crisis, increasing mental health challenges, the health impacts of climate change, and the ongoing threat of antimicrobial resistance.
While our public health system has extended itself to meet the increased demands of COVID-19, it is stretched dangerously thin. The pandemic has highlighted the strengths of our system but it has also exposed long-standing cracks in the foundation. The public health system lacks the necessary resources and tools to carry out its critical work, and is the subject of “boom and bust” funding cycles that leave us ill-prepared in the face of new threats.
Moving forward, we must ensure that our public health system is better equipped to protect all people living in Canada and help them to achieve optimal health.
Simply put, we must act now to ensure that our post-pandemic future is different than our pre-pandemic past.
In my 2020 annual report, I examined the broader consequences of the pandemic, and how persisting health and social inequities have resulted in disproportional impacts of COVID-19 on some populations. The report highlighted the need for a strengthened public health system that is centred on health equity and working towards good health and wellness for all.
My 2021 annual report builds on these findings. It draws from the diverse input of public health leaders, researchers, community experts, intersectoral collaborators, and First Nations, Inuit, and Métis leaders. Working from the foundational building blocks of public health systems in Canada, my report outlines strategic opportunities and key actions for achieving a transformed public health system that best protects us all against current and emerging public health challenges.
While the pandemic is not yet over, we are at a pivotal moment where we can come together to reflect on what we have learned and, collectively, define a new way forward. Joining forces across communities and sectors, we can build the public health system that we all need and expect, in pursuit of the healthy and thriving society that we all want. It is in working together that we can make sure that we get it right.
About this report
This year’s annual report of the Chief Public Health Officer of Canada (CPHO) examines the current state of public health in Canada. It describes the impacts of the COVID-19 pandemic and provides a forward-looking vision to transform Canada’s public health system, in order for it to excel and be better prepared for the next public health crisis.
Like SARS and H1N1 in the past, COVID-19 was a stress-test of our health, social, and economic systems. It underscored the critical importance of the public health system in protecting us from the potentially crippling effects of emerging viruses. This includes the vital role the system plays in helping to mitigate excessive pressure on healthcare resources.
As we continue to face evolving and worsening threats to human health, such as climate change, antimicrobial resistance, or the burden of non-communicable diseases, we need to ensure that our public health systems are better equipped to capably address these complex challenges.
This report builds on last year’s CPHO annual report From Risk to Resilience: An Equity Approach to COVID-19 which documented the unequal impacts of COVID-19 on the health of Canadians. It highlighted the need for stronger public health systems to keep people well and healthy, while contributing to a flourishing society.
This year’s report, A Vision to Transform Public Health in Canada, is divided into the following main sections:
Section one sets the context with an overview of the key epidemiological COVID-19 events in Canada between August 2020 and August 2021. By illustrating inequities, broader pandemic impacts, and lessons learned, this section provides compelling evidence on the need to strengthen the public health system in Canada.
Section two describes the unique role and impact of public health systems on the health of populations. It presents the foundational building blocks of Canada’s system, and outlines the opportunities for system-level improvements.
Section three builds on these opportunities, to offer a vision of a world-class public health system. It then outlines the elements needed to achieve this vision and ensure that the conditions are in place for Canada to be ready for current and future public health challenges.
Note to the reader: This report was written with the knowledge that the COVID-19 pandemic and its impacts continue to evolve. Given the need to finalize the report well in advance of publication, it does not cover changes in epidemiology, emerging events, or implementation of additional public health measures beyond the end of August 2021. Further details on the methods and limitations are provided in Appendix A.
This report benefits from the leadership and expertise of many contributors. In particular 4 independent commissioned reports were prepared to inform its content, which will be available on the National Collaborating Centres for Public Health website:
- The experiences, visions, and voices of First Nations, Inuit, and Métis Peoples on the future of public health in Canada are reflected in a companion report entitled Visioning the Future: First Nations, Inuit, & Métis Population and Public Health, which was developed and led by Indigenous public health leaders, in collaboration with Indigenous scholars and national Indigenous organizations.
- The components, approaches, and overarching factors to support a pan-Canadian public health data system are summarized in a companion report entitled An Evidence-Informed Vision for a Public Health Data System in Canada, which was developed by Dr. David Buckeridge.
- Opportunities to strengthen, improve, or transform existing public health governance are discussed in a companion report entitled Governing for the Public’s Health: Governance Options for a Strengthened and Renewed Public Health System in Canada, which was led by Dr. Erica Di Ruggiero.
- Proposed key actions to better incorporate and support the capacity of communities beyond COVID-19 are presented in a companion report entitled Strengthening Community Connections: The Future of Public Health is at the Neighbourhood Scale, which was developed by Dr. Kate Mulligan.
Finally, also available is a “What We Heard” report, entitled A Renewed and Strengthened Public Health System in Canada that provides a summary of discussion groups and key informant interviews conducted to inform the development and drafting of this report.
We respectfully acknowledge that the land on which we developed this report is in traditional First Nation, Inuit, and Métis territory, and we acknowledge their diverse histories and cultures. We strive for respectful partnerships with Indigenous Peoples as we search for collective healing and true reconciliation. Specifically, this report was developed in Ottawa, on the traditional and unceded territory of the Algonquin Anishnaabe people; in Halifax, on the ancestral and unceded territory of the Mi’kmaq people; in Montreal, on the traditional and unceded territory of the Mohawk (Kanien’kehá:ka) Nation; and in Toronto, on the traditional territory of the Wendat, the Anishnaabeg, Haudenosaunee, Métis, and the Mississaugas of the New Credit First Nation.
Section 1. COVID-19 in Canada and the world
COVID-19 pandemic in Canada
Overview of COVID-19 epidemiology
The COVID-19 pandemic remains one of the most significant public health crises in recent memory. As of August 31, 2021, there were about 1,500,000 reported COVID-19 cases and close to 27,000 COVID-19-related deaths in CanadaFootnote 1. COVID-19 was estimated to be the third leading cause of death in 2020, following only cancer and heart diseaseEndnote i Footnote 2. This marks the first time since the mid-20th century that an infectious disease has ranked among the top 3 causes of death in CanadaFootnote 3 Footnote 4. The 2020 CPHO Annual Report detailed the early epidemiology of the COVID-19 crisis until the end of the first wave in August 2020Footnote 5. Since that time, Canada has experienced additional waves, including one in the winter of 2020-21 and another in the spring of 2021Endnote ii. As of August 2021, at the time of writing this report, rising incidence signalled the beginning of a fourth waveFootnote 6. Figure 1 shows an overview of nationally reported COVID-19 cases and related outcomes, such as daily number of patients in hospital, daily number of intensive care unit (ICU) patients, and deaths in Canada for the period of March 2020 to August 2021Footnote 1.
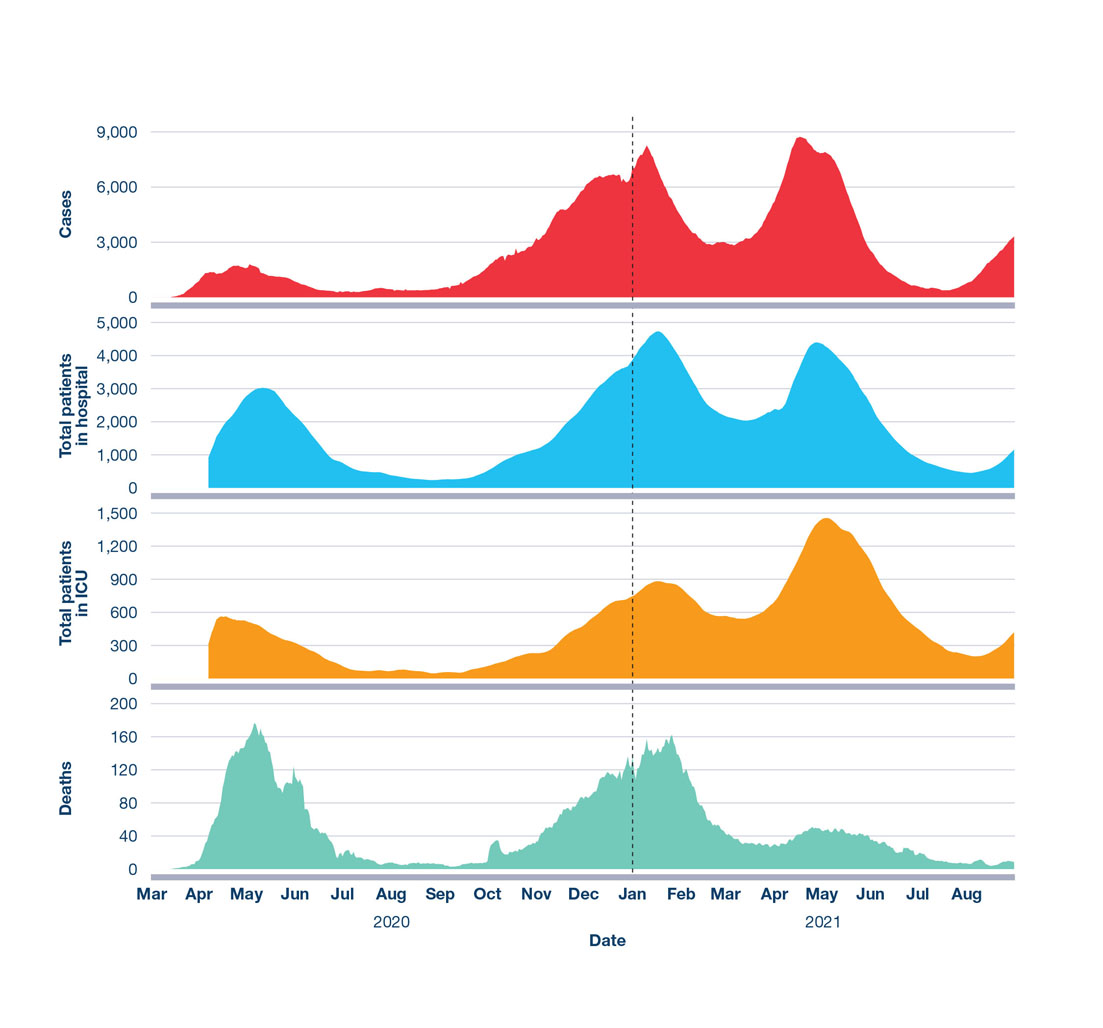
Figure 1: Text description
The figure is an overview of Canada’s COVID-19 pandemic from March 2020 to August 2021. The vertical axes display 4 different indicators as 7-day moving averages of daily data by reported date in separate panels, from top to bottom: cases, total patients in hospital, total patients in ICU, and deaths. The horizontal axis displays elapsed time in months.
| Date (selected time points) | Cases | Deaths | Total patients in hospital | Total patients in ICU |
|---|---|---|---|---|
| 2020-03-31 | 327.7 | 3.6 | Not available | Not available |
| 2020-04-30 | 1,427.1 | 88.9 | 1,939.0 | 514.0 |
| 2020-05-31 | 1,287.8 | 134.3 | 2,788.1 | 420.0 |
| 2020-06-30 | 491.0 | 55.0 | 1,398.3 | 219.7 |
| 2020-07-31 | 380.2 | 12.5 | 525.5 | 76.1 |
| 2020-08-31 | 398.7 | 6.5 | 287.1 | 65.7 |
| 2020-09-30 | 877.6 | 5.6 | 314.0 | 70.8 |
| 2020-10-31 | 2,329.1 | 24.9 | 890.5 | 177.9 |
| 2020-11-30 | 4,462.1 | 61.8 | 1,730.2 | 337.8 |
| 2020-12-31 | 6,456.4 | 107.9 | 3,234.5 | 637.0 |
| 2021-01-31 | 6,657.2 | 141.5 | 4,376.8 | 841.8 |
| 2021-02-28 | 3,295.6 | 78.6 | 2,836.8 | 655.1 |
| 2021-03-31 | 3,494.9 | 32.8 | 2,131.6 | 578.0 |
| 2021-04-30 | 7,628.2 | 39.8 | 3,423.8 | 1,072.6 |
| 2021-05-31 | 5,747.8 | 44.2 | 3,610.2 | 1,321.0 |
| 2021-06-30 | 1,321.7 | 26.5 | 1,577.6 | 706.3 |
| 2021-07-31 | 496.0 | 10.8 | 638.0 | 306.5 |
| 2021-08-31 | 1,966.8 | 7.7 | 671.3 | 265.0 |
Note that the vertical axes for each variable are differently scaled. All variables are 7-day moving averages of daily data by reported date. Complete hospitalization and ICU data are unavailable before April 2020Footnote 1.
The patterns of principal disease severity indicators changed over time. Compared to the first wave and despite significantly higher case counts, a smaller proportion of the total number of people with COVID-19 died, were hospitalized, or were admitted to ICU in the second and third waves (Table 1)Footnote 1. It is important to note that, once better testing and surveillance infrastructure became available after the first wave, the detection of mild and asymptomatic cases was more likelyFootnote 7. In addition to changes in testing, another factor that influenced this trend is better protection of those at higher risk of the most severe outcomes, such as residents of long-term care facilities, by enhanced public health interventions and targeted vaccination programs (further described below).
However, as a result of the prolonged high incidence and, therefore, the high number of ICU admissions (Figure 1), the third wave greatly challenged ICU capacity, especially in the most populous provincesFootnote 8. In some provinces, patients had to be transferred to other regions in response to overcrowded treatment settings, and many areas reduced or postponed elective medical procedures and surgeriesFootnote 8.
| COVID-19 indicators | Total number 1st wave (Jan 2020 – Aug 2020) |
Total number 2nd wave (Aug 2020 – Feb 2021) |
Total number 3rd wave (Feb 2021 – Aug 2021) |
|---|---|---|---|
| Cases | 126,707 | 751,158 | 640,293 |
| Males | 57,107 (45%) | 369,989 (49%) | 327,180 (51%) |
| Females | 69,383 (55%) | 380,177 (51%) | 311,806 (49%) |
| Other | 14 (<1%) | 56 (<1%) | 82 (<1%) |
| Case median age (range) | 47 years (0 to 119) | 37 years (0 to 115) | 33 years (0 to 113) |
| Deaths | 9,363 (7%) | 13,573 (2%) | 4,463 (1%) |
| Males | 4,294 (46%) | 6,931 (51%) | 2,627 (59%) |
| Females | 5,054 (54%) | 6,625 (49%) | 1,822 (41%) |
| Other | 0 (0%) | 0 (0%) | 0 (0%) |
| Death median age (range) | 86 years (0 to 112) | 85 years (0 to 109) | 75 years (1 to 105) |
| Hospitalizations | 13,428 (11%) | 36,251 (5%) | 29,920 (5%) |
| Males | 6,865 (51%) | 19,296 (53%) | 16,401 (55%) |
| Females | 6,554 (49%) | 16,924 (47%) | 13,477 (45%) |
| Other | 0 (0%) | 2 (<1%) | 3 (<1%) |
| Hospitalizations median age (range) | 73 (0 to 106) | 71 (0 to 108) | 59 (0 to 107) |
| ICU admissions | 2,733 (2%) | 5,996 (1%) | 6,557 (1%) |
| Males | 1,740 (64%) | 3,798 (63%) | 4,024 (61%) |
| Females | 993 (36%) | 2,191 (37%) | 2,524 (38%) |
| Other | 0 (0%) | 0 (0%) | 0 (0%) |
| ICU admissions median age (range) | 65 (0 to 99) | 66 (0 to 104) | 59 (0 to 99) |
| This data may be influenced by variation in testing approaches over time as well as between regions. In addition, some evidence suggested that COVID-19-related deaths were undercounted in the spring and fall of 2020Footnote 9. The denominator for the deaths, hospitalizations, and ICU admissions percentages is the total number of reported cases. For each disaggregation by gender/sex the denominator is the total number for each respective indicatorFootnote 1. | |||
Each wave of the pandemic in Canada has been marked by key characteristics (summarized in Table 2). This section describes some of the main epidemiological features of the pandemic, with a primary focus on the period between August 2020 and August 2021.
| Time period | Brief description of key characteristics |
|---|---|
1st wave (Jan 2020 – Aug 2020) |
|
2nd wave (Aug 2020 – Feb 2021) |
|
3rd wave (Feb 2021 – Aug 2021) |
|
4th wave (began Aug 2021) |
|
| For references and more detail on these topics, refer to the following content. The details of this section were finalized in August 2021; therefore, the included data do not represent a complete review of the fourth wave. | |
Second wave: August 2020 – February 2021
Easing of public health measures fuelled epidemic growth
By the summer of 2020 at the end of the first wave, nationally reported COVID-19 cases had declined to low levels (Figure 1)Footnote 1. Although there was variation among jurisdictions, many of the most restrictive public health measures implemented as part of Canada’s initial pandemic response, such as closures of businesses, workplaces and schools, stay-at-home orders, cancellation of public events, and restrictions on social gatherings, were relaxed. International border protocols, case detection and isolation, and contact tracing, as well as advice around individual personal preventive practices and population-based measures to reduce contacts, remained in placeFootnote 10.
Canadians’ increasing contact rates amplified the spread of the virus by the fall of 2020Footnote 11. At the time, mathematical modelling predicted that, if these rates of contact were maintained, the epidemic could quickly resurge with higher case countsFootnote 11. This was an early warning indicator for the large second wave that began at the end of August 2020, and peaked nationally in January 2021 (Figure 1)Footnote 1. While long-term care facilities continued to be the most frequent outbreak setting, social gatherings and workplace outbreaks greatly contributed to community spread in the second wave, especially as infection rates increased among younger, more socially active and mobile age groups with higher contact ratesFootnote 12.
In the winter of 2020-21, in response to surging numbers of cases and hospitalizations (Figure 1), many areas of the country reintroduced more restrictive public health measuresFootnote 10. With the resulting decline in cases to less than half of the daily number peak observed in January 2021, many regions eased restrictions by March 2021 before tightening them once again in April 2021Footnote 8. This was in line with modelling forecasts that accurately predicted another surge in cases that would become the third waveFootnote 13.
Public health measures were the primary tools available to limit spread
During most of the second wave, public health measures continued to be the primary means to manage the epidemic in Canada, since effective pharmaceutical interventions (e.g., vaccines) were not yet widely available. Implemented measures included a range of interventions to reduce community transmission of SARS-CoV-2 with the goal of “minimizing serious illness and overall deaths while minimizing societal disruption”Footnote 14. These encompassed both individual practices (e.g., masks, physical distancing, hand hygiene) and population-based measures (e.g., case management and contact tracing, school and business closures, stay-at-home orders)Footnote 15. It was difficult to mitigate the social, psychological, and economic consequences of public health measures, while also reducing transmission by limiting community-wide contact rates. In addition, some individuals had limited ability to follow recommendations as a result of their health, age, economic, or social circumstancesFootnote 15.
Public health authorities at federal, provincial/territorial, and local levels adapted public health measures as new scientific evidence and expert opinion from Canadian and international researchers became available. For instance, outbreak investigations and scientific studies revealed that SARS-CoV-2 can spread via respiratory droplets that vary in size, from large droplets that fall to the ground rapidly near the infected person, to smaller droplets, called aerosols, that linger in the air in some circumstancesFootnote 16. Short-range aerosol transmission was suggested to be particularly relevant for poorly ventilated indoor crowded spacesFootnote 16. As a result, the Public Health Agency of Canada (PHAC) updated guidance on the construction, fit, and proper wearing of face masks and on improving indoor ventilation during the second waveFootnote 17 Footnote 18 Footnote 19. National guidance on public health measures was based on pan-Canadian pandemic planning that jurisdictions adapted to their local epidemiological context, such as using curfews or designating more granular regional zones, to tailor approaches specific to the local areaFootnote 10 Footnote 14.
The pandemic response required rapid adoption and broad acceptance of public health measures, with consistent and sustained adherence for extended periods of time. Many Canadians reported high adherence to, and support of the use of, measures to limit the spread of the virusFootnote 20 Footnote 21 Footnote 22 Footnote 23. For example, a survey conducted by Impact Canada in March 2021 indicated that the vast majority of respondents were “always” or “almost always” complying with measures, such as mask wearing, hand washing, and physical distancingFootnote 24. Statistical modelling indicated that the strongest factors driving adherence to public health measures include anxiety related to family’s health, trust in government sources, and trust in medical expertsFootnote 25.
A variety of non-traditional data sources provided insight into overall adherence to public health measures that aimed to reduce movement and contact with others. For example, mobility data gathered from cellular networks showed that there was a significant decrease in the proportion of time Canadians spent at home after the first wave, which appears to align with the relaxation of public health measuresFootnote 10. While there were a variety of factors that influenced adherence to public health measures, it is important to note that some people had higher mobility and more contact with others regardless of the measures, due to factors such as essential work or high-density housing arrangements, respectivelyFootnote 26.Third wave: February 2021 – August 2021
Highly transmissible variants of concern contributed to rapid epidemic growth
Following a decline in average daily cases nationally from January through February 2021, infection rates rose sharply in March 2021 in most provinces and territories (Figure 1)Footnote 1. This was driven by increased contact rates following the easing of restrictions and the emergence and spread of more contagious virus variants of concernFootnote 13. As with all viruses, SARS-CoV-2 accumulates genetic mutations over time. Some of them may lead to virus variants that are considered to be variants of concern because they spread more easily, cause more severe illness, or decrease the effectiveness of available diagnostics, vaccines, therapeutics, or public health measuresFootnote 27. In early 2021, more contagious virus variants began to be detected in Canada, and as of August 2021, included the Alpha, Beta, Gamma, and Delta variants. These variants of concern had spread to most provinces and territories and were responsible for about 80% of all cases in August 2021Footnote 28. While Alpha initially accounted for the majority of national COVID-19 cases at the beginning of the third wave, in early July 2021, Delta replaced Alpha as the most frequently reported variantFootnote 28.
Early evidence from Ontario suggested that, compared to the original strain of SARS-CoV-2, the Alpha variant was associated with a 62% increase in hospitalizations, a 114% increase in ICU admissions, and a 40% increase in deaths, among those infectedFootnote 29. Preliminary findings indicated that the Delta variant was more transmissible and also more virulent than the Alpha variantFootnote 30.
International border measures were deployed and adjusted over time as knowledge of SARS-CoV-2 and variants of concern evolved. Throughout the pandemic, air and land traveller volumes remained at less than 90% of pre-pandemic levelsFootnote 31. To further reduce the risk of virus importation, especially variants of concern, Canada implemented enhanced testing and quarantine measures at international borders, in addition to those already in place, beginning in the winter of 2020-21. These included mandatory testing before departure and in-Canada for all non-exempt travellers, as well as a 3-day mandatory hotel stopover in a government-approved accommodation for non-exempt travellers arriving by air at the 4 main airports permitting international arrivalsFootnote 32.
In early 2021, Canada quickly increased surveillance and genomic sequencing efforts to detect known and emerging variants of concernFootnote 33. PHAC worked with partners at all levels of government as well as academic researchers to establish a pan-Canadian surveillance network that used new genetic assays to detect SARS-CoV-2 variants from wastewater samplesFootnote 34. This acted as part of a system of early warning indicators, in combination with predictions from mathematical models, which facilitated the adaptation of the COVID-19 response to evolving information. For example, in the Northwest Territories, a positive COVID-19 signal in wastewater led to the identification of an infected individual, prompting wider community testing. This rapid response allowed for the early detection of additional COVID-19 cases, which interrupted further spread and potentially prevented a larger outbreakFootnote 34.
COVID-19 vaccines as vital tools to control the virus
Towards the end of 2020, less than a year after the emergence of the SARS-CoV-2 virus, researchers developed the first safe and effective COVID-19 vaccines – a feat unprecedented in scientific history. This marked a turning point in the response to the pandemic. These vaccines were the result of collaboration of academic and private sector researchers around the world and increased funding that, together, enabled them to build on scientific and technological advancements made over the past decadeFootnote 35. For information on how vaccines protect populations, see text box “Vaccines provide protection for everyone through enhanced community protection”.
On December 9, 2020, Canada authorized the first COVID-19 vaccine, which uses novel messenger RNA (mRNA) technology, for use in adults in CanadaFootnote 36. Subsequent vaccine authorizations included another mRNA-based vaccine as well as viral vector-based vaccines. At the time, most required 2 doses for the best possible protectionFootnote 37. Rapid authorization was supported by the ability of Health Canada to review new evidence as it became available, and the dedication of more scientific resources to the vaccine safety and efficacy review processFootnote 38 Footnote 39. Vaccine safety assessment and monitoring is an ongoing process throughout a vaccine’s life cycle (see text box “Creation of the Vaccine Injury Support Program”). As of August 31, 2021, over 53 million doses of safe and highly effective vaccine products had been administered in CanadaFootnote 40.
Vaccines provide protection for everyone through enhanced community protection
Vaccines are one of the most important preventive health interventions for many serious infectious diseases. They can provide both direct protection for vaccinated individuals as well as indirect protection for a community. The higher the proportion of people vaccinated, the less opportunity a pathogen has to circulate, thereby minimizing the risk of larger outbreaks. High community vaccination rates further protect those who cannot be vaccinated, or who are not as well protected by vaccination, and reduce the opportunities for the pathogen to mutateFootnote 41. This enhanced community-level protection is especially important for those at highest risk of severe health outcomes, including hospitalization and death. Mass vaccination is one of the most effective ways to protect the population against COVID-19Footnote 42.
The distribution and administration of COVID-19 vaccines was the largest and most complex vaccination program Canada has ever implemented. The federal government took on the responsibility of procuring vaccines, overseeing logistics, coordinating surveillance, and working very closely with provincial/territorial governments, as well as public health partners, to ensure a timely, fair, and well-coordinated rolloutFootnote 43.
Canada’s National Advisory Committee on Immunization (NACI) provided independent expert advice to support the provinces and territories in prioritizing an initially limited supply of COVID-19 vaccines. NACI takes into consideration the broader, real-world context and the best evidence available at the time when making recommendationsFootnote 44. NACI identified the key populations for prioritization in Stage 1 of their Guidance on the Prioritization of Initial Doses of COVID-19 Vaccine(s) to be residents and staff of congregate living settings that provide care for seniors, adults aged 70 years or older, healthcare workers, and adults living in Indigenous communitiesFootnote 45. These populations were generally considered at greatest risk of severe illness and in most urgent need of protection. Before offering vaccines to the general population as vaccine supply increased, NACI recommended that Stage 2 of the vaccine rollout include healthcare workers not part of Stage 1, residents and staff of all other congregate settings, and essential workersFootnote 45. In March 2021, based on emerging evidence of the degree of protection provided by one dose, NACI recommended that jurisdictions extend the interval for those vaccines requiring a second dose to maximize the number of people with some protection and reduce transmission in the context of limited initial vaccine supplyFootnote 46. Provincial and territorial governments, who were responsible for delivering and administering vaccines, largely adopted NACI’s recommendations.
Creation of the Vaccine Injury Support Program
All vaccines authorized for use in Canada meet the highest standards for safety and efficacyFootnote 47. As with any medication, vaccines may cause reactions and side effects. Severe adverse events are very rare, but they do occurFootnote 47. PHAC created the federal Vaccine Injury Support Program to offer fair and timely compensation to Canadians who have experienced a serious and permanent injury as a result of receiving any Health Canada-authorized vaccine administered in Canada on or after December 8, 2020Footnote 47 Footnote 48. This no-fault program builds on a program that Quebec has had in place for over 30 years and brings Canada in line with other Group of Seven (G7) countriesFootnote 47. Vaccine injury compensation can also support vaccine innovation and procurement by reducing legal risks for manufacturersFootnote 49.
Once initial vaccine supply limitations were overcome, vaccine delivery rapidly accelerated beginning in the spring of 2021. Beneficial vaccine impacts became readily apparent in prioritized populations, such as among long-term care facility residents and people who work in healthcare settings, who saw significant decreases in COVID-19 cases as vaccine coverage increasedFootnote 50. Early evidence showed that COVID-19 vaccines are highly protective, especially at preventing severe outcomes. Between July 18, 2021 and August 14, 2021, data from 11 provinces and territories revealed that the average rate of new COVID-19 cases was 12 times higher among unvaccinated people, and the rate of COVID-19 hospitalizations was 36 times higher among unvaccinated people than in fully vaccinated individualsFootnote 51. Strengthened public health measures in combination with increasing vaccination coverage brought COVID-19 activity to low levels in most areas of Canada by July 2021 (Figure 1)Footnote 52. This also allowed for Canada to begin a phased approach to easing border measures for fully vaccinated travellersFootnote 53.
Disproportionate impacts of the second and third waves of the pandemic
The second and third waves of the pandemic looked different from the first wave. Some areas and populations faced continued difficulties and/or new challenges. Evolving science and lessons learned led to jurisdictions adapting their public health response, which changed the dynamics of subsequent waves. This section will discuss some of the key observations made during later waves, including the continued disproportionate impact on Canadians who experienced poorer health, social, and economic circumstances prior to the pandemic due to pre-existing inequitiesFootnote 14.
COVID-19 spread differently across the country
In contrast to the first wave, subsequent waves of the pandemic were felt all across the country. However, not all regions experienced distinct second and third waves at the same time or with the same intensity (Figure 2).
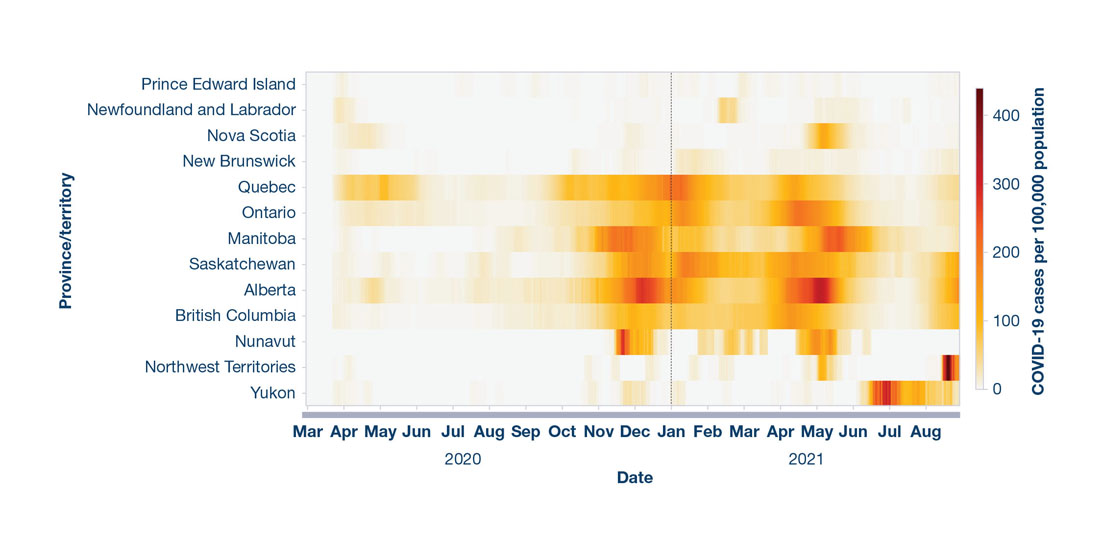
Figure 2: Text description
The figure is a heat map describing the rate of COVID-19 cases per 100,000 population for each province/territory over time from March 2020 to August 2021. The 2 vertical axes display the number of COVID-19 cases per 100,000 population and by province or territory, respectively. The horizontal axis displays elapsed time in months. A colour gradient using light (i.e., low) to dark (i.e., high) shading indicates rate changes over time.
| Date (selected time points) | NU | NT | YT | BC | AB | SK | MB | ON | QC | NB | PE | NS | NL |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2020-03-31 | 0.0 | 0.3 | 1.9 | 2.3 | 2.0 | 1.9 | 0.8 | 1.4 | 6.2 | 1.1 | 1.5 | 2.0 | 4.7 |
| 2020-04-30 | 0.0 | 2.1 | 4.0 | 5.3 | 21.7 | 4.6 | 3.5 | 21.6 | 61.0 | 2.0 | 2.1 | 18.9 | 6.4 |
| 2020-05-31 | 0.0 | 0.0 | 0.0 | 2.4 | 11.6 | 5.3 | 0.4 | 18.4 | 64.9 | 0.2 | 0.1 | 3.6 | 0.1 |
| 2020-06-30 | 0.0 | 0.0 | 0.0 | 1.5 | 5.3 | 2.6 | 0.5 | 12.1 | 15.1 | 1.2 | 0.0 | 0.2 | 0.0 |
| 2020-07-31 | 0.0 | 0.0 | 1.6 | 2.8 | 12.8 | 8.8 | 1.3 | 6.7 | 9.8 | 0.1 | 1.3 | 0.1 | 0.2 |
| 2020-08-31 | 0.0 | 0.0 | 0.5 | 8.5 | 15.1 | 7.2 | 11.6 | 4.7 | 8.6 | 0.6 | 1.1 | 0.3 | 0.1 |
| 2020-09-30 | 0.0 | 0.0 | 0.0 | 15.1 | 21.9 | 5.2 | 12.8 | 12.7 | 26.6 | 0.3 | 2.1 | 0.1 | 0.2 |
| 2020-10-31 | 0.0 | 2.2 | 3.8 | 22.0 | 45.8 | 20.1 | 48.6 | 35.2 | 81.7 | 4.0 | 0.8 | 0.4 | 0.8 |
| 2020-11-30 | 96.1 | 2.9 | 11.1 | 77.2 | 142.6 | 93.9 | 183.6 | 60.7 | 96.1 | 4.1 | 1.0 | 3.9 | 1.8 |
| 2020-12-31 | 59.3 | 4.5 | 9.6 | 86.1 | 229.7 | 138.7 | 139.0 | 96.1 | 148.9 | 3.4 | 3.4 | 4.8 | 2.5 |
| 2021-01-31 | 10.7 | 3.5 | 5.4 | 69.2 | 124.2 | 157.1 | 81.6 | 135.5 | 168.2 | 17.5 | 2.2 | 2.3 | 0.7 |
| 2021-02-28 | 44.2 | 6.1 | 1.2 | 61.3 | 54.1 | 108.0 | 45.4 | 59.3 | 77.7 | 7.3 | 1.6 | 1.3 | 27.0 |
| 2021-03-31 | 23.6 | 0.0 | 0.5 | 81.3 | 70.9 | 91.8 | 36.9 | 69.8 | 60.4 | 4.4 | 5.0 | 1.9 | 2.1 |
| 2021-04-30 | 46.0 | 4.2 | 4.3 | 134.5 | 205.3 | 146.5 | 69.4 | 173.1 | 104.7 | 8.9 | 3.1 | 11.9 | 2.1 |
| 2021-05-31 | 0.0 | 0.0 | 0.0 | 2.4 | 11.6 | 5.3 | 0.4 | 18.4 | 64.9 | 0.2 | 0.1 | 3.6 | 0.1 |
| 2021-06-30 | 6.2 | 0.4 | 110.0 | 18.1 | 28.8 | 48.1 | 99.2 | 25.1 | 14.3 | 4.3 | 0.7 | 8.0 | 4.2 |
| 2021-07-31 | 0.0 | 0.0 | 158.1 | 8.7 | 10.8 | 21.1 | 25.8 | 8.7 | 6.6 | 0.9 | 0.2 | 1.4 | 2.3 |
| 2021-08-31 | 0.0 | 134.7 | 57.9 | 64.3 | 81.8 | 71.7 | 17.3 | 21.0 | 28.2 | 10.9 | 3.0 | 2.8 | 1.4 |
| Provinces/Territories listed in table are abbreviated using the alpha code. | |||||||||||||
Daily data are shown by province and territory and by reported dateFootnote 54.
National incidence rates were driven by the provinces west of the Atlantic region, partly due to population size and densityFootnote 54. Since the first wave, the Atlantic provinces were largely able to sustain sufficient measures (e.g., interprovincial travel restrictions) to manage and limit case importations, interrupt spread, and maintain strong control of COVID-19 (Figure 2)Footnote 55 Footnote 56 Footnote 57. However, there were surges that provincial governments quickly interrupted with rapid implementation of stringent public health measures to prevent further spread. These measures were particularly important given limited health system capacity in some of these jurisdictions.
Other regions that had relatively low COVID-19 rates in the first wave saw an increase in disease activity after the summer of 2020. For example, while the territories had no to very few cases initially, by late 2020, some communities experienced a rapid rise in cases, with community transmission following importation of the virus (Figure 2)Footnote 54. This necessitated fast implementation of stringent public health measures locally and territorially to prevent further spread. The territories, whose communities were prioritized in the initial vaccination rollout, achieved high vaccine uptake and, as of July 20, 2021, 84% of adults aged 18 years or older had received at least one dose of a COVID-19 vaccine and 76% were fully vaccinatedFootnote 40. The territories’ early success in expanding vaccine coverage was supported by prioritized allocation of vaccines that were somewhat easier to transport and store as well as robust community-level outreach and leadershipFootnote 58 Footnote 59 Footnote 60.
Shift towards spread in younger Canadians
As older Canadians became better protected through public health measures, adaptation of the COVID-19 response in long-term care facilities, and ultimately, high vaccination rates, the median age of COVID-19 cases dropped (Table 1)Footnote 1. Until the end of the second wave, Canadians aged 80 years or older had the highest national incidence rate. However, starting in early 2021, incidence rates in this age group decreased sharply. At the time of report writing in August 2021, Canadians aged 80 years or older had maintained the lowest incidence rates out of all age groups since March 2021 (Figure 3), largely as a result of high vaccine coverageFootnote 1. As of August 28, 2021, 93% of adults aged 80 years or older were fully vaccinated against COVID-19Footnote 40.
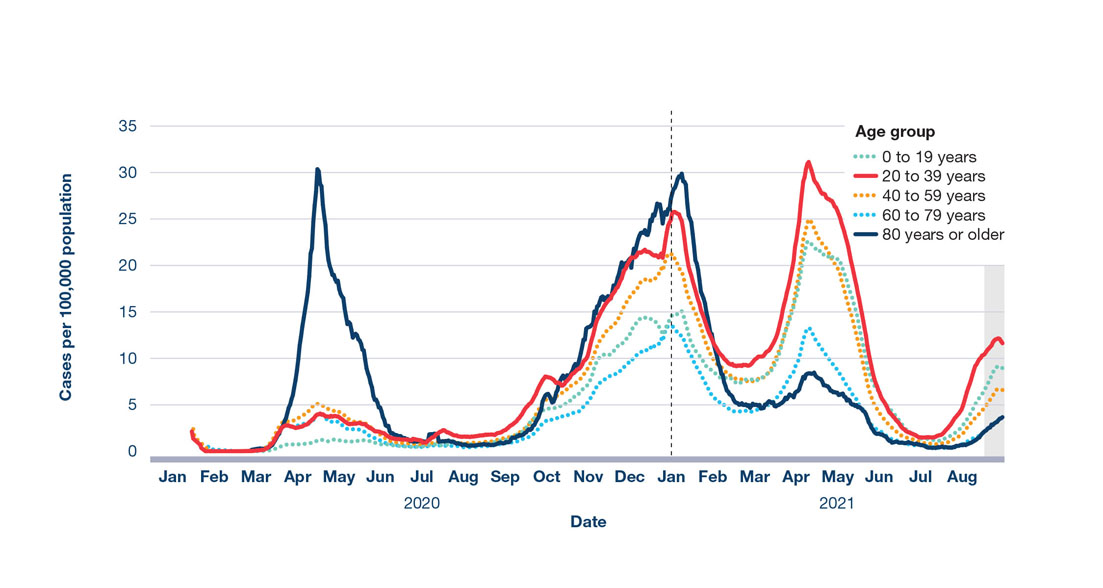
Figure 3: Text description
The figure is a line graph displaying the number of COVID-19 cases by date of illness onset and age group in Canada from January 2020 to September 2021. The vertical axis displays the number of cases (7-day moving average) per 100,000 population. The horizontal axis displays the date of illness onset in months. The age groups are represented by different coloured trend lines: green (0 to 19 years), red (20 to 39 years), orange (40 to 59 years), light blue (60 to 79 years), and dark blue (80 years or older). The 20 to 39 years and 80 years or older age groups are displayed as solid lines, respectively, to better indicate their trend change over time, versus dashed lines for all other groups.
| Date (selected time points) |
0 to 19 years | 20 to 39 years | 40 to 59 years | 60 to 79 years | 80 years or older |
|---|---|---|---|---|---|
| 2020-01-31 | 0.0 | 0.5 | 0.7 | 0.8 | 1.2 |
| 2020-02-29 | 0.0 | 0.0 | 0.0 | 0.0 | 0.3 |
| 2020-03-31 | 0.4 | 1.4 | 1.8 | 1.5 | 2.2 |
| 2020-04-30 | 1.0 | 3.4 | 4.5 | 3.3 | 20.3 |
| 2020-05-31 | 1.1 | 2.9 | 3.1 | 2.2 | 11.4 |
| 2020-06-30 | 0.6 | 1.4 | 1.0 | 0.7 | 1.9 |
| 2020-07-31 | 0.7 | 1.7 | 0.9 | 0.6 | 1.2 |
| 2020-08-31 | 0.9 | 1.8 | 1.0 | 0.6 | 0.7 |
| 2020-09-30 | 2.8 | 4.8 | 2.9 | 1.6 | 2.5 |
| 2020-10-31 | 5.6 | 8.2 | 6.8 | 4.0 | 8.4 |
| 2020-11-30 | 10.6 | 16.1 | 13.0 | 7.8 | 17.1 |
| 2020-12-31 | 13.8 | 21.6 | 18.7 | 11.3 | 24.2 |
| 2021-01-31 | 11.6 | 19.0 | 15.6 | 9.9 | 22.3 |
| 2021-02-28 | 7.8 | 9.7 | 8.3 | 4.7 | 6.6 |
| 2021-03-31 | 10.4 | 13.1 | 10.3 | 5.8 | 2.2 |
| 2021-04-30 | 20.9 | 27.7 | 22.0 | 11.1 | 7.4 |
| 2021-05-31 | 13.7 | 17.3 | 12.3 | 5.5 | 4.6 |
| 2021-06-30 | 3.4 | 3.4 | 0.7 | 1.2 | 1.1 |
| 2021-07-31 | 1.5 | 2.2 | 1.0 | 0.5 | 0.5 |
| 2021-08-31 | 6.2 | 9.5 | 4.5 | 2.0 | 1.9 |
All variables are 7-day moving averages of daily data by date of illness onset. Shaded area indicates data uncertainty due to reporting lagFootnote 1.
Age is one of the most significant risk factors for developing severe COVID-19Footnote 61 Footnote 62. Despite the decrease in overall case burden, as of the end of August 2021, Canadians aged 80 years or older continued to have the highest rate of COVID-19 deaths per 100,000 population. However, this rate fell significantly after the second waveFootnote 1. Of the 15,300 people who died of COVID-19 in 2020, 89% had at least one other health condition listed on their death certificate. Dementia and Alzheimer’s disease were the most common conditions, followed by hypertensive disease, diabetes, and ischemic heart diseaseFootnote 63.
Emerging evidence also showed an increased rate of pre-term births and stillbirths among pregnant people with COVID-19Footnote 64. Compared to their non-pregnant counterparts, pregnant people testing positive for COVID-19 were 4 times more likely to be hospitalized and 11 times more likely to be admitted to the ICUFootnote 64.
One of the key differences between the first wave of the pandemic and subsequent waves was a shift to more widespread detection of community transmission in younger adults. Individuals aged 20 to 39 years, who generally have higher contact rates and thereby an increased risk of virus exposure, have had the highest incidence rate since February 2021 (Figure 3)Footnote 1. Although severe illness is less common in younger individuals, in the spring of 2021, the number of COVID-19 hospitalizations in individuals aged 40 to 59 years increasedFootnote 57. This was likely due to a combination of the shift in the age distribution of cases as a result of better protection of older age groups, the increased severity of some variants of concern, and the easing of public health measures.
Differential impact of COVID-19 across the sexes and genders
Since the summer of 2020, women and men accounted for an equal proportion of COVID-19 cases (Table 1)Footnote 1. This is in contrast to the first wave when women made up 55% of all cases, possibly due to their overrepresentation among healthcare workers and residents of long-term care facilities, and therefore an increased probability of being exposed to, and tested for, the virusFootnote 5. This could also explain the larger percentage of deaths in women during the first wave. During the second and third waves, these groups may have been better protected by improved access to personal protective equipment and vaccinesFootnote 65.
However, men comprised a larger percentage of hospitalized cases and ICU admissions throughout the pandemic as well as a larger percentage of deaths after the first wave (Table 1)Footnote 1. Researchers propose that fundamental biological differences mainly tied to immunology are a likely driver of the increased risk of severe outcomes from COVID-19 in males. Behavioural differences, such as men being more likely to smoke and less likely to seek health care, could also be possible influencing factorsFootnote 66 Footnote 67 Footnote 68 Footnote 69.
Variation in impacts across different outbreak settings
Long-term care facilities
Long-term care facilities remained a high-risk setting in many provinces and territoriesFootnote 8. However, the proportion of total COVID-19-related deaths associated with these facilities dropped from 79% during the first wave to 50% during the second and third wavesFootnote 1. Beginning in January 2021, the number and size of outbreaks in these settings steadily declined, largely due to the impact of vaccinationsFootnote 8.
Healthcare settings
In April 2020, 25% of all COVID-19 cases were in people who work in healthcare settingsFootnote 1. Due to improved infection control measures, vaccine prioritization, as well as wider community case detection outside healthcare settings, this proportion dropped to 3% by March 2021Footnote 1. People who work in healthcare settings represent a wide range of individuals including healthcare professionals and support workers, who experience varying risks of exposure to SARS-CoV-2 in the workplace. For example, based on data from Ontario, Manitoba, and British Columbia, personal support workers had a 1.8 times greater risk compared to nurses and a 3.3 times greater risk compared to physicians of contracting COVID-19Footnote 70.
Congregate living and working conditions
Federal prisons reported a substantial increase in COVID-19 cases during the winter of 2020-21. While 13 out of 43 institutions experienced outbreaks during the second wave, 70% of the total 880 cases occurred at the country’s 2 largest penitentiaries, one in Manitoba and one in SaskatchewanFootnote 71. Indigenous Peoples were disproportionately impacted as a result of overrepresentation in the prison system in CanadaFootnote 71. Vaccinations were accelerated for people incarcerated in federal institutions and, as of August 8, 2021, 78% of this population had received at least one dose of a COVID-19 vaccineFootnote 72.
Regional medical officers of health reported that workplace outbreaks became one of the most common drivers of transmission in some provinces and territories during the second and third wavesFootnote 73 Footnote 74 Footnote 75. Many jurisdictions experienced outbreaks at large employment sites where workers faced challenges in maintaining physical distancing. Many of these outbreaks required additional efforts to contain. For example, the Canadian Red Cross provided contact tracing in response to a COVID-19 variant of concern outbreak at a fly-in mine in Nunavut for employees who had left the work location and returned to homes across the countryFootnote 76. As in the first wave, several public health authorities reported large outbreaks at meat-processing plants during subsequent waves, some of which required temporary facility closuresFootnote 77 Footnote 78. This led several jurisdictions to prioritize vaccinations for food-manufacturing workersFootnote 79 Footnote 80.
Tracking workplace outbreaks at a provincial/territorial and national level was limited, but is necessary for the adoption of policy measures targeting specific industries and settings to limit future spreadFootnote 81. Some local authorities launched initiatives during the pandemic to collect this type of data. For example, Toronto Public Health began publicly posting the names of workplaces in active outbreaks that employ 20 people or more, and Ottawa Public Health required employers to report if 2 or more people in their workplace tested positive for COVID-19Footnote 82 Footnote 83.
COVID-19 burden disproportionately impacted certain communities
During the first wave, neighbourhoods in Canada in the highest ethno-cultural composition quintile had an age-standardized COVID-19 mortality rate 2 times higher than those in the lowest quintileFootnote 69 Footnote 84 Footnote 85. Similarly, Canadians living in areas in the lowest income quintile had twice the age-standardized COVID-19 mortality rate compared to Canadians living in areas in the highest quintileFootnote 69 Footnote 84. In both analyses, men had much higher mortality rates compared to womenFootnote 69 Footnote 84.
While these populations had differential exposure to SARS-CoV-2 due to factors such as essential work and living conditions, the reasons for the differences in mortality rates include long-standing socioeconomic differences in the distribution of underlying risk factors and access to health careFootnote 5 Footnote 86. While similar national data for the second and third waves were not available at the time of report writing, racialized communities and low-income groups in general were likely to continue experiencing higher rates of COVID-19 and severe outcomes in subsequent waves. This is a result of the fundamental inequities that predate the pandemic and continued disproportionate risk of SARS-CoV-2 exposure.
Seroprevalence data collected from blood donors in May 2021 indicated that racialized donors were more than twice as likely to have antibodies acquired through past COVID-19 infectionFootnote 87. Additionally, Toronto Public Health reported that, between May 20, 2020 and May 31, 2021, 73% of all individuals testing positive for SARS-CoV-2 identified with a racialized group, which usually make up 52% of the Toronto population. Similarly, 45% of reported cases were in individuals living in lower-income households, which represent 30% of the population of TorontoFootnote 88.
Recognizing that a possible inequitable allocation of vaccines threatened to exacerbate social and health inequities already intensified by the pandemic, in February 2021, NACI updated their initial guidance on the prioritization for COVID-19 vaccinations in Canada to include adults in racialized communities disproportionately affected by COVID-19Footnote 89. As with other national guidance, jurisdictions adapted these recommendations based on their own local context.
For instance, after analysis revealed unequal vaccine coverage across Ontario, likely as a result of complex institutional and social factors, the province diverted 50% of its vaccine supply to hotspots with the highest incidence of infection for 2 weeks in May 2021Footnote 90. These neighbourhoods often had higher concentrations of racialized and low-income populations as well as the highest proportion of essential workers.
Place-based targeting of vaccines (e.g., geographic hotspots) also needed to be accompanied by initiatives directly aimed at confronting social inequitiesFootnote 91. For example, the Health Association of African Canadians, the Association of Black Social Workers, and African Nova Scotian Affairs, along with community leaders, hosted vaccine clinics for members of African Nova Scotian communitiesFootnote 92. Additionally, many urban centres, including Montreal and Vancouver, prioritized vaccines for people experiencing homelessness in January 2021 and used targeted strategies to increase vaccine uptake in this populationFootnote 93 Footnote 94.
COVID-19 and Indigenous communities
During the first months of the pandemic, First Nations, Inuit, and Métis communities swiftly took control of the response and worked collaboratively to successfully limit the spread of COVID-19Footnote 5. As in many areas of Canada, case numbers rose rapidly in many Indigenous communities during the second waveFootnote 95.
Given the intersection of social and economic challenges, and the lasting and ongoing impacts of intergenerational trauma and systemic oppression, Indigenous communities in general were at high risk for rapid spread of COVID-19 and potentially more severe outcomes compared to the general Canadian population. Difficulties included inadequate and crowded housing, geographic isolation, and reduced access to health and critical care servicesFootnote 5.
At the peak of the second wave in January 2021, the rate of new COVID-19 cases in First Nations living on-reserve was triple the rate in the general Canadian population (Figure 4)Footnote 95. Statistics on First Nations individuals who do not live on-reserve were unavailable nationally. However, regional evidence suggested that the COVID-19 burden may have been higher for those individuals residing off-reserve compared to those living on-reserve. For example, as of August 14, 2021, individuals that live off-reserve represented 56% of First Nations COVID-19 cases in British ColumbiaFootnote 96.
After successfully preventing any case importations during the first wave, Nunavut, whose population is 85% Inuit, reported its first COVID-19 case in November 2020 (Figure 2)Footnote 54 Footnote 97. The territory swiftly interrupted further outbreaks and prevented resurgences through targeted public health measures, including proactive wastewater surveillance testing and territorial travel restrictionsFootnote 98 Footnote 99 Footnote 100. As of August 31, 2021, Nunavut’s last reported case of COVID-19 occurred in June 2021, and the territory had administered at least one vaccine dose to 80% of the eligible populationFootnote 54 Footnote 60.
First Nations, Inuit, and Métis communities were prioritized for vaccines and demonstrated strong leadership in administering vaccination programs. Community groups, Indigenous governments, and leaders reacted quickly to set up clinics and provide culturally adapted educational materialsFootnote 101 Footnote 102 Footnote 103. Initiatives to safely and effectively deliver vaccines were implemented, such as Operation Remote Immunity, led by Ontario’s Ornge air ambulance service in partnership with Nishnawbe Aski Nation that provided vaccinations to 31 remote First Nations communities in the provinceFootnote 104.
Given prior experiences of stigmatization and racism, First Nations, Inuit, and Métis Peoples in Canada expressed a desire for knowledge and understanding of vaccine risks and benefits to come from trusted sources and for interventions to be specifically tailored to community needs and cultural practicesFootnote 105 Footnote 106. One such example was the partnership between the Indigenous Primary Health Care Council and the National Reconciliation Program at Save the Children for leading an Indigenous youth vaccine advocacy program. Young people developed social media strategies to share their reasons for getting vaccinated under the hashtags #IndigenousYouth4Vaccine and #SmudgeCOVIDFootnote 107. As of August 10, 2021, over 86% of individuals aged 12 years or older in First Nations, Inuit, and territorial communities had received at least one vaccine doseFootnote 95 Footnote 108.
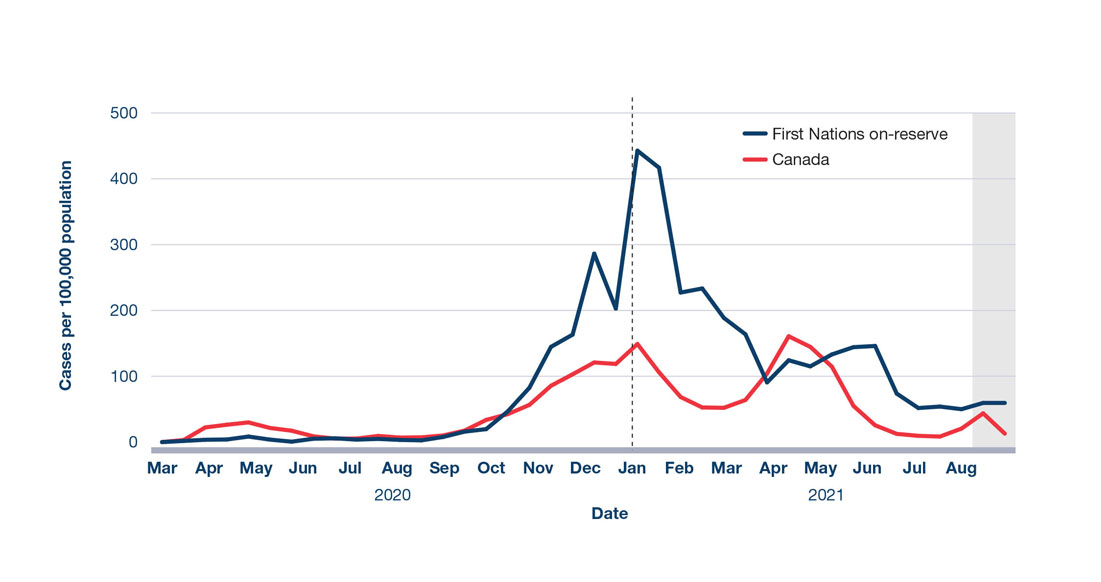
Figure 4: Text description
The figure is a line graph displaying the rate of reported COVID-19 cases in First Nations Peoples living on-reserve compared to the general Canadian population from March 2020 to August 2021. The blue line displays the number of cases in First Nations Peoples on-reserve and the red line displays the number of cases for all of Canada. The vertical axis show cases per 100,000 population. The horizontal axis displays date of illness onset in months.
| Date (selected time points) |
First Nations on-reserve | Canada |
|---|---|---|
| 2020-03-31 | 1.8 | 8.5 |
| 2020-04-30 | 6.2 | 28.1 |
| 2020-05-31 | 2.2 | 19.4 |
| 2020-06-30 | 5.4 | 7.1 |
| 2020-07-31 | 4.3 | 7.4 |
| 2020-08-31 | 4.6 | 8.1 |
| 2020-09-30 | 17.8 | 25.6 |
| 2020-10-31 | 64.6 | 49.5 |
| 2020-11-30 | 154.0 | 94.3 |
| 2020-12-31 | 244.6 | 119.9 |
| 2021-01-31 | 362.2 | 107.8 |
| 2021-02-28 | 211.1 | 52.3 |
| 2021-03-31 | 127.2 | 84.1 |
| 2021-04-30 | 119.7 | 152.7 |
| 2021-05-31 | 138.7 | 84.8 |
| 2021-06-30 | 109.8 | 19.0 |
| 2021-07-31 | 52.9 | 9.0 |
| 2021-08-31 | 56.3 | 25.7 |
All variables are weekly data by date of illness onset. Shaded area indicates data uncertainty due to reporting lagFootnote 95.
Expected impact of vaccination on the fourth wave
At the time of report writing in August 2021, rising incidence signalled the beginning of a fourth wave (Figure 1). Driven primarily by the more contagious Delta variant, long-range modelling in July 2021 predicted that daily cases in the fall of 2021 could exceed previous wave peaks as many jurisdictions planned to move into the final phases of their reopening plansFootnote 30 Footnote 109.
As of August 28, 2021, 83% of the eligible population in Canada had received at least one dose of a COVID-19 vaccine and 76% were fully vaccinatedFootnote 40. Given ramp-up in vaccination coverage at the population level, the epidemiology and associated public health response for this wave was expected to be significantly different than in the past. Public health experts anticipated that transmission would be concentrated in areas with lower vaccine coverage and among children not yet eligible for vaccination as schools reopened for in-person learningFootnote 109.
Achieving high vaccination coverage across eligible populations was predicted to significantly reduce the severity profile of disease going forward. However, updated modelling in August 2021 showed that there was still the potential for healthcare capacity to be overwhelmed if less than 80% of the eligible population remained not fully vaccinated, especially among Canadians aged 18 to 39 years, and if additional easing of public health measures further increased contact rates. This was partly due to the elevated risk of hospitalization and ICU admission associated with the Delta variant, particularly in unvaccinated individualsFootnote 51.
In the summer of 2021, many jurisdictions focused on increasing vaccine uptake using more targeted campaigns (see text box “Supporting vaccine confidence in Canada”). Several regions also required proof of vaccination for certain groups or for participation in certain activitiesFootnote 109. For example, in August 2021, Quebec became the first province to announce that individuals would need to be adequately vaccinated (or granted an exemption for medical reasons) to access some non-essential servicesFootnote 110. Alberta Health Services also announced plans to require all employees and contracted healthcare providers to be fully vaccinatedFootnote 111.
Supporting vaccine confidence in Canada
National survey results from September to December 2020 found that 77% of Canadians aged 12 years or older reported being “somewhat” or “very willing” to receive the COVID-19 vaccineFootnote 112. By February 2021, after the administration of vaccines was underway, this percentage rose to 82%Footnote 113. Reported reasons for vaccine hesitancy are multifaceted, including concerns about vaccine safety and effectiveness, the accessibility of vaccination services, and mistrust of the vaccine approval processFootnote 105 Footnote 114 Footnote 115 Footnote 116. Overcoming vaccine hesitancy is critical to the ongoing management of COVID-19, since achieving high vaccine coverage is necessary to limit future outbreaks. In recognition of this, many communities and businesses, as well as all levels of government, considered opportunities to support vaccine uptake. One example of an initiative to encourage vaccine uptake and vaccine confidence is the Vaccine Community Innovation Challenge. Through this initiative, the Government of Canada selected up to 140 creative projects that will develop and execute information campaigns to empower community leaders to increase people’s confidence in COVID-19 vaccines and reinforce public health measures targeted at populations that were more greatly impacted by the pandemicFootnote 117. This challenge is one of several programs, including others that were part of the Immunization Partnership Fund, that supported increasing vaccine confidence and addressing mis- and disinformation by engaging trusted community voicesFootnote 117.
Given high vaccine coverage, jurisdictions planned to focus the public health response more on localized surges in cases and monitoring severity indicators rather than applying broad restrictive public health measures. Ensuring sufficient public health system capacity was especially important as other pressing health priorities and a return to a more typical influenza/respiratory virus season would put added pressure on an already exhausted public health workforceFootnote 118. Personal protective measures such as staying home when sick, hand hygiene, and respiratory etiquette continued to be important even after jurisdictions lifted restrictive public health measures. However, it was imperative to remain responsive to signals of increased SARS-CoV-2 activity, maintain vigilance and preparedness for existing and emerging variants of concern, and monitor vaccine effectiveness, both across the country and internationally.
Canada’s COVID-19 situation in the global context
As of August 31, 2021, globally, there were over 215 million reported COVID-19 cases and close to 4.5 million COVID-19-related deathsFootnote 119. Similar to Canada, many other benchmark countries in the Organisation for Economic Co-operation and Development (OECD) experienced outbreaks and resurgences after the summer of 2020, including those that were initially successful in preventing or limiting a first waveFootnote 119. Each country’s individual epidemiological trajectory is influenced by a multitude of factors, and thus their respective data must be interpreted with caution.
In 2021, many OECD countries transitioned to focusing their public health response on achieving high vaccination coverage. Compared to countries such as the USA, UK, and Israel, mass vaccination in Canada began somewhat later (Figure 5)Footnote 119. However, as a result of accelerated supply, expansion of provincial/territorial vaccination campaigns, and an extended dose interval strategy, as of August 31, 2021, Canada had administered at least one dose of a COVID-19 vaccine to 73% of the total populationFootnote 40. These combined efforts contributed to Canada’s ranking of #7 for highest first-dose coverage among OECD countries at the timeFootnote 119.
Canada looked to the experiences of other countries as they faced resurgences driven by more contagious variants. For example, Israel, Iceland, and the UK all experienced rapid increases in cases in the summer of 2021 caused by the Delta variant, even with relatively high vaccination coverage (Figure 5). However, as of August 2021, the number of COVID-19-related hospitalizations or deaths in all 3 countries was far less than those reported during previous wavesFootnote 119. The experiences of these countries, as well as emerging evidence that vaccine-acquired immunity may wane over time, emphasized the need for continued caution as vaccine coverage increasedFootnote 120. Easing of public health measures must be controlled, gradual, and responsive to the local epidemiological context, even once infection rates are brought to low levels.
As of August 31, 2021, only 40% of the world’s population and 2% of people in low-income countries had received at least one dose of a COVID-19 vaccineFootnote 119 Footnote 121. Globally, the lack of supply and access to COVID-19 vaccines means that many places will remain in the acute stage of the pandemic for the foreseeable future. Canada remains committed to working with partners to reach equitable global vaccination targets, for example through the donation of vaccines and funds to the COVID-19 Vaccines Global Access (COVAX) initiativeFootnote 122. The support that Canada provides internationally benefits Canadians as well because the future course of COVID-19 in Canada is dependent on working with all countries to end the pandemic.
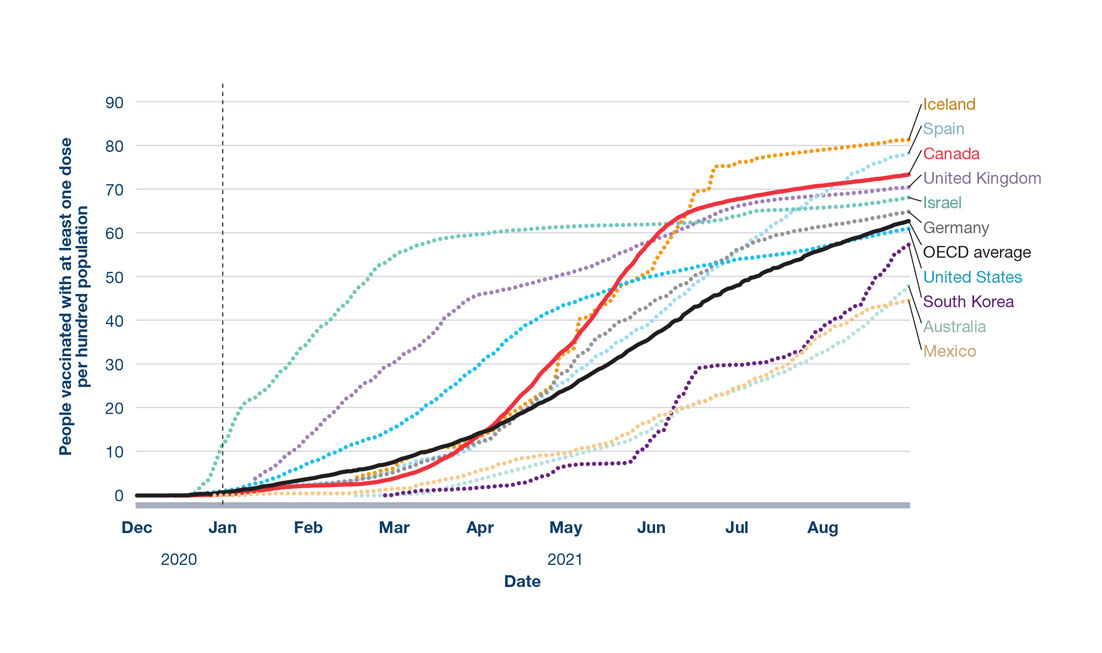
Figure 5: Text description
The figure is a line graph displaying the cumulative number of people who have received at least one dose of a COVID-19 vaccine in Canada and selected countries from December 2020 until August 2021. The vertical axis displays the number of people vaccinated with at least one dose per hundred. The horizontal axis displays the elapsed time in months. The countries are represented by different coloured trend lines: Iceland (orange), Spain (light blue), United Kingdom (light purple), Israel (green), Germany (grey), South Korea (dark purple), United States (bright blue), Australia (light green), and Mexico (light orange). Canada and the OECD average are depicted as red and black solid lines, respectively, for ease of comparison versus dashed lines for all other countries.
| Date (selected time points) |
People vaccinated with at least one dose per hundred population |
|---|---|
| Australia | |
| 2021-02-28 | 0.1 |
| 2021-03-31 | 2.6 |
| 2021-04-30 | 7.7 |
| 2021-05-31 | 14.5 |
| 2021-06-30 | 23.8 |
| 2021-07-31 | 32.5 |
| 2021-08-31 | 47.3 |
| Canada | |
| 2020-12-31 | 0.3 |
| 2021-01-31 | 2.2 |
| 2021-02-28 | 3.6 |
| 2021-03-31 | 13.2 |
| 2021-04-30 | 32.4 |
| 2021-05-31 | 57.2 |
| 2021-06-30 | 67.6 |
| 2021-07-31 | 70.9 |
| 2021-08-31 | 73.4 |
| Germany | |
| 2020-12-31 | 0.3 |
| 2021-01-31 | 2.3 |
| 2021-02-28 | 4.9 |
| 2021-03-31 | 11.9 |
| 2021-04-30 | 27.7 |
| 2021-05-31 | 43.0 |
| 2021-06-30 | 55.3 |
| 2021-07-31 | 61.5 |
| 2021-08-31 | 64.8 |
| Iceland | |
| 2020-12-31 | 1.4 |
| 2021-01-31 | 3.1 |
| 2021-02-28 | 5.7 |
| 2021-03-31 | 14.4 |
| 2021-04-30 | 31.9 |
| 2021-05-31 | 49.9 |
| 2021-06-30 | 75.5 |
| 2021-07-31 | 78.4 |
| 2021-08-31 | 81.4 |
| Israel | |
| 2020-12-31 | 11.3 |
| 2021-01-31 | 35.3 |
| 2021-02-28 | 53.7 |
| 2021-03-31 | 59.7 |
| 2021-04-30 | 61.5 |
| 2021-05-31 | 62.1 |
| 2021-06-30 | 63.7 |
| 2021-07-31 | 65.9 |
| 2021-08-31 | 68.1 |
| Mexico | |
| 2020-12-31 | 0.0 |
| 2021-01-31 | 0.5 |
| 2021-02-28 | 1.5 |
| 2021-03-31 | 5.3 |
| 2021-04-30 | 9.6 |
| 2021-05-31 | 16.7 |
| 2021-06-30 | 24.2 |
| 2021-07-31 | 36.4 |
| 2021-08-31 | 44.5 |
| South Korea | |
| 2021-02-28 | 0.0 |
| 2021-03-31 | 1.7 |
| 2021-04-30 | 6.6 |
| 2021-05-31 | 11.3 |
| 2021-06-30 | 29.9 |
| 2021-07-31 | 37.9 |
| 2021-08-31 | 57.1 |
| Spain | |
| 2021-01-31 | 2.7 |
| 2021-02-28 | 5.5 |
| 2021-03-31 | 11.4 |
| 2021-04-30 | 25.2 |
| 2021-05-31 | 38.9 |
| 2021-06-30 | 54.8 |
| 2021-07-31 | 68.1 |
| 2021-08-31 | 78.2 |
| United Kingdom | |
| 2020-12-31 | 1.5 |
| 2021-01-31 | 13.6 |
| 2021-02-28 | 29.7 |
| 2021-03-31 | 45.7 |
| 2021-04-30 | 50.4 |
| 2021-05-31 | 57.9 |
| 2021-06-30 | 65.8 |
| 2021-07-31 | 68.6 |
| 2021-08-31 | 70.5 |
| United States | |
| 2020-12-31 | 0.8 |
| 2021-01-31 | 7.5 |
| 2021-02-28 | 14.8 |
| 2021-03-31 | 29.0 |
| 2021-04-30 | 43.1 |
| 2021-05-31 | 49.9 |
| 2021-06-30 | 53.7 |
| 2021-07-31 | 56.8 |
| 2021-08-31 | 61.0 |
| OECD average | |
| 2020-12-31 | 0.7 |
| 2021-01-31 | 3.8 |
| 2021-02-28 | 7.3 |
| 2021-03-31 | 13.9 |
| 2021-04-30 | 23.6 |
| 2021-05-31 | 35.5 |
| 2021-06-30 | 47.5 |
| 2021-07-31 | 56.0 |
| 2021-08-31 | 62.6 |
Reporting across countries may be based on different standards and frequencies. Therefore, these data should be interpreted with caution. Vaccination coverage may include non-residentsFootnote 119.
Broader health and social consequences of COVID-19 in Canada
While the influence of the COVID-19 pandemic on health can be detected in many indicators of population health in Canada, as seen in the first wave, the consequences of the pandemic are not confined to the health domain.
As with the direct COVID-19 health impacts discussed in the previous section, the broader health and social impacts of the pandemic are disproportionally experienced among some key populations in Canada. Differential impacts are often connected to pre-existing health and economic inequities as well as access to resources and supports. As a result, the pandemic further worsened many of the structural and systemic factors that contribute to the inequitable distribution of power and resourcesFootnote 5 Footnote 14. This section will highlight a selection of examples that illustrate the complex and interconnected broader economic, social, and health impacts of COVID-19 and some of the governmental, community, and private sector initiatives to address them.
Overall life expectancy likely declined during the pandemic
An examination of life expectancy can provide a broad view of the most serious health impacts of the pandemic in Canada at the population level. Life expectancy is the number of years that an individual at a given age would be expected to live, given observed mortality rates. During 2020, there was an estimated reduction in life expectancy at birth of nearly 5 months for both sexes nationally, attributed to COVID-19 deaths aloneFootnote 123. Life expectancy in Canada has generally been increasing by about 2.5 months per year for the past 4 decadesFootnote 124. Increases in life expectancy at birth began to stall at the onset of the opioid crisis in 2016Footnote 124 Footnote 125. Even though life expectancy for 2020 was not yet calculated at the time of report writing, it is clear that COVID-19 will have a significant impactFootnote 123 Footnote 126.
While most excess deaths can be directly attributed to COVID-19, the pandemic also had indirect consequences on mortality. This can be seen most clearly for younger populations. Although 1,600 COVID-19-related deaths were reported in Canadians younger than 65 years of age between March 2020 and May 2021, there were 7,150 more deaths than expected in this age group over the same time periodFootnote 127. The worsening opioid overdose crisis is the likely cause of a significant portion of this excess mortalityFootnote 128.
Anticipated health issues on the horizon
COVID-19 has put enormous pressure on the Canadian healthcare system, and the negative long-term impact is likely to be profound.
During the pandemic, the use of some health services noticeably decreased. This may be driven both by fewer people seeking care as well as a decrease in the number and types of services availableFootnote 129. Within the first 10 months of the pandemic, the number of emergency room visits and hospitalizations decreased across the country. Advice to stay home may have resulted in fewer unintentional injuries and less transmission of other communicable diseasesFootnote 129 Footnote 130. Additionally, service providers in Canada that deliver sexually transmitted and blood-borne infection (STBBI) prevention, testing, and treatment reported a 66% decrease in demand for their servicesFootnote 131. This could be a result of people experiencing difficulty accessing services due to reduced hours or closures as a consequence of public health measures.
Given the pandemic’s burden on the healthcare system and the impact of public health measures, some services had reduced availability. Many jurisdictions postponed elective and other surgeries to ensure that enough resources were available for COVID-19 patientsFootnote 129. For example, in Ontario, the Financial Accountability Office estimated that, by the end of September 2021, it would take over 3 years to clear the surgery and diagnostic backlog that had accumulated during the pandemicFootnote 132. Researchers also project a future surge of cancer cases once diagnostic screening and surgeries resume after COVID-19-related interruptionsFootnote 133. However, contrary to adults, childhood cancer incidence rates and early outcomes appear to have remained stable throughout the pandemicFootnote 134. The pandemic also diverted public health resources from other programs, thereby limiting their capacity to work on other public health prioritiesFootnote 7. See text boxes “Post-COVID-19 condition” and “Public health measures impacted the spread and management of other communicable diseases” for more examples of the impact of the pandemic on health.
Post-COVID-19 condition
Post-COVID-19 condition (also known as long COVID) is defined as symptoms that persist or recur after acute COVID-19 illness, either in the short term (4 to 12 weeks after diagnosis) or long term (more than 12 weeks after diagnosis)Footnote 135. Preliminary findings from a systematic review indicated that 56% of people who tested positive for COVID-19 reported persistence or presence of one or more symptoms in the long termFootnote 135. While there are over 100 reported outcomes (i.e., symptoms, sequelae, and difficulties conducting usual activities), the most common symptoms include fatigue, general pain or discomfort, sleep disturbances, shortness of breath, and anxiety or depressionFootnote 135. Challenges are expected moving forward for the management of these patients, who may face long-term disability, putting additional pressure on the healthcare system. Canada has multiple specialized clinics that were created to manage post-COVID-19 conditionFootnote 136.
In partnership with Statistics Canada, academic institutions, and provinces and territories, PHAC is assessing a number of data sources that could be used to track cases of post-COVID-19 condition and related symptoms. The Government of Canada continues to monitor national and international evidence and support systematic reviews investigating the spectrum of complications associated with this conditionFootnote 137. Additionally, the Canadian Institutes of Health Research have funded prospective studies that will increase our understanding of the risk factors and long-term outcomes of COVID-19Footnote 138.
Rapid transition to virtual care
In order to minimize the risk of exposure to SARS-CoV-2, many healthcare providers quickly shifted to offering virtual care appointments. Across 5 provinces for which data were available, in February 2020 48% of physicians had provided at least one virtual care service. This increased to 83% by September 2020Footnote 139. Older adults, who are at the highest risk of adverse COVID-19 outcomes, were the main users of virtual care, and researchers expected them to benefit the most from avoiding in-person visits when appropriateFootnote 140. However, using virtual care was challenging for individuals lacking digital literacy or reliable access to the Internet or telephoneFootnote 141. Further studies are needed to determine which health issues and circumstances are the most appropriate for the use of virtual care, and to ensure it does not exacerbate inequitable access to healthcare servicesFootnote 142.
Public health measures impacted the spread and management of other communicable diseases
The adoption of public health measures intended to manage the transmission of COVID-19 may have also curbed the spread of other infectious diseases. Despite increased testing, the number of laboratory-confirmed influenza cases reported between September 2020 and August 2021 was less than 0.2% of the number of cases reported during the same time period in 2018-19. Similarly, no influenza deaths were recorded in 2020-21 in the 8 reporting provinces/territories, compared to 223 influenza deaths recorded in 2018-19Footnote 143 Footnote 144.
Rates of other infectious diseases may also have been lower than previous years, although for some this could be due to decreases in testing as a result of broader COVID-19 consequences, rather than decreases in disease incidence. In 2020, both Alberta and Ontario reported a decline in incidence rates for chlamydia, HIV, and hepatitis CFootnote 145 Footnote 146. However, not all infectious diseases experienced a downward trend. For example, the rate of infectious syphilis increased by 8% in AlbertaFootnote 145. This continues a concerning pre-pandemic trend, especially impacting younger Canadians and under-served populationsFootnote 147. Additionally, emerging evidence showed that antimicrobial use in the community dropped significantly. From March to October 2020, the average national rate of antibiotic dispensing decreased by 27% compared to the pre-COVID-19 period. This may be related to a decrease in overall physician visits during the pandemicFootnote 148.
Canadians experienced worsening mental health during the pandemic
For many Canadians, the pandemic experience was coupled with the stress of job loss, isolation from loved ones, restrictions on community and recreational activities, and/or the need to balance work and caregiving responsibilities. There are indications that the breadth and depth of these challenges negatively impacted feelings and perceptions of mental health and well-being of many Canadians, especially among women, younger Canadians, and frontline workers.
Data collected in March and April 2021 as part of the Canadian Community Health Survey revealed that 42% of Canadians reported that their perceived mental health was “somewhat worse” or “much worse” compared to before the pandemicFootnote 149. Perceived worsening mental health was more frequently reported by females (44%) than males (39%), and it was also most commonly reported among Canadians aged 18 to 34 years (45%), 35 to 49 years (48%), and 50 to 64 years (40%) compared to seniors aged 65 years or older (33%)Footnote 149.
About 70% of healthcare workers who participated in a Statistics Canada crowdsourced survey during November to December 2020 reported perceptions of worsening mental health during the COVID-19 pandemic. Those who had contact with people with confirmed or suspected cases of COVID-19 reported higher rates of feelings of worsening mental health (77%) compared to those who did not report having direct contact with other people (62%)Footnote 150. While a direct pre-pandemic comparison was not available, according to the Survey on COVID-19 and Mental Health (SCMH), among Canadian adults, frontline workers were 2 times more likely to screen positive for post-traumatic stress disorder and 1.5 times more likely to screen positive for generalized anxiety disorder and/or major depressive disorder than those who were not frontline workersFootnote 151 Footnote 152.
Although individuals aged 12 to 17 years were one of the age groups least likely to report feelings of worsening mental health in January and February 2021, the proportion reporting perceptions of poorer mental health doubled since September 2020Footnote 149. While there was limited national evidence at the time of report writing, a study conducted in the Greater Toronto Area from April to June 2020 suggested that deterioration of mental health during the pandemic occurred at a higher rate in children/adolescents with pre-existing psychiatric diagnosesFootnote 153. Kids Help Phone, an e-mental health service offering free confidential support to young Canadians, reported that the number of calls, texts, and clicks on their online resources more than doubled in 2020 compared to 2019Footnote 154. In response, the Government of Canada provided $7.5 million in additional funding for the crisis line to provide young people with mental health support during the pandemicFootnote 155.
Parents of young children also reported feelings and perceptions of worsening mental health. According to a survey conducted in May 2020, 44% of parents with children living at home reported worsening mental health. In the same survey, 36% of respondents without children living at home reported worsening mental healthFootnote 156. Perceptions of worsening mental health appeared highest among parents with a child less than 4 years of age (55%)Footnote 156.
While reported feelings of stress and anxiety increased over the course of the pandemic, preliminary evidence suggested there was not a general increase in diagnosed mental disordersFootnote 157. As data from the pandemic continues to be collected and analyzed, changes in mental health disorders will need to be examined further.
Despite reports of worsening mental health, the SCMH conducted from September to December 2020 did not find an increase in the prevalence of respondents having seriously contemplated suicide compared to 2019Footnote 158. Preliminary research suggested this may be for a number of reasons, including increased access to mental health services and financial supports, as well as the potential benefit of more time spent with household membersFootnote 159 Footnote 160. Some population groups disproportionately impacted by the pandemic (e.g., people who reported job/income loss, people experiencing feeling of loneliness/isolation due to the pandemic) were more likely than others to report seriously contemplating suicideFootnote 158. As suicide rates can be influenced by lasting disruptions to civic life and the economy, it will take time to better understand the long-term impacts on suicide rates due to the pandemic, especially since cause of death reporting can be delayedFootnote 9 Footnote 161.
COVID-19 impacts on substance use
The stress and uncertainty of the pandemic, including its associated social and economic upheavals, altered the substance use patterns of many Canadians.
Dual epidemics: The worsening opioid overdose crisis and COVID-19
The opioid overdose crisis has been a national public health priority for many years with a high health, economic, and social burden across communities, ages, and socioeconomic groups in CanadaFootnote 162 Footnote 163. Despite efforts to address the opioid overdose crisis and signs of a decline in apparent opioid toxicity deaths prior to the pandemic, the number of deaths in 2020 (6,214) exceeded the number of deaths in 2018 (4,389) at the previous peak of the crisisFootnote 128. From April to December 2020, apparent opioid toxicity deaths increased by 89% compared to the same time period in 2019Footnote 128. In 2020, similar to pre-pandemic trends, most apparent opioid toxicity deaths were among males (77%) and individuals aged 20 to 49 years (69%)Footnote 128. Western Canada and Ontario continued to be the most impacted; however, many jurisdictions saw increased opioid-related harms during the pandemicFootnote 128.
While updated data were not yet available nationally at the time of report writing, data from some provinces suggested that this trend continued. For example, there were 46% more suspected illicit drug toxicity deaths in March of 2021 in British Columbia compared to March of 2020Footnote 164. Additionally, a model of opioid-related deaths during the pandemic predicted that the number of deaths would remain high or even increase through the remainder of 2021Footnote 165.
The health and well-being of Indigenous Peoples in Canada continues to be negatively impacted by stigma and discrimination, the legacy of forced displacements, abuse and disruption of traditional culture in residential schools, and the associated intergenerational traumaFootnote 166. Although First Nations people made up only 3% of British Columbia’s population, in 2020, 15% of all toxic substance deaths were among First Nations Peoples compared to 12% in 2019Footnote 167. In Alberta, First Nations Peoples made up 6% of its population, but represented 22% of all opioid poisoning deaths from January to June 2020Footnote 168. To address some of these challenges, the First Nations Health Authority in British Columbia expanded access to culturally safe harm reduction and healing strategies, such as launching the First Nations Virtual Substance Use and Psychiatry ServiceFootnote 167.
Non-pharmaceutical fentanyl continued to be a major driver of the observed surges in opioid-related hospitalizations and deaths during COVID-19Footnote 128. Increasing feelings of isolation, stress, and anxiety, and limited availability or accessibility of public health services, such as harm reduction services for people who use substances, might also have contributedFootnote 128 Footnote 169. Public health measures implemented to manage COVID-19 also disrupted substance supply chains, which could have created additional risks for individuals who had to modify their usual substance use as a resultFootnote 169.
At the outset of the COVID-19 pandemic, the Government of Canada took action to enable the health system to better meet the needs of people who use substances. Health Canada created and extended a temporary exemption to the Controlled Drugs and Substances Act, including allowing pharmacists to prescribe and physicians to verbally prescribe controlled substances in order to help patients adhere to public health measuresFootnote 170. Similarly, in September 2020, British Columbia issued a public health order that authorized registered nurses to prescribe pharmaceutical alternatives in an effort to prevent people from accessing a potentially toxic street supply and to provide more opportunities for ongoing care, treatment, and supportFootnote 171. Another example of ensuring safer supply was the innovative MySafe vending machines set up in Victoria, London, Dartmouth, and Vancouver. After verifying an individual’s identity with a palm scan, the machines provided access to medication for patients with existing prescriptionsFootnote 172.
Alcohol-related hospitalizations increased during the pandemic
Some Canadians appear to have increased their use of alcohol during the pandemic. Sixteen percent of respondents to the SCMH conducted from September to December 2020 reported that their consumption had increased, especially among those reporting perceptions of worse mental healthFootnote 173. Compared to 2019, from March to September 2020, overall hospitalizations for alcohol harms rose by 5%Footnote 169. In addition to increased consumption and availability of alcohol, this may also reflect a broader trend of delaying seeking necessary care, resulting in more severe outcomesFootnote 169. Alcohol-related hospitalizations increased the most (14%) in the lowest-income areas during the pandemic, compared to no change in the highest-income areasFootnote 169. This could be due to low-income Canadians being more impacted by the pandemic as well as having a higher prevalence of multiple chronic conditionsFootnote 5 Footnote 174.
Social determinants of health
The health of Canadians is dependent on a set of fundamental social determinants. The 2020 CPHO Annual Report examined how the social determinants of health, such as income, employment, and racism, influenced differential risk of COVID-19 and reinforced societal inequitiesFootnote 5. Consistent with findings from the first wave, emerging evidence from the second and third waves suggested that the broader social and economic impacts of the pandemic were also being disproportionately experienced by groups who have been historically under-served, such as racialized populations, Indigenous Peoples, populations that are low-income, and women.
The pandemic affected financial security
As a result of the economic impacts of COVID-19, millions of Canadians lost their jobs, worked reduced hours, and/or were in precarious financial situationsFootnote 175. Industries most impacted by the unintended consequences of public health measures, such as retail trade, accommodation, and food services, saw the largest job lossesFootnote 176. Since a peak of 14% in May 2020, the unemployment rate generally trended downward (8% in July 2021), but remained above pre-pandemic levels at the time of report writingFootnote 177.
Some racialized populations disproportionately experienced higher rates of unemployment. In June 2021, the unemployment rate among Canadians designated as visible minorities was 10% compared to 6% among Canadians who were not Indigenous or a visible minorityFootnote 178. Compared to February 2020, the unemployment rates in February 2021 for youth aged 15 to 24 years had increased by nearly 7 percentage points, and employment losses among women in that age group were nearly double those seen in menFootnote 179.
Long-term unemployment is associated with negative health impacts, difficulty returning to work, and delays in acquiring work experienceFootnote 176. As of July 2021, 28% of unemployed people were experiencing long-term unemployment, an increase from approximately 12 percentage points before the pandemicFootnote 180. COVID-19 also magnified the consequences of precarious employment conditions (e.g., low-paid work, part-time work, irregular hours) faced by many working people in Canada, who are disproportionately women, people who are racialized, immigrants, and people with disabilities. This is increasingly recognized as an important social determinant of health and has been linked to a number of adverse worker, family, and community health outcomesFootnote 181 Footnote 182 Footnote 183.
The lowest-income earners and households in which the major income earner is younger than 35 years of age had the most pronounced wage losses in 2020Footnote 184. However, as a result of COVID-19-related income support transfers by federal and provincial/territorial governments that were implemented to compensate financial losses, both of these groups saw the greatest increases in income in 2020 compared to 2019Footnote 184. In particular, income for the lowest-income households in Canada increased 18% in 2020, more than other household typesFootnote 184. Furthermore, the gap between lowest- and highest-income earners decreased by 2% in 2020 compared to 2019Footnote 184. It is important to note that some groups were not eligible for these income support programs. Nonetheless, the lessons learned from these programs may be used to facilitate discourse around a basic income across the country that could lessen financial impacts on health, especially during future health emergenciesFootnote 185.
Additional impacts on social determinants of health during the pandemic
Changes in Canadians’ financial security were just one of several ways in which the pandemic impacted social determinants of health. For many others, such as the examples highlighted in Table 3, it will take further time to gather data and understand the long-term effects of COVID-19.
| Social determinant of health | Potential impact of COVID-19 |
|---|---|
| Food insecurity |
|
| Family and gender-based violence |
|
| Stigma and discrimination |
|
| Education |
|
| Childhood development |
|
Many consequences of COVID-19 are likely still to come
This section has detailed some of the broader consequences of the pandemic on social determinants of health, substance use, and non-COVID-19 health outcomes. In some areas, the interventions taken to mitigate challenges were focused on the short term, and the long-term impacts remained unknown. These longer-term impacts on the health of Canadians will only surface in years to come. For example, very little is known about the potential for long-lasting impacts of the pandemic on children. It will therefore be important to continue to work towards a better understanding of the broader consequences of COVID-19 and to monitor well-being indicators that encompass multiple dimensions of Canadians’ quality of lifeFootnote 204 Footnote 205.
As a result of the pandemic, public health is front of mind for many Canadians. Examining some of the broader consequences of the pandemic emphasizes that public health is much more than infectious disease prevention and control, and demonstrates that focused and coordinated efforts by the public health system and related sector partners are needed to address the future consequences. The following section will examine how the public health system adapted to the pandemic, including challenges and innovations, and how work needs to continue across sectors to protect population health and well-being in future public health emergencies.
Key public health system challenges and solutions highlighted by the COVID-19 pandemic
The COVID-19 pandemic highlighted priority areas for strengthening public health systems in Canada. It also provided a critical opportunity to address long-standing gaps through innovation and collaborative efforts. The joining of forces across all levels of government, the private sector, nongovernmental organizations, and communities was unprecedented, although there continue to be key areas requiring further attention.
Ensuring access to the right data and information to support complex decision-making
Throughout the pandemic, collecting and sharing health data, knowledge, and information to support an effective pandemic response posed a constant challenge. Obtaining consistent, timely, and complete national COVID-19 case data was difficult, given that provincial and territorial jurisdictions do not always collect or report information in the same wayFootnote 7 Footnote 206. Additionally, information on geographic location, hospitalization status, pre-existing conditions, and deaths, was not always available, highlighting historic challenges with data infrastructure, limited workforce capacity, and data-sharing agreementsFootnote 7 Footnote 206 Footnote 207. These delays in access to complete national data sets reduced the quality of analyses characterizing features, such as disease symptoms and close contacts, as well as the power of models to predict spread of the virusFootnote 7.
Similarly, the ability to collect and link health data to socio-demographic information, such as Indigeneity, race, income, and occupation, was not available at a national levelFootnote 7 Footnote 208. This was mainly due to incomplete collection of these data at a local level, as well as the lack of an interoperable health data ecosystem that could combine different types of data while ensuring proper protection of personal informationFootnote 207.
The disproportionate impact of COVID-19 on certain populations underscores the need for timely socio-demographic information during public health emergencies to understand existing health inequities and implement the most appropriate targeted approachesFootnote 5. To address these challenges at a local level, several public health units began publishing COVID-19 data disaggregated by race and income in the spring of 2020Footnote 209. This allowed for the development of targeted strategies to curb COVID-19 spread and increased vaccine uptake in communities with high vaccine hesitancyFootnote 210. It also spurred a new Black Scientists’ Task Force on Vaccine Equity to develop public health recommendations to address Black community concernsFootnote 211.
Temporary and/or local solutions, such as the one described above, were often put in place to address issues around data availability and access. Recognizing that many of these strategies were neither easily sustainable nor scalable, sparked renewed interest nationally to address long-standing gaps in Canada’s health data ecosystem.
In October 2020, PHAC took the lead on behalf of the Government of Canada to work directly with provinces, territories, Indigenous organizations, and key stakeholders to develop a Pan-Canadian Health Data StrategyFootnote 207. The strategy supported Canada’s COVID-19 response by addressing immediate data needs presented by the pandemicFootnote 212. In the longer term, it will advance efforts to vastly improve health data collection, sharing, and usage by understanding the root causes of problems, identifying opportunities for improvement, and developing a set of guiding principlesFootnote 207. This will lay the groundwork for a coherent, shared, sustainable, and impactful health data foundation that honours data protection and enables the collective use of individual and aggregate health data to improve outcomes for individuals, communities, and societyFootnote 207.
Navigating through the pandemic’s information landscape
The pandemic underscored the need for coherent, consistent, and transparent messaging and risk communication. Providing accurate, reliable, and timely information is critical for informing actions to protect population health, build public trust, and minimize social and economic disruption, and is a responsibility shared among all levels of governmentFootnote 213. Knowledge about COVID-19 has continuously evolved as new scientific information becomes available. It took considerable effort for public health decision-makers to incorporate new expert advice, research findings, epidemiological trends, and other contextual data.
This is the first pandemic to occur during a time in which digital technology and virtual information-sharing platforms are heavily relied upon to keep people safe, informed, and connectedFootnote 214. At the same time, the extensive use of social media during the pandemic created multiple ways for competing views, mis- and disinformation, and different official messages to proliferateFootnote 215 Footnote 216. This caused an infodemic, an overabundance of information, both online and offline, which may have contributed to poor adherence to public health measures, undermining the ability to bring the epidemic under controlFootnote 215. For example, providing too much information can generate vaccine hesitancy; whereas good communication can lead to trust in the effectiveness and safety of vaccinesFootnote 217.
Public health professionals had to find different approaches and mechanisms to counter mis- and disinformation and build trust in the public health system. Accordingly, public health leaders across the country invested considerable time and effort to communicate directly with the public in unprecedented ways, including frequent press and technical briefings, media scrums, interviews, and public awareness campaigns across multiple media formatsFootnote 218 Footnote 219.
ScienceUpFirst, a collaboration between the Canadian Association of Science Centres, COVID-19 Resources Canada, and the Health Law Institute at the University of Alberta, is one example of an innovative social media initiative to address misinformationFootnote 220 Footnote 221. This national social media movement connects scientists, healthcare providers, and science communicators by providing credible, science-based information in creative ways to address the spread of misinformation and help Canadians navigate through the infodemicFootnote 220 Footnote 221. See text box “Rapidly changing evidence led to innovative academic-practice partnerships” for more examples of academic collaboration.
Tailoring communication to communities was also important to ensure that information was accessible and relevant to intended audiences. One example of this was a tool developed by the Centre for Wise Practices in Indigenous Health in partnership with other Indigenous health and community organizations, to support vaccine uptake called Maad’ookiing Mshkiki - Sharing Medicine. This was a community-centred resource designed to empower informed consent for Indigenous PeoplesFootnote 222. It provided culturally relevant and trauma-informed information about COVID-19 vaccines for First Nations, Inuit, and Métis communities. For instance, an infographic was created that effectively explains the various components of mRNA COVID-19 vaccines, incorporating traditional knowledge and healing practicesFootnote 222.
Targeting information based on regional epidemiological context was critical. However, there were times during the pandemic marked by jurisdictional or organizational differences across governments in key communication strategies, highlighting the need for consistent and coherent communicationFootnote 10 Footnote 223. At times, the desire for information created communication opportunities for medical professionals and scientists without comprehensive public health expertise, possibly leading to confusion and reduced trust in public health systemsFootnote 219 Footnote 223. Over the course of the pandemic, the Council of Chief Medical Officers of Health, composed of the Chief Medical Officers of Health from each federal and provincial/territorial jurisdiction, released joint statements to help establish a unified, expert, and trusted voice from the public health system speaking to all CanadiansFootnote 224. This included guidance and advice on COVID-19 in Canada from vaccination efforts to managing COVID-19 at individual, organizational, and community levelsFootnote 225 Footnote 226.
Rapidly changing evidence led to innovative academic-practice partnerships
Amidst the rapidly changing COVID-19 evidence landscape, several initiatives were put in place to help public health organizations quickly find and use evidence. COVID-END, CanCOVID, and CoVaRR-Net are 3 examples of partnerships with academic expertise.
The COVID-19 Evidence Network to support Decision-making (COVID-END), housed at the McMaster Health Forum, was composed of knowledge synthesis and assessment experts. This network used systematic methods to produce evidence syntheses and horizon scans on a range of topics. including pandemic response, public health measures, economic and social responses, and clinical managementFootnote 227.
In April 2020, Canada’s Chief Science Advisor established CanCOVID to offer “an evidence-informed response to the COVID-19 pandemic”Footnote 228. This network was comprised of Canadian researchers, “patient partners, decision-makers, and industry partners”Footnote 228. During the pandemic, CanCOVID supported PHAC by facilitating the rapid convening of experts to help bring new research and insights for discussion.
The Coronavirus Variants Rapid Response Network (CoVaRR-Net) was created as a network of interdisciplinary researchers across Canada who worked with the Government of Canada to address the potential threat of emerging SARS-CoV-2 variants. The goal of CoVaRR-Net was to rapidly respond to critical questions aboutthe characteristics of variants, such as their increased transmissibility, severity of disease, and resistance to vaccinesFootnote 229.
Strengthening collaboration
The scope and impact of the pandemic created an unprecedented need for collaboration across all levels of government and communities as well as across health and other allied sectors. Engaging communities throughout a pandemic response is particularly important to reach priority populations and to support equity-informed responsesFootnote 230.
A collaborative approach to the pandemic required expanding existing and creating new partnerships, roles and responsibilities, and decision-making processes. Across jurisdictions, the Special Advisory Committee on COVID-19 (SAC) has been recognized as a successful example of joint federal and provincial/territorial leadershipFootnote 206 Footnote 218 Footnote 231. All Chief Medical Officers of Health and senior public health officials met up to several times a week since January 2020 to discuss coordination across Canada’s health system. SAC also published national recommendations and guidance on a wide array of pandemic-related topicsFootnote 231.
At the federal level, PHAC teamed up with other departments to ensure Canada’s pandemic response was nationally coordinated and supported. For example, Health Canada expedited access to medical supplies; the Canadian Border Services Agency implemented and enforced border restrictions and mandatory quarantine measures; Innovation, Science and Economic Development Canada introduced measures to directly support businesses developing products to help with the efforts against COVID-19; and Indigenous Services Canada (ISC) worked with Indigenous partners to empower communities to implement their own customized public health emergency preparedness plans and responseFootnote 206 Footnote 232. The Government of Canada also supported several regional and/or local programs, such as providing $4.2 million for local public health units to operate safe voluntary isolation sites in Nova Scotia for individuals living in crowded housingFootnote 233.
Of particular importance have been cross-government collaborations that were anchored in principles of self-governance. First Nations, Inuit, and Métis leaders worked with multiple levels of government to support exemplary community-led and culturally safe immunization programsFootnote 234. For example, Indigenous leadership drove rapid and widespread rollout of COVID-19 vaccines in First Nations communities, including the guidance offered by Elders and Knowledge KeepersFootnote 234. Métis Nation-Saskatchewan hosted easily accessible and culturally safe vaccination sites across Saskatchewan as part of the Vaccinated Métis Strong public health campaignFootnote 235. The Manitoba Inuit Association also hosted vaccination clinics throughout Manitoba, where culturally safe clinics displayed Inuit art and signs written in InuktitutFootnote 236.
In addition, many Indigenous communities undertook the development of community-based rapid point-of-care testing for COVID-19 with support from the National Microbiology Laboratory (NML) and ISC. As of July 28, 2021, through the Northern, Remote, and Isolated Initiative, 302 sites were able to provide diagnostic test results within minutes. These communities worked directly with NML to acquire diagnostic testing devices and access supportive training, building capacity to design and perform their own testing to inform the implementation of local public health measures and limit outbreaksFootnote 237.
Integrating lessons learned to prepare for future public health emergencies
COVID-19 has been the most significant health crisis of the last decades. It has tested the limits and capacity of Canada’s preparedness, and presented the need and opportunity to increase Canada’s readiness for future public health crises.
Updated pandemic plans and surveillance systems
Federal organizations playing an important role in public health in Canada, such as PHAC and ISC, adapted existing plans quickly to respond to the pandemicFootnote 206 Footnote 238. As the pandemic progressed, the scientific knowledge around COVID-19 increased greatly and rapidly. Additionally, the necessity became clear for public health measures to better balance minimizing morbidity and mortality with the impact on societal disruptionFootnote 14. Building on these experiences, PHAC worked with provincial and territorial governments and related partners to develop and continuously update the Federal-Provincial-Territorial Public Health Response Plan for Ongoing Management of COVID-19Footnote 14. This evergreen document was instrumental to ensure a common forward planning approach. PHAC has committed to working with provincial/territorial and Indigenous partners to incorporate lessons learned from COVID-19 in updating and testing future pandemic plansFootnote 206. The pandemic also highlighted the need for event-based surveillance systems that produce early warning signals to be better integrated with governance structures and risk assessment processes that promote coordination across surveillance functionsFootnote 206 Footnote 239.
Equity in pandemic readiness and response
The disproportionate direct (e.g., SARS-CoV-2 exposure, COVID-19 mortality) and indirect (e.g., mental health, substance use) impacts of COVID-19 on key populations emphasized the need for an equity approach to pandemic readiness. During the pandemic, the Government of Canada put in place several programs to specifically address social determinants of health. For example, the temporary Canadian Emergency Response Benefit (CERB) and Employment Insurance (EI) helped more than 8.9 million individuals who lost their jobs or otherwise experienced negative financial impacts from the pandemicFootnote 240. Additionally, to support Canadians experiencing housing insecurity who faced challenges with physical distancing and access to hygiene products, the Rapid Housing Initiative will help address urgent housing needs through the construction of 4,500 affordable housing unitsFootnote 241. Future response plans need to use an equity approach and consider how impacts of a public health emergency might be driven by social determinants of health as well as worsen pre-existing inequitiesFootnote 5. This also points to the importance of improving social determinants of health and supports before the next public health emergency, using the lessons learned from the pandemic.
Surge capacity
The pandemic put an unprecedented strain on available health resources. Responding to such a large-scale and enduring health emergency is challenging since it requires a rapid expansion of health services to meet the increased demands for space, staff, and supplies (see text box “Multi-organizational effort to strengthen surge capacity across Canada”)Footnote 242. For example, many jurisdictions lacked the laboratory capacity to process large volumes of COVID-19 tests within short timeframesFootnote 243. Particularly early in the pandemic, there were also challenges with meeting the extraordinary demand for supplies like personal protective equipment and medical devices. This pointed to the importance of a strategy for maintaining an inventory of essential items in the health system for future public health threatsFootnote 244.
Multi-organizational effort to strengthen surge capacity across Canada
A never-before-seen mobilization of human resources with specialized skills was needed to support a complex and ongoing emergency responseFootnote 218. This need for expanded resources required significant contributions from nongovernmental and governmental partners from both within and outside the health sector.
For instance, the Canadian Red Cross (CRC) was instrumental in boosting surge capacity with large numbers of well-trained medical and non-medical personnel, and leading initiatives at more than 400 sites across the countryFootnote 245. This included providing help at vaccination clinics in at least 6 provinces/territories and deploying field hospitals and health equipment in Alberta, British Columbia, Ontario, and QuebecFootnote 246. CRC also supported voluntary isolation sites for seasonal agricultural workers in Ontario and aided in the logistics and set-up of self-supervised sample collection sites at 19 Canadian land border crossingsFootnote 245. During the third wave of the pandemic, it provided supplies and on-site logistic support to 14 northern villages in NunavikFootnote 247.
The Canadian Armed Forces (CAF) also provided considerable support. During the first wave, CAF deployed medical and support personnel to 54 long-term care facilities in Ontario and Quebec to assist with day-to-day operations, infection control and prevention, as well as general support where needed. Between October 2020 and August 2021, Canadian Rangers were activated in more than 10 First Nation communities to provide humanitarian assistance and address immediate needs as part of COVID-19 mitigation and relief efforts. During the third wave, CAF provided military medical resources to Ontario and Manitoba to augment healthcare providers in medical care facilities and was vital in assisting with the complex logistics of distributing COVID-19 vaccines all over Canada through Operation VECTOR – especially in remote areasFootnote 248 Footnote 249.
A well-prepared public health system must have scalable, flexible, and resilient surge capacity, not only to respond to the immediate needs of a public health emergency, but also to have sufficient resources to attend to other existing or emerging health priorities (e.g., the opioid overdose crisis, climate change) without risking workforce burnout. During the COVID-19 pandemic, many responders were stretched as they dealt with multiple crises at the same time. For example, the July 2021 heat wave that caused a rapid increase in sudden deaths in Western Canada further exacerbated the emotional and physical toll of the pandemic on paramedicsFootnote 250 Footnote 251. The COVID-19 pandemic further underscored the historical need for improved surge capacity in public health, health care, and in allied sectorsFootnote 252.
Future public health emergencies will require a whole-of-society response that includes a stronger public health system
The direct and indirect consequences of COVID-19 continue to impact our health and social systems. The pandemic has made even more apparent many existing gaps in public health systems, and there are additional impacts of COVID-19 yet to come.
A number of the innovative solutions to the challenges highlighted by COVID-19 were designed as immediate short-term crisis responses. Sustainable strategies are needed to forge a more resilient public health system with strengthened partnerships that works for all people living in Canada. This begins with reflecting on how Canada’s public health systems are governed, organized, and resourced so that we can move forward with the right solutions.
Section 2. Public health in Canada: Opportunities for transformation
The COVID-19 pandemic has brought the world’s attention to public health, revealing its essential role in a nation’s well-being. Similar to previous pandemics, it highlighted a core function of public health – emergency preparedness and response. However, this role is only one of the many ways that public health systems protect and support the health of populations.
COVID-19 tested public health systems across Canada and the world. The continued struggles and successes during the pandemic have amplified known weaknesses, revealed new challenges, and underscored the need for resilient public health systems that can best support the health and well-being of people living in Canada. The pandemic also demonstrated that innovations and new ways of working together are needed. There have been numerous calls to reform the public health system, both historically and during the COVID-19 response, but there are additional and increasingly urgent signs that we need to act nowFootnote 7 Footnote 253 Footnote 254 Footnote 255 Footnote 256 Footnote 257 Footnote 258 Footnote 259.
Already stretched thin before the pandemic, the public health workforce is overextended and may not have the capacity to counter the next emergency. There are still unacceptable delays in getting the right data to inform public health decision-making. Society-wide inequities persist, and key social and economic policies started during COVID-19 may not be sustained. These vulnerabilities could weaken Canada’s resilience to future health threats.
As Canada looks toward pandemic recovery, heavy demands on the healthcare system threaten to overshadow the equally critical need to bolster the public health system. As COVID-19 has shown, both systems must be sufficiently supported for Canada to have a reliable and responsive health system that can meet the needs of its people.
Before discussing opportunities to strengthen the public health system, a shared understanding is required of the true scope of public health, and how it touches people’s lives every day.
What is public health
For many people in Canada, COVID-19 opened a window into an important aspect of the work of public health systems. However, public health has long been working to keep people healthy and prevent injury, illness, and premature death, and contribute to health equityFootnote 260. To do all of this, public health professionals take on multiple roles – as leaders, coordinators, motivators, and supporters – to address demanding health challenges.
COVID-19 is one of many pressing issues facing public health systems. Other ongoing challenges include antimicrobial resistance, the opioid overdose crisis, non-communicable diseases (e.g., cardiovascular disease), mental health, and the growing health impacts of climate changeFootnote 261 Footnote 262 Footnote 263. Tackling these complex public health issues requires a deep understanding of what makes populations healthyFootnote 264 Footnote 265 Footnote 266 Footnote 267.
Public health organizations view the population as the “patient”, compared to healthcare institutions that provide one-on-one services to individuals. These populations are organized into different groups – neighbourhoods, specific communities, provinces/territories, or, as was clear with COVID-19, the world.
By its nature, the work of public health is often invisible and behind the scenes. However, its impact on the collective health of populations is profound.
Quote: “If you prolong the life of someone for 2 hours, you can know what you have done. If you prevented 4 million deaths because of COVID, no one will know, because [the deaths] didn’t happen. It is the nature of what we are doing [in public health]: when we are successful, we are invisible.” – Key informant interview
In the 20th century alone, it has been estimated that advances in public health increased the average life expectancy at birth in Canada by 25 years (see text box “Defining moments in the history of public health in Canada”)Footnote 268. This has been linked to key public health achievements such asFootnote 269:
- Improved maternal and infant health through advancements in hygiene, nutrition, education, perinatal death prevention, access to care, and contraception;
- Improvements to sanitation and reduction of environmental toxins, including sewage and water treatment systems and reduction of air pollution from motorized vehicles;
- Fluoridation of drinking water for the prevention of tooth decay and dental disease;
- Tobacco control, including the recognition of tobacco as a health hazard, advertising regulations and limits on selling tobacco, anti-smoking campaigns, and smoke-free environments;
- Occupational safety, including the reduction of workplace injuries and an increase in workplace health promotion;
- Motor vehicle safety, including the prevention of injury and death due to seat belt use, child safety seats, and the decrease of alcohol-related collisions;
- Declines in deaths due to cardiovascular disease and stroke due to a combination of advances in prevention, detection, and treatment, including lifestyle changes and risk-factor modification;
- Infectious disease control and prevention through interventions such as vaccines, public education and campaigns, public health measures, and antimicrobial therapies; and
- Safer and healthier foods, including pasteurization, food inspections, salt iodization, and better nutrition.
Vaccines are one of the most well-known and important public health interventions. The introduction of mass vaccination efforts spurred a dramatic decline in infectious diseases (Figure 6), related illnesses, and deathsFootnote 268 Footnote 270. Notably, the success of vaccinations led to the global eradication of smallpox in 1980 and the certification of Canada as polio-free in 1994Footnote 271 Footnote 272. Today, people routinely receive vaccines to protect against a range of diseases including pertussis, measles, mumps, rubella, tetanus, hepatitis B, human papillomavirus (HPV), influenza, and moreFootnote 273.
Without a continued concerted effort to keep vaccine-preventable diseases in check, previously controlled infectious diseases will returnFootnote 272 Footnote 274. This presents an ongoing challenge for public health, as childhood vaccination programs have been so successful that people may underestimate the risks of vaccine-controlled diseasesFootnote 273.
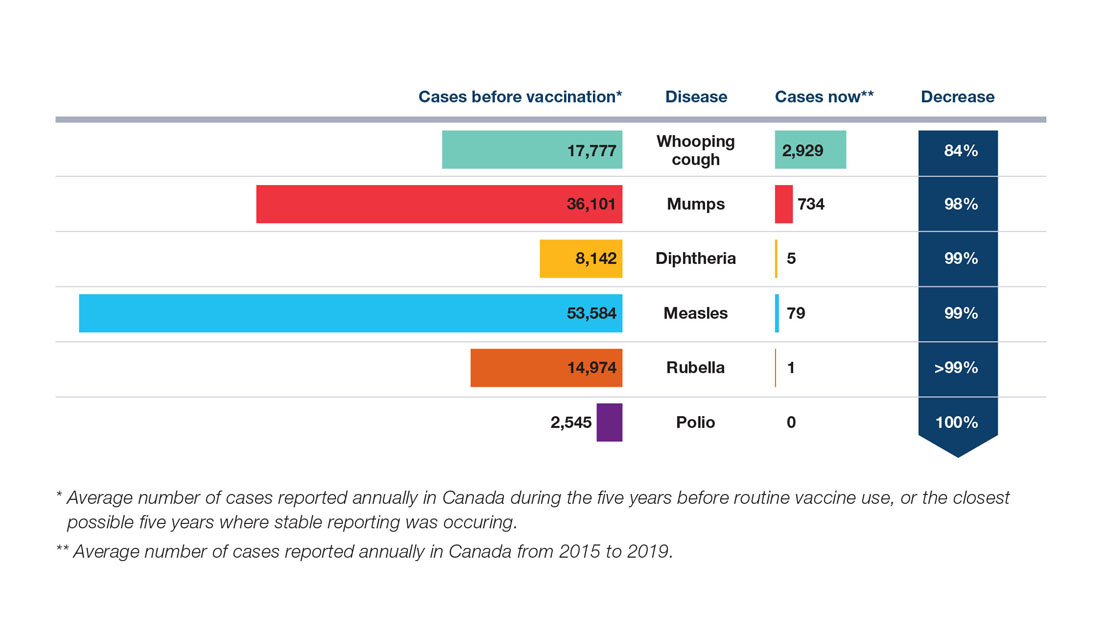
Figure 6: Text description
The figure shows the impact of childhood vaccinations on key infectious disease cases in Canada. They are depicted using horizontal bars that compare the number of cases of vaccine preventable diseases before vaccination to the number of cases now. Decreased cases, in percentage, are displayed to the right.
Cases before vaccination refers to average number of cases reported annually in Canada during the 5 years before routine vaccine use, or the closest possible 5 years where stable reporting was occurring. Cases now refers to the average number of cases reported annually in Canada from 2015 to 2019.
| Disease | Cases before vaccinationFootnote * | Cases nowFootnote ** | Decrease |
|---|---|---|---|
| Whooping cough | 17,777 | 2,929 | 84% |
| Mumps | 36,101 | 734 | 98% |
| Diphtheria | 8,142 | 5 | 99% |
| Measles | 53,584 | 79 | 99% |
| Rubella | 14,974 | 1 | >99% |
| Polio | 2,545 | 0 | 100% |
|
|||
Sources: Measles and rubella data were obtained from the Canadian Measles and Rubella Surveillance System, while data for all other diseases were obtained from the Canadian Notifiable Disease Surveillance SystemFootnote 275 Footnote 276.
Defining moments in the history of public health in Canada
Present-day public health systems in Canada are rooted in historical efforts to control infectious diseases, specifically quarantine legislation developed in the 18th century (Figure 7)Footnote 277. This history was intertwined with social reform movements and increased interest in how social conditions affect the spread of diseaseFootnote 278 Footnote 279. This underscores that health inequities have been a focus of the science and practice of public health for centuries.
At the beginning of the 20th century, the scope of public health expanded to include maternal and child health, nutrition and food safety, injury prevention, environmental contamination, chronic disease, and other issuesFootnote 253 Footnote 259 Footnote 277. This occurred alongside a broader focus on health care in Canada by the mid-20th century, including rapid investment in hospitals and policies to improve access to health careFootnote 280. Medicare was implemented in Saskatchewan (1962) and then expanded across the country with the adoption of the Canada Health Act in 1984Footnote 281.This milestone in population health policy ensured that all residents of Canada were entitled to universal, accessible, comprehensive, portable, and publicly administered health services across the countryFootnote 281.
In the late 20th century, Canada gained international attention due to its formal recognition of the broader social determinants of health, starting with the 1974 “Lalonde Report”, A New Perspective on the Health of CanadiansFootnote 282 Footnote 283. In 1986, the Ottawa Charter for Health Promotion was developed by participants at the first World Health Organization (WHO) International Conference on Health Promotion as a commitment to “Health for All” by 2000. The Charter was a seminal document for public health globally, representing a shift towards situating health squarely as a product of the conditions in which people live, not just as a result of their behaviours or access to health careFootnote 277 Footnote 284. The Charter is still referenced internationally today.
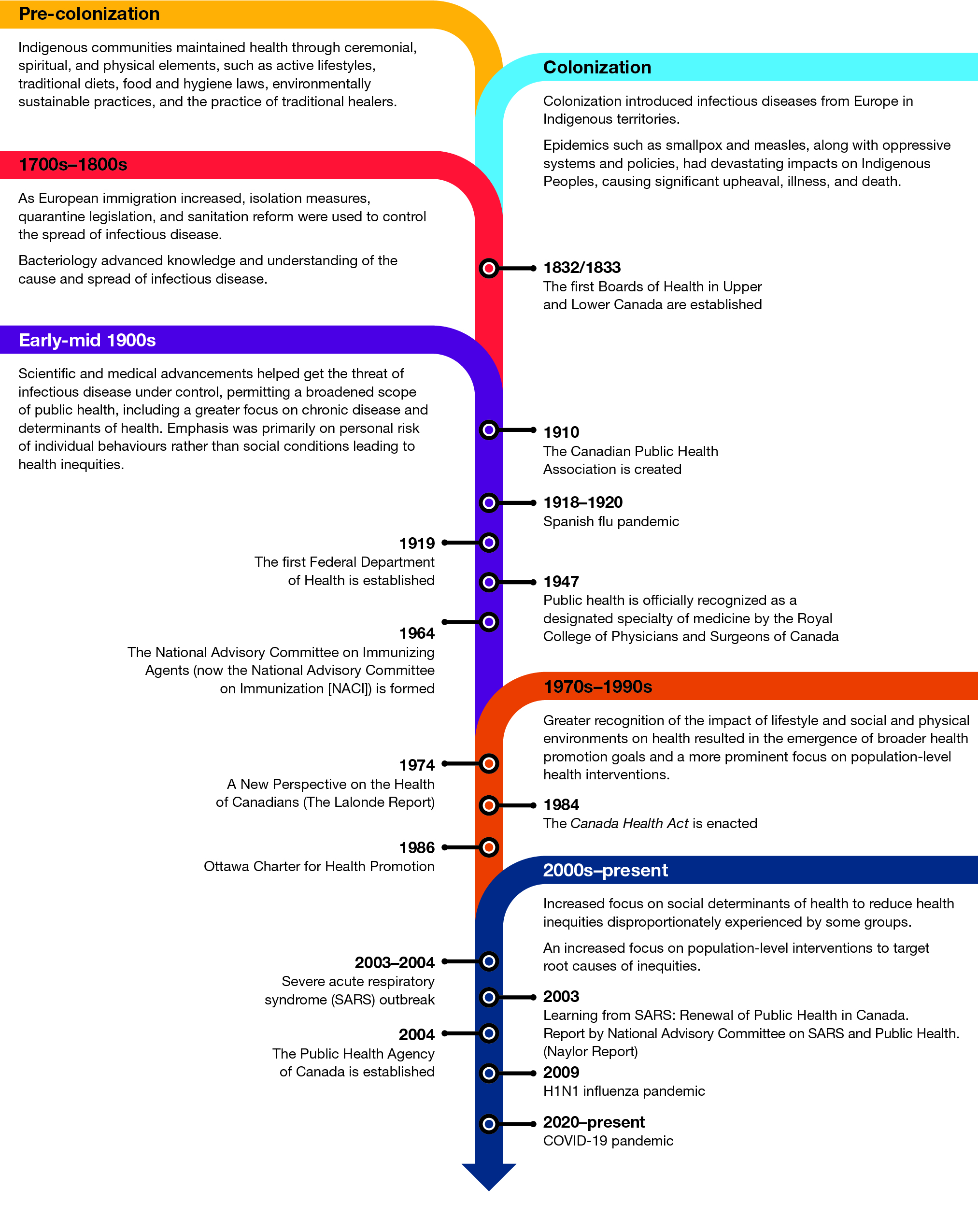
Figure 7: Text description
The figure shows a vertical timeline describing key milestones and shifts in public health in Canada. From top to bottom, the figure describes the following components:
Pre-colonization: Indigenous communities maintained health through ceremonial, spiritual, and physical elements such as active lifestyles, traditional diets, food and hygiene laws, environmentally sustainable practices, and the practice of traditional healers.
Colonization: Colonization introduced infectious diseases from Europe to Indigenous territories. Epidemics such as smallpox and measles, along with oppressive systems and policies, had devastating impacts on Indigenous communities, causing significant upheaval, illness, and death.
1700s-1800s: As European immigration increased, isolation measures, quarantine legislation, and sanitation reform were used to control the spread of infectious disease.Bacteriology advanced knowledge and understanding of the cause and spread of infectious disease.
- 1832/1833: The first Boards of Health in Upper and Lower Canada are established
Early-mid 1900s: Scientific and medical advancements helped get the threat of infectious disease under control, permitting a broadened scope of public health, including a greater focus on chronic disease and determinants of health. Emphasis was primarily on personal risk of individual behaviours rather than social conditions leading to health inequities.
- 1910: The Canadian Public Health Association is created
- 1918-1920: Spanish flu pandemic
- 1919: The first Federal Department of Health is created
- 1947: Public health is officially recognized as a designated specialty of medicine by the Royal College of Physicians and Surgeons of Canada
- 1964: The National Advisory Committee on Immunizing Agents (now the National Advisory Committee on Immunization [NACI]) is formed
1970s-1990s: Greater recognition of the impact of lifestyle and social and physical environments on health resulted in the emergence of broader health promotion goals and a more prominent focus on population-level health interventions.
- 1974: A New Perspective on the Health of Canadians (The Lalonde Report)
- 1984: The Canada Health Act is established
- 1986: Ottawa Charter for Health Promotion
2000s-present: Increased focus on social determinants of health to reduce health inequities disproportionately experienced by some groups. An increased focus on population-level interventions target root causes of inequities.
- 2003-2004: Severe acute respiratory syndrome (SARS) outbreak
- 2003: Learning from SARS: Renewal of Public Health in Canada. Report by National Advisory Committee on SARS and Public Health (Naylor Report)
- 2004: The Public Health Agency of Canada is established
- 2009: H1N1 influenza pandemic
- 2020-present: COVID-19 pandemic
Sources: Adapted from Canadian Public Health Association. Immunization Timeline and This Is Public Health: A Canadian HistoryFootnote 271 Footnote 277.
Acknowledging colonial impacts on public health
The history of public health in Canada cannot be uncoupled from its colonial history. Colonization disrupted Indigenous approaches and systems for health, medicine, and well-being. Colonial policies dismantled traditional ways of knowing, cut off connections to the land, and broke family and social structuresFootnote 285 Footnote 286 Footnote 287 Footnote 288. Intergenerational impacts of colonialism continue to affect the health and well-being of Indigenous Peoples, including experiences of systemic racism, ongoing challenges to self-determination, disconnection from the land, and barriers to high-quality, accessible, and relevant health servicesFootnote 285 Footnote 286 Footnote 289 Footnote 290 Footnote 291.
Today, public health continues to be dominated by Western knowledge and practice, which does not adequately respond to the social and health realities of Indigenous PeoplesFootnote 292. First Nations, Inuit, and Métis Peoples are diverse, with rich histories, cultures, languages, and approaches to health and healing. However there are also shared holistic and relational understandings of health and wellness across many communitiesFootnote 292 Footnote 293 Footnote 294. Traditional knowledge and cultural practices have crucial roles in supporting First Nations, Inuit, and Métis Peoples. During the COVID-19 pandemic, self-determination, Indigenous leadership, and place-based knowledge all informed successful protection efforts for Indigenous communitiesFootnote 292.
These approaches are central to reconciliation, an ongoing process of healing relationshipsFootnote 295. Reconciliation requires, alongside self-determination and Indigenous leadership, an understanding of history and a commitment to truth and justiceFootnote 295. It also requires action to address the policies, systems, and structures that continue to cause social, economic, and health inequities between Indigenous and non-Indigenous people in CanadaFootnote 295.
The Final Report of the Truth and Reconciliation Commission of Canada highlighted the urgent need to work to eliminate the health inequities experienced by Indigenous Peoples. These findings have been echoed and preceded by many Indigenous-led reportsFootnote 285 Footnote 286 Footnote 289 Footnote 292 Footnote 296.
Interplay between public health, society, the economy, and the environment
Current directions in public health are converging around the interrelated nature of health challenges. This includes the connections between human and animal infectious diseases, the health risks driven by climate change, and the interplay between social, economic, environmental, and health inequities. The following 2 approaches consider these interrelated factors and are aligned in their continued prioritization of the social determinants of health.
One Health
The One Health approach explores ways to design and implement intersectoral research and action to concurrently promote the health of humans, animals, and ecosystems Footnote 297 Footnote 298. Issues such as COVID-19 and climate change have highlighted the importance of addressing the complex interconnections between human health and the environment and the potential value of the One Health approachFootnote 297 Footnote 300 Footnote 301. Currently, the pan-Canadian framework for action on AMR and antimicrobial use is grounded in a One Health approach, requiring collaboration across levels of government, academia, industry, and nongovernmental organizations, including participation of subject matter experts in human health, animal health, and agriculture Footnote 302 Footnote 303.
Equity, inclusion, and the social determinants of health
As was evident in Canada and around the world, the social, political, and environmental conditions that created differential risks for COVID-19 overlapped with factors that drive inequities in non-communicable diseases Footnote 5 Footnote 304 Footnote 305. The pandemic left no question about the crucial importance of addressing these inequities Footnote 5 Footnote 86 Footnote 306 Footnote 307 Footnote 308. Globally, many chronic diseases were associated with higher COVID-19 severity or mortality, such as diabetes, hypertension, obesity, cardiovascular disease, and chronic kidney diseaseFootnote 309. These are unequally prevalent in the Canadian population based on factors such as income, education, race, or Indigenous statusFootnote 304 Footnote 305 Footnote 309 Footnote 310 Footnote 311 Footnote 312 Footnote 313 Footnote 314 Footnote 315 Footnote 316 Footnote 317 Footnote 318 Footnote 319 Footnote 320 Footnote 321 Footnote 322.
Infectious and non-communicable diseases are often divided in public health policies, interventions, and practices. Better understanding of the connections across social determinants of health and diverse health outcomes will help to inform public health actions to improve the overall health of populations and decrease societal vulnerabilities to future health emergencies Footnote 323 Footnote 324. This includes attention to systemic racism and other forms of stigma that continue to impact the health of Indigenous and racialized communities, LGBTQ2+ communities, people living with disabilities, and others experiencing marginalization Footnote 324 Footnote 325 Footnote 326 Footnote 327 Footnote 328 Footnote 329 Footnote 330 Footnote 331.
Although public health has historically reported on the social determinants of health that lead to health inequities, concerted action and the application of health equity concepts has not been broadly institutionalized Footnote 259 Footnote 332 Footnote 333 Footnote 334 Footnote 335. Addressing health inequities will strengthen society’s collective ability to withstand future health crises.
How public health systems work in Canada
The public health system of systems
Many organizations, groups, communities, and sectors contribute to improving the health and well-being of populations (Figure 8). Public health institutions form the hub of public health systems.
To serve all communities and populations, public health mandates are spread across jurisdictional public health systems. These comprise Canada’s public health system, which itself is part of the country’s larger federated and universal health systemFootnote 336.

Figure 8: Text description
The figure describes organizations in the public health system.
A circle in the centre of the image describes public health institutions, which have roles and responsibilities for public health and are able to legislate public health policies. These organizations are:
- Indigenous health organizations,
- Local/municipal health authorities,
- Provincial and Territorial Ministries of Health,
- National and provincial public health organizations and institutions; and,
- Federal agencies and departments.
Surrounding this circle are institutions and organizations that do not have a public health mandate, but work closely with the public health system. These organizations are:
- Professional associations,
- Healthcare delivery systems,
- NGOs and community-based organizations,
- Universities, laboratories, and research institutions,
- Media,
- Private sector and industry; and,
- Other government departments (e.g., housing, economic, social services, employment, defense).
Public health is organized differently within Canada’s 13 provincial/territorial jurisdictionsFootnote 253. There are approximately 80 regional health authorities and municipal or local public health units across the country, depending on the provincial/territorial structure. This is where public health services are delivered directly to local populationsFootnote 253. Provincial governments are responsible for coordinating these authorities and units, and among other roles, support overall planning, administer budgets, and provide technical assistanceFootnote 253.
At the federal level, the Public Health Agency of Canada (PHAC) provides a national leadership role for public health within the broader Health Portfolio that includes Health Canada, the Canadian Food Inspection Agency, the Canadian Institutes of Health Research, and the Patented Medicine Prices Review BoardFootnote 337. There are also 6 federally funded National Collaborating Centres for Public Health that serve as knowledge hubs for scientific research and other knowledge to inform public health action.
Public health services for First Nations, Inuit, and Métis communities are divided between federal and provincial/territorial governmentsFootnote 338. Federally, roles and responsibilities are shared across Indigenous Services Canada, Crown-Indigenous Relations and Northern Affairs Canada, and PHACFootnote 339. Indigenous Services Canada funds or directly provides services, such as primary health care and health promotion programs, for First Nations and Inuit, as well as some funding and services provided for Métis communitiesFootnote 257 Footnote 340. PHAC also supports health initiatives for First Nations, Inuit, and Métis living off-reserveFootnote 339. Provincial and territorial governments complement these efforts in varying ways. For example, the First Nations Health Authority in British Columbia, which works with First Nations, government partners, and others to improve health outcomes for First Nations Peoples in British ColumbiaFootnote 341. Additionally, there are national Indigenous organizations, which represent and advocate the interests of First Nations, Inuit, and Métis Peoples across Canada.
The what, why, and how of the public health system in Canada
The overarching purpose of the public health system involves working toward optimal health and well-being for all people in Canada (Figure 9). In support of this purpose are 3 aims centred on protecting and enhancing the health of populations while achieving equitable health outcomes.
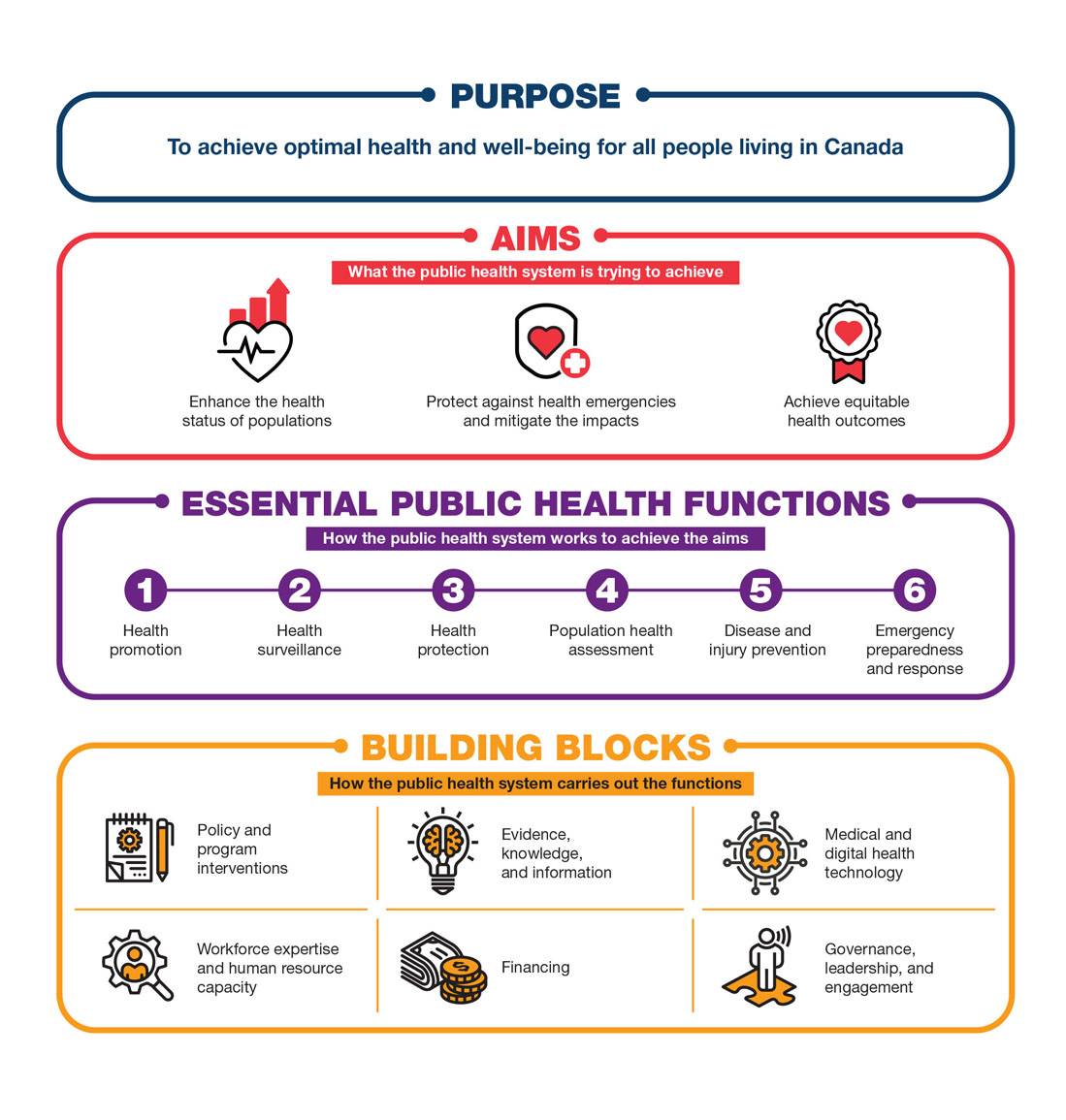
Figure 9: Text description
This figure describes the purpose, aims, functions, and building blocks of public health systems in Canada. The figure works from top to bottom and describes the following components:
Purpose: to achieve optimal health and well-being for all people living in Canada.
Aims (what the public health system is trying to achieve): (1) enhance the health status of populations; (2) protect against health emergencies and mitigate the impacts; and (3) achieve equitable outcomes.
Essential public health functions (how the public health system works to achieve the aims): (1) health promotion; (2) health surveillance; (3) health protection; (4) population health assessment; (5) disease and injury prevention; and, (6) emergency preparedness and response.
Building blocks (how the public health system carries out the functions): (1) policy and program interventions; (2) evidence, knowledge, and information; (3) medical and digital health technology; (4) workforce expertise and human resource capacity; (5) financing; and (6) governance, leadership, and engagement.
To accomplish these aims, public health systems in Canada engage in 6 essential functions that help to organize and unify activities across the systems (Table 4).
Over the past 3 decades, there have been serious efforts to define and redefine the functions of public health within the wider health system, both in Canada and beyondFootnote 253 Footnote 342 Footnote 343. The functions were first developed for Canada in 2003 by the National Advisory Committee on Population Health in response to SARSFootnote 344. Describing the functions of public health became a priority as the scope and complexity of public health practice grew considerably over the 20th century.
Public health practice continues to evolve. Given the globalized spread of emerging diseases, the increasing importance of working in collaboration to secure public trust, and the urgent imperative to address systemic inequities in health, there have been global efforts to revisit the essential functions of public healthFootnote 342 Footnote 345 Footnote 346.
| Function | Description |
|---|---|
| 1. Health promotion | Working collaboratively with communities and other sectors to understand and improve health through healthy public policy, community-based interventions, public participation, and advocacy or action on determinants of health |
| 2. Health surveillance | Collecting health data to track diseases, the health status of populations, and determinants of health trends, in order to promote health, prevent and reduce the impact of disease, and monitor health inequities |
| 3. Health protection | Protecting the population from infectious disease, environmental threats, and unsafe water, air, and food |
| 4. Population health assessment | Understanding the health of communities, specific populations, and the determinants of health to create better services, policies, and research to identify the most effective interventions |
| 5. Disease and injury prevention | Promoting safe and healthy lifestyles to prevent illness and injury, and reducing risk of infectious disease outbreaks through investigation and preventive measures |
| 6. Emergency prediction, preparedness, and response | Planning for natural or human-made disasters to minimize serious illness and death, and responding to emergencies while minimizing societal disruption |
| The National Advisory Committee on Population Health originally developed the list of essential public health functions in the wake of SARS. Subsequent reports, including Naylor et al. (2003) and the first CPHO report (2008) reiterated these functions. | |
In some cases, public health functions are actioned in a clinic or other healthcare delivery setting. For example, hospital networks collect crucial data for health surveillance, many primary care networks provide health protection and promotion interventions; and, throughout the healthcare delivery system, health education is offered in support of disease and injury prevention. These efforts are best accomplished in close collaboration with local public health authorities and communities.
During the COVID-19 pandemic, public health systems activated these functions simultaneously. For example:
- Emergency preparedness and response to coordinate activities across the country, secure vaccine supplies, and create public health guidance and communication tools;
- Health surveillance from first developing technologies to detect SARS-CoV-2 and then data systems to track the spread of the virus;
- Health protection by implementing public health measures to slow the spread of the virus;
- Health promotion to inform and develop policies, programs, and other interventions with communities and other sectors around mental health, food security, economic supports, etc.;
- Disease prevention through vaccination and other interventions to reduce the impact of other illnesses and risk factors that exacerbate the impact of COVID-19 (e.g., mental health, substance use harms); and,
- Population health assessment of the changing strengths, vulnerabilities, and needs of communities due to COVID-19 and public health measures, and rapid synthesis of research on ways to prevent infection and reduce the spread.
Building blocks of Canada’s public health system
If the essential public health functions illustrate how public health systems do their work, the building blocks represent how the systems are organized to support these functions (Figure 9)Endnote iii Footnote 347. These building blocks are foundational and inherently interrelated.
For example, effective surveillance systems are the cornerstone of a strong Evidence, knowledge, and information building block. For those systems to be interoperable and responsive to health emergencies, components and actions are needed from all other building blocks, including: data sharing agreements (Governance, leadership, and engagement); innovative and predictive digital tools and infrastructures (Medical and digital technology); sustainable resources to maintain the technological infrastructure (Financing); expertise to analyze the data (Workforce expertise and human resource capacity); and, input from communities to understand the context of the data and how it could be used to inform interventions (Policy and program interventions).
Building block 1: Policy and program interventions
Population health interventions are policies, programs, services, and strategies that are developed to improve mental and physical health and health equity at the population levelFootnote 348. Public health professionals, community organizations, researchers, and other sectors design interventions for entire populations (e.g., all children in all schools) or for priority subgroups (e.g., children attending schools in economically disadvantaged areas). Actions are evidence-informed and can be universal or targeted approaches delivered at the group, community, and/or population levelFootnote 349 Footnote 350 Footnote 351 Footnote 352.
Because there are no “one-size-fits-all” solutions for addressing complex public health issues, a range of interventions implemented simultaneously are most effective. Public health systems deliver interventions directly to populations (e.g., outreach, vaccination, programming to support communities experiencing marginalization), or indirectly through supporting community and sectoral partners to take action. To implement the right combination of policies and programming, public health professionals require the best available evidence, the right resources, strong partnerships with communities, and the mechanisms to learn and course correct multiple actions in real-time.
Building block 2: Evidence, knowledge, and information
Public health decision-making is informed by evidence from various sources, including research, practitioner experience, and community knowledgeFootnote 353 Footnote 354 Footnote 355 Footnote 356 Footnote 357. Evidence can consist of research findings from different disciplines, community health status reports, data from surveillance and health information systems, insights from communities about their lived experience, evaluation and intervention research, analysis of the policy landscape, and examination of political, social, and economic contexts.
This evidence is assessed and synthesized by researchers, public health professionals, and knowledge hubs, such as the National Collaborating Centres for Public HealthFootnote 358. The methods used to obtain and analyze evidence can be quantitative (e.g., surveillance, epidemiological research), qualitative (e.g., interviews, consultations), or a combination of both (e.g., mixed methods used in evaluations and intervention research).
Public health experts critically appraise different pieces of information as they build a picture of the issue under considerationFootnote 354 Footnote 359 Footnote 360 Footnote 361:
- Who is affected and where?
- What is the impact?
- What is the context?
- What are the determinants, causes, and risks?
- Which interventions might be most effective?
Other groups outside of public health systems also rely on public health evidence. For example, professionals from the healthcare sector, experts from social and environmental policy sectors, key stakeholders (e.g., community organizations, the public), and population health researchers can all use this evidence and analyses to inform their work or actionsFootnote 362.
Building block 3: Medical and digital health technology
Public health professionals rely on effective medical and health technologies and supplies, a stable and responsive laboratory infrastructure, and innovative digital technologies to identify and respond to health issues. Canada’s public health laboratories are a critical part of the country’s medical technology ecosystem, providing backbone support for detecting, understanding, and addressing public health threats. For example, the National Microbiology Laboratory focuses on surveillance, diagnostics, applied research (e.g., mathematical modelling, geographic information system mapping), and emergency response servicesFootnote 363.
Governments across Canada also have systems in place to maintain emergency stockpiles of medical supplies, technologies, and equipment (e.g., personal protective equipment, ventilators, triage and minor treatment clinics)Footnote 364. For example, the National Emergency Strategic Stockpile can be accessed at any time to support provincial and territorial responses to emergencies or be pre-positioned to ensure readiness for other public health eventsFootnote 364.
Public health systems leverage digital information infrastructure and emerging technologies, such as advanced surveillance systems, computing, and artificial intelligenceFootnote 239. Canada’s event-based surveillance system, the Global Public Health Intelligence Network (GPHIN), uses digital technologies to identify potential public health risks by searching reports, stories, rumours, and other sources of informationFootnote 239. Canada also contributes to, and utilizes information from, the Epidemic Intelligence from Open Sources initiative, a collaborative and international effort facilitated by the WHOFootnote 239 Footnote 365.
Public health leaders are increasingly relying on digital innovations to support real-time decision-making. This includes the use of open source data, open source code and sharing of data, and novel approaches to modelling, visualization, and communication with the publicFootnote 366.
Building block 4: Workforce expertise and human resource capacity
The public health workforce is diverse and distributed across different professions, working in all levels of government, the healthcare system, communities, laboratories, and academic settings. These professions include, but are not limited to:
- Public health physicians and nurses
- Health and natural sciences researchers
- Mathematical modellers
- Microbiologists and infectious disease experts
- Policy analysts
- Veterinarians
- Social and behavioural scientists
- Public health inspectors
- Public health dieticians
- Epidemiologists and biostatisticians
- Health promotion specialists
- Community development
- Communications experts
- Elders, traditional healers, and cultural Knowledge Keepers
A diversity of skill sets and disciplinary expertise is vital for ensuring that the public health workforce can respond to the varied and complex challenges in public health.
Since SARS, there has been an emphasis on structuring and building the essential components of Canada’s public health workforce. For example, the Joint Task Group on Public Health Human Resources delivered the Pan-Canadian Framework for Public Health Human Resources Planning (2005), setting the stage for the development of the Core Competencies for Public Health in Canada (2007)Footnote 367 Footnote 368. These initiatives also contributed to the growth of graduate programs in public health schools across CanadaFootnote 369.
Building Block 5: Financing
Public health systems in Canada are financed through tax dollars at the federal and provincial/territorial levels, and in some cases municipallyFootnote 281 Footnote 370 Footnote 371. PHAC receives funding directly from the federal health budget. Conditions for federal health funding to provinces and territories are set by the Canada Health Act, which focuses on health care and does not specifically address public health fundingFootnote 372. The provinces and territories are responsible for deciding where and how to invest in their public health system. There may also be ad hoc funding arrangements with federal departments, provinces/territories, or nongovernmental organizations to address emerging or pressing population health issues such as COVID-19Footnote 373 Footnote 374.
The funding of health services for Indigenous Peoples is an area of shared jurisdiction. Jurisdictional ambiguity has led to fragmentation in funding and governance for public health systems serving Indigenous Peoples in CanadaFootnote 339.
Estimating public health funding is difficult and estimates vary, but one approximation suggests that public health spending accounts for just under 6% of total health expenditures in CanadaFootnote 375. In contrast, hospitals receive approximately 26% of total heath expenditures, and costs for medications consume 15%Footnote 375.
An economic argument underlines the importance of financial allocations to public health. For example, research demonstrates that investing in public health can have a high return on investment (see text box “Investing in public health generates significant long-term financial benefits”)Footnote 376 Footnote 377. In addition, some have arguedthat investing in strategies to achieve optimal health is imperative to social justiceEndnote iv, one that supports a commitment to the well-being of all citizensFootnote 378.
Investing in public health generates significant long-term financial benefits
There are many different approaches to calculating the impact of public health interventions. In a systematic review of the return on investment (ROI) of public health interventions in industrialized countries with universal health care, researchers found that, even when considering all caveats, both local and national public health interventions are substantially cost savingFootnote 376:
- The median ROI across all assessed interventions was 14.3, meaning that every dollar invested in public health generated more than 14 dollars in cost savings. This is achieved by preventing additional downstream costs to the health and economic sector. Importantly, public health actions that can effectively target a large part of the population, such as legislative, health protective, or national-level interventions yield the largest ROIs (27.2 – 46.5).
- In contrast to typical healthcare or social service investments, it may take considerable time before the positive impacts of public health interventions are noticeable. Therefore, long-term commitment and planning, rather than short-term political and economic considerations, are essential.
Building block 6: Governance, leadership, and engagement
Public health governance refers to the ways in which public, nongovernmental, or private organizations and sectors work together to support communities in preventing disease and achieving optimal health, well-being, and health equityFootnote 379. Governance functions and actions include developing policies and strategies, legislating, stewarding resources, engaging partners and communities, and facilitating continuous improvement. All of these may be formally embedded in institutions or involve informal mutual arrangements.
All levels of government have public health roles and responsibilities and are able to legislate policies that improve the health of populationsFootnote 254 Footnote 255. Cross-jurisdictional governance involves leveraging networks to facilitate flexible intergovernmental collaboration and coordination in public health. In Canada, the most influential of these is the Pan-Canadian Public Health Network, which was established in the wake of SARS to strengthen and enhance public health policy and practice in CanadaFootnote 224 Footnote 253. As part of this network, the Special Advisory Committee on COVID-19 (SAC) was activated in 2020 to lead the pan-Canadian pandemic response.
Challenges and opportunities for Canada’s public health system
Within the building blocks are key opportunities for strengthening Canada’s public health systems, reflecting evolving ideas that have gained further momentum during COVID-19 Footnote 7 Footnote 253 Footnote 258 Footnote 259. Although not exhaustive, these opportunities represent important entry points for system-wide conversations about public health transformation. Section 3 provides the conditions required for these opportunities to come to fruition and support a world-class public health system for Canada.
Building block 1: Policy and program interventions
Discussions with public health experts have indicated the need to have a more comprehensive, coordinated, and coherent approach to public health interventionsFootnote 380. The complexity of public health issues, combined with variations across populations and contexts, demands purposeful planning of interventions that can have the broadest impact across the determinants of health. Adopting a whole-of-society orientation to public health challenges would support the realization of this goalFootnote 323 Footnote 381 Footnote 382 Footnote 383. Community and civil society have an essential role to play, both as partners and originators of local actions to address inequitiesFootnote 323. To be most effective in this role, communities and the organizations that serve them need the right resources and connections to researchers, public health, and the wider health systemFootnote 384 Footnote 385.
Amplifying upstream action to address complex public health issues
Inequitable and disproportionate COVID-19 case burdens and outcomes were a stark reminder of the ongoing need for public health systems to catalyse action on the social determinants of health. The pandemic showed that collective action across sectors is central to achieving optimal health for all CanadiansFootnote 5. This requires a comprehensive public health focus on the “causes of the causes”, with action targeting structural drivers of health and the circumstances of daily life (see text box “Improving the health of populations requires a combination of upstream and downstream efforts ”)Footnote 386. This approach would also help to orient action around the determinants of health rather than being confined to siloed disease-centred approachesFootnote 386.
Improving the health of populations requires a combination of upstream and downstream efforts
The health of populations is shaped by social determinants, which then shape the conditions in which people liveFootnote 378. Public health professionals often use the analogy of a river and the relative concepts of “upstream” and “downstream” to describe how these determinants of health influence risk behaviours and health (Figure 10).
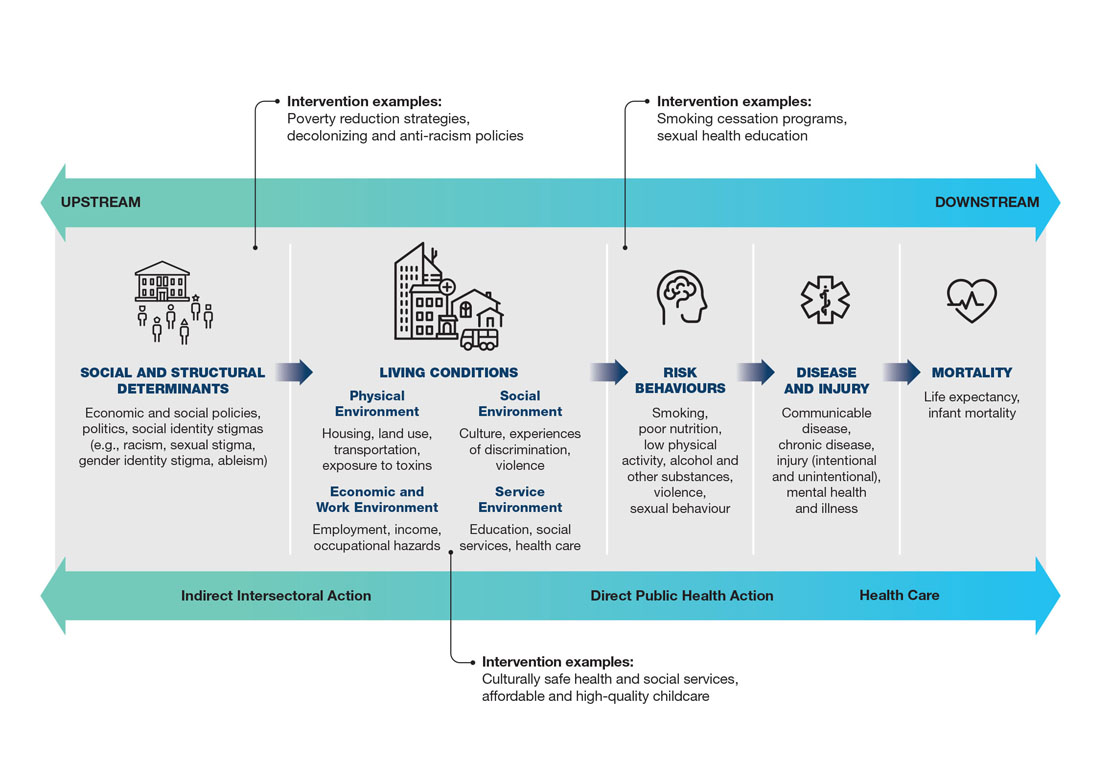
Figure 10: Text description
This figure depicts a continuum of interventions to address determinants of health.
The figure shows upstream and downstream influences on health, as well as examples of upstream, midstream, and downstream interventions. From left to right, the figure also depicts indirect intersectoral action, direct public health action, and health care. From left to right the figure describes the following components:
- Social, and structural determinants: economic and social policies, politics, social identity stigmas (e.g., racism, sexual stigma, gender identity stigma, ableism).
- Living conditions:
- Physical environment: housing, land use, transportation, exposure to toxins.
- Social environment: culture, experiences of discrimination, violence
- Economic and work environment: employment, income, occupational hazards.
- Service environment: education, social services, health care.
- Risk behaviors: smoking, poor nutrition, low physical activity, alcohol and other substances, violence, sexual behavior.
- Disease and injury: communicable disease, chronic disease, injury (intentional and unintentional), mental health and illness.
- Mortality: life expectancy, infant mortality.
Examples of upstream interventions: poverty reduction strategies, decolonizing and anti-racism policies.
Examples of midstream interventions: Culturally safe health and social services, affordable and high-quality childcare.
Examples of downstream interventions: Smoking cessation programs, sexual health education.
Figure adapted from A Public Health Framework for Reducing Health Inequities: Bay Area Regional Health Inequities InitiativeFootnote 387.
This analogy comes from a parable: “A witness sees a person caught in a river current. The witness is able to pull the person from the river, saving them from drowning, only to be drawn to the rescue of more drowning people. After many have been rescued, the witness walks upstream to investigate why so many people have fallen into the river”Footnote 388.
Upstream interventions target the social and structural determinants of health (i.e., stopping people from falling into the river in the first place). This means targeting the policies and underlying inequities that shape both the conditions of people’s lives and their behaviours. Because these factors influence many other risk factors, addressing them can impact a number of health outcomes at once. This requires public health to provide data, analysis, and knowledge translation to inform and support upstream interventions.
Midstream interventions are aimed at reducing group vulnerabilities and mitigating existing inequities. These vulnerabilities mainly manifest in the environmental and living conditions of people’s lives. Again, addressing these for affected groups can impact a number of health outcomes. Public health systems act both directly and indirectly on these issues.
Downstream interventions support people who are already experiencing the health impacts (i.e., helping people after they are caught in the current). These interventions are focused on changing individual behavioural risk factors, building skills, and/or treating the resulting health issue. Public health systems are able to provide direct action in these areas, although they are generally the least influential for broad population-level change Footnote 349 Footnote 389.
As public health systems continue to promote and advance upstream solutions, there is a need to clearly articulate their role in intersectoral actions Footnote 349 Footnote 390 Footnote 391. For example, public health systems often have technical expertise and knowledge that can support other sectors to take action on the social, structural, and environmental determinants of health Footnote 390 Footnote 392 Footnote 393. However, this requires buy-in from sectors with the mandate to act on these determinants (e.g., housing, employment, and education) Footnote 349 Footnote 390 Footnote 391 Footnote 394.
Discussions with stakeholders during the development of this report echoed the importance of public health systems providing support to other sectors and the need for solidified mechanisms to encourage intersectoral collaborationFootnote 380. There are several examples currently gaining momentum internationally and in Canada. First, health impact or equity assessments (HIA) are tools that other sectors can use to identify and consider the health and equity consequences of projects, programs, or policiesFootnote 395 Footnote 396 Footnote 397 Footnote 398. Second, the collective impact approach recognizes that complex social and public health problems require coordinated efforts with common goals and mutually reinforcing actions across sectors Footnote 399 Footnote 400. The collective impact framework offers concrete ways to promote and implement shared accountability across participating organizationsFootnote 399.
The right combination of interventions can effectively address the range of upstream, midstream, and downstream determinants of health. However, there are many challenges in identifying which actions are the most impactful and amendable to scaling across disease areas, populations, and contexts Footnote 267 Footnote 401 Footnote 402 Footnote 403 Footnote 404. Applied public health research offers important insights into the sustainability, equity, and effectiveness of public health interventionsFootnote 405. Work in this field could be strengthened by prioritizing policy-relevant research and working with practitioners to identify practical translations of research knowledge about interventions into public health actionFootnote 405.
Mobilizing community involvement in public health decision-making
Community involvement is central to both health equity and building a resilient public health systemFootnote 385. Community-based organizations improve the health of their populations in multiple ways, by mobilizing and empowering local communities to take action, as well as providing health and social services to meet immediate needsFootnote 385 Footnote 406. Such organizations are also well-positioned to inform public health interventions, given their close connection to community members, community governance structures, and nimble networksFootnote 324. Working with the public health system, communities can be partners in public health decisions, improve access to and relevance of services, and act as important on-the-ground mobilizers for public health interventions during health emergenciesFootnote 230 Footnote 407 Footnote 408 Footnote 409 Footnote 410 Footnote 411.
There are many examples of strong and effective partnerships between communities and public health organizations across Canada; this was particularly apparent during the COVID-19 pandemicFootnote 385. Immediate opportunities exist to better integrate community involvement and action equitably into public health interventions. Text box “Community leadership and COVID-19 in Toronto” offers one example. Other specific examples from the pandemic include the coalitions and voluntary organizations that worked closely with public health systems, such as the South Asian Health NetworkFootnote 412, the Black Scientists Task Force on Vaccine EquityFootnote 413, and Inclusion Nova ScotiaFootnote 414.
Key ways to support communities in their population health efforts include providing stable and ongoing resources, supporting community self-determination, focusing on equitable engagement and power sharing, building trust, co-developing processes and initiatives, and evaluating the nature and impacts of engagementFootnote 408 Footnote 415 Footnote 416.
The opportunity exists to build on the synergistic relationship between communities, local public health systems, and primary care services, though there is noticeable variability across provincial and territorial healthcare systems. Comprehensive primary healthcare models emphasize this synergy and offer a way to consider the coordination of public health practice at the community levelFootnote 385. Local public health systems have an important role to play in bridging the expertise from this triad relationship into broader federal, provincial, and territorial tables on program and policy design.
Community leadership and COVID-19 in Toronto
Community-led actions in response to COVID-19 emerged early in the pandemic response. Over time, both the city and province learned from these approaches and resourced community organizations directly for their leadership role in advising and carrying out trusted responsesFootnote 417. COVID-19 community ambassadors – multilingual, local, and trusted leaders – were recruited and trained to engage with the community, provide information, and connect members with vaccination optionsFootnote 418. Resources were focused on supporting populations disproportionately impacted by the pandemic, including Black and Latin Canadian/Hispanic Torontonians, LGBTQ2+ communities, people experiencing homelessness, people with disabilities, seniors, South Asian, Southeast Asian and West Asian Torontonians, undocumented persons, and youth. Furthermore, Indigenous-led approaches brought culturally safe and accessible vaccination and testing services to communities across the cityFootnote 419.
For First Nations, Inuit, and Métis communities, effective engagement for interventions is rooted in self-determination and cultural safety. Indigenous public health leadership, robust engagement, co-creation of interventions, and culturally relevant evaluations will maximize the effectiveness of public health interventionsFootnote 420. Particularly important are culturally safe processes for engagement that recognize and address power dynamics in the health systemFootnote 147 Footnote 285 Footnote 421 Footnote 422 Footnote 423. Implementing these processes requires mutual trust, the elimination of bias and discrimination, systemic validation of Indigenous ways of knowing, self-reflection for non-Indigenous partners, and cultural humilityFootnote 147 Footnote 285 Footnote 421 Footnote 422 Footnote 423 Footnote 424. With this approach, public health relationships and environments can be spiritually, socially, and emotionally safe for First Nations, Inuit, and Métis communitiesFootnote 425.
Building block 2: Evidence, knowledge, and information
Public health systems require high-quality and accessible evidence, supported by adaptable information ecosystems and processes. When these systems are in place, real-time decision-making and continuous improvements are possible (see text box “A culture of learning”).
The knowledge needed to guide public health system actions, however, cannot come from the system alone. To be both effective and equitable, evidence-informed decision-making requires greater focus on the experiences and perspectives of diverse populations and increased use of various methodological approaches. This includes communities that have been historically excluded in Canada, such as First Nations, Inuit, and Métis Peoples, racialized groups, LGBTQ2+, older adults, and people living with disabilities.
A culture of learning
A learning health system uses data to identify and respond to health issues in a continuous manner, with the goal of improving care and reducing cost. Learning health systems do this by connecting data and research for learning, improvement, and innovation Footnote 426 Footnote 427. Originally focused on health care, learning health systems can be adapted to address public health considerations in pursuit of population health outcomesFootnote 426. This would require greater connections between the public health system, the health system, evolving research and evidence, communities, and ongoing, conscious efforts to embed an equity focusFootnote 426 Footnote 428.
Building an interoperable data and information ecosystem to support decision-making
Quote: “Surveillance and monitoring is one of the core public health functions. It’s our lab test, our physical exam, our way of keeping pulse on the community.”
The first step for understanding any public health issue, and a prerequisite for public health decision-making, is information on the health status, health risks, and determinants of health for the population of interest and key sub-groupsFootnote 362. Canada uses a range of indicator- and event-based surveillance systems to systematically capture and analyze data on a range of public health issues, such as infectious and chronic diseases, the opioid overdose crisis, and mental healthFootnote 429.
These information systems are crucially important to guide decisions and inform evidence-based practice. However, the national data landscape is fragmented across jurisdictions, governmental organizations, and community-level data owners. Multiple independent data systems and frameworks have evolved over time, but have limited capacities to allow for standardized data collection, sharing across systems, and broader synthesis of informationFootnote 207. These issues limit the utility of existing data systems to support public health decision-makingFootnote 7.
This fragmentation, alongside outdated technology, has especially pronounced consequences during health emergencies when access to data for real-time decision-making is paramountFootnote 206 Footnote 207 Footnote 253. Delays in getting the right information can hinder important public health surveillance goals early in a pandemic, such as detecting the virus and understanding how it spreadsFootnote 206.
Due to these historical and ongoing challenges, there have been numerous reviews and calls for reformsFootnote 206 Footnote 334 Footnote 430 Footnote 431. Learning from previous attempts to reform national health data systems identified systemic barriers, such as lack of trust and clear accountabilities between data owners and users, limited public interest or involvement, differing policy goals, and a failure to “spread and scale excellence”Footnote 207 Footnote 432.
Quote: “There is data we don’t collect, data we collect and don’t share, data we share and use poorly, data we use to oppress and stigmatize, and data we have but don’t use to address issues.”
COVID-19 underscored the need for effective processes around epidemiological, biomedical, and clinical data linkages. Interoperable data, information systems, and processes would support this cross-system data flow and analysis. It is important to recognize that “interoperability” does not imply one centralized system, but rather a cooperative ecosystem that honours data ownershipFootnote 207. Common goals and a shared understanding of data requirements and roles for all system partners are neededFootnote 207. This also includes appropriate processes to ensure that data are collected, stored, processed, and used in ways that are culturally safe, as well as mechanisms to protect personal informationFootnote 433 Footnote 434 Footnote 435.
Innovative technology and analytic capacity are both necessary for this work. Interconnected data, large data sets, and complex databases require public health professionals with specialized skills in data analysis and training in health informaticsFootnote 7 Footnote 430 Footnote 436 Footnote 437. The ideal technical infrastructure would be fit-for-purpose to meet data collection and management needs, and include mechanisms to network across systemsFootnote 438. Open-source data sharing in the form of innovative data platforms can help to fill gaps in current surveillance systems in relation to real-time decision-makingFootnote 366. However, many of the data systems used by public health professionals in Canada are currently outdated or offer limited functionalitiesFootnote 436.
Federal, provincial, and territorial governments, alongside First Nations, Inuit, and Métis groups and key stakeholders, are co-developing a Pan-Canadian Health Data Strategy to strengthen health data foundations for better decision-making. It will take time to develop this strategy, and it is not expected to be implemented prior to 2030Footnote 207. Therefore, more immediate actions are needed to strengthen data systems before the next crisis, for example, building on some of the short-term solutions implemented during the pandemicFootnote 14. For instance, PHAC invested in long-term digital transformation through VaccineConnect, a digital vaccine management platform that addresses the immediate need to manage COVID-19 vaccine distribution, tracking, and administrationFootnote 439. Through its agile and scalable approach, VaccineConnect is adaptable to various operational needs and provides the foundation for future uses to meet evolving health priorities post‑pandemic.
Broadening the knowledge base for public health systems
Qualitative and mixed-methods research approaches and the resulting evidence have been underutilized in public healthFootnote 440. Qualitative inquiry can help researchers explore the social aspects of health and illness, such as why people behave in certain ways and how they understand or make sense of their experiencesFootnote 440 Footnote 441 Footnote 442. These qualitative questions add depth and context to epidemiological models and provide insights that help inform the development of interventions Footnote 440 Footnote 441 Footnote 442. For example, qualitative methods can provide important insight into the social, cultural, and political aspects of a pandemic by helping public health professionals understand what drives risk, what influences adherence to public health measures, which unintended consequences might arise from public health actions, and how to better create community buy-in for public health initiatives Footnote 442 Footnote 443. Further, while evidence-informed approaches in public health have historically been guided by Western science-based principles, these do not adequately include the knowledge and realities of all people living in Canada Footnote 433 Footnote 444 Footnote 445. For example, Indigenous ways of knowing, such as oral histories and storytelling, have often been unacknowledged or undervaluedFootnote 420.
For quantitative evidence, the lack of disaggregated data, such as by race, ethnicity, sexual orientation, income, education, and gender identity has been an ongoing challenge for public health practitioners and communities Footnote 210 Footnote 306 Footnote 334 Footnote 446. Without these data, the differential impacts across populations cannot be measured, and inequities are more likely to be remain unaddressed Footnote 210 Footnote 306 Footnote 334. In Canada, there have been challenges to linking or pooling individual-level data, which has hindered research on these areasFootnote 436. Similarly, core population health data sources have inconsistent approaches to identifying Indigenous Peoples across jurisdictions, and some provinces do not collect these type of data at allFootnote 447 Footnote 448 Footnote 449.
These gaps are not just a technical issue, but also an equity issue. For decades, communities have advocated for approaches to data governance that are inclusive of community interests and redress power imbalances around data ownershipFootnote 450. Some examples of community-determined principles for data sovereignty are offered in text box “Indigenous data sovereignty principles: First Nations principles of OCAP, the Inuit Quaujimajayuquangit, and the Métis OCAS principles.” Additionally, the Black Health Equity Working Group in Ontario has released an engagement, governance, access, and protection framework for data collection, use, and stewardshipFootnote 433. Broader calls for equity-oriented data have echoed the importance of community involvement in these processes and subsequent public health action Footnote 208 Footnote 446.
Indigenous data sovereignty principles: First Nations principles of OCAP, the Inuit Quaujimajayuquangit, and the Métis OCAS principles
First Nations principles of OCAP
First Nations have a long history of collecting, using, and governing the information needed to make decisions related to health and well-being. The First Nations ownership, control, access, and possession (OCAP) principles are the standard approach to First Nations data governance and support data sovereignty Footnote 434 Footnote 451. Given the diversity within and across Nations, expression of the principles may be asserted differently from one Nation to another, in line with world view, traditional knowledge, and protocolsFootnote 434.
Inuit Quaujimajayuquangit
The Inuit Quaujimajayuquangit (IQ) framework represents the Indigenous knowledge of the Inuit. IQ is based on 4 elements: working for the common good, respecting all living things, maintaining harmony and balance, and continually planning and preparing for the futureFootnote 452. This approach forms the foundation for well-being in Inuit communities, as does the valuing, preserving, and promoting of traditional knowledgeFootnote 452.
Manitoba Métis principles of OCAS
Métis health information should be collected in accordance with the ownership, control, access, and stewardship (OCAS) principles, and under the ownership and control of the Métis NationFootnote 420. The Métis National Council supports knowledge translation agreements with federal, provincial, and territorial governments towards evidence-based interventions that benefit Métis health and well-beingFootnote 420.
Enhancing the research-practice interface
Research is essential to effective public health practiceFootnote 453. However, there are gaps in this interface, between the context in which research is done and the local needs and resources of the setting in which it is applied. As a result, evidence may not be translated into the settings where it could do the most goodFootnote 453 Footnote 454.
The COVID-19 pandemic illustrated the need for rapid generation and synthesis of emerging knowledge. Closer and adaptable relationships between public health agencies, institutes, and academic institutions could lead to more solutions-driven research outcomes to directly inform public health decisionsFootnote 455. Initiatives such as the COVID-END and CanCOVID research networks were created to synthesize evolving evidence during the COVID-19 pandemic (see text box “Rapidly changing evidence led to innovative academic-practice partnerships” in first section for more information)Footnote 227 Footnote 228. These may serve as models for future research-practice networks. Applied public health research is also key to supporting connections between public health research and practice. For example, the Applied Public Health Chair program – a collaboration between the Canadian Institutes of Health Research (CIHR) and PHAC – builds links between researchers and decision makers to help support evidence-informed decision-making that improves health and health equityFootnote 456. Continuation of this model will help ensure that applied public health research remains responsive to public health practice in Canada.
Additional areas for attention include arrangements for surge capacity during crises, collaboration on public health systems research, and public health-academic partnerships for education and trainingFootnote 455 Footnote 457 Footnote 458. For the latter, student training and professional development could be aligned with priority competency areas, including equity, Indigenous health, ecological determinants of health, and leadershipFootnote 455.
If Canada is to have an exceptional public health evidence base, ongoing knowledge exchange and established arrangements between public health organizations and a range of disciplines (e.g., social science, geography, economics) must be prioritized. Interdisciplinary collaborations are particularly important for understanding and responding to the complex, layered, and interconnected determinants of healthFootnote 459 Footnote 460 Footnote 461 Footnote 462 Footnote 463. For example, social scientists examined the social, political, and economic factors that have influenced the COVID-19 crisis and public health responseFootnote 464.
Building block 3: Medical and digital health technology
A well-functioning health system is able to use a range of tools to support equitable access and distribution of medical products, vaccines, and technologyFootnote 465. This includes the manufacturing, procurement, supply, and storage of essential medicines, medical supplies, and other resourcesFootnote 465. It also includes infrastructure, such as public health laboratories that provide critical support for detecting, understanding, and responding to new and ongoing public health threats. As the public health system learns from past and present challenges, innovative tools and processes evolve to meet the needs of populations.
As society becomes increasingly accustomed to digital solutions, aligning objectives and evaluating innovations will be important for successfully harnessing digital opportunities and technological advancements across jurisdictionsFootnote 366 Footnote 466.
Strengthening early warning systems
Early warning systems identify signals of potential public health threats to support rapid response and mitigate public health impactFootnote 239 Footnote 467. Such systems are a key part of broader surveillance systems, drawing from a number of sources, such as media, social networks, and information on animal health and environmental disastersFootnote 467. Their operation requires the right expertise, structures, and technology. An independent review of Canada’s event-based surveillance system (i.e., GPHIN) in 2021 suggested strengthening these componentsFootnote 239. Expertise and structures could be improved by clarifying the role of event-based surveillance in broader surveillance and risk assessment frameworks, and improving consultation and coordination with subject matter experts, including data-modelling specialistsFootnote 239. Academic and private sector partners also have a role, including providing additional support to refine artificial intelligence algorithms for event-based surveillanceFootnote 239.
Given the international nature of public health, this work cannot be undertaken by any country alone. Global efforts to improve event-based surveillance are ongoing, and Canada can continue to contribute and learn through alignment and collaborationFootnote 239.
Supporting innovation in the health technology and supplies infrastructure
The COVID-19 pandemic reiterated the crucial role of testing in controlling infectious disease outbreaks and guiding public health decisions. Therefore, efforts are needed to strengthen Canada’s public health laboratoriesFootnote 468. During the pandemic, laboratories rapidly pivoted to support the COVID-19 response by implementing new testing protocols for SARS-CoV-2, increasing human resources capacity, and sourcing additional equipment, all in the context of high global demand for critical testing suppliesFootnote 468 Footnote 469.
The Canadian COVID-19 Genomics Network (CanCOGen) is an example of one of the innovative partnerships created during the pandemic to strengthen virus- and host- sequencing capacities in support of time-sensitive pandemic decision-making. Through CanCOGen, the Government of Canada’s National Microbiology Laboratory, Genome Canada, regional public health laboratories, healthcare partners, and academic researchers worked together to coordinate large-scale viral sequencing and epidemiological data collection of SARS-CoV-2 samplesFootnote 470 Footnote 471. These efforts supports rapid learning and improved tracking of how the virus mutates and spreads, offering key insights on transmission trends that could impact viral detection or the effectiveness of treatments and vaccinesFootnote 471.
Additionally, researchers at the British Columbia Centre for Disease Control’s Public Health Laboratory, in partnership with public and private laboratories across the province, combined large-scale genome sequencing with epidemiological analysis to successfully monitor the spread and evolution of virus variants of concern in vaccinated and unvaccinated populationsFootnote 472. This study demonstrated the value of innovative, cross-disciplinary, and integrative approaches by providing accurate, timely, and local data to inform public health interventions. Local tracking of virus variant transmission patterns also support national and global learning efforts, enhancing efficacy of counter measuresFootnote 473 Footnote 474. This further underlines the importance of building sufficient capacity and infrastructure to support complex analyses.
The pandemic also highlighted an opportunity to improve the efficiency of vaccine delivery systems. Despite a relatively slower start compared to some benchmark countries, Canada quickly achieved high vaccination rates once vaccine shipments acceleratedFootnote 475 Footnote 476. Moving forward, general vaccine delivery processes could be strengthened by improved coordination and collaboration, as well as greater innovation in supportive digital infrastructure and workforce integration. Digital advances that support tracking of real-time vaccine supply and use may facilitate greater precision in distribution and minimize product wasteFootnote 477.
During COVID-19, many countries, including Canada, were not well-prepared for the sudden and high demand for personal protective equipment and medical devices, including test swabs and ventilatorsFootnote 244. Identifying, authorizing, and procuring the necessary supplies required the Government of Canada to revise existing procurement approaches, including changing supplier and quality assurance policies or processes, and quickly mobilizing resources for purchaseFootnote 244. Through these adaptations, national investment, re-tooling, and bulk purchasing, Canada was able to increase supplies of personal protective equipment in the national stockpile and help bolster provincial and territorial inventories of medical devicesFootnote 244. Strategies to better monitor and manage emergency stockpiles, within clearly defined roles and responsibilities across jurisdictions, would improve preparedness and ensure the relevance and reliability of suppliesFootnote 244.Leveraging digital health technologies
A number of digital health technologies were used in Canada, and globally, in response to the COVID-19 pandemic (see text box “Vaccine Hunters Canada: Digital innovation from the ground up”). Some were extensions of pre-existing approaches, like technology-based solutions to counter the online infodemic. For example, Google’s SOS alert prioritized the WHO and other trusted public health sources in search results, and the WHO’s machine learning chatbot was launched on social media platforms like Facebook to combat mis- and disinformation around COVID-19Footnote 366 Footnote 478 Footnote 479. Others were more novel, such as the use of anonymous cellphone mobility data to understand adherence to local public health measures and digital exposure notification (e.g., COVID Alert app)Footnote 366 Footnote 480 Footnote 481 Footnote 482. These advances are notable, as public health has generally been slow to leverage digital innovationsFootnote 366. Evaluation of such apps, along with other public health measures, could yield important insights to support more successful adoption of these tools. Particularly in support of technological innovations around climate change, which are rapidly emerging to support public health, including ClimateData.ca and HealthADAPTFootnote 483 Footnote 484.
These rapidly implemented digital health initiatives require evaluation and adequate consideration of legal, ethical, and privacy concernsFootnote 366 Footnote 481 Footnote 485 Footnote 486. It is also important to ensure attention to potential inequities associated with using technology, such as artificial intelligence in public health, which is susceptible to issues caused by algorithmic bias and a lack of data diversityFootnote 487 Footnote 488 Footnote 489. Moving forward, concerns of inequitable access to technology must also be addressed for these innovations to be meaningful in public healthFootnote 366 Footnote 466.
Where appropriate, successful initiatives could be integrated into broader public health systems and infrastructureFootnote 366 Footnote 466, such as VaccineConnect, which will remain a critical tool for managing other vaccination programs. Other examples, including technological advances such as big data, machine learning, and artificial intelligence, could support the development of public health learning systemsFootnote 366 Footnote 426 Footnote 490 Footnote 491. This would help ensure that technologies remain a tool for public health, rather than a focus in and of themselvesFootnote 366.
Vaccine Hunters Canada: Digital innovation from the ground up
In March 2021, volunteers committed to helping Canadians get vaccinated against COVID-19 formed Vaccine Hunters Canada. They had over 40,000 members and dozens of active volunteers across multiple social media platformsFootnote 492.
Using digital tools to crowdsource vaccine availability, personalized support from volunteers, and accounts on Twitter, Facebook, Instagram, TikTok, Snapchat, and Discord, Vaccine Hunters Canada helped Canadians all over the country understand vaccine eligibility and find available vaccination appointmentsFootnote 492.
In June 2021, Vaccine Hunters Canada launched Find Your Immunization (FYI), a new website that connects users to appointments, based on their postal code and vaccine eligibility, across a range of vaccination service sites. FYI was available in 22 languages, and as of the time of report writing, had over two million unique usersFootnote 493.
Prior to shifting to fully automated support in August 2021, Vaccine Hunters Canada announced that the open source FYI platform would be available to any country free of charge, for customizable and multilingual useFootnote 494.
Building block 4: Workforce expertise and human resources
The public health system requires a well-trained, interdisciplinary, and sustainable public health workforce to meet the increasingly complex challenges and threats to the health of populations. The workforce must be equipped with the competencies for carrying out essential functions, in addition to mastering increasingly important skills for working across sectors and influencing public policies that address the determinants of healthFootnote 367 Footnote 455 Footnote 495.
After SARS, numerous initiatives were developed to bolster the public health workforce and develop public health expertise across organizationsFootnote 253 Footnote 368 Footnote 369 Footnote 371. Some initiatives continued, such as university graduate programs in public health, while others stagnated or stoppedFootnote 258 Footnote 455. The COVID-19 pandemic revealed the ongoing and critical need to better support the people who protect the public’s health.
Growing and supporting the public health workforce
During a health emergency, public health systems need workers who have the right training, experience, and specialized expertise. The COVID-19 pandemic amplified challenges in these areas, including system-level gaps in public health and medical expertise, emergency management, risk communications, policy and planning, and operationsFootnote 218.
COVID-19 added strain on public health professionals with in-demand expertiseFootnote 218 Footnote 469. For example, input from public health experts indicated that case managers, who were often nurses, could be pulled away from public health work to treat patients when COVID-19 case numbers rose. Such capacity issues had a number of potential consequences for public health systems, including testing delays, challenges following through with contact tracing, quality of communication products, operation challenges, and difficulties mobilizing a long-term responseFootnote 218 Footnote 243 Footnote 496. To meet these competing demands, the public health workforce must be supported by enough human resources for backup and interoperabilityFootnote 497.
Workforce diversity is also essential to a well-functioning public health system and supports greater innovation in public healthFootnote 446 Footnote 498 Footnote 499 Footnote 500. Diversity and inclusion can be nurtured through initiatives such as recruitment drives for underrepresented staff, professional mentorship programs, projects to improve workplace equity, and effective processes for reporting discriminationFootnote 498 Footnote 501.
As has been noted among healthcare workers and in international research, the pandemic impacted the mental health and well-being of the public health workforceFootnote 502 Footnote 503. While there are research gaps on this issue in Canada, government reviews have highlighted the long hours and stress experienced by public health and emergency management staff, as well as numerous media reports of harassment and threats against public health officials and workersFootnote 218 Footnote 504. Staff turnover and burnout among workers and experts is a very real threat to the stability of public health systems and their ability to respond to health emergenciesFootnote 505.
As noted in discussions with stakeholders, these issues were compounded by a lack of data about the number, structure, skills, and racialized and Indigenous identities of workers in public health systems, including where to find qualified personnel to perform tasks like testing and contact tracingFootnote 380. Differences in the organization of public health structures across Canada, as well as the breadth and depth of public health practice, make it difficult to track and evaluate the nature and extent of the workforceFootnote 252 Footnote 258. These infrastructure and data gaps hinder workforce planning and preparation efforts across federal, provincial/territorial, and municipal public health systemsFootnote 380 Footnote 506. The absence of demographic data also impedes tracking of the public health workforce against the recommendations from the Truth and Reconciliation Commission of Canada and employment equity commitmentsFootnote 380. Public health workforce capacity is an urgent area for attention given the continued burden of COVID-19 on the public health workforce and the risk of concurrent public health crises.
Strengthening core competencies and scientific expertise
Public health is a specific field of practice, and the number and variety of competencies required underlines the importance of comprehensive training and a correspondingly prepared workforceFootnote 367. Core competencies encompass the interdisciplinary knowledge, skills, and attitudes essential to public health practice. Current competency areas include public health science, data assessment and analysis, policy and program planning, intervention implementation and evaluation, collaboration and partnerships, advocacy, diversity and inclusiveness, communication, and leadershipFootnote 367.
Ongoing calls to clarify, and possibly expand public health competencies and/or expertise, reflect how the practice of public health has evolved and learned from health emergencies. For example, additional or enhanced competencies could include those related to working in complex government systems, collaboration for intersectoral action, healthy public policy-making, social and racial equity, ecological determinants linked to climate change, community engagement, and Indigenous healthFootnote 252 Footnote 408 Footnote 455 Footnote 495 Footnote 507 Footnote 508 Footnote 509 Footnote 510 Footnote 511 Footnote 512 Footnote 513 Footnote 514 Footnote 515 Footnote 516 Footnote 517.
Since the onset of the pandemic, additional priorities have emerged. These include navigating and communicating within an infodemic, countering mis- and disinformation, crisis communication, working within a context of uncertainty, advanced understanding and use of data and analysis technologies, risk assessment and management, priority setting, and resource allocationFootnote 239 Footnote 518 Footnote 519. Examples of important leadership level competencies are leadership across disciplines and in the political sphere, tailoring communication to target audience, situational awareness, and decisiveness with flexibilityFootnote 510 Footnote 520. Skills in risk management and decision-making in complex environments are also important for advanced practice and leadershipFootnote 455.
Building block 5: Financing
Sufficient financing is essential for health systems to maintain and improve population health and well-being Footnote 465 Footnote 515. Public health systems require resources not only to fulfill essential public health functions, but also to work effectively with other sectors to address determinants of health. Resourcing has to be “right-sized” to ensure that public health systems can be nimble enough to respond when neededFootnote 253. This is especially important given that emerging and concurrent health crises are expected to rise due to influencing factors, such as climate change and the loss of natural habitatFootnote 521.
With the breadth of the work and the ongoing need to build dynamic surge capacity, public health systems need stable and dedicated resourcesFootnote 520. However, it is unclear what an appropriately financed system should look like in Canada. This requires knowing how much is spent on public health, for which activities, and to what end.
Investing in the public health system to match the mandate
Despite its broad mandate, the public health system has historically had only a small share of total health spending. Estimating public health funding is difficult and there are multiple methods to do so. One assessment from the Canadian Institute of Health Information suggests that just under 6% of all annual health spending was allocated to public health systems prior to the pandemic (Figure 11)Footnote 375. Variations in how these percentages are calculated make comparisons across jurisdictions difficult. Nonetheless, funding for public health activities has been estimated to be as low as 1% of some provincial health budgetsFootnote 522 Footnote 523.
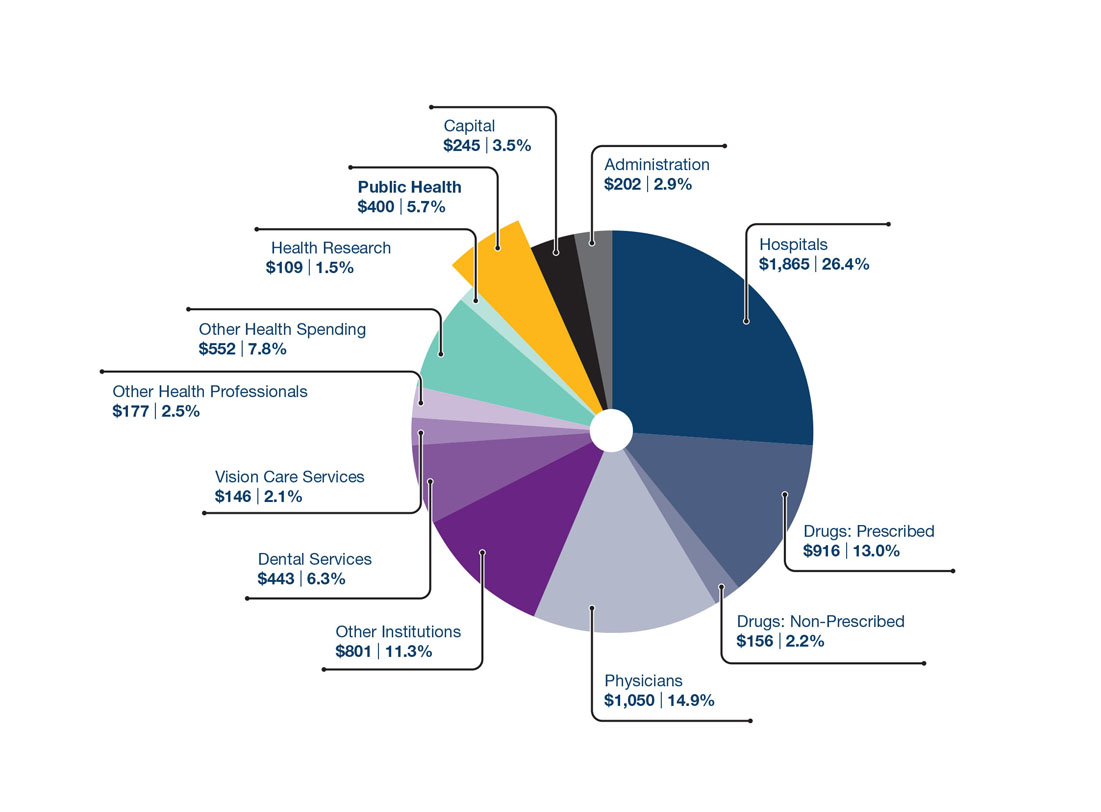
Figure 11: Text description
The figure is a pie chart which shows the breakdown of total health expenditure per capita in Canada in 2019.
| Category | Dollar share | Percentage |
|---|---|---|
| Public Health | $400 | 5.70% |
| Capital | $245 | 3.50% |
| Administration | $202 | 2.90% |
| Hospitals | $1,865 | 26.40% |
| Drugs: Prescribed | $916 | 13.00% |
| Drugs: Non-Prescribed | $156 | 2.20% |
| Physicians | $1,050 | 14.90% |
| Other Institutions | $801 | 11.30% |
| Dental Services | $443 | 6.30% |
| Vision Care Services | $146 | 2.10% |
| Other Health Professionals | $177 | 2.50% |
| Other Health Spending | $552 | 7.80% |
| Health Research | $109 | 1.50% |
Source: Canadian Institute for Health Information, National Health Expenditure TrendsFootnote 375.
There are several methodological issues with these estimates. The diversity and range of activities carried out by public health systems makes it difficult to separate the work of public health from other social service and healthcare activities. Additionally, standardized definitions for public health activities across the country are lackingFootnote 372. Resulting inconsistencies lead to jurisdictional variations in how public health spending is calculatedFootnote 522. Therefore, clear limitations in reporting on, and measuring the effectiveness of, public health investments across Canada existFootnote 372 Footnote 522. These gaps must be urgently addressed, but methodological challenges should not impede efforts to infuse public health systems in Canada with the financial resources needed to execute the essential work of protecting populations.
Despite the difficulty in capturing reliable estimates, evidence indicates that public health funding in Canada may be insufficient and vulnerable to cuts, including previous reductions in several provincial public health budgetsFootnote 258 Footnote 372 Footnote 458 Footnote 522 Footnote 523. These funding reductions are felt particularly strongly at the local levelFootnote 252. If these trends continue, considerable additional downstream costs are likely to occur for the healthcare system and the broader economyFootnote 376.
Quote: “The danger is that we will have current interest (in public health) because it is pandemic related, but we have been through several cycles. Panic, and then people forget about public health. Once [COVID-19] disappears, newer political priorities and a backlog of surgeries will take over and we will shift back to investing in treatment and underinvesting in prevention.” – Discussion group participant
Another challenge is that funding tends to fluctuate according to health crises and election cycles, yet the aims and mandates of public health extend long beyond these timelinesFootnote 253 Footnote 458 Footnote 524. Determining how to best fund public health systems to match the scope and long-term mandate requires a shared commitment to the core functions of public health, as well as a strengthened evidence base and common understanding on how to effectively apply themFootnote 372 Footnote 522.
It is also important to have flexible funding models and sustainable long-term actions to strengthen the public health system in a way that supports self-determination among First Nations, Inuit, and Métis communities. This would minimize jurisdictional fragmentation and increase community control over health program design and deliveryFootnote 339 Footnote 525 Footnote 526. Going in such direction also aligns the public health system with the National Inquiry on Missing and Murdered Indigenous Women and Girls’ Call for Justice no. 3.2Footnote 286.
Building block 6: Governance, engagement, and leadership
Effective governance requires a clear vision, clarity on the authorities, mandate, roles, and essential functions of public health. Adequate and sustainable resources and capacity are necessary to enable this work. For public health governance to be equitable, commitment to core values of anti-colonialism, diversity and inclusion, transparency, and accountability will be requiredFootnote 379.
Successful governance is resilient, adaptive, and built on competent leadershipFootnote 379. It also relies on the coordinated and collective action of government and other actors, including collaborations across jurisdictions within the public health system, shared expertise at the international level, supporting First Nations, Inuit, and Métis Peoples in self-determination and self-governance, partnerships with other sectors, and community leadership at public health governance tablesFootnote 383 Footnote 393 Footnote 527 Footnote 528 Footnote 529 Footnote 530.
Strengthening coherence across public health systems
The decentralized governance structure of the health system in Canada allows for public health actions to be guided by regional and local contexts and needs. However, coordination, collaboration and regular accountability across the system and to decision makers, including federal, provincial, territorial, and Indigenous partners, is vital for a well-functioning, strategic, and cohesive public health system. This was seen during the COVID-19 response, when pan-Canadian approaches were balanced with flexible, customized measures at provincial and territorial levelsFootnote 14. The complex multi-jurisdictional governance of public health in Canada can make it difficult to understand roles and responsibilities at different levels, sometimes resulting in confusion, inconsistencies, and gapsFootnote 258 Footnote 372 Footnote 379. Governance for public health and leadership for intersectoral action to address specific public health challenges (e.g., AMR) add additional complexitiesFootnote 379.
Governance mechanisms to improve collaboration across public health systems include pan-Canadian frameworks, strategies, or legislative acts. The Canada Health Act outlines shared principles, criteria, and conditions that the provinces and territories must meet to receive federal funds for healthcare services. The Act provides accountability to ensure that eligible residents of Canada have access to publicly funded health servicesFootnote 531. However, unlike the Canada Health Act for health care, a formal legal structure with public health accountabilities for residents in Canada does not exist.
Some have argued that the lack of a legislated anchor for the public health system has prevented a consistent and coordinated approach to public health across CanadaFootnote 7. Other public health experts have noted that cross-jurisdictional discussions on shared roles, goals, and values have taken years without any final decisions or commitmentsFootnote 380. For example, after SARS, the provincial and territorial Ministers of Health agreed on a set of public health goals for improving the health of Canadians, but this was not translated into defined accountabilitiesFootnote 532.
Quote: “We need prolonged sustained commitment to the public health agenda that doesn’t swing widely.” – Discussion group participant
On the international front, Canada has a long history of collaborating with other countries and multi-lateral organizations to address global health challenges (see text box “Global solutions to global public health challenges”). Collaborative efforts were intensified during COVID-19 as the virus quickly transcended international bordersFootnote 533. This global spread reflects the reality of public health risks in today’s world and has given the international community a preview of future challenges to global health security. It has also reaffirmed the need to strengthen these collaborative efforts and look beyond borders when planning for, and responding to, global emergenciesFootnote 534. Information sharing around research, knowledge, and experiences also helps the global health system learn faster and respond smarterFootnote 535.
Global solutions to global public health challenges
International health regulations
After SARS, the global health community came together to strengthen systems of cooperation. In 2005, the WHO and its member states adopted new International Health Regulations that detail the legal responsibilities of each country for major public health events, as well as systems for accountabilityFootnote 536. In 2007, the International Health Regulations came into effect, requiring signatory countries to build and maintain the capacity to detect, assess, report, and respond to public health eventsFootnote 536. It emphasized an increased focus on surveillance, informed in part by the use of the GPHIN during the 2003 SARS outbreakFootnote 239. The structure and outputs of GPHIN were used by several countries to inform expansions to their own event-based surveillance systemsFootnote 537. Reviewing and adapting these processes to incorporate the lessons of the COVID-19 pandemic will help ensure improved readiness at global and national levelsFootnote 534.
The WHO Hub for pandemic and epidemic intelligence
A 2021 WHO initiative has taken a visionary approach to fostering global cooperation and shared solutions for addressing pandemic risks. This hub leverages the WHO’s unique convening role to bring together expertise and resources from nearly 200 member statesFootnote 538. Funded by the Government of Germany, the WHO Hub will use a collaborative intelligence approach to improve data and analytics and support pandemic-related decision-making. The hub will build a global trust architecture to support international data and knowledge sharing, and foster connections across political, public policy, scientific, and civil society stakeholders. Researchers, government, and private sector partners will be encouraged to create shared databases using public health, social, behavioural, media, mobility, travel, and environmental data. This innovative approach will bring researchers together for intensive investigations of specific issues, using state-of-the-art technology and multidisciplinary collaborations to help countries around the world detect, assess, and respond to outbreaksFootnote 538 Footnote 539 Footnote 540.
Honouring indigenous self-determination and governance in the public health system
Public health governance requires a focus on Indigenous self-determination and reconciliation. Reconciliation is the ongoing process of building mutually respectful relationships between Indigenous and non-Indigenous populations in Canada, based on truth, justice, and healingFootnote 287. This requires awareness and acknowledgement of the past, atonement for the harms of colonization, concrete actions for societal change, and reconciliation with the natural worldFootnote 287. The Truth and Reconciliation Commission of Canada concluded that self-determination is a precondition to reconciliation (see text box “The right to self-determination”)Footnote 288.
The right to self-determination
The right to self-determination is acknowledged by the United Nations Declaration on the Rights of Indigenous Peoples (UNDRIP)Footnote 541. It states that “Indigenous Peoples have the right to determine and develop priorities and strategies for exercising their right to development. In particular, Indigenous Peoples have the right to be actively involved in developing and determining health, housing, and other economic and social programs affecting them and, as far as possible, to administer such programs through their own institutions”Footnote 541. However, these principles have not always been implemented in CanadaFootnote 339.
Legal decisions in recent decades, including Jordan’s Principle and Daniels Decision, speak to addressing these gapsFootnote 541. Additionally, Bill C-15 (June 2021) aims to begin the process of aligning Canadian law with UNDRIPFootnote 542. This Act provides a road map for the federal government and Indigenous Peoples to work together to implement the declaration, including self-determination.
Self-determination is an important determinant of health and well-being among First Nations, Inuit, and Métis communities, and is key to closing health gaps between Indigenous and non-Indigenous populationsFootnote 288. Models of self-determination in health may vary across Canada, driven by diverse needs, experiences, and interests, as articulated by different nations and communitiesFootnote 339.
Health-related self-determination is about ensuring that First Nations, Inuit, and Métis populations can design, deliver, and manage their own health programs and services through Indigenous self-governance and supportive fiscal arrangementsFootnote 339. It also requires equal inclusion for Indigenous populations in broader health policy development and decision-making to ensure that self-determination is not undermined by the policies of non-Indigenous organizations and governmentsFootnote 329.
No single model of governance will work across all Indigenous communities, and governments at all levels have a responsibility to support processes of self-determinationFootnote 339. One example of a reform prioritizing self-determination is the province-wide, Indigenous-governed and managed First Nations Health Authority in British Columbia (see text box "Northern British Columbia rural and remote and First Nations communities COVID-19 response framework")Footnote 543 Footnote 544.
Northern British Columbia rural and remote and First Nations communities COVID-19 response framework
The Northern BC Rural and Remote and First Nations Communities COVID-19 Response Framework (June 2020) responds to a request from British Columbia’s Minister of Health to develop processes necessary to plan and deliver testing services, clinical pathways, patient transport, and other tools in response to the COVID-19 pandemic.
The Northern Framework was co-developed by leadership and representatives from Northern Health, the First Nations Health Authority (provincial and northern region), First Nations communities, local rural and remote communities, and Provincial Health Services Authority. The Northern Framework not only respects the unique realities of northern, rural, remote, and First Nations and Métis communities and its citizens, it also calls for flexibility and partnership in the actual implementation of the work.
This initiative started as a group of committed leaders, professionals, and community members – gathered virtually and in person – working together to produce the Northern Framework that would later inform the provincial Rural, Remote, First Nations and Indigenous COVID-19 Response Framework. But it also became a place for transforming relationships. The deepening connections between partners gained through shared goals and collective work on the Northern Framework redefined their ongoing ways of working together. Relational change, like this, enables system change and a brighter future for all.
Thank you to contributing Authors:
Dr. Margo Greenwood, Academic Leader, National Collaborating Centre for Indigenous Health; Vice President of Indigenous Health, Northern Health; and, Professor of First Nations Studies, University of Northern British Columbia
Dr. Shannon McDonald, Acting Chief Medical Officer, First Nations Health Authority, British Columbia
Nicole Cross, Executive Director of Indigenous Health, Ministry of Health, British Columbia
Stewarding multisectoral action and collaboration
The COVID-19 pandemic has led to renewed calls for whole-of-government and intersectoral action on the social, structural, and environmental conditions that lead to poor health. To do this, bold and comprehensive governance models are needed. The most well-known approach that can fulfill this need is Health in All Policies (see text box "Taking a health in all policies approach in Canada: Two examples"). As a mechanism to systemize intersectoral governance, this approach ensures attention to health and well-being within policy decision-making across all sectors that influence the social determinants of healthFootnote 394 Footnote 545. It can also include engagement with stakeholders or industry.
One notable international example is the Health in All Policies approach established by the state government of South Australia in 2007, which builds intersectoral connections across government to benefit both health and partnering sectorsFootnote 546. A five-year evaluation of this approach found that prioritizing action on the social determinants of health resulted in actions and processes across sectors that can contribute to overall improved population healthFootnote 394.
Taking a health in all policies approach in Canada: Two examples
Health in All Policies refers to “an approach to public policies across sectors that systematically takes into account the health implications of decisions, seeks synergies, and avoids harmful health impacts in order to improve population health and health equity”Footnote 547.
Newfoundland and Labrador
The Government of Newfoundland and Labrador’s strategic plan “The Way Forward” consists of policy actions designed to achieve 4 objectives: a more efficient public sector, a stronger economic foundation, better services, and better health outcomesFootnote 548. As part of this plan, the Protection and Promotion of Public Health Act (2018) was put forward to support the provincial government in responding more effectively to emerging public health challenges and emergencies.
The Act is rooted in a Health in All Policies approach. It enables the Government of Newfoundland and Labrador to build health impact considerations into policy decisions and to make decisions with a focus on measurable health status improvements. This is done with the aim of improving population health determinants (i.e., employment, education, crime prevention) and reducing healthcare costs in the long term.
Quebec
Quebec has developed a series of programs, laws, action plans, policies, and other tools to serve as levers towards a Health in All Policies approach. Although this approach is not explicitly stated as a strategy in Quebec legislation, the Public Health Act benefits from a legal mandate and dedicated resources to support health impact assessments (HIA). It also makes the Minister of Health and Social Services an “adviser to the government on all matters of public health” and stipulates that every ministry should evaluate the health impact of their actions. If this impact is deemed significant, the ministry should consult with health and social servicesFootnote 398 Footnote 549. A local example of this approach in action is when the region of Montérégie included HIA in the 2011 regional public health action plan to support municipal decision-makers. The HIA responsibility was assumed by a full-time professional from the public health directorate who collaborated with numerous government bodies.
In developing a Health in All Policies approach, health equity metrics can be used to support stewardship among the sectors, representing priority determinants of health, and highlighting where health equity gaps need to be closed. Prior to the pandemic, Canadian initiatives to measure and analyze health equity were under way. The Pan-Canadian Health Inequalities Reporting initiative is the first national initiative to document health inequalitiesFootnote 550. This collaborative effort produces the Key Health Inequalities in Canada report and a Health Inequalities Data Tool with 70 indicators of health outcomes and social determinants of healthFootnote 84 Footnote 551.
Other jurisdictions across the globe have integrated health equity metrics into decision-making structures. Recognizing that Greater Manchester had higher mortality rates than other parts of England prior to the pandemic, the city region placed health equity as a focal point for action using the Marmot indicatorsFootnote 552. Originally published in 2011, the Marmot Indicators were revised in 2014 by the University College of London’s Institute of Health Equity, in collaboration with Public Health England to support local authorities to measure and understand health and social inequities, as well as the social determinants of healthFootnote 553. The region subsequently used these indicators to develop a roadmap to “build back fairer (PDF)” after the pandemic, in order to reduce health, economic, social, environmental, and cultural inequitiesFootnote 554. Indicators are centred upon 6 themes: early years, children and young people; work and employment; income, poverty and debt; housing, transport and the environment; communities and place; and public healthFootnote 552 Footnote 555 Footnote 556.
Section 3. A vision to transform public health in Canada
It is clear that, now more than ever, Canada’s public health system requires transformation in order to effectively support people in Canada to attain optimal health and protect them from current and future health crises.
This section offers a vision for that transformed system, a vision that is anchored in evidence and knowledge from peer-reviewed literature, seminal reviews, and discussions among public health professionals, community leaders, and other experts who make Canada’s public health systems work.
The work to achieve this vision cannot be done by one person or organization alone, rather it requires collective learning and a cross-system cultivation of excellence.
Achieving a world-class public health system
As described in the previous section, the purpose of the public health system is to achieve optimal health and well-being for all people living in Canada. This is also the vision for transformation. Figure 12 illustrates elements of a public health system that is equipped and supported to achieve its purpose and carry out the aims.
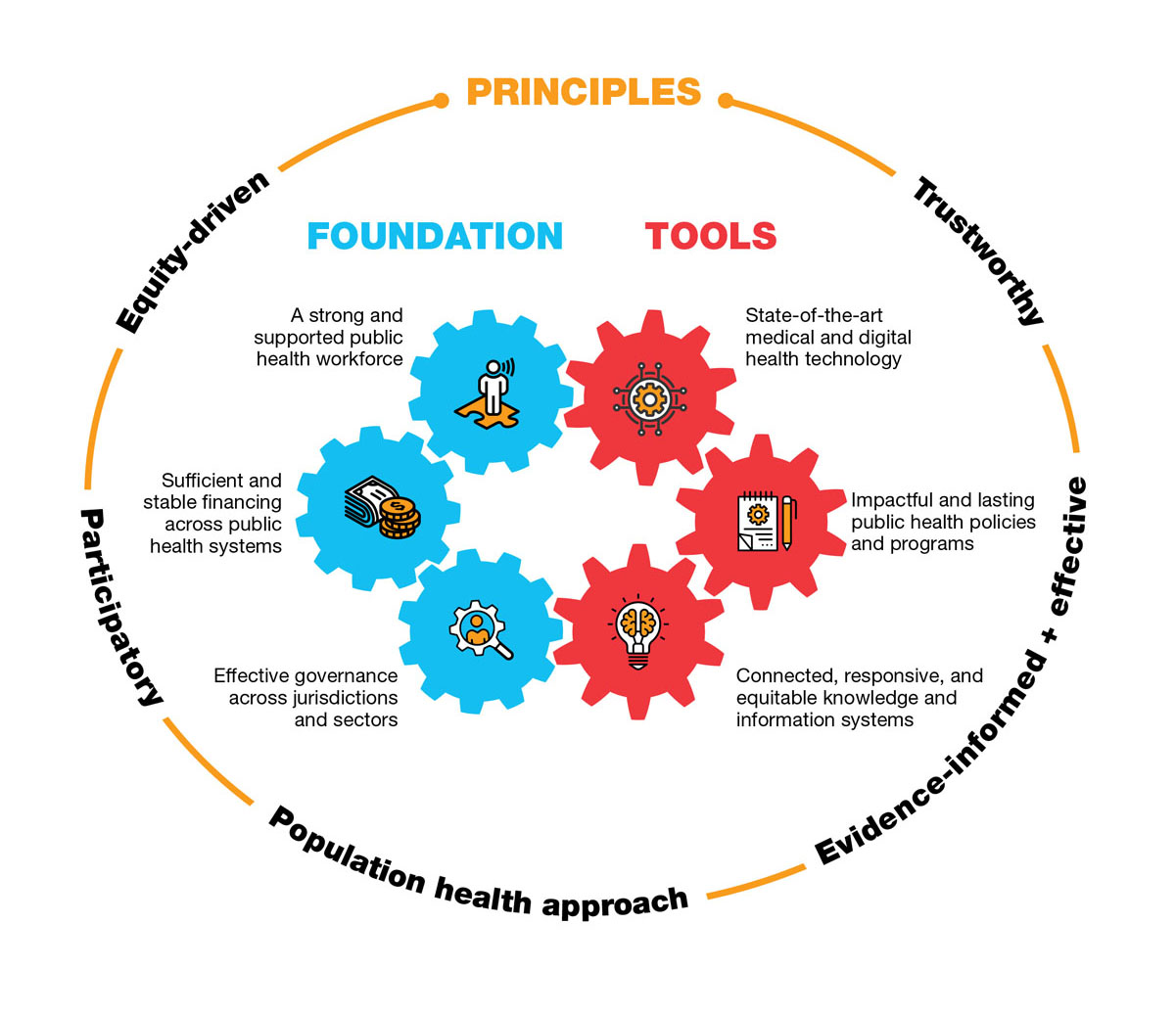
Figure 12: Text description
The figure describes the elements needed for a world-class public health system to achieve optimal health and well-being for all people living in Canada.
The elements of a world-class public health system are displayed in 3 categories.
- Foundation of the public health system, displayed as interconnected gears:
- A strong a supported public health workforce;
- Sufficient and stable financing across public health systems; and,
- Effective governance across jurisdictions and sectors.
- Tools of the public health system, displayed as interconnected gears:
- State of the art medical and digital health technology;
- Impactful lasting public health policies and programs; and,
- Connected, responsive, and equitable knowledge and information systems.
- Principles:
- Surrounding the foundation and tools in a circle are principles of the public health system: trustworthy, evidence-informed and effective, population health approach, participatory, and equity-driven.
Principles to guide transformation and beyond
These principles illuminate overarching values that drive the work of public health systems. They can help steer the collective efforts of the people, organizations, and institutions that make up the public health systems in Canada as they move through and achieve transformation (Table 5).
| Principle | Goal | In practice |
|---|---|---|
| Trustworthy | Earn trust through continuous reflection and transparency, and being accountable to the people it serves | A public health system that is credible and trusted translates into better health outcomes. Actions that promote and foster trust require open and clear communication, equitable partnerships, accountability, and transparency. A trusted public health system works to prevent unintended consequences that could compromise trust. The importance of trust was underscored in national responses to COVID-19 across countriesFootnote 557. |
| Evidence-informed and effective | Value inclusive, diverse, and high-quality systems of knowledge and evidence to make the best decisions for the health of populations | Effectiveness refers to policies and programs achieving their potential impact under real-word conditionsFootnote 558. It is the ability of public health to affect positive change to improve the population’s health, across a wide range of settings, while also promoting equitable outcomesFootnote 559. Effectiveness in public health includes innovation, partnership and engagement, evidence-informed decision-making, translating science into action, monitoring and evaluation, and supporting researchFootnote 559 Footnote 560. |
| Population health approach | Stimulate action across sectors to improve the health of all populations and reduce inequities among communities | Actions live at the population level, rather than the individual levelFootnote 561. The focus is on improving the health status and reducing health inequities among and between populations. Crucial to this approach is intersectoral action and the recognition that good health is a shared goal and responsibility is joint among many sectors, organizations, and actorsFootnote 253. |
| Participatory | Seamlessly integrate community and citizen participation and co-creation into the core of public health practice and action | Public participation informs public health action and engages individuals and communities around issues that are important to their experiences. Strengthening community participation within public health systems across networks and scales can be achieved through consistent collaboration, ensuring clear accountabilities, and centring community self-determination through processes of engagement, co-production, and governanceFootnote 385. |
| Equity-driven | Prioritize inclusion and diversity of voices at decision-making tables while striving for reconciliation | Actions are purposefully designed and implemented to address often long-standing inequities that impact the populations’ health. This requires a robust agenda that includes social investments, cross-sectoral and cross-jurisdictional action, and stronger leadership within and beyond the health sectorFootnote 290. Particular attention is needed to strive towards decolonizing public health. |
Foundation and tools of a strong system
With the principles as guides, the building blocks introduced in Section 2 offer a frame to articulate elements that make up the foundation and tools of a stronger and more resilient system (Table 6).
While many of these ideas may not be new, when advanced together they can lead to a true culture shift, one that brings population health into focus and elevates health and well-being to a fundamental priority for society.
These ambitious but necessary elements are not the only areas that need attention. This list is intended to be a starting point to wider discussions, reflection, and action.
| Tools |
|---|
| Building block 1: Impactful and lasting public health policies and programs |
|
| Building block 2: Connected, responsive, and equitable knowledge and information systems |
|
| Building block 3. State-of-the-art medical and digital health technology |
|
| Foundation |
| Building block 4. A strong and supported public health workforce |
|
| Building block 5. Sufficient and stable financing across public health systems |
|
| Building block 6. Effective governance across jurisdictions and sectors |
|
The way forward
COVID-19 tested public health systems across Canada and around the world. It amplified known weaknesses, revealed new challenges, and highlighted the need for resilience. As we continue to face evolving and worsening threats to human health, such as climate change, the opioid overdose crisis, antimicrobial resistance, and the burden of non-communicable diseases, we need to ensure that our public health systems are better equipped to address these complex challenges. Simply put, we were not adequately prepared to face an emergency of the scale and magnitude of COVID-19. We must do better for the future.
The pandemic has underscored the importance of public health’s role in preventing disease, promoting healthy behaviours, and working upstream across sectors to address the drivers of poor health. It has demonstrated how public health can protect the sustainability of the healthcare system by preventing people from getting sick and hospitals from becoming overwhelmed. It has also demonstrated that when we work to improve the living conditions and well-being of those most at risk, we are collectively safer and healthier. When kids are healthy, they learn better. When employees are in good health, they are more likely to obtain and maintain employment. Investments in public health are therefore investments in a healthier society overall.
There have been numerous calls to reform the public health system, both historically and during the COVID-19 response, but there are additional and increasingly urgent signs that we need to act now. As Canada looks toward pandemic recovery, heavy demands on the healthcare system threaten to overshadow the equally critical need to bolster the public health system. As COVID-19 has shown, both systems must be sufficiently supported for Canada to have a reliable and responsive health system that can meet the needs of its people.
We now have an important window of opportunity to begin the transformation journey. One that aims to achieve a more sustainable health system and a more equitable society.
Priority action areas for public health renewal
The pandemic has shown the need for a strong and agile public health system that is able to innovate and adapt to new and emerging issues and challenges. As the urgency of the pandemic subsides, there will be opportunities for transformation across health, social, and economic systems. Ensuring a world-class public health system that is equity-driven, trustworthy, participatory, and effective is Canada’s best defence against future public health threats.
Building on the elements set out in Section 3, this Way Forward proposes 4 priority areas of action, along with a suite of “actionable ideas” to stimulate system transformation. Transformation will take sustained commitment and investment. It will also require public health to embrace a culture of continuous learning, be on the cutting-edge of innovation, and build strong bridges between communities and sectors, both locally and with our global partners.
In a nutshell, transformation will require:
- Fostering excellence in the public health workforce;
- Improving our tools;
- Modernizing our models of governance; and,
- Ensuring stable and consistent funding.
Fostering excellence in the public health workforce
The pandemic has placed unprecedented demands on Canada’s health workforce, including those in public health. Many have been working day and night for close to 2 years. Our public health professionals are highly trained in keeping populations healthy and protecting them from injuries and disease threats – but reports of burnout are increasing and resources are stretched thin.
Investing in public health workforce capacity requires urgent attention, given the continued burden of COVID-19 on public health practitioners and the ever-present risk of concurrent public health crises. The goal is to recruit and retain a workforce that has both deep expertise in public health and the ability to work across many related disciplines, including from the fields of data science, behavioural science, economics, sociology, and even engineering, in order to develop and scale innovative solutions.
As a start, we need to update our public health competencies to ensure our workforce has the diversity of skills it needs to meet today’s complex public health challenges. Ensuring that staff have a strong foundation in the essential functions of public health (i.e., surveillance, health assessment, health promotion and protection, emergency preparedness and response, as well as disease and injury prevention) is critical but insufficient. Public health practitioners must also have the ability to work across sectors and communities, and to effectively interpret data and communicate rapidly evolving science in the information age.
Importantly, the public health workforce must lead by example and demonstrate the power of what an inclusive and diverse workforce can do. When all staffing levels of an organization represent the communities they serve, they are better able to meet their needs and reduce systemic stigma in policies and services. This is especially vital in the field of public health, which aims to reduce inequities that lead to poor health
Finally, workforce planning must be future-oriented. This includes developing present and future generations of public health professionals and ensuring there is surge capacity, through partnerships with academic institutions and nongovernmental organizations, such as the Canadian Red Cross, in order to rapidly mobilize additional resources in times of emergency. Transition and continuity planning are also important. The success of public health relies on cultivating strong relationships both within and outside of the sector. High employee turnover and attrition not only leads to a loss of knowledge and experience, but also means that organizations must start over in forging these relationships. By prioritizing learning and development, fostering excellence among staff, and improving human resource planning, public health institutions can become magnets for new and emerging talent and be better positioned to meet future demands.
Actionable ideas to foster excellence in the public health workforce
- Modernize public health competencies to match current requirements for public health practice. This includes the ability to co-design initiatives across communities, disciplines, and sectors; to deliver risk communications to address mis- and disinformation; to translate science into policy options; and, to embed cultural safety and cultural humility into public health policy and practice.
- Build surge capacity to increase system responsiveness and nimbleness. This includes standing agreements with universities and nongovernmental organizations, maintaining rosters of public health expertise, and community networks that can mobilize local capacity.
- Support dynamic on-the-job training and learning for public health students and professionals. This includes joint appointments and exchanges between academic and public health institutions, review of university curricula, and expansion of effective training programs, such as the Canadian Field Epidemiology Program, the Public Health Officers Program, and support for the development of an Indigenous field epidemiology training program.
Improving our tools
More and better data
Good data and intelligence are fundamental to understanding patterns of illness, injury, and harm, and how best to target public health interventions. During a pandemic, having the right information at the right time is vital to understanding how diseases spread, to identifying those who are most at risk, and to predicting future scenarios to guide public health measures.
There is no doubt that our pandemic response was limited, in part, due to significant gaps in our public health surveillance and data systems. This includes a lack of data on race and ethnicity, a lack of comparable data between provinces and territories, and information gaps at the local level. These gaps in our system are not new. Public health reviews over the course of the past 40 years have pointed to the need to strengthen our surveillance systems. In this day and age, it is unacceptable that public health does not have the information it needs at all levels to monitor public health challenges and to effectively target intervention efforts.
A pan-Canadian data ecosystem that is interoperable, equitable, and ethical
In Canada, we are still working with multiple independent data systems that do not speak or connect with each other. As a result, data are fragmented across jurisdictions, governmental organizations, and communities. It is imperative that we work together to improve data sharing and comparability, in order to provide decision makers across the country with the intelligence they need to inform policies and programs, and to provide more transparency for Canadians on the health of their communities.
One key step will be to establish an interoperable system that facilitates the linking and pooling of data from various sources, including epidemiological, clinical, and administrative data. This could function as a cooperative network, with clear standards to ensure that data are handled in ways that are secure and culturally safe. At the heart of this system, we must prioritize and embed equity, including a commitment to gather disaggregated data, foster community collaboration, and ensure access to data in a privacy-sensitive manner. Fundamentally, such a system must respect the rights of First Nations, Inuit, and Métis Peoples, for communities to own, share, and control their own data.
Better insights
In order to turn data into actionable insights, public health needs the right analytic tools. This includes cutting-edge predictive modelling to forecast disease patterns, and leveraging the power of technology, such as artificial intelligence, to detect early warning signals of a new public health threat.
Effective early warning, foresighting, and health emergency surveillance requires working more closely with academic and private sector experts, and with our international partners, to strengthen and combine human analysis and machine learning about emerging threats. As we have learned in the pandemic, our early warning systems need to be well-integrated with government decision-making structures and include strengthened risk assessment processes that are coordinated across jurisdictions.
Accelerating knowledge translation
We must continue our work to find innovative ways to close the gap between knowledge generation, policy, and practice. The pandemic highlighted the need for the rapid generation and synthesis of emerging research on COVID-19 in order to inform public health actions. Innovative initiatives, such as COVID-END and the CanCOVID networks, created to review and synthesize evolving research, as well as the COVID-19 modelling network and the Canadian COVID-19 Genomics Network, can serve as models for the future by connecting public health leaders, university scientists, and governments across the country. The National Collaborating Centres for Public Health act as a knowledge hub for policy and practice across Canada. Moving forward, we need to find more effective ways to mobilize the work of knowledge translation hubs, both within the public health community as well as with partners and actors in other sectors that influence population health.
When evidence is quickly evolving, healthcare workers and service providers need clear, timely, and culturally safe guidance on how best to prevent the spread of infection and how to most effectively treat infected patients. While there are well-established, independent expert committees, such as the National Advisory Committee on Immunization, that have provided advice to public health officials prior to and during the COVID-19 pandemic, there is no mechanism to regularly update clinical management guidelines at the national level. Moving forward, we need to ensure that the right advisory bodies and supports are in place, including surge capacities, to rapidly develop a range of technical guidance for the prevention, control, and treatment of emerging infectious diseases.
A stronger public health research agenda
Public health is a science-based field that prides itself on working from the best available evidence, but there is still a lot that we have yet to learn about public health policy and practice in Canada and around the world. For example, more research is required on public health governance, organization models, and standards, to build on our understanding of which models work best to improve health and reduce inequities.
We also need more interdisciplinary research to measure the impact of upstream actions on health outcomes. It has often been said that Canada is a nation of pilot projects, with different interventions being tested in different parts of the country to address public health issues or social factors that affect health, such as precarious employment, harms from opioid use, or maternal health. Working with the Canadian Institutes of Health Research and other partners, we need a research agenda to more systematically evaluate the effectiveness and sustainability of local interventions in order to be able to identify, scale, and spread best practices in partnership with communities.
A more inclusive knowledge base
Finally, we must reconsider our knowledge base in public health and broaden its scope. For example, traditional Indigenous concepts of health and well-being are holistic and relational in nature, connecting individual health with the health of the land, the environment, the community, and the vibrancy of one’s culture. Historically, Indigenous ways of knowing, such as oral histories, storytelling, and community participation have often been unacknowledged or undervalued. Collaborations that include and value First Nations, Inuit, and Métis knowledge can enrich both the science and practice of public health in Canada and lead to innovative services that better address the needs of communities.
Improving our pipeline of biomedical solutions
COVID-19 underscored the need to work with domestic and global partners to undertake research, scale up production, and address barriers to equitable access to state-of-the-art vaccines, diagnostics, and therapeutics. The pandemic has ushered in a new era of health innovation and catalyzed important partnerships between public health institutions, academia, and industry. Looking to the future, this collaboration should be sustained and enhanced. Ensuring that Canada is able to effectively respond to emerging health threats requires all actors across the research, development, and production pipeline to work together in order to define health technology requirements and drive solutions that protect the public’s health. Through international cooperation and collaboration in this arena, we not only contribute to health security globally, but also to ensuring that the people of Canada are protected both at home and abroad.
The Government of Canada’s Biomanufacturing and Life Sciences Strategy is an important step in this direction. Governments must continue to work closely with scientists and industry to develop Canada’s talent pipeline, manufacturing, and distribution capacity to produce state-of-the-art emergency tests, equipment, vaccines, and treatments that can rapidly be deployed. As part of this work, public health institutions need to be systematically engaged to define public health priorities and translate these into guidance for economic and industrial policy, and ultimately, into life saving products and technologies.
Actionable ideas to improve public health tools
- Accelerate the implementation of the Pan-Canadian Health Data Strategy with clear phased milestones. This includes prioritizing systems for interoperable use, such as a national network of vaccine registries that includes socio-demographic data as well as linkages across epidemiological, biomedical, clinical, and health administrative data.
- Re-invigorate national and cross-jurisdictional threat detection and foresight systems, including risk assessment, modelling, scenario planning, and situational awareness.
- Prioritize implementation of ownership and control principles for First Nations, Inuit, and Métis Peoples across data systems.
- Enhance rapid and ongoing population health intervention research for prevention and well-being initiatives, and strengthen interdisciplinary knowledge synthesis models, such as the National Collaborating Centres for Public Health.
- Leverage Canada’s Biomanufacturing and Life Sciences Strategy to systematically engage the public health and research and development sectors to identify strategic and critical health technologies and countermeasures to inform industrial policy and decision-making.
Modernizing our models of governance
Stronger mandate and accountability for public health across federal, provincial, and territorial governments
Public health is a shared responsibility between federal, provincial, and territorial (FPT) governments and local public health authorities. While COVID-19 has demonstrated the strengths of our collective response, it has also highlighted gaps in our pandemic preparedness plans and the need to revisit our governance models in order to be better prepared for the future. This starts with strengthening the mandate of public health within the FPT health system, and making governments more accountable for public health objectives and outcomes.
As a critical first step in this transformation process, we need to clarify the role of public health across jurisdictions and ensure essential functions are consistent with evolving global definitions to meet today’s complex cross-border challenges, from antimicrobial resistance to climate change. Governments must then work together to identify common public health priorities and outcomes tied to funding commitments that can be measured and reported back to Canadians in an annual report card. This will require the development of comparable performance indicators to measure the effectiveness and outcomes of public health policies. This level of accountability will help identify areas in need of improvement, and ensure that public health is better equipped to reduce health inequities and better prepared for the next emergency.
Finally, it is important that public health governance mechanisms include Indigenous public health expertise and perspectives to enable self-determination, for First Nations, Inuit, and Métis Peoples. This means ensuring that Indigenous communities and partners are adequately supported to develop and implement their own public health plans and priorities, including holistic, community-based local solutions in partnership with public health authorities.
A stronger voice for public health at the decision-making table
Public health leaders have provided valuable scientific advice to decision-makers throughout the COVID-19 pandemic. It will be important that public health leaders continue to have regular access to decision-makers in the future, in order to ensure that Canada is prepared to address the next public health crisis, that the health system is oriented towards enhancing wellness, and to continue the critical work of reducing health inequities. Within the FPT health arena, this includes ensuring that public health continues to have a more prominent place on the FPT health agenda and ongoing support for the participation of Chief Medical Officers of Health in governance discussions. Engagement with other governance tables beyond health should also be encouraged.
Strengthening intersectoral connections
The pandemic put in stark relief the complex interaction of the social determinants of health – factors such as education, economic stability, job security, and stable housing – in shaping health outcomes and driving health inequities. Perhaps now, more than at any other point in recent history, the vital connection between good health and social, environmental, and economic conditions has become apparent to both decision-makers and the public alike.
It is, by now, a well-accepted fact that much of what makes us healthy lies outside of the health system. Those most at risk of COVID-19 are also those most affected by structural inequities and chronic illnesses. While biomedical solutions, such as vaccines, have been important tools in combatting COVID-19, social solutions, including income support, paid sick leave, and other housing and employment supports, have also been critical.
New ways of working are required to improve the social conditions that drive health outcomes. The pandemic has made visible the importance of bringing together all sectors of society in the fight against COVID-19 – including businesses, civil society, and other government departments. We must now bring that same energy of collaboration to create upstream policy alliances to reduce health inequities, where collective action is based on clear and measurable indicators. One encouraging approach from the field of social innovation is “collective impact”. This provides a framework for addressing health and social priorities by developing common goals and coordinating mutually reinforcing action across sectors, all driven by shared accountability.
Harnessing the power of communities
Public health’s patient is the population. To be effective at protecting the health of populations requires strong collaboration and decision-making across sectors and jurisdictions, including with communities across the country. From organizing vaccine campaigns, to food deliveries for those in need, community leaders have been instrumental in developing tailored solutions that take into account the lived experience, unique challenges, and specific needs of their members.
The leadership of Indigenous communities in developing holistic well-being and tailored pandemic planning offers a glimpse of what can be done when First Nations, Inuit, and Métis public health leaders and organizations are supported to own governance of Indigenous health. Likewise, the power of African, Caribbean, and Black Canadian leadership in improving vaccine uptake demonstrated that community-determination has a strong role in achieving positive health outcomes.
Community-first initiatives require innovative new models of shared governance and collaboration that allow local expertise. The closer we work to bridge local realities with global evidence, harnessing our collective expertise, the better equipped we will be to organize quickly and respond to emergencies effectively.
Actionable ideas for modernizing governance
- Modernize essential public health functions (or public health roles across the country) to respond to changes in the current public health landscape and in alignment with global reflections.
- Develop a pan-Canadian mandate on public health with clear priorities, objectives, essential functions, and roles to guide FPT decision-making and investments. This would include annual reporting on progress towards meeting common goals. Also ensure that First Nations, Inuit, and Métis public health planning and priorities are supported to meet needs in a proactive and flexible way that supports self-determination and holistic local solutions.
- Develop a public health systems research strategy to inform standardized performance indicators and annual reporting on public health policies and services across Canada.
- Re-tool pandemic plans to include health, social, and economic sectors, and ensure pandemic preparedness with sustainable funding, testing, and annual public reporting on state of readiness.
- Create a health equity monitoring and reporting system with intersectoral leaders to improve and track the social factors that can protect populations from future pandemics and other health challenges.
- Build community and equity into public health decision-making processes by incorporating accountabilities for community engagement, co-design, and implementation at the community level.
Ensuring stable and consistent funding
Future-proofing our public health system requires appropriate investments in our people, our tools, and our governing structures. It also requires more consistent, stabilized funding to meet today’s complex crises and better prepare for tomorrow.
Public health resources are often scaled back after public health emergencies as governments move to address other priorities. This is referred to as the “boom and bust” cycle of public health spending. This places the public health system at a disadvantage at the onset of each crisis by not having the capacity or the networks required for a rapid response.
Investing in public health is a smart investment with direct and indirect impacts to both social and economic well-being. Public health is the outbreak that did not happen, the traumatic injury that did not occur, and the overdose that was avoided. Public health protects the sustainability of our healthcare system by reducing demand for costly medical treatments, and helping people to stay healthy and well. As the pandemic has clearly demonstrated, when we fail to prioritize public health, people get sick, the healthcare system can become overwhelmed, and the economy suffers.
Though difficult to measure precisely, the Canadian Institute for Health Information estimates that in 2019, just under 6% of all health spending was allocated to public health in Canada. We must ask ourselves if this is a sufficient level of investment given the critical role that public health plays in keeping Canadians healthy and safe.
Spending on public health needs to be more transparent in government budgets and tied to clear performance objectives and results to make it more visible and accountable to the public. Flexible funding models are also required to support First Nations, Inuit, and Métis self-determination, and ensure Indigenous communities are supported to develop approaches and interventions, tailored to their needs.
Actionable ideas for funding
- Step up funding to reach permanent budget levels that match the public health mandate.
- Work with FPT governments to ensure that budgets clearly identify priorities and funding for public health policies and services, as public health investments reduce healthcare costs and lost economic opportunities.
- Support First Nations, Inuit, and Métis health and well-being with targeted funding for Indigenous-led public health programs.
- Use federal funds to achieve common public health priorities and objectives, and develop indicators to report on outcomes at the FPT level.
A call to action
We are now at a pivotal moment. Public health in Canada has risen to the challenge of COVID-19, but its resources are stretched thin.
Reflecting on our pandemic experience, we can decide what kind of public health system, and ultimately, society we want to have, moving forward. A world-class public health system that is resilient and protects all of us will be our best insurance policy against future public health crises. It will also ensure that we are well-equipped to navigate the increasingly complex health threats that we see on the horizon.
As we speak, countries around the world are beginning to undertake similar critical reflections. Lessons learned and emerging best practices can be shared across borders and inform our path forward to transform our public health system and achieve optimal health for all people in Canada.
The pandemic has awakened many to the understanding that our health system is more than managing illness through medicines and hospital procedures — it means preventing these illnesses from happening in the first place, whenever possible.
By working together, learning from one another, across communities, governments, sectors, and society, and collaborating with others around the world, we can begin the process of building a world-class public health system and a healthier and stronger society at large.
Appendix A: Methodology
Process
The 2021 Chief Public Health Officer of Canada (CPHO) Annual Report was drafted based on a review of the best available evidence, including evidence from research, academic expertise, practical and applied public health expertise, community expertise, and traditional ways of knowing. Instead of completing rapid reviews based on a point-in-time search, the identification and synthesis of new knowledge occurred during the entire writing process to allow for adoption of the continuously changing state of the evidence and cumulative experience. In response to content priorities, some of the information presented in the report was synthesized from commissioned, independent evidence reviews and pertinent themes emerging in expert consultations. For research, sources beyond systemic reviews were required, including primary research through peer-reviewed publications, pre-prints, grey literature, and expert consultation. Where possible, Canadian research and representative data were prioritized. Epidemiological data were derived from federal, provincial, territorial, or municipal government sources, as much as possible.
Developed during the ongoing COVID-19 pandemic, the information about COVID-19 reflects the evolving nature of the science and our understanding of the virus and its impacts.
The evidence was identified through:
Research reviews
- Ongoing and frequent literature searches, completed by sub-topic using online databases such as Medline and Scopus, as well as identifying new and existing research maintained by various academic publishers, such as BMJ, the Lancet, and Elsevier
- Rapid review initiatives across Canada such as the COVID-19 Evidence Network to Support Decision-Making (COVID-END), CanCOVID, and the National Collaborating Centre for Methods and Tools evidence platform
Surveillance updates, public health reports, and other grey literature
- A review of national, provincial/territorial, and municipal public health publications, particularly epidemiological and public survey reports
- Grey literature and policy reviews of trusted sources, such as: public health organizations (e.g., World Health Organization) and government publications (e.g., Public Health Ontario)
- Epidemiological information, as per the following order of priority: COVID-19 case report information shared with the Public Health Agency of Canada (PHAC) by provincial/territorial governments and national research networks, publicly reported data from provincial and territorial websites, press briefings by health authorities, and media reports
- Information published or shared by other federal departments, such as Statistics Canada and Indigenous Services Canada
Engaged evidence reviews
- Commissioned reports from independent public health experts:
- An Evidence-Informed Vision for a Public Health Data System in Canada by Dr. David Buckeridge
- Governing for the Public’s Health: Governance Options for a Strengthened and Renewed Public Health System in Canada by Dr. Erica Di Ruggiero, Ms. Dominika Bhatia, Ms. Imaan Umar, Ms. Emmanuelle Arpin, Ms. Clara Champagne, Dr. Carole Clavier, Dr. Jean-Louis Denis, Dr. David Hunter
- Visioning the Future: First Nations, Inuit, & Métis Population and Public Health by Dr. Margo Greenwood (Editor), Dr. Evan Adams (Editor), Dr. Marcia Anderson, Donna Atkinson, Dr. Danièle Behn Smith, Dr. Sarah Funnell, Theresa Koonoo (with contributions from: Rebecca Lonsdale, Sarah MacRury, Igah Sangoya, Meeka Kiguktak, Janice Panimera, and Jeanie Aulaqiaq), Dr. Shannon McDonald, Clara Morin Dal Col, Dr. Christopher Mushquash, Dr. Janet Smylie, Dr. Shannon Waters, Dr. Eduardo Vides, and National Indigenous Organizations: Assembly of First Nations, Inuit Tapiriit Kanatami, and Métis National Council
- Strengthening Community Connections: The Future of Public Health is at the Neighbourhood Scale by Dr. Kate Mulligan
Discussion groups and key informant interviews
- Collaboration with internal and external expert stakeholders, Public Health Agency of Canada (PHAC) programs and surveillance leads, and the Canadian Institute for Health Information (CIHI)
- A targeted consultation process, engaging a diversity of stakeholders from public health organizations, academia, community-based organizations, and government. The summary of the key themes from these discussions was published in a “What We Heard” Report entitled A Renewed and Strengthened Public Health System in Canada. This stakeholder engagement process included:
- A Best Brains Exchange meeting, co-hosted between PHAC and the Canadian Institutes of Health Research (CIHR)
- Five discussion groups, each focussing on a different group of participants:
- Researchers and thought leaders involved in systems thinking and social innovation;
- CIHR grantees involved in research on public health system and infrastructure innovation;
- Members of the CPHO Health Professional Forum;
- Members of the Special Advisory Committee on COVID-19; and
- Local Medical Officers of Health
- Six key informant interviews with public health experts and leaders
- Informed by the national consultation process, “Community Dialogue on the Future of Canadian Public Health Systems” led by CIHR’s Institute of Population and Public Health
Limitations
Scope and literature search
The 2021 CPHO Annual Report explores the broad impacts of COVID-19 and a vision for the future of the public health system in Canada. Since the purpose of the report is to provide an overview of presented topics and concepts, there are necessary restrictions on the level of detail provided in each section. Given the available evidence at the time and the tight timeframe for producing the report, this document does not represent an exhaustive evidence review or extensive consultations across all public health systems’ stakeholders in Canada. Only literature published in English and French was reviewed. A detailed assessment of study quality and risk of bias was not conducted in this review, and this may be particularly consequential given the preliminary nature of some resources and findings.
Language
To the extent possible, we attempted to use standardized, inclusive, and culturally appropriate language when drawing on evidence related to different communities and their experiences of health. However, in some instances we relied on the terminology included in the source documents (e.g., visible minorities), if appropriate alternative language could not be identified.
Acknowledgements
Many people and organizations provided invaluable insights and advice in the development of this report.
I would like to express my gratitude to expert advisors who provided strategic advice and guidance in framing the report and reading many drafts:
- Dr. M. Mustafa Hirji, Medical Officer of Health (Acting), Niagara Region, Ontario
- Dr. David Mowat, Public health consultant; former Medical Officer of Health, Peel Public Health
- Dr. Cory Neudorf, Professor, Department of Community Health and Epidemiology, College of Medicine, University of Saskatchewan, and interim Senior Medical Health Officer, Saskatchewan Health Authority
- Prof. Duncan Selbie, President of the International Association of National Public Health Institutes and former chief executive of Public Health England
- Dr. Gaynor Watson-Creed, Assistant Dean, Serving and Engaging Society, and Assistant Professor, Department of Community Health and Epidemiology, Faculty of Medicine, Dalhousie University
In addition, I would like to thank colleagues who led the development of independent reports that inform my annual report and who provided additional subject matter expertise:
- Dr. Evan Adams, Deputy Chief Medical Officer of Public Health, Indigenous Services Canada
- Dr. David Buckeridge, Professor, Department of Epidemiology, Biostatistics and Occupational Health, McGill University
- Dr. Erica Di Ruggiero, Associate Professor, Dalla Lana School of Public Health, University of Toronto
- Dr. Margo Greenwood, Academic Leader, National Collaborating Centre for Indigenous Health
- Dr. Kate Mulligan, Assistant Professor (status), Dalla Lana School of Public Health, University of Toronto
I would also like to extend sincere thanks to the many staff at the Public Health Agency of Canada who provided significant insights and guidance throughout the development of the report.
I want to acknowledge the Canadian Institute for Health Information and Health Canada for contributing data and information cited in this report. In addition, I would like to thank partners at Employment and Social Development Canada, Statistics Canada, and Indigenous Services Canada for sharing information and/or critically reviewing report content. Thanks also to our colleagues at the Canadian Institutes of Health Research for co-hosting a Best Brains Exchange, assisting with engagement activities, and providing valuable advice and evidence sources.
My sincere appreciation to the nearly 150 leaders from across Canada, including medical officers of health, public health practitioners and leaders, researchers, policy-makers, and other service providers who participated in interviews and discussion groups. The latter includes members of the Chief Public Health Officer Health Professional Forum, the Public Health Network's Special Advisory Committee on COVID-19, and the Local Medical Officers of Health. Your insights and feedback helped inform my report on what is needed to transform public health in Canada and improve people's health.
My thanks to the teams in the Office of the Chief Public Health Officer who came together to support the development of my report. Special thanks to the Reports team for their commitment and dedication in seeing this report from conception to publication: Tammy Bell, Fabienne Boursiquot, Dr. Marie Chia, Dr. Charlene Cook, Dr. Sarah Drohan, Elyse Fortier, Rhonda Fraser, Dr. Kimberly Gray, Dr. David Grote, Bonnie Hostrawser, Jessica Lepage, Danielle Noble, Kelly Kavanagh Salmond, Kelsey Seal, and Inès Zombré.
References
- Footnote 1
-
Public Health Agency of Canada. COVID-19 Epidemiology Internal Data. Public Health Agency of Canada; 2021.
- Footnote 2
-
Statistics Canada. Provisional Death Counts and Excess Mortality, January 2020 to March 2021. The Daily; 2021.
- Footnote 3
-
Statistics Canada. Changes in Causes of Death, 1950 to 2012. Government of Canada; 2016.
- Footnote 4
-
Bourbeau, R, Ouellette, N. Trends, Patterns, and Differentials in Canadian Mortality over Nearly a Century, 1921-2011. Canadian Studies in Population. 2016; 43(1-2):48–77.
- Footnote 5
-
Tam, T. From Risk to Resilience: An Equity Approach to COVID-19. Ottawa, ON: Public Health Agency of Canada; 2020.
- Footnote 6
-
Public Health Agency of Canada. Statement from the Chief Public Health Officer of Canada on August 27, 2021. Government of Canada; 2021.
- Footnote 7
-
Canadian Public Health Assocation. Review of Canada’s Initial Response to the COVID-19 Pandemic. Canadian Public Health Assocation; 2021.
- Footnote 8
-
Public Health Agency of Canada. Weekly COVID Surveillance Indicator Report - Week Ending May 7, 2021. Public Health Agency of Canada; 2021.
- Footnote 9
-
Moriarty, T, Boczula, AE, Thind, EK, Loreto, N, McElhaney, JE. Excess All-Cause Mortality During the COVID-19 Epidemic in Canada. Royal Society of Canada; 2021.
- Footnote 10
-
Cameron-Blake, E, Breton, C, Sim, P, Tatlow, H, Hale, T, Wood, A, et al. Variation in the Canadian Provincial and Territorial Responses to COVID-19. Blavatnik School of Government Working Paper. 2021.
- Footnote 11
-
Public Health Agency of Canada. Update on COVID-19 in Canada: Epidemiology and Modelling - September 22, 2020. Government of Canada; 2020.
- Footnote 12
-
Public Health Agency of Canada. Update on COVID-19 in Canada: Epidemiology and Modelling - October 30, 2020. Government of Canada; 2020.
- Footnote 13
-
Public Health Agency of Canada. Update on COVID-19 in Canada: Epidemiology and Modelling - April 23, 2021. Government of Canada; 2021.
- Footnote 14
-
Public Health Agency of Canada. Federal/Provincial/Territorial Public Health Response Plan for Ongoing Management of COVID-19. Government of Canada; 2021.
- Footnote 15
-
Government of Canada. Individual and Community-Based Measures to Mitigate the Spread of COVID-19 in Canada. Government of Canada; 2021.
- Footnote 16
-
Government of Canada. COVID-19: Main Modes of Transmission. Government of Canada; 2021.
- Footnote 17
-
Public Health Agency of Canada. Statement from the Chief Public Health Officer of Canada on February 10, 2021. Government of Canada; 2021.
- Footnote 18
-
Government of Canada. Non-Medical Masks: About. Government of Canada; 2021.
- Footnote 19
-
Public Health Agency of Canada. COVID-19: Guidance on Indoor Ventilation during the Pandemic. Government of Canada; 2021.
- Footnote 20
-
Parkin, A. All in This Together? Canadians’ Views on Masks, Vaccines and Lockdowns during the COVID-19 Pandemic. The Confederation of Tomorrow. 2021.
- Footnote 21
-
Desveaux, L, Mosher, R, Buchan, JL, Burns, R, Corace, KM, Evans, GA, et al. Behavioural Science Principles for Enhancing Adherence to Public Health Measures. Science Briefs of the Ontario COVID-19 Science Advisory Table. 2021.
- Footnote 22
-
Impact Canada. COVID-19 Snapshot Monitoring Study (COSMO Canada). Government of Canada; 2021.
- Footnote 23
-
Dionne, M, Dubé, E, Pelletier, C. COVID-19 - Pandémie et Impacts sur la Vie Personnelle. Institut national de santé publique du Québec:2021.
- Footnote 24
-
Impact Canada. COVID-19 Snapshot Monitoring Study (COSMO Canada) Wave 12 Report. Government of Canada; 2021.
- Footnote 25
-
Impact Canada. COVID-19 Snapshot Monitoring Study (COSMO Canada) Wave 11 Report. Government of Canada; 2021.
- Footnote 26
-
Brankston, G, Merkley, E, Fisman, DN, Tuite, AR, Poljak, Z, Loewen, PJ, et al. Socio-Demographic Disparities in Knowledge, Practices, and Ability to Comply with COVID-19 Public Health Measures in Canada. Canadian Journal of Public Health. 2021; 112(3):363-75.
- Footnote 27
-
Government of Canada. SARS-Cov-2 Variants: National Definitions, Classifications and Public Health Actions. Government of Canada; 2021.
- Footnote 28
-
Public Health Agency of Canada. Weekly COVID Surveillance Indicator Report - Week Ending July 30, 2021. Public Health Agency of Canada; 2021.
- Footnote 29
-
Tuite, AR, Fisman, DN, Odutayo, A, Bobos, P, Allen, V, Bogoch, II, et al. COVID-19 Hospitalizations, ICU Admissions and Deaths Associated with the New Variants of Concern. Ontario COVID-19 Science Advisory Table. 2021.
- Footnote 30
-
Public Health Agency of Canada. Update on COVID-19 in Canada: Epidemiology and Modelling - July 30, 2021. Government of Canada; 2021.
- Footnote 31
-
Public Health Agency of Canada. COVID-19 Border Response Provides Case Study for Assessing Canada’s Future Approach to Border and Travel Health. Public Health Agency of Canada; 2021.
- Footnote 32
-
Transport Canada. Government of Canada Introduces Further Restrictions on International Travel. Government of Canada; 2021.
- Footnote 33
-
Public Health Agency of Canada. Government of Canada Invests $53 Million to Address COVID-19 Virus Variants of Concern. Government of Canada; 2021.
- Footnote 34
-
Public Health Agency of Canada. Statement from the Chief Public Health Officer of Canada on June 7, 2021. Government of Canada; 2021.
- Footnote 35
-
Public Health Agency of Canada. CPHO Issue Statement Series on COVID-19: mRNA Vaccines. Government of Canada; 2021.
- Footnote 36
-
Health Canada. Health Canada Authorizes First COVID-19 Vaccine. Government of Canada; 2020.
- Footnote 37
-
Government of Canada. Drug and Vaccine Authorizations for COVID-19: List of Authorized Drugs, Vaccines and Expanded Indications. Government of Canada; 2021.
- Footnote 38
-
Government of Canada. Vaccines and Treatments for COVID-19: Progress. Government of Canada; 2021.
- Footnote 39
-
Public Health Agency of Canada. CPHO Sunday Edition: Vaccine Safety in Canada: What You Should Know. Government of Canada; 2021.
- Footnote 40
-
Government of Canada. COVID-19 Vaccination in Canada. Government of Canada; 2021.
- Footnote 41
-
Canadian Public Health Association. The Value of Immunization in the Future of Canada’s Health System. Commission on the Future of Health Care in Canada; 2001.
- Footnote 42
-
Public Health Agency of Canada. Update on COVID-19 in Canada: Epidemiology and Modelling - May 28, 2021. Government of Canada; 2021.
- Footnote 43
-
Public Health Agency of Canada. Canada’s COVID-19 Immunization Plan: Saving Lives and Livelihoods. Government of Canada; 2020.
- Footnote 44
-
Public Health Agency of Canada. CPHO Sunday Edition: Canada’s Two New COVID-19 Vaccines: What You Should Know. Government of Canada; 2021.
- Footnote 45
-
National Advisory Committee on Immunization. Guidance on the Prioritization of Initial Doses of COVID-19 Vaccine(s). Government of Canada; 2020.
- Footnote 46
-
National Advisory Committee on Immunization. NACI Rapid Response: Extended Dose Intervals for COVID-19 Vaccines to Optimize Early Vaccine Rollout and Population Protection in Canada. Government of Canada; 2021.
- Footnote 47
-
Immunize Canada. Pan-Canadian Vaccine Injury Support Program. Immunize Canada; 2021.
- Footnote 48
-
Public Health Agency of Canada. Vaccine Injury Support Program (VISP). Public Health Agency of Canada; 2021.
- Footnote 49
-
Murray, T. Canada’s Long Road to a Vaccine Injury Compensation Program. Canadian Medical Association Journal. 2021; 193(8):E294-E5.
- Footnote 50
-
Public Health Agency of Canada. Weekly COVID Surveillance Indicator Report - Week Ending June 15, 2021. Public Health Agency of Canada; 2021.
- Footnote 51
-
Public Health Agency of Canada. Update on COVID-19 in Canada: Epidemiology and Modelling - September 3, 2021. Government of Canada; 2021.
- Footnote 52
-
Public Health Agency of Canada. Weekly COVID Surveillance Indicator Report - Week Ending July 23, 2021. Public Health Agency of Canada; 2021.
- Footnote 53
-
Public Health Agency of Canada. Government of Canada Announces Easing of Border Measures for Fully Vaccinated Travellers. Government of Canada; 2021.
- Footnote 54
-
Public Health Agency of Canada. COVID-19 Daily Epidemiology Update. Government of Canada; 2020.
- Footnote 55
-
Province of Nova Scotia. Border and Other Restrictions to Reduce Spread of COVID-19. Province of Nova Scotia; 2021.
- Footnote 56
-
Province of Nova Scotia. New Brunswick Border Restrictions Reinstated. Province of Nova Scotia; 2021.
- Footnote 57
-
Public Health Agency of Canada. Weekly COVID Surveillance Indicator Report - Week Ending May 14, 2021. Public Health Agency of Canada; 2021.
- Footnote 58
-
Government of Northwest Territories. Government of the Northwest Territories Announces Preliminary COVID-19 Vaccination Approach. Government of Northwest Territories; 2020.
- Footnote 59
-
Government of Yukon. Statement from Minister of Health and Social Services Pauline Frost on the Arrival of Moderna’s COVID-19 Vaccine in Yukon. Government of Yukon; 2020.
- Footnote 60
-
Government of Nunavut. COVID-19 Vaccination. Government of Nunavut; 2021.
- Footnote 61
-
Levin, AT, Hanage, WP, Owusu-Boaitey, N, Cochran, KB, Walsh, SP, Meyerowitz-Katz, G. Assessing the Age Specificity of Infection Fatality Rates for COVID-19: Systematic Review, Meta-Analysis, and Public Policy Implications. European Journal of Epidemiology. 2020; 35(12):1123-38.
- Footnote 62
-
Booth, A, Reed, AB, Ponzo, S, Yassaee, A, Aral, M, Plans, D, et al. Population Risk Factors for Severe Disease and Mortality in COVID-19: A Global Systematic Review and Meta-Analysis. PLOS ONE. 2021; 16(3):e0247461.
- Footnote 63
-
Statistics Canada. Provisional Death Counts and Excess Mortality, January 2020 to February 2021. The Daily; 2021.
- Footnote 64
-
Public Health Agency of Canada. Canadian Surveillance of Covid-19 in Pregnancy: Epidemiology, Maternal and Infant Outcomes - Report #4. Public Health Agency of Canada; 2021.
- Footnote 65
-
Statistics Canada. Impacts of COVID-19 on Health Care Workers: Infection Prevention and Control, Public Use Microdata File. Statistics Canada; 2021.
- Footnote 66
-
Peckham, H, de Gruijter, NM, Raine, C, Radziszewska, A, Ciurtin, C, Wedderburn, LR, et al. Male Sex Identified by Global COVID-19 Meta-Analysis as a Risk Factor for Death and ITU Admission. Nature Communications. 2020; 11(1):6317.
- Footnote 67
-
Okpechi, SC, Fong, JT, Gill, SS, Harman, JC, Nguyen, TH, Chukwurah, QC, et al. Global Sex Disparity of COVID-19: A Descriptive Review of Sex Hormones and Consideration for the Potential Therapeutic Use of Hormone Replacement Therapy in Older Adults. Aging and Disease. 2021; 12(2):671-83.
- Footnote 68
-
Shastri, MD, Shukla, SD, Chong, WC, Kc, R, Dua, K, Patel, RP, et al. Smoking and COVID-19: What We Know So Far. Respiratory Medicine. 2021; 176.
- Footnote 69
-
Public Health Agency of Canada. Social Inequalities in COVID-19 Mortality by Area- and Individual-Level Characteristics in Canada, January to July/August 2020. Ottawa, ON: Public Health Agency of Canada; 2021.
- Footnote 70
-
Canadian Institute for Health Information. COVID-19 Cases and Deaths in Health Care Workers in Canada. Canadian Institute for Health Information; 2021.
- Footnote 71
-
Office of the Correctional Investigator. Third COVID-19 Status Update. Office of the Correctional Investigator; 2021.
- Footnote 72
-
Correctional Services Canada. Vaccines Administered to Inmates in the Federal Correctional System. Government of Canada; 2021.
- Footnote 73
-
Henry, B. COVID-19 Press Conference on February 5, 2021. Press Conference; 2021.
- Footnote 74
-
The Conversation Piece. E27: Dr Deena Hinshaw on the Network of Humanity in the Face of a Virus: The Walrus; 2020.
- Footnote 75
-
Henry, B. COVID-19 Press Conference on April 8, 2021. Press Conference; 2021.
- Footnote 76
-
Canadian Red Cross. How Red Cross Is Responding to COVID-19 in Nunavut. Canadian Red Cross; 2021.
- Footnote 77
-
City of Toronto. Two COVID-19 Cases in Toronto Appear Linked to the B.1.1.7 Variant. City of Toronto; 2021.
- Footnote 78
-
Alberta Health Services. Meat Processing Plant COVID-19 Outbreaks. Alberta Health Services; 2021.
- Footnote 79
-
Ontario Ministry of Health. COVID-19: Guidance for Prioritization of Phase 2 Populations for COVID-19 Vaccination. Government of Ontario; 2021.
- Footnote 80
-
Hinshaw, D. COVID-19 Press Conference on March 15, 2021. Press Conference; 2021.
- Footnote 81
-
Ontario Health Coalition. Tracking of COVID-19 Outbreaks in Non-Health Care Settings – Data Updated to October 13. Ontario Health Coalition; 2020.
- Footnote 82
-
City of Toronto. Toronto Public Health Releases COVID-19 Workplace Outbreak Data. City of Toronto; 2021.
- Footnote 83
-
Ottawa Public Health. Outbreaks in Workplaces. Ottawa Public Health; 2021.
- Footnote 84
-
Public Health Agency of Canada. COVID-19 Mortality Data Tool. Pan-Canadian Health Inequalities Reporting Initiative; 2021.
- Footnote 85
-
Subedi, R, Greenberg, L, Trucotte, M. COVID-19 Mortality Rates in Canada's Ethno-Cultural Neighbourhoods. Statistics Canada; 2020.
- Footnote 86
-
Statistics Canada. Impacts on Immigrants and People Designated as Visible Minorities. Government of Canada; 2020.
- Footnote 87
-
COVID-19 Immunity Task Force. Poorer Neighbourhoods and Racialized Communities Continue to Lag Behind in Vaccine Coverage: Latest Canadian Blood Services Results. COVID-19 Immunity Task Force; 2021.
- Footnote 88
-
City of Toronto. COVID 19: Ethno-Racial Identity and Income. City of Toronto; 2021.
- Footnote 89
-
National Advisory Committee on Immunization. Guidance on the Prioritization of Key Populations for COVID-19 Immunization. Government of Canada; 2021.
- Footnote 90
-
Government of Ontario. Ontario Expands COVID-19 Vaccination Booking for More People. Government of Ontario; 2021.
- Footnote 91
-
Iveniuk, J, Leon, S. An Uneven Recovery: Measuring COVID-19 Vaccine Equity in Ontario. Wellesley Institute; 2021.
- Footnote 92
-
Angus, M. “Champions for Immunization against COVID-19” African Nova Scotian Communities and Partners Work Together to Create Positive Vaccine Experience. Nova Scotia Health; 2021.
- Footnote 93
-
Plante, V. City of Montreal COVID-19 Press Conference on January 13. Press Conference; 2021.
- Footnote 94
-
CBC News. Vancouver Health Authority Rolls out COVID-19 Vaccine on Downtown Eastside. CBC News. 2021.
- Footnote 95
-
Indigenous Services Canada. COVID-19 Epidemiology Internal Data. Indigenous Services Canada; 2021.
- Footnote 96
-
First Nations Health Authority. Community Situation Report August 14, 2021. First Nations Health Authority; 2021.
- Footnote 97
-
Statistics Canada. Focus on Geography Series, 2016 Census - Nunavut. Ottawa, ON: Statistics Canada; 2017.
- Footnote 98
-
Government of Nunavut. Travel and Isolation. Government of Nunavut; 2021.
- Footnote 99
-
Government of Nunavut. Public Health Restrictions Eased in Iqaluit, Wastewater Testing Introduced. Government of Nunavut; 2021.
- Footnote 100
-
Government of Nunavut. COVID-19 Positive Wastewater in Rankin Inlet. Government of Nunavut; 2021.
- Footnote 101
-
Assembly of Manitoba Chiefs, Southern Chiefs’ Organization Inc., Manitoba Keewatinowi Okimakanak Inc., Keewatinohk Inniniw Minoayawin Inc., First Nations Health, Social Secretariat of Manitoba. Protect Yourself. Protect Our People. 2021; Available from: https://protectourpeoplemb.ca/.
- Footnote 102
-
Indigenous Services Canada. COVID-19 Vaccines and Indigenous Peoples. Government of Canada; 2021.
- Footnote 103
-
Anishnabek News. Connecting Indigenous Communities with Culturally-Relevant COVID-19 Vaccine Information. Anishnabek News. 2021.
- Footnote 104
-
Northern Policy Institute. Taking to the Skies: Vaccination Delivery in the Far North. Northern Policy Institute; 2021; Available from: https://www.northernpolicy.ca/article/taking-to-the-skies-vaccination-delivery-in-the-far-north--41534.asp.
- Footnote 105
-
National Collaborating Centre for Methods and Tools. Rapid Review: What Is Known About Reasons for Vaccine Confidence and Uptake in Populations Experiencing Inequities? National Collaborating Centre for Methods and Tools; 2021.
- Footnote 106
-
MacDonald, N, Comeau, J, Dubé, È, Graham, J, Greenwood, M, Harmon, S, et al. Enhancing COVID-19 Vaccine Acceptance in Canada. Royal Society of Canada; 2021.
- Footnote 107
-
Public Health Agency of Canada. Statement from the Chief Public Health Officer of Canada on May 22, 2021. Government of Canada; 2021.
- Footnote 108
-
Indigenous Services Canada. Government of Canada COVID-19 Update for Indigenous Peoples and Communities, Week of August 9. Government of Canada; 2021.
- Footnote 109
-
Public Health Agency of Canada. Weekly COVID Surveillance Indicator Report - Week Ending August 13, 2021. Public Health Agency of Canada; 2021.
- Footnote 110
-
Gouvernement du Québec. COVID-19 Vaccination Passport. Gouvernement du Québec; 2021.
- Footnote 111
-
Alberta Health Services. Alberta Health Services Implementing Immunization Policy for Physicians, Staff and Contracted Providers. Alberta Health Services; 2021.
- Footnote 112
-
Statistics Canada. COVID-19 Vaccine Willingness among Canadian Population Groups. Government of Canada; 2021.
- Footnote 113
-
Statistics Canada. Most Canadians Willing to Get Vaccinated, and More Stayed Home at the Beginning of 2021. The Daily; 2021.
- Footnote 114
-
Statistics Canada. COVID-19 Vaccination Coverage Survey. The Daily; 2021.
- Footnote 115
-
Office of the Chief Public Health Officer, Privy Council Office/Impact & Innovation Unit. Augmenting Vaccination Data among Priority Populations. Government of Canada; 2021.
- Footnote 116
-
Dionne, M, Dubé, E, Hamel, D, Rochette, L, Tessier, M. Pandémie et Vaccination Contre la COVID-19 - 24 Août 2021. Institut national de santé publique du Québec; 2021.
- Footnote 117
-
Public Health Agency of Canada. Vaccine Community Innovation Challenge: Objectives and Principles. Government of Canada; 2021.
- Footnote 118
-
Public Health Agency of Canada. COVID-19 Internal Transition Briefing. Public Health Agency of Canada; 2021.
- Footnote 119
-
Ritchie, H, Mathieu, E, Rodés-Guirao, L, Appel, C, Giattino, C, Ortiz-Ospina, E, et al. Coronavirus Pandemic (COVID-19). Our World in Data; 2020.
- Footnote 120
-
Callaway, E. COVID Vaccine Boosters: The Most Important Questions. Nature. 2021; 596:178-80.
- Footnote 121
-
Mathieu, E, Ritchie, H, Ortiz-Ospina, E, Roser, M, Hasell, J, Appel, C, et al. A Global Database of COVID-19 Vaccinations. Nature Human Behaviour. 2021.
- Footnote 122
-
Global Affairs Canada. Canada Announces New Contribution to Global Vaccination Efforts. Government of Canada; 2021.
- Footnote 123
-
Statistics Canada. Reductions in Life Expectancy Directly Associated with COVID-19, 2020. The Daily; 2021.
- Footnote 124
-
Statistics Canada. Table 13-10-0114-01 Life Expectancy and Other Elements of the Life Table, Canada, All Provinces except Prince Edward Island. Government of Canada; 2021.
- Footnote 125
-
Statistics Canada. Life Tables, 2016/2018. The Daily; 2020.
- Footnote 126
-
Dion, P. Reductions in Life Expectancy Directly Associated with COVID-19 in 2020. Government of Canada; 2021.
- Footnote 127
-
Statistics Canada. Provisional Death Counts and Excess Mortality, January 2020 to May 2021. The Daily; 2021.
- Footnote 128
-
Special Advisory Committee on the Epidemic of Opioid Overdoses. Opioid- and Stimulant-Related Harms in Canada. Ottawa, ON: Public Health Agency of Canada; 2021.
- Footnote 129
-
Canadian Institute for Health Information. Impact of COVID-19 on Canada’s Health Care Systems. Canadian Institute for Health Information; 2021.
- Footnote 130
-
Canadian Institute for Health Information. How COVID-19 Affected Emergency Departments. Canadian Institute for Health Information; 2020.
- Footnote 131
-
Public Health Agency of Canada. Survey of the Impact of COVID-19 on the Ability to Provide STBBI Prevention, Testing and Treatment Including Harm Reduction Services in Canada. Government of Canada; 2021.
- Footnote 132
-
Devakos, T, Gordon, M, Gurnham, M, Kim, J, Stephenson, M. Ministry of Health Spending Plan Review. Toronto, ON: Financial Accountability Office of Ontario; 2021.
- Footnote 133
-
Yong, JH, Mainprize, JG, Yaffe, MJ, Ruan, Y, Poirier, AE, Coldman, A, et al. The Impact of Episodic Screening Interruption: COVID-19 and Population-Based Cancer Screening in Canada. Journal of Medical Screening. 2020; 28(2):100-7.
- Footnote 134
-
Pelland-Marcotte, MC, Xie, L, Barber, R, Elkhalifa, S, Frechette, M, Kaur, J, et al. Incidence of Childhood Cancer in Canada during the COVID-19 Pandemic. Canadian Medical Association Journal. 2021.
- Footnote 135
-
Domingo, FR, Waddell, LA, Cheung, AM, Cooper, CL, Belcourt, VJ, Zuckermann, AME, et al. Prevalence of Long-Term Effects in Individuals Diagnosed with COVID-19: A Living Systematic Review. medRxiv. 2021.
- Footnote 136
-
Survivor Corps. Post COVID Care Centers. Survivor Corps; 2021; Available from: https://www.survivorcorps.com/pccc-canada.
- Footnote 137
-
Government of Canada. Post COVID-19 Condition. Government of Canada; 2021.
- Footnote 138
-
CANCOV. The Canadian COVID-19 Prospective Cohort Study (CANCOV). CANCOV; 2020; Available from: https://cancov.net/.
- Footnote 139
-
Canadian Institute for Health Information. Health Workforce in Canada: Highlights of the Impact of COVID-19. Canadian Institute for Health Information; 2021.
- Footnote 140
-
Bhatia, RS, Chu, C, Pang, A, Tadrous, M, Stamenova, V, Cram, P. Virtual Care Use before and during the COVID-19 Pandemic: A Repeated Cross-Sectional Study. Canadian Medical Association Open Access Journal. 2021; 9(1):E107-E14.
- Footnote 141
-
Audy, E, Gamache, L, Gauthier, A, Lemétayer, F, Lessard, S, Melançon, A. Inégalités D’accès et D’usage des Technologies Numériques : Un Déterminant Préoccupant pour la Santé de la Population? Institut national de santé publique du Québec; 2021.
- Footnote 142
-
Task Team on Equitable Access to Virtual Care. Enhancing Equitable Access to Virtual Care in Canada: Principle-Based Recommendations for Equity. Ottawa, ON: Health Canada; 2021.
- Footnote 143
-
Public Health Agency of Canada. Fluwatch Report: July 21, 2019 to August 24, 2019 (Weeks 30 to 34). Government of Canada; 2019.
- Footnote 144
-
Public Health Agency of Canada. Fluwatch Report: July 25 to August 28, 2021 (Weeks 30 to 34). Government of Canada; 2021.
- Footnote 145
-
Alberta Health. Alberta Sexually Transmitted Infections and HIV. Edmonton, AB: Government of Alberta; 2020.
- Footnote 146
-
Ontario Agency for Health Protection and Promotion (Public Health Ontario). Monthly Infectious Diseases Surveillance Report: Diseases of Public Health Significance Cases for January to December 2020. Toronto, ON: Queen's Printer for Ontario; 2021.
- Footnote 147
-
Tam, T. Addressing Stigma: Towards a More Inclusive Health System. Ottawa, ON: Public Health Agency of Canada; 2019.
- Footnote 148
-
Shurgold, J, Avery, B, Rank, C, Volling, C, Béïque, L, Gravel-Tropper, D, et al. Canadian Antimicrobial Resistance Surveillance System Report. Public Health Agency of Canada; 2021.
- Footnote 149
-
Statistics Canada. Table 13-10-0806-01 Canadians Health and COVID-19, by Age and Gender. Government of Canada; 2021.
- Footnote 150
-
Statistics Canada. COVID-19 in Canada: A One-Year Update on Social and Economic Impacts. Government of Canada; 2021.
- Footnote 151
-
Public Health Agency of Canada. Symptoms of Posttraumatic Stress Disorder (PTSD) during the COVID-19 Pandemic. Public Health Agency of Canada; 2021.
- Footnote 152
-
Public Health Agency of Canada. Symptoms of Anxiety and Depression during the COVID-19 Pandemic. Public Health Agency of Canada; 2021.
- Footnote 153
-
Cost, KT, Crosbie, J, Anagnostou, E, Birken, CS, Charach, A, Monga, S, et al. Mostly Worse, Occasionally Better: Impact of COVID-19 Pandemic on the Mental Health of Canadian Children and Adolescents. European Child & Adolescent Psychiatry. 2021:1-14.
- Footnote 154
-
Yousif, N. 4 Million Cries for Help: Calls to Kids Help Phone Soar Amid Pandemic. Toronto Star. 2020.
- Footnote 155
-
Office of the Prime Minister of Canada. Prime Minister Announces Support for Vulnerable Canadians Affected by COVID‑19. Government of Canada; 2020.
- Footnote 156
-
Gadermann, AC, Thomson, KC, Richardson, CG, Gagné, M, McAuliffe, C, Hirani, S, et al. Examining the Impacts of the COVID-19 Pandemic on Family Mental Health in Canada: Findings from a National Cross-Sectional Study. British Medical Journal Open. 2021; 11(1).
- Footnote 157
-
Sun, Y, Wu, Y, Bonardi, O, Krishnan, A, He, C, Boruff, JT, et al. Comparison of Mental Health Symptoms Prior to and during COVID-19: Evidence from a Living Systematic Review and Meta-Analysis. medRxiv. 2021.
- Footnote 158
-
Liu, L, Capaldi, CA, Dopko, RL. Original Quantitative Research – Suicide Ideation in Canada during the COVID-19 Pandemic. Health Promotion and Chronic Disease Prevention in Canada. 2021.
- Footnote 159
-
Mise à Jour Annuelle des Suicides au Québec. Association québécoise de prévention du suicide; 2021; Available from: https://www.aqps.info/semaine/communique-presse-mise-jour-annuelle-des-675.html.
- Footnote 160
-
Pirkis, J, John, A, Shin, S, DelPozo-Banos, M, Arya, V, Analuisa-Aguilar, P, et al. Suicide Trends in the Early Months of the COVID-19 Pandemic: An Interrupted Time-Series Analysis of Preliminary Data from 21 Countries. The Lancet Psychiatry. 2021; 8(7):579-88.
- Footnote 161
-
Botchway, S, Fazel, S. Remaining Vigilant About COVID-19 and Suicide. The Lancet Psychiatry. 2021; 8(7):552-3.
- Footnote 162
-
Belzak, L, Halverson, J. The Opioid Crisis in Canada: A National Perspective. Health Promotion and Chronic Disease Prevention in Canada. 2018; 38(6):224-33.
- Footnote 163
-
Morin, KA, Eibl, JK, Franklyn, AM, Marsh, DC. The Opioid Crisis: Past, Present and Future Policy Climate in Ontario, Canada. Substance Abuse Treatment, Prevention, and Policy. 2017; 12(1).
- Footnote 164
-
British Columbia Coroners Service. Illicit Drug Toxicity Deaths in Bc January 1, 2011 – June 30, 2021. Government of British Columbia; 2021.
- Footnote 165
-
Government of Canada. Modelling Opioid-Related Deaths during the COVID-19 Outbreak. Government of Canada; 2021.
- Footnote 166
-
Adelson, N. The Embodiment of Inequity: Health Disparities in Aboriginal Canada. Canadian Journal of Public Health. 2005; 96(2):S45-S61.
- Footnote 167
-
First Nations Health Authority. First Nations Toxic Drug Deaths Doubled During the Pandemic in 2020. First Nations Health Authority; 2021.
- Footnote 168
-
Government of Alberta. Alberta Opioid Response Surveillance Report: First Nations People in Alberta. Government of Alberta; 2021.
- Footnote 169
-
Canadian Institute for Health Information. Unintended Consequences of COVID-19: Impact on Harms Caused by Substance Use. Ottawa, ON: Canadian Institute for Health Information; 2021.
- Footnote 170
-
Health Canada. Subsection 56(1) Class Exemption for Patients, Practitioners and Pharmacists Prescribing and Providing Controlled Substances in Canada during the Coronavirus Pandemic. Government of Canada; 2020.
- Footnote 171
-
Henry, B. Order of the Provincial Health Officer: Registered Nurse and Registered Psychiatric Nurse Public Health Pharmacotherapy. Government of British Columbia; 2021.
- Footnote 172
-
Health Canada. Government of Canada Supports Expansion of Innovative Safer Supply Project to Operate in Four Cities across Canada. Government of Canada; 2021.
- Footnote 173
-
Varin, M, Hill MacEachern, K, Hussain, N, Baker, MM. At a Glance – Measuring Self-Reported Change in Alcohol and Cannabis Consumption during Wave 2 of the COVID-19 Pandemic in Canada. Health Promotion and Chronic Disease Prevention in Canada. 2021.
- Footnote 174
-
Statistics Canada. Alcohol and Cannabis Use during the Pandemic: Canadian Perspectives Survey Series 6. The Daily; 2021.
- Footnote 175
-
Statistics Canada. Labour Force Survey, December 2020. The Daily; 2021.
- Footnote 176
-
Statistics Canada. Labour Force Survey, April 2021. The Daily; 2021.
- Footnote 177
-
Statistics Canada. Labour Force Survey, July 2021. The Daily; 2021.
- Footnote 178
-
Statistics Canada. Labour Force Survey, June 2021. The Daily; 2021.
- Footnote 179
-
Statistics Canada. Labour Force Survey, February 2021. The Daily; 2021.
- Footnote 180
-
Statistics Canada. Table 14-10-0342-01 Duration of Unemployment, Monthly, Seasonally Adjusted. Government of Canada; 2021.
- Footnote 181
-
Muntaner, C, Solar, O, Vanroelen, C, Martínez, JM, Vergara, M, Santana, V, et al. Unemployment, Informal Work, Precarious Employment, Child Labor, Slavery, and Health Inequalities: Pathways and Mechanisms. International Journal of Health Services. 2010; 40(2):281-95.
- Footnote 182
-
Benach, J, Vives, A, Amable, M, Vanroelen, C, Tarafa, G, Muntaner, C. Precarious Employment: Understanding an Emerging Social Determinant of Health. Annual Review of Public Health. 2014; 35(1):229-53.
- Footnote 183
-
Tran, M, Sokas, RK. The Gig Economy and Contingent Work: An Occupational Health Assessment. Journal of Occupational and Environmental Medicine. 2017; 59(4):e63-e6.
- Footnote 184
-
Statistics Canada. Household Economic Well-Being during the COVID-19 Pandemic, Experimental Estimates, Fourth Quarter 2020. The Daily; 2021.
- Footnote 185
-
Segal, H, Forget, E, Banting, K. A Federal Basic Income within the Post COVID-19 Economic Recovery Plan. Royal Society of Canada; 2020.
- Footnote 186
-
Men, F, Tarasuk, V. Food Insecurity Amid the COVID-19 Pandemic: Food Charity, Government Assistance, and Employment. Canadian Public Policy. 2021.
- Footnote 187
-
Polsky, JY, Gilmour, H. Food Insecurity and Mental Health during the COVID-19 Pandemic. Health Reports. 2020.
- Footnote 188
-
Statistics Canada. Food Insecurity during the COVID-19 Pandemic, May 2020. Government of Canada; 2020.
- Footnote 189
-
Gionet, L, Roshanafshar, S. Select Health Indicators of First Nations People Living Off Reserve, Métis and Inuit. Statistics Canada; 2015.
- Footnote 190
-
Statistics Canada. Canadian Perspectives Survey Series 1: Impacts of COVID-19. The Daily; 2020.
- Footnote 191
-
Shields, M, Tonmyr, L, Gonzalez, A, Weeks, M, Park, S, Robert, A, et al. Original Quantitative Research – Symptoms of Major Depressive Disorder during the COVID-19 Pandemic: Results from a Representative Sample of the Canadian Population. Health Promotion and Chronic Disease Prevention in Canada. 2021.
- Footnote 192
-
Prokopenko, E, Kevins, C. Vulnerabilities Related to COVID-19 among LGBTQ2+ Canadians. Statistics Canada; 2020.
- Footnote 193
-
Thompson, N. Reports of Domestic, Intimate Partner Violence Continue to Rise during Pandemic. CBC News. 2021.
- Footnote 194
-
Statistics Canada. Experiences of Discrimination during the COVID-19 Pandemic. The Daily; 2020.
- Footnote 195
-
Manojlovic, D. Year-End 2020 Year-to-Date Key Performance Indicators Report. Vancouver Police Board; 2021.
- Footnote 196
-
City of Ottawa. Incidents of Anti-Asian Racism on the Rise in Ottawa. Ottawa, ON: City of Ottawa; 2021.
- Footnote 197
-
Statistics Canada. School Closures and COVID-19: Interactive Tool. Government of Canada; 2021.
- Footnote 198
-
Gallagher-Mackay, K, Srivastava, P, Underwood, K, Dhuey, E, McCready, L, Born, KB, et al. COVID-19 and Education Disruption in Ontario: Emerging Evidence on Impacts. Ontario COVID-19 Science Advisory Table; 2021. Available from: https://doi.org/10.47326/ocsat.2021.02.34.1.0.
- Footnote 199
-
Melançon, A. COVID-19 : Impacts de la Pandémie sur le Développement des Enfants de 2 à 12 Ans. Institut national de santé publique du Québec; 2021.
- Footnote 200
-
Representative for Children and Youth. Left Out: Children and Youth with Special Needs in the Pandemic. Representative for Children and Youth; 2020.
- Footnote 201
-
Zwaigenbaum, L, Brian, JA, Ip, A. Early Detection for Autism Spectrum Disorder in Young Children. Paediatrics & Child Health. 2019; 24(7):424-32.
- Footnote 202
-
Shaw, M, Hodgkins, P, Caci, H, Young, S, Kahle, J, Woods, AG, et al. A Systematic Review and Analysis of Long-Term Outcomes in Attention Deficit Hyperactivity Disorder: Effects of Treatment and Non-Treatment. BioMed Central Medicine. 2012; 10.
- Footnote 203
-
Chudley, AE, Conry, J, Cook, JL, Loock, C, Rosales, T, LeBlanc, N, et al. Fetal Alcohol Spectrum Disorder: Canadian Guidelines for Diagnosis. Canadian Medical Association Journal. 2005; 172(5 Suppl):S1-S21.
- Footnote 204
-
Charnock, S, Heisz, A, Kaddatz, J, Spinks, N, Mann, R. Canadians' Well-Being in Year One of the COVID-19 Pandemic. Statistics Canada; 2021.
- Footnote 205
-
Department of Finance Canada. Budget 2021 - a Recovery Plan for Jobs, Growth, and Resilience. Government of Canada; 2021.
- Footnote 206
-
Auditor General of Canada. Report 8—Pandemic Preparedness, Surveillance, and Border Control Measures. Office of the Auditor General of Canada; 2021.
- Footnote 207
-
Pan-Canadian Health Data Strategy. Expert Advisory Group Report 1: Charting a Path toward Ambition. Public Health Agency of Canada; 2021.
- Footnote 208
-
McKenzie, K. Race and Ethnicity Data Collection during COVID-19 in Canada: If You Are Not Counted You Cannot Count on the Pandemic Response. Ottawa, ON: Royal Society of Canada; 2020.
- Footnote 209
-
City of Toronto. Toronto Public Health Releases New Socio-Demographic COVID-19 Data. City of Toronto; 2020.
- Footnote 210
-
McKenzie, K. Socio-Demographic Data Collection and Equity in Covid-19 in Toronto. EClinicalMedicine. 2021; 34.
- Footnote 211
-
City of Toronto. Black Scientists’ Task Force on Vaccine Equity to Deliver Final Report and Recommendations to the Board of Health Today. City of Toronto; 2021.
- Footnote 212
-
Public Health Agency of Canada. The Pan-Canadian Health Data Strategy: Expert Advisory Group Overview. Government of Canada; 2021.
- Footnote 213
-
Henry, B. Canadian Pandemic Influenza Preparedness: Communications Strategy. Canada Communicable Disease Report. 2018; 44(5):106-9.
- Footnote 214
-
Public Health Agency of Canada. CPHO Sunday Edition: Equipping Ourselves against Mis- and Disinformation during COVID-19. Government of Canada; 2021.
- Footnote 215
-
World Health Organization, United Nations, United Nations Children’s Emergency Fund (UNICEF), United Nations Development Programme, United Nations Educational, SaCOU, Joint United Nations Programme on HIV/AIDS, et al. Managing the COVID-19 Infodemic: Promoting Healthy Behaviours and Mitigating the Harm from Misinformation and Disinformation. World Health Organization; 2020.
- Footnote 216
-
Zarocostas, J. How to Fight an Infodemic. The Lancet. 2020; 395(10225):676.
- Footnote 217
-
Dubé, E, Gagnon, D, Vivion, M. Optimizing Communication Material to Address Vaccine Hesitancy. Canada Communicable Disease Report. 2020; 46(2/3):48-52.
- Footnote 218
-
Office of Audit and Evaluation (Health Canada, Public Health Agency of Canada). Lessons Learned from the Public Health Agency of Canada's COVID-19 Response (Phase One). Government of Canada; 2020.
- Footnote 219
-
MacDonald, NE. COVID-19, Public Health and Constructive Journalism in Canada. Canadian Journal of Public Health. 2021; 112(2):179-82.
- Footnote 220
-
Public Health Agency of Canada. Government of Canada Funds Two New Projects to Encourage Vaccine Uptake in Canada. Government of Canada; 2021.
- Footnote 221
-
Together against Misinformation. ScienceUpFirst; 2021; Available from: https://www.scienceupfirst.com/.
- Footnote 222
-
Maad’ookiing Mshkiki — Sharing Medicine: Connecting Indigenous Communities with Culturally Relevant COVID-19 Vaccine Information. University Health Network; 2021; Available from: https://www.uhn.ca/corporate/News/Pages/Sharing_Medicine_connecting_Indigenous_communities_with_culturally_relevant_COVID19_vaccine_information.aspx.
- Footnote 223
-
Greenberg, J, Gauthier, B. Canada Needs a Fresh Strategy for Pandemic Communications. Policy Options. 2021.
- Footnote 224
-
About the Pan-Canadian Public Health Network. Pan-Canadian Public Health Network; 2020; Available from: http://www.phn-rsp.ca/network-eng.php.
- Footnote 225
-
Public Health Agency of Canada. Statement from the Council of Chief Medical Officers of Health: Working with Canadians on the Ongoing Management of COVID-19 in the Months Ahead. Government of Canada; 2020.
- Footnote 226
-
Public Health Agency of Canada. Statement from the Council of Chief Medical Officers of Health Implementing COVID-19 Vaccination in Canada. Government of Canada; 2021.
- Footnote 227
-
COVID-END. COVID-END; 2021; Available from: https://www.mcmasterforum.org/networks/covid-end.
- Footnote 228
-
CanCOVID. About CanCOVID. CanCOVID; 2021; Available from: https://cancovid.ca/about/.
- Footnote 229
-
CoVaRR-Net. CoVaRR-Net; 2021; Available from: https://covarrnet.ca/.
- Footnote 230
-
Gilmore, B, Ndejjo, R, Tchetchia, A, de Claro, V, Mago, E, Diallo, AA, et al. Community Engagement for COVID-19 Prevention and Control: A Rapid Evidence Synthesis. British Medical Journal Global Health. 2020; 5(10).
- Footnote 231
-
Special Advisory Committee on COVID-19. Pan-Canadian Public Health Network; 2021; Available from: http://www.phn-rsp.ca/sac-covid-ccs/index-eng.php.
- Footnote 232
-
Public Services and Procurement Canada. Supplying the Canadian Response to COVID-19: Standing Committee on Government Operations and Estimates—July 23, 2020. Government of Canada; 2020.
- Footnote 233
-
Public Health Agency of Canada. Government of Canada Announces Funding for COVID-19 Safe Voluntary Isolation Sites in Nova Scotia. Government of Canada; 2021.
- Footnote 234
-
Indigenous Services Canada. Government of Canada COVID-19 Update for Indigenous Peoples and Communities, Week of June 14. Government of Canada; 2021.
- Footnote 235
-
Vaccinated Métis Strong. Saskatoon, SK: Métis Nation Saskatchewan; 2021; Available from: https://metisnationsk.com/vaccine/.
- Footnote 236
-
Connecting Culture Services & Community. Winnipeg, MB: Manitoba Inuit Association; 2021; Available from: https://www.manitobainuit.ca/.
- Footnote 237
-
Government of Canada. Point-of-Care Testing Brings Rapid COVID-19 Testing to Underserved Communities. Government of Canada; 2021.
- Footnote 238
-
Auditor General of Canada. Report 11—Health Resources for Indigenous Communities—Indigenous Services Canada. Office of the Auditor General of Canada; 2021.
- Footnote 239
-
Global Public Health Intelligence Network (GPHIN) Review Panel. Global Public Health Intelligence Network (GPHIN) Independent Review Panel Final Report. Public Health Agency of Canada; 2021.
- Footnote 240
-
Government of Canada. Canada Emergency Response Benefit and EI Statistics. Government of Canada; 2021.
- Footnote 241
-
Office of the Prime Minister of Canada. 4,500 More Homes for Canadians. Government of Canada; 2021.
- Footnote 242
-
Public Health Agency of Canada. Canadian Pandemic Influenza Preparedness: Planning Guidance for the Health Sector. Government of Canada; 2018.
- Footnote 243
-
Office of the Auditor General of Ontario. COVID-19 Preparedness and Management: Special Report on Laboratory Testing, Case Management and Contact Tracing. Toronto, ON: Office of the Auditor General of Ontario; 2020.
- Footnote 244
-
Auditor General of Canada. Report 10—Securing Personal Protective Equipment and Medical Devices. Office of the Auditor General of Canada; 2021.
- Footnote 245
-
Canadian Red Cross. Operations Report on September 7. Canadian Red Cross; 2021.
- Footnote 246
-
Canadian Red Cross. How Red Cross Is Helping in Canada. Canadian Red Cross; 2021.
- Footnote 247
-
Canadian Red Cross. COVID-19 Response Timeline. Canadian Red Cross; 2020.
- Footnote 248
-
National Defence. Operation LASER. Government of Canada; 2021.
- Footnote 249
-
National Defence. Operation VECTOR. Government of Canada; 2021.
- Footnote 250
-
Hager, M, Lee, C. B.C. Vows to Improve Ambulance System after Heat Wave Overwhelms Emergency Services. The Globe and Mail. 2021.
- Footnote 251
-
Roffel, B. B.C.'s Heat Wave Likely Contributed to 719 Sudden Deaths in a Week, Coroner Says — Triple the Usual Number. CBC News. 2021.
- Footnote 252
-
Canadian Public Health Association. Public Health in the Context of Health System Renewal in Canada: Position Statement. Canadian Public Health Association; 2019.
- Footnote 253
-
Naylor, D, Basrur, S, Bergeron, MG, Brunham, RC, Butler-Jones, D, Dafoe, G, et al. Learning from SARS: Renewal of Public Health in Canada. Ottawa, ON: National Advisory Committee on SARS and Public Health; 2003.
- Footnote 254
-
Eggleton, A, Ogilvie, KK, Standing Senate Committee on Social Affairs Science and Technology. Canada’s Response to the 2009 H1N1 Influenza Pandemic. Ottawa, ON: Senate, Government of Canada; 2010.
- Footnote 255
-
Public Health Agency of Canada. Lessons Learned Review: Public Health Agency of Canada and Health Canada Response to the 2009 H1N1 Pandemic. Ottawa, ON: Public Health Agency of Canada; 2010.
- Footnote 256
-
Frank, J, Di Ruggiero, E, Moloughney, B. The Future of Public Health in Canada: Developing a Public Health System for the 21st Century. Ottawa, ON: Canadian Institutes for Health Research; 2003.
- Footnote 257
-
McMahon, M, Nadigel, J, Thompson, E, Glazier, RH. Informing Canada's Health System Response to COVID-19: Priorities for Health Services and Policy Research. Healthcare Policy. 2020; 16(1):112-24.
- Footnote 258
-
Canadian Institutes of Health Research. Building Public Health Systems for the Future: CIHR Institute of Population and Public Health Dialogue Background Paper. Canadian Institutes of Health Research; 2021.
- Footnote 259
-
Jones, E, MacDougall, H, Monnais, L, Hanley, J, Carstairs, C. Beyond the COVID-19 Crisis: Building on Lost Opportunities in the History of Public Health. Royal Society of Canada; 2021.
- Footnote 260
-
Canadian Public Health Association. History of Public Health. Canadian Public Health Association; 2010.
- Footnote 261
-
Health Canada, Public Health Agency of Canada, Canadian Food Inspection Agency. Antibiotic (Antimicrobial) Resistance. Government of Canada; 2018.
- Footnote 262
-
Canadian Public Health Association. Position Statement: Climate Change and Human Health. Ottawa, ON: Canadian Public Health Association; 2019.
- Footnote 263
-
Government of Canada. Responding to Canada’s Opioid Crisis. Government of Canada; 2021.
- Footnote 264
-
Rutter, H, Savona, N, Glonti, K, Bibby, J, Cummins, S, Finegood, DT, et al. The Need for a Complex Systems Model of Evidence for Public Health. The Lancet. 2017; 390(10112):2602-4.
- Footnote 265
-
Zukowski, N, Davidson, S, Yates, MJ. Systems Approaches to Population Health in Canada: How Have They Been Applied, and What Are the Insights and Future Implications for Practice? Canadian Journal of Public Health. 2019; 110(6):741-51.
- Footnote 266
-
Riley, BL, Robinson, KL, Gamble, J, Finegood, DT, Sheppard, D, Penney, TL, et al. Knowledge to Action for Solving Complex Problems: Insights from a Review of Nine International Cases. Health Promotion and Chronic Disease Prevention in Canada. 2015; 35(3):47-53.
- Footnote 267
-
McGill, E, Er, V, Penney, T, Egan, M, White, M, Meier, P, et al. Evaluation of Public Health Interventions from a Complex Systems Perspective: A Research Methods Review. Social Science & Medicine. 2021; 272:113697.
- Footnote 268
-
Decady, Y, Greenberg, L. Ninety Years of Change in Life Expectancy. Statistics Canada; 2014.
- Footnote 269
-
Canadian Public Health Association. 12 Great Achievements. Canadian Public Health Association.
- Footnote 270
-
Ehreth, J. The Value of Vaccination: A Global Perspective. Vaccine. 2003; 21(27):4105-17.
- Footnote 271
-
Canadian Public Health Association. Immunization Timeline. Canadian Public Health Association.
- Footnote 272
-
Public Health Agency of Canada. Vaccine Preventable Disease: Surveillance Report to December 31, 2017. Ottawa, ON: Public Health Agency of Canada; 2020.
- Footnote 273
-
Government of Canada. Canadian Immunization Guide: Introduction. Government of Canada; 2020.
- Footnote 274
-
Pless, R. Doing Well Still Needs to Sell: Bringing Vaccine-Preventable Diseases under Further Control in Canada Requires a Shift in Thinking. Paediatrics & Child Health. 1999; 4(1):16-8.
- Footnote 275
-
Public Health Agency of Canada. Canadian Measles/Rubella Surveillance System. Public Health Agency of Canada; 2021.
- Footnote 276
-
Public Health Agency of Canada. Canadian Notifiable Disease Surveillance System. Public Health Agency of Canada; 2021.
- Footnote 277
-
Rutty, C, Sullivan, SC. This Is Public Health: A Canadian History. Ottawa, ON: Canadian Public Health Association; 2010.
- Footnote 278
-
Jackson, BE. Situating Epidemiology. In: Texler Segal M, Demos V, Kronenfeld JJ, editors. Gender Perspectives on Health and Medicine: Emerald Group Publishing Limited; 2003. p. 11-58.
- Footnote 279
-
Belshaw, JD. 7.2 - Social Reform. In: Canadian History: Post-Confederation. Victoria, BC: BCcampus; 2016.
- Footnote 280
-
Bryant, T. Health Policy in Canada. Second Edition. Toronto, ON: Canadian Scholars' Press Inc.; 2016.
- Footnote 281
-
Health Canada. Canada's Health Care System. Government of Canada; 2019.
- Footnote 282
-
Public Health Agency of Canada. Canadian Reference Group on Social Determinants of Health. World Health Organization; 2011.
- Footnote 283
-
Lalonde, M. A New Perspective on the Health of Canadians: A Working Document. Ottawa, ON: Minister of Supply and Services Canada; 1974.
- Footnote 284
-
Potvin, L, Jones, CM. Twenty-Five Years after the Ottawa Charter: The Critical Role of Health Promotion for Public Health. Canadian Journal of Public Health. 2011; 102(4):244-8.
- Footnote 285
-
Allan, B, Smylie, J. First Peoples, Second Class Treatment: The Role of Racism in the Health and Well-Being of Indigenous Peoples in Canada. Toronto, ON: Wellesley Institute; 2015.
- Footnote 286
-
National Inquiry into Missing and Murdered Indigenous Women and Girls. Reclaiming Power and Place: The Final Report of the National Inquiry into Missing and Murdered Indigenous Women and Girls. National Inquiry into Missing and Murdered Indigenous Women and Girls; 2019.
- Footnote 287
-
Truth and Reconciliation Commission of Canada. Truth and Reconciliation Commission Reports. National Center for Truth and Reconciliation; 2015; Available from: https://nctr.ca/records/reports/#trc-reports.
- Footnote 288
-
The Truth and Reconciliation Commission of Canada. Honouring the Truth, Reconciling for the Future: Summary of the Final Report of the Truth and Reconciliation Commission of Canada. The Truth and Reconciliation Commission of Canada; 2015.
- Footnote 289
-
Turpel-Lafond, ME. In Plain Sight: Addressing Indigenous-Specific Racism and Discrimination in B.C. Health Care. Office of the British Columbia Minister of Health; 2020.
- Footnote 290
-
Commission of the Pan American Health Organization on Equity and Health Inequalities in the Americas. Just Societies: Health Equity and Dignified Lives. Washington, D.C.: Pan American Health Organization; 2019.
- Footnote 291
-
Allen, L, Hatala, A, Ijaz, S, Courchene, ED, Bushie, EB. Indigenous-Led Health Care Partnerships in Canada. Canadian Medical Association Journal. 2020; 192(9):E208.
- Footnote 292
-
Richmond, C, Ambtman-Smith, V, Bourassa, C, Cassidy-Mathews, C, Duhamel, K, Keewatin, M, et al. COVID-19 and Indigenous Health and Wellness: Our Strength Is in Our Stories. Royal Society of Canada; 2020.
- Footnote 293
-
Health Canada, Assembly of First Nations. First Nations Mental Wellness Continuum Framework - Summary Report. Ottawa, ON: Health Canada; 2015.
- Footnote 294
-
Health Canada, Assembly of First Nations, National Native Addictions Partnership Foundation Inc. Honouring Our Strengths: A Renewed Framework to Address Substance Use Issues among First Nations People in Canada. Ottawa, ON: Health Canada; 2011.
- Footnote 295
-
Truth and Reconciliation Commission of Canada. What We Have Learned: Principles of Truth and Reconciliation. Truth and Reconciliation Commission of Canada; 2015.
- Footnote 296
-
Royal Commission on Aboriginal Peoples. The Path to Healing: Report of the National Round Table on Aboriginal Health and Social Issues. Vancouver, BC: Royal Commission on Aboriginal Peoples; 1993.
- Footnote 297
-
World Health Organization. One Health. World Health Organization; 2017.
- Footnote 298
-
Mackenzie, JS, Jeggo, M. The One Health Approach-Why Is It So Important? Tropical Medicine and Infectious Disease. 2019; 4(2):88.
- Footnote 299
-
Ruckert, A, Zinszer, K, Zarowsky, C, Labonté, R, Carabin, H. What Role for One Health in the COVID-19 Pandemic? Canadian Journal of Public Health. 2020; 111(5):641-4.
- Footnote 300
-
Kahn, LH. Antimicrobial Resistance: A One Health Perspective. Transactions of The Royal Society of Tropical Medicine and Hygiene. 2017; 111(6):255-60.
- Footnote 301
-
University of Calgary. Antimicrobial Resistance - One Health Consortium. University of Calgary; 2021; Available from: https://research.ucalgary.ca/amr.
- Footnote 302
-
Mehrotra, M, Li, XZ, Ireland, MJ. Enhancing Antimicrobial Stewardship by Strengthening the Veterinary Drug Regulatory Framework. Canada Communicable Disease Report. 2017; 43(11):220-3.
- Footnote 303
-
Public Health Agency of Canada. Pan-Canadian Framework for Action on Antimicrobial Resistance and Antimicrobial Use. Canada Communicable Disease Report. 2017; 43(11):217-9.
- Footnote 304
-
Upshaw, TL, Brown, C, Smith, R, Perri, M, Ziegler, C, Pinto, AD. Social Determinants of COVID-19 Incidence and Outcomes: A Rapid Review. PloS one. 2021; 16(3):e0248336.
- Footnote 305
-
Etowa, J, Hyman, I. Unpacking the Health and Social Consequences of COVID-19 through a Race, Migration and Gender Lens. Canadian Journal of Public Health. 2021; 112(1):8-11.
- Footnote 306
-
Thompson, E, Edjoc, R, Atchessi, N, Striha, M, Gabrani-Juma, I, Dawson, T. COVID-19: A Case for the Collection of Race Data in Canada and Abroad. Canada Communicable Disease Report. 2021; 47(7-8):300-4.
- Footnote 307
-
Government of Manitoba. COVID-19 Infections in Manitoba: Race, Ethnicity, and Indigeneity. Government of Manitoba; 2021.
- Footnote 308
-
Wellesley Insititute, Ontario Health. Tracking COVID-19 through Race-Based Data. Ontario Health; 2021.
- Footnote 309
-
Thakur, B, Dubey, P, Benitez, J, Torres, JP, Reddy, S, Shokar, N, et al. A Systematic Review and Meta-Analysis of Geographic Differences in Comorbidities and Associated Severity and Mortality among Individuals with COVID-19. Scientific Reports. 2021; 11(1):8562.
- Footnote 310
-
Pan-Canadian Public Health Network. Key Health Inequalities in Canada: A National Portrait. Pan-Canadian Public Health Network; 2018.
- Footnote 311
-
Gagné, T, Veenstra, G. Inequalities in Hypertension and Diabetes in Canada: Intersections between Racial Identity, Gender, and Income. Ethnicity & Disease. 2017; 27(4):371-8.
- Footnote 312
-
Chu, M, Truscott, R, Young, S, Harrington, D, Keller-Olaman, S, Manson, H, et al. The Burden of Chronic Diseases in Ontario: Key Estimates to Support Efforts in Prevention. Cancer Care Ontario, Public Health Ontario; 2019.
- Footnote 313
-
Dai, H, Younis, A, Kong, JD, Bragazzi, NL, Wu, J. Trends and Regional Variation in Prevalence of Cardiovascular Risk Factors and Association with Socioeconomic Status in Canada, 2005-2016. Journal of the American Medical Association Network Open. 2021; 4(8):e2121443.
- Footnote 314
-
Anand, SS, Abonyi, S, Arbour, L, Balasubramanian, K, Brook, J, Castleden, H, et al. Explaining the Variability in Cardiovascular Risk Factors among First Nations Communities in Canada: A Population-Based Study. The Lancet Planetary Health. 2019; 3(12):e511-e20.
- Footnote 315
-
Vanasse, A, Courteau, J, Asghari, S, Leroux, D, Cloutier, L. Health Inequalities Associated with Neighbourhood Deprivation in the Quebec Population with Hypertension in Primary Prevention of Cardiovascular Disease. Chronis Diseases and Injuries in Canada. 2014; 34(4):181-94.
- Footnote 316
-
Nash, DM, Dirk, JS, McArthur, E, Green, ME, Shah, BR, Walker, JD, et al. Kidney Disease and Care among First Nations People with Diabetes in Ontario: A Population-Based Cohort Study. Canadian Medical Association Journal Open. 2019; 7(4):E706.
- Footnote 317
-
Thomas, DA, Huang, A, McCarron, MCE, Kappel, JE, Holden, RM, Yeates, KE, et al. A Retrospective Study of Chronic Kidney Disease Burden in Saskatchewan’s First Nations People. Canadian Journal of Kidney Health and Disease. 2018; 5.
- Footnote 318
-
Choi, KH, Denice, P, Haan, M, Zajacova, A. Studying the Social Determinants of COVID-19 in a Data Vacuum. Canadian Review of Sociology. 2021; 58(2):146-64.
- Footnote 319
-
Sundaram, ME, Calzavara, A, Mishra, S, Kustra, R, Chan, AK, Hamilton, MA, et al. Individual and Social Determinants of SARS-Cov-2 Testing and Positivity in Ontario, Canada: A Population-Wide Study. Canadian Medical Association Journal. 2021; 193(20):E723.
- Footnote 320
-
Yeates, K, Tonelli, M. Chronic Kidney Disease among Aboriginal People Living in Canada. Clinical Nephrology. 2010; 74(1):57-60.
- Footnote 321
-
Garcia-Garcia, G, Jha, V, on behalf of the World Kidney Day Steering Committee. CKD in Disadvantaged Populations. Canadian Journal of Kidney Health and Disease. 2015; 2(1):3-6.
- Footnote 322
-
Public Health Ontario. Enhanced Epidemiological Summary: COVID-19 in Ontario – a Focus on Material Deprivation. Public Health Ontario; 2020.
- Footnote 323
-
Solar, O, Irwin, A. A Conceptual Framework for Action on the Social Determinants of Health. Social Determinants of Health Discussion Paper 2 (Policy and Practice). Geneva, Switzerland: World Health Organization; 2007.
- Footnote 324
-
Ndumbe-Eyoh, S, Muzumdar, P, Betker, C, Oickle, D. 'Back to Better': Amplifying Health Equity, and Determinants of Health Perspectives during the COVID-19 Pandemic. Global Health Promotion. 2021; 28(2):7-16.
- Footnote 325
-
Knaak, S, Livingston, J, Stuart, H, Ungar, T. Combating Mental Illness- and Substance Use-Related Structural Stigma in Health Care: A Framework for Action. Ottawa, ON: Mental Health Commission of Canada; 2020.
- Footnote 326
-
Johnson-Agbakwu, CE, Ali, NS, Oxford, CM, Wingo, S, Manin, E, Coonrod, DV. Racism, COVID-19, and Health Inequity in the USA: A Call to Action. Journal of Racial and Ethnic Health Disparities. 2020:1-7.
- Footnote 327
-
Kunins, HV. Structural Racism and the Opioid Overdose Epidemic: The Need for Antiracist Public Health Practice. Journal of Public Health Management and Practice. 2020; 26(3):201-5.
- Footnote 328
-
Dryden, O, Nnorom, O. Time to Dismantle Systemic Anti-Black Racism in Medicine in Canada. Canadian Medical Association Journal. 2021; 193(2):E55-E7.
- Footnote 329
-
Richardson, L, Crawford, A. COVID-19 and the Decolonization of Indigenous Public Health. Canadian Medical Association Journal. 2020; 192(38):E1098-E100.
- Footnote 330
-
Annals of Family Medicine. A Shared Bibliography on Systemic Racism and Health Disparities. Annals of Family Medicine; 2020; Available from: https://www.annfammed.org/content/shared-bibliography-systemic-racism-and-health-disparities.
- Footnote 331
-
Krieger, N. Enough: COVID-19, Structural Racism, Police Brutality, Plutocracy, Climate Change—and Time for Health Justice, Democratic Governance, and an Equitable, Sustainable Future. American Journal of Public Health. 2020; 110(11):1620-3.
- Footnote 332
-
National Collaborating Centre for Determinants of Health. Integrating Social Determinants of Health and Health Equity into Canadian Public Health Practice: Environmental Scan 2010. Antigonish, NS: National Collaborating Centre for Determinants of Health; 2010.
- Footnote 333
-
Jensen, N, Kelly, AH, Avendano, M. The COVID-19 Pandemic Underscores the Need for an Equity-Focused Global Health Agenda. Humanities and Social Sciences Communications. 2021; 8(1):15.
- Footnote 334
-
Blair, A, Warsame, K, Naik, H, Byrne, W, Parnia, A, Siddiqi, A. Identifying Gaps in COVID-19 Health Equity Data Reporting in Canada Using a Scorecard Approach. Canadian Journal of Public Health. 2021; 112(3):352-62.
- Footnote 335
-
National Collaborating Centre for Determinants of Health. Building a Culture of Equity in Canadian Public Health: An Environmental Scan. Antigonish, NS: National Collaborating Centre for Determinants of Health; 2018.
- Footnote 336
-
Marchildon, GP, Allin, S, Merkur, S. Canada: Health System Review. Third Edition. Copenhagen, Denmark: North American Observatory on Health Systems and Policies & European Observatory on Health Systems and Policies, WHO Regional Office for Europe; 2020.
- Footnote 337
-
Health Canada. Health Portfolio. Government of Canada; 2017.
- Footnote 338
-
Indigenous Services Canada. Indigenous Health Care in Canada. Government of Canada; 2021.
- Footnote 339
-
Halseth, R, Murdock, L. Supporting Indigenous Self-Determination in Health: Lessons Learned from a Review of Best Practices in Health Governance in Canada and Internationally. Prince George, BC: National Collaborating Centre for Indigenous Health; 2020.
- Footnote 340
-
Indigenous Services Canada. Indigenous Health. Government of Canada; 2021.
- Footnote 341
-
First Nations Health Authority. FNHA Mandate. First Nations Health Authority.
- Footnote 342
-
World Health Organization. Essential Public Health Functions, Health Systems, and Health Security: Developing Conceptual Clarity and a WHO Roadmap for Action. Geneva, Switzerland: World Health Organization; 2018.
- Footnote 343
-
Bettcher, DW, Sapirie, S, Goon, EH. Essential Public Health Functions: Results of the International Delphi Study. World Health Statistics Quarterly. 1998; 51(1):44-54.
- Footnote 344
-
Report of the National Advisory Committee on Population Health (ACPH). In: Naylor D, Basrur S, Bergeron MG, Brunham RC, Butler-Jones D, Dafoe G, et al., editors. Learning from SARS: Renewal of Public Health in Canada. Ottawa, ON: National Advisory Committee on SARS and Public Health; 2003.
- Footnote 345
-
Centres for Disease Control and Prevention. 10 Essential Public Health Services. Centres for Disease Control and Prevention; 2020.
- Footnote 346
-
Pan American Health Organization. The Essential Public Health Functions in the Americas: A Renewal for the 21st Century - Conceptual Framework and Description. Washington, D.C.: Pan American Health Organization; 2020.
- Footnote 347
-
World Health Organization. Everybody's Business: Strengthening Health Systems to Improve Health Outcomes - WHO’s Framework for Action. World Health Organization; 2007.
- Footnote 348
-
Hawe, P, Potvin, L. What Is Population Health Intervention Research? Canadian Journal of Public Health. 2009; 100(1):I8-I14.
- Footnote 349
-
Frieden, TR. A Framework for Public Health Action: The Health Impact Pyramid. American Journal of Public Health. 2010; 100(4):590-5.
- Footnote 350
-
Carey, G, Crammond, B, De Leeuw, E. Towards Health Equity: A Framework for the Application of Proportionate Universalism. International Journal for Equity in Health. 2015; 14(1):81.
- Footnote 351
-
Rideout, K, Oickle, D. Glossary of Health Equity in the Context of Environmental Public Health Practice. Journal of Epidemiology and Community Health. 2019; 73(9):806.
- Footnote 352
-
National Collaborating Centre for Determinants of Health. Let’s Talk: Universal and Targeted Approaches to Health Equity. Antigonish, NS: National Collaborating Centre for Determinants of Health; 2013.
- Footnote 353
-
National Collaborating Centre for Method and Tools. Evidence-Informed Decision Making. National Collaborating Centre for Method and Tools; 2021.
- Footnote 354
-
Brownson, RC, Fielding, JE, Maylahn, CM. Evidence-Based Public Health: A Fundamental Concept for Public Health Practice. Annual Review of Public Health. 2009; 30(1):175-201.
- Footnote 355
-
Dubois, A, Lévesque, M. Canada's National Collaborating Centres: Facilitating Evidence-Informed Decision-Making in Public Health. Canada Communicable Disease Report. 2020; 46(2-3):31-5.
- Footnote 356
-
Husson, H, Howarth, C, Neil-Sztramko, S, Dobbins, M. The National Collaborating Centre for Methods and Tools (NCCMT): Supporting Evidence-Informed Decision-Making in Public Health in Canada. Canada Communicable Disease Report. 2021; 47(5-6):292-6.
- Footnote 357
-
Peters, DH, Tran, NT, Adam, T. Implementation Research in Health: A Practical Guide. Alliance for Health Policy and Systems Research, World Health Organization; 2013.
- Footnote 358
-
National Collaborating Centres for Public Health. National Collaborating Centres for Public Health; Available from: https://nccph.ca/.
- Footnote 359
-
Mackintosh, J, Ciliska, D, Tulloch, K. Evidence-Informed Decision Making in Public Health in Action. Environmental Health Review. 2015; 58(1):15-9.
- Footnote 360
-
Ciliska, D, Thomas, H, Buffett, C. An Introduction to Evidence-Informed Public Health and a Compendium of Critical Appraisal Tools for Public Health Practice. National Collaborating Centre for Methods and Tools; 2008.
- Footnote 361
-
Jacobs, JA, Jones, E, Gabella, BA, Spring, B, Brownson, RC. Tools for Implementing an Evidence-Based Approach in Public Health Practice. Preventing chronic disease. 2012; 9:E116-E.
- Footnote 362
-
Brownson, RC, Baker, EA, Deshpande, AD, Gillespie, KN. Evidence-Based Public Health. 3rd. Oxford University Press; 2017.
- Footnote 363
-
Public Health Agency of Canada. National Microbiology Laboratory. Government of Canada; 2021.
- Footnote 364
-
Public Health Agency of Canada. National Emergency Strategic Stockpile. Government of Canada; 2019.
- Footnote 365
-
World Health Organization. Epidemic Intelligence from Open Sources (EIOS) - Zero Impact from Health Threats. World Health Organization; 2021.
- Footnote 366
-
Budd, J, Miller, BS, Manning, EM, Lampos, V, Zhuang, M, Edelstein, M, et al. Digital Technologies in the Public-Health Response to COVID-19. Nature Medicine. 2020; 26(8):1183-92.
- Footnote 367
-
Public Health Agency of Canada. Core Competencies for Public Health in Canada. Ottawa, ON: Government of Canada; 2007.
- Footnote 368
-
Joint Task Group on Public Health Human Resources. Building the Public Health Workforce for the 21st Century: A Pan-Canadian Framework for Public Health Human Resources Planning. Government of Canada; 2005.
- Footnote 369
-
Massé, R, Moloughney, B. New Era for Schools of Public Health in Canada. Public Health Reviews. 2011; 33:277-88.
- Footnote 370
-
Tikkanen, R, Osborn, R, Mossialos, E, Djordjevic, A, Wharton, GA. International Health Care System Profiles - Canada. The Commonwealth Fund; 2020.
- Footnote 371
-
Mowat, DL, Butler-Jones, D. Public Health in Canada: A Difficult History. Healthcare Papers. 2007; 7(3):31-6.
- Footnote 372
-
Canadian Public Health Association. Public Health in the Context of Health Systems Renewal in Canada: Background Document. Canadian Public Health Association; 2019.
- Footnote 373
-
Norris, S. Federal Funding for Health Care: Background Paper. Ottawa, ON: Library of Parliament; 2020.
- Footnote 374
-
Government of Canada. COVID-19: Support to Provinces and Territories. Government of Canada; 2021.
- Footnote 375
-
Canadian Institute for Health Information. National Health Expenditure Trends. Ottawa, ON: Canadian Institute for Health Information; 2020.
- Footnote 376
-
Masters, R, Anwar, E, Collins, B, Cookson, R, Capewell, S. Return on Investment of Public Health Interventions: A Systematic Review. Journal of Epidemiology and Community Health. 2017; 71(8):827-34.
- Footnote 377
-
Nurse, J, Dorey, S, Yao, L, Sigfrid, L, Yfantopolous, P, McDaid, D, et al. The Case for Investing in Public Health: A Public Health Summary Report for EPHO 8. World Health Organization; 2014.
- Footnote 378
-
World Health Organization. Commission on Social Determinants of Health, 2005-2008. World Health Organization; 2008.
- Footnote 379
-
Di Ruggiero, E, Bhatia, D, Umar, I, Arpin, E, Champagne, C, Clavier, C, et al. Governing for the Public’s Health: Governance Options for a Strengthened and Renewed Public Health System in Canada. National Collaborating Centres of Public Health; [In Press].
- Footnote 380
-
Dyke, E. What We Heard Report: A Renewed and Strengthened Public Health System in Canada. Public Health Agency of Canada; [In Press].
- Footnote 381
-
Ndumbe-Eyoh, S, Moffatt, H. Intersectoral Action for Health Equity: A Rapid Systematic Review. BioMed Central Public Health. 2013; 13(1):1056.
- Footnote 382
-
Lucyk, K. Commentary – Intersectoral Action on the Social Determinants of Health and Health Equity in Canada: December 2019 Federal Government Mandate Letter Review. Health Promotion and Chronic Disease Prevention in Canada. 2020; 40(10):10.
- Footnote 383
-
Diallo, T. Five Examples of Intersectoral Action for Health at the Local and Regional Level in Canada. Montréal, QC: National Collaborating Centre for Healthy Public Policy; 2020.
- Footnote 384
-
National Academies of Sciences Engineering and Medicine. 7 - Partners in Promoting Health Equity in Communities. In: Baciu A, Negussie Y, Geller A, et al., editors. Communities in Action: Pathways to Health Equity. Washington, DC: National Academies Press; 2017. p. 383-446.
- Footnote 385
-
Mulligan, K. Strengthening Community Connections: The Future of Public Health Is at the Neighbourhood Scale. National Collaborating Centres of Public Health; [In Press].
- Footnote 386
-
Commission on Social Determinants of Health. Closing the Gap in a Generation: Health Equity through Action on the Social Determinants of Health. World Health Organization; 2008.
- Footnote 387
-
Bay Area Regional Health Inequities Initiative. A Public Health Framework for Reducing Health Inequities: Bay Area Regional Health Inequities Initiative; 2020. Available from: https://www.barhii.org/barhii-framework.
- Footnote 388
-
National Collaborating Centre for Determinants of Health. Let’s Talk: Moving Upstream. Antigonish, NS: National Collaborating Centre for Determinants of Health; 2014.
- Footnote 389
-
Lorenc, T, Petticrew, M, Welch, V, Tugwell, P. What Types of Interventions Generate Inequalities? Evidence from Systematic Reviews. Journal of Epidemiology and Community Health. 2013; 67(2):190.
- Footnote 390
-
Litvak, E, Dufour, R, Leblanc, É, Kaiser, D, Mercure, S-A, Nguyen, CT, et al. Making Sense of What Exactly Public Health Does: A Typology of Public Health Interventions. Canadian Journal of Public Health. 2020; 111(1):65-71.
- Footnote 391
-
Jarvis, T, Scott, F, El-Jardali, F, Alvarez, E. Defining and Classifying Public Health Systems: A Critical Interpretive Synthesis. Health Research Policy and Systems. 2020; 18(1):68.
- Footnote 392
-
Liburd, LC, Hall, JE, Mpofu, JJ, Williams, SM, Bouye, K, Penman-Aguilar, A. Addressing Health Equity in Public Health Practice: Frameworks, Promising Strategies, and Measurement Considerations. Annual Review of Public Health. 2020; 41(1):417-32.
- Footnote 393
-
National Collaborating Centre for Determinants of Health. Assessing the Impact and Effectiveness of Intersectoral Action on the Social Determinants of Health and Health Equity: An Expedited Systematic Review. Antigonish, NS: National Collaborating Centre for Determinants of Health; 2012.
- Footnote 394
-
Tonelli, M, Tang, K-C, Forest, P-G. Canada Needs a “Health in All Policies” Action Plan Now. Canadian Medical Association Journal. 2020; 192(3):E61.
- Footnote 395
-
National Collaborating Centre for Healthy Public Policy. Health Impact Assessment. National Collaborating Centre for Healthy Public Policy; 2010.
- Footnote 396
-
Freeman, S. Health Impact Assessment (HIA) Knowledge and Needs Scan: Findings, Gaps and Recommendations. Vancouver, BC: National Collaborating Centre for Environmental Health; 2019.
- Footnote 397
-
McCallum, LC, Ollson, CA, Stefanovic, IL. Advancing the Practice of Health Impact Assessment in Canada: Obstacles and Opportunities. Environmental Impact Assessment Review. 2015; 55:98-109.
- Footnote 398
-
Diallo, T, Freeman, S. Health Impact Assessment—Insights from the Experience of Québec. Environmental Health Review. 2020; 63(1):6-13.
- Footnote 399
-
National Collaborating Centre for Determinants of Health. Collective Impact and Public Health: An Old/New Approach - Stories of Two Canadian Initiatives. Antigonish, NS: National Collaborating Centre for Determinants of Health; 2017.
- Footnote 400
-
Kania, J, Kramer, M. Collective Impact. Stanford Social Innovation Review. 2011; 9(1):36-41.
- Footnote 401
-
Evans, RE, Moore, G, Movsisyan, A, Rehfuess, E. How Can We Adapt Complex Population Health Interventions for New Contexts? Progressing Debates and Research Priorities. Journal of Epidemiology and Community Health. 2021; 75(1):40.
- Footnote 402
-
Minary, L, Alla, F, Cambon, L, Kivits, J, Potvin, L. Addressing Complexity in Population Health Intervention Research: The Context/Intervention Interface. Journal of Epidemiology and Community Health. 2018; 72(4):319.
- Footnote 403
-
McGill, E, Marks, D, Er, V, Penney, T, Petticrew, M, Egan, M. Qualitative Process Evaluation from a Complex Systems Perspective: A Systematic Review and Framework for Public Health Evaluators. PLOS Medicine. 2020; 17(11):e1003368.
- Footnote 404
-
Rychetnik, L, Frommer, M, Hawe, P, Shiell, A. Criteria for Evaluating Evidence on Public Health Interventions. Journal of Epidemiology and Community Health. 2002; 56(2):119-27.
- Footnote 405
-
McLaren, L, Braitstein, P, Buckeridge, D, Contandriopoulos, D, Creatore, MI, Faulkner, G, et al. Why Public Health Matters Today and Tomorrow: The Role of Applied Public Health Research. Canadian Journal of Public Health. 2019; 110(3):317-22.
- Footnote 406
-
Nickel, S, von dem Knesebeck, O. Do Multiple Community-Based Interventions on Health Promotion Tackle Health Inequalities? International Journal for Equity in Health. 2020; 19(1):157.
- Footnote 407
-
Jewett, RL, Mah, SM, Howell, N, Larsen, MM. Social Cohesion and Community Resilience During COVID-19 and Pandemics: A Rapid Scoping Review to Inform the United Nations Research Roadmap for COVID-19 Recovery. International Journal of Health Services. 2021; 51(3):325-36.
- Footnote 408
-
National Collaborating Centre for Determinants of Health. Let’s Talk: Community Engagement for Health Equity. Antigonish, NS: National Collaborating Centre for Determinants of Health; 2021.
- Footnote 409
-
National Academies of Sciences Engineering and Medicine. 4 - The Role of Communities in Promoting Health Equity. In: Baciu A, Negussie Y, Geller A, et al., editors. Communities in Action: Pathways to Health Equity. Washington, DC: National Academies Press; 2017. p. 185-210.
- Footnote 410
-
O’Mara-Eves, A, Brunton, G, Oliver, S, Kavanagh, J, Jamal, F, Thomas, J. The Effectiveness of Community Engagement in Public Health Interventions for Disadvantaged Groups: A Meta-Analysis. BioMed Central Public Health. 2015; 15(1):129.
- Footnote 411
-
James, W. 4 - The Community. In: Institute of Medicine (US) Committee on Assuring the Health of the Public in the 21st Century, editor. The Future of the Public's Health in the 21st Century. Washington, DC: National Academies Press; 2002.
- Footnote 412
-
South Asian Health Network. South Asian Health Network; Available from: https://southasianhealthnetwork.ca/.
- Footnote 413
-
Black Scientists’ Task Force on Vaccine Equity. Black Scientists’ Task Force on Vaccine Equity; 2021; Available from: http://www.torontoblackcovid.com/.
- Footnote 414
-
InclusionNS. InclusionNS; Available from: https://www.inclusionns.ca/.
- Footnote 415
-
South, J, Phillips, G. Evaluating Community Engagement as Part of the Public Health System. Journal of Epidemiology and Community Health. 2014; 68(7):692.
- Footnote 416
-
National Collaborating Centre for Determinants of Health. Review Summary: Community Engagement to Reduce Inequalities in Health. Antigonish, NS: National Collaborating Centre for Determinants of Health; 2015.
- Footnote 417
-
Government of Ontario. Ontario Supporting COVID-19 Response in High Priority Communities. Government of Ontario; 2021.
- Footnote 418
-
City of Toronto. City of Toronto Awards $5.5 Million in COVID-19 Vaccine Engagement Teams Grants to Local Agencies for Vaccine Outreach in Vulnerable Communities. City of Toronto; 2021.
- Footnote 419
-
Ireland, N. Here's How Community Groups Are Getting COVID-19 Vaccinations to Indigenous People in Canada's Largest City. CBC News. 2021.
- Footnote 420
-
Assembly of First Nations, Métis National Council, Inuit Tapiriit Kanatami, Greenwood, M, Adams, E, Anderson, M, et al. Visioning the Future: First Nations, Inuit, & Métis Population and Public Health. Greenwood M, Adams E, editors. National Collaborating Centres of Public Health; [In Press].
- Footnote 421
-
Baba, L. Cultural Safety in First Nations, Inuit and Métis Public Health: Environmental Scan of Cultural Competency and Safety in Education, Training and Health Services. Prince George, BC: National Collaborating Centre for Aboriginal Health; 2013.
- Footnote 422
-
Greenwood, M, Lindsay, N, King, J, Loewen, D. Ethical Spaces and Places: Indigenous Cultural Safety in British Columbia Health Care. AlterNative: An International Journal of Indigenous Peoples. 2017; 13(3):179-89.
- Footnote 423
-
Churchill, M, Parent-Bergeron, M, Smylie, J, Ward, C, Fridkin, A, Smylie, D, et al. Evidence Brief: Wise Practices for Indigenous-Specific Cultural Safety Training. Well Living House Action Research Centre for Indigenous Infant, Child and Family Health and Wellbeing, Centre for Urban Health Solutions, St. Michael’s Hospital; 2017.
- Footnote 424
-
First Nations Health Authority, First Nations Health Council, First Nations Health Director’s Association. Anti-Racism, Cultural Safety & Humility Framework. First Nations Health Authority; 2021.
- Footnote 425
-
Williams, R. Culturally Safe - What Does It Mean for Our Work Practice? Australian and New Zealand Journal of Public Health. 1999; 23(2):213-4.
- Footnote 426
-
Feng, P, Di Ruggiero, E, Reid, R, Pinto, A, Upshur, R. Public Health and Learning Health Systems White Paper. Toronto, ON: Institute of Health Policy, Management and Evaluation, University of Toronto; 2021.
- Footnote 427
-
Institute of Medicine (US) Committee on the Learning Health Care System in America. Best Care at Lower Cost: The Path to Continuously Learning Health Care in America. Smith M, Saunders R, Stuckhardt L, McGinnis JM, editors. Washington, DC: National Academies Press (US); 2013.
- Footnote 428
-
Glazier, R. The Lessons of COVID-19 for Canadian Learning Health Systems. Longwoods Breakfast Series: Canadian Institute of Health Research; 2020
- Footnote 429
-
Public Health Agency of Canada. Public Health Surveillance. Government of Canada; 2021.
- Footnote 430
-
Huston, P, Edge, VL, Bernier, E. Reaping the Benefits of Open Data in Public Health. Canada Communicable Disease Report. 2019; 45(11):252-6.
- Footnote 431
-
Mishra, S, Kwong, JC, Chan, AK, Baral, SD. Understanding Heterogeneity to Inform the Public Health Response to COVID-19 in Canada. Canadian Medical Association Journal. 2020; 192(25):E684.
- Footnote 432
-
van Panhuis, WG, Paul, P, Emerson, C, Grefenstette, J, Wilder, R, Herbst, AJ, et al. A Systematic Review of Barriers to Data Sharing in Public Health. BioMed Central Public Health. 2014; 14(1):1144.
- Footnote 433
-
Black Health Equity Working Group. Engagement, Governance, Access, and Protection (EGAP): A Data Governance Framework for Health Data Collected from Black Communities in Ontario. Alliance for Healthier Communities; 2021.
- Footnote 434
-
First Nations Infomation Governance Centre. The First Nations Principles of OCAP®. First Nations Infomation Governance Centre; 2021; Available from: https://fnigc.ca/ocap-training/.
- Footnote 435
-
Wolfe, S, Hill, M. Cultural Safety: The Criticality of Indigenous Knowledges and Data Governance. Canadian Science Policy Centre; 2020.
- Footnote 436
-
Council of Canadian Academies. Accessing Health and Health-Related Data in Canada. Ottawa, ON: Council of Canadian Academies; 2015.
- Footnote 437
-
Buckeridge, DL, Goel, V. Health Informatics Education: An Opportunity for Public Health in Canada. Canadian Journal of Public Health. 2001; 92(3):233-6.
- Footnote 438
-
Buckeridge, D. An Evidence-Informed Vision for a Public Health Data System in Canada. National Collaborating Centres of Public Health; [In Press].
- Footnote 439
-
Public Health Agency of Canada. Vaccineconnect: It System for Managing Vaccination Rollout. Government of Canada; 2021.
- Footnote 440
-
Padgett, DK. Qualitative and Mixed Methods in Public Health. Thousand Oaks, CA: SAGE Publications, Inc.; 2012.
- Footnote 441
-
Baum, F. Researching Public Health: Behind the Qualitative-Quantitative Methodological Debate. Social Science & Medicine. 1995; 40(4):459-68.
- Footnote 442
-
Teti, M, Schatz, E, Liebenberg, L. Methods in the Time of COVID-19: The Vital Role of Qualitative Inquiries. International Journal of Qualitative Methods. 2020; 19(1):1-5.
- Footnote 443
-
Tremblay, S, Castiglione, S, Audet, L-A, Desmarais, M, Horace, M, Peláez, S. Conducting Qualitative Research to Respond to COVID-19 Challenges: Reflections for the Present and Beyond. International Journal of Qualitative Methods. 2021; 20(1):1-8.
- Footnote 444
-
Rogers, BJ, Swift, K, van der Woerd, K, Auger, M, Halseth, R, Atkinson, D, et al. At the Interface: Indigenous Health Practitioners and Evidence-Based Practice. Prince George, BC: National Collaborating Centre for Aboriginal Health; 2019.
- Footnote 445
-
Smylie, J, Olding, M, Ziegler, C. Sharing What We Know About Living a Good Life: Indigenous Approaches to Knowledge Translation. Journal of the Canadian Health Libraries Association. 2014; 35:16-23.
- Footnote 446
-
Haworth-Brockman, M, Betker, C. Measuring What Counts in the Midst of the COVID-19 Pandemic Equity Indicators for Public Health. National Collaborating Centre for Infectious Diseases; 2020.
- Footnote 447
-
First Nation Advisory Council. Katop Wasis Sesomiw Nokalawin Mo Nagelameg Neoteetjit Mitjoaatjitj: No Child Left Behind. First Nation Advisory Council; 2021.
- Footnote 448
-
Smylie, J, Firestone, M. Back to the Basics: Identifying and Addressing Underlying Challenges in Achieving High Quality and Relevant Health Statistics for Indigenous Populations in Canada. Statistical Journal of the IAOS. 2015; 31(1):67-87.
- Footnote 449
-
Pollock, NJ, Healey, GK, Jong, M, Valcour, JE, Mulay, S. Tracking Progress in Suicide Prevention in Indigenous Communities: A Challenge for Public Health Surveillance in Canada. BMC Public Health. 2018; 18(1):1320.
- Footnote 450
-
First Nations Information Governance Centre. A First Nations Data Governance Strategy - a Response to Direction Received from First Nations Leadership, Funded through Federal Budget 2018 in Support of the New Fiscal Relationship. First Nations Information Governance Centre; 2020.
- Footnote 451
-
Nickerson, M. First Nations’ Data Governance: Measuring the Nation-to-Nation Relationship. British Columbia First Nations’ Data Governance Initiative; 2017.
- Footnote 452
-
Tagalik, S. Inuit Qaujimajatuqangit: The Role of Indigenous Knowledge in Supporting Wellness in Inuit Communities in Nunavut. Prince George, BC: National Collaborating Centre for Aboriginal Health; 2012.
- Footnote 453
-
Brownson, RC, Kreuter, MW, Arrington, BA, True, WR. Translating Scientific Discoveries into Public Health Action: How Can Schools of Public Health Move Us Forward? Public health reports (Washington, DC : 1974). 2006; 121(1):97-103.
- Footnote 454
-
Nutbeam, D. Achieving ‘Best Practice’ in Health Promotion: Improving the Fit between Research and Practice. Health Education Research. 1996; 11(3):317-26.
- Footnote 455
-
Di Ruggiero, E, Papadopoulos, A, Steinberg, M, Blais, R, Frandsen, N, Valcour, J, et al. Strengthening Collaborations at the Public Health System–Academic Interface: A Call to Action. Canadian Journal of Public Health. 2020; 111(6):921-5.
- Footnote 456
-
Canadian Institutes of Health Research. Applied Public Health Chair Launch. Canadian Institutes of Health Research; 2021.
- Footnote 457
-
Paradis, G, Hamelin, A-M, Malowany, M, Levy, J, Rossignol, M, Bergeron, P, et al. The University–Public Health Partnership for Public Health Research Training in Quebec, Canada. American Journal of Public Health. 2016; 107(1):100-4.
- Footnote 458
-
Graham, JR, Sibbald, SL. Rebuilding Public Health on More Than Thoughts and Prayers. Canadian Journal of Public Health. 2021; 112(4):548-51.
- Footnote 459
-
Transdisciplinary Public Health: Research, Education, and Practice. Haire-Joshu D, McBride TD, editors. San Francisco, CA: John Wiley & Sons, Inc.; 2013.
- Footnote 460
-
Dankwa-Mullan, I, Rhee, KB, Stoff, DM, Pohlhaus, JR, Sy, FS, Stinson, N, et al. Moving toward Paradigm-Shifting Research in Health Disparities through Translational, Transformational, and Transdisciplinary Approaches. American Journal of Public Health. 2010; 100(S1):S19-S24.
- Footnote 461
-
Johnson, MT, Johnson, EA, Nettle, D, Pickett, KE. Designing Trials of Universal Basic Income for Health Impact: Identifying Interdisciplinary Questions to Address. Journal of Public Health. 2021:1-9.
- Footnote 462
-
Holmes, EA, O'Connor, RC, Perry, VH, Tracey, I, Wessely, S, Arseneault, L, et al. Multidisciplinary Research Priorities for the COVID-19 Pandemic: A Call for Action for Mental Health Science. The Lancet Psychiatry. 2020; 7(6):547-60.
- Footnote 463
-
Kivits, J, Ricci, L, Minary, L. Interdisciplinary Research in Public Health: The ‘Why’ and the ‘How’. Journal of Epidemiology and Community Health. 2019; 73(12):1061.
- Footnote 464
-
Leslie, M, Fadaak, R, Davies, J, Blaak, J, Forest, PG, Green, L, et al. Integrating the Social Sciences into the COVID-19 Response in Alberta, Canada. British Medical Journal Global Health. 2020; 5(7):e002672.
- Footnote 465
-
World Health Organization. Monitoring the Building Blocks of Health Systems: A Handbook of Indicators and Their Measurement Strategies. World Health Organization; 2010.
- Footnote 466
-
World Health Organization. Global Strategy on Digital Health 2020-2025. Geneva, CH: World Health Organization; 2021.
- Footnote 467
-
World Health Organization. Early Detection, Assessment and Response to Acute Public Health Events: Implementation of Early Warning and Response with a Focus on Event-Based Surveillance: Interim Version. Geneva, CH: World Health Organization; 2014.
- Footnote 468
-
Health Canada. Priority Strategies to Optimize Testing and Screening for COVID-19 in Canada: Report. Government of Canada; 2021.
- Footnote 469
-
Pabbaraju, K, Wong Anita, A, Douesnard, M, Ma, R, Gill, K, Dieu, P, et al. A Public Health Laboratory Response to the Pandemic. Journal of Clinical Microbiology. 2020; 58(8):e01110-20.
- Footnote 470
-
Government of Canada. Cracking the COVID-19 Code. Government of Canada; 2021.
- Footnote 471
-
Genome Canada. CanCOGeN. Genome Canada; 2020.
- Footnote 472
-
Hogan, C, Jassem, A, Sbihi, H, Joffres, Y, Tyson, J, Noftall, K, et al. Rapid Increase in SARS-Cov-2 P.1 Lineage Leading to Codominance with B.1.1.7 Lineage, British Columbia, Canada, January–April 2021. Emerging Infectious Disease Journal. 2021; 27(11).
- Footnote 473
-
Cyranoski, D. Alarming COVID Variants Show Vital Role of Genomic Surveillance. 2021;Sect. 337-8.
- Footnote 474
-
World Health Organization. Tracking SARS-Cov-2 Variants. World Health Organization; 2021.
- Footnote 475
-
Detsky, AS, Bogoch, II. COVID-19 in Canada: Experience and Response to Waves 2 and 3. Journal of the American Medical Association. 2021; 326(12):1145-6.
- Footnote 476
-
Organisation for Economic Co-Operation and Development. Access to COVID-19 Vaccines: Global Approaches in a Global Crisis. Organisation for Economic Co-Operation and Development (OECD); 2021.
- Footnote 477
-
Snowdon, AW, Wright, A, Saunders, M. An Evidence-Based Strategy to Scale Vaccination in Canada. Healthcare Quarterly. 2021; 24(1):28-35.
- Footnote 478
-
World Health Organization. WHO Launches a Chatbot on Facebook Messenger to Combat COVID-19 Misinformation. World Health Organization; 2020.
- Footnote 479
-
World Health Organization. WHO Health Alert Brings COVID-19 Facts to Billions Via Whatsapp. World Health Organization; 2021.
- Footnote 480
-
Brown, KA, Soucy, J-PR, Buchan, SA, Sturrock, SL, Berry, I, Stall, NM, et al. The Mobility Gap: Estimating Mobility Thresholds Required to Control SARS-Cov-2 in Canada. Canadian Medical Association Journal. 2021; 193(17):E592.
- Footnote 481
-
Sun, S, Shaw, M, Moodie, E, Ruths, D. COVID Alert Application Effectiveness. McGill University; 2021.
- Footnote 482
-
Government of Canada. Download COVID Alert Today. Government of Canada; 2021.
- Footnote 483
-
Health Canada. Healthadapt. Government of Canada; 2020.
- Footnote 484
-
ClimateData.ca. Learning Zone. ClimateData.ca; 2021; Available from: https://climatedata.ca/learn/.
- Footnote 485
-
Seto, E, Challa, P, Ware, P. Adoption of COVID-19 Contact Tracing Apps: A Balance between Privacy and Effectiveness. Journal of Medical Internet Research. 2021; 23(3):e25726.
- Footnote 486
-
Colizza, V, Grill, E, Mikolajczyk, R, Cattuto, C, Kucharski, A, Riley, S, et al. Time to Evaluate COVID-19 Contact-Tracing Apps. Nature Medicine. 2021; 27(3):361-2.
- Footnote 487
-
Panch, T, Pearson-Stuttard, J, Greaves, F, Atun, R. Artificial Intelligence: Opportunities and Risks for Public Health. The Lancet Digital Health. 2019; 1(1):e13-e4.
- Footnote 488
-
Dankwa-Mullan, I, Scheufele, EL, Matheny, ME, Quintana, Y, Chapman, WW, Jackson, G, et al. A Proposed Framework on Integrating Health Equity and Racial Justice into the Artificial Intelligence Development Lifecycle. Journal of Health Care for the Poor and Underserved. 2021; 32(2):300-17.
- Footnote 489
-
Smith, MJ, Axler, R, Bean, S, Rudzicz, F, Shaw, J. Four Equity Considerations for the Use of Artificial Intelligence in Public Health. Bulletin of the World Health Organization. 2020; 98(4):290-2.
- Footnote 490
-
Canadian Institute for Advanced Research. Building a Learning Health System for Canadians: Report of the Cifar Task Force on Artificial Intelligence for Health Task Force. Canadian Institute for Advanced Research; 2020.
- Footnote 491
-
Dixon, BE, Rahurkar, S, Apathy, NC. Interoperability and Health Information Exchange for Public Health. In: Magnuson JA, Dixon BE, editors. Public Health Informatics and Information Systems. Cham: Springer International Publishing; 2020. p. 307-24.
- Footnote 492
-
Vaccine Hunters. About Us. Vaccine Hunters; 2021; Available from: https://vaccinehunters.ca/about.
- Footnote 493
-
Vaccine Hunters. Vaccine Hunters Canada to Pivot Operations. Vaccine Hunters; 2021; Available from: https://vaccinehunters.ca/pivot.
- Footnote 494
-
VaxHuntersCan. We've Developed a Free, Customizable, Multilingual, Open-Source Platform to Find Vaccine Appointments.: https://twitter.com/VaxHuntersCan/status/1430300283532419082?s=20 Aug 24, 2021[Tweet]. Available from: @VaxHuntersCan.
- Footnote 495
-
Kamwa Ngne, A, Morrison, V. Public Policy Competencies for Public Health: A Review of the Literature. National Collaborating Centre for Healthy Public Policy; 2021.
- Footnote 496
-
Bhatia, D, Vaga, K, Roerig, M, Pawa, J, Allin, S, Marchildon, G. COVID-19 Case and Contact Management Strategies in Canada. Toronto, ON: North American Observatory on Health Systems and Policies; 2020.
- Footnote 497
-
Khan, Y, O’Sullivan, T, Brown, A, Tracey, S, Gibson, J, Généreux, M, et al. Public Health Emergency Preparedness: A Framework to Promote Resilience. BioMed Central Public Health. 2018; 18(1):1344.
- Footnote 498
-
Coronado, F, Beck, AJ, Shah, G, Young, JL, Sellers, K, Leider, JP. Understanding the Dynamics of Diversity in the Public Health Workforce. Journal of Public Health Management and Practice. 2020; 26(4).
- Footnote 499
-
Sellers, K, Leider, JP, Gould, E, Castrucci, BC, Beck, A, Bogaert, K, et al. The State of the US Governmental Public Health Workforce, 2014–2017. American Journal of Public Health. 2019; 109(5):674-80.
- Footnote 500
-
Shahi, A, Karachiwalla, F, Grewal, N. Walking the Walk: The Case for Internal Equity, Diversity, and Inclusion Work within the Canadian Public Health Sector. Health Equity. 2019; 3(1):183-5.
- Footnote 501
-
Khan, MS, Lakha, F, Tan, MMJ, Singh, SR, Quek, RYC, Han, E, et al. More Talk Than Action: Gender and Ethnic Diversity in Leading Public Health Universities. The Lancet. 2019; 393(10171):594-600.
- Footnote 502
-
Statistics Canada. Mental Health among Health Care Workers in Canada during the COVID-19 Pandemic. The Daily; 2021.
- Footnote 503
-
Bryant-Genevier, J, Rao, CY, Lopes-Cardozo, B, Kone, A, Rose, C, Thomas, I, et al. Symptoms of Depression, Anxiety, Post-Traumatic Stress Disorder, and Suicidal Ideation among State, Tribal, Local, and Territorial Public Health Workers During the COVID-19 Pandemic — United States, March–April 2021. Morbidity and Mortality Weekly Report. 2021; 70:947-52.
- Footnote 504
-
Office of the Auditor General of Ontario. COVID-19 Preparedness and Management: Special Report on Emergency Management in Ontario—Pandemic Response. Toronto, ON: Office of the Auditor General of Ontario; 2020.
- Footnote 505
-
Public Health Ontario. COVID-19 – Strategies Adaptable from Healthcare to Public Health Settings to Support the Mental Health and Resilience of the Workforce during the COVID-19 Pandemic Recovery. Public Health Ontario; 2021.
- Footnote 506
-
Glynn, MK, Jenkins, ML, Jr., Ramsey, C, Simone, PM. Public Health Workforce 3.0: Recent Progress and What's on the Horizon to Achieve the 21st-Century Workforce. Journal of Public Health Management and Practice. 2019; 25(1):S6-S9.
- Footnote 507
-
Edwards, NC, MacLean Davison, C. Social Justice and Core Competencies for Public Health: Improving the Fit. Canadian Journal of Public Health. 2008; 99(2):130-2.
- Footnote 508
-
National Collaborating Centre for Determinants of Health. Core Competencies for Public Health in Canada: An Assessment and Comparison of Determinants of Health Content. Antigonish, NS: National Collaborating Centre for Determinants of Health; 2012.
- Footnote 509
-
Cabaj, JL, Musto, R, Ghali, WA. Public Health: Who, What, and Why? Canadian Journal of Public Health. 2019; 110(3):340-3.
- Footnote 510
-
Brownson, RC, Burke, TA, Colditz, GA, Samet, JM. Reimagining Public Health in the Aftermath of a Pandemic. American Journal of Public Health. 2020; 110(11):1605-10.
- Footnote 511
-
Bowes, C, Cote-Meek, S, Cutler, H, Labre, S, Lemieux, S. Talking Together to Improve Health: Gathering and Sharing Learning. Sudbury, ON: Locally Driven Collaborative Projects; 2020.
- Footnote 512
-
National Collaborating Centre for Determinants of Health. Let’s Talk: Racism and Health Equity (Rev. Ed.). Antigonish, NS: National Collaborating Centre for Determinants of Health; 2018.
- Footnote 513
-
National Collaborating Centre for Determinants of Health. Communicating to Propel Organizational Capacity for Action on Health Equity. Antigonish, NS: National Collaborating Centre for Determinants of Health; 2021.
- Footnote 514
-
Machado, S, Goldenberg, S. Sharpening Our Public Health Lens: Advancing Im/Migrant Health Equity during COVID-19 and Beyond. International Journal for Equity in Health. 2021; 20:57.
- Footnote 515
-
DeSalvo, KB, Wang, YC, Harris, A, Auerbach, J, Koo, D, O’Carroll, P. Public Health 3.0: A Call to Action for Public Health to Meet the Challenges of the 21st Century. Preventing Chronic Disease. 2017; 14:170017.
- Footnote 516
-
Jagals, P, Ebi, K. Core Competencies for Health Workers to Deal with Climate and Environmental Change. International Journal of Environmental Research and Public Health. 2021; 18(8):3849.
- Footnote 517
-
Lemery, J, Balbus, J, Sorensen, C, Rublee, C, Dresser, C, Balsari, S, et al. Training Clinical and Public Health Leaders in Climate and Health. Health Affairs. 2020; 39(12):2189-96.
- Footnote 518
-
Ghaffar, A, Rashid, SF, Wanyenze, RK, Hyder, AA. Public Health Education Post-COVID-19: A Proposal for Critical Revisions. British Medical Journal Global Health. 2021; 6(4):e005669.
- Footnote 519
-
Czabanowska, K, Kuhlmann, E. Public Health Competences through the Lens of the COVID-19 Pandemic: What Matters for Health Workforce Preparedness for Global Health Emergencies. International Journal of Health Planning and Management. 2021; 36(1):14-9.
- Footnote 520
-
Denis, J-L, Potvin, L, Rochon, J, Fournier, P, Gauvin, L. On Redesigning Public Health in Québec: Lessons Learned from the Pandemic. Canadian Journal of Public Health. 2020; 111(6):912-20.
- Footnote 521
-
Austin, SE, Ford, JD, Berrang-Ford, L, Araos, M, Parker, S, Fleury, MD. Public Health Adaptation to Climate Change in Canadian Jurisdictions. International Journal of Environmental Research and Public Health. 2015; 12(1):623-51.
- Footnote 522
-
Fiset-Laniel, J, Guyon, A, Perreault, R, Strumpf, EC. Public Health Investments: Neglect or Wilful Omission? Historical Trends in Quebec and Implications for Canada. Canadian Journal of Public Health. 2020; 111(3):383-8.
- Footnote 523
-
Caldwell, HAT, Scruton, S, Fierlbeck, K, Hajizadeh, M, Dave, S, Sim, SM, et al. Fare Well to Nova Scotia? Public Health Investments Remain Chronically Underfunded. Canadian Journal of Public Health. 2021; 112(2):186-90.
- Footnote 524
-
Hoffman, SJ, Creatore, MI, Klassen, A, Lay, AM, Fafard, P. Building the Political Case for Investing in Public Health and Public Health Research. Canadian Journal of Public Health. 2019; 110(3):270-4.
- Footnote 525
-
Bratina, B. COVID-19 and Indigenous Peoples: From Crisis Towards Meaningful Change. Standing Committee on Indigenous and Northern Affairs; 2021.
- Footnote 526
-
Waakebiness-Bryce Institute for Indigenous Health. What We Heard: Indigenous Peoples and COVID-19: Public Health Agency of Canada’s Companion Report. Public Health Agency of Canada; 2021.
- Footnote 527
-
Baum, F, Delany-Crowe, T, MacDougall, C, Lawless, A, van Eyk, H, Williams, C. Ideas, Actors and Institutions: Lessons from South Australian Health in All Policies on What Encourages Other Sectors’ Involvement. BioMed Central Public Health. 2017; 17(1):811.
- Footnote 528
-
Commission on Social Determinants of Health. Closing the Gap in a Generation: Health Equity through Action on the Social Determinants of Health - Executive Summary. World Health Organization; 2008.
- Footnote 529
-
Delany, T, Lawless, A, Baum, F, Popay, J, Jones, L, McDermott, D, et al. Health in All Policies in South Australia: What Has Supported Early Implementation? Health Promotion International. 2016; 31(4):888-98.
- Footnote 530
-
Kickbusch, I, Gleicher, D. Governance for Health in the 21st Century. Copenhagen: World Health Organization, Regional Office for Europe; 2013.
- Footnote 531
-
Government of Canada. Canada Health Act. Government of Canada; 2020.
- Footnote 532
-
Kermode-Scott, B. Canada Tries Once More to Set Public Health Goals. British Medical Journal. 2005; 331(7514):422-.
- Footnote 533
-
Government of Canada. Coronavirus Disease (COVID-19): Canada’s Response. Government of Canada; 2021.
- Footnote 534
-
Review Committee on the Functioning of the International Health Regulations. WHO’s Work in Health Emergencies - Strengthening Preparedness for Health Emergencies: Implementation of the International Health Regulations (2005). World Health Organization; 2021.
- Footnote 535
-
Bump, JB, Friberg, P, Harper, DR. International Collaboration and COVID-19: What Are We Doing and Where Are We Going? British Medical Journal. 2021; 372:n180.
- Footnote 536
-
World Health Organization. International Health Regulations. World Health Organization; 2005.
- Footnote 537
-
Dion, M, AbdelMalik, P, Mawudeku, A. Big Data and the Global Public Health Intelligence Network (GPHIN). Canada Communicable Disease Report. 2015; 41(9):209-14.
- Footnote 538
-
World Health Organization. WHO Hub for Pandemic and Epidemic Intelligence. World Health Organization; 2021.
- Footnote 539
-
Maxmen, A. Leader of WHO’s New Pandemic Hub: Improve Data Flow to Extinguish Outbreaks. Nature. 2021.
- Footnote 540
-
World Health Organization. WHO, Germany Open Hub for Pandemic and Epidemic Intelligence in Berlin. World Health Organization; 2021.
- Footnote 541
-
United Nations General Assembly. United Nations Declaration on the Rights of Indigenous Peoples. United Nations General Assembly; 2007.
- Footnote 542
-
Department of Justice. Backgrounder: United Nations Declaration on the Rights of Indigenous Peoples Act. Government of Canada; 2021.
- Footnote 543
-
First Nations Health Authority. First Nations Health Authority; 2021; Available from: https://www.fnha.ca/.
- Footnote 544
-
Northern Inter-Tribal Health Authority (NITHA). Northern Inter-Tribal Health Authority; 2021; Available from: https://www.nitha.com/.
- Footnote 545
-
McQueen, DV, Wismar, M, Lin, V, Jones, CM, Davies, M, ed. Intersectoral Governance for Health in All Policies: Structures, Actions and Experiences. World Health Organization on behalf of the European Observatory on Health Systems and Policies; 2012.
- Footnote 546
-
South Australia's HiAP Approach. Government of South Australia; 2018.
- Footnote 547
-
World Health Organization. Health in All Policies (HiAP) Framework for Country Action. World Health Organization; 2014.
- Footnote 548
-
Government of Newfoundland and Labrador. Take a Health-in-All-Policies Approach. Government of Newfoundland and Labrador.
- Footnote 549
-
Gagnon, F, Turgeon, J, Dallaire, C. L'évaluation D'impact sur la Santé au Québec: Lorsque la Loi Devient Levier D'action. Télescope. 2008; 14(2):79-94.
- Footnote 550
-
National Collaborating Centre for Indigenous Health. Pan-Canadian Health Inequities Reporting Initiative. Prince George, BC: National Collaborating Centre for Indigenous Health.
- Footnote 551
-
Pan-Canadian Public Health Network. Key Health Inequalities in Canada: A National Portrait - Executive Summary. Pan-Canadian Public Health Network; 2018.
- Footnote 552
-
Marmot, M, Allen, J, Boyce, T, Goldblatt, P, Morrison, J. Build Back Fairer in Greater Manchester: Health Equity and Dignified Lives. London, UK: Institute of Health Equity; 2021.
- Footnote 553
-
Marmot Indicators. Public Health England; 2015; Available from: https://fingertips.phe.org.uk/profile-group/marmot.
- Footnote 554
-
Marmot, M, Allen, J, Boyce, T, Goldblatt, P, Morrison, J. Build Back Fairer in Greater Manchester: Health Equity and Dignified Lives - Executive Summary. London, UK: Institute of Health Equity; 2021.
- Footnote 555
-
Health Equity in Greater Manchester: The Marmot Review 2020. Institute of Health Equity; 2020.
- Footnote 556
-
Michael Marmot and Jessica Allen: Building Back Fairer in Greater Manchester. The BMJ Opinion; 2021.
- Footnote 557
-
Bargain, O, Aminjonov, U. Trust and Compliance to Public Health Policies in Times of COVID-19. Journal of Public Economics. 2020; 192:104316.
- Footnote 558
-
Waters, E, Doyle, J, Jackson, N, Howes, F, Brunton, G, Oakley, A, et al. Evaluating the Effectiveness of Public Health Interventions: The Role and Activities of the Cochrane Collaboration. Journal of Epidemiology and Community Health. 2006; 60(4):285-9.
- Footnote 559
-
Frieden, TR. Six Components Necessary for Effective Public Health Program Implementation. American Journal of Public Health. 2013; 104(1):17-22.
- Footnote 560
-
Hyland-Wood, B, Gardner, J, Leask, J, Ecker, UKH. Toward Effective Government Communication Strategies in the Era of COVID-19. Humanities and Social Sciences Communications. 2021; 8(1):30.
- Footnote 561
-
Health Canada. What Is the Population Health Approach? Government of Canada; 2013.
Endnotes
- Endnote i
-
Based on 93% complete provisional information available, COVID-19 was the third most common cause of death (5%), following cancer (26%) and heart disease (17%).
- Endnote ii
-
This report will use the term “wave” to refer to significant resurgences of the virus.
- Endnote iii
-
These building blocks have been adapted for Canada’s public health systems from the World Health Organization’s (WHO) building blocks for health systems, which are used for monitoring health systems in many countries (PDF).
- Endnote iv
-
The Ottawa Charter for Health Promotion (1986) sets out fundamental conditions and resources for health. They are peace, shelter, education, food, income, a stable eco-system, sustainable resources, social justice, and equity. These basic prerequisites are foundational to improving health.

