COVID-19 infections among healthcare workers and other people working in healthcare settings
Updated: March 4, 2022
On this page
Key findings
- Overall, 7% of COVID-19 cases are people working in healthcare settings (PWHS). This proportion has been declining since a peak in April 2020.
- Additional data is required to assess COVID-19 exposure among PWHS.
- PWHS with COVID-19 tend to be female and are younger than those with COVID-19 in the general population.
- PWHS with COVID-19 are less likely to be hospitalized or die than people with COVID-19 who do not work in healthcare settings, even after accounting for their younger age.
Overview
People working in healthcare settings (PWHS) are on the frontline of the COVID-19 pandemic and are a cornerstone of our healthcare capacity. They may face differential exposure to the SARS-CoV-2 virus and differential susceptibility to infection shaped by numerous factors including extended and close contact with COVID-19 cases, stressful work environments, long hours and fatigue, burnout, and in some instances, stigma and discriminationFootnote 1.
In addition, intersecting factors such as gender, race, ethnicity/culture, ability status, as well as other socioeconomic and demographic factors may put individuals at a greater risk of the many impacts of COVID-19, from illness and/or severe health outcomes to negative impacts arising from the public health measures put in place to mitigate transmission (e.g., economic-related).
It is important to understand the impact of the COVID-19 pandemic on PWHS given their critical role in response effortsFootnote 2. PWHS represent a wide range of individuals, including medical or healthcare professionals (for example, nurses, dentists, and pharmacists) and support workers (such as food service workers, housekeeping staff, and office administrators) (Data sources and limitations).
This report summarizes current information on COVID-19 infection among PWHS in Canada using the national COVID-19 surveillance system (Data sources and limitations). The report discusses the limitations of this data set (Data sources and limitations) and describes work being done to address the remaining data gaps (Addressing data gaps), to better understand the impact of COVID-19 on PWHS. The national COVID-19 surveillance system characterizes the clinical and epidemiologic features of COVID-19 and is not intended to specifically assess risk or exposures among PWHSFootnote 3. Additional strategies are in development to capture information specifically about COVID-19 among PWHS (Addressing data gaps), which can inform interventions for this important and diverse category of workers.
COVID-19 disease is caused by the SARS-CoV-2 virus. In this report, the term COVID-19 will be used to refer to both the virus and the disease.
7% percent of COVID-19 cases are PWHS, but their infections were not necessarily acquired in healthcare settings
In 2020, Statistics Canada estimated that health care and social assistance workers made up approximately 14% of the workforce, and approximately 7% of all CanadiansFootnote 4. As of September 30, 2021, there were 1,639,202 COVID-19 cases reported in Canada and 1,552,069 (95%) had occupation data available. Of these, 7% (n=111,268) considered themselves to be PWHS. As the COVID-19 surveillance system defines PWHS differently from Statistics Canada, we cannot comment on whether PWHS test positive for COVID-19 more or less often than the general Canadian population. PWHS may have more exposures to COVID-19 as frontline workers, they may also be more likely to seek testing given more knowledge of COVID-19, greater access to testing at worksites, and/or have workplace requirements for regular testing as part of infection prevention and control guidelines.
Proportion of all COVID-19 cases that are PWHS has changed over time
The proportion of reported COVID-19 cases that are PWHS has declined steadily since a peak in April 2020. From February, 2020 to June, 2020 the proportion of all cases occurring in PWHS was between 14% and 25%. After the April, 2020 peak, this proportion declined notably to 3% in June 2021, suggesting that more recently PWHS are less likely to contract COVID-19 (Table 1; Figure 1). It should be noted that PWHS have been identified as a priority group for COVID-19 vaccination and vaccination likely contributed to reduced infections among those workers. Proportions are based on cases for which occupation is known. Reporting on occupation declined between October, 2020 and May, 2021 and steadily increased from June, 2021 to September, 2021.
| Month | Cases in PWHS | Total COVID-19 cases | % of total cases |
|---|---|---|---|
| January 2020 | 3 | 43 | 7.0% |
| February 2020 | 31 | 217 | 14.3% |
| March 2020 | 2,865 | 18,092 | 15.8% |
| April 2020 | 11,554 | 45,891 | 25.2% |
| May 2020 | 6,536 | 30,225 | 21.6% |
| June 2020 | 1,520 | 10,788 | 14.1% |
| July 2020 | 1,146 | 12,337 | 9.3% |
| August 2020 | 1,119 | 13,136 | 8.5% |
| September 2020 | 3,051 | 39,736 | 7.7% |
| October 2020 | 6,861 | 77,861 | 8.8% |
| November 2020 | 12,267 | 147,494 | 8.3% |
| December 2020 | 17,881 | 207,230 | 8.6% |
| January 2021 | 13,940 | 161,513 | 8.6% |
| February 2021 | 4,497 | 79,859 | 5.6% |
| March 2021 | 4,699 | 124,689 | 3.8% |
| April 2021 | 7,583 | 233,752 | 3.2% |
| May 2021 | 4,352 | 127,536 | 3.4% |
| June 2021 | 749 | 25,283 | 3.0% |
| July 2021 | 711 | 16,412 | 4.3% |
| August 2021 | 3,967 | 72,838 | 5.4% |
| September 2021 | 5,936 | 107,137 | 5.5% |
| Data as of September 30, 2021. This table includes cases for whom occupation status is known. | |||
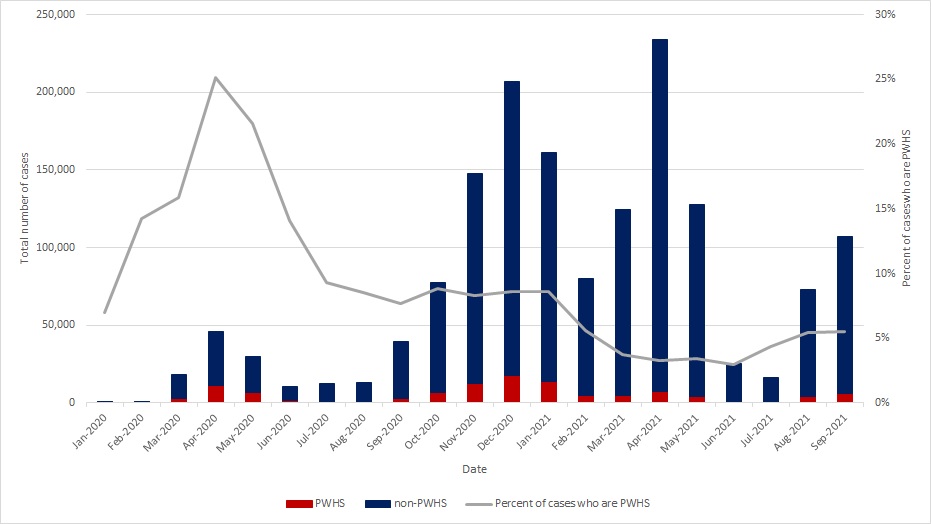
Data as of September 30, 2021.
Figure 1: Text description
| Month | PWHS | Non-PWHS | % of cases who are PWHS |
|---|---|---|---|
| January 2020 | 3 | 40 | 7.0% |
| February 2020 | 31 | 186 | 14.3% |
| March 2020 | 2,865 | 15,227 | 15.8% |
| April 2020 | 11,554 | 34,337 | 25.2% |
| May 2020 | 6,536 | 23,689 | 21.6% |
| June 2020 | 1,520 | 9,268 | 14.1% |
| July 2020 | 1,146 | 11,191 | 9.3% |
| August 2020 | 1,119 | 12,017 | 8.5% |
| September 2020 | 3,051 | 36,685 | 7.7% |
| October 2020 | 6,861 | 71,000 | 8.8% |
| November 2020 | 12,267 | 135,227 | 8.3% |
| December 2020 | 17,881 | 189,349 | 8.6% |
| January 2021 | 13,940 | 147,573 | 8.6% |
| February 2021 | 4,497 | 75,362 | 5.6% |
| March 2021 | 4,699 | 119,990 | 3.8% |
| April 2021 | 7,583 | 226,169 | 3.2% |
| May 2021 | 4,352 | 123,184 | 3.4% |
| June 2021 | 749 | 24,534 | 3.0% |
| July 2021 | 711 | 15,701 | 4.3% |
| August 2021 | 3,967 | 68,871 | 5.4% |
| September 2021 | 5,936 | 101,201 | 5.5% |
| Data as of September 30, 2021. | |||
Additional data are required to assess COVID-19 exposure for PWHS
Like all Canadians, PWHS may be exposed to COVID-19 through their interactions in the community, their homes, travel or work (Figure 2, Table 2). Given their role as frontline workers and increased likelihood of contact with a person with COVID-19, understanding occupational exposure for PWHS is important. We have exposure history for 70,645 (63%) of the 111,268 of the cases of COVID-19 who identified as PWHS. Of these:
- 62% reported exposure in Canada to a known COVID-19 case;
- 36% reported exposure in Canada to an unknown source;
- 2% reported exposure to someone who had travelled; and
- 1% reported having travelled outside of Canada during the exposure period.
For those reporting exposure in Canada to a known COVID-19 case, it is not possible to determine whether PWHS became infected at work or elsewhere (Data sources and limitations).

Data as of September 30, 2021.
Figure 2: Text description
| Week | Domestic acquisition: contact of covid case | Domestic acquisition: contact with traveler | Domestic acquisition: unknown source | Information pending | International travel |
|---|---|---|---|---|---|
| 2020-01-16 to 2020-01-22 | 0 | 0 | 0 | 2 | 0 |
| 2020-01-23 to 2020-01-29 | 0 | 0 | 0 | 1 | 0 |
| 2020-01-30 to 2020-02-05 | 0 | 0 | 0 | 0 | 1 |
| 2020-02-06 to 2020-02-12 | 1 | 0 | 1 | 0 | 0 |
| 2020-02-13 to 2020-02-19 | 0 | 0 | 0 | 0 | 1 |
| 2020-02-20 to 2020-02-26 | 7 | 0 | 2 | 1 | 2 |
| 2020-02-27 to 2020-03-04 | 14 | 0 | 19 | 0 | 13 |
| 2020-03-05 to 2020-03-11 | 43 | 2 | 72 | 0 | 51 |
| 2020-03-12 to 2020-03-18 | 223 | 8 | 205 | 8 | 146 |
| 2020-03-19 to 2020-03-25 | 453 | 19 | 310 | 10 | 114 |
| 2020-03-26 to 2020-04-01 | 908 | 11 | 425 | 16 | 86 |
| 2020-04-02 to 2020-04-08 | 1718 | 8 | 560 | 6 | 37 |
| 2020-04-09 to 2020-04-15 | 2115 | 11 | 806 | 17 | 7 |
| 2020-04-16 to 2020-04-22 | 2004 | 15 | 840 | 15 | 4 |
| 2020-04-23 to 2020-04-29 | 1827 | 13 | 877 | 21 | 5 |
| 2020-04-30 to 2020-05-06 | 1483 | 8 | 736 | 13 | 1 |
| 2020-05-07 to 2020-05-13 | 1181 | 8 | 555 | 12 | 3 |
| 2020-05-14 to 2020-05-20 | 982 | 3 | 539 | 6 | 2 |
| 2020-05-21 to 2020-05-27 | 705 | 1 | 307 | 2 | 3 |
| 2020-05-28 to 2020-06-03 | 411 | 2 | 177 | 7 | 0 |
| 2020-06-04 to 2020-06-10 | 302 | 5 | 119 | 1 | 2 |
| 2020-06-11 to 2020-06-17 | 259 | 0 | 118 | 5 | 2 |
| 2020-06-18 to 2020-06-24 | 186 | 0 | 87 | 3 | 0 |
| 2020-06-25 to 2020-07-01 | 132 | 1 | 77 | 2 | 1 |
| 2020-07-02 to 2020-07-08 | 143 | 2 | 80 | 3 | 2 |
| 2020-07-09 to 2020-07-15 | 205 | 5 | 92 | 16 | 2 |
| 2020-07-16 to 2020-07-22 | 103 | 3 | 96 | 15 | 2 |
| 2020-07-23 to 2020-07-29 | 97 | 2 | 68 | 117 | 1 |
| 2020-07-30 to 2020-08-05 | 87 | 5 | 50 | 103 | 2 |
| 2020-08-06 to 2020-08-12 | 93 | 5 | 63 | 59 | 0 |
| 2020-08-13 to 2020-08-19 | 110 | 6 | 71 | 63 | 0 |
| 2020-08-20 to 2020-08-26 | 110 | 7 | 69 | 66 | 0 |
| 2020-08-27 to 2020-09-02 | 125 | 6 | 70 | 113 | 1 |
| 2020-09-03 to 2020-09-09 | 108 | 4 | 83 | 193 | 3 |
| 2020-09-10 to 2020-09-16 | 172 | 4 | 133 | 266 | 1 |
| 2020-09-17 to 2020-09-23 | 238 | 17 | 129 | 492 | 2 |
| 2020-09-24 to 2020-09-30 | 250 | 13 | 162 | 674 | 2 |
| 2020-10-01 to 2020-10-07 | 295 | 17 | 207 | 646 | 0 |
| 2020-10-08 to 2020-10-14 | 309 | 9 | 218 | 781 | 1 |
| 2020-10-15 to 2020-10-21 | 415 | 16 | 239 | 898 | 2 |
| 2020-10-22 to 2020-10-28 | 617 | 21 | 303 | 968 | 2 |
| 2020-10-29 to 2020-11-04 | 795 | 42 | 355 | 1182 | 3 |
| 2020-11-05 to 2020-11-11 | 790 | 35 | 419 | 1316 | 2 |
| 2020-11-12 to 2020-11-18 | 853 | 38 | 533 | 1271 | 1 |
| 2020-11-19 to 2020-11-25 | 1040 | 44 | 541 | 1412 | 3 |
| 2020-11-26 to 2020-12-02 | 1171 | 72 | 577 | 1765 | 5 |
| 2020-12-03 to 2020-12-09 | 1225 | 67 | 579 | 1966 | 6 |
| 2020-12-10 to 2020-12-16 | 1122 | 96 | 538 | 2148 | 8 |
| 2020-12-17 to 2020-12-23 | 1133 | 117 | 513 | 2415 | 4 |
| 2020-12-24 to 2020-12-30 | 1206 | 89 | 540 | 2371 | 8 |
| 2020-12-31 to 2021-01-06 | 1252 | 91 | 546 | 2434 | 12 |
| 2021-01-07 to 2021-01-13 | 1025 | 67 | 491 | 2253 | 12 |
| 2021-01-14 to 2021-01-20 | 821 | 55 | 372 | 1760 | 8 |
| 2021-01-21 to 2021-01-27 | 637 | 35 | 307 | 1329 | 4 |
| 2021-01-28 to 2021-02-03 | 469 | 28 | 227 | 973 | 4 |
| 2021-02-04 to 2021-02-10 | 387 | 21 | 173 | 643 | 3 |
| 2021-02-11 to 2021-02-17 | 338 | 14 | 159 | 503 | 2 |
| 2021-02-18 to 2021-02-24 | 356 | 12 | 202 | 489 | 0 |
| 2021-02-25 to 2021-03-03 | 345 | 9 | 166 | 411 | 3 |
| 2021-03-04 to 2021-03-10 | 338 | 7 | 180 | 366 | 4 |
| 2021-03-11 to 2021-03-17 | 383 | 6 | 179 | 367 | 6 |
| 2021-03-18 to 2021-03-24 | 425 | 12 | 240 | 426 | 1 |
| 2021-03-25 to 2021-03-31 | 529 | 5 | 241 | 519 | 0 |
| 2021-04-01 to 2021-04-07 | 707 | 16 | 360 | 656 | 5 |
| 2021-04-08 to 2021-04-14 | 792 | 10 | 408 | 691 | 3 |
| 2021-04-15 to 2021-04-21 | 736 | 9 | 381 | 519 | 5 |
| 2021-04-22 to 2021-04-28 | 800 | 8 | 393 | 547 | 2 |
| 2021-04-29 to 2021-05-05 | 728 | 5 | 402 | 468 | 2 |
| 2021-05-06 to 2021-05-12 | 616 | 7 | 308 | 367 | 0 |
| 2021-05-13 to 2021-05-19 | 437 | 7 | 229 | 277 | 3 |
| 2021-05-20 to 2021-05-26 | 286 | 1 | 156 | 182 | 0 |
| 2021-05-27 to 2021-06-02 | 197 | 2 | 93 | 142 | 0 |
| 2021-06-03 to 2021-06-09 | 102 | 1 | 66 | 83 | 1 |
| 2021-06-10 to 2021-06-16 | 75 | 2 | 35 | 68 | 5 |
| 2021-06-17 to 2021-06-23 | 43 | 0 | 21 | 48 | 0 |
| 2021-06-24 to 2021-06-30 | 35 | 0 | 17 | 31 | 3 |
| 2021-07-01 to 2021-07-07 | 34 | 1 | 32 | 47 | 1 |
| 2021-07-08 to 2021-07-14 | 24 | 1 | 25 | 31 | 2 |
| 2021-07-15 to 2021-07-21 | 48 | 3 | 52 | 44 | 2 |
| 2021-07-22 to 2021-07-28 | 81 | 8 | 85 | 62 | 4 |
| 2021-07-29 to 2021-08-04 | 168 | 10 | 164 | 105 | 7 |
| 2021-08-05 to 2021-08-11 | 195 | 18 | 212 | 157 | 3 |
| 2021-08-12 to 2021-08-18 | 297 | 14 | 297 | 220 | 5 |
| 2021-08-19 to 2021-08-25 | 311 | 6 | 483 | 251 | 7 |
| 2021-08-26 to 2021-09-01 | 223 | 4 | 604 | 262 | 4 |
| 2021-09-02 to 2021-09-08 | 298 | 4 | 780 | 336 | 7 |
| 2021-09-09 to 2021-09-15 | 335 | 2 | 813 | 345 | 4 |
| 2021-09-16 to 2021-09-22 | 310 | 2 | 693 | 346 | 1 |
| 2021-09-23 to 2021-09-29 | 346 | 3 | 651 | 270 | 5 |
| Data as of September 30, 2021. | |||||
Please note that exposure history is not available for all cases and jurisdictions have not all consistently reported exposure history to PHAC throughout the pandemic.
| Month of onset | Domestic acquisition: unknown source | Domestic acquisition: contact of COVID-19 case | International travel | Domestic acquisition: contact with traveller |
|---|---|---|---|---|
| January-February 2020 | 9 | 15 | 6 | - |
| March 2020 | 961 | 1,443 | 393 | 36 |
| April 2020 | 3,270 | 8,097 | 70 | 53 |
| May 2020 | 2,121 | 4,354 | 9 | 19 |
| June 2020 | 461 | 1,032 | 4 | 7 |
| July 2020 | 361 | 584 | 8 | 13 |
| August 2020 | 288 | 462 | 3 | 27 |
| September 2020 | 528 | 811 | 8 | 41 |
| October 2020 | 1,107 | 1,926 | 6 | 78 |
| November 2020 | 2,133 | 3,995 | 14 | 199 |
| December 2020 | 2,405 | 5,241 | 28 | 396 |
| January 2021 | 1,778 | 3,835 | 37 | 257 |
| February 2021 | 723 | 1,460 | 8 | 65 |
| March 2021 | 920 | 1,848 | 12 | 36 |
| April 2021 | 1,668 | 3,293 | 17 | 44 |
| May 2021 | 1,059 | 2,011 | 3 | 21 |
| June 2021 | 161 | 306 | 9 | 3 |
| July 2021 | 236 | 241 | 11 | 16 |
| August 2021 | 1,751 | 1,162 | 25 | 51 |
| September 2021 | 3,140 | 1,385 | 18 | 13 |
| Total | 25,080 | 43,501 | 689 | 1,375 |
| Data as of September 30, 2021. | ||||
COVID-19 cases in PWHS with missing exposure information were excluded. Please note that exposure history is not available for all cases and jurisdictions have not all consistently reported exposure history to PHAC throughout the pandemic.
Although exposure data is incomplete, other available evidence suggests that workplace-related exposure is an important source of COVID-19 in PWHSFootnote 5. However, not all PWHS contracted their illnesses at or from work. There is evidence from other reported outbreaks that some PWHS may be acquiring their infection from contact with known cases outside of their workplace (e.g. social gatherings, household member with confirmed COVID-19)Footnote 5Footnote 6. Surveys of PWHS would allow for better assessment of the relative contribution of occupational exposure to overall transmission risk and whether the risk for acquisition of COVID-19 is different for different types of PWHS.
PWHS with COVID-19 tend to be female and are mostly of working age
On average, COVID-19 cases who are PWHS are younger compared with non-PWHS. While most COVID-19 cases in PWHS are between the ages of 20 and 59, non-PWHS are more distributed across all age groups (Figure 3). Of the COVID-19 cases who are PWHS for whom sex information is known, 79% are female. This is expected and reflects the healthcare workforce composition where a large proportion of individuals are female (80%)Footnote 7. Similarly, most of the PWHS with COVID-19 were of working age with 97% between the ages of 20-69, in comparison to 69% of non-PWHS. Work is underway through the updated COVID-19 national surveillance system to obtain more information about PWHS with COVID-19, including their specific occupations, race/ethnicity, and gender identity. To date, the level of completeness of these new fields added to the national case report form on February 15, 2021, does not allow for analysis.

Data as of September 30, 2021.
| Age group (years) | People working in healthcare settings | People not working in healthcare settings |
|---|---|---|
0 to 19 |
2,180 (2%) |
309,606 (21%) |
20 to 29 |
24,174 (22%) |
276,727 (19%) |
30 to 39 |
27,846 (25%) |
231,691 (16%) |
40 to 49 |
27,175 (24%) |
198,709 (14%) |
50 to 59 |
21,631 (19%) |
174,382 (12%) |
60 to 69 |
7,572 (7%) |
113,595 (8%) |
70 to 79 |
626 (1%) |
62,729 (4%) |
80 or plus |
52 (0%) |
72,881 (5%) |
| Data as of September 30, 2021. This table includes cases for whom occupation status is known. | ||
Since PWHS are by definition in the workforce, it is more relevant to restrict the comparison of age distributions to age groups most likely to be in the workforce. When the youngest and oldest age groups are removed, the age distribution of PWHS and non-PWHS are much more similar, with a higher percentage of case in PWHS among individuals aged 20 to 59 years of age (Table 4, Figure 4).
| Age group (years) | People working in healthcare settings | People not working in healthcare settings |
|---|---|---|
20 to 29 |
24,174 (22%) |
276,727 (28%) |
30 to 39 |
27,846 (26%) |
231,691 (23%) |
40 to 49 |
27,175 (25%) |
198,709 (20%) |
50 to 59 |
21,631 (20%) |
174,382 (18%) |
60 to 69 |
7,572 (7%) |
113,595 (11%) |
| Data as of September 30, 2021. This table includes cases for whom occupation status is known. | ||

Data as of September 30, 2021.
PWHS have been affected by COVID-19 in most jurisdictions
There are currently twelve jurisdictions providing information about PWHS status to PHAC as part of the national COVID-19 dataset. Although PWHS have been affected in all reporting provinces and territories, the majority of PWHS with COVID-19 have been reported in Alberta, Ontario and Quebec. These three provinces have also reported the highest number of cases overall.
Outbreaks have been an important driver of COVID-19 transmission. Based on outbreak surveillance data and publicly reported information, at least 2,435 outbreaks in long-term care facilities, retirement residences, acute care settings, or community healthcare settings were reported between January 2021 and September 2021, where PWHS may have contracted COVID-19. The number of outbreaks reported in health care settings declined between January and September 2021. Information in these settings does not distinguish between the role of the cases (PWHS, patients, residents, etc.). PWHS and residents of long-term care facilities and retirement residences were identified as priority groups for COVID-19 vaccination. By the end of September 2021, over 85% of Canadians aged 12 years and over had received at least one dose of COVID-19 vaccine and over 80% were fully vaccinatedFootnote 8. Vaccination likely contributed to reduced number and/or size of outbreaks in healthcare settings.
PWHS are less likely to experience severe outcomes, even when adjusting for their younger age
Hospitalized COVID-19 cases in Canada tend to be older than non-hospitalized casesFootnote 9, with men reporting more severe symptoms and requiring hospitalization more often than womenFootnote 10. When all age groups are considered, 4.5% of non-PWHS cases have been hospitalized, compared to only 1.6% of PWHS (Table 5). Although fewer PWHS are hospitalized, similar proportions of those hospitalized require admission to the ICU (27.2%) compared with non-PWHS COVID-19 patients (25.1%) for all ages. The proportion of non-PWHS cases that died was about 33 times higher than PWHS. Since PWHS with COVID-19 infection tend to be younger individuals, this may help explain why they require less hospitalization than non-PWHS.
| Outcome | People working in healthcare settings | People not working in healthcare settings |
|---|---|---|
| Hospitalized | 1.6% (n=1,734/111,268) | 4.5% (n=39,563/875,936) |
| Admitted to ICU among those hospitalized | 27.2% (n=471/1,734) | 25.1% (n=9,923/39,563) |
| Deaths among all cases | 0.06% (n=63/111,268) | 2.0% (n=17,437/875,936) |
| Data as of September 30, 2021.This table includes cases for whom occupation status is known. | ||
When the populations under comparison are restricted to those between 20 and 69 years of age, the proportion that is hospitalized among PWHS is half that among non-PWHS (1.5% in PWHS vs. 3.3% in non-PWHS). Once hospitalized, the proportions admitted to ICU are similar (27.1% in PWHS vs. 34.2% in non-PWHS) (Table 6). While the proportion of cases that die in non-PWHS is still eight times higher than in PWHS (0.42% vs. 0.05%), this difference is far less than in the unadjusted population.
| Outcome | People working in healthcare settings | People not working in healthcare settings |
|---|---|---|
| Hospitalized | 1.5% (n=1,659/108 398) | 3.3% (n=19,104/580,511) |
| Admitted to ICU among those hospitalized | 27.1% (n=449/1,659) | 34.2% (n=6,532/19,104) |
| Deaths among all cases | 0.05% (n=57/108,398) | 0.4% (n=2,413/580,511) |
| Data as of September 30, 2021. This table includes cases for whom occupation status is known. | ||
It is uncommon for PWHS to die from COVID-19. Less than 1% of PWHS with COVID-19 have died after contracting COVID-19 and PWHS represent less than 0.2% (63/28,491) of all reported COVID-19 deaths in Canada as of September 30, 2021.
There are currently no surveillance data available on other severe consequences of COVID-19 infection, such as lung or other organ damage. Case surveillance may not be the mechanism best suited to exploring long-term effects of COVID, including risk of long-term health problems such as post COVID-19 condition. Research should be undertaken to assess the overall impact of this new disease, and its impact on PWHS in particular.
Case surveillance data is limited in the amount of detail it can provide about COVID-19 in PWHS. Strategies to capture information about COVID-19 among PWHS are in development (Addressing data gaps) and will be able to inform interventions for this important category of worker.
Data sources and limitations
The Public Health Agency of Canada (PHAC) receives data for cases reported by provinces and territories (P/Ts) through case report forms (PDF). PWHS were identified as those who responded “Yes” to the case report form question: “Is the case currently a healthcare worker?”
The national COVID-19 surveillance system was developed to characterize the clinical and epidemiologic features of COVID-19 to better inform prevention and control efforts. It was not intended to specifically collect information about exposures among PWHS.
PWHS may have acquired COVID-19 travelling outside Canada, in the community, in their homes, or in the workplace.
- It is difficult to ascertain where and how PWHS with COVID-19 were exposed because:
- limited or no information on the exposure setting is collected;
- PWHS could be exposed in multiple settings such as to patients, to other PWHS, or within the community;
- no information is collected on whether PWHS wore personal protective equipment (PPE) upon exposure;
- some PWHS also reported travel and/or contact with cases in the community.
- Current workplace/healthcare exposure information has not been provided.
P/Ts collect and report on occupation with varying degrees of completeness:
- information on PWHS status relied on self-identification;
- definition of PWHS may vary by P/Ts and may include individuals with or without direct patient contact;
- not all P/Ts systematically collect data on occupation;
- reporting on occupation has varied over time.
PWHS include a wide range of roles and healthcare settings. Roles can include:
- medical or healthcare professionals (physician, nurses, dentists, pharmacists, physiotherapists, etc.);
- support workers (aides, residential home workers, food service workers, cleaners/janitorial, office administrators, volunteers, etc.); and
- current, previous, and retired PWHS.
Setting can include acute care facilities, long-term care facilities, community health care setting (e.g., clinics) and home care.
Lack of a standard surveillance definition means variability in roles and settings reported by P/Ts.
Addressing data gaps
Several strategies under development will strengthen data on COVID-19 in people working in healthcare settings:
- In the fall of 2020, the National COVID-19 case dataset was revised to fill critical data gaps, including more precision on data from healthcare worker (role, setting, direct patient care) and other occupations. There remains variation in how data are captured and reported across the country and PHAC continues to work collaboratively with provincial and territorial public health authorities to improve data completeness. The revised National COVID-19 case dataset allows for:
- more detailed and standardized information on PWHS’ likely source(s) of exposure and acquisition and on asymptomatic status to better understand where and how transmission and exposures are occurring;
- standardization and finer categorization of PWHS roles in order to understand differences in risk by occupation and sector, and to allow for comparison of cases working in other settings; and
- defined exposure settings to allow better assessment of occupational vs. other types of exposures (e.g. travel, close contact with a case).
- Improving surveys and use of data on health and social inequities of COVID-19 among PWHS to inform the decision-making will help us:
- assess the impact of COVID-19 and associated workplace changes on the general health and well-being of people working in healthcare settings;
- understand the experience of PWHS with respect to Personal Protective Equipment and Infection Control Practices in their worksites, the organizational supports made available to them and their perceived level of risk for contracting COVID-19;
- provide more detail on intersectional issues, such as the role of race and ethnicity in relation to the health workforce and level of risk; and
- facilitate policy and decision making within specific health care settings.
- Performing genetic sequencing concurrent with epidemiological data will:
- facilitate contact tracing and outbreak control within PWHS settings;
- inform whether or not PWHS shared a common exposure setting; and
- estimate the true number of people with COVID-19 to assess the impact and burden of COVID-19 on PWHS.
Endnotes
- Endnote a
-
The earliest of the following dates was used to define the week: onset date, laboratory specimen collection date, laboratory testing date, date reported to province or territory, or date reported to PHAC.
- Footnote b
-
Cases with missing age information were excluded.
- Footnote c
-
Cases with missing age information or under 20 years or over 70 years of age were excluded.
References
- Footnote 1
-
Kisely S, Warren N, McMahon L, Dalais C, Henry I, Siskind D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ. 2020 May 5;369:m1642. doi: 10.1136/bmj.m1642. PMID: 32371466; PMCID: PMC7199468.
- Footnote 2
-
World Health Organization. Mar 2020. Coronavirus disease (COVID-19) outbreak: rights, roles and responsibilities of health workers, including key considerations for occupational safety and health.
- Footnote 3
-
Government of Canada. Interim national surveillance guidelines for human infection with Coronavirus disease (COVID-19), February 10, 2020. Available at https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/health-professionals/interim-guidance-surveillance-human-infection.html.
- Footnote 4
-
Statistics Canada. Table 14-10-0023-01 Labour force characteristics by industry, annual (x 1,000).
- Footnote 5
-
Chou R, Dana T, Buckley DI, Selph S, Fu R, Totten AM. Update Alert 3: Epidemiology of and Risk Factors for Coronavirus Infection in Health Care Workers. Ann Intern Med. 2020 Sep 15;173(6):W123-W124. doi: 10.7326/L20-1005. Epub 2020 Aug 3. PMID: 32744870; PMCID: PMC7418491.
- Footnote 6
-
Akinbami, L. J., Vuong, N., Petersen, L. R., Sami, S., Patel, A., Lukacs, S. L., and Atas, J. (2020). SARS-CoV-2 seroprevalence among healthcare, first response, and public safety personnel, Detroit metropolitan area, Michigan, USA, May–June 2020. Emerging infectious diseases, 26(12), 2863.
- Footnote 7
-
Statistics Canada. Labour Force Survey, 2019. Table 14-10-0027-01 Employment by class of worker, annual (x 1,000). Available at https://doi.org/10.25318/1410002701-eng.
- Footnote 8
-
Public Health Agency of Canada. COVID-19 vaccination in Canada. Available at https://health-infobase.canada.ca/covid-19/vaccination-coverage/.
- Footnote 9
-
Government of Canada. COVID-19 daily epidemiology update. Available at https://health-infobase.canada.ca/covid-19/epidemiological-summary-covid-19-cases.html#a7.
- Footnote 10
-
Maleki Dana P, Sadoughi F, Hallajzadeh J, Asemi Z, Mansournia MA, Yousefi B, Momen-Heravi M. An Insight into the Sex Differences in COVID-19 Patients: What are the Possible Causes? Prehosp Disaster Med. 2020 Aug;35(4):438-441. doi: 10.1017/S1049023X20000837. Epub 2020 Jun 18. PMID: 32600476; PMCID: PMC7327162.