Archived Evaluation of Healthcare-Associated Infection Activities at the Public Health Agency of Canada 2012-13 to 2016-17
Download the alternative format
(PDF format, 586 KB, 47 pages)
Organization: Public Health Agency of Canada
Published: March 2018
Prepared by
Office of Audit and Evaluation
Health Canada and the Public Health Agency of Canada
March 2018
Table of Contents
- Executive Summary
- Management Response and Action Plan
- 1.0 Evaluation Purpose
- 2.0 Program Description
- 3.0 Evaluation Description
- 4.0 Findings
- 5.0 Conclusions
- 6.0 Recommendations
- Appendix 1 – Description of PHAC's HAI Activities
- Appendix 2 – Logic Models
- Appendix 3 – Evaluation Description
- Appendix 4 – Citation Analysis
List of Tables
- Table 1: Program Expenditures ($M)
- Table 2: Limitations and Mitigation Strategies
- Table 3: Change of HAI Incidence Over Time
- Table 4: PHAC Surveillance Reports by Year of Publication and Year of Data Covered
- Table 5: PHAC Guidance Documents
- Table 6: Planned Spending and Expenditure
List of Acronyms
- AMR
- Antimicrobial Resistance
- AMU
- Antimicrobial Utilization
- CARSS
- Canadian Antimicrobial Resistance Surveillance System
- C. auris
- Candida auris
- CA-UTI
- Catheter-associated urinary tract infections
- CCDIC
- Centre for Communicable Diseases and Infection Control
- C. difficile
- Clostridium difficile
- CLABSI
- Central line-associated bloodstream infections
- CNISP
- Canadian Nosocomial Infection Surveillance Program
- CPE
- Carbapenemase-producing Enterobacteriaceae
- CPO
- Carbapenemase-producing organisms
- CRE
- Carbapenem-resistant Enterobacteriaceae
- CRGN
- Carbapenem-resistant gram-negative
- F/P/T
- Federal/provincial/territorial
- HAI
- Healthcare-associated infection
- IPC-EWG
- Infection Prevention and Control – Expert Working Group
- MERS-CoV
- Middle East respiratory syndrome coronavirus
- MRSA
- Methicillin-resistant Staphylococcus aureus
- NML
- National Microbiology Laboratory
- O&M
- Operations and Maintenance
- PHAC
- Public Health Agency of Canada
- USD
- United States dollars
- VRE
- Vancomycin-resistant Enterococci
Executive Summary
The purpose of this evaluation was to assess the relevance and performance of the Public Health Agency of Canada's (PHAC) healthcare-associated infection (HAI) activities. The evaluation covered guidance, surveillance, and outbreak response assistance activities provided by PHAC in relation to HAIs from April 2012 to September 2017. This first evaluation of HAI activities fulfills the requirements of the Treasury Board of Canada's Policy on Results (2016).
Program Description
The World Health Organization defines HAIs as “infections occurring in a patient during the process of care in a hospital or other healthcare facility, which were not present or incubating at the time of admission”.Endnote 1 Common types of HAIs include central line-associated bloodstream infections (CLABSI), catheter-associated urinary tract infections (CA-UTI), surgical site infections, and antimicrobial-resistant organism infections, such as Clostridium difficile infections (C. difficile), methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant Enterococci (VRE), and carbapenem-resistant gram negative (CRGN) infections. HAIs also include infectious diseases, such as severe acute respiratory syndrome, H1N1 flu, and Ebola hemorrhagic fever, that typically start in the community and are then spread within healthcare settings.Endnote 2
PHAC's HAI activities aim to reduce and prevent health risks related to HAIs. Overall, the activities carried out by PHAC can be categorized into three broad groups: surveillance, advice/guidance, and outbreak response assistance. Total expenditures for these activities approximate $3.4M per year.
Conclusions
Relevance of PHAC's HAI Activities
HAIs remain persistent in Canada but are often preventable. In fact, the World Health Organization identified HAIs as the most frequent adverse event in healthcare delivery worldwide. More than 200,000 patients are infected every year while receiving healthcare in Canada aloneEndnote 3 and the consequences of HAIs are significant. For example, C. difficile episodes that occurred in 2012 in Canada cost society approximately $281 million nationally.Endnote 4 As well, recent outbreaks of HAIs have underlined the need to monitor emerging threats. Such considerations illustrate the continued need for PHAC to prevent and reduce health risks related to those infections.
PHAC's HAI activities align with the Government of Canada priority to prevent and control infectious diseases. However, according to stakeholders interviewed for the evaluation, there is a lack of clarity about how PHAC prioritizes its HAI activities. Furthermore, PHAC's mandate for its HAI activities comes from overarching program and policy authorities that have not been updated since 2006. While the evaluation did not find any evidence of this affecting PHAC's ability to carry out its HAI activities, the context in which these activities are delivered is evolving with the emergence of antimicrobial resistance (AMR) as a global priority. Moreover, the lack of clarity around PHAC's priorities for HAI activities suggests a need to clearly articulate the mandate around these activities in order to ensure that PHAC's role in this area remains relevant.
PHAC has a role in the prevention and control of HAIs, although the area involves many players at the provincial, territorial, and national levels (e.g., provincial and territorial governments are responsible for the delivery of healthcare services in settings where patients are most likely to acquire HAIs). The majority of key informants interviewed mentioned that PHAC has a clear public health leadership role to conduct HAI surveillance, to provide evidence-based HAI guidance to healthcare and public health professionals, and to liaise with international partners, such as the World Health Organization. Moreover, the roles played by PHAC are generally well understood by external key informants. For the most part, the roles played by PHAC, the provinces and territories, and other organizations are complementary. There is, however, a potential for duplication of efforts in surveillance, as the Canadian Nosocomial Infection Surveillance Program's (CNISP) definitions for surveillance data collection and reporting are not necessarily consistent with those used by provinces and territories that have a surveillance system in place.
Performance
PHAC produces guidance and surveillance knowledge products in order to provide stakeholders with knowledge they can apply in their practice. During the evaluation period, PHAC produced many knowledge products, such as scientific publications, HAI surveillance reports, and infection prevention and control guidelines and tools. It also contributed to a range of learning opportunities (e.g., webinars, publications). The evaluation found some evidence that stakeholders use PHAC's HAI surveillance and guidance knowledge products. However, both the external key informants and a citation analysis conducted for the evaluation suggest that older guidance documents such as the 1999 and 2012 versions of Routine Practices and Additional Precautions for Preventing the Transmission of Infection in Healthcare Settings and the 2002 Prevention and Control of Occupational Infections in Health Care: An Infection Control Guide are used more often, as compared to documents issued in the last few years.
The majority of internal and external key informants also indicated that the potential use of PHAC's guidance and surveillance products is limited, due to the difficulties in accessing timely and up-to-date information. Key informants explained that, when they cannot find national level guidance or surveillance data from PHAC, they seek information from other provinces and territories, countries (e.g., the U.S. Centers for Disease Control and Prevention) and the World Health Organization. This creates challenges, as information from other sources is not necessarily applicable to the Canadian context. As well, several external key informants reported that the lack of timely guidance from PHAC could potentially create confusion, as national-level guidelines from PHAC may be inconsistent with those already developed by provinces and territories. A few key informants also noted that the lack of timeliness in releasing guidelines may undermine the credibility of PHAC's national leadership role.
The limited coverage of CNISP data was also seen as limiting the potential use of PHAC surveillance products. Currently, 65 acute-care hospitals (mostly tertiary) participate in CNISP. Although approximately 78% of the Canadian population lives within 100 kilometres of a CNISP hospital, several external key informants working in surveillance and guidance noted that CNISP lacks community, rural, and northern hospital data. They mentioned that including these hospitals and healthcare facilities would provide a more complete picture of HAIs across Canada.
Demonstration of Economy and Efficiency
PHAC HAI activities represent approximately $3.4M per year in expenditures. For the years 2015-16 to 2016-17, approximately $1M a year was spent on guidance, $1.6M a year on surveillance activities and the remaining expenditures were split between antimicrobial resistance (AMR) coordination, the National Microbiology Laboratory for CNISP, and the Canadian Antimicrobial Resistance Surveillance System. Over the past five years, expenditures for guidelines were either close to being entirely spent or exceeded planned budget. Expenditures for CNISP surveillance were consistently underspent in part due to fewer staff than planned.
PHAC carries out many of its HAI activities by leveraging expertise through CNISP and other collaborations, many of whom volunteer their time in order to provide PHAC with valuable expert advice.
Recommendations
Recommendation 1
Clearly articulate the Public Health Agency of Canada's (PHAC) role and priorities for HAI activities and communicate those to stakeholders.
Considering that policy and program authorities for PHAC's HAI activities have not been updated since 2006 and considering the lack of clarity around PHAC's priorities for its HAI activities, there is an opportunity to articulate what role PHAC could assume in the HAI area, and where it should prioritize its activities. This would help ensure that PHAC's role remains relevant. There is also a need to clearly communicate those priorities with stakeholders.
Recommendation 2
Explore options to improve program effectiveness and efficiency, focusing on improving: a) the timeliness of surveillance and guidance knowledge products and b) the coverage of Canadian Nosocomial Infection Surveillance Program (CNISP) surveillance data.
There is an opportunity to explore options for improving the timeliness of guidance and surveillance products. In this regard, the evaluation identified a few options, such as establishing a mechanism to endorse existing provincial and territorial guidelines where appropriate, streamlining the approval process for low-risk surveillance products, and exploring opportunities to use the Canadian Network for Public Health Intelligence platform to expand CNISP. There is also an opportunity to examine options to increase representativeness within CNISP to help ensure the continued usefulness of PHAC's surveillance data.
Management Response and Action Plan
| Recommendations | Response | Action Plan | Deliverables | Expected Completion Date | Accountability | Resources |
|---|---|---|---|---|---|---|
Clearly articulate PHAC's role and priorities for HAI activities and clearly communicate those to stakeholders. |
Management agrees with the recommendation. |
Organize a facilitated workshop to engage PHAC program and policy areas involved in HAI surveillance, guidance and laboratory activities on:
|
Facilitated workshop Facilitator's report of the workshop results Internal document detailing PHAC's role and priorities Stakeholder Engagement Plan including mechanisms for an F/P/T community of practice |
October 31, 2018 December 31, 2018 March 31, 2019 March 31, 2019 |
VP |
Utilise resources from within CCDIC; |
Explore options to improve program effectiveness and efficiency. In particular, examine options to improve the timeliness of surveillance and guidance knowledge products and the coverage of CNISP surveillance data. |
Management agrees with the recommendation. |
Include discussions and analyses around efficiencies and effectiveness in facilitated workshop under recommendation 1 above. |
Internal document detailing PHAC's role and priorities with recommendations for improving program effectiveness and efficiency, including timeliness of products |
March 31, 2019 |
VP |
Utilise resources from within CCDIC and the contract with external services identified under recommendation 1 |
1.0 Evaluation Purpose
The purpose of this evaluation was to assess the relevance and performance of the healthcare-associated infection (HAI) activities conducted by the Public Health Agency of Canada (PHAC) during the period of 2012-13 to 2016-17.
The evaluation was required by the Treasury Board of Canada's Policy on Results (2016). This is the first departmental evaluation of PHAC's HAI activities.
2.0 Program Description
2.1 Program Context
In 2002, the World Health Organization released a guide containing recommendations for the implementation of infection control programs,Endnote 5 including surveillance, in healthcare settings to prevent the occurrence and spread of HAIs.
The World Health Organization recognizes HAIs as a public health problem and defines them as “infections occurring in a patient during the process of care in a hospital or other health care facility that were not present or incubating at the time of admission”.Endnote 6 These infections can affect patients in any type of healthcare setting where they receive care, and can also appear after discharge. In addition, they include occupational infections among healthcare staff. One or multiple factors leading to increased risk of developing HAIs include advanced age, underlying illness, complex treatment modalities, the emergence of novel infectious agents, the emergence of community-associated communicable diseases, MRSA, C. difficile, the prevalence of antibiotic-resistant organisms, and international travel.
Types of HAIs
Common types are:
- Central line-associated bloodstream infections (CLABSI)
- Catheter-associated urinary tract infections (CA-UTI)
- Surgical site infections
HAIs include those caused by antimicrobial-resistant organisms such as:
- Clostridium difficile (C. difficile),
- Methicillin resistant staphylococcus aureus (MRSA),
- Vancomycin-resistant enterococci (VRE)
- Carbapenem-resistant gram negative (CRGN) bacteria
HAI also include infectious diseases that start in the community and spread in healthcare settings such as
- Severe acute respiratory syndrome,
- Middle East respiratory syndrome
In Canada, the bodies involved in preventing and controlling HAIs include federal departments and agencies, provincial and territorial governments and health authorities, local and municipal governments, national professional associations, non-governmental organizations, and healthcare settings, such as acute-care hospitals, ambulatory surgical centres, dialysis facilities, outpatient establishments, long-term care facilities, and home care. While each jurisdiction, agency, authority, non-governmental organization, and professional association has its own role, the activities of these bodies rely on collaboration and coordination of efforts.
2.2 Program Profile
PHAC's HAI activities aim to prevent and control the spread of infectious diseases by protecting people living in Canada from communicable diseases acquired in community and healthcare settings.
PHAC HAI activities are conducted by the Centre for Communicable Diseases and Infection Control and the National Microbiology Laboratory (NML) in the Infectious Disease Prevention and Control Branch. These activities can be categorized into three broad groups: surveillance, advice/guidance, and outbreak response assistance. A detailed description is provided in Appendix A.
Through existing resources, including its HAI activities, PHAC provides program-specific expertise, supporting the development of a pan-Canadian framework and antimicrobial resistance (AMR) infection prevention and control action plan.
Surveillance
PHAC develops, collects, analyzes, and disseminates HAI surveillance data to monitor trends in rates, strain types and antimicrobial resistance, to provide early detection of new organisms, and to monitor severe causes of morbidity and mortality during an outbreak. PHAC also provides national reference laboratory services for outbreak investigations and surveillance, and engages in research activities targeted at reducing the impacts of pathogens (e.g., AMR).
The Canadian Nosocomial Infection Surveillance Program (CNISP) is PHAC's main surveillance mechanism to track and monitor infections transmitted in healthcare settings, including antimicrobial-resistant organisms. CNISP is a sentinel surveillance program that funds targeted acute-care hospitals to track and monitor specific healthcare associated infections.
The Canadian Antimicrobial Resistance Surveillance System (CARSS), which uses targeted surveillance of identified priority antimicrobial organisms, also contributes to surveillance in the area of HAIs. CARSS provides an integrated picture of AMR and antimicrobial use in Canada based on data from PHAC's surveillance systems and laboratory reference services. It uses data to develop an overall picture of AMR and antimicrobial utilization (AMU), and works with domestic and international scientific experts and health professionals to monitor global trends and impacts.
Advice/guidance
PHAC provides advice in the development of infection prevention and control guidance and guidelines for Canadian healthcare settings. Guidelines, by definition, include principles and recommendations based on research and evidence, and do not represent rigid standards.
PHAC's Infection Control Guideline Series includes specific reference documents such as the Routine Practices and Additional Precautions for Preventing the Transmission of Infection in Healthcare Settings (2013 revision) and the Hand Hygiene Practices in Healthcare Settings (2012).
Outbreak Response Assistance
PHAC also provides technical support and advice in various capacities in the event of outbreaks, or the emergence or re-emergence of infections that may directly or indirectly affect or occur in healthcare settings (e.g., development of guidelines on Ebola).
Overall, through these three areas of activity, PHAC generates evidence-based information on the prevention and control of HAIs that stakeholders can apply in their practice. Stakeholders include federal, provincial, and territorial governments, public health authorities, healthcare providers, and non-governmental organizations.
2.3 Program Resources
As shown in Table 1 below, expenditures for PHAC HAI activitiesFootnote i totalled $16.77M over the years 2012-13 to 2016-17.
| Year | O&M | Salary | Total |
|---|---|---|---|
| 2012-13 | 0.97 | 2.14 | 3.11 |
| 2013-14 | 1.11 | 1.97 | 3.09 |
| 2014-15 | 1.24 | 2.20 | 3.43 |
| 2015-16 | 0.99 | 2.57 | 3.57 |
| 2016-17 | 1.07 | 2.63 | 3.68 |
| Total | 5.35 | 11.51 | 16.70 |
|
|||
3.0 Evaluation Description
3.1 Evaluation Scope, Approach and Design
The evaluation covered the period from April 2012 to September 2017. It included the following Public Health Agency of Canada (PHAC) HAI activities:
- development of infection prevention and control guidance and guidelines for Canadian healthcare settings;
- advice in the development of policy;
- partnerships and other products (e.g., awareness);
- development, collection and dissemination of surveillance information;
- HAI laboratory-related services and research provided by PHAC; and
- AMR-related HAI activities.
The evaluation did not examine activities that are the responsibility of other jurisdictions (e.g., provincial and territorial responsibility for hospitals).
The evaluation examined questions pertaining to the relevance and performance of HAI activities, as shown in Appendix 3. Data for the evaluation were collected using various methods, including a review of program documents, files, literature, media articles, financial data, and performance measurement data. As well, 42 key informant interviews were conducted with PHAC staff and management, CNISP hospitals, professional associations, non-governmental organizations, and academia. Of these, just over a quarter were affiliated with PHAC's advice/guidance activities (see Appendix 3 for more information).
Data were analyzed by triangulating information gathered from the different methods listed above. The use of multiple lines of evidence and triangulation were intended to increase the reliability and credibility of the evaluation findings and conclusions.
3.2 Limitations and Mitigation Strategies
The following table outlines the limitations encountered during the implementation of the methods selected for this evaluation. Also noted are the mitigation strategies put in place to ensure that the evaluation findings can be used with confidence to guide program planning and decision making.
| Limitation | Impact | Mitigation Strategy |
|---|---|---|
| Key informant interviews are retrospective in nature. | As interviews are retrospective in nature, this may lead to the provision of recent perspectives on past events. This can impact the validity of assessing activities or results relating to improvements in the program area. | Triangulation of other lines of evidence to substantiate or provide further information on data received in interviews. |
| Access to information for the citation analysis was limited to publicly available information on the internet and the evaluators did not have access to the members-only site or resources sections. | It is possible that not all provincial and territorial guidance documents were available online. Therefore, other guidance products may be more predominantly citied in members-only sites or resources sections. | Results from the citation analysis provide a conservative assessment of the use of PHAC's guidance documents by provinces and territories. |
| Lack of systematically tracked performance measurement data. | Performance data available to evaluate outcomes over time are limited. | Interviews and document reviews were used as main line of evidence of this evaluation and were supplemented with performance information available in some areas (e.g., webinar surveys, report user surveys). |
4.0 Findings
4.1 Relevance
4.1.1 Needs Addressed by PHAC's HAI Activities
There is a continued need for PHAC's HAI activities, as preventable HAIs remain persistent in Canada. HAIs result in prolonged hospital stays, increased resistance to antimicrobials, increased morbidity and mortality, and significant financial burden. There is also a need for PHAC to prepare for, and support, responses to emerging infectious diseases that have HAI infection prevention and control components.
Prevalence and Incidence of HAIs
According to the World Health Organization, HAIs are the most frequent adverse event in healthcare delivery worldwide. HAIs are also prevalent in Canada as more than 200,000 patients get infected every year while receiving healthcare.Endnote 7 Compared to 11 other developed countries, the World Health Organization identified Canada as having the highest national prevalence of HAIs in 2008 at 11.6%. This means that 1 in 12 adults and 1 in 10 children admitted to a Canadian hospital had developed a HAI.Endnote 8 In comparison, the prevalence rate in the United States was 4.5%.Endnote 9
In Canada, it is estimated that surgical site infections affect 26,000 to 65,000 patients annually.Endnote 10 The national incidence rates vary across other common types of HAIs. As shown in Table 3, some rates have decreased, while others have increased over the years. For example:
| Healthcare-associated C. difficile | Decreased from 6.64 cases per 10,000 patient-days in 2011 to 4.05 cases per 10,000 patient-days in 2016.Endnote 11 |
|---|---|
| Methicillin-resistant Staphylococcus aureus (MRSA) | Increased in sentinel hospitals from 2.84 to 3.13 cases per 10,000 patient-days between 2011 and 2016.Endnote 12 |
| Vancomycin-resistant Enterococci (VRE) | Decreased from 2012 with 0.61 cases per 10,000 patient-days to 0.41 cases per 10,000 patient-days in 2015 and then, increased slightly in 2016 with 0.44 cases per 10,000 patient-days.Endnote 13 |
| Carbapenemase-producing Enterobacteriaceae (CPE)Footnote ii and other carbapenemase-producing organisms | Globally, infections have increased over time. However, the rates of CPE infections in sentinel Canadian hospitals have remained low and relatively stable (e.g., varied between 0.007 cases per 10,000 patient-days and 0.013 cases between 2011 and 2015.Endnote 14) |
While in any healthcare setting a patient may develop an HAI, these infections are more likely to affect vulnerable individuals. These include the elderly, the very young, critical care patients, and those who are immune-compromised. In addition, those who are being treated with immune-suppressing drugs, as well as those who have had previous antimicrobial-resistant infections, are considered vulnerable populations.Endnote 15
Burden of HAIs
AMR, in general, represents a significant cost to society. The United Kingdom Review on AMR stated that unless action is taken to address global AMR, there will be an additional 10 million lives lost annually by 2050. As well, by that year, annual deaths due to AMR could reach 317,000 in North America alone and 10 million worldwide, overtaking deaths due to diabetes and cancer combined. The potential financial burden of AMR could represent a cumulative cost of at least $100 trillion (USD).Endnote 16
HAIs alone also constitute a significant burden to society, as they cause significant morbidity and mortality in hospitalized patients. In Canada, researchers have estimated that HAIs are linked to between 8,500 and 12,000 deaths per year, making these infections the fourth leading cause of death for Canadians (behind cancer, heart disease, and stroke), which is up from the eleventh leading cause it was two decades ago.Endnote 17 As well, HAIs result in important costs for the healthcare system. As an example, there were an estimated 37,900 C. difficile episodes in Canada in 2012, resulting in an estimated cost of $281 million. Of this amount, 92% ($260 million) was in-hospital costs while 4% ($12 million) was direct medical costs for the community, and 3.5% ($10 million) was for costs related to lost productivity. Management of C. difficile relapses alone accounted for $65.1 million (23%).Endnote 18
After discharge, patients with HAIs have significantly higher personal medical costs than uninfected patients. They require more visits from community nurses, greater reliance on hospital outpatient and emergency services, and more visits to their family doctor.Endnote 19
Consistent with the significant burden HAIs represent for society, they are also an issue of public concern, as suggested by a media review, which found 465 news articles published over the past two years on C. difficile and MRSA alone. A number of the articles reviewed highlight a continuing concern about the incidence of bacterial infection and the challenges posed by AMR. Many of the articles also focus on infection prevention and control to prevent the spread of MRSA.
HAIs are Preventable
Much of the suffering and death caused by HAIs could be reduced, as these infections are a major, yet often preventable, threat to patient safety.Endnote 20 Researchers estimated that about 70% of some types of HAIs could reasonably be prevented if infection prevention and control strategies were followed. Reports have also stated that health care workers, patients and visitors spread about 80% of common infections. Overall, best practices in preventing infection can reduce the risk of some infections to close to zero.Endnote 21
Emerging Threats
Recent outbreaks of HAIs have underlined the need to continue work in this area and to monitor emerging threats. Infection prevention and control experts are aware that another outbreak of an emerging pathogen is inevitable. For example, Candida auris (C. auris) has emerged as a global threat to public health. First discovered in Japan in 2009, Candida auris is a multi-drug resistant emerging fungal infection that can cause invasive HAIs, bloodstream infections, wound infections, and inflammation of the ear. Its mode of transmission is unknown. C. auris has since been reported in 17 countries, with the first Canadian case reported in May 2017.Endnote 22 The U.S. Centers for Disease Control and Prevention estimates that the mortality rate from C. auris ranges from 30 to 60%.Endnote 23
The World Health Organization reported that antimicrobial resistance is an increasingly serious threat to global public health that requires action across all government sectors and society. More than 50% of HAIs are caused by bacteria that are resistant to at least one type of antibiotic.Endnote 24
4.1.2 Alignment with Government Priorities
PHAC's HAIs activities align with Government of Canada priorities that focus on health promotion, and the prevention and control of infectious diseases and AMR, including activities to prevent its occurrence and spread.
As outlined in a number of strategic documents, health promotion, and the prevention and control of infectious diseases, have been priorities for the Government of Canada for many years. For example, Speeches from the Throne,Endnote 25,Endnote 26 as well as the Minister of Health's Mandate LetterEndnote 27 have indicated that the health and safety of Canadians is a priority for the Government of Canada. Reports from the Auditor General have identified the importance of infectious disease surveillance and the risks of AMR.Endnote 28,Endnote 29 In 2014, the Government of Canada released Antimicrobial Resistance and Use in Canada: A Federal Framework for Action,Endnote 30 followed by the Federal Action Plan on Antimicrobial Resistance and Use in Canada in 2015.Endnote 31 Both of these incorporate a multi-departmental approach to dealing with AMR.
PHAC and the Government of Canada have international obligations to reduce and prevent health risks related to HAI and AMR. The World Health Organization identified effective infection prevention and control as a key action for dealing with AMR. It also noted the importance of infection prevention and control to achieve the United Nations Sustainable Development Goal on health.Endnote 32> As a member state of the World Health Organization, Canada has signed on to the Global Action Plan on Antimicrobial Resistance.Endnote 33 Leaders at the 2017 G20 summit agreed that AMR is a priority,Endnote 34 and prior to the summit, health ministers from G20 countries identified AMR as a critical issue in the Berlin Declaration of the G20 Health Ministers.Endnote 35 Canada is also one of the leading countries of the Global Health Security Agenda Antimicrobial Action Package, whose five-year target includes strengthened surveillance and conservation of existing antimicrobial medications.Endnote 36
PHAC's strategic plansEndnote 37 identify priorities around strengthening science leadership through surveillance and laboratory work, and leadership on disease prevention by providing governments and health providers with guidelines to support decision making. For example, PHAC has been the lead on the development of the Pan-Canadian Antimicrobial Framework.Endnote 38 As part of its priority for leadership and for health promotion and disease prevention, PHAC will release the Framework and develop an action plan on AMR.Endnote 39
Overall, PHAC's priorities align with Government of Canada priorities to promote the health of Canadians and prevent and control infectious diseases.Endnote 40,Endnote 41 As well, PHAC-specific HAI surveillance, guidance, and AMR activities align with these priorities. However, the evaluation found that there is a lack of clarity on how PHAC prioritizes its HAI activities, and a number of key informants noted that PHAC does not have a strategic plan for these activities. Some key informants explained that having a strategic plan could allow PHAC to be proactive, rather than reactive. As well, it would provide direction on which area of guidance and surveillance should be prioritized.
4.1.3 Federal Roles in the HAI Area
Preventing and controlling HAIs is an area of shared jurisdiction. Provincial and territorial governments are responsible for hospitals, long-term care facilities, and home care facilities; in other words, those healthcare settings where patients are most likely to acquire HAIs. However, the evaluation found evidence that PHAC has a clear public health leadership role to conduct HAI surveillance, and provide evidence-based HAI guidance to healthcare and public health professionals.
Mandate for HAI Activities
Legislative, policy, and program authorities establish the role for PHAC's HAI activities. These activities are aligned with the Minister's legislative authority under the Department of Health Act (1996) and the Public Health Agency of Canada Act (2006), which established PHAC for the purpose of assisting the Minister of Health in exercising or performing the Minister's powers, duties, and functions in relation to public health. More specifically, PHAC has a legislative mandate to protect Canadians against risks to health and the spread of diseases, conduct investigations and research into public health, including disease monitoring, and cooperate with provincial authorities to improve public health.Endnote 42,Endnote 43
PHAC has policy and program authorities to detect, diagnose and respond to infectious disease threats and coordinate public health efforts across jurisdictions by conducting the following activities:
- updating surveillance guidelines;
- drafting and maintaining guidelines for infection control and hospital-based surveillance;
- conducting surveillance of multi-drug resistant organisms; and
- using laboratory technology to define emerging and re-emerging infectious diseases.
HAI activities align with PHAC's mandate to decrease the incidence and transmission of communicable diseases and infections, such as HAIs, through targeted prevention, control, support, and research activities.Endnote 44 Finally, PHAC also has a mandate to liaise with key international organizations, such as the World Health Organization, the Pan American Health Organization and the U.S. Centers for Disease Control and Prevention. In particular, as a World Health Organization member state, Canada works to further progress in the World Health Organization priority areas of infection prevention and control, and AMR.
The mandate for providing HAI guidance and surveillance partly comes from policy and program authorities that date or pre-date PHAC's creation. This provides general overarching authority regarding control of infectious diseases, through guidance and surveillance, coordination across jurisdictions, and liaison with international partners. The mandate for targeted surveillance around one precise respiratory related HAI infection was also provided in 2006. Overall, although HAI guidance and surveillance align with PHAC's mandate, there are no specific or recent authorities regarding HAI activities. The evaluation did not find evidence of this affecting PHAC's ability to carry out its HAI activities. However, the context in which HAI activities are delivered is evolving with the emergence of AMR as a global priority, among other factors. Furthermore, the evaluation did find a lack of clarity around PHAC's priorities for its HAI activities. This suggests a need to clearly articulate the mandate around those activities, in order to ensure PHAC's role in this area remains relevant.
Clarity and Need Identified for a Federal Role in HAIs
Although there are many players in this area, most internal and external key informants identified clear roles for PHAC in the prevention and reduction of health risks related to HAIs. A few internal key informants have a different view when it comes to this role, stating that it might not be part of PHAC's mandate.
Most internal and external key informants also identified a need for PHAC to assume a role in HAI surveillance, and infection prevention and control guidelines development, such as:
- Providing national-level leadership in bringing together and supporting provinces and territories;
- Providing national-level aggregate surveillance data of ongoing and emerging HAIs, which is then used by provinces, territories, and hospitals for benchmarking purposes;
- Providing common case definitions for the entire country;
- Providing a national picture of infection prevention and control guidance;
- Supporting response to emergency outbreaks;
- Communicating a national strategy for preventing and controlling HAIs; and
- Liasing with international organizations such as the World Health Organization, the U.S. Centers for Disease Control and Prevention, and the Pan American Health Organization.
The evaluation found evidence that PHAC currently provides aggregate surveillance data, national guidelines, outbreak response assistance, and liaises with international partners. Several external key informants noted that PHAC could enhance its activities to provide national leadership, a national strategy, common case definitions, and pan-Canadian surveillance data.
Some external key informants noted that PHAC's guidelines are a trusted source of information because they are informed by, and take into account, international evidence.
Roles of PHAC and Other Health Organizations
HAI is an area of shared responsibility between federal, provincial, and territorial governments, as well as other national stakeholder organizations who are active in infection prevention and control. The potential for duplication is mitigated by the focus of each organization's work and the partnerships between PHAC and its stakeholders. For example:
- Both the Association of Medical Microbiology and Infectious Disease Canada and Infection Prevention and Control Canada promote best practices among their members who are infectious disease and infection control professionals. Infection Prevention and Control Canada distributes PHAC knowledge products and provides education and networking for its members. It relies on PHAC to provide national guidelines for its members to use in their practices.
- The Canadian Patient Safety Institute is focused on infection prevention and control, but its mandate is much broader, and includes all aspects of patient safety.
Furthermore, the evaluation found that PHAC and its stakeholder organizations have established partnerships to ensure that there is no duplication of efforts. In November 2014, the Canadian Patient Safety Institute and PHAC co-hosted a national Infection Prevention and Control Summit. This Summit brought together HAI experts and stakeholders, and resulted in the Infection Prevention and Control Canada Action Plan. One of the goals of this Action Plan was to look at ways to have more pan-Canadian surveillance data. In particular, the Canadian Institute for Health Information collects administrative data based on discharge summaries across most healthcare facilities in Canada, including local surveillance data. To that end, PHAC and other national organizations, including the Canadian Patient Safety Institute, and the Canadian Institute for Health InformationFootnote iii, have held meetings to identify the capabilities of PHAC's CNISP surveillance system and Canadian Institute for Health Information's data systems.Endnote 45
External key informants expressed a clear understanding of the roles of the Association of Medical Microbiology and Infectious Disease Canada, and Infection Prevention and Control Canada, regarding CNISP. CNISP itself is a collaborative effort between PHAC and the Canadian Hospital Epidemiology Committee, which is a steering committee of the Association of Medical Microbiology and Infectious Disease Canada.
Within the Health Portfolio, a few internal and external key informants expressed confusion over the roles of Health Canada and PHAC regarding contaminated medical devices that transmit infections during medical or surgical procedures. In 2016-17, there was an outbreak of Mycobacterium chimaera (M. chimaera) in heater/cooler devices used during cardiac surgery, which was primarily related to the design of the devices. While Health Canada was leading on device mitigation actions, including recommendations to hospitals that were using the devices, there was some confusion as to whether or not the outbreak was considered a public health threat, and if PHAC should have been supporting provinces and territories in preventing and controlling M. chimaera. In the end, discussions were held among various stakeholders to clarify the role PHAC had to play in the outbreak.
Duplication and Complementarity Between PHAC's and Provincial and Territorial Activities
Provincial and territorial governments are responsible for the delivery of healthcare services in healthcare settings where patients are most likely to acquire HAIs and, although both internal and external key informants noted a PHAC role in HAI surveillance, there is the potential for duplication of efforts. In particular, many provinces and territories have mandated hospitals to report on HAIs by providing surveillance data directly to PHAC through CNISP, but also to their individual provincial or territorial government. This adds extra work for the hospitals, especially if different case definitions are used at the federal and provincial or territorial levels. That being said, according to a few external key informants, some provinces and territories may not have a surveillance system as well established as others.
Many provinces and territories take PHAC guidelines and either adopt them as is, or adapt them based on local conditions and risks. However, PHAC's HAI guidelines may take years to develop and release and, as a result, are not issued in a timely manner. Provinces that have the capacity to develop their own guidelines are often able to do so before PHAC can releases its own guidelines. This could lead to a potential duplication or contradiction with provincial and territorial guidelines. As well, a few key informants noted that the lack of timeliness in releasing guidelines may undermine PHAC's credibility in assuming its national leadership role.
Overall, the need for national-level leadership on HAI surveillance and guidance is clear. However, there are no recent and specific authorities for PHAC HAI activities. While the roles of provinces and territories and non-governmental organizations are clear, the role of the Canadian Patient Safety Institute and the Canadian Institute for Health Information in HAI surveillance is less clear to external stakeholders. Furthermore, there is a potential for duplication with provincial and territorial surveillance and guidance activities.
4.2 Performance
4.2.1 Stakeholders Have and Use Knowledge to Prevent Healthcare-Associated Infections
PHAC produces many HAI surveillance and guidance knowledge products and contributes to a range of learning opportunities (e.g., webinars, publications). Some external key informants noted that PHAC's activities have increased their knowledge of HAIs, while others could not say this was the case due to a lack of awareness of PHAC products and challenges in accessing the information.
PHAC Knowledge Products
PHAC produces knowledge products for provinces and territories, public health authorities, healthcare providers, and non-governmental organizations to increase stakeholders' understanding of HAIs in Canada. As shown in Tables 4 and 5 on the following page, between 2012 and 2017, PHAC published a number of surveillance reports and related products, as well as a variety of guidance documents.
In addition to these key products, PHAC contributes to a number of publications, such as academic journal articles, and conducts literature reviews for emerging issues. For example, PHAC has contributed to approximately 100 HAI-related publications since 2012 covering the following infections among others: AMR, CPE, Carbapenem-resistant Enterobacteriaceae (CRE), MRSA, and C. difficile. CNISP has contributed to over 260 HAI-related scientific publications such as C. difficile, CPE, carbapenem-resistant gram negative (CRGN), influenza, MRSA, surgical site infections, and VRE, among others. In addition, PHAC's guidance group contributed to several publications, such as its infection control guideline series.
PHAC also conducts webinars upon release of reports or guidelines, and for Antibiotic Awareness Week, such as the Critical Appraisal Toolkit, Stop! Clean Your Hands Day, Middle East respiratory syndrome coronavirus (MERS-CoV), Routine Practices and Additional Precautions, AMR Awareness Week, and the Canadian Antimicrobial Resistance Surveillance System (CARSS).
Surveillance and Guidance Products Released by PHAC from 2012 to 2017
| Surveillance Documents with Year of Data Covered in the Documents | Year Published | |||||
|---|---|---|---|---|---|---|
| 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | |
| CARSS reports | 2015 | 2016 | 2017Footnote a | |||
| Antimicrobial-resistant organism reports | 2009-14 | 2011-15 | ||||
| Antimicrobial-resistant organism Infographic | 2016 | |||||
| MRSA Surveillance report | 2008-12 | |||||
| CRGNB Surveillance report | 2010-12 | |||||
| C-Difficile Surveillance report | 2007-12 | |||||
| CA-BSI Surveillance report | 2006 & 2009-11 | |||||
| VRE Surveillance Report | 1999-2011 | |||||
|
||||||
| Guidance Documents | Year Published |
|---|---|
| Infection Prevention and Control Measures for Prehospital Care and Ground Transport of Patients with Suspected or Confirmed Ebola Virus Disease | 2017 |
| Mycobacterium chimaera infections in post–operative patients exposed to heater-cooler devices: An overview | 2017 |
| Summary assessment of public health risk associated with Mycobacterium chimaera infections in patients exposed to heater-cooler devices in Canada | 2017 |
| Infection Prevention and Control Guidance for Middle East Respiratory Syndrome Coronavirus (MERS-CoV) in Acute Care Settings | 2016 |
| Notice: Recommended practices for the prevention of endoscopy-related infections | 2016 |
| Poster: Help Reduce the Spread of Antimicrobial Resistance | 2016 |
| Infection Prevention and Control Expert Working Group: Advice on Infection Prevention and Control Measures for Ebola Virus Disease in Healthcare Settings | 2015 |
| Infection Prevention and Control Expert Working Group: Advice on the Management of Ebola Virus Disease-associated Waste in Canadian Healthcare Settings | 2015 |
| Infection Prevention and Control Guidelines: Critical Appraisal Tool Kit | 2014 |
| Routine Practices and Additional Precautions for Preventing the Transmission of Infection in Healthcare Settings | 2013 |
| Routine Practices and Additional Precautions Assessment and Educational Tools | 2013 |
| Seasonal Influenza – Infection Prevention and Control Guidance for Management in Home Care Settings | 2012 |
| Hand Hygiene Practices in Healthcare Settings | 2012 |
Dissemination of Surveillance and Guidance Products
HAI-related knowledge products are disseminated through presentations at several conferences and workshops. For example, PHAC previously hosted booths at stakeholder conferences to highlight its HAI work. However, internal key informants reported that this has not taken place in recent years and believed that this could affect the visibility of PHAC at national conferences, and its ability to interact with the community of practice. PHAC has also participated in other opportunities to share HAI knowledge. The most recent examples are as follows:
- In 2014, PHAC participated in Cool Science Saturday at the Canada Science and Technology Museum by setting up two interactive booths to raise awareness on hand hygiene, and to demonstrate how infectious diseases are handled safely in laboratories.
- In August 2014, PHAC participated in a delegation visit from the Kingdom of Saudi Arabia that was dealing with a MERS-CoV outbreak. The delegation met with experts from across different levels of government to learn about Canada's experience in responding to the severe acute respiratory syndrome. This provided an opportunity for Saudi Arabian and Canadian experts to share ideas, best practices, and lessons learned.
In addition to sharing surveillance products via the Canadian Network for Public Health Intelligence platform, knowledge is also exchanged through various working groups and collaborations, including CNISP face-to-face and working group meetings, Infection Prevention and Control – Expert Working Group (IPC-EWG) meetings and various guideline development working groups. Working group face-to-face meetings were seen by almost all external key informants as a valuable way to exchange knowledge.
Knowledge products are posted on the canada.ca website. Social media, such as Twitter and Facebook, have also been used in recent years to promote Antibiotic Awareness Week, which takes place every November, and coincides with the World Health Organization's World Antibiotic Awareness Week.
Overall, PHAC has produced a range of surveillance and guidance products to provide stakeholders with evidence-based information they can apply in their practice. As further discussed below, it is not clear whether these products have increased stakeholders' knowledge, but there is evidence that such products are valued and used to some extent.
Increase in Stakeholders' Knowledge
External key informants (federal, provincial, and territorial representatives, public health authorities, healthcare providers, and non-governmental organizations) working in both surveillance and guidance were mixed in their perception that PHAC's surveillance and guidance activities have increased their knowledge. Some said that their knowledge has increased through CNISP and PHAC's guidelines, while others said that they were not really aware of PHAC's products, nor could they say that their knowledge had increased as a direct result of PHAC's activities. A few external key informants working in both surveillance and guidance mentioned that HAIs are the focus of their work and, as such, they were not sure if PHAC is responsible for increasing their knowledge, indicating that they themselves share a great deal of knowledge and expertise with PHAC.
The lack of awareness of PHAC knowledge could be due to difficulty in finding them online. In this regard, external key informants working in both surveillance and guidance were of mixed opinion on the ease of access to the PHAC website, with a few stating the documents are easy to find, while others noted that the migration to canada.ca has made it difficult to find documents. The migration to canada.ca has led to confusion among some external stakeholders, because they either cannot find documents, or once found, they are unsure as to who produced the document (i.e., Government of Canada, Health Canada, or PHAC).
As previously mentioned, PHAC conducts webinars upon the release of reports and guidelines. While the majority of stakeholders indicated in the webinar feedback forms that they had learned something new by participating in the webinar, the proportion of respondents who responded positively to such statements varied (from 59% to 94%), which supports findings from key external informants on their mixed perception of the impact of PHAC's activities on increasing knowledge.
A few internal and external key informants stated that PHAC could do more to increase its knowledge translation activities, such as providing a one-page infographic to accompany the larger guidelines documents for healthcare practitioners, as they may not have the time to refer to the full guideline. While there is a recognized need to develop and disseminate PHAC's infection prevention and control guidelines to support dissemination and uptake of evidence-based recommendations, there is an opportunity for PHAC to engage with other organizations, such as the Association of Medical Microbiology and Infectious Disease Canada, the Canadian Patient Safety Institute, Infection Prevention and Control Canada and the National Collaborating Centre for Infectious Diseases, who focus on knowledge translation.
Use of Knowledge Products by Stakeholders
While it is not clear whether PHAC's products have increased stakeholders' knowledge, the evaluation found evidence that PHAC's surveillance, webinars, other knowledge products, and guidance documents are useful to stakeholders.
Internally, CNISP data are used to help inform PHAC's HAI guidelines. Almost all external key informants noted that CNISP data are used by participating CNISP hospitals, provinces, and territories as a benchmark to compare themselves with others across Canada. CNISP data is also used by a few external key informants to teach college and university courses aimed at infection control practitioners. Some external key informants noted that they use the network of CNISP hospitals as an expert resource, asking questions as they arise.
Surveys conducted internally to measure the use of various PHAC HAI knowledge products confirm what was reported by key informants. For example, in 2011, PHAC released a CNISP MRSA Surveillance Report (1995-2009). Its use was evaluated in 2012-13 via a survey completed by 188 hospitals (out of the 553 that received it). Of the respondents who had accessed the report (n=138 hospitals), almost three quarters reported using the information, mostly as a benchmark.
Webinars conducted upon the release of surveillance reports and guidelines are also generally very well-received by participants. Specifically, between 86% and 100% of respondents found the material presented in the webinars useful for their work (e.g., as reference material, in preparation for meetings or briefings, and to share with healthcare practitioners).
The evaluation also found evidence that many external key informants use infection prevention and control guidelines to develop their own jurisdictional guidance, based on local conditions and risks. In particular, external key informants working in both surveillance and guidance reported using the following PHAC guidelines:
- Infection Prevention and Control Expert Working Group: Advice on Infection Prevention and Control Measures for Ebola Virus Disease in Healthcare Settings (2015);
- Routine Practices and Additional Precautions for Preventing the Transmission of Infection in Healthcare Settings (2013);
- Hand Hygiene Practices in Healthcare Settings (2012); and
- Prevention and Control of Occupational Infections in Health Care (2002).
As well, a citation analysis found that the documents mentioned above, with the exception of the Ebola guidelines, which were not included in the citation analysis, are the most frequently referenced on provincial/territorial websites (see Appendix 4 for further information about the analysis, including a list of documents examined). Each of these three documents are referenced by eight or nine provinces as listed below:
- Routine Practices and Additional Precautions for Preventing the Transmission of Infection in Healthcare (2012 and 2013 versions) – referenced by at least nine provinces and territories, while the 1999 version was found to be referenced by nine provinces;
- Infection Control Guidelines: Handwashing, Cleansing, Disinfection and Sterilization in Health Care (1998) – referenced by at least eight provinces;
- Prevention and Control of Occupational Infections in Health Care. An Infection Control Guide (2002) – referenced by at least eight provinces; and
- Hand Hygiene Practices in Healthcare Settings (2012) – referenced by at least seven provinces.
The analysis also found that every province referenced at least three of the 15 selected HAI-related PHAC guidance documents published between 2002 and 2016 as part of the Infection Control Guideline Series.
Some of the selected documents were less frequently referenced, such as the Infection Control Guideline for the Prevention of Healthcare-Associated Pneumonia (2010, referenced twice), and Routine Practices and Additional Precautions Assessment and Educational Tools (2013, referenced twice). Two recent documents were found not to have been referenced: the poster Help reduce the spread of antimicrobial resistance - Follow recommendations for routine practices in settings where health care is provided (2016), and Recommended practices for the prevention of endoscopy-related infections (2016).
Further analysis found that many of the provincial and territorial documents and websites examined also referenced HAI-related material from other provinces and territories. Material from Ontario was the most frequently referenced by other provinces and territories, in particular documents on hand hygiene, infection prevention and control, and routine practices. It was noted that some of the provincial and territorial documents had very similar names to those of PHAC documents.
Overall, it seems that the documents that were found to be the most used are older documents, compared to more recent guidelines. The documents that were found to be the most used tend to focus on more general or overarching subjects, such as occupational infections or handwashing, instead of more targeted guidance for specific infections or area, such as 2017 guidance on Mycobacterium chimaera infections in patients exposed to heater-cooler devices in Canada or 2016 guidance on Middle East Respiratory Syndrome Coronavirus (MERS-CoV). More recent guidance documents tended to be focused on specific or targeted areas.
Although the evaluation has found that PHAC's surveillance and guidance knowledge products are valued by external stakeholders, according to key informants, the timeliness of development and release, and lack of up-to-date information, limits their use.
Nearly all external key informants identified a need for more timely surveillance data. While some external key informants noted that the timeliness of PHAC's surveillance products is somewhat better than it was five years ago, the majority reported that they are dependent on PHAC's surveillance data for benchmarking purposes. Data that are two years old were perceived as no longer relevant, because HAI incidence could have changed within that time period. Such findings are reflected in Table 4, presented on page 13 of this report, which demonstrates frequent gaps of one or two years between the period of data covered by the reports, and the release of the reports. As well, as shown in that table, the evaluation has not found an example of an infection-specific surveillance report (e.g., MRSA surveillance report) released since 2014.
Internal key informants attribute the challenge with timely surveillance reports to a lack of human resources. Several internal and external key informants also noted that the lack of timely surveillance data appeared to be due to the approval process for surveillance reports. While some delays may also be due to the length of time necessary to post information on the canada.ca website, PHAC has tried to work around those delays by posting information on partner websites (e.g., the Association of Medical Microbiology and Infectious Disease Canada). It has also tried to improve timeliness by producing infographics instead of full reports.
Recognizing that the development of guidelines is a lengthy process regardless of the area, the evaluation also found evidence of a lack of timeliness for the development of guidance products. There have been instances where guidance products took years to release. For example, guidance on healthcare workers infected with blood-borne pathogens began with a needs assessment in late 2011. As of December 2017, this guideline has yet to be released. In this particular case, the work had to stop while staff shifted focus for a year to work on the outbreak response for Ebola, which included drafting guidelines. This significant stoppage resulted in the need to review the literature again to ensure that the most up-to-date evidence was used to inform the guideline development.
In the absence of PHAC guidelines, external key informants reported looking for information elsewhere (e.g., other provinces and territories, the U.S. Centers for Disease Control and Prevention, Australia, the United Kingdom, the European Union, and the World Health Organization). These guidance documents might not be entirely appropriate for the Canadian context, as other countries, provinces, and territories have different systems and processes in place. Several external key informants reported that if provincial or territorial guidelines are released prior to national ones, they may contradict each other, thereby leaving it to healthcare providers to determine which ones to follow. This evaluation has, however, not examined the consequences of potential contradiction or duplication between federal and provincial or territorial guidelines.
Another factor that is perceived as restricting the use of surveillance data is the limited coverage of CNISP. Although 65 acute-care hospitals (mostly tertiary) participate in CNISP, and approximately 78% of the Canadian population lives within 100 kilometres of a CNISP hospital, several external key informants working in surveillance and guidance noted that it lacks community, rural, and northern hospital data. External key informants who are not a part of CNISP noted that inclusion of more hospitals and healthcare facilities would increase access to PHAC's surveillance knowledge products, as these data are not readily available to non-CNISP hospitals, unless a participating hospital can share the data with them. A few external key informants noted that PHAC's activities are more acute-care focused and they would like to see PHAC focus on the continuum of care, including long-term care and home care, as it has in the past.
4.2.2 Demonstration of Economy and Efficiency
As previously mentioned, HAIs represent a significant financial burden for health systems and society as a whole. Preventing and controlling HAIs can help reduce these costs.
PHAC HAI activities are allocated approximately $3.4 million per year. Annual expenditures are approximately $900,000 for guidance, $1.6 million for surveillance activities, $200,000 for AMR coordination, $560,000 for the National Microbiology Laboratory's CNISP activities and $550,000 for CARSS activities for fiscal years 2015-16 to 2016-17. A summary of budgets and expenditures is presented in Table 6 on the next page.
Over the past five years, expenditures for guidelines were either close to being entirely spent, or exceeded planned budget. CNISP has consistently underspent on operations and maintenance (O&M) and salaries, which can be explained by CNISP having fewer full-time equivalents than planned, over the course of the five years. Of note, both internal and external key informants mentioned that CNISP has been successful in securing longer-term funding after years of uncertainty, which is considered a positive step forward, as this type of funding is seen as a commitment to the program.
As previously mentioned, in March 2015, the Government of Canada released its Federal Action Plan on Antimicrobial Resistance and Use in Canada: Building on the Federal Framework for Action, which outlines PHAC's contribution in the areas of AMR surveillance, stewardship and innovation.Endnote 46 In 2014-15, the Office of the Auditor General conducted an audit of the Government of Canada's AMR activities and released its report in 2015, recommending that PHAC work with its federal partners, provinces and territories, and other stakeholders in the development of a pan-Canadian strategy to address AMR, and ensure that adequate surveillance data on AMR is available.Endnote 47 As a result, PHAC launched CARSS in March 2015 as a key component of the Government of Canada's Federal Action Plan on Antimicrobial Resistance and Use in Canada.Endnote 48 However, CARSS has no permanent budget to carry out its activities, relying instead on temporary internal funding reallocations to continue its work. AMR activities in relation with HAIs are also carried out with temporary funding.
PHAC's National Microbiology Laboratory's (NML) planned work for CNISP-related projects is part of the Antimicrobial Resistance and Nosocomial Infections Section's budget. Planned and actual spending for CNISP was calculated as a percentage of the total section budget.
| Planned Spending ($) | Expenditures ($) | Variance ($) | % planned budget spent |
|||||
|---|---|---|---|---|---|---|---|---|
| O&M | Salary | Total | O&MFootnote b | Salary | Total | |||
| 2012-13 | ||||||||
| CNISP (Surveillance) | 700 | 1,178 | 1,878 | 674 | 1,126 | 1,800 | -78 | 96% |
| NML - CNISP | 153 | 294 | 447 | 156 | 294 | 450 | 3 | 101% |
| Infection Prevention and Control (Guidance) | 168 | 716 | 884 | 141 | 717 | 858 | -26 | 97% |
| Total | - | - | - | 971 | 2,136 | 3,108 | - | |
| 2013-14 | ||||||||
| CNISP (Surveillance) | 685 | 1,129 | 1,814 | 652 | 938 | 1,590 | -224 | 88% |
| NML - CNISP | 124 | 419 | 543 | 186 | 419 | 605 | 62 | 111% |
| Infection Prevention and Control (Guidance) | 200 | 652 | 852 | 276 | 614 | 890 | 38 | 104% |
| Total | - | - | - | 1,114 | 1,971 | 3,085 | - | |
| 2014-15 | ||||||||
| CNISP (Surveillance) | 830 | 1,165 | 1,995 | 801 | 915 | 1,716 | -279 | 86% |
| NML - CNISP | 135 | 384 | 519 | 195 | 384 | 579 | 60 | 112% |
| Infection Prevention and Control (Guidance)Footnote c | 241 | 652 | 893 | 226 | 862 | 1,088 | 195 | 122% |
| AMRFootnote d | 0 | 0 | 0 | 14 | 36 | 49 | 49 | - |
| Total | - | - | - | 1,236 | 2,197 | 3,432 | - | |
| 2015-16 | ||||||||
| CNISP (Surveillance) | 713 | 873 | 1,586 | 671 | 694 | 1,365 | -221 | 86% |
| NML - CNISP | 160 | 406 | 566 | 178 | 406 | 584 | 18 | 103% |
| Infection Prevention and Control (Guidance)Footnote c | 99 | 689 | 788 | 81 | 691 | 772 | -16 | 98% |
| AMRFootnote d | 0 | 0 | 0 | 42 | 366 | 408 | 408 | - |
| CARSSFootnote e | 0 | 512 | 512 | 27 | 417 | 444 | -68 | 87% |
| Total | - | - | - | 999 | 2,573 | 3,573 | - | |
| 2016-17 | ||||||||
| CNISP (Surveillance) | 715 | 837 | 1,552 | 647 | 705 | 1,351 | -200 | 87% |
| NML - CNISP | 139 | 408 | 547 | 194 | 408 | 603 | 56 | 110% |
| Infection Prevention and Control (Guidance) | 107 | 767 | 874 | 64 | 838 | 902 | 29 | 103% |
| AMRFootnote d | 0 | 0 | 0 | 3 | 180 | 182 | 182 | - |
| CARSSFootnote e | 0 | 512 | 512 | 158 | 503 | 661 | 148 | 129% |
| Total | - | - | - | 1,066 | 2,634 | 3,699 | - | |
Numbers may not add up to the total column due to rounding. |
||||||||
Collaborations and Governance
PHAC carries out many activities by leveraging expertise through the CNISP, IPC-Expert Working Group (IPC-EWG), AMR-AMU Stewardship working groups, many of whom volunteer their time in order to provide PHAC with valuable expert advice. Each CNISP surveillance project has a working group comprised of the Canadian Hospital Epidemiology Committee and PHAC members who direct the development and implementation of surveillance projects. The working groups include subject matter experts and representatives from a number of internal and external organizations, including Infection Prevention and Control Canada, as well as hospitals and universities from across Canada. CNISP has surveillance protocols for working group topics that outline the objectives and methodologies of each subject for each project.
The IPC-EWG, which is in the process of transitioning to an External Advisory BodyFootnote iv, guides the development and maintenance of PHAC's infection prevention and control Guidelines Series. It provides PHAC with advice and recommendations on current and emerging infection prevention and control issues in healthcare settings. The IPC-EWG is comprised of PHAC staff, infection prevention and control experts, and non-voting liaison representatives, such as the Canadian Patient Safety Institute, Infection Prevention and Control Canada, the Canadian Medical Association, the Canadian Nurses Association, and the U.S. Centers for Disease Control and Prevention, among others. Between January 2012 and July 2017, the IPC-EWG held three face-to-face meetings and 46 teleconferences to provide PHAC with technical expertise in the development, dissemination, evaluation, and implementation of infection prevention and control recommendations.Endnote 49
PHAC's AMR group collaborates with a number of stakeholders, nationally and internationally, allowing them to disseminate information and link partners. For example, PHAC brought HealthCareCAN and the National Collaborating Centre for Infectious Diseases together to discuss antimicrobial stewardship. The latter was at the table because it plays an important role in knowledge translation, and also has AMR on its work plan.
Some of PHAC's AMR key national stakeholders include Mount Sinai Hospital, HealthCareCAN, and the National Collaborating Centre for Infectious Diseases, and campaigns such as Choosing Wisely Canada. International stakeholders include the World Health Organization, the European Centre for Disease Prevention and Control, and the U.S. Centers for Disease Control and Prevention.
In addition, PHAC established an AMR-AMU Stewardship working group to support its work on this key pillar by developing a common PHAC-wide approach to antimicrobial stewardship.
PHAC collaborates internationally in activities such as the 2014 Coordinated AMR Global Twitter Chat. PHAC is responsible for AMR-AMU Stewardship, one of the key pillars identified in the Antimicrobial Resistance and Use in Canada: A Federal Framework for Action.
PHAC participates in meetings held by the U.S. Centers for Disease Control and Prevention, including Healthcare Infection Control Practices Advisory Committee meetings. It participates in the World Health Organization's Global Infection Prevention and Control Network, the Guidelines International Network, the AMR Surveillance System group, the Transatlantic Task Force on Antimicrobial Resistance Working Group, and also attends G20 AMR public health experts meetings. In November 2017, PHAC sent a member of its staff to Haiti to assist the Pan American Health Organization with its infection prevention and control program.
The Centre for Communicable Diseases and Infection Control collaborates internally with other areas of PHAC by providing expert advice to the Centre for Immunization and Respiratory Infectious Diseases, various areas of Health Canada, such as the First Nations and Inuit Health Branch for HAI training, and the Health Products and Food Branch for heater/cooler medical device contamination issues, as well as providing support for broader PHAC emergency response activities, such as the Ebola outbreak in 2014.
PHAC's National Microbiology Laboratory (NML) participates in a number of other working groups including:
- CNISP working groups on MRSA, VRE, C. difficile, CPOs, data quality and paediatrics;
- CARSS;
- Global Laboratory Antimicrobial Resistance Surveillance System (GLASS);
- Transatlantic Task Force on Antimicrobial Resistance Working Group; and
- Canadian Public Health Laboratory Network and Reference Centre Advisory Subcommittee, among others.
Most internal and external key informants noted the strength of the collaborations through CNISP, PHAC's National Microbiology Laboratory and IPC-EWG, stating that working relationships were very good. A few external key informants reported that through CNISP and the collaboration with NML, they have a better sense of what is relevant, in terms of the bigger picture for the nation as a whole. CNISP face-to-face meetings enable a discussion of common approaches, patterns, and plans for new surveillance. With regards to guidance, a few internal and external key informants noted that greater collaboration with the U.S. Centers for Disease Control and Prevention provides a better understanding of why its guidance may differ from PHAC's.
Potential Efficiency
The evaluation examined potential efficiency to be gained in PHAC's HAI activities. Some internal and external key informants identified areas where HAI activities are seen as being particularly efficient, and where alternative approaches could be explored.
For surveillance, the collaboration among the CNISP Canadian Hospital Epidemiology Committee members was seen to improve efficiency; however, as previously mentioned, many external key informants believe that expanding CNISP is necessary. A few external key informants felt that PHAC could make better use of the Canadian Network for Public Health Intelligence platform to increase efficiency. A couple even suggested that the Canadian Network for Public Health Intelligence platform could be used to pilot an expansion of CNISP hospitals. The majority of internal and external key informants reported that PHAC's surveillance products are not timely, and it was therefore noted that the approval process for low-risk surveillance products could be streamlined to help ensure a more timely release of all surveillance products.
A few internal and external key informants saw the contracting process with CNISP hospitals as being more efficient when PHAC managed the contracts. PHAC technical experts were available to answer questions, and this was seen as helpful, considering that hospitals are not necessarily familiar with Government of Canada contracting processes. At present, each individual CNISP hospital has an independent contract with Public Services and Procurement Canada.
While there are several examples of collaboration between PHAC and external HAI experts, many provincial and territorial key informants noted that they would benefit from a working-level HAI federal/provincial/territorial committee to build connections, and share experiences and lessons learned. One example was noted where an established federal/provincial/territorial working-level group would have been useful. During 2016-17, there was an outbreak of M. chimaera in cardiac surgery patients where contaminated heater/cooler medical devices were identified as the source. Within each jurisdiction, only a few hospitals worked with these devices. Federal/provincial/territorial teleconferences allowed stakeholders to exchange information in real time, with the added benefit of conveying the same messages, which was helpful to those in the field. Currently, there is no working group designed to encourage a regular exchange of information. There is a federal/provincial/territorial network through the Communicable and Infectious Disease Steering Committee, which is a subcommittee of the Public Health Network, but HAIs is not the focus of the Committee's work.
Many internal and external key informants noted that PHAC could work with provinces and territories to endorse existing provincial and territorial guidelines where appropriate, in an effort to avoid long delays in producing guidelines. However, no such mechanism presently exists. PHAC staff can sit on a provincial/territorial working group and know they have shown due diligence in analyzing the most up-to-date evidence available to draft guidelines, but they have no mechanism for endorsing these guidelines.
Finally, while several external key informants noted that available PHAC guidance documents are useful, they found them to be outdated (some date back to 2002). Ideally, these documents would be kept evergreen and updated on a regular basis (e.g., every three years).
5.0 Conclusions
There is a continued need for Public Health Agency of Canada (PHAC)'s HAI activities, as these infections are often preventable, but remain persistent in Canada, and result in a significant burden to society. Activities to prevent and reduce health risks associated with HAIs align with the Government of Canada priority to prevent and control infectious diseases. However, stakeholders interviewed for the evaluation identified a lack of clarity on how PHAC prioritizes its HAI activities. The evaluation also found that PHAC's mandate for HAI activities comes from overarching program and policy authorities that have not been updated since 2006. The evaluation did not find evidence of this affecting PHAC's ability to carry out its HAI activities. However, the context in which HAI activities are delivered is evolving with the emergence of AMR as a global priority. Additionally, the evaluation found a lack of clarity around PHAC's priorities for its HAI activities, so there may be a need to clearly articulate the mandate around those activities to ensure PHAC's role in this area remains relevant.
PHAC's HAI activities touch an area of shared responsibilities as provincial and territorial governments are responsible for the delivery of healthcare services in settings where patients are most likely to acquire HAIs (e.g., hospitals). Many national-level health organizations, such as the Canadian Institute for Health Information are also involved in this area. Despite there being players in the field, the evaluation found evidence that PHAC has a clear public health leadership role to conduct HAI surveillance, to provide evidence-based HAI guidance to healthcare and public health professionals, and to liaise with international partners, such as the World Health Organization. Moreover, the roles played by PHAC are generally well understood by external key informants. For the most part, the roles played by PHAC, the provinces and territories, and other organizations are complementary, but there is the potential for duplication in surveillance, mainly because CNISP and provinces and territories that have a surveillance system in place are not necessarily using the same case definitions.
PHAC's guidance and surveillance knowledge products are valued and used to some extent by stakeholders. However, the potential use of these products is limited due to difficulties in accessing timely and up-to-date information. The limited coverage of CNISP surveillance data was also seen as restricting the potential use of PHAC surveillance products. Currently, 65 acute-care hospitals (mostly tertiary) participate in CNISP. Although approximately 78% of the Canadian population lives within 100 kilometres of a CNISP hospital, several external key informants working in surveillance and guidance noted that CNISP lacks community, rural, and northern hospital data. Including these hospitals and healthcare facilities would provide a more complete picture of HAIs across Canada.
PHAC HAI activities represent approximately $3.4M per year in expenditures. Over the past five years, expenditures on guidelines were either close to being entirely spent, or exceeded the planned budget. CNISP has consistently underspent on O&M and salaries, and some variance in salaries can be explained by CNISP having fewer full-time equivalents than planned over the course of the five years.
PHAC carries out many of its HAI activities by leveraging expertise through CNISP and other collaborations, many of whom volunteer their time in order to provide PHAC with valuable expert advice.
6.0 Recommendations
Recommendation 1
Clearly articulate the Public Health Agency of Canada's (PHAC)'s role and priorities for HAI activities and communicate those to stakeholders.
Considering that policy and program authorities for PHAC's HAI activities have not been updated since 2006, and considering the lack of clarity around PHAC's priorities for its HAI activities, there is an opportunity to articulate what role PHAC could assume in the HAI area, and where it should prioritize its activities. This would help ensure that PHAC's role remains relevant. There is also a need to clearly communicate those priorities with stakeholders.
Recommendation 2
Explore options to improve program effectiveness and efficiency focusing on improving: a) the timeliness of surveillance and guidance knowledge products and, b) the coverage of Canadian Nosocomial Infection Surveillance Program (CNISP) surveillance data.
There is an opportunity to explore options to improve the timeliness of guidance and surveillance products. In this regard, the evaluation identified a few options, such as establishing a mechanism to endorse existing provincial and territorial guidelines where appropriate, streamlining the approval process for low-risk surveillance products, and exploring opportunities to use the Canadian Network for Public Health Intelligence platform to expand CNISP. There is also an opportunity to examine options to increase representativeness within CNISP to help ensure the continued usefulness of PHAC's surveillance data.
Appendix 1 – Description of PHAC's HAI Activities
The Centre for Communicable Diseases and Infection Control's HAI activities aim to reduce and prevent health risks related to HAIs, focusing on complementing provincial and territorial public health efforts, and establishing national guidance for appropriate precautions for the management of infections attributed to healthcare procedures in hospitals and other healthcare settings. The National Microbiology Laboratory (NML) provides input into surveillance plans, and supports laboratory-based reference services and research for pathogens such as Methicillin resistant staphylococcus aureus (MRSA), C. difficile, Vancomycin-resistant enterococci (VRE) and carbapenem-resistant Enterobacteriaceae (CRE).Footnote v NML also conducts antimicrobial susceptibility and molecular typing to monitor the distribution of resistant strains across Canada and globally.
Infection prevention and control is a core aspect of the fight against antimicrobial resistance (AMR), and the conservation of antibiotics is a valuable after-effect of promoting and protecting human health. Well-established and consistent infection prevention and control measures and practices can reduce the occurrence of infection, and prevent the spread of harmful bacteria. Preventing any infection, whether or not it is caused by AMR micro-organisms, reduces the need for antimicrobial utilization. Through existing resources, PHAC provides program-specific expertise, supporting the development of a pan-Canadian framework and AMR infection prevention and control action plan.
PHAC HAI activities can be regrouped around surveillance, advice/guidance, and outbreak response.
Surveillance
PHAC develops, collects, analyzes, and disseminates HAI surveillance data to monitor trends in rates, strain types and AMR, provide early detection of new organisms, and monitor severe causes of morbidity and mortality during an outbreak. Vigilant surveillance within healthcare settings, including hospitals, is seen as being important, due to the nature of infection communicability and transmissibility, preventability, treatability, clinical impact, and mortality of antimicrobial-resistant pathogens. PHAC also provides national reference laboratory services for outbreak investigations and surveillance, and engages in research activities targeted at reducing the impacts of pathogens (e.g., AMR).
The Canadian Nosocomial Infection Surveillance Program (CNISP) is PHAC's main surveillance mechanism to track and monitor infections transmitted in healthcare settings, including antimicrobial-resistant organisms. It is a collaborative effort between PHAC and the Canadian Hospital Epidemiology Committee, a committee of the Association of Medical Microbiology and Infectious Disease Canada. CNISP is a sentinel surveillance program that funds targeted acute-care hospitals to track and monitor specific healthcare-associated infections including Carbapenem-producing organisms (CPOs), Central line-associated bloodstream infections (CLABSI), C. difficile, Methicillin resistant staphylococcus aureus (MRSA), Vancomycin-resistant enterococci (VRE), surgical site infections, antimicrobial utilization and other antimicrobial-resistant organisms (e.g., E. coli). In addition, CNISP collects data on antimicrobial utilization in CNISP hospitals, antibiogram data on E. coli, conducts periodic point prevalence studies on HAIs, and combines both laboratory and epidemiological data. In addition to producing national rates and trends, summary data tables, surveillance reports, and other publishable peer-reviewed journal articles, CNISP provides epidemiological technical advice and support upon request to provinces and territories in the event of an outbreak.
CNISP surveillance aims to provide national benchmark data that will enable comparison of rates between various Canadian health care settings, and internationally. Furthermore, CNISP surveillance aims to establish and use standardized surveillance methods, document the prevalence of HAIs in Canada, and describe temporal trends in HAI rates, antimicrobial susceptibility patterns, and molecular characterizationFootnote vi of selected HAIs. In addition, CNISP data helps to inform the development of federal, provincial, and territorial infection prevention and control programs and policies.
The Canadian Antimicrobial Resistance Surveillance System (CARSS) uses targeted surveillance of identified priority antimicrobial organisms and contributes to surveillance in the area of HAIs. CARSS provides an integrated picture of AMR and antimicrobial use (AMU) in Canada, based on data from PHAC's surveillance systems and laboratory reference services. It uses data to develop an overall picture of AMR and AMU and works with domestic and international scientific experts and health professionals to monitor global AMR and AMU trends and impacts.
PHAC also provides advice on a number of ongoing HAI-AMR-related initiatives. PHAC offers technical support to two AMR Task Groups established by the Pan-Canadian Public Health Network's Communicable and Infectious Disease Steering Committee. PHAC acts as the Secretariat for the Task Group on Antimicrobial Use Stewardship, and remains an ongoing content resource for the Task Group on AMR Surveillance. More specifically, PHAC delivers technical content to these task groups, as well as to interdepartmental governance committees that include Health Canada and Global Affairs Canada, with respect to surveillance and stewardship topics. PHAC facilitates the development and dissemination of reports and technical materials coming out of these groups.
Advice/Guidance
PHAC provides advice in the development of infection prevention and control guidance and guidelines for Canadian healthcare settings.
Guidelines, by definition, include principles and recommendations based on research and evidence, and do not represent rigid standards. The World Health Organization defines guidance as systematically developed, evidence-based statements that assist providers, recipients, and other stakeholders in making informed decisions about appropriate health interventions, and guidelines are a type of guidance product.Endnote 50
Infection prevention and control guidelines are also intended to provide a framework for developing policies and procedures for routine practices and infection precautions in healthcare settings, taking into consideration local conditions and risks. They are intended to assist infection prevention and control professionals, and other healthcare providers responsible for developing infection and control policies and procedures in all settings where healthcare is provided.
PHAC's Infection Control Guideline Series includes specific reference documents, such as the Routine Practices and Additional Precautions for Preventing the Transmission of Infection in Healthcare Settings (2013 revision) and the Hand Hygiene Practices in Healthcare Settings (2012). These documents identify and promote practices and precautions for preventing the transmission of microorganisms in healthcare settings.
PHAC also develops and publishes information materials and resources for healthcare and public health professionals in provinces and territories, as well as the public at large. This material presents information in a summarized format, with key points on highly infectious viruses and bacteria. Reference materials such as PHAC's “Fact Sheets” on different HAI, viruses, and bacteria can be accessed on the PHAC website, and are aimed at providing thorough, plain-language information to a broad range of users on how to protect oneself against infection and illness, as well as how to prevent or reduce the risk of transmission of infection when ill.
Outbreak Response Assistance
PHAC also provides technical support and advice in various capacities in the event of outbreaks, or the emergence or re-emergence of infections that may directly or indirectly affect or occur in healthcare settings. PHAC also monitors organisms that can cause significant morbidity and mortality to Canadians and are transmitted within healthcare settings, such as antimicrobial-resistant organisms. PHAC addresses them on an ad hoc basis or upon request through the development of technical reports or interim guidelines or statements. Guidelines, such as those developed for Ebola, are examples of PHAC's technical ad hoc input towards the development of resources related to HAI prevention and control.
Appendix 2 – Logic Models

Image 1 - Text description
According to the program logic model, the Centre for Communicable Diseases and Infection Control has three activity areas: knowledge creation and analysis; knowledge translation, transfer and mobilization; and public health intervention. These activities are expected to produce the following outputs: surveillance datasets; knowledge assessments-systematic review; models; knowledge products (public health guidance / surveillance / epidemiological); educational modules and workshops; educational modules / training materials / workshops; and G&C contract agreements. These activities and outputs are expected to lead to the follow short, medium, and long-term outcomes. Short-term outcomes: stakeholders have knowledge to prevent and control communicable diseases (stakeholders: F/P/T, public health authorities, healthcare providers, NGOs); and target populations have skills and abilities to prevent and control communicable diseases (target populations: priority population, healthcare providers and front-line workers). Medium-term outcomes: stakeholders apply knowledge in the practice of public health (stakeholders: F/P/T, public health authorities, healthcare providers, NGOs); and target populations' personal behaviours prevent the transmission of communicable diseases (target populations: priority populations, healthcare providers and front-line workers). Long-term outcome: people living in Canada are protected from communicable diseases acquired in community and healthcare settings.
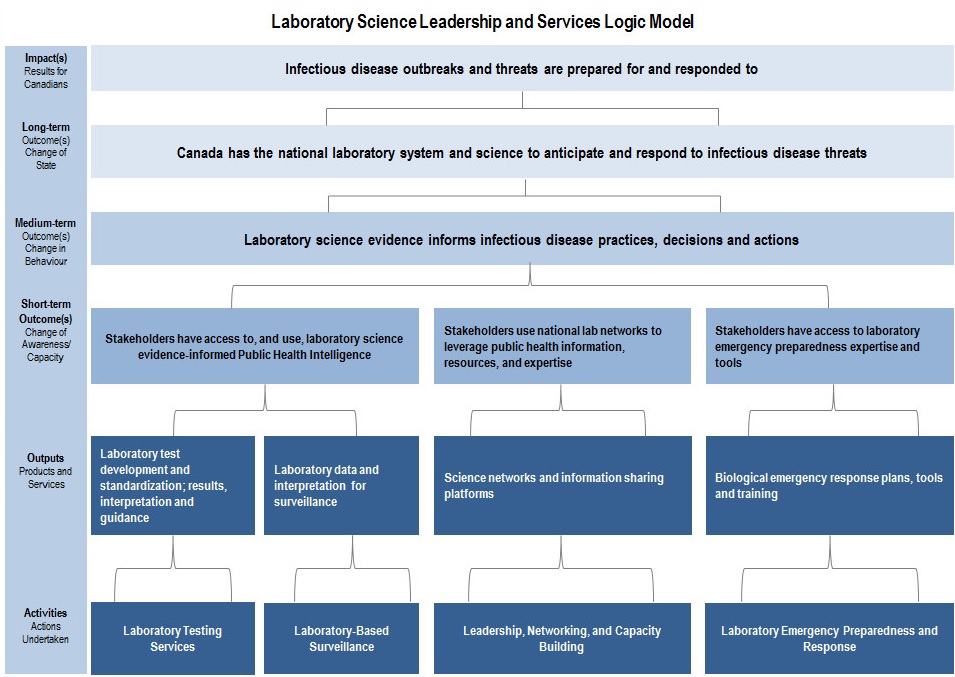
Image 2 - Text description
According to the program logic model, the National Microbiology Laboratory's Laboratory Science Leadership and Services has four activity areas: laboratory testing services; laboratory-based surveillance; leadership, networking, and capacity building; and laboratory emergency preparedness and response. These activities are expected to produce the following outputs: laboratory test development and standardization; results, interpretation and guidance; laboratory data and interpretation for surveillance; science networks and information sharing platforms; and biological emergency response plans, tools and training. These activities and outputs are expected to lead to the following short, medium, and long-term outcomes. Short-term outcomes: stakeholders have access to, and use, laboratory science evidence-informed public health intelligence; stakeholders use national lab networks to leverage public health information, resources, and expertise; and stakeholders have access to laboratory emergency preparedness expertise and tools. Medium-term outcome: laboratory science evidence informs infectious disease practices, decisions and actions. Long-term outcome: Canada has the national laboratory system and science to anticipate and respond to infectious disease threats.
Appendix 3 – Evaluation Description
Evaluation scope
The evaluation covered the period from April 1, 2012 to September 30, 2017, and included PHAC HAI activities. It did not cover activities that are the responsibility of other jurisdictions (e.g., provincial and territorial responsibility for hospitals).
As per the Treasury Board of Canada's Policy on Results (2016), the evaluation examined question in relation to the relevance and performance of HAI activities, as shown in the Table below.
| Core Issues | Evaluation Questions |
|---|---|
| Relevance | |
| Issue #1: Continued Need |
|
| Issue #2: Alignment with Government Priorities |
|
| Issue #3: Alignment with Federal Roles and Responsibilities |
|
| Performance (effectiveness, economy and efficiency) | |
| Issue #4: Achievement of Expected Outcomes |
|
| Issue #5: Demonstration of Economy and Efficiency |
|
An outcome-based approach was used for this evaluation to assess the relevance and performance in achieving HAI-related outcomes.
Data Collection and Analysis Methods
Evaluators collected and analyzed data from multiple sources. Data collection started in April 2017 and ended in October 2017. Data for the evaluation were collected using the following methods:
- Literature review – A search of Canadian literature from the past five years using search terms such as “nosocomial infections”, “Healthcare-associated infections”, “surgical site infections”, “Clostridium difficile”, and “central line-catheter-associated bloodstream”. After examining documents to ensure relevance, 61 articles were reviewed.
- Media review – A search of Canadian media references to MRSA and C. difficile from the past two years was conducted using search terms such as “nosocomial infection”, “Clostridium Difficile infection”, and “Canadian Nosocomial Infections Surveillance Program”. After examining documents to ensure relevance, 465 articles were reviewed.
- Document review – Approximately 80 documents pertinent to HAI were reviewed for information regarding the relevance (priorities, roles, and responsibilities) of the activities.
- Program document and file review – Approximately 420 documents, held by the divisions responsible for the healthcare-associated infection activities, were reviewed to obtain information regarding all aspects of the activities related to HAIs, and in particular the performance (achievement of outcomes, economy and efficiency) of activities.
- Financial data review – A review of financial data from 2012-13 to 2016-17 was conducted, including budgeted and actual expenditures.
- Key informant interviews – Interviews were conducted with 42 stakeholders: internal staff and management (n=11), and external stakeholders and other organizations (n=31) representing CNISP hospitals, provincial and territorial representatives, academia, experts, and non-governmental organizations. Twelve of the external stakeholders are affiliated with PHAC's Infection Prevention and Control - Expert Working Group (IPC-EWG). Key informants were selected for their knowledge of, and experience with, healthcare-associated infection activities at PHAC, or issues related to healthcare-associated infections.
- Citation analysis – A search was done of provincial and territorial websites and online documents for references to PHAC HAI-related guidance documents, as well as for references to provincial and territorial HAI-related guidance documents. Over 600 documents were reviewed.
Data were analyzed by triangulating information gathered from the different methods listed above. The use of multiple lines of evidence and triangulation were intended to increase the reliability and credibility of the evaluation findings and conclusions.
Appendix 4 – Citation Analysis
Methodology
A citation analysis was conducted to examine whether PHAC HAI products are being used by provinces and territories and a selection of external organizations as part of their own information products (i.e. information and documents published or available on their websites). Each provincial and territorial website was searched for references to selected PHAC's HAI-related guidance documents that are part of the Infection Control Guideline Series. This search involved the use of keywords (e.g., hand hygiene, infection prevention and control, PHAC), as well as examining any manuals or guidance documents available. The documents were also searched for references to other provincial and territorial documents, and to the provinces and territories themselves.
There were certain limitations in the citation analysis. There is the possibility that some references to PHAC material were missed in the search, as some challenges in searching the websites were encountered (e.g., difficult to use search engines). Additionally, websites for five organizations (i.e., the Association of Medical Microbiology and Infectious Disease Canada, Infection Prevention and Control Canada, the Canadian Patient Safety Institute, the Canadian Medical Association, and the Canadian Nurses Association) were searched for references to the selected guidance documents. There were difficulties finding material on several sites because the evaluators did not have access to members-only sites or resource sections. As well, it should be noted that it was not clear whether all provincial, territorial, and organizational guidance documents and manuals were posted online. Therefore, findings presented in this report may not provide a complete picture of the extent to which PHAC guidelines are referenced.
Findings
The analysis showed that all provinces referenced at least three of the 15 selected HAI-related PHAC guidance documents, but only one territory was found to have made a reference to the guidance documents. The following table shows how many provinces and territories referenced each of the documents included this analysis.
| Date of Publication | Guidance Document Examined | Number of Provinces/Territories that Referenced the Document |
|---|---|---|
| 2012 & 2013 | Routine Practices and Additional Precautions for Preventing the Transmission of Infection in Healthcare Settings | 9 |
| 1999 | Routine Practices and Additional Precautions for Preventing the Transmission of Infection in Health Care | 9 |
| 2002 | Prevention and Control of Occupational Infections in Health Care. An Infection Control Guide | 8 |
| 1998 | Infection Control Guidelines: Handwashing, Cleansing, Disinfection and Sterilization in Health Care | 8 |
| 2012 | Hand Hygiene Practices in Healthcare Settings | 7 |
| 2013 | Clostridium difficile Infection - Infection Prevention And Control Guidance For Management In Acute Care Settings | 5 |
| 2013 | Clostridium difficile Infection - Infection Prevention And Control Guidance For Management In Long-Term Care Facilities | 5 |
| 2011 | Infection Prevention and Control Guideline for Flexible Gastrointestinal Endoscopy and Flexible Bronchoscopy | 5 |
| 2010 | Infection Prevention and Control Measures for Healthcare Workers in All Healthcare Settings - Carbapenem-resistant Gram-negative Bacilli | 5 |
| 2016 | Infection Prevention and Control Guidance for Middle East Respiratory Syndrome Coronavirus (MERS-CoV) in Acute Care Settings | 4 |
| 2010 | Infection Prevention and Control Measures for Healthcare Workers in Acute Care and Long-term Care Settings for Seasonal Influenza | 4 |
| 2013 | Routine Practices and Additional Precautions Assessment and Educational Tools | 3 |
| 2012 | Seasonal Influenza - Infection Prevention and Control Guidance for Management in Home Care Settings | 3 |
| 2010 | Infection Control Guideline for the Prevention of Healthcare-Associated Pneumonia | 2 |
| 2014 | Infection Prevention and Control Guidelines – Critical Appraisal Tool | 2 |
| 2016 | Help reduce the spread of antimicrobial resistance - Follow recommendations for routine practices in settings where health care is provided [poster] | 0 |
| 2016 | Recommended practices for the prevention of endoscopy-related infections | 0 |
Footnotes
- Footnote i
-
The financial data include the following: CNISP and National Microbiology Laboratory surveillance, infection prevention and control guidance, CARSS and antimicrobial resistance activities.
- Footnote ii
-
CPEs are enterobacteriaceae that are resistant to carbapenem antimicrobials through the production of carbapenemase.
- Footnote iii
-
Organizations involved were the Canadian Patient Safety Institute, Infection Prevention and Control Canada, the Association of Medical Microbiology and Infectious Disease Canada, and the Canadian Institute for Health Information.
- Footnote iv
-
External advisory bodies provide PHAC with expert advice from individuals who have valuable knowledge, expertise, or experience.
- Footnote v
-
Carbapenem-resistant enterobacteriaceae are gram-negative bacteria that are resistant to carbapenem antibiotics.
- Footnote vi
-
Molecular characterization means characterizing an organism at the molecular level without an effect on the environment or development or physiological state of the organism.
Endnotes
- Endnote 1
-
World Health Organization. (2017-12-07). The burden of health care-associated infection worldwide. Retrieved from http://www.who.int/gpsc/country_work/burden_hcai/en/
- Endnote 2
-
Centers for Disease Control and Prevention. (2015-07-22). Ebola (Ebola Virus Disease): Transmission. Retrieved from https://www.cdc.gov/vhf/ebola/transmission/index.html
- Endnote 3
-
Public Health Agency of Canada (2014). The Chief Public Health Officer's Report on the State of Public Health in Canada, 2013: Infectious Disease—The Never-ending Threat -Healthcare-associated infections-due diligence. Retrieved from https://www.canada.ca/content/dam/phac-aspc/migration/phac-aspc/cphorsphc-respcacsp/2013/assets/pdf/2013-eng.pdf
- Endnote 4
-
Adrian R. Levy, Shelagh M. Szabo, Greta Lozano-Ortega, Elisa Lloyd-Smith, Victor Leung, Robin Lawrence, and Marc G. Romney. (2015-09). Incidence and Costs of Clostridium difficile Infections in Canada. Open Forum Infectious Diseases, 2(3): 1-10.
- Endnote 5
-
World Health Organization. (2002). Prevention of hospital-acquired infections: A practical guide (2nd edition). Retrieved from http://apps.who.int/iris/bitstream/10665/67350/1/WHO_CDS_CSR_EPH_2002.12.pdf
- Endnote 6
-
World Health Organization. (2017-12-07). The burden of health care-associated infection worldwide. Retrieved from http://www.who.int/gpsc/country_work/burden_hcai/en/
- Endnote 7
-
Public Health Agency of Canada (2014). The Chief Public Health Officer's Report on the State of Public Health in Canada, 2013: Infectious Disease—The Never-ending Threat -Healthcare-associated infections-due diligence. Retrieved from https://www.canada.ca/content/dam/phac-aspc/migration/phac-aspc/cphorsphc-respcacsp/2013/assets/pdf/2013-eng.pdf
- Endnote 8
-
Public Health Agency Canada (2015) Canadian Nosocomial Infection Surveillance Program (CNISP) Overview, HAI case definitions & rates. Retrieved from https://ottawa.ipac-canada.org/photos/custom/CNISP%20overview%20-%20SAEIG%20Feb%2010%202015.pdf
- Endnote 9
-
World Health Organization. (2017-12-07). The Burden of Health Care-Associated Infection Worldwide. A Summary. Retrieved from http://www.who.int/gpsc/country_work/summary_20100430_en.pdf
- Endnote 10
-
Canadian Surgical Site Infection- Safer Healthcare Now!(2016-02). Prevention Audit Month – February 2016. Retrieved from http://www.patientsafetyinstitute.ca/en/toolsResources/Documents/SSI%20Audit%202016_Recap%20Report%20EN.pdf
- Endnote 11
-
Public Health Agency of Canada (2017-11-06) Canadian Antimicrobial Resistance Surveillance System 2017 Report. Retrieved from https://www.canada.ca/en/public-health/services/publications/drugs-health-products/canadian-antimicrobial-resistance-surveillance-system-2017-report-executive-summary.html
- Endnote 12
-
Public Health Agency of Canada (2017-11-06) Canadian Antimicrobial Resistance Surveillance System 2017 Report. Retrieved from https://www.canada.ca/en/public-health/services/publications/drugs-health-products/canadian-antimicrobial-resistance-surveillance-system-2017-report-executive-summary.html
- Endnote 13
-
Public Health Agency of Canada (2017-11-06) Canadian Antimicrobial Resistance Surveillance System 2017 Report. Retrieved from https://www.canada.ca/en/public-health/services/publications/drugs-health-products/canadian-antimicrobial-resistance-surveillance-system-2017-report-executive-summary.html
- Endnote 14
-
Public Health Agency of Canada (2017-11-06) Canadian Antimicrobial Resistance Surveillance System 2017 Report. Retrieved from https://www.canada.ca/en/public-health/services/publications/drugs-health-products/canadian-antimicrobial-resistance-surveillance-system-2017-report-executive-summary.html
- Endnote 15
-
Public Health Agency of Canada (2013). The Chief Public Health Officer's Report on the State of Public Health in Canada, 2013: Infectious Disease—The Never-ending Threat -Healthcare-associated infections-due diligence . Retrieved from https://www.canada.ca/content/dam/phac-aspc/migration/phac-aspc/cphorsphc-respcacsp/2013/assets/pdf/2013-eng.pdf
- Endnote 16
-
Pan-Canadian Public Health Network. (2016-04). Antimicrobial Stewardship Final Report. Retrieved from http://www.phn-rsp.ca/pubs/anstew-gestan/pdf/pub-eng.pdf
- Endnote 17
-
Canadian Union of Public Employees (2009). Health care associated infections: A backgrounder. Retrieved from https://cupe.ca/sites/cupe/files/healthcare-associated-infections-cupe-backgrounder.pdf
- Endnote 18
-
Adrian R. Levy, Shelagh M. Szabo, Greta Lozano-Ortega, Elisa Lloyd-Smith, Victor Leung, Robin Lawrence, and Marc G. Romney. (2015-09). Incidence and Costs of Clostridium difficile Infections in Canada. Open Forum Infectious Diseases, 2(3): 1-10.
- Endnote 19
-
Nasia Safdar et al. (2014-05). Evolving Landscape of Healthcare - Associated Infections. Infection Control and Hospital Epidemiology, 35(5): 480–493.
- Endnote 20
-
Centers for Disease Control and Prevention. (2018-01-31).HAI Data and Statistics. Retrieved from https://www.cdc.gov/hai/surveillance/index.html
- Endnote 21
-
Public Health Agency of Canada (2014). The Chief Public Health Officer's Report on the State of Public Health in Canada, 2013: Infectious Disease—The Never-ending Threat -Healthcare-associated infections-due diligence. Retrieved from https://www.canada.ca/content/dam/phac-aspc/migration/phac-aspc/cphorsphc-respcacsp/2013/assets/pdf/2013-eng.pdf
- Endnote 22
-
Schwartz, I S; Hammond, G. (2017) First reported case of multidrug-resistant Candida auris in Canada. Canada Communicable Disease Report, 43.7/8: 150-153.
- Endnote 23
-
Bhagyashri D. Navalkele, Sanjay Revankar & Pranatharthi Chandrasekar. (2017). Candida auris: a worrisome, globally emerging pathogen . Expert Review of Anti-infective Therapy, 15 (9): 819-827.
- Endnote 24
-
Public Health Agency of Canada (2014). The Chief Public Health Officer's Report on the State of Public Health in Canada, 2013: Infectious Disease—The Never-ending Threat -Healthcare-associated infections-due diligenc . Retrieved from https://www.canada.ca/content/dam/phac-aspc/migration/phac-aspc/cphorsphc-respcacsp/2013/assets/pdf/2013-eng.pdf
- Endnote 25
-
Government of Canada. (2010). Speech from the Throne to open the Third Session, Fortieth Parliament of Canada. Retrieved from: http://www.lop.parl.gc.ca/ParlInfo/Documents/ThroneSpeech/40-3-e.html
- Endnote 26
-
Government of Canada. (2013). Speech from the Throne to open the Second Session, Forty-First Parliament of Canada. Retrieved from: http://www.lop.parl.gc.ca/ParlInfo/Documents/ThroneSpeech/41-2-e.html
- Endnote 27
-
Office of the Prime Minister (2017). Minister of Health Mandate Letter (October 4, 2017). Retrieved from http://pm.gc.ca/eng/minister-health-mandate-letter
- Endnote 28
-
Office of the Auditor General of Canada. (2008). 2008 May Report of the Auditor General of Canada: Chapter 5—Surveillance of Infectious Diseases—Public Health Agency of Canada. Retrieved from http://www.oag-bvg.gc.ca/internet/English/parl_oag_200805_05_e_30701.html
- Endnote 29
-
Office of the Auditor General of Canada. (2015). 2015 Spring Reports of the Auditor General of Canada: Report 1—Antimicrobial Resistance. Retrieved from http://www.oag-bvg.gc.ca/internet/English/parl_oag_201504_01_e_40347.html
- Endnote 30
-
Public Health Agency of Canada. (2014). Antimicrobial Resistance and Use in Canada: A Federal Framework for Action. Retrieved from https://www.canada.ca/en/public-health/services/antibiotic-antimicrobial-resistance/antimicrobial-resistance-use-canada-federal-framework-action.html
- Endnote 31
-
Public Health Agency of Canada. (2015). Federal Action Plan on Antimicrobial Resistance and Use in Canada: Building on the Federal Framework for Action. Retrieved from https://www.canada.ca/content/dam/canada/health-canada/migration/healthy-canadians/alt/pdf/publications/drugs-products-medicaments-produits/antibiotic-resistance-antibiotique/action-plan-daction-eng.pdf
- Endnote 32
-
World Health Organization. (2016). Guidelines on core components of infection prevention and control programmes at the national and acute health care facility level. Retrieved from http://apps.who.int/iris/bitstream/10665/251730/1/9789241549929-eng.pdf?ua=1
- Endnote 33
-
World Health Organization. (2015). Global action plan on antimicrobial resistance. Retrieved from http://www.who.int/antimicrobial-resistance/publications/global-action-plan/en/.
- Endnote 34
-
G20. (2017). The Outcomes of the G20 Summit. Retrieved from https://www.g20.org/Content/EN/Artikel/2017/07_en/2017-07-10-erfolge-g20-hamburg_en.html
- Endnote 35
-
G20. (2017). Berlin Declaration of the G20 Health Ministers Together Today for a Healthy Tomorrow. Retrieved from http://www.g20.utoronto.ca/2017/170520-health-en.html
- Endnote 36
-
Global Health Security Agenda. (2017-12-07). Antimicrobial Resistance Action Package. Retrieved from https://www.ghsagenda.org/packages/p1-antimicrobial-resistance
- Endnote 37
-
Public Health Agency of Canada. (2013). Strategic Horizons 2013-2018: Protecting Canadians from Illness. Retrieved from http://publications.gc.ca/collections/collection_2014/aspc-phac/HP55-1-2013-eng.pdf
- Endnote 38
-
Public Health Agency of Canada. (2016). Public Health Agency of Canada 2015-2016 Departmental Performance Report. Retrieved from https://www.canada.ca/en/public-health/corporate/transparency/corporate-management-reporting/departmental-performance-reports/2015-2016-departmental-performance-report.html?_ga=2.57547626.1992363112.1511790466-1719114292.1503933987
- Endnote 39
-
Public Health Agency of Canada. (2017). 2017–18 Departmental Plan: Public Health Agency of Canada. Retrieved from https://www.canada.ca/en/public-health/corporate/transparency/corporate-management-reporting/reports-plans-priorities/2017-2018-report-plans-priorities.html
- Endnote 40
-
Public Health Agency of Canada. (2013-05). Strategic Horizons 2013-2018. Retrieved from http://publications.gc.ca/collections/collection_2014/aspc-phac/HP55-1-2013-eng.pdf
- Endnote 41
-
Public Health Agency of Canada. (2011-06). Infectious Disease Prevention and Control Strategic Plan. Retrieved from internal files.
- Endnote 42
-
Government of Canada. (1996). Department of Health Act. Retrieved from http://lois-laws.justice.gc.ca/PDF/H-3.2.pdf
- Endnote 43
-
Government of Canada. (2006). Public Health Agency of Canada Act. Retrieved from http://lois-laws.justice.gc.ca/PDF/H-3.2.pdf
- Endnote 44
-
Public Health Agency of Canada. (2017-12-03). Infectious Disease Prevention and Control Branch. Retrieved from https://www.canada.ca/en/public-health/corporate/mandate/about-agency/infectious-disease-prevention-control-branch.html
- Endnote 45
-
Canadian Patient Safety Institute. (2015-07). An Infection Prevention and Control Action Plan. Retrieved from http://www.patientsafetyinstitute.ca/en/About/PatientSafetyForwardWith4/Documents/Infection%20Prevention%20and%20Control%20%28IPAC%29%20Action%20Plan.pdf
- Endnote 46
-
Public Health Agency of Canada. (2015-03). Federal Action Plan on Antimicrobial Resistance and Use in Canada: Building on the Federal Framework for Action. Retrieved from http://healthycanadians.gc.ca/alt/pdf/publications/drugs-products-medicaments-produits/antibiotic-resistance-antibiotique/action-plan-daction-eng.pdf
- Endnote 47
-
Office of the Auditor General of Canada. (2015). 2015 Spring Reports of the Auditor General of Canada Report 1—Antimicrobial Resistance. Retrieved from http://www.oag-bvg.gc.ca/internet/English/parl_oag_201504_01_e_40347.html#hd2a
- Endnote 48
-
Centre for Communicable Diseases and Infection Control. (2016-05). The Canadian Antimicrobial Resistance Surveillance System: Generic Presentation Slides. Retrieved from internal files
- Endnote 49
-
Public Health Agency of Canada. (2016-03-24). Terms of Reference: Infection Prevention and Control Expert Working Group. Retrieved from internal files
- Endnote 50
-
Public Health Agency of Canada. (2017-07-05). Deck: Defining and Supporting the Public Health Agency of Canada in Guidance Development. Retrieved from internal files