Modernizing preventive health care guideline development in Canada: A way forward
Download in PDF format
(13.31 MB, 104 pages)
Organization: Public Health Agency of Canada
Date published: 2025-06-13
Foreword by the Chair
Preventive health care is a cornerstone of a strong and equitable health care system — one that not only treats illness, but actively works to prevent it. Throughout my career in public health, research, and evidence-based policymaking, I have seen firsthand how preventive measures can improve health outcomes, reduce disparities, and strengthen health care systems. Enhancing our preventive health care framework is one of the most impactful ways we can enhance the well-being of all Canadians.
The Canadian Task Force on Preventive Health Care (CTFPHC) has long been a trusted voice in evidence-based guideline development and is internationally recognized for its work. As the health care landscape continues to evolve, so too must the structures and processes that guide it. The External Expert Review Panel, composed of thirteen experts from diverse fields, approached this work with a shared commitment to ensuring that the Task Force remains a leader in preventive health care — responsive to the needs of primary health care professionals and the public, as well as the provincial and territorial screening program managers, quality councils, and other key interest holders who support professionals and the public in the delivery of primary care and clinical preventive services.
Throughout this process, we listened to family physicians, medical specialists, other health care professionals and members of the public. In addition, we gathered perspectives from academic institutions, health professional associations, non-governmental organizations, provincial and territorial health authorities, and others. Their insights painted a clear picture: while the Task Force is widely respected for its scientific rigour, there is a pressing need to modernize its approach to be more inclusive, transparent, and responsive to the diverse realities of health care delivery across Canada. In particular, many emphasized the importance of ensuring that guidance is contextualizable — adaptable to different provincial and territorial systems, provider roles, and population needs — so that evidence-based recommendations can be meaningfully implemented where they matter most. In order to achieve everything that is expected of it, it needs to be adequately resourced and supported. Preventive health care is not static, and neither should be the structures that support it.
This report presents findings and recommendations that will not only bolster the Task Force's credibility but also enhance its ability to serve the evolving needs of primary care professionals and people living across Canada. By broadening the evidence base, embedding contextual flexibility into its methods, adopting more systematic, equity-centred engagement, and by strengthening governance, we can ensure that preventive health care guidelines remain both scientifically rigorous and practically relevant.
The recommendations in this report are not only about modernizing the approach but about ensuring that preventive health care remains responsive to evolving scientific evidence, inclusive of diverse perspectives, adaptable to real-world delivery settings and to local public health priorities.
At a time when misinformation and disinformation challenge public trust in health care, the role of independent, evidence-based bodies such as the Task Force has never been more vital. As this report was being prepared, the work of the Task Force was temporarily paused. It is essential that it be enabled and supported continuing its critical contributions to preventive health care in Canada.
I want to thank my fellow Panel members for bringing their knowledge, expertise and diversity of views to our meetings where openness and respect were not only evident but also felt. Their collaboration and dedication have been essential to fulfilling our mandate. I am also grateful to the many national and international experts and interest holders who contributed their time and expertise to this review, as well as the organizations that provided valuable insights and perspectives. They all helped to shape the recommendations outlined in this report.
This report is not the end of the conversation — it is the beginning of an important transformation. In the final section of this report, we make broader observations about the need for reform of the pan-Canadian approach to guideline development. I urge policymakers, health care leaders, and the public to embrace these ideas and work together in a coordinated approach to build a stronger, context-sensitive, and responsive approach to preventive health services and guideline development in Canada.
Vivek Goel, C.M., O.Ont.
Chair, External Expert Review Panel
March 2025
On this page
- Chapter 1: Introduction and context
- Chapter 2: Key findings
- 2.1 Redefining the mandate and strategic focus
- 2.2 Advancing evidence, methods, and guideline relevance
- 2.3 Embedding equity: Towards inclusive guideline development
- 2.4 Strengthening governance for inclusive and contextualizable guidance
- 2.5 Securing the foundations for sustainability and independence
- Chapter 3: Broader considerations
- Conclusion: A way forward
- Glossary
- Appendices
- Appendix 1: External expert review-terms of reference
- Appendix 2: External expert review members
- Appendix 3: Technical advisors
- Appendix 4: Persons who submitted a written presentation
- Appendix 5: Persons, interest holder organizations, government entities and academic institutions who provided input
- Appendix 6: Summary of interest holder submissions
- Appendix 7: Comparison with international guideline development organizations
- Appendix 8: Proposed organizational chart for the task force
- Figures
- References
- Footnotes
Acknowledgments
We extend our deepest gratitude to all those who contributed to this review and played a crucial role in shaping this report. First and foremost, we acknowledge the invaluable guidance and expertise provided by the dedicated secretariat within the Public Health Agency of Canada. Under the distinguished leadership of Dr. Howard Njoo, Deputy Chief Public Health Officer, and Director General Marie-Hélène Lévesque, the team provided steadfast support throughout the review process. In particular, we express our sincere appreciation to Mariellen Chisholm, Kim Davis, Sylvie Desjardins, Ashley Gilbert, Vivianne Z. Lamoureux, and Marisha Tardif for their unwavering commitment and exceptional efforts.
We are also profoundly grateful for the counsel and contributions of our technical advisors, whose diverse expertise in public health, policy, research, and public engagement helped refine our analysis and enhanced the rigour of our findings. Their insightful feedback, rigorous review, and meaningful engagement in key discussions significantly strengthened the coherence and credibility of this report.
Furthermore, we extend our appreciation to the key presenters who generously shared their knowledge and perspectives on national and international best practices on topics surrounding guideline development. Their insights provided valuable context, deepened our understanding of emerging challenges, and helped shape our recommendations.
We were equally fortunate to engage with a diverse range of individuals and interest holder groups from across the country, whose thoughtful input greatly contributed to our work.
While these contributions have been instrumental in shaping this report, we assume full responsibility for its content, including any remaining limitations or errors. The interpretations, conclusions, and recommendations presented herein reflect our independent assessment and judgment.
List of acronyms
- AI
- Artificial Intelligence
- CIHR
- Canadian Institutes of Health Research
- COI
- Conflict of Interest
- CTFPHC
- Canadian Task Force on Preventive Health Care (Task Force)
- EAB
- External Advisory Body
- EER
- External Expert Review
- ERSC
- Evidence Review and Synthesis Centre
- GRADE
- Grading of Recommendations Assessment, Development and Evaluation
- HHS
- Health and Human Services (federal department in the United States)
- KT
- Knowledge Translation
- NACI
- National Advisory Committee on Immunization
- NHMRC
- National Health and Medical Research Council
- NICE
- National Institute for Health and Care Excellence
- PHAC
- Public Health Agency of Canada
- PT
- Provinces and Territories
- RCT
- Randomized Controlled Trial
- SME
- Subject Matter Expert
- SPOR
- Strategy for Patient-Oriented Research
- TF-PAN
- Task Force Public Advisors Network
- UK
- United Kingdom
- USPSTF
- United States Preventive Services Task Force
- US
- United States
- WG
- Working Group
Executive summary
In May 2024, the Minister of Health directed the Public Health Agency of Canada (PHAC) to initiate an external review of the Canadian Task Force on Preventive Health Care (CTFPHC — hereafter referred to as the Task Force). The review assessed the Task Force's governance, mandate, and processes.
Composed of a Panel of thirteen independent experts, the External Expert Review (EER — hereafter referred to as the Panel) was asked to provide actionable recommendations to enhance the Task Force's capacity to support Canada's health care system, using primary health care as the vehicle to improving population health outcomes.
The Panel conducted focused assessments, engaged with a wide range of interest holders, and reviewed international comparators and expert analyses to identify strategic opportunities for modernizing the Task Force. As Canada's preventive health landscape continues to evolve, the Task Force must adapt to better serve the needs of patients, families, and caregivers — as well as those of diverse primary care health professionals, and the provincial programs and quality councils that support them.
This evolution is critical to ensuring that Task Force guidance remains rigorous, inclusive, contextualizable, and responsive to real-world practice.
The vision guiding this review is to ensure that everyone in Canada regardless of geography, background, socioeconomic status, or identity — including those from equity-denied groups such as Indigenous and Black communities — has access to high-quality, equity-centred, context-sensitive, evidence-based, and coordinated guidance on preventive health services.
The Task Force plays a central role in delivering scientifically sound recommendations to support preventive health care in clinical settings across the country. To better align the Task Force with current system realities and ensure long-term effectiveness, this report presents twelve recommendations that provide a clear and coherent roadmap for modernization, strengthened governance, and stable operational support. It also includes three supplementary recommendations aimed at addressing broader system-wide challenges and advancing national coordination in preventive health guideline development.
A. Reframe the mandate to reflect today's health system
- Modernize the mandate and rename the Task Force (Recommendation 1): PHAC should establish a clear and updated mandate for the Task Force that reflects its evolving role in supporting the delivery of preventive health services. This mandate should focus on the development of guidance that is inclusive, up-to-date, equity-centred and contextualizable for frontline health professionals. As part of this realignment, PHAC should consider renaming the group as the Canadian Task Force on Preventive Health Services to better reflect its focus on the full spectrum of preventive interventions delivered in primary care settings.
- Clarify the Task Force's role in a crowded landscape (Recommendation 2): PHAC should establish a recurring, structured process to determine when the Task Force should lead the development of new preventive health guidelines, and when it would be more efficient to adopt or adapt existing high-quality recommendations from other sources. This process should be guided by a transparent prioritization framework and inform an annual workplan that sets the Task Force's strategic direction over a three-year horizon. By clarifying the Task Force's role within Canada's broader guideline ecosystem, this approach will reduce duplication, improve coordination, and address fragmentation across the system.
B. Strengthen methods and evidence use for relevance and rigour
- Evolve the Task Force methodological framework (Recommendation 3): PHAC should enable and support the Task Force to streamline its methodological framework, building on the evolving GRADE approach — particularly Core GRADE — to ensure rigorous and inclusive guideline development. This should be supplemented with additional evidence-to-decision frameworks suited to supporting recommendations for equity-denied populations and in areas where evidence is limited or emerging. PHAC should also support the refinement of methods and communication strategies for population-based interventions that are clinically applied in primary care (e.g., screening), ensuring clarity and relevance for diverse audiences.
- Implement a phased living guidelines model (Recommendation 4): PHAC should enable and support the Task Force to implement a phased approach to maintaining and updating high priority guidelines using living methods. This includes continuous evidence monitoring, the use of emerging technologies, and collaboration with international partners. PHAC should seize opportunities to share in evidence infrastructure to enable greater efficiency and lower redundancy. This approach will also allow provinces and territories to rely on shared evidence and focus their efforts on contextualizing guidance for their own service delivery models.
- Strengthen practice adoption through partnership and adaptation (Recommendation 5): PHAC should enable and support the Task Force in collaborating with provincial and territorial partners to support the system-level conditions necessary for the effective implementation of preventive health service guidelines. This includes structured engagement with prevention intervention delivery programs, quality councils, and other implementation and evaluation partners to co-develop practical tools and identify barriers and enablers across diverse care settings. Each guideline cycle should integrate knowledge translation resources — such as provider decision aids, implementation toolkits, and user-specific summaries — tailored to the needs of primary care teams and the systems that support them. PHAC should also support the development of mechanisms to assess feasibility, uptake, and impacts in coordination with jurisdictions.
C. Embed equity and public voice in guideline development
- Prioritize equity in topic selection (Recommendation 6): PHAC should support the Task Force in applying transparent, equity-focused criteria to topic selection, with a focus on equity-denied populations — including Black and Indigenous communities — and the priorities of provinces and territories. A topic sequencing approach should guide progress toward full preventive service coverage, while also addressing current uneven coverage of guideline topics — such as duplication in some areas (e.g., cancer) and lack of guidance in others (e.g., mental health). Topic framing should emphasize opportunities to improve outcomes across the health system, especially in areas that support health equity and align with the quadruple aim.Footnote 1
- Establish a model for equity-centred patient and public engagement (Recommendation 7): PHAC should enable and support the Task Force to adopt structured, consistent mechanisms for engaging patients, community groups — including Black, Indigenous and other communities historically underrepresented in health policy and clinical decision-making —, and the public throughout guideline development, ensuring that lived experience, patient preferences and community values are meaningfully reflected in final recommendations.
D. Enhance governance, membership, and expert input
- Build a competency-based and inclusive membership and nomination framework (Recommendation 8): PHAC should enable and support the Task Force to adopt an integrated framework for inclusive, competency-based membership and a transparent nomination process. This framework should define essential qualifications, expertise, and lived experience — ensuring representation from equity-denied communities and across primary care, public health, and Indigenous health systems. It should also establish a public nomination process, including clear eligibility criteria, targeted outreach, and an independent nominations committee with diverse representation. These measures will ensure the Task Force is equipped to develop guidance that is relevant, equitable, and contextualizable across Canada's diverse health systems.
- Formalize Subject Matter Expert (SME) engagement (Recommendation 9): PHAC should enable and support the Task Force to create structured roles for SMEs to contribute at key stages of guideline development working groups, without compromising the Task Force's independence in decision-making. This will support the integration of expertise from primary care practitioners alongside domain-specific expertise from specialists.
- Adopt a tiered Conflict of Interest (COI) Framework (Recommendation 10): PHAC should enable and support the Task Force to adopt a two-tier approach — distinguishing voting members on the Task Force from those participating in topic-specific working groups — to managing conflict of interest, enabling transparent and risk-proportionate participation of subject matter experts (SMEs).
E. Secure stable funding and operational infrastructure
- Establish long-term funding and secretariat support (Recommendation 11): To fulfill its mandate effectively, the Task Force requires stable, multi-year funding, including appropriate compensation for its members, when required. PHAC should support a dedicated or shared Secretariat to provide continuity, infrastructure, as well as methodological and operational support.
F. Transition to an accountable, independent governance model
- Reconstitute the Task Force as an External Advisory Body (Recommendation 12): PHAC should constitute the Task Force as an independent External Advisory Body, supported by transparent governance, formalized engagement with interest holders, and accountable decision-making processes.
Looking beyond the Task Force: System-wide coordination opportunities
Beyond the Task Force, the Panel identified broader systemic gaps that hinder Canada's ability to deliver guidelines for health professionals in a coordinated manner and equity-centred preventive health care at the clinical, community and population levels. These include the absence of a national body to assess evidence and provide recommendations on community-level interventions, limited coordination between research funders, data agencies, quality councils, and guideline development and implementation, and the lack of shared frameworks for engaging interest holders.
There is also an urgent need to ensure that guidelines are not only rigorous but also adaptable to the specific health system structures, population needs, and delivery contexts of each province and territory.
While beyond the formal mandate of the review, these challenges merit serious consideration. The Panel encourages federal leadership and collaboration with provinces and territories to explore structural solutions — such as a national coordination hub for evidence-based health guidelines, a dedicated Task Force on Community Preventive Services, and a network to enhance coordination with relevant agencies — to strengthen alignment and build a more inclusive, future-ready guideline and development preventive health system.
To this end, the Panel sets out three supplementary recommendations:
Supplementary recommendation A: Create a national coordination hub
The federal government, in collaboration with provincial and territorial partners, should explore the creation of a national coordination hub for guideline development — bringing together funders, health providers, researchers, and implementers to strengthen alignment, reduce duplication, and accelerate the translation of evidence into effective policy and practice. This hub should enable formal coordination across advisory and decision-making structures, including learning and improvement platforms, and support system-level integration. It should also help contextualize by enabling the adaptation of guidance to different provincial and territorial settings, supported by a shared infrastructure for producing localized summaries of key recommendations. This includes aligning funding mechanisms and operational enablers to embed a modernized, population-responsive approach to clinical practice guidelines development and implementation.
Supplementary recommendation B:
Launch a Task Force on Community Preventive Services: The federal government, in collaboration with provincial and territorial partners, is encouraged to explore the creation of a Task Force on Community Preventive Services, in collaboration with organizations such as the National Collaborating Centres for Public Health (NCCs), to provide independent, evidence-based guidance for public health and community-level interventions beyond clinical care.
Supplementary recommendation C:
Build a network for research, data, and evaluation alignment: The federal government is encouraged to establish a network to strengthen coordination with Canada's health research funders, data agencies, and quality councils. This network should also position Canada to engage with, and contribute to, an emerging global infrastructure for living evidence synthesis — enabling provinces and territories to access shared, high-quality evidence bases and focus their efforts on local adaptation, rather than duplicative evidence review and guidance development.
By acting on these insights, we can contribute to a more cohesive, coordinated, and forward-looking approach to preventive health — one that ensures all people in Canada have equitable access to up-to-date evidence-based guidance that promotes health and well-being across communities and generations.
Chapter 1: Introduction and context
1.1 External Expert Review Panel mandate
In May 2024, Canada's Minister of Health directed the Public Health Agency of Canada (PHAC) to launch an independent review of the Canadian Task Force on Preventive Health Care (CTFPHC — henceforth referred to as the Task Force). This review was tasked with examining the Task Force's governance, mandate, and processes, as well as providing actionable recommendations on modernizing its role and structure.
The goal was to ensure that its guidelines remain evidence-based, up-to-date, and relevant to primary care health professionals. This effort aims to align preventive health guidelines with the evolving needs of Canada's health care systems and to support equitable population health outcomes.
While concerns surrounding the Task Force's 2024 release of its draft breast cancer screening recommendations served as a catalyst for the review, the Panel was not tasked with reviewing or evaluating the specific events or decisions that led to their development.
1.2 Approach
PHAC appointed members to the External Expert Review (EER) in September 2024, establishing an independent Panel of thirteen experts to review the Task Force structure, governance, and scientific methods. The full terms of reference for the review are available in Appendix 1, while the biographies of Panel members can be reviewed in Appendix 2. Additionally, four Technical Advisors provided specialized insights into key areas such as medical research, public health, public engagement, and health equity. These experts played a critical role in ensuring that the review addressed both systemic challenges and patient-centred concerns. The biographies of Technical Advisors are included in Appendix 3.
The Review Panel began its work in October 2024, using a structured approach that considered previous assessments and evaluations of the Task Force, national and international best practices in guideline development and input from consultations. It concluded its mandate with the publication of this report.
The Panel consulted with national and international experts — including health care professionals, researchers, and patient representatives — to ensure the inclusion of a diverse range of perspectives. A full list of those consulted is available in Appendix 4.
The Panel also engaged directly with the current and former Task Force leadership and gathered public input through direct engagement and an open consultation process. This included written submissions and a series of roundtable discussions with individuals, health professional associations, non-governmental organizations and academic institutions. It also included engagement with guideline developers in Canada. A complete list of participants is presented in Appendix 5, and a summary of perspectives from the consultation is presented in the "What We Heard" report in Appendix 6.
To benchmark Canada's approach against international models and to identify best practices that could inform improvements to Canada's system, the Panel examined governance structures, interest holder engagement practices, and guideline development processes in the United Kingdom (UK), Australia, and the United States (US). An international comparative analysis is provided in Appendix 7.
To further contextualize its findings, the Panel conducted an extensive review of key documents on the Task Force's evolution, successes, and areas for improvement. The insights gathered through this process informed the Panel's recommendations to strengthen Canada's preventive health guideline development system.
Finally, the Panel has been intentional in its choice of wording throughout this report, recognizing that terminology plays a key role in shaping the vision for a modernized Task Force. Key terms — such as "equity-centred" — have been chosen to reflect a commitment to clarity, relevance, and precision. A detailed glossary is included at the end of the report to support consistent understanding.
1.3 Guiding principles for recommendations
To ensure that the review process was independent and transparent, the Panel adhered to three core principles intended to uphold public trust and strengthen the integrity of the review:
Independence: The review was carried out free of external influence, political pressure, or conflicts of interest, ensuring that findings and recommendations were based solely on evidence. The Panel appreciates the support provided by the Secretariat staff assigned by PHAC; an arm's length relationship was maintained throughout this process. The Panel held in-camera discussions as needed to support independent deliberations. The Panel assumes full responsibility for the content of this report.
Transparency and accountability: Openness and accountability were prioritized at every stage of the review. The Panel regularly discussed its mandate, methodology, and approach to consensus decision-making. To support transparency, summaries of each meeting were published, providing the public with information on the topics that were reviewed and discussed.
Inclusivity and equity: To build public confidence in the guideline development process, the Panel actively engaged a diverse range of interest holders, including health care professionals, researchers, patient representatives and the public, as well as methodologists. This approach ensured that multiple perspectives were considered throughout the review, strengthening the credibility and fairness of the process.
By upholding these principles, the Panel aimed to reinforce trust in the review process and to contribute meaningfully to the development of a more inclusive, responsive, and transparent preventive health care guideline system in Canada.
1.4 Report structure
This report is structured as follows to provide a comprehensive review of the Task Force, outlining key findings, recommendations, and a broader vision for the future.
Chapter 2 presents the key findings of the review. It examines the Task Force's scope, mandate, governance, and structure, while identifying strengths and areas for improvement. The Chapter also considers how the Task Force operates within the context of Canada's broader health system and identifies opportunities to enhance its impact and alignment with this evolving landscape.
Chapter 3 outlines broader considerations for the future. Building on insights gleaned during the Panel's consultation and deliberations, it proposes courses of action to modernize the wider ecosystem of guideline development in Canada. The chapter highlights concrete opportunities to expand the scope of guidelines to better address community and population health needs.
The Conclusion summarizes key insights and highlights the importance of adopting a more inclusive, transparent, and responsive approach to preventive health guideline development in Canada.
Chapter 2: Key findings
This chapter presents the key findings of the review for clinical preventive guideline development, highlighting both the strengths of the current approach, as well as areas for improvement. It synthesizes insights from interest holder consultations, expert analysis, and international comparisons, identifying opportunities for enhancing governance, inclusivity, transparency, and responsiveness. These findings underscore the need for modernization and serve as the groundwork for the Panel's recommendations.
2.1 Redefining the mandate and strategic focus
Since its establishment in 1976 as the Canadian Task Force on Periodic Health Examination, the Task Force has played a pivotal role in shaping Canada's approach to preventive health. Initially focused on routine check-ups, it evolved to support evidence-based targeted, preventive health services in primary care settings. It has earned international recognition for its contributions and has served as a model for similar bodies in other jurisdictions.
Throughout the 1980s, the Task Force pioneered guidelines on preventive screening for healthy individuals, emphasizing the importance of population-based approaches. This work helped to lay the foundation for what are now well-established screening programs for breast, cervical, and colorectal cancer across provinces and territories.
Although it was disbanded in 2005 following a decision by the Conference of Deputy Ministers of Health, the Task Force was re-established in 2009 with support from the Public Health Agency of Canada (PHAC). Since that time, it has developed clinical practice guidelines for primary care practitioners, with a particular focus on family physicians.
The Task Force has long been a trusted source of evidence-based recommendations. It has fulfilled its mandate with a strong emphasis on evidence-based medicine. However, as the structure of primary care services delivery and the organization of preventive services have evolved, so too must the Task Force's mandate to ensure it remains, inclusive, transparent, and responsive to the full spectrum of primary care providers, provincial and territorial implementation mechanisms, and the diverse needs of populations.
Adapting to a changing primary care landscape
Canada's primary care landscape is evolving from a physician-centric model to more interdisciplinary team-based care, with nurse practitioners, pharmacists, and other primary care health professionals now playing an increasingly significant role in delivering preventive health services. Simultaneously, the landscape is shifting from a model where physicians and teams independently manage all preventive health services to one in which they, alongside their patients, increasingly rely on provincial programs and quality councils for support. Despite this shift, the Task Force's recommendations are still largely perceived as physician-oriented, limiting their accessibility and applicability across the broader primary care workforce and its support structures.
Beyond primary care, Task Force recommendations often influence population and public health programs, including provincial screening initiatives. While these guidelines are developed with clinical practice in mind, their impact extends far beyond individual primary care providers, shaping broader public health policies and service delivery at the population level. This underscores the importance of ensuring that guidelines are not only relevant to primary care health professionals, but also effectively align with public health programs and quality councils to maximize their reach and effectiveness.
The delivery of preventive health services continues to evolve, with provinces and territories expanding their cancer screening programs over the years and developing tailored guidelines to support them. To ensure coherence, guideline development needs to be coordinated with provincial and territorial programs and quality councils.
To enhance its impact, the modernized Task Force must explicitly integrate the perspectives of a broader range of primary care providers and ensure its guidelines are inclusive, relevant, contextualizable, and responsive to the operational realities of diverse health care settings — particularly those built around team-based care. Reframing its recommendations as "guidelines on preventive health services for primary care health professionals and teams" will reinforce their practical application across different clinical settings and team structures. While family physicians continue to play a central role in preventive health services, other leading interest holders such as public health, other primary care health professionals, and provincial and territorial screening program managers and quality councils, among others, would benefit from the knowledge translation tools and resources necessary to seamlessly implement evidence-based guidelines in policy and practice. Embedding contextual adaptability into the guideline development cycle will also help ensure that recommendations remain relevant and adaptable to different models of team-based care and evolving delivery contexts.
Furthermore, many people in Canada lack regular access to primary care, including to physicians and other health professionals. Guidelines must be flexible and adaptable to account for different patterns of access across jurisdictions — ensuring they remain meaningful even in non-traditional care settings. The implementation of preventive health services guidelines must consider how these populations may access preventive care through alternate health services, such as walk-in clinics or emergency departments, while also acknowledging that some individuals do not consistently engage with any health care services.
The Panel heard concerns that physicians with expertise in diagnosing and managing specific diseases were not consistently included in the Task Force's work. Some interest holders expressed that guidelines on specific diseases should be developed and led by specialists in that field. We recognize that greater engagement with subject matter experts (SMEs) is necessary to incorporate their scientific and clinical expertise. However, the expertise required for developing guidelines for preventive health services targeted at healthy individuals at the population level goes beyond subject matter expertise. Primary care and public health practitioners are uniquely trained to work with healthy individuals, communities and populations, and their expertise and leadership remains essential to the development of preventive service guidelines.
Similarly, the lived experience of patients with specific diseases is invaluable in the development of disease-specific guidelines and knowledge translation tools, particularly concerning treatment. The development of preventive health services guidelines for healthy individuals should also incorporate the perspectives of those without the disease, as well as individuals who may have experienced unexpected negative outcomes related to recommended preventive health services — such as false positives, overdiagnosis, overtreatment, and psychological distress.
Since the Task Force operates independently of provincial and territorial health care systems, its role is to inform — not implement — PT policy decisions. However, the absence of a structured liaison mechanism limits alignment across national, provincial and territorial levels. Establishing such a mechanism is essential to strengthen coordination and ensure greater policy coherence and practice-level impacts.
Navigating a fragmented preventive care landscape
The landscape of guideline development in Canada is becoming increasingly complex and fragmented. Provincial and territorial health agencies, professional associations, specialist societies and the private sector each independently issue their own recommendations for preventive care and public health practice. Figure 1 shows the rapid growth in all guidelines being produced on an annual basis across organizations, with this likely being an underestimate of the total (SPOR Evidence Alliance, 2025).
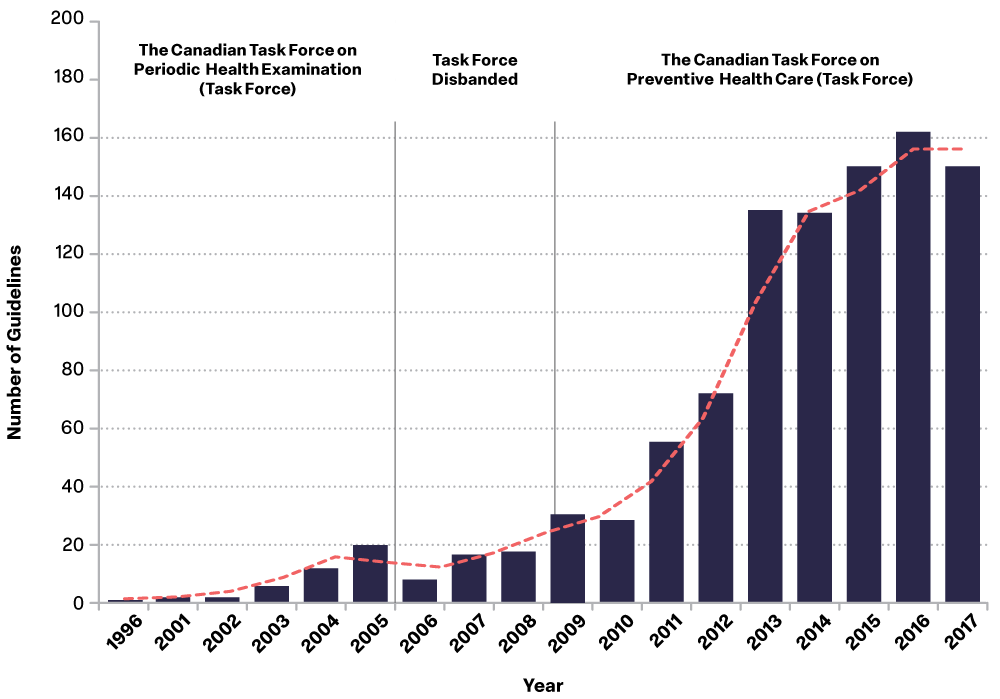
Figure 1: Text description
Figure 1 shows the total number of national preventive health guidelines published in Canada each year from 1996 to 2017. It reflects contributions from various organizations, including the Task Force, and is divided into three phases based on changes in the Task Force's structure and activity over time.
Phase 1 (1996-2005):
During this period, the Canadian Task Force on the Periodic Health Examination was active and contributed to the development of national guidelines. Overall guideline production was relatively modest but gradually increased. In 1996, only 1 national guideline was published. This number rose to 12 by 2004 and reached 20 in 2005.
| Guidelines published in Canada | 1996 | 2001 | 2002 | 2003 | 2004 |
|---|---|---|---|---|---|
| Total | 1 | 2 | 2 | 6 | 12 |
Phase 2 (2005-2008):
The Task Force was disbanded during these years. Despite this, some national guidelines continued to be developed by other organizations, though at a slower pace. Between 2005 and 2008, the total number of guidelines published each year ranged from 8 to 18.
| Guidelines published in Canada | 2005 | 2006 | 2007 | 2008 |
|---|---|---|---|---|
| Total | 20 | 8 | 17 | 18 |
Phase 3 (2009-2017):
In 2009, the Task Force was re-established and became a significant contributor to national guideline development. During this period, the number of guidelines published nationally rose sharply. From 31 guidelines in 2009, the total grew to a peak of 164 in 2016. In 2017, 152 guidelines were published, still far above the levels seen in earlier years.
| Guidelines published in Canada | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 |
|---|---|---|---|---|---|---|---|---|---|
| Total | 31 | 29 | 56 | 73 | 137 | 136 | 152 | 164 | 152 |
This can lead to overlapping, inconsistently produced, and sometimes conflicting guidance, creating uncertainty for primary care providers, patients and the public. Additionally, guideline development can also inadvertently focus on specific health topics, driven by factors such as changing research priorities, advocacy, or available funding.
As highlighted in Figure 2, considerable effort is already directed toward cancer guidelines. As a result, gaps may emerge in key areas such as mental health screening and chronic disease prevention.
To address this problem of uneven coverage and fragmentation, an appropriate working group within a Federal-Provincial-Territorial mechanism should be developed to support pan-Canadian collaboration in preventive health service guideline development. This group should help clarify and coordinate the Task Force's role in leading, adopting, or adapting guidelines that fall within its mandate.
Establishing a structured mechanism for sharing and aligning recommendations with other guideline developers — including provincial and territorial programs — would help create a more consistent approach to preventive care, promoting alignment and reducing duplication. This engagement could also lay the groundwork for future efforts to draw on the emerging global infrastructure for living evidence syntheses and to adapt or adopt high-quality guidelines developed in other countries and globally.
The Task Force should focus its efforts on addressing gaps in preventive health services rather than developing recommendations when strong, evidence-based guidelines already exist at the provincial, territorial, or national level. A clear process for determining when the Task Force should lead, adopt, or adapt guidance will reduce duplication, support alignment, and maximize its contributions across the system.
In areas where well-established evidence-based processes within other services exist — such as in provincial cancer screening programs — the Task Force should reassess its involvement to focus on areas where its contributions add the most value, enhancing consistency and maximizing its impact. Ultimately, the goal should be to ensure that guidance is available for all preventive interventions across the life course.
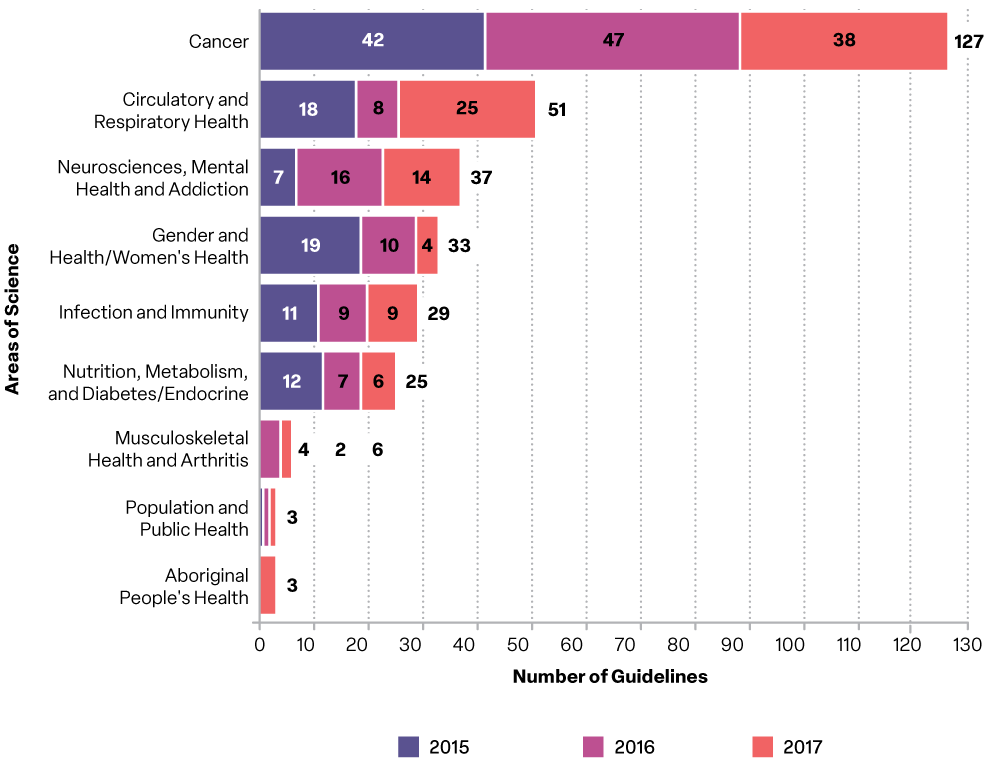
Figure 2: Text description
Figure 2 displays the number of national preventive health guidelines published in Canada by scientific area for 2015, 2016, and 2017, with a total count for each area over the three-year period.
- Cancer had the highest number overall, with 127 guidelines published: 42 in 2015, 47 in 2016, and 38 in 2017.
- Circulatory and Respiratory Health followed with 51 guidelines, showing steady attention to this area.
- Neurosciences, Mental Health and Addiction had 37 guidelines, mostly in 2015 and 2016.
- Gender and Women's Health saw 33 guidelines, with a notable peak in 2015 (19 guidelines).
- Infection and Immunity had 29 guidelines, fairly evenly spread across the three years.
- Nutrition, Metabolism, and Diabetes/Endocrine had 25 guidelines, with a clear increase in 2017.
- Musculoskeletal Health and Arthritis accounted for 6 guidelines, mostly in the first two years.
- Population and Public Health had 3 guidelines, with one published each year.
- Aboriginal People's Health also had 3 guidelines, all published in 2016 and 2017.
This breakdown shows that while a range of topics are covered, the focus remains concentrated on cancer and chronic diseases, with notable gaps in other preventive areas.
Over the course of the Panel's consultation process, a number of interest holders highlighted the need for greater attention to upstream determinants of health and to guidance on primordial prevention.Footnote 2 The Panel believes that a modernized Task Force should maintain a focused mandate on preventive health services for primary care health professionals to ensure its recommendations are clear, targeted, and directly relevant to primary care practice.
As discussed in Chapter 3, the Panel suggests that PHAC explore options — such as increased coordination with the National Collaborating Centres for Public Health or a separate community-focused Task Force — to address the important gaps identified for guidance on primordial prevention.
Making guidelines work: The need for contextualizable preventive health guidance
Given these challenges and opportunities, the Panel believes that a modernized Task Force must adopt an approach to guidance that is not only evidence-based but also operationally relevant across Canada's diverse health systems.
To be effective across Canada's diverse health systems, preventive health guidelines must be designed as contextualizable — meaning they can be adapted to local realities, while preserving scientific integrity. This includes aligning with the organizational structures, resources, populations, and policy environments that vary across provinces and territories. Without this adaptability, even rigorously developed guidelines may remain underutilized, misunderstood, or poorly integrated into local practice.
Currently, Task Force recommendations are typically issued as universal guidance with limited support for local adaptation. This places the burden of contextualization on provinces, territories, and local health professionals, many of whom must reinterpret or redevelop guidance to ensure relevance within their systems. This leads to duplicated efforts, resource inefficiencies, and slower uptake, and can also increase the risk of misalignment with existing provincial and territorial programs or health priorities.
Embedding contextual adaptability into the Task Force's approach can resolve many of these issues. It allows for provincial and territorial health systems to tailor implementation based on their existing infrastructure, patient needs, and workforce capacity. It also supports primary care professionals — whether in large urban centres or rural areas — in applying guidelines in a way that fits their specific operational and community contexts.
Crucially, contextualizable guidance can help close equity gaps. It enables targeted adaptation to meet the needs of underserved or equity-denied populations, whose access to preventive care may be shaped by social determinants of health, geographic barriers, or systemic inequities. By encouraging alignment with local priorities and realities, contextualization supports a more inclusive and impactful approach to population health.
However, the Task Force currently lacks the capacity to routinely produce contextualized summaries or implementation supports. Embedding role clarity at the outset — whether the Task Force is producing new guidance or adapting existing sources — will make contextualization efforts more focused and efficient. In the short term, the most effective step may be to engage provinces and territories directly in the guideline development process, ensuring that their system-level realities and delivery models inform upstream decisions. This could take the form of structured collaboration with provincial screening programs, professional networks, and implementation bodies.
Looking ahead, the development of a national coordination hub — as proposed in Chapter 3 — offers an opportunity to build the infrastructure needed to support contextualization at scale. Such a hub could also support a recurring prioritization process, helping to define when the Task Force should develop guidance, versus when it should adopt or adapt existing materials. A hub could also facilitate information sharing and leveraging findings from open-source living evidence syntheses, as well as practical tools that provinces and territories can use to adapt guidelines efficiently. This approach would allow the Task Force to focus on scientific integrity while enabling local partners to translate recommendations into meaningful action and engagement with global partners to share work.
Ultimately, embedding contextualization within the Task Force's mandate will improve the clarity, usability, and reach of its guidance — ensuring that preventive health services are not only evidence-based, but also aligned with local delivery realities and equitably implemented across regions.
Recommendation 1: Modernize the mandate and rename the Task Force
PHAC should establish a clear and updated mandate for the Task Force that reflects its evolving role in supporting the delivery of preventive health services. This mandate should focus on the development of guidance that is inclusive, up-to-date, equity-centred and contextualizable for frontline health professionals. As part of this realignment, PHAC should consider renaming the group as the Canadian Task Force on Preventive Health Services to better reflect its focus on the full spectrum of preventive interventions delivered in primary care settings.
To support a modernized and future-ready Task Force, PHAC should revise its mandate to clearly define its role in addressing gaps in preventive health services through up-to-date, inclusive, and equity-centred guidance. This renewed mandate should go beyond consultation with key interest holders to include formalized alignments with provincial and territorial advisory and decision-making processes — including screening programs — and out to learning and improvement platforms (e.g., quality councils).
As part of the renewal, PHAC should consider renaming the Task Force to the Canadian Task Force on Preventive Health Services to reflect its full scope.
These updates should be formalized through revised terms of reference, a new mandate letter, and corresponding updates to governance, performance expectations, and funding agreements.
PHAC should also coordinate the development of an annual workplan, in which the Task Force outlines its upcoming priorities within a standard three-year planning horizon, adjusted yearly. This workplan should be shared with relevant provincial and territorial committees as well as other key interest holders to support priority setting, ranking, and the coordinated organization of work.
Recommendation 2: Clarify the Task Force's role in a crowded landscape
PHAC should establish a recurring, structured process to determine when the Task Force should lead the development of new preventive health guidelines, and when it would be more efficient to adopt or adapt existing high-quality recommendations from other sources. This process should be guided by a transparent prioritization framework and inform an annual workplan that sets the Task Force's strategic direction over a three-year horizon. By clarifying the Task Force's role within Canada's broader guideline ecosystem, this approach will reduce duplication, improve coordination, and address fragmentation across the system.
To ensure coordination and reduce duplication, PHAC should implement a structured recurring process to clarify the most appropriate role for the Task Force — whether to lead on emerging guideline topics, or to adopt or adapt existing high-quality recommendations. This process should be supported by a transparent methodological framework for topic prioritization that is co-developed with key interest holders (including provinces and territories) and which takes into account population needs, existing guidance from other national or provincial developers, and resource considerations. Once established, it should be applied consistently at the beginning of each planning cycle and integrated into the Task Force's reporting and accountability structures to support alignment, efficiency, and systemwide value.
Summary: Modernizing the Task Force mandate
Modernizing the Task Force's mandate is essential to ensuring its continued relevance and effectiveness in a rapidly evolving health system. Recommendations 1 and 2 call for a refocused mandate that clearly defines the Task Force's role in providing inclusive, evidence-based, and equity-centred and contextualizable guidance on preventive health services for all primary care health professionals. This includes renaming the Task Force to better reflect its expanded focus and responsibilities. To promote alignment and reduce duplication across Canada's guideline ecosystem, PHAC should also implement a structured recurring process to determine when the Task Force should develop new guidance, adopt existing high-quality guidance from other sources, or adapt existing recommendations. This process should be supported by a transparent methodological framework for activity prioritization, grounded in evidence gaps, population needs, and resource considerations. Embedding contextual adaptability as a design principle will also help ensure that recommendations can be meaningfully adapted across jurisdictions — supporting implementation and improving equity. Together, these actions will clarify the Task Force's strategic focus, reinforce its value across jurisdictions, and support a more coordinated, applicable and efficient approach to preventive care guidance.
2.2 Advancing evidence, methods, and guideline relevance
In today's rapidly evolving health systems, modernizing the Task Force's methodological approach is essential. Expectations for preventive health guidelines have increased: they must not only be based on the best available evidence, but also be relevant to diverse clinical settings, contextualizable within (and ideally supported by appropriate) health system arrangements, sensitive to health inequities, and reflective of diverse forms of lived experience. Improving the inclusiveness, applicability, and impact of recommendations requires updating how evidence is defined, appraised, and applied.
Streamlining and expanding methodological approaches
Developing high-quality preventive health services guidelines requires a methodological approach and an evidence review and recommendation development process that is not only scientifically rigorous but also structured to support contextualizable applications across the diversity of real-world health care.
The GRADE (Grading of Recommendations Assessment, Development and Evaluation) methodology has long served as the cornerstone of the Task Force's approach. Its transparent and structured process has contributed significantly to the scientific credibility of its recommendations. However, in a context where preventive interventions are increasingly interdisciplinary, community-based, and equity-centred, over-reliance on GRADE can become limiting.
To address such challenges, the Task Force should streamline its methodological framework by building on the evolving GRADE approach — in particular, the development of core GRADE, which seeks to reconcile disparate guidance and provide a more coherent foundation (Iorio, 2024). Core GRADE offers a more flexible and current foundation for weighting diverse forms of evidence across various types of interventions. This should be supplemented with additional evidence-to-decision frameworks to support the development of guidelines in areas where evidence is limited or emerging — particularly for equity-denied populations.
While "Evidence to Decision" (EtD) tables are typically published, interest holders have raised concerns about the subjectivity in interpreting criteria, especially in the absence of a full evidence review. Ongoing concerns persist about how working groups weigh different criteria to determine thresholds for recommendations (e.g., in cancer screening).
To address these limitations, the Task Force should consider incorporating complementary frameworks that allow for the structured and transparent mapping of the rationale behind recommendations. These tools would not replace GRADE, but rather strengthen its application — particularly in cases where value judgments must be made explicit, where complexity and contextual factors influence implementation across jurisdictions, or where evidence is limited and equity considerations have historically been overlooked.
In parallel, methods and communications should be refined to clearly distinguish between primary care interventions targeting individuals and population-based interventions (like screening) that are clinically applied. This distinction is essential to ensure that recommendations are interpreted and applied appropriately across clinical communities and system-level settings.
A more inclusive and pluralistic approach — informed by transparent, equity-centred appraisal criteria and enhanced methodological clarity — would strengthen the scientific foundations of recommendations and help foster more equitable health outcomes nationwide.
Recommendation 3: Evolve the Task Force methodological framework
PHAC should enable and support the Task Force to streamline its methodological framework, building on the evolving GRADE approach — particularly Core GRADE — to ensure rigorous and inclusive guideline development. This should be supplemented with additional evidence-to-decision frameworks suited to supporting recommendations for equity-denied populations and in areas where evidence is limited or emerging.
PHAC should also support the refinement of methods and communication strategies for population-based interventions that are clinically applied in primary care (e.g., screening), ensuring clarity and relevance for diverse audiences.
We do note that GRADE is regularly updated and has evolved to allow for a broad range of methodological approaches to be integrated into guideline development. For example, core GRADE is the latest evolution, which takes disparate, sometimes contradictory guidance in GRADE papers and helps to create a coherent whole.
Preventive services involve offering interventions to individuals who are generally healthy. As a result, assessing the balance of potential benefits and harms is significantly more complex than in clinical contexts involving diagnosis and treatment. This complexity often requires consideration of a broader range of evidence such as observational studies, economic modelling, and qualitative research.
Transitioning to a living guidelines model
To keep pace with emerging evidence and evolving practice, the Task Force should gradually transition to a living guidelines model — one that responds to new research findings on a continuous basis.
The COVID-19 pandemic demonstrated the importance of timely, evidence-based updates and highlighted the value of real-time synthesis and international collaboration in adapting to rapidly changing conditions and evidence.
Given the complexity of this transition, the Panel recommends a phased and flexible approach. This should begin with a limited number of high-priority topics and use a hybrid approach — adapting trusted international guidelines where appropriate, while developing Canadian-specific recommendations in areas requiring local context, enabling the Task Force to build capacity incrementally and gradually expand toward the full spectrum of preventive health services, while ensuring contextual relevance and operational efficiency.
International collaboration will be essential to this strategy. Emerging initiatives — such as the Evidence Synthesis Infrastructure Collaborative (working across health and many other sectors) and the Alliance for Living Evidence on Anxiety, Depression, and Psychosis (working in a specific part of the health sector) — demonstrate the potential of shared platforms to enable real-time synthesis, reduce costs, and expand access to high-quality evidence. By engaging with global efforts, the Task Force can contribute to and benefit from innovative efforts to improve the efficiency of preventive health guideline development.
PHAC should explore opportunities to scale up the application of promising digital tools (for example, Artificial Intelligence (AI) assisted evidence synthesis, or automated literature surveillance), which are currently in pilot stages within the Agency. These technologies can help streamline the process of updating guidelines, reduce workload, and improve timeliness. Pilot projects focused on select guidelines can serve as test cases to assess operational feasibility, user experience, and equity.
To ensure success, this transition must be supported by sustained investment, dedicated staffing, and robust infrastructure. It will also require attention to equity — ensuring that living updates remain inclusive, accessible, and adaptable across diverse health care settings and populations in Canada.
Recommendation 4: Implement a phased living guidelines model
PHAC should enable and support the Task Force to implement a phased approach to maintaining and updating high priority guidelines using living methods. This includes continuous evidence monitoring, the use of emerging technologies, and collaboration with international partners. PHAC should seize opportunities to share in evidence infrastructure to enable greater efficiency and lower redundancy. This approach will also allow provinces and territories to rely on shared evidence and focus their efforts on contextualizing guidance for their own service delivery models.
PHAC should support the Task Force in phasing in a living guideline model and continuous evidence monitoring — beginning with a gradual approach focused on high-priority topics — to ensure that guidelines remain current, relevant and responsive to changing context and emerging evidence. This should include identifying suitable guideline areas, establishing continuous evidence surveillance mechanisms, and applying continuous reassessment protocols. PHAC should also scale up established and emerging digital tools currently in pilot stages within the Agency and provide the operational infrastructure and staff required for sustainable implementation. Partnerships with international organizations and methodologists experienced in living guideline models can accelerate capacity building and ensure alignment with global best practices. This phased transition should ultimately enable the expansion of living guidelines across the full spectrum of preventive services, ensuring recommendations are up-to-date, as well as applicable to Canada's diverse health care systems.
Supporting the equitable uptake of preventive health guidelines
To ensure that preventive health services guidelines are not only evidence-based but also effectively implemented across Canada's diverse health care settings, the Task Force should strengthen its capacity to assess feasibility, uptake, and equity impacts. Currently, limited capacity exists within the Task Force to evaluate how its recommendations are applied in practice or to support adaptive implementation. Without such mechanisms, valuable insights are missed, and gaps in equitable service delivery may persist.
To address this, the Task Force should establish an implementation and impact support framework as part of its guideline development process. This framework should include structured engagement with relevant provincial and territorial bodies — such as screening programs and quality councils, where these exist, and preventive service delivery organizations — to identify practical enablers and barriers, align with local resources and support a system-wide implementation planning.
This shift does not require creating new structures but rather is based on strengthening alignment and partnership with existing implementation actors that are already well positioned to support implementation — such as screening programs and quality councils, and electronic health records initiatives. Each guideline cycle should include co-developed knowledge translation tools — such as provider decision aids, user-specific summaries, and implementation toolkits — tailored to primary care professionals and public health programs. As part of this effort, particular attention should be given to improving the clarity and accessibility of communications about risks and benefits associated with Task Force recommendations, ensuring that both providers and the public are equipped to make informed decisions.
PHAC should support this work by providing the necessary resources and technical expertise to co-develop these tools and ensure their broad dissemination. By embedding implementation planning and real world monitoring and light-touch evaluation into its core functions, the Task Force will improve the reach, relevance, and population-level impact of its preventive service guidance — particularly for underserved populations and in under-resourced settings.
Recommendation 5: Strengthen practice adoption through partnership and adaptation
PHAC should enable and support the Task Force in collaborating with provincial and territorial partners to support the system-level conditions necessary for the effective implementation of preventive health service guidelines. This includes structured engagement with prevention intervention delivery programs, quality councils, and other implementation and evaluation partners to co-develop practical tools and identify barriers and enablers across diverse care settings. Each guideline cycle should integrate knowledge translation resources — such as provider decision aids, implementation toolkits, and user-specific summaries — tailored to the needs of primary care teams and the systems that support them. PHAC should also support the development of mechanisms to assess feasibility, uptake, and impacts in coordination with jurisdictions.
Rather than focusing solely on individual clinician behaviour, this approach emphasizes working alongside health system actors to adapt and strengthen programs, policies, and operational infrastructure — ensuring that Task Force recommendations are not only evidence-based, but also deliverable in practice. By fostering ongoing collaboration with provincial and territorial implementation partners, the Task Force can narrow the gap between evidence and action to support a more consistent adoption of preventive health recommendations.
Summary: Modernizing evidence synthesis and review
To maintain the relevance, equity, and impact of its recommendations, the Task Force must modernize its methodological approach. This involves thoughtfully broadening the types of evidence considered, integrating complementary frameworks alongside GRADE, and enhancing transparency in decision-making processes. Embracing a living guidelines model will facilitate continuous updates based on emerging evidence, increasing responsiveness and relevance. PHAC can support this evolution through strategic investments in digital tools, international collaboration, and a phased implementation strategy. Strengthening engagement with provincial and territorial implementation partners will help ensure that Task Force recommendations are not only evidence-based but also deliverable in practice, fostering consistent adoption and narrowing the gap between evidence and action.
2.3 Embedding equity: Towards inclusive guideline development
Embedding equity at every stage of the guideline development process is critical to ensuring that preventive health recommendations are relevant, actionable, and inclusive for all people in Canada. While the Task Force has established a strong foundation in evidence-based guidance, equity considerations are not yet systematically embedded across all stages — from topic framing and evidence review to interest holder engagement and implementation planning. Without a deliberate and structured approach, guidelines risk unintentionally reinforcing existing disparities by overlooking the unique needs and lived experience of Indigenous, Black, rural, and other equity-denied communities.
Moreover, without clear equity-centred criteria to guide prioritization, health conditions that disproportionately affect equity-denied populations may continue to receive insufficient attention. Strengthening the integration of equity considerations stands to enhance the real-world relevance, credibility, and impact of Task Force recommendations, ultimately supporting more equitable health outcomes nationwide.
Enhancing transparency in topic selection
A transparent and equity-driven approach to topic selection is a key first step. To ensure that preventive service guidelines address the most pressing health needs — particularly those affecting populations facing systemic barriers to care — the Task Force must improve the clarity and consistency of its topic selection process.
Interest holders expressed concerns about the lack of transparency in how topics are prioritized and on the absence of clear, equity-sensitive criteria. Some expressed that it is not clear how or why specific topics are chosen, or how population needs, health equity, or system impacts are factored into these decisions.
Conditions such as chronic disease prevention or mental health screenings — both of which disproportionately impact marginalized groups — have not always received sufficient focus under the current approach (Georgiades, 2021; Price et al., 2013). This risks perpetuating the very disparities that preventive guidance is meant to address.
To build trust, ensure responsiveness, and promote accountability, the Task Force should implement a structured and transparent topic selection framework that explicitly incorporates equity considerations. The framework should explicitly include clear, public-facing criteria such as potential equity impact, disease burden, relevance to primary care practice, and the extent of current guidelines gaps. It should also be developed in collaboration with provincial and territorial partners and informed by the lived experience of diverse interest holders.
Embedding equity in topic selection is not only a matter of fairness — it is essential to ensuring that future guidelines are targeted, aligned with population needs, and capable of driving meaningful improvements in health equity and system performance.
Recommendation 6: Prioritize equity in topic selection
PHAC should support the Task Force in applying transparent, equity-focused criteria to topic selection, with a focus on equity-denied populations — including Black and Indigenous communities — and the priorities of provinces and territories. A topic sequencing approach should guide progress toward full preventive service coverage, while also addressing current uneven coverage of guideline topics — such as duplication in some areas (e.g., cancer) and lack of guidance in others (e.g., mental health). Topic framing should emphasize opportunities to improve outcomes across the health system, especially in areas that support health equity and align with the quadruple aim.Footnote 1
To strengthen equity in guideline development, PHAC should enable and support the Task Force to adopt a transparent and equity-centred approach to topic selection — one that explicitly prioritizes equity-denied populations and aligns with provincial and territorial program priorities. This framework should include published criteria for prioritization, including measures of health disparities — such as differences in the burden of disease, access to services, and in health outcomes resulting from those services.
PHAC should support the establishment of regular engagement mechanisms — such as advisory input from equity-denied communities, Indigenous partners, frontline primary care providers, as well as equity offices in provincial programs and quality councils — to identify emerging issues and validate topic relevance. In addition, PHAC should enable and support routine review cycles to reassess priorities in light of evolving population health trends and system feedback. These expectations should be formalized in the Task Force's mandate letter and supported by dedicated resources for coordination, engagement, and transparent reporting of selection decisions.
Integrating patient and public perspectives for more inclusive guidelines
Preventive service guidelines must reflect the lived experiences, patient preferences, community, and cultural contexts of the people they are intended to serve. At present, patient and public involvement in the Task Force guideline development process is limited. This gap represents missed opportunities to identify access barriers, feasibility in real-world settings, and incorporate diverse perspectives on risk, benefits, as well as acceptability and feasibility of care.
Systematic and equity-centred engagement with patients and communities — particularly those historically underrepresented in health policy and clinical decision-making — would strengthen the legitimacy, fairness, and uptake of recommendations. It would also improve the relevance of guidelines across diverse social, cultural, and geographic contexts.
International examples, such as the UK's National Institute for Health and Care Excellence (NICE), demonstrate the value of meaningful engagement through mechanisms such as public advisory panels, targeted consultations including surveys, focus groups, and citizen juries. These approaches not only enhance transparency and trust, but also improve the practical applicability of recommendations.
The Task Force should adopt a similar model, embedding patient and public perspectives at all stages of its work — from topic selection and evidence interpretation to guideline formulation and implementation planning. In support of this goal, PHAC could also explore the development of a cross-guideline development body engagement infrastructure (e.g., a shared network of public and patient advisory panels) to support consistency, efficiency, and inclusivity across Canadian guidance bodies.
Recommendation 7: Establish a model for equity-centred patient and public engagement
PHAC should enable and support the Task Force to adopt structured, consistent mechanisms for engaging patients, community groups — including Black, Indigenous and other communities historically underrepresented in health policy and clinical decision-making — and the public throughout guideline development, ensuring that lived experience, patient preferences and community values are meaningfully reflected in final recommendations.
To embed lived experience and community perspectives into preventive guidance, PHAC should enable and support the Task Force to implement a formal, equity-centred patient and public engagement strategy. This should include the creation of standing advisory panels, structured opportunities for input at each stage of guideline development, and transparent reporting on how feedback was considered. Engagement processes should prioritize the inclusion of individuals from underserved and equity-denied communities. PHAC should also explore the development of shared infrastructure — such as a national roster or engagement support services — to improve consistency and efficiency across Canadian health guidance bodies. Dedicated resources should be allocated to capacity building to support meaningful, accessible, and sustained engagement.
In conclusion, embedding equity into the preventive service guideline development process is not a separate initiative — it must be a foundational principle that shapes how topics are selected and framed, evidence is assessed, communities are engaged, and recommendations are articulated. A more inclusive, transparent, up-to-date, and responsive approach will ensure that preventive service guidelines serve all Canadians fairly and effectively. With sustained policy support, investment in capacity, and commitment to innovation and collaboration, the Task Force can lead the way in setting a new standard for equity-centred guideline development in Canada.
Summary: Embedding equity: Towards inclusive guidelines
To ensure preventive guidelines are relevant, inclusive, and actionable for all people in Canada, equity must be embedded across every stage of the Task Force's work. Recommendations 6 and 7 provide a roadmap for operationalizing this commitment — from topic selection to equity-centred patient and public engagement. These reforms will strengthen the Task Force's ability to address health disparities and ensure that guidance reflects the lived experiences and priorities of equity-denied populations. Together, they reinforce the importance of developing preventive health service recommendations that are not only scientifically rigorous, but also equitable, practical, and aligned with the needs of those most often left behind.
2.4 Strengthening governance for inclusive and contextualizable guidance
A strong and transparent governance framework is essential to ensuring the long-term sustainability, credibility, and operational efficiency of the Task Force. It is also necessary to support the development of guidance that is both methodologically sound and adaptable to the diverse operational contexts across Canada. Targeted reforms can enhance its capacity to respond to evolving health care challenges while preserving public trust. This section outlines key changes to strengthen the Task Force, starting with broadening its membership to incorporate diverse expertise, to enrich guideline development with a wider range of perspectives. It also explores the balance between rigorous conflict of interest management and inclusivity, ensuring that diverse perspectives can be integrated without compromising impartiality. Securing stable and sufficient funding is highlighted as essential to sustaining Task Force operations and supporting resource-intensive activities such as greater engagement and evidence synthesis.
Collectively, these proposed enhancements lay the groundwork for a core recommendation — namely, for PHAC to re-establish the Task Force as an external advisory body, with a reconceptualized organizational structure. Drawing on the established framework of other external advisory bodies, such as the National Advisory Committee on Immunization (NACI), these reforms aim to strengthen decision-making, improve transparency, and ensure that guideline development reflects both cutting-edge expertise and the lived experience of diverse populations across Canada.
Strengthening membership diversity through inclusive selection and transparent nomination
To ensure that preventive health service guidelines are relevant, trusted, and applicable across diverse Canadian contexts, The Task Force's membership must reflect a balance of expertise, lived experience, and system perspectives. This includes representation from different professions, jurisdictions, and communities — particularly those facing systemic barriers to equitable care.
Ensuring that Task Force members reflect a wide range of care delivery settings — including those from jurisdictions with unique program structures or access challenges — will also strengthen the Task Force's ability to develop contextualizable recommendations that can be meaningfully adapted by provinces, territories, and diverse provider groups.
Consultation feedback raised concerns about a lack of clarity in the current selection process, with some interest holders perceiving an over-representation of certain professional backgrounds and underrepresentation in areas such as health equity, lived experience, and implementation. Strengthening the inclusivity and transparency of the membership and nomination process is essential to maintaining the Task Force's credibility, independence, and connection to frontline realities.
PHAC should enable and support the development of a transparent, competency-based membership framework, accompanied by a revised, inclusive nomination process. The framework should outline the full range of qualifications and disciplinary perspectives required — including expertise in primary care, Indigenous health, Black health, public health, and lived experience as a patient or caregiver.
It should designate specific roles for rural and urban family physicians, nurse practitioners, Indigenous health leaders, public health practitioners, citizen partners and individuals with lived experience, including those from equity-denied communities. It should also encompass disciplinary expertise in areas such as epidemiology, behavioural and social science, health equity, public health, and knowledge translation, as well as methodological expertise in living evidence and living guidelines.
Using this framework, PHAC should launch open and transparent calls for nominations and conduct targeted outreach to engage professional, academic, and community organizations identifying candidates from diverse backgrounds (Public Health Agency of Canada, 2022c).Footnote 3 A standing nominations committee — independent of the Task Force membership — should be established to assess applicants against the competency matrix and make recommendations. Final selections should be approved by the Chief Public Health Officer to ensure accountability and maintain public confidence in the process.
These measures will help ensure that the Task Force is equipped to develop inclusive, equity-centred, and context-sensitive guidance that reflects the needs of diverse communities and health systems across Canada.
Recommendation 8: Build a competency-based and inclusive membership and nomination framework
PHAC should enable and support the Task Force to adopt an integrated framework for inclusive, competency-based membership and a transparent nomination process. This framework should define essential qualifications, expertise, and lived experience — ensuring representation from equity-denied communities and across primary care, public health, and Indigenous health systems. It should also establish a public nomination process, including clear eligibility criteria, targeted outreach, and an independent nominations committee with diverse representation. These measures will ensure the Task Force is equipped to develop guidance that is relevant, equitable, and contextualizable across Canada's diverse health systems.
Enhancing guidance through targeted subject matter expert engagement
While maintaining a core voting membership grounded in competency areas identified above — to ensure preventive service guidelines remain practically, clinically, and programmatically relevant — the Task Force should expand its multidisciplinary reach by formally engaging relevant subject matter experts (SMEs) as non-voting members in the working groups. These SMEs may include medical specialists and clinical experts whose disease-specific knowledge is critical to interpreting emerging evidence and contextualizing population-level recommendations, those with specific academic expertise and those with knowledge of specific community needs.
To fully leverage this expertise, the Task Force should establish a structured, topic-specific mechanism for SME engagement, allowing for advisory input at clearly defined stages of guideline development — particularly during evidence interpretation, and the review of draft recommendations. Their input is especially valuable for identifying contextual factors — such as system capacity, delivery models, or population characteristics — that may influence how recommendations are interpreted and implemented in practice. SMEs should be engaged on a guideline-by-guideline basis through dedicated working groups. This targeted, time-limited participation model will ensure that guidelines are informed by deep technical knowledge while maintaining the Task Force's independence and methodological integrity.
Decision-making authority must remain solely with the core voting members. SME involvement should be guided by clear protocols that define roles, timelines, criteria for participation, and expectations for transparency, documentation, and public disclosure. To uphold impartiality and reinforce public trust, a modernized conflict-of-interest framework (discussed in the following section) should be applied consistently to all SME contributors.
Taken together, these measures will enable the Task Force to benefit from specialized expertise while preserving its independence, credibility, and ability to produce impartial, evidence-based preventive health guidance.
Recommendation 9: Formalize subject matter expert (SME) engagement
PHAC should enable and support the Task Force to create structured roles for SMEs to contribute at key stages of guideline development working groups, without compromising the Task Force's independence in decision-making. This will support the integration of expertise from primary care practitioners alongside domain-specific expertise from specialists.
To strengthen the scientific quality and relevance of its guidelines, PHAC should enable and support the Task Force to establish a structured process for engaging subject matter experts (SMEs) in an advisory, non-voting capacity at defined points in the guideline development process — particularly during the evidence review and the formulation of draft recommendations. SME engagement should be organized on a topic-by-topic basis, enabling the Task Force to access relevant expertise without compromising its impartiality or decision-making integrity. This process should be governed by transparent protocols outlining roles, timelines, and criteria for participation, with all inputs appropriately documented. PHAC should embed this requirement in the Task Force's mandate letter and ensure regular reporting on SME engagement activities. This approach will enhance the credibility, depth, and contextual accuracy of guideline content while safeguarding scientific independence and public trust.
Balancing conflict of interest management with inclusivity
The Task Force's rigorous conflict of interest (COI) policy has been a cornerstone of its credibility and independence. However, concerns have been raised that overly rigid COI standards may unintentionally and indiscriminately exclude valuable expertise. As the landscape of preventive health grows increasingly complex, a more pragmatic and structured approach is needed to balance independence with the need for specialized knowledge.
To modernize its COI framework while preserving public trust, the Task Force should adopt a two-tier model, similar to that used by the US Preventive Services Task Force (USPSTF) and the National Advisory Committee on Immunization (NACI). This model distinguishes between two levels of responsibility — maintaining strict COI standards for core voting members while allowing a limited number of non-voting advisors with disclosed and managed conflicts to participate in specific phases of guideline development. It provides the necessary flexibility to access deep expertise while preserving the integrity of final recommendations.
Under this framework, COI standards for voting members will remain rigorous. They should be precluded from having any significant financial interests, such as research funding or consulting income, or other financial relationships that could influence their judgment. Additionally, their intellectual or non-financial conflicts should be minimal, fully disclosed, and actively managed. This would ensure that final decision-making remains transparent, evidence-based, and free from undue influence.
In contrast, non-voting advisors — such as medical specialists or academic experts — could be engaged through topic-specific working groups, with a limited and controlled proportion permitted to hold disclosed and managed conflicts of interest. These individuals would not participate in final decision-making, but would nevertheless provide crucial insights during evidence appraisal or the drafting of recommendations.
This model reflects current best practices in the governance of external advisory bodies, allowing the Task Force to access relevant expertise without compromising independence. As seen in the approach used by NACI, safeguards such as the public disclosure of COI declarations and the transparent documentation of working group processes will further reinforce accountability and build public trust.
By adopting a two-tier COI framework, PHAC and the Task Force can enhance both the quality and legitimacy of guideline development — ensuring that recommendations are not only scientifically sound but also informed by the expertise needed in preventive health services.
Recommendation 10: Adopt a tiered conflict of interest (COI) framework
PHAC should enable and support the Task Force to adopt a two-tier approach — distinguishing voting members on the Task Force from those participating in topic-specific working groups — to managing conflict of interest, enabling transparent and risk-proportionate participation of subject matter experts (SMEs).
This framework should define clear distinctions between financial, intellectual, and non-financial conflicts of interest (COI). It should also include a mechanism for public reporting of COI disclosures to strengthen transparency and interest holder confidence. PHAC should formalize this requirement through the Task Force's mandate letter, and monitor the implementation through periodic reporting. This approach will safeguard the credibility of the Task Force while broadening access to essential expertise.
In conclusion, taken together, these reforms will ensure that the Task Force's membership, nomination and advisory processes are inclusive, transparent, and aligned with the complex realities of preventive health care across Canada.
Embedding these perspectives into the governance and structure of the Task Force will strengthen its ability to address systemic disparities and promote equitable preventive service for all Canadians.
2.5 Securing the foundations for sustainability and independence
A predictable and sustainable funding model is critical to ensuring long-term viability, operational effectiveness, and credibility of the Task Force. At present, inconsistent and insufficient funding currently limits the Task Force's ability to update guidelines in a timely manner, support inclusive participation — particularly from non-salaried members such as citizen partners and fee-for-service clinicians — and engage meaningfully with key interest holders to foster public trust and implementation success.
An international comparison shows that the Task Force operates with significantly fewer and less stable resources than similar bodies, which benefit from robust infrastructure and broader capacity for equity-oriented and high-volume guideline development.
The Task Force is funded through a contribution agreement between PHAC and the institution with which a Task Force current or former member is affiliated — typically the chair. This institution serves as the primary recipient of funds and subcontracts with other service providers to support Task Force operations. While this model offers flexibility, it also presents limitations — particularly during leadership transitions that require the renegotiations of hosting arrangements. Such factors impose administrative burdens and may constrain the Task Force's agility to respond efficiently to evolving priorities.
To continue delivering up-to-date, trusted, and evidence-based preventive health guidance that reflects the needs of Canada's diverse health systems, stable funding and institutional support are essential. A restructured, multi-year funding model — with appropriate compensation for non-salaried members and embedded methodological and operational support — would strengthen the Task Force's capacity to fulfill its national mandate effectively.
Recommendation 11: Establish long-term funding and secretariat support
To fulfill its mandate effectively, the Task Force requires stable, multi-year funding, including appropriate compensation for its members, when required. PHAC should support a dedicated or shared Secretariat to provide continuity, infrastructure, as well as methodological and operational support.
To fulfill its mandate and maintain public trust, the Task Force requires a stable, multi-year funding model supported by a dedicated Secretariat. PHAC should establish a structured funding mechanism. This would provide secure, indexed operational funding and appropriate compensation for non-salaried members, including patient partners and community-based clinicians. This model should include embedding a permanent Secretariat within PHAC — either dedicated to the Task Force, or shared — to provide coordination, methodological support, infrastructure, and administrative continuity. A formalized agreement should also outline clear performance expectations and reporting requirements to ensure transparency and accountability. Implementing this funding structure will ensure the Task Force can continue delivering up-to-date, credible, and independent preventive health guidance responsive to Canada's evolving health systems.
Establishing the Task Force as an External Advisory Body (EAB)
A modernized and clearly defined governance structure is crucial to strengthening the Task Force's credibility, transparency, and long-term impact as a leader in the guideline development landscape. Addressing structural inefficiencies — such as unclear divisions of roles and responsibilities between various branches of the Task Force structure, administrative burdens, and concerns about independence — requires a refined governance model that balances stability with operational flexibility.
Optimizing structure for greater effectiveness
The current governance structure of the Task Force has been the subject of ongoing scrutiny, with concerns about its ability to effectively support its mandate. Input from current and former members, as well as consultations with interest holders, highlighted opportunities to enhance transparency, strengthen accountability, and improve clarity around the Task Force's relationship with PHAC. Similar concerns were raised in past evaluations, which highlight unclear divisions of responsibility between the Task Force, its Evidence Review and Synthesis Centres (ERSCs), and PHAC (Public Health Agency of Canada, 2022a). Such challenges ultimately constrained the Task Force's ability to operate with clarity, independence, and efficiency.
Strengthening independence and governance mechanisms
Ensuring the Task Force's independence from political influence is essential to maintaining its credibility. During the Panel's consultation, interest holders emphasized that its evidence-based recommendations must be free from external pressures — including from the perception of undue influence. While some proposed relocating the Task Force to a non-governmental host institution — such as a professional association — this may only shift the problem, rather than resolve it. A more sustainable approach would be to strengthen safeguards and governance mechanisms that guarantee independence, impartiality, and transparency — regardless of the Task Force's institutional home.
Improving transparency and accessibility
Transparency is a critical enabler of both public and professional trust. Many interest holders noted that some key decision-making processes remain opaque — such as the manner in which topics are selected, or how evidence is synthesized. While the principal aspects of the Task Force's methods and processes are outlined its Methods Manual (Canadian Task Force on Preventive Health Care, 2023) interest holders have called for greater clarity, including the publication of meeting minutes, rationales for given decisions, and user-friendly access to foundational information and documents. It was also emphasized that materials must be made accessible to support equitable engagement — including through ensuring their availability in both official languages.
Addressing administrative burdens
Governance challenges are further compounded by limited resources and operational inefficiencies. Volunteer members face persistent administrative burdens, diverting time and energy from their core function of developing high-quality guidelines. Coordination across the Task Force, its ERSCs, and PHAC often lacks cohesion. Previous evaluations and consultation feedback also highlighted the need for fair compensation of non-salaried members, particularly patient and community representatives (Public Health Agency of Canada, 2022a). These issues raise the need for more financial support, but also for structural reforms that can strengthen governance, clarify roles, and streamline operations.
To address these challenges, the Panel recommends transitioning the Task Force to an External Advisory Body (EAB)Footnote 4 model. This approach would preserve federal support while reinforcing the Task Force's independence and reducing administrative strain through a clearly defined governance structure, a permanent Secretariat, and enhanced public accountability. While this model may somewhat limit flexibility in administrative processes, it nevertheless offers significant benefits, including greater stability, improved coordination, and strengthened public trust. Success will depend on ensuring transparency in key governance processes, including in membership selection and in guideline-related decision-making.
Reconceptualizing the organizational structure
To operationalize this new governance model, the External Advisory Body (formerly the Task Force) should adopt a multilayered organizational framework designed to integrate diverse expertise and lived experience. At its core, a panel of members would oversee recommendation development, supported by a full-time Secretariat providing administrative, scientific, and communications capacity.
This panel of members would be advised by a standing Equity Advisory Panel, bringing together expertise in health equity, anti-racism, decolonial practices, and Indigenous knowledge systems. This structural layer can also help ensure that guidance produced by the External Advisory Body is more attuned to the social, cultural, and jurisdictional contexts in which it will be implemented — reinforcing the goal of producing contextualizable recommendations.
The existing Task Force Patient Engagement Network (TF-PAN) should be maintained and formally embedded within the new structure to ensure that the perspectives of patients, caregivers, and community members are reflected in guideline development. For individual guidelines, topic-specific working groups — chaired by a member of the External Advisory Body and including relevant subject matter experts — would provide targeted input. Clear terms of reference should define the roles, responsibilities, and accountability mechanisms for each component of this structure.
This proposed structure is illustrated in Appendix 7: Proposed Organizational Chart for the Task Force.
Recommendation 12: Reconstitute the Task Force as an External Advisory Body
PHAC should reconstitute the Task Force as an independent External Advisory Body, supported by transparent governance, formalized engagement with interest holders, and accountable decision-making process.
To implement this transition, PHAC should re-establish the Task Force as an External Advisory Body. This structure should be supported by a permanent Secretariat embedded within PHAC or an appropriate host institution, with a clear mandate to provide administrative, scientific, and operational coordination. A skill and competency-based member panel should oversee guideline development, supported by standing advisory bodies — including an Equity Advisory Panel and the Patient Engagement Network — as well as topic-specific working groups to draw in subject matter expertise. PHAC should define transparent terms of reference for each governance component and establish formal reporting and appointment processes to safeguard independence, ensure accountability, and foster inclusive engagement — consistent with the PHAC External Advisory Body Policy (Public Health Agency of Canada, 2024). Transitioning to this model will enhance the Task Force's credibility, improve operational agility, and strengthen its ability to deliver up-to-date, trusted, and relevant preventive health service guidance across Canada's health systems.
Summary: Strengthening the governance
Strengthening the governance of the Task Force is essential to ensuring its continued relevance, independence, and impact. Recommendations 8 to 12 set out a comprehensive roadmap to modernize its structure, processes, and composition. This includes implementing a transparent, competency-based membership framework that reflects the diversity of Canada's population and health systems; establishing a structured nomination process to enhance legitimacy and accountability; and formalizing mechanisms for engaging subject-matter experts while safeguarding decision-making independence. Additionally, a tiered conflict-of-interest framework will provide access to specialized knowledge while maintaining public confidence in the integrity of the recommendations. To improve long-term sustainability and operational effectiveness, the Task Force should be transitioned to an External Advisory Body, supported by stable, predictable multi-year funding and a permanent Secretariat. Together, these reforms will position the Task Force to deliver scientifically rigorous, up-to-date, inclusive, and evidence-based preventive health guidance in a more responsive, transparent, and coordinated manner.
Chapter 3: Broader considerations
3.1 System-wide opportunities for a coordinated and future-ready ecosystem
While this review focused on the mandate, governance, and processes of the Canadian Task Force on Preventive Health Care, the Panel's consultations and deliberations revealed broader systemic challenges that extend beyond the scope of our formal terms of reference. While falling outside the Panel's immediate mandate, these issues are significant and warrant serious consideration by the Public Health Agency of Canada (PHAC) and federal, provincial, and territorial governments.
3.2 Building a cohesive guideline infrastructure
A recurring concern raised by interest holders across Canada was the widespread duplication of efforts in the development of clinical practice guidelines. Currently, numerous actors — including federal, provincial and territorial governments, health agencies and institutes, professional associations, and private sector organizations — develop guidelines independently. This leads to unnecessary overlap, inconsistent of conflicting guidance, and ultimately, confusion for frontline practitioners.
To address this issue, there is a pressing need not only to improve coordination, but to formalize alignments across the full spectrum of advisory and decision-making processes — such as provincial and territorial screening programs — as well as learning and improvement platforms, including quality councils. This alignment must extend beyond traditional interest-holder consultations, and extend into operational and system-level infrastructure required to embed guidance into practice. It should also include shared mechanisms to ensure that nationally developed guidance can be adapted to local delivery models, helping to operationalize contextualizable summaries at the point of care.
This includes addressing critical health system enablers that can help institutionalize a modernized approach to guideline development. Key enablers include updating Electronic Medical Records and Electronic Health Records (EMRs and EHRs respectively), integrating guideline prompts into clinical workload and digital tools, and adjusting funding arrangements to support implementation across jurisdictions.
Supplementary recommendation A: Create a National Coordination Hub
The federal government, in collaboration with provincial and territorial partners, should explore the creation of a national coordination hub for guideline development — bringing together funders, health providers, researchers, and implementers to strengthen alignment, reduce duplication, and accelerate the translation of evidence into effective policy and practice. This hub should enable formal coordination across advisory and decision-making structures, including learning and improvement platforms, and support system-level integration. It should also help contextualize by enabling the adaptation of guidance to different provincial and territorial settings, supported by a shared infrastructure for producing localized summaries of key recommendations. This includes aligning funding mechanisms and operational enablers to embed a modernized, population-responsive approach to clinical practice guidelines development and implementation.
Establishing such a hub would not necessarily require the creation of a new organization. An existing pan-Canadian health organization could serve as a Secretariat to support this function. Models from other jurisdictions — such as NICE — could offer valuable lessons in effective coordination.
3.3 Integrating public and community health perspectives
Preventive health care is critical to improving population health outcomes, reducing long-term system costs, and addressing health inequities. However, Canada's current approach to prevention remains fragmented, with limited coordination across jurisdictions and sectors.
During the consultation process, participants — including public health officials, clinicians, researchers, and patient partners — consistently pointed to the absence of a national mechanism for aligning clinical preventive guidance with the community, public and population health initiatives and research. Several also emphasized the need to support upstream, or primordial, prevention strategies that address social and structural determinants of health.
Ensuring that clinical and public guidance are contextually aligned — with each other and with local system realities — will be essential to maximizing the relevance, equity, and uptake of preventive guidance in Canada.
Supplementary recommendation B: Launch a Task Force on Community Preventive Services
The federal government, in collaboration with provincial and territorial partners, is encouraged to explore the creation of a Task Force on Community Preventive Services, in collaboration with organizations such as the National Collaborating Centres for Public Health (NCCs), to provide independent, evidence-based guidance for public health and community-level interventions beyond clinical care.
3.4 Aligning research funders, data agencies, quality councils and global collaboration
Another key area of concern is the limited coordination between research funding, health data infrastructure, and the development, implementation, and evaluation of guidelines. This disconnect contributes to inefficiencies, unnecessary duplication, and slower uptake of evidence-in practice.
There is a need for shared tools, common frameworks, and sustained investment in equity-centred research to better support interest holder engagement, knowledge translation, and systemwide learning across Canada's preventive health ecosystems. At the same time, global initiatives such as the Evidence Synthesis Infrastructure Collaborative are documenting how shared platforms and AI-supported methods can dramatically reduce the cost and time required to produce living evidence synthesis — creating opportunities for Canada to align, collaborate, and help shape this evolving international infrastructure. Through such platforms, Canada can ensure that provinces and territories have equitable access to living evidence syntheses — reducing the need for duplicative reviews and enabling jurisdictions to focus their efforts on contextualizing summaries to fit their population needs and delivery models.
At the same time, Canada must move beyond a parochial lens to engage with the global evidence infrastructure that is rapidly taking shape. By aligning with, and contributing to international initiatives, the federal government can avoid duplicating efforts, share costs, and help ensure that the Canadian system can benefit from global advancements in evidence production and use.
Supplementary recommendation C: Build a network for research, data, and evaluation alignment
The federal government is encouraged to establish a network to strengthen coordination with Canada's health research funders, data agencies, and quality councils. This network should also position Canada to engage with, and contribute to, an emerging global infrastructure for living evidence synthesis — enabling provinces and territories to access shared, high-quality evidence bases and focus their efforts on local adaptation, rather than duplicative evidence review and guidance development.
3.5 Looking ahead
While the proposals outlined in this chapter extend beyond the immediate mandate of the Panel, they reflect a strong and recurring message heard throughout this review process: Canada needs more of an integrated national infrastructure and strategic coordination to maximize the impact of guidelines and preventive health services.
By acting on these insights, we can contribute to a more cohesive, coordinated, future-ready approach to preventive health — one that ensures all people in Canada have equitable access to up-to-date evidence-based guidance that promote health and well-being across communities and generations.
Conclusion: A way forward
This report responds to the Minister of Health's directive to assess the governance, mandate, and processes of the Canadian Task Force on Preventive Health Care. The Panel's findings underscore the importance of modernizing the Task Force to ensure that it remains a credible, independent, and inclusive source of preventive health guidance for primary care health professionals across Canada and the provincial and territorial programs and quality councils that support them.
The twelve recommendations outlined in Chapter 2 presents a clear and actionable roadmap for its renewal. They emphasize improved governance, greater transparency, a more adaptable methodological approach and a stronger commitment to equity — ensuring the Task Force is equipped to respond to the changing needs of Canada's health system. Informed by consultations, evidence reviews, and international best practices, these recommendations are designed to strengthen the Task Force's capacity, relevance, and impact well into the future.
Beyond the Task Force itself, Chapter 3 highlights broader opportunities to improve the coherence and effectiveness of Canada's guideline development ecosystem. It proposes steps to enhance coordination, reduce duplication, and expand the scope of guidance to better address community, public, and population health needs.
While this report outlines a clear and achievable pathway to modernization, several strategic challenges must be addressed to ensure successful implementation. Sustained coordination across national, provincial and territorial partners will be essential to reduce fragmentation and promote alignment in the development and use of preventive health guidelines. Realizing long-term impact will require predictable federal investment and structural reforms to secure stable funding and operational capacity.
Transitioning to a living guideline model will necessitate new partnerships, adoption of digital tools and infrastructure, skilled technical staff, and thoughtful change management. Embedding equity throughout the guidelines process — from topic selection to implementation — will require sustained commitment, targeted strategies, and transparent accountability mechanisms.
The proposed structures and processes will strengthen the Task Force, but they will also require appropriate levels of resourcing and increased coordination among its members, working groups, and partners. The inclusion of multiple types of members — voting, non-voting, subject matter experts, and public representatives — will add complexity to its governance and require more structured oversight. In this context, adequate support — particularly for the Task Force's Chair — will be essential to manage the different levels of governance and ensure effective functioning overall.
Crucially, success will also depend on making national guidelines more contextualizable — ensuring provinces and territories are equipped to adapt recommendations to their unique systems and populations without duplicating development efforts. This calls for shared infrastructure, collaborative processes, and deliberate design of guidance that bridges scientific integrity with practical utility across Canada's diverse health care contexts.
Together, the findings and recommendations in the report provide a practical way forward, serving as a clear guide for PHAC leadership and decision-makers to implement changes that can create a more integrated, responsive, and future-ready preventive health system — one that advances health equity and delivers real benefits for people and communities across Canada.
Glossary
- Clinical (care) guidelines
- Also called practice guidelines, clinical guidelines are systematically developed statements to assist health care practitioners deliver appropriate, evidence-based care to patients. Guidelines make explicit recommendations for care with the specific intent to influence what health care providers do. Guidelines are not rules; they support clinical decision-making, not supplant it (Public Health Agency of Canada, 2017).
- Contextualization
- Contextualizing a guideline occurs when a guideline produced elsewhere is adopted or adapted, and effective implementation requires the addition of caveats and/or supplementary considerations to address local contexts (Dizon et al., 2016).
- Diversity
- The demography characteristic of populations attributable to perceptible ethnic, linguistic, cultural, visible or social variation among groups of individuals in the general population (Public Health Agency of Canada, 2022b).
- Equity-centred
- An equity-centred approach places fairness and justice at the core of topic selection and framing, evidence reviews, recommendations development, contextualization, implementation, and monitoring and evaluation. This involves engaging communities affected by inequities in these steps. It also involves examining impacts on equity-centred quadruple-aim metrics (Venkateswaran et al., 2023).
- Equity-denied
- In Canada, groups generally considered to be equity-denied groups include women, Indigenous Peoples, people with disabilities, people who are part of 2SLGBTQI+ communities, religious minority groups, as well as Black people and racialized individuals. The types of equity-denied groups may vary based on factors such as geography, sociocultural context or the presence of specific subpopulations (Interdepartmental Terminology Committee on Equity Diversity and Inclusion, 2024).
- Evidence-based
- Evidence-based refers to practices or decisions that are informed by the best available scientific evidence. In the context of medicine, this concept finds application within the principles of Evidence-Based Medicine, which emphasizes the conscientious, explicit, and judicious use of current best evidence in making decisions about the care of individual patients (Sackett et al., 1996).
- Evidence synthesis
- Evidence synthesis is a research method that combines all relevant information from primary studies and grey literature to answer a research question. Different types of evidence synthesis include systematic reviews, scoping reviews, rapid reviews, umbrella reviews, and meta-analyses. As a step in the systematic review process, evidence synthesis involves combining appraised data from eligible studies and analyzing it to determine if there is enough evidence to state conclusively that together the studies answer a research question (University of Texas Libraries, 2025).
- External Advisory Body (EAB)
- Established by the Minister of Health or the department/agency to provide advice on specific medical, scientific, technical, policy or program matters within the scope of its mandate. All members are external to the federal government and provide advice as a group, and not as individuals or representatives of organizations (Health Canada, 2023).
- Governance
- Governance refers to the processes and structures used to direct and manage an organization's operations and activities. It defines the division of power and establishes mechanisms to achieve accountability among stakeholders, the board of directors and management (SaskCulture, 2024).
- GRADE
- GRADE (Grading of Recommendations Assessment, Development and Evaluation) is a systematic and transparent approach used to assess the quality of scientific evidence and the strength of health care recommendations. GRADE helps ensure that guideline decisions are based on the best available research and are clearly linked to the certainty of the underlying evidence. It has been adapted for different types of evidence, including qualitative research (GRADE-CERQual) and diagnostic studies (The GRADE Working Group, 2025).
- Health equity
- Health equity is the absence of unfair, avoidable or remediable differences in health status among population groups defined socially, economically, demographically or geographically (World Health Organization, 2021).
- Interest holders
- Interest holders, as defined by (Akl et al., 2024), are those with legitimate interests in a health issue due to their role in, or impact from, related decisions, and this term is offered as a more respectful alternative to "stakeholders" in health research and policy.
- Knowledge translation (KT)
- Knowledge translation (KT) is defined as a dynamic and iterative process that includes synthesis, dissemination, exchange and ethically sound application of knowledge to improve the health of Canadians, provide more effective health services and products, and strengthen the health care system (Public Health Agency of Canada, 2017).
- Lived and living experience (LLE)
- Lived experience is defined as personal knowledge about the world gained through direct, first-hand involvement in everyday events rather than through representations constructed by other people. It may also refer to knowledge of people gained from direct face-to-face interaction rather than through a technological medium (Oxford University Press, 2025).
- Living evidence
- Living evidence syntheses are systematically appraised and continually updated summaries of research evidence. These syntheses are driven by the commitment to frequent ongoing surveillance for new research evidence, where frequency is decided by the likelihood of new evidence emerging, anticipated changes in policy or practice contexts change, or the need and urgency for decision-making (Chakraborty et al., 2024).
- Preventive health care
- Refers to proactive measures aimed at reducing the risk of illness or injury before they occur. This includes immunizations, routine check-ups, and lifestyle interventions such as healthy eating and regular exercise. It also encompasses screening strategies to identify health issues at an early stage — before symptoms arise — when treatment is most effective and the likelihood of complications is lower (Lenartowicz, 2023; Nyantakyi, 2023).
- Primary health care
- Primary health care is a comprehensive approach to health that encompasses a broad range of services beyond traditional medical care. It addresses the wider determinants of health, including social, economic, and environmental factors, alongside direct health care services like health promotion, prevention, diagnosis, and treatment. Primary care is a key component of primary health care, focusing specifically on the delivery of these health care services (Health Canada, 2012; World Health Organization, 2025).
- Primary care health professional
- Health care providers who deliver frontline care to individuals. This group includes physicians, nurses, pharmacists, physiotherapists, and dieticians (Canadian Institute for Health Information, 2025; Health Canada, 2025a, 2025b).
- Primordial prevention
- Primordial prevention consists of actions to modify population health determinants and to inhibit the establishment of factors (environmental, economic, social, and behavioural) known to increase the risk of future disease. It targets determinants at the societal level rather than modifying personal risk factors, which is the focus of primary prevention (Association of Faculties of Medicine of Canada, 2025)
- Quadruple aim
- The quadruple aim is a framework for optimizing health system performance by focusing on four interconnected goals: improving the patient experience of care, enhancing population health, supporting the well-being of health care providers, and ensuring value for money through cost-effective care delivery (Canadian Institutes of Health Research, 2022).
- Racialized group
- A group of people categorized according to ethnic or racial characteristics and subjected to discrimination on that basis (Interdepartmental Terminology Committee on Equity Diversity and Inclusion, 2022).
Appendices
Appendix 1: External expert review-terms of reference
- 1.0 Preamble
- 1.1 This External Expert Review of the Canadian Task Force on Preventive Health Care ("the Review") is being set up pursuant to the PHAC (Public Health Agency of Canada) External Advisory Body Policy ("the EAB Policy") wherein the Agency seeks external expert advice from individuals who have the requisite knowledge, expertise, and experience to advise on a specific scientific, technical, policy or program matter. Section 14 of the Public Health Agency of Canada Act provides the legislative authority to establish the Review.
- 1.2 The Terms of Reference conform with the EAB Policy, which ensures transparency and reliance on a diversity of expertise in gathering independent, informed, and well-rounded advice.
- 1.3 The Review Panel provides their independent advice in the form of a Final Report to the Executive Secretary of the Review, who receives it on behalf of the President of the Public Health Agency of Canada. PHAC retains decision-making authority and accountability for all decisions taken as a result of recommendations made by the Review.
- 1.4 Through its deliberations and conclusions, the Review Panel will apply the following principles:
- Aim to uphold scientific excellence and integrity.
- Aim to contribute to reconciliation by including considerations of Indigenous Peoples, based on recognition of their rights, respect, cooperation and partnership.
- Aim to support the implementation of sex and gender-based analysis plus (SGBA Plus) by ensuring the consideration of how factors such as sex, gender, race, ethnicity, age, disability, and other factors interact and intersect with each other. This approach helps to inform how diverse people and populations in Canada may experience our policies and programs.
- 2.0 Mandate of the review
- 2.1 The Review Panel is mandated to review the Canadian Task Force on Preventive Health Care ("the Task Force") model and provide recommendations for its improvement.
- Specifically, the Review Panel mandate is twofold:
- 2.1.1 Study whether the Task Force is structured appropriately to develop preventive health care guidelines for primary care that meet the needs of Canada's health care system, and recommend consequential improvements or changes that may be needed to modernize the development of preventive health care guidance; and
- 2.1.2 Assess the rigour, agility, inclusiveness, and timeliness of the scientific review processes of the evidence and data sources that are needed to support the development of well rounded, useful, and timely guidelines.
- The Review Panel is instructed to:
- 2.1.3 Review domestic and international approaches and best practices for the development of clinical practice and public health preventive guidelines, and consider the findings of this comparative review in its recommendations; and
- 2.1.4 Engage with experts and key interest holders, both domestic and international, to ensure a comprehensive review that takes into account the best practices integrating elements such as the clinical (patient) interests, lived experience, community preventive health, ethics, and economic analysis.
- 2.1.5 The Review Panel will consider the outcomes of ancillary reviews, consultations, evaluations to the extent that they provide relevant evidence for Panel consideration.
- Specifically, the Review Panel mandate is twofold:
- 2.2 The Review Panel shall produce a Final Report outlining its findings and include a set of actionable recommendations for a robust governance framework, structure, and administration, as well as the scientific review processes.
- 2.1 The Review Panel is mandated to review the Canadian Task Force on Preventive Health Care ("the Task Force") model and provide recommendations for its improvement.
- 3.0 Time frame of the review
- Phase 1: Preliminary research and data collection (September 2024)
- Phase 2: Interest holder consultations (October to December 2024)
- Phase 3: Analysis and report writing (January to March 2025)
- Phase 4: Presentation of findings and recommendations to PHAC (March 2025)
- 4.0 Membership
- 4.1 The Review Panel is composed of 13 members, including a Chair.
- 4.2 The Executive Secretary or their representative will be an ex-officio member. Ex-officio members will not be voting members.
- 4.3 Members have been selected to ensure the Review Panel is composed of a range of relevant knowledge, expertise, and experience including clinical practice, bioethics, methodology, and representative of the diversity of Canada. Members understand PHAC's commitment to Sex and Gender-based Analysis Plus (SGBA+) and, through its review, will apply an intersectional approach to assess how factors such as sex, gender, age, race, ethnicity, socioeconomic status, disability, sexual orientation, cultural background, and geographic location interact and intersect.
- 4.4 All members have agreed to the following obligations as prerequisites to the appointment:
- 4.4.1 be subject to and abide by the terms laid out in PHAC's External Advisory Body Policy.
- 4.4.2 obtain a Reliability status security clearance.
- 4.4.3 sign a Confidentiality Agreement Form.
- 4.4.4 complete and sign an Affiliation and Interests Declaration Form and, if participation is permitted despite a conflict of interest, accept limitations on participation as described in Chapter 3 of the EAB policy; and
- 4.4.5 provide a brief autobiography and review, including a summary of their affiliations and interests (with the understanding, that documents are to be published online by PHAC).
- 4.5 Terms of Reference
- 4.5.1 Members are appointed by PHAC for the duration of the External Expert Review only. The Panel's activities are expected to conclude in March 2025 or shortly after.
- 4.5.2 The Chair will be appointed by the Executive Secretary, to serve at their pleasure.
- 4.6 Resignation process
- 4.6.1 A member may resign from the Panel by providing written notice to the Executive Secretary, with a copy to the chair, including the effective date of the resignation. It is preferred that the member give 14 days' notice of their intent to resign. Once a Panel member decides to resign, the member should be offered an exit interview.
- 4.6.2 The Executive Secretary will determine if a replacement member must be appointed.
- 4.7 Reasons for Termination
- The Executive Secretary may end a member's appointment for a variety of reasons including the member's term is complete; the mandate of the Panel has been completed; the Panel's mandate has changed, thus requiring a different membership, etc. The Executive Secretary may also end an appointment if a member has not acted according to the Terms of Reference. Examples include if a member breaches his/her confidentiality obligations or reneges on its participation in Panel activities, including meetings. PHAC will notify a member in writing about the termination and will provide the member with the reason the appointment is being concluded and the termination date.
- 4.8 Remuneration
- Members agree to participate on a volunteer basis.
- 5.0 Executive Secretary and Secretariat to the Review
- 5.1 The Deputy Chief Public Health Officer serves as Executive Secretary to the Review. The Executive Secretary ensures the good management of the Review on behalf of the President, provides guidance to the Secretariat and the Chair of the Review on PHAC's External Advisory Body Policy, and engages with key officials in PHAC (e.g., the Chief Science Officer) on administrative processes as well as on questions of mandate clarification.
- 5.2 A Secretariat, made up of PHAC officials, provides organizational and administrative support to the Chair and members of the Review Panel, in accordance with Executive Secretary directions. The Secretariat ensures that the ongoing support of the Review is done in accordance with internal PHAC policies and practices, and specifically executes its responsibilities as detailed in section 4.10 of the External Advisory Body Policy.
- 6.0 Non-member experts
- 6.1 The Review Panel should make all efforts to invite experts to appear before them or provide submissions, to the extent that these non-member experts advance understanding while recognizing the time constraints imposed by a time-limited review.
- 6.2 Non-member experts who are not part of the Panel may observe meetings or parts of meetings on specific topics or agenda items. Such individuals are not entitled to information or materials, and their participation remains at the discretion of the Chair and/or the Secretariat. Non-member experts shall not participate in the formulation of any advice or recommendations to PHAC.
- 6.3 Remuneration in the form of honorarium will only be considered for non-member experts with precarious economic situations and those who must give up an hourly wage to participate, assessed on a case-by-case basis.
- 7.0 Transparency
- 7.1 PHAC is committed to transparency as an operating principle. The following documents, at a minimum, will be posted online by PHAC:
- 7.1.1 Terms of Reference.
- 7.1.2 Mandate.
- 7.1.3 Membership List, together with the biographies and summaries of members' affiliations and interests; and
- 7.1.4 Contact information (e-mail) for the Secretariat.
- 7.1 PHAC is committed to transparency as an operating principle. The following documents, at a minimum, will be posted online by PHAC:
- 8.0 Meeting management
- 8.1 With due consideration to PHAC's Green Meeting Guide, the Secretariat will ensure planning, communications, selecting event venues, accommodations, hospitality, procurement, and travel. By following this guide, the Secretariat will aim to minimize meeting waste, water, energy consumption, and air emissions; maximize economic and social benefits.
- 8.1.1 Meeting frequency and location. Meetings will be held approximately every three (3) weeks, for the duration of the mandate, until the Final report is submitted. Meetings will be held either in person at a mutually convenient location or through videoconference. Additional meetings may be held on an as-needed basis at the discretion of the Secretariat, in consultation with the Chair.
- 8.1.2 Meeting Attendance and invitations. Meetings will be limited to voting and non-voting Panel members and Secretariat staff. Presenters and other participants will attend by invitation only.
- 8.1.3 Meeting agendas. The Secretariat, in consultation with the Chair and with input from the members, sets the meeting agenda, and shares documentation in advance of scheduled meetings. The Secretariat will support members by contributing to the identification of questions and issues for discussion.
- 8.1.4 Quorum, Recommendations and Voting. The Panel must have a quorum when making recommendations or providing advice to PHAC. The quorum will be composed of five (5) members and the Chair. The Panel is encouraged to reach a consensus in providing advice whenever possible. When a consensus is not possible, the meeting record will reflect the diversity of opinions.
- 8.2 Deliberations and Reports. Minutes and/or records of proceedings will summarize the proceedings to effectively reflect deliberations. Remarks will not be attributed to individuals in the minutes or records of proceedings.
- 8.2.1 Minutes and/or records of proceedings will be prepared by the Secretariat and circulated to members for review and approval.
- 8.2.2 Advice from the Panel will be provided to PHAC in the form of a Final Report.
- 8.1 With due consideration to PHAC's Green Meeting Guide, the Secretariat will ensure planning, communications, selecting event venues, accommodations, hospitality, procurement, and travel. By following this guide, the Secretariat will aim to minimize meeting waste, water, energy consumption, and air emissions; maximize economic and social benefits.
- 9.0 Public communications and social media
- 9.1 Members who receive media requests or public inquiries related to the Review should inform the Secretariat upon reception and prior to responding. Members of the media should be referred to the Health Portfolio media relations line. PHAC may request a member of the Review Panel to respond to a media question.
- 9.2 Per the EAB Policy (section 4.7), Review Panel members must seek consent from PHAC before disclosing information about the roles, functions, and topics of relevance to the Review in any public communications. These public communications, including social media content developed by a Review Panel member, must be reviewed, and approved by PHAC before being disseminated. More generally, expectations around social media use of members, in respect to communicating about the Review, will be outlined, and agreed to as part of the Confidentiality Agreement that is signed before the appointment.
- 10.0 Travel and expenses
- 10.1 Members of the Review Panel who are authorized to travel by the Executive Secretary or other appropriate authority, for official Panel purposes will have their travel, accommodation and expenses reimbursed according to the National Joint Council Travel Directive and the Treasury Board of Canada Secretariat's Directive on Travel, Hospitality, Conference and Event Expenditures.
- 10.2 Members of the Review Panel will be reimbursed for applicable security screening expenses to conform with 4.4.2, including fingerprinting.
Appendix 2: External expert review members
Dr. Vivek Goel, Chair
Dr. Vivek Goel is the University of Waterloo's President and Vice-Chancellor. He previously held a number of senior leadership roles at the University of Toronto, including as Vice- President and Provost and most recently as Vice-President of Research and Innovation. He served as founding president and CEO of Public Health Ontario from 2008 until 2014 and was also a founding scientist at the Institute for Clinical Evaluative Sciences (ICES). His areas of research expertise include economic evaluation of health interventions, cancer screening, and assessing accessibility and quality of health services using administrative data. Dr. Goel obtained his medical degree from McGill University and completed postgraduate medical training in Public Health and Preventive Medicine at the University of Toronto. Dr. Goel obtained a Master of Science degree (MSc) in Community Health from the University of Toronto and a Master's degree (MS) in biostatistics from the Harvard University School of Public Health. He currently serves as the Chair of the Board of the Canadian Institute for Health Information.
Ms. Brenda Andreas
Ms. Brenda Andreas brings lived and living experience within the health care system. She collaborates at the provincial, national and international level with health system partners in the areas of accreditation, evaluation, patient-oriented research, policy, as well as patient and community engagement.
Current memberships include a community member role on the Canadian Institutes of Health Research (CIHR) Institute Advisory Board for the Institute of Health Services and Policy Research and a patient partner role with the Canadian Primary Care Research Network. She is also a member of the Saskatchewan Health Authority Patient Family Leadership Council, the North American Primary Care Research Network Board, the University of Saskatchewan Research Ethics Board, and Accreditation Canada, where she serves as a Patient Surveyor.
Brenda is a registered retired social worker and holds a Bachelor of Social Work from the University of Calgary and a Certificate in Health Care Administration from the University of Saskatchewan. She is a published author, research collaborator, patient partner, as well as an active community member, deeply committed to health system transformation.
In 1992, Brenda received the Commemorative Medal for the 125th Anniversary of the Confederation of Canada for volunteerism.
Dr. Michael Barry
Dr. Michael Barry directs the Informed Medical Decisions Program (IMDP) at Massachusetts General Hospital (MGH). He previously served as chief of its General Medicine Unit. He has provided adult primary care for over 40 years at MGH. Dr. Barry is a champion of shared decision-making between patients and clinicians. He is a past president of the Society for Medical Decision Making and the Society of General Internal Medicine. Dr. Barry has served as Chief Science Officer at Healthwise and was president of the Informed Medical Decisions Foundation. He is a Master of the American College of Physicians (ACP). In 2020, he won the ACP's Henry D. Bruce Memorial Award for Distinguished Contributions to Preventive Medicine. Dr. Barry served as a member, vice chair and chair of the US Preventive Services Task Force (USPSTF) between 2017 and 2024, and recently stepped down as Immediate Past Chair. Dr. Barry graduated from Trinity College and from the University of Connecticut School of Medicine. He completed his residency training in internal medicine at Strong Memorial Hospital in Rochester, New York. He is participating in this Panel in a personal capacity, and not on behalf of the USPSTF. His input does not necessarily represent the views and policies of the USPSTF.
Mr. Gregory Doyle
Mr. Gregory Doyle is the Manager of Population Cancer Screening and Registries with Newfoundland and Labrador Health Services. Mr. Doyle is also Chair of the Canadian Breast Cancer Screening Network and an Expert Advisor to the Canadian Partnership Against Cancer. He has over 25 years of professional experience in population health and the cancer care system. Mr. Doyle has been involved in the breast, cervical, colon, and lung cancer screening on the provincial and national levels for many years. He is a current member of the Canadian Council of Cancer Registries and has served as the Chair of the Translational Advisory Committee of the PERSPECTIVE Project, which will inform both risk-based breast screening and the incorporation of oncogenetics into the breast screening paradigm. He has extensively published in the areas of population cancer screening and has contributed to the body of knowledge of screening implementation. Mr. Doyle holds degrees from Memorial University of Newfoundland and Queen's University at Kingston.
Dr. Alika Lafontaine
Dr. Alika Lafontaine is an award-winning physician and the first Indigenous physician named among Canada's 50 Most Powerful Doctors by the Medical Post. He is also the youngest and first Indigenous physician to have led the Canadian Medical Association in its 156-year history. A Red River Metis with mixed Indigenous ancestry, Dr. Lafontaine has worked across multiple dimensions of advocacy for the past 20 years, serving on the boards of the Royal College of Physicians and Surgeons of Canada, HealthCareCAN, Canadian Medical Association Journal, Alberta Medical Association and Canadian Medical Association. As a rural specialist, he provides front-line care and is a past Zone Leader. He has founded and led several national projects, including the Indigenous Health Alliance and Safespace Networks. On September 18, 2024, the Canadian Medical Association presented a national apology to First Nations, Inuit and Métis Peoples, a process which he led over his three-year term in the Canadian Medical Association (CMA) presidency cycle. Dr. Lafontaine continues to be a thought leader in health policy, change management, and advocacy.
Dr. John Lavis
Dr. John Lavis supports efforts to address health and broader societal challenges using the best-available research evidence and experiences and insights from citizens, professionals, organizational leaders, and government policymakers. He is co-lead of and lead report writer for the Global Commission on Evidence to Address Societal Challenges, as well as co-lead of Rapid-Improvement Support and Exchange (RISE). He led the development of the 'SHOW ME the evidence' features of an approach to reliably deliver research evidence to decision-makers and interest holders who need it. He was co-lead of the COVID-19 Evidence Network to support decision-making (COVID-END). He is the Director of the McMaster Health Forum and Director of the World Health Organization Collaborating Centre for Evidence-Informed Policy. He is a professor in the Department of Health Evidence and Impact at McMaster University and the Tier 1 Canada Research Chair in Evidence-Support Systems. He holds an MD from Queen's University, a Master of Science (MSc) from the London School of Economics, and a Ph.D. (in Health Policy) from Harvard University.
Dr. Lawrence Loh
Dr. Lawrence Loh is a Medical Officer of Health with Newfoundland and Labrador Health Services. He is a public health and physician leader with senior-level experience at all three levels of government in two Canadian provinces and within the non-profit sector, where he served as the sixth Chief Executive Officer for the College of Family Physicians of Canada. Best known for his leadership during the COVID-19 pandemic, Dr. Loh's service in public health has been recognized with a Key to the City of Mississauga, a Queen Elizabeth II Diamond Jubilee Medal, an honorary degree from Toronto Metropolitan University, and recognition on Toronto Life 2021 list of the Top 50 Most Influential Torontonians, among other academic and professional awards. Dr. Loh holds fellowships in family medicine in Canada and public health and preventive medicine in Canada and the United States. He completed MD training at Western University, a Master of Public Health (MPH) at Johns Hopkins, and residency at the Dalla Lana School of Public Health University of Toronto, where he remains on the faculty as an Adjunct Professor.
Dr. Onye Nnorom
Dr. Onye Nnorom is a family doctor and public health and preventive medicine specialist. She is a Senior Medical Consultant for the Ontario Ministry of Health, in the Office of the Chief Medical Officer of Health; she is the Black Health Faculty Lead at the Department of Family and Community Medicine at the University of Toronto, and a clinical consultant at the Centre for Addiction and Mental Health (CAMH). Dr. Nnorom has dedicated her career to addressing health disparities and improving health outcomes for marginalized communities, with a particular focus on Black populations. Dr. Nnorom completed her medical school at McGill University, obtained a Master of Public Health (MPH) from the Dalla Lana School of Public Health at the University of Toronto in epidemiology and completed her residency at the University of Toronto. Dr. Nnorom is the co-founder of the Black Health Education Collaborative, which was established to provide online educational resources on anti-Black racism and Black health for health professional students, clinicians and public health practitioners. She is also the past president of the Black Physicians' Association of Ontario.
Dr. Gina Ogilvie
Dr. Gina Ogilvie is a Canada Research Chair in the Global Control of HPV-related diseases and prevention and Professor at the University of British Columbia (UBC) Faculty of Medicine's School of Population and Public Health. She is also the Associate Director of the Women's Health Research Institute and Senior Public Health Scientist at BC Centre for Disease Control. Dr. Ogilvie is currently the principal investigator on over 10 million dollars in research grants. She received her MD from McMaster University and completed a specialty in Family Medicine and a fellowship in Population Health and Primary Care. She received her Master of Science (MSc) in Clinical Epidemiology at UBC, and her Doctorate in Public Health from the University of North Carolina. She is a member of the College of Family Physicians of Canada. She has provided advice to national and global institutions on STI, HIV and HPV vaccine and cervical cancer policy development and programming. Dr. Ogilvie is the recipient of many honours, including being a member of both the Royal Society of Canada (2024) and the Canadian Academy of Health Sciences (2022). She has received the UBC Killam Research Prize (2021); Provincial Health Officer's Award for Excellence in Public health (2015); and Researcher of the Year from the College of Family Physicians of Canada (2014).
Dr. Louise Potvin
Dr. Potvin is a full professor at the School of Public Health at the Université de Montréal. She is the Scientific Director of the Centre for Public Health Research and the Canada Research Chair in Community Approaches and Health Inequalities. Her research focuses on community-based prevention interventions and the role of living conditions in the creation of social inequalities in health. She has edited or co-edited eleven anthologies and twelve thematic issues in specialized journals, and has published over 350 articles, book chapters, editorials and commentaries. She was Editor-in-Chief of the Canadian Journal of Public Health from 2014 to 2023. She is a member of the Canadian Academy of Health Sciences. She is the recipient of the 2019 Canadian Institutes of Health Research (CIHR) Institute of Population and Public Health Trailblazer Award and the recipient of the 2021 Canadian Public Health Association R.D. Defries award in recognition of her outstanding contributions to public health. Dr. Potvin holds a master's degree in Psychology from Concordia University and a doctorate in Community Health from the Université de Montréal.
Dr. Caroline Quach-Thanh
Dr. Caroline Quach-Thanh started her career at McGill University before joining the Université de Montréal as a full professor at the Microbiology, Infectious Diseases & Immunology Department and the Pediatrics Department. Dr. Quach-Thanh is a clinician scientist and the Canada Research Chair, Tier 1 in Infection Prevention and Control: from Hospital to Community. She is the director of the POPCORN network (www.popcornpediatrics.ca). Dr. Quach-Thanh is the former Chair of the Public Health Agency of Canada's National Advisory Committee on Immunization (NACI) and is the current Chair of the Quebec Immunization Committee. She was named a Fellow of the Canadian Academy of Health Sciences and of the Society for Health care Epidemiology of America, and was recognized as one of the most Powerful Women in Canada. In 2022, she was made Officière de l'Ordre national du Québec, received the Distinguished Scientist Award from the Canadian Society for Clinical Investigation, and the Women of Distinction Award — Public Service — from the Women's Y Foundation. She received the 2023 Certificate of Merit from the Canadian Public Health Association and was admitted as a foreign member of the Académie Royale de Médecine de Belgique in 2024. Dr. Quach-Thanh graduated from the Université de Montréal Medical School, completed her pediatric residency training at the Centre hospitalier universitaire Sainte-Justine, and her postgraduate training in Infectious Diseases and Medical Microbiology at McGill University, where she also completed a Master of Science (MSc) in Epidemiology.
Dr. Janet Tootoosis
Dr. Tootoosis is a Cree woman from Poundmaker Cree Nation and has been a practising family physician since 2001 in North Battleford, Saskatchewan. She has served as a Clinical Associate Professor at the University of Saskatchewan College of Medicine since 2008 and is the owner/operator of North Battleford Medical Clinic Inc. Dr. Tootoosis has a long-standing commitment to health care delivery and medical education initiatives — both regionally and provincially. She has also worked as an instructor and site director for the University of Saskatchewan College of Medicine's North Battleford Family Medicine Residency Training Program. Additionally, she brings formal governance experience as a former Board member of the Saskatchewan Medical Association (2014-2017) and as an inaugural Board member of the Saskatchewan Health Authority (2017-2021). Dr. Tootoosis currently holds the position of Vice Dean of Indigenous Health at the University of Saskatchewan's College of Medicine.
Dr. Gaynor Watson-Creed
Dr. Gaynor Watson-Creed joined Dalhousie University in 2018 as the inaugural Associate Dean of Serving and Engaging Society for the Faculty of Medicine and is also an Assistant Professor at the Department of Community Health and Epidemiology. She is a public health specialist physician and served as the Medical Officer of Health for the Halifax area from 2005 to 2017, and Deputy Chief Medical Officer of Health for Nova Scotia from 2017 to 2021. Dr. Watson-Creed has an MD from Dalhousie University, a Master of Science (MSc) from the University of Guelph, a Bachelor of Science (BSc) from the University of Prince Edward Island, and honorary doctorates from Acadia University and the University of Prince Edward Island. She serves as chair or member of several national population health councils and boards. In 2023, Dr. Watson-Creed was appointed to the Canadian Institutes of Health Research (CIHR) Institute Advisory Board for the Institute of Population and Public Health. She also serves as chair of the Advisory Board for the National Collaborating Centre for Determinants of Health.
Appendix 3: Technical advisors
Dr. Ève Dubé
Eve Dubé is a professor of Anthropology at Laval University in Quebec City, Canada and a researcher at the Centre de recherche du Centre hospitalier universitaire de Québec-Université Laval. Her field of expertise is anthropology of public health. She is particularly interested in the social, cultural, historical and religious dimensions of infectious disease prevention. She holds a Canadian Institute of Health Research Applied Public Health Chair on the Anthropology of Vaccination. Since 2014, she chairs the Social Science and Humanities Network of the Canadian Immunization Research Network. She sits on several Canadian (e.g., National Advisory Committee on Immunization, Canadian Association for Immunization Research and Evaluation) and international (e.g., World Health Organization's (WHO) Strategic and Technical Advisory Group on Infectious Hazards, WHO's Global Advisory Committee on Vaccine Safety) as an expert of vaccine acceptance.
Dr. Craig Earle
Craig Earle, MD MSc FRCP(C), is Chief Executive Officer of the Canadian Partnership Against Cancer, a medical oncologist at Sunnybrook Hospital in Toronto specializing in gastrointestinal cancers, a health services researcher and Senior Scientist at the Institute for Clinical Evaluative Sciences (ICES), and a Professor of Medicine at the University of Toronto. Dr. Earle originally trained and practiced in Ottawa, after which he spent 10 years — 1998 to 2008 — in Boston at Harvard Medical School, Dana-Farber Cancer Institute and the Harvard School of Public Health. From 2008 to 2017 he was Director of Health Services Research and Head of Clinical Translation at the Ontario Institute for Cancer Research.
Dr. Cordell (Cory) Neudorf
Dr Cordell Neudorf is a physician with 30 years of leadership experience in public health and a professor in the Department of Community Health and Epidemiology, College of Medicine, University of Saskatchewan. He is the former Senior Medical Health Officer roles with the Saskatchewan Health Authority and the Saskatoon Health Region. His past roles include: Chair of the Canadian Population Health Initiative Council (CIHI), President of the Canadian Public Health Association and President of the Public Health Physicians of Canada. He obtained his M.D. from the University of Saskatchewan, and his post graduate medical training in public health and preventive medicine from the University of Toronto. He obtained a master's degree (MH Sc) from U of T. He is a senior editor for the Canadian Journal of Public Health, President of the Urban Public Health Network of Canada and is a liaison member with the Regions for Health Network (WHO Europe). In 2020, he was awarded the R.D. Defries medal by the Canadian Public Health Association for outstanding contributions in the broad field of public health.
Ms. Maureen Smith
Ms. Smith is a patient/citizen partner who collaborates on national and global projects. She is strongly committed to both partnerships with citizens and patients depending on the context. Her interest as both a user of evidence and producer of evidence is rooted in her health care journey since childhood and desire to ensure that patient and public voices are embedded in health research and guidelines. She led the COVID-19 Evidence Network to support Decision-making (COVID-END) citizen engagement. Ms. Smith was a Commissioner on the Global Commission on Evidence to Address Societal Challenges and co-led the Citizen Leadership group of its Implementation Council. In 2024, she was appointed to the Board of Directors of Canada's Drug Agency as the inaugural Board member with lived experience. Ms. Smith is an Adjunct Professor at the University of Toronto Dalla Lana School of Public Health, a recognition of her patient engagement expertise over the past 25 years.
Appendix 4: Persons who submitted a written presentation
| Name | Organization |
|---|---|
| Elie Akl | American University of Beirut |
| Lisa Askie | The World Health Organization |
| Julian Elliott | McMaster University, Health Forum |
| Jeremy Grimshaw | The Ottawa Hospital Research Institute/Ottawa University |
| Doris Grinspun | Registered Nurses Association of Ontario |
| Alfonso Iorio | McMaster University, Health Forum |
| Gillian Leng | National Institute for Health and Care Excellence, England |
| Jennifer Petkovic | The Ottawa Centre for Health Equity, University of Ottawa |
| Rob Reid | Rapid Improvement and Support Exchange (RISE), Trillium Health Partners' Institute for Better Health, Canada |
| Donna Reynolds | Canadian Task Force on Preventive Health Care |
| Lena Salach | Centre for Effective Practice, University of Toronto, Canada |
| Sharon Straus | University of Toronto — Department of Medicine / Unity Health Toronto |
| Guylaine Thériault | Canadian Task Force on Preventive Health Care |
| Matthew Tunis | Public Health Agency of Canada |
| Ross Upshur | University of Toronto, Joint Centre for Bioethics, Dalla Lana School |
| Per Olav Vandvik | MAGIC Evidence Ecosystem Foundation, Norway |
| Sarah Viehbeck | Public Health Agency of Canada |
Appendix 5: Persons, interest holder organizations, government entities and academic institutions who provided inputFootnote 5
Persons
- Kimberly Anderson-hill
- Shiela Appavoo
- Monique A Bertrand
- Mylaine Breton
- Samuel Boudreault
- Carol Cancelliere
- Simon Coiteux
- Nicole Corrado
- James A. Dickinson
- Michel Donoff
- Andrea Douglas
- Maxine Dumas Pilon
- Duncan Etches
- Isabelle Gaboury
- Roland Grad
- Ilona Hale
- Jason Hamm
- Beth Hayhoe
- Fanny Hersson-edery
- Chloé Jamaty
- Ian Johnston
- Ümit Kiziltan
- Julie Laurence
- Michael May
- Adrienne Lindblad
- Samantha Moe
- Anthony Morham
- Kim Moshurchak
- Eli Newman
- Jessica Otte
- Nav Persaud
- Donna Reynolds
- Janet Reynolds
- Davin Shikaze
- Daniel Sin
- E. R. Snyman
- Jerrett Stephenson
- Marcello Tonelli
- Mark Tremblay
- Joan Tu
- Anna Wilkinson
- Martin J. Yaffe
Interest holder organizations, government entities, and academic institutions
- Alberta Health Services — Cancer Care
- Anxiety Disorders Association of Canada
- Association des médecins omnipraticiens de l'Outaouais
- Association of Specialists in Preventive Medicine of Quebec
- BC Cancer Provincial Health Services Authority
- Breast Cancer Canada (Kimberly Carson)
- British Columbia Centre for Disease Control
- Canadian Anesthesiologists' Society (CAS)
- Canadian Association of Cardiac Rehabilitation (CACPR)
- Canadian Association of Psychosocial Oncology (CAPO)
- Canadian Association of Radiologists
- Canadian Breast Cancer Network
- Canadian Cancer Society
- Canadian Chiropractic Association (Ayla Azad)
- Canadian Chiropractic Guideline Initiative
- Canadian Coalition for Seniors' Mental Health (CCSMH)
- Canadian Council of Motor Transport Administrators (CCMTA)
- Canadian Health Food Association (Sonia Parmar)
- Canadian Hereditary Angioedema Network
- Food Allergy Canada
- McGill University, Department of Family Medicine (Marion Dove)
- Manitoba Health
- Ordre professionnel de la physiothérapie du Québec.
- Canadian Labour Congress
- Canadian Nurses Association (Valerie GRDISA, Kimberly Leblanc)
- Canadian Partnership Against Cancer
- Canadian Pharmacists Association (CPhA) (Danielle Paes)
- Canadian Pharmacogenomics Network for Drug Safety (CPNDS)Canadian Psychiatric Association (CPA)
- Canadian Psychiatric Association (CPA)
- Canadian Society for Breast Imaging
- Canadian Urological Association
- Cancer Care Manitoba
- Centre for Effective Practice
- Centre for Immunization Surveillance and Programs (CISP-IDVPB)
- Choisir avec soin Québec (René Wittmer)
- Choosing Wisely Canada (Wendy Levinson)
- Collège des médecins du Québec
- College of Family Physicians of Canada (Michael Allan)
- College of Physicians and Surgeons of Ontario
- Committee to Advise on Tropical Medicine and Travel (CATMAT)
- Dense Breasts Canada (Jennie Dale)
- Fédération des médecins omnipraticiens du Québec
- Osteoporosis Canada
- Quebec College of Family Physicians
- Quebec's physiotherapy association
- Rethink Breast Cancer
- Society of Gynecologic Oncology of Canada (Sharon Salvador)
Appendix 6: Summary of interest holder submissions
What We Heard report: Help modernize the development of preventive health care guidelines in Canada
Background
On October 9, 2024, the Government of Canada announced the launch of an External Expert Review (EER) of the Canadian Task Force on Preventive Health Care (Task Force). The Panel — composed of 13 experts from various fields across the health sector — was mandated to assess the Task Force and propose improvements to its governance, mandate, and operations.
As part of its process, the Panel held a public consultation from November 21 to December 21, 2024, to gather input on how to modernize the development of preventive health care guidelines in Canada.
Who participated
The Panel received 74 written submissions from individuals and organizations across the country.
By region
The geographic distribution of submissions is shown in Figure A:

Figure A: Text description
Figure A shows the geographic distribution of submissions received from across Canada as part of a public consultation or feedback process. The data is organized by province or territory, and the number of submissions varies by region.
- Ontario had the highest number of submissions, with a total of 35, representing the largest share of participation.
- Quebec followed with 17 submissions, making it the second most represented province.
- Alberta contributed 12 submissions, also showing strong engagement.
- British Columbia submitted 7 responses, indicating moderate participation.
- Manitoba had 1 submission.
- No submissions were recorded from the other provinces or territories.
Most submissions came from Ontario, Quebec, and Alberta, with additional input from British Columbia and Manitoba.
By type of respondent
- 53% of submissions came from individuals, specifically:
- Family physicians (19)
- Medical specialists (5)
- Non-physician experts (6)
- Members of the public and private sector representatives (9)
- 47% came from organizations, specifically:
- Health professional associations (15)
- Non-governmental organizations (15)
- Academic institutions (1)
- Provincial and Territorial health authorities (2)
- Other organizations (2)
This consultation captured a wide range of perspectives from across disciplines and jurisdictions.
Consultation questions
Participants were asked to respond to three questions:
- Governance: Which practices should be maintained or what changes to the Canadian Task Force on Preventive Health Care (Task Force) governance or structure could further support transparency, accountability, independence, and leadership, towards scientifically rigorous, timely, agile, and inclusive guidelines?
- Mandate: Considering the broader preventive health care landscape, what should be the mandate of the Task Force of the future and how can it collaborate with other entities involved in guideline development nationally and internationally?
- Engagement: How can the Task Force strengthen interest holder engagement including subject-matter experts, equity-denied communities, and other groups to address health equity disparities and reflect Canadian diversity in guideline development and implementation?
What we heard
Feedback on the Task Force reflected various perspectives on its governance, mandate, and engagement efforts, with respondents highlighting both support and areas for improvement. Respondents proposed a series of changes that were classified as not very important, fairly important or very important. Many recognized that the Task Force achieves significant outcomes despite its limited resources and reliance on volunteer members, many of whom sacrifice clinical income to contribute to its work.
While challenges were noted, respondents also identified opportunities for improvement, with the majority advocating some level of change regarding the adoption of new approaches-as represented in Figure B

Figure B: Text description
Figure B presents feedback gathered during the public consultation on the Task Force, specifically focusing on participants' views regarding the importance of making changes in three areas: governance, mandate, and engagement.
Respondents were asked whether they believed changes in each area were very important, fairly important, not very important, or whether the status quo should be maintained. A no response option captures those who did not provide an answer for a given category.
Governance:
- 15% of respondents felt that changes to the Task Force's governance were very important.
- 23% said they were fairly important.
- 45% indicated change was not very important.
- 11% preferred maintaining the current governance structure (status quo).
- 7% did not respond.
Mandate:
- 0% of respondents said that changing the mandate was very important.
- 27% considered it fairly important.
- A majority (51%) said changes to the mandate were not very important.
- 8% supported maintaining the status quo.
- 14% did not respond.
Engagement:
- 9% viewed changes to the Task Force's engagement practices as very important.
- 26% considered them fairly important.
- 45% felt they were not very important.
- 5% preferred the status quo.
- 15% did not respond.
The remainder of this report summarizes the main ideas from the consultation organized by theme.
Key themes
1. Governance
The Task Force is generally well respected, but many believe there is room for improvement to its structure and to the way it is supported. Some suggested expanding its membership beyond physicians to include other health care professionals, patients, ethicists, and community representatives, ensuring a wider range of perspectives. Others stressed the importance of keeping family doctors at the core, given their key role in primary care and prevention.
Another concern was the Task Force's reliance on volunteers. Many felt this approach limits who can participate, especially for those without institutional funding, such as professionals outside academic settings. Offering compensation or other support could help attract a more diverse group and strengthen the Task Force's work.
Additionally, some respondents expressed concerns that the current decision-making structure may benefit from greater inclusion of medical specialists to enhance the diversity of perspectives in recommendations. A balanced approach that integrates both generalists and specialists while ensuring transparent conflict-of-interest management could enhance credibility and trust in the Task Force's recommendations.
Overall, many highlighted the need for greater transparency and accountability to maintain public trust in the Task Force's recommendations.
2. Mandate
The Task Force is recognized for the quality of its evidence-based recommendations on preventive care. Its work enjoys the support of many family doctors, but some respondents feel there is room for improvement to increase its impact and adaptability to the current realities of the health care system.
Some believe the Task Force should take a broader approach by considering how factors such as housing, income, and access to services can impact people's health. These elements play an essential role in the well-being of individuals, and directly influence the effectiveness of preventive care. Expanding its focus to promote health equity could help reduce disparities and better support higher-risk communities.
While the scientific rigour of the Task Force's methodology is acknowledged, some expressed concerns about the weight given to older studies in the assessment of evidence. To further improve the relevance of recommendations, many suggested broadening the evidence bases by integrating complementary sources, such as real-world data, observational studies and cost-effectiveness analyses.
Another challenge concerns the frequency with which recommendations are updated, with respondents urging more frequent updates. One proposed solution would be to adopt "living guidelines", which are updated continuously as new evidence emerges. In addition, strengthening collaboration with national and international health organizations would facilitate the updating of recommendations and ensure that guidelines remain aligned with global best practices, while meeting Canada's specific needs.
3. Engagement
Opinions differ as to how the Task Force interacts with other health care professionals in its ecosystem. Some appreciate its close involvement with family doctors. However, with the evolution of health care systems and the diversification of players involved in preventive care, others feel that it should also strengthen its links with other primary health care players. This broader collaboration would foster better integration of different areas of expertise and enable the development of recommendations that are more representative of the realities and challenges on the ground, while adapting to the changing needs of the health care system.
Many people suggested setting up advisory groups bringing together primary care health professionals, researchers, patients and members of the public, in order to integrate a wider range of viewpoints. Emphasis was placed on the need to increase the diversity of voices consulted and to adopt more inclusive decision-making processes. To improve communication, recommendations included the use of simple, accessible language, the dissemination of material in both official languages, and more proactive interaction with the public. Increased dialogue with medical specialists, Indigenous communities and equity deserving groups was deemed essential to developing relevant and inclusive guidelines.
To encourage more active participation, several approaches were suggested. Among them, the organization of structured consultations, such as focus groups, surveys and public comment periods to gather a wide range of perspectives. It was also suggested to offer onboarding to patient partners to support their engagement, and to take advantage of digital tools to reach people living in remote areas more effectively.
Setting up structured feedback mechanisms could ensure continuous improvement and better integration of the viewpoints of the different groups concerned. By adopting these measures, the Task Force would be able to formulate recommendations that are even better adapted to the needs and diversity of people living in Canada.
Conclusion
As the health care system evolves, and expectations of fairness, inclusiveness and scientific rigour increase, it is essential that the Task Force continue to adapt its methods and mandate. Strengthening the diversity of perspectives included in guideline development, regularly updating recommendations and fostering greater collaboration with interest holders will help ensure guidelines that are more representative and adapted to the needs of people living in Canada. By pursuing these improvements, the Task Force will be able to consolidate its role as a benchmark for preventive care and strengthen the confidence of the public and health care professionals.
The Panel values all the feedback that was received, as it provides important insights to help modernize the Task Force and improve guideline development.
Appendix 7: Comparison with international guideline development organizations
Appendix 7 provides an overview of how four countries — the United States, United Kingdom, Australia, and Canada — develop national preventive health guidelines. The comparison covers each organization's role, governance structure, methods for assessing evidence, and approaches to public and professional engagement.
United States — US Preventive Services Task Force (USPSTF)
What they do:
The USPSTF develops guidelines for primary prevention, including screening, counseling, and preventive medications. It published 13 guidelines between 2022 and 2023.
Governance:
The Task Force is an independent Panel supported by the Agency for Healthcare Research and Quality (AHRQ), part of the US Department of Health and Human Services. It includes 16 volunteer experts in prevention and evidence-based medicine. The group is federally funded and bases its decisions on systematic evidence review and expert consensus.
Methodology:
The USPSTF uses systematic reviews and a grading system similar to GRADE. Panels of clinical and public health experts review evidence and make recommendations. Cost-effectiveness is not considered.
Public engagement:
The USPSTF invites public comments at multiple stages, including on research plans and draft recommendations. Its methodology and drafts are freely accessible online.
United Kingdom — National Institute for Health and Care Excellence (NICE)
What they do:
NICE develops a broad range of guidelines, covering clinical care, public health interventions, and cost-effectiveness. It published 17 guidelines between 2022 and 2023.
Governance:
NICE operates independently under the UK Department of Health and Social Care. Its board includes 13 paid members, such as executives, healthcare professionals, and public representatives. Committee sizes vary based on the guideline topic. The institute is publicly funded by the UK government.
Methodology:
NICE assesses both clinical and cost-effectiveness. Committees include health economists, statisticians, patient representatives, and subject matter experts. Interest holders are actively consulted throughout the process.
Public engagement:
NICE holds public consultations, engages professionals and patients, and ensures full transparency by publishing reports, decision documents, and consultation summaries.
Australia — National Health and Medical Research Council (NHMRC)
What they do:
While NHMRC primarily funds health research, it also develops health and prevention guidelines. It published 11 guidelines between 2022 and 2023.
Governance:
NHMRC is a statutory authority under the Australian Government. Its council includes 19 appointed members from government and independent expert backgrounds. Committees vary in size depending on the topic. The Council is publicly funded, including through research grants.
Methodology:
NHMRC uses systematic reviews, often based on GRADE principles. Committees are multidisciplinary, involving economists, statisticians, patient representatives, and experts. Broad consultation is conducted with academic, clinical, and public stakeholders.
Public engagement:
NHMRC regularly consults with key interest holder groups and provides open access to research findings and guidelines.
Canada — Canadian Task Force on Preventive Health Care (CTFPHC)
What they do:
The CTFPHC develops preventive health guidelines tailored to the Canadian health care system. It published 2 guidelines between 2022 and 2023.
Governance:
The Task Force is an independent body reporting to the Public Health Agency of Canada (PHAC). It is composed of 15 volunteer experts in preventive health. Panel sizes vary depending on the guideline topic. The Task Force is funded by the Government of Canada through PHAC.
Methodology:
The Task Force uses systematic reviews guided by GRADE methodology. Its Panels include clinical, public health, and methodological experts. Like the US, it does not include cost-effectiveness in its recommendations.
Public engagement:
The Task Force consults with clinicians, researchers, and the public, and provides open access to its guidelines, evidence summaries, and methodology.
Conclusion
These four countries share a commitment to evidence-based preventive health guidance, but their approaches vary. By understanding these differences, Canada can learn from international leading practices to strengthen the transparency, relevance, and impact of its own preventive health guideline development process.
Appendix 8: Proposed organizational chart for the task force
Proposed organizational chart for the Task Force
The proposed structure outlines how the Task Force should be organized to improve transparency, equity, and accountability in developing preventive health care guidelines. The structure includes three levels with clear roles and responsibilities, as well as several advisory groups to ensure diverse perspectives are included.
Level 1: Federal oversight and core support
At the top level, the President of the Public Health Agency of Canada (PHAC) would provide federal oversight and accountability.
Supporting this level:
- A Standing Nomination Committee should advise on the selection of Task Force members. It should include people from key interest holder groups, such as equity-denied communities and primary care professionals.
- A Permanent PHAC Secretariat should provide administrative and scientific support. This should be a full-time team that manages coordination, communications, and evidence review to support the Task Force's work.
Level 2: Decision-making and equity advisory
At the core of the structure is the External Advisory Body (formerly the Task Force). This group should be responsible for making decisions and voting on preventive health guidelines.
Advisory groups at this level should include:
- An Equity Advisory Panel, to ensure that all work includes a strong equity lens. This Panel should include individuals with expertise in health equity, decolonization, anti-racism, and Indigenous knowledge systems.
- A Task Force-Public Advisors Network (TF-PAN), to bring a community-driven perspective. This network should include diverse members of the public, such as patients, caregivers, and community leaders from across Canada.
Level 3: Topic-specific working groups
The third level should include temporary (ad hoc) working groups focused on specific guideline topics. These groups:
- Should be chaired by a Task Force member.
- Should include experts with clinical knowledge and subject matter expertise.
- Would not have voting rights, but would provide technical input to inform recommendations.
Summary
This proposed structure is designed to:
- Ensure national oversight and transparency,
- Provide ongoing support through a dedicated secretariat,
- Strengthen equity and public involvement through specialized advisory panels, and
- Bring in expert input through working groups that inform evidence-based decisions.
References
- Akl, E. (2024). Key Principles and Best Practices for the Management of Conflicts of Interest [PowerPoint Presentation]. External Expert Review Meeting (EER),Canada.
- Akl, E. A., Khabsa, J., Petkovic, J., Magwood, O., Lytvyn, L., Motilall, A., Campbell, P., Todhunter‐Brown, A., Schünemann, H. J., Welch, V., Tugwell, P., & Concannon, T. W. (2024). "Interest‐holders": A new term to replace "stakeholders" in the context of health research and policy.
- Askie, L. (2024). WHO Normative Product Development: What Works, What Could we Still do Better? [PowerPoint Presentation]. External Expert Review Meeting (EER), Canada.
- Association of Faculties of Medicine of Canada. (2025). Chapter 4 Basic Concepts in Prevention and Health Promotion | AFMC Primer on Population Health.
- Canadian Institute for Health Information. (2025). Primary care | CIHI.
- Canadian Institutes of Health Research. (2022). Transforming Health with Integrated Care : Areas of Focus and Essential Elements - CIHR.
- Canadian Task Force on Preventive Health Care. (2023). Methods Manual.
- Chakraborty, S., Kuchenmüller, T., Lavis, J., El-Jardali, F., Mahlanza-Langer, L., Green, S., Reveiz, L., Carter, V., McFarlane, E., Pace, C., Askie, L., Glen, F., & Turner, T. (2024). Implications of living evidence syntheses in health policy. 102, 757.
- Dizon, J. M., Machingaidze, S., & Grimmer, K. (2016). To adopt, to adapt, or to contextualise? The big question in clinical practice guideline development. BMC Research Notes, 9(1).
- Elliott, J. H. (2024). Living Evidence: Accelerating Research to Use and Enabling Better Health Outcomes for All [PowerPoint Presentation]. External Expert Review Meeting (EER), Canada.
- Georgiades, K. (2021). Expanding the evidence for population mental health in canada: A call to action for evidence-informed policy and practice. Health Promot Chronic Dis Prev Can.
- Grimshaw, J. (2024). Presentation to the External Expert Review of the CTFPHC [PowerPoint Presentation]. External Expert Review Meeting (EER), Canada.
- Grinspun, D. (2024). BPSO Program and its Social Movement [PowerPoint Presentation]. External Expert Review Meeting (EER), Canada.
- Health Canada. (2012). ARCHIVED About primary health care - Canada.ca.
- Health Canada. (2023). Guidelines on public engagement 2023: Glossary of terms - Canada.ca.
- Health Canada. (2025a). Caring for Canadians: Canada's Future Health Workforce - The Canadian Health Workforce Education, Training and Distribution Study - Canada.ca.
- Health Canada. (2025b). Health workforce - Canada.ca.
- Interdepartmental Terminology Committee on Equity Diversity and Inclusion, G. o. C. (2022). Guide on Equity, Diversity and Inclusion Terminology.
- Interdepartmental Terminology Committee on Equity Diversity and Inclusion, G. o. C. (2024). Guide on Equity, Diversity and Inclusion Terminology.
- Iorio, A. (2024). Core GRADE [PowerPoint Presentation]. External Expert Review Meeting (EER), Canada.
- Lenartowicz, M. (2023). Overview of Preventive Care - Fundamentals - Merck Manual Consumer Version.
- Leng, G. (2024). Experience from the NICE guidelines programme [PowerPoint Presentation]. External Expert Review Meeting (EER), Canada.
- Nyantakyi, A. (2023). The Importance of Preventive Healthcare: Strategies for Better Health and Wellness. American Journal of Preventive Medicine and Public Health,.
- Oxford University Press. (2025). Lived experience - Oxford Reference.
- Petkovic, J. (2024). GIN-McMaster Guideline Development Checklist - Engagement Extension [PowerPoint Presentation]. External Expert Review Meeting (EER), Canada.
- Price, J. H., Khubchandani, J., McKinney, M., & Braun, R. (2013). Racial/Ethnic Disparities in Chronic Diseases of Youths and Access to Health Care in the United States. BioMed Research International, 2013, 787616.
- Public Health Agency of Canada. (2017). Glossary: Canadian Pandemic Influenza Preparedness: Planning Guidance for the Health Sector - Canada.ca.
- Public Health Agency of Canada. (2022a). Evaluation of Canadian Task Force on Preventive Health Care - Canada.ca.
- Public Health Agency of Canada. (2022b). Glossary of Terms - Canada.ca.
- Public Health Agency of Canada. (2022c). National Advisory Committee on Immunization (NACI): Terms of reference - Canada.ca.
- Public Health Agency of Canada. (2024). PHAC external advisory body policy. Public Health Agency of Canada.
- Reid, R. (2024). Learning Health System Action Framework [PowerPoint Presentation]. External Expert Review Meeting (EER), Canada.
- Sackett, D. L., Rosenberg, W. M. C., Gray, J. A. M., Haynes, R. B., Richardson, W. S., & (1996). Evidence based medicine: what it is and what it isn't. 312, 71-72.
- Salach, L. (2024). External Expert Review - Canadian Task Force on Preventive Health Care [PowerPoint Presentation]. External Expert Review Meeting (EER), Canada.
- SaskCulture. (2024). Definitions of Governance.
- SPOR Evidence Alliance. (2025). Asset Map of Canadian Clinical Practice Guidelines
- Straus, S. E. (2024). Optimising Guideline Development and Dissemination [PowerPoint Presentation]. External Expert Review Meeting (EER), Canada.
- The GRADE Working Group. (2025). GRADE home.
- Thériault, G., & Reynolds, D. (2024). The Canadian Task Force on Preventive Health Care [PowerPoint Presentation]. External Expert Review Meeting (EER), Canada.
- Tunis, M. (2024). NACI approach to interest holders [PowerPoint Presentation]. External Expert Review Meeting (EER), Canada.
- University of Texas Libraries. (2025). Glossary of Terms - Systematic Reviews & Evidence Synthesis Methods - LibGuides at University of Texas at Austin.
- Upshur, R. E. G. (2024). Ethics and Evidence [PowerPoint Presentation]. External Expert Review Meeting (EER), Canada.
- Vandvik, P. O. (2024). MAGICapp and Guidelines - Enhancing the Evidence Ecosystem in Canada [PowerPoint Presentation]. External Expert Review Meeting (EER), Canada.
- Venkateswaran, N., Feldman, J., Hawkins, S., Lewis, M. A., Armstrong-Brown, J., Comfort, M., Lowe, A., & Pineda, D. (2023). Bringing an Equity-Centered Framework to Research: Transforming the Researcher, Research Content, and Practice of Research
- Viehbeck, S. (2024). Administrative Mechanisms for Guidance Development at the Public Health Agency of Canada [PowerPoint Presentation]. External Expert Review Meeting (EER), Canada.
- World Health Organization. (2021). Health Promotion Glossary of Terms 2021.
- World Health Organization. (2025). Primary health care.